Flying while pregnant? Here’s what you need to know

Editors note: This guide has been updated with the latest information.
During pregnancy, seemingly harmless things like eating deli meat and cleaning your cat's litter box are suddenly off-limits, along with more obvious restrictions on sports like skiing and scuba diving.
But what about "grey area" activities like flying in an airplane?
There's no single set of guidelines governing air travel during pregnancy and every airline has different restrictions, timelines and requirements. Some airlines may also require a medical certificate from a primary attending doctor or midwife for air travel during the final months of pregnancy, though even that varies, with U.S. airlines typically offering more flexibility than international carriers.
For more TPG news delivered each morning to your inbox, sign up for our daily newsletter .
In the absence of clear guidelines, TPG turned to Dr. Nithya Gopal , a board-certified OB-GYN physician and the Director of OB-GYN services at Viva Eve in New York City, for her expert recommendations on safe air travel during pregnancy.
Here's what she had to say:

Is it safe to fly when you are pregnant?
There is no evidence of adverse pregnancy outcomes due to flying, according to Dr. Gopal.
"The general consensus is that it is safest to fly in the first and second trimesters," Dr. Gopal told The Points Guy. "While the first and third trimesters tend to be when the most obstetric emergencies are going to happen, I personally become more cautious with my patients after 32 weeks because of the increased risk for premature labor and the possibility of needing urgent medical attention when you are in the sky."

The most important thing you can do, no matter how far along you are in your pregnancy, is to consult with your healthcare provider before flying.
"Any time you are planning to fly during pregnancy , you should be having that conversation," Dr. Gopal said. Your provider will be familiar with any safety precautions you should take to ensure a safe and healthy flight.
Related: Guide to flying in each trimester of pregnancy
The airline you are flying may have its own cutoff, so you will want to confirm with it beforehand whether you will be allowed to fly if you are in (or nearing) your third trimester. We've included a chart below that outlines the rules for most major airline carriers.
What can you do to stay comfortable on a flight?

When you factor in morning sickness and general pregnancy discomfort with the increased risk for blood clots that all fliers need to be aware of, flying during pregnancy can be uncomfortable even when it is deemed safe.
Dr. Gopal shared her recommendations for addressing these common issues when you take to the (baby-) friendly skies during pregnancy. Her number one tip for staying comfortable while in flight is to wear compression socks to help maintain blood flow and reduce swelling in the legs.
In addition, "I also tell my patients to get up and move at least every hour when they are on the plane," Dr. Gopal said.
To prevent clotting, "some doctors may also prescribe a low-dose aspirin," she added. "It isn't something that is recommended by the American College of Obstetricians and Gynecologists (ACOG), but it isn't harmful, either."
If it's nausea or acid reflux that ail you, there are medications generally considered safe that you can take to alleviate your symptoms. These would be the same ones prescribed by your doctor for morning sickness, so speak with your provider before your flight to ensure you have what you need at the ready.
Dr. Gopal also advises wearing loose, unrestrictive clothing (along with your seatbelt, or course) and drinking extra fluids to counteract the pressurized air in the cabin and keep you hydrated.
"Over-the-counter Gas-X may also help with bloating that can happen as a result of the pressurized air," Dr. Gopal said.
Related: What happens when a baby is born in flight?
Must you speak with your healthcare provider before flying?

Even if your pregnancy is considered low-risk, it's always a smart idea to speak with your healthcare provider before flying. "There are a number of potential risks that go along with flying during pregnancy and those risks can change from week to week and month to month, so it's important to have that honest conversation with your doctor," Dr. Gopal said.
Related: Things You Should Do Before, During and After Flying to Stay Healthy
There are certain pregnancy conditions that may make flying more risky or unadvisable. If you are hypertensive, asthmatic or prone to clotting disorders, it's even more critical to speak with your doctor before flying.
Airline policies differ, but if you need documentation, it never hurts to include enough detail to satisfy the most stringent airline requirements.
"As with many things related to air travel, it's better to be safe than sorry," Dr. Gopal said. "It's definitely worth it, and sometimes necessary, to have medical documentation from your provider's office."
A thorough medical certificate or waiver should state:
- The number of weeks of pregnancy.
- The estimated delivery date.
- Whether the pregnancy is single or multiple.
- Whether there are any complications.
- That you are in good health and fit to travel through the date of your final flight.
Additionally, the certificate should be:
- Written on official clinic or hospital letterhead if possible.
- Signed by the doctor or attending midwife.
- Be dated no later than 72 hours before the departure date.
- Be written in clear, simple English.
Carry this certificate with you on your flight. Some airlines won't ask to see it, but others will. Some airlines also may have their own documentation requirements. See the chart below to find out which airlines require it.
Airline policies for pregnant women
Bottom line.

Even though it may be deemed safe, flying during pregnancy can be uncomfortable — and it is perfectly acceptable to implement your own cutoff for flying with your baby bump in tow. The majority of the time, though, flying is perfectly safe during pregnancy, providing that you follow the guidelines of the airline and your healthcare provider. Read on to learn more about traveling before, during and after pregnancy:
- What to expect in every trimester of pregnancy
- 4 tips for planning travel while planning a pregnancy
- Babymoon boom! These are the top 10 spots for a US getaway before the baby comes
- Flying with a baby checklist
Additional reporting by Katherine Fan and Tarah Chieffi.
Appointments at Mayo Clinic
- Pregnancy week by week
Is it safe to fly during pregnancy?
Generally, air travel before 36 weeks of pregnancy is considered safe for people who aren't dealing with any pregnancy problems. Still, if you're pregnant, it's a good idea to talk with your health care provider before you fly.
Your provider might suggest that you not fly if you have certain pregnancy complications that could get worse because of air travel or that could require emergency care. Examples include a history of miscarriage or vaginal bleeding, severe anemia, and high blood pressure or diabetes that's not well controlled. If you had preeclampsia during a previous pregnancy — a condition that causes high blood pressure and extra protein in urine — flying may not be advised. The same is true if you're pregnant with twins or other multiples.
Tell your provider how far you are flying, as the length of the flight might make a difference. Also, be aware that some airlines may not allow pregnant people on international flights. Check with your airline before you make travel arrangements.
After 36 weeks of pregnancy, your health care provider may advise against flying. And some airlines don't allow pregnant people to fly after 36 weeks. The airline also may require a letter from your health care provider that states how far along in your pregnancy you are and whether flying is advised.
If your health care provider says it's okay for you to fly, and your plans are flexible, the best time to travel by air might be during the second trimester. The risks of common pregnancy emergencies are lowest during that time.
When you fly:
- Buckle up. During the trip, keep your seatbelt fastened when you are seated, and secure it under your belly.
- Drink plenty of fluids. Low humidity in the airplane could cause you to become dehydrated.
- Avoid gassy foods and drinks before you fly. Gases expand during flight, and that could make you uncomfortable. Examples of foods and drinks to avoid include broccoli and carbonated soda.
- Think about medical care. Plan for how you'll get obstetric care during your trip if you need it. Bring copies of your medical information in case you need care while you're away.
Blood clots
Air travel can raise the risk for blood clots in the legs, a condition called venous thrombosis. The risk is higher for pregnant people. Moving your legs may help prevent this problem. Take a walk up and down the aisle every hour during the flight. If you must remain seated, flex and extend your ankles from time to time. In general, it's best to avoid tightfitting clothing, as that can hinder blood flow. Wearing compression stockings can help with blood circulation during a long flight.
Radiation exposure linked to air travel at high altitudes isn't thought to be a problem for most people who fly during pregnancy. But pilots, flight attendants and others who fly often might be exposed to a level of radiation that raises concerns during pregnancy. If you must fly frequently during your pregnancy, talk about it with your health care provider.
Mary Marnach, M.D.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Allergy medications during pregnancy
- AskMayoExpert. Health considerations for air travelers: Pregnancy considerations. Mayo Clinic; 2022.
- Air Travel During Pregnancy: ACOG Practice Bulletin No. 746. American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/08/air-travel-during-pregnancy. Accessed Dec. 1, 2022.
- Ram S, et al. Air travel during pregnancy and the risk of venous thrombosis. American Journal of Obstetrics and Gynecology. 2022; doi:10.1016/j.ajogmf.2022.100751.
Products and Services
- A Book: Obstetricks
- Available Solutions for Prenatal Nutrition from Mayo Clinic Store
- A Book: Taking Care of You
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- Ankle swelling during pregnancy
- Antibiotics and pregnancy
- Aspirin during pregnancy
- Pregnancy back pain
- Falling during pregnancy: Reason to worry?
- Fetal ultrasound
- Flu shot in pregnancy
- Headaches during pregnancy: What's the best treatment?
- Iron deficiency anemia during pregnancy: Prevention tips
- Leg cramps during pregnancy
- Pregnancy acne
- Pregnancy and fish
- Pregnancy constipation
- Pregnancy diet: Essential nutrients
- Pregnancy due date calculator
- Pregnancy exercises
- Pregnancy nutrition don'ts
- Pregnancy stretches
- Pregnancy weight gain
- Pregnant. Now What Happens?
- Prenatal testing
- Prenatal vitamins and pregnancy
- Sex during pregnancy
- Twin pregnancy
- Vaccines during pregnancy
- Vaping during pregnancy
- Working during pregnancy
- X-ray during pregnancy
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Expert Answers
- Air travel during pregnancy Is it safe
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
Pregnancy Travel Tips
Medical review policy, latest update:, can you travel while pregnant , read this next, when should you stop traveling while pregnant, how should you prepare for a trip during pregnancy, what do pregnant women need to know about travel and the zika virus, travel tips for pregnant people, when should you seek medical care while traveling during pregnancy.
While traveling during pregnancy is generally considered safe for most moms-to-be, you’ll need to take some precautions before making any plans — and get the green light from your practitioner first.
What to Expect When You’re Expecting , 5th edition, Heidi Murkoff. WhatToExpect.com, Zika Virus and Pregnancy , October 2020. WhatToExpect.com, What to Know About COVID-19 if You’re Pregnant , February 2021. American College of Obstetricians and Gynecologists, Travel During Pregnancy , August 2020. Johns Hopkins Medicine, Traveling While Pregnant or Breastfeeding , 2021. Centers for Disease Control and Prevention, COVID-19 Travel Recommendations by Destination , May 2021. Centers for Disease Control and Prevention, Pregnant and Recently Pregnant People , May 2021. Centers for Disease Control and Prevention, Pregnant Travelers , December 2020. Centers for Disease Control and Prevention, Travel: Frequently Asked Questions and Answers , April 2021. Centers for Disease Control and Prevention, COVID-19 and Cruise Ship Travel , March 2020.
Jump to Your Week of Pregnancy
Trending on what to expect, signs of labor, pregnancy calculator, ⚠️ you can't see this cool content because you have ad block enabled., top 1,000 baby girl names in the u.s., top 1,000 baby boy names in the u.s., braxton hicks contractions and false labor.
Travelling in pregnancy
With the proper precautions such as travel insurance, most women can travel safely well into their pregnancy.
Wherever you go, find out what healthcare facilities are at your destination in case you need urgent medical attention. It's a good idea to take your maternity medical records (sometimes called handheld notes) with you so you can give doctors the relevant information if necessary.
Find out more about getting healthcare abroad .
Make sure your travel insurance covers you for any eventuality, such as pregnancy-related medical care during labour, premature birth and the cost of changing the date of your return trip if you go into labour .
When to travel in pregnancy
Some women prefer not to travel in the first 12 weeks of pregnancy because of nausea and vomiting and feeling very tired during these early stages. The risk of miscarriage is also higher in the first 3 months, whether you're travelling or not.
Travelling in the final months of pregnancy can be tiring and uncomfortable. So, many women find the best time to travel or take a holiday is in mid-pregnancy, between 4 and 6 months.
Flying in pregnancy
Flying isn't harmful to you or your baby, but discuss any health issues or pregnancy complications with your midwife or doctor before you fly.
The chance of going into labour is naturally higher after 37 weeks (around 32 weeks if you're carrying twins), and some airlines won't let you fly towards the end of your pregnancy. Check with the airline for their policy on this.
After week 28 of pregnancy, the airline may ask for a letter from your doctor or midwife confirming your due date, and that you are not at risk of complications. You may have to pay for the letter and wait several weeks before you get it.
Long-distance travel (longer than 4 hours) carries a small risk of blood clots (deep vein thrombosis (DVT)) . If you fly, drink plenty of water and move about regularly – every 30 minutes or so. You can buy a pair of graduated compression or support stockings from the pharmacy, which will help reduce leg swelling.
Travel vaccinations when you're pregnant
Most vaccines that use live bacteria or viruses aren't recommended during pregnancy because of concerns that they could harm the baby in the womb.
However, some live travel vaccines may be considered during pregnancy if the risk of infection outweighs the risk of live vaccination. Ask your GP or midwife for advice about specific travel vaccinations. Non-live (inactivated) vaccines are safe to use in pregnancy.
Malaria tablets
Some anti-malaria tablets aren't safe to take in pregnancy so ask your GP for advice.
Zika virus is mainly spread by mosquitoes found in some parts of the world. For most people it's mild and not harmful, but can cause problems if you're pregnant.
If you are pregnant, it is not recommended to travel to parts of the world where the Zika virus is present, such as parts of:
- South and Central America
- the Caribbean
- the Pacific islands
Check before you travel
It's important to check the risk for the country you're going to before you travel.
Find out more about the Zika virus risk in specific countries on the Travel Health Pro website
Car travel in pregnancy
It's best to avoid long car journeys if you're pregnant. However, if it can't be avoided, make sure you stop regularly and get out of the car to stretch and move around.
You can also do some exercises in the car (when you're not driving), such as flexing and rotating your feet and wiggling your toes. This will keep the blood flowing through your legs and reduce any stiffness and discomfort. Wearing compression stockings while on long car journeys (more than 4 hours) can also increase the blood flow in your legs and help prevent blood clots.
Tiredness and dizziness are common during pregnancy so it's important on car journeys to drink regularly and eat natural, energy-giving foods, such as fruit and nuts.
Keep the air circulating in the car and wear your seatbelt with the cross strap between your breasts and the lap strap across your pelvis under your bump, not across your bump.
Road accidents are among the most common causes of injury in pregnant women. If you have to make a long trip, don't travel on your own. You could also share the driving with your companion.
Sailing in pregnancy
Ferry companies have their own restrictions and may refuse to carry heavily pregnant women (often beyond 32 weeks on standard crossings and 28 weeks on high-speed crossings ). Check the ferry company's policy before you book.
For longer boat trips, such as cruises, find out if there are onboard facilities to deal with pregnancy and medical services at the docking ports.
Food and drink abroad in pregnancy
Take care to avoid food- and water-borne conditions, such as stomach upsets and travellers' diarrhoea . Some medicines for treating stomach upsets and travellers' diarrhoea aren't suitable during pregnancy.
Always check if tap water is safe to drink. If in doubt, drink bottled water. If you get ill, keep hydrated and continue eating for the health of your baby, even if you're not hungry.
Find out about a healthy diet in pregnancy , and foods to avoid in pregnancy .
Page last reviewed: 17 August 2022 Next review due: 17 August 2025
Find support
Many parents and parents-to-be face a world of unknowns, but they all want a healthy and strong start. That's where we come in. Explore a variety of topics and resources here.
- Community Stories
- Support In Your Area
- Compass by March of Dimes™
- Ovulation calculator
- Ovulation calendar
Ways to give
There are so many ways to support our research, education, advocacy and programs. Give today to ensure that every family is healthy and strong now and tomorrow.
- Give with Donor-Advised Fund
- Stock and IRA Charitable Rollovers
- March for Babies
- Fundraise Your Way
- March of Dimes Innovation Fund
- Roosevelt Society
- Legacy Giving: Wills, Trusts, and Estates
Addressing the maternal and infant health crisis is not straightforward with one solution. It takes strategic and collaborative efforts in different areas to ultimately benefit thousands of moms, babies and families every day. Discover more here.
- ICBD Conference
- Mom and Baby Action Network
- Policy & Advocacy
- Public Health Data Reports
- For Health Professionals
- NICU Initiatives
- NICU Family Support
We're committed to ending preventable maternal health risks and death, ending preventable preterm birth and infant death and closing the health equity gap for all families. Learn more about our legacy and impact here.
- Accomplishments
- Annual Reports
- In Your Area Find opportunities to get involved
- Volunteer Help us by being on the frontlines
- Advocate Join us in the fight of all moms and babies
- Partner Collaborate to make a difference for families
- Donate Help us by making a donation
- Careers Discover your chance to make a big impact
- See all ways to Get Involved
Travel during pregnancy
Being pregnant doesn’t mean you have to be stuck at home. If you’re going on a business trip or taking a vacation, there are ways you can stay healthy and safe when traveling during pregnancy.
Is it safe to travel when you’re pregnant?
If you have a healthy pregnancy, it’s usually safe to travel. But talk to your health care provider before planning any trip.
If you have a health condition, such as heart disease, or if you’ve had pregnancy complications, such as gestational diabetes , your provider may suggest you limit travel.
Even if your pregnancy is healthy, tell your provider about your travel plans. You may need to rearrange your prenatal care visits so you don’t miss any while you’re away.
When is the best time to travel during pregnancy?
The best time to travel depends on how you feel. Many pregnant women like to travel during the second trimester. At this time, you may not have as much morning sickness or be as tired as you were at the beginning of your pregnancy. And while your belly’s getting bigger, it’s still comfortable for you to move around. As you get closer to your due date , walking, sitting and even sleeping can be very uncomfortable.
During the second trimester, you’re also less likely to have a pregnancy emergency, such as miscarriage or preterm labor. Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy. Preterm labor is labor that happens too early, before 37 weeks of pregnancy.
How can you get ready for your trip?
Plan ahead and follow these tips to stay safe when traveling during pregnancy:
- Ask your airline if they have a cut-off time for traveling during pregnancy. You can fly on most airlines up to 36 weeks of pregnancy. But if you’re flying out of the country, the cut-off time may be earlier.
- Check to see what medical care your health insurance covers. Health insurance helps you pay for medical care. Most insurance plans cover emergency medical care no matter where you are. But you need to know what your plan means by “emergency” to know exactly what it will pay for.
- Think about buying travel insurance. This is insurance you buy in addition to your regular health insurance. It covers you for medical care while traveling in another country. You also can buy travel insurance that refunds some of your costs if you have to cancel your trip. Visit USA.gov to learn more about the different kinds of travel insurance.
- Learn about medical care available where you’re headed. Your provider may be able to recommend a provider in the area where you’re going. If you’re traveling in the United States, you can find a provider through the American Medical Association . If you’re traveling overseas, find a provider through the International Association for Medical Assistance to Travelers’ database .
- Pack a copy of your medical records, your provider’s phone number, your prenatal vitamins and any medicine you need. Keep these things in your purse, a carry-on or a bag you plan to have with you at all times. This way, they’re always handy.
- Visit the Centers for Disease Control and Prevention (CDC) for information about vaccinations , travel alerts , managing health conditions during your trip and other ways you can stay healthy during travel.
- If you can, travel with someone. Don’t travel alone if you don’t have to.
Is it safe to travel to places where Zika is spreading if you're pregnant?
Zika virus (also called Zika) can cause illness that lasts several days to a week. It usually spreads to people through mosquito bites. But if you get infected with Zika during pregnancy , you can pass the virus to your baby. Zika infection during pregnancy can cause serious problems for your baby.
If you're pregnant or trying to get pregnant, don't travel to a Zika-affected area unless you absolutely have to. If you do travel, protect yourself and your family from mosquito bites. Check CDC travel alerts often for updates.
When should you seek medical care during travel?
If you have any of the following signs and symptoms during your trip, get medical help right away:
- Belly pain or cramps
- Contractions (when the muscles of your uterus get tight and then relax)
- Severe headaches
- Leg swelling or pain
- Vaginal bleeding (when blood comes out of your vagina) or you pass blood tissue or clots
- Vision problems
- Your water breaks. This can be in a large gush or a continuous trickle.
How can you stay safe when traveling by plane?
If your pregnancy is healthy, it’s usually safe to travel by plane.
Follow these tips when traveling by air:
- If you’ve had morning sickness during pregnancy, ask your provider if you can take medicine to help with nausea.
- Book an aisle seat so you don't have to climb over other passengers when you need to get up to use the restroom or walk around. Try sitting towards the front of the plane where the ride feels smoother.
- Drink plenty of water. Don’t drink carbonated drinks, such as soda. And don’t eat foods, such as beans, that may cause gas. Gas in your belly can expand at high altitudes and make you feel uncomfortable.
- Fasten your seat belt when you’re in your seat. This can help keep you from getting hurt in case of turbulence. Turbulence happens when the air around a flying plane causes a bumpy ride.
- Wear loose, comfortable clothing. Flex your ankles during the flight, and take a walk when it's safe to leave your seat. Doing these things can help your blood flow and lower your risk of deep vein thrombosis (DVT), a blood clot inside a vein. Sitting for long stretches of time during any kind of travel raises your chances of having DVT. Ask your health care provider if you should wear support stockings during your flight. They may help prevent DVT. But if you have diabetes or problems with blood circulation, you probably shouldn’t wear them.
- Tell the flight attendant if you feel sick or very uncomfortable during your flight. Contact your provider as soon as you can.
How can you stay safe when traveling by car?
If you're pregnant and traveling by car, follow these tips:
- Wear your seat belt.
- Try not to drive more than 5 to 6 hours per day. If you can, break your trip into several days with shorter drive times each day.
- During long drives, drink water, wear loose-fitting clothes and take breaks to get out of the car to walk around and stretch. And ask your provider if you should wear support stockings. Doing these things can lower your risk of DVT. Don’t turn off your car’s air bags. Airbags can keep you and your baby safe in a crash.
- Tilt your seat and move it as far as possible from the dashboard or steering wheel. If you’re driving, though, make sure you can reach the foot pedals.
- If you’re in an accident, get medical help right away.
How can you stay safe when traveling by ship?
If you’re pregnant and traveling on a ship, such as a cruise vacation, follow these tips:
- Call your cruise line to confirm that a health care provider will be on the ship at all times. Ask what medical care may be available at each port stop. Ask if your ship has passed a CDC health inspection .
- Ask your provider if you can take medicine to help prevent or treat sea sickness.
- Wash your hands often and wash any fruits and vegetables you eat during the cruise to help avoid getting infections.
How can you stay safe when traveling out of the country?
If your pregnancy is healthy, it may be safe for you to travel abroad. But check with your provider before you make plans. If you have certain pregnancy complications, such as incompetent cervix (when the cervix opens too early), or if you’re pregnant with twins, triplets or more , your provider may recommend that you not travel out of the country.
If you’re thinking about traveling out of the country, follow these tips:
- Talk to your provider about your travel plans. Ask about pregnancy complications and if it’s safe to travel to the country you’re planning to visit. Ask your provider about vaccinations you need before your trip and about taking medicine with you.
- Find out what your health insurance covers when traveling outside the country. And think about buying travel insurance.
- Find a provider or a medical center in the country you’re planning to visit before you leave home. Look for a center where providers can manage pregnancy complications, perform emergency cesarean sections (c-sections) and care for premature babies. The International Association for Medical Assistance can help find this kind of information.
- Make sure the country you’re planning to visit regularly screens stored blood for HIV , hepatitis B and hepatitis C. This is very important if you need a blood transfusion or if your baby is at risk of Rh disease . Visit the U. S. Department of State website for information on blood screening by country.
- Take a copy of your medical records with you. Know what your blood type is.
- Register with the American embassy or consulate once you arrive. Staff there can help if you need to get out of the country during an emergency.
- If you don’t speak the local language, take a dictionary.
Last reviewed: April, 2016
- Skip to main content
- Skip to site information
Language selection
Help us to improve our website. Take our survey !
Travelling while pregnant
Find useful information and considerations to help you prepare for safe and healthy travels outside Canada while pregnant.
With careful preparation, travelling while pregnant can be safe. The decision to travel should be made in consultation with your health care professional, based on your personal health circumstances.
On this page
Before you go, while you're away, if you need help.
Medical practices, health standards and infection control measures vary from country to country. You may not have access to the same level of care, procedures, treatments and medications as you would in Canada.
You could also be at increased risk of getting an infection and/or developing severe complications from certain infections, which could also affect the fetus.
Before leaving Canada:
- consult a health care professional or visit a travel health clinic at least 6 weeks before travelling to get personalized health advice and recommendations
- check our Travel Advice and Advisories for country-specific information, including about possible health risks
- know how to seek medical assistance outside of Canada
- review the policy and the coverage it provides
- most policies do not automatically cover pregnancy-related conditions or hospital care for premature infants
- ask your insurance provider about coverage for medical care during pregnancy, giving birth and intensive care for you and your fetus or newborn
- carry a copy of your prenatal records
- talk to your health care professional about any additional items you may want to bring that are specific to your health needs
Local laws and medical services relating to pregnancy can differ from Canada. Learn the local laws, and how these may apply to you before you travel.
Pre-travel vaccines and medications
Many vaccines can be safely given during pregnancy. Due to a higher risk of more severe outcomes for you and your fetus, some vaccines are recommended specifically during pregnancy, such as tetanus-diphtheria-pertussis (DTaP) and influenza.
Don’t take medications you may still have from prior trips. Tell the health care professional about your pregnancy, or intended pregnancy, before filling any prescriptions. The decision to get any pre-travel vaccinations or medications should be discussed with your health care professional.
The decision can depend on:
- your purpose of travel (e.g., tourism, visiting friends and relatives)
- your planned destination(s)
- the length of your trip
- your risk of getting a disease
- how severe the effect of a disease would be to you and/or your fetus
- your planned activities
- any underlying medical issues and/or pregnancy-related complications
Malaria could cause major health problems for a mother and her unborn baby. A pregnant woman may want to consider avoiding travel to areas where malaria transmission occurs.
Description of malaria risk by country and preventative measures.
If you can’t avoid travelling to an area where malaria is present:
- some medications to prevent or treat malaria may not be safe during pregnancy
- take extra care to protect yourself from mosquito bites
Zika virus infection during pregnancy can pose significant risks to your fetus even if you don’t develop symptoms. While pregnant, you may want to consider avoiding travelling to a country or areas with risk of Zika virus.
Latest travel health advice on Zika virus.
If you choose to travel, take precautions to avoid infection with Zika virus:
- prevent mosquito bites at all times
- protect yourself from contact with semen, vaginal fluid and blood
- always use condoms correctly or avoid sexual contact while in countries or areas with risk of Zika virus
Learn more about Zika virus and pregnancy:
- Zika virus: Pregnant or planning a pregnancy
- Zika virus: Advice for travellers
- Pregnancy and travel (tropical medicine and travel)
Monitor your health and be prepared
Emergencies can happen at any time. Know where the nearest hospital or medical centre is while you are travelling and confirm they will accept your medical insurance.
Seek medical attention immediately if you develop any of the following symptoms while travelling:
- persistent vomiting and/or diarrhea
- dehydration
- vaginal bleeding
- passing tissue or clots
- abdominal pain, cramps or contractions
- your water breaks
- excessive swelling of face, hands or legs
- excessive leg pain
- severe headaches
- visual problems
If you develop these symptoms after your return to Canada, you should see a health care professional immediately and tell them about your recent trip.
Transportation
Always wear a seatbelt when travelling by plane or car. When using a diagonal shoulder strap with a lap belt, the straps should be placed carefully above and below your abdomen. If only a lap belt is available, fasten it at the pelvic area, below your abdomen.
If you have any medical or pregnancy-related complications, discuss with your health care professional whether air travel is safe for you.
Most airlines restrict travel in late pregnancy or may require a written confirmation from a physician. Check this with the airline before booking your flight.
During long flights, you may be at higher risk of developing blood clots, known as deep vein thrombosis (DVT). The risk of deep vein thrombosis can be reduced by:
- getting up and walking around occasionally
- exercising and stretching your legs while seated
- selecting an aisle seat when possible
- wearing comfortable shoes and loose clothing
Your health care professional may recommend additional ways to reduce your risk such as wearing compression stockings.
Always stay well hydrated while travelling.
Land travel
The risk of deep vein thrombosis can be reduced by:
- stopping the vehicle to walk around every couple of hours
Motion sickness
Certain medications used to treat nausea and vomiting during pregnancy may also be effective in relieving motion sickness.
If you think you might experience motion sickness during your trip, speak to your health care professional about the use of these medications.
Environmental and recreational risks
Some activities may not be recommended or may require additional precautions. Discuss your travel plans, including any planned or potential recreational activities with a health care professional.
High altitude
You should avoid travelling to an altitude above 3,658 metres (12,000 feet).
However, if you have a high-risk pregnancy and/or are in the late stages of pregnancy, the highest altitude should be 2,500 metres (8,200 feet).
If you have pregnancy-related complications, you should avoid unnecessary high-altitude exposure.
Keep in mind that most high-altitude destinations are far from medical care services.
Personal protective measures
Food-borne and water-borne diseases.
Eat and drink safely while travelling while travelling. Many food-borne and water-borne illnesses can be more severe during pregnancy and pose a risk to the fetus.
This can include:
- toxoplasmosis
- listeriosis
- hepatitis A and E
To help avoid food-borne and water-borne diseases:
- before eating or preparing food
- after using the bathroom or changing diapers
- after contact with animals or sick people
- before and after touching raw meat, poultry, fish and seafood
- if you’re at a destination that lacks proper sanitation and/or access to clean drinking water, only drink water if it has been boiled or disinfected or if it’s in a commercially sealed bottle
- use ice made only from purified or disinfected water
- this could cause the fetus or newborn to develop thyroid problems
- unpasteurized dairy products, such as raw milk and raw milk soft cheeses
- unpasteurized juice and cider
- raw or undercooked eggs, meat or fish, including shellfish
- raw sprouts
- non-dried deli meats, including bologna, roast beef and turkey breast
- don’t use bismuth subsalicylate (Pepto-Bismol®)
- Information on travellers’ diarrhea
Illnesses acquired from insect and other animals
Protect yourself from insect bites:
- wear light-coloured, loose clothes made of tightly woven materials such as nylon or polyester
- prevent mosquitoes from entering your living area with screening and/or closed, well-sealed doors and windows
- use insecticide-treated bed nets if mosquitoes can’t be prevented from entering your living area
- information on insect bite and pest prevention
Some infections, such as rabies and influenza, can be shared between humans and animals. You should avoid contact with animals including dogs, livestock (pigs, cows), monkeys, snakes, rodents, birds, and bats.
Information for if you become sick or injured while travelling outside Canada.
For help with emergencies outside Canada, contact the:
- nearest Canadian office abroad
- Emergency Watch and Response Centre in Ottawa
More information on services available at consular offices outside Canada.
Related links
- Immunization in pregnancy and breastfeeding: Canadian Immunization Guide
- Advice for Canadians travelling to Zika-affected countries
- Advice for women travellers
- If you get sick before or after returning to Canada
- Receiving medical care in other countries
- Travel vaccinations
- What you can bring on a plane

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Travel Tips: Pregnant Travelers
All screening equipment at the airport security checkpoint is safe for all travelers, including women who are pregnant. Watch this travel tips video if you have questions about the security screening process when traveling while pregnant.

How to Make Long Flights More Comfortable When You're Pregnant
By Joanna Carrigan

All products featured on Condé Nast Traveler are independently selected by our editors. However, when you buy something through our retail links, we may earn an affiliate commission.
Preparing for a newborn can feel like an exhilarating task; on the one hand, there’s a long-anticipated, already much-loved new arrival making an entrance into your life. On the other, getting yourself into a birthing headspace can feel like a marathon. I’ve already lost count of the amount of stroller reviews , hypno-birthing manuals, crib catalogs, and paint samples I’ve flicked through in my quest for newborn nirvana.
With that in mind, many couples are now opting to take a break from the organizational overload in the form of a long-haul babymoon —a pre-birth couples vacation—as a way of spending those last special moments together as a family of two. And in fact, air travel can generally be considered safe for most expectant mothers , with advice from your doctor recommended.
“All pregnancies and mums have individual needs and varying circumstances,” says Marie Louise, midwife and author of The Modern Midwife’s Guide To Pregnancy . “If mums have any health complications or are close to giving birth, travel should be very carefully considered. Otherwise, mums need a break—it’s good to enjoy and relax on your travels.”
Pregnancy can often feel like a long-haul adventure in itself, and whilst the thought of an extensive flight may not jump out at the top of your to-do list, there are ways to make that coveted trip—and any other air travel during pregnancy that comes up—more comfortable.
Below, I’ve curated an essential list for what to pack in your carry-on for air travel during pregnancy, based in part on my own experience traveling to Europe whilst expecting.
Strategic carry-ons
A great place to start is your carry-on itself, as the right style can help not only to make your essentials more accessible, but the correct product can be re-used as a diaper bag once your pre-baby vacation is a distant happy memory. The key to choosing the perfect carry-on is not only to be mindful of the airline guidelines set out around dimensions and weight restrictions, but to think from your own perspective about what will be easiest for you to carry. If back issues prevail—a common complaint during pregnancy—a stylish rucksack may be more suitable than a tote. And if you’re looking for post-pregnancy practicality, a duffel can tick that cross-functional box.

Pregnancy support bands
Glamour takes a back seat with this essential, but your posture and ligaments will thank me later. If you’re flying internationally or just maneuvering your way through a large airport, you may face long walks between terminals, which can place strain on the lower back. Bump support bands are designed to help relieve the pressure that the additional weight of your bump is putting on your back, and therefore can make a sensible addition to your carry-on packing list.

Anti-nausea pregnancy methods
Not every foray into the world of parenthood is a smooth one, and unfortunately nausea and sickness can play a starring role in pregnancy, especially in the early stages. My first 16 weeks of pregnancy were punctuated with frequent trips to the restroom, and with many flights taken during this time, I became accustomed to having to rely on a few tricks to see me through those difficult moments.
Travel bands can be an excellent way to relieve pregnancy related nausea, and they’ve taken a high-tech turn in recent years. Hypnotherapy podcasts can also be a calming way to reduce feelings of sickness, and are best listened to with noise-canceling headphones and an eye mask .

Hydrating skincare for expectant mothers
Pregnancy can present some interesting skincare dilemmas , with many people experiencing a change at some point across their nine months. Dry patches, oily T-zones, and acne outbreaks are all common complaints. To help skin stay hydrated when flying, there are many pregnancy-safe products out there which can help replenish and restore your skin's natural barrier. La Mer The Mist Facial Spray is a particular favorite of mine—easy to apply, super lightweight, and long-lasting.

Travel pillows
During pregnancy, ligaments in the hips and back loosen in preparation for birth and this can often cause secondary strain across the top of the shoulders and neck which can be very uncomfortable for expectant mothers. If you’re traveling whilst pregnant, I recommend investing in a travel neck pillow , and packing your pregnancy pillow if you’re flying in a seat with a lie-flat bed.
Compression socks
“During pregnancy, you are at an increased risk of developing a blood clot,” Louise says. “That’s why compression socks , hydration, and movement—walking, stretching, and circling ankles—is recommended.”
Again, it’s not the most glamorous addition to your carry-on, but this footwear is important nonetheless. Try to stretch your legs every hour or so if possible, with a walk down the aisle or some lower leg exercises.

While packing a well-stocked carry-on will undoubtedly enhance your flying experience, there are other ways to ensure that you’re prepared for a relaxing trip. Here are my top three tips for flying while pregnant:
Food and beverage choices
Whilst it’s unlikely you’ll be able to see the full on-board menu in advance, it’s often a good idea to pre-select your meal genre if you’re having aversions or preferences during your pregnancy. Being able to rule out meat, dairy, or even opt for a lighter option may be preferable for some mothers-to-be. It could be worth packing a couple of extra snacks in your carry-on, just in case. I’ve been stashing ginger tea bags and plenty of dried fruit and nuts ( dried banana chips are a particular craving of mine) to see me through.
The airport experience
Lounge access can not only be an enjoyable way to kick-off your vacation, it can also be a lifesaver for tired feet. Having access to a clean and comfortable restroom can also often be advantageous, so if your travel tickets don’t include a lounge as standard, it could be worth a pay-for-access option to give you peace of mind that you’ll be spending time in a calm and restful environment before or in between flights.
Your travel outfit
While a stylish airport look is always desirable, comfort should definitely reign supreme during this important period, since your body is already coping with so much. Activewear can provide comfort and support during long-haul travel, and there are plenty of options out there. I look to brands like Alo Yoga and Lululemon for pieces that satisfy both the style and comfort stakes.

Pregnancy is an exciting time.
Knowing that you are doing all you can to stay healthy during pregnancy and give your baby a healthy start in life will help you to have peace of mind.
Find tips to get ready for pregnancy.
Learn how to give your baby a healthy start in life.
Keep yourself and baby healthy and safe after birth.
Read about causes and find resources for getting pregnant.
Learn ways to prevent pregnancy.
Use of multiple substances in pregnancy is common
Opioid use during pregnancy can affect women and their babies.
Learn about Zika virus and pregnancy.
Read about the goals and impact of surveillance for emerging threats to mothers and babies.
Learn about Cytomegalovirus (CMV) and Congenital CMV Infection
- Safe in Pregnancy – Living Systematic Review
- Clinical Considerations for Monkeypox in People Who are Pregnant or Breastfeeding
Learn about vaccines you will need before, during, and after pregnancy to best protect yourself and baby against serious diseases.

Learn more about medication use during pregnancy.

Learn how infections can complicate pregnancy and may have serious consequences for a woman, her pregnancy outcomes, and her baby.

Read stories from real pregnancy and find peace of mind in knowing your baby will have a healthy start.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 5 - Rubella
- Section 5 - Smallpox & Other Orthopoxvirus-Associated Infections
Rubeola / Measles
Cdc yellow book 2024.
Author(s): Paul Gastañaduy, James Goodson
Infectious Agent
Transmission, epidemiology, clinical presentation.
INFECTIOUS AGENT: Measles virus
TRAVELER CATEGORIES AT GREATEST RISK FOR EXPOSURE & INFECTION
PREVENTION METHODS
Rubeola is a vaccine-preventable disease
DIAGNOSTIC SUPPORT
Measles virus is a member of the genus Morbillivirus of the family Paramyxoviridae .
Measles is transmitted from person to person via respiratory droplets and by the airborne route as aerosolized droplet nuclei. Infected people are usually contagious from 4 days before until 4 days after rash onset. Measles is among the most contagious viral diseases known; secondary attack rates are ≥90% among susceptible household and institutional contacts. Humans are the only natural host for sustaining measles virus transmission, which makes global eradication of measles feasible.
Measles was declared eliminated (defined as the absence of endemic measles virus transmission in a defined geographic area for ≥12 months in the presence of a well-performing surveillance system) from the United States in 2000. Measles virus continues to be imported into the country from other parts of the world, however, and recent prolonged outbreaks in the United States resulting from measles virus importations highlight the challenges faced in maintaining measles elimination.
Given the large global measles burden and high communicability of the disease, travelers could be exposed to the virus in any country they visit where measles remains endemic or where large outbreaks are occurring. Most measles cases imported into the United States occur in unvaccinated US residents who become infected while traveling abroad, often to the World Health Organization (WHO)–defined Western Pacific and European regions. These travelers become symptomatic after returning to the United States and sometimes infect others in their communities, causing outbreaks.
Nearly 90% of imported measles cases are considered preventable by vaccination (i.e., the travelers lacked recommended age- and travel-appropriate vaccination). Furthermore, observational studies in travel clinics in the United States have shown that 59% of pediatric and 53% of adult travelers eligible for measles-mumps-rubella (MMR) vaccine at the time of pretravel consultation were not vaccinated at the visit, highlighting a missed opportunity to reduce the likelihood of measles introductions and subsequent spread. Encourage all eligible travelers to receive appropriate MMR vaccination. Outbreak investigations are costly and resource intensive, and infected people—in addition to productivity losses—can incur direct costs for the management of their illness, including treatment, quarantine, and caregiving.
The incubation period averages 11–12 days from exposure to onset of prodrome; rash usually appears ≈14 days after exposure. Symptoms include fever, with temperature ≤105°F (≤40.6°C); conjunctivitis; coryza (runny nose); cough; and small spots with white or bluish-white centers on an erythematous base appearing on the buccal mucosa (Koplik spots). A characteristic red, blotchy (maculopapular) rash appears 3–7 days after onset of prodromal symptoms. The rash begins on the face, becomes generalized, and lasts 4–7 days.
Common measles complications include diarrhea (8%), middle ear infection (7%–9%), and pneumonia (1%–6%). Encephalitis, which can result in permanent brain damage, occurs in ≈1 per 1,000–2,000 cases of measles. The risk for serious complications or death is highest for children aged ≤5 years, adults aged ≥20 years, and in populations with poor nutritional status or that lack access to health care.
Subacute sclerosing panencephalitis (SSPE) is a progressive neurologic disorder caused by measles virus that usually presents 5–10 years after recovery from the initial primary measles virus infection. SSPE manifests as mental and motor deterioration, which can progress to coma and death. SSPE occurs in ≈1 of every 5,000 reported measles cases; rates are higher among children <5 years of age.
Measles is a nationally notifiable disease. Laboratory criteria for diagnosis include a positive serologic test for measles-specific IgM, IgG seroconversion, or a significant rise in measles IgG level by any standard serologic assay; isolation of measles virus; or detection of measles virus RNA by reverse transcription PCR (RT-PCR) testing. The Centers for Disease Control and Prevention’s Measles Virus Laboratory is the national reference laboratory; it provides serologic and molecular testing for measles and technical assistance to state public health laboratories for the collection and shipment of clinical samples for molecular diagnostics and genetic analysis. See detailed information on diagnostic support .
A clinical case of measles illness is characterized by generalized maculopapular rash lasting ≥3 days; temperature ≥101°F (38.3°C); and cough, coryza, or conjunctivitis. A confirmed case is one with an acute febrile rash illness with laboratory confirmation or direct epidemiologic linkage to a laboratory-confirmed case. In a laboratory-confirmed or epidemiologically linked case, the patient’s temperature does not need to reach ≥101°F (38.3°C) and the rash does not need to last ≥3 days.
Treatment is supportive. The WHO recommends vitamin A for all children with acute measles, regardless of their country of residence, to reduce the risk for complications. Administer vitamin A as follows: for infants <6 months old, give 50,000 IU, once a day for 2 days; for infants 6 months old and older, but younger than 12 months, give 100,000 IU once a day for 2 days; for children ≥12 months old give 200,000 IU once a day for 2 days. For children with clinical signs and symptoms of vitamin A deficiency, administer an additional (i.e., a third) age-specific dose of vitamin A 2–4 weeks following the first round of dosing.
Measles has been preventable through vaccination since a vaccine was licensed in 1963. People who do not have evidence of measles immunity should be considered at risk for measles, particularly during international travel. Acceptable presumptive evidence of immunity to measles includes birth before 1957; laboratory confirmation of disease; laboratory evidence of immunity; or written documentation of age-appropriate vaccination with a licensed, live attenuated measles-containing vaccine 1 , namely, MMR or measles-mumps-rubella-varicella (MMRV). For infants 6 months old and older, but younger than 12 months, this includes documented administration of 1 dose of MMR; for people aged ≥12 months, documentation should include 2 doses of MMR or MMRV (the first dose administered at age ≥12 months and the second dose administered no earlier than 28 days after the first dose). Verbal or self-reported history of vaccination is not considered valid presumptive evidence of immunity.
1 From 1963–1967, a formalin-inactivated measles vaccine was available in the United States and was administered to ≈600,000–900,000 people. It was discontinued when it became apparent that the immunity it produced was short-lived. Consider people who received this vaccine unvaccinated.
Vaccination
Measles vaccine contains live, attenuated measles virus, which in the United States is available only in combination formulations (e.g., MMR and MMRV vaccines). MMRV vaccine is licensed for children aged 12 months–12 years and can be used in place of MMR vaccine if vaccination for measles, mumps, rubella, and varicella is needed.
International travelers, including people traveling to high-income countries, who do not have presumptive evidence of measles immunity and who have no contraindications to MMR or MMRV, should receive MMR or MMRV before travel per the following schedule.
Infants (6 months old and older, but younger than 12 months): 1 MMR dose. Infants vaccinated before age 12 months must be revaccinated on or after the first birthday with 2 doses of MMR or MMRV separated by ≥28 days. MMRV is not licensed for children aged <12 months.
Children (aged ≥12 months): 2 doses of MMR or MMRV separated by ≥28 days.
Adults born in or after 1957: 2 doses of MMR separated by ≥28 days.
One dose of MMR is ≈85% effective when administered at age 9 months; MMR and MMRV are 93% effective when administered at age ≥1 year. Vaccine effectiveness of 2 doses is 97%.
Adverse Reactions
In rare circumstances, MMR vaccination has been associated with anaphylaxis (≈2–14 occurrences per million doses administered); febrile seizures (≈1 occurrence per 3,000–4,000 doses administered, but overall, the rate of febrile seizures after measles-containing vaccine is much lower than the rate with measles disease); thrombocytopenia (≈1 occurrence per 40,000 doses during the 6 weeks after immunization); or joint symptoms (arthralgia develops among ≈25% of nonimmune postpubertal females from the rubella component of the MMR vaccination, and ≈10% have acute arthritis-like signs and symptoms that generally persist for 1–21 days and rarely recur; chronic joint symptoms are rare, if they occur at all). No evidence supports a causal link between MMR vaccination and autism, type 1 diabetes mellitus, or inflammatory bowel disease.
Contraindications
People who experienced a severe allergic reaction (difficulty breathing, hives, hypotension, shock, swelling of the mouth or throat) following a prior dose of MMR or MMRV vaccine, or who had an anaphylactic reaction to topically or systemically administered neomycin, should not be vaccinated or revaccinated. People who are allergic to eggs can receive MMR or MMRV vaccine without prior routine skin testing or the use of special protocols.
Immunosuppression
Enhanced replication of live vaccine viruses can occur in people who have immune deficiency disorders. Death related to vaccine-associated measles virus infection has been reported among severely immunocompromised people; thus, severely immunosuppressed people should not be vaccinated with MMR or MMRV vaccine. For a thorough discussion of recommendations for immunocompromised travelers, see Sec. 3, Ch. 1, Immunocompromised Travelers .
MMR vaccination is recommended for all people with HIV infection aged ≥12 months who do not have evidence of measles, mumps, and rubella immunity, and who do not have evidence of severe immunosuppression. The assessment of severe immunosuppression can be based on CD4 values (count or percentage); absence of severe immunosuppression is defined as CD4 ≥15% for ≥6 months for children aged ≤5 years, or CD4 ≥15% and CD4 count ≥200 cells/mL for ≥6 months for people aged >5 years.
People with leukemia in remission and off chemotherapy, who were not immune to measles when diagnosed with leukemia, may receive MMR vaccine. At least 3 months should elapse after termination of chemotherapy before administering the first dose of vaccine.
Steroids & Other Immunosuppressive Therapies
Avoid vaccinating people who have received high-dose corticosteroid therapy (in general, considered to be ≥20 mg or 2 mg/kg body weight of prednisone, or its equivalent, daily for ≥14 days) with MMR or MMRV for ≥1 month after cessation of steroid therapy. Corticosteroid therapy usually is not a contraindication when administration is short-term (<14 days) or a low to moderate dose (<20 mg of prednisone or equivalent per day).
In general, withhold MMR or MMRV vaccine for ≥3 months after cessation of other immunosuppressive therapies and remission of the underlying disease. See Sec. 3, Ch. 1, Immunocompromised Travelers , for more details.
MMR vaccines should not be administered to pregnant people or people attempting to become pregnant. Because of the theoretical risk to the fetus, people should be counseled to avoid becoming pregnant for 28 days after receiving a live-virus (e.g., MMR) vaccine.
Precautions
Personal or family history of seizures of any etiology.
Compared with administration of separate MMR and varicella vaccines at the same visit, use of MMRV vaccine is associated with a higher risk for fever and febrile seizures 5–12 days after the first dose among children aged 12–23 months. Approximately 1 additional febrile seizure occurs for every 2,300–2,600 MMRV vaccine doses administered. Use of separate MMR and varicella vaccines avoids this increased risk for fever and febrile seizures.
Thrombocytopenia
The benefits of primary immunization are usually greater than the potential risks for vaccine- associated thrombocytopenia. Avoid giving subsequent doses of MMR or MMRV vaccine, however, if an episode of thrombocytopenia occurred ≤6 weeks after a previous dose of vaccine.
Postexposure Prophylaxis
Measles-containing vaccine or immune globulin (IG) can be effective as postexposure prophylaxis. MMR or MMRV administered ≤72 hours after initial exposure to measles virus might provide some protection. If the exposure does not result in infection, the vaccine should induce protection against subsequent measles virus infection.
When administered ≤6 days of exposure, IG can be used to confer temporary immunity in a susceptible person. If the exposure does not result in modified or typical measles, vaccination with MMR or MMRV is still necessary to provide long-lasting protection. Six months after receiving intramuscularly administered IG, or 8 months after receiving intravenously administered IG, administer MMR or MMRV vaccine, provided the patient is aged ≥12 months and the vaccine is not otherwise contraindicated.
CDC website: Measles
The following authors contributed to the previous version of this chapter: Paul A. Gastañaduy, James L. Goodson
Bibliography
Centers for Disease Control and Prevention. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2013;62(RR-04):1–34.
Gastañaduy P, Redd S, Clemmons N, Lee AD, Hickman CJ, Rota PA, et al. Measles. In: Roush SW, Baldy LM, Kirkconnell Hall MA, editors. Manual for the surveillance of vaccine-preventable diseases. Atlanta: Centers for Disease Control and Prevention; 2019. Available from: www.cdc.gov/vaccines/pubs/surv-manual/chpt07-measles.html .
Hyle EP, Fields NF, Fiebelkorn AP, Taylor Walker A, Gastañaduy P, Rao SR, et al. The clinical impact and cost-effectiveness of measles-mumps-rubella vaccination to prevent measles importations among US international travelers. Clin Infect Dis. 2019;69(2):306–15.
Hyle EP, Rao SR, Bangs AC, Gastañaduy P, Parker Fiebelkorn A, Hagmann SHF, et al. Clinical practices for measles-mumps-rubella vaccination among US pediatric international travelers. JAMA Pediatr. 2020;174(2):e194515.
Hyle EP, Rao SR, Jentes ES, Parker Fiebelkorn A, Hagmann SHF, Taylor Walker A, et al. Missed opportunities for measles, mumps, rubella vaccination among departing U.S. adult travelers receiving pretravel health consultations. Ann Intern Med. 2017;167(2):77–84.
Lee AD, Clemmons NS, Patel M, Gastañaduy PA. International importations of measles virus into the United States during the post-elimination era, 2001–2016. J Infect Dis. 2019;219(10):1616–23.
National Notifiable Diseases Surveillance System. Measles (rubeola): 2013 case definition. Atlanta: CDC; 2013. Available from: https://ndc.services.cdc.gov/conditions/measles/ .
Patel MK, Goodson JL, Alexander JP Jr., Kretsinger K, Sodha SV, Steulet C, et al. Progress toward regional measles elimination—Worldwide, 2000–2019. MMWR Morb Mortal Wkly Rep. 2020;69(45):1700–5.
Pike J, Leidner AJ, Gastañaduy PA. A review of measles outbreak cost estimates from the US in the post-elimination era (2004–2017): Estimates by perspective and cost type. Clin Infect Dis. 2020;1(6):1568–76.
World Health Organization. Measles vaccines: WHO position paper—April 2017. Wkly Epidemiol Rec. 2017;92(17):205–27.
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Marketplace
- Marketplace Morning Report
- Marketplace Tech
- Make Me Smart
- This is Uncomfortable
- The Uncertain Hour
- How We Survive
- Financially Inclined
- Million Bazillion
- Marketplace Minute®
- Corner Office from Marketplace

- Latest Stories
- Collections
- Smart Speaker Skills
- Corrections
- Ethics Policy
- Submissions
- Individuals
- Corporate Sponsorship
- Foundations

Abortion included among pregnancy-related conditions covered under new EEOC guidelines

Share Now on:
- https://www.marketplace.org/2024/04/18/eeoc-pregnant-workers-fairness-act-abortion-care/ COPY THE LINK
HTML EMBED:
This week, the Equal Employment Opportunity Commission finalized regulations for carrying out the 2022 Pregnant Workers Fairness Act . Most employees around the country are now entitled to unpaid time off and other accommodations for a range of pregnancy-related medical needs, from nausea and gestational diabetes to abortion care.
While a 1978 law prohibits discrimination against pregnant people in the workplace, that didn’t solve everything, explained Elizabeth Gedmark with A Better Balance, which advocates for working parents.
“There were gaps in the law that were causing pregnant workers to fall through the cracks,” she said.
Under the old legal landscape, if a pregnant worker needed an accommodation — “like a stool to sit on, a water bottle or light duty for their health,” said Gedmark — they had to prove that their employer was providing that accommodation to nonpregnant workers.
Under the EEOC’s new rules, employers have to provide reasonable accommodations that workers ask for. And that includes at least unpaid time off for abortion care and recovery.
“That part of the regulation is actually not very surprising,” said Jennifer Shinall, a law professor at Vanderbilt.
Under that 1978 antidiscrimination law, abortion was considered a protected pregnancy-related condition, she said. Since then, “abortion has generally been recognized by federal courts as within the purview of pregnancy.”
Shinall doesn’t expect legal challenges to the new regulations to get very far. But given the political climate , she said workers seeking an abortion might feel it’s too risky to ask for accommodations.
“I would tell them just to tell their employer, ‘I am pregnant. It’s not going to be a successful pregnancy, and I need time to recover from that,'” Shinall said.
“That’s it. Employers are not allowed to dig deeper,” said Gillian Thomas with the ACLU’s Women’s Rights Project.
It’s gotten trickier for workers to maintain privacy when seeking an abortion since the Supreme Court’s Dobbs decision , Thomas said.
“Simply getting to and from, let alone the time that’s necessary for the procedure and recovery from the procedure — it’s just become exponentially longer,” she said.
These new regulations will help low-wage and hourly workers who may not have sick time, she said. But the cost of that travel and threat of lost wages could still prevent workers from getting care.
Stories You Might Like

A new law aims to better protect pregnant and postpartum workers

New federal law seeks to protect pregnant workers


40 years after the Pregnancy Discrimination Act, pregnant employees still face workplace discrimination

Crisis pregnancy centers are key to many anti-abortion groups’ strategy. But what are they?

Abortion providers in states with bans ask: What now?
Georgia recognizes embryos as dependents, for a $3,000 state income tax deduction
There’s a lot happening in the world. Through it all, Marketplace is here for you.
You rely on Marketplace to break down the world’s events and tell you how it affects you in a fact-based, approachable way. We rely on your financial support to keep making that possible.
Your donation today powers the independent journalism that you rely on . For just $5/month, you can help sustain Marketplace so we can keep reporting on the things that matter to you.
Also Included in
- Abortion Access
- Health care
- Pregnant workers
- Worker accommodations
Latest Episodes From Our Shows

Climate change is the focus in shared curriculum for business schools

CHIPS funds are heading to Phoenix, “ground zero for the new economy”

Student protestors have a long history of demanding financial divestment

Could the Fed cut interest rates based on this week's economic data?
Advertisement
Tracking Abortion Bans Across the Country
By The New York Times Updated May 1, 4:40 P.M. ET
- Share full article
Twenty-one states ban abortion or restrict the procedure earlier in pregnancy than the standard set by Roe v. Wade, which governed reproductive rights for nearly half a century until the Supreme Court overturned the decision in 2022.
In some states, the fight over abortion access is still taking place in courtrooms, where advocates have sued to block bans and restrictions. Other states have moved to expand access to abortion by adding legal protections.
Latest updates
- The Arizona state legislature voted to repeal an 1864 ban on nearly all abortions. Officials warned that the near-total ban may be briefly enforceable this summer until the repeal takes effect in the fall. A 15-week ban remains in effect.
- A ban on abortion after about six weeks of pregnancy took effect in Florida , following a ruling by the Florida Supreme Court that the privacy protections of the state’s Constitution do not extend to abortion.
The New York Times is tracking abortion laws in each state after the Supreme Court’s decision in Dobbs v. Jackson Women’s Health Organization , which ended the constitutional right to an abortion.
Where abortion is legal
In a few states that have enacted bans or restrictions, abortion remains legal for now as courts determine whether these laws can take effect. Abortion is legal in the rest of the country, and many states have added new protections since Dobbs.
Ban in effect
Note: TK note here.
Legal for now
State details.
More details on the current status of abortion in each state are below.
An earlier version of this article misstated the legal status of abortion in Utah. As of 4 p.m. on June 24, the state attorney general had issued a statement saying the state’s abortion ban had been triggered, but it had not yet been authorized by the legislature’s general counsel. By 8:30 p.m., the counsel authorized the ban and it went into effect.
A table in an earlier version of this article misstated which abortion ban is being challenged in Texas state court. Abortion rights supporters are challenging a pre-Roe ban, not the state’s trigger ban.
An earlier version of this article referred incorrectly to the legal status of abortion in Indiana. While Indiana abortion providers stopped offering abortion services in anticipation of an abortion ban taking effect on Aug. 1, the law did not take effect.
PWFA Final Rule is Now Published — It Takes Effect June 18, 2024
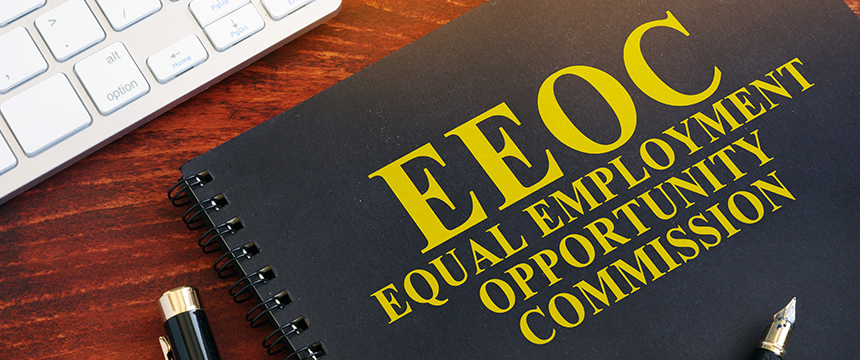
On April 15, 2024, the Equal Employment Opportunity Commission (EEOC) published a final rule to implement the Pregnant Workers Fairness Act (PWFA) (the “Rule”). By way of background, the PWFA requires covered employers to provide reasonable accommodations to employees with known limitations related to, affected by, or arising out of pregnancy, childbirth, or related medical conditions, unless to do so would cause undue hardship to the employer.
The Rule, which takes effect June 18, 2024, provides much-needed clarity regarding the PWFA. In particular, the Rule provides definitions for several terms, including defining a “known limitation” as a limitation that the employee or the employee’s representative has communicated to the employer. Likewise, the Rule defines the term “limitation” broadly, including minor or episodic conditions. The Rule also clarifies that a condition need not be considered a “disability” under the Americans With Disabilities Act (ADA) to qualify under the PWFA.
In addition to defining these terms, the Rule provides several examples of the types of reasonable accommodations that can be made available to employees under the PWFA. Such examples include frequent breaks, schedule changes, light duty, modifying equipment, and even temporarily suspecting essential functions. The Rule confirms that the definition of “undue hardship” mirrors the ADA definition of the same term (meaning significant difficulty or expense for the employer). Along with implementing the Rule, the EEOC put out a Summary of Key Provisions which walks through the various highlights of the Rule, including: covering key definitions in the Rule and summarizing processes including the interactive process; the ability to require documentation from an employee’s treating health care provider; and the Rule’s non-discrimination and anti-retaliation provisions. Employers should familiarize themselves with the Rule and seek advice from counsel in the event of any questions as to the Rule’s requirements, necessary policy updates, interplay between the PWFA and other laws, and following the PWFA in practice.

Krista M. Cabrera
Related insights, dol increases compensation threshold for exempt employees, utah enacts h.b. 55, impacting the use of confidentiality clauses in employment settlement agreements, bump in the road: federal judge selectively halts enforcement of the pregnant workers fairness act in texas.
- Latest News
- Emergencies
- Ask the Law
- GN Fun Drive
- Visa+Immigration
- Phone+Internet
- Reader Queries
- Safety+Security
- Banking & Insurance
- Dubai Airshow
- Corporate Tax
- Top Destinations
- Corporate News
- Electronics
- Home and Kitchen
- Consumables
- Saving and Investment
- Budget Living
- Expert Columns
- Community Tips
- Cryptocurrency
- Cooking and Cuisines
- Guide to Cooking
- Art & People
- Friday Partner
- Daily Crossword
- Word Search
- Philippines
- Australia-New Zealand
- Corrections
- From the Editors
- Special Reports
- Pregnancy & Baby
- Learning & Play
- Child Health
- For Mums & Dads
- UAE Success Stories
- Live the Luxury
- Culture and History
- Staying Connected
- Entertainment
- Live Scores
- Point Table
- Top Scorers
- Photos & Videos
- Course Reviews
- Learn to Play
- South Indian
- Arab Celebs
- Health+Fitness
- Gitex Global 2023
- Best Of Bollywood
- Special Features
- Investing in the Future
- Know Plan Go
- Gratuity Calculator
- Notifications
- Prayer Times
UAE after the rains: Latest road status, travel updates and more
Uae weather.
- Environment
Take a look at the latest weather updates and advisories from across the UAE
Heavy rain lashed the UAE on Thursday morning, but cloud cover has since significantly receded. The National Centre of Meteorology (NCM) says the unstable weather was caused by an extension of low pressure from the Red Sea, along with humid south-easterly winds, which caused rain clouds to migrate from Saudi Arabia towards the UAE. Will it rain on Friday? NCM expert explains what to expect over the weekend.
Here are the latest updates from across the UAE.
Taking E16 from Dubai to Hatta? Check this update
In response to a commuter's inquiry, the RTA advised that the E16 bus route from Dubai to Hatta is currently suspended.
Here are your alternative options:
- Take bus route H02 from Dubai Mall to Hatta Bus Station.
- For a smoother journey, planning your trip in advance is recommended. You can do this using: The S'hail app
- The RTA journey planner on their website.
This information is according to the RTA.
Abu Dhabi replants trees damaged by recent weather
Abu Dhabi City Municipality replanted trees affected by recent weather and maintained public and recreational facilities.
Abu Dhabi: Al Mina Street reopens to Corniche Street exit
Abu Dhabi Police announce Al Mina Street reopened towards Corniche Street exit via Sheikh Zayed Tunnel. Drive safely!
Dubai marine services resume rormal operations after rain
Dubai's Roads and Transport Authority (RTA) announces that marine services are back to normal operations following a day of heavy rains across the country. Read more
Abu Dhabi Police announce traffic diversion
Abu Dhabi Police have announced a traffic diversion from Al Mina Street to Corniche Street exit via Sheikh Zayed Tunnel, following a day of heavy rains that lashed different parts of the country.
Intercity buses are fully operational
Dubai’s Roads, and Transport Authority (RTA) posted on X that Intercity Bus services are back to normal after it was temporarily suspended due to the adverse weather conditions .
DXB returns to normal operations
Dubai International Airport (DXB) has returned to normal operations this afternoon, following disruptions caused by unsettled weather.
Dubai's beaches, parks reopen
As Dubai swiftly rebounded from recent weather fluctuations, public beaches, dubai public parks, and markets affiliated with Dubai Municipality are open again.
In a post on X, the municipality said "Dubai's beaches, public parks and markets managed by Dubai Municipality are reopening to welcome you according to ther regular working hours."
Reminder: Extended Dubai Metro timings
To facilitate travel to and from Dubai International Airport, the Roads and Transport Authority (RTA) has extended Dubai Metro operating hours today, Thursday, May 2nd. Trains will run from midnight 12am until 5am the following morning.
Follow safety instructions to prevent vehicle fires
Dubai Police urge drivers to adhere to safety guidelines to lower the chances of vehicle fires, particularly in waterlogged areas.
Ras Al Khaimah road collapse
Ras Al Khaimah: Emirates Road heading to the Al Shuhadaa (Martyrs) Street exit in Ras Al Khaimah caved in on Thursday afternoon following heavy rains .
RTA enhances safety measures
Due to the current unstable weather conditions in Dubai, RTA is stepping up its efforts to ensure your safety on the roads.
Look: Traffic flow resumes in Abu Dhabi
In pictures: Abu Dhabi reports normal traffic flow following rainfall in the emirate.
Dubai ferry services temporarily suspended
RTA announces temporary disruptions to Dubai Ferry routes due to UAE weather conditions. See list of affected routes below.
➡ Al Ghubaiba - Marina Mall (in both directions)
➡ Dubai Water Canal - Al Ghubaiba (in both directions)
➡Dubai Water Canal - Bluewaters (in both directions)
➡Bluewaters - Marina Mall (in both directions)
➡Al Ghubaiba - Sharjah Aquarium (in both directions)
Watch: Ajman beefs up patrols during heavy rain
Ajman Police have intensified their presence on various internal and external roads of the emirate, to deal with the heavy rains and provide assistance to the public.
Sharjah suspends intercity bus services
Sharjah announces the temporary suspension of its intercity bus service, due to the prevailing unstable weather conditions. Sharjah's RTA has informed the public that updates on the service resumption will be communicated through official channels.
Dubai suspends buses to other emirates
The Roads and Transport Authority (RTA) of Dubai has suspended intercity bus services to Abu Dhabi, Sharjah, Ajman, and other emirates.
On Guard 24/7: Dubai Police ensure safety
Watch : Dubai's dedicated police officers, armed with diverse expertise, are committed to around-the-clock public safety.
Dubai-Sharjah bus service temporarily suspended
The Roads and Transport Authority (RTA) of Dubai announced the temporary suspension of intercity bus services between Dubai and Sharjah on Thursday due to the heavy rain brought on by the weather situation.
Dubai Metro operating in both directions now: RTA
Dubai Metro is operating on the Red line in both directions without stopping at the following stations: ONPASSIVE, Equiti, Al Marsheq and Energy.
Speed limits back to normal on key roads
Abu Dhabi Police have stated that speed limits on Abu Dhabi's external roads are back to normal.
Ajman Police ensure smooth traffic flow
The Ajman Police General Command has prepared all resources to manage the event, ensuring the safety of lives and the smooth flow of traffic on the roads. This ensures readiness to face challenges and swift recovery from any consequences.
Residents advised to avoid beaches and valleys
Ajman Police urge the public to exercise caution and vigilance during rainfall. Stay away from areas with accumulated water, beaches, valleys, and torrents.
Dubai Airports cancels 13 flights
Dubai International Airport (DXB) confirmed a total of 13 flights were cancelled Thursday morning. Moreover, five inbound flights were diverted overnight. Passengers departing from Dubai's airports have been advised to allocate additional time for their journey to the airport, as road congestion may be anticipated.
Look: Dubai tackles rain impact
Dubai authorities deployed teams from the Municipality, RTA, and Police to minimise rain disruptions on city streets. Images show their efforts in action. Read more
RTA suspends intercity bus services until further notice
Intercity bus services between Dubai have been suspended until further notice due to unstable weather conditions, Dubai’s Roads and Transport Authority (RTA) has announced on X. RTA advised commuters to follow social media channels for further updates regarding the service resumption.
Plan ahead: Travel advisory issued
Air Arabia advises passengers flying from Abu Dhabi, Sharjah, and Ras Al Khaimah to plan for additional travel time to the airport due to weather conditions. The airline also recommends updating contact information in bookings to receive the latest flight updates.
Several Dubai flights cancelled amid heavy rainfall
Adverse weather conditions across the UAE are impacting flights to and from Dubai on May 2. Passengers can expect delays, diversions, and cancellations.
Emirates Airlines has announced reduced flight operations at Dubai Airport due to the weather. Passengers flying into or out of Dubai on May 2nd should be prepared for potential delays and rescheduling. The following Emirates flights have been cancelled for May 2:
EK 123/124: Dubai - Istanbul
EK 763/764: Dubai - Johannesburg
EK 719/720: Dubai - Nairobi
EK 921/922: Dubai - Cairo
EK 903/904: Dubai - Amman
EK 352/353: Dubai - Singapore (EK353 departs May 3rd at 12:50 AM)
UAE urges caution: Follow safety instructions
The National Center of Emergency Management and Crisis (NCEMA) encourages the public to strictly follow all instructions and guidelines issued by relevant authorities for the safety of lives and property.
Watch: Waterlogging hits Abu Dhabi streets after heavy rainfall
See: Waterlogging on the streets in some parts of Abu Dhabi as rains hit the UAE. Heavy rain and thunderstorms hit Abu Dhabi early on Thursday morning.
Dubai Police issue guidelines
Dubai Police issued guidelines, stating: "Let's work together to ensure everyone's safety during rainy weather conditions by following the necessary guidelines on the road, at work, and at home."
Sharjah medical fitness centers closed today
The Sharjah City Municipality announces the closure of medical fitness centers on Thursday, May 2, due to the weather conditions, out of its concern for the safety of the public.
Watch: Cloudy skies over Dubai this morning
Heavy cloud cover greeted parts of Dubai on Thursday morning. The NCM issued an amber alert across the country, indicating rain-bearing clouds had covered most areas.
Drivers alert: Jebel Ali hit by strong morning winds
Jebel Ali experienced strong winds early Thursday morning. Expect occasional strong winds, especially near cloud formations, which could cause reduce visibility on roads. The NCM warns motorists driving during this time to be cautious of reduced visibility.
Watch: Heavy rains and strong winds hit Sharjah early today
Rta prepares for unstable weather: issues safety tips.
The Dubai Roads and Transport Authority (RTA) is prepared to handle upcoming weather conditions and maintain smooth traffic flow. In a recent post on X, the RTA urged drivers to "adhere to the guidelines while driving your vehicle during the prevailing weather" for everyone's safety. They have also shared additional safety tips on their website for your reference.
Flying from Sharjah? Check early arrival times
Sharjah Airport advises travellers to arrive at the airport 3 hours before their departure time due to weather conditions and to check with the airline companies on their flight updates.
Watch out for revised speed limits on Abu Dhabi roads
1. Sheikh Tahnoon Bin Mohammed Road: Speed Limit Reduced to 100 km/h on Sheikh Tahnoon Bin Mohammed Road (Al Saja - Masakin).
2. Abu Dhabi - Al Ain Road: Speed Limit Reduced to 100 km/h on Abu Dhabi - Al Ain Road (Complex Bridges - Al Wathbah).
3. Sheikh Zayed Bin Sultan Road: New 100 km/h Speed Limit on Sheikh Zayed Bin Sultan Road Sheikh Zayed Bridge - Al Bahyah).
4. Sheikh Khalifa Bin Zayed Road: Sheikh Khalifa Bin Zayed Road Speed Change: New Limit 100 km/h (Yas - Al Saadiyat).
5. Al Khaleej Al Arabi Road : Speed Limit Reduced to 100 km/h on Al Khaleej Al Arabi Road (Musaffah Bridge - Abu Dhabi).
6. Abu Dhabi-Al Ain Road: Speed Limit Reduced to 100 Km/h on Abu Dhabi-Al Ain Road (Al Mahawi - Al Sad)
Distance learning
Following an advisory by the National Emergency, Crisis and Disaster Management Authority (NCEMA), schools and colleges will be implementing distance learning today and tomorrow.
Work from home advised
Both government and private organisations have been urged to consider remote work. This, however, will not apply to those who are required to be physically present at work or be involved in potential response and recovery efforts.
Airport advisory
Dubai International (DXB) and Al Maktoum International Airport (DWC), have urged passengers to avoid delays due to possible road congestion, utilise smart apps for real-time traffic updates and consider using theDubai Metro. Emirates also advised passengers with travel plans today to arrive early. flydubai also advised passengers to allow extra time for their journey to DXB.
Dubai Metro timings extended
Dubai Metro operating hours have been extended from 12am to 5am. Trains will depart from Centrepoint Metro Station and will only stop at Emirates Metro Station, Airport Terminal 1, Airport Terminal 3 and GGICO stations.
Police advisory for bikers
Abu Dhabi Police have called upon delivery bike riders to avoid riding in volatile weather conditions.Police has called on delivery bicycle drivers to commit to the need to stop transportation and delivery services during volatile weather conditions.
Residents alerted
Dubai Municipality, Dubai Electricity and Water Authority (Dewa) and other departments have alerted residents about various precautionary measures they should take amid unstable weather conditions. The Ministry of Energy and Infrastructure has shared its preparedness measures in ensuring the safety of infrastructure, roads and dams.
More From Weather

More rain in UAE? What to expect over weekend

Why rains have ceased to be fun anymore

Rain in UAE: Cloud cover decreases in Abu Dhabi, Dubai

In pictures: Rain, thundershowers across the UAE
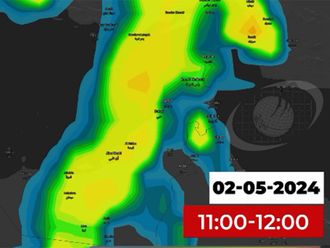
Rain in UAE: NCM video shows what to expect

New bus station next to Al Qusais’ Metro station

Unstable weather conditions end, UAE confirms

Revealed: Reasons behind 4,391 road accidents in UAE

RTA resumes marine transport, intercity bus operations
Saudi arabia issues alert for heavy rain this week, 70 fall ill with vomiting in mauritius-frankfurt flight, from near paralysis, to running for those who can’t, 'the crown' inspires new series of gandhi's early life, last 2 days of global village – longer hours announced.

Get Breaking News Alerts From Gulf News
We’ll send you latest news updates through the day. You can manage them any time by clicking on the notification icon.
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
The CDC says maternal mortality rates in the U.S. got better, after a pandemic spike

Selena Simmons-Duffin

After an alarming spike in 2021, maternal mortality numbers the next year went back down, according to a report released Thursday. CDC Director Mandy Cohen says the rates are still too high. Rich Legg/Getty Images hide caption
After an alarming spike in 2021, maternal mortality numbers the next year went back down, according to a report released Thursday. CDC Director Mandy Cohen says the rates are still too high.
After spiking in 2021, the maternal mortality rate in the U.S. improved significantly the following year, according to a new report from the Centers for Disease Control and Prevention.
The data shows that 817 women died of maternal causes in the U.S. in 2022, compared to 1,205 in 2021. These are deaths that take place during pregnancy or within 42 days following delivery, according to the World Health Organization , "from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes."
"I think that the bump [in 2021] reflects the pandemic and we're returning to pre-pandemic levels," says study author Donna Hoyert, who a health scientist at the CDC's National Center for Health Statistics.
The maternal mortality rate in 2022 was 22.3 deaths per 100,000 live births. That's a significant decrease from the 2021 rate of 32.9, but it's still much higher than the rate in other wealthy countries.
There continue to be enormous racial disparities in the U.S. maternal mortality rate as well – the rate for Black women was 49.5 deaths per 100,000 births in 2022, compared to a rate of 19 deaths for white women. Research shows the vast majority of these deaths are preventable .
Dr. Veronica Gillispie-Bell is an OB-GYN in New Orleans who was not involved in the CDC report. She agrees that COVID-19 was likely the reason for the major spike in maternal mortality.
"I really think that 2021 was actually an outlier because of the circumstances," Gillispie-Bell says. "We know that because of COVID-19, there were disruptions to care that obviously impacted our ability to care for pregnant individuals, plus there were pregnant individuals who were dying from COVID." It's hard to know for certain since the CDC report did not include cause of death, she adds.
She's encouraged that the 2022 numbers are slightly lower than 2020 – 817 in 2022 versus 861 in 2020. "It could mean that we're moving in the right direction – I think we need more years of data to know," she says.
CDC's newest data comes several weeks after an academic study cast doubt on the agency's methodology, suggesting that a pregnancy checkbox on death certificates was causing the numbers to be much higher than they are in reality. CDC strongly rejected the study's findings.
Hoyert also defends CDC's methodology. "There was plenty of literature before we made the changes that we were underestimating [maternal deaths] without a checkbox, and so we did add the checkbox," she says, explaining that they have continued to do evaluations and issue guidance to ensure it's being used correctly.
"I think CDC is doing great work in collecting the data and sharing that back," CDC Director Mandy Cohen told NPR last month. "We disagree with how that study was looking at it, and think it's unacceptable for moms to be dying at that rate here in the United States."
The stakes for getting these numbers right are high in a post- Roe America. Reproductive health advocates warn that abortion bans threaten women's lives, and if CDC's data is not viewed as reliable by the public, that could make it hard to evaluate the impact of these restrictions.
In a statement about CDC's latest report, Dr. Verda Hicks, president of the American College of Obstetricians and Gynecologists, connected the maternal mortality figures to "the worsening state of reproductive health care since the Dobbs decision."
"When treating pregnancy complications, abortion care can be lifesaving, and withholding that care unquestionably compromises patient lives and outcomes," Hicks wrote.
Despite the challenges with the data, Dr. Gillispie-Bell says the public should still put a "great bit of stock" into CDC's analysis. She also pointed to the work of state maternal mortality review committees around the country – she is the medical director of the committee in Louisiana. They are supported and funded by CDC.
"The first step for our maternal mortality review committee – once we get the death certificate with that pregnancy checkbox – is to then start extracting data to confirm ... so our numbers are very accurate," she says.
Not all states have these committees validating maternal deaths and making recommendations to reduce their numbers. CDC Director Cohen pointed out the agency now has funding available for each state. She also pointed out that CDC's data has already led to policy changes to reduce maternal deaths, including allowing Medicaid coverage to continue for a year postpartum .
"I think we're making strides, which is great," Cohen added. "We have more work to do."
- Centers for Disease Control and Prevention
- reproductive health
- maternal mortality

IMAGES
VIDEO
COMMENTS
In most cases, pregnant women can travel safely until close to their due dates. But travel may not be recommended if you have pregnancy complications.If you are planning a trip, talk with your obstetrician-gynecologist (ob-gyn).And no matter how you choose to travel, think ahead about your comfort and safety.
Pregnant travelers should avoid travel to areas with malaria, as it can be more severe in pregnant women. Malaria increases the risk for serious pregnancy problems, including premature birth, miscarriage, and stillbirth. If you must travel to an area with malaria, talk to your doctor about taking malaria prevention medicine.
Guidelines for vaccinating pregnant women. Atlanta: The Centers; 2014. Available from: ... Air travel and pregnancy outcomes: a review of pregnancy regulations and outcomes for passengers, flight attendants, and aviators. Obstet Gynecol Surv. 2010;65(6):396-402. Rasmussen SA, Jamieson DJ, Honein MA, Petersen LR. Zika virus and birth defects ...
Follow general safety guidelines. These commonsense travel tips will help keep you healthy and safe when you travel. ... Cruise ships typically have some restrictions on pregnancy travel, so be ...
Virgin Australia. No restrictions. Travel permitted; requires a medical certificate dated within 10 days of departure date once you reach 28 weeks. For flights longer than four hours, travel is not permitted after 36 weeks of pregnancy (32 weeks if pregnant with multiples), or within 48 hours of normal vaginal delivery.
Share. Travel During Pregnancy offers clear and useful guidance for your pregnant patients. This resource covers: Give your patients this easy reference to help them travel safely and comfortably while pregnant. Published: 2023. This ACOG patient education pamphlet explains how to safely travel during pregnancy.
Travel During Pregnancy. As long as there are no identified complications or concerns with your pregnancy, it is generally safe to travel during your pregnancy. The ideal time to travel during pregnancy is the second trimester. In most cases, you are past the morning sickness of the first trimester and several weeks from the third stage of ...
Generally, air travel before 36 weeks of pregnancy is considered safe for people who aren't dealing with any pregnancy problems. Still, if you're pregnant, it's a good idea to talk with your health care provider before you fly. Your provider might suggest that you not fly if you have certain pregnancy complications that could get worse because ...
Stand up and stretch. Pregnant women are at higher risk for developing blood clots, so it's important to avoid sitting still for long periods of time. Wear loose clothes and keep the blood flowing in your legs: Whether you're flying or driving, take breaks to get up, walk around and stretch every half hour or so.
Wear well-fitted compression stockings when traveling during pregnancy. Stay hydrated by drinking plenty of water. Avoid drinking caffeinated beverages and alcohol, as these can lead to dehydration. If possible, try to exercise or walk every 30 minutes. If you're traveling by car, arrange rest breaks and take short walks.
Some women prefer not to travel in the first 12 weeks of pregnancy because of nausea and vomiting and feeling very tired during these early stages. The risk of miscarriage is also higher in the first 3 months, whether you're travelling or not. Travelling in the final months of pregnancy can be tiring and uncomfortable.
Ask your airline if they have a cut-off time for traveling during pregnancy. You can fly on most airlines up to 36 weeks of pregnancy. But if you're flying out of the country, the cut-off time may be earlier. Check to see what medical care your health insurance covers. Health insurance helps you pay for medical care.
If you're taking a long road trip or getting on an airplane, try to do some stretching at least every two hours. Pregnancy increases your risk for blood clots, but moving around helps keep your blood flowing normally. If you're on a plane, compression stockings can help keep blood from pooling in your legs. Make sure you add plenty of down ...
Do not travel to areas with a Zika outbreak (red areas on the Zika map ). Before travel to other areas with risk of Zika (purple areas on the Zika map), pregnant women should talk with their doctors and carefully consider risks and possible consequences of travel. If you must travel to these areas, talk to your doctor first and strictly follow ...
Pregnancy is a precaution for YF vaccine administration, compared with most other live vaccines, which are contraindicated in pregnancy. If travel is unavoidable, and the risks for YFV exposure are felt to outweigh the vaccination risks, a pregnant woman should be vaccinated.
Travelling while pregnant. Find useful information and considerations to help you prepare for safe and healthy travels outside Canada while pregnant. With careful preparation, travelling while pregnant can be safe. The decision to travel should be made in consultation with your health care professional, based on your personal health circumstances.
Travel Tips: Pregnant Travelers. All screening equipment at the airport security checkpoint is safe for all travelers, including women who are pregnant. Watch this travel tips video if you have questions about the security screening process when traveling while pregnant. Select Filter.
When you are pregnant, the safest time to fly is: Before 37 weeks, if you are carrying one baby. From 37 weeks of pregnancy you could go into labour at any time, which is why many women choose not to fly after this time. Before 32 weeks, if you are carrying an uncomplicated twin pregnancy.
Air travel during pregnancy was associated with neglectable effects on gestational age (39+0 ±1.6 weeks in air travel group vs 39+1 ±1.7 weeks in control group, p-value <0.0001) and weight at birth (3263 ±477 grams in air travel group vs 3269±492 grams in control group, p-value = 0.01) (see Table A in S1 Appendix).
Compression socks. "During pregnancy, you are at an increased risk of developing a blood clot," Louise says. "That's why compression socks, hydration, and movement—walking, stretching ...
Learn how infections can complicate pregnancy and may have serious consequences for a woman, her pregnancy outcomes, and her baby. Read stories from real pregnancy and find peace of mind in knowing your baby will have a healthy start. Learn steps to take, before, during, and after pregnancy or when trying to avoid getting pregnant.
Air Travel and Pregnancy. This is the third edition of this paper, which was published in 2001 and 2005 under the title 'Advice on Preventing Deep Vein Thrombosis (DVT) for Pregnant Women Travelling by Air'. 1. Background. Obstetricians are commonly asked to give advice on whether it is suitable for women who are pregnant to fly during ...
Pregnancy. MMR vaccines should not be administered to pregnant people or people attempting to become pregnant. Because of the theoretical risk to the fetus, people should be counseled to avoid becoming pregnant for 28 days after receiving a live-virus (e.g., MMR) vaccine. Precautions Personal or Family History of Seizures of Any Etiology
Guidelines for the Pregnant Workers Fairness Act detail accommodations pregnant workers can seek under the law, including for abortion care. ... But the cost of that travel and threat of lost ...
Twenty-one states ban abortion or restrict the procedure earlier in pregnancy than the standard set by Roe v. Wade, which governed reproductive rights for nearly half a century until the Supreme ...
On April 15, 2024, the Equal Employment Opportunity Commission (EEOC) published a final rule to implement the Pregnant Workers Fairness Act (PWFA) (the "Rule"). By way of background, the PWFA requires covered employers to provide reasonable accommodations to employees with known limitations related to, affected by, or arising out of pregnancy, childbirth, or related medical conditions ...
Florida has been a major access point for abortion in the South. Now its residents, along with thousands more in the region, will have to seek abortion care elsewhere after six weeks of pregnancy.
Dubai Police issued guidelines, stating: "Let's work together to ensure everyone's safety during rainy weather conditions by following the necessary guidelines on the road, at work, and at home ...
The maternal mortality rate in the U.S. in 2022 - while still high - went back to where it was before deaths surged during the height of the COVID-19 pandemic, according to the latest CDC report.