Blog / 2023 Physician Work RVU Increases Finalized by Medicare
The 2023 Medicare Physician Fee Schedule Final Rule was released on November 1, 2022. The final rule includes CPT code changes recommended by the American Medical Association (AMA). The changes are numerous and vary in type, but the result is an overall increase in work Relative Value Units (RVUs) for nearly all physicians who provide evaluation and management (E&M) services in hospitals and nursing facilities .

2023 Inpatient E&M Code Changes
The Medicare Physician Fee Schedule Final Rule (2023 Final Rule) includes both increases and decreases in work RVU values for E&M services provided in hospital and nursing facility settings. Generally, the most used billing codes (99232, 99233, 99308, and 99309) within this subset are all going to realize double digit increases in work RVUs.
Table 1: Proposed 2023 E&M Code Updates
Source: Comparison of 2023 Final Rule to RVU22C
The work RVU changes in the 2023 Final Rule are more complex than those in the 2021 Final Rule. The 2021 Final Rule only increased work RVUs for seven outpatient services codes. Forecasting the 2023 Final Rule accurately requires crosswalking many deleted codes with substitute codes. The AMA and Medicare have deleted hospital observation E&M procedure codes and merged those services into the codes for hospital inpatient E&M services. Visit codes for E&M services in assisted living and custodial care facilities are also being consolidated into the general home visit service codes.
Table 2: 2023 Deleted Codes & Substitutes
Source: AMA CPT Evaluation and Management Code and Guideline Changes
2023 Overall Medicare Work RVU Impact by Specialty
LBMC calculated the overall work RVU impact of the 2023 Final Rule changes by specialty by applying the new work RVU values to the billing data contained in the public 2019 Medicare Provider Utilization and Payment data set.
This analysis indicates that hospitalists, infectious disease physicians, geriatricians, PM&R, hematologists, psychiatrists, internists, palliative care, and other specialists who practice in hospital and nursing facilities will realize the most increases in work RVUs from the 2023 Final Rule changes. Advanced Practice Providers (APPs) specializing in geriatrics, acute medicine, mental health, and other facility-based specialties are similarly affected.
When combined with the 2021 outpatient E&M changes, dozens of specialties will realize double-digit increases in work RVUs.
Table 3: Estimated Overall Changes in Work RVUs by Specialty
Note: Overall wRVU % change by specialty does not reflect the skewed impact within specialties. Disclaimer: No estimate is made for changes in existing coding patterns other than substitutes.
Highly Variable Work RVU Impacts within Specialties
The overall work RVU increases projected in the previous section do not reflect the expected variation in work RVU changes among physicians within each specialty. The 2023 Final Rule includes both increases and decreases in work RVUs among the CPT codes affected. The severity and complexity of patient illnesses varies from physician-to-physician within each specialty. The proportion of E&M services provided in hospitals, offices, and nursing facilities can also vary substantially within specialties like hospital medicine, psychiatry , and geriatrics .
For example, the table below summarizes the separate and combined changes for the 2021 Final Rule and 2023 Final Rule. The percentage changes from 2020 to 2021 in the left-most column illustrate the distribution of work RVU increases exclusively for outpatient E&M services. The percentage changes from 2022 to 2023 in the center column illustrate the distribution of work RVU increases exclusively for inpatient E&M services. The percentage changes in the right-most column illustrate the combined effects of both the 2021 and 2023 rules. Predictably, the sample of 13,529 hospitalists analyzed in the following table were not impacted by the 2021 outpatient E&M work RVU changes at all. The variation of inpatient E&M service severity and coding among these hospitalists yields a wide range of estimated effects from 2% decreases in work RVUs at the 10 th percentile to 15% increases in work RVUs at the 90 th percentile.
Table 4: Estimated Work RVU Change Variability within Hospital Medicine (n=13,529)
Disclaimer: No estimate is made for changes in existing coding patterns other than substitutes
Forecasts estimate about half of physicians practicing Geriatric Medicine will realize increases in work RVUs during 2023 as a result of E&M updates for both inpatient and nursing facility services. When combined with the prior outpatient E&M changes from 2021, nearly all geriatricians are forecast to experience work RVU increases from 2020 to 2023.
Table 5: Estimated Work RVU Change Variability within Geriatric Medicine (n=3,013)
Adapting to changes in work rvu production, compensation & reimbursement.
On a combined basis, the 2023 Final Rule and the 2021 Final Rule materially change the Resource-Based Relative Value System on which physician reimbursement, productivity, and compensation is built. Commercial insurance carriers will not emulate Medicare’s changes in their own reimbursement systems overnight. Accordingly, an added level of thoughtfulness is required when using industry compensation and production surveys to set physician compensation. Employers of specialists that were unaffected by the 2021 Final Rule may find that they are materially affected by the 2023 Final Rule.
The path forward begins with identifying the financial impact of the 2021 and 2023 work RVU changes on production, compensation, and reimbursement for your healthcare professionals. Once the financial impact is known, the various options of partially or fully adopting the new production system changes can be assessed within your budgetary resources and restrictions.
LBMC Advisory Services has a team of experts exclusively dedicated to physician compensation analysis, planning, strategy and valuation. Contact LBMC today for assistance with productivity and compensation forecasts, scenario analyses, compensation planning, and questions regarding the impact of the 2023 Final Rule on Fair Market Value compensation analysis.
LBMC’s Nick Newsad recently discussed how the 2023 Medicare Physician Fee Schedule Rule will affect physician productivity measurement, compensation, and reimbursement during a webinar on August 4, 2022. Watch the webinar On-Demand: https://www.lbmc.com/blog/webinar-new-physician-work-rvu-increases/
Nicholas A. Newsad, MHSA works in the Advisory Services Group at LBMC. He can be contacted at [email protected] or 615-309-2489.
We’re happy to answer any questions you may have on what our experts can do for you. Please send us an email using the form and one of our professionals will get back to you promptly.
Privacy Overview

How the E/M code RVU increases could affect family physicians’ pay
The work relative value units (RVUs) for office-based E/M codes 99202-99215 increased on Jan. 1 as part of the 2021 Medicare Physician Fee Schedule. (See the new values in the table below.) The increased values were part of a broader effort to reform E/M coding and reduce the documentation burden .
How the increased RVUs will affect family physicians depends on several factors, including their payer contracts and their compensation model.
For Medicare, total RVUs (comprised of work, practice expense, and malpractice RVUs) are multiplied by the year’s conversion factor ($34.89 for 2021) to determine the payment allowance for each code. Overall, Medicare payments for family physicians are expected to increase more than 10% due to the E/M revaluation and other changes.
For private payers, the Medicare physician fee schedule often forms the basis of their own fee schedules, but they may use a prior year’s fee schedule or pay only a negotiated percentage of the Medicare physician fee schedule. If private payers do not automatically adjust their fees based on the updated RVUs, physicians may need to renegotiate these contracts. Physicians in solo and independent practice should check with their private payers on this issue. (See “ Questions to Ask Private Payers .”)
For employed physicians, compensation usually takes the form of a base salary supplemented with an incentive/productivity bonus based on factors such as work RVUs, collections, and quality. If RVUs make up a significant portion of your compensation formula, talk to your administrator about how the increased values for office visit E/M codes will affect your pay and whether productivity targets will change. (See “ Talking Points for Employed Physicians .”)
Read about additional payment and coding changes in the full article in FPM : “ The 2021 Medicare Payment and CPT Coding Update .”
- Chronic care
- Medicare/Medicaid
- Physician compensation
- Practice management
- Reimbursement
- Value-based payment
Other Blogs
- Quick Tips from FPM journal
- AFP Community Blog
- Fresh Perspectives
- In the Trenches
- Leader Voices
- RSS ( About RSS )
Disclaimer: The opinions and views expressed here are those of the authors and do not necessarily represent or reflect the opinions and views of the American Academy of Family Physicians. This blog is not intended to provide medical, financial, or legal advice. Some payers may not agree with the advice given. This is not a substitute for current CPT and ICD-9 manuals and payer policies. All comments are moderated and will be removed if they violate our Terms of Use .
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- Echocardiography CPT Codes and RVU
In this article we will outline the CPT Codes for Echocardiography and also the associated Echocardiography work RVU’s also known as Echocardiography wRVU’s.
Transthoracic echocardiogram with Doppler – CPT code, work RVU, wRVU Transthoracic echocardiogram without Doppler – CPT code, work RVU, wRVU Transthoracic echocardiogram Rest and Stress – CPT code, work RVU, wRVU Transthoracic echo Rest and Stress with EKG – CPT code, work RVU, wRVU Transesophageal echocardiogram – CPT code, work RVU, wRVU Transesophageal echo with Doppler – CPT code, work RVU, wRVU Transesophageal echo with Color – CPT code, work RVU, wRVU Transesophageal echo with Color & Doppler – CPT code, work RVU, wRVU Transthoracic echocardiogram with Doppler CPT code 93306 Transthoracic echocardiogram with Doppler Work RVU 1.3
Transthoracic echocardiogram without Doppler CPT code 93307 Transthoracic echocardiogram without Doppler Work RVU 0.92
Transthoracic echocardiogram Rest and Stress CPT code 93350 Transthoracic echocardiogram Rest and Stress Work RVU 1.46
Transthoracic echo Rest and Stress with EKG CPT code 93351 Transthoracic echo Rest and Stress with EKG Work RVU 1.75
Transesophageal echocardiogram CPT code 93312 Transesophageal echocardiogram Work RVU 2.2
Transesophageal echo with Doppler CPT code 93312, +93320 Transesophageal echo with Doppler Work RVU 2.2, + 0.38
Transesophageal echo with Color CPT code 93312, +93325 Transesophageal echo with Color Work RVU 2.2, + 0.07
Transesophageal echo with Color & Doppler CPT code 93312, +93325, +93320 Transesophageal echo with Color & Doppler Work RVU 2.2, + 0.07, +0.38
- Cardiology Coding Center
- Combined Right and Left Heart Catheterization CPT Codes and RVU
- Coronary Intervention CPT Codes and RVU
- Left Heart Catheterization CPT Codes and RVU
- Left Heart Catheterization Miscellaneous CPT Codes and RVU
- Right Heart Catheterization CPT Codes and RVU
- Structural Heart Intervention CPT Codes and RVU
- Coronary Artery Imaging CPT Codes and RVU
- 99233 CPT Code, Level 3 Hospital Followup Note –Dummies Guide 2017-2018
- 99232 CPT Code, Level 2 Hospital Followup Note –Dummies Guide 2017-2018
Optimizing RVU Production In An Academic Medicine Practice
- Post author By James Allen, MD
- Post date June 8, 2019

The work RVU is the current medium of exchange in clinical practice for all physicians, both private and academic. And as the numbers of physicians employed by academic medical centers swells at the same time as the percentage of these physicians’ time dedicated to clinical practice grows, academic physicians in particular are under increasing pressure to maximize their RVU output. Consequently, many academic physicians find themselves struggling to produce their required numbers of RVUs. Historically, private practices were built around efficient RVU productivity but academic practices were not and consequently, the academic inpatient and outpatient practice environment and practice culture is not conducive to RVU maximization . Failure to meet annual RVU targets can result in loss of bonuses, salary reduction, career disillusionment, and general unhappiness. On the other hand, consistently meeting or exceeding RVU targets can provide job security and the freedom to chart one’s own career path in academic medicine. Here are some of the ways that academic physicians can optimize their RVU production.


In The Inpatient Setting:
- Don’t forget to submit your bill for your clinical services. This seems so simple but a few years ago, I did an analysis at our own hospital and found that 7% of inpatient services and procedures that were documented in the electronic medical record went unbilled. This was not because of a conspiracy by the physicians, it was simply because they forgot to enter a charge for a given day’s clinical work. It is easy to forget to submit a bill (often called the “charge capture” application in an electronic medical record). If you are busy trying to save a patient’s life, the lowest priority in your day is to put in a bill for that service. I consider myself pretty compulsive when it comes to billing and even I found times when I forgot to enter a bill for a consult, a return hospital visit, or a bedside procedure. Two strategies can help minimize forgotten charges: (1) work with your electronic medical record to create charge entry prompts when completing progress notes or procedure notes to make entering those charges easier and (2) develop a personal strategy to ensure that all services are billed each day – I print out a rounding list of all of my patients each day and note my E/M service & procedure charge on each patient as I enter charges; at the end of the day, I can take a quick look at the printout to confirm that every patient had a charge entered.
- Don’t avoid submitting a bill for your service. A number of years ago, one of our very best clinical educators stopped signing resident inpatient notes and inpatient charges. The excuse was that there just wasn’t enough time in the work day and it got in the way of bedside teaching. No note meant no bill for service. No bill meant no income. No income meant no job.
- Don’t under bill. Most large academic medical practices do billing audits by billing compliance personnel. These audits are largely defensive, designed to prevent over billing. This is because large medical practices (and particularly academic practices) are subject to billing audits by Medicare or other insurance companies. The bias from compliance audits is that it is better to err on the side of under billing than over billing. Over billing jeopardizes the organization but under billing jeopardizes the individual physician by making him/her do more work than is necessary to meet annual wRVU targets.

- There should be no such thing as a curbside consult. The curbside consult is when an admitting physician (or more likely a resident) asks an “off-the-record” clinical question of a consultant. There is no entry into the medical record by the consultant and there is no bill generated. If a consultant’s expert opinion is sought, that consultant should be paid for it. I was once an expert witness in defense of a university medical center. One of the residents had called a pathologist to ask an opinion about an inpatient case and made the mistake of documenting that conversation (and the pathologist’s name) in the medical record. The pathologist was named as a co-defendant in the malpractice suit. Even an off the record opinion can result in legal liability so you should bill for your expertise and opinion.
- Don’t sign-off too quickly. For many consulting physicians in academic practice, a major goal of the workday is getting the consult census list shortened as much as possible. Consult follow-up visits are beneficial to patient and the primary service because the consultant’s expertise can be applied to new test results and changes in the patient’s condition. This can reduce inpatient hospital length of stay. Those follow up inpatient encounters do not pay as much as initial consult encounters but they often take very little time and on a per-hour basis can generate more RVUs per hour than initial consults. Most initial inpatient consults require at least 2-3 follow-up visits and many will require daily follow-up visits until the patient is discharged. In academic practice, there is a strong tradition of being a “one and done” when it comes to consults. For a consultant, those follow-up visits take far less time than a follow-up visit by the admitting service (hospitalist, etc.) so you can perform a lot of follow-up visits in an hour. I believe that this is the #1 low-hanging fruit in academic medicine for increased wRVU generation .

- Mundane tasks generate a lot of wRVUs but can melt your brain. EKGs and pulmonary function tests are commonly performed in large medical centers. On an individual basis, neither generates very many work RVUs. However, they take very little time to interpret and document and consequently, the cardiologist or pulmonologist can generate huge numbers of wRVUs very quickly. The problem is that reading PFTs and EKGs is boring and are often seen as an unpleasant necessity of specialty practice. My brain would melt if the only thing I did all day was read PFTs but by reading them for an hour or two a week, I can generate enough wRVUs to free me up to do the uncompensated things that I really like to do.

- Make your EMR work for you. Investing a little time developing disease-specific note templates, order sets, and order preference lists can pay enormous long-term benefits by creating time-saving shortcuts in your electronic medical record charting. I have different new consult templates for the inpatient conditions that I most commonly encounter: COPD exacerbations, pneumonia, asthma exacerbations, abnormal chest x-ray, pulmonary embolism, etc. I incorporate my own self-designed “smart lists” into the physical exam portion of my notes that default to the expected findings; for example, for an asthma consult note, the lung exam smart list defaults to “diffuse wheezing” whereas the pulmonary embolism consult lung exam smart list defaults to “normal breath sounds bilaterally”. This allows me to rapidly click through the physical exam and saves me precious keystrokes when creating my consult note. Copying and pasting can also shorten your documentation time but it can be hazardous if you are copying too much data from a previous day’s progress note because of the danger of importing out-of-date information (like vital signs, lab results, NPO status, etc.). By using templates for notes that automatically import new data into the daily note, you can avoid this. I limit my copying/pasting to just my “impression and plan” list so that I can remember what problems I am actively following and what my previous day’s recommendations were – I then edit the impression and plan as appropriate.

- You will get more efficient producing RVUs with age. There is a Starling curve of physician productivity. It takes about 7 years after finishing residency or fellowship to get proficient in getting clinical work done. Not only do physicians continue to learn new knowledge but they get more efficient in getting their daily work done with everything from history taking to progress note writing. For most physicians, productivity peaks in their mid-50’s. After that, they often start dialing back the amount of time they spend in clinical practice.
In The Outpatient Setting:
- Pre-chart your patient encounters. Each outpatient encounter will require a certain amount of time in the patient exam room and a certain amount of time outside of the exam room. You can either finish your charting at the end of the day, after the patient leaves or you can do that additional charting before the patient arrives in the clinic. Either way, it will be the same amount of time – either before clinic or after clinic. But by pre-charting and preparing for the patient’s visit, you can often shorten the amount of time spent during actual clinic hours – this can free you up to spend more time communicating with individual patients and allow you to see more patients in a given period of time.
- Utilize CPT code 99358. This code is for “prolonged service without patient contact”. It requires documentation that you spent at least 31 minutes doing the service and I primarily use it (1) when reviewing a lot of medical records in advance of a new outpatient consult or (2) after an initial consult when I receive a lot of requested records and radiographic images. In my own practice, most new outpatients come with lots of chest x-ray & CT images that I need to review and interpret, office notes that I need to review, lab results I need to review, and pulmonary function tests that I need to review and interpret. About half of my new patients have > 31 minutes of records to be reviewed and documented. This CPT code is worth 2.10 wRVUs and when combined with a level 5 new outpatient visit (3.17 wRVUs), you can generate a whopping 5.27 wRVUs (7.91 total RVUs) for that visit. I use this code 2-3 times a week. Also, if that new patient does not show up, I still am able to generate some wRVUs for my efforts.
- Utilize the other CPT codes that you forgot to bill. The common ones are 99497 (advanced care planning, 30 minutes: 1.50 wRVUs), 99406 (smoking cessation 3-10 minutes: 0.24 wRVUs), 99495 (transition care management, moderate complexity: 2.11 wRVUs), and 99354 (prolonged services > 30 minutes: 2.33 wRVUs). I wrote about these and other often-overlooked CPT codes in a previous post .
- Cultivate a referral base. For specialists, new patients can come from self-referrals, emergency department referrals, or physician referrals. Self-referrals and ER referrals are notorious for being no-shows and for having no insurance (or having Medicaid). You are better off filling your schedule with referrals from primary care providers and other specialists because those patients are more likely to show up for their scheduled appointment and generally constitute a better payer mix. The best way to cultivate those referrals is by human contact, either introducing yourself in person or by the occasional phone call. Those referral physicians will remember your name the next time they need a consult if they have shaken your hand or heard your voice. This is especially true for nurse practitioner or physician assistant primary care practices – NPs and PAs don’t have the same opportunities to network with specialists at medical staff meetings, the hospital’s physician lounge, or CME events. A phone call to a primary care NP can endear you to him/her for life. Referral letters are also a good way to cultivate referrals. Each referral letter is an advertisement opportunity for your practice: a poorly constructed letter that consists of 4 pages of electronic medical record documentation will create animosity but a 1-paragraph readable note in prose form will create goodwill.
- Make the outpatient EMR work for you. Reducing keystrokes saves you time that you can spend seeing more patients and generating more wRVUs. Just as in the inpatient setting, by creating note templates for common conditions that you use, you can reduce your documentation time; in my pulmonary practice, I have different templates for COPD, interstitial lung disease, asthma, abnormal x-ray, and bronchiectasis office notes. Pre-designed order preferences and smart lists can streamline your practice. Outpatient EMR optimization is a huge topic and I’ll devote a post just to this in the future.

- Convert patient phone calls into wRVUs. There are two ways to do this: get the patient into the office or use the new CPT code for telephone/EMR encounters. CPT code G2012 is for phone or EMR patient encounters that last 5-10 minutes for patients that are not seen for 7 days before or 24 hours after the phone/EMR encounter. It pays 0.25 wRVUs. The other strategy is to get those patients into the office – either at the end of the day or to fill in holes in the office schedule created by late cancelations. Alternatively, keep a open 15 or 30 minutes at the end of the day for add-on sick visits. I prescribe way too much steroids/antibiotics over the phone for COPD exacerbations, etc. that could at least be billed as a G2012.

- Use the entire day. I often see physicians start their morning schedule at 9:00 even though the nurses and registration staff all arrive at 7:30. Similarly, I see physicians schedule their last patient at 3:30 or 4:00 even though the staff are paid to be there until 5:30. Time = wRVUs. Be sure to fill the entire day’s clinic time with patients.
- Double book strategically. In my practice, there are almost always late cancelations and no-shows. By double booking a couple of slots in expectation of those cancelations and no-shows, you can ensure that the schedule stays full. I often see physicians double book at the beginning of their schedule – I think this is hazardous because if both patients show up, then the physician is behind the schedule for hours, creating exasperation for the physician and dissatisfaction for the patients. I think you are better off double booking a slot in the middle of the morning (or afternoon) and at the end of the day. this is because there are inevitably patients who show up 30 or 45 minutes early for their appointments so if there is a late cancelation, you can slip an early arriver into that slot, thus creating an opening in the middle of the afternoon (or morning) or at the end of the day that the double booked patient can fill.
- Make up canceled clinics. There should not be an expectation for making up clinics canceled for vacations and scheduled CME time off. However, in academic practice, there are always things that come up that conflict with the regular clinic times: academic retreats, medical staff meetings, visiting lecturers, new faculty candidate interviews, medical student lectures, etc. These activities fall under “academic time” (release time) and when those conflict with regular clinic time, necessitating canceling that afternoon’s clinic, then a make-up clinic should be scheduled. If your academic time temporarily displaces your usual clinic time then you should have an equal displacement of your usual academic time by make-up clinic time in order to keep your total weekly academic:clinic time ratio constant.
- Do point of care testing. For me, this means having an office spirometer (0.17 wRVUs per test). For others, it may mean an INR machine, an EKG machine, or a hemoglobin A1C machine. In order to determine if you need a piece of equipment to do point of care outpatient testing, you have to do a pro forma that compares the cost of the equipment to the estimated income generated by that piece of equipment. It takes about 44 spirometry tests to pay for the cost of a spirometer, after that, all of the income generated by spirometry is profit.
- Partner with advanced practice providers. Everyone wants an NP/PA/LISW/pharmacist in order to make their practice more efficient and generate more wRVUs. But everyone also wants someone else to pay for that NP/PA/LISW/pharmacist. In a healthy clinical environment, the physician should work synergistically with advanced practice providers so that the total RVU productivity is greater than the sum of what that physician & advanced practice provider could generate operating individually. Examples are a physician assistant who does the post-op office visits so that the surgeon can do more surgeries or a nurse practitioner who sees routine follow-up heart failure visits so that the cardiologist can see more new patient consults that in turn lead to more cardiac stress tests and echos.
June 8, 2019
By James Allen, MD
I am a Professor Emeritus of Internal Medicine at the Ohio State University and former Medical Director of Ohio State University East Hospital

- Revenue Cycle Management
- Reimbursement
- Diabetes Awareness Month
- Risk Management
- Patient Retention
- Medical Economics® 100th Anniversary
- Coding and documentation
- Business of Endocrinology
- Physicians Financial News
- Cybersecurity
- Cardiovascular Clinical Consult
- Locum Tenens, brought to you by LocumLife®
- Weight Management
- Business of Women's Health
- Practice Efficiency
- Finance and Wealth
- Remote Patient Monitoring
- Sponsored Webinars
- Medical Technology
- Billing and collections
- Acute Pain Management
- Exclusive Content
- Value-based Care
- Business of Pediatrics
- Concierge Medicine 2.0 by Castle Connolly Private Health Partners
- Practice Growth
- Concierge Medicine
- Business of Cardiology
- Implementing the Topcon Ocular Telehealth Platform
- Malpractice
- Sexual Health
- Chronic Conditions
- Legal and Policy
- Practice Management
- Patient Relations
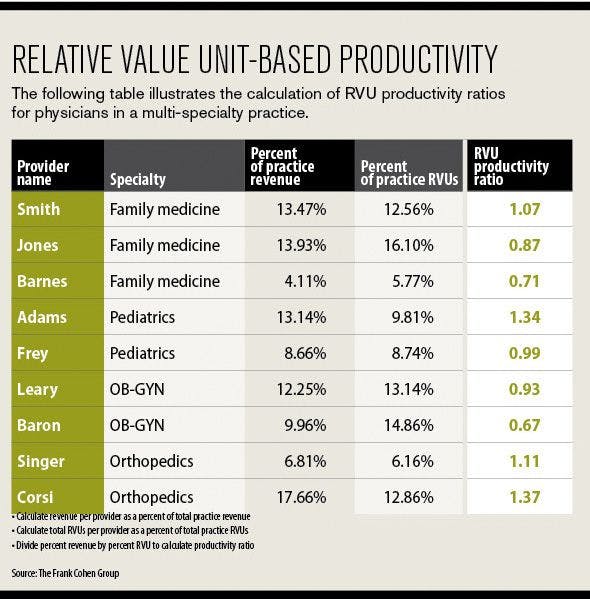
RVUs: A valuable tool for aiding practice management
Understanding the basics of the RVU can assist physicians and practice managers in a wide variety of finance and management-related tasks.
When it comes to managing practice finances , physicians have few better tools at their disposal than the Relative Value Unit (RVU). RVUs can be used for everything from helping to determine compensation in a multi-physician practice to deciding whether to take a buyout offer from a hospital system .
How AI threatens the privacy of patient health data

The FTC’s noncompete rule is a concerning development for physicians

Is too much regulation stifling health care innovation?
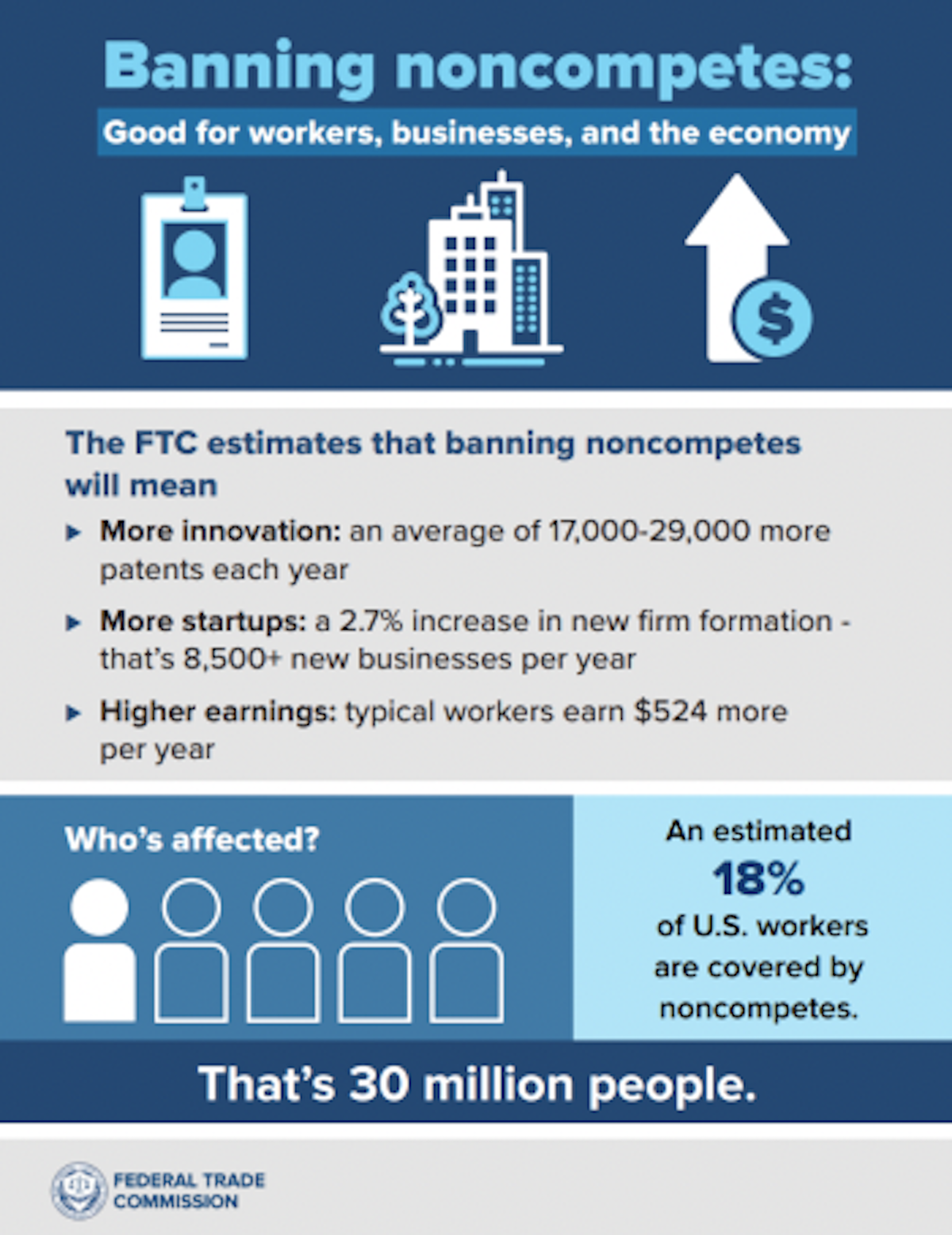
FTC votes to ban noncompete clauses for all but high-level execs
ACP renews call for physicians to vote, make health care an issue for presidential election year
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps
2022 Physician Fee Schedule: What You Need to Know About Ablation Services
Acc news story.
As part of the proposed 2022 Medicare Physician Fee Schedule , the Centers for Medicare and Medicaid Services (CMS) is proposing reduced work RVUs for EP ablation services.
Through its ongoing review of potentially misvalued services, the American Medical Association (AMA) Relative Value-Scale Update Committee (RUC) in 2019 flagged EP ablation services for scrutiny because of significant growth in volume. While the growth in services is appropriate and reflects evolving patterns of care in the past decade, it also reflects changes in performance of the services themselves. When the current codes and descriptors were written in 2011, 3D mapping, left-atrial pacing, and ICE were not typically performed with the underlying ablations. However, with new technology and clinical practices, these services are now nearly universally performed with SVT and/or AFib ablations.
As such, while the CPT® code numbers remain the same for these services, two of the five codes underwent significant revisions of code descriptors to incorporate (bundle) related services. These revisions would also translate to the add-on codes for additional ablations. Starting in 2022, these components will not be separately reportable.
The revised code descriptors are shown below, with bolded phrases showing the newly bundled work.
93653: Comprehensive electrophysiologic evaluation with insertion and repositioning of multiple electrode catheters, induction or attempted induction of an arrhythmia with right atrial pacing and recording, and catheter ablation of arrhythmogenic focus, including intracardiac electrophysiologic 3-dimensional mapping , right ventricular pacing and recording, left atrial pacing and recording from coronary sinus or left atrium , and His bundle recording, when performed treatment of supraventricular tachycardia by ablation of fast or slow atrioventricular pathway, accessory atrioventricular connection, cavo-tricuspid isthmus or other single atrial focus or source of atrial re-entry
93564: Comprehensive electrophysiologic evaluation with insertion and repositioning of multiple electrode catheters, induction or attempted induction of an arrhythmia with right atrial pacing and recording, and catheter ablation of arrhythmogenic focus, including intracardiac electrophysiologic 3-dimensional mapping, right ventricular pacing and recording, left atrial pacing and recording from coronary sinus or left atrium, and His bundle recording, when performed; with treatment of ventricular tachycardia or focus of ventricular ectopy including left ventricular pacing and recording, when performed
93655: Intracardiac catheter ablation of a discrete mechanism of arrhythmia which is distinct from the primary ablated mechanism, including repeat diagnostic maneuvers, to treat a spontaneous or induced arrhythmia (List separately in addition to code for primary procedure)
93656: Comprehensive electrophysiologic evaluation including transseptal catheterizations, insertion and repositioning of multiple electrode catheters with intracardiac catheter ablation of atrial fibrillation by pulmonary vein isolation, including intracardiac electrophysiologic 3-dimensional mapping, intracardiac echocardiography including imaging supervision and interpretation , induction or attempted induction of an arrhythmia including left or right atrial pacing/recording, right ventricular pacing/recording, and His bundle recording, when performed
93657: Additional linear or focal intracardiac catheter ablation of the left or right atrium for treatment of atrial fibrillation remaining after completion of pulmonary vein isolation (List separately in addition to code for primary procedure)
Time is a key factor in fee-for-service RVU rate setting. Physician work surveys executed by the ACC and Heart Rhythm Society (HRS) in the fall of 2020 for the RUC demonstrated notable reductions in procedure times. The reductions in time were significant for the bundled codes. Additional surveys were launched by ACC and HRS in the winter of 2021 to check the accuracy of the first. Those surveys also showed significant reductions in procedure times.
Shorter procedure times are likely due to a variety of factors, including improved systems that offer more detailed and accurate anatomical and electrical activation mapping, often completely eliminating the need for fluoroscopy. Catheter technology has also advanced, providing real-time assessment of the quality of contact between the catheter tip and the endocardial tissue. Additionally, 3-D mapping systems that function in concert with new catheter technology now provide real-time assessment of the quality of the radiofrequency ablation lesion formation, allowing shorter duration of each radiofrequency application while also improving the quality of the lesions delivered.
Because additional surveys were underway for the April RUC meeting to check the accuracy of the January surveys to resolve any flaws from the initial survey, such as survey respondents probably not realizing that a new descriptor includes services is now bundled to the existing CPT code (and not a newly issued CPT code), CMS proposes to maintain the current work RVUs of SVT code 93653 and AF code 93656 until the AMA RUC returns with a more definitive and accurate valuation based on feedback from additional surveys conducted this past spring to to ensure survey participants understand that a new descriptor includes services now bundled to the existing CPT code (and not a newly issued CPT code). As written, this would represent a reduction commensurate with the RVUs for the newly-bundled add-on services. The Agency also disagreed with the RUC-recommended values for the two add-on codes, 93655 and 93657, proposing to further reduce those. Additional refinement and possible reductions are possible as part of the final 2022 rulemaking.
ACC and HRS staff and member leaders continue to share information, questions, and concerns with AMA and CMS staff working on the physician fee schedule to ensure proposals are clearly understood and informed by the best available information. After two rounds of work RVU surveys completed by ACC and HRS members, some reduction in RVUs reflecting decreased effort and complexity is likely to be finalized. A table showing these differences are displayed below. The ACC will submit formal comments to CMS on this topic in September. Members can also share their insights or concerns about how reduced work RVUs would impact patients directly to the agency here .
Ablation Coding Format
Clinical Topics: Arrhythmias and Clinical EP, Noninvasive Imaging, EP Basic Science, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Echocardiography/Ultrasound, Nuclear Imaging
Keywords: ACC Advocacy, Atrial Fibrillation, Centers for Medicare and Medicaid Services, U.S., Pulmonary Veins, Ventricular Premature Complexes, Cardiac Catheters, Coronary Sinus, Relative Value Scales, Current Procedural Terminology, Fee-for-Service Plans, American Medical Association, Bundle of His, Drug Repositioning, Medicare, Heart Atria, Catheter Ablation, Tachycardia, Supraventricular, Tachycardia, Ventricular, Echocardiography, Fluoroscopy, Catheterization, Health Policy
You must be logged in to save to your library.
Jacc journals on acc.org.
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Email: [email protected]
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- ACC.org Quick Start Guide
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.

IMAGES
VIDEO
COMMENTS
Work, practice expense and liability relative value units (RVUs) are updated annually through Medicare Physician Fee Schedule rulemaking. In response to the recently finalized 2023 Medicare Physician Fee Schedule and related addenda, the ACC developed a new Physician Fee Schedule Calculator.This tool allows clinicians and practice managers to estimate the impacts of the slated changes to ...
Coding Corner: Overview of 2024 Coding Changes Impacting Cardiology ACC 2024 Medicare Physician Fee Schedule Final Rule Calculator Now Available Coding Solutions For Renal Denervation. Appropriate Use of Modifier 25 Compliance. Appeals; Audit Programs; Coverage; Fraud and Abuse; Provider Enrollment;
Code 99204 generates 2.43 work RVUs while 99495 generates 2.11 work RVUs, at roughly the same payment rate, so 99204 would have higher production.". To create your list of RVUs for common codes ...
Budget neutrality adjustment required by law to account RVU increases of E/M codes CY 2021 conversion factor is $32.41 decrease of $3.68 from CY2020 CMS estimates that the physician rule will increase payments to cardiologists by 1% from 2020 to 2021 Estimate is based on the entire cardiology profession and can vary widely depending on the mix
The Medicare Physician Fee Schedule Final Rule (2023 Final Rule) includes both increases and decreases in work RVU values for E&M services provided in hospital and nursing facility settings. Generally, the most used billing codes (99232, 99233, 99308, and 99309) within this subset are all going to realize double digit increases in work RVUs.
In response to the recently finalized 2021 Medicare Physician Fee Schedule and related addenda, the ACC developed a new Physician Fee Schedule Calculator. This tool allows clinicians and practice managers to estimate the impacts of the slated changes to practices. Over time, the goal of the tool is to help facilitate a thorough understanding of ...
The ACC has created a Physician Fee Schedule Calculator that allows clinicians and practice managers to estimate the practice impact of changes included in the 2023 Medicare Physician Fee Schedule proposed rule and related addenda. Over time, the goal of the tool is to help facilitate a thorough understanding of impacts from one year to the next.
RVU stands for relative value unit. It is a value assigned by CMS to certain CPT ® and HCPCS Level II codes to represent the cost of providing a service. An RVU is made up of three components: physician work, practice expense, and malpractice. Medicare payments are determined by RVUs multiplied by a monetary conversion factor and a geographic ...
Work, practice expense and liability relative value units (RVUs) are updated annually through Medicare physician fee schedule rulemaking. In response to the recently finalized 2021 Medicare Physician Fee Schedule and related addenda, the ACC developed a new Physician Fee Schedule Calculator.This tool allows clinicians and practice managers to estimate the impacts of the slated changes to ...
Next, complete the following calculations: Work RVUs per session ÷ Visits per session = Work RVUs per visit. 16.88 ÷ 10 = 1.69. Workdays per year x Visits per day = Visits per year. 220 x 20 ...
A. A. A. The Centers for Medicare and Medicaid Services (CMS) on Nov. 2 released the 2022 Medicare Physician Fee Schedule (PFS) final rule, addressing Medicare payment and quality provisions for physicians in the next fiscal year. Under the rule, the conversion factor will decrease by $1.30 on Jan. 1, 2022, going from $34.89 to $33.59.
RVU. 2. 2024 facility PE RVU. 2. 2 2024 malpractice RVU. 2. 2024 total facility RVU 2024 non-facility PE RVU. 2. 2 2024 total non-facility RVU . Insertion of permanent transvenous defibrillator system 33249 Insertion or replacement of permanent implantable defibrillator system, with transvenous lead(s), single or dual chamber 14.92 8.53 3.40 26 ...
Impella CPT code and Impella work RVU / Impella wRVU. Impella Insertion CPT Code 33390. Impella Insertion Work RVU 12.92. Impella Repositioning CPT Code 33393. Impella Repositioning Work RVU 5.49. Impella Removal CPT Code 33392. Impella Removal Work RVU 6.23.
The work relative value units (RVUs) for office-based E/M codes 99202-99215 increased on Jan. 1 as part of the 2021 Medicare Physician Fee Schedule. (See the new values in the table below.)
Transthoracic echocardiogram without Doppler Work RVU 0.92. Transthoracic echocardiogram Rest and Stress CPT code 93350. Transthoracic echocardiogram Rest and Stress Work RVU 1.46. Transthoracic echo Rest and Stress with EKG CPT code 93351. Transthoracic echo Rest and Stress with EKG Work RVU 1.75. Transesophageal echocardiogram CPT code 93312.
Work, practice, expense and liability relative value units (RVUs) are updated annually through the Centers for Medicare and Medicaid Services' Medicare Physician Fee Schedule rulemaking. ... Clinical Topics: Geriatric Cardiology. Keywords: Costs and Cost Analysis, Physicians, Fee Schedules, Medicare, Centers for Medicare and Medicaid Services ...
The work RVU is the current medium of exchange in clinical practice for all physicians, both private and academic. ... the cardiologist or pulmonologist can generate huge numbers of wRVUs very quickly. ... and when combined with a level 5 new outpatient visit (3.17 wRVUs), you can generate a whopping 5.27 wRVUs (7.91 total RVUs) for that visit ...
When the corresponding GPCI adjustments of a locality are applied to the three RVU types, total RVUs for a procedure can vary significantly. For example, for the first quarter of 2024, Medicare assigns 22.89 total RVUs for both facility and nonfacility sites to CPT ® code 24341 Repair, tendon or muscle, upper arm or elbow, each tendon or muscle, primary or secondary (excludes rotator cuff).
Work, practice expense and liability relative value units (RVUs) are updated annually through Medicare physician fee schedule rulemaking. ACC's Physician Fee Schedule Calculator allows clinicians and practice managers to estimate the practice impact of changes included in the proposed 2021 Medicare Physician Fee Schedule and related addenda.Over time, the goal of the tool is to facilitate a ...
What are RVUs? RVUs are part of the system Medicare uses to decide how much it will reimburse physicians for each of the 9,000-plus services and procedures covered under its Physician Fee Schedule, and which are assigned current procedural terminology (CPT) code numbers. The dollar amount for each service is determined by three components: physician's work, practice expenses, and malpractice ...
These changes only apply to the office E/M codes and include an increase in values. Some changes include: ... (MDM) or total time personally spent by the reporting practitioner on the day of the visit (includes face-to-face and non-face-to-face ... 2020 Work RVU: 2021 Work RVU: 2021 Day of Encounter Time Range Selection: 2021 Typical Total Time ...
other words, each RVU is composed of 3 parts: wRVU (for physician compensation) + Practice expense RVU + Malpractice RVU. Example: for a new office visit, Medicare will pay the practice 4.6 RVUs which will be allocated as follows. 2.43 wRVU for physician, 1.98 practice RVU for the hospital or facility and 0.2 RVU for malpractice expenses.
As part of the proposed 2022 Medicare Physician Fee Schedule, the Centers for Medicare and Medicaid Services (CMS) is proposing reduced work RVUs for EP ablation services.. Through its ongoing review of potentially misvalued services, the American Medical Association (AMA) Relative Value-Scale Update Committee (RUC) in 2019 flagged EP ablation services for scrutiny because of significant ...