- Patient Portal
- Classes and Events
- Find a Doctor
- Schedule Appointment


The Role of a Midwife in Maternity Care
In the world of maternity care , a group of health care professionals often work quietly in the background, providing crucial support and care to expectant parents. These unsung heroes are midwives, and their role is often misunderstood or underestimated. What is a midwife, and what responsibilities do midwives have to birthing parents and the child before, during and after childbirth?

What is a Midwife?
A midwife is a trained health care professional specializing in childbirth and reproductive health. They are distinct from obstetricians, as their approach emphasizes a more natural and holistic perspective on pregnancy and childbirth . Midwives provide care before, during, and after pregnancy, offering services that promote maternal and fetal well-being.
What Role Do Midwives Play in Prenatal Care?
One of the fundamental roles of midwives is to provide prenatal care , such as regular checkups and monitoring throughout pregnancy to ensure the health and well-being of the birthing parent and the developing baby. These checkups include physical exams, ultrasound scans and blood tests to track the progress of the pregnancy.
“Prenatal care provided by midwives focuses on building a strong and supportive relationship with the birthing parent,” said Waverly Lutz, CNM, midwife at Inspira Medical Group’s Gentle Beginnings. “They aim to educate and empower patients to make informed choices about their pregnancy and birthing experience.”
How Do Midwives Support Labor and Delivery?
Midwives play a pivotal role during labor and delivery . They provide emotional support, pain management techniques and guidance during this intense and transformative process. While midwives are skilled in managing uncomplicated births, they are trained to recognize and respond to possible complications.
“Midwives advocate for a patient-centered approach, ensuring the birthing experience aligns with the birthing parent’s preferences and values,” said Lutz. “But they are also well-prepared to safely handle emergencies and collaborate with obstetricians when necessary.”
What Postpartum Care Do Midwives Provide?
The care midwives provide doesn't end with the baby's birth. They continue to provide support throughout the postpartum period, offering guidance on breastfeeding, postpartum recovery and emotional well-being. This ongoing care is essential for the health and bonding of both parent and child.
What Else Do Midwives Do?
Midwives play a crucial role in advocating for the birthing parent’s rights and choices in childbirth. They promote informed decision-making and work to ensure that parents have the autonomy to choose the type of birth experience they desire, whether it's a home birth, hospital birth or birthing center experience.
They also provide comprehensive wellness care, including preventive gynecological exams, pap tests, birth control counseling, sexual health advice, and overall reproductive well-being, regardless of pregnancy intent.
“Empowering patients to make choices that align with their values is at the core of midwifery care,” Lutz emphasized. “They believe every parent should have access to safe and respectful maternity care that honors her preferences and cultural beliefs.”
To learn more about Inspira’s approach to midwifery, visit our website or to make an appointment, call 888-31-BIRTH
News From Inspira

New mother was concerned about a potentially serious complication, but the care team at Inspira...

In celebration of National Breastfeeding Awareness Month, Inspira Health hosted a special Tea and...

Ensure your baby's safety and wellbeing with simple steps from Inspira Health. Learn how to reduce...
Appointments at Mayo Clinic
- Pregnancy week by week
Prenatal care: 1st trimester visits
Pregnancy and prenatal care go hand in hand. During the first trimester, prenatal care includes blood tests, a physical exam, conversations about lifestyle and more.
Prenatal care is an important part of a healthy pregnancy. Whether you choose a family physician, obstetrician, midwife or group prenatal care, here's what to expect during the first few prenatal appointments.
The 1st visit
When you find out you're pregnant, make your first prenatal appointment. Set aside time for the first visit to go over your medical history and talk about any risk factors for pregnancy problems that you may have.
Medical history
Your health care provider might ask about:
- Your menstrual cycle, gynecological history and any past pregnancies
- Your personal and family medical history
- Exposure to anything that could be toxic
- Medications you take, including prescription and over-the-counter medications, vitamins or supplements
- Your lifestyle, including your use of tobacco, alcohol, caffeine and recreational drugs
- Travel to areas where malaria, tuberculosis, Zika virus, mpox — also called monkeypox — or other infectious diseases are common
Share information about sensitive issues, such as domestic abuse or past drug use, too. This will help your health care provider take the best care of you — and your baby.
Your due date is not a prediction of when you will have your baby. It's simply the date that you will be 40 weeks pregnant. Few people give birth on their due dates. Still, establishing your due date — or estimated date of delivery — is important. It allows your health care provider to monitor your baby's growth and the progress of your pregnancy. Your due date also helps with scheduling tests and procedures, so they are done at the right time.
To estimate your due date, your health care provider will use the date your last period started, add seven days and count back three months. The due date will be about 40 weeks from the first day of your last period. Your health care provider can use a fetal ultrasound to help confirm the date. Typically, if the due date calculated with your last period and the due date calculated with an early ultrasound differ by more than seven days, the ultrasound is used to set the due date.
Physical exam
To find out how much weight you need to gain for a healthy pregnancy, your health care provider will measure your weight and height and calculate your body mass index.
Your health care provider might do a physical exam, including a breast exam and a pelvic exam. You might need a Pap test, depending on how long it's been since your last Pap test. Depending on your situation, you may need exams of your heart, lungs and thyroid.
At your first prenatal visit, blood tests might be done to:
- Check your blood type. This includes your Rh status. Rh factor is an inherited trait that refers to a protein found on the surface of red blood cells. Your pregnancy might need special care if you're Rh negative and your baby's father is Rh positive.
- Measure your hemoglobin. Hemoglobin is an iron-rich protein found in red blood cells that allows the cells to carry oxygen from your lungs to other parts of your body. Hemoglobin also carries carbon dioxide from other parts of your body to your lungs so that it can be exhaled. Low hemoglobin or a low level of red blood cells is a sign of anemia. Anemia can make you feel very tired, and it may affect your pregnancy.
- Check immunity to certain infections. This typically includes rubella and chickenpox (varicella) — unless proof of vaccination or natural immunity is documented in your medical history.
- Detect exposure to other infections. Your health care provider will suggest blood tests to detect infections such as hepatitis B, syphilis, gonorrhea, chlamydia and HIV , the virus that causes AIDS . A urine sample might also be tested for signs of a bladder or urinary tract infection.
Tests for fetal concerns
Prenatal tests can provide valuable information about your baby's health. Your health care provider will typically offer a variety of prenatal genetic screening tests. They may include ultrasound or blood tests to check for certain fetal genetic problems, such as Down syndrome.
Lifestyle issues
Your health care provider might discuss the importance of nutrition and prenatal vitamins. Ask about exercise, sex, dental care, vaccinations and travel during pregnancy, as well as other lifestyle issues. You might also talk about your work environment and the use of medications during pregnancy. If you smoke, ask your health care provider for suggestions to help you quit.
Discomforts of pregnancy
You might notice changes in your body early in your pregnancy. Your breasts might be tender and swollen. Nausea with or without vomiting (morning sickness) is also common. Talk to your health care provider if your morning sickness is severe.
Other 1st trimester visits
Your next prenatal visits — often scheduled about every four weeks during the first trimester — might be shorter than the first. Near the end of the first trimester — by about 12 to 14 weeks of pregnancy — you might be able to hear your baby's heartbeat with a small device, called a Doppler, that bounces sound waves off your baby's heart. Your health care provider may offer a first trimester ultrasound, too.
Your prenatal appointments are an ideal time to discuss questions you have. During your first visit, find out how to reach your health care team between appointments in case concerns come up. Knowing help is available can offer peace of mind.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Lockwood CJ, et al. Prenatal care: Initial assessment. https://www.uptodate.com/contents/search. Accessed July 9, 2018.
- Prenatal care and tests. Office on Women's Health. https://www.womenshealth.gov/pregnancy/youre-pregnant-now-what/prenatal-care-and-tests. Accessed July 9, 2018.
- Cunningham FG, et al., eds. Prenatal care. In: Williams Obstetrics. 25th ed. New York, N.Y.: McGraw-Hill Education; 2018. https://www.accessmedicine.mhmedical.com. Accessed July 9, 2018.
- Lockwood CJ, et al. Prenatal care: Second and third trimesters. https://www.uptodate.com/contents/search. Accessed July 9, 2018.
- WHO recommendations on antenatal care for a positive pregnancy experience. World Health Organization. http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/anc-positive-pregnancy-experience/en/. Accessed July 9, 2018.
- Bastian LA, et al. Clinical manifestations and early diagnosis of pregnancy. https://www.uptodate.com/contents/search. Accessed July 9, 2018.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 1st trimester pregnancy
- Can birth control pills cause birth defects?
- Fetal development: The 1st trimester
- Implantation bleeding
- Nausea during pregnancy
- Pregnancy due date calculator
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Prenatal care 1st trimester visits
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Trying to Conceive
- Signs & Symptoms
- Pregnancy Tests
- Fertility Testing
- Fertility Treatment
- Weeks & Trimesters
- Staying Healthy
- Preparing for Baby
- Complications & Concerns
- Pregnancy Loss
- Breastfeeding
- School-Aged Kids
- Raising Kids
- Personal Stories
- Everyday Wellness
- Safety & First Aid
- Immunizations
- Food & Nutrition
- Active Play
- Pregnancy Products
- Nursery & Sleep Products
- Nursing & Feeding Products
- Clothing & Accessories
- Toys & Gifts
- Ovulation Calculator
- Pregnancy Due Date Calculator
- How to Talk About Postpartum Depression
- Editorial Process
- Meet Our Review Board
Your Prenatal Care Appointments
If you're pregnant, especially if it's for the first time, you may be wondering what will happen at your prenatal care appointments with your doctor or midwife . Here's a rundown of everything you can expect at each appointment, including tests and exams.
Your First Prenatal Care Appointment
Your first prenatal appointment will probably be your longest one. Here you will give your doctor, midwife, or nurse your complete health and pregnancy history. This information is important because it will give your practitioner a good idea of how healthy you are and what type of problems you are most likely to experience during your pregnancy. You will learn what your estimated due date is as well.
There are many areas that may be checked during your physical exam, including:
- Blood pressure
- Breast exam
- Pelvic exam
- Pregnancy test
- Ultrasound (if you're having pain or bleeding or underwent fertility treatments)
- Urine screen for protein and sugar
You will probably be seen for your first appointment between 8 and 10 weeks gestation, though you may be seen earlier if you're having problems or if it's your doctor or midwife's policy.
Your Second Appointment
Your second prenatal appointment usually takes place about a month after your first appointment, unless you're having problems or need specific prenatal testing that is best performed in a specific time range. Here is what will most likely happen during this visit:
- Blood pressure check
- Listen to a fetal heartbeat using a Doppler
- Record your weight
- Urine screen for sugar and protein
Your baby's first heartbeat can usually be heard with a Doppler between 8 and 12 weeks gestation. If you have trouble hearing the baby's heartbeat, you will probably be asked to wait until your next visit when your baby is a bit bigger. Sometimes an ultrasound will be ordered as well.
Additional Testing
Additional testing may be performed at this appointment as needed. There are some optional tests you, your doctor, or your midwife may request:
- Chorionic villus sampling (CVS) (diagnostic test for many genetic diseases)
- Early amniocentesis (diagnostic test for many genetic diseases)
- Nuchal fold test (screening for Down syndrome)
Be sure to discuss all of your options regarding these tests, including the risks and benefits, how the test results are given, and whether the test is a screening test or a diagnostic test.
Your Third Appointment
Towards the third prenatal visit, you're most likely around 14 to 16 weeks pregnant. You're probably feeling better and the most dangerous part of pregnancy is over. You are now probably feeling more confident in your pregnancy and sharing your good news .
It has been about a month since you've seen the midwife or doctor. Here's what this appointment may look like:
- Check your blood pressure
- Listen for baby's heartbeat
- Measure your abdomen, called "fundal height," to check baby's growth
- Urine sample to screen for sugar and protein
Optional Testing
You may also have the following prenatal testing done if you request it:
- Amniocentesis (diagnostic test for many genetic diseases)
- Neural tube defect (NTD)/Down syndrome screening by way of maternal blood work (several tests can be used including alpha-fetoprotein (AFP), triple screen, and quad screen)
Your Fourth Appointment
You are most likely between 16 to 20 weeks at this point, and it has been about a month since your last appointment. You probably feel like you've grown a lot since your last appointment and you may now be wearing maternity clothes and possibly even feeling your baby move . Here's what this visit may involve:
- Measure your fundal height to check baby's growth
You may also have a mid-pregnancy ultrasound screening if you request it or if it's your doctor or midwife's policy.
Your Fifth Appointment
Between 18 to 22 weeks you'll likely have your fifth prenatal care visit. Here's what this appointment may involve:
- Check for swelling in your hands and feet
- Listen to the baby's heartbeat
Your Sixth Appointment
Your next prenatal care appointment will likely be between 22 to 26 weeks of pregnancy . You are probably still being seen monthly. Here's what this appointment may look like:
- Listen to the baby's heartbeat
- Measure your fundal height to check baby's growth
- Questions about baby's movements
Your Seventh or Eighth Appointment
Between 26 to 28 weeks of pregnancy , you'll likely have another prenatal care appointment. Here's what may happen:
- Check blood pressure
- Questions about baby's movements
Other Testing and Information
You may have other tests or procedures ordered, like the glucose tolerance test (GTT) used to screen for gestational diabetes or the RhoGam , shot around 28 weeks of gestation for women who are Rh-negative. Your doctor or midwife may also give you information on screening for preterm labor on your own.
Your Eighth, Ninth Appointments and Beyond
Your next appointment will likely be between 28 to 36 weeks of pregnancy. In fact, you're likely to have at least two prenatal visits during this period because you're now being seen every other week. Here's what these appointments may involve:
- Palpate to check baby's position (vertex, breech, posterior, etc.)
Screening for Group B strep (GBS) will normally be done between weeks 34 to 36. This involves rectal and vaginal swab. You will continue to be seen every other week until about the 36th week of pregnancy. At this point, your visits will likely be fairly routine with very few extra tests being performed.
Weekly Visits
Between 36 to 40 weeks of pregnancy, you're usually seen every week. Here's what these visits may entail:
You will continue to be seen every week until about the 41st week of pregnancy, at which point you may be seen every few days until your baby is born. Your visits are most likely fairly routine, with very few extra tests being performed.
You may also have an ultrasound to determine what position the baby is in at this point. Your doctor will also try to predict the size of your baby , but this is usually not very accurate. Because of this tendency for inaccuracy, it's not a great idea to have an induction of labor based on the predicted size of your baby.
If you're having a home birth , you may have a home visit during this time frame if your midwife doesn't do her normal prenatal visits there. You will be able to give her a tour of your home and answer questions she may have about where everything is located.
Overdue Pregnancy Visits
At 40 or 41 weeks of pregnancy, you may begin to see your midwife or doctor every few days. Here is what these visits may look like:
Since you are officially past your due date, your midwife or doctor may want to watch you and your baby more carefully until labor begins. This may include the following tests:
- Non-stress test (NST)
- Biophysical profile (BPP)
These tests will help determine if your practitioner needs to intervene with an induction of labor for the health of your baby or let your pregnancy continue.
National Institute of Child Health and Human Development. What Happens During Prenatal Visits ?
National Institute of Child Health and Human Development. What are some common complications of pregnancy ?
American College of Obstetricians and Gynecologists. How Your Fetus Grows During Pregnancy .
Mayo Clinic Staff. Prenatal Care: 1st Trimester Visits . Mayo Clinic.
By Robin Elise Weiss, PhD, MPH Robin Elise Weiss, PhD, MPH is a professor, author, childbirth and postpartum educator, certified doula, and lactation counselor.
Ready Steady Baby
Home visits.
You should be visited several times by your midwife or family nurse at home during the first 10 days. Friends and family will want to visit to meet your baby too.
It’s OK to ask visitors to:
- call you first and to sometimes say no
- help with other things so you can have a rest or spend time with your baby
Extra support
Some new parents need more support than others. You’ll get extra support from your midwife, family nurse or other health professionals if your baby:
- was born early
- spent time in special or intensive care
- has additional needs
Tests and checks
During the first 10 days your midwife will:
- weigh your baby
- do a newborn blood spot test if you agree
You’ll also need to register your baby with a GP
More about newborn blood spot tests
Your health visitor
A health visitor’s a registered nurse or midwife who’s done further study in public health nursing.
Your health visitor will:
- take over from your midwife when your baby’s 11 days old
- get to know you and your baby
- ensure you get all the help and support you need as your baby grows
Your baby’s named person
In Scotland, the aim is that every child, young person and their parents have a `named person’ who is a clear and safe point of contact to seek support and advice about any aspect of your child’s wellbeing.
From when your child is born until they start school, your named person is your health visitor.
Your baby’s named person will:
- be a good person for you to ask for information or advice about being a parent
- talk to about any worries
- support you to look after yourself and your baby
They can also:
- put you in contact with other community professionals or services
- help you make the best choices for you and your family
The Red Book
You’ll be given a personal child health record called the Red Book. You can use it to record information about your baby’s growth, development, tests and immunisations.
Keep it safe and take it to any appointments you have with a healthcare professional.
The family nurse

Family nurses offer the Family Nurse Partnership (FNP) programme to young, first-time parents from early in their pregnancy until their child’s 2 years old. This program is available to first-time parents under the age of 20.
The programme includes home visits from a family nurse while you’re pregnant, and after your baby’s born. These visits help:
- to have a healthy pregnancy
- you and your baby grow and develop together
- you to be the best parent you can be.
Your health visitor will take over from your family nurse when your baby is two until they go to school.
The Scottish Government has more information about Family Nurse Partnership
Translations and alternative formats of this information are available from Public Health Scotland .
If you need a different language or format, please contact [email protected].
- Ready Steady Baby leaflet in Arabic, Polish, Simplified Chinese (Mandarin) and Ukrainian
- Ready Steady Baby leaflet in English (Easy Read)
Source: Public Health Scotland - Opens in new browser window
Last updated: 19 December 2023
Help us improve NHS inform
Your feedback has been received
Don’t include personal information e.g. name, location or any personal health conditions.
Also on NHS inform
Other health sites.
- Disabled Living Foundation (DLF)
- Rica: consumer research charity
- Health & Care Professions Council (HCPC)

Your Guide to Prenatal Appointments
Medical review policy, latest update:.
Minor copy changes.
Typical prenatal appointment schedule
Read this next, what happens during a prenatal care appointment, what tests will i receive at my prenatal appointments, what will i talk about with my practitioner at prenatal care appointments , first trimester prenatal appointments: what to expect, second trimester prenatal appointments: what to expect, third trimester prenatal appointments: what to expect, questions to ask during prenatal appointments .
Prenatal care visits are chock-full of tests, measurements, questions and concerns, but know that throughout the process your and your baby’s wellbeing are the main focus. Keep your schedule organized so you don’t miss any appointments and jot down anything you want to discuss with your doctor and your prenatal experience should end up being both positive and rewarding.
What to Expect When You’re Expecting , 5th edition, Heidi Murkoff. American College of Obstetricians and Gynecologists, Having a Baby After Age 35: How Aging Affects Fertility and Pregnancy , 2020. American College of Obstetricians and Gynecologists, Routine Tests During Pregnancy , 2020. US Department of Health & Human Services, Office on Women’s Health, Prenatal Care and Tests , January 2019. Journal of Perinatology , Number of Prenatal Visits and Pregnancy Outcomes in Low-risk wWomen , June 2016. Mayo Clinic, Edema , October 2017. Mayo Clinic, Prenatal Care: 2nd Trimester Visits , August 2020. Mayo Clinic, Prenatal Care: 3rd Trimester Visits , August 2020. Jennifer Leighdon Wu, M.D., Women’s Health of Manhattan, New York, NY. WhatToExpect.com, Preeclampsia: Symptoms, Risk Factors and Treatment , April 2019. WhatToExpect.com, Prenatal Testing During Pregnancy , March 2019. WhatToExpect.com, Urine Tests During Pregnancy , May 2019. WhatToExpect.com, Fetal Heartbeat: The Development of Baby’s Circulatory System , April 2019. WhatToExpect.com, Amniocentesis , Mary 2019. WhatToExpect.com, Ultrasound During Pregnancy , April 2019. WhatToExpect.com, Rh Factor Testing , June 2019. WhatToExpect.com, Glucose Screening and Glucose Tolerance Test , April 2019. WhatToExpect.com, Nuchal Translucency Screening , April 2019. WhatToExpect.com, Group B Strep Testing During Pregnancy , August 2019. WhatToExpect.com, The Nonstress Test During Pregnancy , April 2019. WhatToExpect.com, Biophysical Profile (BPP) , May 2019. WhatToExpect.com, Noninvasive Prenatal Testing , (NIPT), April 2019. WhatToExpect.com, The Quad Screen , February 2019. WhatToExpect.com, Chorionic Villus Sampling (CVS) , February 2019. WhatToExpect.com, The First Prenatal Appointment , June 2019. WhatToExpect.com, Breech Birth: What it Means for You , September 2018.
Updates history
Jump to your week of pregnancy, trending on what to expect, signs of labor, pregnancy calculator, ⚠️ you can't see this cool content because you have ad block enabled., top 1,000 baby girl names in the u.s., top 1,000 baby boy names in the u.s., braxton hicks contractions and false labor.
Need to talk? Call 1800 882 436. It's a free call with a maternal child health nurse. *call charges may apply from your mobile
Is it an emergency? Dial 000 If you need urgent medical help, call triple zero immediately.

Checkups, scans and tests
Find out what checkups, scans and tests you might have during your pregnancy.
Can my partner come along too?
Yes. It’s a good idea for your birth support partner , family member or friend to come to your appointments with you, particularly when discussing your birth plan and if you want them to support you during the birth.
Resources and support
If you have any questions about antenatal care or concerns about your pregnancy, contact:
- Pregnancy, Birth and Baby on 1800 882 436 to speak to a maternal child health nurse
- your midwife
- the hospital where you're planning to give birth

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call . Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: May 2020
Related pages
- Questions to ask your doctor about tests and scans
- Health professionals involved in your pregnancy
Routine antenatal tests
- Prenatal screening and testing
- Antenatal classes
Checkups, tests and scans available during your pregnancy
Your first antenatal visit, search our site for.
- Antenatal Care
Need more information?
Top results
If you are pregnant, find out when to have your first antenatal care visit and what will happen at the appointment with your doctor or midwife.
Read more on Pregnancy, Birth & Baby website

Antenatal Care during Pregnancy
Once you are pregnant, your first antenatal appointment will ideally take place when you are about 6 to 8 weeks pregnant.
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website

Antenatal care includes several checkups, tests and scans, some of which are offered to women as a normal part of antenatal care in Australia.
Pregnancy at week 7
Your baby is now about 1cm long and if you haven’t seen your doctor yet, now is a good time to start your antenatal care.
During pregnancy, you'll be offered various blood tests and ultrasound scans. Find out what each test can tell you about you and your baby's health.
Checkups, scans and tests during pregnancy
Handy infographic that shows what you can expect and what you might be offered at each antenatal appointment during your pregnancy.
Pregnancy and birth care options - Better Health Channel
Pregnant women in Victoria can choose who will care for them during their pregnancy, where they would like to give birth and how they would like to deliver their baby.
Read more on Better Health Channel website

What does an obstetrician do?
Obstetricians are specialists in pregnancy and birth. Learn more about how to choose one and the costs involved in having a private obstetrician.
Blood tests during pregnancy
Find out more about the blood tests you be offered during your pregnancy. what they test for and when you’ll be offered them.
Cervical screening during pregnancy
Cervical screening can be performed at any time, including during pregnancy. Regular cervical screening can protect you against cervical cancer.
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Call us and speak to a Maternal Child Health Nurse for personal advice and guidance.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.

An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- U.S. Department of Health & Human Services

Call the OWH HELPLINE: 1-800-994-9662 9 a.m. — 6 p.m. ET, Monday — Friday OWH and the OWH helpline do not see patients and are unable to: diagnose your medical condition; provide treatment; prescribe medication; or refer you to specialists. The OWH helpline is a resource line. The OWH helpline does not provide medical advice.
Please call 911 or go to the nearest emergency room if you are experiencing a medical emergency.
Prenatal care and tests

Medical checkups and screening tests help keep you and your baby healthy during pregnancy. This is called prenatal care. It also involves education and counseling about how to handle different aspects of your pregnancy. During your visits, your doctor may discuss many issues, such as healthy eating and physical activity, screening tests you might need, and what to expect during labor and delivery.
Choosing a prenatal care provider
You will see your prenatal care provider many times before you have your baby. So you want to be sure that the person you choose has a good reputation, and listens to and respects you. You will want to find out if the doctor or midwife can deliver your baby in the place you want to give birth , such as a specific hospital or birthing center. Your provider also should be willing and able to give you the information and support you need to make an informed choice about whether to breastfeed or bottle-feed.
Health care providers that care for women during pregnancy include:
- Obstetricians (OB) are medical doctors who specialize in the care of pregnant women and in delivering babies. OBs also have special training in surgery so they are also able to do a cesarean delivery . Women who have health problems or are at risk for pregnancy complications should see an obstetrician. Women with the highest risk pregnancies might need special care from a maternal-fetal medicine specialist .
- Family practice doctors are medical doctors who provide care for the whole family through all stages of life. This includes care during pregnancy and delivery, and following birth. Most family practice doctors cannot perform cesarean deliveries.
- A certified nurse-midwife (CNM) and certified professional midwife (CPM) are trained to provide pregnancy and postpartum care. Midwives can be a good option for healthy women at low risk for problems during pregnancy, labor, or delivery. A CNM is educated in both nursing and midwifery. Most CNMs practice in hospitals and birth centers. A CPM is required to have experience delivering babies in home settings because most CPMs practice in homes and birthing centers. All midwives should have a back-up plan with an obstetrician in case of a problem or emergency.
Ask your primary care doctor, friends, and family members for provider recommendations. When making your choice, think about:
- Personality and bedside manner
- The provider's gender and age
- Office location and hours
- Whether you always will be seen by the same provider during office checkups and delivery
- Who covers for the provider when she or he is not available
- Where you want to deliver
- How the provider handles phone consultations and after-hour calls
What is a doula?
A doula (DOO-luh) is a professional labor coach, who gives physical and emotional support to women during labor and delivery. They offer advice on breathing, relaxation, movement, and positioning. Doulas also give emotional support and comfort to women and their partners during labor and birth. Doulas and midwives often work together during a woman's labor. A recent study showed that continuous doula support during labor was linked to shorter labors and much lower use of:
- Pain medicines
- Oxytocin (ok-see-TOHS-uhn) (medicine to help labor progress)
- Cesarean delivery
Check with your health insurance company to find out if they will cover the cost of a doula. When choosing a doula, find out if she is certified by Doulas of North America (DONA) or another professional group.
Places to deliver your baby
Many women have strong views about where and how they'd like to deliver their babies. In general, women can choose to deliver at a hospital, birth center, or at home. You will need to contact your health insurance provider to find out what options are available. Also, find out if the doctor or midwife you are considering can deliver your baby in the place you want to give birth.
Hospitals are a good choice for women with health problems, pregnancy complications, or those who are at risk for problems during labor and delivery. Hospitals offer the most advanced medical equipment and highly trained doctors for pregnant women and their babies. In a hospital, doctors can do a cesarean delivery if you or your baby is in danger during labor. Women can get epidurals or many other pain relief options. Also, more and more hospitals now offer on-site birth centers, which aim to offer a style of care similar to standalone birth centers.
Questions to ask when choosing a hospital:
- Is it close to your home?
- Is a doctor who can give pain relief, such as an epidural, at the hospital 24-hours a day?
- Do you like the feel of the labor and delivery rooms?
- Are private rooms available?
- How many support people can you invite into the room with you?
- Does it have a neonatal intensive care unit (NICU) in case of serious problems with the baby?
- Can the baby stay in the room with you?
- Does the hospital have the staff and set-up to support successful breastfeeding?
- Does it have an on-site birth center?
Birth or birthing centers give women a "homey" environment in which to labor and give birth. They try to make labor and delivery a natural and personal process by doing away with most high-tech equipment and routine procedures. So, you will not automatically be hooked up to an IV. Likewise, you won't have an electronic fetal monitor around your belly the whole time. Instead, the midwife or nurse will check in on your baby from time to time with a handheld machine. Once the baby is born, all exams and care will occur in your room. Usually certified nurse-midwives, not obstetricians, deliver babies at birth centers. Healthy women who are at low risk for problems during pregnancy, labor, and delivery may choose to deliver at a birth center.
Women can not receive epidurals at a birth center, although some pain medicines may be available. If a cesarean delivery becomes necessary, women must be moved to a hospital for the procedure. After delivery, babies with problems can receive basic emergency care while being moved to a hospital.
Many birthing centers have showers or tubs in their rooms for laboring women. They also tend to have comforts of home like large beds and rocking chairs. In general, birth centers allow more people in the delivery room than do hospitals.
Birth centers can be inside of hospitals, a part of a hospital or completely separate facilities. If you want to deliver at a birth center, make sure it meets the standards of the Accreditation Association for Ambulatory Health Care, The Joint Commission, or the American Association of Birth Centers. Accredited birth centers must have doctors who can work at a nearby hospital in case of problems with the mom or baby. Also, make sure the birth center has the staff and set-up to support successful breastfeeding.
Homebirth is an option for healthy pregnant women with no risk factors for complications during pregnancy, labor or delivery. It is also important women have a strong after-care support system at home. Some certified nurse midwives and doctors will deliver babies at home. Many health insurance companies do not cover the cost of care for homebirths. So check with your plan if you'd like to deliver at home.
Homebirths are common in many countries in Europe. But in the United States, planned homebirths are not supported by the American Congress of Obstetricians and Gynecologists (ACOG). ACOG states that hospitals are the safest place to deliver a baby. In case of an emergency, says ACOG, a hospital's equipment and highly trained doctors can provide the best care for a woman and her baby.
If you are thinking about a homebirth, you need to weigh the pros and cons. The main advantage is that you will be able to experience labor and delivery in the privacy and comfort of your own home. Since there will be no routine medical procedures, you will have control of your experience.
The main disadvantage of a homebirth is that in case of a problem, you and the baby will not have immediate hospital/medical care. It will have to wait until you are transferred to the hospital. Plus, women who deliver at home have no options for pain relief.
To ensure your safety and that of your baby, you must have a highly trained and experienced midwife along with a fail-safe back-up plan. You will need fast, reliable transportation to a hospital. If you live far away from a hospital, homebirth may not be the best choice. Your midwife must be experienced and have the necessary skills and supplies to start emergency care for you and your baby if need be. Your midwife should also have access to a doctor 24 hours a day.
Prenatal checkups
During pregnancy, regular checkups are very important. This consistent care can help keep you and your baby healthy, spot problems if they occur, and prevent problems during delivery. Typically, routine checkups occur:
- Once each month for weeks four through 28
- Twice a month for weeks 28 through 36
- Weekly for weeks 36 to birth
Women with high-risk pregnancies need to see their doctors more often.
At your first visit your doctor will perform a full physical exam, take your blood for lab tests, and calculate your due date. Your doctor might also do a breast exam, a pelvic exam to check your uterus (womb), and a cervical exam, including a Pap test. During this first visit, your doctor will ask you lots of questions about your lifestyle, relationships, and health habits. It's important to be honest with your doctor.
After the first visit, most prenatal visits will include:
- Checking your blood pressure and weight
- Checking the baby's heart rate
- Measuring your abdomen to check your baby's growth
You also will have some routine tests throughout your pregnancy, such as tests to look for anemia , tests to measure risk of gestational diabetes , and tests to look for harmful infections.
Become a partner with your doctor to manage your care. Keep all of your appointments — every one is important! Ask questions and read to educate yourself about this exciting time.
Monitor your baby's activity
After 28 weeks, keep track of your baby's movement. This will help you to notice if your baby is moving less than normal, which could be a sign that your baby is in distress and needs a doctor's care. An easy way to do this is the "count-to-10" approach. Count your baby's movements in the evening — the time of day when the fetus tends to be most active. Lie down if you have trouble feeling your baby move. Most women count 10 movements within about 20 minutes. But it is rare for a woman to count less than 10 movements within two hours at times when the baby is active. Count your baby's movements every day so you know what is normal for you. Call your doctor if you count less than 10 movements within two hours or if you notice your baby is moving less than normal. If your baby is not moving at all, call your doctor right away.
Prenatal tests
Tests are used during pregnancy to check your and your baby's health. At your fist prenatal visit, your doctor will use tests to check for a number of things, such as:
- Your blood type and Rh factor
- Infections, such as toxoplasmosis and sexually transmitted infections (STIs), including hepatitis B , syphilis , chlamydia , and HIV
- Signs that you are immune to rubella (German measles) and chicken pox
Throughout your pregnancy, your doctor or midwife may suggest a number of other tests, too. Some tests are suggested for all women, such as screenings for gestational diabetes, Down syndrome, and HIV. Other tests might be offered based on your:
- Personal or family health history
- Ethnic background
- Results of routine tests
Some tests are screening tests. They detect risks for or signs of possible health problems in you or your baby. Based on screening test results, your doctor might suggest diagnostic tests. Diagnostic tests confirm or rule out health problems in you or your baby.
Understanding prenatal tests and test results
If your doctor suggests certain prenatal tests, don't be afraid to ask lots of questions. Learning about the test, why your doctor is suggesting it for you, and what the test results could mean can help you cope with any worries or fears you might have. Keep in mind that screening tests do not diagnose problems. They evaluate risk. So if a screening test comes back abnormal, this doesn't mean there is a problem with your baby. More information is needed. Your doctor can explain what test results mean and possible next steps.
Avoid keepsake ultrasounds
You might think a keepsake ultrasound is a must-have for your scrapbook. But, doctors advise against ultrasound when there is no medical need to do so. Some companies sell "keepsake" ultrasound videos and images. Although ultrasound is considered safe for medical purposes, exposure to ultrasound energy for a keepsake video or image may put a mother and her unborn baby at risk. Don't take that chance.
High-risk pregnancy
Pregnancies with a greater chance of complications are called "high-risk." But this doesn't mean there will be problems. The following factors may increase the risk of problems during pregnancy:
- Very young age or older than 35
- Overweight or underweight
- Problems in previous pregnancy
- Health conditions you have before you become pregnant, such as high blood pressure , diabetes , autoimmune disorders , cancer , and HIV
- Pregnancy with twins or other multiples
Health problems also may develop during a pregnancy that make it high-risk, such as gestational diabetes or preeclampsia . See Pregnancy complications to learn more.
Women with high-risk pregnancies need prenatal care more often and sometimes from a specially trained doctor. A maternal-fetal medicine specialist is a medical doctor that cares for high-risk pregnancies.
If your pregnancy is considered high risk, you might worry about your unborn baby's health and have trouble enjoying your pregnancy. Share your concerns with your doctor. Your doctor can explain your risks and the chances of a real problem. Also, be sure to follow your doctor's advice. For example, if your doctor tells you to take it easy, then ask your partner, family members, and friends to help you out in the months ahead. You will feel better knowing that you are doing all you can to care for your unborn baby.
Paying for prenatal care
Pregnancy can be stressful if you are worried about affording health care for you and your unborn baby. For many women, the extra expenses of prenatal care and preparing for the new baby are overwhelming. The good news is that women in every state can get help to pay for medical care during their pregnancies. Every state in the United States has a program to help. Programs give medical care, information, advice, and other services important for a healthy pregnancy.
Learn more about programs available in your state.
You may also find help through these places:
- Local hospital or social service agencies – Ask to speak with a social worker on staff. She or he will be able to tell you where to go for help.
- Community clinics – Some areas have free clinics or clinics that provide free care to women in need.
- Women, Infants and Children (WIC) Program – This government program is available in every state. It provides help with food, nutritional counseling, and access to health services for women, infants, and children.
- Places of worship
More information on prenatal care and tests
Read more from womenshealth.gov.
- Pregnancy and Medicines Fact Sheet - This fact sheet provides information on the safety of using medicines while pregnant.
Explore other publications and websites
- Chorionic Villus Sampling (CVS) (Copyright © March of Dimes) - Chorionic villus sampling (CVS) is a prenatal test that can diagnose or rule out certain birth defects. The test is generally performed between 10 and 12 weeks after a woman's last menstrual period. This fact sheet provides information about this test, and how the test sample is taken.
- Folic Acid (Copyright © March of Dimes) - This fact sheet stresses the importance of getting higher amounts of folic acid during pregnancy in order to prevent neural tube defects in unborn children.
- Folic Acid: Questions and Answers - The purpose of this question and answer sheet is to educate women of childbearing age on the importance of consuming folic acid every day to reduce the risk of spina bifida.
- For Women With Diabetes: Your Guide to Pregnancy - This booklet discusses pregnancy in women with diabetes. If you have type 1 or type 2 diabetes and you are pregnant or hoping to get pregnant soon, you can learn what to do to have a healthy baby. You can also learn how to take care of yourself and your diabetes before, during, and after your pregnancy.
- Genetics Home Reference - This website provides information on specific genetic conditions and the genes or chromosomes responsible for these conditions.
- Guidelines for Vaccinating Pregnant Women - This publication provides information on routine and other vaccines and whether they are recommended for use during pregnancy.
- How Your Baby Grows (Copyright © March of Dimes) - This site provides information on the development of your baby and the changes in your body during each month of pregnancy. In addition, for each month, it provides information on when to go for prenatal care appointments and general tips to take care of yourself and your baby.
- Pregnancy Registries - Pregnancy registries help women make informed and educated decisions about using medicines during pregnancy. If you are pregnant and currently taking medicine — or have been exposed to a medicine during your pregnancy — you may be able to participate and help in the collection of this information. This website provides a list of pregnancy registries that are enrolling pregnant women.
- Pregnancy, Breastfeeding, and Bone Health - This publication provides information on pregnancy-associated osteoporosis, lactation and bone loss, and what you can do to keep your bones healthy during pregnancy.
- Prenatal Care: First-Trimester Visits (Copyright © Mayo Foundation) - This fact sheet explains what to expect during routine exams with your doctor. In addition, if you have a condition that makes your pregnancy high-risk, special tests may be performed on a regular basis to check the baby's health.
- Ten Tips for a Healthy Pregnancy (Copyright © Lamaze International) - This easy-to-read fact sheet provides 10 simple recommendations to help mothers have a healthy pregnancy.
- Ultrasound (Copyright © March of Dimes) - This fact sheet discusses the use of an ultrasound in prenatal care at each trimester.
Connect with other organizations
- American Academy of Family Physicians
- American Association of Birth Centers
- American College of Obstetricians and Gynecologists
- Center for Research on Reproduction and Women's Health, University of Pennsylvania Medical Center
- Dona International
- March of Dimes
- Maternal and Child Health Bureau, HRSA, HHS
- National Association for Down Syndrome
- National Center on Birth Defects and Developmental Disabilities, CDC
- Public Information and Communications Branch, NICHD, NIH, HHS
- HHS Non-Discrimination Notice
- Language Assistance Available
- Accessibility
- Privacy Policy
- Disclaimers
- Freedom of Information Act (FOIA)
- Use Our Content
- Vulnerability Disclosure Policy
- Kreyòl Ayisyen
A federal government website managed by the Office on Women's Health in the Office of the Assistant Secretary for Health at the U.S. Department of Health and Human Services.
1101 Wootton Pkwy, Rockville, MD 20852 1-800-994-9662 • Monday through Friday, 9 a.m. to 6 p.m. ET (closed on federal holidays).

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Effectiveness of Home Visits in Pregnancy as a Public Health Measure to Improve Birth Outcomes
Kayoko ichikawa.
1 Department of Health Informatics, Kyoto University School of Public Health, Kyoto, Japan
2 Department of Social Medicine, National Research Institute for Child Health and Development, Tokyo, Japan
Takeo Fujiwara
Takeo nakayama.
Conceived and designed the experiments: TF. Performed the experiments: KI. Analyzed the data: KI TF. Contributed reagents/materials/analysis tools: KI TF. Wrote the paper: KI TF TN. Significant contribution to obtain data from the field: KI TF TN.
Associated Data
Data is not made publicly available due to the restriction of the Kyoto City and Ethics Committee at Kyoto University. If data is requested, please contact to Dr. Takeo Fujiwara, Head of Department of Social Medicine National Research Institute for Child Health and Development, Tokyo, Japan ( pj.og.dhccn@kt-arawijuf ).
Birth outcomes, such as preterm birth, low birth weight (LBW), and small for gestational age (SGA), are crucial indicators of child development and health.
To evaluate whether home visits from public health nurses for high-risk pregnant women prevent adverse birth outcomes.
In this quasi-experimental cohort study in Kyoto city, Japan, high-risk pregnant women were defined as teenage girls (range 14–19 years old), women with a twin pregnancy, women who registered their pregnancy late, had a physical or mental illness, were of single marital status, non-Japanese women who were not fluent in Japanese, or elderly primiparas. We collected data from all high-risk pregnant women at pregnancy registration interviews held at a public health centers between 1 July 2011 and 30 June 2012, as well as birth outcomes when delivered from the Maternal and Child Health Handbook (N = 964), which is a record of prenatal check-ups, delivery, child development and vaccinations. Of these women, 622 women were selected based on the home-visit program propensity score-matched sample (pair of N = 311) and included in the analysis. Data were analyzed between January and June 2014.
In the propensity score-matched sample, women who received the home-visit program had lower odds of preterm birth (odds ratio [OR], 0.62; 95% confidence interval [CI], 0.39 to 0.98) and showed a 0.55-week difference in gestational age (95% CI: 0.18 to 0.92) compared to the matched controlled sample. Although the program did not prevent LBW and SGA, children born to mothers who received the program showed an increase in birth weight by 107.8 g (95% CI: 27.0 to 188.5).
Home visits by public health nurses for high-risk pregnant women in Japan might be effective in preventing preterm birth, but not SGA.
Introduction
Adverse birth outcomes, such as preterm birth, low birth weight (LBW), and small for gestational age (SGA), can have a long-term impact on child development and health [ 1 – 6 ]. Adverse birth outcomes are a known risk factor for maternal mental health and child maltreatment [ 7 – 9 ]. In Japan, like other developed countries [ 10 , 11 ], the proportion of preterm birth (5.8%) and LBW (boys: 8.5%, girls: 10.7%) has increased over the past three decades [ 11 – 14 ]. The causes of preterm birth or LBW have been considered multifactorial [ 15 ], and include, for example, maternal infection during pregnancy [ 16 ], smoking [ 17 ], low maternal BMI [ 18 ], maternal depression [ 19 , 20 ], lack of social support [ 21 ], maternal disease [ 22 ], and social disadvantage[ 23 – 25 ]. To prevent adverse health outcomes, a comprehensive intervention approach is needed because these risk factors are likely to be co-occurring.
Implementation of a home-visit program during pregnancy is a comprehensive strategy to prevent adverse birth outcomes [ 26 , 27 ]. Although the exact mechanism of this approach is not well clarified, many previous studies have suggested that providing tangible in-home or one-on-one psychosocial support, and improving linkages to medical providers, social services and nutrition support can encourage healthy prenatal behaviors[ 28 – 31 ]. However, previous randomized controlled trials (RCTs) of home-visit programs and pregnancy outcomes showed inconsistent results [ 32 – 35 ]. For example, Lee and colleagues [ 36 ] found that home visits before 30 weeks’ gestation for women (Black and Hispanic: 65%; under 18 years old: 24.6%) were effective for preventing LBW (5.1% versus 9.8%; p = 0.022), however McLaughlin and colleagues [ 37 ] found home visits for women (Black women: 35%, mean age: 21.8 years old) showed no significant effect in reducing LBW incidence. This is likely due to several factors, including differences in the characteristics of target participants and methods of program delivery, the reluctance of high-risk women to participate, and variation in the timing of home-visit implementation between trials [ 38 , 39 ]. Therefore, an assessment of the effectiveness of home visits for a wide range of high-risk women, and the timing of implementation, is needed.
Japan has a unique data collection and prenatal support system that was first established by the Maternal and Child Health (MCH) Act and MCH Law in 1965 for the promotion of maternal, newborn, and infant health. The Act promotes continuity of care through the MCH Handbook [ 40 ], which is provided for free to expectant mothers who submit a notice of pregnancy to their local government office. Women in Japan are supposed to register their pregnancy within the 11th gestational week [ 41 ]. The Handbook unifies maternal and child health into one resource, serving as a maternal health record during pregnancy and a child health record from 0–6 years, which parents can keep and take with them to appointments. In addition to the MCH Handbook, which has almost 100% coverage [ 40 ] for expectant mothers, the Act also provides health guidance to pregnant and postpartum women, and health check-ups for newborns and infants at local government health centers.
In July 2011, Kyoto city in Japan established the population-based home-visit program for all high-risk pregnant women. High-risk pregnant women were defined as teenage girls (range 14–19 years old), women with a twin pregnancy, women who registered their pregnancy late, had a physical or mental diseases, were of single marital status, non-Japanese women who were not fluent in Japanese, or elderly primiparas. At the time of pregnancy registration at the public health center, public health nurses assessed the risk level of pregnant women by conducting an interview in person using a registration questionnaire. As some women receive the home-visit program and others do not, we were provided with the opportunity to conduct a quasi-experimental study on the effectiveness of the home-visit program. As the baseline information is known at registration, the propensity of receiving the home-visit program can be assessed.
The objective of this study is to evaluate the effectiveness of the home-visit program conducted by public health nurses to high-risk pregnant women to prevent adverse birth outcomes (preterm, LBW, and SGA) by using the propensity score-matching model. We also investigated whether timing of program implementation had an effect on adverse birth outcomes.
Ethics statement
We used secondary administrative data from Kyoto city government in this study, which did not contain identifying information about individuals. In addition, public health nurses obtained written informed consent from pregnant women. We obtained written informed consent from Kyoto city government’s ethical committee to use this secondary administrative data which did not contain identifying information about individuals, and published an announcement about this study on the official homepage of Kyoto city government. The announcement stated that if individuals who met the inclusion criteria did not want their own data to be used, even though it was anonymised, they could request for their data to be omitted by calling the Kyoto city government. However, no one requested for their data to be omitted from the study. The study was approved by the Kyoto University Graduate School and Faculty of Medicine Ethics Committee (E1833).
Study design and population
This was a quasi-experimental cohort study using administrative data collected in Kyoto, Japan. Data was obtained from the Department of Child and Maternal Health in Kyoto, including the baseline questionnaire conducted at pregnancy registration in public health centers, MCH handbook data, which includes data from prenatal checkups, delivery, child development, vaccinations, and home-visits. The population of Kyoto is around 1,467,000. During the period of 1 July 2011 to 30 June 2012, 11,749 women registered their pregnancy at public health centers in Kyoto. Trained public health nurses conducted interviews in person at the public health center using unified standard questionnaires to assess high-risk pregnancy. Target participants of our study were all high-risk pregnant women who registered their pregnancy in Kyoto city. High-risk pregnant women were administratively defined as follows: 1) women who had past or current physical or mental illness; 2) primiparas under the age of 20; 3) primiparas over the age of 35 with some unfavorable conditions such as poverty; 4) women who were pregnant with twins; 5) women who were late to register their pregnancy (i.e. after the 22 nd week of gestation) or women who were unhappy about being pregnant; 6) women with single marital status (unmarried or divorced); 7) non-Japanese women who were not fluent in Japanese, and 8) women who were assessed by public health nurses at registration as requiring any additional support including both medical, psycho-social, nutrition counseling.
The target population of high-risk prenatal mothers in this project was 1,023 women, and all data were used in the initial analysis to calculate propensity scores for receiving the home-visit program. That is, all high-risk pregnant women were supposed to receive home visits from public health nurses; however, 594 women (58.1%) did not receive any visits because they were not reachable. This group was used as a control sample ( Fig 1 ).

Home-visit programs for pregnant women in Kyoto
In this program, trained public health nurses were to make at least 1 home visit to high-risk pregnant women lasting for more than 1 hour during mid- or late-term pregnancy (mean gestational age: 27.2 (SD = 6.9) weeks, range: 7–40 weeks). Nurses received specific training about home visiting about once a year and were expected to consult with supervisors about difficult cases. The contents of the home visit were as follows: 1) checking women’s social support status and linking them to other services in the community, if needed; 2) providing information about appropriate nutrition during pregnancy, prenatal care, dental care, and child care, and 3) asking women about their physical or psychological health and linking them to medical facilities if needed. If nurses concluded that the women required more support, they provided follow-up support by phone, made another home visit, or introduced women to further social services support. Detailed components of the home visit are shown in Table 1 .
Birth outcomes, birth weight (crude value) and gestational age were obtained from birth records in the MCH handbook. Z-scores of birth weight (ZBW) were calculated and we adjusted for gestational age, sex, and parity [ 42 ]. Binary indicators were low birth weight, defined as less than 2500g; preterm birth, defined as less than 37 weeks, and small for gestational age, defined as <10 percentile.
Covariates and independent variables
The following covariates were obtained from baseline questionnaires and interviews from trained public health nurses at the time of pregnancy registration: maternal age, paternal age, employment status during pregnancy, living with family members, marital status, parity, history of miscarriage and stillbirth, experiences of fertility treatment, late submission of pregnancy registration (over 22 weeks), twin pregnancy, maternal smoking or alcohol consumption, smoking among women’s family members, maternal physical or mental illness, limited Japanese ability among non-Japanese women, unintended pregnancy, worries about child-rearing, finances, and relationship with partner, having someone to consult with on child care, experiences of good relationships with parents, subjective economic status, maternal and paternal attitudes to child-rearing, and experiences of child-rearing. Categorical variables were used for childcare services (“Yes”, “Rarely”, or “Never”) and knowing someone with experience of child-rearing (“Yes, many people”, “Yes, a few people”, or “No, do not know anyone”). The remaining variables were binominal (see Table 2 ).
Note from questionnaire
a "Do you have any disease that is currently under treatment or was treated in the past?"
b From risk assessment by public health nurses in first interview.
c From risk assessment by public health nurses in first interview.
d Prenatal mothers who emigrated to Japan or were staying in Japan long-term.
e ‘ satogaeri’ : a tradition in which pregnant women return to the family home prior to delivery to stay with their parents for support before and after childbirth.
Statistical analysis
Of the 1,023 baseline samples, we excluded participants who had missing birth-outcome data (home-visit program: n = 19, no home-visit program: n = 40, 5.8% in total participants) from the analysis (total N = 964 women, home-visit program: n = 410, no home-visit program: n = 554). Then, propensity score-matched analysis was performed to reduce potential bias on receiving the home-visit program. The probability of home-visit participation was estimated by all baseline characteristics using logistic regression, because these characteristics possibly associate with participation in the home-visit program. Propensity-score matching was performed by using the following algorithm: 1:1 nearest-neighbor match method with a caliper of 0.4 SD and no replacement. Finally, 311 women who received the home-visit program and 311 women who did not were included in the analysis (that is, N = 622). Variables used to estimate the propensity to participate in the program were sufficiently high, with C-statistics at 0.77. No significant difference was observed between the baseline characteristics of the home-visit program group and the no home-visit group ( Table 2 , right columns). The propensity-matched pairs were compared using logistic regression analysis, and multivariate regression analysis after adjusting for all baseline variables. In addition, sub-group analysis was performed for the timing of home-visit implementation, which was divided into two subgroups (home visits at <28 gestational weeks, home visits at ≥28 weeks). Missing data of covariates such as alcohol consumption (n = 4), experiences of fertility treatment (n = 12), physical or mental illness (n = 2), employment status (n = 25), living with family members (n = 162), experiences of good relationships with parents (n = 25), maternal and paternal attitudes of child rearing (n = 32) and experiences of child-rearing (n = 12) were treated as dummy variables. Where paternal age was missing in the data, the mean age was imputed. Stata version 13 was used to perform the analysis between January 2014 and June 2014.
Table 2 shows the baseline characteristics of prenatal mothers at pregnancy registration in the home-visit group (n = 410) and the no home-visit group (n = 554) before propensity-score matching. Mean gestational age for infants of mothers in the home-visit group was 27.2 (SD = 6.9) weeks. Pregnant women who received home visits were more likely to be experiencing their first pregnancy (n = 333, 81.2%), diagnosed with a disease (n = 163, 39.8%), and worried about child-rearing (n = 192, 46.8%) or relationships with neighbors (n = 64, 15.6%) compared with women who did not receive home visits. Pregnant women who did not receive home visits were more likely to smoke (n = 111, 20.0%), drink alcohol (n = 67, 12.1%), be unmarried (n = 197, 35.6%), feel unhappy about their pregnancy (n = 111, 20.0%), or had partners who were unhappy about their pregnancy (n = 85, 15.3%) compared with women in the home-visit group. After performing propensity-score matching with the comparison group, no significant difference was observed between variables (see Table 2 ).
Table 3 shows the birth outcomes before and after propensity-score matching. Before propensity-score matching, women from the home-visit group had a heavier birth weight (2905.3 g, SD = 499.5 g), longer gestational age (38.7 weeks, SD = 1.8 weeks), higher ZBW (-0.04, SD = 1.1), less LBW infants (n = 85, 19.2%), less preterm birth (n = 40, 9.8%), and less SGA infants (n = 52, 11.7%) compared to participants who did not receive the home-visit program. After propensity-score matching, women from the home-visit group had a heavier birth weight (2933.3 g, SD = 473.4 g), longer gestational age (38.6 weeks, SD = 1.8 weeks), and less preterm birth (n = 34, 10.9%) compared to women who did not receive the home-visit program.
Abbreviations: LBW: low birth weight; SGA: small for gestational age.
Table 4 shows the coefficient and odds ratios (ORs) of the home-visit program for birth outcomes. Before propensity-score matching was conducted in the univariate model, women in the home-visit program during their pregnancy had a significantly heavier birth weight (coefficient: 138.3g, 95% confidence interval [CI]: 63.2 to 213.4), longer gestational age (coefficient: 0.67 week, 95% CI: 0.33 to 1.00), higher ZBW (coefficient: 0.25, 95% CI: 0.11 to 0.38), LBW (OR: 0.70, 95% CI: 0.49 to 0.98), preterm birth (OR: 0.62, 95% CI: 0.41 to 0.94), SGA (OR: 0.62, 95% CI: 0.43 to 0.91) than women who did not receive the home-visit program. These associations remained significant in the multivariate adjusted model, except for ZBW and SGA. Further, in the propensity-matched sample for the home-visit group, a heavier birth weight, longer gestational age, and lower odds of preterm birth remained significant during pregnancy, although odds of LBW became non-significant. In the final model—the multivariate adjustment of the propensity-score matched sample—pregnant women in the home-visit group delivered infants with a heavier birth weight of 99.1g (95% CI: 20.5 to 177.6) and a longer gestational age of 0.61 weeks (95% CI: 0.25 to 0.96), and were 74% less likely to deliver preterm, compared to pregnant women who did not receive home visits.
Abbreviations: CI: confidence interval; LBW: low birth weight; SGA: small for gestational age. Bold value signifies p<0.05.
Table 5 shows the subgroup analyses of the effectiveness of the home-visit program by timing of implementation (i.e. whether the program was implemented before or after 28 weeks’ gestation). In the propensity-score matched sample, women who entered the home-visit program late (after 28 gestational weeks, n = 159) showed a longer gestational age (coefficient: 0.65 weeks, 95% CI: 0.09 to 1.20) compared to women who did not receive home visits. Further, a marginal protective effect on preterm birth was found among women who entered the program late compared to women who were registered in the program earlier (OR: 0.57, 95% CI: 0.31 to 1.06). However, early implementation of the home-visit program (before 28 gestational weeks, n = 145) failed to show longer gestational age nor a protective effect on preterm than women in the comparison group, suggesting that joining the home-visit program after 28 weeks’ gestation was more effective to achieve longer gestational age and to be protective for preterm.
a no home visit (n = 554)
b p = 0.07.
Abbreviations: CI: confidence interval; LBW: low birthweight; SGA: small for gestational age. Bold value signifies p<0.05.
The present study evaluated the effectiveness of the home-visit program for high-risk pregnant women in Japan on birth outcomes (birth weight, gestational age, Z-scores of birth weight) using a propensity-score matched sample. We found that home visits from trained public health nurses at least once during pregnancy were effective to prevent preterm birth, but not small for gestational age among high-risk pregnant women in Japan.
To our knowledge, this is the first study to investigate the effectiveness of the home-visit program for a wide range of high-risk pregnant women as a public healthcare measure. However, two randomized controlled trials of home-visit programs [ 36 , 37 ], which investigated the efficacy of birth outcomes, suggested that the effectiveness of such programs is still inconsistent, while two recent observational studies conducted in the United States (US) using propensity score-matched analysis found home-visit programs to be effective [ 33 , 43 ]. Both US studies concluded that participating in the home-visit program reduced the risk of adverse birth outcomes in disadvantaged populations (i.e. people who received Medicaid). Our finding is consistent with these previous studies in showing the effectiveness of the home-visit program in preventing adverse birth outcomes, although the definition of disadvantaged population is different (i.e. our definition of ‘high-risk pregnant women’ did not only focus on economic status but on medical conditions, social disadvantages and other factors).
In the Japanese healthcare system, all pregnant women are screened by public health nurses at registration of their pregnancy, or within 11 weeks’ gestation. In addition, high-risk women receive comprehensive support and are referred to appropriate follow-up services[ 44 ]. This system enables high-risk women to be followed-up from the prenatal to postnatal period, and facilitates the first contact between public health services and high-risk pregnant women. Some components of the home-visit program, such as consultations on maternal anxiety, nutrition education and health-check ups, might improve birth weight. Although we tried to provide the home-visit program for all high-risk pregnant women, approximately half of the high-risk women (n = 554) were not reachable and showed worse risk factors, such as smoking and drinking alcohol, for poor birth outcomes. It is another challenge to support the super-high-risk pregnant women who were not reachable in general health care system.
We found that late admission to the home-visit program was effective to prevent preterm birth, although early admission to the home-visit program did not. The reason for this difference is unknown. It is possible that perinatal care or advice from public health nurses might be more effective closer to delivery. Further study is needed to elucidate the mechanism on why receiving home visits later in pregnancy is more effective to prevent preterm birth.
This study has some limitations. First, this study was of a quasi-experimental cohort design, so there may be unobserved variables and unknown confounding factors, such as maternal personality or characteristics. These factors may affect birth outcomes despite adjusting for baseline variables using the propensity score. Second, potential selection bias exists because approximately 5.8% (59/1023) of the data was omitted due to missing outcome data. However, there were no significant differences in the baseline characteristics between analyzed and omitted samples, so the present results represent the overall sample data. Finally, we could not count the dosage of the program and the number of times nurses visited participants’ homes. Further study is needed to investigate the association between outcomes and dosage of the program.
Despite these limitations, we found that the home-visit program for high-risk pregnant women by public health nurses significantly prevented preterm birth. Further studies with larger sample sizes are needed to measure the timing and dosage of the intervention in order to clarify the dose-response relationship in the home-visit program.
Our findings suggest that home visits by public health nurses for high-risk pregnant women in Japan might be effective in preventing preterm birth, but not SGA. This study adds to the evidence of the effectiveness of population-based home-visit programs as a public healthcare measure.
Acknowledgments
We gratefully thank all staff of the Kyoto City Health and Welfare Department of the Health and Health Promotion Office, Health and Medical Division (Kyoto City Public Health Center), especially Ms. Yoshimi Kimura, Dr. Masahiro Ito, Ms. Makiko Yoshiyama, Ms. Yoshiko Awazu, and Ms. Yoshie Nishimura, who agreed and cooperated to collect the data. We also thank Ms. Yuri Hiramoto, who developed the database system for data collection, Mr. Toshiaki Sekiguchi, Ms. Yumina Yamane, Ms. Yukiko Honda, Dr. Hiroki Mishina, who helped with data collection, and Ms. Emma Barber for her editorial assistance.
Funding Statement
This study was partly supported by a grant from the Ministry of Health and Labour Sciences Research Grant (H23-Seisaku-Ippan-005) and the Japan Health Foundation 2014.
Data Availability
- Book your antenatal a course
- Volunteer with us
What does a midwife do and other FAQs
Read time 6 minutes

They’ll be one of the most important people in your life for nine months (and beyond). So here’s what you need to know about your midwife’s role.
What is a midwife?
A midwife is a health professional (male or female) who supports women through pregnancy, labour, birth and the early days of parenthood (MIDIRS, 2017) . They will see you through scans, tests and welcoming your baby into the world.
What does a midwife do?
A midwife can be based in hospital, in a community setting like a midwife-led unit or a doctor’s surgery, or they can visit you at home (MIDIRS, 2017) . Community midwives will monitor you during your pregnancy, give advice and arrange access to any medical care you need.
For the birth, a hospital midwife will support and guide you and help you to get medical support if you need it. After your baby is born, a community midwife will be around to help you feed and care for your baby. That is, until you’re ready to say goodbye to them and switch over to a health visitor.
Do I have to see my GP for a referral to a midwife?
No, it’s much simpler than that – you can go directly to a midwife for your antenatal care (NICE, 2008) . Your GP practice or health centre can give you contact details for an NHS midwife. Your local NHS Hospital Trust website might also contain NHS midwives’ contact details.
"You don’t have to see a GP or an obstetrician while you’re pregnant or giving birth if you’d prefer not to, as long there are no complications (NICE, 2008) ."
Can I choose a private midwife, rather than NHS?
Of course, if you’re happy to pay. Independent midwives work for themselves so they charge for their services (IMUK, 2014a) .
If you opt for this route the same midwife – possibly with a colleague – will care for you throughout. This can improve a woman’s chance of achieving the kind of birth she is aiming for (IMUK, 2014b) . Independent midwives are often very experienced in more complicated births, such as vaginal breech, twin, and after caesarean (VBAC ) births too (IMUK, 2014b) .
Many women who choose indpendent midwives plump for a home birth but it’s not restricted: you are still able to access NHS care if it’s needed (IMUK, 2014c) . Find out how to access an independent midwife at IMUK or the Positive Birth Movement or go for a personal recommendation from a friend.
Is a doula the same as a midwife?
No. You might have heard mention of doulas but have never been quite sure how they’re different from midwives. The main distinction is that they are not acting medically but as a person who supports you during labour, birth and postnatally (Doula UK, 2017) .
What happens at my midwife appointments?
If this is your first baby you’ll probably have 10 appointments, but if you already have children it will likely drop down to seven (NICE, 2008) . You might have extra appointments if you see a specialist; if so, this should be written in your maternity notes that you’ll get at your ‘booking’ (first) appointment (NICE, 2008) . Here’s what to expect:
- You’ll have your ‘booking’ appointment between eight to 12 weeks of pregnancy.
- At each appointment, you’ll have specific topics to talk through. This will include things like which screening and antenatal tests are available, your lifestyle or what type of birth you’d like. You’ll always be given the chance to ask questions.
- At every appointment, your midwife will ask permission to take your blood pressure and check your urine for glucose and protein.
- Your midwife will feel your tummy to see how your baby is growing, and listen to your baby’s heartbeat. Towards the end of your pregnancy, they’ll also ask about their activity and check which position your baby is in.
(NHS, 2015)
Do I call my midwife when I go into labour?
The process on the big day varies throughout the country, so talk to your midwife about what happens in your area. Your local NHS Hospital Trust might also provide details. Some areas have a single telephone number to call when you’re in labour, where you speak to a midwife and discuss what to do.
Whether you’re having your baby at home, a midwife-led unit or an obstetric unit, the midwife will support you and liaise with medical staff if needed (NICE, 2014) . Straight after the birth, your midwife will check you both over and offer help with feeding and stitches if needed. They might also refer you on to further medical support if you need it (NICE, 2006, 2014) .
Will I see the midwife after my baby is born?
Technically, your midwife will continue to support you for six to eight weeks after you welcome your baby into the world and will also make sure you’re both adjusting well (Raynor, 2017) . If you’re doing ok though, you’re more likely to move over to the care of a health visitor around day ten. Check your maternity notes or ask your midwife to find out how and when the transition works in your area.
This page was last reviewed in September 2017.
Further information
Our support line offers practical and emotional support with feeding your baby and general enquiries for parents, members and volunteers: 0300 330 0700.
We also offer antenatal courses which are a great way to find out more about having a baby, labour and life with a new child.
For more information on everything that midwives do, check out the Nursing and Midwifery Council or the Royal College of Midwives
Doula UK (2017) About doulas. Available at: https://doula.org.uk/about-doulas/ [Accessed 12th September 2017].
IMUK (2014a) FAQs. http://www.imuk.org.uk/professionals/faqs/#about [Accessed 6th September 2017].
IMUK (2014b) What we do. http://www.imuk.org.uk/families/what-we-do/ [Accessed 6th September 2017].
IMUK (2014c) Hospital birth and NHS care. http://www.imuk.org.uk/families/faqs/#hospital [Accessed 12th September 2017].
MIDIRS (2017) Definition of the midwife. https://www.midirs.org/how-to-become-a-midwife/definition-midwife/ [Accessed 10th August 2017].
NHS (2015) Your antenatal care. Available at: http://www.nhs.uk/Conditions/pregnancy-and-baby/pages/antenatal-midwife… [Accessed 10th August 2017].
NICE (2006) Postnatal care up to 8 weeks after birth CG37. https://www.nice.org.uk/guidance/cg37 [Accessed 6th September 2017].
NICE (2008) Antenatal care for uncomplicated pregnancies. https://www.nice.org.uk/guidance/cg62 [Accessed 10th August 2017].
NICE (2014) Intrapartum care for healthy women and babies CG 190 https://www.nice.org.uk/guidance/cg190 [Accessed 6th September 2017].
Raynor MD (2017) Myles survival guide to midwifery Ebook. Available at: https://books.google.co.uk/books [Accessed 12th September 2017].
Further reading
Department of Health (2014) Independent midwives: insurance options outlined. Available at: https://www.gov.uk/government/news/independent-midwives-insurance-optio… [Accessed 6th September 2017].
MIDIRS (2017) Midwifery education: academic and clinical course content. Available at: https://www.midirs.org/how-to-become-a-midwife/midwifery-education-acad… [Accessed 6th September 2017].
NMC (2015) The Code. Available at: https://www.nmc.org.uk/standards/code/ [Accessed 6th September 2017].
NMC (2017) Standards for competence for registered midwives. Available at: https://www.nmc.org.uk/globalassets/sitedocuments/standards/nmc-standar… 6th September 2017].
RCM (2018) Independent midwives FAQs. Available at: https://www.rcm.org.uk/content/independent-midwives-faqa [Accessed 5th March 2018].
Information you can trust from NCT
When it comes to content, our aim is simple: every parent should have access to information they can trust.
All of our articles have been thoroughly researched and are based on the latest evidence from reputable and robust sources. We create our articles with NCT antenatal teachers, postnatal leaders and breastfeeding counsellors, as well as academics and representatives from relevant organisations and charities.
Read more about our editorial review process .
Related articles

Courses & workshops

In-person NCT Antenatal course

NCT Antenatal refresher course

Midwives: Care during pregnancy and delivery

Ever since midwifery was legalized in Quebec in 1999, women have been able to choose a midwife to provide prenatal and postpartum care as well as support during labour and delivery. A midwife offers personalized care, establishing a relationship with the mother-to-be that is based on equality and collaboration.
The practice of midwifery
A midwife is a health care professional who provides care and services during pregnancy, delivery, and the first 6 weeks after birth . To be cared for by a midwife, a woman must be healthy, and her pregnancy must be progressing normally. This is usually the case for 80% of expectant mothers.
A midwife is a member of a professional order that ensures the protection of the public. Entering the profession requires completing a four-and-a-half-year university program. Midwives therefore have the necessary knowledge to provide women with safe care, quickly detect potential complications, and respond appropriately to emergency situations. They can also prescribe any medications or tests that mom or baby may require while under their care. If complications arise, the midwife will consult a physician or transfer the mother’s care to a physician.
Midwifery is based on respect for pregnancy and childbirth as normal physiological processes. Midwives therefore favour a holistic approach and respect parents’ choices.
They work in teams of two or three to ensure there is always a midwife available to look after the mother’s needs (24 hours a day, 7 days a week). One member of the team will be specifically assigned to the client and provide most of her care. However, she will meet the other midwives during her third trimester so that she feels at ease should one of them be on call when she goes into labour.
A midwife can provide support during labour and birth in a birthing centre, at the hospital, or at home. Their approach will be the same regardless of the birth location. In all cases, midwifery services are covered by the Régie de l’assurance maladie du Québec.
Finding and being cared for by a midwife
A woman who is interested in midwifery care must first apply at her local birthing centre. She will then be invited to an information meeting with a midwife, which will be held at the birthing centre prior to the start of care. At the first appointment, the midwife will assess the woman’s eligibility for midwifery care.
In general, moms-to-be have 10–12 prenatal visits with a midwife. Appointments occur once a month for the first few months, becoming more frequent as the pregnancy advances. Each one lasts approximately 50 minutes.
The expectant mom may bring her partner or anyone else she’d like, including kids. Most consultations take the form of a dialogue, where the woman can discuss any concerns with her midwife. Potential topics include nutrition, common ailments during pregnancy, and available tests. The midwife will also help her client prepare for childbirth by discussing the options at her disposal, among other things. In addition, the midwifery team will offer prenatal classes.
During prenatal visits, the midwife checks that the pregnancy is going well . They perform clinical examinations and can order tests and analyses, as well as ultrasounds. They can also take samples to have them analyzed at a hospital centre, which will send back the results.
Pregnancy monitoring takes place at the birthing centre. However, the midwife will help the expectant mom choose a birth location during pregnancy. About 75% of births overseen by a midwife take place at birthing centres, 20% occur at home, and 5% occur in hospitals.
Childbirth with a midwife
At the first signs of labour, the pregnant woman will contact her primary midwife or a team member, depending on the on-call schedule provided in advance. The midwife will then head to the chosen birth location to meet her. Midwives are alone with their client during the first stage of labour.
While the midwife is responsible for ensuring that labour goes smoothly and that the baby is okay, the mother-to-be chooses the positions she finds most comfortable. She’s also free to choose whether she wants to eat, listen to music, or relax in a bath.
Another midwife will arrive just before delivery , when it’s time to push. This may be their first time meeting the client. The second midwife’s role is to assist the primary midwife during the second stage of labour. A birth attendant may also be present to provide additional assistance.
In the event of complications during labour, the midwife will consult a physician and transfer care to a medical team if necessary. About 16%–18% of births that begin with a midwife are ultimately transferred to a hospital. These are rarely urgent cases; most are done on a preventive basis. The two main reasons for transferring care are prolonged labour and a request for an epidural.
Birthing centres
Birthing centres are small, welcoming spaces that operate within the health care system and provide an alternative to hospitals . The number of women being cared for at a particular birthing centre is limited to maintain a sense of intimacy.
Birthing centres are also designed to provide a family setting for the women they serve. Family and children are welcome. Many birthing centres have a playroom for kids, as well as a kitchen and living room for parents.
Birthing centres offer all the necessary conditions for a safe delivery. They have all the equipment and medications required to respond to emergencies. In addition, they are fully prepared to transfer clients by ambulance to a hospital if necessary. If transfer of care to a physician is necessary, the midwife will accompany mother and baby and remain in charge of their care until the team at the hospital takes over.
Home delivery
If a woman chooses to give birth at home, her midwife will provide her with a form to sign with the information she needs to make an informed choice. This document will cover the details, advantages, and risks of each birth location. It will also describe situations requiring transfer to a hospital, emergency measures in the event of complications, and the criteria for transportation from the client’s home to the hospital.
Prior to the 36th week of pregnancy, the midwife conducts a home visit. This allows them to determine whether the residence is accessible to paramedics and within reasonable distance of a hospital.
When attending to a home birth, midwives have all the necessary equipment and medications to respond in an emergency . An agreement with the nearest hospital also ensures that the client or her baby can be transferred quickly if necessary.
A 2015 Ontario study concluded that planned, midwife-assisted home births are safe and may even result in fewer interventions for healthy women.
Things to keep in mind
- A midwife is a health care professional who provides care and services during pregnancy, delivery, and the postpartum period.
- A midwife can attend a birth in a birthing centre, at home, or in a hospital.
- To be followed by a midwife, the mother-to-be must be healthy, and her pregnancy must be progressing normally, which is the case in about 80% of pregnancies.
Photo: iStock.com/kzenon
Healthdirect Free Australian health advice you can count on.
Medical problem? Call 1800 022 222. If you need urgent medical help, call triple zero immediately
healthdirect Australia is a free service where you can talk to a nurse or doctor who can help you know what to do.
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
Maternity care in Australia
Select language: (Arabic) العربية , বাংলা (Bengali) , 简体中文 (Simplified Chinese) , 繁體中文 (Traditional Chinese) , Tiếng Việt (Vietnamese)
- In Australia, your choices for pregnancy care are linked to where you plan to give birth. A wide range of options is available.
- During your pregnancy you can get care from a midwife, GP or obstetrician — or a combination.
- You can give birth in a public or private hospital, a birth centre or at home, depending on whether your pregnancy is high or low risk and where you live.
- Once you find out that you’re pregnant, see your doctor as soon as possible to plan your care options.
- Pregnancy care is very important even if your pregnancy is going well. It helps to keep you and your baby healthy and to manage any problems early.
If you are pregnant or planning to become pregnant, there are many different options for care and support during pregnancy and birth. This article gives options for pregnancy care, where you can give birth and the costs involved so you can make the choices that are best for you.
If you have just found out that you are pregnant, it’s important to see your doctor (GP) or midwife to start your antenatal care .
In Australia, your options for antenatal care are linked to where you plan to give birth. If you want to give birth in a hospital or birthing centre, it’s a good idea to book in as early as possible.
Who will I see during my pregnancy?
There are 3 types of health professionals who can look after you during your pregnancy, depending on your health needs and where you plan to have your baby.
A midwife has special training to support and care for you during pregnancy, labour and birth. Midwives work in public and private hospitals, with obstetricians and in the community. They help you to stay healthy in pregnancy. If there are no complications, they can also help you give birth. Midwives also care for you and your baby in the first few weeks after the birth.
An obstetrician is a doctor who has had special training to look after you and your baby during pregnancy, birth and straight after birth. You might choose to have an obstetrician look after you throughout your pregnancy and to deliver your baby. If you are having your baby in a public hospital, you might only see an obstetrician if there is a medical need.
General practitioners (GPs) are doctors who promote general health and treat many different health problems. Often your GP will be the first health professional you see if you think you are pregnant.
GP obstetricians are GPs who have additional training in women’s health. They offer shared care. This is where you see your GP as well as midwives or obstetricians for your pregnancy care. If you live in a rural or remote area, your GP might provide all of your pregnancy care and deliver your baby.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, obstetricians, hospitals and other health services.
What is antenatal care?
Antenatal care is the care you receive during pregnancy. You will have antenatal appointments throughout your pregnancy. Most females who have uncomplicated pregnancies have about 8 to 10 appointments. If you’ve had a previous pregnancy with no complications, you may have about 7 to 10 appointments.
Antenatal appointments are important even if you are healthy and your pregnancy is going well. They allow your midwife or doctor to check your health and your baby’s health so they can find and manage any problems early on. These appointments are also a good opportunity for you to ask questions and talk about any concerns you have.
When should I make an appointment?
It’s best to make your first antenatal appointment when you are about 6 to 8 weeks pregnant (usually, this is 6 to 8 weeks after your last period started). This appointment can be with a midwife, your doctor or at a clinic or hospital. Typically this appointment will be with your GP.
At this appointment, the doctor or midwife will confirm that you are pregnant. They will do a thorough health check. This will include asking about your medical history and your family’s medical history.
They will discuss your pregnancy care with you, including:
- where you plan to give birth
- where you will go for antenatal care appointments and which health professionals you will see
- how many appointments you will most likely have
- where you can go for antenatal classes
They may also offer you tests to check for health conditions that may cause problems during pregnancy or labour. You can decide whether to have the tests or not.
How often will I have antenatal appointments?
You will have regular appointments throughout your pregnancy. At these appointments your doctor or midwife will check yours and your baby’s health, and offer you tests that are available at your stage of pregnancy. Many people start off having appointments every 4 to 6 weeks. From about 24 weeks of pregnancy, your appointments will become more frequent. Most people who have uncomplicated pregnancies usually have about 7 to 10 appointments in total. If you or your baby develop a health risk during your pregnancy, you may need extra appointments or tests.
You can also go to antenatal classes to help you and your partner, if you have one, get ready for the birth. Many hospitals run antenatal classes. You can ask your doctor or midwife what they recommend.
Where can I give birth?
There are several options for where you can have your baby . The options available to you depend on whether there are complications and where you live.
Making the best choice for you depends on what’s important for you and your partner. For example:
- What can you afford?
- Do you want to see the same doctor or midwife at every visit?
- Would you like your GP to look after you through your pregnancy?
- What kind of medical intervention or pain relief would you like during birth?
Your GP can discuss your options and help you decide what’s best for you. You may also choose to talk to your friends and family about their experiences. Keep in mind, pregnancy and birth preferences and experiences are different for everyone.

Public hospital
If you choose to give birth in a public hospital and your pregnancy is low-risk, you will most likely book in at the local maternity hospital for your area.
The hospital may offer several models of antenatal care that you can choose from, such as seeing midwives at the hospital’s antenatal clinic or shared care between the hospital and a GP. Many hospitals offer a service where you can see the same midwife or group of midwives throughout your pregnancy. You will be referred to a doctor if there are complications.
The first step is to see your GP who will discuss the options at different hospitals in your area and give you a referral.
Some advantages of public hospital care are:
- You may be able to choose your model of antenatal care.
- You can have minimal intervention during birth if you choose, while still having access to medical intervention if you need.
- Medicare covers most of the cost of care during the pregnancy and birth.
- Most major public hospitals can care for you and your baby if there are complications.
- You may be able to see allied health professionals if needed.
Some disadvantages are:
- You might not be able to see the same midwife or doctor throughout your pregnancy.
- The midwives or doctors you see during pregnancy might not be at the birth.
- You won’t be able to choose which midwife or doctor you see.
- After the birth, you’re more likely to be in a shared hospital room.
Private hospital
If you decide to give birth in a private hospital , you will be cared for by a private obstetrician or GP obstetrician. You will need to book in at one of the hospitals where your doctor works.
You will see the same doctor throughout your pregnancy and develop a relationship with them. The hospital midwives will look after you during your labour and your doctor will usually be there for the birth. The hospital midwives and your doctor will look after you after the birth. Most people who choose a private hospital pay for it with their private health insurance .
The first step is to see your GP for a referral to an obstetrician, who will then book you into the private hospital.
Some advantages of private hospital care are:
- You can choose the doctor who will care for you throughout pregnancy, labour and after birth.
- You might be able to choose a more convenient location for your care.
- You will have the option to stay in hospital for a few days after birth.
- It’s expensive if you don’t have private health insurance.
There are usually extra costs that your insurance doesn’t cover. This may include a fee for an anaesthetist or paediatrician if you need one.
Birth centre
Birth centres provide a more home-like environment to give birth than a hospital. They are an option if your pregnancy is low-risk and your birth is expected to be uncomplicated. A midwife or team of midwives will care for you during pregnancy, labour and birth. You might also see an obstetrician if there are any complications during your pregnancy. Birth centres usually don’t offer epidurals .
You’ll probably go home within 24 hours after birth, with care from midwives at home afterwards.
Birthing centres are often attached to hospitals. If a problem develops during your labour, you may need to move to the hospital for medical care.
See your doctor as soon as possible to find out what’s in your area and book in.
You can choose to have your baby at home as long as your pregnancy is low risk. You might still be transferred to hospital during the birth if there are any complications.
If you want to have a homebirth, you can choose to have your antenatal care with a private midwife or through a public hospital that has a homebirth service, if this is available in your area. If any problems develop, you may need to see an obstetrician.
You will need a referral from your doctor for a public homebirth service. You can find a private midwife on the Homebirth Australia website. You can book in to your local hospital as well, just in case complications arise.
It’s important to make sure that your midwife is registered and qualified for homebirths. Check that they have procedures in place to refer you to an obstetrician if you need this and to transfer you quickly and safely to hospital if a problem arises during your pregnancy or birth.
You will also need to make sure that your baby get any treatments they need after birth, and that your midwife or doctor will care for you after birth, examine your baby within the first week and refer your baby for standard newborn tests.
What is shared care?
Shared care is when your pregnancy care is shared by your GP and the hospital or birth centre. You see your own doctor throughout your pregnancy and go to the hospital for some appointments and to give birth. This is an option if your pregnancy is low risk.
If your GP doesn’t offer shared care, your hospital can give you a list of GPs who do. Some hospitals offer shared care with midwives or obstetricians.
How long after the birth will I come home?
After the birth, you might go home the next day, or you might need to stay in hospital for several days. Some people can go home from 6 hours after giving birth. How long you stay will depend on your recovery, where you give birth, whether you have had a caesarean birth , and whether you or your baby have any complications.
How much does it cost?
The cost of having a baby will vary depending on whether you give birth in the public or private system . There are advantages and disadvantages to both.
In Australia, pregnancy care in a public hospital or birth centre costs very little because it is mostly covered by Medicare , which covers Australian citizens and some visitors to Australia. In the private system, you will need to pay for your care or take out private health insurance . Medicare and your health fund will cover some of the costs of a private hospital stay, but you may still have to pay extra fees (known as 'out-of-pocket' costs).
Be sure to check that your private health insurance covers maternity care, and whether there is a waiting time before you can claim.
It can be difficult to understand the costs of different care options. Talk to your doctor, hospital or health fund if you are unsure, or call Pregnancy, Birth and Baby on 1800 882 436.
Resources and support
For information, advice and support during your pregnancy:
- Talk to your doctor or midwife.
- Contact Pregnancy, Birth and Baby to speak with a maternal child health nurse by phone on 1800 882 436 or via video call .
- Call healthdirect on 1800 022 222 to speak with a nurse.
Last reviewed: June 2022
Related Pages
- Your baby and the first few weeks
Need more information?
These trusted information partners have more on this topic.
Top results
Pregnancy and Maternity Care
The midwife and any other medical staff who are present should talk with you throughout your labour and birth.
Read more on Rahma Health website

If you are pregnant or planning a pregnancy, find out what care, support and services may be available to you in Australia.
Read more on Pregnancy, Birth & Baby website

Antenatal Care during Pregnancy
Once you are pregnant, your first antenatal appointment will ideally take place when you are about 6 to 8 weeks pregnant.
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website

Antenatal care during your pregnancy
You receive antenatal care from your GP, midwife or obstetrician. You’ll be offered tests and scans and your health and your baby’s will be checked.
Labour and Birth
Read this article to learn about your right to receive respectful maternity care.
Preconception & Early Pregnancy
There are many different types of antenatal care and birth options in Australia.
Pregnancy at week 7
Your baby is now about 1cm long and if you haven’t seen your doctor yet, now is a good time to start your antenatal care.
What does your GP do in pregnancy care?
Your doctor, or GP, is likely to be the first health professional you see when you’re pregnant. Read more about how GPs help with your antenatal care.
Pregnancy and birth care options - Better Health Channel
Pregnant women in Victoria can choose who will care for them during their pregnancy, where they would like to give birth and how they would like to deliver their baby.
Read more on Better Health Channel website

Your first antenatal visit
If you are pregnant, find out when to have your first antenatal care visit and what will happen at the appointment with your doctor or midwife.
Alternative packages of antenatal care for low-risk pregnant women | Cochrane
Authors' conclusions: In settings with limited resources where the number of visits is already low, reduced visits programmes of antenatal care are associated with an increase in perinatal mortality compared to standard care, although admission to neonatal intensive care may be reduced
Read more on Cochrane Australia website

RACGP - Type 2 diabetes, reproductive health and pregnancy
Reproduced with permission from The Royal Australian College of General Practitioners. The spectrum of reproductive health problems in diabetes is broad, topics include pregnancy and sexual health.
Read more on RACGP - The Royal Australian College of General Practitioners website

Intermittent regimens of iron supplementation during pregnancy | Cochrane
Authors' conclusions: This review is the most comprehensive summary of the evidence assessing the benefits and harms of intermittent iron supplementation in pregnant women on haematological and pregnancy outcomes
COVID-19 vaccination when pregnant or breastfeeding and for those planning pregnancy - RANZCOG
The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) acknowledges the risk posed to the community, healthcare workers, and all patients, due to the COVID-19 (coronavirus) pandemic
Managing Mastitis | Ausmed
Mastitis is characterised by an area of inflamed breast tissue and accompanied by pain and fever, it is a distressing condition which can negatively impact a mother’s ability to breastfeed.
Read more on Ausmed Education website

RACGP - Red Book - Preventive activities in children and young people
Reproduced with permission from The Royal Australian College of General Practitioners
Healthdirect Australia is not responsible for the content and advertising on the external website you are now entering.
Healthdirect 24hr 7 days a week hotline
24 hour health advice you can count on
1800 022 222
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
Support for this browser is being discontinued
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.

Primary Navigation
Secondary navigation.

Mayor Adams Announces Over 12,000 Families Served With Maternal and Infant Health Services Since Expanding Access to Doulas and Home Visitors
May 13, 2024
Services Address Racial Disparities in Maternal Health for Black and Brown New Yorkers
Advances Adams Administration's Goal in HealthyNYC to Reduce Black Maternal Mortality by 10 Percent by 2030
NEW YORK – New York City Mayor Eric Adams and New York City Department of Health and Mental Hygiene (DOHMH) Commissioner Dr. Ashwin Vasan today announced that, since expanding access to doula and midwifery services two years ago , over 12,000 families have been served with home visits by the New Family Home Visits Initiative . The $34 million initiative offers support services and referrals to new and expectant parents by having trained health workers – such as a nurses, doulas, lactation consultants, or community health workers – make in-person or virtual visits to the home of a new or expecting parents, identifying maternal health needs during pregnancy or soon after childbirth, preparing families for delivery and a new baby, and connecting families to needed services essential to the well-being of mothers, children, and families. The New Family Home Visits Initiative includes the Newborn Home Visits Program, Nurse Family Partnership, and Citywide Doula Initiative.
As of December 2023, approximately 9,500 families were served by the Newborn Home Visit Program, 1,200 by the Nurse Family Partnership, and 1,900 by the Citywide Doula Initiative. As the city aims to reduce Black maternal mortality by 10 percent by 2030 through HealthyNYC – New York City's ambitious plan to improve and extend the average lifespan of all New Yorkers – this milestone represents the Adams administration's continued commitment to building healthier families and communities across the five boroughs.
"Since day one, our administration has been committed to supporting expecting families and tackling maternal mortality," said Mayor Adams . "The numbers are clear: Black New Yorkers are four times more likely than white New Yorkers to experience a pregnancy-associated death. Our administration has taken action to boost birth equity – expanding the doula program citywide, signing a package of bills to strengthen maternal health, and setting the ambitious goal of reducing Black maternal mortality by 10 percent by 2030. Since we expanded access to doulas, lactation consultants, and nurse visits, we are proud to have connected over 12,000 families across New York City with services that are supporting families. Our children are our most precious resource, and by investing in them and their families from the start, we'll build a safer and healthier city for generations to come."
"Today's announcement demonstrates our long-standing commitment to reshaping our maternal health system to engage a broader care team including doulas, lactation specialists, and others to give every expectant person and family the support they need before and after welcoming their new family member," said Deputy Mayor for Health and Human Services Anne Williams-Isom . "Furthermore, we set a goal through HealthyNYC to reduce Black maternal mortality by 10 percent by 2030, as Black women are four times more likely to experience a pregnancy associated death compared to white women in New York City. We will continue to work to close these equity gaps and give every family the healthy, supportive foundation they need to thrive."
"Supporting maternal and infant health in a way that centers an individual family's needs is essential to building trust and a strong foundation for a healthy future," said DOHMH Commissioner Dr. Vasan . "We are committed to reducing maternal mortality rates as part of our efforts to increase New Yorkers' lifespans and healthspans, and the New Family Home Visits Initiative offers valuable accompaniment and support to ensure the healthiest start to life possible."
To simplify the referral process and make it easier for families to be quickly connected to home visiting programs, the New Family Home Visits Initiative implemented the nation's first citywide, web-based coordinated intake and referral system. This system matches families to programs and community resources that best fit their needs and for this effort, DOHMH was awarded the Government Technology Best of New York City Award in November 2023.
Comprised of three programs, the New Family Home Visits Initiative connects new and expecting parents with thoughtful care for every expecting and new family. The Newborn Home Visits Program has served approximately 9,500 families in just over two years and offers no-cost in-person and virtual home visits to families with a new infant (zero to three months) to facilitate the adjustment to parenthood, assure a safe living environment for families, provide topic-specific education, and identify health and social issues that require referral to community-based services. The Nurse Family Partnership is an evidence-based nurse home visiting program that pairs clients with registered nurses to receive regular visits from early pregnancy until their child's second birthday. The program has served approximately 1,200 families since March 2023. Finally, the Citywide Doula Initiative served more than 1,900 clients since its launch in March 2022, including support during approximately 1,300 births. As part of the city's program, doulas provide prenatal home visits, continuous support during childbirth, and four postpartum visits. Doulas also help clients establish and maintain breastfeeding and help with parent-infant bonding. In addition to this traditional doula care, clients receive case management services through screenings and referrals. Additionally, through a partnership with Ancient Song Doula Services, the Citywide Doula Initiative trains at least 30 community members as doulas each year.
Tackling maternal mortality is an urgent priority for the Adams administration, as research shows that Black New Yorkers are four times more likely than white New Yorkers to experience a pregnancy-associated death. From 2016 to 2018, data shows that 72 percent of pregnancy-associated deaths among Black mothers were preventable , compared to 43 percent for white mothers and 65 percent for Latina mothers. The Adams administration has taken action to strengthen birth equity, expanding the doula program citywide, signing a package of bills to strengthen maternal health, and setting the ambitious goal of reducing Black maternal mortality by 10 percent by 2030 through HealthyNYC.
In January 2024, following his State of the City address , Mayor Adams announced Women Forward NYC , a more than $43 million investment aimed at making New York City a national leader on gender equity, including for transgender and gender expansive New Yorkers, with the ambitious goal of becoming the most women-forward city in the United States. Supported through city dollars, private and public partnerships, academic institutions, and federal grant funding, the action plan addresses gender disparities by connecting women to professional development and higher-paying jobs; dismantling barriers to sexual, reproductive, and chronic health care; reducing gender-based violence against women; and providing holistic housing services, including for formerly incarcerated women and domestic and gender-based violence survivors.
"I commend Mayor Adams and Dr. Vasan for making strong investments in the New Family Home Visits Initiative two years ago and ultimately bringing needed services to some 12,000 new and expectant parents in our city," said New York State Senator Roxanne J. Persaud . "This $34 million initiative, built on a strong base of existing maternal health supports, expanded access to the doula and midwifery care that many expectant mothers want."
"This Mother's Day, we recommit to uplifting all the mothers that are the lifeblood of our families and our city," said New York State Assemblymember Jenifer Rajkumar . "I applaud Mayor Adams and Dr. Vasan on reaching the historic milestone of serving over 12,000 families under the New Family Home Visits Initiative. Through this program, new and expectant mothers have received convenient house calls from expert health workers, so they have the best possible outcomes. The program is an essential tool to reach our goal of reducing Black maternal mortality by 10 percent by 2030, a critical objective to close the gap of Black mothers being 2.5 times more likely to die in pregnancy. In Albany, I have built upon this work by introducing legislation to provide benefits to women who suffer the tragedy of stillbirth. Together, we are committed to the health of women in our city."
"For Black New Yorkers, and others in communities of color, doula care can make the difference between life and death," said New York City Council Speaker Adrienne Adams . "As a women-majority Council, we have consistently prioritized addressing racial disparities in maternal health outcomes, enacting 11 laws to expand access to doula care and other critical services for birthing people. Through investments by the city, over 12,000 families in underserved neighborhoods have been provided with life-saving resources, which will have lasting health benefits for children, mothers, and communities for years to come. We are proud of the impact these commitments have produced and will continue to prioritize expanded access to maternal health care that ensures families have access to these vital services."
"New York City is demonstrating how local governments across the United States can and must take bold action to address racial disparities in maternal health and defend access to safe reproductive healthcare," said New York City Councilmember Carlina Rivera. "I commend the administration for their continued commitment to creating and enhancing services to serve new parents that improve outcomes across the boroughs."
"Maternal health has been a priority for the City Council since day one, resulting in legislation and funding to support doula and mid-wife services which are so crucial to pregnant people," said New York City Councilmember, chair, Health Committee, Lynn Schulman . "Today's announced milestone demonstrates the importance of bridging healthcare disparities and empowering families to thrive."
Media Contact
[email protected] (212) 788-2958
Home visits by midwives in the early postnatal period
The postnatal period is a vulnerable time that involves reorientation and new experiences. Early visits by a midwife may therefore help enhance the women’s perception of coping.
Background: Postnatal care has changed over the years. The period spent in the maternity ward has gradually been reduced from five to six days to approximately two days. According to health policy, women’s and their families’ experience of pregnancy, childbirth and maternity should be coherent and holistic and provide a sense of security.
Objectives: The aim of the study is to shed light on women's experiences with home visits by a local midwife in the early postnatal period.
Method: The study is qualitative. We conducted nine semi-structured individual interviews. We analysed data by using a qualitative content analysis inspired by hermeneutic interpretation and a systematic condensation of text. The study is based on the theory of health promotion, empowerment, coping, autonomy and the relationship between the midwife and the mother.
Main results: Three main categories describe the women’s experiences:
- having control themselves,
- knowledge and support, and
- continuity and relationship with the midwife.
Conclusion: This study indicates that home visits by local midwives may contribute to women being able to cope with the new circumstances in their lives. Being able to meet women’s individual needs seems to enhance empowerment. Midwives and health visitors have different skills that can complement each other and contribute to promoting health in the postpartum period.
Postnatal care has gradually changed over recent years. Previously, the mother and child would spend five or six days in the maternity ward after a normal birth. Now, they generally go home after one or two days, depending on the woman’s health condition (1). The programme for follow-up in the early postnatal period has not been organised to keep pace with these changes. Most pregnant women are followed up by a midwife and doctor in the municipality throughout the pregnancy and give birth in a hospital with the assistance of a midwife employed at the hospital. The woman then moves to a maternity hotel or ward, where she meets other midwives whom she does not know from before.
The health visitor is usually the first person to establish contact with the woman after her return home, seven to fourteen days after the birth. The postnatal period is a vulnerable time of reorientation and new experiences, during which most women may feel a need for information and support. As a result of the pregnancy and birth, the bodily, mental and social changes may represent challenges for the women concerned (2, 3).
Guidelines for postnatal care
The national professional guidelines for postnatal care were published in 2014 to help ensure appropriate and predictable postnatal care. The municipalities provide maternity services that vary in scope and content, and the Board of Health Supervision has pointed out that the time elapsing from the women’s discharge from hospital until they contact the public health centre represents a critical period (1). The Coordination Reform provides instructions for more effort in health promotion and disease prevention. The reform proposes to bestow a key role on the municipal midwife services in the follow-up of mother and child during the first days after birth (4).
The objective of postnatal care is to help the woman establish a better sense of coping and enable her to take charge of her new life situation to the greatest possible extent, in the best interests of herself and her family (1). The midwife and the health visitor possess different skills, but in their follow-up in the early postnatal period their focus in overlapping. The national professional guidelines for postnatal care recommend that both of them undertake home visits (1).
Before the publication of the national professional guidelines for postnatal care, only very few women were visited at home by the midwife immediately after giving birth, since home visits were not included in the tasks of municipal midwives. At the time of writing, only a few municipalities have made provisions for early home visits by a midwife, and there are few studies available of postnatal care practices in Norway (1, 5).
The importance of home visits
Searches for previous research on this topic show that some studies investigate postnatal care in hospitals, while others focus on women and post-partum depression. A number of studies conclude that home visits by a midwife are important. These conclusions are based on investigations of the differences between provision of postnatal care in hospitals and in the home (6, 7), women’s experience of early discharge (8) and parents’ perception of relational continuity when midwifery students provided follow-up during the antenatal, perinatal and postnatal period (9). This study details women’s perceptions and experiences with home visits by a municipal midwife immediately after being discharged following childbirth.
Our research questions are the following:
- What could be the importance of early visits by a midwife with regard to the woman’s perception of coping in her new life situation?
- How can the midwife help in accommodating the woman’s needs in the context of home visits?
- What significance does it have for the woman that the home visit is undertaken by a midwife?
The study is based on theories of empowerment, in the sense of having as much control as possible over issues that may affect personal health. The study emphasised co-determination, redistribution of power and recognition of the woman’s competence in relation to herself (11). The correlation between relational work, perception of coping and autonomy can be regarded as fundamental for health promotion.
The research design is descriptive, with some explorative elements. We chose to use a qualitative methodology to elucidate the research question (12, 13).
We conducted nine semi-structured individual interviews. The interview guide focused on the woman’s perception of her new life situation, the experience of coping in the early postnatal period, perceptions and experiences associated with the home visit by a midwife and the relationship to the midwife.
Regional committees for medical and health research ethics (REC) have determined that the study falls outside of their mandate (reference number 2013/1140 A). The study has been reported to the Norwegian Centre for Research Data (NSD) (project number 34872) and has been implemented in compliance with guidelines for research ethics (14).
Participants
Since the first author was familiar with the field, she contacted the director of the health services and midwives in the three municipalities that conducted projects on early home visits by a midwife. Most of the visits were undertaken by the same midwife. The women were recruited through convenience sampling (15). The first author requested the municipal midwives to recruit participants consecutively after having undertaken the visit, in order to avoid selective recruitment. All the women who were asked consented to participate in the study.
The inclusion criteria were the following: a healthy child born at full term, home visit by a midwife from one to six days after birth, Norwegian-speaking, and the participation should not represent an undue burden. The participants included six primiparous and three multiparous women. The home visits were undertaken by four different midwives.
Data collection
The first author, who had no previous knowledge of the women involved, was responsible for the collection of data. She interviewed the women in their homes in the period from November 2013 to January 2014. Only the mother and child were present during the interviews, which lasted for an average of one hour. The interviews were recorded on an audio device and transcribed verbatim.
We analysed the data with inspiration from hermeneutic content interpretation and systematic text condensation (12, 16). The systematic procedure for text condensation helped achieve an appropriate handling of the large amount of text. In addition, the principles for hermeneutic content interpretation helped elicit valid interpretations in a hermeneutic perspective. This perspective implies that any interpretation depends on the prior understanding on which it is based (12).
Table 1 shows the four stages of the analysis process.
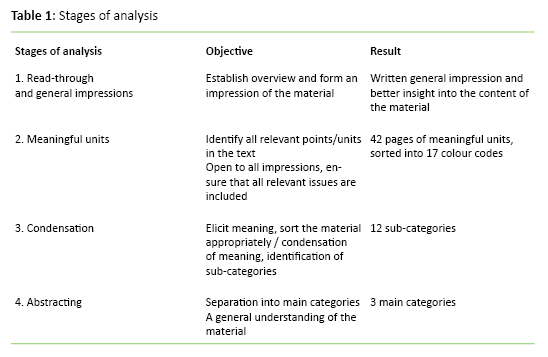
The first author repeatedly read through the entire material. She made notes of reflections and ideas along the way, before writing down the general impression. The condensation took place in an iterative process that involved all the authors, back and forth between the research questions, general impressions and units of meaning. The abstracting took place in the same way. Research questions, general impressions and sub-categories were assessed in light of each other until the categorisation became meaningful on the basis of findings and research questions. During the analysis process we focused on being aware of our preconceptions, using notes and discussions as an aid, in order to ensure valid interpretations.
Table 2 shows the categories that emerged during the analysis.
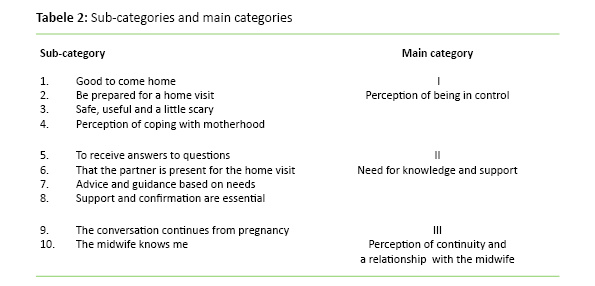
The perception of being in control
The women felt that the home visit helped provide security and calm in a hectic postnatal period. Many of them told us that they looked forward to the midwife’s visit. The women were aware of what the midwife could provide, and that the visit was voluntary and agreed beforehand. The women thus felt that they were prepared for the visit and in control of the situation:
‘When you come home, it’s much calmer than being in the hospital, it’s easier to think through the things that you wonder about or questions to be asked.’
‘It was very good that we were prepared ... that way, the entire process becomes natural and informal.’
The women felt more secure when receiving support and confirmation from the midwife.
Prior to the home visit, many of the women had believed that the visit would entail checking or assessment of the home and of them as parents. One of the mothers described it as ‘scary’. All the women described the sense of security and the advantage of receiving help based on their own needs as the key element of the home visit:
‘The impression that I had beforehand, what I learned from others, was that they come to check that everything is in order in the house and all that, but certainly also because it was the midwife, it felt just like having a friend visiting, a friend who also has the knowledge.’
The women described various experiences of coping associated with matters being as expected, and that they were able to cope with new roles and tasks. One woman had a strong perception of coping in the context of the birth itself. She described it as important for her to share this experience with the midwife during the home visit:
‘So that was really great, because now I can finally do it, and had the confirmation that I can’ (breastfeeding).
‘We did everything ourselves ... I really felt that sense of coping.’
The need for knowledge and support
During the home visit, it is crucial that the women receive answers to their questions, advice and guidance. The participants described the conversation with the midwife about the pregnancy and birth as essential for their understanding and confirmation:
‘We had prepared ourselves ... made notes of questions and such, so that we could ask about what we were unsure of.’
‘Then we talked a lot about the birth ... I really needed that – that it was her I told what I felt about or what my hopes were before the birth ... because she had been involved all the way, even though she hadn’t been present during the birth itself.’
The partner’s role in the home visit was underscored as essential, because the partner could support the woman. The partner’s questions and experiences were considered:
‘It was good that he could be there too, then we receive the same information, and he also had some questions.’
Many reported that preparing adequately for the postnatal period was difficult, and that manoeuvring through the available information could present problems:
‘No matter how well one prepares, one can never prepare enough, because one cannot know what lies ahead.’
The women’s need for counselling and guidance varied from simple advice and confirmation of normality to more comprehensive guidance regarding matters such as breastfeeding, the birth or how to cope with overwhelming emotions. The women reported feeling safer in their new role after having been provided with support and confirmation by the midwife:
‘I feel quite a lot more trust in the midwife, it’s because I know that she’s a midwife, she knows about me too, not just the baby.’
‘It’s important to hear when one is so uncertain and emotional and very fearful of doing something wrong’ (about confirmation).
Perception of continuity and the relationship to the midwife
The home visit was described as meaningful and informal. The continuity in the relationship between the woman and the midwife emerged when the woman reported that the midwife was familiar with her condition during pregnancy and that the conversation ‘flowed’ immediately. Many described how they continued the conversation with the midwife during the consultations at the public health centre:
‘With the midwife it’s like: “Hello, how did the birth go?” and then we just start chatting.’
‘After all, the midwife knows how things have gone from day one, that makes it a different conversation.’
Many of the women reported that they felt confident in discussing their emotions and experiences. The relationship to the midwife was important and appeared to help reinforce the woman’s sense of coping. One of the women was previously unfamiliar with the midwife, but described how she felt the visit was useful because of the help and support that it provided to her:
‘It wouldn’t have been as easy to sit there and be open about emotions and the birth experience with someone who does not know you a little from before.’
‘When we were talking and I was telling her about it all, I could breathe, I felt relieved.’
The women felt confident about their early discharge from the maternity ward when knowing that the midwife would come in a couple of days. Because information about the visit was provided beforehand, the woman could take control of the situation and choose whether or not to make use of this option. We interpret this to mean that predictability was important to the women. A Norwegian study confirms that being able to choose for oneself inspires confidence (17). Pursuant to the Patients’ and Users’ Rights Act, the woman is entitled to choose whether or not to accept a home visit (18).
The fact that the women believed that the visit involved being checked, can be seen as indicating that the women were in a vulnerable situation in their new role. The asymmetry of the situation, in which the woman was in need of the midwife’s help, may also have had an effect. Ruyter and collaborators claim that autonomy is not a constant, but varies in light of the condition and situation of the individual (19). The postpartum woman is in a vulnerable situation, and it may therefore be said that her autonomy may be limited. Establishing a good relationship may help the party involved in the relationship reinforce and regain her autonomy (20, 21). After the visit, none of the women felt that it had constituted a control measure. This might be associated with the fact that the relationship between the woman and the midwife was known, and that the midwife was skilled in building relationships.
All the women felt a need to discuss issues associated with the child’s weight and breastfeeding.
Other research shows that women who have received home visits are more satisfied than those who have been in a maternity ward. This is most likely due to the busy environment at the hospital and the perceived importance of continuity and relational interaction between the midwife and the woman (7, 8). When the woman feels accommodated and trusts the midwife and her skills, she can work to enhance her own insight and self-confidence through this relationship. Thereby, she obtains a better opportunity to make correct and autonomous decisions for herself and her child. This is crucial in the formation of a secure basis for the ties between mother and child, as well as for the child’s health in later life (20).
At the stage when breastfeeding had barely started, guidance in breastfeeding and feeding was essential. Breastfeeding is appropriate both in terms of child nutrition and bonding. Guidance on breastfeeding in the early postnatal period, combined with home visits, may help sustain breastfeeding over time (22, 23). All the women felt the need to discuss issues associated with the child’s weight and breastfeeding. Other important topics included how to understand the child’s signals, sleep balance and the woman’s own health.
This study shows that the ability to accommodate the child’s needs may help the women to feel a sense of coping. Other studies confirm that the child’s health and well-being are crucial for the mothers’ feeling of confidence (6, 24, 25). Seemingly, when the women felt confident about the condition of the child, they could start thinking of themselves and their own needs. Talking about the birth was important to the women. We interpret this to mean that a discussion of expectations and actual experiences could help enhance the understanding of the birth process. Most of the women described it as appropriate and natural to have this conversation with the midwife, whom they knew from before. However, one woman described it as rewarding despite her not having previous acquaintance with the midwife.
The women felt confident in talking to a midwife they knew from their pregnancy period.
Aune et al. found that during the home visit, attention was focused on perceptions and experiences from pregnancy and birth, more than on future events (9). These findings may confirm that the perception of coherence and understanding of the process are important to the women. This may corroborate the argument that midwifery skills are crucial in the early postnatal period. The women expressed difficulty in preparing adequately for the postnatal period, and felt secure when the midwife could contribute her knowledge and skills. Women may need support to take care of themselves during the first week of the postnatal period (26, 10).
The objective of the guidance is to support the woman and to provide her with better knowledge and skills to enhance her self-confidence and self-efficacy. She can thus better address her new life situation and have power, influence and control of the situation (27, 28). The study appears to show that attention to individual needs and the ability to cope helped promote empowerment in the woman, which is consistent with other studies (8, 9, 29).
Having their partner present during the home visit was important for the majority of the women. Giving both of them the opportunity to discuss their questions and thoughts may help bolster the chances of a positive and equal collaboration in their new family setting (30, 31). If the woman is provided with information to be shared later with her partner, this may result in an asymmetric relationship (19, 20).
Perception of continuity and the relationship with the midwife
The study shows that the women felt confident in speaking with a midwife they knew from their pregnancy period and who had competence with regard to the newborn child as well to them as women. The continuity in the relationship is claimed to help bolster the women’s trust in the midwife’s expertise, advice and guidance, and in addition, the midwife can reinforce the women’s trust in their own resources (9, 32).
Many of the women described how they were overwhelmed by the initial period. The postnatal period is a vulnerable time for the woman because of the major changes that occur in her life (20, 33, 34). The midwife’s skills in communication and relationship-building appear to have an impact on the benefits that the woman derives from the home visit. Razurel et al. emphasise that emotional and social support is more crucial than practical knowledge during the early postnatal period (35). Whether the women were facing challenges or a normal process appeared to have little bearing on the need to obtain support or confirmation from the midwife. The support and confirmation that the midwife gave regarding the women’s choices or understanding of the situation could provide them with confidence, self-efficacy and a sense of coping. These are the main elements of empowerment thinking and can thus be interpreted as evidence that the midwife may help promote empowerment in the woman (11, 28).
The midwife may use her skills and previous relationship with the mother to accommodate her individual needs (32, 36). This could be an opportunity for continuity, even if the woman and the midwife are not known to each other from the pregnancy period. The midwife’s professional skills may help the woman perceive consistency and continuity in her understanding of the process. Studies show that women are greatly satisfied with the information and guidance provided by the midwife during the home visit (7, 8).
Whether the women were facing challenges or a normal process appeared to have little bearing on the need to obtain support or confirmation from the midwife.
The tasks of the midwife and the health visitor overlap during the home visit; for example, both may provide guidance on breastfeeding. They both focus on health promotion and include the family, the woman and the newborn child, but they possess different skills. The midwife’s skills include maternal health, pregnancy, birth and the postnatal period (37). She makes a home visit one to six days after the woman’s discharge from hospital, when she mainly focuses on the woman and the newborn child. The midwife may, for example, help strengthen the woman in her new life situation, which may assist in developing her skills as a mother. The health visitor has competence with regard to children, adolescents and their families (38). She makes a home visit six days to two weeks after discharge, focusing on the child’s health and development within the family. The health visitor may, for example, help in establishing positive bonding and good family relationships.
Better collaboration and understanding between health visitors and midwives during home visits may help better adapt the follow-up options for the early postnatal period to the woman, the child and the individual needs of the family. Moreover, it is likely that better interdisciplinary collaboration and familiarity with each other’s competencies may help ensure a better utilisation of resources and competencies.
Validity of the study
The study elucidates the perceptions and experiences of women from home visits by a municipal midwife in the early postnatal period. This topic has not previously been highlighted in Norwegian studies. The first author is a midwife with experience from community midwifery services. She is familiar with the conditions related to the topic that the study seeks to explore. This knowledge may help lend considerable relevance to the questions in the interview guide, but may also entail the risk that certain elements are overlooked or underestimated. We attempted to reduce this risk by clarifying our preconceptions throughout the research process (12, 16, 39).
The fact that the first author is a midwife may have influenced the women, causing them not to report any negative aspects out of fear of appearing unfriendly. To reduce the risk of such an effect, the first author informed the participants about her role as a researcher prior to the interview. No questions related to midwifery were brought up during or after the interview. Reflections were noted immediately after the interview and used for purposes of validation during the analysis. We believe that undertaking the interviews in the woman’s home environment helps reinforce the validity and credibility of the study (40). The women were recruited by locally employed midwives on the basis of availability, which may have had an effect, in that the women’s attitude to home visits by a midwife was known in advance (15). Efforts were made to reduce this effect by recruiting the women consecutively after the home visits had been undertaken. This may help enhance the validity of the study.
The study shows that a community midwife may help establish a perception of consistency and continuity by maintaining regular contact with the woman throughout the pregnancy until the home visit. The visit may provide an opportunity to accommodate the women’s individual needs, in light of the previously established relationship and the midwife’s competence in maternal health, pregnancy, birth and the postnatal period. When the woman feels that she is regarded as ‘an expert on her own situation’, is permitted to participate in the process of identifying the best solutions and thus remain in control of her own life situation, this may help reinforce her empowerment.
Home visits by a midwife may thus help advance the woman’s perception of coping and reinforce her empowerment, which will promote the health of the woman, the child and the family. The midwife and the health visitor possess different skills, and home visits by both may be appropriate in terms of health promotion. Interdisciplinary collaboration is important, and more research on how best to make use of resources and skills is needed.
1. Helsedirektoratet. Nasjonal retningslinje for barselomsorgen. Nytt liv og trygg barseltid for familien. Oslo. 2014. Available at: https://helsedirektoratet.no/retningslinjer/nasjonal-faglig-retningslinje-for-barselomsorgen-nytt-liv-og-trygg-barseltid-for-familien . (Downloaded 18.06.2015).
2. Venheim MA. Barselomsorg : Plager og komplikasjoner. In: Tegnander E, Brunstad A. (ed). Jordmorboka: ansvar, funksjon og arbeidsområde. Oslo: Akribe; 2010.
3. Lundgren I, Berg M. Central concepts in the midwife-woman relationship. Scandinavian journal of caring sciences. 2007;21(2):220–8.
4. Helse- og omsorgsdepartementet. Samhandlingsreformen: rett behandling – på rett sted – til rett tid. Oslo: Regjeringen. 2009.
5. Den norske jordmorforening. Høringssvar. 2015. Availabe at: http://www.jordmorforeningen.no/Media/Filer/Hoeringssvar/Dnj_hoeringsvar_prioteringer_helsetjenesten_2015 . (Downloaded 15.05.15).
6. Hildingsson IM, Sandin-Bojö A-K. «What is could indeed be better» – Swedish women’s perceptions of early postnatal care. Midwifery. 2011;27(5):737–44.
7. Fenwick J, Butt J, Dhaliwal S, Hauck Y, Schmied V. Western Australian women's perceptions of the style and quality of midwifery postnatal care in hospital and at home. Women and Birth. 2010;23(1):10–21.
8. Johansson K, Aarts C, Darj E. First-time parents' experiences of home-based postnatal care in Sweden. Uppsala Journal of Medical Sciences. 2010;115(2):131–7.
9. Aune I, Dahlberg MU, Ingebrigtsen O. Parents’ experiences of midwifery students providing continuity of care. Midwifery. 2012;28(4):432–8.
10. Hjälmhult E, Lomborg K. Managing the first period at home with a newborn: a grounded theory study of mothers’ experiences. Scandinavian journal of caring sciences. 2012;26(4):654–62.
11. Tveiten S. Empowerment og veiledning : sykepleierens pedagogiske funksjon i helsefremmende arbeid. I: Gammersvik Å, Larsen T. (red). Helsefremmende sykepleie – i teori og praksis. Bergen: Fagbokforlaget Vigmostad & Bjørke. 2012.
12. Kvale S, Brinkmann S. Det kvalitative forskningsintervju. 2. ed. Oslo: Gyldendal Akademisk. 2009.
13. Polit DF, Beck CT. Nursing research. Generating and assessing evidence for nursing practice. 9. ed. Wolters Kluwer Health Lippincott Williams & Wilkins. 2012.
14. De nasjonale forskningsetiske komiteer. Forskningsetiske retningslinjer for samfunnsvitenskap, humaniora, juss og teologi. 2006. Available at: https://www.etikkom.no/forskningsetiske-retningslinjer/Samfunnsvitenskap-jus-og-humaniora/ . (Downloaded 18.06.2015).
15. Thagaard T. Systematikk og innlevelse. En innføring i kvalitativ metode. 4. ed. Bergen: Fagbokforlaget Vigmostad & Bjørke. 2013.
16. Malterud K. Kvalitative metoder i medisinsk forskning. En innføring. Oslo: Universitetsforlaget. 2013.
17. Henriksen L. Hva betyr helhet og kontinuitet i svangerskap, fødsel og barselomsorg for kvinner? En evaluering av Barsel hjemme, et prosjekt fra Oslo. 2010.
18. Lovdata. Lov om pasient- og brukerrettigheter. 2. juli 1999; nr. 63. [Pasient- og brukerrettighetsloven].
19. Ruyter KW, Førde R, Solbakk JH. Medisinsk og helsefaglig etikk. Oslo: Gyldendal Akademisk. 2014.
20. Schibbye A-LL. Relasjoner: et dialektisk perspektiv på eksistensiell og psykodynamisk psykoterapi. Oslo: Universitetsforlaget. 2012.
21. Goering S. Postnatal reproductive autonomy: promoting relational autonomy and self-trust in new parents. Bioethics. 2009;23(1):9–19.
22. Hansen MN. Barseltiden og amming. In: Tegnander E, Brunstad A. (ed). Jordmorboka: ansvar, funksjon og arbeidsområde. Oslo: Akribe. 2010.
23. Kronborg H, Vaeth M, Kristensen I. The effect of early postpartum home visits by health visitors: a natural experiment. Public health nursing (Boston, Mass). 2012;29(4):289–301.
24. Forster DA, McLachlan HL, Rayner J, Yelland J, Gold L, Rayner S. The early postnatal period: exploring women's views, expectations and experiences of care using focus groups in Victoria, Australia. BMC Pregnancy & Childbirth. 2008;8:27.
25. Persson EK, Fridlund B, Kvist LJ, Dykes A-K. Mothers’ sense of security in the first postnatal week: interview study. Journal of Advanced Nursing. 2011;67(1):105–16.
26. Fahey JO, Shenassa E. Understanding and meeting the needs of women in the postpartum period: The perinatal maternal health promotion model. Journal of Midwifery & Women's Health. 2013;58(6):613–21.
27. Tveiten S. Veiledning: mer enn ord. Bergen: Fagbokforlaget. 2013.
28. Askheim OP. Empowerment i helse- og sosialfaglig arbeid: floskel, styringsverktøy, eller frigjøringsstrategi? Oslo: Gyldendal Akademisk. 2012.
29. Askelsdottir B, Lam-de Jonge W, Edman G, Wiklund I. Home care after early discharge: impact on healthy mothers and newborns. Midwifery. 2013;29(8):927–34.
30. Rudman A, Waldenstrom U. Critical views on postpartum care expressed by new mothers. BMC Health Serv Res. 2007;7:178.
31. Ellberg L, Högberg U, Lindh V. «We feel like one, they see us as two»: new parents’ discontent with postnatal care. Midwifery. 2010;26(4):463–8.
32. Hunter B, Berg M, Lundgren I, Ólafsdóttir ÓÁ, Kirkham M. Relationships: The hidden threads in the tapestry of maternity care. Midwifery. 2008;24(2):132–7.
33. Brodén M. Graviditetens muligheder: en tid hvor relationer skabes og udvikles. København: Akademisk Forlag. 2004.
34. Reinar L,M. Barselomsorg; Plager og komplikasjoner. In: Tegnander E, Brunstad A. Jordmorboka: ansvar, funksjon og arbeidsområde. Oslo: Akribe. 2010.
35. Razurel C, Bruchon-Schweitzer M, Dupanloup A, Irion O, Epiney M. Stressful events, social support and coping strategies of primiparous women during the postpartum period: a qualitative study. Midwifery. 2011;27(2):237–42.
36. Aune I, Dahlberg U, Ingebrigtsen Or. Relational continuity as a model of care in practical midwifery studies. British Journal of Midwifery. 2011;19(8):515–23.
37. Rammeplan for jordmorutdanningen. Oslo: Regjeringen. 2005. Available at: https://www.regjeringen.no/globalassets/upload/kilde/kd/pla/2006/0002/ddd/pdfv/269373-rammeplan_for_jordmorutdanning_05.pdf . (Downloaded 18.06.2015).
38. Rammeplan for helsesøsterutdanningen. Oslo: Regjeringen. 2005. Available at: https://www.regjeringen.no/globalassets/upload/kilde/kd/pla/2006/0002/ddd/pdfv/269386-rammeplan_for_helsesosterutdanning_05.pdf . (Downloaded 18.06.2015).
39. Fog J. Med samtalen som udgangspunkt: det kvalitative forskningsinterview. København: Akademisk Forlag. 2004.
40. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004;24(2):105–12.

Barselomsorgen er til å gråte av
De fødende blir sendt hjem nesten før de er ferdige med fødselen, skriver leg

Kvinner med barseltraumer må ikke overlates til psykiatrien
Oppfølgingen av den nybakte morens mentale helse er helt tilfeldig, skriver G

Jordmødre etterlyser mobilvettregler for kvinner i barsel
Mange barselkvinner er ikke klar over hvor mye tid de bruker på mob
– Dette er vårt siste varsel, nå vil vi ha bedre barsel
Barselomsorgen er kampsak på årets 8. mars.

Her blir ingen barselkvinner skrevet ut etter seks timer
I Helse Nord-Trøndelag får barselkvinner være på sykehuset så lenge de har be

Jordmorforbundet kritisk til ny foreldrepermisjon
Jordmorforbundet frykter at det nye forslaget om en tredelt foreldrepermisjon

– Jordmorstillinger må øremerkes
Halvparten av landets kommuner mangler kommunal jordmortjeneste. De siste fir

Desperasjon fra barsel
Kristin Storrusten fikk et barn som skrek. Mye. Så fikk hun et barn til.

Må øke barselpermisjonen for kvinnen
Norge har for kort permisjon for mor etter fødsel ifølge EUs barseldirektiv,

Bekymret for barsel
Når Marte-Kari Løve har født, får hun være på barsel i 48 timer.

4 om barselomsorgen
Tre jordmødre og en helsesøster sier hva de mener.

Prioriter jordmødre, nå!

Jordmødre får ikke gjort det de skal
En av fire jordmødre avviser fødende kvinner.

Her er sykepleierne garantert riktig lønn for masterløp

Florence Nightingale: – Jeg beundrer innsatsen, men ville ikke pleiet nær kontakt

Vi lider av et fast ansatt-syndrom

Alvorlig talt, Ahus. Pleieportør?

Helseplattformen: Bruker avatarer for å dokumentere i pasientjournalen

Helse Møre og Romsdal prioriterer ikke AKS-sykepleiere eller masterlønn

Vil du jobbe på en spennende avdeling i sommer? Søk hos oss!

Journalist i Sykepleien – 100 % fast stilling
Spesialrådgiver med geriatrikompetanse.

Anestesisykepleier
Rådgiver ved fylkeskontoret i NSF Rogaland

Ønsker du faglig utvikling? Søk jobb på lungeavdelingen!

Teammedarbeidere FACT Ung

Sykepleier og spesialsykepleier til Thoraxkirurgisk intermediær og sengepost
Operasjonssykepleier - dagkirurgi.

Vil du være med å bidra til å gi våre brukere trygghet og økt livsmestring?
Book reviews.
Alle sykepleiere vil møte mennesker som i barndommen ble påført traumer
Hvordan få det bedre med seg selv og de rundt seg
Du kan bli en bedre sykepleier av å dele erfaringer
Heseblesende om et rotløst og omflakkende liv

Test deg selv
Har du full kontroll? Test deg selv med Sykepleiens fagquiz'er.

Har du et nyhetstips?
Women's experiences of remote video calls with a labour ward midwife during early labour
Affiliations.
- 1 Department of Health Sciences, University West, Trollhättan, Sweden; Institute of Health and Care Sciences, Sahlgrenska Academy, Gothenburg University, Gothenburg, Sweden; Department of Research and Development, NU-Hospital Group, Trollhättan, Sweden. Electronic address: [email protected].
- 2 School of Business, Economics and IT, University West, Trollhättan, Sweden. Electronic address: [email protected].
- 3 Institute of Health and Care Sciences, Sahlgrenska Academy, Gothenburg University, Gothenburg, Sweden; Region Västra Götaland, Research and Development Primary Healthcare, Sweden. Electronic address: [email protected].
- 4 Department of Health Sciences, University West, Trollhättan, Sweden. Electronic address: [email protected].
- PMID: 38704959
- DOI: 10.1016/j.wombi.2024.101620
Background: In an increasingly strained maternity care system with a shortage of midwives and great demands for service, pregnant women in their early labour are at risk of receiving insufficient support. Women make calls and visit the labour ward on multiple occasions before being admitted. A video call with a labour ward midwife during early labour is an unknown practice but could support pregnant women and their partners during this uncertain period.
Aim: The study aimed to describe women's experiences of remote video calls with a labour ward midwife during early labour.
Methods: A qualitative study comprising nine semi-structured interviews followed by an inductive thematic analysis was conducted.
Results: The results revealed that video calls prepared women and their partners by means of practical support. They received an assessment of early labour and the interaction with labour ward midwives prepared them for the impending birth. The participants reported feeling secure and strengthened by being met at their current stage of labour. Furthermore, they found the service accessible, easy to use and emphasised the need for increased availability and continuity.
Conclusion: This study highlights the positive impact of video calls in early labour when conducted by competent labour ward midwives. The perceived accessibility and ease of use e-health system underscore a demand for extended availability. These findings indicate the potential benefits of integrating video calls in labour care to enhance support, security, accessibility and overall satisfaction for pregnant women and their partners.
Keywords: Early labour; Midwife; Pregnancy; Remote video calls; Support; Thematic analysis.
Copyright © 2024 The Authors. Published by Elsevier Ltd.. All rights reserved.
Ritual Midwifery
Photos & videos.
See all 35 photos

Review Highlights

“ I had planned from the beginning to have a hospital birth and was working with Alana for additional support. ” in 19 reviews

“ My experience of the birth , itself, was everything that I wanted, even though nothing went the way I expected! ” in 17 reviews

“ This was such a gift for me-- I got to be in my body, focus on labor, and relax into the web of support around me. ” in 10 reviews
You Might Also Consider

Jamie S. said "I don't usually post things on yelp or do much social media because I am a fairly private person. However, after my experience as an infertility patient who can finally say I am done creating my family, I felt compelled to write…" read more
in Fertility

Sutter Urgent Care - Berkeley
0.9 miles away from Ritual Midwifery
Jamie B. said "I went to this clinic a half hour before it opened. The visit was $125 if you don't have insurance. They took me in early and I was ready to see the doctor at 1 pm. There was no wait!!!! The facility is SUPER clean and the parking…" read more
in Doctors, Pediatricians, Walk-in Clinics

Regenerate Men’s Health Medical Clinic
13.8 miles away from Ritual Midwifery
We offer innovative treatments for ED and Low T including focused shockwave therapy, intracavernosal injections, topical and injectable testosterone, sublingual medications read more
in Urologists
About the Business
We are a home birth Midwifery practice that also offers hybrid prenatal and postpartum care for families planning hospital births. …
Location & Hours
Suggest an edit
Serving Berkeley Area
Amenities and More
Ask the community.
Ask a question
Yelp users haven’t asked any questions yet about Ritual Midwifery .
Recommended Reviews
- 1 star rating Not good
- 2 star rating Could’ve been better
- 3 star rating OK
- 4 star rating Good
- 5 star rating Great
Select your rating
Overall rating

I am so grateful to Alana for her amazingly compassionate and thoughtful care. I worked with her during my third pregnancy and birth. From the very beginning Alana was so open to hearing my experience and needs and rather than trying to fit my experience into a preconceived notion, she seemed totally dedicated to listening to and responding to what was happening for me without any judgement. I felt totally supported in both talking through the emotional aspects of pregnancy and birth and medical/scientific ones. I have worked with home birth midwives before and when things got complicated I felt a slight undertone of judgement like if I had just believed more in the beautiful possibilities of birth I wouldn't be facing the more complicated medical choices that I was. With Alana I felt that all aspects of my experience and thinking was respected. She really helped me feel good about a pregnancy that I had some challenges trusting in, given my age and previous experiences. I had planned from the beginning to have a hospital birth and was working with Alana for additional support. This arrangement turned out to be invaluable. Although I had a good experience at the hospital, there was nothing like having someone I trusted deeply and had more knowledge of me as a person and my pregnancy history. I felt like Alana was really there for me even when I was at the hospital and especially when I was facing some confusing and scary medical situations. I also had a strong sense from Alana through so many little things - from the structure of her forms to the way she talked about midwifery care and issues in society that she is deeply committed to justice and sees her midwifery practice as part of it. That perspective also meant a lot to me. I deeply recommend Alana as a midwife to anyone - especially anyone who may be dealing with a more complicated pregnancy or who may be combining midwifery care with hospital care.

I had the BEST homebirth experience not only once but twice with Alana! I was pregnant with my 3rd during covid when I first sought a midwife for a natural birth at home because there was just no way I would birth at a hospital (if I could help it). So I searched and prayed that I would find a midwife that could provide care for me and would respect my beliefs and lo and behold I found Alana! Prior to meeting Alana, I did my research and came up with a birth plan. Initially, I was nervous about sharing my birth plan because I was not interested in most of the protocols that are forced upon us by the medical world. After sharing my thoughts with her, she actually welcomed me and respected my approach to birth. Under Alana's care (w/both pregnancies), I felt supported and empowered to make my own decisions. During our sessions, she always held space to discuss what was important to me and I never felt rushed. During labor, she was that comforting voice that helped me through contractions and her presence alone was very calming and reassuring. And once baby arrived (both times), she followed through with my birth plan and I felt baby and I were in good hands. Alana was also a huge part of my post-partum recovery because she would look into things for me and provide resources that would come in handy for even 4th time mom's. What I love about Alana the most is how comfortable and confident I felt around her and the level of support she gave. I appreciated the whole process and would pick her all over again because you just can't get this type of pre and post-natal care from a doctor. So if you're looking to birth your baby into a calm, caring, and peaceful environment look no further because Alana is amazing!
UPDATE: it has been nearly 9 months since our son was born. Unfortunately, the billing outfit that Ritual Midwifery partners with, which is called EarthSide Billing, has proven to be an absolute disaster. 9 months, and we are still completely mired in billing madness. To be fair, and to be clear, this situation isn't the fault of Ritual Midwifery, which is why I'm leaving 5 stars. It may not even be 100% the fault of EarthSide Billing, as it appears Aetna's profound incompetence is also contributing to our ongoing dilemma. But EarthSide has made many missteps to put us in this situation. Consequently, I wanted to post an update because this has been such a Kafkaesque bureaucratic nightmare of aimless time wasting that potential clients should be aware--that this may be an issue you'll face as well, as you are trying to settling into new routines of parenthood and back into the grind at work. If I had nothing better to do, this would be deeply annoying, but with parenting and work and the million other things we all have to deal with, its actually maddening. While I am sure that the vast majority of clients don't experience issues with billing, I have found at least one other person online whose had as bad of an experience as we have with EarthSide. Thankfully I found this person online, as they have been 100 times more helpful in directing us on how to resolve our problem than has EarthSide. And yet, I still see no path for this issue being resolved before our son's first birthday. In fact, it literally might never get resolved. Its completely possible that we have to simply forfeit thousands of dollars, not to mention dozens of wasted hours, because EarthSide and Aetna cannot work together to figure it out. We are filing complaints with the state's Department of Managed Healthcare, as well as the Health Community Alliance in a last ditch effort to force Aetna and EarthSide to sort it out. All of this is to say, I still highly suggest working with Ritual Midwifery, but if you can somehow do so without involving EarthSide, and instead use a more reputable service, I highly recommend it.
We interviewed a number of midwives and midwife groups, and none of them gave me the warm and fuzzy feeling that I immediately got with Alana. When she referred to our future child as a "pipsqueak" I was immediately sold. It may sound stupid, but that's actually how it happened for me. She was so obviously a kind and compasionate and bubbly and positive person that we knew right away she was who we wanted. The level of care and compassion and thoughtful guidance we received was above and beyond what either my wife or I expected. All of our visits were calm and not rushed, and Alana's patience with fielding endless questions, day or night, was incredible. As for the labor itself, we labored at home for 24 hours. Alana came immediately when we called on her in the middle of the night, early in labor. We were experiencing weird symptoms and she didn't hesitate to come right over and asses the situation. She made the right call to have the baby checked at the hospital to make sure everything was okay and the symtoms we were experiencing weren't in fact a breach baby (thankfully they weren't), then we went back home with Alana to continue laboring there. We did end up having to deliver in a hospital after 24 hours of laboring at home because our progress was very obviously stalled, my wife and I were totally burnt out, and my wife was ready to go in. Alana was patient and proactive the whole way though, giving us all of our options every step of the way and supporting us fully in whatever decision we wanted to make. She made it clear that there were certain symptoms that would *require* us to transfer to the hospital (blood pressure, etc), in which case we wouldn't have a say in the matter, but this is her top notch professionalism and concern for safety above all shining through. Even after transfering to the hospital, Alana was there to support us until baby finally came, 12 hours later. There isn't much more to say, we couldn't be happerier with the service we received, and we feel like we made a genuine friend along the way. Stop looking, book with Alana. Alana, we love you and we thank you :) - A Very Happy New Dad
My partner and I are so grateful for the care we received from Alana. Alana's steady hand made a huge difference during our journey into parenthood. She offered practical and thoughtful guidance throughout all stages of pregnancy and into postpartum. We always knew we had someone in our corner: she helped us navigate difficult questions regarding the medical system, including our birthing and care options, she provided us with resources so that we could make informed decisions, and she advocated for us and offered counsel and comfort during the tough times. And that's just the tip of the iceberg. Our visits with her gave us confidence and were a wonderful way for my partner to receive care. As the father, I was particularly grateful for how Alana incorporated and included me in my partner's care. She helped me to be a better partner -- more informed and attuned -- and a more confident and capable father. If it were an option, we'd give Alana 10 stars.
When we were shopping for a midwife.. I said I wanted someone magical. Alana was magical. She was so genuinely caring, knowledgeable and able to connect with who we are and how we envision our pregnancy and birth journey. Having her after the birth was most helpful as we then navigated so many new parts of life in caring for a newborn. I love Alana and will forever be grateful for her support.

I just want to say that every pregnant mama needs Alana in their pregnancy journey to becoming a mother I just have no words to express my gratitude ... All I can say is that she has been such a blessing in my life I met her through one of my best friends back in 2021 when I found out I was pregnant for the first time Alana is one of a kind; she is one of the best human beings you will ever meet in your life. She is very wise, she holds space for you and your family in one of the most important days of your life. She is so knowledgeable, strong, bright, thoughtful, caring, nurturing, and knows how to advocate for you, baby's and pretty much for the whole family's wellbeing. She is one step ahead of the game and has great resources if something is not within her scope of practice. Back in 2021 I saw her for prenatal care for my first pregnancy because I wanted to have my husband be a part of the process since he was not able to go with me to the Dr appt due to COVID guidelines. Her appointment was so different from the Dr appt. A Plus is that she also speaks Spanish which is our preferred language and she was able to explain the prenatal care, delivery and postpartum process to my husband in Spanish in a very clear way. We were very excited to come for the prenatal appointment I was able to have my husband her appointment was very thorough and we were able to hear baby's heartbeat a moment that I will cherish forever. Sadly, I lost my baby boy at 4 months pregnant due to cervical insufficiency something I was not aware of and didn't have symptoms. The day I found out I was at the anatomy ultrasound appointment and found I was already 4 cm dilated and there was no way to save my pregnancy. Alana came to the hospital that day to be with me and my husband; I delivered my baby boy it was the worst day of my life filled with shock and trauma but Alana helped me and my husband to get through it she was the best support person we could have during that moment; she was light during that moment of darkness. She was so caring and advocated for the whole family that day. She came to the funeral ceremony we did for our son. It was needed for us so we could have closure and she checked on me constantly during the postpartum period; she did a beautiful ceremony which was healing to me emotionally and spiritually and she filled me with hope. I won't forget all they ways she cared for me as a first time mama who lost her first baby my baby angel boy. She was nurturing in so many ways and I can say she helped me overcome those dark days. I believe that the care I received from Alana after I lost my first baby helped me to not lose hope on becoming a mother in the future. Fast forward a year later I found out I was pregnant for a second time. Knowing my previous history of cervical insufficiency and having a high risk pregnancy I did not doubt for one second we needed Alana to be part of our journey again Her prenatal care, support during delivery and postpartum was top notch and amazing. I was seeing a perinatologist every two weeks after my cerclage procedure and Alana was always available and wanted to be updated of any changes. Any questions I had she was available to answer. Every time I asked her opinion she gave me all the information and if I needed to make a decision. I had to be induced at 37 weeks due to having IUGR (Intrauterine Growth restriction ) Alana was there for me during the induction process and really advocated for me when I encountered a Dr and RN who wanted to push procedures on their own time. Alana gave me the strength to advocate for myself. I ended up having emergency C- section due to baby not tolerating induction. But having Alana there right after delivery being attentive to do skin to skin, start breastfeeding right away and helping managing symptoms made a whole difference. After a high risk and stressful pregnancy we were able to deliver a healthy baby girl Post partum care was so important for me Alana was there again checking on me and my family. She made another beautiful ceremony after following my "cuarentena" she respected our culture and traditions. I can honestly say I was able to breastfeed thanks to her help at the beginning where I felt lost she was there for me and baby the first few days she also has great resources and recommendations she recommended a lactation consultant who found out baby had a tongue tie, she has made so many great recommendations along the way Alana has been such an important person in my life and my journey to becoming a mother She is a wonderful mom herself and she is an inspiration. Thank you Alana for everything you have done I already told my husband if we have another baby we have to have her by our side again. Alana May God Bless you and continue to give you wisdom, strength and love to keep caring for all the mamas out there the way you know to care for them We love you and appreciate you

Alana is the kindest human who instantly makes you calm. She allowed the journey of pregnancy, childbirth, and postpartum to be such a joy. My husband and I were so sad when we had our last postpartum meeting with her. She's the kind of person you'd love to have around you for a lifetime. As someone who has worked as a doula at many hospital births and seen far too many inductions, I decided I wanted to try for a home birth. Being in my 40's and having my first child I felt the odds were already stacked against me, but Alana provided great support and information from our very first conversation. Every meeting made me trust my instincts and feel even more confident in my body. And she was amazing with my husband, making him feel empowered and part of the journey as well. She always took time to answer any questions while making sure we had information and tools to make each step of pregnancy, birth, and postpartum seamless. I was so lucky to have a smooth pregnancy and birth, but there is no doubt that Alana's support and care allowed this to happen. I never felt stressed with her and I felt attuned to my body. She also made sure my husband felt the same way and allowed him to feel confident in supporting me when I felt the emotional difficulties of transition. Alana got to know me and my support team so well that it was easy for me to trust her suggestions throughout labor. I felt held and cared in such a beautiful way. Lastly Alana caught feeding issues with our daughter when she was only six days old. I cannot imagine how things would have gone if she didn't spot this when she did! Our daughter is healthy and thriving because Alana took time in her meetings and genuine care in our family. And if you work with Alana she will become like family. She's an incredible person that we are grateful for... thanks Alana for all you do!

We just had our six week postpartum visit with Alana, and we're so sad that our time with her has come to an end! I'm a midwife myself, and I loved how Alana seamlessly merges evidence based practice with years of experience and a kind, compassionate, caring approach that meets families where they're at. We felt cared for and supported throughout my pregnancy, birth, and postpartum period, and even my 3 year old is attached to her. I felt well supported and safe during my labor and birth, and my husband also felt like we were in good hands, which allowed him to focus fully on supporting me. We got to have the beautiful home birth we had wanted, and we are so glad Alana was there to support us. You'll be in safe, supportive, compassionate and experienced hands with Alana, and I can't recommend her enough.

Alana weighing our baby, with our 3 year old "helping"

I did not know I needed... did not know I WANTED... a homebirth midwife. I had had a hospital birth with my first and a midwife/homebirth with my second. I was pregnant with my third and, since both my previous birthing experiences had been... ahem... rough, I didn't feel motivated to invest in another homebirth. I am so, so grateful that my doula kept urging me toward Alana and that she so gently invited me to reconsider a home birth. It is one thing for someone to say they support someone no matter what their decisions are. It is another to really feel that's true, that the whole of that other will support you, and believes in you. I felt that with Alana. As I made the many decisions on the path to birth, through birth, and in postpartum, I never worried that I would be judged about anything. There was a dicey mid-birthing decision to be made and Alana was with me fully. I had no idea all a midwife could and would do for me and my family to make birth and postpartum so much more sane, and kind. Alana's visits to our home put us all in a sort of womb space--a sacred space of really deep presence to how precious life is. These were once or twice in a lifetime moments that I will always treasure, and could easily have missed if I'd had hospital-only prenatal care. Alana will gently help you prepare for birth and postpartum so that you don't have to grapple with the things that can become major stressors when unprepared. (In my experiences, it was easy to slip through the cracks at the hospital, despite so many great people there.) Alana will also make sure that your preparation is paced such that you are ready to move on from preparation to savoring for a sweet space of time before your baby is due. Even as we prepare, so much can happen in the birthing journey, and we had some curves during ours. Alana was present, affirming, and Calm. After our baby was born, he needed some support. Alana was fully with us, masterful, and deeply attuned. Her support continued postpartum. I was repeatedly shocked at how loving and enthusiastically Alana responded to my every text, call or question. Postpartum care matters, and Alana was genuinely there. This was not "just" a profound birthing experience, it was a profound life experience. Alana is there for your baby, and she is there for you and your wellbeing. (If you have other family involved, she is there for them, too-she sees you in your wholeness.) She is also more broadly ethical, looking at midwifery within the context of our culture in addition to how midwifery can serve individuals and families, and she is, frankly, a badass, but not in the way that makes you feel like you can't be naked in front of her--literally and metaphorically! She is gentle, humble, and brings a deep joy... and sometimes pastries. :) ANY way that a woman births is "right", and, I would strongly encourage anyone I loved to consider what a homebirth has to offer and allow, that a hospital birth does not. I hope you have YOUR birth. I am so grateful that Alana helped us have ours.

Words can't express how grateful I am for the incredible support and care provided by our midwife Alana during the birth of our daughter. From the very beginning, she made us feel comfortable and empowered, answering all our questions and easing our anxieties. During labor, her presence was a source of strength. She guided my wife with unwavering confidence, offering reassurance and expert guidance every step of the way. Her calm demeanor and deep knowledge of childbirth were truly remarkable. Alana's dedication to ensuring a safe and positive birth experience for both my wife and our baby was awe-inspiring. She played a pivotal role in making the entire process as smooth as possible. I can't thank her enough for being a part of this beautiful journey into parenthood. She's not just a midwife; she's an angel who brought our child into this world with grace and expertise."
3 other reviews that are not currently recommended

East Bay Hand & Upper Extremity
3.9 miles away from Ritual Midwifery
Board Certified Harvard & Manhattan Trained Hand & Upper Extremity Surgeons with over 20 years of experience Dr. Douglas Chin & Dr. Glen Lau are premier hand surgeons in the San Francisco Bay Area. read more
in Surgeons

Divine Doulas
Through consistent, continuous, & compassionate Doula services customized to who you are, what you want, while offering the skilled postpartum doula and live-in support that you need. read more
in Doulas, Lactation Services
People Also Viewed

Nourish Midwifery & Take Root Home Insemination

Collective Birth Midwifery

Ellie Griffinger, CNM - Golden Oak Midwives

Aimée Tom, CNM

Golden Oak Midwives

Awakenings Birth Services

Lindy Johnson, CNM

Ellen Levitt, LM Wombservice Midwifery

Eva Goodfriend-Reaño, CNM

Doula Keelia
Browse Nearby
Obstetricians & Gynecologists
Birthing Centers
Restaurants
Department Stores
Conveyor Belt Sushi
Other Midwives Nearby
Find more Midwives near Ritual Midwifery

- Government & Politics
- Energy & Environment
- Criminal Justice
- Health Care
- Election 2024
- children & families
- Reproductive Rights
Casey to introduce bill expanding Medicaid maternity care to include doulas and midwives
The ‘mamas first act’ is similar to legislation that passed the pa. house this week as part of focus on black maternal health, by: peter hall - may 9, 2024 9:00 am.

(Getty Images)
Pennsylvania U.S. Sen. Bob Casey is among a group of congressional Democrats who introduced the “Mamas First Act” on Thursday to require Medicaid coverage for prenatal, delivery, and postpartum care by doulas, midwives and tribal midwives.
The federal legislation follows the passage of a similar bill that passed the Pennsylvania House of Representatives to cover doula services for expectant and new mothers here.
Both bills are intended to help address the racial and ethnic disparity in maternal mortality rates between women in the United States.
“Every mother deserves support and care before, during, and after birth,” Casey said. “This legislation will help address the maternal health crisis in this country by ensuring that Medicaid covers the full spectrum of care that mothers and infants need.”
Casey introduced the bill in the U.S. Senate with Sens. Elizabeth Warren (D-MA), and Cory Booker (D-NJ). A House companion bill was also introduced today by U.S. Reps. Gwen Moore (D-WI), Ayanna Pressley (D-MA), Lauren Underwood (D-IL), Alma Adams (D-NC), and Debbie Dingell (D-NC).
“America’s ongoing maternal health crisis magnifies the need for federal interventions that can save lives. The Mamas First Act is an important effort because it will expand access to providers who can offer emotional and physical support during and after the birthing process – comprehensive beyond the hospital setting where nearly all U.S. births occur,” Moore said.
According to a draft of the Senate bill, the Centers for Disease Control and Prevention finds the maternal mortality rate of 69.9 deaths per 100,000 live births for Black women is nearly three times that for white women. Deaths among American Indian and Alaskan Native women number about 49 per 100,000 live births while there are 28 deaths per 100,000 live births among Hispanic women.
“While maternal mortality disparately impacts Black women and indigenous women, this urgent public health crisis traverses race, ethnicity, socioeconomic status, educational background, and geography,” Casey’s bill says.
About 80% of these deaths are preventable, Casey’s bill says, but United States maternal mortality rates are the highest in the developed world and are increasing rapidly. In Pennsylvania, a report this year by the newly formed Maternal Mortality Review Committee showed 107 Pennsylvania women died in 2020 during pregnancy or within one year of giving birth.
Doulas are non-medical, trained professionals who provide emotional, informational, and physical support before, during, and after pregnancy and childbirth, such as helping with breastfeeding and breathing techniques during labor.
According to the NIH, mothers who have the assistance of a doula are four times less likely to have a low-birth weight baby, two times less likely to have a birth complication with their baby or themselves, and significantly more likely to begin breastfeeding.
A midwife is a trained medical professional who provides care for healthy mothers during pregnancy, in delivery and after giving birth. Midwives deliver babies in the home, birth centers and in hospitals.
A tribal midwife is a person recognized by an indiginous tribe to practice midwifery for that tribe, Casey’s bill says.
Midwife-led care correlates with cost savings, decreased rates of intervention, lower cesarean rates, lower preterm birth rates, and healthier outcomes for mothers and babies, according to Casey’s bill..
Pennsylvania’s House Bill 1608 is part of a package of legislation on Black maternal health — dubbed the “Momnibus” by supporters — that also includes a requirement for Medicaid to cover blood pressure monitors for pregnant women and new moms.
Both state House bills will now go to the Republican-controlled state Senate for consideration, where a similar bill to require Medicaid reimbursement for doulas was introduced last year by Sen. Judith Schwank (D-Berks). It has yet to be considered since it was referred to the to Senate Health and Human Services Committee in January 2023.
Other bills in the Momnibus package call for investment in maternal health care deserts, maternal mental health, eliminating implicit biases in maternal health care and providing new parents with supplies to care for newborn babies.
(This article was updated at 2:15 p.m. on Thursday, May 9, 2024, to include information about cosponsors of the Mamas First Act and quotes from Casey and Moore.)
Our stories may be republished online or in print under Creative Commons license CC BY-NC-ND 4.0. We ask that you edit only for style or to shorten, provide proper attribution and link to our website. AP and Getty images may not be republished. Please see our republishing guidelines for use of any other photos and graphics.

Peter Hall has been a journalist in Pennsylvania and New Jersey for more than 20 years, most recently covering criminal justice and legal affairs for The Morning Call in Allentown. His career at local newspapers and legal business publications has taken him from school board meetings to the Pennsylvania Supreme Court and many points of interest between. He earned a degree in journalism from Susquehanna University.
Pennsylvania Capital-Star is part of States Newsroom , the nation’s largest state-focused nonprofit news organization.
Related News

Antenatal support: meet the team
While you're pregnant, you'll normally see a small number of healthcare professionals.
They want to make you feel as comfortable as possible while you're pregnant and when you have your baby.
You'll usually have the same midwife or a small team of midwives who will care for you during pregnancy and the birth of your baby. But in some cases you may see several different professionals. You can ask what's available in your area.
At each appointment, the professionals you see should introduce themselves and explain what they do. If they forget, ask them. Make a note of who you've seen and what they've said in case you need to discuss something later on.
This page lists the people you're most likely to meet. Some may have trainee students with them – you'll be asked if you mind the students being present.
A midwife is an expert in normal pregnancy and birth.
Midwives are specially trained to care for mothers and babies throughout normal pregnancy, labour and after the birth. They provide care in hospital or at home.
Midwives sometimes work both in hospitals and in the community (GP surgeries and home visits) so the same midwife may be able to provide antenatal care and be present at the birth.
The name of the midwife or team of midwives responsible for your care will be in your pregnancy notes.
Find out more about things to talk about with your midwife when making your birth plan .
A midwife will look after you during labour if everything is straightforward, and they'll probably deliver your baby.
If any complications develop during your pregnancy or delivery, you'll see a doctor as well as being cared for by your midwife.
After the birth, you and your baby will be cared for by midwives or maternity support workers.
Head of midwifery
The head of midwifery can support you if you're having problems with your care or you feel your wishes are not being considered.
The charity Birthrights has factsheets on your rights and the law in pregnancy and birth that you might find useful.
If you've had your baby and want to talk about your birth experience, even if this was some time ago, the head of midwifery will be able to arrange this for you. The hospital's website may also have contact details for this service.
Obstetrician
An obstetrician is a doctor who specialises in care during pregnancy, labour and after birth.
Your midwife or GP will refer you to an obstetrician if they have any concerns about your pregnancy – for example, you had a previous complication in pregnancy or have a long-term illness.
You can ask to see an obstetrician if you have any concerns you want to discuss.
Anaesthetist
An anaesthetist is a doctor who specialises in providing pain relief and anaesthesia.
If you decide to have an epidural for pain relief during labour, it'll be given by an anaesthetist.
If you require a caesarean section , an anaesthetist will provide the appropriate anaesthesia.
They'll also be present if you require an epidural for an instrumental delivery – for example, with forceps or a vacuum device that helps deliver the baby's head (ventouse).
Paediatrician
A paediatrician is a doctor specialising in the care of babies and children.
A paediatrician may check your baby after the birth to make sure everything is OK, and they'll be present when your baby is born if you've had a difficult labour.
If your baby has any problems, you'll be able to discuss these with the paediatrician.
If your baby is born at home or your hospital stay is short, you may not see a paediatrician at all. Your midwife or GP can check on you and your baby.
Neonatal nurse
Neonatal nurses are specially trained to care for babies who are premature or unwell when they're born.
They usually work within specialist neonatal units in the hospital or in the community.
They also have an important role in providing support for parents whose babies need neonatal care.
Sonographer
A sonographer is trained to carry out ultrasound scans .
A sonographer will perform your:
- 12-week scan (dating scan)
- 20-week scan
- screening test for Down's syndrome, Edwards' syndrome and Patau's syndrome
You may be scanned at other times in your pregnancy.
Obstetric physiotherapist
An obstetric physiotherapist is trained to help you cope with physical changes during and after pregnancy and childbirth.
Some go to antenatal classes and teach antenatal exercises, relaxation and breathing, active birth positions, and other ways to keep yourself fit and healthy during pregnancy and labour.
After the birth, they advise on postnatal exercises to tone up your muscles.
Health visitor
Health visitors are trained nurses who support and educate families from pregnancy through to a child's 5th birthday.
You may meet your health visitor before the birth of your baby and in the first few weeks after the birth.
You may continue to see your health visitor or a member of the team at home, or at your child health clinic, children's centre, health centre or GP surgery.
GOV.UK: find a children's centre near you
If you have any concerns about special diets or eating healthily – for example, if you develop gestational diabetes – a dietitian can give you the advice you need.
Video: What can my baby understand and feel in the womb?
In this video, a clinical psychologist talks about what your unborn baby may feel in the womb.
Page last reviewed: 26 October 2023 Next review due: 26 October 2026
- Open access
- Published: 15 May 2024
An online survey of women’s views of respectful and disrespectful pregnancy and early labour care in the Czech Republic
- Deirdre Daly 1 ,
- Natalie Sedlicka 2 ,
- Kateřina Švanderlíková 2 ,
- PetraAnn Ann Kovařčíková 2 ,
- Radka Wilhelmová 3 &
- Cecily Begley 1
BMC Pregnancy and Childbirth volume 24 , Article number: 370 ( 2024 ) Cite this article
Metrics details
To ascertain and explore the views of women and their partners, giving birth in the Czech Republic, of the level of respectful or disrespectful care provided during pregnancy and early labour.
Ethical approval was granted for a descriptive, online anonymous survey of 65 questions, with quantitative and qualitative responses.
The Czech Republic.The survey was completed by 8,767 women and 69 partners in 2018.
Measurements and findings
Descriptive statistics and thematic analysis were used to present results. The majority of women were aged 26-35 years. Most had birthed in one of 93 hospitals, with 1.5% home births. Almost 40% never had an abdominal examination.in pregnancy. Quantitative data analysis revealed that less than half were given information on place of birth, or how to keep labour normal or non-interventionist. Almost 60% did not get information on positions for birth. Most (68%) commenced labour naturally, 25% had labour induced, 40% of them before term, and 7% had an elective caesarean section; 55% stated they had not been given any choice in the decision. Over half of those who had a membrane sweep said permission had not been sought. Half (54%) only had ‘checking’ visits from the midwife in labour.
Key conclusions
Findings reveal a lack of information-giving, discussion and shared decision-making from healthcare professionals during pregnancy and early labour. Some practices were non-evidenced-based, and interventions were sometimes made without consent.
Implications for practice
The examples of disrespectful care described in this study caused women distress during childbirth, which may result in an increased fear of childbirth or an increase in free-birthing.
Peer Review reports
The Czech Republic became a separate state in 1993, after 40 years of socialism and communism in Czechoslovakia ended in 1989. Under communism, the rights of the whole population were repressed and their freedom was restricted. Women, in particular, had little autonomy in what was a very patriarchal country. Since 1993, restrictions have been reduced and women are now more independent and autonomous. However, in the maternity care services, little has changed and the model of care is still one of hierarchy and paternalism, where midwives are not recognised or respected [ 1 ]. Midwifery as a profession was eliminated by the former regime and its reintroduction is a slow process. The professionalisation and the professional authority of midwives is part of the debate on structural health care system change in the context of resistance to giving up the dominant position of Czech gynaecologists and obstetricians in delivery rooms [ 2 ]. In many hospitals, normal births are conducted by obstetricians, with midwives assisting. Midwives are suppressed [ 2 ], not permitted to work autonomously, or to attend home births [ 3 ] and a recent Ministry of Health publication on perinatal care does not mention midwives as core care providers [ 4 ]. In their book, Games of Life, Šmídová et al. (2015) discuss biomedicine’s approach to childbirth in the Czech Republic as being as a state of emergency and high risk and dealt with as a highly medicalised event using routine interventions as precautions [ 2 ]. Although the Czech Republic joined the EU in 2004, midwives are precluded from using their full range of competencies or from offering private independent care [ 3 ]. In addition, the cost of midwifery care to women is not covered by the standard public health insurance and some women opt to give birth at home, either alone or with the help of a doula [ 3 ]. Set in the context of improving the quality of maternity care, the Ministry of Health sought ‘Experiences of Obstetrics’ from parents via their Facebook page in 2016. A total of 689 contributions from 486 original comments were posted and analysed to identify recommendations. Overall, the analysis showed clear requirements for changing the system which the authors described as medically-guided childbirth and care with a high level of intervention. The authors concluded that practically all proposed recommendations were aimed at enabling non-interventional births. Other recommendations referred to the choice of place of birth and using of the latest scientific evidence to inform practice [ 5 ]. In addition, some maternity hospitals have introduced radically different regimens of care and embraced practises such as gentle birthing, acupuncture, fathers in labour rooms, and other innovations that aimed humanise childbirth [ 6 ].
There were 93 maternity hospitals in the Czech Republic in 2018. Since 2019, pilot Centres of Midwifery (CPA) were opened. First, two birth apartments were built in Prague with midwives starting to provide prenatal care for women with no, or low, medical and obstetric risks, in addition to additional obstetric care provided elsewhere. However, an obstetrician must decide if the midwife can be the primary carer during birth. The second CPA opened in Brno in 2021, with midwives supporting and leading physiological birth. It is important to acknowledge that two midwifery centres existed in the early 2000s but, despite having favourable birth outcomes, the second of these was closed in 2007 ( http://www.biostatisticka.cz/jak-to-byvalo-ve-vrchlabi/ ).
Respectful maternity care is a human right [ 7 ]. In 2014, the World Health Organization (WHO) re-emphasised that being disrespected in childbirth not only infringed women’s rights but also discouraged women from using maternity care services [ 8 ], which could adversely impact on their health [ 9 ]. Disrespectful care can comprise physical abuse, discrimination, abandonment, or detention in facilities but also care that is non-consented, non-confidential, or non-dignified [ 10 ]. Miller et al. [ 11 ] associated evidence-based care with respectful care indicating that care that is non-evidence based is un-dignified, and disrespects women’s rights. More recently Lappeman and Swartz [ 12 ] suggested that silence between healthcare providers and the women in their care also can be a form of neglect. Findings from systematic reviews [ 13 , 14 ] and numerous empirical quantitative and qualitative studies demonstrate its widespread existence across the world [ 15 , 16 , 17 , 18 , 19 ]. Disrespectful care during childbirth is not a new phenomenon and, by exploring the long history of obstetric violence, O’Brien and Rich [ 20 ] locate biological reproduction as a site of social violence.
In the context of the post-socialist transformation in the Czech Republic, many women’s maternity care needs are still not paramount and many have no autonomy [ 1 , 3 ], shown by healthcare professionals not preserving women’s dignity or privacy during examinations or when in labour and, sometimes, ignoring women’s refusal of consent or interventions [ 1 , 21 ].
The Czech Republic does not publish complete data on maternity care practices, intervention rates or statistics either in individual hospitals, or on births at home. In 2017, a private statistician started a court case to seek access to data on care in all maternity hospitals, but her request has not yet been granted [ 22 ].
This paper presents results from an anonymous online survey of women’s, or their partners, views on the care experienced when pregnant with and giving birth to their first baby in the Czech Republic. It follows a similar study of healthcare professionals’ views [ 23 ], conducted following a television documentary shown in the Czech Republic that appeared to indicate the use of some poor practices in maternity care [ 21 ]. A later documentary, which included women’s narratives, also highlighted the continuing existence of malpractices and lack of evidence-based practices [ 24 ]. Apart from these documentaries, and anecdotal evidence, there are minimal data on women’s or couples’ experiences of maternity care and services in the Czech Republic.
The study aimed to ascertain and explore the views of women, and partners of women, who had given birth in the Czech Republic of the level of respectful or disrespectful care provided for them during pregnancy and early labour. A descriptive online anonymous survey containing 65 questions was designed (Additional file S1 ). Five questions related to respondents and the age of their child(ren). Thirteen questions related to specific antenatal and intrapartum actions/interventions (e.g., induction of labour, application of electronic fetal monitoring etc.) had ‘Yes/No/Not applicable’ responses and 47 questions included open text comments to enable respondents to elaborate on the care, intervention(s) experienced or interactions with healthcare professionals. The quantitative questions were based on evidence and recommendations from relevant Cochrane reviews which were used in a previous survey of maternity care professionals’ views of respectful and disrespectful maternity care in the Czech Republic [ 23 ]. We also incorporated questions relating to nine of the 12 domains identified in a review of 67 studies from 32 countries on women’s perspectives of respectful maternity care [ 25 ]. These included: being free from harm and mistreatment, maintaining privacy and confidentiality, preserving women’s dignity, prospective provision of information and seeking informed consent, ensuring continuous access to family and community support, engaging with effective communication, respecting women’s choices that strengthens their capabilities to give birth, and provision of efficient and effective care and continuity of care. We did not include questions on the physical environment or resources, equity of services or competence and motivations of personnel.
The survey content was developed with nine midwives, doulas and women who had birthed in the Czech Republic, and assessed for acceptability and face validity with 20 women. The survey was prepared in English by CB and DD and translated into the Czech language, and back-translated from Czech to English by NS, KS, PK. Consistency was also checked between the two versions by two other bilingual volunteers. Ethical approval was granted by the Research Ethics Committee, School of Nursing and Midwifery, Trinity College Dublin [14 November 2016].
Participants
Participants were women aged 18 years and over, or partners of women, who had given birth in the Czech Republic. All participants were informed about the study and given the opportunity to ask questions. All were asked to complete the survey in relation to their experiences while pregnant and giving birth to their first baby.
Recruitment
We identified volunteer representatives in each region, through national professional organisations, universities, midwifery schools, hospitals, other health/helping professional fields, participants at birthing seminars (APODAC, UNIPA, etc.), who advertised and provided information on the study in local places/services such as maternity centres, kindergartens, lactation advisors, doulas, associations concerned about birth topics or child education, national magazines and other media. The survey was mainly distributed through personal recruitment (emailing/facebook notices, messages and sharing), with women sharing it with others thereafter. The main channel was Facebook (APODAC pages, JakJinak and other personal profiles of the members of the association) but the survey was then also advertised by various maternal centres and mother and baby websites, and other professional organisations. Those willing to take part completed the survey online, between 1st March 2018 and 31st May 2018. At the start of the survey, participants were informed that the survey was anonymous and that submission of the survey was taken as giving consent to participate.
Data collection
The survey was anonymous, prepared in the Czech language, and administered via Survey Monkey®.
Participants were asked;
their age range, how old their youngest and oldest children were, the name of the hospital they gave birth in (or if they had a home birth);
to answer all questions in relation to their first-born baby;
what information they were given on aspects such as: choices available for place of birth, mode of birth or how to keep labour remaining natural or non-interventionist;
whether or not they had abdominal examinations performed in pregnancy;
whether or not they had, and whether or not they were offered choice regarding induction of labour or elective caesarean section.
Data analysis
Quantitative data were analysed using descriptive statistics, and the frequency with which care practices or interventions occurred are presented as proportions. Respondents’ open text comments were analysed by a team of four researchers applying descriptive codes, merging codes under category headings, followed by thematic analysis using a data-driven approach [ 26 ]. For example, comments relating to consenting to/declining an intervention were categorised as ‘Consent’, ‘Refusal’, or ‘Healthcare practitioners’ reaction’ when care was declined, etc., and comments relating to induction of labour were categorised as ‘Reasons given for induction’, ‘Reasons given for timing of induction’, etc. The team worked together initially to develop code definitions, and then independently, with a final phase of consensus-seeking to ensure comparability across all codes and categories. The first and last authors then acted as peer debriefers [ 27 ], adjudicating on the appropriateness of the thematic analysis, once translated into English. When appropriate, direct quotations (translated, as necessary, into English), are used to complement the quantitative data.
Characteristics of the sample
A total of 10,200 people completed part of the survey, and 8,920 completed the full survey. Data from one respondent aged less than 18 years was removed, under the terms of our ethical approval. Of the remaining sample, 8,767 (98.31%) were women who had had a baby in the Czech Republic, and 69 (0.77%) were partners of women who had birthed in the Czech Republic and were reporting in relation to their partner’s experiences. The remainder were ‘another person interested in maternity care’ ( n = 23), a midwife ( n = 43), a doula ( n = 6), and ‘other healthcare worker providing maternity care in the Czech Republic’ ( n = 11). Although all participants had been asked (if they were a healthcare professional) to answer about their own experiences, for the purpose of this arm of the study, these participants’ responses ( n = 83, 0.92%) were omitted, as we had published healthcare professionals’ views already [ 23 ]. This left a final sample size of 8,836. For half the participants, their first baby’s birth had taken place either within the month prior to completing the survey (5.25%, n = 462) or between one month to one year previously (43.70%, n = 3,846), with the remaining participants (51.05%, n = 4,493) completing the survey more than one year after the first birth.
Responses to questions varied according to question type and place in the survey. For example, response rates for the first 21 questions varied from 91% to 100%, while those for the more detailed questions on labour and birth (questions 22–35) varied from 80% to 89%. Later questions (36 to 65) had response rates from 76% to 80%, with question 39 (‘Were you allowed to eat light diet in labour?’) gaining the lowest response rate of 73%. In all questions, results are given as percentages of the actual number responding.
The majority of those who gave their age ( n = 8,817) were between 26 and 30 years old ( n = 3,258, 36.95%), with a further 33.33% ( n = 2,939) aged 31–35 years (Table 1 ). The average age was 30 years.
Half of the respondents had just one child ( n = 4,428, 50.23%) and the remainder had other children aged one to four years ( n = 2,500, 28.36%), five to eight years ( n = 1,023, 11.60%) or more than 8 years of age ( n = 864, 9.80%). Respondents were asked where they, or their partner, had given birth. A small number ( n = 132, 1.50%) had given birth at home. The remainder had birthed in one of 93 hospitals (Additional file S2 ).
The quantitative findings on experiences are presented in tables and complemented with illustrative direct quotes from respondents’ free-text comments. The proportion of comments are also given, when available, to show the frequency of their use.
Choice and care during pregnancy
Care in pregnancy included the obstetrician/gynaecologist, staff in the hospital (e.g., hospital midwife, nurse, other health care professionals – postnatal nurse, doctor etc., or private midwife permitted to provide care in hospital but as a doula only, or doula), or the woman’s ‘secret home-birth midwife’ performing an abdominal examination once or twice ( n = 2,227, 25.53%), on every visit ( n = 3,058, 35.06%) or never ( n = 3,438, 39.41%). Less than half of the women, when attending for care in their first pregnancy, were given information by staff caring for them on where or how they might give birth, and only a quarter were given information on how they might keep labour natural or avoid interventions (Table 2 ).
Mode of birth and gestation at birth
Table 3 shows mode of birth, method of induction of labour and gestation at birth. For the majority of women in their first pregnancy, labour started spontaneously at, or after, their due date ( n = 5,652, 63.96%). The overall induction of labour rate was 25.03% ( n = 2,077/8,299) and the overall elective CS rate was 7.04% ( n = 584/8,299). Half of all women who had labour induced said this occurred before term ( n = 944, 38.16%) or at term ( n = 282, 11.40%). Of those who had a CS, 835 women (49.29%) said this was performed before term, and 195 (11.51%) at term, with a further 21.84% ( n = 370) having their elective CS by 41 weeks’ gestation.
The majority ( n = 2,543, 94.71%) gave qualitative comments on why they or their carers had not waited for labour to start spontaneously. The reasons for inducing labour included, mainly, ‘pregnancy after term ’ ( n = 709, 27.88%), which had been explained to some women as being between 40 weeks and 40 weeks and 4 days to 41 weeks and 6 days. Very few women stated ‘after 42 weeks’ ( n = 14, 0.55%), and 191 women (7.51%) stated ‘before term’ without adding comments. Some women ( n = 126) said that they were informed by their doctors that it was illegal to permit pregnancy to go far over-due (sometimes as little as 40 weeks plus one day); for example, one woman said that her doctor had said: ‘C zech law does not allow us to wait more than 41 weeks and 3 days’ . Comments made by the women as to how ‘post-term’ had been described to them included: ‘Everything over 41 weeks may be dangerous for the baby, there is no more time for waiting ’; ‘ You are already a couple of days after term so we make it a bit quicker’; ‘You are overdue, it’s already after 38th week’ , or ‘ From week 40 it is post-term so we have to induce it’. One woman said: ‘ Doctor was afraid of overdue. That’s why she did Hamilton manoeuvre the 9th of March, the little one was born 10th. My expected date of birth was 17th’.
The second most common reason for induction was ‘Medical reasons due to maternal factors’ ( n = 583, 22.93%) (e.g., pre-eclampsia) and ‘ Medical reasons due to baby factors ’ was third ( n = 332, 13.06%). This included ‘ baby is too big ’ ( n = 167); ‘ position of the baby ’ ( n = 140 (92 women were induced because of fetal breech presentation and 29 of those were born by CS, 14 with fetal breech presentation as the primary reason for CS)); ‘ bad fetal heart tracing ’ ( n = 109) or ‘ baby is not growing ’ ( n = 46, of whom 11 had actual growth restriction diagnosed). Women often gave a combination of reasons therefore percentages are not given. One woman commented that ‘ the doctor said the placenta could be old already but I was not at term yet and after birth the midwife said it was perfectly ok’ , and a further 309 women (14.88%) stated that no reason was given for induction.
Women who had had an induced labour or a CS were asked if they felt the reason why this was necessary was discussed sufficiently with them (including all the positives and negatives). Just under half ( n = 1,624, 49.11%) thought that it had been discussed sufficiently and the remainder ( n = 1,683, 50.89%) did not. Less than half of women ( n = 1,472, 45.14%) felt they had been offered choice in the decision but 1,789 women (54.86%) stated that they had no choice. The majority had labour induced by rupturing the membranes, with or without use of drugs (Table 3 ). Of those who had a membrane sweep performed, 908 (56.33%) said the doctor had not asked for their permission before doing this.
Care provider and support during labour and birth
The quantitative data showed that women were usually cared for in labour with their first baby by an obstetrician/gynaecologist or doctor ( n = 6,778, 76.88%), and/or a hospital midwife ( n = 6,626, 75.16%). Small numbers of women were cared for by a private midwife who had a contract with the hospital (and was permitted to care for them in labour as a midwife) ( n = 212, 2.41%), or a private midwife without a contract with the hospital (who was permitted to care for them in labour as a doula only) ( n = 197, 2.24%). Doulas cared for 246 women (2.79%), and 388 (4.40%) were cared for by ‘other people’. No additional comments on ‘others’ were provided. Ninety-seven women (1.10%) were cared for by an obstetrician/gynaecologist or doctor who was given an extra payment directly by them.
A small minority of women ( n = 615, 7.57%) were not accompanied by any lay person in labour. The majority were supported by the baby’s father ( n = 6,617, 81.32%), a private midwife ( n = 276, 3.39%), doula ( n = 242, 2.97%), or another person ( n = 385, 4.73%). In general, these companions were allowed to stay with them (pre-Covid pandemic) for the whole of their labour (with short breaks) ( n = 5,911, 82.05%) or for about half the labour ( n = 502, 6.87%); however, 11% of women were only permitted to have their companions for a short time at the start, or end, of labour ( n = 475, 6.50%) or not at all ( n = 316, 4.35%). Almost three-quarters of the women ( n = 5,700, 71.12%) had no birth plan documented. Of the 2,315 women who had a birth plan, 1,035 (44.71%) said that it was respected, 601 (25.96%) said that it was not respected and 679 (29.33%) said that they were convinced by the doctor and/or midwife to change their birth plan during their labour. One-third of women ( n = 2,585, 34.89%) said that the health professional(s) who cared for them in labour introduced themselves when they entered the labour room or when they met them for the first time, and a further 49.61% ( n = 3,675) said that some of the health professional(s) did this; however, 1,148 of the women (15.50%) said that the health professional(s) looking after them never introduced themselves.
The majority of women were in labour (in hospital) on their first birth for more than 10 h ( n = 2,858, 38.56%), with a further 1,705 (23%) in labour for over six and up to 10 h and 2,071 women (28.34%) in labour for over two and up to six hours. Most women ( n = 5,811, 79.78%) felt that they were given privacy in the first stage of labour, but 1,473 women (20.22%) did not. Less than 40% of women had a midwife or other healthcare professional staying with them and supporting them during labour all of the time except for short breaks ( n = 1,245, 17.36%) or most of the time ( n = 1,565, 21.82%). The majority ( n = 3,846, 53.63%) said they only had visits from the midwife to check how they were and 284 (3.96%) said they did not have a midwife caring for them at all.
Data from the 8,836 women who had birthed in one of the 93 hospitals in the Czech Republic, or at home, shed light on women’s recent experiences of prenatal and early labour and birth care in the Czech Republic. Overall, our descriptive statistics show the frequency of aspects of care and interventions performed, and women’s qualitative comments provide rich context on these. The inclusion of the proportions of comments provided serves to show that many women’s experiences are, in some instances, common practices.
We asked women minimal information on the content of their pregnancy care because of the variation in the scheduling and content of care provided in the Czech Republic, but it was clear that abdominal examination was not performed regularly, with 39% of women stating that they never had one performed. It is possible that many of these women had ultrasound scans performed throughout their pregnancy, instead of clinical examination. Forty percent of women were never given information by staff caring for them on where or how they might give birth, a finding in common with a number of studies from other countries [ 28 , 29 ]. Information-giving on available places of birth has been identified as an essential component of women’s autonomy [ 30 ], a key tenet of respectful care. A study exploring satisfaction with maternity care in the Czech Republic, with 1,195 respondents, also found that ‘information giving’ and an ‘empathic and respectful approach’ were lacking, and the aspect rated lowest (34%) was ‘control and involvement in decision-making’ [ 31 ].Women who have had a poor previous childbirth experience may be driven away from formal healthcare to give birth alone, if they are not provided with, and are aware of, other possibilities such as homebirth, midwife-led care or birthing centres [ 32 ]. Even when women are aware of other options, it may be difficult, if not impossible, to find an alternative healthcare provider or facility because of limited options. It may also be prohibitively expensive for women to employ a private midwife when the fee is not covered by insurance. The lack of discussion, together with unsatisfying conditions in hospitals [ 31 ], are the main reasons why women choose homebirth in the Czech Republic [ 9 ].
Only one quarter of women in this study were given information on how they might keep their labour normal or non-interventionist as it progressed. Given the documented ill-effects of too much intervention given too soon in labour [ 11 ], this is a key area for the provision of information for women, to increase their empowerment and self-efficacy.
The overall induction of labour rate of 25% among this group of women is similar to many other European countries [ 33 ]. Induction of labour, when necessary, is a useful and important method of care. However, half of all women who had their labour induced said this occurred before or at term, with a further 25% having labour induced by 41 weeks’ gestation, despite the recommendation from the Czech Gynaecological and Obstetrical Society (CGOS) [ 34 ] that there ‘ should be steps taken to end pregnancy in between 41 and 42 weeks ’, so that ‘ pregnancy should be ended by 42 weeks + 0 days’ (not 41 weeks + 0 days). Interpretation of this recommendation by individual healthcare providers is permitted, and earlier definitions of ‘term’ appear to be used frequently.
Qualitative comments from the women also seemed to indicate confusion around the meaning of ‘term’ and ‘post-term’. It is questionable that 75% of all the women who had induction of labour before the ‘post-term’ period, as recommended by the CGOS, required it for a genuine medical, obstetrical or fetal reason. Considerable variation is seen across the world in induction of labour rates, with no difference in outcomes, indicating that some inductions are unnecessary [ 35 ], as seems to be the situation in the Czech Republic. Induction of labour for subjective, non-medical, reasons was also noted in research from the United States [ 36 ], and is linked in a number of countries with increasing CS rates [ 35 ].
Just over half of the women who had labour induced thought that the reason that this was necessary was discussed sufficiently with them, but 55% had not been given any choice in the decision. The greater involvement of obstetricians at all levels of care in the Czech Republic may account for this lack of choice, as other countries such as the US [ 37 ] have shown that midwifery care encourages women’s decision-making.
When labour is induced by artificial rupture of membranes and/or use of oxytocin infusion or prostaglandin pessaries, the woman is aware of the procedure in advance and, by presenting at the hospital on the date requested, has given tacit (and, usually, written) consent. Thirty-five percent of women in this study had labour induced by the Hamilton manoeuvre (sweeping the membranes) which can be effective in achieving a spontaneous onset of labour and can potentially reduce the incidence of a more formal method of induction of labour [ 38 ]. However, 56% of the 1,364 women who had the Hamilton manoeuvre performed said that the doctor had not asked for their permission beforehand. This is an example of very disrespectful care and may be occurring, unacknowledged, in many other countries as a recent systematic review [ 39 ] failed to find any research in this area. Not gaining women’s consent for interventions or procedures is not uncommon, as is shown in systematic reviews [ 40 , 41 ] and in studies conducted in a myriad of settings globally [ 15 , 16 , 17 , 41 , 42 , 43 ].
The majority of women had a companion of their choice with them throughout labour. However, 11% of women were only permitted to have their companion with them for a short time at the start, or end, of labour, a practice that should never occur; having a companion to support one in labour is a basic human right, upheld by the WHO [ 44 ]. An obstetrician/gynaecologist or doctor provided intrapartum care for 77% of women, and 75% said that they were cared for by a midwife instead of, or as well as, an obstetrician. However, the majority of women (54%) said that they ‘ only had visits ’ from the midwife to check how they were, with no-one present with them throughout the birth process, and 4% said that they did not have a midwife caring for them at all. Lappeman and Swartz’s [ 12 ] qualitative study, which used labour ward observations as the primary data collection method, revealed the ‘silence of the labour ward’ and the ‘neglect of the neglect’ where women in labour ‘lay in beds alone’, rarely with companions. Research findings from across the world show that women who receive continuous labour support (from midwives, doulas, or lay companions), especially from one or two known midwives, are more likely to have shorter labours with less use of pain medication, less intervention, birth spontaneously [ 37 , 45 , 46 ]and be more satisfied [ 47 , 48 , 49 ].
Other instances of non-respectful care are revealed in the responses from 16% of women who said that clinicians looking after them never introduced themselves when they entered the labour room or met them for the first time. Analysis of the psychosocial climate in maternity hospitals in the Czech Republic similarly indicates the need for enhanced communication skills by healthcare providers, especially when communicating consistent information [ 31 , 50 ]. Less than one-third of women had a birth plan but over half of those who had said their plan was not respected or that they were persuaded by the clinician to change their plan during labour. In addition, 20% were not given privacy in the first stage of labour, similar to findings from other studies in Jordan [ 51 ] and Turkey [ 52 ]. Experiencing privacy and healthcare provider courtesy in labour have been shown to be key determinants of maternal satisfaction, in a review of 54 research papers from low-income countries [ 53 ].
Overall, our quantitative and qualitative data reveal aspects of disrespectful prenatal and intrapartum care. Taken in their entirety, there was a considerable number of women who had no information on and no choice in their place of birth, procedures and interventions performed without explanation or consent and who were ‘persuaded’ to alter their plan for their care. Our qualitative comments very much resonate with those in Kuipers et al.’s [ 18 ] study which explored the experiences of women, including women who birthed in the Czech Republic, who had a negative or traumatic birth and the value, sense and meaning assigned to the social space of birth. The authors stated that women frequently experienced their birth environment as coercive and disrespectful, described being ‘physically forced into positions or spaces’ repeatedly (p4) and an environment that depicted ‘scenes of horror’ (p5).
Cohen Shabot [ 54 ] characterises obstetric violence, and any and all forms of disrespecting pregnant women, as a feminist issue which must be examined through feminist views on violence i.e., violence directed at women and part of a general patriarchal oppression of women. She describes it as gender violence because women are its main victims. According to Šmídová et al. (2015), the privately-held and shared convictions amongst obstetricians that change is needed in healthcare relating to childbirth contrasts markedly with their reluctance to say this publicly and be critical of the system. Whilst the opinions of the obstetricians, those who dominate and currently hold the power within the maternity hospitals and services, remain polarised and open discussions are absent, implementation of a woman-centred approach to care and service may be slow. On a more positive note, the Government’s Gender Equality Strategy for 2021–2030 acknowledges that there has long been a strong social demand for a respectful approach and humanisation of obstetrics care for women (acknowledged as being most women) who experience physiological pregnancy and birth (most women). It also states that the Ministry of Health has begun to respond to this by working on the concept for supporting the establishment of midwifery centres within maternity hospitals [ 55 ]. The Strategy also recognises the persistent legislative and restrictions that midwives have long faced and the resulting negative impact on women and their families in terms of choice of place, method and circumstances of childbirth. It also acknowledges that this is further complicated by the absence of national standards of care, the links between the various professions that offer peripartum care, and the repeated criticisms from international institutions and others.
Strengths and limitations
A strength of this study is that data were provided by a large sample: 8,836 women who had experienced birth in one of the 93 hospitals in the Czech Republic, or at home. The inclusion of women’s qualitative comments, including proportions when relevant, provide rich and detailed context on interventions and procedures. The main limitation is that surveys were completed by a self-selecting sample of women, or their partners, and are therefore potentially biased. Whilst we sought to recruit participants from a wide range of sources, including maternity hospitals, obstetric and gynaecology clinics, postnatal centres, kindergartens etc., it is possible that the experiences reported here may not be representative of women birthing in the Czech Republic. Whilst 51% of respondents had birthed their baby more than one year previously, which may raise issues of recall bias, the accuracy of women’s memories of their experiences, and their agreement with data recorded in their maternity care records [ 56 ] even up to five years after the birth, has been documented [ 57 ]. Whilst the views of 69 partners were included, partners answered the questions in relation to their partner’s experiences. We did not analyse these separately but including their information about their partners was deemed important.
Conclusions
Findings reveal a lack of information-giving, discussion and shared decision-making from healthcare professionals in the maternity care services. There are also some indications that some practices were not based on evidence. A thorough audit of clinical practices, in individual hospitals and nationally, and the open publication on labour and birth outcomes, and women’s experiences of care, is needed. Women described unacceptable aspects of care such as having procedures performed without their consent, and concerns around discourtesy of healthcare professionals and lack of privacy. Without doubt, these experiences cause women great distress during, and even after, childbirth. Our findings highlight areas in need of urgent improvement in maternity care services in the Czech Republic. Initiatives such as the Ministry of Health‘s 2015 call for comments from parents on their experiences of services are to be commended and continued, as is the implementation of the Government’s Gender Equality Strategy and other initiatives that target women-centred reformations within the maternity care system.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Hrešanová E. Nobody in a maternity hospital really talks to you: socialist legacies and consumerism in Czech women’s childbirth narratives. Sociologický časopis/Czech Sociol Rev. 2014;50(6):961–85. https://doi.org/10.13060/00380288.2014.50.6.150 .
Article Google Scholar
Šmídová I, Šlesingerová E, Slepičková L. Games of Life. Czech Republic: Masarykova Univerzita.201. Availabe at: https://www.perlego.com/book/3514299/games-of-life-czech-reproductive-biomedicine-sociological-perspectives-pdf .
Hořejší A. Analysis of the current situation in obstetrics with regard to the position of midwives and the possibility of free choice of women. 2020. https://www.unipa.cz/analyza-soucasneho-stavu-v-porodnictvi-s-ohledem-na-postaveni-porodnich-asistentek-a-moznosti-svobodne-volby-zen/ .
Ministry of Health. Methodical recommendation of Ministry of Health for providers of care in fields of gynaecology, obstetrics and neonatology 2020. https://www.mzcr.cz/metodicke-doporuceni-mz-pro-poskytovatele-zdravotnich-sluzeb-v-oboru-gynekologie-a-porodnictvi-a-neonatologie/ .
Vondráčková L, Šmídová I, Working Group on Obstetrics of the Government Council for Gender Equality. Analysis of the discussion Experiences from maternity hospitals established by the Ministry of Health on Facebook. Research report for the. 2015. Masaryk University: Czech Republic. https://vlada.gov.cz/cz/ppov/rovne-prilezitosti-zen-a-muzu/dokumenty/analyza-diskuse-_zkusenosti-z-porodnic_-zalozene-ministerstvem-zdravotnictvi-na-facebooku-146451/ .
Hrešanová E. The Island of Alternatives: power, Medical Science, and Gentle Birthing in Socialist Czechoslovakia. J Hist Med Allied Sci. 2018;73(1):73–95. https://doi.org/10.1093/jhmas/jrx056 .
Article PubMed Google Scholar
White Ribbon Alliance. Respectful Maternity Care: The Universal Rights of Childbearing Women. 2011. http://whiteribbonalliance.org/campaigns2/respectful-maternity-care/ .
WHO. The prevention and elimination of disrespect and abuse during facility-based childbirth. 2014. http://apps.who.int/iris/bitstream/10665/134588/1/WHO_RHR_14.23_eng.pdf?ua=1&ua=1
Durnová A, Hejzlarová E. Domácí porody v Česku: motivace, důvody a názory žen, které rodily plánovaně doma (2015–2020) [Data set]. Zenodo [Role of the intimacy in Czech controversy about home births (GAČR, 18-10042S)]. 2021. https://doi.org/10.5281/zenodo.4767126 .
Bowser D, Hill K. Exploring Evidence for Disrespect and Abuse in Facility-Based Childbirth Report of a Landscape Analysis. USAID-TRAction Project. Harvard School of Public Health. 2020. https://www.ghdonline.org/uploads/Respectful_Care_at_Birth_9-20-101_Final1.pdf .
Miller S, Abalos E, Chamillard M, Ciapponi A, Colaci D, Comande D, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet. 2016;388(10056):2176–92. https://doi.org/10.1016/s0140-6736(16)31472-6 .
Lappeman M, Swartz L. Rethinking obstetric violence and the neglect of neglect: the silence of a labour ward milieu in a South African district hospital. BMC Int Health Hum Rights. 2019;19(1):30. https://doi.org/10.1186/s12914-019-0218-2 .
Article PubMed PubMed Central Google Scholar
Bohren MA, Vogel JP, Hunter EC, Lutsiv O, Makh SK, Souza JP, et al. The mistreatment of women during Childbirth in Health facilities globally: a mixed-methods systematic review. PLoS Med. 2015;12(6):e1001847. https://doi.org/10.1371/journal.pmed.1001847 .
Watson HL, Downe S. Discrimination against childbearing Romani women in maternity care in Europe: a mixed-methods systematic review. Reprod Health. 2017;14(1):1. https://doi.org/10.1186/s12978-016-0263-4 .
Annborn A, Finnbogadóttir HR. Obstetric violence a qualitative interview study. Midwifery. 2022;105:103212. https://doi.org/10.1016/j.midw.2021.103212 .
Correa M, Klein K, Vasquez P, Williams CR, Gibbons L, Cormick G, et al. Observations and reports of incidents of how birthing persons are treated during childbirth in two public facilities in Argentina. Int J Gynaecol Obstet. 2022;158(1):35–43. https://doi.org/10.1002/ijgo.13938 .
Greely JT, Dongarwar D, Crear L, Adeyeye M, Reyna-Carrillo A, Salihu HM. Violence against pregnant women and adverse maternal/ fetal outcomes in the United States: racial/ethnic disparities. Women Health. 2022;62(6):513–21. https://doi.org/10.1080/03630242.2022.2074610 .
Kuipers YJ, Thomson G, Goberna-Tricas J, Zurera A, Hresanová E, Temesgenová N et al. The social conception of space of birth narrated by women with negative and traumatic birth experiences. Women Birth. 2022;S1871-5192(22):00079 – 8. https://doi.org/10.1016/j.wombi.2022.04.013 .
van der Pijl MSG, Verhoeven CJM, Verweij R, van der Linden T, Kingma E, Hollander MH, et al. Disrespect and abuse during labour and birth amongst 12,239 women in the Netherlands: a national survey. Reprod Health. 2022;19(1):160. https://doi.org/10.1186/s12978-022-01460-4 .
O’Brien E, Rich M. Obstetric violence in historical perspective. Lancet. 2022;399(10342):2183–5. https://doi.org/10.1016/s0140-6736(22)01022-4 .
Český Žurnál. Pět zrození, Žurnál Č. Editor. 2015. https://www.youtube.com/watch?v=f-CZgwTC5bk .
Hnilicová J. Jak se kde rodí? 2021. http://jaksekderodi.cz/soudni-spor-2/ .
Begley C, Sedlicka N, Daly D. Respectful and disrespectful care in the Czech Republic: an online survey. Reprod Health. 2018;15(1):198. https://doi.org/10.1186/s12978-018-0648-7 .
Formánková L, Hejzlarová E. Giving birth as a struggle between bodily needs and medical practice, in Making and Doing Exhibition Society for Social Studies of Science (4S). 2020. Available at; https://www.youtube.com/watch?v=5jHBw8NB_8Y .
Shakibazadeh E, Namadian M, Bohren MA, Vogel JP, Rashidian A, Nogueira Pileggi V, et al. Respectful care during childbirth in health facilities globally: a qualitative evidence synthesis. BJOG. 2018;125(8):932–42. https://doi.org/10.1111/1471-0528.15015 .
Article CAS PubMed Google Scholar
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. https://doi.org/10.1191/1478088706qp063oa .
Kitto SC, Chesters J, Grbich C. Quality in qualitative research. Med J Aust. 2008;188(4):243–6. https://doi.org/10.5694/j.1326-5377.2008.tb01595.x .
Hinton L, Dumelow C, Rowe R, Hollowell J. Birthplace choices: what are the information needs of women when choosing where to give birth in England? A qualitative study using online and face to face focus groups. BMC Pregnancy Childbirth. 2018;18(1):12. https://doi.org/10.1186/s12884-017-1601-4 .
Naylor Smith J, Taylor B, Shaw K, Hewison A, Kenyon S. I didn’t think you were allowed that, they didn’t mention that.’ A qualitative study exploring women’s perceptions of home birth. BMC Pregnancy Childbirth. 2018;18(1):105. https://doi.org/10.1186/s12884-018-1733-1 .
Halfdansdottir B, Wilson ME, Hildingsson I, Olafsdottir OA, Smarason AK, Sveinsdottir H. Autonomy in place of birth: a concept analysis. Med Health Care Philos. 2015;18(4):591–600. https://doi.org/10.1007/s11019-015-9624-y .
Takács L, Seidlerová J. [Psychosocial climate in maternity hospitals from the perspective of parturients I. results from a national survey on perinatal care satisfaction using a representative sample of 1195 Czech parturients]. Ceska Gynekol. 2013;78(2):157–68. PMID: 23710980.
PubMed Google Scholar
Holten L, de Miranda E. Women׳s motivations for having unassisted childbirth or high-risk homebirth: an exploration of the literature on ‘birthing outside the system’. Midwifery. 2016;38:55–62. https://doi.org/10.1016/j.midw.2016.03.010 .
Amyx M, Philibert M, Farr A, Donati S, Smárason AK, Tica V, Velebil P, Alexander S, Durox M, Elorriaga MF, Heller G, Kyprianou T, Mierzejewska E, Verdenik I, Zīle-Velika I, Zeitlin J. Trends in caesarean section rates in Europe from 2015 to 2019 using Robson’s Ten Group classification system: a Euro-Peristat study. BJOG. 2023. https://doi.org/10.1111/1471-0528.17670 .
Czech Gynecological and Obstetrical Society. Post-term pregnancy. 2016. https://www.figo.org/czech-gynecological-and-obstetrical-society .
Seijmonsbergen-Schermers AE, van den Akker T, Rydahl E, Beeckman K, Bogaerts A, Binfa L, et al. Variations in use of childbirth interventions in 13 high-income countries: a multinational cross-sectional study. PLoS Med. 2020;17(5):e1003103. https://doi.org/10.1371/journal.pmed.1003103 .
Salahuddin M, Davidson C, Lakey DL, Patel DA. Characteristics Associated with induction of Labor and Delivery Route among Primiparous Women with Term deliveries in the listening to mothers III study. J Womens Health (Larchmt). 2018;27(5):590–8. https://doi.org/10.1089/jwh.2017.6598 .
Declercq ER, Belanoff C, Sakala C. Intrapartum Care and experiences of women with midwives Versus obstetricians in the listening to mothers in California Survey. J Midwifery Womens Health. 2020;65(1):45–55. https://doi.org/10.1111/jmwh.13027 .
Finucane EM, Murphy DJ, Biesty LM, Gyte GM, Cotter AM, Ryan EM, et al. Membrane sweeping for induction of labour. Cochrane Database Syst Rev. 2020;2(2):Cd000451. https://doi.org/10.1002/14651858.CD000451.pub3 .
Roberts J, Evans K, Spiby H, Evans C, Pallotti P, Eldridge J. Women’s information needs, decision-making and experiences of membrane sweeping to promote spontaneous labour. Midwifery. 2020;83:102626. https://doi.org/10.1016/j.midw.2019.102626 .
Bohren MA, Mehrtash H, Fawole B, Maung TM, Balde MD, Maya E, et al. How women are treated during facility-based childbirth in four countries: a cross-sectional study with labour observations and community-based surveys. Lancet. 2019;394(10210):1750–63. https://doi.org/10.1016/s0140-6736(19)31992-0 .
Khalil M, Carasso KB, Kabakian-Khasholian T. Exposing Obstetric Violence in the Eastern Mediterranean Region: a review of women’s narratives of disrespect and abuse in Childbirth. Front Glob Womens Health. 2022;3:850796. https://doi.org/10.3389/fgwh.2022.850796 .
Mayra K, Sandall J, Matthews Z, Padmadas SS. Breaking the silence about obstetric violence: body mapping women’s narratives of respect, disrespect and abuse during childbirth in Bihar, India. BMC Pregnancy Childbirth. 2022;22(1):318. https://doi.org/10.1186/s12884-022-04503-7 .
Smith-Oka V. Cutting women: unnecessary cesareans as iatrogenesis and obstetric violence. Soc Sci Med. 2022;296:114734. https://doi.org/10.1016/j.socscimed.2022.114734 .
WHO. WHO recommendation on companionship during labour and childbirth. 2018. https://extranet.who.int/rhl/topics/preconception-pregnancy-childbirth-and-postpartum-care/care-during-childbirth/who-recommendation-companionship-during-labour-and-childbirth .
Begley C, Devane D, Clarke M, McCann C, Hughes P, Reilly M, et al. Comparison of midwife-led and consultant-led care of healthy women at low risk of childbirth complications in the Republic of Ireland: a randomised trial. BMC Pregnancy Childbirth. 2011;11:85. https://doi.org/10.1186/1471-2393-11-85 .
Loewenberg Weisband Y, Klebanoff M, Gallo MF, Shoben A, Norris AH. Birth outcomes of women using a midwife versus women using a physician for prenatal care. J Midwifery Womens Health. 2018;63(4):399–409. https://doi.org/10.1111/jmwh.12750 .
Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2017;7(7):Cd003766. https://doi.org/10.1002/14651858.CD003766.pub6 .
Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev. 2016;4:Cd004667. https://doi.org/10.1002/14651858.CD004667.pub5 .
Hildingsson I, Karlström A, Larsson B. A continuity of care project with two on-call schedules: findings from a rural area in Sweden. Sex Reprod Healthc. 2020;26:100551. https://doi.org/10.1016/j.srhc.2020.100551 .
Takács L, Seidlerová J. [Psychosocial climate in maternity hospitals from the perspective of parturients II. Predictors of womens satisfaction with perinatal care in the Czech Republic]. Ceska Gynekol. 2013;78(3):269–75. PMID: 23869834.
Hussein S, Dahlen HG, Ogunsiji O, Schmied V. Uncovered and disrespected. A qualitative study of Jordanian women’s experience of privacy in birth. Women Birth. 2020;33(5):496–504. https://doi.org/10.1016/j.wombi.2019.10.006 .
Deliktas Demirci A, Kabukcuglu K, Haugan G, Aune I. I want a birth without interventions: women’s childbirth experiences from Turkey. Women Birth. 2019;32(6):e515–22. https://doi.org/10.1016/j.wombi.2018.12.011 .
Srivastava A, Avan BI, Rajbangshi P, Bhattacharyya S. Determinants of women’s satisfaction with maternal health care: a review of literature from developing countries. BMC Pregnancy Childbirth. 2015;15:97. https://doi.org/10.1186/s12884-015-0525-0 .
Cohen Shabot S. Making loud bodies feminine: a Feminist-Phenomenological analysis of Obstetric Violence. Hum Stud. 2016;39(2):231–47. https://doi.org/10.1007/s10746-015-9369-x .
Office of the Government of the Czech Republic. Gender Equality Strategy for 2021–2030. 2021: Czech Republic. https://vlada.gov.cz/assets/ppov/gcfge/Gender-Equality-Strategy-2021-2030.pdf .
Gartland D, Lansakara N, Flood M, Brown SJ. Assessing obstetric risk factors for maternal morbidity: congruity between medical records and mothers’ reports of obstetric exposures. Am J Obstet Gynecol. 2012;206(2):e1521–10. https://doi.org/10.1016/j.ajog.2011.10.863 .
Takehara K, Noguchi M, Shimane T, Misago C. A longitudinal study of women’s memories of their childbirth experiences at five years postpartum. BMC Pregnancy Childbirth. 2014;14(1):221. https://doi.org/10.1186/1471-2393-14-221 .
Download references
Acknowledgements
We would like to thank all the respondents for taking the time to complete the survey and including their detailed comments. We thank Veronika Nezbedová for helping with the preparation of the questionnaire and translating the survey from English to Czech. We would like to thank Dominika Kůželová (APODAC) who contributed to the data analysis and the numerous other people who helped distribute the survey.
This study was unfunded.
Author information
Authors and affiliations.
School of Nursing and Midwifery, Trinity College Dublin, 24 D’Olier Street, Dublin, DO2 T283, Ireland
Deirdre Daly & Cecily Begley
Association for Birth Houses & Centers (APODAC), Týnská ulička 1064/6, , Prague 1, 11000, Czech Republic
Natalie Sedlicka, Kateřina Švanderlíková & PetraAnn Ann Kovařčíková
Faculty of Medicine, Department of Health Sciences, Masaryk University, Brno, Czech Republic
Radka Wilhelmová
You can also search for this author in PubMed Google Scholar
Contributions
DD: contributed to the survey design, and manuscript writing/editing.CB: study development, survey design, data analysis, manuscript writing/editing. NS: contributed to the survey design, translated the study information and survey questions from English to the Czech language, data analysis, translated the qualitative data from Czech to English, manuscript writing/editing. KS: project administration in CZ, contributed to data analysis and review. PK: contributed to translation, data analysis, review and editing. RW: contributed to review and editing. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Deirdre Daly .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was granted by the Research Ethics Committee, School of Nursing and Midwifery, Trinity College Dublin [14 November 2016]. At the start of the survey, participants were informed that the survey was anonymous and that submission of the survey was taken as giving consent to participate.
Consent for publication
Not applicable. The manuscript does not manuscript contain any individual person’s data in any form.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Daly, D., Sedlicka, N., Švanderlíková, K. et al. An online survey of women’s views of respectful and disrespectful pregnancy and early labour care in the Czech Republic. BMC Pregnancy Childbirth 24 , 370 (2024). https://doi.org/10.1186/s12884-024-06448-5
Download citation
Received : 06 January 2023
Accepted : 26 March 2024
Published : 15 May 2024
DOI : https://doi.org/10.1186/s12884-024-06448-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Decision-making
- Maternity care
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Introduction
- Conclusions
- Article Information
Evidence reviews for the US Preventive Services Task Force (USPSTF) use an analytic framework to visually display the key questions that the review will address to allow the USPSTF to evaluate the effectiveness and safety of a preventive service. The questions are depicted by linkages that relate to interventions and outcomes. A dashed line depicts a health outcome that follows an intermediate outcome. Further details are available in the USPSTF Procedure Manual. 22
Articles could be reviewed for more than 1 key question (KQ). Reasons for exclusion: Intervention: Study intervention included prognostic evaluations to inform disease management, secondary diagnostic evaluations, or other interventions in addition to screening. Population: Study was not conducted in an included population. Design: Study did not use an included design. Comparator: Study not conducted with an included comparison group. Outcomes: Study did not have relevant outcomes or had incomplete outcomes. Quality: Study was poor quality. Setting: Study was not conducted in a country relevant to US practice. Screening: Study did not have an included screening test.
eMethods. Literature Search Strategies for Primary Literature
eTable 1. Inclusion and Exclusion Criteria
eTable 2. Quality Assessment Criteria
- Trends in Cardiovascular Health Counseling Among Postpartum Individuals JAMA Original Investigation July 25, 2023 Using data from the Pregnancy Risk Assessment Monitoring System, this study evaluates trends (2016-2020) in prevalence of postpartum counseling for healthy eating, exercise, and losing weight gained during pregnancy among individuals with prepregnancy cardiovascular disease risk factors or adverse pregnancy outcomes. Natalie A. Cameron, MD, MPH; Lynn M. Yee, MD, MPH; Brigid M. Dolan, MD, MEd; Matthew J. O’Brien, MD; Philip Greenland, MD; Sadiya S. Khan, MD, MSc
- USPSTF Recommendation: Screening for Hypertensive Disorders of Pregnancy JAMA US Preventive Services Task Force September 19, 2023 This 2023 Recommendation Statement from the US Preventive Services Task Force recommends screening for hypertensive disorders in pregnant persons with blood pressure measurements throughout pregnancy (B recommendation). US Preventive Services Task Force; Michael J. Barry, MD; Wanda K. Nicholson, MD, MPH, MBA; Michael Silverstein, MD, MPH; Michael D. Cabana, MD, MA, MPH; David Chelmow, MD; Tumaini Rucker Coker, MD, MBA; Esa M. Davis, MD, MPH; Katrina E. Donahue, MD, MPH; Carlos Roberto Jaén, MD, PhD, MS; Li Li, MD, PhD, MPH; Gbenga Ogedegbe, MD, MPH; Goutham Rao, MD; John M. Ruiz, PhD; James Stevermer, MD, MSPH; Joel Tsevat, MD, MPH; Sandra Millon Underwood, PhD, RN; John B. Wong, MD
- Hypertension Screening in Pregnancy JAMA Editorial September 19, 2023 Anna E. Denoble, MD, MSc; Christian M. Pettker, MD
- Patient Information: Screening for High Blood Pressure Disorders During Pregnancy JAMA JAMA Patient Page September 19, 2023 This JAMA Patient Page describes the pros and cons of screening for high blood pressure disorders during pregnancy, and who should be screened. Jill Jin, MD, MPH
- Early Identification of Individuals at Risk for Hypertensive Disorders of Pregnancy JAMA Network Open Editorial September 19, 2023 Janelle Santos, MD; Mauro H. Schenone, MD; Vesna D. Garovic, MD, PhD
- Screening for Hypertensive Disorders of Pregnancy in the US—A New Hypertensive Urgency JAMA Internal Medicine Editorial November 1, 2023 Srilakshmi Mitta, MD; Cary P. Gross, MD; Melissa A. Simon, MD, MPH
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
- CME & MOC
Henderson JT , Webber EM , Thomas RG , Vesco KK. Screening for Hypertensive Disorders of Pregnancy : Updated Evidence Report and Systematic Review for the US Preventive Services Task Force . JAMA. 2023;330(11):1083–1091. doi:10.1001/jama.2023.4934
Manage citations:
© 2024
- Permissions
Screening for Hypertensive Disorders of Pregnancy : Updated Evidence Report and Systematic Review for the US Preventive Services Task Force
- 1 Kaiser Permanente Evidence-based Practice Center, Center for Health Research, Kaiser Permanente, Portland, Oregon
- 2 CareOregon, Portland
- Editorial Hypertension Screening in Pregnancy Anna E. Denoble, MD, MSc; Christian M. Pettker, MD JAMA
- Editorial Early Identification of Individuals at Risk for Hypertensive Disorders of Pregnancy Janelle Santos, MD; Mauro H. Schenone, MD; Vesna D. Garovic, MD, PhD JAMA Network Open
- Editorial Screening for Hypertensive Disorders of Pregnancy in the US—A New Hypertensive Urgency Srilakshmi Mitta, MD; Cary P. Gross, MD; Melissa A. Simon, MD, MPH JAMA Internal Medicine
- Original Investigation Trends in Cardiovascular Health Counseling Among Postpartum Individuals Natalie A. Cameron, MD, MPH; Lynn M. Yee, MD, MPH; Brigid M. Dolan, MD, MEd; Matthew J. O’Brien, MD; Philip Greenland, MD; Sadiya S. Khan, MD, MSc JAMA
- US Preventive Services Task Force USPSTF Recommendation: Screening for Hypertensive Disorders of Pregnancy US Preventive Services Task Force; Michael J. Barry, MD; Wanda K. Nicholson, MD, MPH, MBA; Michael Silverstein, MD, MPH; Michael D. Cabana, MD, MA, MPH; David Chelmow, MD; Tumaini Rucker Coker, MD, MBA; Esa M. Davis, MD, MPH; Katrina E. Donahue, MD, MPH; Carlos Roberto Jaén, MD, PhD, MS; Li Li, MD, PhD, MPH; Gbenga Ogedegbe, MD, MPH; Goutham Rao, MD; John M. Ruiz, PhD; James Stevermer, MD, MSPH; Joel Tsevat, MD, MPH; Sandra Millon Underwood, PhD, RN; John B. Wong, MD JAMA
- JAMA Patient Page Patient Information: Screening for High Blood Pressure Disorders During Pregnancy Jill Jin, MD, MPH JAMA
Importance Hypertensive disorders of pregnancy are a leading cause of pregnancy-related morbidity and mortality in the US.
Objective To conduct a targeted systematic review to update the evidence on the effectiveness of screening for hypertensive disorders of pregnancy to inform the US Preventive Services Task Force.
Data Sources MEDLINE and the Cochrane Central Register of Controlled Trials for relevant studies published between January 1, 2014, and January 4, 2022; surveillance through February 21, 2023.
Study Selection English-language comparative effectiveness studies comparing screening strategies in pregnant or postpartum individuals.
Data Extraction and Synthesis Two reviewers independently appraised articles and extracted relevant data from fair-or good-quality studies; no quantitative synthesis was conducted.
Main outcomes and measures Morbidity or mortality, measures of health-related quality of life.
Results The review included 6 fair-quality studies (5 trials and 1 nonrandomized study; N = 10 165) comparing changes in prenatal screening practices with usual care, which was routine screening at in-person office visits. No studies addressed screening for new-onset hypertensive disorders of pregnancy in the postpartum period. One trial (n = 2521) evaluated home blood pressure measurement as a supplement to usual care; 3 trials (total n = 5203) evaluated reduced prenatal visit schedules. One study (n = 2441) evaluated proteinuria screening conducted only for specific clinical indications, compared with a historical control group that received routine proteinuria screening. One additional trial (n = 80) only addressed the comparative harms of home blood pressure measurement. The studies did not report statistically significant differences in maternal and infant complications with alternate strategies compared with usual care; however, estimates were imprecise for serious, rare health outcomes. Home blood pressure measurement added to prenatal care visits was not associated with earlier diagnosis of a hypertensive disorder of pregnancy (104.3 vs 106.2 days), and incidence was not different between groups in 3 trials of reduced prenatal visit schedules. No harms of the different screening strategies were identified.
Conclusions and Relevance This review did not identify evidence that any alternative screening strategies for hypertensive disorders of pregnancy were more effective than routine blood pressure measurement at in-person prenatal visits. Morbidity and mortality from hypertensive disorders of pregnancy can be prevented, yet American Indian/Alaska Native persons and Black persons experience inequitable rates of adverse outcomes. Further research is needed to identify screening approaches that may lead to improved disease detection and health outcomes.
Hypertensive disorders of pregnancy include gestational hypertension; preeclampsia-eclampsia; and chronic hypertension with superimposed preeclampsia. 1 , 2 The incidence of hypertensive disorders of pregnancy has been steadily increasing over the last several decades, from 500 cases per 10 000 deliveries in 1993 to 1021 cases per 10 000 deliveries in 2016 to 2017, with more than half of these having a diagnosis of preeclampsia-eclampsia (555 cases per 10 000 deliveries). 3 Between 2014 and 2017 hypertensive disorders of pregnancy were responsible for 6.8% of pregnancy-related deaths overall, with the majority of deaths (65%) occurring in the 6 weeks following delivery. 4 , 5 In addition to risks of mortality to pregnant individuals, hypertensive disorders of pregnancy contributes to pregnancy-related morbidity and risks to the fetus, including fetal growth restriction and indicated preterm delivery. 6 - 10
Hypertensive disorders of pregnancy account for a larger proportion of pregnancy-related mortality and morbidity among Black populations than among White populations. 11 - 16 Due to higher incidence and severity, alongside inequities in the quality of health care due to structural and systemic factors, 17 , 18 the risk of dying of preeclampsia-eclampsia complications is about 5 times greater for Black individuals (3.93 per 100 000 live births) than for White individuals (0.78 per 100 000 live births). 12 , 16 Hypertensive disorders of pregnancy are also a leading cause of pregnancy-related mortality (≈13% of deaths) among American Indian/Alaska Native people and contributes to higher pregnancy-related mortality among American Indian/Alaska Native persons compared with White persons (29.7 compared with 12.7 per 100 000 live births in 2007-2016). 7 , 11 , 19
In 2017, the US Preventive Services Task Force (USPSTF) recommended screening pregnant women for preeclampsia with blood pressure measurements throughout pregnancy (grade B). 20 Routine screening for new-onset hypertension via office-based blood pressure measurement can identify individuals who develop hypertensive disorders of pregnancy, allowing for evidence-based interventions that reduce the risk of pregnancy complications for the pregnant individual and infant. 1 , 20 , 21 This review of comparative effectiveness studies sought evidence on potential refinements to recommended screening practice.
An analytic framework and 3 key questions (KQs) guided the evidence update ( Figure 1 ). Detailed methods and results of this systematic review are available in the full evidence report. 23 This review examines the comparative effectiveness of different screening protocols for hypertensive disorders of pregnancy, including preeclampsia.
A search of MEDLINE and the Cochrane Central Register of Controlled Trials was conducted for literature published between January 1, 2014, and January 4, 2022 (eMethods in the Supplement ). These searches were supplemented by examining reference lists of primary studies and reviews. ClinicalTrials.gov was searched for ongoing trials. From January 2022 through February 1, 2023, ongoing surveillance of the literature to identify new studies that might affect the review conclusions or interpretation of the evidence was conducted using article alerts and targeted searches of journals with high impact factors; we identified no new studies that would meet inclusion criteria for this review.
For all KQs, studies were eligible if they addressed the comparative effectiveness of screening for hypertensive disorders of pregnancy using approaches that varied the frequency, setting, or methods of measurement using either randomized or nonrandomized designs. Studies that evaluated the changes in the frequency or timing of prenatal care visits were included if frequency of blood pressure measurement could be determined from study methods. Included studies enrolled populations of pregnant women and pregnant persons of all genders without a known diagnosis of HDP or chronic hypertension. Gender of the included populations in this review and in epidemiologic evidence tends to be inferred based on physiology (ie, pregnancy) rather than reported by patients. Therefore, we adopt inclusive language throughout this review, recognizing that not all pregnant individuals are cisgender women.
Studies were excluded if effects of changes to screening programs could not be separated from the effects of concurrent interventions (eg, patient education, service delivery model). Studies that evaluated the effectiveness of diagnostic testing or monitoring among people with hypertensive disorders of pregnancy, including those with chronic hypertension in pregnancy, were not eligible for inclusion. The definition of hypertensive disorders of pregnancy includes pregnant individuals with chronic hypertension. However, this review only included studies evaluating screening for new-onset hypertension because individuals entering pregnancy with a diagnosis of chronic hypertension would be subject to ongoing monitoring and assessment recommended for individuals with hypertensive disorders of pregnancy. Studies of the performance of risk prediction tools were not included in this review, although comparative effectiveness trials involving risk assessment would have been eligible for inclusion (eTable 1 in the Supplement ).
Two investigators independently evaluated whether articles met the review inclusion criteria and rated the risk of bias of included studies following USPSTF procedures for assessing the internal validity of randomized clinical trials (RCTs) and nonrandomized studies of interventions (eTable 2 in the Supplement ). 22 Discrepancies were resolved through discussion and consultation with a third investigator as needed. Study data were extracted into structured forms and checked for errors by a second investigator. Included outcomes were mortality, morbidity related to hypertensive disorders of pregnancy, measures of health-related quality of life, and adverse events (including missed diagnosis). The strength of the overall body of evidence for each KQ was judged using an adaptation of the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) Working Group approach. 24 The Evidence-based Practice Center adaptation 25 addresses 4 domains: consistency, precision, reporting bias, and study quality. Strength of evidence was independently assessed as “High,” “Moderate,” “Low,” or “Insufficient” by at least 2 investigators, with discrepancies resolved through consensus discussion. Given the limited number of studies and their clinical heterogeneity, we did not conduct any quantitative synthesis. Detailed results are available in the full evidence synthesis report. 23
The search identified 6316 titles and abstracts and 82 full-text articles ( Figure 2 ). Six fair-quality studies, 5 RCTs 26 - 30 and 1 nonrandomized study with a historical control 31 (N = 10 165) were included ( Table 1 ). The studies compared usual screening with strategies involving home blood pressure measurement (2 studies, n = 2521), prenatal care schedules with less frequent office visits compared with the usual number (3 studies, n = 5203), and urine screening tests conducted for patients selected based on specific clinical indications, rather than routinely (1 study, n = 2441). Five of the studies 26 , 28 - 31 were included for examination of benefits of alternative screening strategies (KQ1, KQ2), and 1 study 27 of home blood pressure measurement screening was additionally included for harms (KQ3). All studies were conducted during the prenatal period, with no studies examining screening for new-onset hypertensive disorders of pregnancy during the postpartum period. Overall, the strength of the evidence was judged to be insufficient for nearly all comparisons and outcomes available ( Table 2 ).
The effectiveness of home blood pressure measurement in addition to office-based measurement was addressed in 1 fair-quality RCT conducted in the UK (n = 2441). 29 The BUMP 1 (Blood Pressure Monitoring in High Risk Pregnancy to Improve the Detection and Monitoring of Hypertension 1) trial examined the effect of home blood pressure measurement and automated feedback from a mobile-phone application as supplements to routine office-based prenatal care screening. The comparison group received routine office-based screening. Individuals were recruited into the trial based on an increased risk of a hypertensive disorder of pregnancy based on common clinical risk factors (eg, nulliparity, age, pregnancy, family history, previous preeclampsia, body mass index >30 [calculated as weight in kilograms divided by the square of height in meters], twin pregnancy, diabetes). The study population was reported as Asian or Asian British (10%), Black or Black British (8%), White (British, Irish, other) (74%), and “other or mixed” race and ethnicity (not specified by authors) (7%). Approximately 1 of 5 (17%) had a clinical history of a hypertensive disorder of pregnancy in a prior pregnancy, and a majority were nulliparous (61%). The study examined several serious maternal and infant health outcomes; none were statistically significant between study groups, but most were rare events with imprecise estimated effects. A composite outcome defined as 1 or more serious maternal health complications related to hypertensive disorders of pregnancy (eclampsia; transient ischemic attack; stroke; HELLP [hemolysis, elevated liver enzyme levels, low platelet count] syndrome; pulmonary edema; and liver, kidney, or hematologic involvement) was not statistically different between groups (relative risk [RR], 0.79 [95% CI, 0.40-1.55]). The primary study outcome, mean difference between groups in days to detection of hypertensive disorder of pregnancy, was less than 2 days (SD, 1.6) and not statistically significant (95% CI, −8.1 to 4.9). The BUMP 1 trial 29 and an additional RCT (n = 80) 27 met inclusion criteria for examining harms of home blood pressure measurement in addition to regular office-based screening (KQ3). Neither study reported differences in anxiety or health-related quality of life during pregnancy or postpartum for individuals using home blood pressure measurement devices.
We identified 3 fair-quality RCTs (n = 5203) that compared different prenatal visit schedules among individuals identified as at low risk for pregnancy complications. 26 , 28 , 30 Those in the intervention group were assigned to reduced prenatal care visit schedules (6-9 visits) relative to standard visit schedules (≈14 visits), thus receiving fewer in-office blood pressure measurements to screen for a hypertensive disorder of pregnancy, as well as other counseling and screening services. In all 3 of these trials, the difference in the overall number of visits between study groups was smaller than intended by the trial design, with the difference between groups ranging from 2.2 to 3.2 visits. The studies were underpowered for rare, serious health outcomes and reported no differences between study groups in preterm delivery, perinatal mortality, placental abruption, or postpartum hemorrhage; nor were there differences in the proportion diagnosed with preeclampsia. No differences in anxiety or depression were identified between groups receiving standard compared with reduced prenatal visit schedules.
We identified 1 fair-quality single nonrandomized study that compared a historical control group with routine urine screening at every prenatal visit vs screening only when clinically indicated (eg, based on weight loss, elevated blood pressure, urinary symptoms) (n = 2441). 31 The study enrolled Black women (9%), Hispanic women (75%), White women (19%), and “others” without race and ethnicity information reported (6%). There was no difference in the proportion of individuals diagnosed with a hypertensive disorder of pregnancy after the transition to indicated urine screening only (RR, 1.00 [95% CI, 0.74-1.36]). There was a reduced risk of preterm delivery with indicated screening compared with the historical comparison group that underwent routine screening (RR, 0.64 [95% CI, 0.45-0.90]); no other differences in health outcomes were found. However, reviewers assessed this study as having considerable risk of bias owing to changes in the population and the health care setting over the course of the study.
This review did not find evidence that specific strategies for screening for hypertensive disorders of pregnancy in addition to or as an alternative to standard prenatal visit schedules with in-office blood pressure assessment improved health outcomes or led to earlier or increased detection relative to standard prenatal care. The available evidence on the comparative effectiveness of screening did not suggest that any specific features of screening programs improved health outcomes relative to standard prenatal care. However, the studies addressing these questions were few in number and were underpowered for important pregnancy health outcomes and potential harms of different screening programs. A 2022 literature review of screening for hypertensive disorders of pregnancy also examined evidence regarding prenatal visit schedules and the use of telehealth visits for routine antenatal care and similarly found limited evidence available for comparing different prenatal schedules and virtual care approaches for antenatal health care and their effects on health outcomes. 32 Telehealth interventions using home blood pressure measurements could improve access to care and strengthen health care connections over the course of pregnancy, especially in settings that have instituted virtual care for some prenatal visits, but the evidence available to assess whether specific innovations involving telehealth might improve outcomes or lead to adverse or unintended consequences is limited. Whether telehealth could help address inequities in health also is uncertain. Evidence from natural experiments in telehealth-delivered prenatal care during the COVID-19 pandemic may stimulate further research and innovation. 33 , 34
None of the studies identified in this review had adequate power to evaluate outcomes specifically for American Indian/Alaska Native or Black persons, who are the US populations with the highest rates of hypertensive disorders of pregnancy. Few or none of the participants in the included studies were from these populations. Inequities in hypertensive disorders of pregnancy and related morbidity and mortality for Black individuals are well documented and persistent. 35 , 36 Several frameworks have been developed to describe the individual, interpersonal, community, and societal factors contributing to health inequities and the higher incidence of hypertensive disorders of pregnancy and greater disease severity and mortality among American Indian/Alaska Native and Black individuals. 17 , 37 - 40
Despite evidence that complications from missed diagnoses or emergent hypertensive disorders of pregnancy are known to arise postpartum and contribute to poor outcomes, 41 none of the included studies evaluated hypertensive disorders of pregnancy screening in the postpartum period. Opportunities to be screened during the postpartum period may be limited due to clinician and insurance transitions, a focus on the neonate, and reduced continuity of support. 42 - 44 A 2019 systematic review that included 9 observational studies on postpartum monitoring of hypertensive disorders of pregnancy and gestational diabetes reported a pattern of lower rates of follow-up for Black and Hispanic people than White people in the 6 weeks after delivery. 42 Routine screening during the postpartum period could be important for reducing health inequities, especially in light of emerging evidence that the risk of postpartum preeclampsia diagnosis is twice as high for non-Hispanic Black individuals compared with non-Hispanic White individuals. 45
Another area with limited research is the use of home blood pressure measurement to screen for new-onset hypertensive disorders of pregnancy. Although home blood pressure measurement and self-measurement have been used as part of management of care for individuals with diagnosed hypertensive disorder of pregnancy, limited evidence exists for its use as a primary screening tool. The single included trial evaluating supplemental home blood pressure measurement accompanied by automated feedback using a mobile-phone application reported null findings for health benefits but no harms associated with the intervention. 29
Routine measurement of blood pressure during pregnancy has long been a standard of prenatal care. 46 Innovations in screening programs involving changes to standard prenatal visit schedules, virtual visits, and telehealth applications, or the use of home blood pressure measurement, have the potential to influence pregnancy outcomes. Large, well-designed studies to refine prenatal and postpartum screening programs for individuals at different levels of risk for developing hypertensive disorders of pregnancy are needed, with attention to populations at increased risk for complications from hypertensive disorders of pregnancy. Establishing evidence-based screening practices will require large studies to evaluate changes to hypertensive disorders of pregnancy screening programs that could improve health outcomes without incurring harms.
This review did not identify evidence that any alternative screening strategies for hypertensive disorders of pregnancy were more effective than routine blood pressure measurement at in-person prenatal visits. Morbidity and mortality from hypertensive disorders of pregnancy can be prevented, yet American Indian/Alaska Native persons and Black persons experience inequitable rates of adverse outcomes. Further research is needed to identify screening approaches that may lead to improved disease detection and health outcomes.
Accepted for Publication: March 14, 2023.
Corresponding Author: Jillian T. Henderson, PhD, Kaiser Permanente Evidence-based Practice Center, Center for Health Research, Kaiser Permanente Northwest, 3800 N Interstate Ave, Portland, OR 97227 ( [email protected] ).
Author Contributions: Dr Henderson had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: All authors.
Acquisition, analysis, or interpretation of data: Henderson, Webber, Vesco.
Drafting of the manuscript: Henderson.
Critical revision of the manuscript for important intellectual content: Webber, Thomas, Vesco.
Administrative, technical, or material support: Webber, Thomas.
Supervision: Henderson.
Conflict of Interest Disclosures: Dr Vesco reported receiving grants from Pfizer Independent Grants for Learning and Change Funding awarded to her institution for a project to develop and test a novel menopause curriculum for medial residents. No other disclosures were reported.
Funding/Support: This research was funded under contract 75Q80120D00004, Task Order 1, from the Agency for Healthcare Research and Quality (AHRQ), US Department of Health and Human Services.
Role of the Funder/Sponsor: Investigators worked with USPSTF members and AHRQ staff to develop the scope, analytic framework, and key questions for this review. AHRQ had no role in study selection, quality assessment, or synthesis. AHRQ staff provided project oversight; reviewed the report to ensure that the analysis met methodological standards; and distributed the draft for peer review. Otherwise, AHRQ had no role in the conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript findings. The opinions expressed in this document are those of the authors and do not reflect the official position of AHRQ or the US Department of Health and Human Services.
Additional Contributions: We gratefully acknowledge the following individuals for their contributions to this project: Iris R. Mabry-Hernandez, MD, MPH (AHRQ); current and former members of the USPSTF who contributed to topic deliberations; and Evidence-based Practice Center staff members Sarah I. Bean, MPH, Neon Brooks, PhD, and Melinda Davies, MAIS, for technical and editorial assistance at the Kaiser Permanente Center for Health Research. USPSTF members, peer reviewers, and federal partner reviewers did not receive financial compensation for their contributions.
Additional Information: A draft version of this evidence report underwent external peer review from 4 content experts (Kimberly D. Gregory, MD, MPH, Cedars-Sinai Medical Center; Laura A. Magee, MD, King’s College London; Alex Friedman Peahl, MD, MS, University of Michigan; Katherine Tucker, PhD, University of Oxford), and 3 federal partners (Centers for Disease Control and Prevention; the National Heart, Lung, and Blood Institute; and the National Institutes of Health Office of Research on Women’s Health). Comments were presented to the USPSTF during its deliberation of the evidence and were considered in preparing the final evidence review.
Editorial Disclaimer: This evidence report is presented as a document in support of the accompanying USPSTF recommendation statement. It did not undergo additional peer review after submission to JAMA .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

COMMENTS
One of the fundamental roles of midwives is to provide prenatal care, such as regular checkups and monitoring throughout pregnancy to ensure the health and well-being of the birthing parent and the developing baby. These checkups include physical exams, ultrasound scans and blood tests to track the progress of the pregnancy.
Prenatal care: 1st trimester visits. Pregnancy and prenatal care go hand in hand. During the first trimester, prenatal care includes blood tests, a physical exam, conversations about lifestyle and more. By Mayo Clinic Staff. Prenatal care is an important part of a healthy pregnancy. Whether you choose a family physician, obstetrician, midwife ...
For people with uncomplicated pregnancies, prenatal appointments generally happen every four weeks until approximately week 36 of pregnancy. The next visit is usually around week 38, and then once per week until birth. However, every pregnancy is different, and different health care providers stick to different schedules.
Overdue Pregnancy Visits . At 40 or 41 weeks of pregnancy, you may begin to see your midwife or doctor every few days. Here is what these visits may look like: Check your blood pressure; Listen for baby's heartbeat; Measure your fundal height to check baby's growth; Palpate to check baby's position (vertex, breech, posterior, etc.)
The programme includes home visits from a family nurse while you're pregnant, and after your baby's born. These visits help: to have a healthy pregnancy. you and your baby grow and develop together. you to be the best parent you can be. Your health visitor will take over from your family nurse when your baby is two until they go to school.
Typical prenatal appointment schedule. The number of visits you'll have in a typical pregnancy usually total about 10 to 15, depending on when you find out you're expecting and the timing of your first checkup. In most complication-free pregnancies, you can expect to have a prenatal appointment with the following frequency: Weeks 4 to 28 ...
Midwives are healthcare providers who deal with pregnancy, childbirth, newborn care and postpartum health. Some midwives provide routine reproductive care like pelvic exams, Pap tests, or counseling on birth control. Midwives tend to be more holistic and supportive of natural approaches to pregnancy and birth. People often choose a midwife when ...
The antenatal care you get throughout your pregnancy depends on: your health and any risks you or your baby may have. your stage of pregnancy. any problems you may be experiencing. There will be a number of checks, scans, tests and discussions, such as: when the baby is due, what trimester you are in and what this means for you and your baby.
A certified nurse-midwife (CNM) and certified professional midwife (CPM) are trained to provide pregnancy and postpartum care. Midwives can be a good option for healthy women at low risk for problems during pregnancy, labor, or delivery. A CNM is educated in both nursing and midwifery. Most CNMs practice in hospitals and birth centers.
Background. Approximately 303,000 women and adolescent girls died from pregnancy and childbirth-related complications in 2015.1 That same year, 2.6 million babies were stillborn. Almost all of the maternal deaths (99%) and child deaths (98%) occurred in low- and middle-income countries.
This microsite is coordinated by the Office of Disease Prevention and Health Promotion, Office of the Assistant Secretary for Health, Office of the Secretary, U.S. Department of Health and Human Services. Last updated: May 11, 2024. U.S. Department of Health and Human ServicesOASH - Office of Disease Prevention and Health PromotionMyHealthfinder.
Introduction. Adverse birth outcomes, such as preterm birth, low birth weight (LBW), and small for gestational age (SGA), can have a long-term impact on child development and health [1-6].Adverse birth outcomes are a known risk factor for maternal mental health and child maltreatment [7-9].In Japan, like other developed countries [10,11], the proportion of preterm birth (5.8%) and LBW ...
Years later, with my daughter's birth in hindsight, I realize now, those were not good enough reasons for me for choosing my birth team. What I had been wanting during that pregnancy was to find a team that would allow me to feel safe, supported, heard, special, honored, and not judged. All things I did not have during my first pregnancy and birth.
Objective: The aim of the present study is to gain a deeper understanding of women's experiences of midwifery care in connection with home visits during the early postnatal period. Research design/setting: A qualitative approach was chosen for data collection, and the data presented are based on six focus group interviews (n: 24). The women were both primiparous and multiparous, aged 22-37 ...
A midwife can be based in hospital, in a community setting like a midwife-led unit or a doctor's surgery, or they can visit you at home (MIDIRS, 2017). Community midwives will monitor you during your pregnancy, give advice and arrange access to any medical care you need. For the birth, a hospital midwife will support and guide you and help ...
A midwife is a health professional who looks after pregnant mothers and birthing people and their babies during pregnancy, labour and after the birth. If you have a low-risk pregnancy, midwives will do most of your antenatal care. You may see your midwife or midwifery team at home, at your GP surgery, health or family centre or in hospital. GP
Antenatal care is the care you get from health professionals during your pregnancy. It's sometimes called pregnancy care or maternity care. You'll be offered appointments with a midwife, or sometimes a doctor who specialises in pregnancy and birth (an obstetrician). You should start your antenatal care as soon as possible once you know you're ...
Your antenatal appointments. You'll have a number of antenatal appointments during your pregnancy, and you'll see a midwife or sometimes an obstetrician (doctor specialising in pregnancy). They'll check the health of you and your baby, give you useful information and answer any questions. Pregnant employees have the right to paid time off for ...
Potential topics include nutrition, common ailments during pregnancy, and available tests. The midwife will also help her client prepare for childbirth by discussing the options at her disposal, among other things. In addition, the midwifery team will offer prenatal classes. During prenatal visits, the midwife checks that the pregnancy is going ...
In Australia, your choices for pregnancy care are linked to where you plan to give birth. A wide range of options is available. During your pregnancy you can get care from a midwife, GP or obstetrician — or a combination. You can give birth in a public or private hospital, a birth centre or at home, depending on whether your pregnancy is high ...
A children's doctor (paediatrician), midwife or newborn (neonatal) nurse will check your baby is well and will offer him or her a newborn physical examination within 72 hours of birth. In the early days, the midwife will check your baby for signs of: jaundice. infection of the umbilical cord or eyes. thrush in the mouth.
The $34 million initiative offers support services and referrals to new and expectant parents by having trained health workers - such as a nurses, doulas, lactation consultants, or community health workers - make in-person or virtual visits to the home of a new or expecting parents, identifying maternal health needs during pregnancy or soon ...
Studies show that women are greatly satisfied with the information and guidance provided by the midwife during the home visit (7, 8). ... help establish a perception of consistency and continuity by maintaining regular contact with the woman throughout the pregnancy until the home visit. The visit may provide an opportunity to accommodate the ...
Background: In an increasingly strained maternity care system with a shortage of midwives and great demands for service, pregnant women in their early labour are at risk of receiving insufficient support. Women make calls and visit the labour ward on multiple occasions before being admitted. A video call with a labour ward midwife during early labour is an unknown practice but could support ...
I am so grateful to Alana for her amazingly compassionate and thoughtful care. I worked with her during my third pregnancy and birth. From the very beginning Alana was so open to hearing my experience and needs and rather than trying to fit my experience into a preconceived notion, she seemed totally dedicated to listening to and responding to what was happening for me without any judgement.
A midwife is a trained medical professional who provides care for healthy mothers during pregnancy, in delivery and after giving birth. Midwives deliver babies in the home, birth centers and in hospitals. A tribal midwife is a person recognized by an indiginous tribe to practice midwifery for that tribe, Casey's bill says.
A midwife is an expert in normal pregnancy and birth. Midwives are specially trained to care for mothers and babies throughout normal pregnancy, labour and after the birth. They provide care in hospital or at home. Midwives sometimes work both in hospitals and in the community (GP surgeries and home visits) so the same midwife may be able to ...
Community health workers and doulas are uniquely positioned to provide personalized care and serve as bridges between clinicians and patients. Their reach can expand from home visits to telehealth consultations and other wraparound services, such as identifying and supporting barriers to care like transportation, food and housing.
To ascertain and explore the views of women and their partners, giving birth in the Czech Republic, of the level of respectful or disrespectful care provided during pregnancy and early labour. Ethical approval was granted for a descriptive, online anonymous survey of 65 questions, with quantitative and qualitative responses. The Czech Republic.The survey was completed by 8,767 women and 69 ...
Routine measurement of blood pressure during pregnancy has long been a standard of prenatal care. 46 Innovations in screening programs involving changes to standard prenatal visit schedules, virtual visits, and telehealth applications, or the use of home blood pressure measurement, have the potential to influence pregnancy outcomes. Large, well ...