
ANDREW BAZEMORE, MD, MPH, AND MARK HUNTINGTON, MD, PhD
Am Fam Physician. 2009;80(6):583-590
A more recent article on pretravel consultation is available .
Author disclosure: Nothing to disclose.
The increase in travel and travel medicine knowledge over the past 30 years makes pretravel counseling an essential part of comprehensive family medicine. Effective counseling begins with assessment of individual and itinerary-based risks, using a growing body of evidence-based decision-support tools and resources. Counseling recommendations should be tailored to the patient's risk tolerance and experience. An essential component of the pretravel consultation includes reviewing routine and destination-specific immunizations. In addition to implementing behavioral adaptations, travelers can guard against vector-borne disease by using N,N -diethyl- m -toluamide (DEET, 30%), a safe and effective insect repellent. Patients should also receive malarial chemoprophylaxis when traveling to areas of risk. Proper precautions can reduce the risk of food- and waterborne disease. Travelers should take appropriate precautions when traveling to high altitudes. Strategies for minimizing the risk of deep venous thrombosis during air travel include keeping mobile and wearing compression stockings. Accident avoidance and coping strategies for health problems that occur while abroad are also important components of the pretravel consultation.
Travel medicine is often relegated to the purview of infectious diseases. However, its emphasis is prevention—not only of tropical disease, but also of common disease—and it takes into consideration preexisting chronic conditions, behavioral risk factors, nonbiologic health threats, and the individual traveler's risk tolerance. Multidisciplinary in its scope, travel medicine lends itself well to the family physician's broad training, counseling skills, and focus on prevention and continuity. In the United States, surveys of travel physicians show that 38 percent trained in family medicine or general internal medicine; in Canada, 54 percent trained in family medicine. 1

Risk Stratification and Shared Decision Making
A successful pretravel consultation involves risk identification, stratification, and counseling to make the patient aware of and comfortable with travel risks ( Table 1 ). 1 – 11 Physicians should remind travelers that risk is present at home and abroad, and that the risk of exotic or unusual conditions is low for many destinations and can be minimized for others ( Figure 1 ). 12 Effective pretravel consultation begins with a process of assessing and conveying the epidemiologic likelihood of disease and injury connected with the trip ( Table 2 ) , which depends on traveler- and itinerary-specific factors. A two-week trip through Western Europe has a far different risk profile than a two-year Peace Corps tour in West Africa. 2 , 12 Point-of-care references are essential for primary care physicians to be able to provide the most appropriate advice for a specific destination ( Table 3 ). Similarly, traveler factors such as age, chronic disease, immunocompromise, and pregnancy potentially influence the epidemiologic risk associated with specific destinations, and consultation with a travel medicine subspecialist may be indicated for optimal care of patients at higher risk. Figure 2 presents an algorithm for identifying travelers who may require specialized advice.
Travel epidemiology should be balanced with shared decision making, which requires assessing and incorporating the patient's health belief model and level of risk tolerance into decisions about disease prophylaxis. Furthermore, such assessment helps to determine the direction of the physician's limited counseling time; for example, additional time may be needed for counseling on topics such as local risk of sexually transmitted disease exposure, food safety, and crime avoidance.
Topics for Discussion
Morbidity and mortality.
Reported morbidity among travelers varies widely, but as many as 75 percent of short-term travelers to developing nations report experiencing some health impairment. 12 Minor ailments are quite prevalent, with traveler's diarrhea by far the most common. Patients should be counseled that average mortality rates for travelers to developing nations may actually be lower than those of nontravelers 12 , 13 ; that trauma, not infectious disease, is the leading cause of death in younger travelers; and that cardiovascular disease is the greatest threat in older travelers. 7 , 13 Among infectious sources, the most common cause of death is falciparum malaria, which is easily prevented with appropriate precautions and awareness.
IMMUNIZATIONS
Immunization is the most common reason cited by patients for seeking pretravel medical consultations. Appropriate immunization greatly enhances a traveler's likelihood of remaining healthy ( Table 4 ). In addition to ensuring that all routine immunizations are up-to-date, special immunizations may be advisable based on individual risk tolerance, geographic destination, behavioral or occupational risk factors, seasonal disease variations, and current outbreaks. Information and current recommendations for travel vaccination are available from the Centers for Disease Control and Prevention ( http://www.cdc.gov/travel ).
Use of decision support is essential to safe and appropriate vaccine administration in travelers. Some vaccines may be contraindicated for certain travelers. Depending on the destination, immunizations may be advisable that are not available in the typical family physician's office or that require special certification, such as yellow fever vaccine. To meet the pretravel vaccine needs of their patients, physicians should locate and offer a list of local clinics that are certified to deliver these vaccines; consider which suppliers can deliver these vaccines quickly; and contemplate the cost implications for the office and patient, who may choose to return for a nurse visit to receive the vaccine.
INSECT AVOIDANCE
Vector-borne disease is a significant source of traveler morbidity. Although reasonably effective malaria prophylaxis regimens are available, other diseases can be prevented only by insect avoidance. N,N -diethyl- m -toluamide (DEET, 30%) is the most effective and safest insect repellent available, and should be recommended to all travelers. 1 Other agents, such as picaridin, have also been shown to offer some protection. 14
Proper clothing, insecticide-impregnated bednets in high-risk areas, and behavioral measures decrease the risk of acquiring vector-borne illness and should be encouraged. Insect precautions, awareness of seasonal importance in the prevalence of insect vectors and disease, antimalarial chemoprophylaxis, and vaccination against vector-borne illnesses (where available) should be advised to persons traveling to high-risk areas. 1 – 6 This information is best rendered with the aid of decision-support tools that offer maps of vector and disease exposure. However, evidence for the effect of such counseling on adherence and ultimate disease risk is variable. 3 , 4
FOOD AND WATER PRECAUTIONS
A leading cause of morbidity among travelers is gastrointestinal disturbance from food- and waterborne diseases. Traveler's diarrhea is the most common disease among travelers, increasing in frequency when food and water precautions are not strictly practiced. Fluoroquinolones are the first choice for treatment, although Campylobacter resistance is developing in some regions. Dosages and agents differ for children and pregnant women. Because recommendations to lower the risk of these diseases are quite restrictive and the evidence supporting the effectiveness of counseling is lacking, shared decision making about acceptable risk is critical. More adventuresome travelers may be willing to risk disease to fully participate in the local cultural experiences, whereas a business traveler may wish to be as cautious as possible.
ENVIRONMENTAL PRECAUTIONS
Water ingestion is not the only swimming-related risk; immersion also presents risks. Various diseases, such as schistosomiasis and Naegleria infection, may be acquired by swimming in unchlorinated freshwater. Although salt-water is generally safer than tropical freshwater, persons swimming in saltwater should consider currents, pollutants, and hazardous marine life. Decision-support tools can help physicians identify regions where travelers should carefully consider swimming.
Temperature extremes and sun exposure are other environmental hazards encountered in traveling. Whether by hypothermia and frostbite, or heat exhaustion and dehydration, being unprepared for the local climate can risk the health of a traveler. Local weather is influenced by a variety of factors, not merely distance from the equator, and many travelers arrive at their destination ill-prepared for the climate encountered. Ensuring that travelers are aware of what weather to expect at their destination can keep them healthy, as can reminders of the importance of hydration during acclimation to tropical heat. The risk of sunburn and its sequelae increases with travel to higher altitudes and lower latitudes. Counseling travelers to wear sun-protective clothing and use sunscreen with a sun protection factor of at least 30 is sage advice.
It is important to acquaint travelers to altitudes above 8,000 ft with the symptoms and risks of altitude-related illnesses, as well as measures to avoid these illnesses. Assessing risk tolerance and discussing plans for acclimation, particularly among adventure travelers drawn to high altitude, may help these travelers avoid potential hazards. Some preexisting medical conditions, particularly cardiopulmonary and cerebral diseases, may exacerbate or be exacerbated by altitude-related illness. Determining the altitude of the patient's destination and counseling about ways to minimize risks above 8,000 ft (e.g., acetazolamide [formerly Diamox] prophylaxis, appropriate time for acclimation) should be part of the pretravel visit for anyone traveling to mountainous regions.
Comprehensive pretravel consultation includes assessment of fitness for air travel and advice on avoiding associated hazards, particularly for pregnant women; scuba divers; and persons with history of hemoglobinopathies, hypercoagulability, recent surgery, or cardiopulmonary disease. Key areas to cover include avoidance of deep venous thrombosis with prolonged flights, infectious disease and cabin air quality, and minimizing jet lag.
OTHER CONSIDERATIONS
The primary cause of death in travelers is accidents, usually motor vehicle crashes and falls. Physicians should remind travelers that safety regulations and practices are not as prevalent in many nations as they are in the United States, and should advise them to become familiar with the hazards associated with local transportation and activities. Staying abreast of warnings from the U.S. State Department ( http://www.travel.state.gov ) before and even during travel may be important in high-risk destinations. Travelers also should be counseled about the high cost of medical evacuation in the event of emergency, and they should be directed to sources of evacuation insurance as indicated by the risk assessment and tolerance.
Travelers may be at risk of exposure to sexually transmitted diseases. They should be reminded of the hazards of casual sex and of the increased prevalence of human immunodeficiency virus and hepatitis B in many developing nations, and that proper condom use can decrease, but not eliminate, this risk.
Travelers should be reminded that the risk of crime abroad varies based on destination and traveler behavior. In addition to familiarity with local patterns and prevalence of crime, safety-enhancing behaviors such as minimizing the appearance of wealth, traveling in pairs or groups, conducting business with established vendors, and locking hotel rooms can decrease risk. Awareness of the local customs, attitudes, laws, and geopolitical conditions can also reduce risk.
The resources listed in Table 3 , as well as guidebooks and online travel review sites, are important sources of information to inform physicians and travelers about events and customs that affect risk. Travelers may register their itineraries and travel dates with the U.S. State Department, and they may wish to carry embassy or consulate and local health care resource information with them in the event of unforeseen emergencies, such as natural disasters or political disturbances.
Hill DR, et al. The practice of travel medicine: guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2006;43(12):1499-1539.
Chen LH, Wilson ME, Schlagenhauf P. Prevention of malaria in long-term travelers. JAMA. 2006;296(18):2234-2244.
Lobel HO, et al. Use of malaria prevention measures by North American and European travelers to East Africa. J Travel Med. 2001;8(4):167-172.
Lobel HO, Kozarsky PE. Update on prevention of malaria for travelers. JAMA. 1997;278(21):1767-1771.
Batchelor T, Gherardin T. Prevention of malaria in travellers. Aust Fam Physician. 2007;36(5):316-320.
Chen LH, Wilson ME, Schlagenhauf P. Controversies and misconceptions in malaria chemoprophylaxis for travelers. JAMA. 2007;297(20):2251-2263.
DuPont HL. New insights and directions in travelers' diarrhea. Gastroenterol Clin North Am. 2006;35(2):337-353.
Rao G, Aliwalas MG, Slaymaker E, Brown B. Bismuth revisited: an effective way to prevent travelers' diarrhea. J Travel Med. 2004;11(4):239-241.
Keystone JS. Travel Medicine . 2nd ed. London:Mosby Elsevier; 2008.
Milledge JS. Altitude medicine and physiology including heat and cold: a review. Travel Med Infect Dis. 2006;4(3–4):223-237.
Luks AM, Swenson ER. Medication and dosage considerations in the prophylaxis and treatment of high-altitude illness. Chest. 2008;133(3):744-755.
Steffen R, Amitirigala I, Mutsch M. Health risks among travelers—need for regular updates. J Travel Med. 2008;15(3):145-146.
Freedman DO, et al. Spectrum of disease and relation to place of exposure among ill returned travelers [published correction appears in N Engl J Med . 2006;355(9):967]. N Engl J Med. 2006;354(2):119-130.
Frances SP, Waterson DG, Beebe NW, Cooper RD. Field evaluation of commercial repellent formulations against mosquitoes (Diptera: Culicidae) in Northern Territory, Australia. J Am Mosq Control Assoc. 2005;21(4):480-482.
Continue Reading
More in afp, more in pubmed.
Copyright © 2009 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
MassGeneral Home
- Conditions & Treatments
- Centers & Services
- Research & Clinical Trials
- Education & Training
- Career Opportunities
- About Mass General
Global TravEpiNet
A national consortium of travel health providers.
Please let us know if you have suggestions or comments by email .
This tool is provided by the Massachusetts General Hospital and supported by funding from grant U01CK000175 of the U.S. Centers for Disease Control and Prevention (CDC). This software is a reference tool intended to be used as an adjunct to the management of clinical care. The healthcare professional must review and verify information obtained by using the software to ensure that the information is accurate, complete and correctly associated with, and relevant to, individual cases. The tool should not be used to replace, overrule, or substitute the healthcare professional’s medical judgment, diagnosis, or treatment decisions. By using this tool, you agree that the Massachusetts General Hospital and the tool’s developers and supporters are not liable for any adverse outcomes, including those relating to your patient’s travel.

- Billing & Insurance
- Medical Records
- Accessibility
- Your Rights & Concerns
- Privacy & Security
- Social Media Policy
- 55 Fruit Street, Boston, MA 02114
- Maps & Directions
- 617-726-2000
- TDD: 617-724-8800
- Research article
- Open access
- Published: 02 May 2012
A cross-sectional study of pre-travel health-seeking practices among travelers departing Sydney and Bangkok airports
- Anita E Heywood 1 ,
- Rochelle E Watkins 2 ,
- Sopon Iamsirithaworn 3 ,
- Kessarawan Nilvarangkul 4 &
- C Raina MacIntyre 1 , 5
BMC Public Health volume 12 , Article number: 321 ( 2012 ) Cite this article
6998 Accesses
55 Citations
1 Altmetric
Metrics details
Pre-travel health assessments aim to promote risk reduction through preventive measures and safe behavior, including ensuring travelers are up-to-date with their immunizations. However, studies assessing pre-travel health-seeking practices from a variety of medical and non-medical sources and vaccine uptake prior to travel to both developing and developed countries within the Asia-Pacific region are scarce.
Cross-sectional surveys were conducted between July and December 2007 to assess pre-travel health seeking practices, including advice from health professionals, health information from other sources and vaccine uptake, in a sample of travelers departing Sydney and Bangkok airports. A two-stage cluster sampling technique was used to ensure representativeness of travelers and travel destinations. Pre-travel health seeking practices were assessed using a self-administered questionnaire distributed at the check-in queues of departing flights. Logistic regression models were used to identify significant factors associated with seeking pre-travel health advice from a health professional, reported separately for Australian residents, residents of other Western countries and residents of countries in Asia.
A total of 843 surveys were included in the final sample (Sydney 729, response rate 56%; Bangkok 114, response rate 60%). Overall, pre-travel health information from any source was sought by 415 (49%) respondents with 298 (35%) seeking pre-travel advice from a health professional, the majority through general practice. Receipt of a pre-travel vaccine was reported by 100 (12%) respondents. Significant factors associated with seeking pre-travel health advice from a health professional differed by region of residence. Asian travelers were less likely to report seeking pre-travel health advice and uptake of pre-travel vaccines than Australian or other Western travelers. Migrant Australians were less likely to report seeking pre-travel health advice than Australian-born travelers.
Conclusions
This study highlights differences in health-seeking practices including the uptake of pre-travel health advice by region of residence and country of birth. There is a public health need to identify strategies targeting these travel groups. This includes the promotion of affordable and accessible travel clinics in low resource countries as traveler numbers increase and travel health promotion targeting migrant groups in high resource countries. General practitioners should play a central role. Determining the most appropriate strategies for increasing pre-travel health preparation, particularly for vaccine preventable diseases in travelers is the next stage in advancing travel medicine research.
Peer Review reports
International travel has increased dramatically over the last few decades, in magnitude, speed and geographical reach with 940 million arrivals reported in 2010 [ 1 ]. Furthermore, the last decade has seen an increase in travel in the Asia-Pacific region well above the global average, resulting in a 21% share of international arrivals in 2010, up from 16% in 2000 [ 1 ]. Travelers play a significant role in the spread of infectious diseases across international borders, through their travel patterns and behaviors. Travel maybe the only risk factor for infectious diseases that are well controlled in the travelers’ country of residence, particularly vaccine-preventable diseases such as hepatitis A, typhoid, polio and measles. The role of vaccination among travelers is an essential component of national control of travel-associated infectious diseases. Understanding the behaviors of travelers and their attitudes towards a variety of communicable diseases can inform policy aimed at protecting the individual traveler, their contacts and the communities into which they travel. Behavioral studies of travelers provide insights into risks of both acquiring and importing infectious diseases.
A pre-travel consultation with a health professional can provide the international traveler with the necessary preventive advice on minimizing health risks during travel, including the risk of infectious disease and the opportunity for relevant vaccination and chemoprophylaxis. Travelers who seek pre-travel health advice from a health professional have been found to have better knowledge of infectious disease risk, more accurate risk perceptions and a higher level of intended risk-reducing behaviors [ 2 – 5 ]. Yet studies have shown that many Western travelers do not consult a health professional prior to travel and may not be aware of their need to protect themselves from infectious diseases [ 6 – 10 ]. Studies on the pre-travel health seeking behavior of travelers within the Asia-Pacific are limited; however, recent evidence suggests that the proportion of Asian travelers seeking pre-travel health advice is significantly lower than that of Western travelers [ 10 ]. Our study aimed to identify health-seeking practices among travelers and assess the proportion of travelers who sought pre-travel health advice and the uptake of pre-travel vaccines in a representative sample of travelers departing Sydney and Bangkok airports. The study also aimed to identify significant factors associated with pre-travel health seeking from a health professional.
Cross-sectional surveys of travelers were conducted prior to their departure from international airports in Sydney, Australia for destinations in Asia between July and September 2007 and Bangkok, Thailand bound for Australia between October and December 2007. Asian destinations were defined according to the United Nations World Macro classification of regions and included countries in Eastern Asia and South-Eastern Asia [ 11 ]. Asian destinations were selected due to their close proximity to Australia and the high proportion of air traffic flow between these regions. The methods used in this study have been published previously [ 12 ]. Briefly, a two-stage cluster sampling technique was developed at each study site to randomly sample travelers. At Sydney airport, in the first stage, sample sizes for each destination were calculated based on the proportion of passengers departing for the selected destinations, derived from aviation statistics for the previous calendar year [ 13 ]. Total sample size was sufficient to estimate a population proportion of 50% with ±3.5% precision at the 5% confidence level. A representative sample of direct flights on all available days and times of departure for each pre-approved airline carrier for each of the selected destinations were included in an interviewing timetable. Airline carriers representing both Australian and non-Australian carriers were selected based on their total share of passengers with 11 of the 13 approached airlines providing approval.
The second stage of the cluster sampling method involved the distribution of questionnaires to every fifth passenger joining check-in queues of selected flights. Bilingual interviewers attended check-in counters 3 h before scheduled departure until 1 h before departure. A similar method was employed at the Bangkok airport, with selected flights proportionate to the number of traveler arrivals at Australian airports from Thailand and representative of Thai, Australian, and other carriers. Approximately 175 flights were sampled between July and September 2007 at the Sydney site comprising 2.7% of the flights to Asia during this period, and 13 flights between October and December 2007 at the Bangkok site, comprising 2.4% of the flights to Australia from Thailand during this period.
Eligible respondents were both visitors and residents aged 18 years or older, departing on the day of interview, excluding passengers in transit. The questionnaire was developed in simplified English and piloted at Sydney Airport. The revised questionnaire was translated into Chinese, Vietnamese and Thai with back-translation employed to ensure consistent interpretation of questions. The self-administered questionnaire included questions on socio-demographic characteristics and travel characteristics of their current trip. Respondents were provided with a list of health professionals and non-medical sources of travel health information. Pre-travel health seeking practices refer to both the seeking of health advice from a health professional as well as health information from other sources. Pre-travel health advice refers only to information obtained from a health professional. A list of common routine and travel vaccines were provided to respondents, who were asked to record vaccines received for the specific purpose of their current trip.
The sample obtained at the Sydney study site was weighted by flight destination to reflect the proportion of passenger departures from aviation statistics [ 13 ], due to over sampling of some destinations, thereby providing a representative sample of travelers departing Australia for destinations in Asia and avoiding sampling bias. No weighting was applied to the Bangkok sample. Data were analyzed using SPSS version 18 (SPSS Inc., Chicago, Illinois) and missing data were excluded from analysis. Statistical significance in bivariate analysis was assessed using the chi-squared test and we considered a p-value of <0.05 to be significant. Logistic regression analysis was undertaken to determine associations between socio-demographic and travel characteristics and the reported uptake of pre-travel health advice from a health professional. All variables which may plausibly predict uptake of pre-travel health advice with a significance of <0.25 on bivariate analysis were considered for inclusion in the logistic regression analysis [ 14 ], and final models were assessed for adequacy of sample sizes [ 15 ]. Variables considered plausible include: demographics; age, gender, marital status, education, employment, resident of birth country, and trip characteristics; length of stay, reason for travel, travel companions, destination sub-region, number of destination countries, within country air and train travel and attendance at crowded events. During multivariate logistic regression model fitting, significant independent variables associated with seeking pre-travel health advice differed for Australian travelers, other Western travelers and Asian travelers and separate models were developed. Travelers from other regions were too few to model. The proportion reporting uptake of pre-travel vaccination was insufficient to determine a valid logistic regression model and is reported as univariate analysis. The research was approved by the Human Research Ethics Committees of the University of Sydney, Australia (12–2006/9727), the University of New South Wales, Australia (08254), the Ministry of Public Health, Thailand (3–2399-00051–49-4) and the relevant airport authorities.
Study sample and travel profile
A total of 843 surveys, including 729 weighted surveys of travelers departing Sydney to destinations in Asia (response rate; 56%), and 114 surveys of travelers departing Bangkok (response rate 60.0%) were included in the final sample. The number of respondents by flight destination has been reported previously [ 12 ]. Of the Sydney sample, 329/729 (45.1%) were residents of Australia, 170 (23.3%) were residents of other Western countries including New Zealand and countries in North America and Europe and 211 (28.9%) were residents of countries in Asia. Of the Bangkok sample, 55/114 (48.2%) were residents of Australia, 29 (25.4%) were residents of other Western countries and 14 (12.3%) were residents of countries in Asia. The demographic and travel characteristics, including travel activities by region of residence are shown in Table 1 .
Pre-travel health-seeking
At least one visit to a health professional in the past year for any reason was reported by 532/843 (63.1%) respondents, including 320 (38.0%) reporting two or more visits. Overall, 415 (49.2%) respondents sought some form of travel health information prior to their present trip. Pre-travel health advice was sought from a health professional by 298 (35.3%) respondents with 237 (79.5%) of these respondents seeking advice from their general practitioner. A travel specialist or travel clinic was attended by 35 (4.2%) respondents prior to travel or 11.7% of those who sought professional pre-travel health advice. Non-medical sources of travel health information were reported by 290 (34.4%) respondents. The Internet was reported as a source of pre-travel health information by 162 (19.2%) respondents, with 71/162 (43.8%) including a government travel advisory website in their web searches. Travel agents were reported as a source of travel health information by 114/843 (13.5%) respondents. Differences in pre-travel health seeking by region of residency are shown in Table 2 . Seeking any pre-travel health information differed between study sites and was reported by 346 (47.5%) respondents departing Sydney and 69 (60.5%) respondents departing Bangkok (p = 0.009). No association was found between study sites in the proportions seeking professional health advice overall (p = 0.1), from a general practitioner (p = 0.3), travel specialist (p = 0.1) or a non-medical source (p = 0.1). Factors independently associated with seeking pre-travel health advice from a health professional on multivariate analysis differed by region of residence and are reported in Table 3 .
Pre-travel vaccination
Pre-travel vaccination rates were low across both study sites with 100 (11.9%) respondents reporting receipt of one or more vaccines specifically for this trip, including 73/298 (24.5%) of those reporting a pre-travel heath visit. Pre-travel vaccination differed by region of residence (Table 2 ). Travelers who reported seeking advice from a travel medicine specialist were more likely to report a pre-travel vaccine (21/36, 58.3%) compared to travelers reporting a pre-travel visit to a general practitioner (48/237, 20.3%, p < 0.001). The most commonly reported vaccines were hepatitis A vaccine (58, 6.9%), hepatitis B vaccine (46, 5.5%), typhoid vaccine (30, 3.6%), tetanus vaccine (28, 3.3%) and influenza vaccine (24, 2.8%). Other vaccines were reported by between 0.4% and 1.4% of respondents. Of those reporting a pre-travel vaccination, 40/102 (39.2%) recalled only one vaccine, predominantly influenza vaccine (16/40, 40.0%) or hepatitis A vaccine (10/40, 25.0%). Two pre-travel vaccines were recalled by 21/102 (20.6%) respondents and 41 (40.2%) reported three or more vaccines. Respondents departing Bangkok were more likely to report pre-travel vaccine uptake (21/114, 18.4%) than those departing Sydney (81/729, 11.1%, p = 0.03).
Seeking health-related information prior to travel may prepare travelers for health risks at their destination and studies have shown an association between receiving advice and accurate risk perception and undertaking preventative behaviors [ 4 , 5 , 16 ]. Considerable variation exists in the published literature on the proportion of surveyed travelers seeking pre-travel health advice, ranging from as low as 32% of departing travelers from Australasian airports [ 10 ] to 85-94% of those traveling to sub-Saharan Africa and Central and South America [ 7 , 17 – 19 ]. In our study, less than half of all respondents (49%) reported seeking health information from any source prior to travel, similar to a number of published studies [ 6 – 8 , 10 , 20 ]. We found travel to tropical regions, such as countries in South East Asia associated with higher rates of health seeking compared to travel to more temperate regions such as countries in North East Asia. The risk of infectious disease is not limited to low resource countries and travelers to Australia may still be at risk of infectious diseases, particularly in the tropical regions [ 21 ]. Visitors to Australia should be aware of the risks of travel at any destination.
While numerous health resources are available to travelers, it is recommended that travelers seek advice from a health professional prior to international travel [ 3 , 4 ]. In our survey, approximately two thirds of respondents traveled without professional medical advice. General practice was the main source of professional pre-travel health advice, reflecting results from other airport surveys of travelers [ 5 , 6 , 8 , 10 ] and providing further weight to the importance of general practice in preventative travel medicine. Despite differences in health systems, the majority of travelers internationally seek advice from their general practitioner [ 8 , 20 , 22 ]. This is particularly so in Australia, where general practitioners play a central role in the delivery of primary and preventative health care [ 23 , 24 ]. While some studies report increased knowledge and accurate risk perception in travelers who consult travel medicine specialists [ 4 , 5 ], only 4.2% of travelers in our study (ranging from 2.2% to 8.5% depending on region of residence) attended a travel clinic prior to travel. The role of the general practitioner is under-valued in travel medicine research and few studies of travelers who consult general practice are available. With this key role in the health of travelers, general practice is challenged with the provision of accurate and tailored advice during consultations that are limited by time and resources.
Pre-travel health seeking is influenced by many factors including traveler demographic characteristics, reasons for travel and previous travel experience. Few studies investigate differences in health-seeking norms by nationality. Our study showed that uptake of pre-travel health advice from a health professional differed considerably by region of residence. Health seeking is likely to differ by nationality due to differences in health seeking practices, country-specific healthcare systems including national vaccination programs and travel health facilities as well as promotional activities undertaken by health departments and private travel medicine groups. While it is likely that pre-travel health practices and vaccine uptake differs by destination and prior travel experience, pre-travel health advice may still be warranted and provides the opportunity to vaccinate if required. In Australia, a number of recent cases of measles have been imported from developed countries, and high risk Australian travelers to Europe and North America during the northern hemisphere winter are advised to receive the influenza vaccine [ 25 ]. Furthermore, many travelers travel to multiple destinations and may not be aware of the individual risks. Alongside other studies, our study confirms the low uptake of pre-travel health advice and vaccination among Asian travelers. Another airport survey conducted in the region found only 26% of Asian travelers reported seeking pre-travel health advice compared to 63% of Western travelers [ 10 ], while a separate study reported 23.9% of South Korean travelers to India [ 26 ], a high risk destination for many infectious diseases [ 27 ], sought pre-travel health advice. Expansion of the Asian travel market has been forecast due to increasing wealth within the region and growth in intra-regional tourist arrivals [ 28 ]. As more people within the Asia-Pacific region can afford to travel, it is important to increase the uptake of pre-travel advice, particularly from medical sources. The limited number of specialist travel clinics in low resource countries may be a current barrier to uptake of pre-travel health advice and differences in health seeking behaviors and associated factors by region of residence may limit the generalisability of traveler studies, highlighting the growing need to better understand travelers from emerging travel markets.
Travel to visit friends and relatives (VFR) is an established risk factor for acquiring infectious diseases during travel [ 29 ] and for poor uptake of pre-travel health advice [ 8 , 30 ]. We did not identify a significant association between VFR travel and uptake of professional pre-travel health advice. However, we found migrant Australian travelers to be half as likely to seek pre-travel advice from a health professional and more likely to be traveling to visit friends and relatives than Australian-born travelers. Recent evidence also suggests that ethnicity, in addition to travel to visit friends and relatives, is an important indicator of infectious disease risk during travel [ 30 ]. Australian migrants who travel may be at a greater risk of infectious diseases than Australian-born travelers due to their lower uptake of pre-travel health advice, regardless of reason for travel.
We acknowledge some limitations to our study. A brief self-administered questionnaire design, although appropriate to maximize the response rate in high volume airport surveys, limits the amount of detail obtainable and is also subject to recall bias. Additional factors which have been found to be associated with uptake of pre-travel health advice, such as previous travel experience and economic barriers were not obtained. Due to strict security measures at Sydney Airport, we were not able to gain access beyond customs and conducted our interviews in the departures check-in area. This resulted in a lower response rate than those reported by other airport surveys conducted in the departure lounges [ 26 , 31 , 32 ] in which a response rates have been reported. However, our method allowed for the recruitment of passengers from a variety of carriers and flight times including weekends and evenings during the study period, providing a representative cross-section of departing passengers. We utilized a number of techniques to ensure a representative sample of travelers including a multistage sampling method of flight selection and random participant recruitment in which all passengers joining selected check-in queues had an equal probability of selection excluding those few who exceeded the recommended check-in time before departure. The use of simplified English and the provision of additional language versions of the questionnaire by bi-lingual interviewers aimed to reduce language barriers and subsequent selection biases of visitors to Australia from Asia.
A low proportion of participants in this study reported receipt of pre-travel vaccines (12%) with lower rates of pre-travel vaccination reported by Asian travelers compared to Western travelers. Wilder-Smith et al. also reported low uptake of pre-travel vaccines among Asian travelers, with 5% of Asian resident respondents reporting any pre-travel vaccination and low rates of self-reported prior vaccination against common vaccine-preventable diseases [ 10 ]. The findings of this airport study were similar to other traveler surveys in that the most commonly reported vaccines received prior to travel were hepatitis A, hepatitis B, tetanus and typhoid [ 2 , 8 , 10 , 33 ]. Influenza vaccine was reported by <3% of participants, a vaccine not often reported in other traveler surveys. It is likely that awareness of influenza as a travel-associated disease has increased for both providers and travelers with a post-pandemic survey of travel clinic attendees reported 13% uptake of seasonal influenza vaccine [ 34 ]. The proportion reporting a pre-travel vaccine after pre-travel attendance at a specialist travel medicine clinic was almost three times that reported at a general practice visit. Sample size limitations precluded a detailed analysis of factors associated with individual vaccine choices. However, the demographic and travel characteristics significantly associated with travel vaccination differed by residency group. A limitation to this study is that we did not collect data on prior vaccine uptake and are unable to determine the proportion of travelers who did not receive vaccines prior to this trip due to prior disease or vaccine-induced immunity. This airport study, like much research assessing vaccine uptake, relies on the self-reported history of previous vaccination and is subject to recall bias. As the time since vaccination is likely to influence recall, pre-travel vaccines may not be as vulnerable to recall bias as those vaccines received routinely, particularly childhood vaccines. Errors introduced by self-reported history include the misclassification of the vaccine received, particularly hepatitis A and B vaccine [ 35 ] and underestimation of the number of vaccines received. Other surveys have found that respondents report vaccines for non-vaccine preventable diseases such as hepatitis C and malaria, indicating a poor knowledge of their vaccination history [ 36 ] and other studies have shown wide differences between perceived vaccination status and vaccination certificates or blood antibody levels in travelers and other population groups [ 7 , 37 – 39 ]. Without serological testing it is difficult to ascertain if those who visited a medical professional prior to travel were up-to-date with their vaccinations, if they were vaccinated but could not recall the vaccines received or if their visits were a missed opportunity to vaccinate. Difficulties in assessing vaccination history for travel vaccines would be alleviated by the carriage of a vaccination record card for all vaccines received by travelers along with their passport and other travel documents, such as the requirement for entry and exit from yellow fever endemic regions.
Lack of time has been reported as a reason for not seeking pre-travel advice and vaccinations in other studies [ 6 – 8 ]. Other studies have reported that approximately one third of travelers seek advice for their trip within 2 weeks of departure [ 8 , 23 , 33 ]. Almost half of travelers departing from airports in Australasia reported planning their trip less than two weeks prior to departure [ 10 ]. This results in lower rates of pre-travel health seeking, particularly from a health professional as well as the reduced uptake of vaccines, incomplete vaccination schedules for vaccines requiring more than one dose and lack of adequate protection at the time of departure. Although the length of time between health seeking and departure was not assessed in this airport survey, 63% of respondents had visited a health professional at least once in the past year, providing an opportunity for health professionals to inquire about possible overseas trips during their consultation and improve the provision of pre-travel health advice, particularly for migrants and those traveling to visit friends and relatives.
The few travelers seeking advice suggests that public health strategies aimed at travelers may be warranted. These would include increasing uptake of pre-travel medical advice, ensuring vaccines, both routine and those recommended for travel, are up to date as well as the promotion of affordable and accessible travel clinics in low resource countries as traveler numbers increase. Limited data from the Asia-Pacific region are available and few studies assess traveler preparedness in residents of low resource countries, despite the strong growth of the international travel market in Asia. There is variability in pre-travel health advice seeking and vaccine uptake by region of residence and in migrant travelers. The role of general practitioners in the provision of pre-travel health advice and traveler health promotion is central and opportunities for improvement exist. Considering the increasing volume of international travel, a greater integration of travel history and travel plans into general practice consultations would identify those who intend to travel but are not aware of the need for a pre-travel health consultation, particularly migrant travelers. Determining the most appropriate strategies for increasing pre-travel health preparation, particularly for vaccine preventable diseases in travelers is the next stage in advancing travel medicine research.
World Tourism Organization (UNWTO). UNWTO Tourism Highlights. 2011, Edition [Available at http://mkt.unwto.org/sites/all/files/docpdf/unwtohighlights11enhr_1.pdf [Accessed 18/10/2011]
Lopez-Velez R, Bayas JM: Spanish travelers to high-risk areas in the Tropics: Airport survey of travel health knowledge, attitudes, and practices in vaccination and malaria prevention. JTravelMed. 2007, 14 (5): 297-305.
Google Scholar
Piyaphanee W, Wattanagoon Y, Silachamroon U, Mansanguan C, Wichianprasat P, Walker E: Knowledge, attitudes, and practices among foreign backpackers toward malaria risk in southeast Asia. JTravelMed. 2009, 16 (2): 101-106.
Provost S, Soto JC: Perception and knowledge about some infectious diseases among travelers from Quebec, Canada. JTravelMed. 2002, 9 (4): 184-189.
Ropers G, van Beest Holle MR, Wichmann O, Kappelmayer L, Stuben U, Schonfeld C, Stark K: Determinants of malaria prophylaxis among German travelers to Kenya, Senegal, and Thailand. JTravelMed. 2008, 15 (3): 162-171.
Hamer DH, Connor BA: Travel health knowledge, attitudes and practices among United States travelers. JTravelMed. 2004, 11 (1): 23-26.
Toovey S, Jamieson A, Holloway M: Travelers' knowledge, attitudes and practices on the prevention of infectious diseases: results from a study at Johannesburg International Airport. JTravelMed. 2004, 11 (1): 16-22.
Van Herck K, Van Damme P, Castelli F, Zuckerman J, Nothdurft H, Dahlgren AL, Gisler S, Steffen R, Gargalianos P, Lopez-Velez R, et al: Knowledge, attitudes and practices in travel-related infectious diseases: the European airport survey. JTravelMed. 2004, 11 (1): 3-8.
Van Herck K, Zuckerman J, Castelli F, Van Damme P, Walker E, Steffen R, Board ETHA: Travelers' knowledge, attitudes, and practices on prevention of infectious diseases: results from a pilot study. JTravelMed. 2003, 10 (2): 75-78.
Wilder-Smith A, Khairullah NS, Song JH, Chen CY, Torresi J: Travel health knowledge, attitudes and practices among Australasian travelers. JTravelMed. 2004, 11 (1): 9-15.
United Nations (UN). World macro regions and components ST/ESA/STAT/SER.R/29. [Available at http://www.un.org/depts/dhl/maplib/worldregions.htm [Accessed 20/04/2007]]
Heywood AE, Watkins RE, Pattanasin S, Iamsirithaworn S, Nilvarangkul K, MacIntyre CR: Self-reported symptoms of infection among travelers departing from Sydney and Bangkok airports. JTravelMed. 2010, 17 (4): 243-249.
Australian Federal Bureau of Infrastructure Transport and Regional Economics (BITRE). International Airline Activity Time Series. [Available at: [Accessed 24/03/2007] http://www.bitre.gov.au ]
Hosmer DW, Lemeshow S: Model-building strategies and methods for logistic regression. Applied logistic regression. Edited by: Hoboken . 2000, John Wiley & Sons, New York, 2
Chapter Google Scholar
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR: A simulation study of the number of events per variable in logistic regression analysis. JClinEpidemiol. 1996, 49 (12): 1373-1379.
CAS Google Scholar
Packham CJ: A survey of notified travel-associated infections: implications for travel health advice. Journal of Public Health Medicine. 1995, 17 (2): 217-222.
CAS PubMed Google Scholar
Laver SM, Wetzels J, Behrens RH: Knowledge of malaria, risk perception, and compliance with prophylaxis and personal and environmental preventive measures in travelers exiting Zimbabwe from Harare and Victoria Falls International airport. JTravelMed. 2001, 8 (6): 298-303.
Lobel HO, Baker MA, Gras FA, Stennies GM, Meerburg P, Hiemstra E, Parise M, Odero M, Waiyaki P: Use of malaria prevention measures by North American and European travelers to East Africa. JTravelMed. 2001, 8 (4): 167-172.
Cabada MM, Maldonado F, Quispe W, Serrano E, Mozo K, Gonzales E, Seas C, Verdonck K, Echevarria JI, Gotuzzo E: Pretravel health advice among international travelers visiting Cuzco, Peru. JTravelMed. 2005, 12 (2): 61-65.
LaRocque RC, Rao SR, Tsibris A, Lawton T, Barry MA, Marano N, Brunette G, Yanni E, Ryan ET: Pre-travel health advice-seeking behavior among US international travelers departing from Boston Logan International Airport. J Travel Med. 2010, 17 (6): 387-391. 10.1111/j.1708-8305.2010.00457.x.
Article PubMed Google Scholar
Kelly-Hope LA, Purdie DM, Kay BH: Risk of mosquito-borne epidemic polyarthritis disease among international visitors to Queensland, Australia. JTravelMed. 2002, 9 (4): 211-213.
Wilder-Smith A, Boudville I, Earnest A, Heng SL, Bock HL: Knowledge, attitude, and practices with regard to adult pertussis vaccine booster in travelers. JTravelMed. 2007, 14 (3): 145-150.
Zwar N, Streeton CL: Pretravel advice and hepatitis A immunization among Australian travelers. JTravelMed. 2007, 14 (1): 31-36.
Leggat PA, Zwar NA, Hudson BJ: Hepatitis B risks and immunisation coverage amongst Australians travelling to Southeast Asia and East Asia. TravelMedInfectDis. 2009, 7 (6): 344-349.
National Health and Medical Research Council: Vaccination for international travel. The Australian Immunisation Handbook. 9th edition. 2008, Australian Government Department of Health and Ageing, Canberra
Yoo YJ, Bae GO, Choi JH, Shin HC, Ga H, Shin SR, Kim MS, Joo KJ, Park CH, Yoon HJ, et al: Korean travelers' knowledge, attitudes and practices regarding the prevention of malaria: Measures taken by travelers departing for India from Incheon International Airport. JTravelMed. 2007, 14 (6): 381-385.
Freedman DO, Weld LH, Kozarsky PE, Fisk T, Robins R, von Sonnenburg F, Keystone JS, Pandey P, Cetron MS, Network GS: Spectrum of disease and relation to place of exposure among ill returned travelers. NEnglJ Med. 2006, 354 (2): 119-130. 10.1056/NEJMoa051331.
Article CAS Google Scholar
World Tourism Organization (UNWTO). UNWTO Tourism highlights. 2008, [Available at: www.unwto.org [Accessed 11/12/2008]]
Angell SY, Cetron MS: Health disparities among travelers visiting friends and relatives abroad. AnnInternMed. 2005, 142 (1): 67-72.
Baggett HC, Graham S, Kozarsky PE, Gallagher N, Blumensaadt S, Bateman J, Edelson PJ, Arguin PM, Steele S, Russell M, et al: Pretravel health preparation among US residents traveling to India to VFRs: importance of ethnicity in defining VFRs. JTravelMed. 2009, 16 (2): 112-118.
Johnson JY, McMullen LM, Hasselback P, Louie M, Saunders LD: Travelers' knowledge of prevention and treatment of travelers' diarrhea. JTravelMed. 2006, 13 (6): 351-355.
Dahlgren AL, Deroo L, Steffen R: Prevention of travel-related infectious diseases: Knowledge, practices and attitudes of Swedish travellers. ScandJInfectDis. 2006, 38 (11): 1074-1080.
Schunk M, Wachinger W, Nothdurft HD: Vaccination status and prophylactic measures of travelers from Germany to subtropical and tropical areas: results of an airport survey. JTravelMed. 2001, 8 (5): 260-262.
Pfeil A, Mutsch M, Hatz C, Szucs TD: A cross-sectional survey to evaluate knowledge, attitudes and practices (KAP) regarding seasonal influenza vaccination among European travellers to resource-limited destinations. BMC Public Health. 2010, 10: 402-10.1186/1471-2458-10-402.
Article PubMed PubMed Central Google Scholar
Zuckerman JN, Hoet B: Hepatitis B immunisation in travellers: poor risk perception and inadequate protection. TravelMedInfectDis. 2008, 6 (5): 315-320.
Hartjes LB, Baumann LC, Henriques JB: Travel health risk perceptions and prevention behaviors of US study abroad students. J Travel Med. 2009, 16 (5): 338-343. 10.1111/j.1708-8305.2009.00322.x.
De Juanes JR, Gil A, San-Martin M, Gonzalez A, Esteban J, de Garcia CA: Seroprevalence of varicella antibodies in healthcare workers and health sciences students. Reliability of self-reported history of varicella. Vaccine. 2005, 23 (12): 1434-1436. 10.1016/j.vaccine.2004.10.003.
Article CAS PubMed Google Scholar
Skull SA, Andrews RM, Byrnes GB, Kelly HA, Nolan TM, Brown GV, Campbell DA: Validity of self-reported influenza and pneumococcal vaccination status among a cohort of hospitalized elderly inpatients. Vaccine. 2007, 25 (25): 4775-4783. 10.1016/j.vaccine.2007.04.015.
Trevisan A, Frasson C, Morandin M, Beggio M, Bruno A, Davanzo E, Di ML, Simioni L, Amato G: Immunity against infectious diseases: predictive value of self-reported history of vaccination and disease. InfectControl HospEpidemiol. 2007, 28 (5): 564-569.
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2458/12/321/prepub
Download references
Acknowledgements
Funding support for this study was provided by the Australian Research Council (ARC) Discovery grant. AH’s doctorate was funded by the National Health and Medical Research Council (NHMRC) Postgraduate Public Health Scholarship and the National Centre for Immunisation Research and Surveillance (NCIRS), Australia.
We wish to thank those who assisted with the questionnaire translation and data collection, the travelers who participated in the study and the airport authorities and individual airlines who allowed us to undertake this study.
Author information
Authors and affiliations.
School of Public Health and Community Medicine, Faculty of Medicine, University of New South Wales, Kensington, NSW, 2052, Australia
Anita E Heywood & C Raina MacIntyre
Telethon Institute of Child Health Research, Centre for Child Health Research, The University of Western Australia, Perth, Australia
Rochelle E Watkins
Bureau of Epidemiology, Department of Disease Control, Ministry of Public Health, Bangkok, Thailand
Sopon Iamsirithaworn
Research and Training Center for Enhancing Quality of Life of Working-Age People, Faculty of Nursing, Khon Kaen University, Khon Kaen, Thailand
Kessarawan Nilvarangkul
National Centre for Immunisation Research and Surveillance of Vaccine Preventable Diseases (NCIRS), The Children’s Hospital at Westmead and Discipline of Paediatrics and Child Health, University of Sydney, New South Wales, Australia
C Raina MacIntyre
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Anita E Heywood .
Additional information
Competing interests.
CRM receives funding from GSK and CSL Biotherapies for investigator-driven research. These payments were not associated with this study. The remaining authors have no competing interests.
Authors’ contributions
CRM and RW conceived and supervised the study. AH organized airport access in Australia, undertook data collection and analysis and drafted the manuscript. SI and KN organized airport access in Thailand and undertook data collection. CRM, RW, SI and KN reviewed the manuscript. Selected results appearing in this manuscript were presented at the Asia-Pacific International Conference on Travel Medicine, Melbourne, Australia, 24–28 February 2008 and the 13th International Congress on Infectious Diseases, Kuala Lumpur, Malaysia, June 19–22, 2008. All authors read and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Heywood, A.E., Watkins, R.E., Iamsirithaworn, S. et al. A cross-sectional study of pre-travel health-seeking practices among travelers departing Sydney and Bangkok airports. BMC Public Health 12 , 321 (2012). https://doi.org/10.1186/1471-2458-12-321
Download citation
Received : 26 October 2011
Accepted : 02 May 2012
Published : 02 May 2012
DOI : https://doi.org/10.1186/1471-2458-12-321
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Influenza Vaccine
- Vaccine Uptake
- Travel Medicine
- Travel Characteristic
- Travel Clinic
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Pre-travel risk assessment for international business travellers during the COVID-19 pandemic
There has been significant disruption to travel caused by COVID-19 due to its international spread and restrictions imposed by countries in their bids to control transmission.
International travel is essential for many types of business, despite the increasing use of telecommunication. Preparation for safe travel must be thorough and include additional considerations compared to the pre-COVID era.
Business travel may be defined as travel for the purpose of working, including corporate travel, field work and attending meetings or conferences. Business travellers may have different health-seeking behaviour due to employment requirements as well as better access to medical care while overseas due to company insurance and medical assistance programmes.
International business travellers have been compared to non-occupational travellers in previous analysis of 23,534 travellers [ 1 ]. More business travellers were men (61% vs 43%), more had less time to departure, over half sought pre-travel consultations largely on the advice of their employer and they had shorter periods of travel. Hotel accommodation was most common (>80%) with more travel to urban areas and they often travelled multiple times a year.
Studies in travel-related illness in business travellers show a similar range of disease to non-occupational travellers, but illness rates and particularly psychological problems, tend to be higher. The rates of medical insurance claims in World Bank travellers were 80% higher in men and 18% higher in women, compared with colleagues who did not travel. Rates were highest for psychological illness, then intestinal disease and respiratory disease [ 2 ].
For a business, defining what is ‘essential travel’ helps to avoid unnecessary and potentially risky travel, whilst ensuring that those who do need to travel get appropriate support before, during and after the trip.
An overseas business travel policy should state what criteria need to be met; either travel is required to fulfil compliance and regulatory obligations and/or without the trip the company would be liable to financial loss, legal implications, damages or penalties and/or the business travel is needed to support critical business activity. For the last criterion it is important that the most senior decision maker, for example executive officers, are deciding criticality, not the individual traveller who may have a conflicting self-interest.
The process for who travels is a dynamic assessment taking into account external factors as well as internal factors. External changes, for example reduced local medical care as a result of a global pandemic, will change the risk profile of a trip making it more dangerous, or the sudden loss of a supply chain due to locally increasing cases can make a trip more important. Internal changes to an individual's medical condition or willingness to travel can mean substituting who goes as well as when they go.
It is in the best interest of employers to ensure the health and wellbeing of their employees working internationally; before, during and after travel, which may be via a provider organisation or on-site occupational health department. Illness may disrupt business activities during or after travel, cause loss of time and productivity and increase medical costs. It is important for an employer to ensure health insurance policies give coverage if their employee should become severely ill abroad with COVID-19.
Quality and infrastructure of local healthcare in the destination country may be negatively impacted by the COVID-19 pandemic, leading to an increased need for medical evacuation if a traveller were to develop a severe COVID-19 infection. Medical evacuation of patients with COVID-19 is complex, with lengthier processes and subsequent cost impact. In some cases air evacuation may be deemed too high a risk, due to severity of illness.
The risk of developing severe or fatal infection with COVID-19 depends largely on the traveller's personal vulnerability should infection occur. The Association of Local Authority Medical Advisors (ALAMA) has developed an evidence-based risk model that can be used to estimate personal vulnerability [ 3 , 4 ]. This tool, known as ‘covid-age’ was first published on 20 th May 2020 and has been periodically updated as new data becomes available.
At our organisation we have developed a detailed health questionnaire to collate relevant medical information from employees prior to business travel.
As return to some essential travel for business commenced following the UK's first lockdown, our questionnaire reviewed Covid-19 infection exposure including confirmed and probable COVID-19 infection, and close contacts with suspected or confirmed cases as well as antibody test results. We also reviewed adverse life events during the pandemic such as hospital admissions, loss of loved ones, relationship breakdowns and significant loss of motivation. This enabled us to have a holistic picture of the employees' experience during lockdown and provide relevant advice, such as current understanding on immunity, and suggestions on mental health support and how it can be accessed.
The medical information requested on the questionnaire enables a review of risk factors known to increase vulnerability and calculation of covid-age. This may also involve review of medical reports from specialists and telephone consultations with the employees to gain further understanding and assessment. Medical factors that may increase risk of sudden incapacity or other need for medical care while travelling are also reviewed. These include cardiovascular risk factors and level of control of chronic conditions such as diabetes, asthma and epilepsy.
There is also the importance of subtle incapacity, involving aspects of lifestyle that can impact the traveller over time. Factors such as alcohol use, smoking and BMI are reviewed, providing opportunity for health promotion advice.
An important part of our risk assessment is a review of factors that may have affected the traveller's psychological wellbeing. Individuals with a pre-existing mental health disorder in the last year have been shown to score significantly higher on the COVID Stress Scales than those without [ 5 ]. Travel may exacerbate or precipitate a variety of psychological disorders. Data on occupational travellers has shown that frequent international travel is associated with increased insurance claims for psychological illness [ 2 ]. Review of previous or existing mental health disorders, coupled with details on adverse life events over the lockdown period such as hospital admissions, loss of loved ones, relationship breakdowns and significant loss of motivation, have enabled identification of employees that may require additional mental health support. This may include referral to an appropriate health professional or Employee Assistance Programme for further assessment and management, as well as provision of information and self-help resources.
Psychological sequalae occurring after traumatic life events are well documented [ 6 ], however, the study of collective traumatic occurrences is limited to physically and mentally extreme situations affecting relatively small sections of populations, for example arctic explorers, soldiers in combat and people experiencing natural disasters. The COVID-19 pandemic has refocussed attention on psychological resilience and initial concerns that a global disaster would have different psychological consequences has not manifested at the time of writing.
However, the pandemic has reinforced previous knowledge that people experience distress after their exposure to an extreme event. In the case of people with good psychosocial resilience and access to social support, their distress may be relatively transient as people call on a set of inner capabilities and supporting relationships to spring back and begin the processes of adaptation.
Employers have a big part to play in ensuring that conditions are optimised for this to occur. Mental disorders occur often, but less commonly than distress, and in some cases they may require intensive and long term continuing interventions and treatment. The Department of Health in the UK [ 7 ] and work done by NATO [ 8 ] differentiate between distress and mental disorders following a disaster. Early identification of a mental health disorder or psychological distress can prevent long-term impacts on the traveller and the business and therefore their wider communities.
As the covid-age tool is based on health data from adults in England, it is likely that it can only reliably be used for risk stratification for workers in the UK. Multiple confounders would come into play to affect the risk of individuals based in other countries. Genetic risk factors have been implemented for increased severity of disease with COVID-19, which are present in about 50% of people in South Asia [ 9 ]. With the number of deaths from COVID-19 being relatively low in Africa, it has been hypothesised that regular exposure to malaria or other infectious diseases could prime the immune system to fight new pathogens like SARS-CoV-2 [ 10 ].
However, particularly when assessing UK-based travellers, the covid-age tool should still give an indication of vulnerability when travelling internationally.
Several studies have identified factors affecting geographical vulnerability of disease with COVID-19. Low levels of national preparedness, scale of testing and population characteristics have been associated with increased national case load and overall mortality [ 11 ]. Low temperature and low humidity have been seen to likely favour the transmission of COVID-19 [ 12 ].
Public health infrastructure in the destination country and their ability to appropriately detect cases and implement isolation and quarantine is an important factor in reduction of COVID-19 transmission. The employer will need to consider quarantine requirements in the destination country and on return. If new restrictions are imposed during time abroad, such as border closures or lockdowns, the employees may risk being stranded abroad for a period of time.
There will be a certain amount of responsibility laid on the employee during travel to ensure they are taking appropriate precautions according to local guidance and company policy.
Airlines or country entry requirements may include negative results from COVID-19 swab tests on arrival or within a timeframe before departure, which needs to be included in timing of business trips. Confirmed in-flight cases have been published [ 13 ], although the risk of in-flight transmission is considered to be very low when stringent hygiene measures are enforced inflight [ 14 ].
As the roll-out of safe and effective vaccines continues, there may be scope for business travel to be less restricted. It is the employer's duty to protect their workers from harm by delivering risk management for all staff, including identification of those with increased vulnerability to COVID-19. This pandemic has further raised the importance of pre-travel risk assessment for business travellers, including consideration of psychological effects; the outcome of which may affect who is chosen to travel and when.
This page requires JavaScript to work properly. Please enable JavaScript in your browser.
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 1 - Improving the Quality of Travel Medicine Through Education & Training
- Section 2 - Perspectives : Travelers' Perception of Risk
The Pretravel Consultation
Cdc yellow book 2024.
Author(s): Lin Hwei Chen, Natasha Hochberg
The pretravel consultation offers a dedicated time to prepare travelers for health concerns that might arise during their trips. During the pretravel consultation, clinicians can conduct a risk assessment for each traveler, communicate risk by sharing information about potential health hazards, and manage risk by various means. Managing risk might include giving immunizations, emphasizing to travelers the importance of taking prescribed malaria prophylaxis and other medications (and highlighting the risks of not taking them correctly), and educating travelers about steps they can take to address and minimize travel-associated risks. The pretravel consultation also serves a public health purpose by helping limit the role international travelers could play in the global spread of infectious diseases.
The Travel Medicine Specialist
Travel medicine specialists have in-depth knowledge of immunizations, risks associated with specific destinations, and the implications of traveling with underlying conditions. Therefore, a comprehensive consultation with a travel medicine expert is indicated for all international travelers and is particularly important for those with a complicated health history, anyone taking special risks (e.g., traveling at high elevation, working in refugee camps), or those with exotic or complicated itineraries. Clinicians aspiring to be travel medicine providers can benefit from the resources provided by the International Society of Travel Medicine (ISTM) and might consider specialty training and certification (see Sec. 1, Ch. 4, Improving the Quality of Travel Medicine Through Education & Training ).
Components of a Pretravel Consultation
Effective pretravel consultations require attention to the traveler’s health background, and incorporate the itinerary, trip duration, travel purpose, and activities, all of which determine health risks ( Table 2-01 ). The pretravel consultation is the best opportunity to educate the traveler about health risks at the destination and how to mitigate them. The typical pretravel consultation does not include a physical examination, and a separate appointment with the same or a different provider might be necessary to assess fitness for travel. Because travel medicine clinics are not available in some communities, primary care physicians should seek guidance from travel medicine specialists to address areas of uncertainty. The Centers for Disease Control and Prevention (CDC) Travelers’ Health website also has materials and an interactive web-tool to guide primary care physicians through a pretravel consultation.
Personalize travel health advice by highlighting likely exposures and reminding the traveler of ubiquitous risks (e.g., injury, foodborne and waterborne infections, vectorborne diseases, respiratory tract infections—including coronavirus disease 2019 [COVID-19]—and bloodborne and sexually transmitted infections). Balancing cautions with an appreciation of the positive aspects of the journey can lead to a more meaningful pretravel consultation. In addition, pay attention to the cost of recommended interventions. Because some travelers are unable to afford all the recommended immunizations and medications, prioritize interventions (see Sec. 2, Ch. 15, Prioritizing Care for Resource-Limited Travelers ).
Table 2-01 The pretravel consultation: medical history & travel risk assessment
Health background.
Past medical history
- Allergies (especially any pertaining to vaccines, eggs, or latex)
- Medications
- Underlying conditions
Special conditions
- Breastfeeding
- Cardiopulmonary event (recent)
- Cerebrovascular event (recent)
- Disability or handicap
- Guillain-Barré syndrome (history of)
- Immunocompromising conditions or medications
- Pregnancy (including trimester)
- Psychiatric condition
- Seizure disorder
- Surgery (recent)
- Thymus abnormality
Immunization history
- Routine vaccines
- Travel vaccines
Prior travel experience
- High-elevation travel/ mountain climbing
- Malaria chemoprophylaxis
- Prior travel-related illnesses
Travel Risk Assessment (Trip Details)
- Countries and specific regions, including order of countries if >1 country
- Outbreaks at destination
- Rural or urban destinations
- Season of travel
- Time to departure
- Trip duration
Reason for travel
- Education or research
- Medical tourism (seeking health care)
- Visiting friends and relatives
- Volunteer, missionary, or aid work
Travel style
- Accommodations (e.g., camping/ tent, dormitory, guest house, hostel/ budget hotel, local home or host family, tourist/ luxury hotel)
- "Adventurous" eating
- Independent travel or package tour
- Level of hygiene at destination
- Modes of transportation
- Traveler risk tolerance
- Travel with children
Special activities
- Animal interactions (including visiting farms, touring live animal markets)
- Cruise ship
- Cycling/motorbiking
- Disaster relief
- Extreme sports
- High elevations
- Medical care (providing or receiving)
- Rafting or other water exposure
- Sexual encounters (planned)
Assess Individual Risk
Traveler characteristics and destination-specific risk provide the background to assess travel-associated health risks. Such characteristics include personal health background (e.g., past medical history, special conditions, immunization history, medications); prior travel experience; trip details, including itinerary, timing, reason for travel, travel style, and specific activities; and details about the status of COVID-19 and other infectious diseases at the destination. Certain travelers also might confront special risks. Recent hospitalization for serious problems might lead to a decision to recommend delaying travel. Air travel is contraindicated for patients with certain conditions. For instance, patients should not travel by air <3 weeks after an uncomplicated myocardial infarction or <10 days after thoracic or abdominal surgery. Consult relevant health care providers most familiar with the traveler’s underlying illnesses.
Other travelers with specific risks include those who have chronic illnesses, are immunocompromised, or are pregnant. Travelers visiting friends and relatives, long-term travelers, and travelers with small children also face unique risks. More comprehensive discussion on advising travelers with additional health considerations is available in Section 3. Determine whether recent outbreaks or other safety notices have been posted for the traveler’s destination by checking information available on CDC Travelers’ Health and US Department of State websites and other resources.
In addition to recognizing the traveler’s characteristics, health background, and destination-specific risks, discuss anticipated exposures related to special activities. For example, river rafting could expose a traveler to schistosomiasis or leptospirosis, and spelunking in Central America could put the traveler at risk for histoplasmosis. Flying from lowlands to high-elevation areas and trekking or climbing in mountainous regions introduces the risk for altitude illness. Inquire about plans for specific leisure, business, and health care-seeking activities.
Communicate Risk
Once destination-specific risks for a particular itinerary have been assessed, communicate them clearly to the traveler. Health-risk communication is an exchange of information in which the clinician and traveler discuss potential health hazards for the trip and any available preventive measures. Communicating risk is one of the most challenging aspects of a pretravel consultation, because travelers’ perception of and tolerance for risk can vary widely. For a more detailed discussion, see Sec. 2, Ch. 2, . . . perspectives: Travelers’ Perception of Risk .
Manage Risk
Vaccinations.
Vaccinations are a crucial component of pretravel consultations, and the risk assessment forms the basis of recommendations for travel vaccines. Consider whether the patient has sufficient time to complete a vaccine series before travel; the purpose of travel and specific destination within a country will inform the need for vaccines. At the same time, the pretravel consultation presents an opportunity to update routine vaccines (Table 2-02) and to ensure that eligible travelers are up to date with their COVID-19 vaccinations .
Pay attention to vaccine-preventable diseases for which immunity might have waned over time or after a recent immunocompromising condition (e.g., after a hematopoietic stem cell transplant). Asking whether travelers plan to travel again in the next 1–2 years can help them justify an immunization for travel over several years (e.g., rabies preexposure, Japanese encephalitis) rather than only the upcoming trip. Provide travelers with a record of administered immunizations and instructions to follow up as needed to complete a vaccine series.
Table 2-02 The pretravel consultation: vaccines to update & consider 1
Abbreviation: HBsAg, hepatitis B surface antigen.
1 Based on Advisory Committee on Immunization Practices guidelines, current as of October 21, 2021
Malaria Prevention
Self-treatable conditions.
Despite health care providers’ best efforts, some travelers will become ill. Obtaining reliable and timely medical care during travel can be problematic in many destinations. Consequently, consider prescribing certain medications in advance to enable the traveler to treat common health problems. Box 2-01 provides a list of some of the most common situations for which travelers find self-treatment useful.
Travel health providers need to recognize conditions for which travelers might be at risk and provide information about appropriate self-diagnosis and treatment. Keys to a successful treatment strategy include sharing a simple disease or condition definition, recommending or prescribing treatment, and educating the traveler about the expected outcome of treatment. As an example, for travelers’ diarrhea, inform travelers that most symptoms can be managed with fluid replacement plus loperamide or bismuth subsalicylate; prescribe travelers antibiotics they can carry with them for use in selected cases of incapacitating diarrhea (see Sec. 2, Ch. 6, Travelers’ Diarrhea , and Sec. 2, Ch. 7 . . . perspectives: Antibiotics in Travelers’ Diarrhea—Balancing Benefit & Risk ); and tell them to seek medical attention if symptoms persist for 24–36 hours or are particularly severe.
With some activities in remote settings (e.g., trekking), the only alternative to self-treatment would be no treatment. Pretravel counseling might result in a more accurate self-diagnosis and treatment than relying on local medical care in some areas. In addition, the increasing awareness of substandard and counterfeit drugs in pharmacies in certain countries makes it important for travelers to bring quality manufactured drugs with them from a reliable supplier (see Sec. 6, Ch. 3, . . . perspectives: Avoiding Poorly Regulated Medicines & Medical Products During Travel ).
Encourage travelers to carry a travel health kit with prescription and nonprescription medications and review each traveler’s medication list for possible drug–drug interactions. More detailed information for providers and travelers is included in Sec. 2., Ch. 10, Travel Health Kits , and Section 3 has supplementary travel health kit information for travelers who have additional health needs and considerations.
Box 2-01 The pretravel consultation: self-treatable conditions
The following list includes common situations for which travelers might find self-treatment useful. The extent of self-treatment recommendations offered to travelers should reflect the remoteness and difficulty of travel and the availability of reliable medical care at the destination. Recommended self-treatment options for each of the listed diseases are provided below or in the designated sections of this text.
ALTITUDE ILLNESS: Sec. 4, Ch. 5, High Elevation Travel & Altitude Illness
HIV EXPOSURE (OCCUPATIONAL): Sec. 9, Ch. 4, Health Care Workers, Including Public Health Researchers & Medical Laboratorians
JET LAG: Sec. 8, Ch. 4, Jet Lag
MALARIA: Sec. 5, Part 3, Ch. 16, Malaria
MOTION SICKNESS: Sec. 8, Ch. 7, Motion Sickness
TRAVELERS’ DIARRHEA: Sec. 2, Ch. 6, Travelers’ Diarrhea
URINARY TRACT INFECTIONS: common among many women; carrying a prescribed antibiotic for empiric treatment can be helpful.
VAGINAL YEAST INFECTIONS: self-treatment course of patient’s preferred antifungal medication can be prescribed for people who are prone to infections, sexually active, or who might be receiving antibiotics for other reasons, including doxycycline for malaria chemoprophylaxis.
Address Special Health Risks
Travelers with underlying health conditions require additional attention to health issues related to the destination and activities. For instance, travelers with a history of cardiac disease should carry medical reports, including a recent electrocardiogram. Asthma can flare in a traveler visiting a polluted city or from physical exertion during a hike; recommend that travelers discuss with their primary care provider a plan for treatment and carry necessary medication in case of asthma exacerbation.
Instruct travelers on how to obtain travel medical insurance and direct them to resources that provide lists of reputable medical facilities at their destination (e.g., the ISTM website; the American Society of Tropical Medicine and Hygiene website; the US Department of State’s Your Health Abroad website). Advise travelers to identify any allergies or serious medical conditions on a bracelet or a card to expedite medical care in emergency situations (see Sec. 3, Ch. 4, Highly Allergic Travelers ). Section 6 provides more information on preparing for and obtaining health care abroad.
Educate to Change Behavior
The pretravel consultation provides another setting to remind travelers of basic health and safety practices during travel, including frequent handwashing, wearing seatbelts, using car seats for infants and children, safe sexual practices, and COVID-19 prevention. Organize topics into a checklist and place priority on the most serious and frequently encountered issues ( Table 2-03 and Box 2-02 ). In addition, address general issues (e.g., preventing injury, sunburn). Written information is essential to supplement oral advice and enables travelers to review the instructions from their clinic visits. CDC’s Travelers’ Health website provides educational material. By giving advice on health risks and self-treatable conditions, clinicians can minimize the traveler’s need to seek medical care while abroad and possibly help them return to good health faster.
Table 2-03 The pretravel consultation: key discussion topics
TRAVEL-ASSOCIATED RISK
DISCUSSION POINTS
Altitude illness
- Determine if the itinerary puts the traveler at risk of altitude illness.
- Discuss preventive measures (e.g., gradual ascent, adequate hydration, medications to prevent and treat).
Bloodborne pathogens
- Avoid potential exposures (e.g., injections, piercings, tattoos, shared razors).
- Inform travelers who will provide health care overseas what to do in case of needlesticks or bloodborne pathogen exposures; discuss use of HIV postexposure prophylaxis.
- See Box 2-02 for summary on sexual health recommendations for travelers.
Disease-specific counseling
- Advise travelers to prepare for exacerbations or complications from underlying disease(s).
- Remind travelers to keep medications and supplies in carry-on luggage, to keep medications in their original prescription bottles, and to carry copies of their written prescriptions.
Environmental hazards
- Advise travelers to avoid walking barefoot to reduce their chances of certain parasitic infections.
- Advise travelers to avoid wading or swimming in freshwater where where risk for schistosomiasis or leptospirosis is possible.
- Caution travelers to avoid contact with animals to reduce the potential for bites and scratches that can transmit rabies. This is particularly important advice for the parents of young children.
- Remind travelers to apply sunscreen to sun- exposed skin.
Immunizations
- Discuss indications for, effectiveness of, and adverse reactions to immunizations.
- Discuss benefit of antibody titers when past vaccine records are unavailable or unreliable, particularly for hepatitis A, measles, mumps, rubella, and varicella.
- Review routine immunizations and travel immunizations indicated for the specific itinerary and based on the traveler's medical history.
- Screen for chronic hepatitis B for people born in countries with HBsAg prevalence ≥2% (see Map 5-07 ).
Malaria, yellow fever, & other vectorborne diseases
- Define vectorborne disease risks at the destination.
- Discuss personal protective measures and recommended insect bite precautions.
- For itineraries where malaria transmission is a risk: discuss risks and benefits of malaria chemoprophylaxis and recommended chemoprophylaxis choices.
- For itineraries where yellow fever virus transmission is a risk (see Sec. 2, Ch. 5, Yellow Fever Vaccine & Malaria Prevention Information, by Country , and Sec. 5, Part 3, Ch. 16, Yellow Fever ): assess individual traveler precautions and contraindications for receiving yellow fever vaccine; discuss risks and benefits of vaccination; discuss alternatives to vaccination for travelers at increased risk for adverse events from yellow fever vaccine.
Personal safety
- Advise travelers to look for security bulletins related to their destination and consider areas to avoid.
- Discuss precautions travelers can take (including avoiding excess alcohol consumption) to minimize risk for traffic accidents, personal assault, robbery, or drowning.
- Provide information on travel health and medical evacuation insurance.
Respiratory illnesses
- Consider influenza self-treatment for high-risk travelers.
- Discuss diseases and destinations of particular concern.
Travelers’ diarrhea and other food/waterborne illnesses
- Discuss food and water safety.
- Discuss antibiotics for self- treatment, adjunct medications (e.g., loperamide), and staying hydrated.
- Recommend strategies to decrease risk of diarrhea.
Abbreviation: HBsAg, hepatitis B surface antigen
Box 2-02 The pretravel consultation: summary of sexual health recommendations for travelers
Before travel.
- Get recommended vaccinations, including those that protect against sexually transmitted infections (STIs).
- Get recommended tests for HIV and treatable STIs. Be aware of STI symptoms in case any develop.
- Obtain condoms to carry on trip.
- Consider preexposure prophylaxis medication for HIV for high-risk travelers.
- Review local laws about sexual practices and obtain contact information for medical and law enforcement services.
- If pregnant or considering pregnancy, review whether Zika virus infection is a risk at destination.
During Travel
- Use condoms consistently and correctly to decrease the risk of HIV and STIs.
- If indicated, be prepared to start taking medications for HIV postexposure prophylaxis or unintended pregnancy within 72 hours after a high-risk sexual encounter.
- Never engage in sex with a minor (<18 years old), child pornography, or trafficking activities in any country.
- Report suspicious activity to US and local authorities as soon as it occurs.
After Travel
- Avoid exposing sexual partners at home. See a clinician to get recommended tests for HIV and STIs.
- Get treatment for all diagnosed, treatable STIs.
The following authors contributed to the previous version of this chapter: Lin H. Chen, Natasha S. Hochberg
Bibliography
Freedman DO, Chen LH. Vaccines for international travel. Mayo Clin Proc. 2019;94(11):2314–39.
Hatz CFR, Chen LH. Pre-travel consultation. In: Keystone JS, Freedman DO, Kozarsky PE, Connor BA, Nothdurft HD, editors. Travel medicine, 4th ed. Philadelphia: Saunders Elsevier; 2019. pp. 25–30.
Hill DR, Ericsson CD, Pearson RD, Keystone JS, Freedman DO, Kozarsky PE, et al. The practice of travel medicine: guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2006;43(12):1499–539.
International Society of Travel Medicine. The ISTM Body of knowledge for the practice of travel medicine, revised 2017. Atlanta: International Society of Travel Medicine; 2017. Available from: www.istm.org/bodyofknowledge2
Kozarsky PE, Steffen R. Travel medicine education—what are the needs? J Travel Med. 2016;23(5):taw039.
Leder K, Chen LH, Wilson ME. Aggregate travel vs. single trip assessment: arguments for cumulative risk analysis. Vaccine. 2012;30(15):2600–4.
Leder K, Torresi J, Libman MD, Cramer JP, Castelli F, Schlagenhauf P, et al. GeoSentinel surveillance of illness in returned travelers, 2007–2011. Ann Intern Med. 2013;158(6):456–68.
Leung DT, LaRocque RC, Ryan ET. In the clinic: travel medicine. Ann Intern Med. 2018 Jan 2;168(1):ITC1–16.
Steffen R. Travel vaccine preventable diseases—updated logarithmic scale with monthly incidence rates. J Travel Med. 2018;25(1):tay046.

File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Open access
- Published: 05 December 2023
International health regulations and pre-travel health practices of international travelers at Nigerian airport: a cross-sectional study
- Oluwatosin Samson Jegede 1 ,
- Grace Ijitade 2 ,
- Oyedoyin Aanu Fatoye 3 ,
- Timilehin Mercy Jegede 4 ,
- Nicholas Aderinto 5 ,
- Oluwafunmilayo Adenike Oguntoye 6 ,
- Oluwatosin Oluwagbenga Oguntoye 6 ,
- Oluwatosin Ruth Ilori 7 ,
- Olugbemiga Lanre Abodunrin 7 ,
- Adenike Iyanuoluwa Olugbenga-Bello 7 ,
- James Bamidele 8 &
- Dauda Bayo Parakoyi 7
Tropical Diseases, Travel Medicine and Vaccines volume 9 , Article number: 21 ( 2023 ) Cite this article
604 Accesses
1 Altmetric
Metrics details
International Health Regulations (IHR) were developed by the World Health Organization (WHO) to curb the trans-border spread of epidemics. To our knowledge, no airport-based studies have assessed travelers’ health practices against a combination of diseases subject to IHR 2005. Therefore, we aimed to generate and describe the baseline travelers’ pre-travel health practices towards Cholera, Yellow Fever (YF), and Plague at Murtala Muhammed International Airport (MMIA) in Nigeria.
A cross-sectional study was employed to collect data from 486 international travelers using a multistage sampling technique. Pre-travel health practices (a combination of pre-travel consultation, pre-travel vaccination, and preventive measures against insect bites) were assessed using an interviewer-administered questionnaire. Logistic regression models were used to estimates the association between selected variables and pre-travel health practices. Statistical significance level was set at 5%.
A total of 479 complete questionnaires were analyzed. The median age of respondents was 34.0 years Interquartile range (IQR) = 28.0, 44.0). Of the total respondents, 311 (64.3%) were aware of pre-travel health consultation and sources of information, amongst others, including friends/relatives in 180 (37.6%) travelers, social media/internet in 155 (32.4%) travelers, and health professionals in 102 (21.3%) travelers. Two hundred and seventy-one (56.6%) had pre-travel consultation, 156 (32.6%) had YF vaccination, and 226 (47.2%) were prepared to use preventive measures against insect bites. Only 10.6% had good pre-travel practices against the diseases subject to 2 International Health Regulations (IHR). Travelers with bachelor/college degrees, when compared to those with secondary/high education, had 2.91 times higher odds of having good practices when adjusting for other factors (95% C.I: 1.10, 7.70; p < 0.03). Also, those traveling to destinations endemic for YF infection, when compared to those who are not traveling to endemic countries/areas, had 48% lower odds of having good practices after adjusting for other factors (95% C.I: 1.41, 7.77; p < 0.01).
Conclusions
Our study revealed a low prevalence of good pre-travel health practices among participants. Educational level and endemicity of YF at the destination were predictors of pre-travel health practices. Introducing topics on travelers’ health into schools’ curriculums may have a ripple positive effect on health practices among international travelers. Also, there is a need for public enlightenment programs on pre-travel health practices using social media platforms.
Introduction
International Health Regulation is a set of guidelines developed by the World Health Organization (WHO) to prevent the transnational spread of deadly epidemics. Compared to the IHR released in 1969, the latest IHR 2005 is better suited to current trends in the epidemiology of infectious diseases and new and re-emerging health risks [ 1 ]. The IHR 2005 includes diseases like Cholera, Pneumonic Plague, Yellow Fever (YF), Viral hemorrhagic fevers like Ebola, Lassa, and Marburg, and other potential public health concerns such as those with an unknown cause or source [ 2 ].
International travelers are at risk of contracting infections at their new destinations. They may spread the disease from one country to another depending on their premorbid state, length of stay, and mode of transportation [ 3 , 4 , 5 ]. Some examples of diseases reported to have been related to travel include Ebola, Zika, YF, Cholera, and, more recently, COVID-19 [ 6 , 7 , 8 , 9 ].
The WHO recommends mandatory vaccination against YF to stop the YF virus from being imported into vulnerable countries [ 10 ]. In addition, the YF vaccine is recommended for people aged nine months or older and traveling to or living in areas at risk for YF virus in Africa and South America [ 11 ]. Despite this guidance, imported cases of YF have been documented in non-endemic countries due to a lack of vaccinations for travelers [ 8 ]. Similarly, there is a risk of Cholera infection in travelers to areas where Cholera is prevalent [ 12 ]. One hundred fifty cases of travel-related Cholera infections have been documented in different countries between 1990 and 2018 [ 13 ]. In Nigeria, between weeks 1 and 39 of 2020 [ 14 ], 1140 suspected Cholera cases, 40 laboratory-confirmed confirmed cases, and 63 deaths were reported compared with 14,310 suspected Cholera cases with 389 laboratory-confirmed and 236 deaths during the same period in 2018 [ 15 ]. Besides the associated morbidity and mortality, food-borne conditions impede socioeconomic development by straining healthcare systems, harming national economies, tourism, and trade [ 16 ]. Plague often manifests as a severe illness [ 17 ]. An outbreak of Plague occurred in Madagascar in 2017, following which the WHO identified a probable case of Plague in a traveler who had returned from Madagascar to Seychelles [ 18 , 19 ].
To prepare for, detect, and respond to YF epidemics, the Nigerian Government rolled out a national guideline for YF preparedness and response in 2019 [ 20 ]. This guideline aligns with the global Eliminate yellow fever YF Yellow Fever epidemics (EYE) strategy 2017–2026 guideline. In addition, the Nigeria Centers for Disease Control (NCDC) does weekly epidemiological reporting of epidemiological-prone diseases.
To mitigate the risk of person-to-person transmission of infectious diseases, prophylactic health measures are crucial for both travelers and the general population [ 21 ]. Some examples of prophylactic measures include pre-travel vaccination, booster vaccination, serology monitoring, and other preventive measures such as taking precautions against flea and insect bites, of using prophylactic medications, avoiding direct contact with infected body fluids and tissues, and not handling animal carcasses [ 22 , 23 , 24 ]. Pre-travel health assessments or consultation for travelers is carried out to promote risk reduction through preventive measures, including ensuring that travelers seek health advice before embarking on international travel and are up-to-date with their immunizations [ 25 ]. International travelers are expected to seek medical consultation at least 4 to 8 weeks before starting their journey [ 26 ].
There is lack of data on pre-travel health practices against Cholera, YF, and Plague, a group of infectious diseases endemic in Africa and subject to the IHR of 1969 and 2015. Previous studies have assessed vaccination and pre-travel health practices against YF among travelers from non-endemic areas (such as the USA and Europe) to endemic areas in Africa [ 27 , 28 , 29 ]. Still, there is needs to be more research that assesses the vaccination practices of travelers from developing countries to other parts of the world. Also, to our knowledge, there has been no airport-based study on pre-travel health practices against a group of diseases subject to IHR. Therefore, we aimed to generate and describe the baseline travelers’ pre-travel health practices towards Cholera, YF, and Plague at Murtala Muhammed International Airport (MMIA) in Nigeria.
Study design
A cross-sectional study design was employed to collect data from travelers embarking on international travel through the airport.
Study setting
This study was conducted at Murtala Muhammed International Airport (MMIA) in Nigeria. Nigeria’s premier international air gateway. MMIA is located in Lagos and was commissioned in 1978 [ 30 ]. According to the Nigerian Bureau of Statistics, 3,202,837 passengers traveled through the international airport in 2019 [ 31 ]. The Port Health Services, a government agency located within the airport arena, provides pre-travel health vaccination services. The activities at the airport are overseen by the Federal Airport Authority of Nigeria (FAAN).
Recruitment process
This study was planned for January 2020, but data collection was carried out from October to November 2020 after easing the COVID-19 lockdown in Nigeria. Data collection took place daily at the departure gates of MMIA based on a pre-determined and Institutional Review Boards (IRB) approved study protocol.
Participants – inclusion and exclusion criteria and sample size
We included travelers aged 18 years and above and excluded travelers using MMIA for transfer or transit to other countries. A brief screening survey was conducted to identify eligible participants. The sample size was determined using Leslie Fisher’s formula for prevalence studies. The assumed proportion of YF vaccination was 76% from a previous study, and the level of precision was set at 0.04 [ 32 ]. The computed sample size was increased by 10% to compensate for non-responses. This gave a total sample size of 486.
Participants recruitment: sampling technique and selection of study participants
Stage 1: selection of travelers’ destinations based on who regions.
Four out of the six WHO regions were included in this study [ 33 ]. The four areas were African, American, European, and Eastern Mediterranean because Nigeria does not have direct flights to the remaining two regions (i.e. South-East Asian and Western Pacific Regions).
Stage 2: proportional allocation of travelers to WHO regions using a stratified sampling method
Based on the 2019 Winter flight schedule received from the Commercial Travel Section of the Operation Unit of MMIA, the expected monthly traveler volume was estimated to be 223,704. This was proportionally allocated to 4 WHO regions to ensure the representativeness of travelers and travel destinations. The African region, comprising 113,316, was further stratified into the West African, East African, Central African, and Southern African regions.
Stage 3: selection of study participants using simple random sampling
A simple random sampling method was used to select study participants per region. The samples were randomly selected using electronically generated random numbers. The data collection was completed in four weeks using a daily data collection plan to meet the data target for each WHO region. Questionnaires were administered at the departure gates of each flight. If a selected traveler declines to participate in the study, the traveler representing the following randomly selected number was approached to participate.
Data collection
A semi-structured questionnaire, adapted from the International Health Travel Questionnaires [ 7 , 13 ] and questionnaires from previous studies, was used to collect relevant data from study participants (supplementary document 1 ). The questionnaire was pre-tested at the Nnamdi Azikiwe International Airport, Abuja, Nigeria.
The independent variables of interest were educational level, nationality, Cholera endemicity at the destination, YF endemicity at the destination, traveler’s awareness of pre-travel vaccination, and inspection of vaccination cards during the previous trip(s). Their covariates are listed as a footnote under Table 1 .
The dependent variable is pre-travel health practices (a composite score of the practice of pre-travel consultation/advice, pre-travel vaccination status, and pre-travel preventive measures). Pre-travel consultation or advice was defined as information obtained from a health professional [ 22 ]. Pre-travel consultation was categorized as taken and not taken; vaccination was categorized as vaccinated and not vaccinated based on reported vaccination for YF among those traveling to endemic countries. Self-reported YF vaccination was used as a proxy for vaccination because it was readily accessible at the Nigerian Port Health Services compared to the Cholera vaccine. To validate the vaccination status, we inspected the vaccination cards of travelers. Pre-travel preventive measures were categorized as taken and not taken among travelers going to YF endemic and Plague endemic regions. The preventive measures assessed were actions to prevent (a) the bite of infected vector fleas for Plague and mosquitoes for YF, (b) contact with infectious bodily fluids or contaminated materials, and (c) the inhalation of respiratory droplets/small particles from a patient with pneumonic Plague.
The composite score of pre-travel health practices ranged from 0 to 3. Having taken pre-travel consultation/advice was scored 1 while not taken was scored 0, pre-travel vaccination was scored 1 while non-vaccination was scored 0, and having taken pre-travel preventive measures was scored 1 while non-practice was scored 0. Those with a score of 3 were categorized as having good practices, while those with scores of 2 or less were categorized as having poor practices. We ensured no overlap of the scores to prevent misclassification of travelers.
Statistical analysis
Data analysis was done using IBM SPSS Statistics 25.0. Descriptive statistics were presented in frequency tables, while pre-travel health practices were visually represented using a pie chart. A binary logistic regression analysis was employed to examine the association between the independent and dependent variables of interest and pre-travel health practices. Furthermore, a multivariable analysis was conducted to reduce the influence of potentially confounding variables, controlling for relevant covariates (Table 1 ). Before fitting the model, variables with cell counts less than 5 were recategorized. Educational level was recategorized into 3 levels: secondary/high school or less, undergraduate or College, and Graduate (Masters/Ph.D./Professional). The undergraduate or College and Graduate (Masters/Ph.D./Professional) were also referred to as higher educational levels under the discussion.
We used a directed acyclic graph (DAG) to identify possible confounders of our selected exposures and controlled for them in the multivariable analysis. The significance level was set at 5%, and the odds ratio was presented with a 95% confidence interval.
Four hundred and seventy-nine valid questionnaires were analyzed. The median age of respondents was 34.0 years (IQR = 28.0, 44.0). As regards the gender of respondents, 332 (69.3%) were males, giving an M:F ratio of 2.3 to 1. One hundred and eighty-five (38.6%) were single, and 201 (42.0%) had an undergraduate degree (Table 2 ). Twenty-six airlines from 21 countries were operating at MMIA as of the time of this study. The top three nationalities of the travelers who participated in this study were Nigeria 321 (67.0%), India 91 (19.0%), and Ghana 20 (4.1%). In contrast, the top three places our respondents were traveling to were the UAE 99 (20.7%), India 88 (18.3%), and the United Kingdom 61 (12.7%), respectively. Using the World Economic Situations and Prospects (WESP) [ 34 ] classification, travelers were mostly from developing countries 451 (94.2%) (Table 2 ).
Overall, 59 (12.3%) were not aware of any of the three diseases, while 90 (18.8%) were aware of only one of the diseases, 255 (53.2%) were aware of two conditions, and 75 (15.7%) were of all the three diseases. Their sources of information about these diseases included friends/relatives 31 (6.5%), social media/internet 61 (12.7%), and health professionals 27 (5.6%), amongst others. In terms of travelers’ awareness of the specific diseases, 331 (69.1%) were aware of Cholera, 407 (85.0%) were aware of YF, and 87 (18.2%) travelers were aware of the Plague (Fig. 1 ). Of the 87 travelers aware of Plague disease, 2 (0.4%) could identify avoiding dead animals as a way of protecting themselves from acquiring the infection. Also displayed in Table 2 is the Endemicity of Cholera, YF, or Plague diseases at travelers’ final destination. One hundred and one (21.1%) of participants were traveling to Cholera-endemic countries, and 50 (10.4%) were traveling to YF-endemic countries.
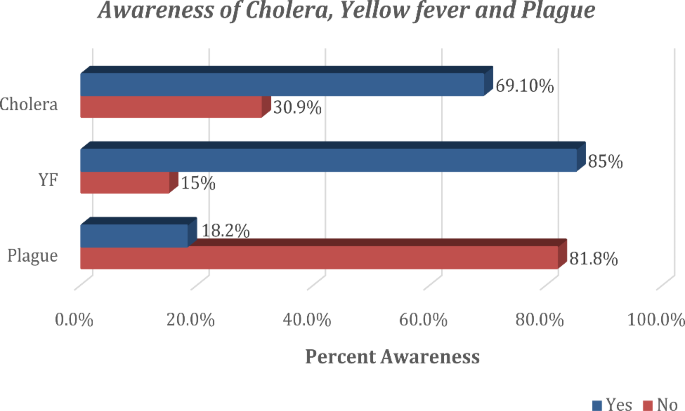
Awareness about Cholera, YF and Plague among study participants
As displayed in Tables 3 , 311 (64.3%) of the total respondents were aware of pre-travel consultation. Their sources of information, amongst others, include friends/relatives in 180 (37.6%) travelers, social media/internet in 155 (32.4%) travelers, and health professionals in 102 (21.3%) travelers. Two hundred and seventy-one (56.6%) of travelers who were aware of pre-travel consultation have ever done it. The time interval between receiving pre-travel consultation and departure time was less than one week in 227 (47.4%) travelers (Table 3 ). Two hundred and sixty-two (54.7%) were aware of pre-travel vaccination, 156 (32.6%) reported to have been vaccinated before embarking on this journey, 260 (54.3%) said to have traveled in the past without being vaccinated, and another 120 (25.1%) had traveled before without holding vaccination cards. During this study, 105 (21.9%) traveled without holding vaccination cards. The self-reported vaccination rate for YF and Cholera were 29.4% and 1.9%, respectively; however, among all travelers, only 271 (56.6%) provided vaccination cards for inspection as evidence of claim. Travelers’ practices of preventive measures against insect bites are also displayed in Table 3 . Overall, 226 (47.2%) respondents were ready to protect themselves against insect bites.
Figure 2 shows the status of pre-travel health practices among respondents. Of the 479 travelers, 51 (10.6%) had good practices, while 428 (89.4%) had poor practices.
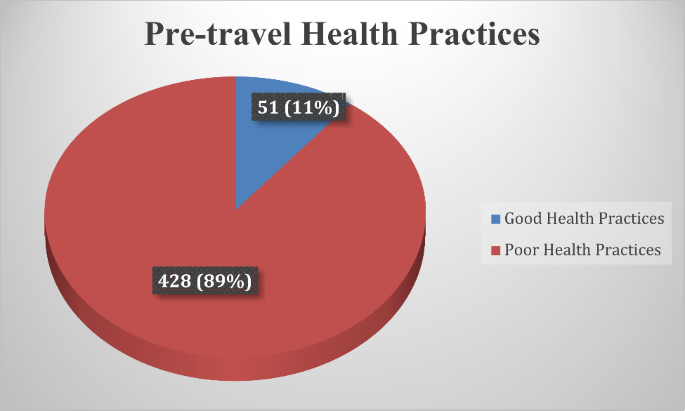
Status of pre-travel health practices among study participants
Travelers with bachelor/college degrees, when compared to those with secondary/high school education, had 2.91 times higher odds of having good practices when adjusting for other factors (95% C.I: 1.10, 7.70; p < 0.03). Also, those traveling to destinations endemic for YF infection, when compared to those who are not traveling to endemic countries/areas, had 48% lower odds of having good practices when adjusting for other factors (95% C.I: 1.41, 7.77; p < 0.01) (Table 1 ).
Our study fills a significant research gap and was the first to investigate travelers’ pre-travel health practices towards Cholera, YF, and Plague at MMIA in Nigeria.
The male-to-female ratio found in our study can be explained by the fact that there are more males than females in Nigeria [ 35 ].
Our study found social media/websites to be one of the primary sources of information on the awareness of the diseases subjected to IHR. In contrast, a previous study at MMIA reported that 77.4% of travelers mentioned travel agents as their primary source of information [ 36 ].
The difference could be attributed to the focus of their study, which was on general information for travelers rather than on disease-specific information. Health professionals were also found to rank among the first three leading sources of information for travelers on awareness of YF, awareness of Plague understanding, and pre-travel health consultation or advice. These two primary sources (social media/internet and health professionals) may serve as channels for disseminating information about pre-travel health preparedness for international travelers.
In this study, only one-tenth of travelers had good pre-travel health practices against the diseases subject to IHR. This rate is below expectation as we expected at least 31.1% (i.e., the proportion of participants traveling to countries endemic for Cholera, YF, and Plague) to have good pre-travel health practices. The implication is that many travelers could risk being infected with Cholera, YF, or Plague at their destinations. Only a few (2.3%) of those seeking pre-travel consultation did so more than four weeks before their journey. This low proportion is far from expectation when evaluated against the recommendation of WHO that consultation should be done at least 4–8 weeks before a proposed journey [ 5 ]. The public health implication of seeking consultation late or not taking pre-travel consultation is that travelers may not get adequate information about the endemic diseases at their proposed destinations or may not have enough time to take preventive measures, including vaccinations.
Notably, despite the YF outbreak in Nigeria at the time of this study, only one-third of travelers took the YF vaccine [ 37 ]. This proportion was lower than the vaccination rate in previous studies conducted at MMIA and Ethiopia, where 66.2% and 83.1% of participants reported being vaccinated, respectively [ 38 , 39 ]. The low rates of Plague awareness and practice of preventive measures against insect bites are not unexpected as Plague is not a common disease globally and is not endemic in Nigeria.
Having good health practices among travelers to countries endemic to YF could be partially attributed to historical knowledge of the disease among people living in Nigeria and widespread access to the internet by international travelers. The relationship between higher educational levels and pre-travel health practices has also been established in a study conducted in Taiwan [ 40 ]. This association could be attributed to high curiosity for knowledge among travelers with advanced and widespread access to the internet.
Research limitation
This study left out two WHO regions (South-East Asian and Western Pacific Regions) in selecting study participants. However, those regions were considered and included in categorizing and analyzing travelers’ final destinations.
Research strength
This study was the first to examine a combination of diseases subject to international health regulation. In addition, our analysis used a directed acyclic graph (DAG) to identify and control for possible confounders of our selected exposures.
Generalizability
This study can be generalized because of its large sample size and the stratified selection of study participants to ensure the representativeness of participants. We also used a multivariate statistical method to identify the predictors of good pre-travel health practices.
This study revealed that good pre-travel health practices against diseases subject to IHR were deficient among international travelers departing from MMIA. Travelers’ educational status and travel destinations were predictors of good practices.
One crucial recommendation to the Nigerian Government is to include travelers’ health in the existing secondary/high school curriculum on health. This initiative will build a culture of harnessing travel-related health information among students as they grow. We envisage this would have a ripple effect on travelers and the general population. There is a need for the Government of Nigeria to implement public enlightenment programs on pre-travel health consultation and pre-travel vaccination; we believe that social media will be a vital tool in achieving this by the result of this study. Healthcare practitioners are also encouraged to give their clients adequate information about pre-travel health preparations when they visit for pre-travel health consultations.
Data Availability
The datasets used and analyzed during the current study are available from the first author upon reasonable request.
Abbreviations
African Regional Office
American Regional Office
Adjusted Odds Ratio
Crude Odds Ratio
Eastern Mediterranean Regional Office
European Regional Office
International Health Regulations
Institutional Review Boards
Interquartile Range
Southeast Asia Regional Office
Statistical Package for the Social Sciences
United Arab Emirates
World Economic Situations and Prospects
World Health Organization
Western Pacific Regional Office
Yellow Fever
Hardiman M, Wilder-Smith A. The revised international health regulations and their relevance to travel medicine. J Travel Med. 2007;14(3):141–4. https://doi.org/10.1111/j.1708-8305.2007.00117.x .
Article PubMed Google Scholar
World Health Organization. International Health Regulations. Second.; 2005. https://doi.org/10.1177/146642407109100301 .
Heywood AE, Nothdurft H, Tessier D, et al. Pre-travel advice, attitudes and hepatitis A and B vaccination rates among travelers from seven countries. J Travel Med. 2016;24(1):1–8. https://doi.org/10.1093/jtm/taw069 .
Article Google Scholar
Adongo PB, Tabong PTN, Asampong E, Ansong J, Robalo M, Adanu RM. Health workers perceptions and attitude about Ghana’s preparedness towards preventing, containing, and managing Ebola Virus Disease. BMC Health Serv Res. 2017;17(1):1–13. https://doi.org/10.1186/s12913-017-2225-0 .
World Health Organization. International travel and health. World Health Organization. World Health Organization; 2012:1–11.
Schuh AJ, Kyondo J, Graziano J, et al. Rapid establishment of a frontline field laboratory in response to an imported outbreak of Ebola virus disease in western Uganda, June 2019. PLoS Negl Trop Dis. 2021;15(12). https://doi.org/10.1371/journal.pntd.0009967 .
Slesak G, Schäfer J, Fleck R, Jacob D, Grunow R. Imported Cholera with acute renal failure after a short business-trip to the Philippines, Germany, October 2015. Euro Surveill. 2016;21(1):30099. https://doi.org/10.2807/1560-7917.ES.2016.21.1.30099 .
Schlagenhauf P, Chen LH. YFYF importation to China – a failure of pre- and post-travel control systems? Int J Infect Dis. 2017;60:91–2. https://doi.org/10.1016/j.ijid.2017.06.003 .
Holshue ML, DeBolt C, Lindquist S, et al. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med. 2020;382(10):929–36. https://doi.org/10.1056/nejmoa2001191 .
Article PubMed PubMed Central Google Scholar
World Health Organization. Countries with risk of YFYF transmission and countries requiring YFYF vaccination. International Travel and Health. World Health Organization; 2018:1–4.
Centers for Disease Control and Prevention. (2021). YFYF Vaccine Recommendations. Retrieved from https://www.cdc.gov/yellowfever/vaccine/vaccine-recommendations.html#:~:text=Yellow%20 fever%20vaccine%20is%20recommended,the%20vaccine%20is%20not%20needed.
Hammad S, N’cho KK, Wong EDM. Travel-Related Infectious Diseases. Centres for Disease Control and Prevention. Published 2020. Accessed January 7, 2021. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/Cholera .
Connor BA, Dawood R, Riddle MS, Hamer DH. Cholera in travelers:a systematic review. J Travel Med. 2019;26(8):1–8. https://doi.org/10.1093/jtm/taz085 .
Nigerian Centers for Disease Control (NCDC). (2020, September). Weekly Epidemiological Report. Retrieved from https://ncdc.gov.ng/reports/weekly/2020/9/39 .
Nigerian Centers for Disease Control (NCDC). (2018). Strengthening Nigeria’s Rapid Response Teams. Weekly Epidemiological Report. Retrieved from https://ncdc.gov.ng/reports/weekly .
World Health Organization. (2021). Food safety. World Health Organization Website. Retrieved from https://www.who.int/news-room/fact-sheets/detail/food-safety .
World Health Organization. Plague. World Health Organization Fact sheets. Published 2017. Accessed August 31., 2018. http://www.who.int/news-room/fact-sheets/detail/Plague .
World Health Organization (WHO). WHO Seychelles – Suspected Plague (Ex- Madagascar). Emergencies preparedness, response. Published 2017. Accessed September 15., 2018. http://www.who.int/csr/don/15-october-2017-Plague-seychelles/en/ .
World Health Organization (WHO). 18-10-2017-suspected-cases-from-seychelles-test-negative-for-Plague @ www.who.int. World Health Organization News Release. Published 2017. Accessed September 17., 2018. http://www.who.int/news-room/detail/18-10-2017-suspected-cases-from-seychelles-test-negative-for-Plague .
Nigeria Centre for Disease Control. (2019). Retrieved from https://ncdc.gov.ng/themes/common/docs/protocols/118_1581155661.pdf .
Herck K, Van, Castelli F, Zuckerman J, et al. Knowledge, Attitudes and Practices in Travel-related infectious Diseases : the european Airport Survey. J Travel Med. 2004;11(1):3–8.
CDC Advisory Committee on Immunization Practices (ACIP). YFYF Vaccine Recommendations [Internet]. Centers for Disease Control and Prevention. 2017 [cited 2023 July 23]. Available from: https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/yf.html .
Chen LH, Natasha Hochberg. The Pretravel Consultation CDC Yellow Book 2024 Preparing International Travelers [Internet]. CDC Travelers’ Health Webpage. 2023 [cited 2023 Jul 25]. Available from: https://wwwnc.cdc.gov/travel/yellowbook/2024/preparing/pretravel-consultation .
World Health Organization. Plague [Internet]. World Health Organization Fact sheets. 2017 [cited 2023 July 21]. Available from: http://www.who.int/news-room/fact-sheets/detail/Plague .
Heywood AE, Watkins RE, Iamsirithaworn S, Nilvarangkul K, Macintyre CR. A cross-sectional study of pre-travel health-seeking practices among travelers departing Sydney and Bangkok airports. BMC Public Health. 2012;12:1–9. https://doi.org/10.1186/1471-2458-12-321 .
World Health Organization. International travel and health. In: World Health Organization [Internet]. Geneva: World Health Organization. ; 2012. p. 1–11. Available from: http://apps.who.int/bookorders/MDIbookPDF/Book/18000079.pdf .
Hagmann SHF, Rao SR, LaRocque RC, et al. Travel characteristics and pretravel health care among pregnant or breastfeeding U.S. women preparing for international travel. Obstet Gynecol. 2017;130(6):1357–65. https://doi.org/10.1097/AOG.0000000000002360 .
Khan NM, Jentes ES, Brown C, et al. Pre-Travel Medical Preparation of Business and an analysis of the global TravEpiNet Consortium, 2009 to 2012. J Occup Environ Med. 2016;58(1). https://doi.org/10.1097/JOM.0000000000000602 .
Schonenberger S, Hatz C, Buhler S. Unpredictable checks of YFYF vaccination certificates upon arrival in Tanzania. J Travel Med. 2016;23(5):1–5. https://doi.org/10.1093/jtm/taw035 .
Federal Airports Authority of Nigeria. International Airports. FAAN website. Published 2022. Accessed January 25, 2023. https://faan.gov.ng/international-airports/ .
National Bureau of Statistics. (2021). Air Transportation Data (Full Year). Retrieved from https://nigerianstat.gov.ng/resource/Air%20Transport_full%20year%202021.xlsx .
Toovey S, Jamieson A, Holloway M. Travelers ’ knowledge, Attitudes and Practices on the Prevention of Infectious Diseases : results from a study at Johannesburg International Airport. J Travel Med. Published online 2004:16–22.
United Nations. World Economic Situation and Prospects - Annex. In: World Economic Situation and Prospects [Internet]. New York: United Nations. ; 2020. p. 161–200. Available from: https://www.un.org/development/desa/dpad/wp-content/uploads/sites/45/WESP2020_FullReport.pdf .
World Health Organisation. WHO regional offices. World Health Organization. Published 2017. Accessed August 25., 2018. http://www.who.int/About/Regions/En/ .
National Bureau of Statistics. Statistical report on women and men in Nigeria.; 2019.
Nwagwu W, Kolapo A. Information needs, information sources and information search strategies of International Air Travelers in Nigeria. Pearl: A Journal of Library and Information Science. 2012;6(4):216. https://doi.org/10.5958/j.0973-7081.6.4.024 .
Centres for Disease Control and Prevention. YFYF in Nigeria. CDC Travelers’ Health Webpage. Published November 2020. Accessed January 11., 2023. https://wwwnc.cdc.gov/travel/notices/alert/yellow-fever-nigeria .
Akodu BA, Ogwu FO, Abiola AHO. Knowledge, attitude and compliance towards travel vaccines among nigerian travelers at an international airport. Afr J Prim Health Care Fam Med. 2019;11(1):1–9. https://doi.org/10.4102/PHCFM.V11I1.2063 .
Jegede OS, Ali A, Ayele W. Awareness and practice of Pre-travel Vaccination among International Travelers departing from Addis Ababa Bole International Airport. Int J Travel Med Glob Health. 2020;8(2):58–65. https://doi.org/10.34172/ijtmgh.2020.10 .
Chuang PN, Yang CJ, Huang HL, et al. Pretravel preparation and factors associated with willingness to seek pretravel consultation among taiwanese travelers. Travel Med Infect Dis. 2022;49:102397. https://doi.org/10.1016/j.tmaid.2022.102397 .
United Nations. World Economic Situation and prospects - Annex. World Economic Situation and prospects. United Nations; 2020:161–200.
Download references
Acknowledgements
We appreciate Dr. Morenike Alex-Okoh (Director of Public Health in Nigeria) and Mrs. Victoria Shin-Aba (Airport Manager of MMIA) for approving the conduct of this study. We are grateful to Dr. Abdullahi (Head of Department, Port Health Services, Lagos), Dr. Bukunmi Bolarinwa, who organized airport entry, our research assistants who ensured the quality of data collected, and all the travelers who participated in this study.
The researchers fully funded the study; there was no external funding/support.
Author information
Authors and affiliations.
Herbert Wertheim School of Public Health and Human Longevity Science, University of California, San Diego, CA, USA
Oluwatosin Samson Jegede
Department of Biostatistics and Epidemiology, College of Public Health, Johnson City, East Tennessee State, USA
Grace Ijitade
Department of Community Medicine, LAUTECH Teaching Hospital, Ogbomoso, Nigeria
Oyedoyin Aanu Fatoye
Department of Anesthesia and Intensive Care Unit, Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife, Nigeria
Timilehin Mercy Jegede
Department of Medicine and Surgery, Ladoke Akintola University of Technology, Ogbomoso, Nigeria
Nicholas Aderinto
Department of Medicine, Afe Babalola University, Ado-Ekiti, Nigeria
Oluwafunmilayo Adenike Oguntoye & Oluwatosin Oluwagbenga Oguntoye
Department of Community Medicine, College of Health Sciences, Ladoke Akintola, University of Technology, Ogbomoso, Nigeria
Oluwatosin Ruth Ilori, Olugbemiga Lanre Abodunrin, Adenike Iyanuoluwa Olugbenga-Bello & Dauda Bayo Parakoyi
Department of Community Medicine, Ekiti State University, Ado Ekiti, Nigeria
James Bamidele
You can also search for this author in PubMed Google Scholar
Contributions
O.S.J conceived the study idea and study design. O.S.J, G.I, O.A.F, and T.M.J supervised data collection. O.S.J, G.I, O.R.I, O.L.A, A.I.O-B, J.B, and D.B.P participated fully in data analysis O.S.J , G.I,O.A.F, T.M.J, O.A.O, O.O.O, O.R.I, O.L.A, A.I.O-B, J.B, N.A, and D.B.P participated fully in the reporting and interpretation of the data. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Nicholas Aderinto .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
Ethical approval was obtained from the Ethical Review Committee of LAUTECH Teaching Hospital, Ogbomoso, Nigeria (LTH/OGB/EC/2019/191). This study did not involve any physical/clinical examinations or investigations, and thus, the study did not pose any health risk to the respondents. The respondents were told that participation is voluntary and would not suffer any consequences if they chose not to participate in the study. Respondents had the right to decline or withdraw from the study at any time. Before collecting data, we obtained consent from study participants and identified them using only serial numbers to guarantee confidentiality.
Consent for publication
Not Applicable.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jegede, O.S., Ijitade, G., Fatoye, O.A. et al. International health regulations and pre-travel health practices of international travelers at Nigerian airport: a cross-sectional study. Trop Dis Travel Med Vaccines 9 , 21 (2023). https://doi.org/10.1186/s40794-023-00207-8
Download citation
Received : 11 May 2023
Accepted : 28 September 2023
Published : 05 December 2023
DOI : https://doi.org/10.1186/s40794-023-00207-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Vaccinations
- International Health Regulation
- Pre-travel health practices
Tropical Diseases, Travel Medicine and Vaccines
ISSN: 2055-0936
- Submission enquiries: [email protected]

The Pretravel Consultation
The pretravel consultation offers a dedicated time to prepare travelers for the health concerns that might arise during their trips. The objectives of the pretravel consultation are to:
- Perform an individual risk assessment.
- Communicate to the traveler anticipated health risks.
- Provide risk management measures, including immunizations, malaria prophylaxis, and other medications as indicated.
The Travel Medicine Specialist
Travel medicine specialists have in-depth knowledge of immunizations, risks associated with specific destinations, and the implications of traveling with underlying conditions. Therefore, a comprehensive consultation with a travel medicine expert is indicated for all travelers, and is particularly important for those with a complicated health history, special risks (such as traveling at high altitudes or working in refugee camps), or exotic or complicated itineraries. Clinicians who wish to be travel medicine providers are encouraged to join the International Society of Travel Medicine (ISTM) and consider specialty training and certification.
Components of a Pretravel Consultation
Effective pretravel consultations require attention to the health background of the traveler and incorporate the itinerary, trip duration, travel purpose, and activities, all of which determine health risks (Table 2-1 ). The pretravel consultation is the major opportunity to educate the traveler about health risks at the destination and how to mitigate them. The typical pretravel consultation does not include a physical examination; a separate appointment with the same or a different provider may be necessary to assess a person’s fitness to travel. Because travel medicine clinics are not available in some communities, primary care physicians should seek guidance (by phone or other communication, if available) from travel medicine specialists to address areas of uncertainty.
Travel health advice should be personalized, highlighting the likely exposures and also reminding the traveler of ubiquitous risks, such as injury, foodborne and waterborne infections, vectorborne disease, respiratory tract infections, and bloodborne and sexually transmitted infections. Balancing the cautions with an appreciation of the positive aspects of the journey leads to a more meaningful pretravel consultation. Attention to the cost of recommended interventions may be critical. Some travelers may not be able to afford all of the recommended immunizations and medications, a situation that requires prioritizing interventions. (See Prioritizing Care for the Resource-Limited Traveler later in this chapter.)
Assess Individual Risk
Many elements merit consideration in assessing a traveler’s health risks (Table 2-1 ). Certain travelers may confront special risks. Recent hospitalization for serious problems may lead the travel health provider to recommend delaying travel. Air travel is contraindicated for certain conditions, such as <3 weeks after an uncomplicated myocardial infarction and <10 days after thoracic or abdominal surgery. The travel health provider and traveler should consult with the relevant health care providers most familiar with the underlying illnesses. Other travelers with specific risks include travelers who are visiting friends and relatives, long-term travelers, travelers with small children, travelers with chronic illnesses, immunocompromised travelers, and pregnant travelers. More comprehensive discussion on advising travelers who have additional health considerations is available in Chapter 5. Providers should determine whether recent outbreaks or other safety notices have been posted for the traveler’s destination; information is available on the CDC and US Department of State websites, and in various other resources.
In addition to recognizing the traveler’s characteristics, health background, and destination-specific risks, the exposures related to special activities also merit discussion. For example, river rafting could expose a traveler to schistosomiasis or leptospirosis, and spelunking in Central America could put the traveler at risk of histoplasmosis. Flying from lowlands to high-altitude areas and trekking or climbing in mountainous regions introduces the risk of altitude illness. Therefore, the provider should inquire about plans for specific leisure, business, and health care–seeking activities.
Communicate Risk
Once destination-specific risks for a particular itinerary have been assessed by the provider, they should be clearly communicated to the traveler. The process of risk communication is a 2-way exchange of information between the clinician and traveler, in which they discuss potential health hazards at the destination and the effectiveness of preventive measures, with the goal of improving understanding of risk and promoting more informed decision making. Risk communication is among the most challenging aspects of a pretravel consultation, because travelers’ perception of and tolerance for risk can vary widely. For a more detailed discussion, see Perspectives : Travelers’ Perception of Risk in this chapter.
Manage Risk
Immunizations are a crucial component of pretravel consultations, and the risk assessment forms the basis of recommendations for travel vaccines. For example, providers should consider whether there is sufficient time before travel to complete a vaccine series; the purpose of travel and specific destination within a country will inform the need for particular vaccinations. At the same time, the pretravel consultation presents an opportunity to update routine vaccines (Table 2-2 ). Particular attention should be paid to vaccines for which immunity may have waned over time or following a recent immunocompromising condition (such as after a hematopoietic stem cell transplant). Asking the question, “Do you have any plans to travel again in the next 1–2 years?” may help the traveler justify an immunization for travel over a number of years rather than only the upcoming trip, such as rabies preexposure or Japanese encephalitis. Travelers should receive a record of immunizations administered and instructions to follow up as needed to complete a vaccine series.
Another major focus of pretravel consultations for many destinations is the prevention of malaria. Malaria continues to cause substantial morbidity and mortality in travelers. Since 1973, the annual number of US malaria cases reported to CDC has shown an increasing trend; therefore, pretravel consultation must carefully assess travelers’ risk for malaria and recommend preventive measures. For travelers going to malaria-endemic countries, it is imperative to discuss malaria transmission, ways to reduce risk, recommendations for prophylaxis, and symptoms of malaria.
Travelers with underlying health conditions require attention to their health issues as they relate to the destination and activities. For example, a traveler with a history of cardiac disease should carry medical reports, including a recent electrocardiogram. Asthma may flare in a traveler visiting a polluted city or from physical exertion during a hike; travelers should be encouraged to discuss with their primary care provider how to plan for treatment and bring necessary medication in case of asthma exacerbation. Travelers should be counseled on how to obtain travel medical insurance and how they can find reputable medical facilities at their destination, such as using the ISTM website ( www.istm.org ), the American Society of Tropical Medicine and Hygiene website ( www.astmh.org ), or the State Department Travel website ( https://travel.state.gov/content/travel/en/international-travel/before-you ...). Any allergies or serious medical conditions should be identified on a bracelet or a card to expedite medical care in emergency situations.
The pretravel consultation also provides another setting to remind travelers of basic health practices during travel, including frequent handwashing, wearing seatbelts, using car seats for infants and children, and safe sexual practices. Topics to be explored are numerous and could be organized into a checklist, placing priority on the most serious and frequently encountered issues (Table 2-3 , Box 2-1 ). General issues such as preventing injury and sunburn also deserve mention. Written information is essential to supplement oral advice and enable travelers to review the instructions from their clinic visits; educational material is available on the CDC Travelers Health webpage ( www.cdc.gov/travel ). Advice on self-treatable conditions may minimize the need for travelers to seek medical care while abroad and possibly lead to faster return to good health.
Self-Treatable Conditions
Despite providers’ best efforts, some travelers will become ill. Obtaining reliable and timely medical care during travel can be problematic in many destinations. As a result, prescribing certain medications in advance can empower the traveler to self-diagnose and treat common health problems. With some activities in remote settings, such as trekking, the only alternative to self-treatment would be no treatment. Pretravel counseling may result in a more accurate self-diagnosis and treatment than relying on local medical care in some areas. In addition, the increasing awareness of substandard and counterfeit drugs in pharmacies in the developing world makes it more important for travelers to bring quality manufactured drugs with them from a reliable supplier in their own country (see Chapter 6, Perspectives : Avoiding Poorly Regulated Medicines and Medical Products during Travel ).
Travel health providers need to recognize the conditions for which the traveler may be at risk, and educate the traveler about the diagnosis and treatment of those conditions. The keys to successful self-treatment strategies are providing a simple disease or condition definition, providing a treatment, and educating the traveler about the expected outcome of treatment. Using travelers’ diarrhea as an example, a practitioner could provide the following advice:
- “Travelers’ diarrhea” is the sudden onset of abnormally loose, frequent stools.
- Most cases will resolve within 2–5 days, and symptoms can be managed with loperamide or bismuth subsalicylate.
- For diarrhea severe enough to interrupt travel plans, an antibiotic can be prescribed that travelers can carry with them (see Travelers’ Diarrhea section in this chapter).
- The traveler should feel better within 6–24 hours.
- If symptoms persist for 24–36 hours despite self-treatment, it may be necessary to seek medical attention.
To minimize the potential negative effects of a self-treatment strategy, the recommendations should follow a few key points:
- Drugs recommended must be safe, well tolerated, and effective for use as self-treatment.
- A drug’s toxicity or potential for harm, if used incorrectly or in an overdose situation, should be minimal.
- Simple and clear directions are critical. Consider providing handouts describing how to use the drugs. Keeping the directions simple will increase the effectiveness of the strategy.
The following are some of the most common situations in which people would find self-treatment useful. The extent of self-treatment recommendations offered to the traveler should reflect the remoteness and difficulty of travel and the availability of reliable medical care at the destination. The recommended self-treatment options for each disease are provided in the designated section of the Yellow Book or discussed below.
- Travelers’ diarrhea ( Chapter 2 , Travelers’ Diarrhea)
- Altitude illness ( Chapter 3 , High-Altitude Travel & Altitude Illness)
- Jet lag ( Chapter 8 , Jet Lag)
- Motion sickness (Chapter 8, Motion Sickness )
- Respiratory infections ( Chapter 11 , Respiratory Infections)
- Skin conditions such as allergic reactions or superficial fungal infections ( Chapter 11 , Skin & Soft Tissue Infections)
- Urinary tract infections: common among many women; carrying an antibiotic for empiric treatment may be valuable
- Vaginal yeast infections: self-treatment course of patient’s preferred antifungal medication can be prescribed for women who are prone to infections, sexually active, or who may be receiving antibiotics for other reasons (including doxycycline for malaria chemoprophylaxis)
- Occupational exposure to HIV (Chapter 9, Health Care Workers , Including Public Health Researchers and Laboratorians)
- Malaria self-treatment (see Chapter 4 , Malaria)
In sum, travelers should be encouraged to carry a travel health kit with prescription and nonprescription medications. Providers should review medication lists for possible drug interactions. More detailed information for providers and travelers is given in Chapter 6, Travel Health Kits; supplementary travel health kit information for travelers with specific needs is given in Chapter 5.
Box 2-1. Summary of sexual health recommendations for travelers
Before travel.
- Obtain recommended vaccinations, including those that protect against sexually transmitted infections.
- Get recommended tests for HIV and treatable STDs. Be aware of STD symptoms in case any develop.
- Check condom packaging and expiration dates.
- Review local laws about sexual practices and obtain contact information for medical and law enforcement services.
- If pregnant or considering pregnancy, review whether Zika virus infection is a risk at destination.
During Travel
- Use good judgment in choosing consensual adult sex partners.
- Use condoms consistently and correctly to decrease the risk of HIV and STDs.
- If indicated, be prepared to start taking medications for HIV postexposure prophylaxis or unintended pregnancy within 72 hours after a high-risk sexual encounter.
- Never engage in sex with a minor (<18 years old), child pornography, or trafficking activities in any country.
- Report suspicious activity to US and local authorities as soon as it occurs.
After Travel
- To avoid exposing sex partners at home, see a clinician to get recommended tests for HIV and treatable STDs.
Bibliography
- Freedman DO, Chen LH, Kozarsky P. Medical considerations before travel. N Engl J Med. 2016 July 21;375:247–60.
- Hatz CFR, Chen LH. Pre-travel consultation. In: Keystone JS, Freedman DO, Kozarsky PE, Connor BA, Nothdurft HD, editors. Travel Medicine. 3rd ed. Philadelphia: Saunders Elsevier; 2013. pp. 31–6.
- Hill DR, Ericsson CD, Pearson RD, Keystone JS, Freedman DO, Kozarsky PE, et al. The practice of travel medicine: guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2006 Dec 15;43(12):1499–539.
- International Society of Travel Medicine. Body of knowledge for the practice of travel medicine—2012. Atlanta: International Society of Travel Medicine; 2012 [cited 2018 Feb 18]. Available from: www.istm.org/bodyofknowledge .
- Kozarsky PE, Steffen R. Travel medicine education—what are the needs? J Travel Med. 2016 Jul 4;23(5).
- Leder K, Chen LH, Wilson ME. Aggregate travel vs. single trip assessment: arguments for cumulative risk analysis. Vaccine. 2012 Mar 28;30(15):2600–4. [PMID:22234265]
- Leder K, Torresi J, Libman MD, Cramer JP, Castelli F, Schlagenhauf P, et al. GeoSentinel surveillance of illness in returned travelers, 2007–2011. Ann Intern Med. 2013 Mar 19;158(6):456–68. [PMID:23552375]
- Schwartz BS, Larocque RC, Ryan ET. In the clinic: travel medicine. Ann Intern Med. 2012 Jun 5;156(11):ITC6:1–16. [PMID:22665823]
- Steffen R, Behrens RH, Hill RD, Greenaway C, Leder K. Vaccine-preventable travel health risks: what is the evidence—what are the gaps? J Travel Med. 2015;22(1):1–12.
- Riddle MS, Connor BA, Beeching NJ, DuPont HL, Hamer DH, Kozarsky P, et al. Guidelines for the prevention and treatment of travelers’ diarrhea: a graded expert panel report. J Travel Med. 2017 Apr 1;24(suppl_1):S57–S74.
Lin H. Chen, Natasha S. Hochberg
1. Download the Relief Central app by Unbound Medicine
2. Select Try/Buy and follow instructions to begin your free 30-day trial

Want to regain access to Relief Central?
Renew my subscription
Not now - I'd like more time to decide
Log in to Relief Central
Forgot your password, forgot your username, contact support.
- unboundmedicine.com/support
- [email protected]
- 610-627-9090 (Monday - Friday, 9 AM - 5 PM EST.)

IMAGES
VIDEO
COMMENTS
CDC Yellow Book 2024. Author (s): Lin Hwei Chen, Natasha Hochberg. The pretravel consultation offers a dedicated time to prepare travelers for health concerns that might arise during their trips. During the pretravel consultation, clinicians can conduct a risk assessment for each traveler, communicate risk by sharing information about potential ...
Assessment: Upcoming trip: dates, itinerary, reason for trip, travel style, special activities (e.g., mountain climbing, diving, rafting) Medical history: medications ...
The increase in travel and travel medicine knowledge over the past 30 years makes pretravel counseling an essential part of comprehensive family medicine. Effective counseling begins with ...
Welcome to Pre-travel PREP! Pre-Travel PREP is a free clinical tool that guides you through preparing a US traveler for a safe and healthy international trip. It was developed to act as an interactive Yellow Book (Health Information for International Travel) , and its output is based on the recommendations of the US Centers for Disease Control ...
Please fill out and submit this form prior to your appointment with the Travel Health Consultant Pharmacist name Contact Information Your travel history ¨ New to travel ¨ If previous trips, w hich C anadian regions or international countries ... pre-travel-assessment-form_2022 Author: Jensen, Karen
Highlights. Learn about CDC's Traveler Genomic Surveillance Program that detects new COVID-19 variants entering the country. Sign up to get travel notices, clinical updates, & healthy travel tips. CDC Travelers' Health Branch provides updated travel information, notices, and vaccine requirements to inform international travelers and provide ...
Perform an individual risk assessment. 2. Communicate to the traveler anticipated health risks. 3. Provide risk management measures, including immunizations, malaria prophylaxis, and other medications as indicated. ... Travel health advice should be personalized, highlighting the likely exposures and also reminding the traveler of. ubiquitous ...
The pre-travel consultation is a risk-based assessment process that provides a guide to prioritizing and customizing pre-travel health care to the traveler's itinerary, risks, and needs. The goal of the pre-travel consultation is the effective and efficient preparation of travelers with the appropriate counseling, vaccinations, and medications ...
The Travel Health Program offers pre-travel assessment, counseling, and immunizations. The Tropical Medicine Program offers post-travel evaluation and treatment of illness. Clinical Care Providers. Noreen A. Hynes, MD, MPH, DTM&H. ...
The recruitment method (convenience sampling from three pre-travel centres) may also have led to selection bias that favours people who are more aware and focused on risk assessment and management. Finally, the questionnaire was administered in a paper format and by telephone before and after the trip, respectively, leading to potential ...
Currently, over a billion people travel annually, with over 65 million visits made from the UK. Seeking pre-travel advice should be an essential part of any trip for a traveller. The key elements of pre-travel advice are health risk assessment, health promotion and risk management; this involves advice on prevention of malaria, travellers ...
Pre-Travel Health Assessment Form. Immunization History. Travel vaccine History - Have you ever received the following immunizations? Are your regular immunizations . up-to-date? Yes No Not sure When was the date of your last tetanus shot? Date (dd/mm/yyyy): Not sure Have you had the: Annual flu vaccine Yes
Pre-travel health assessments aim to promote risk reduction through preventive measures and safe behavior, including ensuring travelers are up-to-date with their immunizations. However, studies assessing pre-travel health-seeking practices from a variety of medical and non-medical sources and vaccine uptake prior to travel to both developing and developed countries within the Asia-Pacific ...
Pre-Travel Health Assessment Form Your personal details Name: Date of birth (dd/mm/yyyy): _____ Address: (street, city, postal code) Male Female ... Please let us know your primary concerns with your trip or this travel health assessment (check all that apply) Getting sick while away . Travellers' diarrhea . Safety and efficacy of vaccines .
RCN TRAVEL HEALTH NURSING: CAREER AND COMPETENCE DEVELOPMENT. ... for example, the pre-travel risk assessment and risk management which underpin the pre-travel consultation and form the keystone of travel medicine practice. Following a Nursing and Midwifery Council (NMC) Fitness to Practice case related to travel health advice, these forms were ...
Individuals with a pre-existing mental health disorder in the last year have been shown to score significantly higher on the COVID Stress Scales than those without . Travel may exacerbate or precipitate a variety of psychological disorders. ... This pandemic has further raised the importance of pre-travel risk assessment for business travellers ...
A pre-travel consultation is a medical appointment scheduled before a person departs for a trip. This is highly beneficial for those who are scheduled to go abroad for a vacation, a business trip, or for other travel reasons. During the consultation, the patient will undergo a health assessment to check whether he might be in need of additional ...
725-6908 211 Quarry Road, Suite 202 Palo Alto, CA 94304. S T A N F O R l) Tropical Medicine and Travelers' Health Clinic Palo Alto, CA 94034 Stanford Phone (650) 736-5700 Fax (650) 498-7873 Phone. Date of Bilth: Travel Form Affix Label here Name: Depa1tment/Group Sponsoring trip: Departure date: Date: AITival date at first destination.
The pretravel consultation offers a dedicated time to prepare travelers for the health concerns that might arise during their trips. The objectives of the pretravel consultation are to: Perform an individual risk assessment. Communicate to the traveler anticipated health risks.
International Health Regulations (IHR) were developed by the World Health Organization (WHO) to curb the trans-border spread of epidemics. To our knowledge, no airport-based studies have assessed travelers' health practices against a combination of diseases subject to IHR 2005. Therefore, we aimed to generate and describe the baseline travelers' pre-travel health practices towards Cholera ...
The pretravel consultation offers a dedicated time to prepare travelers for the health concerns that might arise during their trips. The objectives of the pretravel consultation are to: Perform an individual risk assessment. Communicate to the traveler anticipated health risks. Provide risk management measures, including immunizations, malaria ...
NSW Ministry of Health ABN 92 697 899 630 1 Reserve Rd St Leonards NSW 2065 Locked Mail Bag 2030 St Leonards NSW 1590 Tel. (02) 9391 9000 Fax. (02) 9391 9101 Website. www.health.nsw.gov.au Rabies risk in Timor-Leste Alert: Pre and Post Travel Assessment . Information for GPs and AMSs - please distribute to all medical and nursing staff