

This Is How Skipping Appointments & Not Seeing Your Doctor Can Impact A Pregnancy
Pregnancy can change your body and health in a myriad of ways, and of course, it's a complicated process for the baby you're carrying, too. Appropriate and affordable healthcare for women in our country is at the verge of being pulled, and if you're pregnant or trying to conceive, you might be especially concerned for what's to come. Can you have a healthy baby without seeing a doctor ? Some moms without insurance find this to be reality while some simply skip out on their ultrasounds and appointments. But is it safe?
According to Dr. Adrienne Zertuche , MD, MPH, OB-GYN and Georgia Maternal and Infant Health Research Group President, it is possible to have a healthy baby even if you do not get prenatal care, but, she notes, "I do not recommend skipping out on doctor’s visits or recommended labs and ultrasounds." Meeting with your obstetrician frequently throughout your pregnancy provides for close monitoring of the health of both you and your baby, Zertuche tells Romper. "Early detection of complications is absolutely vital to formulating a plan of care for high-risk pregnancies. These visits are also important because they give you a chance to hear general guidance, ask questions, and communicate your preferences regarding your birth experience."
So, what is prenatal care exactly? As the March of Dimes noted, prenatal care is medical care you get during pregnancy . At each visit, your healthcare provider checks on you and your growing baby, offers input on staying healthy, and answers any questions you might have regarding your pregnancy.
You can ask your provider anything — even personal things you might be embarrassed about. They will be there to support you in every way possible during your pregnancy and after.
Getting early and regular prenatal care can help you have a healthy pregnancy and a full-term baby, which gives your baby the right amount of time he needs in the womb to grow and develop. NPR noted that women without prenatal care are seven times more likely to give birth to premature babies , and five times more likely to have infants who pass away. The consequences are not only poor health, but also higher costs in the long run. The average medical cost for a baby with problems of prematurity is $79,000, compared to $1,000 for a healthy newborn. In fact, studies show that every dollar spent on prenatal care can result in a savings of $5 thereafter.
Prenatal care is extremely important during pregnancy, particularly in determining when there are health problems and treating those problems when possible, according to Fit Pregnancy . This care also minimizes risks and provides guidance, education, and structure so patients can be as healthy as possible.
However, it's also true that no doctor will be able to make you healthy — that's all on you. It’s something you have to make an effort to maintain within yourself for the sake of your own body and your baby's. Of course, not everyone has access to the same resources and support system, but you have to take what you have and do the best that you can.
Considering what you breathe, drink, and eat is also majorly impactful in sustaining a healthy body and pregnancy. Exercising regularly is essential for brain, heart, bone and immune-system health and, just as vital, is your mental health — sleep, low stress levels, and periods of meditation can all help to support a healthy pregnancy.
Dr. Boyd Cooper , MD and OB-GYN for over 50 years tells Romper, "Countless healthy babies are born all over the world, without any prenatal care. We are all here, and have been before modern technology. But, there are many babies that could be saved by having prenatal care, therefore, your chances of having a strong, healthy baby increases with prenatal care."
If nothing else, Boyd continues, the ability to at least understand if there is an issue can be determined prior to birth. When available and accessible, getting prenatal care during pregnancy is the better choice.
If you're unsure if you have access to appropriate medical care during your pregnancy, check with your state's health department. Most states offer programs to help women pay for prenatal care, and so do many social service organizations. You don't have to navigate this alone.
Check out Romper's new video series, Romper's Doula Diaries :
Check out the entire Romper's Doula Diaries series and other videos on Facebook and the Bustle app across Apple TV, Roku, and Amazon Fire TV.
- Trying to Conceive
- Signs & Symptoms
- Pregnancy Tests
- Fertility Testing
- Fertility Treatment
- Weeks & Trimesters
- Staying Healthy
- Preparing for Baby
- Complications & Concerns
- Pregnancy Loss
- Breastfeeding
- School-Aged Kids
- Raising Kids
- Personal Stories
- Everyday Wellness
- Safety & First Aid
- Immunizations
- Food & Nutrition
- Active Play
- Pregnancy Products
- Nursery & Sleep Products
- Nursing & Feeding Products
- Clothing & Accessories
- Toys & Gifts
- Ovulation Calculator
- Pregnancy Due Date Calculator
- How to Talk About Postpartum Depression
- Editorial Process
- Meet Our Review Board
How to Find Low-Cost or Free Prenatal Care
Jose Luis Pelaez Inc/Blend/Getty Images
Sometimes, pregnancy occurs and you are not ready. This can often mean the lack of quality prenatal care . This lack of prenatal care can be dangerous because you do not have anyone to help you figure out the ins and outs of pregnancy or to pick up on the rare serious complication. In essence, without prenatal care, you have no lifeguard.
Where to Find Affordable Care
Here are some places that you can look for locally to help you get prenatal care.
Affordable Care Act (ACA)
Also known as Obamacare, this law passed in 2010 includes prenatal care as a covered benefit for the vast majority of health insurance plans. This says that women who have health insurance will have free coverage for their prenatal care. If you don't have insurance, you may qualify for your state's version of Medicaid (see below).
The reason that this is now covered is that it falls under a blanket of preventative care. While the average cost of an uncomplicated birth can be over $4,000 in some cases, a birth with complications can be even more expensive. Providing good prenatal care can not only help lower the risks to the mother and the baby for the period of the pregnancy, but also offer benefits extending throughout their lifetime. This makes prenatal care a very wise investment.
Local Health Department
Your local health department will be able to tell you where a prenatal care clinic is run. They may have one that they run or can help you find free or reduced prices on prenatal care depending on your income level.
You can call 1-800-311-BABY (1-800-311-2229) to connect you to your local healthcare department. This information is also available in Spanish by calling 1-800-504-7081.
Local Medical School
If you live in an area with a medical school or have a bigger medical school in your state, even if it is not in your town, call their clinics. They often run clinics for prenatal care both at the medical school and in local towns within a certain distance.
These are staffed by trained and qualified doctors and midwives who are training residents (doctors who have graduated from medical school but are learning the specialty of obstetrics), midwives, and sometimes student doctors and nurses. Costs will vary depending on income.
Planned Parenthood
There are many cities that are serviced by Planned Parenthood. They do provide sliding scale prenatal care. This means it will be based on your ability to pay.
This is a sponsored program for women who do not have the money to pay for prenatal care. After the application process, you will be given a list of providers of care. This should include doctors and midwives in your area who have already agreed to take Medicaid.
They will provide you with the exact same medical care as a private pay or insurance-based providers. Check the blue pages of your phone book. The ACA expanded Medicaid to increase the number of women covered. It is important to note that not all states chose this expansion.
Other Resources
You may have local resources that are helpful for finding prenatal care . It may be that your religious family has a prenatal care provider who will work with you. Or perhaps you can make payment arrangements with a local midwife or doctor. Be upfront about your situation. Be truthful about what you can and can't afford.
Prenatal care is a comprehensive package of services. It includes a variety of prenatal screenings, testing, and monitoring. This is the safest way for you and your baby to progress through the pregnancy. You can make the most of your prenatal care by being prepared for your appointments .
Healthcare.gov. Preventative care benefits for women .
Moniz MH, Fendrick AM, Kolenic GE, Tilea A, Admon LK, Dalton VK. Out-of-pocket spending for maternity care among women with employer-based insurance, 2008-15 . Health Affairs. 2020;39(1). doi:10.1377/hlthaff.2019.00296
U.S. Department of Health and Human Services. Are there any health assistance programs for pregnant women, mothers, and children ?
McLeod AY, LaClair C, Kenyon T. Interdisciplinary prenatal group visits as a significant learning experience . J Grad Med Educ. 2011;3(3):372-375. doi:10.4300/JGME-D-10-00139.1
Planned Parenthood. Where can I get prenatal care?
Searing A, Cohen Ross D. Medicaid expansion fills gaps in maternal health coverage leading to healthier mothers and babies . Georgetown University Health Policy Institute, Center for Children and Families.
By Robin Elise Weiss, PhD, MPH Robin Elise Weiss, PhD, MPH is a professor, author, childbirth and postpartum educator, certified doula, and lactation counselor.
Find support
Many parents and parents-to-be face a world of unknowns, but they all want a healthy and strong start. That's where we come in. Explore a variety of topics and resources here.
- Community Stories
- Support In Your Area
- Compass by March of Dimes™
- Ovulation calculator
- Ovulation calendar
Ways to give
There are so many ways to support our research, education, advocacy and programs. Give today to ensure that every family is healthy and strong now and tomorrow.
- Give with Donor-Advised Fund
- Stock and IRA Charitable Rollovers
- March for Babies
- Fundraise Your Way
- March of Dimes Innovation Fund
- Roosevelt Society
- Legacy Giving: Wills, Trusts, and Estates
Addressing the maternal and infant health crisis is not straightforward with one solution. It takes strategic and collaborative efforts in different areas to ultimately benefit thousands of moms, babies and families every day. Discover more here.
- ICBD Conference
- Mom and Baby Action Network
- Policy & Advocacy
- Public Health Data Reports
- For Health Professionals
- NICU Initiatives
- NICU Family Support
We're committed to ending preventable maternal health risks and death, ending preventable preterm birth and infant death and closing the health equity gap for all families. Learn more about our legacy and impact here.
- Accomplishments
- Annual Reports
- In Your Area Find opportunities to get involved
- Volunteer Help us by being on the frontlines
- Advocate Join us in the fight of all moms and babies
- Partner Collaborate to make a difference for families
- Donate Help us by making a donation
- Careers Discover your chance to make a big impact
- See all ways to Get Involved
Prenatal care checkups
Prenatal care is medical care you get during pregnancy. at each prenatal care visit, your health care provider checks on you and your growing baby., call your provider to schedule your first prenatal care checkup as soon as you know you’re pregnant., getting early and regular prenatal care can help you have a healthy pregnancy and a full-term baby., go to all your prenatal care checkups, even if you’re feeling fine..
What is prenatal care and why is it important?
Prenatal care is medical care you get during pregnancy. At each visit, your health care provider checks on you and your growing baby. Call your provider and go for your first prenatal care checkup as soon as you know you’re pregnant. And go to all your prenatal care checkups, even if you’re feeling fine.
Getting early and regular prenatal care can help you have a healthy pregnancy and a full-term baby. Full term means your baby is born between 39 weeks (1 week before your due date) and 40 weeks, 6 days (1 week after your due date). Being born full term gives your baby the right amount of time he needs in the womb to grow and develop.
Don’t be afraid to talk to your provider about personal things. Your provider needs to know all about you so she can give you and your baby the best care. She asks lots of questions about you, your partner and your families. Your medical information and anything you tell her are confidential. This means she can’t share them with anyone without your permission. So don’t be afraid to tell her about things that may be uncomfortable or embarrassing, like if your partner hurts or scares you or if you smoke , drink alcohol , use street drugs or abuse prescription drugs .
Who can you go to for prenatal care?
You can get prenatal care from different kinds of providers:
- An obstetrician/gynecologist (also called OB/GYN) is a doctor who has education and training to take care of pregnant women and deliver babies. The American College of Obstetricians and Gynecologists can help you find an OB in your area.
- A family practice doctor (also called a family physician) is a doctor who can take care of every member of your family. This doctor can take care of you before, during and after pregnancy. The American Board of Family Medicine can help you find a family practice doctor in your area.
- A maternal-fetal medicine (also called MFM) specialist is an OB with education and training to take care of women who have high-risk pregnancies. If you have health conditions that may cause problems during pregnancy, your provider may want you to see a MFM specialist. The Society for Maternal-Fetal Medicine can help you find a specialist in your area.
- A certified nurse-midwife (also called CNM) is a nurse with education and training to take care of women of all ages, including pregnant women. The American College of Nurse-Midwives can help you find a CNM in your area.
- A family nurse practitioner (also called FNP) or a women’s health nurse practitioner (also called WHNP). A FNP is a nurse with education and training to take care of every member of your family. A WHNP is a nurse with education and training to take care of women of all ages, including pregnant women. The American Association of Nurse Practitioners can help you find these kinds of nurse practitioners in your area.
Think about these things to help you choose a provider:
- Is the provider licensed and board certified to take care of you during pregnancy, labor and birth? Licensed means the provider can legally practice medicine in a state. To have a license, a provider has to have a certain amount of education and training and pass certain tests to make sure he can safely take care of patients. Board certified means that a provider has had extra training in a certain area (called a specialty).
- Is the provider covered by your health insurance ?
- Have you heard good things about the provider? Is she recommended by your friends or family? How does your partner feel about her as your prenatal care provider?
- Would you rather see a man or a woman provider? How old to you want the provider to be? Does he explain things clearly?
- Is the office easy to get to? Do the office hours fit into your schedule? Is the office staff friendly and helpful?
- Who takes care of phone calls during office hours? Who handles them after hours or in an emergency? Do you have to pay if your provider spends time with you on the phone?
- Is the provider in group practice? If yes, will you always see your provider at prenatal care checkups? Or will you see other providers in the practice? Who will deliver your baby if your provider’s not available when you go into labor?
- What hospital or birthing center does the provider use? What do you know about it? Is it easy for you to get to?
How often do you go for prenatal care checkups?
Most pregnant women can follow a schedule like this:
- Weeks 4 to 28 of pregnancy. Go for one checkup every 4 weeks (once a month).
- Weeks 28 to 36 of pregnancy. Go for one checkup every 2 weeks (twice a month).
- Weeks 36 to 41 of pregnancy. Go for one checkup every week (once a week).
If you have complications during pregnancy, your provider may want to see you more often.
Your partner or support person (a friend or someone from your family) is welcome at your prenatal checkups.
How can you get ready for your first prenatal care checkup?
Be ready to talk with your provider about:
- The first day of your last menstrual period (also called LMP). Your provider can use this to help find out your baby’s due date .
- Health conditions you have, like depression , diabetes , high blood pressure , and not being at a healthy weight . Conditions like these can cause problems during pregnancy. Tell your provider about your family health history . This is a record of any health conditions and treatments that you, your partner and everyone in your families have had. Use the March of Dimes Family Health History Form and share it with your provider. If you have a record of your vaccinations , take it to your checkup. A vaccination is a shot that contains a vaccine that helps protect you from certain harmful infections.
- Medicines you take, including prescription medicine , over-the-counter medicine, supplements and herbal products . Some medicines can hurt your baby if you take them during pregnancy, so you may need to stop taking it or switch to another medicine. Don’t stop or start taking any medicine without talking to your provider first. And tell your provider if you’re allergic to any medicine. You may be allergic to a medicine if it makes you sneeze, itch, get a rash or have trouble breathing when you take it.
- Your pregnancy history. Tell your provider if you’ve been pregnant before or if you’ve had trouble getting pregnant. Tell her if you’ve had any pregnancy complications or if you’ve had a premature baby (a baby born before 37 weeks of pregnancy), a miscarriage or stillbirth . Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy. Stillbirth is when a baby dies in the womb after 20 weeks of pregnancy.
- Smoking, drinking alcohol, using street drugs and abusing prescription drugs. All of these can hurt your baby. Alcohol includes beer, wine and liquor. Street drugs are illegal to use, like heroin and cocaine. Abusing prescription drugs means you use them differently than your provider tells you to. This means you take more than your provider says you can take, you take it with alcohol or other drugs or you use someone else’s prescription drugs.
- Stress you feel. Stress is worry, strain or pressure that you feel in response to things that happen in your life. Talk to your provide about ways to deal with and reduce your stress. High levels of stress can cause complications during pregnancy.
- Your safety at home and work. Tell your provider about chemicals you use at home or work and about what kind of job you have. If you’re worried about abuse during pregnancy and ask about ways you can stay healthy and safe at home and work.
What happens at your first prenatal care checkup?
Your first checkup is usually the longest because your provider asks you lots of questions about your health. At your first prenatal care checkup, your provider:
- Gives you a physical exam and checks your overall health. Your provider checks your weight and height to figure out how much weight you should gain during pregnancy.
- Checks your blood, blood pressure and urine. Blood tests can tell your provider if you have certain infections, like syphilis , hepatitis B and HIV. Your provider also uses a blood test to find out your blood type and Rh factor and to check for anemia. Anemia is when you don't have enough healthy red blood cells to carry oxygen to the rest of your body. Rh factor is a protein that most people have on their red blood cells. If you don’t have it and your baby does, it can cause Rh disease in your baby. Treatment during pregnancy can prevent Rh disease. Blood pressure and urine tests can help your provider diagnose a serious condition called preeclampsia . This is a kind of high blood pressure that can happen during pregnancy. Having too much protein in your urine may be a sign of preeclampsia. Urine tests also can tell your provider if you have a kidney or bladder infection or other conditions, like diabetes.
- Gives you a pelvic exam and a Pap smear. Your provider checks the pelvic organs (pelvis and womb) to make sure they’re healthy. For the Pap smear, your provider collects cells from your cervix to check for cancer and for infections, like chlamydia and gonorrhea. The cervix is the opening to the uterus (womb) that sits at the top of the vagina.
- May give you vaccinations, like a flu shot. It’s safe to get a flu shot any time during pregnancy. But some vaccinations are best at certain times and some aren’t recommended during pregnancy. Talk to your provider about what’s best and safe for you and your baby.
- Tells you your due date. Your provider usually uses your LMP to figure out your due date. But you may get an early ultrasound to confirm that you’re pregnant and help your provider figure out your baby’s age. An ultrasound uses sound waves and a computer screen to show a picture of your baby inside the womb.
- Prescribes a prenatal vitamin. This is a multivitamin made for pregnant women. Your prenatal vitamin should have 600 micrograms of folic acid in it. Folic acid is a vitamin that every cell in your body needs for healthy growth and development. If you take it before pregnancy and during early pregnancy, it can help protect your baby from birth defects of the brain and spine called neural tube defects (also called NTDs), and birth defects of the mouth called cleft lip and palate .
- Talks to you about prenatal tests. These are medical tests you get during pregnancy. They help your provider find out how you and your baby are doing. You may want to have certain tests only if you have certain problems or if you’re at high risk of having a baby with a genetic or chromosomal condition , like Down syndrome . If your provider thinks you’re at risk for having a baby with one of these conditions, he may recommend that you see a genetic counselor . This person has training to help you understand about genes, birth defects and other medical conditions that run in families, and how they can affect your health and your baby’s health.
What happens at later prenatal care checkups?
Later prenatal care checkups usually are shorter than the first one. At your checkups, tell your provider how you’re feeling. There’s a lot going on inside your body during pregnancy. Your provider can help you understand what’s happening and help you feel better if you’re not feeling well. Between visits, write down questions you have and ask them at your next checkup.
At later prenatal care checkups, your health care provider:
- Checks your weight and blood pressure. You also may get urine and blood tests.
- Checks your baby’s heartbeat. This happens after about 10 to 12 weeks of pregnancy. You can listen, too!
- Measures your belly to check your baby’s growth. Your provider starts doing this at about 20 weeks of pregnancy. Later in pregnancy, she also feels your belly to check your baby’s position in the womb.
- Gives you certain prenatal tests to check you and your baby. For example, most women get an ultrasound at 18 to 20 weeks of pregnancy. You may be able to tell if your baby’s a boy or a girl from this ultrasound, so be sure to tell your provider if you don’t want to know! Later in pregnancy, your provider may use ultrasound to check the amount of amniotic fluid around your baby in the womb. Between 24 and 28 weeks, you get a glucose screening test to see if you may have gestational diabetes . This is a kind of diabetes that some women get during pregnancy. And at 35 to 37 weeks, you get a test to check for group B strep . This is an infection you can pass to your baby.
- Asks you about your baby’s movement in the womb. If it’s your first pregnancy, you may feel your baby move by about 20 weeks. If you’ve been pregnant before, you may feel your baby move sooner. Your provider may ask you to do kick counts to keep track of how often your baby moves.
- Gives you a Tdap vaccination at 27 to 36 weeks of pregnancy. This vaccination protects both you and your baby against pertussis (also called whooping cough). Pertussis spreads easily and is dangerous for a baby.
- Does a pelvic exam . Your provider may check for changes in your cervix as you get close to your due date.
How can you get free or low-cost prenatal care?
If you don't have health insurance or can't afford prenatal care, find out about free or low-cost prenatal care services in your community:
- Call (800) 311-BABY [(800) 311-2229]. For information in Spanish, call (800) 504-7081.
- Visit healthcare.gov to find a community health center near you. Community health centers can provide low-cost prenatal care.
Last reviewed: June, 2017
Join our email newsletter to find out how our community is helping families.


An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- U.S. Department of Health & Human Services

Call the OWH HELPLINE: 1-800-994-9662 9 a.m. — 6 p.m. ET, Monday — Friday OWH and the OWH helpline do not see patients and are unable to: diagnose your medical condition; provide treatment; prescribe medication; or refer you to specialists. The OWH helpline is a resource line. The OWH helpline does not provide medical advice.
Please call 911 or go to the nearest emergency room if you are experiencing a medical emergency.
Prenatal care
Prenatal care is the health care you get while you are pregnant.
What is prenatal care?
Prenatal care is the health care you get while you are pregnant. Take care of yourself and your baby by:
- Getting early prenatal care. If you know you're pregnant, or think you might be, call your doctor to schedule a visit.
- Getting regular prenatal care. Your doctor will schedule you for many checkups over the course of your pregnancy. Don't miss any — they are all important.
- Following your doctor's advice.
Why do I need prenatal care?
Prenatal care can help keep you and your baby healthy. Babies of mothers who do not get prenatal care are three times more likely to have a low birth weight and five times more likely to die than those born to mothers who do get care.
Doctors can spot health problems early when they see mothers regularly. This allows doctors to treat them early. Early treatment can cure many problems and prevent others. Doctors also can talk to pregnant women about things they can do to give their unborn babies a healthy start to life.
I am thinking about getting pregnant. How can I take care of myself?
You should start taking care of yourself before you start trying to get pregnant. This is called preconception health. It means knowing how health conditions and risk factors could affect you or your unborn baby if you become pregnant. For example, some foods, habits, and medicines can harm your baby — even before he or she is conceived. Some health problems also can affect pregnancy.
Talk to your doctor before pregnancy to learn what you can do to prepare your body. Women should prepare for pregnancy before becoming sexually active. Ideally, women should give themselves at least 3 months to prepare before getting pregnant.
The five most important things you can do before becoming pregnant are:
- Take 400 to 800 micrograms (400 to 800 mcg or 0.4 to 0.8 mg) of folic acid every day for at least 3 months before getting pregnant to lower your risk of some birth defects of the brain and spine. You can get folic acid from some foods. But it's hard to get all the folic acid you need from foods alone. Taking a vitamin with folic acid is the best and easiest way to be sure you're getting enough.
- Stop smoking and drinking alcohol. Ask your doctor for help.
- If you have a medical condition, be sure it is under control. Some conditions include asthma , diabetes , depression , high blood pressure , obesity , thyroid disease, or epilepsy . Be sure your vaccinations are up to date.
- Talk to your doctor about any over-the-counter and prescription medicines you are using. These include dietary or herbal supplements. Some medicines are not safe during pregnancy. At the same time, stopping medicines you need also can be harmful.
- Avoid contact with toxic substances or materials at work and at home that could be harmful. Stay away from chemicals and cat or rodent feces.
I'm pregnant. What should I do — or not do — to take care of myself and my unborn baby?
Follow these do's and don'ts to take care of yourself and the precious life growing inside you:
Health care do's and don'ts
- Get early and regular prenatal care. Whether this is your first pregnancy or third, health care is extremely important. Your doctor will check to make sure you and the baby are healthy at each visit. If there are any problems, early action will help you and the baby.
- Take a multivitamin or prenatal vitamin with 400 to 800 micrograms (400 to 800 mcg or 0.4 to 0.8 mg) of folic acid every day. Folic acid is most important in the early stages of pregnancy, but you should continue taking folic acid throughout pregnancy.
- Ask your doctor before stopping any medicines or starting any new medicines. Some medicines are not safe during pregnancy. Keep in mind that even over-the-counter medicines and herbal products may cause side effects or other problems. But not using medicines you need could also be harmful.
- Avoid x-rays. If you must have dental work or diagnostic tests, tell your dentist or doctor that you are pregnant so that extra care can be taken.
- Get a flu shot. Pregnant women can get very sick from the flu and may need hospital care.
Food do's and don'ts
- Eat a variety of healthy foods. Choose fruits, vegetables, whole grains, calcium-rich foods, and foods low in saturated fat. Also, make sure to drink plenty of fluids, especially water.
- Get all the nutrients you need each day, including iron. Getting enough iron prevents you from getting anemia, which is linked to preterm birth and low birth weight . Eating a variety of healthy foods will help you get the nutrients your baby needs. But ask your doctor if you need to take a daily prenatal vitamin or iron supplement to be sure you are getting enough.
- Protect yourself and your baby from food-borne illnesses, including toxoplasmosis (TOK-soh-plaz-MOH-suhss) and listeria (lih-STEER-ee-uh). Wash fruits and vegetables before eating. Don't eat uncooked or undercooked meats or fish. Always handle, clean, cook, eat, and store foods properly.
- Don't eat fish with lots of mercury, including swordfish, king mackerel, shark, and tilefish.
Lifestyle do's and don'ts
- Gain a healthy amount of weight. Your doctor can tell you how much weight gain you should aim for during pregnancy.
- Don't smoke, drink alcohol, or use drugs. These can cause long-term harm or death to your baby. Ask your doctor for help quitting.
- Unless your doctor tells you not to, try to get at least 2 hours and 30 minutes of moderate-intensity aerobic activity a week. It's best to spread out your workouts throughout the week. If you worked out regularly before pregnancy, you can keep up your activity level as long as your health doesn't change and you talk to your doctor about your activity level throughout your pregnancy. Learn more about how to have a fit pregnancy .
- Don't take very hot baths or use hot tubs or saunas.
- Get plenty of sleep and find ways to control stress.
- Get informed. Read books, watch videos, go to a childbirth class, and talk with moms you know.
- Ask your doctor about childbirth education classes for you and your partner. Classes can help you prepare for the birth of your baby.
Environmental do's and don'ts
- Stay away from chemicals like insecticides , solvents (like some cleaners or paint thinners), lead, mercury, and paint (including paint fumes). Not all products have pregnancy warnings on their labels. If you're unsure if a product is safe, ask your doctor before using it. Talk to your doctor if you are worried that chemicals used in your workplace might be harmful.
- If you have a cat, ask your doctor about toxoplasmosis . This infection is caused by a parasite sometimes found in cat feces. If not treated toxoplasmosis can cause birth defects. You can lower your risk of by avoiding cat litter and wearing gloves when gardening.
- Avoid contact with rodents, including pet rodents, and with their urine, droppings, or nesting material. Rodents can carry a virus that can be harmful or even deadly to your unborn baby.
- Take steps to avoid illness, such as washing hands frequently.
- Stay away from secondhand smoke.
I don't want to get pregnant right now. Should I still take folic acid every day?
Yes! Birth defects of the brain and spine happen in the very early stages of pregnancy, often before a woman knows she is pregnant. By the time she finds out she is pregnant, it might be too late to prevent those birth defects. Also, half of all pregnancies in the United States are not planned. For these reasons, all women who are able to get pregnant need 400 to 800 mcg of folic acid every day.
How often should I see my doctor during pregnancy?
Your doctor will give you a schedule of all the doctor's visits you should have while pregnant. Most experts suggest you see your doctor:
- About once each month for weeks 4 through 28
- Twice a month for weeks 28 through 36
- Weekly for weeks 36 to birth
If you are older than 35 or your pregnancy is high risk, you'll probably see your doctor more often.
What happens during prenatal visits?
During the first prenatal visit, you can expect your doctor to:
- Ask about your health history including diseases, operations, or prior pregnancies
- Ask about your family's health history
- Do a complete physical exam, including a pelvic exam and Pap test
- Take your blood and urine for lab work
- Check your blood pressure, height, and weight
- Calculate your due date
- Answer your questions
At the first visit, you should ask questions and discuss any issues related to your pregnancy. Find out all you can about how to stay healthy.
Later prenatal visits will probably be shorter. Your doctor will check on your health and make sure the baby is growing as expected. Most prenatal visits will include:
- Checking your blood pressure
- Measuring your weight gain
- Measuring your abdomen to check your baby's growth (once you begin to show)
- Checking the baby's heart rate
While you're pregnant, you also will have some routine tests. Some tests are suggested for all women, such as blood work to check for anemia, your blood type, HIV, and other factors. Other tests might be offered based on your age, personal or family health history, your ethnic background, or the results of routine tests you have had. Visit the pregnancy section of our website for more details on prenatal care and tests .
I am in my late 30s and I want to get pregnant. Should I do anything special?
As you age, you have an increasing chance of having a baby born with a birth defect. Yet most women in their late 30s and early 40s have healthy babies. See your doctor regularly before you even start trying to get pregnant. She will be able to help you prepare your body for pregnancy. She will also be able to tell you about how age can affect pregnancy.
During your pregnancy, seeing your doctor regularly is very important. Because of your age, your doctor will probably suggest some extra tests to check on your baby's health.
More and more women are waiting until they are in their 30s and 40s to have children. While many women of this age have no problems getting pregnant, fertility does decline with age. Women over 40 who don't get pregnant after six months of trying should see their doctors for a fertility evaluation.
Experts define infertility as the inability to become pregnant after trying for one year. If a woman keeps having miscarriages, it's also called infertility. If you think you or your partner may be infertile, talk to your doctor. Doctors are able to help many infertile couples go on to have healthy babies.
Where can I go to get free or reduced-cost prenatal care?
Women in every state can get help to pay for medical care during their pregnancies. This prenatal care can help you have a healthy baby. Every state in the United States has a program to help. Programs give medical care, information, advice, and other services important for a healthy pregnancy.
To find out about the program in your state:
- Call 800-311-BABY (800-311-2229). This toll-free telephone number will connect you to the Health Department in your area code.
- For information in Spanish, call 800-504-7081.
- Contact your local Health Department.
Did we answer your question about prenatal care?
For more information about prenatal care, call womenshealth.gov at 800-994-9662 (TDD: 888-220-5446) or contact the following organizations:
- American College of Obstetricians and Gynecologists Phone: 202-638-5577
- American Pregnancy Association Phone: 972-550-0140
- Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, HHS Phone: 800-370-2943 (TDD: 888-320-6942)
- March of Dimes Phone: 914-997-4488
- National Center on Birth Defects and Developmental Disabilities, CDC, HHS Phone: 800-232-4636 (TDD: 888-232-6348)
- John W. Schmitt, M.D., Associate Professor of Clinical Obstetrics and Gynecology, University of Virginia Medical School
- HHS Non-Discrimination Notice
- Language Assistance Available
- Accessibility
- Privacy Policy
- Disclaimers
- Freedom of Information Act (FOIA)
- Use Our Content
- Vulnerability Disclosure Policy
- Kreyòl Ayisyen
A federal government website managed by the Office on Women's Health in the Office of the Assistant Secretary for Health at the U.S. Department of Health and Human Services.
1101 Wootton Pkwy, Rockville, MD 20852 1-800-994-9662 • Monday through Friday, 9 a.m. to 6 p.m. ET (closed on federal holidays).

Appointments at Mayo Clinic
- Pregnancy week by week
Prenatal care: 1st trimester visits
Pregnancy and prenatal care go hand in hand. During the first trimester, prenatal care includes blood tests, a physical exam, conversations about lifestyle and more.
Prenatal care is an important part of a healthy pregnancy. Whether you choose a family physician, obstetrician, midwife or group prenatal care, here's what to expect during the first few prenatal appointments.
The 1st visit
When you find out you're pregnant, make your first prenatal appointment. Set aside time for the first visit to go over your medical history and talk about any risk factors for pregnancy problems that you may have.
Medical history
Your health care provider might ask about:
- Your menstrual cycle, gynecological history and any past pregnancies
- Your personal and family medical history
- Exposure to anything that could be toxic
- Medications you take, including prescription and over-the-counter medications, vitamins or supplements
- Your lifestyle, including your use of tobacco, alcohol, caffeine and recreational drugs
- Travel to areas where malaria, tuberculosis, Zika virus, mpox — also called monkeypox — or other infectious diseases are common
Share information about sensitive issues, such as domestic abuse or past drug use, too. This will help your health care provider take the best care of you — and your baby.
Your due date is not a prediction of when you will have your baby. It's simply the date that you will be 40 weeks pregnant. Few people give birth on their due dates. Still, establishing your due date — or estimated date of delivery — is important. It allows your health care provider to monitor your baby's growth and the progress of your pregnancy. Your due date also helps with scheduling tests and procedures, so they are done at the right time.
To estimate your due date, your health care provider will use the date your last period started, add seven days and count back three months. The due date will be about 40 weeks from the first day of your last period. Your health care provider can use a fetal ultrasound to help confirm the date. Typically, if the due date calculated with your last period and the due date calculated with an early ultrasound differ by more than seven days, the ultrasound is used to set the due date.
Physical exam
To find out how much weight you need to gain for a healthy pregnancy, your health care provider will measure your weight and height and calculate your body mass index.
Your health care provider might do a physical exam, including a breast exam and a pelvic exam. You might need a Pap test, depending on how long it's been since your last Pap test. Depending on your situation, you may need exams of your heart, lungs and thyroid.
At your first prenatal visit, blood tests might be done to:
- Check your blood type. This includes your Rh status. Rh factor is an inherited trait that refers to a protein found on the surface of red blood cells. Your pregnancy might need special care if you're Rh negative and your baby's father is Rh positive.
- Measure your hemoglobin. Hemoglobin is an iron-rich protein found in red blood cells that allows the cells to carry oxygen from your lungs to other parts of your body. Hemoglobin also carries carbon dioxide from other parts of your body to your lungs so that it can be exhaled. Low hemoglobin or a low level of red blood cells is a sign of anemia. Anemia can make you feel very tired, and it may affect your pregnancy.
- Check immunity to certain infections. This typically includes rubella and chickenpox (varicella) — unless proof of vaccination or natural immunity is documented in your medical history.
- Detect exposure to other infections. Your health care provider will suggest blood tests to detect infections such as hepatitis B, syphilis, gonorrhea, chlamydia and HIV , the virus that causes AIDS . A urine sample might also be tested for signs of a bladder or urinary tract infection.
Tests for fetal concerns
Prenatal tests can provide valuable information about your baby's health. Your health care provider will typically offer a variety of prenatal genetic screening tests. They may include ultrasound or blood tests to check for certain fetal genetic problems, such as Down syndrome.
Lifestyle issues
Your health care provider might discuss the importance of nutrition and prenatal vitamins. Ask about exercise, sex, dental care, vaccinations and travel during pregnancy, as well as other lifestyle issues. You might also talk about your work environment and the use of medications during pregnancy. If you smoke, ask your health care provider for suggestions to help you quit.
Discomforts of pregnancy
You might notice changes in your body early in your pregnancy. Your breasts might be tender and swollen. Nausea with or without vomiting (morning sickness) is also common. Talk to your health care provider if your morning sickness is severe.
Other 1st trimester visits
Your next prenatal visits — often scheduled about every four weeks during the first trimester — might be shorter than the first. Near the end of the first trimester — by about 12 to 14 weeks of pregnancy — you might be able to hear your baby's heartbeat with a small device, called a Doppler, that bounces sound waves off your baby's heart. Your health care provider may offer a first trimester ultrasound, too.
Your prenatal appointments are an ideal time to discuss questions you have. During your first visit, find out how to reach your health care team between appointments in case concerns come up. Knowing help is available can offer peace of mind.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Lockwood CJ, et al. Prenatal care: Initial assessment. https://www.uptodate.com/contents/search. Accessed July 9, 2018.
- Prenatal care and tests. Office on Women's Health. https://www.womenshealth.gov/pregnancy/youre-pregnant-now-what/prenatal-care-and-tests. Accessed July 9, 2018.
- Cunningham FG, et al., eds. Prenatal care. In: Williams Obstetrics. 25th ed. New York, N.Y.: McGraw-Hill Education; 2018. https://www.accessmedicine.mhmedical.com. Accessed July 9, 2018.
- Lockwood CJ, et al. Prenatal care: Second and third trimesters. https://www.uptodate.com/contents/search. Accessed July 9, 2018.
- WHO recommendations on antenatal care for a positive pregnancy experience. World Health Organization. http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/anc-positive-pregnancy-experience/en/. Accessed July 9, 2018.
- Bastian LA, et al. Clinical manifestations and early diagnosis of pregnancy. https://www.uptodate.com/contents/search. Accessed July 9, 2018.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 1st trimester pregnancy
- Can birth control pills cause birth defects?
- Fetal development: The 1st trimester
- Implantation bleeding
- Nausea during pregnancy
- Pregnancy due date calculator
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Prenatal care 1st trimester visits
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
Can you get in trouble for not having prenatal care? What are the risks of no prenatal care? Find the answers to these questions about no prenatal care during pregnancy here.
- When to Start
- Due Date Calculator
- Prenatal Care Costs
No Prenatal Care During Pregnancy? What to Do Next
If you’re facing an unplanned pregnancy, the odds are that prenatal care has been the furthest thing from your mind. After all, you had no intentions to become pregnant — so why bother taking the time to frequently see your obstetrician outside of your yearly appointment?
However, you may be thinking differently now that you’ve found out you are pregnant. You may be extremely worried about having no prenatal care during pregnancy, however far along you may be in your own journey. During this time, you may have a few big questions:
Can you get in trouble for no prenatal care?
What should I be worried about when having a baby without prenatal care?
What are the effects of no prenatal care on my baby and me?
First off, take a deep breath. You’re not the only woman who has mistakenly avoided prenatal care during your pregnancy, and you won’t be the last. You have nothing to be ashamed of; if you didn’t expect yourself to be pregnant and didn’t know you were pregnant, how could you be expected to get prenatal care?
If you have been pregnant with no prenatal care up until this point, there is one thing you should know: You should make it your goal to obtain prenatal care as soon as possible to keep you and your unborn baby as healthy as possible. No matter how far along you are in your pregnancy, seeing a doctor should be your first step after reading this article.
In the meantime, you can find out more about insufficient prenatal care — and how it can affect your pregnancy — below.
Can You Get in Trouble for Not Having Prenatal Care?
It’s common knowledge that expectant mothers should receive prenatal care during their pregnancy. But, for some women, prenatal care isn’t readily accessible. Worried about the effects of insufficient prenatal care on themselves and their babies, they may also worry about other repercussions, asking:
Is it illegal to not get prenatal care?
There are no laws in the United States requiring expectant mothers to obtain prenatal care. Receiving medical care can be a highly personal decision, and the U.S. government treads lightly in forcing individuals to receive or not to receive certain care during their lives. So, legally, you cannot get in trouble for not having prenatal care — but that doesn’t mean that there aren’t other repercussions for you and your child should you refrain from receiving medical care.
No Prenatal Care: Consequences and Risks
There’s a reason why prenatal care is so encouraged by medical professionals around the world: It is incredibly important for protecting both expectant mother and child.
Having a baby without prenatal care opens you (and your baby) to all kinds of potential risks and complications. While there is always the chance that you and your baby will be perfectly fine with no prenatal care, there is a greater chance that something can go wrong, an underlying condition can go undetected or another health issue may befall you or your child.
Before you decide to refrain from receiving prenatal care at all, consider these risks of no prenatal care during pregnancy:
- Pregnancy complications , including conditions such as gestational diabetes, miscarriage, high blood pressure, preeclampsia and more
- Negative effects on the baby, such as preterm delivery or low birth weight
- Worsening of chronic conditions, such as diabetes, asthma and heart problems
- Ante- and post-partum depression and other mental illnesses
Perhaps the most stunning statistic of all? Babies whose mothers received no prenatal care are five times more likely to die than those whose mothers received regular prenatal care.
Clearly, a pregnancy without prenatal care is a dangerous pregnancy, even if you have no known health conditions or pre-determined pregnancy risks. Don’t take the risk: Find local prenatal care as early as possible in your pregnancy.
Finding Yourself Pregnant with No Prenatal Care Possibilities?
For some women, finding prenatal care seems like an impossible task. Perhaps they are not financially independent, do not have insurance , are not located near a medical professional or have other obstacles in their lives preventing them from obtaining care. For these women, a lack of prenatal care may seem like an unavoidable part of the next nine months.
However, obtaining prenatal care can be done; you do not have to continue your pregnancy without prenatal care or settle for poor prenatal care. It may just take a little more effort on your part.
Here are some tips for finding a prenatal care program that works for your needs:
- Search for low-cost, affordable prenatal care providers, such as local family-planning clinics or organizations like Planned Parenthood.
- Ask your friends and family and other medical professionals for recommendations in your area.
- Contact a local pregnancy counseling service for guidance and assistance.
- Consider placing your child for adoption, at which time you will receive free prenatal care .
Don’t be afraid to start your prenatal care protocol, no matter how far along you are in your pregnancy. A good doctor will not shame you but instead celebrate you for your brave decision .
We know that being pregnant with no prenatal care isn’t anyone’s ideal situation. But, with a little effort, you can still obtain the prenatal care you and your baby need for healthy pregnancy and start to your lives together.

- Pregnancy Classes

Your First Prenatal Visit
If you did not meet with your health care provider before you were pregnant, your first prenatal visit will generally be around 8 weeks after your LMP (last menstrual period ). If this applies to you, you should schedule a prenatal visit as soon as you know you are pregnant!
Even if you are not a first-time mother, prenatal visits are still important since every pregnancy is different. This initial visit will probably be one of the longest. It will be helpful if you arrive prepared with vital dates and information. This is also a good opportunity to bring a list of questions that you and your partner have about your pregnancy, prenatal care, and birth options.
What to Expect at Your First Pregnancy Appointment
Your doctor will ask for your medical history, including:.
- Medical and/or psychosocial problems
- Blood pressure, height, and weight
- Breast and cervical exam
- Date of your last menstrual period (an accurate LMP is helpful when determining gestational age and due date)
- Birth control methods
- History of abortions and/or miscarriages
- Hospitalizations
- Medications you are taking
- Medication allergies
- Your family’s medical history
Your healthcare provider will also perform a physical exam which will include a pap smear , cervical cultures, and possibly an ultrasound if there is a question about how far along you are or if you are experiencing any bleeding or cramping .
Blood will be drawn and several laboratory tests will also be done, including:
- Hemoglobin/ hematocrit
- Rh Factor and blood type (if Rh negative, rescreen at 26-28 weeks)
- Rubella screen
- Varicella or history of chickenpox, rubella, and hepatitis vaccine
- Cystic Fibrosis screen
- Hepatitis B surface antigen
- Tay Sach’s screen
- Sickle Cell prep screen
- Hemoglobin levels
- Hematocrit levels
- Specific tests depending on the patient, such as testing for tuberculosis and Hepatitis C
Your healthcare provider will probably want to discuss:
- Recommendations concerning dental care , cats, raw meat, fish, and gardening
- Fevers and medications
- Environmental hazards
- Travel limitations
- Miscarriage precautions
- Prenatal vitamins , supplements, herbs
- Diet , exercise , nutrition , weight gain
- Physician/ midwife rotation in the office
Possible questions to ask your provider during your prenatal appointment:
- Is there a nurse line that I can call if I have questions?
- If I experience bleeding or cramping, do I call you or your nurse?
- What do you consider an emergency?
- Will I need to change my habits regarding sex, exercise, nutrition?
- When will my next prenatal visit be scheduled?
- What type of testing do you recommend and when are they to be done? (In case you want to do research the tests to decide if you want them or not.)
If you have not yet discussed labor and delivery issues with your doctor, this is a good time. This helps reduce the chance of surprises when labor arrives. Some questions to ask include:
- What are your thoughts about natural childbirth ?
- What situations would warrant a Cesarean ?
- What situations would warrant an episiotomy ?
- How long past my expected due date will I be allowed to go before intervening?
- What is your policy on labor induction?
Want to Learn More?
- Sign up for our weekly email newsletter
- Bonding With Your Baby: Making the Most of the First Six Weeks
- 7 Common Discomforts of Pregnancy
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Leg Cramps During Pregnancy

Prenatal Vitamin Limits

Skin Changes During Pregnancy
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
When to schedule a prenatal visit
Prenatal visitation schedule, how should i prepare for a prenatal visit, what happens during prenatal visits, how can i make the most of my pregnancy appointments.
Make an appointment for your first prenatal visit once you're aware you are pregnant – when you receive a positive home pregnancy test, for example. Booking it around week 8 of pregnancy is typical.
You'll come back regularly in the weeks and months following that initial appointment. Most people have between 8 and 14 prenatal visits throughout the course of their pregnancy.
During this time, you'll see a lot of your healthcare practitioner. That's why it's so important to choose someone you like and trust. If you're not comfortable or satisfied with your provider after your first visit or visits, don't be afraid to find someone with whom you have a better connection.
Typically, a pregnant woman will visit their doctor, midwife , or nurse practitioner every four weeks during the first and second trimesters. In the third trimester, you'll be seen more often – usually every other week until 36 weeks, and then every week until the baby is born.
For more information on what happens at these visits, see:
Your first prenatal visit
Second trimester prenatal visits (14 weeks to 27 weeks)
Third trimester prenatal visits (28 weeks through the end of pregnancy)
The specific number of scheduled appointments you'll have depends on if your pregnancy is considered to be high-risk. This is determined by your medical history and whether you have any complications or conditions that warrant more frequent checkups, such as gestational diabetes , high blood pressure , or a history of preterm labor . If you've had any medical problems in the past or develop any new problems during this pregnancy, you may need more prenatal visits than the average pregnant woman.
In the weeks before each visit, jot down any questions or concerns in a notebook or a notes app on your smartphone. This way, you'll remember to ask your practitioner about them at your next appointment. You may be surprised by how many questions you have, so don't miss the opportunity to get some answers in person.
For example, before you drink an herbal tea or take a supplement or an over-the-counter medication , ask your provider about it. You can even bring the item itself – or a picture of the label – with you to your next appointment. Then, your doctor, midwife, or nurse practitioner can read the label and let you know whether it's okay to ingest.
Of course, if you have any pressing questions or worries, or develop any new, unusual, or severe symptoms , don't wait for your appointment – call your practitioner right away.
In addition to your list, you may want to bring a partner, friend, family member, or labor coach with you to some or all of your prenatal visits. They can comfort you, take notes, ask questions, and help you remember important information.
The goal of prenatal visits is to see how your pregnancy is proceeding and to provide you with information to help keep you and your baby healthy. It's important that you go to all of your prenatal appointments, even if you're feeling just fine and believe that everything is progressing perfectly.
Your practitioner will start by asking how you're feeling physically and emotionally, whether you have any complaints or worries, and what questions you may have. They'll also ask you about your baby's movements once you begin to feel them, typically during the second trimester. Your practitioner will have other questions as well, which will vary depending on how far along you are and whether there are specific concerns.
Your midwife, doctor, or nurse practitioner will also:
- Check your weight , blood pressure , and urine
- Check for swelling
- Measure your abdomen
- Check the position of your baby
- Listen to your baby's heartbeat
- Perform other exams and order tests, as appropriate
- Give you the appropriate vaccinations
- Closely monitor any complications you have or that you develop, and intervene if necessary
Near the end of your pregnancy, your provider may also do a pelvic exam to check for cervical changes. You will also discuss your delivery plan in more depth.
At the end of each visit, your practitioner will review their findings with you. They'll also explain the normal changes to expect before your next visit, warning signs to watch for, and the pros and cons of optional tests you may want to consider. Lifestyle issues will likely be a topic of discussion, as well. Expect to talk about the importance of good nutrition , sleep, oral health, stress management, wearing seatbelts, and avoiding tobacco , alcohol , and illicit drugs.
Many people look forward to their prenatal appointments but are disappointed to find that, with the exception of the first visit, they're in and out of the office in 10 minutes. A quick visit is typical and is usually a sign that everything is progressing normally. Still, you want to make sure your concerns are addressed – and that you and your baby are being well cared for.
Here are some things you can do to ensure that your prenatal visits are satisfying:
- Speak up. Your practitioner isn't a mind reader and won't be able to tell what you're thinking just by performing a physical exam. So, if anything is bothering you, say your piece. Are you having trouble controlling your heartburn ? Managing your constipation ? Suffering from headaches ? This is the time to ask for advice. Consult the notebook of questions you've been compiling. In addition to physical complaints, let your practitioner know if you have emotional concerns or fitness or nutrition questions.
- Ask the staff about the administrative stuff. Save your questions about things like insurance and directions to the hospital for the office staff so your practitioner has more time to answer your health-related questions. Go to the admin staff with any inquiries about payments, scheduling, office policies, and your contact information.
- Be open-minded. When talking with your doctor, midwife, or nurse practitioner, you should feel comfortable speaking freely. But remember to listen, too. Take notes if you find it helpful.
Keep in mind, too, that some days are busier than others. This is especially true during the COVID-19 pandemic. That doesn't mean your practitioner doesn't have to answer your questions, but sometimes a discussion can be continued at the next visit if it's a really busy day or if your practitioner needs to head to the hospital to deliver a baby.
At the same time, don't tolerate a healthcare practitioner who won't give you thorough answers, doesn't show reasonable compassion, or barely looks up from your chart. You and your baby deserve more than that.
Now that you know what to expect during all those prenatal visits, you might like a sneak peek at what else is in store. Here's an overview of the next nine months .
Learn more:
- The ultimate pregnancy to-do list: First trimester
- 12 steps to a healthy pregnancy
- When will my pregnancy start to show?
- Fetal development timeline
Was this article helpful?
What happens at second trimester prenatal appointments

What to expect at your first prenatal appointment

What to expect from third trimester prenatal appointments

Prenatal testing

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
MedlinePlus. (2021). Prenatal care in your first trimester. https://medlineplus.gov/ency/patientinstructions/000544.htm Opens a new window [Accessed September 21, 2021.]
March of Dimes. (2017). Prenatal Care Checkups. https://www.marchofdimes.org/pregnancy/prenatal-care-checkups.aspx Opens a new window [Accessed September 21, 2021.]
Office on Women’s Health. (2019). Prenatal Care and Tests. https://www.womenshealth.gov/pregnancy/youre-pregnant-now-what/prenatal-care-and-tests Opens a new window [Accessed September 21, 2021.]
NIH: Eunice Kennedy Shriver National Institute of Child Health and Human Development. (2017). What happens during prenatal visits? https://www.nichd.nih.gov/health/topics/preconceptioncare/conditioninfo/prenatal-visits Opens a new window [Accessed September 21, 2021.]
NIH: Eunice Kennedy Shriver National Institute of Child Health and Human Development. (2017). What is a high-risk pregnancy? https://www.nichd.nih.gov/health/topics/pregnancy/conditioninfo/high-risk Opens a new window [Accessed September 21, 2021.]
NIH: Eunice Kennedy Shriver National Institute of Child Health and Human Development. (2018). What are some factors that make a pregnancy high-risk? https://www.nichd.nih.gov/health/topics/high-risk/conditioninfo/factors Opens a new window [Accessed September 21, 2021.]
March of Dimes. (2020). Over-the-Counter Medicine, Supplements, and Herbal Products During Pregnancy. https://www.marchofdimes.org/pregnancy/over-the-counter-medicine-supplements-and-herbal-products.aspx Opens a new window [Accessed September 21, 2021.]
Associates in Women’s Healthcare (2021). Preparing for Your First Prenatal Visit. https://www.associatesinwomenshealthcare.net/blog/preparing-for-your-first-prenatal-visit/ Opens a new window [Accessed September 21, 2021.]
National Health Service (UK). (2018). Your baby’s movements. https://www.nhs.uk/pregnancy/keeping-well/your-babys-movements/ Opens a new window [Accessed September 21, 2021.]
MedlinePlus. (2021). Prenatal care in your third trimester. https://medlineplus.gov/ency/patientinstructions/000558.htm Opens a new window [Accessed September 21, 2021.]
UCLA Health. (2021). Schedule of prenatal care. https://www.uclahealth.org/obgyn/workfiles/Pregnancy/Schedule_of_Prenatal_Care.pdf Opens a new window [Accessed September 21, 2021.]
UCR Health. (2021). Healthy Pregnancy: The Importance of Prenatal Care. https://www.ucrhealth.org/2018/07/healthy-pregnancy-the-importance-of-prenatal-care/ Opens a new window [Accessed September 21, 2021.]
Mayo Clinic. (2020). Prenatal care: 1 st trimesters visits. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/prenatal-care/art-20044882 Opens a new window [Accessed September 21, 2021.]

Where to go next

An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Health coverage if you're pregnant, plan to get pregnant, or recently gave birth
An insurance plan that’s certified by the Health Insurance Marketplace®, provides essential health benefits, follows established limits on cost-sharing (like deductibles, copayments, and out-of-pocket maximum amounts), and meets other requirements under the Affordable Care Act. All qualified health plans meet the Affordable Care Act requirement for having health coverage, known as “minimum essential coverage.”
Refer to glossary for more details.

If you don’t have health coverage
If you currently have marketplace coverage, if you may qualify for medicaid or the children’s health insurance program (chip), if you have medicaid or chip, if you’re pregnant or planning to get pregnant:.
- Health coverage makes it easier to get the medical check-ups and screening tests to help keep both you and your baby healthy during pregnancy.
A time outside the yearly Open Enrollment Period when you can sign up for health insurance. You qualify for a Special Enrollment Period if you’ve had certain life events, including losing health coverage, moving, getting married, having a baby, or adopting a child, or if your household income is below a certain amount.
The yearly period (November 1 – January 15) when people can enroll in a Marketplace health insurance plan.
- You'll be asked if you're pregnant if you select the application option to get help paying for coverage and select "Female" for the question about your sex.
- Reporting your pregnancy may help you and your family members get the most affordable coverage.
- If you don’t qualify for a Special Enrollment Period right now, you’ll be eligible to apply within 60 days of your child’s birth. You can also enroll in coverage for the next plan year during the next Open Enrollment Period.
- If eligible for Medicaid or CHIP, your coverage can begin at any time.
- If you want to keep your current Marketplace coverage, don’t report your pregnancy to the Marketplace. When filling out your application for Marketplace coverage, select the “Learn more” link when we ask if you’re pregnant to read tips to help you best answer this question.
- If you keep your Marketplace coverage, update the application after you give birth to add the baby to the plan or enroll them in coverage through Medicaid or CHIP, if they qualify.
- If you report your pregnancy, you may be eligible for free or low-cost coverage through Medicaid or the Children’s Health Insurance Program (CHIP). If you're found eligible for Medicaid or CHIP, your information will be sent to the state agency, and you won't be given the option to keep your Marketplace plan.
- Medicaid and CHIP provide free or low-cost health coverage to millions of Americans, including some low-income people, families and children, and pregnant women.
- Eligibility for these programs depends on your household size, income, and citizenship or immigration status. Specific rules and benefits vary by state.
- You can apply 2 ways: Directly through your state agency, or by filling out a Marketplace application and selecting that you want help paying for coverage.
- Learn how to apply for Medicaid and CHIP .
- Some states offer coverage for a full 12 months after you give birth. Check with your state, or view states (in blue) that offer extended coverage .
- When your state’s coverage period ends, you may no longer qualify.
- Your state will notify you if your coverage is ending. If your coverage will end, you can apply and enroll in a Marketplace plan.
- If you have Medicaid when you give birth, your newborn is automatically enrolled in Medicaid coverage and will remain eligible for at least a year.
If you recently gave birth
- It’s important to have access to health care services for both new parents and baby. Make sure you apply within 60 days after your baby’s birth. Your plan can cover you, your baby, and any other household members.
- If you had Medicaid or CHIP coverage that ended after you gave birth (or if your state told you it’ll end soon), you can apply for Marketplace coverage. Losing other coverage qualifies you for a Special Enrollment Period. When you fill out your application, select that you were found ineligible for Medicaid or CHIP by the state agency.
- Keep your current plan and add your baby to your coverage, OR
- Create a separate enrollment group for your baby and enroll them in any plan for the remainder of the year.
- No matter when your child is born, report their birth to the Marketplace by updating your application as soon as possible. Your coverage options and potential savings may change as a result. You may qualify for more savings than you’re getting now, which could lower what you pay in monthly premiums.
- When you update your application, we’ll also tell you if you or your baby may be eligible for Medicaid or CHIP. If you're found eligible (or possibly eligible) for Medicaid or CHIP, and other household members are still eligible for Marketplace coverage, wait until you have confirmation from the Medicaid or CHIP agency about your eligibility and coverage start date before you make updates to your Marketplace plan.
- Log into your account to “Report a Life Change” .
- Some states offer coverage for a full 12 months after you give birth. Check with your state, o r view states (in blue) that offer extended coverage .
- When your coverage period ends, you may no longer qualify.
- Your state Medicaid or CHIP agency will notify you if your coverage is ending. As soon as you find out that your Medicaid coverage is ending, you can apply and enroll in a Marketplace plan.
- If you have Medicaid when you give birth, your newborn is automatically enrolled in Medicaid coverage and will remain eligible for at least a year.
Health Spending
- Quality of Care
Access & Affordability
- Health & Wellbeing
- Price Transparency
- Affordability
- Prescription Drugs
Health costs associated with pregnancy, childbirth, and postpartum care
By Matthew Rae Twitter , Cynthia Cox Twitter , and Hanna Dingel
July 13, 2022
Stay Connected
Get the best of the Health System Tracker delivered to your inbox.
Pregnancy is one of the most common reasons for a hospitalization among non-elderly people. In addition to the cost of the birth itself, pregnancy care also involves costs associated with prenatal visits and often includes care to treat psychological and medical conditions associated with pregnancy, birth, and the post-partum period.
To examine the health costs associated with pregnancy, childbirth, and post-partum care, we examined a subset of claims from the IBM MarketScan Encounter Database from 2018 through 2020 for enrollees in large employer private health plans. We look at health spending (both the amount paid by insurers and that paid out-of-pocket by enrollees) for female enrollees of reproductive age who give birth, compared to those who do not give birth, holding age constant.
We find that health costs associated with pregnancy, childbirth, and post-partum care average a total of $18,865 and the average out-of-pocket payments total $2,854 for women enrolled in large group plans. We also examine how pregnancy, childbirth, and post-partum health spending among large group enrollees varies by the type of delivery, finding these costs for pregnancies resulting in a vaginal delivery average $14,768 ($2,655 of which is paid out-of-pocket) and those resulting in cesarean section (C-section) average $26,280 ($3,214 of which is paid out-of-pocket).
How we measure the cost of pregnancy, birth, and post-partum care
Some previous analyses of the cost of pregnancy and childbirth have looked at the cost of specific services , such as vaginal and cesarean delivery, or services with a pregnancy diagnosis code . However, looking only at specific claims can miss other care associated with pregnancy and birth, such as psychological care, physical therapy, or treatment of other conditions that arise because of pregnancy but are not necessarily billed as a pregnancy related expense.
In this analysis, we take a different approach. Using a regression model controlling for age, we look at the average difference in health spending for women of reproductive age who give birth compared to those of the same age who do not give birth. The benefit of this approach is that it allows us not only to look at the cost of the delivery, but also at all health costs associated with pregnancy, childbirth, and postpartum care.
Related Content:
The burden of medical debt in the United States
What are the recent trends in employer-based health coverage?
We limit the analysis to people who give birth in a hospital (either a live birth or stillborn) and do not include pregnancies that end in abortion or miscarriage. This analysis only includes the cost of the pregnancy, delivery, and post-partum recovery for the woman, and not any subsequent health spending for care of the infant.
How much does pregnancy, childbirth, and post-partum care cost?
We estimate that pregnant women of reproductive age (ages 15 to 49) enrolled in large group health plans incur an average of $18,865 more in health care costs than women who do not give birth. This additional health spending associated with pregnancy, delivery, and post-partum care includes both the amount paid by insurance (an average of $16,011) and that paid out-of-pocket by the enrollee (an average of $2,854). There is significant variation around these averages, and costs vary significantly by the type of delivery.
Women who give birth incur nearly $19,000 in additional health costs and pay almost $3,000 more out-of-pocket than those who do not give birth
How much pregnancy-related health spending is for hospitalizations and outpatient care.
While pregnant women typically have frequent outpatient office visits prior to giving birth, most pregnancy-related health spending is for the delivery. Women in large group plans with a pregnancy incur an average of $19,906 more in inpatient and outpatient costs than women of the same age who do not give birth. But prescription drug spending averages $1,040 less for women who give birth than for those who do not. Pregnant women are less likely to use prescription drugs than women of the same age who are not pregnant. Birth control pills ( oral contraceptives ) are one of the most used types of prescription drugs for women of reproductive age and some other prescription drugs are unsafe to take during pregnancy. However, these data only include spending on retail prescription drugs and therefore likely miss most out-of-pocket spending on prenatal vitamins or over-the-counter drugs that pregnant women may use.
When looking at out-of-pocket costs over the course of a pregnancy, we find that pregnant women enrolled in large group health plans spend an average of $2,924 more on inpatient and outpatient care than women who are not pregnant spend out-of-pocket, while pregnant women spend an average of $70 less out-of-pocket on prescription drugs. In total, out-of-pocket costs are $2,854 higher for pregnant women than for those of the same age who do not give birth.
These out-of-pocket costs only include amounts paid for cost-sharing (deductibles, coinsurance, and copayments) under the health plan. Therefore, out-of-pocket spending on fertility care is generally missed because these services are not often covered by insurance. Similarly, we do not include any balance bills sent by out-of-network providers directly to patients. We previously estimated that 10% of in-network admissions for maternity care included an out-of-network charge putting patients at risk for surprise medical bills. However, as of January 2022, the No Surprises Act prohibits surprise billing by out-of-network providers when a patient was admitted at an in-network hospital.
How do pregnancy and childbirth costs vary by type of delivery?
Health costs associated with pregnancy, childbirth, and post-partum care vary significantly based on whether the baby is born by cesarean section or vaginal delivery. Over the course of their pregnancy, delivery, and post-partum period, large group enrollees who give birth via cesarean section incur an average of $26,280 more in healthcare costs than those who do not give birth. By contrast, this amount for women with a vaginal delivery averages $14,768.
Pregnancies resulting in C-sections are associated with higher health spending and out-of-pocket costs than those resulting in vaginal deliveries
The higher costs associated with pregnancies that result in cesarean section are not only because of the higher cost of the delivery, but also include higher costs before and after the birth, which may be associated with greater service intensity for care of complications or underlying health conditions that can lead to cesarean section and recovery from the surgery.
Average out-of-pocket costs associated with pregnancy, childbirth, and post-partum care are also higher for women who deliver via cesarean section ($3,214) than for those with vaginal deliveries ($2,655). However, while the average total cost of a pregnancy resulting in a cesarean section ($26,280) is 77% higher than a pregnancy resulting in a vaginal delivery ($14,768), average out-of-pocket costs are 21% higher for women who give birth by cesarean section ($3,214) than those with a vaginal delivery ($2,655). This is largely because enrollees with an inpatient admission often hit their plans’ deductible or out-of-pocket maximum, so higher-cost hospitalizations do not always lead to higher out-of-pocket costs for the admission.
What are the implications of high out-of-pocket costs for pregnancy and childbirth?
The frequency and intensity of services associated with pregnancy and childbirth can lead to considerable out-of-pocket expenses for new parents, particularly those covered by private insurance.
On average, over the course of their pregnancies, pregnant women enrolled in large employer health plans incur $2,854 more in out-of-pocket costs than similar women who are not pregnant. These costs are more than many families can afford. Roughly one third of multi-person households and half of single-person households would not have the liquid assets needed to cover typical out-of-pocket costs associated with pregnancy and childbirth in private health plans. About half of people who give birth in a given year are covered by private insurance, and the remainder are mostly covered by Medicaid, which generally has little or no out-of-pocket liability.
Medical care for the infant can result in even more out-of-pocket costs for families with private insurance coverage. And these out-of-pocket health costs arrive just as these parents begin taking on additional costs of caring for a child. Many new parents also experience income losses due to a lack of paid parental leave, which can leave many new parents vulnerable to incurring medical debt .
Limitations
This analysis has some limitations, including that we do not control for health status before the pregnancy. It is possible women who give birth are somewhat healthier on average going into their pregnancies than women of the same age who do not give birth. Conversely, it is also possible that health conditions present before pregnancy may be incidentally discovered during pregnancy. Although we do not control for health status, health status and spending are strongly correlated with age, for which we do control.
We are only including health spending that happens through the health plan, so do not include care that is paid fully out-of-pocket, which would include most fertility treatments (as this care is often not covered by insurance).
We describe our findings as applying to pregnant women, though some of the births included were for female enrollees under the age of 18. The MarketScan sex variable is binary and our analysis is limited to the classification on the health record.
This analysis uses claims from the IBM Health Analytics MarketScan Commercial Claims and Encounters Database, which contains claims information provided by a sample of large employer plans. MarketScan allows for enrollees to be tracked for their duration at one contributing employer, and we used a subset of claims for enrollees covered in each of three years, 2018 through 2020. All dollar values are reported in 2020 nominal dollars. To make MarketScan data more representative of large group plans, weights were applied to match counts in the Current Population Survey for enrollees at firms of a thousand or more workers by sex, age and state. Weights were trimmed at eight times the interquartile range.
We further limited the sample to female enrollees between ages 15 and 49 who were continuously enrolled during the 2018-2020 period, to avoid including costs for women who changed coverage during the pregnancy. In total, this analysis used claims for almost 2,267,200 female enrollees, which represents about 15% of the estimated 14,800,000 women of reproductive age enrolled in large group market plans (plans offered by employers with one thousand or more workers) in 2018.
IBM assigns a DRG to each admission using the Centers for Medicare & Medicaid Services (CMS) Grouper. This method selects a DRG for the admission based on the diagnosis and procedures a patient received during the stay. We identify women as having a pregnancy if, between August 2018 and September 2020, they had an admission that was designated as a delivery (783-788, 796-798 and 805-807). We then modeled spending for these enrollees between January 2018 and December 2020, controlling for age and whether they had multiple pregnancy related admissions over that period. This method does not include the cost of pregnancy for enrollees who do not give birth (i.e., those pregnancies ending in a miscarriage or abortion).
Claims data available in MarketScan allows an analysis of liabilities incurred by enrollees with some limitations. First, these data reflect cost sharing incurred under the benefit plan and do not include balance-billing payments that beneficiaries may make to health care providers for out-of-network services or out-of-pocket payments for non-covered services, meaning that we may understate the costs associated with pregnancy. Secondly, claims data show the retail cost for prescription drugs and do not include information about the value of rebates that may be received by payers. Third, when showing how spending is divided across types of care (i.e., health services and prescriptions), we combine spending on inpatient and outpatient care because global billing is commonly used for maternity services. In claims data, inpatient costs will therefore sometimes include all services for routine prenatal care, delivery services, and postpartum care since the global maternity claim is typically billed the day of delivery. Lastly, sex is defined as reported on the claim, and we are unable to identify the gender identity of the enrollee.
About this site
The Peterson Center on Healthcare and KFF are partnering to monitor how well the U.S. healthcare system is performing in terms of quality and cost.
More from Health System Tracker
Charges for emails with doctors and other healthcare providers.
Private insurer payments for telehealth and in-person claims during the pandemic
Looking for more data?
Find out more details about U.S. healthcare from our updated dashboard.
A Partnership Of
Share health system tracker.
How Much Does Pregnancy Cost?
Medical review policy, latest update:.
Updated, fact-checked and medically reviewed to ensure accuracy.
Health insurance for pregnancy 101
Recommended reading, how much does pregnancy cost with health insurance, marketplace coverage, employer coverage, pregnancy costs for the uninsured, how to reduce maternity costs, updates history, jump to your week of pregnancy, trending on what to expect, signs of labor, pregnancy calculator, ⚠️ you can't see this cool content because you have ad block enabled., top 1,000 baby girl names in the u.s., top 1,000 baby boy names in the u.s., braxton hicks contractions and false labor.
Thanks for visiting! GoodRx is not available outside of the United States. If you are trying to access this site from the United States and believe you have received this message in error, please reach out to [email protected] and let us know.
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
What the data says about abortion in the U.S.
Pew Research Center has conducted many surveys about abortion over the years, providing a lens into Americans’ views on whether the procedure should be legal, among a host of other questions.
In a Center survey conducted nearly a year after the Supreme Court’s June 2022 decision that ended the constitutional right to abortion , 62% of U.S. adults said the practice should be legal in all or most cases, while 36% said it should be illegal in all or most cases. Another survey conducted a few months before the decision showed that relatively few Americans take an absolutist view on the issue .
Find answers to common questions about abortion in America, based on data from the Centers for Disease Control and Prevention (CDC) and the Guttmacher Institute, which have tracked these patterns for several decades:
How many abortions are there in the U.S. each year?
How has the number of abortions in the u.s. changed over time, what is the abortion rate among women in the u.s. how has it changed over time, what are the most common types of abortion, how many abortion providers are there in the u.s., and how has that number changed, what percentage of abortions are for women who live in a different state from the abortion provider, what are the demographics of women who have had abortions, when during pregnancy do most abortions occur, how often are there medical complications from abortion.
This compilation of data on abortion in the United States draws mainly from two sources: the Centers for Disease Control and Prevention (CDC) and the Guttmacher Institute, both of which have regularly compiled national abortion data for approximately half a century, and which collect their data in different ways.
The CDC data that is highlighted in this post comes from the agency’s “abortion surveillance” reports, which have been published annually since 1974 (and which have included data from 1969). Its figures from 1973 through 1996 include data from all 50 states, the District of Columbia and New York City – 52 “reporting areas” in all. Since 1997, the CDC’s totals have lacked data from some states (most notably California) for the years that those states did not report data to the agency. The four reporting areas that did not submit data to the CDC in 2021 – California, Maryland, New Hampshire and New Jersey – accounted for approximately 25% of all legal induced abortions in the U.S. in 2020, according to Guttmacher’s data. Most states, though, do have data in the reports, and the figures for the vast majority of them came from each state’s central health agency, while for some states, the figures came from hospitals and other medical facilities.
Discussion of CDC abortion data involving women’s state of residence, marital status, race, ethnicity, age, abortion history and the number of previous live births excludes the low share of abortions where that information was not supplied. Read the methodology for the CDC’s latest abortion surveillance report , which includes data from 2021, for more details. Previous reports can be found at stacks.cdc.gov by entering “abortion surveillance” into the search box.
For the numbers of deaths caused by induced abortions in 1963 and 1965, this analysis looks at reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services. In computing those figures, we excluded abortions listed in the report under the categories “spontaneous or unspecified” or as “other.” (“Spontaneous abortion” is another way of referring to miscarriages.)
Guttmacher data in this post comes from national surveys of abortion providers that Guttmacher has conducted 19 times since 1973. Guttmacher compiles its figures after contacting every known provider of abortions – clinics, hospitals and physicians’ offices – in the country. It uses questionnaires and health department data, and it provides estimates for abortion providers that don’t respond to its inquiries. (In 2020, the last year for which it has released data on the number of abortions in the U.S., it used estimates for 12% of abortions.) For most of the 2000s, Guttmacher has conducted these national surveys every three years, each time getting abortion data for the prior two years. For each interim year, Guttmacher has calculated estimates based on trends from its own figures and from other data.
The latest full summary of Guttmacher data came in the institute’s report titled “Abortion Incidence and Service Availability in the United States, 2020.” It includes figures for 2020 and 2019 and estimates for 2018. The report includes a methods section.
In addition, this post uses data from StatPearls, an online health care resource, on complications from abortion.
An exact answer is hard to come by. The CDC and the Guttmacher Institute have each tried to measure this for around half a century, but they use different methods and publish different figures.
The last year for which the CDC reported a yearly national total for abortions is 2021. It found there were 625,978 abortions in the District of Columbia and the 46 states with available data that year, up from 597,355 in those states and D.C. in 2020. The corresponding figure for 2019 was 607,720.
The last year for which Guttmacher reported a yearly national total was 2020. It said there were 930,160 abortions that year in all 50 states and the District of Columbia, compared with 916,460 in 2019.
- How the CDC gets its data: It compiles figures that are voluntarily reported by states’ central health agencies, including separate figures for New York City and the District of Columbia. Its latest totals do not include figures from California, Maryland, New Hampshire or New Jersey, which did not report data to the CDC. ( Read the methodology from the latest CDC report .)
- How Guttmacher gets its data: It compiles its figures after contacting every known abortion provider – clinics, hospitals and physicians’ offices – in the country. It uses questionnaires and health department data, then provides estimates for abortion providers that don’t respond. Guttmacher’s figures are higher than the CDC’s in part because they include data (and in some instances, estimates) from all 50 states. ( Read the institute’s latest full report and methodology .)
While the Guttmacher Institute supports abortion rights, its empirical data on abortions in the U.S. has been widely cited by groups and publications across the political spectrum, including by a number of those that disagree with its positions .
These estimates from Guttmacher and the CDC are results of multiyear efforts to collect data on abortion across the U.S. Last year, Guttmacher also began publishing less precise estimates every few months , based on a much smaller sample of providers.
The figures reported by these organizations include only legal induced abortions conducted by clinics, hospitals or physicians’ offices, or those that make use of abortion pills dispensed from certified facilities such as clinics or physicians’ offices. They do not account for the use of abortion pills that were obtained outside of clinical settings .
(Back to top)
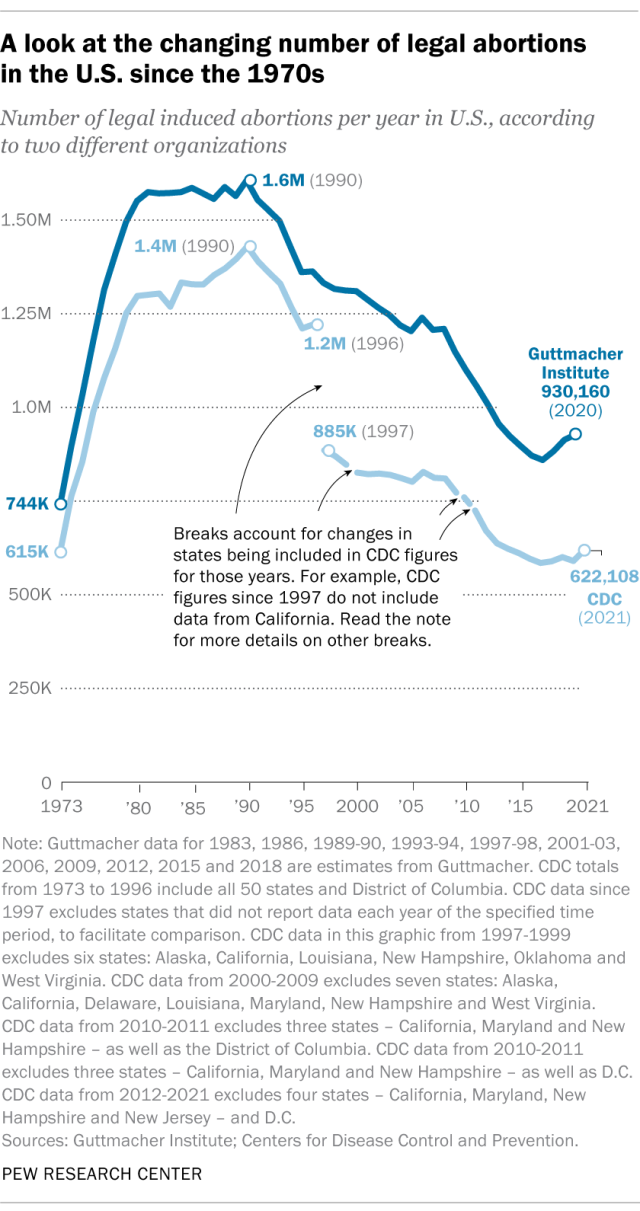
The annual number of U.S. abortions rose for years after Roe v. Wade legalized the procedure in 1973, reaching its highest levels around the late 1980s and early 1990s, according to both the CDC and Guttmacher. Since then, abortions have generally decreased at what a CDC analysis called “a slow yet steady pace.”
Guttmacher says the number of abortions occurring in the U.S. in 2020 was 40% lower than it was in 1991. According to the CDC, the number was 36% lower in 2021 than in 1991, looking just at the District of Columbia and the 46 states that reported both of those years.
(The corresponding line graph shows the long-term trend in the number of legal abortions reported by both organizations. To allow for consistent comparisons over time, the CDC figures in the chart have been adjusted to ensure that the same states are counted from one year to the next. Using that approach, the CDC figure for 2021 is 622,108 legal abortions.)
There have been occasional breaks in this long-term pattern of decline – during the middle of the first decade of the 2000s, and then again in the late 2010s. The CDC reported modest 1% and 2% increases in abortions in 2018 and 2019, and then, after a 2% decrease in 2020, a 5% increase in 2021. Guttmacher reported an 8% increase over the three-year period from 2017 to 2020.
As noted above, these figures do not include abortions that use pills obtained outside of clinical settings.
Guttmacher says that in 2020 there were 14.4 abortions in the U.S. per 1,000 women ages 15 to 44. Its data shows that the rate of abortions among women has generally been declining in the U.S. since 1981, when it reported there were 29.3 abortions per 1,000 women in that age range.
The CDC says that in 2021, there were 11.6 abortions in the U.S. per 1,000 women ages 15 to 44. (That figure excludes data from California, the District of Columbia, Maryland, New Hampshire and New Jersey.) Like Guttmacher’s data, the CDC’s figures also suggest a general decline in the abortion rate over time. In 1980, when the CDC reported on all 50 states and D.C., it said there were 25 abortions per 1,000 women ages 15 to 44.
That said, both Guttmacher and the CDC say there were slight increases in the rate of abortions during the late 2010s and early 2020s. Guttmacher says the abortion rate per 1,000 women ages 15 to 44 rose from 13.5 in 2017 to 14.4 in 2020. The CDC says it rose from 11.2 per 1,000 in 2017 to 11.4 in 2019, before falling back to 11.1 in 2020 and then rising again to 11.6 in 2021. (The CDC’s figures for those years exclude data from California, D.C., Maryland, New Hampshire and New Jersey.)
The CDC broadly divides abortions into two categories: surgical abortions and medication abortions, which involve pills. Since the Food and Drug Administration first approved abortion pills in 2000, their use has increased over time as a share of abortions nationally, according to both the CDC and Guttmacher.
The majority of abortions in the U.S. now involve pills, according to both the CDC and Guttmacher. The CDC says 56% of U.S. abortions in 2021 involved pills, up from 53% in 2020 and 44% in 2019. Its figures for 2021 include the District of Columbia and 44 states that provided this data; its figures for 2020 include D.C. and 44 states (though not all of the same states as in 2021), and its figures for 2019 include D.C. and 45 states.
Guttmacher, which measures this every three years, says 53% of U.S. abortions involved pills in 2020, up from 39% in 2017.
Two pills commonly used together for medication abortions are mifepristone, which, taken first, blocks hormones that support a pregnancy, and misoprostol, which then causes the uterus to empty. According to the FDA, medication abortions are safe until 10 weeks into pregnancy.
Surgical abortions conducted during the first trimester of pregnancy typically use a suction process, while the relatively few surgical abortions that occur during the second trimester of a pregnancy typically use a process called dilation and evacuation, according to the UCLA School of Medicine.
In 2020, there were 1,603 facilities in the U.S. that provided abortions, according to Guttmacher . This included 807 clinics, 530 hospitals and 266 physicians’ offices.
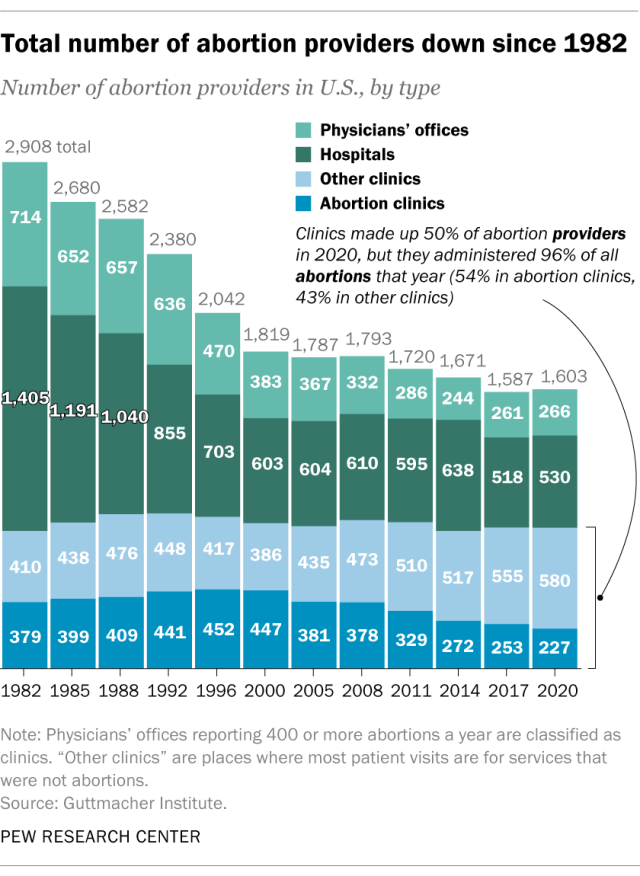
While clinics make up half of the facilities that provide abortions, they are the sites where the vast majority (96%) of abortions are administered, either through procedures or the distribution of pills, according to Guttmacher’s 2020 data. (This includes 54% of abortions that are administered at specialized abortion clinics and 43% at nonspecialized clinics.) Hospitals made up 33% of the facilities that provided abortions in 2020 but accounted for only 3% of abortions that year, while just 1% of abortions were conducted by physicians’ offices.
Looking just at clinics – that is, the total number of specialized abortion clinics and nonspecialized clinics in the U.S. – Guttmacher found the total virtually unchanged between 2017 (808 clinics) and 2020 (807 clinics). However, there were regional differences. In the Midwest, the number of clinics that provide abortions increased by 11% during those years, and in the West by 6%. The number of clinics decreased during those years by 9% in the Northeast and 3% in the South.
The total number of abortion providers has declined dramatically since the 1980s. In 1982, according to Guttmacher, there were 2,908 facilities providing abortions in the U.S., including 789 clinics, 1,405 hospitals and 714 physicians’ offices.
The CDC does not track the number of abortion providers.
In the District of Columbia and the 46 states that provided abortion and residency information to the CDC in 2021, 10.9% of all abortions were performed on women known to live outside the state where the abortion occurred – slightly higher than the percentage in 2020 (9.7%). That year, D.C. and 46 states (though not the same ones as in 2021) reported abortion and residency data. (The total number of abortions used in these calculations included figures for women with both known and unknown residential status.)
The share of reported abortions performed on women outside their state of residence was much higher before the 1973 Roe decision that stopped states from banning abortion. In 1972, 41% of all abortions in D.C. and the 20 states that provided this information to the CDC that year were performed on women outside their state of residence. In 1973, the corresponding figure was 21% in the District of Columbia and the 41 states that provided this information, and in 1974 it was 11% in D.C. and the 43 states that provided data.
In the District of Columbia and the 46 states that reported age data to the CDC in 2021, the majority of women who had abortions (57%) were in their 20s, while about three-in-ten (31%) were in their 30s. Teens ages 13 to 19 accounted for 8% of those who had abortions, while women ages 40 to 44 accounted for about 4%.
The vast majority of women who had abortions in 2021 were unmarried (87%), while married women accounted for 13%, according to the CDC , which had data on this from 37 states.
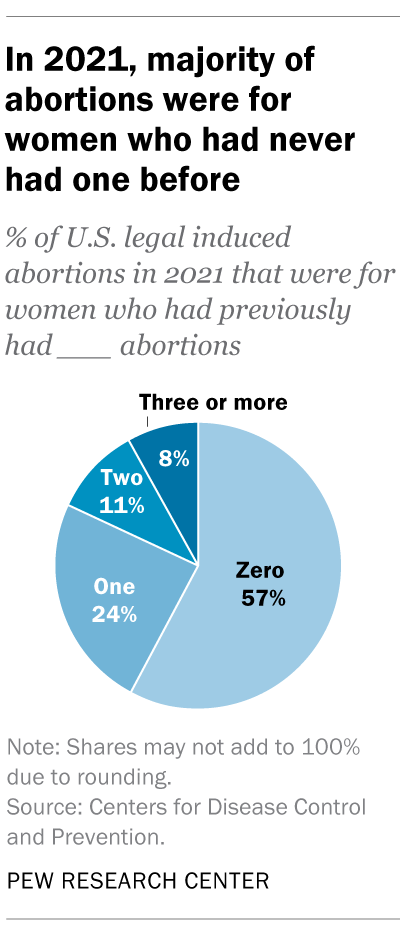
In the District of Columbia, New York City (but not the rest of New York) and the 31 states that reported racial and ethnic data on abortion to the CDC , 42% of all women who had abortions in 2021 were non-Hispanic Black, while 30% were non-Hispanic White, 22% were Hispanic and 6% were of other races.
Looking at abortion rates among those ages 15 to 44, there were 28.6 abortions per 1,000 non-Hispanic Black women in 2021; 12.3 abortions per 1,000 Hispanic women; 6.4 abortions per 1,000 non-Hispanic White women; and 9.2 abortions per 1,000 women of other races, the CDC reported from those same 31 states, D.C. and New York City.
For 57% of U.S. women who had induced abortions in 2021, it was the first time they had ever had one, according to the CDC. For nearly a quarter (24%), it was their second abortion. For 11% of women who had an abortion that year, it was their third, and for 8% it was their fourth or more. These CDC figures include data from 41 states and New York City, but not the rest of New York.
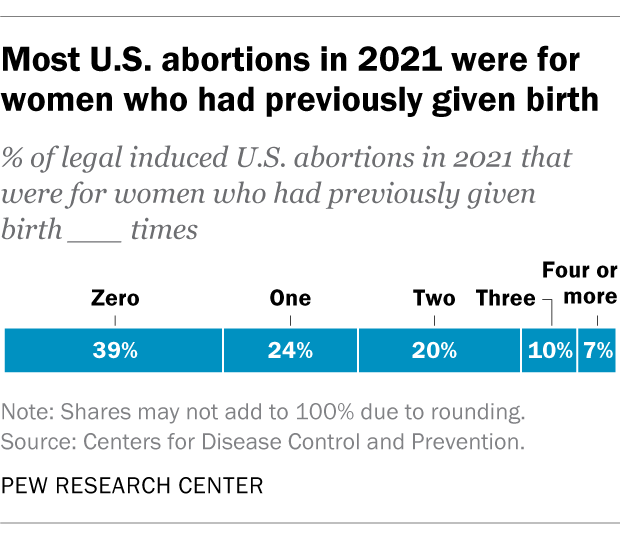
Nearly four-in-ten women who had abortions in 2021 (39%) had no previous live births at the time they had an abortion, according to the CDC . Almost a quarter (24%) of women who had abortions in 2021 had one previous live birth, 20% had two previous live births, 10% had three, and 7% had four or more previous live births. These CDC figures include data from 41 states and New York City, but not the rest of New York.
The vast majority of abortions occur during the first trimester of a pregnancy. In 2021, 93% of abortions occurred during the first trimester – that is, at or before 13 weeks of gestation, according to the CDC . An additional 6% occurred between 14 and 20 weeks of pregnancy, and about 1% were performed at 21 weeks or more of gestation. These CDC figures include data from 40 states and New York City, but not the rest of New York.
About 2% of all abortions in the U.S. involve some type of complication for the woman , according to an article in StatPearls, an online health care resource. “Most complications are considered minor such as pain, bleeding, infection and post-anesthesia complications,” according to the article.
The CDC calculates case-fatality rates for women from induced abortions – that is, how many women die from abortion-related complications, for every 100,000 legal abortions that occur in the U.S . The rate was lowest during the most recent period examined by the agency (2013 to 2020), when there were 0.45 deaths to women per 100,000 legal induced abortions. The case-fatality rate reported by the CDC was highest during the first period examined by the agency (1973 to 1977), when it was 2.09 deaths to women per 100,000 legal induced abortions. During the five-year periods in between, the figure ranged from 0.52 (from 1993 to 1997) to 0.78 (from 1978 to 1982).
The CDC calculates death rates by five-year and seven-year periods because of year-to-year fluctuation in the numbers and due to the relatively low number of women who die from legal induced abortions.
In 2020, the last year for which the CDC has information , six women in the U.S. died due to complications from induced abortions. Four women died in this way in 2019, two in 2018, and three in 2017. (These deaths all followed legal abortions.) Since 1990, the annual number of deaths among women due to legal induced abortion has ranged from two to 12.
The annual number of reported deaths from induced abortions (legal and illegal) tended to be higher in the 1980s, when it ranged from nine to 16, and from 1972 to 1979, when it ranged from 13 to 63. One driver of the decline was the drop in deaths from illegal abortions. There were 39 deaths from illegal abortions in 1972, the last full year before Roe v. Wade. The total fell to 19 in 1973 and to single digits or zero every year after that. (The number of deaths from legal abortions has also declined since then, though with some slight variation over time.)
The number of deaths from induced abortions was considerably higher in the 1960s than afterward. For instance, there were 119 deaths from induced abortions in 1963 and 99 in 1965 , according to reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services. The CDC is a division of Health and Human Services.
Note: This is an update of a post originally published May 27, 2022, and first updated June 24, 2022.

Support for legal abortion is widespread in many countries, especially in Europe
Nearly a year after roe’s demise, americans’ views of abortion access increasingly vary by where they live, by more than two-to-one, americans say medication abortion should be legal in their state, most latinos say democrats care about them and work hard for their vote, far fewer say so of gop, positive views of supreme court decline sharply following abortion ruling, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Coronavirus (COVID-19)
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
- International edition
- Australia edition
- Europe edition

Rise in pregnant women turned away from US emergency rooms, papers show
Cases listed in federal documents raise alarms around emergency pregnancy care, especially in states with strict abortion laws
One woman miscarried in the restroom lobby of a Texas emergency room as front desk staff refused to admit her to the hospital.
Another woman learned that her fetus had no heartbeat at a Florida hospital, the day after a security guard turned her away from the facility. And in North Carolina, a woman gave birth in a car after an emergency room couldn’t offer an ultrasound, and the baby later died.
Complaints that pregnant women were turned away from US emergency rooms spiked in 2022 after the US supreme court overturned Roe v Wade , federal documents obtained by the Associated Press reveal.
The cases raise alarms about the state of emergency pregnancy care, especially in states that enacted strict abortion laws and sparked confusion around the treatment doctors can legally provide.
“It is shocking, it’s absolutely shocking,” said Amelia Huntsberger, an obstetrician/gynecologist in Oregon. “It is appalling that someone would show up to an emergency room and not receive care – this is inconceivable.”
And it has happened despite federal mandates that the women be treated. Federal law requires emergency rooms to treat or stabilize patients who are in active labor and provide a medical transfer to another hospital if they don’t have the staff or resources to treat them. Medical facilities must comply with the law if they accept funding from the federal government Medicare program.
The supreme court will hear arguments next Wednesday that could weaken those protections. The Biden administration has sued Idaho over its abortion ban, even in medical emergencies, arguing it conflicts with the federal law.
“No woman should be denied the care she needs,” Jennifer Klein, director of the White House gender policy council, said in a statement. “All patients, including women who are experiencing pregnancy-related emergencies, should have access to emergency medical care required under the Emergency Medical Treatment and Labor Act [Emtala].”
Pregnant patients have “become ‘radioactive’ to emergency departments” in states with extreme abortion restrictions, said Sara Rosenbaum, a George Washington University health law and policy professor, adding: “They are so scared of a pregnant patient, that the emergency medicine staff won’t even look. They just want these people gone.”
A woman who was nine months pregnant and having contractions arrived at the Falls Community hospital in Marlin, Texas, in July 2022, a week after the supreme court’s ruling on abortion. The doctor on duty refused to see her.
“The physician came to the triage desk and told the patient that we did not have obstetric services or capabilities,” hospital staff told federal investigators during interviews, according to documents. “The nursing staff informed the physician that we could test her for the presence of amniotic fluid. However, the physician adamantly recommended the patient drive to a Waco hospital.”
Investigators with the Centers for Medicare and Medicaid Services federal agency concluded that Falls Community hospital broke the law. Reached by phone, an administrator at the hospital declined to comment on the incident.
The investigation was one of dozens the AP obtained from a Freedom of Information Act request filed in February 2023 that sought all pregnancy-related Emtala complaints the previous year and, one year later, received limited results from just 19 states.
Federal investigators looked into just over a dozen pregnancy-related complaints in those states in the run-up to the Roe ruling, but more than two dozen complaints in the months following. It is not known how many complaints were filed last year as the records request only asked for 2022 complaints and the information is not publicly available otherwise.
The documents did not detail what happened to the patient turned away from the Falls Community hospital. Other pregnancies ended in catastrophe, the documents show.
At Sacred Heart emergency center in Houston, front desk staff refused to check in one woman after her husband asked for help delivering her baby that September. She miscarried in a restroom toilet in the emergency room lobby while her husband called 911 for help.
“She is bleeding a lot and had a miscarriage,” the husband told first responders in his call, which was transcribed from Spanish in federal documents. “I’m here at the hospital but they told us they can’t help us because we are not their client.”
Emergency crews, who arrived 20 minutes later and transferred the woman to a hospital, appeared confused over the staff’s refusal to help the woman, according to 911 call transcripts.
One first responder told federal investigators that when a Sacred Heart emergency center staffer was asked about the gestational age of the fetus, the staffer replied: “No, we can’t tell you, she is not our patient. That’s why you are here.”
A manager for Sacred Heart emergency center declined to comment. The facility is licensed in Texas as a freestanding emergency room, which means it is not physically connected to a hospital. State law requires those facilities to treat or stabilize patients, a spokeswoman for the Texas health and human services agency said in an email to AP.
Sacred Heart emergency’s website says that it no longer accepts Medicare, a change that was made some time after the woman miscarried, according to publicly available archives of the center’s website.
Meanwhile, the staff at Person Memorial hospital in Roxboro, North Carolina, told a pregnant woman, who was complaining of stomach pain, that they would not be able to provide her with an ultrasound. The staff failed to tell her how risky it could be for her to depart without being stabilized, according to federal investigators. While en route to another hospital 45 minutes away, the woman gave birth in a car to a baby who did not survive.
Person Memorial hospital self-reported the incident. A spokeswoman said the hospital continued to “provide ongoing education for our staff and providers to ensure compliance”.
In Melbourne, Florida, a security guard at Holmes Regional medical center refused to let a pregnant woman into the triage area because she had brought a child with her. When the patient came back the next day, medical staff were unable to locate a fetal heartbeat. The center declined to comment on the case.
Emergency rooms are subject to hefty fines when they turn away patients, fail to stabilize them or transfer them to another hospital for treatment. Violations can also put hospitals’ Medicare funding at risk.
But it is unclear what fines might be imposed on more than a dozen hospitals that the Biden administration says failed to properly treat pregnant patients in 2022. It can take years for fines to be levied in these cases.
For Huntsberger, Emtala law was one of the few ways she felt protected to treat pregnant patients in Idaho, despite the state’s abortion ban. She left Idaho last year because of the ban, to practice in Oregon instead.
Joe Biden and Xavier Becerra, the health secretary, have both publicly vowed vigilance in enforcing the law.
Even as states have enacted strict abortion laws, the White House has argued that if hospitals receive Medicare funds they must provide stabilizing care, including abortions.
In a statement to AP, Becerra called it the “nation’s bedrock law protecting Americans’ right to life- and health-saving emergency medical care … And doctors, not politicians, should determine what constitutes emergency care.”
- Reproductive rights
- US healthcare
Most viewed
Emergency rooms refused to treat pregnant women, leaving one to miscarry in a lobby restroom
Washington — One woman miscarried in the restroom lobby of a Texas emergency room as front desk staff refused to admit her. Another woman learned that her fetus had no heartbeat at a Florida hospital, the day after a security guard turned her away from the facility. And in North Carolina, a woman gave birth in a car after an emergency room couldn't offer an ultrasound. The baby later died.
Complaints that pregnant women were turned away from U.S. emergency rooms spiked in 2022 after the U.S. Supreme Court overturned Roe v. Wade, federal documents obtained by The Associated Press reveal.
The cases raise alarms about the state of emergency pregnancy care in the U.S., especially in states that enacted strict abortion laws and sparked confusion around the treatment doctors can provide.
“It is shocking, it’s absolutely shocking,” said Amelia Huntsberger, an OB/GYN in Oregon. “It is appalling that someone would show up to an emergency room and not receive care -- this is inconceivable.”
It's happened despite federal mandates that the women be treated.
Federal law requires emergency rooms to treat or stabilize patients who are in active labor and provide a medical transfer to another hospital if they don’t have the staff or resources to treat them. Medical facilities must comply with the law if they accept Medicare funding.
The Supreme Court will hear arguments Wednesday that could weaken those protections. The Biden administration has sued Idaho over its abortion ban, even in medical emergencies, arguing it conflicts with the federal law.
“No woman should be denied the care she needs,” Jennifer Klein, director of the White House Gender Policy Council, said in a statement. “All patients, including women who are experiencing pregnancy-related emergencies, should have access to emergency medical care required under the Emergency Medical Treatment and Labor Act.”
Pregnancy care after Roe
Pregnant patients have “become radioactive to emergency departments” in states with extreme abortion restrictions, said Sara Rosenbaum, a George Washington University health law and policy professor.
“They are so scared of a pregnant patient, that the emergency medicine staff won’t even look. They just want these people gone," Rosenbaum said.
Consider what happened to a woman who was nine months pregnant and having contractions when she arrived at the Falls Community Hospital in Marlin, Texas, in July 2022, a week after the Supreme Court’s ruling on abortion. The doctor on duty refused to see her.
“The physician came to the triage desk and told the patient that we did not have obstetric services or capabilities,” hospital staff told federal investigators during interviews, according to documents. “The nursing staff informed the physician that we could test her for the presence of amniotic fluid. However, the physician adamantly recommended the patient drive to a Waco hospital.”
Investigators with the Centers for Medicare and Medicaid Services concluded Falls Community Hospital broke the law.
Reached by phone, an administrator at the hospital declined to comment on the incident.
The investigation was one of dozens the AP obtained from a Freedom of Information Act request filed in February 2023 that sought all pregnancy-related EMTALA complaints the previous year. One year after submitting the request, the federal government agreed to release only some complaints and investigative documents filed across just 19 states. The names of patients, doctors and medical staff were redacted from the documents.
Federal investigators looked into just over a dozen pregnancy-related complaints in those states during the months leading up to the U.S. Supreme Court's pivotal ruling on abortion in 2022. But more than two dozen complaints about emergency pregnancy care were lodged in the months after the decision was unveiled. It is not known how many complaints were filed last year as the records request only asked for 2022 complaints and the information is not publicly available otherwise.
The documents did not detail what happened to the patient turned away from the Falls Community Hospital.
'She is bleeding a lot'
Other pregnancies ended in catastrophe, the documents show.
At Sacred Heart Emergency Center in Houston, front desk staff refused to check in one woman after her husband asked for help delivering her baby that September. She miscarried in a restroom toilet in the emergency room lobby while her husband called 911 for help.
“She is bleeding a lot and had a miscarriage,” the husband told first responders in his call, which was transcribed from Spanish in federal documents. “I’m here at the hospital but they told us they can’t help us because we are not their client.”
Emergency crews, who arrived 20 minutes later and transferred the woman to a hospital, appeared confused over the staff's refusal to help the woman, according to 911 call transcripts.
One first responder told federal investigators that when a Sacred Heart Emergency Center staffer was asked about the gestational age of the fetus, the staffer replied: “No, we can’t tell you, she is not our patient. That’s why you are here.”
A manager for Sacred Heart Emergency Center declined to comment. The facility is licensed in Texas as a freestanding emergency room, which means it is not physically connected to a hospital. State law requires those facilities to treat or stabilize patients, a spokeswoman for the Texas Health and Human Services agency said in an email to AP.
Sacred Heart Emergency’s website says that it no longer accepts Medicare, a change that was made sometime after the woman miscarried, according to publicly available archives of the center's website.
Meanwhile, the staff at Person Memorial Hospital in Roxboro, North Carolina, told a pregnant woman, who was complaining of stomach pain, that they would not be able to provide her with an ultrasound. The staff failed to tell her how risky it could be for her to depart without being stabilized, according to federal investigators. While en route to another hospital 45 minutes away, the woman gave birth in a car to a baby who did not survive.
Person Memorial Hospital self-reported the incident. A spokeswoman said the hospital continues to “provide ongoing education for our staff and providers to ensure compliance.”
In Melbourne, Florida, a security guard at Holmes Regional Medical Center refused to let a pregnant woman into the triage area because she had brought a child with her. When the patient came back the next day, medical staff were unable to locate a fetal heartbeat. The center declined to comment on the case.
'What's the penalty?'
Emergency rooms are subject to hefty fines when they turn away patients, fail to stabilize them or transfer them to another hospital for treatment. Violations can also put hospitals' Medicare funding at risk.
But it’s unclear what fines might be imposed on more than a dozen hospitals that the Biden administration says failed to properly treat pregnant patients in 2022.
It can take years for fines to be levied in these cases. The Health and Human Services agency, which enforces the law, declined to share if the hospitals have been referred to the agency's Office of Inspector General for penalties.
For Huntsberger, the OB-GYN, EMTALA was one of the few ways she felt protected to treat pregnant patients in Idaho, despite the state's abortion ban. She left Idaho last year to practice in Oregon because of the ban.
The threat of fines or loss of Medicare funding for violating EMTALA is a big deterrent that keeps hospitals from dumping patients, she said. Many couldn't keep their doors open if they lost Medicare funding.
She has been waiting to see how HHS penalizes two hospitals in Missouri and Kansas that HHS announced last year it was investigating after a pregnant woman, who was in preterm labor at 17 weeks, was denied an abortion.
“A lot of these situations are not reported, but even the ones that are — like the cases out of the Midwest — they're investigated but nothing really comes of it,” Huntsberger said. “People are just going to keep providing substandard care or not providing care. The only way that changes is things like this.”
Next up for EMTALA
President Joe Biden and top U.S. health official Xavier Becerra have both publicly vowed vigilance in enforcing the law.
Even as states have enacted strict abortion laws, the White House has argued that if hospitals receive Medicare funds they must provide stabilizing care, including abortions.
In a statement to THE AP, Becerra called it the “nation's bedrock law protecting Americans' right to life- and health-saving emergency medical care.”
“And doctors, not politicians, should determine what constitutes emergency care," he added.
Idaho’s law does not allow abortions if a mother's health is at risk. But the state's attorney general has argued that its abortion ban is “consistent” with federal law, which calls for emergency rooms to protect an unborn child in medical emergencies.
"The Biden administration has no business rewriting federal law to override Idaho’s law and force doctors to perform abortions,” Idaho Attorney General Raúl Labrador said in a statement earlier this year.
Now, the Supreme Court will weigh in. The case could have implications in other states like Arizona, which is reinstating an 1864 law that bans all abortions, with an exception only if the mother's life is at risk.
EMTALA was initially introduced decades ago because private hospitals would dump patients on county or state hospitals, often because they didn’t have insurance, said Alexa Kolbi-Molinas of the American Civil Liberties Union.
Some hospitals also refused to see pregnant women when they did not have an established relationship with physicians on staff. If the court nullifies or weakens those protections, it could result in more hospitals turning away patients without fear of penalty from the federal government, she said.
“The government knows there’s a problem and is investigating and is doing something about that,” Kolbi-Molinas said. “Without EMTALA, they wouldn’t be able to do that.”
The Cost Of A Pregnancy Doctor Visit Without Insurance: What You Need To Know
- Last updated Dec 30, 2023
- Difficulty Beginner
- Category Complications during pregnancy

Did you know that the cost of medical care, including doctor's visits, can vary greatly depending on whether or not you have health insurance? This is especially true for something as important and frequent as prenatal care during a pregnancy. If you find yourself without insurance and in need of a pregnancy doctor visit, you might be wondering how much it will cost you. The answer is not as straightforward as you may think, as there are many factors that can influence the cost of a pregnancy doctor visit without insurance. In this article, we will explore some of these factors and provide you with an estimate of what you can expect to pay.
What You'll Learn
What is the average cost of a pregnancy doctor visit without insurance, are there any affordable options or payment plans available for pregnant women without insurance, what factors can affect the cost of a pregnancy doctor visit without insurance, are there any government programs or clinics that provide discounted or free prenatal care for uninsured pregnant women, is it possible to negotiate the cost of a pregnancy doctor visit without insurance with the healthcare provider.

The average cost of a pregnancy doctor visit without insurance can vary depending on several factors. It is important to note that prenatal care is crucial for the health and well-being of both the mother and the baby, and seeking proper medical attention is a priority.
On average, prenatal visits can cost anywhere from $100 to $300 per visit without insurance. The number of visits throughout the pregnancy can range from 10 to 15 visits, with more visits typically needed for high-risk pregnancies. This means that the total cost of prenatal care without insurance can be anywhere from $1,000 to $4,500.
It is important to keep in mind that these costs are only for the routine prenatal visits and do not include additional expenses such as lab tests, ultrasounds, and medications. These additional services can significantly increase the overall cost of prenatal care.
For example, prenatal lab work can range from $50 to $200 per test, depending on the type of test and the healthcare provider. Ultrasounds can cost anywhere from $200 to $500 per ultrasound, with multiple ultrasounds usually performed throughout the pregnancy.
Medications prescribed during pregnancy can also add to the cost. Prescription prenatal vitamins can cost anywhere from $10 to $50 per month, while medications for common pregnancy-related conditions such as nausea or gestational diabetes can range from $50 to $200 per prescription.
In addition to the above costs, it is important to consider the cost of prenatal genetic testing and screenings. These tests can assess the risk of certain genetic disorders and birth defects. Non-invasive prenatal testing (NIPT) can range from $800 to $2,500, while other prenatal screenings such as the first-trimester screening and the quad screen typically range from $200 to $500.
It is evident that the cost of prenatal care without insurance can quickly add up, making it crucial for expectant mothers to explore their options for obtaining health insurance coverage. There are several resources available, such as Medicaid or state-sponsored programs, that can provide financial assistance for pregnant women who do not have insurance.
Additionally, many healthcare providers offer sliding scale fees or payment plans to accommodate individuals without insurance. It is essential to discuss financial concerns with your healthcare provider to determine the best approach for managing the costs of prenatal care.
In conclusion, the average cost of a pregnancy doctor visit without insurance can range from $100 to $300 per visit. However, this cost does not include additional expenses such as lab tests, ultrasounds, medications, and prenatal genetic testing. It is crucial for expectant mothers without insurance to explore available resources and options for financial assistance to ensure proper prenatal care for themselves and their babies.
Understanding the Range of Normal Variability in Pregnancy
You may want to see also
Pregnancy can be an exciting and joyous time in a woman's life, but it can also be a time of stress and worry, especially for those without health insurance. The cost of prenatal care and delivery can be overwhelming, but there are options available for pregnant women without insurance to help make pregnancy more affordable.
One option for pregnant women without insurance is to seek out community health clinics or federally qualified health centers. These centers often provide comprehensive prenatal care at a reduced cost or on a sliding scale based on income. They may also be able to connect pregnant women with financial assistance programs or resources to help cover the costs of care.
Another option is to explore Medicaid eligibility. Medicaid is a government-funded health insurance program that provides coverage to low-income individuals and families, including pregnant women. Eligibility requirements vary by state, but many pregnant women may qualify for Medicaid coverage during their pregnancy and for a period after delivery. This can help cover the costs of prenatal care, delivery, and postpartum care.
For those who do not qualify for Medicaid or who are not able to access community health clinics or qualified health centers, some hospitals offer financial assistance or payment plans. Pregnant women without insurance should reach out to hospitals in their area to inquire about any available programs or options for reduced-cost care. It's important to be proactive and discuss financial concerns with healthcare providers to explore potential solutions.
In addition to seeking out low-cost or free healthcare options, pregnant women without insurance can also take steps to reduce the overall cost of pregnancy. This can include researching and comparing prices for prenatal vitamins and other necessary medications, exploring options for childbirth education classes and breastfeeding support, and being mindful of unnecessary medical tests or procedures that may drive up costs.
Finally, pregnant women without insurance should consider looking into maternity support programs or resources in their community. These programs may offer assistance with food, housing, transportation, and other essential needs that can help alleviate some of the financial burden of pregnancy.
While navigating pregnancy without insurance can be challenging, there are options available to make it more affordable. By seeking out community health clinics, exploring Medicaid eligibility, researching hospital financial assistance programs, and being proactive about reducing overall costs, pregnant women without insurance can still receive the care they need during this important time in their lives. It's important to reach out to healthcare providers and community resources for support and guidance throughout the pregnancy journey. Remember, every woman deserves access to quality prenatal care, regardless of insurance status.
When Do Taste Buds Return to Normal During Pregnancy? Understanding Changes in Palate Perception
Pregnancy is an exciting time, but it can also come with unexpected expenses, especially when it comes to healthcare. Without insurance, the cost of a doctor visit during pregnancy can vary based on several factors. In this article, we will explore some of the main factors that can affect the cost of a pregnancy doctor visit without insurance, and provide some tips on how to manage these expenses.
One major factor that can affect the cost of a pregnancy doctor visit is the location. The cost of healthcare services can vary significantly from one area to another, both within and between countries. For example, urban areas tend to have higher healthcare costs compared to rural areas. It is important to research and compare the prices of different healthcare providers in your area to find the most affordable option.
Type of healthcare provider:
The cost of a pregnancy doctor visit can also depend on the type of healthcare provider you choose. Obstetricians, gynecologists, and family doctors all provide pregnancy care, but their fees may differ. Obstetricians specialize in pregnancy and childbirth, so their fees are usually higher compared to family doctors. However, family doctors can still provide excellent care at a more affordable price. It is important to consider your individual needs and budget when choosing a healthcare provider.
Timing and frequency of visits:
The number and timing of pregnancy doctor visits also influence the cost. Typically, the number of visits increases as the pregnancy progresses. During the first trimester, you may have fewer visits, while the third trimester may require more frequent monitoring. Each visit may incur a separate fee, so it is important to plan and budget accordingly. Discussing a schedule and expected costs with your healthcare provider can help you manage these expenses effectively.
Additional tests and procedures:
The cost of a pregnancy doctor visit may increase if additional tests or procedures are required. For example, certain genetic tests, ultrasounds, and bloodwork can add to the overall expenses. It is important to have an open discussion with your healthcare provider to understand which tests are necessary and which ones you can opt out of based on your budget. Being well-informed and asking questions about the necessity and cost of these tests can help you make informed decisions.
Negotiating self-pay rates:
When you do not have insurance, it is possible to negotiate self-pay rates with healthcare providers. Many doctors and hospitals offer discounted rates for self-pay patients. It is important to communicate openly with your healthcare provider about your financial situation and inquire about any available discounts or payment plans. Additionally, exploring free or low-cost clinics, community health centers, or government programs can help offset some of the costs associated with pregnancy care.
In conclusion, the cost of a pregnancy doctor visit without insurance can vary based on several factors. Location, type of healthcare provider, timing and frequency of visits, additional tests and procedures, and the ability to negotiate self-pay rates are all factors that can influence the overall cost. By being proactive, discussing costs with your healthcare provider, and exploring alternative options, you can manage these expenses effectively and ensure a smooth pregnancy journey. Remember, seeking prenatal care is crucial for the health and well-being of both you and your baby, so do not let financial concerns prevent you from seeking the necessary care.
Understanding the Timing of Stretch Marks During Pregnancy
Prenatal care is vital for the health and well-being of both the mother and the baby during pregnancy. However, it can be a financial burden for uninsured pregnant women who may struggle to afford the necessary medical services. Fortunately, there are government programs and clinics that offer discounted or free prenatal care to ensure that every woman has access to the healthcare services she needs.
One such program in the United States is Medicaid. Medicaid is a joint federal and state program that provides health coverage to low-income individuals, including pregnant women. Eligibility and coverage vary by state, but in general, pregnant women with incomes below the poverty level may qualify for Medicaid and receive comprehensive prenatal care at little or no cost. Medicaid covers services such as prenatal visits, lab tests, ultrasounds, and childbirth classes, among others. The program aims to ensure that low-income women have access to the care they need to have a healthy pregnancy and a positive birth experience.
Another government program that provides assistance to uninsured pregnant women is the Children's Health Insurance Program (CHIP). CHIP is a state-run program that offers affordable health insurance coverage to children and pregnant women in low-income households. It provides access to prenatal care, including doctor visits, lab tests, prescription medications, and hospital stays, at a reduced or no cost. The eligibility criteria and coverage options may vary from state to state, but pregnant women in need can check if they qualify for CHIP and receive the prenatal care they require.
In addition to government programs, there are also clinics and nonprofit organizations that offer discounted or free prenatal care to uninsured pregnant women. These clinics are often funded through grants, donations, or government subsidies and aim to provide healthcare services to vulnerable populations, including pregnant women without insurance. Some examples of such clinics include Planned Parenthood, community health centers, and free clinics. These organizations often offer a range of prenatal care services, from routine check-ups to prenatal vitamins and screenings, with fees based on income or provided free of charge.
The process of accessing discounted or free prenatal care for uninsured pregnant women may vary depending on the program or clinic. Some programs require women to meet certain income guidelines and provide documentation of their financial situation. Others may ask for proof of pregnancy, such as a doctor's note or pregnancy test results. It is recommended for pregnant women without insurance to contact their local health department or community organizations to inquire about available programs and clinics in their area. They can also seek assistance from social workers or healthcare providers who can guide them through the application process.
In conclusion, government programs such as Medicaid and CHIP, as well as clinics and nonprofit organizations, provide discounted or free prenatal care to uninsured pregnant women. These programs aim to ensure that every woman has access to the necessary healthcare services during pregnancy, regardless of their financial situation. Pregnant women without insurance should explore these options and reach out to local resources to obtain the prenatal care they need for a healthy pregnancy and the well-being of their baby.
The Optimal Amount of Vitamin C for a Healthy Pregnancy
Pregnancy is a transformative and exciting time in a woman's life. However, it can also be financially challenging, particularly for those without health insurance. Prenatal care is crucial for the health and well-being of both the mother and the baby, but the costs associated with visits to a doctor can add up quickly. This leads many expectant mothers to wonder if it is possible to negotiate the cost of a pregnancy doctor visit without insurance.
The answer to this question is not straightforward, as it largely depends on the healthcare provider and the specific circumstances of the individual. However, there are a few steps that can be taken to potentially reduce the cost of prenatal care:
- Research and comparison: Start by researching the average costs of prenatal visits in your area. This will give you a baseline for negotiation. Contact different healthcare providers and ask for their pricing structure. By comparing costs, you may be able to find a provider with more affordable options.
- Payment plans: Many healthcare providers offer payment plans to patients without insurance. These plans allow patients to break down the cost of their prenatal visits into smaller, more manageable payments. Inquire about any payment options available and discuss your financial situation with the provider. They may be willing to work with you to set up a payment plan that fits your budget.
- Sliding scale fees: Some healthcare providers, particularly community clinics and non-profit organizations, offer sliding scale fees based on income. These fees are often based on a patient's ability to pay, making healthcare services more affordable for those without insurance. Check if there are any clinics or organizations in your area that offer such programs.
- Negotiation: While negotiating healthcare costs may not always be possible, it is worth discussing with your healthcare provider. Speak openly about your financial situation and ask if there is any flexibility in pricing. Depending on the provider, they may be willing to reduce the cost or provide some form of discount.
- Seek out financial assistance programs: There are numerous financial assistance programs available for expectant mothers without insurance. These programs can help cover the costs of prenatal care, including doctor visits. Research government-funded programs, such as Medicaid, as well as local charitable organizations that provide financial assistance to low-income individuals and families.
It is important to approach the negotiation process with open communication and a willingness to compromise. Keep in mind that healthcare providers have costs and expenses to cover, so it's essential to be respectful and understanding. Remember, not all providers may be open to negotiation, but it's worth exploring different options to make prenatal care more affordable.
In conclusion, while negotiating the cost of a pregnancy doctor visit without insurance may not always be possible, there are steps that can be taken to potentially reduce the financial burden. Researching and comparing prices, exploring payment plans and sliding scale fees, negotiating with the healthcare provider, and seeking out financial assistance programs are all strategies that can help make prenatal care more affordable. It is essential to explore all available options and communicate openly with the healthcare provider to find a solution that suits both parties.
Understanding Vagina Pain During Pregnancy: Is It Normal?
Frequently asked questions.
A pregnancy doctor visit without insurance can range in cost, with prices varying depending on the healthcare provider and location. On average, a prenatal visit can cost anywhere from $100 to $300, but this can increase if additional tests or ultrasounds are needed. It's important to contact healthcare providers in your area to get an accurate estimate of costs.
Yes, there are low-cost options available for individuals without insurance who are seeking prenatal care. Some community clinics or federally funded health centers offer sliding scale fees based on income, meaning the cost of the visit will be based on your income level. Additionally, there may be programs or resources available in your area specifically for pregnant individuals without insurance. It's worth reaching out to local healthcare providers or organizations to inquire about these options.
In some cases, it is possible to negotiate the cost of a pregnancy doctor visit without insurance. It's important to be open and honest about your financial situation and discuss your options with the healthcare provider or their billing department. They may be willing to work with you to come up with a payment plan or reduce the cost of the visit. However, it's important to note that not all healthcare providers may be open to negotiating the cost, so it's important to inquire about this possibility before scheduling the visit.

- Elena Tapia Author Editor Reviewer

- Aine Sawyer Author Editor Reviewer
It is awesome. Thank you for your feedback!
We are sorry. Plesae let us know what went wrong?
We will update our content. Thank you for your feedback!
Leave a comment
Complications during pregnancy photos, related posts.

Understanding the Role of Glucose Levels in Pregnancy: Exploring Normal 1-Hour Results
- Dec 28, 2023

Understanding the HCG Levels in Meijer Pregnancy Test
- Jan 02, 2024

The Cost of a Blood Pregnancy Test at Quest: What You Need to Know
- Jan 01, 2024

The Importance of Consuming Liver in Pregnancy: Nutritional Benefits for Both Mother and Baby
- Jan 03, 2024

Potential Risks of Excessive Peanut Butter Consumption During Pregnancy
- Jan 06, 2024

The Timing of the First Ultrasound During Pregnancy: Everything You Need to Know
- Dec 29, 2023
Morning sickness? Prenatal check-ups? What to know about new rights for pregnant workers
Pregnant workers have the right to a wide range of accommodations under new federal regulations for enforcing the Pregnant Workers Fairness Act
Pregnant employees have the right to a wide range of accommodations under new federal regulations for enforcing the Pregnant Workers Fairness Act that supporters say could change workplace culture for millions of people.
The Equal Employment Opportunity Commission, the agency in charge of enforcing the law, adopted an expansive view of conditions related to pregnancy and childbirth in its proposed regulations, including a controversial decision to include abortion, fertility treatment and birth control as medical issues requiring job protections.
The rules, which were adopted on a 3-2 vote along partisan lines, were published Monday and offer extensive guidelines for addressing more routine difficulties of pregnancy, such as morning sickness, back pain and needing to avoid heavy lifting. Labor advocates say the law will be especially transformative for pregnant women in low-wage jobs, who are often denied simple requests like more bathroom breaks.
Here's what to know about the law and the EEOC regulations.
Congress passed the law with bipartisan support in December 2022 following a decade-long campaign by women's rights and labor advocates, who argued that the 1978 Pregnancy Discrimination Act did little to guarantee women would receive the accommodations they might need at work.
The law stated only that pregnant workers should be treated the same as other employees, not that they deserved special consideration. To get their requests met, many pregnant workers therefore needed to demonstrate they had physical limitations covered under the Americans With Disabilities Act, often creating insurmountable hurdles.
The new law treats pregnancy and related conditions as themselves deserving of “reasonable accommodations” and places the burden on employers to prove “undue hardships” for denying any requests.
The law applies to employers of at least 15 workers. The EEOC estimates it will cover roughly 1.5 million pregnant workers in any given year. The EEOC regulations published April 15 are set to go into effect in June.
The EEOC's 400-page document encompasses a wide array of conditions and relevant advice for employers.
It states that workers are entitled to unpaid time off for situations such as prenatal appointments, fertility treatments, abortion, miscarriage, postpartum depression and mastitis, an infection that arises from breastfeeding. This includes workers who are not covered by federal family leave laws and those who have not been on the job long enough to accrue time off.
Workers can ask for flexible working arrangements to deal with morning sickness, such as a later start time, clearance to work from home or permission to carry snacks in workplaces where eating is typically prohibited. If they can't sit or stand for extended periods due to sciatica, which is common in late pregnancy, they can request a schedule adjustment so their commutes happen during less crowded hours.
The regulations also allow workers to be exempted from tasks such as climbing ladders or heavy lifting. If those duties are essential to their jobs, they can still request a temporary dispensation, according to the EEOC.
Employers don’t have to accommodate workers exactly as requested but they must offer reasonable alternatives. They cannot deny a request without clearing a high bar to prove doing so would cause “undue hardships” for the organization’s finances or operations. They cannot force workers to take unpaid leave if a reasonable accommodation is available.
The EEOC emphasizes that it “should not be complicated or difficult” for pregnant workers to request accommodations. Workers don't have to make requests in writing, use specific words, cite any laws, or in most cases, provide documentation such as doctors' notes. Employers must respond quickly and have a conversation about how to reasonably accommodate a worker’s needs.
Still, legal experts advise both workers and employers to document the process. A Better Balance, the non-profit that spearheaded the 10-year campaign for the law's passage, advises workers to familiarize themselves with their legal rights and be as specific as possible about their limitations and the changes they they need.
Workers who believe a request was denied illegally can file a complaint with the EEOC. They have 180 days to do so, though the deadline can be extended in some states.
The EEOC included abortion among the conditions covered under the law. The rules state, however, that employers are not obligated to cover expenses related to the procedure or to offer health insurance that does.
The EEOC regulations argue that including abortion is consistent with the agency's longstanding interpretation of other laws under Title VII of the 1964 Civil Rights Act, including the Pregnancy Discrimination Act.
But the decision drew condemnation from Republican lawmakers who had championed the law's passage. The five-member EEOC's two Republican members voted against the regulations.
In a statement explaining her dissent, Commissioner Andrea Lucas said the agency broadened the scope of the law “to reach virtually every condition, circumstance, or procedure that relates to any aspect of the female reproductive system" in ways that "cannot reasonably be reconciled with the text" of the law.
Melissa Losch, a labor and employment attorney at the New Orleans-based firm McGlinchey Stafford, said she expects the regulations to give rise to further litigation. Losch cited the example of a worker living in a state with a restrictive abortion law requesting time off to undergo the procedure in another state. The EEOC rules provide “no good answer” about whether granting such a request would conflict with restrictive state abortion laws, she added.
On February 27, a federal judge blocked enforcement of the Pregnant Workers Fairness Act for Texas state employees, a ruling that came in response to a lawsuit filed by Texas Attorney General Ken Paxton. Paxton argued the law was unconstitutional because it was part of a spending bill that passed in the House without a majority of members present, and the judge ruled in his favor.
Gedmark, of A Better Balance, said she was optimistic the Biden administration would prevail in its expected appeal of the ruling. In the meantime, federal and private sectors workers in Texas are covered by the law.
But in her dissenting statement, Lucas warned that if the Texas case or any future lawsuits succeed in overturning the law, the EEOC's divisive rules have “all but extinguished” the chances of a bipartisan effort to reenact it.
Employers have been obligated to abide by the Pregnant Workers Fairness Act since it took effect on June 27, 2023, though the EEOC regulations provided guidance on how to do so.
The law swiftly made a difference to many low-wage workers, according to Gedmark.
A Better Balance, which operates a helpline, has “heard an overwhelmingly positive experience from workers,” she said. Last summer, the organization worked with some women whose employers stopped resisting requests for accommodations as soon as the law took effect, Gedmark said.
Some workers reported their employers were still operating under the old legal framework, handing them pages of disability paperwork to fill out in response to requests.
The EEOC said it received almost 200 complaints alleging violations of the law by the time the fiscal year ended on Sept. 30, 2023.
Gedmark said the success of the law will depend on enforcement and raising awareness.
“If workers don’t know about the law and don’t know about their rights, then it really undermines the purpose of the law,” she said.
The Associated Press’ women in the workforce and state government coverage receives financial support from Pivotal Ventures. AP is solely responsible for all content. Find AP’s standards for working with philanthropies, a list of supporters and funded coverage areas at AP.org.
Top Stories

Trump hush money trial: Judge sets opening statements for Monday
- Apr 19, 5:15 PM

State law takes US a step closer to popular vote deciding presidential elections
- 2 hours ago

USC cancels all commencement speakers after canceled valedictorian speech
- Apr 19, 10:02 PM

Savannah Chrisley talks about the fate of her parents Todd and Julie
- Apr 19, 6:48 PM

2 children dead, 15 people injured after vehicle crashes into building
- Apr 20, 9:20 PM
ABC News Live
24/7 coverage of breaking news and live events

Emergency rooms refused to treat pregnant patients, leaving one woman to miscarry in a lobby restroom
O ne woman miscarried in the lobby restroom of a Texas emergency room as front desk staff refused to admit her. Another learned at a Florida hospital that her fetus had no heartbeat, the day after a security guard turned her away from the facility. And in North Carolina, a woman gave birth in a car after an emergency room couldn't offer an ultrasound. The baby died.
Complaints that pregnant women were turned away from U.S. emergency rooms spiked in 2022 after the U.S. Supreme Court overturned Roe vs. Wade , federal documents obtained by the Associated Press reveal.
The cases raise alarms about the state of emergency pregnancy care in the U.S., especially in states that enacted strict abortion laws, and sparked confusion around the treatment doctors can provide.
“It is shocking, it’s absolutely shocking,” said Amelia Huntsberger, an OB-GYN in Oregon. “It is appalling that someone would show up to an emergency room and not receive care — this is inconceivable.”
Federal law requires emergency rooms to treat or stabilize patients who are in active labor or, if they lack the staff or resources to do so, provide a medical transfer to another hospital. Medical facilities must comply with the law if they accept Medicare funding.
The Supreme Court will hear arguments Wednesday that could weaken those protections. The Biden administration has sued Idaho over its abortion ban, even in medical emergencies, arguing that it conflicts with the federal law.
“No woman should be denied the care she needs,” Jennifer Klein, director of the White House Gender Policy Council, said in a statement. “All patients, including women who are experiencing pregnancy-related emergencies, should have access to emergency medical care required under the Emergency Medical Treatment and Labor Act.”
Pregnancy care after Roe
Pregnant patients have “become radioactive to emergency departments” in states with extreme abortion restrictions, said Sara Rosenbaum, a George Washington University health law and policy professor.
“They are so scared of a pregnant patient that the emergency medicine staff won’t even look. They just want these people gone," Rosenbaum said.
Consider what happened to a woman who was nine months pregnant and having contractions when she arrived at the Falls Community Hospital in Marlin, Texas, in July 2022, a week after the Supreme Court’s ruling on abortion. The doctor on duty refused to see her.
“The physician came to the triage desk and told the patient that we did not have obstetric services or capabilities,” hospital staff told federal investigators during interviews, according to documents. “The nursing staff informed the physician that we could test her for the presence of amniotic fluid. However, the physician adamantly recommended the patient drive to a Waco hospital.”
Investigators with the Centers for Medicare and Medicaid Services concluded that Falls Community Hospital broke the law.
Reached by phone, an administrator at the hospital declined to comment on the incident.
The investigation was one of dozens the AP obtained from a Freedom of Information Act request filed in February 2023 that sought all pregnancy-related Emergency Medical Treatment and Labor Act complaints from the previous year. One year after submitting the request, the federal government agreed to release only some complaints and investigative documents filed across just 19 states. The names of patients, doctors and medical staff were redacted from the documents.
Federal investigators looked into just over a dozen pregnancy-related complaints in those states during the months leading up to the U.S. Supreme Court's pivotal ruling on abortion in 2022. But more than two dozen complaints about emergency pregnancy care were lodged in the months after the decision was unveiled. It is not known how many complaints were filed last year, as the records request asked only for those from 2022, and the information is not otherwise publicly available.
The documents did not detail what happened to the patient turned away from the Falls Community Hospital.
'She is bleeding a lot'
Other pregnancies ended in catastrophe, the documents show.
At Sacred Heart Emergency Center in Houston, front desk staff refused to check in a woman after her husband asked for help delivering her baby that September. She miscarried in a restroom toilet in the emergency room lobby while her husband called 911 for help.
“She is bleeding a lot and had a miscarriage,” the husband told first responders in his call, which was transcribed from Spanish in federal documents. “I’m here at the hospital, but they told us they can’t help us because we are not their client.”
Emergency crews, who arrived 20 minutes later and transferred the woman to a hospital, appeared confused over the staff's refusal to help her, according to 911 call transcripts.
One first responder told federal investigators that when a Sacred Heart Emergency Center staffer was asked about the gestational age of the fetus, the staffer replied: “No, we can’t tell you; she is not our patient. That’s why you are here.”
A manager for Sacred Heart Emergency declined to comment. The facility is licensed in Texas as a freestanding emergency room, which means it is not physically connected to a hospital. State law requires those facilities to treat or stabilize patients, a spokeswoman for the Texas Health and Human Services agency said in an email to AP.
Sacred Heart Emergency’s website says it no longer accepts Medicare, a change that was made after the woman miscarried, according to publicly available archives of the website.
Meanwhile, the staff at Person Memorial Hospital in Roxboro, N.C., told a pregnant woman who was complaining of stomach pain that they would not be able to provide her with an ultrasound. The staff failed to tell her how risky it could be for her to depart without being stabilized, according to federal investigators. While en route to another hospital 45 minutes away, the woman gave birth in a car to a baby who did not survive.
Person Memorial Hospital self-reported the incident. A spokeswoman said the hospital continues to “provide ongoing education for our staff and providers to ensure compliance.”
In Melbourne, Fla., a security guard at Holmes Regional Medical Center refused to let a pregnant woman into the triage area because she had brought a child with her. When the patient came back the next day, medical staff were unable to locate a fetal heartbeat. The center declined to comment on the case.
What's the penalty?
Emergency rooms are subject to hefty fines when they turn away patients or fail to stabilize them or transfer them to another hospital. Violations can also put hospitals' Medicare funding at risk.
But it’s unclear what fines might be imposed on more than a dozen hospitals that the Biden administration says failed to properly treat pregnant patients in 2022.
It can take years for fines to be levied in these cases. The Health and Human Services agency, which enforces the law, declined to share if the hospitals have been referred to the agency's Office of Inspector General for penalties.
For Huntsberger, the OB-GYN, the Emergency Medical Treatment and Labor Act, or EMTLA, was one of the few ways she felt protected to treat pregnant patients in Idaho, despite the state's abortion ban. She left Idaho last year to practice in Oregon because of the ban.
The threat of fines or loss of Medicare funding for violating EMTLA is a big deterrent that keeps hospitals from dumping patients, she said. Many couldn't keep their doors open if they lost Medicare funding.
She has been waiting to see how HHS penalizes two hospitals in Missouri and Kansas. HHS announced last year it was investigating the facilities after a woman who was in preterm labor at 17 weeks was denied an abortion.
“A lot of these situations are not reported, but even the ones that are — like the cases out of the Midwest — they're investigated, but nothing really comes of it,” Huntsberger said. “People are just going to keep providing substandard care or not providing care. The only way that changes is things like this.”
Next up for EMTLA
President Biden and Health and Human Services Secretary Xavier Becerra have publicly vowed vigilance in enforcing the law.
Even as states have enacted strict abortion laws, the White House has argued that if hospitals receive Medicare funds, they must provide stabilizing care, including abortions.
In a statement to the AP, Becerra called EMTLA the “nation's bedrock law protecting Americans' right to life- and health-saving emergency medical care.”
“And doctors, not politicians, should determine what constitutes emergency care," he added.
Idaho’s law allows abortion only if the life, not the health, of the woman is at risk. But the state's attorney general has argued that its abortion ban is “consistent” with federal law, which calls for emergency rooms to protect a fetus in medical emergencies.
"The Biden administration has no business rewriting federal law to override Idaho’s law and force doctors to perform abortions,” state Atty. Gen. Raúl Labrador said in a statement this year.
Now the Supreme Court will weigh in. The case could have implications in other states, including Arizona, which is reinstating an 1864 law that bans all abortions, with an exception only if the woman's life is at risk.
The Emergency Medical Treatment and Labor Act was introduced decades ago because private hospitals would dump patients, often those without insurance, on county or state hospitals, said Alexa Kolbi-Molinas of the American Civil Liberties Union. Some hospitals also refused to see pregnant women who did not have an established relationship with physicians on staff. If the court nullifies or weakens those protections, it could result in more hospitals turning away patients without fear of penalty from the federal government, she said.
“The government knows there’s a problem and is investigating and is doing something about that,” Kolbi-Molinas said. “Without EMTALA, they wouldn’t be able to do that.”
Seitz writes for the Associated Press.
This story originally appeared in Los Angeles Times .

- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- Auto Racing
- 2024 Paris Olympic Games
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Morning sickness? Prenatal check-ups? What to know about new rights for pregnant workers
FILE - The emblem of the U.S. Equal Employment Opportunity Commission is shown on a podium in Vail, Colo., Tuesday, Feb. 16, 2016, in Denver. Pregnant workers have the right to a wide range of accommodations under new federal regulations for implementing the Pregnant Workers Fairness Act. The regulations take an expansive view of conditions related to pregnancy, from fertility treatments to abortion and post-childbirth complications. (AP Photo/David Zalubowski, File)
- Copy Link copied
Pregnant employees have the right to a wide range of accommodations under new federal regulations for enforcing the Pregnant Workers Fairness Act that supporters say could change workplace culture for millions of people.
The Equal Employment Opportunity Commission, the agency in charge of enforcing the law, adopted an expansive view of conditions related to pregnancy and childbirth in its proposed regulations, including a controversial decision to include abortion, fertility treatment and birth control as medical issues requiring job protections.
The rules, which were adopted on a 3-2 vote along partisan lines, were published Monday and offer extensive guidelines for addressing more routine difficulties of pregnancy, such as morning sickness, back pain and needing to avoid heavy lifting. Labor advocates say the law will be especially transformative for pregnant women in low-wage jobs, who are often denied simple requests like more bathroom breaks.
Here’s what to know about the law and the EEOC regulations.
WHAT IS THE PREGNANT WORKERS FAIRNESS ACT?
Congress passed the law with bipartisan support in December 2022 following a decade-long campaign by women’s rights and labor advocates, who argued that the 1978 Pregnancy Discrimination Act did little to guarantee women would receive the accommodations they might need at work.
The law stated only that pregnant workers should be treated the same as other employees, not that they deserved special consideration. To get their requests met, many pregnant workers therefore needed to demonstrate they had physical limitations covered under the Americans With Disabilities Act, often creating insurmountable hurdles.
The new law treats pregnancy and related conditions as themselves deserving of “reasonable accommodations” and places the burden on employers to prove “undue hardships” for denying any requests.
The law applies to employers of at least 15 workers . The EEOC estimates it will cover roughly 1.5 million pregnant workers in any given year. The EEOC regulations published April 15 are set to go into effect in June.
WHAT ARE WORKERS ENTITLED TO?
The EEOC’s 400-page document encompasses a wide array of conditions and relevant advice for employers.
It states that workers are entitled to unpaid time off for situations such as prenatal appointments , fertility treatments, abortion, miscarriage, postpartum depression and mastitis, an infection that arises from breastfeeding. This includes workers who are not covered by federal family leave laws and those who have not been on the job long enough to accrue time off.
Workers can ask for flexible working arrangements to deal with morning sickness, such as a later start time, clearance to work from home or permission to carry snacks in workplaces where eating is typically prohibited. If they can’t sit or stand for extended periods due to sciatica, which is common in late pregnancy, they can request a schedule adjustment so their commutes happen during less crowded hours.
The regulations also allow workers to be exempted from tasks such as climbing ladders or heavy lifting. If those duties are essential to their jobs, they can still request a temporary dispensation, according to the EEOC.
Employers don’t have to accommodate workers exactly as requested but they must offer reasonable alternatives. They cannot deny a request without clearing a high bar to prove doing so would cause “undue hardships” for the organization’s finances or operations. They cannot force workers to take unpaid leave if a reasonable accommodation is available.
HOW SHOULD WORKERS REQUEST ACCOMMODATIONS?
The EEOC emphasizes that it “should not be complicated or difficult” for pregnant workers to request accommodations. Workers don’t have to make requests in writing, use specific words, cite any laws, or in most cases, provide documentation such as doctors’ notes. Employers must respond quickly and have a conversation about how to reasonably accommodate a worker’s needs.
Still, legal experts advise both workers and employers to document the process. A Better Balance, the non-profit that spearheaded the 10-year campaign for the law’s passage, advises workers to familiarize themselves with their legal rights and be as specific as possible about their limitations and the changes they they need.
Workers who believe a request was denied illegally can file a complaint with the EEOC . They have 180 days to do so, though the deadline can be extended in some states.
WHAT DO THE EEOC RULES SAY ABOUT ABORTION?
The EEOC included abortion among the conditions covered under the law. The rules state, however, that employers are not obligated to cover expenses related to the procedure or to offer health insurance that does.
The EEOC regulations argue that including abortion is consistent with the agency’s longstanding interpretation of other laws under Title VII of the 1964 Civil Rights Act, including the Pregnancy Discrimination Act.
But the decision drew condemnation from Republican lawmakers who had championed the law’s passage. The five-member EEOC’s two Republican members voted against the regulations.
In a statement explaining her dissent, Commissioner Andrea Lucas said the agency broadened the scope of the law “to reach virtually every condition, circumstance, or procedure that relates to any aspect of the female reproductive system” in ways that “cannot reasonably be reconciled with the text” of the law.
Melissa Losch, a labor and employment attorney at the New Orleans-based firm McGlinchey Stafford, said she expects the regulations to give rise to further litigation. Losch cited the example of a worker living in a state with a restrictive abortion law requesting time off to undergo the procedure in another state. The EEOC rules provide “no good answer” about whether granting such a request would conflict with restrictive state abortion laws, she added.
ARE WORKERS IN TEXAS COVERED?
On February 27, a federal judge blocked enforcement of the Pregnant Workers Fairness Act for Texas state employees, a ruling that came in response to a lawsuit filed by Texas Attorney General Ken Paxton. Paxton argued the law was unconstitutional because it was part of a spending bill that passed in the House without a majority of members present, and the judge ruled in his favor.
Gedmark, of A Better Balance, said she was optimistic the Biden administration would prevail in its expected appeal of the ruling. In the meantime, federal and private sectors workers in Texas are covered by the law.
But in her dissenting statement, Lucas warned that if the Texas case or any future lawsuits succeed in overturning the law, the EEOC’s divisive rules have “all but extinguished” the chances of a bipartisan effort to reenact it.
WHAT HAS THE LAW’S IMPACT BEEN SO FAR?
Employers have been obligated to abide by the Pregnant Workers Fairness Act since it took effect on June 27, 2023, though the EEOC regulations provided guidance on how to do so.
The law swiftly made a difference to many low-wage workers, according to Gedmark.
A Better Balance, which operates a helpline, has “heard an overwhelmingly positive experience from workers,” she said. Last summer, the organization worked with some women whose employers stopped resisting requests for accommodations as soon as the law took effect, Gedmark said.
Some workers reported their employers were still operating under the old legal framework, handing them pages of disability paperwork to fill out in response to requests.
The EEOC said it received almost 200 complaints alleging violations of the law by the time the fiscal year ended on Sept. 30, 2023.
Gedmark said the success of the law will depend on enforcement and raising awareness.
“If workers don’t know about the law and don’t know about their rights, then it really undermines the purpose of the law,” she said.
The Associated Press’ women in the workforce and state government coverage receives financial support from Pivotal Ventures. AP is solely responsible for all content. Find AP’s standards for working with philanthropies, a list of supporters and funded coverage areas at AP.org.


COMMENTS
The consequences are not only poor health, but also higher costs in the long run. The average medical cost for a baby with problems of prematurity is $79,000, compared to $1,000 for a healthy ...
The good news: Insurers cannot deny coverage to uninsured moms-to-be. Thanks to the Affordable Care Act (ACA), also called Obamacare, private insurance companies are required to cover preexisting conditions, including pregnancy. However, there's always a chance that Congress could overturn Obamacare and pregnancy may once again become a pre ...
Step 1: Understand the true costs of prenatal care without insurance. If you find yourself pregnant and uninsured, you may be wary of the extra steps and responsibility involved in getting insurance at this already-stressful time in your life. However, do not underestimate the importance of insurance during your pregnancy.
Typical prenatal appointment schedule. The number of visits you'll have in a typical pregnancy usually total about 10 to 15, depending on when you find out you're expecting and the timing of your first checkup. In most complication-free pregnancies, you can expect to have a prenatal appointment with the following frequency: Weeks 4 to 28 ...
Local Health Department. Your local health department will be able to tell you where a prenatal care clinic is run. They may have one that they run or can help you find free or reduced prices on prenatal care depending on your income level. You can call 1-800-311-BABY (1-800-311-2229) to connect you to your local healthcare department.
Most insurance plans cover the cost of prenatal care. If you don't have health insurance, you may be able to get low-cost or free prenatal care from Planned Parenthood, community health centers, or other family planning clinics. You might also qualify for health insurance through your state if you're pregnant.
If you don't have health insurance or can't afford prenatal care, find out about free or low-cost prenatal care services in your community: Call (800) 311-BABY [ (800) 311-2229]. For information in Spanish, call (800) 504-7081. Visit healthcare.gov to find a community health center near you.
Your doctor will give you a schedule of all the doctor's visits you should have while pregnant. Most experts suggest you see your doctor: About once each month for weeks 4 through 28; Twice a month for weeks 28 through 36; Weekly for weeks 36 to birth; If you are older than 35 or your pregnancy is high risk, you'll probably see your doctor more ...
Prenatal care: 1st trimester visits. Pregnancy and prenatal care go hand in hand. During the first trimester, prenatal care includes blood tests, a physical exam, conversations about lifestyle and more. By Mayo Clinic Staff. Prenatal care is an important part of a healthy pregnancy. Whether you choose a family physician, obstetrician, midwife ...
Pregnancy complications, including conditions such as gestational diabetes, miscarriage, high blood pressure, preeclampsia and more. Negative effects on the baby, such as preterm delivery or low birth weight. Worsening of chronic conditions, such as diabetes, asthma and heart problems. Ante- and post-partum depression and other mental illnesses.
This initial visit will probably be one of the longest. It will be helpful if you arrive prepared with vital dates and information. This is also a good opportunity to bring a list of questions that you and your partner have about your pregnancy, prenatal care, and birth options. What to Expect at Your First Pregnancy Appointment Your doctor ...
The amount your obstetrician charges for each visit could range from about $90 to more than $500. Other services, such as ultrasounds and laboratory tests, are typically billed separately and cost upwards of $100 each. And special tests like an amniocentesis can cost more than $2,500. Women typically have 10 to 15 prenatal visits over the ...
Check your weight, blood pressure, and urine. Check for swelling. Measure your abdomen. Check the position of your baby. Listen to your baby's heartbeat. Perform other exams and order tests, as appropriate. Give you the appropriate vaccinations. Closely monitor any complications you have or that you develop, and intervene if necessary.
There are also complications that may show up after you become pregnant, like pregnancy-related high blood pressure, which can require more frequent visits. Pregnancy appointments timeline example. Visit #1: 6-10 weeks. Visit #2: 10-12 weeks. Visit #3: 16-18 weeks. Visit #4: 20-22 weeks. Visit #5: 24-28 weeks. Visit #6: 32 weeks. Visit #7: 36 weeks
If you don't have health insurance, you can still get help paying for medical care during pregnancy: Get connected with free or low-cost services in your state by calling 1-800-311-BABY (1-800-311-2229) Find a health center near you and ask about prenatal care. Learn more about health insurance options for pregnant people.
Medicaid and CHIP provide free or low-cost health coverage to millions of Americans, including some low-income people, families and children, and pregnant women. Eligibility for these programs depends on your household size, income, and citizenship or immigration status. Specific rules and benefits vary by state.
Your first appointment will be the longest of your first trimester visits. At this initial visit, your healthcare provider will confirm your pregnancy and perform a full physical and pelvic exam. He or she will also do a Pap test to check for cervical cancer and vaginal infections. The staff will check your weight and blood pressure.
Find out steps you can take to have a healthy pregnancy — including information on doctor or midwife visits and tips to help you eat healthy and stay active ... Find out how your doctor or midwife can help you have a healthy pregnancy. Nutrition and Physical Activity. Eating healthy and staying active can help you have a healthy pregnancy ...
Pregnancy is one of the most common reasons for a hospitalization among non-elderly people. In addition to the cost of the birth itself, pregnancy care also involves costs associated with prenatal visits and often includes care to treat psychological and medical conditions associated with pregnancy, birth, and the post-partum period. To examine the health costs […]
A 2020 study published in the journal Health Affairs [2] found that for women with employer-based insurance, the average out-of-pocket cost of a vaginal birth increased from $2,910 in 2008 to $4,314 in 2015, with the cost of a C-section going from $3,364 to $5,161 during that same time period.
Pregnancy, maternity, and newborn care collectively make up 1 of the 10 essential health benefits that the Affordable Care Act (ACA) says qualified health plans must cover. Under the ACA, insurance plans must cover as many prenatal visits as your provider thinks you need, without cost to you. Most routine tests are included in your regular ...
The vast majority of abortions occur during the first trimester of a pregnancy. In 2021, 93% of abortions occurred during the first trimester - that is, at or before 13 weeks of gestation, according to the CDC. An additional 6% occurred between 14 and 20 weeks of pregnancy, and about 1% were performed at 21 weeks or more of gestation.
Complaints that pregnant women were turned away from US emergency rooms spiked in 2022 after the US supreme court overturned Roe v Wade, federal documents obtained by the Associated Press reveal.
The cases raise alarms about the state of emergency pregnancy care in the U.S., especially in states that enacted strict abortion laws and sparked confusion around the treatment doctors can provide.
On average, prenatal visits can cost anywhere from $100 to $300 per visit without insurance. The number of visits throughout the pregnancy can range from 10 to 15 visits, with more visits typically needed for high-risk pregnancies. This means that the total cost of prenatal care without insurance can be anywhere from $1,000 to $4,500.
FILE - The emblem of the U.S. Equal Employment Opportunity Commission is shown on a podium in Vail, Colo., Tuesday, Feb. 16, 2016, in Denver. Pregnant workers have the right to a wide range of ...
The cases raise alarms about the state of emergency pregnancy care in the U.S., especially in states that enacted strict abortion laws, and sparked confusion around the treatment doctors can provide.
Pregnant employees have the right to a wide range of accommodations under new federal regulations for enforcing the Pregnant Workers Fairness Act that supporters say could change workplace culture for millions of people.. The Equal Employment Opportunity Commission, the agency in charge of enforcing the law, adopted an expansive view of conditions related to pregnancy and childbirth in its ...