

List With Office Visit CPT Codes (New & Established Patients)
The CPT codes for office visits can be found in the CPT manual; under range CPT 99202 until 99205 for office visits of new patients . For office visits of established patients, you can use range 99211 to CPT code 99215. We also included CPT 99070 in case you need to bill extra supplies/materials for office visits and CPT code 99072 if extra staff and supplies were needed during a Public Health Emergency.
CPT Code 99070
Long description of CPT 99070 : Supplies and materials [except spectacles] provided by the physician or other qualified health care professional over and above those usually included with the office visit or other services rendered [list drugs, trays, supplies, or materials provided].
Short description: Extra supplies/materials for office visit.
CPT Code 99072
Long description of CPT 99072 : Additional supplies, materials, and clinical staff time over and above those usually included in an office visit or other non-facility service[s], when performed during a Public Health Emergency, as defined by law, due to respiratory-transmitted infectious disease.
Short description: Extra supplies and staff time for office visits during Public Health Emergency.
CPT Code 99202
Long description of CPT 99202 : Office or other outpatient visit for the evaluation and management of a new patient , which requires a medically appropriate history and/or examination and straightforward medical decision making. When using time for code selection, 15-29 minutes of total time is spent on the date of the encounter.
Short description: 15-29 minute office visit for new patient evaluation and management.
CPT Code 99203
Long description of CPT 99203 : Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 30-44 minutes of total time is spent on the date of the encounter.
Short description: 30-44 minute office visit for new patient evaluation and management.
CPT Code 99204
Long description of CPT 99204 : Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and moderate level of medical decision making. When using time for code selection, 45-59 minutes of total time is spend on the date of the encounter.
Short description: 45-59 minute office visit for new patient evaluation and management.
CPT Code 99205
Long description of CPT 99205 : Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and high level of medical decision making. When using time for code+ selection, 60-74 minutes of total time is spent on the date of the encounter.
Short description: 60-74 minute office visit for new patient evaluation and management.
CPT Code 99211
Long description of CPT 99211 : Office or other outpatient visit for the evaluation and management of an established patient that may not require the presence of a physician or other qualified health care professional
Short description: Short office visit for established patient management.
CPT Code 99212
Long description of CPT Code 99212 : Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and straightforward medical decision making. When using time for code selection, 10-19 minutes of total time spent on the date of the encounter.
Short description: 10-19 minute office visit for established patient management.
CPT Code 99213
Long description of CPT 99213 : Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 20-29 minutes of total time is spent on the date of the encounter.
Short description: 20-29 minute office visit for established patient management.
CPT Code 99214
Long description of CPT 99214 : Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and moderate level of medical decision-making. When using time for code selection, 30-39 minutes of total time is spend on the date of the encounter.
Short description: 30-39 minutes office visit for established patient management.
CPT Code 99215
Long description of CPT 99215 : Office or other outpatient visit for the evaluation and management of an established patient, which requires medically appropriate history and/or examination and high level of medical decision making. When using time for code selection, 40-54 minutes of total time is spent on the date of the encounter.
Short description: 40-54 minutes office visit for established patient management .
https://www.aapc.com/codes/cpt-codes-range/99211-99215/
https://www.aapc.com/codes/cpt-codes-range/99202-99205/
https://www.aapc.com/codes/cpt-codes/99070
https://www.aapc.com/codes/cpt-codes/99072
Similar Posts
How to use cpt code 01938.
cpt 01938 describes the anesthesia services provided by a healthcare professional during percutaneous image-guided injection, drainage, or aspiration procedures on the lumbar or sacral spine or spinal cord. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information, and examples of cpt 01938. 1. What is cpt 01938?…
How To Use CPT Code 81252
CPT 81252 describes the analysis of the full gene sequence for GJB2, also known as gap junction protein, beta 2, 26kDa, connexin 26. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information, similar codes and billing examples. 1. What is CPT Code 81252? CPT 81252 is used…
How To Use CPT Code 29855
CPT 29855 describes the arthroscopically aided treatment of a tibial fracture, specifically the proximal (plateau) region. This article will cover the official description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 29855? CPT 29855 is used to describe a specific procedure known as arthroscopically…
How To Use CPT Code 26450
CPT 26450 describes a surgical procedure known as tenotomy, specifically the open division of a flexor tendon in the palm. This article will provide an overview of CPT code 26450, including its official description, the procedure itself, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code…
How To Use CPT Code 85378
CPT 85378 describes the qualitative or semiquantitative testing of fibrin degradation products, specifically D-dimer, in patient blood or plasma. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information, similar codes and billing examples. 1. What is CPT Code 85378? CPT 85378 can be used to describe the…
How To Use CPT Code 49999
CPT 49999 describes a procedure performed on the peritoneum and omentum in the abdomen that does not have a specific code. This article will cover the description, official description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 49999? CPT 49999 can be used to…
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- ACS Foundation
- Diversity, Equity, and Inclusion
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- E/M Coding and Billing Res...
- Office/Outpatient E/M Visi...
Office/Outpatient E/M Codes
2021 e/m office/outpatient visit cpt codes.
The tables below highlight the changes to the office/outpatient E/M code descriptors effective in 2021.
More details about these office/outpatient E/M changes can be found at CPT® Evaluation and Management (E/M) Office or Other Outpatient (99202-99215) and Prolonged Services (99354, 99355, 99356, 99XXX) Code and Guideline Changes.
All specific references to CPT codes and descriptions are © 2023 American Medical Association. All rights reserved. CPT and CodeManager are registered trademarks of the American Medical Association.
Download the Office E/M Coding Changes Guide (PDF)

CPT CODE 99381, 99382 – 99385 – Preventive visit new patient
Sep 25, 2016 | Medical billing basics
CPT Code and description
99381 – Initial comprehensive preventive medicine evaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, new patient; infant (age younger than 1 year)
99382 – Initial comprehensive preventive medicine evaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, new patient; early childhood (age 1 through 4 years)
99383 – Initial comprehensive preventive medicine evaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, new patient; late childhood (age 5 through 11 years) – Average fee amount $110 – $130
99384 – Initial comprehensive preventive medicine evaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, new patient; adolescent (age 12 through 17 years) Average fee amount $120 – $140
99385 – Initial comprehensive preventive medicine evaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, new patient; 18-39 years – Average fee amount – $120 – $ 150
Preventive Medicine Services [Current Procedural Terminology (CPT®) codes 99381-99387, 99391-99397 , Healthcare Common Procedure Coding System (HCPCS) code G0402] are comprehensive in nature, reflect an age and gender appropriate history and examination, and include counseling, anticipatory guidance, and risk factor reduction interventions, usually separate from disease-related diagnoses. Occasionally, an abnormality is encountered or a preexisting problem is addressed during the Preventive visit, and significant elements of related Evaluation and Management (E/M) services are provided during the same visit. When this occurs, Oxford will reimburse Preventive Medicine service plus 50% the Problem-Oriented E/M service code when that code is appended with modifier 25. If the Problem-Oriented service is minor, or if the code is not submitted with modifier 25 appended, it will not be reimbursed.
When a Preventive Medicine service and Other E/M services are provided during the same visit, only the Preventive Medicine service will be reimbursed.
Screening services include cervical cancer screening; pelvic and breast examination; prostate cancer screening/digital rectal examination; and obtaining, preparing and conveyance of a Papanicolaou smear to the laboratory. These Screening procedures are included in (and are not separately reimbursed from) the Preventive Medicine service rendered on the same day.
Prolonged services are included in (and not separately reimbursed from) Preventive Medicine codes.
Counseling services are included in (and not separately reimbursed from) Preventive Medicine codes.
Medical Nutrition Therapy services are included in (and not separately reimbursed from) Preventive Medicine codes.
Visual function screening and Visual Acuity screening are included in (and not separately reimbursed from) Preventive Medicine services.
For a list of specific codes that are included in (and not separately reimbursed from) Preventive Medicine Services see the Applicable Codes section below.
For the purposes of this policy, Same Specialty Physician, Hospital, Ambulatory Surgical Center or Other Health Care Professional is defined as a physician, hospital, ambulatory surgical center, and/or other health care professional of the same group and Same Specialty Physician, Hospital, Ambulatory Surgical Center or Other Health Care Professional reporting the same Federal Tax Identification number.
PREVENTIVE MEDICINE SERVICES, NEW PATIENT
Initial comprehensive preventive medicine evaluation and management of an individual including an age- and gender-appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of appropriate immunizations, laboratory/diagnostic procedures for a new patient.
Code Description
99381 Infant (age under 1 year) 99382 Early childhood (ages 1 through 4 years) 99383 Late childhood (ages 5 through 11 years) 99384 Adolescent (ages 12 through 17 years) 99385 18–39 years 99386 40–64 years 99387 65 years and over
PREVENTIVE MEDICINE SERVICES, ESTABLISHED PATIENT
Periodic comprehensive preventive medicine re-evaluation and management of an individual, including an age- and gender-appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of appropriate immunizations, laboratory/diagnostic procedures for an established patient.
Code Description 99391 Infant (age under 1 year) 99392 Early childhood (ages 1 through 4 years) 99393 Late childhood (ages 5 through 11 years) 99394 Adolescent (ages 12 through 17 years) 99395 18–39 years 99396 40–64 years 99397 65 years and over
New versus Established client: A new client is defined as one who has not received any professional services from a physician/qualified health care professional in your health department, within the last three years, for a billable visit that includes some level of evaluation and management (E/M) service coded as a preventive service using 99381-99387 or 99391-99397, or as an evaluation & management service using 99201-99205 and 99211-99215. If the client’s only visit to the Health Department is WIC or immunizations without one of the above service codes, it does not affect the designation of the client as a new client; the client can still be NEW. Remember that a client may be new to a program but established to the health department if they have received any professional services from a physician/qualified health care professional.
In this case, you would use the forms for a “new” patient for that program even though the client is billed as “established” to the health department. Due to National Correct Coding Initiative (NCCI) edits the practice of billing a 99211, and then later billing a new visit code, has been eliminated. Many LHDs have been billing a 99211 (usually an RN only visit) the first time they see a patient and then, up to 3 years later, bills a 99201 – 99205 or 99381-99387 (New Visit). Examples may include: billing the 99211 for pregnancy test counseling or head lice check by RN and then a new visit when the patient comes in for their first prenatal, Family Planning or Child Health visit. Now that the NCCI edits have been implemented, all of those “new” visits will deny because the LHD will have told the system (via billing a 99211) that the patient is “established.” Consult your PHNPDU Nursing Consultant if you have questions.
ADULT PREVENTIVE CARE PROCEDURE CODES
Code Description 76091 Mammogram (specialty center) 82270 Fecal Occult Blood Test (lab procedure code only) 82465 Total Serum Cholesterol (lab procedure code only) 84153 PSA (lab procedure code only) 86580 Tuberculosis (TB) Screening (PPD) 88150 Pap Smear (lab procedure code only) 90658 Flu Shot 90718 Td-Diphtheria–Tetanus Toxoid–0.5 ml 90732 Pneumovax
REIMBURSEMENT GUIDELINES Preventive Medicine Service and Problem Oriented E/M Service
A Preventive Medicine CPT or HCPCS code and a Problem-Oriented E/M CPT code may both be submitted for the same patient by the Same Specialty Physician, Hospital, Ambulatory Surgical Center or Other Health Care Professional on the same date of service. If the E/M code represents a significant, separately identifiable service and is submitted with modifier 25 appended, Oxford will reimburse the Preventive Medicine code plus 50% of the Problem-Oriented E/M code. Oxford will not reimburse a Problem-Oriented E/M code that does not represent a significant, separately identifiable service and that is not submitted with modifier 25 appended.
Preventive Medicine Service and Other E/M Service
A Preventive Medicine CPT or HCPCS code and Other E/M CPT or HCPCS codes may both be submitted for the same patient by the Same Specialty Physician, Hospital, Ambulatory Surgical Center or Other Health Care Professional on the same date of service. However, Oxford will only reimburse the Preventive Medicine CPT or HCPCS code.
QUESTIONS AND ANSWERS 1 Q: Why does Oxford reduce reimbursement to 50% for an evaluation and management (E/M) service (99201-99205 or 99212-99215 with modifier 25) billed for the same person on the same date of service as a Preventive Medicine service ?
A: Oxford recognizes that a visit may begin as a Preventive Medicine service, and in the process of the examination it may be determined that a disease related condition exists (evaluation and management). When this occurs, the level of decision-making during such a visit may be more complex than the decision-making during a Preventive Medicine visit. However, there are elements of the Preventive Medicine service (e.g., making the appointment, obtaining vital signs, maintaining and stocking the exam room, etc.) that are duplicated in the reimbursement for an E/M code; these duplicated practice expense services are 50% of the E/M cost.
2 Q: In what situation is CPT code 96110 reimbursable?
A: As defined, CPT code 96110 represents developmental screening with interpretation and report. In the introduction to the section in which this code appears, the CPT book states that “it is expected that the administration of these tests will generate material that will be formulated into a report.” Because a physician obtains developmental information as an intrinsic part of a preventive medicine service for an infant or child and because this information is sometimes obtained in the form of a questionnaire completed by the parents, it is expected that this code will be reported in addition to the preventive medicine visit only if the screening meets the code description. Physicians should report CPT code, for developmental screening or other similar screening or testing, separate and distinct from the Preventive medicine service only when the testing or screening results in an interpretation and report by the physician being entered into the medical record.
3 Q: Why is Q0091 not separately reimbursable when billed with a Preventive Medicine code?
A: Oxford considers Q0091 (obtaining, preparing and conveying a cervical or vaginal smear to the laboratory) to be an integral part of a Preventive Health Care service. Therefore, this component of a Preventive visit is not separately reimbursable.
4 Q: Why is 99173 (screening test of visual acuity) not separately reimbursable when billed with a Preventive Medicine code?
A: Oxford considers vision screening using an eye chart to be integral to a Preventive Medicine examination in the same way that measurements of height, weight and blood pressure are integral to a Preventive Medicine examination. Therefore, vision screening using an eye chart is not reimbursed separately from a Preventive Medicine examination.
5 Q: Why is 99172 (visual function screening) not separately reimbursable when billed with a Preventive Medicine code?
A: The CPT Book clearly states that this service should not be reported in addition to an E/M code.
6 Q: How does Oxford reimburse for screening tests based on a questionnaire completed by the patient or a family member when done in conjunction with a Preventive Medicine service?
A: Counseling, anticipatory guidance and risk factor reduction interventions are integral to a Preventive Medicine visit. Historical information may be obtained either through direct questioning or through completion of a written questionnaire. The responses on a questionnaire often identify areas for more focused interventions or treatments. Since this screening is part of a Preventive Medicine service, it is not reimbursed separately. Occasionally, a screening instrument requires interpretation, scoring, and the development of a report separate from the Preventive Medicine encounter. In those situations, where a CPT code exists for that service, screening, interpretation and development of a report is reimbursed separately from a Preventive Medicine service. State Exceptions
Arizona Per Arizona State Regulations, effective 4/1/14 claims for EPSDT services must be submitted on a CMS (formerly HCFA) 1500 form for members up to age 21. Providers must bill for preventative EPSDT services using the preventative service, office or other outpatient services and preventive medicine CPT codes (99381 – 99385, 99391 – 99395) with an EP modifier.
EPSDT visits are paid at a global rate for the services specified and no additional reimbursement is allowed. Providers must use an EP modifier to designate all services related to the EPSDT well child check-ups, including routine vision and hearing screenings.
* A list of preventative, office or other outpatient services that are considered included in the global payment of the preventive medicine CPT code is attached to this policy
* Ocular photoscreening with interpretation and report, bilateral (CPT code 99174) is allowed for members under age 19. Arizona EPSDT Bundled Codes Lis t
A list of preventative, office or other outpatient services that are considered included in the global payment for the preventive medicine CPT codes (99381 – 99385, 99391 – 99395).
DC EPSDT Well-Child Visit Billing Reference Guide
When conducting a well-child visit (WCV), a primary care provider (PCP) must perform all components required in a visit and all age-appropriate screenings and/or assessments as required in the DC Medicaid HealthCheck Periodicity Schedule. Covered screening services are medical, developmental/mental health, vision, hearing and dental. The components of medical screening include:
* Comprehensive health and developmental history that assesses for both physical and mental health as well as for substance use disorders
* Comprehensive, unclothed physical examination
* Appropriate immunizations (as established by ACIP)
* Laboratory testing (including blood lead screening appropriate for age and risk factors)
* Health education and anticipatory guidance for both the child and the caregiver.i
To bill for a well-child visit:
* Use the age-based CPT code (99381-99385; 99391-99395). See Table 1.
o Use the following ICD-9 diagnosis codes listed in Table 1 in conjunction with the CPT Code
* Bill for each separate assessment/screening performed using the applicable CPT code from Table 2.
* If a screening or assessment is positive and requires follow-up or a referral, please use modifier TS with the applicable screening code that had a positive result.
DO NOT USE THE E&M OUTPATIENT VISIT CODES (99201-99205; 99213-99215) TO BILL FOR A WELLCHILD VISIT.
Table1: Age Based Preventive Visit CPT Codes Table 2: Screening/Assessment CPT Codes Patient’s Age CPT Code Dx Code
< 1 year 99381/91 new/established V20.31, 20.32, V20.2
1 – 4 years 99382/92 V20.2
5 – 11 years 99383/93 V20.2
12 – 17 years 99384/94 V20.2
18 – 21 years 99385/95 V70.0
HCY/EPSDT Billing Codes [1][2][3] AGE CPT Code: New Patient AGE CPT Code:
Established Patient Modifiers As Applicable ICD-10-CM Diagnosis Codes Preventive visit, Modifier EP: Used with procedure codes 99381-99385 and 99391-99395 when a Full or Partial screening is performed.
Modifier 52: Used with modifier EP when all components have not been met, but at least the first 5 or more components were completed according to the HCY/EPSDT requirements.
Modifier 59: Used when only components related to developmental and mental health are screened.
Modifier 25: Used on the significant, separately identifiable problem-oriented evaluation and management service when it is provided on (1) the same day as the preventive medicine service and/or (2) with administration of immunizations. Please note that modifier 25 is not to be used on preventive codes and needs to be billed using office or outpatient codes (99201-99215), and that these screenings bundle administration of immunizations.*Documentation must support the use of a modifier 25. See MO HealthNet Provider Manual. Modifier UC: Used when a referral is made for further care.
Z00.110 Newborn under 8 days old
Z00.111 Newborns 8 to 28 days old or
Z00.121 Routine child health exam with abnormal findings
Z00.129 Routine child health exam without abnormal findings Preventive visit, 1-4
99382 Preventive visit, 1-4
99392 Z00.121 Z00.129 Preventive visit, 5-11
99383 Preventive visit, 5-11
99393 Z00.121 Z00.129 Preventive visit, 12-17
99384 Preventive visit, 12-17
99394 Z00.121 Z00.129 Preventive visit, 18 or older
99385 Preventive visit, 18 or older
99395 Z00.00 General adult medical exam without abnormal findings Z00.01 General adult medical exam with abnormal findings
NCCI Edit with preventive visits
National Correct Coding Initiative (NCCI) Impacts on Immunization and Evaluation & Management (E&M) Codes Effective April 1, 2014, the Department will no longer reimburse NCCI procedure-to-procedure (PTP) edits when immunization administration procedure codes (CPT 90460-90474) are paired with preventative medicine E&M service procedure codes (CPT 99381-99397).
If a significant separately identifiable E&M service (e.g. new or established patient office or other outpatient services [99201-99215], office or other outpatient consultation [99241-99245], emergency department service [99281-99285], preventative medicine service [99381-99429] is performed), the appropriate E&M service code should be reported in addition to the vaccine and toxoid administration codes.
Each NCCI PTP edit has an assigned modifier indicator. A modifier indicator of “0” indicates that NCCI PTP-associated modifiers cannot be used to bypass the edit. A modifier indicator of “1” indicates that NCCI PTP-associated modifiers may be used to bypass an editunder appropriate circumstances. A modifier indicator of “9” indicates that the edit has been deleted, and the modifier indicator is not relevant. The Correct Coding Modifier Indicator can be found in the files containing Medicaid NCCI PTP edits on the CMS website.
A modifier should not be added to a HCPCS/CPT code solely to bypass an NCCI PTP edit, if the clinical circumstances do not justify its use. If the E&M service is significant and separately identifiable and performed on the same day, the E&M code should be billed with the vaccine and toxoid administration codes using PTP associated modifier ‘25’. Modifier ‘25’ is only valid when appended to the E&M codes. Do not append to the immunization administration procedure codes 90460-90474.
Therapeutic Injections Office visits (CPT codes 99201-99205; 99212-99215; 99381-99397) will not be separately reimbursed when submitted with therapeutic injections (CPT code 96372). Please append Modifier 25 to the disallowed E/M code if a significant separately identifiable E/M service was performed. Note: CPT code 96372 has been valued to include the work and practice expenses of CPT code 99211. A modifier will not override this edit.
Visual Acuity Testing CPT code 99173, visual acuity screening test, is separately reimbursable when submitted with preventive office visits (CPT codes 99381-99397). Vital Capacity Vital capacity (CPT code 94150) is considered incidental to the overall service provided, whether an office visit or a procedure, and will not be separately reimbursed.
Payment guidelines
Preventive Medicine Services [Current Procedural Terminology (CPT®) codes 99381-99387, 99391-99397, Healthcare Common Procedure Coding System (HCPCS) code G0402] are comprehensive in nature, reflect an age and gender appropriate history and examination, and include counseling, anticipatory guidance, and risk factor reduction interventions, usually separate from disease-related diagnoses. Occasionally, an abnormality is encountered or a preexisting problem is addressed during the Preventive visit, and significant elements of related Evaluation and Management (E/M) services are provided during the same visit. When this occurs, Oxford will reimburse thePreventive Medicine service plus 50% the Problem-Oriented E/M service code when that code is appended with modifier 25. If the Problem-Oriented service is minor, or if the code is not submitted with modifier 25 appended, it will not be reimbursed.
Prolonged services are included in (and not separately reimbursed from) Preventive Medicine codes. Counseling services are included in (and not separately reimbursed from) Preventive Medicine codes. Medical Nutrition Therapy services are included in (and not separately reimbursed from) Preventive Medicine codes. Visual function screening and Visual Acuity screening are included in (and not separately reimbursed from) Preventive Medicine services.
Reporting Evaluation and Management Services With Immunizations
E/M services most often reported with the vaccine product and immunization administration include new and established patient preventive medicine visits (CPT codes 99381–99395), problem-oriented visits ( CPT 99201 –99215), and preventive medicine counseling services (99401–99404). Any of the aforementioned E/M codes can be reported as a single service or in combination when performed and documented on the same day of service by the same physician or physician of the same group and specialty.
The E/M service must be medically indicated, significant, and separately identifiable from the immunization administration.
• Payers may require modifier 25 (significant, separately identifiable E/M service by the same physician on the same day of the procedure or other service) to be appended to the E/M code to distinguish it from the administration of the vaccine.
• CPT code 99211 (established patient E/M, minimal level, not requiring physician presence) should not be reported when the patient encounter is for vaccination only because the Medicare Resource-BasedRelative Value Scale (RBRVS) relative values for the immunization administration codes incl de administrative and clinical services (ie, greeting the patient, routine vital signs, obtaining a vaccine history, presenting the VIS and responding to routine vaccine questions, preparation and administration of the vaccine, and documentation and observation of the patient following the administration of the vaccine). However, if the service is medically necessary, significant, and separately identifiable, it may be reported with modifier 25 appended to the E/M code (99211). Note that the medical record must clearly state the reason for the visit, brief history, physical examination, assessment and plan, and any other counseling or discussion items. The progress note must be signed with the physician’s countersignature. For more information and clinical vignettes on the appropriate use of code 99211 during immunization administration, visit www.aap.org/pubserv/codingforpeds for a copy of the AAP position paper on reporting 99211 with immunization administration. Payers who do not follow the Medicare RBRVS may allow payment of code 99211 with immunization administration. Know your payer guidelines, and if payment is allowed, make certain that the guidelines are in writing and maintained in your office. Be aware that a co-payment will be required when the “nurse” visit is reported.
• The same guidelines apply to physician visits (99201–99215). In other words, if a patient is seen for the administration of a vaccine only, it is not appropriate to report an E/M visit if it is not medically necessary, significant, and separately identifiable.
• If at the time of a preventive medicine visit a patient has a problem or abnormality that is addressed and requires significant additional work to perform the required key components, a problem-oriented E/M code (99201–99215) may be reported in addition to the preventive medicine services code. There should be separate documentation for the 2 services in the medical record. Typically the level of service is based on the level of history and medical decision-making that are performed and documented because the physical examination component is most often performed as part of the age-appropriate examination included in the preventive medicine service. Modifier 25 must be appended to the problemoriented E/M service to alert the payer that it was significant and separately identifiable. Each code is linked to the appropriate ICD-9-CM code.
CPT codes 99401–99404 (preventive medicine counseling, individual) are used for the purpose of promoting health and preventing illness or injury. They are not reported when counseling is related to a condition, disease, or treatment. These are time-based codes that require medical record documentation of the total time spent in counseling and a summary of the issues discussed. Codes 99401–99404 may be reported separately from other E/M services (eg, office visits, preventive medicine visits) when performed on the same day. Modifier 25 must be appended to codes 99401– 99404 to signify to the payer that the preventive medicine counseling was significant and separately identifiable from the preventive medicine or problem-oriented E/M visit.
• Remember that reviewing or discussing the risks and benefits of vaccines and addressing all other patient and parent concerns and questions related to vaccines and immunization administration are included in the immunization administration codes. However, if vaccine counseling is performed and the parent or patient refuses vaccines, the time spent in counseling may be separately reported. Also, if after additional time is spent in vaccine counseling, the parent or patient then decides to accept the immunizations and the time and effort exceeds that normally spent by the physician, it is still appropriate to report these codes in addition to the E/M visit and immunization administration. Make certain that the medical record supports the excess time and effort of counseling.
Billing for Medically Necessary Visit on Same Occasion as Preventive Medicine Service
When a physician furnishes a Medicare beneficiary a covered visit at the same place and on the same occasion as a noncovered preventive medicine service (CPT codes 99381- 99397), consider the covered visit to be provided in lieu of a part of the preventive
medicine service of equal value to the visit. A preventive medicine service (CPT codes 99381-99397) is a noncovered service. The physician may charge the beneficiary, as a charge for the noncovered remainder of the service, the amount by which the physician’s current established charge for the preventive medicine service exceeds his/her current established charge for the covered visit. Pay for the covered visit based on the lesser of the fee schedule amount or the physician’s actual charge for the visit. The physician is not required to give the beneficiary written advance notice of noncoverage of the part of the visit that constitutes a routine preventive visit. However, the physician is responsible for notifying the patient in advance of his/her liability for the charges for services that are not medically necessary to treat the illness or injury.
There could be covered and noncovered procedures performed during this encounter (e.g., screening x-ray, EKG, lab tests.). These are considered individually. Those procedures which are for screening for asymptomatic conditions are considered noncovered and, therefore, no payment is made. Those procedures ordered to diagnose or monitor a symptom, medical condition, or treatment are evaluated for medical necessity and, if covered, are paid.
Medical Billing Update
- Medical billing concept – Patient 1st plan
- DOCUMENTATION OF EXAMINATION – E & M code
- Timely filing limit for BBHHF providers
- Frequency of testing considered medically necessary for ICD 9 codes
- Eligibility Verfication in Medical Billing
Recent Posts
- Denial – Covered by capitation , Modifier inconsistent – Action
- CPT code 10040, 10060, 10061 – Incision And Drainage Of Abscess
- CPT Code 0007U, 0008U, 0009U – Drug Test(S), Presumptive
- CPT code 99499 – Billing and coding guidelines
- CPT 92521,92522,92523,92524 – Speech language pathology
- Medical billing basics
All the contents and articles are based on our search and taken from various resources and our knowledge in Medical billing. All the information are educational purpose only and we are not guarantee of accuracy of information. Before implement anything please do your own research. If you feel some of our contents are misused please mail us at medicalbilling4u at gmail dot com. We will response ASAP.
You are using an outdated browser. Please upgrade your browser to improve your experience.
opensource.google.com
Google open source blog.
The latest news from Google on open source releases, major projects, events, and student outreach programs.
Introducing Jpegli: A New JPEG Coding Library
Wednesday, april 3, 2024.
The internet has changed the way we live, work, and communicate. However, it can turn into a source of frustration when pages load slowly. At the heart of this issue lies the encoding of images. To improve on this, we are introducing Jpegli , an advanced JPEG coding library that maintains high backward compatibility while offering enhanced capabilities and a 35% compression ratio improvement at high quality compression settings.
Jpegli is a new JPEG coding library that is designed to be faster, more efficient, and more visually pleasing than traditional JPEG. It uses a number of new techniques to achieve these goals, including:
- It provides both a fully interoperable encoder and decoder complying with the original JPEG standard and its most conventional 8-bit formalism, and API/ABI compatibility with libjpeg-turbo and MozJPEG.
- High quality results . When images are compressed or decompressed through Jpegli, more precise and psychovisually effective computations are performed and images will look clearer and have fewer observable artifacts.
- Fast . While improving on image quality/compression density ratio, Jpegli's coding speed is comparable to traditional approaches, such as libjpeg-turbo and MozJPEG. This means that web developers can effortlessly integrate Jpegli into their existing workflows without sacrificing coding speed performance or memory use.
- 10+ bits . Jpegli can be encoded with 10+ bits per component. Traditional JPEG coding solutions offer only 8 bit per component dynamics causing visible banding artifacts in slow gradients. Jpegli's 10+ bits coding happens in the original 8-bit formalism and the resulting images are fully interoperable with 8-bit viewers. 10+ bit dynamics are available as an API extension and application code changes are needed to benefit from it.
- More dense: Jpegli compresses images more efficiently than traditional JPEG codecs, which can save bandwidth and storage space, and speed up web pages .
How Jpegli works
Jpegli works by using a number of new techniques to reduce noise and improve image quality; mainly adaptive quantization heuristics from the JPEG XL reference implementation, improved quantization matrix selection, calculating intermediate results precisely, and having the possibility to use a more advanced colorspace . All the new methods have been carefully crafted to use the traditional 8-bit JPEG formalism, so newly compressed images are compatible with existing JPEG viewers such as browsers, image processing software, and others.
Adaptive quantization heuristics
Jpegli uses adaptive quantization to reduce noise and improve image quality. This is done by spatially modulating the dead zone in quantization based on psychovisual modeling . Using adaptive quantization heuristics that we originally developed for JPEG XL, the result is improved image quality and reduced file size. These heuristics are much faster than a similar approach originally used in guetzli .

Improved quantization matrix selection
Jpegli also uses a set of quantization matrices that were selected by optimizing for a mix of psychovisual quality metrics. Precise intermediate results in Jpegli improve image quality, and both encoding and decoding produce higher quality results. Jpegli can use JPEG XL's XYB colorspace for further quality and density improvements.
Testing Jpegli
In order to quantify Jpegli's image quality improvement we enlisted the help of crowdsourcing raters to compare pairs of images from Cloudinary Image Dataset '22 , encoded using three codecs: Jpegli, libjpeg-turbo and MozJPEG, at several bitrates.
In this comparison we limited ourselves to comparing the encoding only, decoding was always performed using libjpeg-turbo. We conducted the study with the XYB ICC color profile disabled since that is how we anticipate most users would initially use Jpegli. To simplify comparing the results across the codecs and settings, we aggregated all the rater decisions using chess rankings inspired ELO scoring .
Our results show that Jpegli can compress high quality images 35% more than traditional JPEG codecs.
Jpegli is a promising new technology that has the potential to make the internet faster and more beautiful.
By Zoltan Szabadka, Martin Bruse and Jyrki Alakuijala – Paradigms of Intelligence, Google Research
- Español – América Latina
- Português – Brasil
- Tiếng Việt
- Android Studio
- Android Developers
Gemini in Android Studio
Gemini in Android Studio is your coding companion for Android development. It's powered by artificial intelligence and can understand natural language and can understand natural language. It helps you be more productive by answering your Android development queries. Gemini can help Android developers generate code, find relevant resources, learn best practices, and save time.
Gemini is still an early experiment, and might sometimes provide inaccurate, misleading or false information while presenting it confidently. Gemini might give you working code that doesn't produce the expected output, or provide you with code that is not optimal or incomplete. Always double-check Gemini's responses and carefully test and review code for errors, bugs, and vulnerabilities before relying on it. Gemini's new capabilities can help you by offering new ways to write code, create test cases, or update APIs.
Get started
Here's how to set up Gemini:
- Download the latest version of Android Studio Jellyfish or higher.
- Recommended: Agree to send data to Google so we can better understand how effective Gemini is. Give permission to share data either when you first install Android Studio or later at File > Settings > Appearance & Behavior > System Settings > Data Sharing ( Android Studio > Settings > Appearance & Behavior > System Settings > Data Sharing on macOS).
- To launch Gemini, open or start an Android Studio project and click View > Tool Windows > Gemini .
- Sign in to your Google account when asked, if you aren't already signed in. The chat box appears and you can start using Gemini's interactive, conversational interface.
Get answers from Gemini
The main interface for interacting with Gemini is the chat window. You can use it to ask questions ranging from very simple and open-ended ones to specific problems that you need help with. Here are some examples of things you might ask; however, feel free to experiment with any topics related to Android development:
- How do I add camera support to my app?
- I want to create a Room database.
- Can you remind me of the format for javadocs?
- What is dark theme?
- What's the best way to get location on Android?
Gemini remembers the context of the conversation, so you can also ask it follow-up questions, such as:
- Can you give me the code for this in Kotlin?
- Can you show me how to do it in Compose?
You can also ask Gemini about Android Studio itself, for example:
- How do I analyze jank in my app?
- Where do I find the CPU profiler?
Tips for engaging with Gemini
Gemini's answers differ based on how you ask your question. Here are some tips on how to optimize the answers from Gemini:
How Gemini can help
In addition to the chat interface, Gemini offers a number of entry points that integrate with your development flow:
- Add generated code with a click : Gemini displays smart actions next to the code it generates, which lets you quickly insert the code into the open editor, insert it into the Android Manifest, or even add required dependencies for popular libraries that are used in the answer.
- Receive helpful resources : for certain topics, Gemini offers to open the relevant documentation page with further information.
- Troubleshoot errors : for common errors, Gemini explains what they mean and offers actions to fix them.
- "Ask Gemini" directly from your codebase : when you select text in the code editor, right-click and select the Ask Gemini action to populate the chat prompt with the selected code. From there you can decide whether or not to send the code—Gemini doesn't send code without your explicit authorization. Ask Gemini is also available to help you troubleshoot warnings and errors in the code editor.
Frequently asked questions (FAQ)
Does gemini send my code to google's servers.
Learn about what data is shared and how you can control your privacy settings at Data and privacy .
Does Gemini give accurate and safe responses?
Accelerating people's ideas with generative AI is truly exciting, but it's still early days, and Gemini is an experiment. Some of the responses might be inaccurate, so double-check information in the responses. With your feedback, Gemini is improving. While Gemini has built-in safety controls and clear mechanisms for feedback in line with our AI Principles , be aware that it might display inaccurate information or offensive statements.
Because AI is an evolving technology, it can generate output that sounds plausible but is factually incorrect. We recommend that you validate all output from Gemini before you use it.
Can Gemini help with coding?
Yes, Gemini can help with coding and topics about coding. It is experimental and you are responsible for your use of code or coding explanations. Use discretion and carefully test all code for errors, bugs, and vulnerabilities before relying on it.
How can I reset chat history?

Why do I get a "code is blocked" error message?
Gemini conducts multiple layers of checks on model-generated responses. For example, there's a check to ensure that the model-generated code doesn't replicate existing content at length. It's possible that your response gets blocked due to one of these checks. In this case, try again with a different prompt.
How and when does Gemini cite sources in its responses?
Gemini should generate original content and not replicate existing content at length. We've designed our systems to limit the chances of this occurring, and we will continue to improve how these systems function. If Gemini does directly quote at length from a code repository, it cites that source. The citation might also reference an applicable open source license. It is your responsibility to comply with any license requirements.
What terms of service apply to my Gemini usage?
Your use of Gemini is subject to the Google Terms of Service and the Generative AI Additional Terms of Service .
How can I report feedback about Gemini?
We're looking for your feedback to help us improve Gemini responses across all of the domains of Android development. To help, use Gemini in your development workflow and mark its responses as helpful or not helpful using the thumbs up and down options in the Gemini UI. This input helps us identify the areas that need more training.
How is Gemini different from other LLM-powered chatbots?
Gemini leverages an LLM that was designed to help with coding scenarios. Gemini is tightly integrated within Android Studio, which means it can provide more relevant responses, and lets you to take actions and apply suggestions with just a click.
What are some tips for using Gemini?
- Be clear and concise when you ask your question.
- Use simple language that Gemini can understand.
- If Gemini does not understand your question, try rephrasing it.
- Review Gemini suggestions before using them.
For more details, see Tips for engaging with Gemini .
Content and code samples on this page are subject to the licenses described in the Content License . Java and OpenJDK are trademarks or registered trademarks of Oracle and/or its affiliates.
Last updated 2024-04-09 UTC.
How to Use Modifier 25
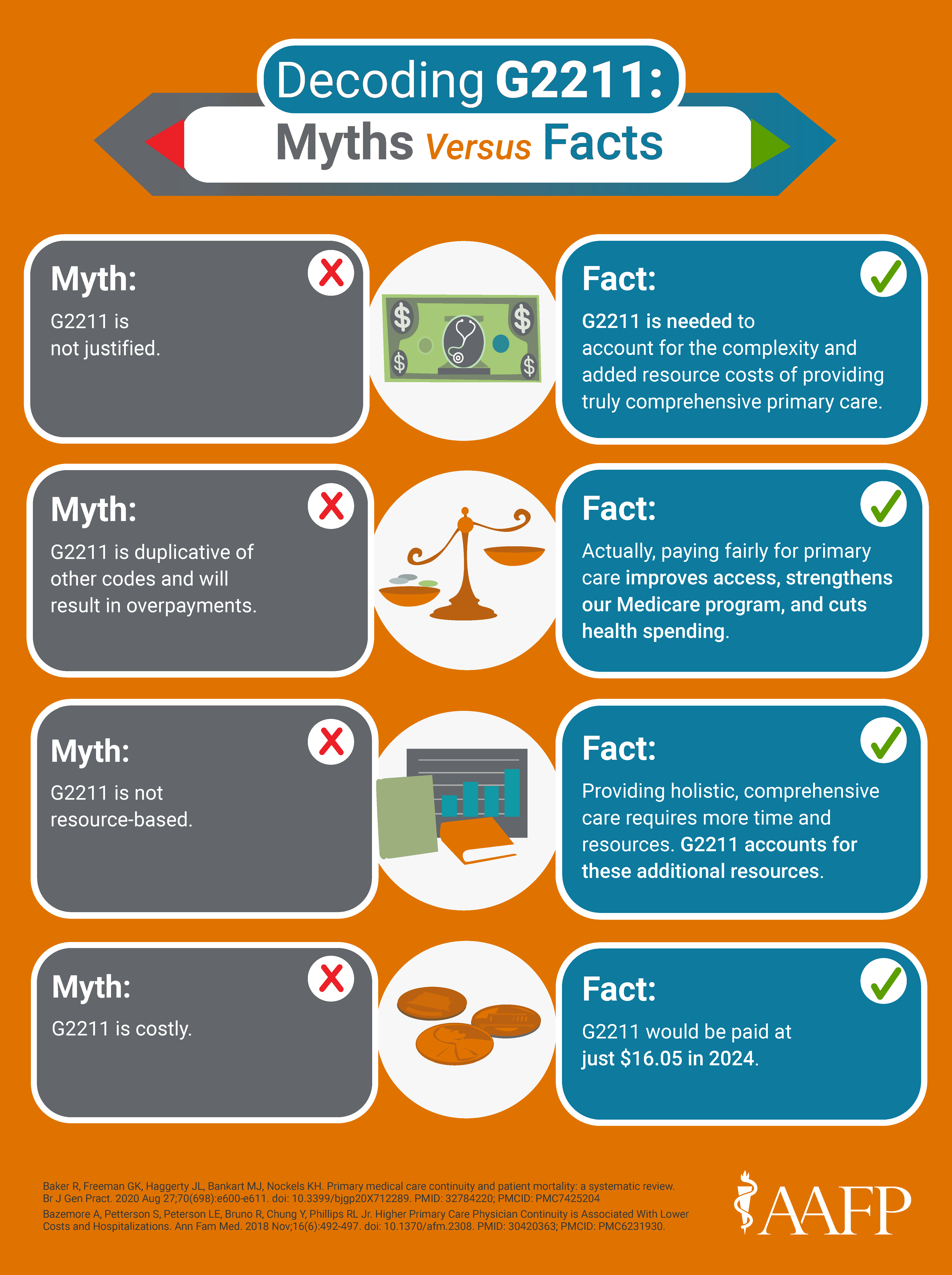
Questions about modifier 25 have increased since add-on code G2211 was implemented in 2024 to reflect the value primary care physicians provide to patients. Learn how to report modifier 25 correctly so that you can get paid accurately.
What is modifier 25?
- Modifier 25 is a way to identify a “significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of the procedure or other service,” according to the CPT 2024 code set .
- Modifier 25 may only be appended to evaluation and management services.
When can it be used?
The E/M service must be significant and distinct from the procedure. The E/M must reflect work that is above and beyond the usual work associated with the procedure or other service.
Asking the following questions can help determine whether it is appropriate to use modifier 25:
✔️ Did you perform and document the key components of a problem-oriented E/M service for the complaint or problem?
✔️ As documented, could the E/M service stand alone as a billable service?
✔️ Is there a different diagnosis for this portion of the visit?
✔️ If the diagnosis will be the same, did you perform extra physician work that went above and beyond the work of the other service or the typical pre- or postoperative work associated with the procedure?
Modifier 25 should not be used when:
❌ The sole purpose of the encounter is for the procedure (e.g., lesion removal), and there is no documented medical necessity for a separate E/M service. The decision to perform a minor procedure is included in the payment for the procedure and should not be reported as a separate E/M service.
Example: Visit for lesion removal
A patient presents to have a mole assessed and the physician decides to remove it. The decision to remove the mole is included in the procedure code and should not be billed as a separate E/M service.
However, in this same scenario, if the mole has a suspicious, potentially malignant appearance that the physician relates to the patient, in a separate identifiable E/M service, and discusses the possible need for a more extensive procedure if the pathology report comes back positive for malignancy, the E/M visit would be reported with a 25 modifier, along with the procedure code for the lesion removal.
- An E/M is related to and within the global period of a previously performed procedure . This includes minor surgical procedures (defined as a 000 or 010 day global period).
- Patient encounter is for a planned/scheduled minor procedure with no other, significant problems “addressed.”
- Patient encounter is for a preventive service, and there is no significant abnormality found that needs to be addressed within the components of a separate E/M office visit.

Understand how to properly document and code for E/M services.
What needs to be documented?
- Documentation must demonstrate the medical necessity of the E/M service.
- If possible, physically separate the documentation for the preventive service or procedure from the documentation for the problem-oriented E/M service within the patient’s medical record.
- Documentation should be able to support each service (i.e., the preventive service or procedure and the E/M) as though it were a standalone service.
Are separate diagnoses required?
No. An E/M service may be reported if it is clinically indicated and reflects work that is above and beyond the preoperative work associated with the procedure — even if both services have the same diagnosis. An example would be a patient who presents with a head laceration and you examine the patient for neurological damage before repairing the laceration.
Is modifier 25 required for E/M services provided at the same encounter as vaccines?
Yes and no. Traditional Medicare does not require modifier 25 for E/M services provided in conjunction with administration of the influenza (Healthcare Common Procedure Coding System [HCPCS] G0008), pneumococcal (HCPCS G0009) or hepatitis B (HCPCS G0010) vaccines. Medicare does require modifier 25 for E/M services provided in conjunction with other vaccine administration codes, including CPT codes 90480, 90460, 90461, 90471, 90472, 90473 and 90474. Private payers may have different policies. The E/M service must be significant and separately identifiable from the vaccine administration.
Can a preventive medicine visit and a problem-oriented visit be billed in the same encounter?
Yes. If a patient presents for a preventive visit and the physician identifies a new problem or changes to an existing problem that are significant enough to require additional work to perform the key components of the problem-oriented E/M service, both the preventive service and the appropriate office/outpatient E/M service may be reported. Append modifier 25 to the office/outpatient E/M service. While preventive and wellness services are not subject to cost-sharing, the office/outpatient E/M service may be subject to deductible and cost-sharing. If the problem is trivial and does not require additional work, an office/outpatient E/M service should not be reported .
For more information and examples, review the FPM article “ Combining a Wellness Visit with a Problem-Oriented Visit: a Coding Guide .”
Do all payers follow the same rules for modifier 25?
Not necessarily. Traditional Medicare adheres to the National Correct Coding Initiative (NCCI) . NCCI edits are updated quarterly. Some Medicare Administrative Contractors have NCCI Lookup tools available ( Novitas , CGS Medicare , First Coast Service Options , Palmetto ). Private payers often use their own claims editing systems and may not always align with Medicare. Review your payers’ policies or contact your local provider relations representative for more information.
How is the new add-on HCPCS code G2211 impacted by modifier 25?
As of January 1, 2024, Medicare implemented a new HCPCS code G2211 to reflect the visit complexity associated with providing comprehensive, longitudinal care.
As part of the implementation of the new HCPCS code G2211, the Centers for Medicare & Medicaid Services (CMS) instituted a policy that prohibits its use when the office/outpatient E/M service is appended with modifier 25. Medicare will not pay for HCPCS code G2211 when modifier 25 is appended to the office/outpatient E/M service.
The AAFP believes this policy is contrary to the intent of the code and is advocating with CMS to change its policy. However, in the interim, Medicare will deny the G2211 line item on a claim if an E/M with a 25 modifier is also reported on the same date. You can read more about the AAFP’s advocacy efforts here . Additional information about G2211 is available on the webpage “ G2211 Add-on Code: What It Is and When To Use It .”
Where can I find more information about modifier 25?
You can find additional information, tools, and tips from the AAFP and the AMA.
- FPM Getting Paid blog: Seven quick tips for using modifier 25 (April 2023)
- F PM article: Combining a Wellness Visit With a Problem-Oriented Visit: a Coding Guide (January/February 2022)
- FPM article: Understanding when to use Modifier -25 (October 2004)
- FPM article: Getting Paid for Screening and Assessment Services (November/December 2017)
- AMA: Setting the record straight on proper use of modifier 25
- AMA CPT® Assistant: Reporting CPT Modifier 25
- CMS Medicare Claims Processing Manual, Chapter 12 and General Correct Coding Policies, Chapter 1 .
Use these G2211 tips to get paid accurately.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

IMAGES
VIDEO
COMMENTS
Short description: 45-59 minute office visit for new patient evaluation and management. CPT Code 99205. Long description of CPT 99205: Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and high level of medical decision making. When using time for code+ selection, 60-74 minutes of total time is ...
NEW PATIENT VISIT CPT Code 99201 99202 99203 99204 99205 Required Key Components *(3/3 required) History and Exam Problem-Focused X Expanded Problem-Focused X ...
CPT® code 99203: New patient office or other outpatient visit, 30-44 minutes. As the authority on the CPT® code set, the AMA is providing the top-searched codes to help remove obstacles and burdens that interfere with patient care. These codes, among the rest of the CPT code set, are clinically valid and updated on a regular basis to ...
Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 30-44 minutes of total time is spent on the date of the encounter. 99204. Office or other outpatient visit for the ...
Step 1: Total time. Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if ...
The provider sees a new patient for an office visit or other outpatient visit involving evaluation and management. The visit involves a high level of medical decision making, and/or the provider spends 60 or more minutes of total time on the encounter on a single date. ... View the CPT® code's corresponding procedural code and DRG. In a click ...
Another important difference between the codes is that the new patient codes (99201-99205) require that all three key components (history, exam and medical decision making) be satisfied, while ...
The E/M visit CPT® codes 99202-99215 (new and established patients) were revised to decrease documentation and coding administrative burden and to ensure that E/M payment is resource-based. The revisions remov e the history and physical examination as key components in choosing the appropriate E/M level of a visit. Now, code level selection for
Visit level * Established patient visit New patient visit; Level 2: 99212 10-19 minutes: 99202 15-29 minutes: ... According to the 2021 CPT code descriptors, 40-54 minutes of total time ...
The basic format of codes with levels of E/M services based on medical decision making (MDM) or time is the same. First, a unique code number is listed. Second, the place and/or type of service is specified (eg, office or other outpatient visit). Third, the content of the service is defined. Fourth, time is specified.
The codes apply to services that a wide range of primary care and specialty providers perform regularly. Some of the most commonly reported E/M codes are 99201-99215, which represent office or other outpatient visits. In 2020, the E/M codes for office and outpatient visits include patient history, clinical examination, and medical decision ...
Billing for new patients requires three key elements and a thorough knowledge of the rules. A persistent concern when reporting evaluation and management (E/M) services is determining whether a an individual is a new patient to the practice or already established. New patient codes carry higher relative value units (RVUs), and for that reason are consistently under the watchful eye of payers ...
New Patient Office Visit (E/M) Services (CPT® 99201-99205) — Documentation Requirements. The metrics reviewed in this CBR are the proportion of billing for each HCPCS code in the E/M grouping with comparisons to peers within the state and Jurisdiction M (JM). This report is an analysis of Medicare Part B claims extracted from the Palmetto ...
Getting clear on the new coding rules can help you eliminate bloated documentation and improve reimbursement to reflect the value of your visits. ... Prolonged visit codes cannot be used with the ...
DO NOT USE THE E&M OUTPATIENT VISIT CODES (99201-99205; 99213-99215) TO BILL FOR A WELLCHILD VISIT. Table1: Age Based Preventive Visit CPT Codes Table 2: Screening/Assessment CPT Codes Patient's Age CPT Code Dx Code < 1 year 99381/91 new/established V20.31, 20.32, V20.2. 1 - 4 years 99382/92 V20.2
Fortunately, the guidelines for using the code remain the same. CPT ® instructs you to use +99417 when service times for 99205 (Office or other outpatient visit for the evaluation and management of a new patient … 60-74 minutes of total time is spent on the date of the encounter) or 99215 (Office or other outpatient visit for the evaluation ...
How do I code an audio-only visit for a new or established patient? CPT Codes: 99441-99443 ... E-visits should not be billed on the same day the physician reports an office visit E/M service (CPT ...
Jpegli is a new JPEG coding library that is designed to be faster, more efficient, and more visually pleasing than traditional JPEG. It uses a number of new techniques to achieve these goals, including: ... images are fully interoperable with 8-bit viewers. 10+ bit dynamics are available as an API extension and application code changes are ...
Always double-check Gemini's responses and carefully test and review code for errors, bugs, and vulnerabilities before relying on it. Gemini's new capabilities can help you by offering new ways to write code, create test cases, or update APIs. Note: Gemini is currently free for developers to try out, and is available in 180 countries.
The preventive medicineservices codes for new patients are 99381 (under 1 year old), 99382 (1 through 4), 99383 (5 through 11), 99384 (12 through 17), and 99385 (18 through 39). The office-visit codes are 99201 through 99205. Note that the sick diagnosis code goes only on the office visit, and the well-care diagnosis code, V20.2, goes only on ...
Other insurers use CPT code 99417, which is for established patient visits of 55 minutes or more and new patient visits of 75 minutes or more. With both codes, prolonged services are billed in 15 ...
In an age of artificial intelligence (AI) and digital recruiting, companies continue to visit St. John's University to search for talent. Skip to main site navigation Skip to main ... New York State's largest health-care provider and private-sector ... Cybersecurity Enthusiasts Gather for St. John's Coding Competition February 8, 2024 ...
Home or residence E/M services, new patient. • 99341, straightforward medical decision making (MDM) or at least 15 minutes total time, • 99342, low level MDM or at least 30 minutes total time ...
Although, "there are some notable differences in this area when it pertains to CPT® versus CMS," Jimenez forewarned. "One of the biggest changes, I think, in the 2023 changes was the elimination of observation codes," Jimenez said. Effective Jan. 1, 2023, hospital observation codes 99217-99220 and 99224-99226 are deleted.
If this is your first visit, be sure to check out the FAQ & read the forum rules.To view all forums, post or create a new thread, you must be an AAPC Member.If you are a member and have already registered for member area and forum access, you can log in by clicking here.If you've forgotten your username or password use our password reminder tool.To start viewing messages, select the forum that ...
How to Use Modifier 25. Questions about modifier 25 have increased since add-on code G2211 was implemented in 2024 to reflect the value primary care physicians provide to patients. Learn how to ...