
- Health & Wellness

What to Expect at Your Postpartum Checkups

During pregnancy, you likely got used to seeing your OB or midwife fairly often, especially as you neared your due date. Consistent visits are a standard part of prenatal care to ensure everything is progressing smoothly and that you and baby are healthy. So what happens now that baby is born? In the past, prenatal care has been far more thorough than postpartum care, but in recent years experts have called for a change. Giving birth is no small feat—it takes both a physical and emotional toll, and new moms need medical care and support, starting with their first postpartum checkup. Here, we talked to two experts to lay out everything you need to know about postpartum checkups, from when to expect them to how to prepare.
What Is a Postpartum Checkup?
Postpartum checkups are the visits to your OB or midwife that you’ll have after giving birth—and they’re just as important as your prenatal visits, as the first few weeks after delivery are a time of major transition for both you and baby.
During these checkups, your doctor will want to make sure you’re adapting well emotionally and recovering well physically. “Issues with blood pressure, infections, breastfeeding issues and hormonal imbalances can all happen postpartum,” says Rebekah Mustaleski , a certified professional midwife and compression director with Motif Medical . “It’s often hard to recognize the subtle differences that signal some of these issues because a new parent is consumed with caring for their newborn. It’s essential to be seen by your doctor or midwife so that they can do an assessment and make sure that your postpartum recovery is going smoothly.”
When Do Postpartum Checkups Happen?
It used to be that you’d have one postpartum checkup, typically six weeks after giving birth or sooner if you delivered via c-section. However, in recent years, experts have called for postpartum checkups to happen sooner and more frequently. The American College of Obstetricians and Gynecologists (ACOG) now recommends that postpartum care start no later than within the first three weeks after birth and should be followed by ongoing care as needed. “To optimize the health of women and infants, postpartum care should become an ongoing process, rather than a single encounter, with services and support tailored to each woman’s individual needs,” the guidance reads. Plus, the ACOG states women should receive a comprehensive postpartum checkup that includes “a full assessment of physical, social and psychological well-being” no later than 12 weeks postpartum.
According to Mustaleski, most providers schedule postpartum checkups the day after birth (where they’ll come see you bedside as you recover), two to three weeks postpartum and then again at six to eight weeks postpartum.
What Happens During Postpartum Checkups?
The postpartum checkups are a time to discuss how you’re healing and adapting to motherhood. During the visit, your doctor will check on several aspects of your physical and emotional recovery. According to the ACOG, it will also cover infant care and feeding, family planning, sleep and fatigue, chronic disease management and health maintenance.
“I usually talk to my patients about how the pregnancy and delivery went," says Laura Riley , MD, department chair of obstetrics and gynecology at Weill Cornell Medicine. She also asks how infant feeding is going, whether Mom has any questions about returning to work and when is a good time to resume exercise…
Postpartum checkups: Physical recovery
During the physical checkup, your doctor or midwife will check your vitals, assess your weight and take your blood pressure. According to Mustaleski and Riley, they’ll also:
- Check your breasts for lumps and abnormal discharge
- If you’re breastfeeding, make sure your ducts aren’t clogged and you don’t have an infection
- Look at your abdomen for returning muscle tone
- Do a pelvic exam to see if your uterus is returning to its normal pre-pregnancy size and that the cervix is closed
- For c-section deliveries, make sure the incision is healing well and has no signs of infection
- Check how well any episiotomy or laceration has healed
- Administer any lab tests they think are necessary (such as a blood count if you lost a lot of blood during birth)
- Ask about your postpartum bleeding
- Ask about your pelvic floor recovery and refer you to a pelvic floor physical therapist, if needed If you’re having excessive pain, bleeding or problems with an incision, definitely tell your doctor, Riley says.
Postpartum checkups: Family planning
Another big item to cover during your postpartum checkups is birth control options . According to Riley, risk of complications in any subsequent pregnancy goes down if you wait at least 12 months after giving birth to conceive again. (The ACOG recommends ideally waiting at least 18 months.) Just because you’re breastfeeding and not menstruating yet doesn’t mean you can’t get pregnant . (After all, you ovulate before your first postpartum period arrives!) Your provider should discuss when you can safely start having sex again and talk you through your family planning options.
“It may seem like it’s too soon for that discussion, but some people do show up to their six-week postpartum appointment and find out they’re pregnant again!” Mustaleski explains, adding, “At your six- to eight-week postpartum appointment, many providers will do a Pap smear, if you’re due to have one done.”
Postpartum checkups: Emotional recovery
While physical recovery is certainly important, your doctor will also want to check in on how you’re coping with the transition to motherhood. During the visit, expect to answer questions about your mood, sleeping patterns and other aspects of your emotional well-being.
One big thing providers look for are signs of postpartum depression , which up to 15 percent of women experience, according to the American Pregnancy Association . The most common assessment is the Edinburgh Postnatal Depression Scale. “It’s a series of 10 questions that gives your doctor or midwife an overview of how you’re doing emotionally over the last seven days,” Mustaleski says. “If your score indicates that you’re experiencing postpartum depression, your doctor or midwife will discuss treatment options with you to help you start feeling your best as soon as possible.”
How to Prepare for a Postpartum Checkup
When you’re exhausted and sore, getting yourself out of the house for a postpartum checkup may seem daunting—but remember, these critical visits are set up to ensure your health and well-being.
Since this post-pregnancy stuff is completely new to you—the aches, the pains, the emotions—be sure to track and flag any symptoms you’re worried about, and write down all your questions beforehand. “Most new parents are functioning on minimal sleep, so attempting to recall your questions in the moment is difficult,” Mustaleski says. Her advice? Start a list on your phone that you can easily bring with you to the appointment. Your questions might touch on the topics mentioned above, plus:
- How your delivery went
- Baby’s safety
- Physical activity and exercise goals
- Breastfeeding or formula-feeding
- Returning to pre-pregnancy activities
- Body changes or new pains (pay attention to worsening pressure in your vagina, difficulty with bowel movement and inability to fully empty your bladder, Mustaleski says)
Make sure to also note any additional support you feel you need, such as a lactation consultant, pelvic floor therapist, mental health therapist or other professional.
As you prepare for a postpartum checkup, remember to also plan for childcare. Due to COVID-19, some offices may not be allowing baby to come with you. It’s always best to call ahead and ask about the office’s policies. “Many midwives will do a well-baby check up at the same time as your postpartum visit, so you can also ask if that is an option with your provider,” Mustaleski says. If you do end up bringing baby to the appointment, remember to pack a change of clothes, diapers, wipes, burp cloths, pacifiers (if baby is using them) and an extra bottle if baby’s not breastfeeding.
Postpartum checkups can be a lot to take in, but they’re ultimately designed to support you. Come prepared with any and all questions! “The postpartum is a time of in-between—you aren’t pregnant anymore, but you aren’t back to your everyday life,” Mustaleski says. “If you have questions about what is okay or safe for you to do during that transition, ask your provider to give you guidance on how to safely help your body recover.”
About the experts:
Laura Riley , MD, is a board-certified obstetrician who specializes in high risk pregnancies. She serves as the department chair of obstetrics and gynecology at Weill Cornell Medicine , as well as the obstetrician and gynecologist-in-chief at NewYork-Presbyterian/Weill Cornell Medical Center, based in New York City. She received her medical degree and completed her residency at the University of Pittsburgh School of Medicine.
Rebekah Mustaleski , CPM-TN, IBCLC, is a certified professional midwife specializing in evidence-based maternity care. She cofounded Roots & Wings Midwifery in Knoxville, Tennessee. Mustaleski received her bachelor’s degree in psychology from Centre College and worked as a doula and birth photographer prior to establishing Roots & Wings.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.
Next on Your Reading List

- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Your postpartum checkup
Your six-week postpartum checkup is a comprehensive visit with your OB or midwife to check on your recovery after childbirth. You'll have a complete examination, including a mental health screening and any tests or immunizations you need. If all is well, you'll get the okay to start exercising and having sex again. This postpartum checkup is a good time to ask for referrals and nail down your plan for birth control. Don't hesitate to call your healthcare provider, though, if you have any concerns or signs of complications before your scheduled visit.

What is the six-week postpartum checkup?
Why is a postpartum checkup so important, what happens at the six-week postpartum checkup, questions to ask your healthcare provider at your six-week postpartum checkup, can i bring my baby with me to my postpartum checkup, concerns that shouldn't wait for the six-week postpartum checkup.
The six-week postpartum checkup is a comprehensive visit with your OB or midwife. The purpose of this appointment is to check on your physical recovery from pregnancy and delivery, see how you're doing emotionally, and address your needs going forward. Many women think of it as the "go-ahead" visit, meaning your practitioner can verify that you're ready for more intense postpartum exercise and having sex again.
This shouldn't be your first postpartum checkup with your provider, though: The American College of Obstetricians and Gynecologists recommends that all women talk to their provider within three weeks after delivery and continue to receive follow-up care as needed, including a comprehensive checkup by 12 weeks postpartum. In many cases, that comprehensive visit happens at six weeks. (Your first contact is generally less comprehensive and may simply be a phone call or a virtual visit.)
Don't feel constrained by appointment dates, though. Sometimes physical or emotional issues come up that need immediate attention, like excessive bleeding , a potential postpartum infection , and any feelings that may lead you to think you might have postpartum depression or another postpartum mood disorder. Never hesitate to call your provider if you have concerns.
When you're busy caring for a newborn – and especially if you're feeling fine – it's easy to think about skipping your postpartum checkup. But this is an important visit. It's an opportunity for your provider to check on you, physically and emotionally. There are potential problems, such as infections and mental health issues, that could be missed without a visit and lead to more serious complications.
Your postpartum checkup is also an opportunity for you to ask questions about your birth experience and recovery, especially if you're recovering from a difficult birth experience . Are you wondering why something went the way it did during labor (why your contractions stopped for a bit or why your doctor used forceps , for example)? Worried about the chances of a repeat ( preterm delivery or cesarean , for example) next time?
You may still be dealing with some pregnancy- or childbirth-related aches and pains, too, and you may have some questions about how your body has changed. You may also have questions about postpartum issues like breastfeeding , birth control, exercise, sex, and going back to work . It helps to jot down the questions you want to ask and any other issues you'd like to discuss ahead of time.
If you've had a miscarriage , stillbirth , or neonatal death (when a baby dies in the first 28 days of life), it's important to see your provider to learn more about why it happened and to determine if you're at risk for it happening again in the future.
Here's what will typically happen at your postpartum checkup:
You'll undergo a physical exam.
During your physical exam, your healthcare provider will:
- Check your weight and blood pressure. They may also take your pulse and listen to your chest.
- Check your abdomen. They'll feel your belly to be sure that there's no tenderness and check your incision if you had a c-section . (Your provider would also have checked your incision a week or two after delivery to make sure it was healing properly.)
- Examine your breasts. They'll be on the lookout for lumps, tenderness, redness, and cracked nipples or abnormal discharge.
- Inspect your external genitalia, including your perineum. If you had an episiotomy , they'll check to see that it's healed.
- Do a speculum exam to look at your vagina and cervix. They'll be checking to see that any bruises, scratches, or tears have healed. And, if you're due for a Pap smear, they'll do that during the speculum exam.
- Do an internal pelvic exam to feel your uterus and check that it has shrunk appropriately, feel your cervix and ovaries to identify any problems, and check your vaginal muscle tone. They may also do a rectal exam.
- Manually check your thyroid (a gland in your neck responsible for hormone production) to make sure it's a normal size.
Your provider will also ask what physical symptoms you're having, such as whether you're still bleeding on occasion, having any abdominal discomfort, vaginal or perineal pain , urinary incontinence or anal incontinence , or breast pain. If you have a bothersome symptom that your healthcare provider didn't cover, don't be afraid to speak up. They'll also ask if you're breastfeeding and how it's going. If you're having any trouble, they can refer you to a lactation consultant .
Your provider will check on your mental health.
How you're doing emotionally is an important element of your follow-up care. Your provider will want to know how you're adjusting to the demands of motherhood and about any emotional problems you may be having. They'll ask you questions – or have you fill out a questionnaire – to screen for postpartum depression .
Don't be shy. Talk about the baby blues , if you felt them. Especially talk about any lingering sadness or depression you're still feeling. It's important to let your provider know if you're feeling overwhelmed, anxious, or depressed. They can provide medication that's safe to take now, even if you're breastfeeding. They can also refer you to a mental health specialist for ongoing care.
Your provider will order any tests or immunizations you need.
You may need lab tests if your provider is concerned about any conditions you had during pregnancy or delivery that might continue to affect you. If you had gestational diabetes , you'll need a glucose tolerance test. Your OB or midwife will provide you with any necessary follow-up care you need for special health conditions.
They'll also offer any immunizations you may need, such as a tetanus, diphtheria, and pertussis booster shot, a flu shot, a COVID-19 shot or booster (the COVID vaccine is safe for pregnant or breastfeeding women), or a rubella or chicken pox vaccine . (If you were not immune to rubella or chicken pox before your pregnancy, you should have been vaccinated before you left the hospital after delivery. If that didn't happen, it's highly recommended that you get vaccinated now.) The chicken pox vaccine requires two doses, so if you got your first dose immediately postpartum, you'll get the second dose now.
Getting vaccinated can help prevent you from getting sick and passing the illness to your baby. In some cases, it can also help you provide your baby with some immunity if you're breastfeeding.
You'll discuss birth control and family planning.
Talk with your provider about if and when you'd like to have more children. Because it's possible to become pregnant at any time postpartum (even if you haven't gotten your first postpartum period yet or you're breastfeeding ), it's important to talk about birth control.
You may need to make changes. For example, if you took the pill before pregnancy and are breastfeeding now, your practitioner will change your prescription to the "minipill" (progesterone only). Or you may decide it's time to try a different method. Talk with your provider about the pros and cons of each method you're considering. If you are planning on getting an IUD or an implant (like Nexplanon), let your OB provider know and they can insert it during this visit.
You'll get the okay to start exercising and having sex.
If all is well, you'll get the go-ahead for exercise, weightlifting, and sex. Ask your provider if there are any restrictions, because of complications you may have had or chronic conditions you have, for example. If you were active throughout pregnancy and had a vaginal delivery without complications, you've probably been able to do light exercise within days of having your baby, if you felt up to it. But if you had a c-section or weren't exercising all along, then your provider may want you to wait until your six-week postpartum checkup to begin exercising.
Don't worry if you don’t feel up to having sex yet, despite your clearance. Many women have little to no interest in sex for several months after giving birth. Wait until you feel ready.
Finishing up
Your provider will let you know when you should return for routine gynecological care (including any follow-up for your chosen contraceptive method) and give you any necessary referrals. Many women may benefit from physical therapy, such as pelvic floor physical therapy , especially if you had (or have) significant perineal tearing, a forceps delivery, diastasis recti , or urinary incontinence, for example. Talk to your provider to see if you need a referral.
They'll take care of necessary paperwork: If you're on maternity leave , for example, you may have forms for your healthcare provider to fill out, stating that you gave birth. The office team at your provider's office will know what to do to get this taken care of.
If you need a prescription refilled, make sure it's taken care of before you leave. And before you go, look at your notes and make sure that your provider has addressed all of your concerns.
Again, your postpartum visit is a great opportunity to ask your provider about your labor and delivery and your health. Come prepared with a list of questions that have come up in the past six weeks. Jot them down or note them on your smartphone.
Here are some examples:
- Can you check me for diastasis recti?
- Can you provide a referral to a lactation consultant?
- Can you provide a referral for pelvic floor therapy?
- Why were forceps (or a vacuum, or any other procedure) used to delivery my baby? It may have been explained to you at the time, but it's understandable if you don't remember! (Now's the time to get any lingering questions about your labor and delivery answered.)
- Will the fact that I had a preterm birth (or emergency c-section, or any other complication) mean that my next birth will be the same?
- How might the condition I had during pregnancy (gestational diabetes or preeclampsia , for example) affect my health now and in the future?
- What do you suggest for constipation ? (Or headaches, or any other discomfort you're having.)
- What supplements should I be taking now?
Most practitioners will be fine with bringing your infant to your follow-up appointment, but ask ahead of time to make sure.
If possible, consider asking someone to take care of your baby during your visit so you can be totally focused on yourself during your time with your provider. If you want to bring your baby along, have someone come with you to hold your baby and comfort them, if needed, during the visit. But don't neglect this follow up. Taking care of yourself now is just as important as taking care of your newborn.
Some postpartum complications are dangerous and warrant immediate action. Don't wait for your six-week postpartum checkup if you have any concerns about something not being quite right. Call your provider and ask. Also get in touch with your provider right away if you have any of these postpartum warning signs or symptoms:
- Excessive bleeding (blood flow that isn't slowing or that increases after three days, passing large clots, passing bright red blood after three days, or soaking more than one sanitary pad in an hour)
- Abdominal pain or tenderness
- Foul-smelling discharge
- A painful, hard, warm, red area or red streaks on your breast, which are signs of mastitis
- Painful urination or difficulty urinating or feeling of having to urinate often
- Swelling or tenderness in your legs and feet
- Pain, red streaks, or discharge from a tear or incision
- Severe, persistent headaches
- Changes in vision
- Pain in the upper right abdomen or shoulder
- Shortness of breath
- Nausea and vomiting
- Signs of postpartum depression, such as extreme sadness or despair, frequent crying, or extreme anxiety or panic
Call for emergency help if you have excessive bleeding and signs of shock (dizziness, chills , heart palpitations, blurry vision, pale or clammy skin, confusion), or if you ever have thoughts of harming yourself or your baby.
How long does postpartum recovery last?
Diet for healthy post-baby weight loss
How to use a sitz bath for postpartum relief
Was this article helpful?
When can I have sex after giving birth?

Ready for sex after pregnancy? Here's what to expect

When will I get my first period after birth?

How soon after giving birth can you get pregnant?

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
ACOG. 2021. Optimizing Postpartum care. ACOG committee opinion. The American College of Obstetricians and Gynecologists. Number 736. https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Optimizing-Postpartum-Care Opens a new window [Accessed March 2022]
CDC. 2022. Adult immunization schedule. https://www.cdc.gov/vaccines/schedules/hcp/imz/adult.html Opens a new window [Accessed March 2022]
March of Dimes. 2018. Your postpartum checkups. https://www.marchofdimes.org/pregnancy/your-postpartum-checkups.aspx Opens a new window [Accessed March 2022]

Where to go next

Appointments at Mayo Clinic
- Labor and delivery, postpartum care
Postpartum care: What to expect after a vaginal birth
When caring for a newborn, you might forget to care for yourself. But that's important too. Learn what's involved as you recover from giving birth.
Pregnancy changes a body in more ways than you might expect. And that doesn't stop when you give birth. Here's what can happen physically and emotionally after a vaginal delivery.
Vaginal soreness
You might have had a tear in your vagina during delivery. Or your healthcare professional may have made a cut in the vaginal opening, called an episiotomy, to make delivery easier. The wound may hurt for a few weeks. Large tears can take longer to heal. To ease the pain:
- Sit on a pillow or padded ring.
- Cool the area with an ice pack. Or put a chilled witch hazel pad between a sanitary napkin and the area between your vaginal opening and anus. That area is called the perineum.
- Use a squirt bottle to spray warm water over the perineum as you urinate.
- Sit in a warm bath just deep enough to cover your buttocks and hips for five minutes. Use cold water if it feels better.
- Take a pain reliever that you can buy without a prescription. Ask your healthcare professional about a numbing spray or cream, if needed.
- Talk to your healthcare professional about using a stool softener. Or ask about taking a laxative. Those medicines may help prevent problems with bowel movements — a condition called constipation.
Tell your healthcare professional if you have intense pain, lasting pain or if the pain gets worse. It could be a sign of an infection.
Vaginal discharge
After delivery, a mix of blood, mucus and tissue from the uterus comes out of the vagina. This is called discharge. The discharge changes color and lessens over 4 to 6 weeks after a baby is born. It starts bright red, then turns darker red. After that, it usually turns yellow or white. The discharge then slows and becomes watery until it stops.
Contact your healthcare professional if blood from your vagina soaks a pad hourly for two hours in a row, especially if you also have a fever, pelvic pain or tenderness.
Contractions
You might feel contractions, sometimes called afterpains, for a few days after delivery. These contractions often feel like menstrual cramps. They help keep you from bleeding too much because they put pressure on the blood vessels in the uterus. Afterpains are common during breastfeeding. That's because breastfeeding causes the release of the hormone oxytocin.
To ease the pain, your healthcare professional might suggest a pain reliever that you can buy without a prescription. They include acetaminophen (Tylenol, others) or ibuprofen (Advil, Motrin IB, others).
Leaking urine
Pregnancy, labor and a vaginal delivery can stretch or hurt your pelvic floor muscles. These muscles support the uterus, bladder and rectum. As a result, some urine might leak when you sneeze, laugh or cough. The leaking usually gets better within a week. But it might go on longer. Leaking urine also is called incontinence.
Until the leaking stops, wear sanitary pads. Do pelvic floor muscle training, also called Kegels, to tone your pelvic floor muscles and help control your bladder.
To do Kegels, think of sitting on a marble. Tighten your pelvic muscles as if you're lifting the marble. Try it for three seconds at a time, then relax for a count of three. Work up to doing the exercise 10 to 15 times in a row, at least three times a day. To make sure you're doing Kegels right, it might help to see a physical therapist who specializes in pelvic floor exercises.
Hemorrhoids and bowel movements
If you notice pain during bowel movements and feel swelling near your anus, you might have swollen veins in the anus or lower rectum, called hemorrhoids. To ease hemorrhoid pain:
- Use a hemorrhoid cream or a medicine that you put into your anus, called a suppository, that has hydrocortisone. You can buy either without a prescription.
- Wipe the area with pads that have witch hazel or a numbing agent.
- Soak your anal area in plain warm water for 10 to 15 minutes 2 to 3 times a day.
You might be afraid to have a bowel movement because you don't want to make the pain of hemorrhoids or your episiotomy wound worse. Take steps to keep stools soft and regular. Eat foods high in fiber, including fruits, vegetables and whole grains. Drink plenty of water. Ask your healthcare professional about a stool softener, if needed.
Sore breasts
A few days after giving birth, you might have full, firm, sore breasts. That's because your breast tissue overfills with milk, blood and other fluids. This condition is called engorgement. Breastfeed your baby often on both breasts to help keep them from overfilling.
If your breasts are engorged, your baby might have trouble attaching for breastfeeding. To help your baby latch on, you can use your hand or a breast pump to let out some breast milk before feeding your baby. That process is called expressing.
To ease sore breasts, put warm washcloths on them or take a warm shower before breastfeeding or expressing. That can make it easier for the milk to flow. Between feedings, put cold washcloths on your breasts. Pain relievers you can buy without a prescription might help too.
Hair loss and skin changes
During pregnancy, higher hormone levels mean your hair grows faster than it sheds. The result is more hair on your head. But for up to five months after giving birth, you lose more hair than you grow. This hair loss stops over time.
Stretch marks on the skin don't go away after delivery. But in time, they fade. Expect any skin that got darker during pregnancy, such as dark patches on your face, to fade slowly too.
Mood changes
Childbirth can trigger a lot of feelings. Many people have a period of feeling down or anxious after giving birth, sometimes called the baby blues. Symptoms include mood swings, crying spells, anxiety and trouble sleeping. These feelings often go away within two weeks. In the meantime, take good care of yourself. Share your feelings, and ask your partner, loved ones or friends for help.
If you have large mood swings, don't feel like eating, are very tired and lack joy in life shortly after childbirth, you might have postpartum depression. Contact your healthcare professional if you think you might be depressed. Be sure to seek help if:
- Your symptoms don't go away on their own.
- You have trouble caring for your baby.
- You have a hard time doing daily tasks.
- You think of harming yourself or your baby.
Medicines and counseling often can ease postpartum depression.
Weight loss
It's common to still look pregnant after giving birth. Most people lose about 13 pounds (6 kilograms) during delivery. This loss includes the weight of the baby, placenta and amniotic fluid.
In the days after delivery, you'll lose more weight from leftover fluids. After that, a healthy diet and regular exercise can help you to return to the weight you were before pregnancy.
Postpartum checkups
The American College of Obstetricians and Gynecologists says that postpartum care should be an ongoing process rather than a single visit after delivery. Check in with your healthcare professional within 2 to 3 weeks after delivery by phone or in person to talk about any issues you've had since giving birth.
Within 6 to 12 weeks after delivery, see your healthcare professional for a complete postpartum exam. During this visit, your healthcare professional does a physical exam and checks your belly, vagina, cervix and uterus to see how well you're healing.
Things to talk about at this visit include:
- Your mood and emotional well-being.
- How well you're sleeping.
- Other symptoms you might have, such as tiredness.
- Birth control and birth spacing.
- Baby care and feeding.
- When you can start having sex again.
- What you can do about pain with sex or not wanting to have sex.
- How you're adjusting to life with a new baby.
This checkup is a chance for you and your healthcare professional to make sure you're OK. It's also a time to get answers to questions you have about life after giving birth.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Landon MB, et al., eds. Postpartum care and long-term health considerations. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed Sept. 6, 2023.
- American College of Obstetricians and Gynecologists' Presidential Task Force on Redefining the Postpartum Visit and the Committee on Obstetric Practice. Committee Opinion No. 736: Optimizing postpartum care. Obstetrics & Gynecology. 2018; doi:10.1097/AOG.0000000000002633.
- Berens P. Overview of the postpartum period: Normal physiology and routine maternal care. https://www.uptodate.com/contents/search. Accessed Sept. 6, 2023.
- Expert view. What to expect at a postpartum checkup — and why the visit matters. American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/experts-and-stories/the-latest/what-to-expect-at-a-postpartum-checkup-and-why-the-visit-matters. Accessed Sept. 6, 2023.
- Kegel exercises. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-control-problems-women/kegel-exercises. Accessed Sept. 7, 2023.
- Frequently asked questions. Labor, delivery, and postpartum care FAQ091. Postpartum depression. American College of Obstetricians and Gynecologists. https://www.acog.org/Patients/FAQs/Postpartum-Depression. Accessed Sept. 6, 2023.
- Berkowitz LR, et al. Postpartum perineal care and management of complications. https://www.uptodate.com/contents/search. Accessed Sept. 7, 2023.
- Postpartum care. Merck Manual Professional Version. https://www.merckmanuals.com/professional/gynecology-and-obstetrics/postpartum-care-and-associated-disorders/postpartum-care#. Accessed Sept. 7, 2023.
- Marnach M (expert opinion). Mayo Clinic. Sept. 11, 2023.
Products and Services
- A Book: Obstetricks
- Available Solutions for Postpartum from Mayo Clinic Store
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- Breastfeeding and medications
- Breastfeeding nutrition: Tips for moms
- C-section recovery
- Eating the placenta
- Exercise after pregnancy
- Kegel exercises
- Postpartum complications
- Postpartum depression
- Pregnancy and breastfeeding when you have psoriasis
- Sex after pregnancy: Set your own timeline
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Postpartum care What to expect after a vaginal birth
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
Order details
You may also like
Postpartum recovery timeline: what to expect in the weeks and months after birth.

You've just had a baby. It's miraculous, beautiful, terrifying and already exhausting in equal measure. Whether you've had a c-section or vaginal birth, whether your baby was delivered in water or while you were hooked up to machines, you've been through a lot to bring your baby safely earth-side.
And all postpartum women deserve the highest praise imaginable for this achievement. In the lead up to your first birth, you may have attended childbirth classes with your birthing partner.
These classes are important for getting you into the headspace of childbirth, for asking your midwife questions and for demystifying the birth suite experience.
But we are so rarely prepared for the bits after birth: The postpartum recovery. Your postpartum recovery timeline will stretch until at least six months after your birth and can be a complicated landscape to navigate.
If this doesn't seem fair to you, you are right— it's really not!
You are soaking up your new baby, completely sleep-deprived and trying to adapt to the new normal of parenthood, but you will also be contending with bruising, scarring, postpartum bleeding, afterbirth pains and cramps, vaginal discharge, swelling and constipation.
Also, you'll cry. A lot. An intense fluctuation of hormones post-birth can give you the baby blues between moments of complete euphoria.
It's an incredible time of change and healing, so drawing upon your support network, as well as having some nifty postpartum care items on hand, will be vital for staying well and recovering as quickly as possible.
How long does it take to recover after giving birth?
Whether you have given birth vaginally or via C-section, you've been through one of the most primal, natural things a person can go through. However, just because it was natural doesn't mean your body didn't go through trauma to get your baby out safely — it's been stressed and stretched to the max.
The recovery timeline will be different for every woman, but the most important thing is this: Do not pressure yourself into a quick recovery. The postpartum period is about bonding with your baby, resting, asking for help, resting, healing and resting. Did I mention rest?
Rest is not just about sleep — it is about slowing down, listening to your body, nourishing it and letting it do its thing. Scars need to heal, blood needs to leave your body and your hormones need levelling out.
According to the American College of Obstetricians, postpartum recovery will normally take at least six to eight weeks, going up to 12 or longer depending on birth complications and your overall health.
The WHO defines the postpartum phase as beginning immediately after the birth of the baby and extending for up to six weeks (roughly 40 days).
How long does it take for your pelvic floor to recover after birth?
The uterus is a muscle that expands with a baby and contracts when the baby is out. By the end of pregnancy, the uterus will have grown outside of the pelvis to just below the breasts, pushing most of your organs to the sides to accommodate your baby.
And, within minutes of the birth, your uterus will start to shrink again, however, it will take about six weeks to fully return to its previous size . As it shrinks, you will feel uterine contractions which is a pain similar to menstrual cramps.
These will be especially painful if you are breastfeeding. Breastfeeding and nipple stimulation trigger a hormone known as oxytocin to be released into your bloodstream , which helps the uterus contract back into its pre-pregnancy size.
Don't worry if you aren't breastfeeding though as oxytocin, also known as the bonding hormone, is released with skin-on-skin contact between you and your baby. Not only is snuggling your baby helping them feel safe, love and bonded to you, it's also helping your uterus recover!
Unfortunately, cramps are a totally normal part of the postpartum recovery process as the body works hard to shrink your uterus and limit bleeding. Painkillers and a heating pad can help ease this pain.
The postpartum recovery timeline
The term "postpartum recovery" is often used to describe the first six to 12 weeks after you give birth, but your physical and mental recovery from pregnancy and birth may take much longer. So much has changed; family dynamics, your sense of self, your body shape and much more so this all plays into your recovery.
Many women still feel like they are in a postpartum stage up until the baby turns one, and that is completely valid.
Here is a non-exhaustive guideline of what to expect.
The first few days
Congratulations! Your baby is here.
The birth itself will be different for every woman, but all women will experience the following bodily and emotional changes as they start to adjust to life with a bub.
We're sorry to say that pain is unavoidable after a baby's birth . Perineal pain, sore nipples, back pain, episiotomy scars, afterbirth cramps and hormonal shifts will mean you need all the support you ask for. The right postpartum equipment is essential , as well as reaching out to your support network to bring you hot meals at home, do your laundry, bring you cups of tea and sometimes to hold your baby while you rest.
Sleep? What sleep?
Apart from the fact it's difficult to sleep in a hospital ward, your baby will be waking up with hungry cries every two to three hours looking for you. Babies are confused at this point — where am I? What happened to the safety of my lovely womb?
The only thing in the whole world they understand is you, that you know them, love them and your body is their home. Skin-to-skin contact, as well as colostrum and milk, is what your baby needs, so whip your top off and let your baby snuggle up to you as often as you can.
Toileting after childbirth
After the birth, your bowels will be blocked up. Your midwife or obstetrician will watch you closely and if you cannot pass urine within a few hours, a catheter will be inserted to help it out. Bowel motions will also be few and far between , so start taking stool softeners straight away.
Breastfeeding
Your midwife will be helping your baby latch within the first few hours of birth. This is often harder than most women anticipate: Your nipples will become sore and there may be some light bruising, and your breasts will become heavy, hot and leaky when your milk comes in.
Use breast pads for soaking up excess milk in your maternity bra and nipple balm for those painful nipples. And don't be afraid to ask for as much help as you need to get that latch right.
Colostrum becomes milk
While in hospital, your midwife or lactation consultant will be helping you get this magical liquid gold into your baby through breastfeeding or through syringe extraction — the latter may happen if your baby takes a bit longer to latch or if you're not going down the breastfeeding path.
Colostrum is a thick, sticky substance that will eventually turn into milk after a few days, and they call it "liquid gold" as it's packed with antibodies for your baby's first ever snack; it helps fight infection, assists with important physiologic functions, maintains the baby's blood sugar and even has a laxative effect. You'll only produce a few teaspoons of this amazing stuff, but that's all your baby needs before it thins out and becomes milk.
Hormonal shifts
After you give birth, you may feel very weepy, fragile and prone to feelings of sadness. This is normal and is not necessarily postpartum depression! Progesterone and estrogen, the hormones you had an abundance of during pregnancy, decrease as soon as both the baby and the placenta are delivered. Oxytocin, the bonding hormone, surges immediately following birth to compensate for the initial drops in progesterone and estrogen.
Oxytocin will help your mothering instincts kick into gear, but the rapid hormonal shift will certainly set off an emotional rollercoaster. Rest assured these hormones start to even out within three to six weeks postpartum.
This won't happen to all women after birth, but many experience swollen legs, face, feet, ankles, hands and arms within the first few days. During your pregnancy, you retained a lot of fluid to keep your baby healthy and that won't disappear overnight.
This, combined with an IV drip with your C-section or epidural, means that there's a lot of water floating around your body. Elevate your legs, walk around the house when you can, dress in light clothing and drink lots of fluids to help ease swelling. Compression stockings and some light massage can also help.
Vaginal delivery recovery
Depending on how much you have torn, your vagina will hurt. A lot. Perineal pain is normal and can be soothed by treating your vagina like an open wound. Use a perineal spray bottle instead of wiping as wiping can accidentally open up stitches. Cold pads for your underwear are lifesavers to help heal and numb the ache.
Witch hazel foam is also extremely helpful for soothing hemorrhoids which may develop from all the pushing you did in labour. And of course, maxi pads are necessary for vaginal bleeding , which will start immediately after the birth and last for a few weeks. You may even need more than one pad an hour. For keeping cooling pads and maxi pads in place, a pair of comfy, high-waisted mesh undies will work wonders.
C-section delivery recovery
One in three Australian women opt for a cesarean birth. You will likely have a longer stay in the hospital than if you had a vaginal delivery just so the midwives and doctors can keep an eye on you. A C-section is a major surgery that requires lots of care and as much rest as possible. The incision will be very delicate and doctors actually recommend you hold your abdomen when you need to sneeze or cough.
A belly band can work well for C-section recovery as they are proven to reduce swelling, protect the incision and even provide pain relief. Unfortunately, C-sections don't let you off the hook with vaginal bleeding, so mesh undies and maxi pads will be your best friends for a while.
The first few weeks
You will be starting to get the hang of this whole baby thing. Great work!
But you should still expect little of yourself physically and emotionally, this is only the beginning of your postpartum recovery timeline.
Call upon family and friends to support you as much as you need — accept help, ask for help and know that this is your time to be looked after.
Over the next few weeks you will be losing a lot of blood from your vagina regardless of your vaginal or c-section delivery — blood is inescapable. After the first three weeks, your blood will go from bright red to a dark brown, just like at the end of your regular period, then you'll experience a decrease in flow and then it will disappear.
You will still be in some pain in your perineum and nipples, but your cramping should have stopped by now. Your perineum wounds will have healed up within four to weeks postpartum as new tissue grows in the torn area. Talk to your healthcare professional if you don't think you're healing properly and use pain meds as directed.
Your breast milk should be established by now and you will be leaking all over the place as you establish a feeding routine with your baby. It will be sticky and you will wet through a number of shirts, but this is totally normal! Breast pads will still be essential for the first six months of breastfeeding.
Constipation
This will likely still be an issue in the first few weeks of birth. Keep stool softeners on hand and, if you can, do some light walking to get things moving down there, but avoid strenuous exercise.
First postpartum checkup and midwife visit
After one week, you will be expected to visit your GP so they can examine your new baby and to ensure you're recovering well. Ask them to check your blood pressure, your perineum or your C-section scar and arrive armed with any questions you might have about recovering.
Within two to three weeks, a midwife will come and visit you in your home to check up on your baby, your recovery and your mental wellbeing. You can ask them as many questions as you need to — they are there to support you. Don't forget you can also hire a private lactation consultant or postpartum physio to visit you at home to give you that extra support.
Postpartum hair loss
The drop in estrogen, the hormone that made your hair and nails strong and shiny throughout your pregnancy, will lead to your hair falling out. Don't be surprised if you find lots of hair in the shower drain, on your pillow and around your house — this is normal and stops around the six-month mark.
Your incision will still be healing and so the belly band and cold packs will still be necessary at this point. You also won't be able to drive until the six-week mark, so make sure you're delegating lots of tasks to those around you.
Avoid strenuous exercise, but do take gentle walks as often as you can. The movement will help your body heal and prevent constipation and blood clots. Plus, walks are a great way to introduce your baby to the world. Keep up those pelvic floor exercises while at home.
Hormonal shift
If you are still feeling the "baby blues" (depressed, anxious or having trouble bonding with your baby), this is OK and nothing to be ashamed of. Your hormones will have balanced out after two to three weeks, but if you believe you may have the beginnings of postpartum depression, contact your midwife, GP, counsellor, psychologist or social worker. They will help you organise a support plan to make sure your emotional health stays well.
One to three months
By the three-month mark, your perineal pain will have subsided completely, and your C-section incision would also have healed up. Keep up the creams and balms on your C-section scar to help it along and to prevent itchiness.
Your baby will grow and need more milk in a short space of time. Cluster feeding will happen at the five to six-week point for both breast and formula-fed bubs, meaning there will be a period of 24 to 48 hours where it will feel like you are constantly feeding your baby. This is normal — your baby is letting your breast milk know they have to increase in production to keep up with your growing baby.
A feeding routine will have been established by now, but if you are experiencing hard, hot, lumpy breasts you may have the beginnings of mastitis . Try heat packs on the breasts, massage them in hot water or use a lactation massager to help unblock ducts and keep breast production moving.
At this point, some light walking is recommended for both C-section and vaginal delivery, but strenuous exercise is still not recommended. Walking can help with constipation, preventing blood clots and aids the overall healing process. Plus, your baby will love being pushed in a pram and getting acquainted with the world.
After birth, your tummy will be wobbly . It's a fact. You might have been hoping to "snap back" quickly after birth, but this timeline will be different for every woman. It is normal for your tummy to look flabby as it recovers from holding a baby for nine months, and it's important you do not put pressure on yourself to change quickly. Eat nourishing foods and do some light exercise at this point. The most important thing is ensuring you and your baby are healthy.
Bladder control
After birth, most women will experience urinary incontinence to some degree. Be prepared to accidentally pee yourself after sneezing, coughing, laughing or during exercise. This is all totally normal due to the stretching of the pelvic floor muscles during pregnancy and delivery. Pelvic floor exercises are vital for helping for preventing long-term incontinence. But if your tummy still looks pregnant or feels abnormally large, call your doctor, as you might be experiencing abdominal separation and require help treating this.
Three to six months
You are doing so well. Your baby will now be smiling, laughing and making little noises at you. But they still need you more than anything else in the world. Skin-to-skin contact is still highly beneficial for your baby as they navigate this whole new world.
Your postpartum symptoms will be starting to completely subside. Your C-section incision/perineum pain should be gone, but if it hasn't, please talk to your doctor.
At this point, you will still be experiencing postpartum hair loss and issues with bladder control (keep up those pelvic floor exercises), but you will also be cleared for sexual activity and more exercise than walking.
Your C-section scar might feel numb or itchy, but it will be generally healed. Your period may come back within three to six months, although this may take longer if you are breastfeeding. And, you may be feeling overwhelmed and exhausted. You are still in the postpartum recovery period, and life has changed forever.
If you are experiencing severe feelings of depression and anxiety, reach out to a mental health professional. Postpartum depression is highly prevalent in Australian women — you are not alone.
Six months to one year
By now, you're a baby expert. Your baby will start to roll over, clap and show signs of wanting to play. Your baby's feeds will be more spaced out, allowing you to sleep slightly longer, and you have survived cluster feeds, leaking breasts, poo explosions, and many a sleepless night. You are amazing.
If your period hasn't returned, it should come back sometime within six to 12 months.
Your milk will be well and truly established and, if you're not breastfeeding, it would have completely dried up by now. Your hair will have stopped falling out and you'll have much more control over your bladder.
Postpartum depression can actually occur at any time within the first year of your baby's birth, and not necessarily within the first few weeks.
According to the American College of Obstetricians and Gynaecologists, a person is more likely to develop postpartum depression if they have had a history of depression, but also if they have little in the way of support from family and friends.
If you think you have postpartum depression, a combination of talk therapy, getting support with your baby, minimising fatigue and, sometimes, antidepressants can help.
Can I speed up the postpartum healing process?
Sometimes in life, you have to let nature take its course. Healing from birth takes time and if you look after yourself as much as your baby after delivery, this will ensure a smooth recovery — it is far better to recover well than to hope for a speedy recovery.
But most importantly, you are in charge here. You are the one who knows your body best, who knows what you can and can't handle and only you know how well you're recovering. This postpartum recovery timeline is not a fixed guide.
Your recovery will depend on many factors including the health of your baby, complications during labour and delivery and many other lifestyle and health-related aspects.
While you technically can't speed up the recovery process, you can slow it down if you do not get enough rest, if you put pressure on yourself to exercise quickly, or if you do not ask for help.
Ease pain, rest, use your postpartum essentials , cuddle your baby and don't worry about your baby weight — all these things will happen in the time that is right for your body.
You are amazing for all you've achieved and now it's time to let your support network take care of you.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6992410/
- https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/05/optimizing-postpartum-care
- https://www.nwh.org/patient-guides-and-forms/postpartum-guide/postpartum-chapter-2/postpartum-care-pain-management
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7495339/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8094397/?report=reader
- https://www.cdc.gov/breastfeeding/data/mpinc/maternity-care-practices.htm
- https://pubmed.ncbi.nlm.nih.gov/32761813/
- https://www.medela.com.au/breastfeeding/mums-journey/colostrum
- https://www.thewomens.org.au/health-information/pregnancy-and-birth/your-health-after-birth/what-to-expect
- https://www.betterhealth.vic.gov.au/health/healthyliving/caesarean-section
- https://pubmed.ncbi.nlm.nih.gov/28241386/
- https://raisingchildren.net.au/grown-ups/looking-after-yourself/new-mums/new-mums-first-weeks
- https://www.aad.org/public/diseases/hair-loss/insider/new-moms
- https://raisingchildren.net.au/newborns/breastfeeding-bottle-feeding/breastfeeding-challenges/blocked-duct-mastitis-abscess
- https://www.ncbi.nlm.nih.gov/books/NBK555904/
- https://www.acog.org/womens-health/faqs/postpartum-depression
The Postpartum Recovery Bundle

Breastfeeding Essentials

Healing Foam

Postnatal - 1 Month Supply

C-Section Recovery Bundle
Related stories.

Postpartum care: What you need and what to expect from the months after birth
A must-read ahead of welcoming your newest addition.

7 postpartum gifts for the new mum in your life
This year, we're giving the gift of postpartum care.

Postpartum hair loss: Your guide to shedding hair after pregnancy
Let's get a handle on how your hair changes after giving birth.

Sign up for our newsletter
All of the tools you need to take your reproductive health into your own hands.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Postpartum Care: A Guide to Taking Care of a Body That Just Delivered
- First 24-Hours Instructions
- Days and Weeks After Birth
- Coping Through Changes
- Postpartum Follow-Up
- Resources and Support
The postpartum period, the time after giving birth, is a crucial time for recovery and the long-term health of the parent and baby. It's also a time of intense physical and emotional changes.
It is normal and expected to experience several physical symptoms like swelling, cramping, breast tenderness , constipation , and leaking milk. It is also common to experience emotional changes like feeling sad and overwhelmed.
This article discusses postpartum care, what to expect, and how to care for yourself.
Yoss Sabalet / Getty Images
Postpartum Care: Instructions for the First 24 Hours
The first 24 hours after birth can feel like a whirlwind. Your focus is both on healing physically and caring for your newborn.
Physical symptoms you may experience in the first 24 hours include:
- Perineum soreness : If you had a vaginal birth , the area between the vagina and the rectum may feel sore or painful. This is because of stretching or tearing during labor and delivery.
- C-section pain : If you had a surgical deliver known as a cesarean section (C-section), you may feel exhausted and pain around your incision. Rest is crucial.
- Afterbirth pains : After giving birth, your uterus will begin to shrink back to its original size, which may cause abdominal cramping.
- Vaginal discharge : Vaginal bleeding after delivery is expected. However, call your provider if you have heavy, bright red bleeding or are passing golf ball–sized blood clots.
- Breast engorgement : This occurs when the breasts fill with milk a few days after delivery.
- Swelling : Pregnancy causes water retention in the body, especially the hands, feet, and face. It may also be a sign of preeclampsia and should be discussed with a medical provider.
- Constipation : It may feel difficult to have a bowel movement after giving birth.
- Pain with urination : If you had vaginal tearing with birth, you may experience pain or burning with urination, leaking, and incontinence .
- Fatigue : Your body will feel tired from the exertion of childbirth, blood loss, and a lack of sleep.
It's common to feel overwhelmed and exhausted or down and sad. The "baby blues" are typical feelings that come after having a baby and are typical for up to two weeks.
Postpartum Care in Days and Weeks After Birth
The days and weeks after giving birth can be emotional. You will likely not feel like yourself because of your physical recovery, changing hormone levels, and caring for a newborn.
It is important to see your healthcare provider during the postpartum period. Your provider can help keep you and your newborn healthy.
Healing From Birth
Giving birth is physically exhausting and requires time to heal. There are many symptoms you might feel during the postpartum period. Fortunately, there are ways to help relieve them.
Postpartum sleep can be challenging. You will likely feel tired in the weeks and months after giving birth. To help your body heal, focus on resting as much as possible. Sleep when your baby sleeps. Consider limiting visitors to help you catch up on rest. If some of your loved ones have offered to help you, ask them to take over household chores so you can use that time to rest.
Mental Health
It's common to feel sad, anxious , or irritable for up to two weeks after giving birth. When frequent feelings of sadness, anxiety, hopelessness, or anger last longer than two weeks, you may have postpartum depression .
Postpartum depression affects about 1 in 8 people in the postpartum period. Symptoms may include:
- Feeling angry, sad, hopeless, guilty, or worthless much of the time
- Eating more or less than usual
- Sleeping more or less than usual
- Crying frequently
- Losing interest in favorite activities
- Withdrawing from friends and family
- Having thoughts of hurting yourself or your baby
If you are concerned about your mood, talk with your healthcare provider right away. Fortunately, postpartum depression is treatable with therapy support groups, medication, and support. Other measures that may help include:
- Rest as much as possible.
- Ask for help.
- Make time to see friends and family.
- Share your experience with fellow parents or a support group.
- Avoid making significant life changes.
Contraception
It may seem too soon to start thinking about future pregnancies, but it is important to have a contraception plan when you are postpartum. Most healthcare providers recommend abstaining from sex for about four to six weeks after giving birth. This is how long it usually takes to heal.
Once you are ready to have sex again, talk with your provider about a contraception plan. You may consider barrier methods like condoms and diaphragms or hormonal methods like pills , patches, intrauterine devices (IUDs), or shots.
Coping Through Postpartum Changes
The postpartum period brings countless changes. It may be helpful to make a plan for changes in this new chapter of life.
Physical and Self-Esteem
The physical exertion of childbirth, lack of sleep, and other factors may make you uncomfortable. Focus on rest and recovery. Caring for a newborn requires a lot of time, but aim to eat, sleep, and shower daily.
Plan to wear a sanitary pad in the days and weeks after birth due to vaginal bleeding. Drink plenty of water, and add healthy, fresh foods to your meals when possible.
Talk with your healthcare provider about an exercise plan. There are several benefits to working out in the postpartum period, including increased energy, better sleep, stress relief, and stronger muscles. Start slow, taking 10-minute walks, and work up from there.
Adjusting to Parenthood
Adjusting to life as a new parent (or a parent with another child) takes time. Try to focus on small things that help you feel like yourself. Sleep whenever you can, and spend time resting throughout the day. Talk to your partner, friends, or loved ones about how they can support you.
It's normal to not feel like yourself at first or to feel sad and overwhelmed in the postpartum period. If you find yourself feeling this way for more than two weeks, speak to your healthcare provider because you could be experiencing postpartum depression.
Learning how to feed your newborn takes time and may be challenging. If you are using formula to feed your baby, discuss recommendations with your child’s pediatrician.
If breastfeeding , seek support from a lactation consultant, midwife, or healthcare provider. They can help with any breastfeeding challenges or questions. It's important for people who breastfeed to drink water throughout the day and consume an extra 500 calories daily.
When your milk first comes in, it may cause engorgement when the breasts fill with milk and feel full and tender. Frequent feedings, breast massage, and warm showers can help. See your healthcare provider if you develop a fever or chills while breastfeeding. Mastitis is a common infection in breastfeeding people and can be treated with antibiotics.
Going Back to Work
Going back to work is an emotional experience after having a baby. If possible, start planning your return to work while pregnant. Talk with your employer about any accommodations you may need, like a flexible schedule or breaks to pump breast milk.
It is also important to develop a childcare plan ahead of time. Decide if you will need to hire a babysitter or nanny or take your baby to a daycare in a home or facility.
As your return to work gets closer, practice for the big day. It may help to have a morning in which you get ready as if for work and think through any possible issues that could come up. If you are planning to continue breastfeeding after going back to work, practice with the breast pump ahead of time.
When you return to work, remember it’s normal to feel different. You have undergone changes. Try to be patient with yourself and those around you. This is a big transition, and it will take time.
Postpartum Follow-Up
It is important to continue seeing your healthcare provider after giving birth. Healthcare providers recommend checking in within three weeks of giving birth and seeing them for a visit within 12 weeks. Most people see their providers about six weeks after giving birth. About 40% of people do not attend their postpartum visit.
During your follow-up visit, your provider will ask about your physical and emotional health. They will talk with you about your mood and any symptoms you are experiencing. Your provider will likely examine your incisions if you have them and will perform a pelvic exam to determine if you have healed from birth. Talk with your provider about any concerns you have.
Resources and Support
Everyone needs support during the postpartum period. If you have friends and family members offering to help, take them up on it. If you do not have people in your life to help you, there are still resources available. These resources include:
- Postpartum: The Birth Injury Center , Centering Pregnancy/Parenting
- Breastfeeding: La Leche League , American Academy of Family Physicians
- Mental health: 988 Suicide & Crisis Lifeline (phone or text 988), National Domestic Violence Hotline , Live Another Day
- Healthy food: Women Infant Children , Cooking Matters
- Affordable housing: Volunteers of America , Catholic Charities
If a loved one recently gave birth, you may wonder how best to support them. Ways to show support include:
- Listening to their concerns
- Learning the signs of postpartum depression
- Providing rides to medical appointments
- Offering to help care for the baby
- Assisting with daily chores
The postpartum period is an intense time of life. You will likely experience several changes, both physical and emotional. It is important to focus on your health and well-being in addition to your newborn.
It is normal and expected to experience several physical symptoms like swelling, cramping, breast tenderness, constipation, and leaking milk. Emotional changes like feeling sad and overwhelmed are common, too. There are resources available to help you during the postpartum period.
MedlinePlus. Postpartum care .
American College of Obstetricians and Gynecologists. Optimizing postpartum care .
Adams YJ, Miller ML, Agbenyo JS, Ehla EE, Clinton GA. Postpartum care needs assessment: women's understanding of postpartum care, practices, barriers, and educational needs . BMC Pregnancy Childbirth . 2023;23(1):502. doi:10.1186/s12884-023-05813-0
Centers for Disease Control and Prevention. Pregnant and postpartum women .
Paladine HL, Blenning CE, Strangas Y. Postpartum care: an approach to the fourth trimester . Am Fam Physician . 2019;100(8):485-491.
Nemours Kids Health. Recovering from delivery .
Reichner CA. Insomnia and sleep deficiency in pregnancy . Obstet Med . 2015 Dec;8(4):168-71. doi:10.1177/1753495X15600572
Office on Women’s Health. Postpartum depression .
American College of Obstetricians and Gynecologists. Postpartum birth control .
Office on Women’s Health. Recovering from birth .
American College of Obstetricians and Gynecologists. Exercise after pregnancy .
Centers for Disease Control and Prevention. Partners, friends, and family of pregnant or postpartum women .
By Carrie Madormo, RN, MPH Madormo is a health writer with over a decade of experience as a registered nurse. She has worked in pediatrics, oncology, chronic pain, and public health.
Your Postpartum Checkups
Medical review policy, latest update:.
Added FAQs to the article with updates to sourcing and check on text for #BumpDay 2023.
What is a postpartum checkup?
When is my first postpartum checkup, is there still a six-week postpartum checkup, read this next, how to prepare for your postpartum checkups, can i bring my baby to my postpartum checkups, what happens at my postpartum checkup, give you an annual exam, examine your post-pregnancy body, make sure no serious health issues have cropped up since you delivered, get the go-ahead of when to start working out again and go back to normal activities, discuss your mental health and how you're feeling, talk about resuming sex after baby and get you back on birth control, chat about any future baby plans (if applicable).
Remember: Your health is important, and taking good care of yourself helps you take good care of your baby. That's why it's necessary to schedule and attend your postpartum doctor's appointments. An added bonus? You'll probably feel better and more reassured after the visit with your practitioner too.
Postpartum Checkup FAQs
How many postpartum checkups do you need, what does a postpartum checkup consist of, what happens if i miss my postpartum checkup, do they test urine at postpartum checkup, updates history, go to your baby's age, trending on what to expect, the covid-19 vaccine for infants, toddlers and young children, how to create a night shift system when you have a newborn, ⚠️ you can't see this cool content because you have ad block enabled., when do babies start laughing, baby-led weaning, what happens in the ‘4th trimester’ (and is it a real thing).
- Getting pregnant
- Preschooler
- Life as a parent
- Baby essentials
- Find your birth club
- Free antenatal classes
- Meet local parents & parents-to-be
- See all in Community
- Ovulation calculator
- Am I pregnant quiz
- How to get pregnant fast
- Best sex positions
- Signs of pregnancy
- How many days after your period can you get pregnant?
- How age affects fertility
- Very early signs of pregnancy
- What fertile cervical mucus looks like
- Think you're pregnant but the test is negative?
- Faint line on pregnancy test
- See all in Getting pregnant
- Pregnancy week by week
- How big is my baby?
- Due date calculator
- Baby movements week by week
- Symptoms you should never ignore
- Hospital bag checklist
- Signs of labour
- Your baby's position in the womb
- Baby gender predictor
- Vaginal spotting
- Fetal development chart
- See all in Pregnancy
- Baby names finder
- Baby name inspiration
- Popular baby names 2022
- Numerology calculator
- Gender-neutral names
- Old-fashioned names
- See all in Baby names
- Your baby week by week
- Baby milestones by month
- Baby rash types
- Baby poop chart
- Ways to soothe a crying baby
- Safe co-sleeping
- Teething signs
- Growth spurts
- See all in Baby
- Your toddler month by month
- Toddler development milestones
- Dealing with tantrums
- Toddler meals
- Food & fussy eating
- When to start potty training
- Moving from a cot to a bed
- Help your child sleep through
- Games & activities
- Vomiting: what's normal?
- See all in Toddler
- Your child month by month
- Food ideas & nutrition
- How kids learn to share
- Coping with aggression
- Bedtime battles
- Anxiety in children
- Dealing with public tantrums
- Great play ideas
- Is your child ready for school?Top tips for starting school
- See all in Preschooler
- Postnatal symptoms to watch out for
- Stitches after birth
- Postpartum blood clots
- Baby showers
- Sex secrets for parents
- See all in Life as a parent
- Best baby products
- Best formula and bottles for a windy baby
- Best car seats if you need three to fit
- Best nappies
- Best Moses baskets
- Best baby registries
- Best baby sleeping bags
- Best baby humidifier
- Best baby monitors
- Best baby bath seat
- Best baby food
- See all in Baby essentials
- Back pain in pregnancy
- Pelvic girdle pain
- Perineal massage
- Signs you're having a boy
- Signs you're having a girl
- Can you take fish oil while pregnant?
- 18 weeks pregnant bump
- Can you eat salami when pregnant?
- Edwards' syndrome
- Missed miscarriage
- Should I harvest my colostrum?
- Rhesus positive vs. Rhesus negative
- What do contractions feel like?
- Hunger in early pregnancy
- First poop after birth
- When do babies sit up?
- When can babies have salt?
- MMR vaccine rash
- Vaping while breastfeeding
- How to transition from formula to milk
- When do babies start grabbing things?
- Sperm allergy: can sperm cause itching?
- How long after taking folic acid can I get pregnant?
Why am I having so few antenatal appointments the second time around?

- 41 weeks , if your baby hasn’t arrived yet
Was this article helpful?
Can I still breastfeed my baby while I'm pregnant?

5 things nobody tells you about being pregnant when you have a toddler

Why I don't feel guilty about sending my son to nursery

20 reasons to be glad you're having another baby

Where to go next

Ready Steady Baby
Your antenatal care.
In Scotland, the NHS provides pregnancy, labour and postnatal (after birth) care.
During your pregnancy, you’ll have regular antenatal (pre-birth) appointments with your midwife or obstetrician.
Some of your appointments will be face to face at a midwife hub, hospital or at home.
Other appointments may be video calls using NHS Near Me.
More information about NHS Near Me video appointments
More about antenatal care and classes during COVID-19
Your rights
You’ll be given information about your rights and choices, to help you make your own decisions about treatment and care.
You have the same rights regardless of your age, sexuality, race, religion, or any other reason. If you feel you are being treated differently, speak to your midwife, GP, or a friend or family member you trust.
Maternity Action has more information about your maternity rights .
Antenatal appointments
You’ll usually have 8 to 10 appointments with your primary midwife during your pregnancy. Your primary midwife is the midwife you see most often.
Some women may need more, or might have appointments with other members of their healthcare team.
Your first main appointment is called your booking appointment.
It’s important to go to all appointments. If you can’t attend an appointment for some reason, then it’s okay to rearrange it for another time close to the original appointment.
These appointments are important for you to build a relationship with your primary midwife. With your permission, your primary midwife will:
- monitor how you and your baby are doing
- support you to have the information you need to make decisions about your care, birth, and becoming a parent
- pick up any issues or concerns early
You’ll be offered some tests each time, such as:
- blood pressure
- growth check
- a urine test
At your appointment, you can:
- ask questions
- talk about your options throughout pregnancy, birth and after you have your baby
- explore any benefits or risks
- be supported to make decisions that feel right for you and your baby
- get advice and support about anything you’re worried about
- talk about how you’re getting on
Growth checks
How a baby grows is different for each woman, and your midwife will do a growth check at each antenatal visit.
One way growth is measured is by measuring the size of your womb or baby bump. This is known as fundal height. The measurements are recorded on a chart and can be used to monitor how your baby is growing.
You might also be offered a growth scan. If you are offered a growth scan, your midwife will explain why.
Read more about how your baby develops
Antenatal classes
Your midwife will tell you about antenatal classes at your appointments.
Antenatal classes, often called parent education classes, will:
- help you prepare for being a parent
- help you plan for the birth and the first few weeks with your baby
The classes are a great opportunity for dads, partners or any person you choose to support you to get involved too.
Groups and classes may be in person or may be virtual, so you can access them on your phone, tablet, or laptop.
Learn more about antenatal classes during COVID-19
Your maternity notes
All of your antenatal care is recorded in your electronic Scottish Women-Held Maternity Record (SWHMR), commonly known as maternity notes. You may be given an app to use instead, which links to your electronic record.
Ask your midwife to go through your maternity notes with you on the app or on paper.
Your maternity notes have information about:
- any previous pregnancies
- your current and previous health and wellbeing
- your test results
- how your baby is growing and your pregnancy is progressing
- your maternity unit, your primary midwife and how to contact them
- your ongoing plan of care
- your birth plan
Your maternity notes also have contact details for your primary midwife and maternity unit.
You might see medical words and abbreviations in the record. If you’re not sure what these mean or if you want more information, ask your midwife to explain.
Looking after your notes
You should:
- take your maternity notes with you to all your appointments (whether they’re on paper or an app)
- keep them in a safe place
- have them with you when labour starts
- take them with you if you’re away from home for any length of time
This helps to make sure all health professionals that care for you know how your pregnancy has been, so they can give you the best possible care.

Screening tests and scans
You’ll be offered tests during your pregnancy to make sure you and your baby are healthy and well.
If any issues or health conditions are found, this will be discussed with you. You’ll be supported to make choices that feel right for you and your baby.
Screening tests and scans can also help you and your baby be monitored more often and receive treatment quickly, if it’s needed. This can help to prevent serious illness and can save lives.
Read more about tests in pregnancy
Home blood pressure and urine monitoring
Your blood pressure and urine will be checked regularly throughout your pregnancy.
Your maternity care team may discuss home monitoring with you and help you decide whether it feels right for you and your baby.
More about home blood pressure and urine monitoring
Paying for care
If you don’t usually live in Scotland, you’ll probably have to pay for NHS maternity care, although there are a few exceptions to this.
You must not be refused treatment or have it delayed because you need to pay.
Read information from the Scottish Government on accessing care for overseas visitors
Source: Public Health Scotland - Opens in new browser window
Last updated: 25 January 2023
Help us improve NHS inform
Your feedback has been received
Don’t include personal information e.g. name, location or any personal health conditions.
Other health sites
- NICE: Antenatal care
- Tommy's: Antenatal care
Also on NHS inform
- Disabled Living Foundation (DLF)
- Rica: consumer research charity
- Health & Care Professions Council (HCPC)

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Eur J Midwifery

Postnatal virtual and home visits by midwives during COVID-19 pandemic
Maria gjoni.
1 Midwifery Department, University of West Attica, Athens, Greece
Efstathia M. Alevizou
Dear Editor,
During the COVID-19 pandemic postnatal midwifery-led care remains a key public health intervention for women and their families 1 , 2 . Home or virtual visits by community midwives should be provided to reduce the number of times women and newborns need to leave their home 1 . In order to comply with social distancing requirements, community midwives could deliver home or virtual visits and individualized postnatal care, according to the needs of the mother and the newborn 1 . Midwifery-led postnatal home visiting could raise consciousness in parents on establishing breastfeeding, family planning and contraception after birth, preparation of milk formula, smoke-free environments at home, home hygiene, and care of the neonatal – especially after NICU discharge 3 . Midwifery-led virtual visits via videoconferencing decrease the number of visits to health facilities and enable mothers to be consulted immediately and from their own home 4 . Virtual visits have been demonstrated to be as safe as in-person visits 5 . Therefore, as early as possible, community midwives (especially those serving rural and remote areas) should receive all the relevant technology equipment and training regarding remote consultation 5 .
The World Health Organization (WHO) recommends at least four postnatal visits for all mothers and newborns, on day 1 (first 24 hours), on day 3 (48–72 hours), between days 7–14 and six weeks after birth 6 . However, a face-to-face consultation is required for physical examination and/or screening of mother and the newborn 1 . Therefore, home visiting should be prioritized for women with psychosocial vulnerabilities, operative birth, premature or low birthweight baby and other medical or neonatal complications 1 . Awareness should be raised about exposure to COVID-19 during a home visit, where midwives should abide by strict infection control equipment and procedures when entering and leaving homes 1 .
Midwifery-led services are vital during the postpartum period for women suspected or confirmed with COVID-19. Parenting and breastfeeding support can be offered through face-to-face or virtual visits 1 . Μothers with COVID-19 should be advised to establish breastfeeding or to express breastmilk, applying appropriate infection prevention and control measures 2 , 7 . All breastfeeding women should be shown how to hand-express their breast milk and be advised on how to correctly store and freeze it. Breastfeeding counseling, neonatal care, family planning counseling, psychosocial parent support, practical feeding support and home hygiene should be provided to all mothers and their families, whether they or their children have suspected or confirmed COVID-19 7 .
Community midwives are a valuable resource either providing face-to-face visits or virtual visits 8 . They need adequate support 8 to provide quality, holistic, women-centered postnatal care to mothers and newborns 9 in these exceptionally complex circumstances in order to promote safe and respectful 10 family-centered care, during periods of crisis including the current COVID-19 pandemic.
CONFLICTS OF INTEREST
The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none was reported.
There was no source of funding for this research.
PROVENANCE AND PEER REVIEW
Not commissioned; externally peer reviewed.
Your baby after the birth
Having skin-to-skin contact with your baby straight after the birth can help keep her or him warm and can help with getting breastfeeding started.
First feed, weight gain and nappies
Some babies feed immediately after birth and others take a little longer.
The midwives will help you whether you choose to:
- feed with formula
- combine breast and bottle feeds
It's normal for babies to lose some weight in the first few days after birth. Putting on weight steadily after this is a sign your baby is healthy and feeding well.
Read more about your baby's weight , and your baby's nappies, including healthy poo .
Tests and checks for your baby
A children's doctor (paediatrician), midwife or newborn (neonatal) nurse will check your baby is well and will offer him or her a newborn physical examination within 72 hours of birth.
In the early days, the midwife will check your baby for signs of:
- infection of the umbilical cord or eyes
- thrush in the mouth
On day 5 to 8 after the birth, you'll be offered the blood spot (heel prick) test for your baby.
Before you baby is 5 weeks old you should be offered a newborn hearing screening test .
If your baby is in special care , these tests may be done there. If your baby is at home, the tests may be done at your home by the community midwife team.
Learn how to tell when a baby is seriously ill .
Safe sleeping for your baby
Make sure you know how to put your baby to sleep safely to reduce the risk of sudden infant death syndrome (SIDS) .
2 weeks and beyond
You don't need to bathe your baby every day. You may prefer to wash their face, neck, hands and bottom carefully instead.
Most babies will regain their birthweight in the first 2 weeks. Around this time their care will move from a midwife to a health visitor.
The health visitor will check your baby's growth and development at regular appointments and record this in your baby's personal child health record (PCHR) , also known as their "red book".
You after the birth
The maternity staff caring for you will check you're recovering well after the birth.
They will take your temperature, pulse and blood pressure.
They'll also feel your tummy (abdomen) to make sure your womb is shrinking back to its normal size.
Some women feel tummy pain when their womb shrinks, especially when they're breastfeeding. This is normal.
Seeing a midwife or health visitor
Midwives will agree a plan with you for visits at home or at a children's centre until your baby is around 10 days old. This is to check that you and your baby are well and support you in these first few days.
Bleeding after the birth (postnatal bleeding)
You'll have bleeding (lochia) from your vagina for a few weeks after you give birth.
The bleeding usually stops by the time your baby is 12 weeks old.
Non-urgent advice: Speak to your GP, midwife or health visitor if you've got postnatal bleeding and any of these:
- a high temperature over 38C
- the bleeding smells unusual for you
- tummy pain that gets worse
- the bleeding gets heavier or doesn't get any less
- lumps (clots) in the blood
- pain between the vagina and anus (perineum) that gets worse
It could be a sign of infection.
Make sure you know the signs of a serious heavy bleed after giving birth (postpartum haemorrhage, or PPH). This is rare and needs emergency care.
Immediate action required: Call 999 if you've got postnatal bleeding and:
- the bleeding suddenly gets heavier
- you feel faint, dizzy or have a pounding heart
This could mean you're having a very heavy bleed (postpartum haemorrhage) and need emergency treatment.
Read more about your body after the birth , including when you might need urgent medical attention.
Feeding your baby
When you're breastfeeding in the early days , breastfeed your baby as often as they want. This may be every 2 hours.
Let your baby decide when they've had enough (this is called baby-led feeding).
You can express your breast milk if you're having problems with breastfeeding . Problems can include breast engorgement or mastitis .
Get breastfeeding and bottle feeding advice .
Your baby's crying
Crying is your baby's way of telling you they need comfort and care. It can be hard to know what they need, especially in the early days.
There are ways you can soothe your crying baby .
How you feel
Find out how to cope if you feel stressed after having a baby . There are support services for new parents that may help.
You may feel a bit down, tearful or anxious in the first week after giving birth. This is normal.
If these feelings start later or last for more than 2 weeks after giving birth, it could be a sign of postnatal depression .
Postnatal depression and anxiety are common, and there is treatment. Speak to your midwife, GP or health visitor as soon as possible if you think you might be depressed or anxious.
Sex and contraception
You can have sex as soon as you feel ready after having a baby.
There are no rules about when to have sex after giving birth. Every woman's physical and emotional changes are different.
You can get pregnant from 3 weeks (21 days) after giving birth. This can happen before you have a period, even if you're breastfeeding.
You need to start using contraception from 21 days after the birth every time you have sex if you don't want to get pregnant again.
Talk to your doctor, midwife or contraception (family planning) nurse about contraception after having a baby . They can arrange contraception before you have sex for the first time.
Being active may feel like a challenge when you're tired, but gentle exercise after childbirth can help your body recover and may help you feel more energetic.
You should also do pelvic floor exercises to strengthen the muscles around your bladder, vagina and anus.
Page last reviewed: 8 July 2022 Next review due: 8 July 2025

My NHS care after birth
After you have your baby, your midwifery team will want to make sure you are recovering from the birth, and that your baby is healthy and feeding well.
When thinking about postnatal care, bear in mind that day one is the day after your baby’s date of birth, day two is the day after that and so on.
Postnatal appointments
You will have at least three appointments with a midwife after the birth. Ideally this will be with your named midwife or a familiar member of the team. This is not always possible, because it is important for you to be seen at certain specific points and your midwife may not be working that day. Your named midwife will make sure to see you where it is possible.
A basic postnatal check will be carried out for both you and your baby each time you see a midwife from the birth until you are discharged from maternity care. Most women will be discharged after a week and a half to two weeks. Some women and babies will be supported by midwives a little longer, up to one month after birth.
At each postnatal check, you will be asked questions about yourself and your baby. All the questions are important ways of picking up any problems. Don’t be surprised to be talking about all sorts of body fluids!
First visit after the birth
You will be seen by a midwife face to face at home the day after having your baby, or the first full day that you are home, if you have been cared for in hospital or birth centre for one or more nights. If there are any concerns, a plan will be made to see you or speak to you within the next day or two depending on what is needed.
Click here for the contact numbers to your midwifery team
Extra support if needed in the first days
Additional support with feeding your baby may be provided by a midwife or a maternity support worker. You may be offered a phone call to check in with how things are going. There may be other reasons that additional visits in the first days are recommended. This might be for yourself or your baby.
The hormonal changes women undergo in the first few days are enormous, and it is quite normal to feel low perhaps for several days. This is known as the baby blues . Contact your midwife for extra support if you or your partner are not sure what is normal baby blues and what is a more serious mental health concern.
Day five visit
You will have a visit or appointment on day five. Scheduling for this visit is important to offer you postnatal blood screening for your baby. This newborn blood spot test, also known as the heel prick test, is explained below. Day five is the ideal day for these. Any earlier and the tests are less reliable. If it’s later this provides less time to put the right care in place for babies with certain rare conditions before problems develop.

On the day five visit, your midwife will ask to weigh your baby (without clothes or nappy). You will already have been asked about your baby’s wees and poos. This is how to make sure your baby is feeding effectively. The weight provides another important check.
It is normal for babies to lose weight for two or three days after the birth, before weight gain starts. When babies are first weighed, they have some extra fluid in their system from being in the womb. Just as mothers will pee more often in the days after the birth to get rid of extra fluid, so will babies.
If your baby has lost more than ten percent of the birth weight on day five, a careful feeding plan or further health checks for your baby will be recommended. There may be other signs that feeding is not going well, for example if your baby has a yellow tinge to their skin or eyes known as jaundice.
NHS.uk information about newborn jaundice (yellow colouring)
How to know your baby is getting enough milk
Discharge from maternity service
Between 10 and 28 days after the birth, you will be discharged from the midwifery team. This may be your third postnatal appointment, or your may have had more. At this point, the midwife will check your baby is well and back to birth weight or will be soon. Your midwife will check that you are well and on track with your recovery from the birth.
Your care passes to the Health Visiting Team , who will support your family and your baby up until your baby is 5 years old. Your GP will also play an important role, carrying out a 6–8-week postnatal check for you and your baby, and being on hand for general health concerns.
Your baby’s cord stump will normally have dropped off by now, allowing you to see your baby’s belly button!

Postnatal health checks

Body Changes after Birth
Give feedback on this page.
Please do not leave any personal details on this form. If you require a response, please go to our contact us page .
Accessibility tools
- Increase text size
- Decrease text size
- Reset text size
- Black and white
- Blue contrast
- Beige contrast
- High contrast
- Reset contrast
After your birth (postnatal care)
- Skip to Navigation
- Accessibility
About care after your birth
The postnatal period can be defined as the first 6-8 weeks after birth. Your body will go through some changes but it is important to know when these are not normal.
If everything is well with you and your baby and depending on the type of birth you’ve had, you will normally be discharged home between 6-24 hours after birth to the care of the community midwifery team, who will continue to support you in your own home.
The first community postnatal visit will be done by a midwife in your home who will discuss and agree with you further visits. You will be given information of who to contact in the event you have any questions or if there is an emergency involving you or your baby.
Call your GP, Midwife or Health Visitor if you are experiencing any of the following:
- A high temperature over 38ºC, sore and tender tummy
- the bleeding smells unusual for you
- lumps (clots) in the blood
- pain between the vagina and anus (perineum) that gets worse
- Pain, swelling or redness in the calf muscle of one leg
- Pain in your chest, difficulty breathing
- Headache, changes in your vision, vomiting
Call 999 if you get sudden or very heavy blood loss from your vagina and you start feeling faint, dizzy and have a rapid heartbeat.
If you have any questions which are not answered here, please ask your midwife for further information.
Infant feeding
Breastfeeding is the healthiest way to feed a baby, it is the only food designed to meet all baby’s needs, both nutritionally and emotionally. We encourage women to breastfeed their babies and aim to support you to achieve this.
North Middlesex hospital is committed to promoting breastfeeding has achieved level 3 Unicef Baby Friendly status. Find more information from the Unicef Baby Friendly web pages, and about breastfeeding in general.
Supporting close and loving relationships
Babies need warm and loving relationships with their primary carers to develop their brains and emotions. Babies need to be kept close and thrive when carers respond to their cues for food, love and comfort. This is essential for babies’ health, wellbeing and brain development. It can also help new parents to also cope with the changes in their lifestyles during the postnatal period.
Infant Feeding Team support
Email: [email protected]
Breastfeeding drop-in support groups
Haringey Council Public Health commission The Breastfeeding Network charity to provide free, non-judgemental, evidence-based baby feeding information to all Haringey families. We will support you in your feeding choices.
Please visit our website for more information on the free face-to-face, email, phone and virtual support that we offer: https://www.breastfeedingnetwork.org.uk/project/haringey/
Contact: [email protected]
Wednesday 13:00-15:00
Dugdale Arts Centre Café, 39 London Rd
Enfield, EN2 6DS
Out of hours support
- National Breastfeeding Helpline 0300 100 0212 (9.30am- 9.30pm)
- La Leche Helpline 0345 120 2918 (8am-11pm)
Latching the baby
C – Close Baby should face the breast and be as close as possible to gain a deep latch
H – Head free Supporting the baby around the neck and shoulders rather than by the head will allow them to tilt their head back and open wide to take in your breast tissue
I – In line Have you tried swallowing with your head twisted over your shoulder? You will soon get tired. Babies also need to have their head in line with their bodies to help them swallow.
N – Nose to nipple T he chin should lead and the mouth should be wide open when the baby latches with the nipple pointing up toward the baby’s nose so that when you latch it reaches far back into the baby’s mouth.
S – Sustainably Will you be able to sit in this position for a whole feed? Do you have water nearby? Reference: acronym developed by Dr Lynette Shotton, Northumbria University
How do I know if my baby is latching on properly?
- They take a large mouthful of breast tissue and you can see more of the darker area of your breast (areola) at the top of the baby’s mouth.
- Baby should have rounded cheeks
- the chin should be the first thing to touch the breast and should indent the breast and massage the tissue during the feed
- Baby’s lips (top and bottom) should be turned outward
- you should hear a 2:1 suck and swallow pattern after the initial let down.
While breastfeeding can be uncomfortable, especially for first-time mothers, it shouldn’t be painful. If you experience pinched, sore or bleeding nipples, or your baby still seems hungry after a feed, these could be signs that your baby isn’t attaching well. Seek help from your midwife.
Breastfeed responsively
You cannot over feed a baby who is only having breast milk. Often babies will feed for comfort as well as for nutrition and responsive feeding means breastfeeding whenever your baby shows feeding cues that it wants to be fed. It also means you can offer a breastfeed if your breasts feel full or for your own needs. Feeding regularly will ensure that you have a good milk supply and that the baby feels loved and supported. However, it is not usual for babies to have large gaps between feeds so if your baby is going for a long time (more than 3 hours) without showing feeding cues try to wake them and offer the breast - a baby should feed at minimum eight to ten times in 24 hours, with feeds lasting between 10 and 45 minutes. If your baby comes off the breast, this can mean the breast is nearly empty, so you can offer the other side.
Additional Resources for mothers
- Global Health Media breastfeeding and expressing videos available in multiple languages.
- Unicef breastfeeding and expressing videos and information leaflets
- Association of Breastfeeding Mothers free online breastfeeding preparation course
- NHS start4life
- First Steps Nutrition Trust
How long will you stay in hospital after the birth of your baby?
If your baby is born in the birth centre.
Immediately after your birth, you and your baby will be made comfortable in the Birth Centre.
Soon after that, your baby will be examined by your midwife, who will then leave you to enjoy your first moments together, during which time you can have breastfeeding guidance from the midwives to ensure you are comfortable.
If there are no complications, most women tend to stay for between 6 - 8 hours after the birth before going home. If you have had a more complicated birth you may be moved to a postnatal ward, where you will be with other mothers and babies, and stay with us between 24 and 48 hours.
If your baby is born in the Labour Ward
As soon as your baby is delivered, both you and the baby will be made comfortable in the Delivery Suite.
In hospital the safety of you and your baby is of paramount importance to us. To help us with this, your baby will have two labels and a security tag, (on admission to the Maternity Ward). It is very important for your baby’s security and safety that they are present. Please inform a member of staff if these become loose. Security is extremely important and these must be replaced if they fall off.
If you notice any other security problems or suspicious behaviour from anyone please inform a member of staff.
If you have a straightforward birth you may be able to go home shortly after from the Delivery Suite/Labour Ward .
If you are on the Maternity Ward you will stay with us for a period of about six to 24 hours, depending on your individual need.
If you have an instrumental birth, (ventouse or forceps) it is anticipated that you will stay for approximately 24 hours, although you may choose to go home before this if both you and your baby are well.
If you have an emergency caesarean section, it is anticipated that you would stay in hospital for about 24 to 48 hours - again depending on the condition of you and your baby.
If you have a planned caesarean, there is an enhanced recovery, it is anticipated that you will stay for approximately 24 hrs
There may also be occasions when a mother and/or her baby may require a longer stay in hospital, and this will be explained to you as soon as possible if this applies to you.
This is the advice provided by the National Institute for Health and Care Excellence (NICE) .
While you are in hospital, and also once you go home, help and support is available 24-hours a day from midwives and the wider maternity care team. On the Maternity Ward staff are made up of a team of doctors, midwives, maternity care assistants, nursery nurses and student midwives.
Once home you will be visited by midwives together with student midwives and maternity care assistants. They are all there to assist you and your family adapt and enjoy your new life together and to help you become confident in caring for your new baby.
Mother and baby health checks
Following the birth of your baby, you will both have health checks performed to ensure that you are recovering well from the birth and your baby is adjusting well to being a newborn.
Your temperature, pulse and blood pressure will be checked at least once during your stay and possibly more depending on the type of birth you have had, and how long you are required to stay.
The midwife will talk to you during the postnatal check to ensure you are happy with feeding your baby. Please ask your midwife about anything you may not be sure of.
The midwife will feel your abdomen daily to ensure your uterus (womb) is contracted and is returning back to the normal position. The blood loss you experience following delivery is often described as a very heavy period. During the first 24 hours you may have to use two maternity pads at a time. If you have sudden profuse blood loss, feel faint, dizzy or have palpitations please tell a member of staff immediately. If you pass any blood clots please save these and inform your midwife.
Once you go home you will notice that your blood loss reduces over time and goes a darker colour. If this loss changes and becomes heavy or bright red in colour or develops an offensive smell please inform your midwife, as this could be a sign of an infection.
During the birth you may have needed a cut (episiotomy) or sustained a tear which required stitches. Even if you have not had stitches, pain and discomfort around your birth canal is common, (this is due to the bruising and swelling).
There are things that you can do to help the discomfort. Firstly you must tell your midwife or doctor, so that they can check that everything is alright and you do not have an infection or a haematoma “an abnormal collection of blood outside a blood vessel” (this is rare).
You must try to keep this area as clean and dry as possible; you can do this by changing your maternity pads regularly and after going to the toilet pat your stitches dry with a clean piece of soft tissue paper. Do not use powder or ointments on your stitches.
The midwife will give you regular pain relief; paracetamol is a good form of pain relief in the post natal period. However remember not to take more than eight tablets in 24 hours. Do not worry if you are breastfeeding as this will not affect your baby or your milk supply.
To avoid constipation try to make sure that you drink plenty of water (at least eight glasses) and fruit juice. Also try to eat a normal diet that includes fresh fruit, vegetables, salads, wholegrain bread and cereals and food with plenty of fibre.).
You may find that you have piles (haemorrhoids). These often occur during the second stage of labour; pushing stage of labour. You need to avoid straining when you go to the toilet as they will become worse. Should these occur ask your midwife for advice. The first time you pass urine, you may find this difficult or it stings. This is normal and you should not worry. Drink plenty of fluids, this will make the urine less concentrated and easier to pass.
If you had a caesarean section, your postnatal check is the same. In addition, your wound is checked daily. However, the plastic 'opsite’ dressing is left on to prevent infection and ensure that your wound heals. Also if you had a caesarean section you will be seen the next day by the anaesthetist to discuss your anaesthetic, and check you have no problems.
If your recovery is straight forward you may not see a doctor during your stay in hospital. However, if the midwife has any concerns about you, a doctor will be asked to see you. If you would like to discuss anything with a doctor please tell the midwife who will arrange this for you.
Your discharge home
You and your baby will be discharged home as soon as you are clinically well to do so; this will usually be within 6-48hrs after birth. Please be aware that discharges occur throughout the day and into the evening Monday to Sunday. For your discharge to be completed, the following milestones will need to be met:
- A postnatal check of the mother by the midwife (you may require a review by a doctor)
- Your newborn is examined by our specialist team
- Medication for you or your baby to go home if needed
- Hearing screening will be offered during your stay in the Maternity Ward , or you may be offered an appointment in the community
- Transfer papers for the community midwife
- Transfer papers for the health visitor
- A child health record book (Red Book)
- Information leaflets about your recovery, contraception, emotional support, safe sleep for babies, birth registration and useful contact details of support groups for parents in your community
- List of contact details for hospitals in your area as well as North Mid in case you become unwell
Birth reflections clinic
What we offer.
The birth reflections clinic runs on Thursday mornings and is offered to women who have had complications at or around the time of delivery. We aim to see women 4-6 weeks after birth and provide a robust clinical review, with a discussion and debrief around the events that occurred. We support women to ensure they understand what happened at their delivery and make any appropriate arrangements for ongoing support. We give advice concerning any future pregnancies and care.
We would usually see women with the following complications:
- Severe pre-eclampsia
- Massive bleeding after delivery (>2.5 litres or needing >4 units of blood transfusion)
- Admission into ITU for any reason
- Failed instrumental delivery leading to Caesarean section
- Category 1 Caesarean section (urgent emergency for low fetal heart rate, placental separation or cord prolapse)
- Baby required admission to SCBU for over 24 hours for reduced oxygen levels at birth
- Complicated Caesarean sections
- Prolonged hospital stay of more than 7 days after delivery
- Repeat operation after delivery
- If your consultant feels it is appropriate
If we see you in this clinic we aim to explain events in a way that you understand and answer all of your questions to the best of our ability. If you have any concerns to raise then we can take action as necessary
Meet the team
- Miss V Sivashanmugarajan - Consultant obstetrician
- Janet Pardo - Midwifery matron
How you get referred
Usually you would be given an appointment prior to discharge from the maternity ward.
If you would like to be seen in the birth reflections clinic but don’t have an appointment then please speak to your midwife or GP who will refer you to the clinic.
Covid-19 and postnatal care
If you have not displayed any symptoms for Covid-19, it is likely the Covid-19 test upon admission to our maternity unit will come back as negative. Should this not be the case and your test result is positive, a Midwife will contact you with your result to discuss how you are feeling and ask you to self-isolate for the recommended time frame.
- If you have symptoms or have tested positive for COVID-19, you must self-isolate for at least 7 days.
- If you do not have a high temperature after 7 days, you no longer need to self-isolate and can leave your home on the 8 th day after your symptoms started or from receiving the positive swab result, adhering to the government’s social distancing measure’s.
- If you still have a high temperature after 7 days, keep self-isolating until your temperature returns to normal and you feel better
Will Covid-19 affect my baby?
As this is a new virus, there is limited evidence about caring for women with coronavirus infection when they have just given birth. A small number of babies have been diagnosed with coronavirus shortly after birth, so there is a chance that infection may have occurred in the womb, but it is not certain whether transmission was before or soon after birth. Your maternity team will maintain strict infection control measures at the time of your birth and closely monitor your baby.
Can I still breastfeed if I have tested positive for Covid-19?
Yes. There is no evidence showing that the virus can be carried or passed on in breastmilk. The well-recognised benefits of breastfeeding and the protection it offers to babies outweigh any potential risks of transmission of coronavirus through breastmilk. Provided your baby is well and doesn’t require care in the neonatal unit, you will stay together after you have given birth so skin-to-skin and breastfeeding can be initiated and supported if you choose.
We've put some small files called cookies on your device to make our site work.
We'd also like to use analytics cookies. These send information about how our site is used to services called Google Analytics. We use this information to improve our site. Read more about our cookies, data and privacy.
- Open access
- Published: 18 April 2024
Midwives’ experiences of professional learning when practicing collegial midwifery assistance during the active second stage of labour: data from the oneplus trial
- Helena Tern ORCID: orcid.org/0000-0002-6063-1432 1 ,
- Malin Edqvist ORCID: orcid.org/0000-0002-0968-6534 2 , 3 ,
- Christine Rubertsson ORCID: orcid.org/0000-0001-7416-6335 1 , 4 &
- Maria Ekelin ORCID: orcid.org/0000-0003-3139-6880 1
BMC Pregnancy and Childbirth volume 24 , Article number: 287 ( 2024 ) Cite this article
300 Accesses
1 Altmetric
Metrics details
Learning is a lifelong process and the workplace is an essential arena for professional learning. Workplace learning is particularly relevant for midwives as essential knowledge and skills are gained through clinical work. A clinical practice known as ‘Collegial Midwifery Assistance’ (CMA), which involves two midwives being present during the active second stage of labour, was found to reduce severe perineal trauma by 30% in the Oneplus trial. Research regarding learning associated with CMA, however, is lacking. The aim was to investigate learning experiences of primary and second midwives with varying levels of work experience when practicing CMA, and to further explore possible factors that influence their learning.
The study uses an observational design to analyse data from the Oneplus trial. Descriptive statistics and proportions were calculated with 95% confidence intervals. Stratified univariable and multivariable logistic regression analysis were performed.
A total of 1430 births performed with CMA were included in the study. Less experienced primary midwives reported professional learning to a higher degree (< 2 years, 76%) than the more experienced (> 20 years, 22%). A similar but less pronounced pattern was seen for the second midwives. Duration of the intervention ≥ 15 min improved learning across groups, especially for the least experienced primary midwives. The colleague’s level of experience was found to be of importance for primary midwives with less than five years’ work experience, whereas for second midwives it was also important in their mid to late career. Reciprocal feedback had more impact on learning for the primary midwife than the second midwife.
Conclusions
The study provides evidence that CMA has the potential to contribute with professional learning both for primary and second midwives, for all levels of work experience. We found that factors such as the colleague’s work experience, the duration of CMA and reciprocal feedback influenced learning, but the importance of these factors were different for the primary and second midwife and varied depending on the level of work experience. The findings may have implications for future implementation of CMA and can be used to guide the practice.
Peer Review reports
Introduction
Learning is a continuous, lifelong process, with the workplace seen as an essential arena for professional development [ 1 ]. Workplace learning serves as a pathway to enhance professional skills and acquire knowledge, and formal programs are no longer seen as the only method of learning [ 2 ]. This is particularly relevant in professions like midwifery, which demand not only theoretical knowledge but also practical skills that are acquired through clinical practice [ 3 ]. Learning in health care settings, such as at obstetric units, is characterised by its complexity and is influenced by numerous factors including organisational, structural, and cultural factors [ 4 , 5 ], where power hierarchies, norms and values can sometimes act as barriers to effective learning [ 6 , 7 ]. Furthermore, when learning in clinical settings, the ability to build relationships with colleagues and adapt to sometimes demanding environments is essential [ 8 ]. It has been demonstrated that, when combined with factors such as open communication, openness to change, and a strong organisational leadership, collaborative learning with colleagues is an important element in a supportive learning environment [ 9 ].
Midwives are required to engage in continuing professional development (CPD) [ 10 ] and upgrade their skills in accordance with scientific evidence [ 3 ]. In addition, previous research implies that certain midwifery skills require more practice to master than is typically offered within the educational program [ 11 , 12 ]. The Swedish midwifery program is a post-graduate 18- months university education program at an advanced level. It is offered to registered nurses with a bachelor’s degree, and is divided evenly between theoretical education and clinical placements in various areas and settings [ 13 , 14 ].
Support for early career midwives is crucial for their professional advancement, particularly during the first years of their career [ 15 , 16 ]. Many find the transition into midwifery to be an overwhelming period since the nature of the position demands a rapid acquisition of skills to ensure efficient job performance [ 17 ]. On-the-job experiential learning, where senior midwives provide feedback and identify knowledge gaps, has been shown to enable early career midwives to develop both safety and confidence in their new positions [ 10 ], but this kind of support can be hard to obtain in a busy organisation [ 18 ]. In addition, there are concerns regarding the challenges of both achieving and maintaining competence, as many midwives are required to rotate between different wards, which leads to them attending fewer births [ 11 ]. It has been suggested that collaborating with a colleague during childbirth can increase professional development and learning, and thus be mutually beneficial for both early-career and senior midwives as their learning needs may differ based on their work experience [ 11 , 19 , 20 ].
Swedish standard care involves one primary midwife responsible for handling a normal birth independently [ 3 ] with assistance from a nurse assistant. A second midwife is summoned if complications arise during the birth and an obstetrician is called if additional medical attention is required. Many of the obstetric units in Sweden have a senior midwife in charge who has the overall responsibility of overseeing the organisation and coordinating care, including providing support to colleagues when necessary. Essentially, collegial collaboration and support are typically reserved for critical situations or if required for other reasons.
A clinical practice referred to as ‘Collegial midwifery assistance’ (CMA) has shown a reduction of severe perineal trauma (SPT) by 30% [ 21 ]. CMA involves an additional midwife being present during the last phase of the second stage of labour with the specific aim of reducing SPT [ 21 ]. Taking part in studies that allow midwives to view childbirth from a new perspective has been found to contribute to professional development [ 20 , 22 ]. However, to date there have been no quantitative studies conducted investigating the primary and second midwives’ experiences of learning while practicing CMA during the active second stage of labour. Previous research has demonstrated that learning is a social process that occurs through interaction between individuals, with reflection and feedback playing crucial roles [ 23 ], particularly when learning specific tasks in clinical practice [ 24 ]. In addition, a positive correlation between the duration of time spent and the extent of learning achieved has also been reported [ 25 ].
Therefore, the primary aim of this study was to investigate the learning experiences ofprimary and second midwives practicing collegial midwifery assistance, taking into account their varying levels of work experience. We also aimed to further explore potential factors that may be associated with midwives’ learning.
Study design and setting
This study applied an observational design utilising data from the Oneplus trial. The primary objective was to evaluate the effectiveness of having an additional midwife present during the active second stage of labour, to prevent SPT [ 21 ]. Five Swedish obstetric units with annual births rates ranging from approximately 2,800 to 5,000 were included in the Oneplus trial. A detailed description of the data collection procedure of the Oneplus trial has been provided elsewhere [ 21 , 26 ], and is presented below in brief.
Data collection procedure
Data collection took place between December 10, 2018, and March 21, 2020. The midwives included in this study assisted nulliparous women or those with one previous caesarean section who were planning for their first vaginal birth. These women were randomised to receive either standard care (one midwife) or the intervention (two midwives) when they entered the second stage of labour. The primary midwife decided when to summon the second midwife during the active second stage of labour, who was ready to assist the primary midwife and support the woman when required. No specific guidelines were given for the intervention, other than to follow the unit’s established preventive models for SPT. All midwives had the opportunity to participate as either the primary or second midwife on multiple occasions throughout the study.
After each birth involving CMA, the participating midwives completed two clinical report forms (CRFs): one by the primary midwife (CRF no 1), and one by the second midwife (CRF no 2). The CRFs covered multiple aspects relating to the birth, including preventive methods used, the midwives’ experiences of the intervention, the duration of the intervention, and elements pertaining to learning and feedback. The items in the CRFs were study specific and had been developed by the research group in collaboration with clinically active midwives who had experience of CMA. The items underwent a face validation process involving midwives having different levels of work experience to ensure that they would be correctly understood and to enhance their validity. For the purpose of this study, items relating to learning and feedback were primarily utilised. All births that received the allocated intervention (two midwives) and where the woman gave birth spontaneously, were included in the study according to the ‘per protocol’ analysis approach (Fig. 1 ).
Due to the aim of the study being to investigate the reported learning experiences of both the primary and second midwives when practicing CMA, two outcomes were used. To assess the learning of the primary midwife, the following item from CRF 1 was employed: ‘I learnt something from the second midwife’ . This item was rated on a 4-grade Likert scale and dichotomised to ‘Completely agree’ , ‘ Mostly agree’ and ‘ Partially agree’ as one category and ‘Disagree ’ as another. This dichotomisation was based on the notion that any level of agreement meant that the intervention had contributed to some degree of learning. To assess the learning of the second midwife, the item ‘Have you learnt something from practicing CMA as the second midwife on this particular birth?’ from CRF 2 was used. The response options were yes/no.
Explanatory variables
Work experience of the primary and the second midwife, reciprocal feedback, and the duration of CMA, were used as explanatory variables in the analyses. These variables were chosen based on the premises that the length of a colleague’s professional work experience influences both the primary and second midwife’s learning [ 20 ], that feedback influences learning [ 27 ], and that a positive correlation between the duration of the intervention and learning has been observed in a different context [ 25 ].
Work experience was categorised from the six original variables [ 21 ] into four groups: <2 years, 2–5 years, 6–20 years, and > 20 years . The categorisation was considered clinically appropriate while it also allowed for insights into the experiences of the least and most experienced midwives. Further, it was created with consideration of the original data, aiming to mitigate overfitting concerns by ensuring a balanced distribution of observations across the groups. Based on the median time of the CMA interventions and clinical reasoning, the duration of CMA was dichotomised into < 15 min and ≥ 15 min. The variable ‘Reciprocal feedback’ was created by combining two items from CRF 1: ‘I received feedback from the second midwife about my management of the second stage of labour’ and ‘ I gave feedback to the second midwife regarding how I experienced her support/presence/help in the birthing room. A positive response to both items indicated that there was reciprocal feedback between the midwives. The response options were yes/no.
Statistical analyses
Descriptive statistics included calculations of frequencies, percentages, medians, and inter quartile ranges (IQR). Proportions were used to analyse learning across groups of work experience for both the primary and second midwife in relation to the explanatory variables. The proportions were derived by dividing the count of reported instances of professional learning during births by the total number of births within each respective group. A 95% confidence interval was established using Jeffrey’s method [ 28 ].
In the secondary analysis, separate univariable and multivariable logistic regression models were employed to assess the learning reported by the primary and second midwives. This approach was based on the assumption that learning varies depending on if the midwife acts as the primary or the second midwife. Furthermore, since learning varies depending on work experience, the models were stratified by work experience categorisation as outlined above, and separate logistic regressions were conducted for each of these subgroups to explore interaction effects. Work experience of less than two years was used as the reference group. The crude and adjusted odds ratios were calculated with 95% confidence intervals. All explanatory variables were added simultaneously in the models and were further adjusted for the study site. All statistical analyses were conducted using IBM SPSS Statistics for Windows, Version 28.0 (IBM Corp, Armonk, New York).
Of the 3,776 women who were randomised in the Oneplus trial, 3,059 gave birth spontaneously [ 21 ]. Of those, 1,546 births were randomised to the intervention, and 1,430 received the allocated intervention so were included in the present study (Fig. 1 ). The median duration of CMA was 15 min (Table 1 ). In 47% of the births, the primary midwife reported having learned something new to some extent (Table 2 ). Similarly, the second midwives reported new learning in 38% of the births. In 70% of the births the primary and second midwives engaged in reciprocal feedback.
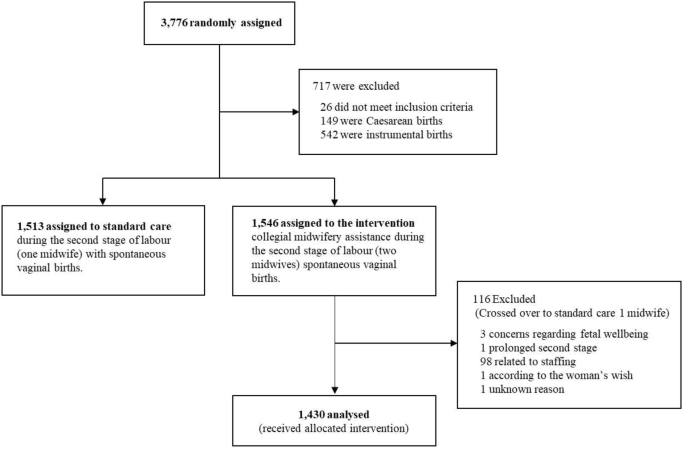
Flowchart of allocation of births to the CMA intervention and exclusions
The length of work experience of the midwives had an impact on reported learning experiences with primary midwives with less work experience reporting new learning more frequently (Table 3 ), ranging from 76% (< 2 years, 95% CI 0.72–0.80) to 22% (> 20 years, 95% CI 0.17–0.27). A similar pattern was seen for the second midwives where those with the least experience reporting learning in 61% of the births (95% CI 0.55–0.67) and those with the most experience reporting learning in 26% of the births (95% CI 0.22–0.30).
The work experience of the colleague influenced the learning for both the primary and second midwives. The figures revealed that learning was reported in around 35% of cases if the colleague had a work experience of less than two years. The highest rates of learning were seen when the colleague had 6–20 years of work experience, with a slightly higher rate among the primary midwives; 53% (95% CI 0.48–0.58) vs. 45% (95% CI 0.39–0.50) (Table 3 ). Both primary and second midwives reported increased learning if reciprocal feedback occurred and if the intervention lasted for 15 min or longer.
When stratified by the work experience of the primary midwife (Fig. 2 ), it was observed that reciprocal feedback was beneficial for learning across all groups of primary midwives, with the exception of those with 2–5 years of experience. A similar pattern was seen when the duration of the intervention was 15 min or longer, particularly among the least experienced midwives (aOR 4.60, 95% CI 2.72–7.78). The colleague’s level of experience was also found to be of importance for learning among the less experienced midwives (0–5 years), however, this was not the case among mid- to late-career midwives.
In comparison, among the mid- to late-career second midwives, a colleague with extensive experience was positively associated with learning (Fig. 3 ). Moreover, the duration of the intervention of 15 min or more was associated with the outcome for the second midwives across all groups, with the exception of those with 6–20 years of work experience. The impact of reciprocal feedback on learning was found to be of less importance when acting as a second midwife, and it was only observed as an influencing factor among those with 6–20 years of work experience (aOR 2.50, 95% CI 1.37–4.59).
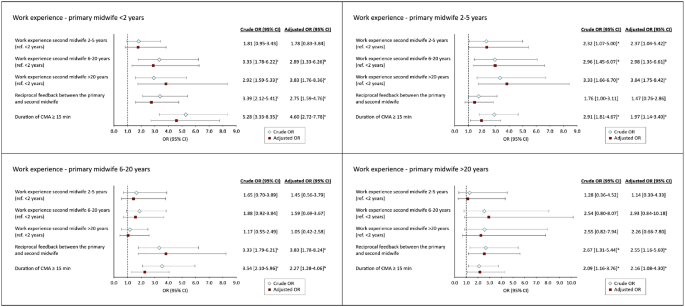
Associations between explanatory variables and the primary midwife’s learning outcomes when practicing CMA, stratified by work experience. Adjusted for study site and explanatory variables. a p < 0.05. b <0.01. c p <0.001
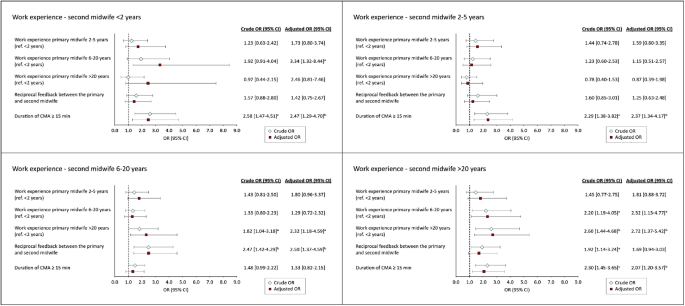
Associations between explanatory variables and the second midwife’s learning outcomes when practicing CMA, stratified by work experience. Adjusted for study site and explanatory variables. a p < 0.05. b <0.01. c p <0.001
The major finding in the current study was that the CMA intervention provided a platform for learning across all groups of work experience, regardless of whether the midwife was in the primary or second midwife role. It was found that if the primary midwife had less than two years of work experience, learning was reported in approximately three out of four births. For the most experienced group (> 20 years of experience), it was reported in just over one in five births. The corresponding results for the most junior second midwives showed that they reported learning in more than three out of five births, whereas the most senior second midwives reported learning in more than one in four births.
Although midwives with less experience reported the highest rates of learning, implying that CMA is particularly beneficial for this group, the study’s findings also confirmed that even the most experienced midwives reported new learning, whether in the role of the primary or second midwife. This is in line with previous qualitative findings, indicating that CMA has the potential to provide lifelong learning opportunities [ 20 ]. This is significant because traditionally the focus on professional development has predominantly been on junior midwives, possibly resulting in lack of support for continuing education among late-career midwives [ 29 ].
In Sweden, where midwives have traditionally worked independently in the birthing room [ 30 ] usually only collaborating with colleagues when the situation demanded it, the introduction of CMA involves a shift in working practices. This change could give senior midwives the opportunity to attend and observe normal uncomplicated births on a daily basis, and not just situations where they are expected to intervene and solve complications.
This study did not investigate what the midwives learnt, but midwives have previously reported knowledge transfer occurring in several areas including manual perineal protection, communication skills, and the interpretation of cardiotocography (CTG) results when practising CMA [ 20 ]. It has been shown that both teaching and acquiring knowledge during the second stage of labour, while concurrently ensuring the wellbeing of the baby, can be demanding [ 31 ]. Therefore, it is interesting that several of the components that make this particular stage complex, such as supporting the birthing woman and protecting the perineum, correspond with what the midwives in the above-mentioned study reported that they learnt when practicing CMA [ 20 ]. Although there is a potential risk of being improperly instructed or misguided when learning from a colleague, this may be less likely to occur given the nature of the intervention, where midwives are exposed to births managed by various colleagues and are also given the opportunity to receive and provide feedback. Moreover, the multifaceted nature of the intervention, where midwives are exposed to births managed by various colleagues, aligns with Albert Bandura’s Social Cognitive Theory [ 32 ] emphasising the role of diverse observational experiences. Bandura contends that individuals are selective in their observational learning, driven by motivational processes. In this context, the exposure to a range of colleagues provides midwives with an extensive repertoire of practices to observe, allowing them to discern and adopt behaviours that align with their professional motivations.
The study found a positive association between the duration of CMA and reported learning, with CMA lasting 15 min or more being positively associated with reported learning, regardless of the midwife’s level of work experience and both for the primary and second midwife. This is in accordance with the ‘ Time on task hypothesis’ , which posits that learning is a function of time, i.e. that the duration of engagement directly influences the learning outcomes in terms of knowledge acquisition and skill development [ 33 ]. While there is evidence to support this, it is inconclusive and available data yield inconsistent findings [ 25 ]. Our models revealed that the duration for CMA had the most prominent impact on the most junior midwives. This could be explained in part by the social aspect of learning [ 24 ], which involves building new relationships and adapting to new environments in the midwives’ transitions [ 8 ]. Further, according to Schön [ 34 ] learning involves reflection in-action , meaning that learning involves being aware of and adapting during the actual performance. For midwives with less experience, this reflection process may require more time. Additionally, when considering the perspective of second midwives, an extended duration allows for the exploration of a more diverse range of impressions, thereby facilitating comprehension of the situation through acquiring more information about the woman giving birth, the birth itself, and the primary midwives’ line of reasoning.
Feedback is a fundamental component of learning, and there is evidence to support its vital part in the learning process [ 23 , 27 ]. However, since feedback can be both positive and negative, it can evoke mixed emotions in individuals [ 35 ]. Some may perceive it as threatening to receive [ 36 ], and it can also be difficult to provide when there is lack of established strategies for delivering feedback [ 37 ]. In addition, it has been shown that the manner in which feedback is delivered plays a significant role in how it is perceived [ 35 , 36 ]. For instance, internal feedback i.e. giving the opportunity for self-assessment prior to receiving external feedback from a colleague can enhance receptiveness [ 36 ]. In addition, personal traits such as an individual’s motivation and desire to receive feedback have been shown to be correlated with how the feedback is perceived [ 35 ]. Although it was found that reciprocal feedback occurred in 70% of the births included in this study, the results indicate that the importance of feedback varied among the primary and second midwives, and across different levels of work experience. These findings underscore the complexity of learning when practicing CMA, where a range of circumstances can influence learning outcomes.
Estimations indicate that in the future there will be a shortage of midwives in Sweden that is likely to last for an extended period of time [ 38 ]. This is primarily due to retirements, which will result in loss of competence [ 38 ]. However, a recent report has indicated that there is in fact an adequate number of midwives in Sweden, but retaining them within the field of intrapartum care is the critical challenge [ 39 ]. This is particularly relevant to early career midwives due to the current challenging work conditions [ 18 ], as beginners are especially vulnerable with their theoretical knowledge but limited clinical experience [ 17 ]. An integrated use of CMA could potentially help ease their transition into professional development. CMA may enable them to both be guided through birth scenarios by colleagues and be exposed to a variety of births, which, in turn, can expedite their skill acquisition and experience, as attaining competence in midwifery is a complex and lengthy process [ 11 , 31 ].
Strengths and limitations
A major strength in this study is that data were collected prospectively as part of a randomised trial [ 26 ] and included data from both the primary and second midwives, enabling a thorough investigation into learning from both perspectives. Furthermore, the stratified analyses conducted in the study rendered a nuanced picture of how midwives experienced learning in each subgroup. However, while informative, the stratified models resulted in smaller subsets of data with less observations in each subgroup, thereby reducing the number of explanatory variables that could be used without risking overfitting the models [ 40 ].
Further limitations include the variability in the outcome variables used for the primary and second midwives, which were originally coded slightly differently and thereby lack consistency. The primary midwife’s outcome was based on a Likert scale that was dichotomised during analysis, whereas the second midwife’s outcome was originally recorded as yes/no alternatives. This inconsistency needs to be considered when comparing and interpreting the results. The study also lacks data regarding how many times each of the midwives participated in CMA. However, it is unlikely that the results were affected by bias due to the large number of births and the fact that all midwives working in each unit were allocated women who were included in the study and participated in both the role of primary and second midwife. Despite this, this lack of information should be considered as a limitation.
The study provides evidence that CMA has the potential to contribute to professional learning both for primary and second midwives, regardless of their levels of work experience. We found that factors such as the colleague’s work experience, the duration of CMA, and the presence of reciprocal feedback influenced learning. However, the importance of these factors varied between primary and second midwives and also depended on their own level of work experience. The findings may have implications for future implementation of CMA and can serve as a guide for the practice.
Data availability
As the data used in this study is not covered by the ethical approval for public sharing, it will not be publicly accessible. However, researchers can upon reasonable requests, get access to anonymised data from the corresponding author.
Abbreviations
Collegial midwifery assistance
- Severe perineal trauma
Clinical report form
Cardiotocography
Goh AYS. Learning journey: conceptualising change over time as a dimension of workplace learning. Int Rev Educ Int Z fur Erziehungswissenschaft Revue Int De Pedagogie. 2022;68(1):81–100.
Google Scholar
Karen C. Defining workplace learning. European Scientific Journal, ESJ 2015; 11(10).
The Swedish Association of Midwives. Description of Required Competences for Registered Midwives. 2019. [Electronic resource]. Retrieved from: https://storage.googleapis.com/barnmorskeforbundet-se/uploads/2019/11/Description-of-Required-Competences-for-Registered-Midwives_The-Swedish-Association-of-Midwives-2019.pdf .
Bleakley A. Broadening conceptions of learning in medical education: the message from teamworking. Med Educ. 2006;40(2):150–7.
Article PubMed Google Scholar
Bleakley A, Bligh J, Browne J. Medical Education for the Future. Identity, Power and Location. 1st ed. 2011. ed: Springer Netherlands; 2011.
Liljedahl M. On learning in the clinical environment [Electronic resource] [dissertation]. Stockholm: Karolinska Institutet; 2016. Retrieved from: http://hdl.handle.net/10616/45259 .
van der Zwet J, Dornan T, Teunissen PW, de Jonge LPJWM, Scherpbier AJJA. Making sense of how physician preceptors interact with medical students: discourses of dialogue, good medical practice, and relationship trajectories. Adv Health Sci Educ. 2014;19(1):85–98.
Article Google Scholar
Teunissen PW, Westerman M. Opportunity or threat: the ambiguity of the consequences of transitions in medical education. Med Educ. 2011;45(1):51–9.
Lancaster S, Di Milia L. Developing a supportive learning environment in a newly formed Organisation. J Workplace Learn. 2015;27(6):442–56.
Embo M, Valcke M. Continuing midwifery education beyond graduation: student midwives’ awareness of continuous professional development. Nurse Educ Pract. 2017;24:118–22.
Article CAS PubMed Google Scholar
Bäck L, Hildingsson I, Sjöqvist C, Karlström A. Developing competence and confidence in midwifery-focus groups with Swedish midwives. Women Birth: J Australian Coll Midwives. 2017;30(1):e32–8.
Bäck L, Sharma B, Karlström A, Tunon K, Hildingsson I. Professional confidence among Swedish final year midwifery students – A cross-sectional study. Sex Reproductive Healthc. 2017;14:69–78.
The Swedish Association of Midwives. Midwifery education. https://www.barnmorskeforbundet.se/barnmorskan/barnmorskeutbildning/ . (accessed July 5, 2023).
Schytt E, Waldenström U. How well does midwifery education prepare for clinical practice? Exploring the views of Swedish students, midwives and obstetricians. Midwifery. 2013;29(2):102–9.
Davis D, Foureur M, Clements V, Brodie P, Herbison P. The self reported confidence of newly graduated midwives before and after their first year of practice in Sydney, Australia. Women Birth. 2012;25(3):e1–10.
Carroll L, Sheehy L, Doherty J, et al. Perineal management: midwives’ confidence and educational needs. Midwifery. 2020;90:102817.
Sheehy DA, Smith MR, Gray PJ, Ao PCH. Understanding workforce experiences in the early career period of Australian midwives: insights into factors which strengthen job satisfaction. Midwifery. 2021;93:102880.
Hansson M, Dencker A, Lundgren I, Carlsson IM, Eriksson M, Hensing G. Job satisfaction in midwives and its association with organisational and psychosocial factors at work: a nation-wide, cross-sectional study. BMC Health Serv Res. 2022;22(1):436.
Article PubMed PubMed Central Google Scholar
Lundborg L, Andersson I-M, Höglund B. Midwives’ responsibility with normal birth in interprofessional teams: a Swedish interview study. Midwifery. 2019;77:95–100.
Tern H, Edqvist M, Ekelin M, Dahlen HG, Rubertsson C. Swedish midwives’ experiences of collegial midwifery assistance during the second stage of labour: a qualitative study. Women Birth: J Australian Coll Midwives. 2023;36(1):72–9.
Edqvist M, Dahlen HG, Häggsgård C et al. The effect of two midwives during the second stage of labour to reduce severe perineal trauma (Oneplus): a multicentre, randomised controlled trial in Sweden. Lancet 2022.
Åhlund S, Zwedberg S, Hildingsson I, Edqvist M, Lindgren H. Midwives experiences of participating in a midwifery research project: a qualitative study. Women Birth. 2018;31(2):e115–21.
Kourgiantakis T, Sewell KM, Bogo M. The importance of feedback in preparing Social Work students for Field Education. Clin Soc Work J. 2019;47(1):124–33.
Dewey J. How we think [Elektronisk Resurs]. Boston: D.C. Heath & Co.; 1910.
Book Google Scholar
Godwin KE, Seltman H, Almeda M et al. The elusive relationship between time on-task and learning: Not simply an issue of measurement. Educational Psychology 2021: No Pagination Specified-No Pagination Specified.
Edqvist M, Dahlen HG, Häggsgård C, et al. One plus one equals two—will that do? A trial protocol for a Swedish multicentre randomised controlled trial to evaluate a clinical practice to reduce severe perineal trauma. Trials. 2020;21(1):945.
Article CAS PubMed PubMed Central Google Scholar
Hattie J, Timperley H. The power of feedback. Rev Educ Res. 2007;77(1):81–112.
IBM Corporation. IBM SPSS Statistics Base 28 Documentation, Armonk NY. IBM; 2022. https://www.ibm.com/docs/en/SSLVMB_28.0.0/pdf/IBM_SPSS_Statistics_Base.pdf . Accessed May 2023.
Price S, Reichert C. The importance of Continuing Professional Development to Career satisfaction and patient care: meeting the needs of novice to Mid- to late-Career nurses throughout their Career Span. Administrative Sci (2076–3387). 2017;7(2):17.
Hansson M, Lundgren I, Hensing G, Carlsson I-M. Veiled midwifery in the baby factory — a grounded theory study. Women Birth. 2019;32(1):80–6.
Ulfsdottir H, Johnson K, Rubertsson C, Ekelin M, Edqvist M. A complex and demanding situation – midwifery preceptors and midwifery students’ experiences of teaching and learning prevention of severe perineal trauma. Women Birth. 2023;36(1):e118–24.
Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ, US: Prentice-Hall, Inc; 1986.
Carroll, JBJTcr. A model of school learning. 1963; 64(8): 1–9.
Schön DA. The reflective practitioner: how professionals think in action. New York: Basic Books; 1983.
Fong CJ, Warner JR, Williams KM, et al. Deconstructing constructive criticism: the nature of academic emotions associated with constructive, positive, and negative feedback. Learn Individual Differences. 2016;49:393–9.
Laudel H, Narciss S. The effects of internal feedback and self-compassion on the perception of negative feedback and post-feedback learning behavior. Stud Educational Evaluation. 2023;77:101237.
Hardavella G, Aamli-Gaagnat A, Saad N, Rousalova I, Sreter KB. How to give and receive feedback effectively. Breathe (Sheffield England). 2017;13(4):327–33.
Trends. and Forecasts 2020: population, education and labour market in Sweden - outlook to year 2035]. Stockholm: Statistiska centralbyrån (SCB); 2021.
Nationella Vårdkompetensrådet. Kompetensförsörjning av barnmorskor i förlossningsvården. 2023. Retrieved from: https://www.nationellavardkompetensradet.se/globalassets/radets/kunskapsunderlag/2023-3-kompetensforsorjning-av-barnmorskor-i/forlossningsvarden.pdf (accessed May 28, 2023).
Babyak MA. What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression-type models. Psychosom Med. 2004;66(3):411–21.
PubMed Google Scholar
Download references
Acknowledgements
We want to thank all midwives who participated in the Oneplus trial for your efforts, commitment, and willingness to share.
Stockholm region pedagogical research grants FoUI-953189. Regional research grants from the south region, Sweden. Region South Funds. Academy of Caring Sciences (Vårdakademin) at Skåne University Hospital. Foundation for Interdisciplinary Scientific Research.
Open access funding provided by Lund University.
Author information
Authors and affiliations.
Department of Health Sciences, Faculty of Medicine, Lund University, P.O. Box 117, Lund, SE-221 00, Sweden
Helena Tern, Christine Rubertsson & Maria Ekelin
Clinical Epidemiology Division, Department of Medicine Solna, Karolinska Institutet, Stockholm, Sweden
Malin Edqvist
Department of Women’s Health, Karolinska University Hospital, Stockholm, Sweden
Department of Obstetrics and Gynecology, Skåne University Hospital, Jan Waldenströms gata 47, Malmö, SE-214 28, Sweden
Christine Rubertsson
You can also search for this author in PubMed Google Scholar
Contributions
Writing - Original draft: HT. Writing - Review & Editing: HT, ME, MEd, CR. Conceptualisation: HT, ME, MEd, CR. Investigation: HT, ME, MEd, CR. Methodology: HT, ME, MEd, CR. Data curation: HT, MEd. Formal analysis: HT, ME, MEd, CR. Supervision: ME, MEd, CR. Project administration: CR. Funding acquisition: HT, CR, Med.
Corresponding author
Correspondence to Helena Tern .
Ethics declarations
Ethical approval.
Ethical approval was received from the regional Ethics Board of Lund University in July 2018 (no. 2018 − 476). Written and oral informed consent were obtained from all respondents including both women giving birth as well as the midwives working at each study site.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Tern, H., Edqvist, M., Rubertsson, C. et al. Midwives’ experiences of professional learning when practicing collegial midwifery assistance during the active second stage of labour: data from the oneplus trial. BMC Pregnancy Childbirth 24 , 287 (2024). https://doi.org/10.1186/s12884-024-06499-8
Download citation
Received : 20 January 2024
Accepted : 10 April 2024
Published : 18 April 2024
DOI : https://doi.org/10.1186/s12884-024-06499-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Skill acquisition
- Labour stage
- Second stage
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- International edition
- Australia edition
- Europe edition

‘I felt myself split into before and after’: how giving birth triggered a life-changing illness
Having a baby led to an unexpected disease and then surgery that altered Lauren Bensted’s body for ever. She talks about the pain she felt in being separated from her newborn, and her journey to learn to accept her new life
“W e’re going to have to disconnect you,” says the man at my bedside. Since I was hospitalised a fortnight ago, this man and his team have been trying to save my colon, a 5ft-long tangle of ulcers and inflammation. The speed and scale of my colon’s fury has fascinated doctors. I imagine them in their morning meetings, poring over my colonoscopy with the mystification usually reserved for the Voynich manuscript. But time is up. Unless they “disconnect” me, my bowel will perforate and I will die.
Disconnection, explains the doctor, involves whipping the whole colon out – here he mimes pulling a rabbit from a hat – and diverting my digestion through a hole in my abdomen called a stoma. He sketches my new anatomy on a piece of paper, quick as a high-street caricaturist. He cannot imagine what it is like to receive this news – to hear your body will change for ever and with it your whole life too – just as I cannot imagine what it is to break it. I want to grab his hand, ask him how. How does a body give birth to a healthy baby and then burst into flames?
I hadn’t planned to be living with my parents when I became a mother, but that’s what happens. My boyfriend, Will, and I have bought a fixer-upper whose every wall, floor and ceiling is, according to my dad, “completely pissed”. The latest in a long line of house-building Irishmen, he sets about restoring its broken bones for us with surgical skill. Meanwhile, Will and I Zipvan our lives back to the London suburb I snubbed aged 21. Now, up the duff at 35, I’m won over by it all – the quiet, the Costa Coffees, the middle-aged blokes reverently soaping their Qashqais. I feel unbelievably lucky to have this time with my mum and dad, this last gulp of being someone’s kid before I become someone’s mum.
I am invited for extra scans, having been classified as “high-risk”. “Because I’m 35 and ‘geriatric’?” I ask one consultant. “No,” she says. “Because of your Crohn’s.” I was diagnosed with the inflammatory bowel disease as a teenager. I don’t remember much, besides a few missed school trips and the dark thrill of no longer being the chubby one in my group of friends. I’ve had no symptoms since. “All looks fine!” beams the sonographer. The baby bobs under the ultrasound wand. It’s the only time my disease history is mentioned.
My son is lifted out of me one Sunday in early July, as Joan Armatrading’s Love and Affection blasts from the delivery-room speakers. Navy-eyed and howling, he is totally alien and powerfully familiar to me all at once . We bring him back to my parents’ house where my brother’s old bedroom is ready for us, shelves of school cricket trophies now stuffed with bottles, muslins, nipple cream. We swaddle the baby the way the midwife showed us – tightly, like a tiny nativity play shepherd – and cannot believe our luck.
I begin to feel porous. Leaking boobs, but other things too: sweat-drenched bedsheets, grinding pain, violent splashes of blood in the toilet. Even the smell of my own breast milk sends me running to the bathroom. I am determined to keep pumping, recording diminishing quantities on my phone: 40ml left boob, 30ml right boob . The baby screams , unsatisfied. I promised I’d go easy on myself if breastfeeding didn’t work out, but now the desire to feed him myself is fierce, irrational, like I need to beat whatever is eating me from the inside out.
When I describe how bad things got before I sought help, people assume I was trying to be invincible. They are thinking, perhaps, of those apocryphal women who lift cars off their young, oblivious to pain. But I’m acutely aware of my pain, I’m just unsure what it means. A suspicion takes hold that I am not tough enough for motherhood. For the sleeplessness, nursing, the magnificent horror of being sliced open.
Unable to get a GP appointment, I pay to see a private doctor, a kind-faced man retired from the NHS. I say I think childbirth has reactivated my Crohn’s. Unlikely, he says. Caesareans famously make the bowels grumpy. He prescribes antibiotics which I immediately throw up. Will drives me to A&E, where the triage doctor calls me “honey”, asks how bad the pain is on a scale of one to ten. Six? Ten? I don’t know the metric. Motherhood has made me an unreliable narrator of my own body. It’s almost a relief when, one morning, delirious with pain, I collapse. At least now there is no ambiguity, I think hazily. As paramedics wheel me out, the baby starts to cry and my mum dashes inside to change his nappy. I do not get to kiss him goodbye.

In TV medical dramas, the patients usually only feature in one episode and then they either get discharged or die. There is a rule that predicts their fate. Demanding patients suffer the most, because they need to be humbled and learn not to be a dick. Sweet, quiet patients – the ones who never press the call bell too often – die first. I hedge my bets and go for “friendly but forthright” in the hope I will make it out alive when the credits roll.
Having never been hospitalised before, there is an initial thrill in observing this ecosystem up close, with its otherworldly machines, bleeps, tourniquets. I am a tourist, just stopping by while the doctors work their magic, then I will step out of this hospital drama, back to my four-week old baby.
I spend the first day on a corridor containing so many patients that staff call it the “Corridor ward”, as if Mr Corridor is a trailblazing scientist. Since there is no space on the gastro ward, I am shipped to an A&E overspill area, where I join the miscellaneously broken. On the bay opposite are two elderly drunks who wind everyone up by singing the same three Beatles songs. Next door is a prisoner with an infected leg who threatens anyone who comes near with legal action. The nurses are kind and visibly stressed. The whole place thrums with the panic of a Panorama documentary, a sensation heightened by the steroids flooding my body.
After a colonoscopy reveals my flaming insides in psychedelic detail, I am diagnosed with severe ulcerative colitis. They will later conclude that my teenage Crohn’s diagnosis was erroneous. The idea is that the gastro doctors will visit me on the A&E ward, but after five days I’ve seen a consultant once. I cannot work out who to badger; it feels like all the people who can help me are elsewhere. A junior doctor mutters that the gastro ward should be renamed the Glasto ward: “That’s how impossible it is to get a ticket.” If only I could chuck on a bucket hat, scale the perimeter wall.
My confidence that I will make a Lazarine recovery falters, chipped away by the tedium of 30 toilet trips a day. I must chronicle them on a daily worksheet, a humiliation compounded by the Comic Sans font. Nevertheless, it sparks a nerdy satisfaction. I add an elaborate asterisk system to denote cramps, spasms, blood. I take it very seriously until the day I hand it in and watch the ward sister shove it straight in the bin.
We decide it’s not safe to bring the baby inside the hospital, as he hasn’t had his jabs yet. So, on the days I can get up, Will brings him to the car park or the garden. My arms are so weak that I’m scared to hold him. Will shows me new winding techniques his mum’s taught him, videos of his dad bathing the baby in the kitchen sink. Some days we laugh a lot. On others, our conversation is a careful dance, each trying to conceal the fullness of our sadness from the other.
Will and the baby are living out of a suitcase between our parents’ homes. I wait for the nightfeeds – midnight, 3am, 6am – when Will sends sleepy voice memos, the baby guzzling in the background. We should be doing this together, sharing the exhaustion and the dirty nappies, the magic chaos of it all. None of us are in the right place. “Has he smiled yet?” I ask. “If I miss his first smile, don’t not tell me.” The baby is changing fast, learning about the world somewhere I am not. This is the unbearable ache, the stone I cannot swallow.
I feel myself crossing over into what Susan Sontag called “the nightside of life”. I’m unable to recognise my own moonface, eyes hollow with insomnia. The kingdom of the sick is where I belong now and it’s no picnic for a people-pleaser. “I’m keeping my pecker up” becomes my party line, like a politician on a media round. But I can see the black puddle of despair in the corner of my room. I am scared to go near in case the questions come (Why me?) and I fall in.
I begin to absent myself from my body. The phlebotomist’s catchphrase comes twice a day – “Sharp scratch” – but I feel nothing when the needle goes in. In the middle of the night, I read about the plan to put people on planes to Rwanda, a newsreader’s sex scandal – things that would normally stir me. But they feel like missives from a universe I don’t exist in any more, so what’s the point? Sickness confirms my impotence to do anything about anything. The world is on fire and so is my body and nothing can be done.
After a weekend passes with no consultant visit, I find the private doctor’s email on his personal website. I say I’ve been diagnosed with severe ulcerative colitis and I’m getting worse. I feel a bit ridiculous, like one of those people who tweet Michael O’Leary for a refund on their Ryanair flight. What can he do, this man? He can’t invent beds on the gastro ward, nor time-travel me through to Monday morning when the consultants will be back. He is literally, according to his out-of-office autoreply, on a walking holiday in Norfolk.
He calls immediately. Apparently I am at risk of developing a very straight-to-DVD-sounding condition called “toxic megacolon” where the whole thing bursts. I need to be on immunosuppressant therapy immediately, he says. And something else: “85% of patients in your position end up needing a colectomy.” What is that? I ask. “The bowel is removed and the patient fitted with a stoma,” he says. “The last resort.”
Like you perhaps, what comes to mind is a bag of waste stuck to a stomach. That’s the visual, that’s the extent of my prior knowledge. I know it must cover something – the “stoma” presumably – but I have no interest in that. Because it will not, cannot be me.
The private gastro pulls the emergency lever all the way from the Norfolk Broads. He used to work here in his NHS days, it turns out. Consultants are paged, the immunosuppressant arrives. But it can only be administered by a specific nurse whose shift ends within the hour. A side-room frees up on the gastro ward, but due to staff shortage it has not been cleaned, so I cannot be transferred. My dad – straight off the scaffold, hair full of plaster dust – runs to find the ward sister. “I will clean that room”, he says, in a low voice that I know means he’s scared. My poor, lovely dad. “Please let me clean it.” Soon I am wheeled to a room on the right ward, hooked up to the new drug. “At last!” we all keep saying, as if that was the worst bit. But over the next fortnight, I will discover there is no limit to how terrifying things can get.
There’s the moment I realise no one has accessed my test results for days because the junior doctors are striking and the consultants don’t know how to log on. The evening an unsympathetic registrar tries to throw me out of my room, claiming a palliative patient has greater need. (I later discover this is a fiction: one of the alcoholic Beatles fans is proving too disruptive.) The moment a trainee stoma nurse tries to draw an X on my stomach where a stoma would go, despite no doctor having made the final call on surgery yet, despite me crying “No, please, I’m not ready.”
There’s the nurse who forgets to warn me she’s about to pull a thick tube from inside my belly (agony!) because she is so stressed, trying to teach junior nurses. The day I’m so desperate to see a psychiatrist about my hallucinations that I try to bribe a millennial female doctor with a Facetime from my bestselling author mate to make it happen. (I’d been asking for a week.) The rage when I discover on a late-night Google trawl that “one in three women with inflammatory bowel disease will flare after giving birth” and “women with IBD should be closely monitored postpartum.” How did I not know? Why did no one tell me?
But there are no villains in this story, I know that now. Just people under huge pressure, in an overstretched, underfunded system that doesn’t work any more, doing their best. And there’s no magic medicine, I know that too. Just good luck and bad luck as to whether the drugs will work, save your colon, save your life, save you from the surgery you think will ruin everything. It’s all luck in the end. And my good luck begins the night three brilliant surgeons walk into my room and promise me a stoma is going to give me my life back and I decide to believe them.
I really have no other choice.
I wake up from the eight-hour operation in what appears to be a large industrial storage unit. No free beds on the recovery ward. Something strange surges in me. I feel stuffed full of love for the earth and all of its creatures. I am the Dalai Lama. I am John and Yoko’s bed!
“Is this the fentanyl?” I ask my surgeon, wondering if he’ll let me hold his hand. “Maybe,” he says. “Or you might just be happy to be alive.” I have questions. Who owns my colon now? “Nobody. It’s biological waste.” Where is my colon, exactly? “A lab in Winnersh Triangle.” This sends me into hysterics. I’ve finally cracked, I think.
I don’t want to ruin the lovely opioid high by looking under the sheets, but the nurse says I can’t be discharged until I prove I can deal with the stoma. So I take a deep breath, pull up my gown.
Most people are too polite to ask what a stoma looks like. Their imagination cuts out at the bag, the way mine used to. But the bag is just the figleaf: the madness is what it conceals. The common assumption is a little tube, discreetly passing waste from body to bag, like a tiny hoover. This is cute, but wrong.
Here’s what I can see. A red spout, 3cm across, protruding between my navel and hip. The end of my small intestine, I realise numbly. Covered with a clear bag for monitoring, it flexes and scrunches like a sea urchin. It feels appalling and amazing to see what I can see, this most private and shameful process brought into daylight. It seems improbable that it should actually work – the bag seems so DIY – but I eat a jacket potato and feel the thing murmur into action.
There’s so much paraphernalia to get my head around: bags, seals, sprays, powders. It’s like I’ve taken up a hobby with a dizzying amount of kit, like vaping or golf. “Some people give their stoma a name,” says the nurse, “to help them accept it.” No chance, I think . It’s not a Tamagotchi, it’s my intestine for god’s sake.
I imagine stepping back into my old life now. Teaching, writing, pubs, gigs, sex, holidays. How could I forget for long enough to enjoy anything? It hits me that no one I know would want to have this body – a very particular kind of loneliness.
The doctors love a metaphor. They refer to my plumbing. Pipework. Shuddering, loveless imagery that recalls our fixer-upper, with its wretched old drains. But their favourite metaphor is “disconnected” . I see it in a letter to my GP: “The patient was disconnected on 18 August.” It’s a good metaphor, maybe too good. It’s not only my bowel that has been disconnected, but me too. From everyone I love. From my old innocence, whoever I used to be.
After Will calls to say he is on his way to visit, I try to rejig my bedsheets. A healthcare assistant called Hassan comes by and I’m suddenly in tears. I don’t want Will to be scared by the drains ferrying awful liquids from my body, I explain. Hassan leaves and returns with a pot of raspberry jelly. “You are feeling shame for what happened to you,” he says gently. “But it’s not your fault.”
No doctor has been able to tell me why having a baby made my body burst into flames. I am all arson with no perpetrator. In the absence of a culprit, I have cast myself. What if I had known more about inflammatory bowel disease? What if I had eaten differently, given birth differently, got myself to hospital quicker? Could things have fallen out some other way?
Hassan’s words reach out to me in the dark. I do some more crying, eat the jelly he has brought me.
It is late summer by the time they discharge me. It feels like a jailbreak. Will and I roll down the car windows, sing along to Rusted Root’s Send Me on My Way. My parents are waiting on the doorstep with the baby – eight weeks old now, plump as a peach. I’ve been away half his lifetime.
The doctors warned my mood would crash when the drugs wore off. I wait for the black puddle to turn tidal. Instead, I find illness has shifted the world by a few centimetres. Jokes are funnier, conversations more sincere. Everyday things feel like unbelievable acts of magic. Cooking dinner with my mum. Making up a song for the baby. Life hums with a kind of Technicolor, like falling in love. My opioid high has mellowed into something as warm and steady as the September sunshine. The surgeon was right: I am just so happy to be alive.
I had planned to tell only those closest to me about my stoma. But at some point I realise that discretion’s closest relative is shame and cannot stop talking. I pick up a sandwich from the Jewish deli and am there half an hour, telling the bewildered owner about my exploding colon. I develop a pathological intolerance for pleasantries. Will starts calling me the Truthbomber on account of my tendency to blow up pointless small talk. Friends visit and I gibber away, pulling stories from my ragbag of hospital traumas, prone on the sofa like Elizabeth Barrett Browning on speed. I write long emails about what happened to family, friends, colleagues, finding release in the way I can control its contours now, find something meaningful in the darkness.
In the quiet of the bathroom, I shower and dodge the mirror’s gaze. The baby trills happily in his bouncer, unaware I bring him along for moral support every morning as I tend to my stoma, change the bag. He’ll never know me any other way than this. I need to face my new punctured body, still stained with orange surgical dye. Unwire all of my shame, old and new. I want to learn to look at myself the way the baby does – with uncomplicated, uncritical love.
I try to think of my body as a collection of stories. The freckles inherited from my mum. The scar from a pair of GHD straighteners on my neck, ultimate badge of early noughties girlhood. The queen of hearts tattoo on my wrist my best mate and I got two summers ago. The curve of a belly that kept the baby safe, the five-inch cut where he was prised from me. The laparoscopic holes, incredible portals through which surgeons cut five feet of disease. I think of my body as an old friend I have lived in for 35 years. And though I no longer trust it, I cannot hate it.
When winter comes, we move into our house and throw a party. We lug beer back from the Wembley Tesco Extra, pick up a firepit in B&Q. At some point, I realise I want to make a speech about Will. About the way he’s held me fast, his love unflinching. “We’ve been together six years,” I tell everyone. “But you know how the old adage goes. You never really know a man till your colon explodes.” Our friend Adam gamely conducts a shamanic ritual over the firepit in the garden, wearing a pagan hood off Amazon. We huddle in the cold, pass round Biros, scribble down the worst things that have happened to us, cast them into the flames. A friend brings a piñata emblazoned with “Fuck 2023” which I take great pleasure in thwumping. Surrounded by everyone I love, I feel the threads between my old and new selves begin to reconnect.
The first year of a baby’s life is peppered with milestone moments, not all of them showstoppers. Many happen without ceremony, as you stoop to unload the dishwasher, fish a stone from your shoe. Sometimes there is no “first” time at all, just a seamless switch from nothing to something. The baby’s first smile comes a few days after I get out of hospital. Just the corners of his mouth, then an unmistakable full beam. I had been so convinced I’d miss it. “He saved it till you got home,” says my nan.
I’ve become aware of all my firsts too, since illness split me into a before and after. First time in a swimming pool. First Christmas. It’s been a long time since I got to do things for the first time. I watch the baby’s face flood with shock and delight as he collides with the world. First ride on a double decker. First taste of pineapple. One day, I’ll tell him how he saved me. How, in the moments that I replay the darkness, his little face pulls me back to the present. I’ll tell him how much he taught me in our first year together. Eyes wide open, looking at the big bright world, both of us brand new.
- The Observer
- Health & wellbeing
- Parents and parenting
Most viewed

Peter Andre announces return to work after birth of baby daughter
The mysterious girl singer shares three children with his wife emily.

Peter Andre is currently on cloud nine following the birth of his baby daughter who came into the world on 2 April.
While the doting dad, who also shares Theo, seven, and Amelia, ten, with his wife Emily, has kept much of his family life under wraps ever since, Peter did share an update at the weekend revealing when he's set to return to work.

In a video shared to Instagram, the Mysterious Girl hitmaker told his followers: "Hi everyone, for all you food and music lovers, please listen up because I'm about to join the UK's biggest food and music festival. It's called Foodies Festival, [it's] in Edinburgh, Cardiff and Tunbridge Wells."
He continued: "The first one's in Cardiff in a couple of weeks, 12 May, so come down, I'm going to be cooking live with TV chefs, and of course doing some music. I can't wait."
.rsme-embed .rsme-d-none { display: none; } .rsme-embed .twitter-tweet { margin: 0 !important; } .rsme-embed blockquote { margin: 0 !important; padding: 0 !important; } .rsme-embed.rsme-facebook-embed .fb-post iframe { width: 100% !important; } .rsme-embed.rsme-facebook-embed .fb-post span { width: 100% !important; } .rsme-spinner { border: 3px solid rgba(0,0,0,0.75); border-right-color: transparent; border-radius: 50%; animation: rsme-spin 1s linear infinite; } @keyframes rsme-spin { 0% { transform: rotate(0deg); } 100% { transform: rotate(360deg); } } View post on Instagram
Peter's update comes amid the singer's struggle to settle on a baby name with his wife Emily. The TV star made the revelation in a social media post, telling fans that the couple are still deciding on a name for their "bubba".
You may also like
While the pair, who tied the knot in 2015, haven't yet selected a moniker, Peter has divulged that there are a plethora of names up in the running. In response to one fan who suggested the name Olivia, Peter replied: "Olivia was my number one choice but Ems not sure."
After another follower offered Athena, the dad-of-five said: "Athena is also in the running. Not sure how Ems feels about it but I LOVE it."

Meanwhile, when a third fan mentioned the moniker Charlotte, Peter revealed: "Charlotte is also in the running. I like Charlie [heart emoji]". Elsewhere, the former I'm a Celebrity contestant agreed that Sydney was "beautiful", while the name Summer was "nice".
Lovebirds Peter and Emily welcomed their bundle of joy into the world earlier this month. The pair announced their happy news over on Instagram with the sweetest photo of NHS doctor Emily cradling the newborn.
"Just minutes old… We feel so overwhelmed right now," the duo penned. "So happy to welcome our beautiful girl to the family.
"Mum and daughter are doing amazing. Born Tuesday 2nd April 2024, 7lb 3oz and thankfully very healthy.
"Baby has been spoilt with cuddles from Junior, Princess, Amelia and Theo who are all in love with their new little sister. As parents, we couldn't be happier."
Shedding a light on the couple's struggles to find the perfect name, they added: "Only thing is… She has no name yet. Help! Thanks to all the doctors, midwives and staff at Musgrove Park Hospital Taunton. You were incredible.
"And Emily's parents, whom I adore. You have both been incredible. I'm so happy. Just off to hold her. Thanks everyone for reading."
Aside from Amelia, Theo and his newborn daughter, Peter is also a doting dad to Junior, 18, and Princess, 16, whom he shares with his ex-wife Katie Price.
- Celebrity Families
- Peter Andre
- Emily Macdonagh
More Celebrity News

Peter and Emily Andre's baby name announcements amid important decision for third child

Peter Andre sparks sweet reaction after sharing candid hospital photo with wife Emily

Peter Andre reveals baby names for newborn daughter that are top of his list - but not wife Emily's

Peter Andre reveals adorable nickname for baby daughter amid name struggle

Emily Andre shows off ultra-rare glimpse of glamorous bedroom she shares with Peter Andre

Emily Andre shares emotional video of son Theo cradling bare baby bump

Pregnant Emily Andre shares rare family video featuring son Theo ahead of due date

Emily Andre reveals husband Peter is 'more sympathetic' during third pregnancy
Emily andre reveals she is pregnant with third baby in sweet photo with husband peter, emily andre opens up about being stepmother to princess and junior andre during touching conversation, peter andre reveals future plans with wife emily as they prepare to welcome third child, peter andre praises 'brilliant' wife emily in new pregnancy update.

IMAGES
COMMENTS
Second Trimester. Third Trimester. Health & Wellness. Morning Sickness. ... Postpartum checkups are the visits to your OB or midwife that you'll have after giving birth—and they're just as important as your prenatal visits, as the first few weeks after delivery are a time of major transition for both you and baby.
Around five days to eight days after your baby's birth, your midwife will carry out a heel-prick test. This is where a tiny amount of blood is taken from your baby's heel to be tested for certain deficiencies and congenital conditions. If you had a caesarean section, you may need your stitches removed.
Your postpartum checkup. Your six-week postpartum checkup is a comprehensive visit with your OB or midwife to check on your recovery after childbirth. You'll have a complete examination, including a mental health screening and any tests or immunizations you need. If all is well, you'll get the okay to start exercising and having sex again.
Vaginal discharge. After delivery, a mix of blood, mucus and tissue from the uterus comes out of the vagina. This is called discharge. The discharge changes color and lessens over 4 to 6 weeks after a baby is born. It starts bright red, then turns darker red. After that, it usually turns yellow or white.
In high‐mortality settings and where access to facility‐based care is limited, at least two home visits are recommended for all home births: the first visit should occur within 24 hours of the birth, the second visit on day three, and if possible, a third visit should be made before the end of the first week of life (day seven).
After your booking appointment at about 10 weeks, you will usually have these appointments: in your second trimester, in weeks 14-16, 25 and 28. in your third trimester in weeks 31, 34, 36, 38, 40 and 41 (if you haven't given birth before 40 weeks) If you have already had a healthy pregnancy and baby, you will have 7 appointments. As well as ...
The days and weeks following childbirth—the postnatal period—are a critical phase in the lives of mothers and newborn babies. Most maternal and infant deaths occur in the first month after birth: almost half of postnatal maternal deaths occur within the first 24 hours,1 and 66% occur during the first week.2 In 2013, 2.8 million newborns ...
The postpartum recovery timeline. The term "postpartum recovery" is often used to describe the first six to 12 weeks after you give birth, but your physical and mental recovery from pregnancy and birth may take much longer. So much has changed; family dynamics, your sense of self, your body shape and much more so this all plays into your recovery.
The postpartum period, the time after giving birth, is a crucial time for recovery and the long-term health of the parent and baby. It's also a time of intense physical and emotional changes. It is normal and expected to experience several physical symptoms like swelling, cramping, breast tenderness, constipation, and leaking milk.
What is a postpartum checkup? A postpartum checkup is a post-birth appointment with your doctor or midwife to check how you're doing physically, mentally and emotionally after having a baby. [1] Your practitioner will examine you to make sure you're recovering as expected physically and also ask you questions about how you're handling your life ...
7 First midwife visit after transfer of care from the place of birth or after a 8 home birth 9 1.1.3 Arrange the first postnatal visit by a midwife to take place between 12 and 10 36 hours after transfer of care from the place of birth or after a home birth. 11 The visit should usually be at the woman's home, depending on her
1.1.14 Ensure that the first postnatal visit by a midwife takes place within 36 hours after transfer of care from the place of birth or after a home birth. The visit should be face-to-face and usually at the woman's home, depending on her circumstances and preferences.
Once you've told your doctor or midwife that you're pregnant, they'll offer you a first appointment. This is called a booking appointment. It should ideally happen before you reach 10 weeks, although most women have theirs at some time between eight weeks and 12 weeks. Your midwife will use this time to advise you about your diet and lifestyle ...
1 Length of postpartum stay and first midwife visit after transfer of care. 1 Length of postpartum stay and first midwife visit after transfer of care. 2 Timing of first health visitor visit. 2 Timing of first health visitor visit. 3 Clinical tools to assess women's health. 3 Clinical tools to assess women's health. 4 Perineal pain. 4 Perineal pain
You'll have a number of antenatal appointments during your pregnancy, and you'll see a midwife or sometimes an obstetrician (doctor specialising in pregnancy). They'll check the health of you and your baby, give you useful information and answer any questions. Pregnant employees have the right to paid time off for antenatal care.
Your antenatal care. In Scotland, the NHS provides pregnancy, labour and postnatal (after birth) care. During your pregnancy, you'll have regular antenatal (pre-birth) appointments with your midwife or obstetrician. Some of your appointments will be face to face at a midwife hub, hospital or at home. Other appointments may be video calls ...
baby, with 24 dry hours of you the to. baby's eyelids separately. a damp him before and cloth wrap bathing (not its a full body the bath) baby. with a clean cloth dipped in cooled, boiled water. and until head the in acord stump. Keep sick people away from the baby. clean dry cloth falls right off. away.
During the COVID-19 pandemic postnatal midwifery-led care remains a key public health intervention for women and their families 1, 2. Home or virtual visits by community midwives should be provided to reduce the number of times women and newborns need to leave their home 1. In order to comply with social distancing requirements, community ...
A children's doctor (paediatrician), midwife or newborn (neonatal) nurse will check your baby is well and will offer him or her a newborn physical examination within 72 hours of birth. In the early days, the midwife will check your baby for signs of: jaundice. infection of the umbilical cord or eyes. thrush in the mouth.
Once your baby is born, you'll likely find that friends and family want to visit the new addition to your family. As lovely as this is, it's common to feel overwhelmed as you navigate caring for and bonding with your newborn and managing visitors. Here, our midwife Lauren highlights how you can delicately establish some boundaries.
Between 10 and 28 days after the birth, you will be discharged from the midwifery team. This may be your third postnatal appointment, or your may have had more. At this point, the midwife will check your baby is well and back to birth weight or will be soon. Your midwife will check that you are well and on track with your recovery from the birth.
Immediately after your birth, you and your baby will be made comfortable in the Birth Centre. Soon after that, your baby will be examined by your midwife, who will then leave you to enjoy your first moments together, during which time you can have breastfeeding guidance from the midwives to ensure you are comfortable. If there are no ...
The MHITH - Postnatal Program allows you to continue your hospital care in your own home with your family. You will be supported by one of our midwives, who will visit your home the day after you leave the hospital. Midwives who provide care to you at home are the same midwives who care for patients in the hospital.
After each birth involving CMA, the participating midwives completed two clinical report forms (CRFs): one by the primary midwife (CRF no 1), and one by the second midwife (CRF no 2). The CRFs covered multiple aspects relating to the birth, including preventive methods used, the midwives' experiences of the intervention, the duration of the ...
I hadn't planned to be living with my parents when I became a mother, but that's what happens. My boyfriend, Will, and I have bought a fixer-upper whose every wall, floor and ceiling is ...
Peter Andre is currently on cloud nine following the birth of his baby daughter who came into the world on 2 April. While the doting dad, who also shares Theo, seven, and Amelia, ten, with his ...