AARP's Brain Health Resource Center offers tips, tools and explainers on brain health.
AARP daily Crossword Puzzle
Hotels with AARP discounts
Life Insurance
AARP Dental Insurance Plans
AARP MEMBERSHIP — $12 FOR YOUR FIRST YEAR WHEN YOU SIGN UP FOR AUTOMATIC RENEWAL
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
- right_container
Work & Jobs
Social Security
AARP en Español
- Membership & Benefits
- AARP Rewards
- AARP Rewards %{points}%
Conditions & Treatments
Drugs & Supplements
Health Care & Coverage
Health Benefits

Staying Fit
Your Personalized Guide to Fitness

AARP Hearing Center
Ways To Improve Your Hearing

Brain Health Resources
Tools and Explainers on Brain Health

A Retreat For Those Struggling
Scams & Fraud
Personal Finance
Money Benefits

View and Report Scams in Your Area

AARP Foundation Tax-Aide
Free Tax Preparation Assistance

AARP Money Map
Get Your Finances Back on Track

How to Protect What You Collect
Small Business
Age Discrimination

Flexible Work
Freelance Jobs You Can Do From Home

AARP Skills Builder
Online Courses to Boost Your Career

31 Great Ways to Boost Your Career

ON-DEMAND WEBINARS
Tips to Enhance Your Job Search

Get More out of Your Benefits

When to Start Taking Social Security

10 Top Social Security FAQs

Social Security Benefits Calculator

Medicare Made Easy
Original vs. Medicare Advantage

Enrollment Guide
Step-by-Step Tool for First-Timers

Prescription Drugs
9 Biggest Changes Under New Rx Law

Medicare FAQs
Quick Answers to Your Top Questions
Care at Home
Financial & Legal
Life Balance

LONG-TERM CARE
Understanding Basics of LTC Insurance

State Guides
Assistance and Services in Your Area

Prepare to Care Guides
How to Develop a Caregiving Plan

End of Life
How to Cope With Grief, Loss
Recently Played
Word & Trivia
Atari® & Retro
Members Only
Staying Sharp
Mobile Apps
More About Games

Right Again! Trivia

Right Again! Trivia – Sports

Atari® Video Games

Throwback Thursday Crossword
Travel Tips
Vacation Ideas
Destinations
Travel Benefits

Beach vacation ideas
Vacations for Sun and Fun

Plan Ahead for Tourist Taxes

AARP City Guide
Discover Seattle

25 Ways to Save on Your Vacation
Entertainment & Style
Family & Relationships
Personal Tech
Home & Living
Celebrities
Beauty & Style

TV for Grownups
Best Reality TV Shows for Grownups

Robert De Niro Reflects on His Life

Looking Back
50 World Changers Turning 50

Sex & Dating
Spice Up Your Love Life

Navigate All Kinds of Connections

Life & Home
Couple Creates Their Forever Home

Store Medical Records on Your Phone?

Maximize the Life of Your Phone Battery

Virtual Community Center
Join Free Tech Help Events

Create a Hygge Haven

Soups to Comfort Your Soul

Your Ultimate Guide to Mulching
Driver Safety
Maintenance & Safety
Trends & Technology

AARP Smart Guide
How to Keep Your Car Running

We Need To Talk
Assess Your Loved One's Driving Skills

AARP Smart Driver Course

Building Resilience in Difficult Times

Tips for Finding Your Calm

Weight Loss After 50 Challenge

Cautionary Tales of Today's Biggest Scams

7 Top Podcasts for Armchair Travelers

Jean Chatzky: ‘Closing the Savings Gap’

Quick Digest of Today's Top News

AARP Top Tips for Navigating Life

Get Moving With Our Workout Series
You are now leaving AARP.org and going to a website that is not operated by AARP. A different privacy policy and terms of service will apply.
Go to Series Main Page

What is the Welcome to Medicare checkup?
| You can get one free Welcome to Medicare checkup anytime during the first 12 months after you enroll in Medicare Part B , which is the part of Medicare that covers doctor visits and outpatient services. This checkup is not a comprehensive physical exam but is an opportunity for your doctor to assess your health and provide a plan of future care.
The Welcome to Medicare checkup is optional, but it serves as a baseline for monitoring your health during the annual wellness visits that Medicare will pay for in subsequent years. You do not need this checkup to qualify for later annual wellness visits, but Medicare won’t pay for a wellness visit during your first 12 months in Part B.

AARP Membership — $12 for your first year when you sign up for Automatic Renewal
What happens at the Welcome to Medicare checkup?
During the exam you can expect your doctor to do the following:
- Record your vital information, including blood pressure, height and weight.
- Calculate your Body Mass Index (BMI).
- Review your health history — your own and that of your family.
- Determine your ability to function independently and your level of safety, such as how well you perform activities of daily living and your risk of falls.
- Assess your potential for depression.
- Check for risk factors that could indicate future serious illnesses.
- Provide a simple vision test.
- Recommend screenings, shots and other preventive services in writing that you may need to stay healthy. Many of these, such as mammograms and vaccinations, may be free under Medicare.
- Offer to talk about advance directives . A health care proxy lets you designate someone else to make medical decisions on your behalf if you can’t, and a living will specifies your preferences for medical treatment at the end of your life.
How can I prepare for my Welcome to Medicare visit?
To make the most of this appointment, you should gather the following information and records in advance:
- Your family medical history Learn as much as you can about your blood relatives’ health history. Any information you can give your doctor can help determine if you are at risk for inherited diseases.
- Your personal medical records That includes providing immunization records if you’re seeing a new doctor.
- Your prescription medications Along with listing the names of your drugs, include dosage, how often you take each medication and why.
How much will I pay for a Welcome to Medicare checkup?
You’ll have no deductible or copayment for the Welcome to Medicare checkup if you meet the following conditions:
If you’re enrolled in original Medicare, you need to go to a doctor who accepts “assignment,” meaning that the physician accepts the Medicare-approved amount as full compensation.
If you’re enrolled in a Medicare Advantage plan that has a provider network, such as an HMO or PPO , you may need to go to a doctor in the plan’s provider network.
Keep in mind
Even though you won’t have to pay for this checkup, the doctor could order other tests or procedures for which you may have to cover deductibles and copayments out of pocket.
Updated June 22, 2022
Return to Medicare Q&A main page
Discover AARP Members Only Access
Already a Member? Login

AARP NEWSLETTERS

%{ newsLetterPromoText }%
%{ description }%
Privacy Policy
More on health
Understanding Medicare’s Options: Parts A, B, C and D
10 Common Medicare Mistakes to Avoid

Medicare Eligibility: Age, Qualifications, Requirements
ARTICLE CONTINUES AFTER ADVERTISEMENT
AARP Value & Member Benefits

Coupons for Local Restaurants
Find delicious discounts at your favorite nearby restaurants

Alexa Emergency Assist from Amazon
25% off emergency assistance subscription plans

AARP® Staying Sharp®
Activities, recipes, challenges and more with full access to AARP Staying Sharp®

AARP Medicare Resource Center
Helpful resources to manage your current Medicare situation
SAVE MONEY WITH THESE LIMITED-TIME OFFERS
New to Medicare? Schedule your "Welcome to Medicare" visit
Published by Medicare Made Clear®

If you’re new to Medicare, you get a free “Welcome to Medicare” visit. You may be wondering what the “Welcome to Medicare” visit is all about and why it’s worth scheduling.
What is the “Welcome to Medicare” visit?
The "Welcome to Medicare" visit is a one-time-only preventative health care visit covered by Medicare Part B. It is not the same as a routine physical exam or annual Medicare Wellness visit . The Welcome to Medicare visit is an introduction to Medicare and focuses on disease prevention and detection to help beneficiaries live a healthier life.
You have twelve months from the date of your initial enrollment into Medicare Part B to complete the visit 1 .
What do I pay for the “Welcome to Medicare” visit?
You pay nothing for this visit if the doctor or other health care professional you see for it accepts Medicare, and the Part B deductible doesn’t apply.
However, if your doctor performs additional tests or services during this visit that are not covered under the preventative benefits, you may have to pay a coinsurance. In this case, the Part B deductible will also apply.
What your “Welcome to Medicare” visit covers
During your “Welcome to Medicare” visit, you and your doctor will discuss disease education and prevention. Your doctor will also review your medical and health history, such as:
- Past medical/surgical history, such as illness, hospital stays, operations, allergies, and injuries
- Current medications and supplements, including over-the-counter vitamins
- Depression and safety screenings
- Family health history
- History of alcohol, tobacco, and illicit drug use
- Diet and exercise
The visit will also include:
- Measurements for your height, weight, blood pressure and body mass index (BMI)
- A simple vision test
- Review of your risks for depression
- A written plan for screenings, shots and other preventive services you may need
- In some cases, a discussion about creating an advance directive
Remember, if diagnostic tests or other services are performed that are not covered by the "Welcome to Medicare" visit, you may be responsible for copays and coinsurance.
Prepare for your “Welcome to Medicare” visit
Make the most of your “Welcome to Medicare” visit by compiling some important information and reference documents beforehand. Gather and take the following items with you to your visit: Medical records, including immunization records; a detailed family health history; and a full list of medications and supplements, including calcium and vitamins, and how often and how much of each is taken.
About Medicare Made Clear
Medicare Made Clear brought to you by UnitedHealthcare provides Medicare education so you can make informed decisions about your health and Medicare coverage.
- Introduction to Medicare
- Types of plans
Get the latest
Boost your Medicare know-how with the reliable, up-to-date news and information delivered to your inbox every month.
*All fields required
More articles
Find a plan.
Enter your ZIP code for plans in your area
Call UnitedHealthcare toll-free at
1-833-301-2052, TTY 711
Hours: 8 a.m. - 8 p.m. 7 days a week
Meet with us
Make an appointment with a licensed insurance agent/producer in your area
- Annual Wellness Visit
- Preventive Care
- Chronic Care Management
- RPM Overview
- Management of Disease States
- Cardiology Patient Monitoring
- Endocrinology Patient Monitoring
- Gastroenterology and Bariatrics Patient Monitoring
- Pulmonology Patient Monitoring
- Resource Library
- ROI Calculator
- Working with Prevounce

- Annual Wellness Visits

- Medicare Annual Wellness Visit
Billing for a Medicare Annual Wellness Visit: Codes G0438 and G0439

- Remote Patient Monitoring (41)
- Chronic Care Management (21)
- Medicare Annual Wellness Visit (19)
- Preventive Care (12)
- Prevounce News (12)
- Compliance (9)
- Remote Care Management (9)
- Centers for Medicare & Medicaid Services (7)
by Lucy Lamboley
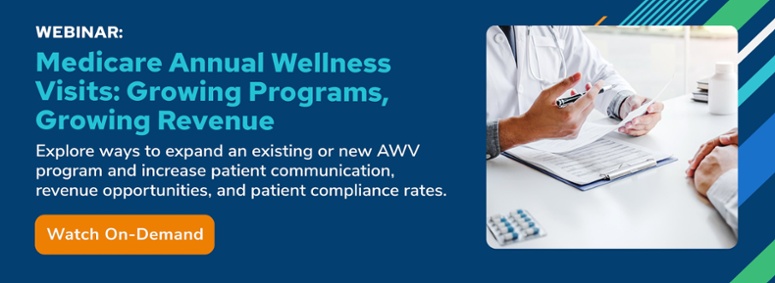
The importance of using preventive medicine to improve the health and ultimately lives of patients is widely recognized. The Medicare annual wellness visit (AWV) plays an important role in helping Medicare beneficiaries stay current with their health and take actions that can prevent illness and reduce risk.
An essential piece of the process required to ensure offering and providing preventive services remains financially viable is for organizations to complete the Medicare annual wellness visit reimbursement coding process accurately. Doing so can help ensure providers receive their earned reimbursements and protect them against possible penalties they might incur from failed coding audits. We know some organizations struggle with meeting compliance requirements set forth by the Centers for Medicare & Medicaid Services.
In this blog post, we take a look at what's required for compliant AWV coding. While this is by no means a comprehensive guide to Medicare annual wellness visit reimbursement, it provides organizations with information that can assist them in avoiding some of the most common AWV coding mistakes that result in rejected claims, lost revenue, or failed audits — all of which can be mitigated when using Prevounce software.
Three Unique Annual Wellness Visit Codes: G0402, G0438, and G0439
Medicare preventive wellness visits fall into three categories; the "Welcome to Medicare" visit, also known as the Initial Preventive Physical Exam (IPPE); the initial annual wellness visit, and the subsequent annual wellness visits. Each has its own Healthcare Common Procedure Coding System (HCPCS) code that must be used in the right circumstances and proper order.
Understanding HCPCS G0402
During the first 12 months a patient is enrolled in Medicare, they are eligible for the Welcome to Medicare visit or IPPE. This is a one-time visit that includes vital measurements, a vision screening, a depression screening, and other assessments meant to gauge the health and safety of an individual patient. This visit must be coded using HCPCS G0402. Once a patient has been enrolled for more than 12 months, the G0402 code will be rejected regardless of whether the IPPE visit previously took place or not.
Understanding HCPCS G0438
After a patient has been enrolled in Medicare for 12 months, they become eligible for an annual wellness visit. Note: If you need assistance with identifying eligible patients, get this AWV quick guide .
If the Medicare beneficiary had an IPPE completed, the patient is eligible for the initial AWV on the first day of the same calendar month the following year. An AWV is similar to the IPPE but includes slightly different required and accepted screenings. This initial AWV must be coded using HCPCS G0438.
Understanding HCPCS G0439
HCPCS G0439 is used to code all subsequent Medicare annual wellness visits that occur after the initial AWV (G0438). So, if used correctly, G0439 would not be used until G0402 was used to code the IPPE and G0438 was used to code the initial AWV. In the case that an IPPE was never completed, G0439 would still be used for any subsequent visits after G0438.
Purpose of Multiple Annual Wellness Visit HCPCS Codes
Though G0402, G0438, and G0439 are commonly confused, the reason for needing three separate codes is pretty straightforward. It is assumed that the different types of visits take different amounts of resources, and so they are reimbursed at different rates.
For example, the initial annual wellness visit is used to collect the library of information that will be continually updated with each subsequent AWV. As a result, the HCPCS G0438 code is reimbursed at a rate that is nearly 50% higher than HCPCS G0439. So if an organization regularly misses using the G0438 code for an initial Medicare AWV and uses G0439 instead, it could mean numerous denials and a significant loss of revenue.
Additional AWV HCPCS and CPT Codes
In addition to the primary annual wellness visit codes (G0402, G0438, and G0439), a select list of other codes may be billed for services performed during a Welcome to Medicare visit or AWV. When using any of these codes, a separate note is required to support each rendered service.
It is important to understand that many of these codes have specific guidelines that require them only to be used with specific visits after meeting certain criteria. For example, HCPCS G0444, which designates a 15-minute annual depression screening, may only be included with subsequent wellness visits billed under G0439. If that specific code is used with the IPPE or initial AWV, it will be rejected as invalid. An abdominal aortic aneurysm (AAA) screening, coded as G0389, may only be performed with the IPPE code G0402. It is not approved for annual wellness visits.
Advance care planning (CPT 99497) is considered an optional element of the annual wellness visit, which includes a discussion with the patient about their advance care wishes and advance directive. Advance care planning, also referred to as ACP, is considered a preventive service (and thus has its co-pay waived) when billed on the same day as an AWV with modifier -33.
HCPCS G0442 and HCPCS G0443 are additional codes that must be used in conjunction with each other to be valid. G0442 is used for an annual alcohol screening, which should take approximately 15 minutes. G0443 is for 15-minute sessions of alcohol counseling. According to the Centers for Medicare & Medicaid Services (CMS), the screening service must take place before a counseling service is approved. In other words, if G0443 is used and there are no claims for G0442 in the preceding 12 months, the screening code will be denied.
Fifteen-minute obesity counseling sessions may be billed in conjunction with IPPE visits or annual wellness visits using HCPCS G0447. This service includes dietary assessments and behavioral counseling, but a patient must have a body mass index of thirty or above to qualify.
If you ever have a wellness visit that takes a particularly long time, there is also a set of add-on codes you can use. HCPCS G0513 and HCPCS G0514 are "prolonged preventive service codes" that can be used when a service takes 30 minutes (G0513) or 60-plus minutes (G0514) past the typical duration of the service.
Staying Current With Annual Wellness Visit Coding Requirements
To avoid risking an audit, it is essential to stay up to date on coding requirements associated with Medicare annual wellness visits as they undergo occasional revisions. For example, in the 2023 Physician Fee Schedule (PFS) final rule , two preventive services had their HCPCS code descriptors modified. HCPCS G0442 was changed to "Annual alcohol misuse screening, 5 to 15 minutes" and HCPCS G0444 was changed to "Annual depression screening, 5 to 15 minutes." The codes currently require a minimum of 15 minutes of services. Such coding revisions and sometimes replacement is relatively common, and utilizing incorrect codes will lead to denied claims.
With changing guidelines and eligibility requirements, the task of coding correctly to better ensure proper reimbursement on preventive health visits can prove challenging for business office staff. But without the necessary revenue, organizations may struggle to support the delivery of preventive health services, which could negatively impact the care given to patients.
Providing the Annual Wellness Visits and Preventive Care in a Financially Sustainable Way
Medicare annual wellness visits and associated preventive services are not just valuable for patients. Organizations that provide these services can increase their revenue opportunities. In fact, by expanding establishing or growing an AWV program, an organization can generate significant, recurring reimbursement, as is covered in this on-demand webinar .
But Medicare hasn't made it easy for organizations to maintain compliance with its various AWV coding, billing, documentation, and service requirements, as rules undergo regular changes that can easily be missed or misunderstood. Enter Prevounce.
Prevounce lifts the burden of sorting through Medicare regulations to help you understand how preventive services can be utilized to best benefit the patient and your organization. Our platform improves everything from AWV eligibility verification to patient outreach and intake, to billing and coding, to completion of documentation, and more. To learn what Prevounce can do for your AWV program, whether it's in its infancy or ready for significant growth, schedule a demo today !
CPT Copyright 2023 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association.
Health economic and reimbursement information provided by Prevounce is gathered from third-party sources and is subject to change without notice as a result of complex and frequently changing laws, regulations, rules, and policies. This information is presented for illustrative purposes only and does not constitute reimbursement or legal advice. Prevounce encourages providers to submit accurate and appropriate claims for services. It is always the provider’s responsibility to determine medical necessity, the proper site for delivery of any services, and to submit appropriate codes, charges, and modifiers for services rendered. It is also always the provider’s responsibility to understand and comply with Medicare national coverage determinations (NCD), Medicare local coverage determinations (LCD), and any other coverage requirements established by relevant payers which can be updated frequently. Prevounce recommends that you consult with your payers, reimbursement specialists, and/or legal counsel regarding coding, coverage, and reimbursement matters. Payer policies will vary and should be verified prior to treatment for limitations on diagnosis, coding, or site of service requirements. The coding options listed here are commonly used codes and are not intended to be an all- inclusive list. We recommend consulting your relevant manuals for appropriate coding options. The Health Care Provider (HCP) is solely responsible for selecting the site of service and treatment modalities appropriate for the patient based on medically appropriate needs of that patient and the independent medical judgement of the HCP.
Lists by Topic
- Medicare (7)
- Telehealth Regulation and Law (6)
- Billing (4)
- Connected Medical Devices (2)
- Patient Resources (2)
- Arthritis (1)
- Chronic Pain Management (1)
- Diabetes (1)
- Mental Health (1)
Subscribe and Get The Latest News
Related posts, examples of remote patient monitoring: 9 top patient applications.
The use of remote patient monitoring — i.e., remote physiologic monitoring or RPM — has surged over the past few years. It's been widely embraced by providers, patients, the federal government, and an increasing number of commercial payers. Numerous statistics show the value of RPM, and when we look at some of the more common examples of remote patient monitoring applications, it is easy how RPM is transforming the delivery of care in the United States.
- Lucy Lamboley
- 17 min read
- April 5, 2024
Quick Guide: Remote Patient Monitoring CPT Codes to Know in 2024
Over the last few years, remote patient monitoring (RPM), also referred to as remote physiologic monitoring, became one of the more lucrative Medicare care management programs. Using average 2024 RPM reimbursement rates, if 100 patients are enrolled in an RPM program and each receives the minimum care management services each month, that will generate annual reimbursement of nearly $113,000.
- 13 min read
- March 22, 2024
AMA Weighing Substantial Expansion of Remote Patient Monitoring Codes
The American Medical Association (AMA) has announced the agenda for its second quarter 2024 CPT Editorial Panel meeting in May, and it includes discussion on what would be a significant and welcome expansion of remote patient monitoring (RPM) and remote therapeutic monitoring (RTM) CPT codes.
- Daniel Tashnek
- March 11, 2024
Prevounce creates wellness that works for everyone, with practice-specific, software-based programs that make preventive care, chronic care management, and remote patient monitoring easier to prep for, perform, document, and bill.
Wellness Program
- Medicare Preventive Services
- Remote Patient Monitoring
- MACRA & MIPS
© Copyright 2023 Prevounce - All Rights Reserved
Status | Privacy Policy | Do Not Sell My Information

- CCM (Chronic Care Managmenet)
- Care Coordination
- Preventitive and Wellness Programs
- Product Updates
- RHCs / FQHCs
« View All Posts
Annual Wellness Visit | CPT codes
2023 Annual Wellness Visit CPT Codes: G0402, G0438, G0439
- Share This Article
January 25th, 2023 | 8 min. read

ThoroughCare
Content Team
Print/Save as PDF
Understanding the billing codes for Medicare Annual Wellness Visits (AWVs) can provide a better idea of what is expected, both by the patient and by the payer. Understanding billing codes may also help you project revenues and optimize your staff’s capacity .
At ThoroughCare , we’ve worked with clinics and physician practices nationwide to help them streamline and capture Medicare reimbursements. Our software solution assists with the rules and regulations for AWVs while also tracking all activities related to providing the program and easing the difficulties of billing.
What are Annual Wellness Visits?
Annual Wellness Visits are free for anyone covered by Medicare Part B and include a yearly assessment of a patient’s health and overall well-being. They are designed not as a yearly physical examination, but as a critical care marker that bridges gaps in the yearly physical exam while developing and updating a patient’s personalized plan of care.
That personalized care plan is designed to help prevent disease and disability and is based on the patient’s current health and determined risk factors. The overall goal is to establish a record of the patient’s physical and mental well-being for the purpose of preventive health planning .
AWVs Include:
- A health risk assessment (HRA)
- A review and update of medical and family history
- A review of current providers, prescriptions/medications, and durable medical equipment suppliers
- Height, weight, blood pressure, BMI, and other routine measurements
- Personalized health advice, health education, and preventative counseling
- A list of identified risk factors, current medical and mental health conditions, and recommended treatment options
- A cognitive impairment screening
- A five to 10-year screening schedule for appropriate preventive services
- A review of the patient’s functional ability and level of safety, including screening for hearing impairments, risk of falling, activities of daily living, and level of home safety
- Identification of patients at risk for alcohol, tobacco, and opioid abuse
- Advance care planning
There are three types of wellness visits : Initial Preventive Physical Examination (IPPE), an Initial Annual Wellness Visit, and the Subsequent Annual Wellness Visit. Each entails a different billing code as well as specific qualifiers for each program.
- Initial Preventive Physical Examination: Patients may only receive this benefit within the first 12 months of their Medicare enrollment . Commonly referred to as the “welcome to Medicare visit,” it is considered a once in a lifetime assessment and after the initial eligibility period, the patient cannot receive an IPPE. It is also dependent on the HRA .
- Initial Annual Wellness Visits : Similar to an IPPE, except it is available to a patient after 11 months of Medicare enrollment . This is for patients that miss their window for an IPPE. However, if the patient does complete an IPPE, they must still complete the Initial Annual Wellness Visit. This screening also includes an optional cognitive exam and end-of-life planning.
- Subsequent Annual Wellness Visit: Is the yearly follow-up to an Initial Annual Wellness Visit . Eleven full months after the Initial Annual Wellness Visit, a patient can attend these visits to modify and maintain their preventive care plan, based on how their health is at any given time.
As the patient’s health evolves over time, a doctor may use the Subsequent Annual Wellness Visit to guide them toward other Medicare preventive programs, such as Chronic Care Management (CCM) , Behavioral Health Integration (BHI) , or Remote Patient Monitoring (RPM) .

Billing Medicare Annual Wellness Visits
Five items are required when submitting a claim through Centers for Medicare & Medicaid Services (CMS) :
- A CPT Code for the specific type of AWV provided
- An ICD-10 code for a general adult medical examination (Z00.00)
- Date of service
- Place of service (most office in-office or telehealth)
- Submit National Provider Identifier (NPI) number
It is helpful to know the care manager assigned to a patient in case of an audit.
Three Steps to Bill for AWVs :
- Verify CMS requirements were met
- Submit claims to CMS annually
- Determine there are no conflicting billing codes
CPT Codes for Annual Wellness Visits
See 2024 reimbursement rates here .
The types of AWVs are reflected in the CPT codes. The crucial qualifying determinant is when a certain AWV can be provided and billed.
.png?width=953&height=419&name=awv_2023_cpt_codes_downloadable_cta%20(3).png)

AWVs for Federally Qualified Health Centers (FQHC) and Advance Care Planning (ACP)
As shown in the chart above, FQHC are able to bill for AWVs, although they utilize additional codes.
In addition to the standard CPT codes associated with AWVs, FQHC may use a special add-on code (G0468) that will allow them to receive additional reimbursement. For example, if an FQHC were to provide an IPPE, the clinic would bill for G0402 + G0468 for a total average reimbursement of $322. This coding indicates to CMS that the service is being provided through an FQHC. The good news is that these organizations receive much higher average reimbursement rates
Advance care planning (ACP) is not a type of AWV , but it can play a meaningful part in the program.
ACP is a formal process to understand the patient’s preferences for potential and future medical care, such as end-of-life planning, a living will, and power of attorney. It is an opportunity to craft a patient-centered care plan and an AWV drives just that opportunity. Providers often complete an ACP during an AWV.
ACP is fully covered for patients under Medicare Part B if it is conducted during the AWV. It is a free service that is an optional element of AWVs. Favorably, it is reimbursable for your practice and can be billed in concurrence with an AWV using CPT code 99497 for the first 30 minutes and 99498 for subsequent 30-minute billing.
Streamline Medicare Annual Wellness Visits
ThoroughCare offers end-to-end workflow for Annual Wellness Visits.
We simplify the process and help providers engage patients to get their most relevant health information. Guided interviews help ask the right questions and ensure all service requirements are met. ThoroughCare includes digital solutions, such as:
- An interactive health risk assessment
- Screening tools, such as ADL, CAGE, DAST-10, GAD-7, MDQ, PAC, PHQ-2, and a mini cognitive exam
- A care gaps summary with recommended interventions
- A full report of Personalized Prevention Plan Services
- Comprehensive care planning tools
- Automated CPT code assignment for accurate billing

Reimbursement rates are based on a national average and may vary depending on your location. Check the Physician Fee Schedule for the latest information.
- Log In Username Enter your ACP Online username. Password Enter the password that accompanies your username. Remember me Forget your username or password ?
- Privacy Policy
- Career Connection
- Member Forums
© Copyright 2024 American College of Physicians, Inc. All Rights Reserved. 190 North Independence Mall West, Philadelphia, PA 19106-1572 800-ACP-1915 (800-227-1915) or 215-351-2600
If you are unable to login, please try clearing your cookies . We apologize for the inconvenience.
Medicare’s Annual Wellness Visit (AWV)
The Medicare Annual Wellness Visit (AWV) is a yearly appointment with a health professional to identify health risks and help reduce them and to create or update a personalized prevention plan. During a Medicare AWV, health professionals should also review any current opioid prescriptions, detect any cognitive impairment, and establish or update medical and family history.
Coding and Billing a Medicare AWV
G0438: Annual wellness visit, includes a personalized prevention plan of service (PPS), initial visit
G0439: Annual wellness visit, includes a personalized prevention plan of service (PPS), subsequent visit
G0468: Federally qualified health center (FQHC) visit, IPPE, or AWV; a FQHC visit that includes an initial preventive physical examination (IPPE) or annual wellness visit (AWV) and includes a typical bundle of Medicare-covered services that would be furnished per diem to a patient receiving IPPE or AWV
Diagnosis code V70.0; Initial Annual Wellness Visit G0438; Subsequent Annual Wellness Visit G0439
Medicare will pay a physician for an AWV service and a medically necessary service, e.g. a mid-level established office visit, Current Procedural Terminology (CPT) code 99213, furnished during a single beneficiary encounter. It is important that the elements of the AWV not be replicated in the medically necessary service. Physicians must append modifier -25 (significant, separately identifiable service) to the medically necessary E/M service, e.g. 99213-25, to be paid for both services.
For example, for the patient who comes in for his Annual Wellness Visit and complains of tendonitis would be billed as follows: CPT ICD9, G0438 V70.0, 99212-25 726.90 (tendonitis)
ACP Tools for the Annual Wellness Visit
The following forms and templates can be customized for use in your practice:
- Practice Checklist
- Patient Letter and Checklist
- Health Risk Assessment :
- View a paper version
- View an electronic version from HowsYourHealth.org
- Women's Prevention Plan
- Men's Prevention Plan
- Adult Health Maintenance Form
- Advanced Care Planning
Patient Handouts
- Patient FACTS
For more details about how to bill these codes, see Module 9 of Coding for Clinicians.
Medicare Interactive Medicare answers at your fingertips -->
Annual wellness visit, preventive services.
You must be logged in to bookmark pages.
Email Address * Required
Password * Required
Lost your password?
The Annual Wellness Visit (AWV) is a yearly appointment with your primary care provider (PCP) to create or update a personalized prevention plan. This plan may help prevent illness based on your current health and risk factors. Keep in mind that the AWV is not a head-to-toe physical. Also, this service is similar to but separate from the one-time Welcome to Medicare preventive visit .
Eligibility
Medicare Part B covers the Annual Wellness Visit if:
- You have had Part B for over 12 months
- And, you have not received an AWV in the past 12 months
Additionally, you cannot receive your AWV within the same year as your Welcome to Medicare preventive visit.
Covered services
During your first Annual Wellness Visit, your PCP will develop your personalized prevention plan. Your PCP may also:
- Check your height, weight, blood pressure, and other routine measurements
- This may include a questionnaire that you complete before or during the visit. The questionnaire asks about your health status, injury risks, behavioral risks, and urgent health needs.
- This includes screening for hearing impairments and your risk of falling.
- Your doctor must also assess your ability to perform activities of daily living (such as bathing and dressing), and your level of safety at home.
- Learn about your medical and family history
- Medications include prescription medications, as well as vitamins and supplements you may take
- Your PCP should keep in mind your health status, screening history, and eligibility for age-appropriate, Medicare-covered preventive services
- Medicare does not require that doctors use a test to screen you. Instead, doctors are asked to rely on their observations and/or on reports by you and others.
- Screen for depression
- Health education and preventive counseling may relate to weight loss, physical activity, smoking cessation, fall prevention, nutrition, and more.
AWVs after your first visit may be different. At subsequent AWVs, your doctor should:
- Check your weight and blood pressure
- Update the health risk assessment you completed
- Update your medical and family history
- Update your list of current medical providers and suppliers
- Update your written screening schedule
- Screen for cognitive issues
- Provide health advice and referrals to health education and/or preventive counseling services
If you qualify, Original Medicare covers the Annual Wellness Visit at 100% of the Medicare-approved amount when you receive the service from a participating provider . This means you pay nothing (no deductible or coinsurance ). Medicare Advantage Plans are required to cover AWVs without applying deductibles, copayments, or coinsurance when you see an in-network provider and meet Medicare’s eligibility requirements for the service.
During the course of your AWV, your provider may discover and need to investigate or treat a new or existing problem. This additional care is considered diagnostic, meaning your provider is treating you because of certain symptoms or risk factors. Medicare may bill you for any diagnostic care you receive during a preventive visit.
Update your browser to view this website correctly. Update my browser now
- Compliance with Medicare’s updated 2024 split (or shared) visit policy
[author: Elin Baklid-Kunz*]
Compliance Today (May 2024)
Split (or shared) visits—the current term used by the Center for Medicare & Medicaid Services (CMS)—allow non-physician practitioners (NPPs) and physicians who work for the same employer/entity to share patient visits on the same day by billing the combined work under the physician’s National Provider Identifier (NPI) and receive 100% of the Medicare Physician Fee Schedule (MPFS), or the NPP’s NPI for reimbursement of 85% of the MPFS.
In the 2024 MPFS Final Rule, CMS revised the definition of “substantive portion” of a split (or shared ) visit to reflect the revisions made by the American Medical Association’s (AMA) Current Procedural Terminology (CPT) Editorial Panel. [1] CMS removed history and exam from the definition of substantive portion and adopted the determination of medical decision making (MDM) as defined by CPT as the provider who “made or approved the management plan.”
There are two ways for providers to meet the guidelines, and the billing provider is determined by the provider who performs:
more than half of the total time, or
a substantive part of the MDM as defined by CPT (except for critical care visits, which use time only and are not MDM).
The revised policy is somewhat unexpected, as CMS has several times delayed a proposed policy that “whichever of the providers who spends the most time” would bill the service.
While there are many articles for providers on how to be compliant going forward, for auditors and providers facing retrospective audits, things are a little bit more confusing—specifically for auditors working in the legal space who frequently perform audits based on the different guidelines in effect for the different dates of service. For example, an auditor may be asked to review evaluation and management (E/M) services where the scope also includes compliance with split (or shared) services from 2021 to 2024. This would be a challenge with the different guidelines for split (or)shared services with different rules based on 2021 and prior, 2022 to 2023 new policy and transition, and 2024 revisions. To complicate this further, AMA had major revisions to the CPT Documentation Guidelines for outpatient office visits (CPT 99202–99215) in 2021 and for the remainder of E/M services in 2023 that impacts how E/M services are documented and reviewed.
Background Medicare’s split (or shared) visits—2021 and prior
Prior to 2002, the role of NPPs and the appropriate billing practices related to the services they provided in the facility setting were not clearly defined. Typically, NPPs such as nurse practitioners and physician assistants—also referred to as qualified healthcare practitioners (QHP) by the AMA—would assist physicians in the hospital with rounding or seeing patients in the emergency room, and these services were billed under the physicians’ NPIs. While certain documentation requirements applied, they were not clearly defined and varied by payer.
In October 2002, CMS Transmittal 1776 introduced Medicare’s payment policy for split (or shared) E/M visits. [2] However, the full definition was introduced in Transmittal 808 in January 2006; it updated CMS Internet Only Manual: Medicare Claims Processing Manual (MCPM) Publication 100-04, Chapter 12, Section 30.6.1.H Split/Shared E/M Visit. (This section has since been removed): [3]
A split/shared E/M visit cannot be reported in the SNF [skilled nursing facility]/NF [nursing facility] setting. A split/shared E/M visit is defined by Medicare Part B payment policy as a medically necessary encounter with a patient where the physician and a qualified NPP each personally perform a substantive portion of an E/M visit face-to-face with the same patient on the same date of service. A substantive portion of an E/M visit involves all or some portion of the history, exam or medical decision making key components of an E/M service. The physician and the qualified NPP must be in the same group practice or be employed by the same employer. The split/shared E/M visit applies only to selected E/M visits and settings (i.e., hospital inpatient, hospital outpatient, hospital observation, emergency department, hospital discharge, office and non facility clinic visits, and prolonged visits associated with these E/M visit codes). The split/shared E/M policy does not apply to consultation services, critical care services or procedures.
This allowed physicians to be reimbursed at 100% of the MPFS, although the NPP may have done most of the work if the physician performed and documented a face-to-face portion on the same calendar day.
These regulations remained in effect until CMS removed the MCPM sections related to split (or shared) E/M visits on May 26, 2021, [4] preparing for the revised payment rules, which were published in the 2022 MPFS Final Rule in November 2021. [5] It should also be noted that with the removal of the guidelines and until CMS published the final rule, CMS stated that “the agency will limit review.”
Revised policy and CMS transition period 2022–2023
Both 2022 and 2023 are considered transition years before CMS revised the policy for 2024; however, the major changes were effective in 2022.
With the revised policy—effective on January 1, 2022—split (or shared) E/M visits can only be performed in the facility setting (i.e., hospital inpatient/outpatient and emergency room); they can no longer be performed in an office setting, such as place of service 11. Prior to 2022, split (or shared) services were allowed in the office setting if incident-to were also met. [6] CMS added SNF E/M visits to services that can be split (or shared) except for SNF E/M visits that are required to be performed in their entirety by a physician; however, NF visits remained not billable as split (or shared) services.
Also new for 2022 was the addition of critical care services to E/M services that may be performed as split (or shared) and a new modifier -FS, which is required on Medicare claims to indicate the services were split (or shared) E/M visits.
For 2022, there were two ways for providers to meet the guidelines for billing split (or shared)—determined by the provider who performed the “substantive portion” of the visit—which was further defined as the provider who:
Performed more than half of the total time of the visit, or
Fully performed one of the three key components, history exam, or MDM.
The exception was critical care services, which must meet the “greater than 50%” definition of substantive portion. Perhaps the biggest change for 2022 was that time can now include non-face-to-face time.
The 2022 MPFS Final Rule also contained a separate definition for the “substantive portion” for 2023: whichever providers spend the most time would bill the service. However, the implementation of billing only based on time spent was delayed until at least December 31, 2024.
This new payment policy and the substantive portion are codified in 42 C.F.R. § 415.140 : [7]
Split (or shared) visit means an evaluation and management (E/M) visit in the facility setting that is performed in part by both a physician and a nonphysician practitioner who are in the same group, in accordance with applicable law and regulations such that the service could be billed by either the physician or nonphysician practitioner if furnished independently by only one of them. Substantive portion means more than half of the total time spent by the physician and nonphysician practitioner performing the split (or shared) visit, or a substantive part of the medical decision making except as otherwise provided in this paragraph. For critical care visits, substantive portion means more than half of the total time spent by the physician and nonphysician practitioner performing the split (or shared) visit.
Prior to 2022, AMA updated their office/outpatient E/M visits guidelines for 2021, allowing providers to select the level of office visits based on the amount of time spent with the patient or the level of MDM. [8] For coding purposes, history and physical exam documentation were eliminated, and total time was updated to include non-face-to-face time personally spent by the provider or NPP, but not other clinical staff. Non-face-to-face time includes activities such as preparing to see the patient, ordering procedures, etc.
It should also be noted that the AMA introduced a split (or shared) visit definition in the CPT manual for the first time in 2021. Although CMS did not adopt the CPT definition, the CPT time guidelines can be used. CPT defines the specific activities, which can be found in the E/M guidelines section of the CPT book.
Documentation
Documentation for split (or shared) visits should follow the guidelines for any E/M service and must support the combined service level reported on the claim. Both providers should personally document their portion of the visit separately in the medical record, as documentation should clearly indicate the services provided by each individual. If time is used for the level, the documentation should include time spent by each provider.
Prior to the 2022 changes, the documentation requirements for split (or shared) visits were focused on ensuring the physician performed and documented a face-to-face encounter with the patient on the same day as the NPP.
The policy then requires the provider who bills the service to perform a “substantive” component, starting with 2022. The new definition of substantive means the provider must document one of the components in its entirety, such as history, exam or MDM, or bill based on time.
Then, for 2024, since history or exam are no longer relevant for coding purposes, the billing provider must document the MDM in its entirety or bill based on time.
Medicare’s conditions of payment require that the documentation in the medical record identify the physician and NPP who performed the visit, and that the billing provider who is performing the substantive portion must sign and date the medical record. [9] For billing purposes, starting with 2022, the designated modifier -FS must be included on the claim to identify that the services are split (or shared).
As for any medical record documentation, it is important to avoid copy-and-paste errors, by ensuring that documentation is unique to each patient encounter and avoiding copying and pasting information from previous encounters. Each encounter should reflect the specific details of that visit. Providers should exercise caution with canned statements.
For example, it is not uncommon to see attestation statements when reviewing split (or shared) services, and often these statements are not sufficient. For example: “I, the attending emergency medicine physician, provided a substantive portion of the care of this patient. I personally performed the medical decision making in its entirety, in addition to components of the history and physical exam, for this encounter.”
This statement alone would not likely pass a payer audit if the medical record also does not contain documentation of what the physician actually performed.
Billing based on time
Before 2023, in the facility setting (2021 for office visits), providers could use time as the determining factor for E/M services by documenting total time, the content of the counseling or coordination of care, and documentation that more than half of the time was spent on counseling or coordination of care. (i.e., “20 minutes of the 30-minute visit spent counseling the patient on . . .”). This is often referred to as using “time based counseling or coordination of care” and was eliminated in 2023 when CPT expanded the 2021 documentation guidelines where visits are based on total time or MDM, to apply to all EM visit codes (except critical care services). [10]
The biggest change with time, however, is allowing “non-face-to-face” time spent on the same date to be used for split (or shared) visits as long as one of the practitioners has face-to-face (in-person) contact with the patient. It does not necessarily have to be the physician or the NPP who performs the substantive portion and bills for the visit. The substantive portion can be entirely with or without direct patient contact and is determined by the proportion of total time—not whether the time involves patient contact.
Examples of non-face-to-face time include time preparing to see the patient, reviewing test results, or discussing the patient’s care with other providers. For example, activities that cannot be counted include traveling and teaching.
It is essential that each provider documents their distinct time in the medical record. And when two or more providers jointly meet with or discuss the patient, only the time of one individual should be counted. For example:
If the NPP sees a hospital patient in the morning and spends 10 minutes, and the physician follows up later the same calendar day with a 15-minute visit, the physician may report the service based on time. The total time for the visit would be 25 minutes, and the provider who spent more than 50% of the visit—the physician—can report the service.
If, in the same situation, the physician and NPP met together for five additional minutes (beyond the 25 minutes) to discuss the patient’s treatment plan, that overlapping time could only be counted once for purposes of establishing total time and who provided the substantive portion of the visit. The total time would be 30 minutes, and the physician would bill for the visit since they spent more than half of the total time (20 of 30 total minutes).
This captures the main intent behind the split (or shared) service, as it allows the NPP to see patients while the physician may be in surgery or otherwise unavailable. The physician would then see the patient later in the day, such as more complex patients who need the physician’s experience. The split (or shared) rules were not designed to encourage physicians to simply stop by to see the patient to capture the additional 15% in revenue or only sign off on the medical records after the NPP visit. However, it should be noted that CMS— in the 2024 Final Rule—specifically stated: “We note that the policy is not about whether the physician’s expertise is ‘necessary’ for the visit but rather whether the physician or the NPP should bill for the service when each of them are performing part of an E/M visit.” [11]
Compliance with split (or shared) E/M visits
Many of the recent overpayments, audits, Civil False Claims Act, and even criminal cases instituted by the federal and state agencies overseeing the Medicare and Medicaid programs involve allegations of improper billing for “incident-to” services and split (or shared) services.
One example is the recent False Claims Act case against TeamHealth, who settled for $48 million in 2021. The realtors alleged that TeamHealth engaged in a scheme to defraud Medicare by overbilling for services provided by NPPs by submitting claims for reimbursement for services performed by NPPs but using physicians’ NPIs, which inflated their reimbursement rate. The relators alleged that TeamHealth covered up this practice by characterizing NPP services as split (or shared) E/M services. [12]
To prepare for potential increased audit scrutiny, if your practice employs NPPs, any E/M audit should include services performed split (or shared) as well as services performed incident-to.
Practices should consider the following steps for compliance:
Understand current policy : Familiarize yourself with Medicare and CPT guidelines for split (or shared) E/M visits. See Figure 1.
Payer difference : Query payers to understand their policy for split (or shared) visits.
Perform baseline audit : Assess your compliance by performing a baseline audit.
Educate providers : If discrepancies or issues are identified, provide feedback to the involved providers and educate them on Medicare and other payers’ specific guidelines.
Implement corrective actions : If necessary, implement corrective actions to address any identified issues. This may include additional training for providers or improvements to documentation processes. It may include changes to workflows and roles affected by the revisions for 2024.
Monitor compliance : Establish an ongoing monitoring process to ensure ongoing compliance with Medicare guidelines for split (or shared) E/M visits. Regularly audit sample documentation to identify and address any issues promptly. A checklist can be used to help with this.
Stay informed : Keep abreast of any updates or changes to Medicare guidelines. Medicare policies can change, and staying informed will help ensure ongoing compliance. And make sure to monitor updates from your Medicare administrative contractors, as we can expect additional information based on the revised policy.
Last, remember that the new modifier -FS will make it easier for Medicare to monitor claims and ensure that providers are correctly billing for split (or shared) E/M services.
Understand the different timelines and guidelines for auditing split (or shared) visits: 2021 and prior, 2022–2023 new and transition and 2024 revisions.
Use an auditor reference tool to help with retrospective audits.
The Centers for Medicare & Medicaid Services only allow split (or shared) visits in the facility setting (i.e., hospital, emergency room) starting with calendar year 2022; however, Current Procedural Terminology is silent on location and may be allowed in the office setting.
Time for split/shared service may include both face-to-face and non-face-to-face activities.
Perform a baseline audit to ensure compliance with Medicare’s updated split (or shared) visit policy.
*Elin Baklid-Kunz is a Healthcare Consultant at KUNZ LLC in Orlando, Fl.
1 Centers for Medicare & Medicaid Services, CY 2024 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program Requirements; Medicare Advantage; Medicare and Medicaid Provider and Supplier Enrollment Policies; and Basic Health Program, 88 Fed. Reg. 78,818 (Nov. 16, 2023), https://www.federalregister.gov/documents/2023/11/16/2023-24184/medicare-and-medicaid-programs-cy-2024-payment-policies-under-the-physician-fee-schedule-and-other .
2 Centers for Medicare & Medicaid Services, “New/Revised Material – Effective Date: July 1, 2001, Implementation Date: October 25, 2002,” Transmittal 1776, Change Request 2321, October 25, 2002, https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R1776B3.pdf .
3 Centers for Medicare & Medicaid Services, “Nursing Facility Service (Codes 99304 – 99318),” CMS Manual System, Pub 100–04 Claims Processing, Transmittal 808, Change Request 4246, January 6, 2006, https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R808CP.pdf .
4 Centers for Medicare & Medicaid Services, “Release: CMS Notice Regarding Split (or Shared) Evaluation and Management Visits and Critical Care Services from May 26, 2021, through December 31, 2021,” May 26, 2021, https://www.cms.gov/files/document/enf-instruction-split-shared-critical-care-052521-final.pdf .
5 Medicare Program; CY 2022 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment Policies; Medicare Shared Savings Program Requirements; Provider Enrollment Regulation Updates; and Provider and Supplier Prepayment and Post-Payment Medical Review Requirements, 86 Fed. Reg. 64,996 (Nov. 19, 2021), https://www.govinfo.gov/content/pkg/FR-2021-11-19/pdf/2021-23972.pdf .
6 Medicare Program; CY 2022 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment Policies.
7 § 415.140 Conditions for payment: Split (or shared) visits, up to date as of March 11, 2024, https://www.ecfr.gov/current/title-42/chapter-IV/subchapter-B/part-415/subpart-C/section-415.140 .
8 American Medical Association, “CPT® Evaluation and Management (E/M) Office or Other Outpatient (99202–99215) and Prolonged Services (99354, 99355, 99356, 99417) Code and Guideline Changes,” January 1, 2021, https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf .
9 42 C.F.R. § 415.140 Conditions for payment, Split (or shared) visits.
10 American Medical Association, “CPT® Evaluation and Management (E/M) Code and Guideline Changes,” January 1, 2023, https://www.ama-assn.org/system/files/2023-e-m-descriptors-guidelines.pdf .
11 Centers for Medicare & Medicaid Services, CY 2024 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies.
12 United States of America, ex rel. Caleb Hernandez & Jason Whaley, Relators v. Team Health Holdings INC., Team Finance, L.L.C., Team Health INC., & Ameriteam Services, L.L.C., Case 2:16-cv-00432-JRG, (E.D. Tex. Nov. 12, 2018).
13 Medicare & Medicaid Services, CY 2024 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program Requirements; Medicare Advantage; Medicare and Medicaid Provider and Supplier Enrollment Policies; and Basic Health Program, 88 Fed. Reg. 78,818 (Nov. 16, 2023), https://www.federalregister.gov/documents/2023/11/16/2023-24184/medicare-and-medicaid-programs-cy-2024-payment-policies-under-the-physician-fee-schedule-and-other .
14 American Medical Association, CPT Professional 2024 (Chicago, IL: American Medical Association, 2023).
15 Medicare and Medicaid Services, CY 2023 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program Requirements; Implementing Requirements for Manufacturers of Certain Single-dose Container or Single-use Package Drugs To Provide Refunds With Respect to Discarded Amounts; and COVID–19 Interim Final Rules, 87 Fed. Reg. 69,904 (Nov. 18, 2022), https://www.federalregister.gov/documents/2022/11/18/2022-23873/medicare-and-medicaid-programs-cy-2023-payment-policies-under-the-physician-fee-schedule-and-other .
16 American Medical Association, “CPT® Evaluation and Management (E/M) Code and Guideline Changes.”
17 Medicare Program; CY 2022 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment Policies.
18 Centers for Medicare & Medicaid Services, 1997 Documentation Guidelines for Evaluation and Management Services , accessed March 25, 2024, https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnedwebguide/downloads/97docguidelines.pdf ; Centers for Medicare & Medicaid Services, 1995 Documentation Guidelines for Evaluation and Management Services , accessed March 25, 2024, https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnedwebguide/downloads/95docguidelines.pdf .
19 American Medical Association, CPT Professional 2022 (Chicago, IL: American Medical Association, 2021).
20 Centers for Medicare & Medicaid Services, “Release: CMS Notice Regarding Split (or Shared) Evaluation and Management Visits and Critical Care Services from May 26, 2021, through December 31, 2021.”
21 American Medical Association, CPT Professional 2021 (Chicago, IL: American Medical Association, 2020).
22 American Medical Association, “CPT® Evaluation and Management (E/M) Office or Other Outpatient (99202–99215) and Prolonged Services (99354, 99355, 99356, 99417) Code and Guideline Changes.”
23 Centers for Medicare & Medicaid Services, “Nursing Facility Service (Codes 99304 – 99318).”
[ View source .]
Latest Posts
- An international standard for healthcare quality management
- Hackers Increasingly Leveraging Threats to Patients to Pressure Health Organizations to Pay Ransom
- Privacy Briefs: April 2024
- [Event] Regional Compliance & Ethics Conference - May 3rd, Lewis Center, OH
See more »
Refine your interests »
Written by:

Published In:
Health care compliance association (hcca) on:.

"My best business intelligence, in one easy email…"
Preventive & screening services
Contact your provider to schedule an appointment. Need a provider? You can find and compare providers in your area.
Here's a list of preventive and screening services Medicare Part B (Medical Insurance) covers:
- Abdominal aortic aneurysm screenings
- Alcohol misuse screenings & counseling
- Blood-based biomarker tests
- Cardiovascular disease screenings
- Cardiovascular disease (behavioral therapy)
- Cervical & vaginal cancer screenings
- Multi-target stool DNA tests
- Screening barium enemas
- Screening colonoscopies
- Screening fecal occult blood tests
- Screening flexible sigmoidoscopies
- Depression screenings
- Diabetes screenings
- Diabetes self-management training
- Glaucoma tests
- Hepatitis B shots
- Hepatitis B Virus (HBV) infection screenings
- Hepatitis C screening tests
- HIV screenings
- Lung cancer screenings
- Mammograms (screening)
- Medicare Diabetes Prevention Program
- Nutrition therapy services
- Obesity screenings & counseling
- One-time “Welcome to Medicare” preventive visit
- Pneumococcal shots
- Prostate cancer screenings
- Sexually transmitted infections screenings & counseling
- COVID-19 vaccines
- Tobacco use cessation counseling
- Yearly "Wellness" visit
Preventive services help you stay healthy, detect health problems early, determine the most effective treatments, and prevent certain diseases. Preventive services include exams, shots, lab tests, and screenings. They also include programs for health monitoring, and counseling and education to help you take care of your own health.
Related resources
- Medicare & You: Medicare's preventive benefits (video)
Is my test, item, or service covered?
Wellcare uses cookies. By continuing to use our site, you agree to our Privacy Policy and Terms of Use.
The search value cannot be empty
Please wait while your request is being processed., this link will leave wellcare.com, opening in a new window., wellcare giveback open (ppo).
- Medicare Basics
- Medication Therapy Management
- 2024 Provider Directories
Welcome to your Medicare Advantage Plan!
Thank you for being a Wellcare member! We want to help you get the most from your plan.
Use our website to explore plan information and benefits and review helpful plan documents such as the Evidence of Coverage, Summary of Benefits, and Annual Notice of Change.
Plan Specific Documents
This document includes any changes in coverage, costs or service area between your previous and current plan year.
- English Last Updated October 10, 2023
- Spanish Last Updated October 10, 2023
This document provides some of the features of this plan. For a complete list of benefits, see your Evidence of Coverage.
- English Last Updated October 01, 2023
- Spanish Last Updated October 01, 2023
This document includes a legal, detailed description of your benefits and costs as a member.
This document provides additional details about the dental benefits, including a list of services and benefit limits.
- Spanish Last Updated October 03, 2023
Use this form to enroll in a Medicare Advantage Plan
Star Ratings judge how well Medicare health and drug plans perform in different categories. They are distributed by Medicare. Medicare evaluates plans based on a 5-Star rating system. Star Ratings are calculated each year and may change from one year to the next.
- English Last Updated October 31, 2023
- Spanish Last Updated October 31, 2023
Related Materials
This document includes information about multi-language interpreter services for speakers of Arabic, Chinese Cantonese, Chinese Mandarin, French Creole, French, German, Hindi, Italian, Japanese, Korean, Polish, Portuguese, Russian, Spanish, Tagalog, and Vietnamese.
- Multi Language
Use this form to authorize us to withdraw your monthly premiums from your bank.
Complete this form to request reimbursement for covered medical services that you paid for out of pocket.
Complete this form to request reimbursement/refund for covered prescription drugs that you paid full price for.
This form confirms your request for a particular person to act as your representative in connection with a claim.
Each member requesting to be disenrolled must complete their own form.
Part D Late Enrollment Penalty (LEP) Reconsideration Request Form
Please complete this form with your provider if you want to change your PCP. Your provider will then send this form to your health plan, letting them know about the change.
The drugs on this list require step therapy. Step therapy means you must try one drug before we will cover another drug.
Helpful Information
- 24 Hour Nurse Advice Line
Krames Health Library
24-hour nurse advice line.
One of the benefits of being a Wellcare member is our 24-Hour Nurse Advice Line. Our nurses will give you answers to your medical questions and help you decide whether to see your doctor or go to the emergency room. Nurses are available 24 hours a day, seven days a week at 1-800-581-9952 . (TTY users dial 711 .)
The Krames Health library is the most up-to-date patient education resource. With Krames Health Library, you'll have access to over 4,000 topics relating to health and medication. Visit the Krames Health Library .
New – Krames/StayWell Library!
We have added a new set of tools to help you. This site has added assessments for wellness and lifestyle improvements. View the new Krames/StayWell Library .
- Plan Materials
- Drug (Formulary) Search Tool
- Drug List (Formulary) and Other Documents
- Medication Guide
- Transition Policy Part D
- New Member Quick Tips
- Coverage Decisions and Appeals
- Exceptions (Part D)
- Rights and Responsibilities
Need help? We're here for you.

Providing Medicare wellness visits can be challenging but can improve quality and practice revenue.
ARNOLD E. CUENCA, DO, CAQSM, FAAFP, AND SUSAN KAPSNER, CCS
Fam Pract Manag. 2019;26(2):25-30
Author disclosures: no relevant financial affiliations disclosed.
Editor's note: This is a corrected version of the article previously published.

The Affordable Care Act of 2010 created the Medicare annual wellness visit (AWV) as a way to provide patients with comprehensive preventive care services at no cost. Yet many practices have been slow to provide substantial numbers of these visits. Only 15.6 percent of eligible patients received an AWV through 2014. 1 In addition to finding lackluster overall participation, researchers have found AWV rates are lower among practices caring for underserved populations, such as racial minorities, rural residents, or those dually enrolled in Medicaid. 2
Physicians and other health care providers do not offer AWVs to their Medicare patients for numerous reasons. Providing and documenting all of the required AWV elements efficiently can be challenging, and some practices may feel their staffing or electronic health record resources are too limited. Many patients and even some physicians may not know what the AWV entails, and patients with complex socioeconomic risk factors may have pressing health conditions that need to take priority over preventive services. These explanations can all be valid, but this article seeks to help physicians reevaluate the AWV, along with the initial preventive physical examination (IPPE) or “Welcome to Medicare” visit, and recognize the value these wellness visits can bring not only to their patients but also to their practices or health care organizations.
The Medicare annual wellness visit (AWV) and the initial preventive physical examination (IPPE) provide a number of benefits to patients and physicians, but many physicians still do not provide them.
Medicare wellness visits can help physicians address care gaps and report quality measures important in pay-for-performance systems.
When billed correctly and delivered efficiently along with other covered Medicare preventive services, AWVs can boost practice revenue.
THE VALUE OF MEDICARE WELLNESS VISITS
The main benefit of the AWV to patients is the creation of a personalized prevention plan, a written plan that can help guide their preventive care decisions for the next five to 10 years. This plan includes age-appropriate preventive services, recommendations offered by both the U.S. Preventive Services Task Force and the Advisory Committee on Immunization Practices, and personalized health advice that identifies risk factors and suggests referrals or programs to address them. 3
Providing Medicare wellness visits also offers a structure that helps physicians to close many pay-for-performance quality measure gaps, including those recognized by the Core Quality Measures Collaborative, the Integrated Healthcare Association’s California Value Based P4P program, and the National Committee for Quality Assurance’s Healthcare Effectiveness Data and Information Set. In addition, accountable care organizations participating in the Medicare Shared Savings Program can use data collected during wellness visits to satisfy specific quality measures for the 2018 and 2019 quality reporting years. 4 (See “ Closing quality measure gaps .”)
There also are financial incentives to implementing AWVs. Physicians participating in Medicare’s Merit-based Incentive Payment System (MIPS) can use AWVs to raise their quality scores, which can potentially lead to positive Medicare payment adjustments. Practices that provide AWVs often generate greater revenue than those that do not – a result of billing AWVs with associated preventive services and same-day problem-oriented services. 2 AWVs also provide physicians another opportunity to assess and report risk-adjusted diagnoses for Medicare Advantage beneficiaries. Future payment rates for higher risk patients are calculated based on risk-adjusted factor (RAF) scores, so addressing Hierarchical Condition Category-related diagnoses in the same visit can be of additional value. (For more on this subject, see “ Is Your Diagnosis Coding Ready for Risk Adjustment? ” FPM , March/April 2018, and “ Diagnosis Coding for Value-Based Payment: A Quick Reference Tool ,” FPM , March/April 2018.)
CLOSING QUALITY MEASURE GAPS
Many pay-for-performance measures can be addressed during Medicare wellness visits, including these, which are associated with the following programs: Core Quality Measures Collaborative (Collaborative), the Integrated Healthcare Association’s California Value Based P4P Program (IHA), and the National Committee for Quality Assurance’s Healthcare Effectiveness Data and Information Set (HEDIS). Measures used by the Medicare Shared Savings Program (MSSP) 2018 and 2019 reporting years are also listed.
HOW TO CODE FOR MEDICARE WELLNESS VISITS
The type of wellness visit you report depends on when the patient joined Medicare.
The IPPE is a one-time physical exam performed within the first 12 months of a patient’s enrollment under Part B Medicare. The initial AWV can be provided 12 months after the patient first enrolled or 12 months after he or she received the IPPE. A subsequent AWV can then be provided annually.
Physicians should bill for preventive services provided in addition to the AWV or IPPE, many of which carry work relative value units (wRVUs) that can affect their productivity scores and revenue. Some of these services are payable by Medicare in addition to the AWV or IPPE and can be performed several times during the year. However, patients and physicians should be aware that a few of these services do have a copay or deductible. (See “ Medicare-covered preventive services .”)
MEDICARE-COVERED PREVENTIVE SERVICES
This table includes preventive services that generate work relative value units (wRVUs). For a complete list of Medicare preventive services, see https://go.cms.gov/2sK65XA .
If you provide advance care planning (ACP), CPT code 99497 or 99498, at the same visit, make sure to append modifier 33, “Preventive service,” so that the usual coinsurance and deductible charged for the ACP is waived. 5 You may need to append modifiers to other preventive service codes as well, to avoid bundling. Practices should check with their Medicare contractor for guidance.
To find out how many wRVUs a particular service is worth, see the 2019 Medicare Physician Fee Schedule ) or the wRVU calculator provided by the American Academy of Professional Coders.
Below are some examples of wellness visits and the wRVUs resulting from each one.
Patient 1 : A 67-year-old male, who is an established patient of your practice, is seeing you for an initial AWV. His chronic problems include hypertension and dyslipidemia. He is taking hydrochlorothiazide 25 mg per day and atorvastatin 20 mg at bedtime. His history and the health risk assessment he completed confirm he has smoked one pack of cigarettes per day for 34 years. He does not have an advance directive. He rarely drinks alcohol, and his PHQ-2 depression screening score is zero. His vital signs are stable with good blood pressure control. His BMI is 33.7. He requests a digital rectal exam (DRE) because his father had prostate cancer. You create the patient’s personalized prevention plan and discuss your clinical recommendations with the patient, who agrees to receive several preventive services, including a lipid panel, diabetes screening, hepatitis C screening, lung cancer screening with a low-dose CT scan, a pneumococcal vaccination, a DRE, and AAA screening with ultrasound. You order the labs and imaging, provide counseling focused on several of the patient’s health risk behaviors, and recommend a follow-up visit in six months or sooner if needed to address test results.
Patient 2 : A 77-year-old female, who is an established patient of your practice, is seeing you for her first AWV. She has a Medicare Advantage insurance plan. Her previous office visit was about nine months ago. She has diabetes, hypertension, peripheral neuropathy, glaucoma, mild major depression, anxiety, and COPD. She is due for her routine lab work and is requesting refills of all her medications. She would like a flu shot, but the rest of her immunizations are current. Her list of medications includes metformin 500 mg twice a day, sitagliptin 50 mg daily, lisinopril 10 mg daily, gabapentin 300 mg three times per day, albuterol as needed, tiotropium daily, alprazolam 0.25 mg daily as needed, sertraline 50 mg daily, and dorzolamide ophthalmic twice a day. She has tried in the past to wean herself off the alprazolam but needs it to control her anxiety; she fills her prescription for 30 pills every three or four months, which you confirm via a controlled substance prescription database. Her history, along with her health risk assessment, shows she drinks up to three glasses of wine per day. She does not have an advance directive. Her vital signs are stable with good blood pressure control, and her BMI is 22.4. You address her concerns and order labs appropriate to her chronic medical conditions, refill her medications, order a flu shot, provide counseling related to her health risk behaviors, and discuss your preventive service recommendations as part of her personalized prevention plan, which includes ordering a DEXA scan.
Given the complexity of her health status, you ask her to schedule a follow-up appointment in one week to go over her lab results. Also, because the patient is a Medicare Advantage beneficiary, you remember to assess and report risk-adjusted diagnoses and HCC codes.
Patient 3 : A 57-year-old female, who is an established patient of your practice, recently became disabled. She now has dual insurance coverage with Medicare and Medicaid. She is scheduled for her “Welcome to Medicare” visit. She was seeing a partner of yours who recently retired, and she has transferred to you for care. Her last visit was four weeks ago, and her diabetes lab work at that time showed that her A1C was 6.7 and her LDL was 94. She had her annual eye exam two months ago. She has diabetes, hypertension, and end-stage renal disease (ESRD). Her list of medications includes insulin glargine 10 units at bedtime, insulin aspart on a sliding scale, amlodipine 5 mg daily, and pravastatin 10 mg at bedtime. Her history, along with her health risk assessment, shows that she has multiple sex partners. She does not drink alcohol and does not smoke. Her PHQ-2 depression screening is 0. Her last mammogram was three years ago, and her last Pap smear was six years ago. She has not received her pneumococcal vaccine. She has never had a colonoscopy or fecal occult blood testing. Her vital signs are stable with good blood pressure control and a BMI of 27.1. She has been feeling sick for the last two weeks with sinus infection symptoms. You treat her for a sinus infection, perform a gynecologic exam and Pap smear, and update her pneumococcal vaccination. You discuss and then order screens for hepatitis B, hepatitis C, HIV, and sexually transmitted infections (STIs), in addition to a mammogram. You also agree to make referrals for a colonoscopy and medical nutrition therapy for ESRD. Finally, you ask her to follow up in four to six months or as needed.
MEETING THE CHALLENGE
Providing wellness visits is not easy, but there are ways to make your practice more prepared. For example, a nurse or medical assistant could handle pre-visit planning to make the physician-led visit more efficient. 6 Another variation of the team-based model, which used a dedicated scheduler to contact Medicare patients about AWVs and then clinical pharmacists and licensed practical nurses to provide the visits, significantly increased use of preventive services. 7 It may also be worthwhile to set aside more time for these types of visits. While some visits can be completed in 30 to 40 minutes, more complicated encounters may take longer. Your EHR may also have templates and other tools available to make providing Medicare wellness visits more efficient, although the range of EHR capabilities is too wide to discuss here.
Regardless of how you schedule and perform these visits, you should recognize that Medicare wellness visits have great value in not only providing important preventive services to the patient but also closing quality measure gaps and contributing financial stability to a practice or organization.
Ganguli I, Souza J, McWilliams JM, Mehrotra A. Trends in use of the U.S. Medicare annual wellness visit, 2011–2014. JAMA . 2017;317(21):2233-2235.
Ganguli I, Souza J, McWilliams JM, Mehrotra A. Practices caring for the underserved are less likely to adopt Medicare’s annual wellness visit. Health Aff (Millwood) . 2018;37(2):283-291.
CMS. Annual wellness visit, including personalized prevention plan services. MLN Matters . March 2, 2016. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/Downloads/MM7079.pdf . Accessed Jan. 30, 2019.
CMS. Medicare Shared Savings Program: Quality Measure Benchmarks for the 2018 and 2019 Reporting Years, Guidance Document . December 2017. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/2018-and-2019-quality-benchmarks-guidance.pdf . Accessed Jan. 30, 2019.
CMS. Advance care planning. MLN Matters fact sheet. June 2018. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/AdvanceCarePlanning.pdf . Accessed Jan. 30, 2019.
Cuenca AE. Making Medicare annual wellness visits work in practice. Fam Pract Manag . 2012;19(5):11-16.
Galvin SL, Grandy R, Woodall T, Parlier AB, Thach S, Landis SE. Improved utilization of preventive services among patients following team-based annual wellness visits. NC Med J . 2017;78(5):287-295.
Continue Reading
More in FPM
More in pubmed.
Copyright © 2019 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

IMAGES
VIDEO
COMMENTS
"WelcoMe To MedIcare" prevenTIve vIsIT overvIeW The "Welcome to Medicare" preventive visit provides you with an accurate benchmark of a patient's overall health. ... For more information about proper billing and coding,please refer to the Medicare learning network article, which is available at .
Annual Wellness Visit (AWV) Visit to develop or update a personalized prevention plan and perform a health risk assessment. Covered once every 12 months. Patients pay nothing (if provider accepts assignment) Routine Physical Exam. Exam performed without relationship to treatment or diagnosis of a specific illness, symptom, complaint, or injury.
Along with settling on a new routine for the Welcome to Medicare exam, you'll also want to make sure you understand its billing requirements. For a complete overview, see "New Year, New ...
The Initial Preventive Physical Examination (IPPE) is also known as the "Welcome to Medicare Preventive Visit.". The IPPE is a preventive visit offered to newly-enrolled Medicare beneficiaries ...
2. Billing for a Medicare AWV when the patient only has Medicare Part A. They must have Part B coverage as well. 3. Using the wrong primary diagnosis code. If the primary diagnosis code is problem ...
The Welcome to Medicare checkup is optional, but it serves as a baseline for monitoring your health during the annual wellness visits that Medicare will pay for in subsequent years. You do not need this checkup to qualify for later annual wellness visits, but Medicare won't pay for a wellness visit during your first 12 months in Part B.
The "Welcome to Medicare" visit is a one-time-only preventative health care visit covered by Medicare Part B. It is not the same as a routine physical exam or annual Medicare Wellness visit. The Welcome to Medicare visit is an introduction to Medicare and focuses on disease prevention and detection to help beneficiaries live a healthier life.
The Welcome to Medicare preventive visit is a one-time appointment you can choose to receive when you are new to Medicare. The aim of the visit is to promote general health and help prevent diseases. Eligibility. Medicare Part B covers your one-time Welcome to Medicare preventive visit. Note that you must receive this visit within the first 12 months of your Part B enrollment.
Understanding HCPCS G0439. HCPCS G0439 is used to code all subsequent Medicare annual wellness visits that occur after the initial AWV (G0438). So, if used correctly, G0439 would not be used until G0402 was used to code the IPPE and G0438 was used to code the initial AWV. In the case that an IPPE was never completed, G0439 would still be used ...
Initial Preventive Physical Examination. The Affordable Care Act provides for an initial preventive physician exam (IPPE) also known as the "Welcome to Medicare" preventative visit, for Medicare beneficiaries as of January 1, 2011. Medicare pays for one IPPE visit per lifetime that must be completed no later than 12 months after the patient's ...
Learn 2023 CPT billing codes for annual wellness visits (AWVs) and understand requirements to maximize the value of G0402, G0438, G0439, 99497, and G0468. ... Commonly referred to as the "welcome to Medicare visit," it is considered a once in a lifetime assessment and after the initial eligibility period, the patient cannot receive an IPPE. ...
HCPCS Code Code Descriptor. G0402. Initial preventive physical examination; face-to-face visit, services limited to new beneficiary during the first 12 months of Medicare enrollment. G0403. Electrocardiogram, routine ECG with 12 leads; performed as a screening for the initial preventive physical examination with interpretation and report.
The "Welcome to Medicare" visit takes place during the first year of a person's Medicare coverage. It offers the individual an opportunity to discuss their state of health with their doctor ...
Physicians must append modifier -25 (significant, separately identifiable service) to the medically necessary E/M service, e.g. 99213-25, to be paid for both services. For example, for the patient who comes in for his Annual Wellness Visit and complains of tendonitis would be billed as follows: CPT ICD9, G0438 V70.0, 99212-25 726.90 (tendonitis)
An initial preventive physical exam (IPPE, or Welcome to Medicare visit) is a one-time physical exam performed within the first 12 months of a patient's Part-B enrollment. An initial annual ...
Annual Wellness Visit. The Annual Wellness Visit (AWV) is a yearly appointment with your primary care provider (PCP) to create or update a personalized prevention plan. This plan may help prevent illness based on your current health and risk factors. Keep in mind that the AWV is not a head-to-toe physical.
• Known as the Welcome to Medicare preventive visit • Original Medicare covers IPPE for patients newly enrolled in Medicare part • Allowed only within first 12 months after effective date of Medicare Part coverage • One-time benefit covered by Humana Medicare Advantage (MA) plans Annual Wellness Visit • Unique to Medicare
Advance care planning is a billable, face-to-face service between a physician (or nurse practitioner, physician assistant, or clinical nurse specialist) and a patient and/or surrogate (e.g., health care agent, designated decisionmaker, family member, or caregiver) to discuss and make known the patient's health care wishes in case the patient becomes unable to make health care decisions for ...
Patients with Medicare Part B are entitled to a free "Welcome to Medicare" visit, also called an Initial Preventive Physical Examination (IPPE, code G0402), in their first 12 months of coverage.
1 Centers for Medicare & Medicaid Services, CY 2024 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program ...
What it is. Preventive services help you stay healthy, detect health problems early, determine the most effective treatments, and prevent certain diseases. Preventive services include exams, shots, lab tests, and screenings. They also include programs for health monitoring, and counseling and education to help you take care of your own health.
Welcome to your Medicare Advantage Plan! Thank you for being a Wellcare member! We want to help you get the most from your plan. Use our website to explore plan information and benefits and review helpful plan documents such as the Evidence of Coverage, Summary of Benefits, and Annual Notice of Change.
More than half of denied claims (51.7%) were eventually overturned and paid. Private payers overturned denials at a higher rate (54.3%) than Medicare and Medicaid (47.9%).
KEY POINTS. The Medicare annual wellness visit (AWV) and the initial preventive physical examination (IPPE) provide a number of benefits to patients and physicians, but many physicians still do ...