How Prisons in Each State Are Restricting Visits Due to Coronavirus
As COVID-19 began spreading in 2020, prison facilities across the country suspended visits from family and lawyers. Over the course of the pandemic, states have eased and tightened those restrictions. We’re rounding up the changes as they occur.
Have you tried to visit a person in prison or jail recently? Tell us about it here.

Regular visits suspended, but legal visits allowed
Personal visits have been suspended since March 13, 2020, but legal visits are allowed.
Learn more from Hawaii →
Personal visits are suspended in all of Vermont's prisons due to active cases among staff or the incarcerated after they had been reopened in July of 2021. They were initially suspended in response to coronavirus on March 13, 2020, but legal visits were allowed.
Learn more from Vermont →
Personal visits have been suspended since March 11, 2020, but legal visits are allowed.
Learn more from West Virginia →
Personal visits were suspended March 18, 2020. Lawyers are allowed access, but may not have physical contact with prisoners and can only meet through phone or video calls. In the summer of 2021, Wyoming resumed in-person visits only to halt them again amid coronavirus outbreaks.
Learn more from Wyoming →
Visits resumed with limitations
On Oct. 9, 2021, Alabama began to reopen a small group of prisons for limited visitation, and the rest . All visitation had been suspended starting March 13, 2020.
Learn more from Alabama →
On April 30, 2021, Alaska reopened most of its prisons to visitors with some restricitons, including mandating the wearing of masks. All visitation, including legal visits, were suspended on March 13, 2020. On March 17, 2021, in-person visits with attorneys resumed.
Learn more from Alaska →
On June 19, 2021, Arizona began to reopen its prisons to visitation for vaccinated prisoners. Personal visits had been suspended since March 13, 2020, and legal visits were stopped as well.
Learn more from Arizona →
All visitation, including legal visits, was suspended on March 16, 2020. In December, Arkansas reopened for some visits but closed again within a few weeks. On March 6, 2021, limited visits resumed in four facilities and later expanded in June to all prisons.
Learn more from Arkansas →
The California Department of Corrections and Rehabilitation resumed in-person visits on April 10, 2021. Wardens of individual prisons could determine whether to reopen based on the number of active caess at their faciliites. Normal visitation was first suspended on March 13, 2020, and legal visits on April 7.
Learn more from California →
On May 4, 2021, Colorado began to allow limited visitation at some of its facilities and expanded it across the system later in the month. In October 2021, the state began to require visitors to show proof of vaccination before being allowed to enter the prisons. Personal visits were initially suspended on March 11, 2020. Legal visits are allowed, but they will be non-contact visits.
Learn more from Colorado →
Personal visits were suspended on March 13, 2020. Legal visits were allowed, but officials strongly recommend communicating by phone instead. On Oct. 15, 2020, Connecticut began to resume limited, pre-scheduled, non-contact visits .
Learn more from Connecticut →
Personal visits resumed on March 16, 2021, with restrictions . Visitation was first suspended on March 12, 2020. Visits resumed briefly in late June and then again in early September, but in November, they were stopped amid rapidly increasing spread of the coronavirus in the state.
Learn more from Delaware →
Washington, D.C., sends its prisoners to the Federal Bureau of Prisons, where all visitation, including legal visits, were suspended on March 13, 2020, though attorneys could be approved for an in-person visit on a case-by-case basis. On Oct. 3, some federal prisons began to reopen for non-contact personal visits, with restrictions .
Learn more from District of Columbia →
Personal visits were suspended on March 11, 2020, but legal visits were allowed. On Oct. 2, Florida began to allow limited visits with some restrictions .
Learn more from Florida →
All visitation, including legal visits, were suspended on March 13, 2020. On April 3, 2021, personal visits resumed with restricitons, such as one visit per prisoner every other month.
Learn more from Georgia →
On June 12, 2021, personal visits began to resume at some Idaho prisons. They had been suspended since March 13, 2020. Legal visits were allowed, but officials strongly recommended communicating by phone instead.
Learn more from Idaho →
On April 12, 2021, limited visitation resumed at one prison in Illinois and expanded to more than 10 additional facillities a week later. Personal visits were initially suspended on March 14, 2020.
Learn more from Illinois →
Non-contact personal visits began again on Aug. 30, 2021 after being suspended since March 11, 2020. Legal visits had been allowed, but attorneys were screened upon arrival for contact visits.
Learn more from Indiana →
Personal visits resumed on July 10, 2021 after being suspended since March 14, 2020. Legal visits were allowed during the suspension.
Learn more from Iowa →
Personal visits resumed in Kansas on April 18, 2021 with limitations, after being suspended since March 12, 2020. Legal visits had been allowed, but officials strongly recommend communicating by phone or in writing.
Learn more from Kansas →
Limited personal visits began again on June 21, 2021, after being suspended since March 14, 2020. Legal visits had been allowed, but non-contact visits were strongly encouraged and attorneys could be screened upon arrival.
Learn more from Kentucky →
Louisiana began to allow personal visits in its prisons on Oct. 18, 2021. They had been halted on on July 27, 2021 after reopening in March, one year after they were originally suspended due to the coronavirus on March 12, 2020.
Learn more from Louisiana →
Personal visits were suspended on March 12, 2020, but legal visits were allowed. Limited, non-contact visits resumed in several Maine prisons on March 18, 2021. Visits had begun in July of 2020 but were suspended again on Nov. 1.
Learn more from Maine →
Maryland's Department of Public Safety and Correctional Services began to permit personal visits on July 19, 2021. Personal visits had been suspended since March 12, 2020, but legal visits were allowed.
Learn more from Maryland →
On May 1, 2021, Massachusetts began to reopen visitation at three prisons , with more added in the following days. Personal visits were first suspended on March 13, 2020 and resumed with limits in July. On Nov. 14, 2020, the prisons again halted visits amid rising coronavirus cases. Legal visits were allowed.
Learn more from Massachusetts →
Personal visits were suspended on March 13, 2020, but legal visits were allowed. On March 26, 2021, limited personal visits resumed at some Michigan prisons that were not in quarantine .
Learn more from Michigan →
Personal visits were suspended on March 12, 2020. Legal visits were allowed, but they will not be face-to-face visits. On July 22, 2020, the state resumed limited personal visits at prisons that did not had two positive cases in the previous two weeks. On Nov. 30, the last prison was closed to visitors due to a rise in cases. On Jan. 6, 2021, visitation resumed at some Minnesota prisons.
Learn more from Minnesota →
Mississippi reopened its prisons for personal visits on Nov. 1, 2021. They had been barred originally on March 12, 2020 and had resumed in May of 2021, only to have them stopped again in late July 2021 due to rising concerns about the delta variant of the coronavirus.
Learn more from Mississippi →
Personal visits for prisoners who are fully vaccinated resumed on June 1, 2021. They had initially been suspended March 12, 2020, but legal visits were allowed. On June 25, 2020, visits resumed with some precautions , and as many as five prisons at a time reopened through the summer and fall. On Dec. 30, 2020, visits were suspended in all prisons while the rollout of vaccines began.
Learn more from Missouri →
On April 24, 2021, Montana began to reopen its prisons with some restrictions, including requiring visitors to wear masks. Personal and legal visits were suspended on March 13, 2020.
Learn more from Montana →
On Dec. 15, 2020, limited visitation resumed at five prisons and at all facilities on Jan. 6. Personal visits were first suspended on March 16, 2020. Legal visits were allowed, but attorneys were screened on entry. On July 15, a limited number of non-contact visits began for those who pre-registered, but visits were again suspended on Aug. 7 .
Learn more from Nebraska →
On May 1, 2021, Nevada reopened its prisons to visitors , with limits on capacity. All visitation, including legal visits, had been suspended since March 7, 2020.
Learn more from Nevada →
All visitation, including legal visits, were suspended on March 16, 2020. Starting on Aug. 10, limited personal and attorney visits resumed .
Learn more from New Hampshire →
New Jersey began to allow limited outdoor visits on May 1, 2021 and later expanded to indoor visits. Personal visits were originally suspended on March 10, 2020, but legal visits were allowed. On Oct. 9, 2020, outdoor visits resumed but were then suspended again on Dec. 8.
Learn more from New Jersey →
On June 14, 2021, New Mexico reopened limited, non-contact visits for vaccinated prisoners and vaccinated visitors. All visits, including contact, non-contact and legal visits had been suspended since March 16, 2020.
Learn more from New Mexico →
On April 28, 2021, New York's Department of Corrections and Community Supervision resumed non-contact personal visits, starting with maximum security prisons. Visitation was originally suspended on March 14, 2020 though legal visits were allowed. On Aug. 6, 2020 visitation began to resume , but on Dec. 30, personal visits were stopped again at all prisons statewide.
Learn more from New York →
Personal visits were suspended on March 13, 2020, but legal and pastoral visits were allowed. On Oct. 1, North Carolina began to allow visits with significant restrictions .
Learn more from North Carolina →
All contact visits were suspended on March 12, 2020. Visits began in June of 2020 and were later suspended in July. On March 29, 2021, visits resumed.
Learn more from North Dakota →
Personal visits were suspended on March 12, 2020. Legal visits were allowed, and attorneys were screened on entry. On July 8, outdoor visits began at some prisons. By Oct. 30, however, all of the prisons were closed to visitors again. On Feb. 16, 2021 visitation resumed at some facilities.
Learn more from Ohio →
Visitation was suspended on March 13, 2020, and legal visits were allowed. Limited visitation resumed in June 5, but was later cancelled again amid another wave of infections in the fall. Oklahoma reopened for visits with restrictions on April 1, 2021.
Learn more from Oklahoma →
All visitation, including legal visits, were suspended on March 12, 2020. On March 29, 2021, Oregon began a pilot program allowing limited, non-contact visits at one prison but later halted the program on April 28, 2021. The program began again on June 14, 2021 and expanded to other facilities.
Learn more from Oregon →
Personal visits began to resume in Pennsylvania prisons on May 22, 2021. They had been suspended since March 13, 2020, but legal visits are allowed. Legal visitation was suspended for one day, March 13.
Learn more from Pennsylvania →
On April 14, 2021, Rhode Island's Department of Corrections resumed non-contact visits with some restrictions . All visitation, including legal visits, had been suspended on March 11, 2020. On Aug. 12, visits with attorneys resumed.
Learn more from Rhode Island →
Personal visits began to resume for vaccinated prisoners at some South Carolina prisons on June 19, 2021. They had been suspended since March 13, 2020, but legal visits were allowed.
Learn more from South Carolina →
Visitation was suspended since March 12, 2020, but legal visits were allowed. On March 8, 2021, non-contact personal visits started again , with new restrictions and health guidelines.
Learn more from South Dakota →
On April 10, 2021, the Tennessee Department of Correction reopened for limited visitation . Personal visits were suspended on March 12, 2020, as were legal visits, though wardens could grant special requests for in-person access. On Oct. 3, 2020, Tennessee reopened three prisons for limited visitation and later a fourth. On Dec. 1, 2020, visitation at all prisons was again suspended .
Learn more from Tennessee →
Personal visits were suspended on March 13, 2020. On March 15, 2021, personal visits began again, with restrictions . Visitors must take a rapid coronavirus test before being admitted.
Learn more from Texas →
Personal visits began again on June 18, 2021. They had been suspended since March 12, 2020. Non-contact legal visits were allowed.
Learn more from Utah →
On Sept. 1, 2021, Virginia began to open some of its prisons to outside visitors, starting with nine facilities and later expanding to more. Personal visits had been suspended since March 13, 2020, as were attorney visits, which resumed July 15, 2021.
Learn more from Virginia →
Non-contact personal visits resumed on May 9, 2021. They had been suspended since March 12, 2020, but legal visits were allowed.
Learn more from Washington →
On July 6, 2021, Wisconsin resumed personal visits , which had been suspended since March 13, 2020.
Learn more from Wisconsin →
All visitation, including legal visits, were suspended by the Federal Bureau of Prisons on March 13, 2020, though attorneys could be approved for an in-person visit on a case-by-case basis. On Oct. 3, some federal prisons began to reopen for non-contact personal visits, with restrictions .
Learn more from Federal →
This is produced in partnership with the Associated Press.
Sources State prison systems
Graphic by Katie Park and Tom Meagher
Reporting by Cary Aspinwall, Keri Blakinger, Jake Bleiberg, Andrew R. Calderón, Maurice Chammah, Andrew DeMillo, Eli Hager, Jamiles Lartey, Claudia Lauer, Nicole Lewis, Weihua Li, Humera Lodhi, Colleen Long, Tom Meagher, Joseph Neff, Alysia Santo, Beth Schwartzapfel, Damini Sharma, Colleen Slevin, Christie Thompson, Abbie VanSickle and Andrew Welsh-Huggins
Additional development by Gabe Isman

- Our Mission
- Our Sponsors
- Editorial Independence
- Write for The Crime Report
- Center on Media, Crime & Justice at John Jay College
- Journalists’ Conferences
- John Jay Prizes/Awards
- Stories from Our Network
- TCR Special Reports
- Research & Analysis
- Crime and Justice News
- At the Crossroads
- Domestic Violence
- Juvenile Justice
- Case Studies and Year-End Reports
- Media Studies
- Subscriber Account

Captives Behind Plexiglass: How COVID Destroyed Prison Visits

Every Saturday morning, private buses drop off groups of people at prisons across New York State.
Women and children, mostly, leave the city in the dead hours of night and travel on these buses for six hours or longer only to wait sometimes for three or more hours to get inside the facility to see their loved ones.
The waiting area usually consists of a dreary small room or trailer encircled with uncomfortable plastic chairs where a few officers approve who will enter the facility.
Often, women are turned away for outfits deemed “too tight” and forced to change.
Most of the time, the outfits they wear are perfectly appropriate. Yet, in these instances, the need to display such power destroys the ability to extend any fairness. Those who have been visiting for a long time come prepared, stashing extra shirts and pants in the duffel bags they shove into lockers that line the back wall.
However, some women do not know yet to plan ahead and must find a nearby store to buy new clothes they hope the officers will find acceptable. Once they pass this “test,” they then sit with the others until they hear their number called, very similar to the dreadful wait at the DMV.
When they are finally called inside, they have to fill out a form, have their picture taken, and walk through a metal detector, another opportunity when they can get turned away. The experienced visitors will wear a bra without underwire and pass through the metal detector with ease. Others will have to enter a changing room, remove their bra, and walk through again.
If the metal detector remains silent, they can then head over to the visiting room.
In a room that resembles a school cafeteria, a few officers sit behind a desk and monitor the interactions. “Stop kissing, stop holding hands, stop hugging” are all common commands during a contact visit that can range anywhere from one hour to six, depending on the facility.
In the case of a no-contact visit, a metal gated partition like a fence will separate visitors from their loved ones.
Despite the strict rules, rigid officers, and long commute, most women find all of these hassles worth the trouble in order to sit face-to-face with their loved ones, to touch them, to share vending machine snacks, to play board games or cards together, and to briefly hug and kiss in the beginning and end of the visit.
These few hours of PG-13 intimacy breathe life and love into relationships that otherwise exist through email, video, or the phone.
However, in March 2020, the COVID-19 pandemic caused prison visiting rooms across the country to shut down, creating a stressful disconnect that would last for the next 14 months, and in some states, even longer.
In an interview with The Crime Report, Cecilia Conley, CEO of the social media enterprise Designed Conviction and wife of an inmate serving a life sentence in Washington State lamented that the last time she saw her husband in-person was on March 6, 2020.

Although Washington has begun to allow in-person visits, they are heavily restricted. Visitors and their incarcerated loved ones must sit behind a plexiglass partition to prevent them from kissing, hugging, and even holding hands. The visits must also be scheduled and approved in advance and only last for one hour.
“They opened visitation, but they have a plexiglass, and you have to be seated in front of them with a mask,” Conley explains. “So, for me, if you go there and they cannot even touch you, that’s torture for me; so we prefer to just stick with the video visits because at least we can be wearing no mask, and it will be almost the same thing.
“They’re very strict there, so we don’t like that.”
While Washington allowed video visits prior to the pandemic, New York has yet to have that option, which forced incarcerated people and their loved ones to rely on only letters, emails, and phone calls to stay connected.
Donna Sorge shared the experience she endured with her significant other while he was incarcerated in Green Correctional Facility, located in Coxsackie, N.Y.
“We were on the phone as much as possible and we would email a bunch of times during the day, so it wasn’t like we felt so out of connect, but a lot of people don’t have that luxury,” she said in an interview.
“They don’t email that much, or the guys don’t get on the kiosk that much, or they don’t get the phones as much. In some places like Attica, they might get a 15-minute phone call every other day.”
Prior to the pandemic, Sorge would visit her loved one every weekend; but for most of 2020, she had to rely on these other forms of communication, which she explains took a toll on her relationship.
“It’s a huge impact on us because one of the main ways we communicate is actually seeing them,” she continued. “I mean, we can talk on the phone, we can write, and email, but it’s not the same as going there and spending time with them.”
In Conley’s case, prior to the pandemic, not only would she get to see her husband face-to-face in the facility’s visiting room; but she was allowed to have overnight family visits with him.
“Last year, before the pandemic, I got to spend the night with him,” Conley recalled.
“He would cook for me, we would sleep together, take a shower, watch TV, like in privacy, which was really nice…Now they canceled it, which is stupid.”
Conley went on to express her frustration, stating, “I wish DOC would’ve managed this better. There’s enough science and tools that they could have used to allow us to see our loved ones earlier.”
She added: “I mean, my husband and I are fully vaccinated, and I’m sure there are a lot of guards that are not even vaccinated, so for me, it’s safer to go there than the guards. So, I don’t understand why I cannot see him.”
In New York, overnight family visits are also allowed―but were canceled during the pandemic.

However, since Sorge and her partner are not married, they never had the option to participate in these kinds of visits.
Instead, they would rely on spending time with each other in the visiting room. When facilities closed their doors to outsiders, she explained, “just not being able to see him is stressful because I can have better conversations and get more information from him when I see him in person as opposed to being on the phone.”
Since April 2021, New York has reopened their visiting rooms, but there are still many restrictions.
Sorge recalls her experience, stating, “We obviously weren’t able to kiss. We had to wear masks the whole time unless we were eating or drinking, and they do enforce it…we just made sure we were eating and drinking something, so we didn’t have to have the masks on the whole time.”
While Washington has been moving in the direction of allowing contact visits sometime this summer, Conley has chosen to continue to rely on video visits with her husband as frequently as possible, despite the many drawbacks.
Conley describes it this way:
Conley describes, “We utilize
visits more but there are some times that either the video visit does not work or there would be low quality. As soon as the pandemic started [they were also] more strict with them. So, it really is stressful.”
However, she remains hopeful that she will see her husband in person soon.
“Of course, I want to see him. I want to share a bag of chips and spend the night with him, and I know it’s gonna happen. The state’s opening today, so I hope that by next month, hopefully, I can go see him, so I’m very excited about that.”
Sorge also maintains a sense of optimism despite the heightened degree of separation from her loved one the pandemic caused.
“It’s either going to do one of two things. It’s either going to make you stronger or it’s going to make it harder.”
In her case, her relationship ended up stronger since she was able to welcome her significant other home only a few weeks ago after standing by his side for the last 17 years.
While Sorge has been reunited with her loved one and now has a new start, many people do not share that reality, and are still deeply impacted by the aftermath of the pandemic that continues to alter facility rules.
One concern many people have is the possibility of facilities phasing out in-person visits all together. With the over-use of video visits during this past year many fear that this will become the only option to see their loved ones.
“I fear that a lot. And I fear that now they want to keep that plexiglass,” Conley said. “Of course, it scares me…I think the only reason why it hasn’t been enforced is because the families are fighting for that not to happen, but of course, that sometimes makes me stay up at night because I don’t know what I would do.
“My relationship would be 100 percent impacted by that.”
Although prison staff and law enforcement officials often claim video visits prevent the spread of contraband within the facility and are easier to monitor, that cannot be further from the truth. According to a study conducted by Prison Policy Initiative in 2018 , nearly all reported cases involved jail workers, rather than visitors.
Specifically, “20 jail workers in 12 jails were arrested, indicted, or convicted of smuggling (or planning to smuggle) goods into their cell blocks,” and most of the 12 jails involved had recently banned in-person visits and replaced them with video calls.
However, worst of all, relying only on video visits rob people of the opportunity to experience a true physical connection that cannot be replicated through a screen.
“They’re human and they need human contact,” Conley emphasized.
When incarcerated people have in-person interactions with their loved ones, even briefly, they are provided with a sense of normalcy and a renewal of hope that would be lost otherwise. Such a loss would only negatively impact their rehabilitation process.
Despite the unnecessary cruelty that goes along with banning in-person visits, many jails across the United States have executed this change. According to a 2015 study from the Prison Policy Initiative, 13 percent of local jails – about 500 in 43 states – have implemented video calling, with 74 percent also prohibiting in-person visitation.
Broward County Sheriff’s Office in Florida even tries to make video calls sound more appealing than having the opportunity to hug and kiss loved ones by exclaiming on their website:
Avoid long lines, scheduling conflicts, and provide a better environment for children to interact with a family member. Video visitation is an easier way to spend time with a loved one in custody at one of our jails.
However, when it comes to a child hugging his or her mother, a wife kissing her husband, or a mother holding the hand of her son, do the prison officials mandating these rules truly believe long lines or scheduling conflicts matter? In fact, the emotional toll of physically separating loved ones for indefinite periods of time cancels out any convenience video visits may offer.
While the fear of facilities phasing out in-person visits for good will always linger in the background due to advancements in technology, as of now, many prisons have begun to open their doors to outsiders.
This in turn has brought new concerns regarding longer lines and wait times to enter once restrictions are completely lifted.

Conley expressed her mixed emotions of excitement and worry succinctly.
“There’s going to be a lot of people making a line to go see their loved ones because we haven’t gone in for a long time. But other than that, when I’m there, I don’t know, I haven’t thought about it. It’s going to be nice.”
Maria DiLorenzo, based in Brooklyn, NY, has written for various publications, including the Alaska Quarterly Review, the Flea, Real Crime, and VTPost.com. She is currently working on a true crime novel about the life and crimes of Maksim Gelman, and recently started a blog called Beyond the Crime, which shares stories of those incarcerated for murder to gain a deeper understanding of criminal behavior and the criminal justice system.
Related Posts
Silent strength: my time as a prisoner’s wife turned advocate, reclaimed identity: keith jesperson’s sixth murder, mississippi regularly fails to investigate rampant abuses by sheriff’s and their departments, leave a reply cancel reply.
Save my name, email, and website in this browser for the next time I comment.

- Reporting Awards
- Events/Fellowships
- Send Us Tips
- Republish Our Stories
Type above and press Enter to search. Press Esc to cancel.

An official website of the United States government, Department of Justice.
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Impact of COVID-19 on State and Federal Prisons, March 2020–February 2021
This report provides details on the effects of COVID-19 on state and federal prisons from March 2020 to February 2021. The report presents data related to COVID-19 tests, infections, deaths, and vaccinations. It also provides statistics on admissions to and releases, including expedited releases, from state and federal prisons during the first year of the COVID-19 pandemic.
- BJS’s survey to measure the impact of COVID-19 on U.S. prisons from the end of February 2020 to the end of February 2021 found that the number of persons in the custody of state, federal, or privately operated prisons under state or federal contract decreased more than 16%.
- The prison population declined by 157,500 persons during the first 6 months of the COVID-19 study period through the end of August 2020, and by 58,300 in the 6 months through the end of February 2021.
- Twenty-four states released a total of 37,700 persons from prison on an expedited basis (earlier than scheduled) during the COVID-19 study period.
- State and federal prisons had a crude mortality rate (unadjusted for sex, race or ethnicity, or age) of 1.5 COVID-19-related deaths per 1,000 prisoners from the end of February 2020 to the end of February 2021.
- From the end of February 2020 to the end of February 2021, a total of 196 correctional staff in state and federal prisons died as a result of COVID-19.
Additional Details
- Press Release, (PDF 191K)
- Summary, (PDF 184K)
- Full report, (PDF 1.4M)
- Data tables, (Zip format 45K)
Related Datasets
- National Prisoner Statistics (NPS) Program
- National Corrections Reporting Program (NCRP)
- 2020-2021 NACJD Data for National Prisoner Statistics Program - Coronavirus Pan…
Related Topics
Similar publications.
- Jails in Indian Country, 2021, and the Impact of COVID-19, July–December 2020
- Methodology: Survey of Prison Inmates, 2016
- PREA Data Collection Activities, 2015
- Skip to main content
- Keyboard shortcuts for audio player
Investigations
As covid spread in federal prisons, many at-risk inmates tried and failed to get out.

Meg Anderson
Huo Jingnan

Waylon Young Bird was at the U.S. Medical Center for Federal Prisoners in Springfield, Mo., when he applied for a compassionate release from prison in the spring of 2020. He was worried about the coronavirus pandemic and had underlying medical conditions, including late-stage kidney disease. John S. Stewart/AP hide caption
Waylon Young Bird was at the U.S. Medical Center for Federal Prisoners in Springfield, Mo., when he applied for a compassionate release from prison in the spring of 2020. He was worried about the coronavirus pandemic and had underlying medical conditions, including late-stage kidney disease.
In a federal prison in Springfield, Mo., Waylon Young Bird quietly wrote a letter to a federal judge.
"Greetings sir, just a quick letter concerning the pandemic of the coronavirus," Young Bird wrote. "Many of us are at high risk of getting this virus because of our health conditions, the overcrowding conditions here and the uncleanliness of this prison medical center."
It was March 15, 2020. That day, New York City announced it was shutting down its public schools , Dr. Anthony Fauci went on network television to prepare Americans to "hunker down significantly," and states began closing their bars and restaurants. It was beginning to dawn on many people that something life-altering was already happening. And it was dawning on Young Bird too.
He had been in the Medical Center for Federal Prisoners in Springfield since the previous September, sentenced to 11 years for charges related to dealing methamphetamine. On April 5, 2020, he wrote again.
"If given the chance I will prove I can stay out of trouble and follow the rules and conditions set for me," Young Bird wrote to Chief Judge Roberto Lange of the U.S. District Court for the District of South Dakota, where he was sentenced. "I'm not a bad person. I just made a few bad decisions in my life."
Young Bird was in his early 50s and, among other conditions, had late-stage kidney disease, for which he required dialysis. He wrote to the court April 8, asking to be released from prison. By then, the coronavirus was spreading rapidly throughout the country.
"Once a guard or staff member brings it in here, it will spread," he wrote again April 19, this time to the 8th U.S. Circuit Court of Appeals.
Young Bird was trying to secure an avenue out of prison faster than the virus could spread.

Waylon Young Bird wrote in his letters that he was concerned about the COVID-19 pandemic arriving in prisons. He was trying to secure an avenue out of prison faster than the virus could spread. Jo Lynn Little Wounded hide caption
Waylon Young Bird wrote in his letters that he was concerned about the COVID-19 pandemic arriving in prisons. He was trying to secure an avenue out of prison faster than the virus could spread.
Over the past two years, thousands of other federal inmates argued the same grim position, trying to use an established process to petition for release before their time in prison effectively became a death sentence.
Many of them ultimately lost. Eventually, Young Bird would too.
As of early March, officials at the Federal Bureau of Prisons (BOP) say 287 federal inmates have died from COVID-19, a count that does not include deaths in privately managed prisons. Bureau officials have been saying since the beginning of the pandemic that they have a plan to keep the situation under control, but an NPR analysis of federal prison death records suggests a far different story.
The federal prison system has seen a significant rise in deaths during the pandemic years. In 2020, the death rate in prisons run by the BOP was 50% higher than the five years before the pandemic. Last year, it was 20% higher, according to the NPR analysis of age-adjusted death rates.
Of those who died from COVID-19, nearly all were elderly or had a medical condition that put them at a higher risk of dying from the virus, NPR found. Many of them seemed to sense their fate — and had tried to get out. And those who made their case in court often faced a slow and complicated process that was unable to meet the pace of a rapidly spreading virus.
"All you heard was just coughing all night, all night"
The Federal Bureau of Prisons had a problem from the day the coronavirus arrived in the U.S.: Prisons were likely to be a petri dish for COVID-19. Because staying away from others is nearly impossible inside a prison, health experts said the most effective way to deal with that problem was to make the prison population much smaller — and quickly.

Ron Shehee had been at the federal prison complex in Lompoc, Calif., only a few months when the pandemic struck. Meron Menghistab for NPR hide caption
Ron Shehee had been at the federal prison complex in Lompoc, Calif., only a few months when the pandemic struck.
Ron Shehee lived through the outbreak at the federal prison complex in Lompoc, Calif., where 70% of inmates tested positive for the coronavirus by May 2020. He lived in the prison camp — also known as a minimum security institution — with more than 100 other men, where they slept closely together in bunks, shared bathrooms and ate together. Convicted in 2019 on charges related to selling methamphetamine, Shehee had been at Lompoc only a few months when the pandemic struck.
"At first, we didn't even know that COVID existed. We just had people start getting real, real sick," Shehee remembers. Some were so sick that Shehee, who is paralyzed from the waist down, said he began letting other inmates use his wheelchair to transport people to the medical room. The atmosphere became tense.
"People trying to hold in their cough because it'll start an argument, and people trying to get up and rush to the bathroom so they don't cough," Shehee recalled. "At nighttime, that's all you heard was just coughing all night, all night."
Shehee was placed in isolation after his friend Jimmie Lee Houston died of COVID in early May. But that isolation, he said, felt more like being punished with solitary confinement, and without the medical care he needed, like the catheter he requires or the medications he takes for spasms and asthma.
"They did put me in a nasty little cell all by myself," Shehee said. "And over there in the hole, they don't talk to you. Every time they come up to the door, they shove your food in. And if you ask a question, they don't care."

Shehee was placed in isolation after his friend Jimmie Lee Houston died of COVID-19 in May 2020. But during isolation, Shehee says, he did not receive the medical care he needed. Meron Menghistab for NPR hide caption
Shehee was placed in isolation after his friend Jimmie Lee Houston died of COVID-19 in May 2020. But during isolation, Shehee says, he did not receive the medical care he needed.
At one point, he said, he fell out of his wheelchair while showering and had to crawl back to his bunk. Experiences like Shehee's sparked fear in other prisons as well, where there were reports of inmates not reporting symptoms because they wanted to avoid isolation. When asked about Shehee's experience at Lompoc, the Bureau of Prisons declined to comment on "anecdotal allegations."
In June of 2020, Michael Carvajal, the BOP director, acknowledged this problem to the Senate Judiciary Committee. "Prisons, by design, are not made for social distancing," Carvajal testified. "They are, on the opposite, made to contain people."
Carvajal, who announced his resignation in January of this year, assured the committee that regardless of social distancing, the bureau had a "sound pandemic plan."
It's difficult to get a full view of how the federal prison system has responded to the pandemic at each of its 122 prisons nationwide, but NPR spoke with several current bureau employees who described issues that went against that plan, including the transfer of COVID-positive inmates between prisons and units.
"Our agency is reactive and not proactive. You know, they waited until it got out of hand and then tried to fix things, but by then it was too late," said Aaron McGlothin, a warehouse worker foreman and local union president at the federal prison in Mendota, Calif.
"I don't trust anything the Bureau of Prisons says," said Eric Speirs, a senior correctional officer and local union president at the federal detention center in Miami. "We've had places catch on fire with COVID."
The bureau declined an interview for this story, but in a statement, a spokesperson wrote that the Bureau of Prisons has worked with the Centers for Disease Control and Prevention, has "implemented a flexible and tiered approach," and is "taking appropriate steps to normalize operations as safety and security permit."

Shehee speaks with his daughter, Sierra Connolly-Shehee, grandson Ezron Alvarez-Connolly and son D'Andre Connolly-Shehee outside the office of the used car lot managed by daughter Shayla Connolly-Shehee in Kennewick, Wash. Meron Menghistab for NPR hide caption
Shehee speaks with his daughter, Sierra Connolly-Shehee, grandson Ezron Alvarez-Connolly and son D'Andre Connolly-Shehee outside the office of the used car lot managed by daughter Shayla Connolly-Shehee in Kennewick, Wash.
Ron Shehee, the prisoner at the Lompoc camp, was eventually granted a compassionate release and now lives in Kennewick, Wash., where he works as a used car salesman. He still hasn't shaken the sense that he averted death.
"I went there to do my time for the crime that I committed and I owned up to that. But I did not plan on going there to die and never see my kids and my family anymore," Shehee said. "We all was lucky to make it through what we went through, and some of us didn't."
"We could have been releasing so many more people"
Some federal criminals will likely never be considered for an early release of any kind, but the pandemic changed the calculation.
On March 26, 2020, then-Attorney General Bill Barr sent a memo to Carvajal, the BOP director, asking him to prioritize home confinement, where a person would be monitored at home and remain in BOP custody. Barr acknowledged that some vulnerable inmates would be safer at home "where appropriate." Still, he wrote: "Many inmates will be safer in BOP facilities where the population is controlled and there is ready access to doctors and medical care."
Barr did, however, include a list of factors to consider when releasing an inmate, including age and medical conditions, the security level of the institution, their conduct in prison, their perceived risk of re-offending, their reentry plan and their crime. Some crimes, like sex offenses, wouldn't be eligible.
The next day, then-President Donald Trump signed the Coronavirus Aid, Relief, and Economic Security Act, known as the CARES Act. It broadened the group of people the BOP could release to home confinement.

Michael Carvajal, director of the Federal Bureau of Prisons, is sworn in during the Senate Judiciary Committee hearing on June 2, 2020. Tom Williams/Pool/AFP via Getty Images hide caption
Michael Carvajal, director of the Federal Bureau of Prisons, is sworn in during the Senate Judiciary Committee hearing on June 2, 2020.
At the time, that new authority was still somewhat hypothetical. But by April, Alison Guernsey, who directs the Federal Criminal Defense Clinic at the University of Iowa College of Law, began to receive panicked phone calls from federal prisons.
"We started to see and hear things from our clients, fear in their voices," said Guernsey. "They called us to say, 'People have been coughing. I'm really afraid that I'm going to get sick. We've been watching things on the news about the need to wear masks. There's no one here with masks.'"
Guernsey, who has been tracking deaths from COVID-19 in prison, estimates she and other clinic staff have spoken with more than 50 prisoners and even more family members throughout the pandemic.
Just over a week after Barr sent his initial memo — on April 3, 2020 — he sent another, more strongly worded message to the BOP.
"While BOP has taken extensive precautions to prevent COVID-19 from entering its facilities and infecting our inmates, those precautions, like any precautions, have not been perfectly successful at all institutions," Barr wrote, adding that there were already "significant levels of infections" at several facilities. Those places, he wrote, should "immediately maximize appropriate transfers to home confinement."
"We have to move with dispatch in using home confinement, where appropriate, to move vulnerable individuals out of these institutions," Barr wrote. He said that prison officials should consider "all at-risk inmates — not only those who were previously eligible for transfer."

Attorney General Bill Barr speaks about the coronavirus during a news conference on April 1, 2020. Alex Brandon/AP hide caption
Attorney General Bill Barr speaks about the coronavirus during a news conference on April 1, 2020.
The determination for who can be sent home — and who cannot — is solely up to the BOP, and by the middle of November 2020, individual wardens became the final authority . After Barr urged the use of home confinement, the BOP added its own criteria to the attorney general's list.
Home confinement existed before the pandemic, for certain inmates in the final six months or 10% of their sentence, whichever was less. And those inmates kept going home in this way during the pandemic. As of early March of this year, more than 38,000 people had been released to home confinement during the pandemic. Of those, about 9,000 — or about 6% of the current federal prison population — were transferred directly because of the CARES Act.
It's unclear how many more people might have been eligible for CARES Act home confinement yet were not released.
"CARES Act home confinement is, frankly, a black box," Guernsey, of the University of Iowa, said. But she feels certain "we could have been releasing so many more people during the pandemic and we just chose not to."
There is evidence suggesting that to be true.
At the Lompoc prison complex, a report by the Office of the Inspector General estimated that in April 2020, about 957 people in low- and minimum-security detention were potentially eligible for home confinement. By the end of June, 124 inmates had been transferred out.
At the complex in Butner, N.C., the OIG estimated that 1,070 people were potentially eligible for home confinement in April 2020. By July of that year, Butner had released 68 people because of the CARES Act. Another 16 had been approved but were waiting to actually be released, and three who were approved died while waiting.
"Case management staff are urgently reviewing all inmates to determine which ones meet the criteria established by the Attorney General," the bureau wrote in a statement in May 2020.
Some federal judges saw things differently. In May 2020, one ordered the prison in Danbury, Conn., to release inmates faster, saying the pace constituted "deliberate indifference." In July 2020, another judge ordered Lompoc to transfer its vulnerable inmates to home confinement, saying the bureau had "likely been deliberately indifferent to the known urgency to consider inmates for home confinement."

An aerial view of the Danbury, Conn., Federal Correctional Institution in 2004. Douglas Healey/AP hide caption
An aerial view of the Danbury, Conn., Federal Correctional Institution in 2004.
Maureen Baird, a former warden at Danbury, said the bar for home confinement was simply too high. For instance, the BOP initially said inmates would not be considered if they had any misconduct on their prison record in the past year. The bureau also prioritized inmates who had served at least half of their sentence or a fourth of their sentence if they had 18 months or less remaining.
"When the CARES Act was established and then the Bureau of Prisons came in and made these additional requirements, I think they overstepped their bounds," Baird said. "You have guys that are in prison now, late 70s, early 80s, mid-80s, that are no danger to the community."
As time progressed, the bureau loosened some of its criteria . Eventually, inmates with misconduct on their records could be considered, so long as they were still considered safe to release. Wardens could also alert the bureau's central office in Washington, D.C., if they thought an inmate should be released to home confinement who didn't otherwise qualify.
To many on the outside and to some bureau employees, the process appeared haphazard, and the release of certain high-profile prisoners who didn't seem to qualify raised eyebrows.
Former Congresswoman Corrine Brown was released from the Coleman prison complex in Florida after serving less than half of her sentence. Her conviction was later overturned. Michael Cohen and Paul Manafort, then-President Trump's former lawyer and campaign chairman, were also both released in 2020 after serving less than half of their sentences.

Michael Cohen arrives at his Manhattan apartment on May 21, 2020, in New York City. Former President Donald Trump's longtime personal lawyer was released from federal prison because of the coronavirus pandemic. John Minchillo/AP hide caption
Michael Cohen arrives at his Manhattan apartment on May 21, 2020, in New York City. Former President Donald Trump's longtime personal lawyer was released from federal prison because of the coronavirus pandemic.
"There was a list of people that were qualified and there was a list of the people who left," said Joe Rojas, a teacher at Coleman and the former southeast regional vice president for the AFGE Council of Prison Locals. "If you're an inmate that has political influence and has money, you will probably get released rather than somebody who probably really should have gotten released."
Other BOP employees told NPR that understaffing made it difficult to quickly assess inmates for home confinement.
Mary Melek, chief union shop steward for the federal detention center in Miami, said part of her job as a case manager is to screen inmates for home confinement. But she often has to cover other shifts. If she needs to finish an inmate's paperwork but is instead walking the halls as a correctional officer, reviewing the lists of who might be eligible to go home can be a struggle.
"They pile up where you have a list and you can't get to it because the next day you'll have to work a custody shift," Melek said. "It takes, on average, one to two months to get everything processed for somebody that could have probably left in a week."
One current administrator, who asked to remain anonymous for fear of retaliation, told NPR that home confinement paperwork at their prison often sat around for months.
"Think about it. Everyone is already overworked and stressed. Who's going to start an inmate's paperwork?" the administrator said.

Prisoners look out of their windows at the federal detention center in downtown Miami on June 12, 2020. Chandan Khanna/AFP via Getty Images hide caption
Prisoners look out of their windows at the federal detention center in downtown Miami on June 12, 2020.
In a statement, a BOP spokesperson told NPR "all inmates are reviewed appropriately" for CARES Act home confinement. Additionally, the BOP spokesperson wrote, "Despite challenges posed by the pandemic, we have managed our staffing levels to maintain the safety and security of our staff and inmates." The spokesperson added that more than 2,000 employees have been hired since March 2021.
"Leadership played down the danger and played up their capacity to deal with it"
By the summer of 2020, Waylon Young Bird had already been denied home confinement.
He continued writing to Judge Lange. Young Bird, who grew up in the Cheyenne River Sioux Tribe and the Mandan, Hidatsa and Arikara Nation, wrote about his family in the Dakotas, his struggles with addiction, and the prayer group he started in prison.
For his part, Lange had been reading Young Bird's letters all along.
"I read them close in time to when they were received," Lange told NPR. "I had very mixed feelings."
In its argument against his release, the government noted an "extensive" criminal history in tribal court. Regarding the pandemic, the U.S. attorney wrote: "Defendant only becomes susceptible to increased risk if he contracts COVID-19."
In June, Lange denied Young Bird's compassionate release motion.
"Researchers have found that ailments like diabetes and chronic kidney disease put individuals suffering from them, like Young Bird, at higher risk of complications if they contract COVlD-19," Judge Lange wrote. "However, there is still much that is unknown about how this virus affects individuals, and this Court cannot say to what extent Young Bird's life is threatened by the existence of COVlD-19."
Additionally, the judge wrote, Young Bird received health care at his prison, and "the BOP has taken precautions to protect him and his fellow inmates."
Lange told NPR he felt he had ruled properly in Young Bird's case, given that Young Bird had served only a small portion of his sentence. And, Lange said, Young Bird had also been using drugs during his pretrial release.
"I just felt that it probably was safest for him to be at a federal medical facility rather than outside," the judge told NPR. "Looking at things in retrospect is a difficult way to try to go about the job I have, because I have to judge with the information that I presently have."
Lange said he didn't know in June 2020 to what extent Young Bird's life was threatened, given that he was at a federal medical center.
"As a district judge in South Dakota, it's hard to know exactly what is going on at a Bureau of Prisons facility," Lange said. "But when I see a medical doctor from the Bureau of Prisons write, in essence, that the individual is receiving appropriate care ... I tend to trust that."

Waylon Young Bird had already been denied home confinement by the summer of 2020. He continued writing to Judge Lange. Jo Lynn Little Wounded hide caption
Waylon Young Bird had already been denied home confinement by the summer of 2020. He continued writing to Judge Lange.
On June 10, just a few days after his denial for release, Young Bird wrote again to Lange.
"I know I just wrote to you but I'm writing again, because this morning around 10 am, an inmate next to me said 'It's finally here,'" Young Bird wrote. "It's official now, that the first case of the coronavirus is here at Springfield, Mo. Medical Center."
Young Bird wrote that he went back to his unit and put on his face mask, one he said he'd had for a few weeks.
"Our beds are right next to each other. We don't practice social distancing here," Young Bird wrote. "I don't know what to do. I'm scared like everyone else."
A few days later, he wrote again.
"This coronavirus will start spreading soon, a lot of us will get it," Young Bird wrote. "I don't want to die here. I got family I miss, a handicap sister, kids who need me, grandkids too. Can you find it in your heart to reconsider?"
Many other inmates were navigating their options just like Young Bird. Finding themselves denied for home confinement, they took to court to make their case to be released early from their sentences.
A federal inmate's ability to ask a judge for compassionate release, where a prison sentence is actually reduced, was only recently made possible. Before the First Step Act in 2018, the bureau was solely responsible for identifying prisoners and bringing their cases to court. The First Step Act gave inmates the right to do that themselves. In the first full year the new law was in effect, 96 inmates filed motions themselves. In 2020, nearly 13,000 motions were filed in federal court.
The road to court, though, still starts in the prison. Before they can file their own compassionate release motion, inmates first have to ask their warden to file a motion on their behalf. Then they must wait 30 days for the bureau to respond, though some courts have waived that requirement.
By April 2021, nearly 31,000 inmates took this first step of asking their warden and waiting for an answer. At least 35 died waiting for the Bureau of Prisons to review their case. Ultimately, the bureau approved just 36 of that initial 31,000.
Once an inmate is allowed to file their own motion in court, whether they succeed depends largely on the district their case is in. In the Southern District of Georgia, for instance, federal judges denied 98% of the compassionate release motions they saw between January 2020 and June 2021. In the District of Oregon, they denied just 35% of the motions. Overall, federal judges nationwide denied more than 80% of the compassionate release motions in that time, according to data from the U.S. Sentencing Commission .
That tendency to deny is the result of a mentality in the criminal justice system to "just say no," said Miriam Krinsky, a former federal prosecutor and the executive director of the group Fair and Just Prosecution.
"That mindset of 'We are going to punish as harshly as possible. We will charge everything possible, we will seek everything possible. And when people want relief from that, we will just say no,'" Krinsky said.

The U.S. is limiting compassionate release in plea deals. Many say that's cruel

Throughline
Mass incarceration.
And some of it, she said, is risk aversion.
"People just don't want to be the ones with their name, their neck, on the line on decisions they view as risky, namely letting people out before their date," Krinsky said. "The focus is on the one case in a thousand where things go wrong rather than the 999 instances where things go well, where people are released or receive a second chance and do perfectly fine."
The success of a compassionate release motion depends ultimately on whether a judge finds a prisoner deserving of release. To determine that, a judge will consider the factors that came into play when the inmate was sentenced , like the seriousness of the crime. They'll also consider whether there are "extraordinary and compelling reasons" that justify release. And that can be influenced in part by whether the COVID conditions in a prison seem dire, said Colin Prince, the chief appellate attorney for the Federal Defenders of Eastern Washington and Idaho.
"My biggest frustration was that the leadership played down the danger and played up their capacity to deal with it," Prince said of the Bureau of Prisons. "Publicly and to the judiciary in briefings, they were just writing 'We've got this. We're experts in infectious disease. Here are the many policies we've put in place.'"
Once the motions related to COVID started coming in, prosecutors repeatedly argued in court against the release of inmates. They said the BOP had taken significant measures to protect prisoners — and was already prioritizing the release of inmates through another avenue: home confinement.
"It would have been much more honest and, frankly, helpful had the leadership of BOP simply come out and said, 'There's only so much we can do," Prince said. "And what they should have done is gone to the judiciary and said, 'This is a big problem. We can't protect these people. You need to help us.'"
Krinsky said that may have made a difference.
"There is often deference to the Bureau of Prisons," she said. "Their mindset can hold great sway in terms of how these cases play out."
Instead, many inmates had to go through what was often a lengthy and fruitless legal process. Of the prisoners who died from COVID-19, at least 1 in 4 filed a motion in court for compassionate release, according to NPR's analysis.
At least three people had their requests granted, yet contracted COVID-19 and died before they could actually be released.
In Kentucky, James Oscar Jones died the same day his release was granted. Andre Williams in North Carolina was granted compassionate release on April 1, 2020, but the court stayed the order. Williams tested positive for COVID on April 5 and died on April 12, two days after the stay was lifted.
In Kansas, Steven Brayfield first asked his warden for compassionate release in July 2020 and was denied about a month later. In early December, he asked again, this time in court, which a judge granted one month later. But Brayfield was already hospitalized with the virus. By then, according to Brayfield's lawyer, his family could not pay for his medical care if he were released. They requested that, instead, he stay in BOP custody so he could remain on a ventilator. He died on Jan. 19, 2021, at age 63.
Many others died while their motion was still moving through the courts, and some had been waiting months to hear back. At least four requests were denied as moot because the people had already died.
In Indiana, James Lee Wheeler, a 78-year-old with diabetes and high blood pressure, among other conditions, told his lawyer he was deeply anxious about what would happen to him if he contracted COVID-19. In the late summer of 2020, Wheeler woke to find one of his cellmates, who had been having trouble breathing, had died during the night, according to a release motion filed by Wheeler's lawyer. That motion had been pending for three months when Wheeler died that December .

Marie Holiday's father, Abdul-Aziz Rashid Muhammad, asked for compassionate release in April 2020. He cited several health conditions that put him at a higher risk of death from COVID-19. Meg Vogel for NPR hide caption
Marie Holiday's father, Abdul-Aziz Rashid Muhammad, asked for compassionate release in April 2020. He cited several health conditions that put him at a higher risk of death from COVID-19.
Others who died were denied not necessarily because they were ineligible but for other, more administrative, reasons: Some because they did not exhaust all avenues with their wardens first. And sometimes, the courts simply seemed to make a mistake — like in the case of Abdul-Aziz Rashid Muhammad.
In the fall of 2020, his daughter Marie Holiday was starting to make plans to spend time with her father without a guard watching over them. Muhammad had been in prison, for charges related to armed robbery, nearly all of Holiday's life.
That fall, Holiday had a glimmer of hope: One of her father's convictions had been ruled unconstitutional, and he had a resentencing hearing scheduled in early 2021.
"He said he was coming home. He was confident," Holiday said. "He's been fighting a long fight, a long battle."

Marie Holiday kept every photo her father, Abdul-Aziz Rashid Muhammad, sent to her from his decades in prison. Meg Vogel for NPR hide caption
Marie Holiday kept every photo her father, Abdul-Aziz Rashid Muhammad, sent to her from his decades in prison.
In April 2020, even before his resentencing hearing was set, he had asked for compassionate release, citing several health conditions that put him at a higher risk of death from COVID-19.
In May, the U.S. attorney wrote in his argument against Muhammad's release that there were no confirmed cases of COVID-19 at the federal medical center in Rochester, Minn., where Muhammad was located.
In September, the court denied Muhammad's motion, writing "speculative concern about catching COVID is not enough" given that, even by that fall, only 0.01% of inmates at his prison had the virus.
But by then, Muhammad wasn't at Rochester. Three months earlier, in June, he had written to the court to tell the judge he had been transferred to Butner, where more than 50% of inmates had tested positive .

Muhammad tested positive for COVID-19 on Jan. 13, 2021. Five days later, he was sent to a hospital, where his daughter Marie Holiday saw him over a video call. Marie Holiday hide caption
Muhammad tested positive for COVID-19 on Jan. 13, 2021. Five days later, he was sent to a hospital, where his daughter Marie Holiday saw him over a video call.
Muhammad eventually tested positive, too, on Jan. 13, 2021.
Five days later, he was transported to a hospital, where Holiday was able to see him through a video call.
"I was speechless when I saw him. There was nothing. He was just hooked up to all these different machines and he was not responding." Holiday remembers. "I just kept repeating that I love him and I'm so sorry."
On Feb. 9, Muhammad died — one month before the hearing he thought would secure his release.
Every time someone dies of COVID-19 in federal prison, the bureau writes a press release. Every letter is structured the same: First, there's a timeline of how the disease ravaged their body. Then it names their crime. The notice for Muhammad was no different.
"He had a family that loved him, and I'm sure all those other inmates had families that loved them," Holiday said. "I'm not saying that everybody is a nice guy that's in prison, but there are some good people and even those that are bad, they still deserve to be treated like humans."
"It's far from over"
People are still regularly contracting COVID-19 and dying from it in federal prison. At least one prisoner, Rasheem Hicks, was denied release, in part, because he chose to be vaccinated, which lowered his medical risk to the virus. Another, Rebecca Marie Adams, was denied, in part, because she chose not to take the vaccine that would lower her risk. Both later died of the virus.
"It's far from over," McGlothin, the employee and union president at the prison in Mendota, said. "You know, people are dying, people are getting sick. And the protocols seem to be a lot more lackadaisical than they were two years ago."

Abdul-Aziz Rashid Muhammad is buried at Crown Hill Memorial Park and Mausoleum in Cincinnati, Ohio. Meg Vogel for NPR hide caption
Abdul-Aziz Rashid Muhammad is buried at Crown Hill Memorial Park and Mausoleum in Cincinnati, Ohio.
Dr. Homer Venters, former chief medical officer of the New York City jail system and a member of the Biden administration's COVID-19 Health Equity Task Force, has conducted dozens of inspections of jails, prisons and immigration detention facilities during the pandemic. He said he has seen strengths in the federal prison response to COVID-19 in many places across the country.
"But I have also encountered significant deficiencies in how or whether basic CDC guidelines and BOP policies were being implemented," Venters testified to the House Judiciary Committee in late January of this year. "There is no doubt that many of these strengths saved lives and, conversely, that many of these deficiencies led to preventable illness and death."
Venters stressed the need for an independent investigation into all COVID-19 deaths that occurred in federal custody.
"The total story is that people were in places where they were more likely to get COVID and more likely to die from COVID," Venters told NPR. "We need to fully understand how the inadequacy of care for them contributed to these deaths."

An envelope that contained one of Waylon Young Bird's letters to Judge Lange. Department of Justice hide caption
An envelope that contained one of Waylon Young Bird's letters to Judge Lange.
By the fall of 2020, Waylon Young Bird's letters were becoming increasingly desperate.
"Nobody cares if you die or not here," he wrote on Sept. 20.
Just under a month later, he wrote again. He told Judge Lange he qualified for home confinement and compassionate release and should be given a second chance.
"We feel like sitting ducks, waiting for the virus to come and infect us," he wrote. "I can prove I'm going to be a law-abiding citizen and do good for myself. I'm no danger to others or the community. I'm not a terrible person."
On Oct. 27, Young Bird wrote again, this time to tell the judge of a major outbreak at the prison. At least 200 inmates and staff were infected. He had been separated from the COVID-positive inmates, he wrote, but he didn't think staff had a protocol they were following. COVID-positive inmates were still serving the food, he wrote. Some staff, he said, had stopped coming to work.
"I'm afraid I may be infected by the time you receive this letter and would not be able to contact my family by then," he wrote, ending his letter simply: "I don't feel good about this at all."
Young Bird tested positive the following day and died a week later. He was 52.
His aunt, Jo Lynn Little Wounded, got a call early the next morning from a prison employee. He was looking for Young Bird's mother, who was sleeping in the next room with his sister.

Jo Lynn Little Wounded holds her nephew Waylon's ribbon shirt beside his pickup truck. Dawnee LeBeau for NPR hide caption
Jo Lynn Little Wounded holds her nephew Waylon's ribbon shirt beside his pickup truck.
"I just couldn't even bring myself to tell her and my niece that he passed away," she said.
Little Wounded sat in the other room for a few hours before she woke them up.
"He didn't have to die like that," Little Wounded said. "He died a horrible death in there by himself. And that's the hardest part, was that he died by himself."
Little Wounded was ready to welcome him home. His truck remained parked in front of her house for more than a year after his death, until the city finally came and towed it away.
Editor's note: Some of Waylon Young Bird's letters contain minor grammatical errors, which NPR has opted to correct for clarity.
NPR’s Barbara Van Woerkom contributed research to this report, and NPR’s Nick McMillan and Robert Benincasa contributed to the data analysis.
‘A living hell’: Inside US prisons during the COVID-19 pandemic
Prisoners and their families describe the emotional, physical and financial toll of the pandemic.

In the days before Christmas, 44-year-old April Harris sat in her prison cell at the California Institution for Women for more than 23 hours a day. In the 20 minutes she was allowed to leave it, she and the other prisoners would flood into the common areas – choosing either to take a shower or to make a short phone call.
Restrictions have fluctuated during the various lockdowns implemented throughout the COVID-19 pandemic, but in the 11 months since the California Department of Corrections and Rehabilitation (CDCR) first banned visitations across state prisons, Harris says she has seen the mental health of those around her steadily deteriorate.
Keep reading
Will the us unemployment rate continue at historic lows, mexico’s teachers seek relief from pandemic-era spike in school robberies, ‘a bad chapter’: tracing the origins of ecuador’s rise in gang violence, why is the us economy so resilient.
“A friend of mine sliced her arms yesterday because she said that she couldn’t handle it anymore,” Harris wrote at the end of 2020 in a message sent via JPay, an electronic messaging system used in prisons.
“Women scream, beat their doors and call fake medical emergencies just to get out of their rooms. The women are definitely breaking.”
Elizabeth Lozano, 46, used to work in the gym, visit the law library and take art therapy and creative writing courses at the Central California Women’s Facility (CCWF) where she is imprisoned, but that all stopped in mid-March. At first, she says she was still allowed outside at intervals – first every other day and then every four days. Now, however, she says she has not smelled fresh air since late December, when the CCWF further restricted movements as the number of COVID cases rose.
“The stress level is super high,” Lozano wrote through JPay, noting that the anxiety was driven by fear of COVID in rooms where women were “packed like sardines.
“We have no control of what [others] do, so even if I take precautions [it] doesn’t mean a roommate is. We can’t social distance or shelter in place safely.”
Lawyer Penny Godbold represents individuals with disabilities in California prisons and says, “The pandemic has had an unbelievable toll on the mental health of people incarcerated in California. People describe watching others – friends, cellmates, those in their housing units – get sick and die around them without knowing whether they, too, will suffer the same fate.”
Six feet apart
Kassan Messiah, 55, last saw Lorraine, his wife of 27 years, in October, when she visited New York’s Sing Sing Correctional Facility. The visit buoyed Kassan.
“My wife is my respirator; my understanding of the world beyond the wall is all attributed to wifey,” Kassan wrote in a message sent over JPay.
But, “after each visit”, Kassan says he experiences “deflation”.
They had not seen each other since January 2020, when their communication and visits were upended.
At the beginning of January 2021, Lorraine only received one call from Kassan a week. Afraid of missing it, she kept her phone with her at all times. But sometimes, just five minutes into the call, she says she would hear the guards yelling at him to hang up.
Then, on January 23, Kassan says he was left with a bloodied mouth, a black eye, bruising and wrist lacerations after he was attacked by guards. When asked about this, the New York Department of Corrections and Community Supervision said they were investigating the incident and would not comment further. Kassan was moved into a Special Housing Unit, where he is able to call Lorraine every day. She says she now gets to hear her husband’s voice more than at any other point during the pandemic.
During her October visit to Sing Sing, social distancing restrictions prevented them from hugging. About two dozen cafeteria tables filled the visiting room. The length of the table, about six or seven feet, separated Kassan from Lorraine.
“It’s more torture than anything else because you’re so close, but yet you’re so far,” Lorraine reflected. “If you’re allowing me into the facility, why am I not able to touch his hand?”
Even so, she had gotten closer than most people with imprisoned family members.

‘Absolutely no support’
In March, as the World Health Organization (WHO) declared a pandemic, US prisons shut down visitations. A handful of states, including New York, restored visits but stopped them again months later. As of early February, only six states and the Federal Bureau of Prisons currently allow personal visits, with varying restrictions. North Carolina only allows one 30-minute visit per month; only two people can visit each time, and no children under 12 are allowed. New Hampshire allows one 45-minute each month. Visits are non-contact and nobody under 18 is allowed into facilities.
Imprisoned people “can’t see friends, and they can’t maintain consistent contact with supports, but they also can’t go to mental health programming,” said Stefen Short, the Supervising Attorney of the Prisoners’ Rights Project run by the New York-based Legal Aid Society. “Well then what’s available to this person? At the middle of a global pandemic, when everybody’s at heightened anxiety, our clients are getting absolutely no support.”
Access to legal representation has also been affected by visitation changes. Earlier this month, 31 prison systems permitted legal visitations but banned personal visits, while 13 forbade all guests. Jails have quarantined new arrivals for 10 to 14 days and only allowed detainees to place calls to lawyers for 15 to 30 minutes each day, according to Corene Kendrick, the deputy director of the ACLU’s National Prison Project.
“It’s critical for defence attorneys to meet with their clients soon after they are arrested so that the attorney can get a thorough account from their clients about witnesses, locations, possible alibi evidence, and to review documents, police reports, and photos, and explain the next steps in the process to the client. Regardless of whether it is in the intake quarantine areas or in the general population sections, most jails often have very few or no options to set up confidential video or telephone calls,” Kendrick explains.
“In prisons, where people may need to speak to their attorney for purposes of a pending appeal, a new lawsuit, or as part of a class-action lawsuit regarding conditions, there are the same limitations.”
‘An ongoing nightmare’
For those with pre-existing mental health conditions who are no longer able to see their therapists, the strain has been even greater.
“It’s a living hell, pretty much,” says one California prisoner, who has been diagnosed with borderline personality disorder and went seven months last year without seeing his social worker. “I can only describe it as an ongoing nightmare.”
Incarceration facilities have, for decades, teemed with people needing mental healthcare. Forty-four states have an incarceration facility detaining more mentally ill people than the state’s largest psychiatric hospital, according to the Treatment Advocacy Center. Thirty-seven percent of people in state and federal prisons and 44 percent of those in jails have been diagnosed with a mental illness. Yet only 37 percent of people held in prisons and 38 percent of people detained in jails with mental health disorders were actually receiving treatment, according to a 2017 Department of Justice report.
But, during the pandemic, while the need for mental healthcare has peaked, the limited services offered in prison have diminished further.
“We’re not seeing counselors or [therapists] right now at all,” Lozano wrote via JPay. Group therapy sessions, which she attends to help with depression, have been shut down since spring, and she sees her therapist much less frequently than before the pandemic. “At one point I was quarantined in isolation and I kept asking to see mental health for that day following protocol, but I wasn’t able to see no one for days.”
“The well-being and safety of the incarcerated population and staff within CDCR and CCHCS [California Correctional Health Care Services] is our top priority,” CDCR Press Secretary Dana Simas wrote in an email statement to Al Jazeera, noting that prisoners are provided with ongoing mental health assessments and the department is conducting crisis intervention to prevent suicides.
“An incarcerated person may request mental health services or they may be referred through institution staff. Mental health and operations leadership meet daily to ensure mental health referrals and requests for services from patients are quickly addressed.”
But imprisoned people and their advocates say that even if services are formally offered, obtaining useful care is often difficult.

After a transgender man in the California Institution for Women – the facility housing April Harris – attempted suicide in May, the prison offered colouring books and crossword puzzles to prisoners. In June, a Virginia prison distributed a “mental minute” newsletter offering tips for relaxation and sleeping. The pamphlet instructed readers to “prepare yourself before going to bed” by exercising earlier in the day, “taking time to relax by meditating, listening to restful music, completing relaxation exercises or reading”.
In September, the Southern Center for Human Rights, an organisation that represents people in the criminal justice system, urged the Department of Justice to investigate “deplorable conditions” in Georgia prisons, after suicides reached unprecedented levels. In the eight months before the letter was sent, 19 people in Georgia prisons died by suicide – a rate twice the national average for suicides in state prisons. About 30 percent of the suicides occurred in a facility that “purportedly specialises in the housing and care of people with serious mental illness,” the letter said.
Employees in a Louisiana prison began walking around once a week, shouting “mental health”. One man, who asked to remain anonymous for fear of retaliation, scoffed at the idea that anyone would try to take advantage of these services. “You don’t show no signs of weakness because there’s a predatory aspect in the environment. You don’t want to be labelled or exposed or even perceived as needing that kind of help. Not to mention the level of stigma that comes with it.”
Even if someone did request help, he doubted he would receive assistance. Instead, he said, men were walking around, having full conversations with themselves.
“If you’re not bleeding, and it’s not obvious that you’re in dire need of medical [help], you’re probably going to be charged with malingering.”
‘They had no record of me’
For many of those who get COVID-19, the situation rapidly deteriorates.
Less than a month before the pandemic tore through New York City, the United Nations special rapporteur on torture rebuked the “excessive use” of solitary confinement in US correctional facilities.
“This deliberate infliction of severe mental pain or suffering may well amount to psychological torture,” Nils Melzer, the rapporteur, said.
Throughout the pandemic, the use of solitary confinement has skyrocketed, as prisons seek to stop the virus from spreading.
While overcrowding has propelled the spread of COVID-19 through prisons, it also leaves facilities with few places to quarantine infected people. In June, a coalition focused on ending solitary confinement released a report estimating a 500 percent increase in the number of people held in isolation – a violation of CDC guidelines saying “staff should ensure that the conditions in medical isolation spaces are distinct from those in punitive isolation”.
As COVID raged through California’s San Quentin State Prison, Patricia Zinnamon’s husband, Rashiyd, who had tested positive, was placed in solitary confinement, without access to a phone. He was told in June that he would be in solitary for two weeks. Rashiyd was not released until August.
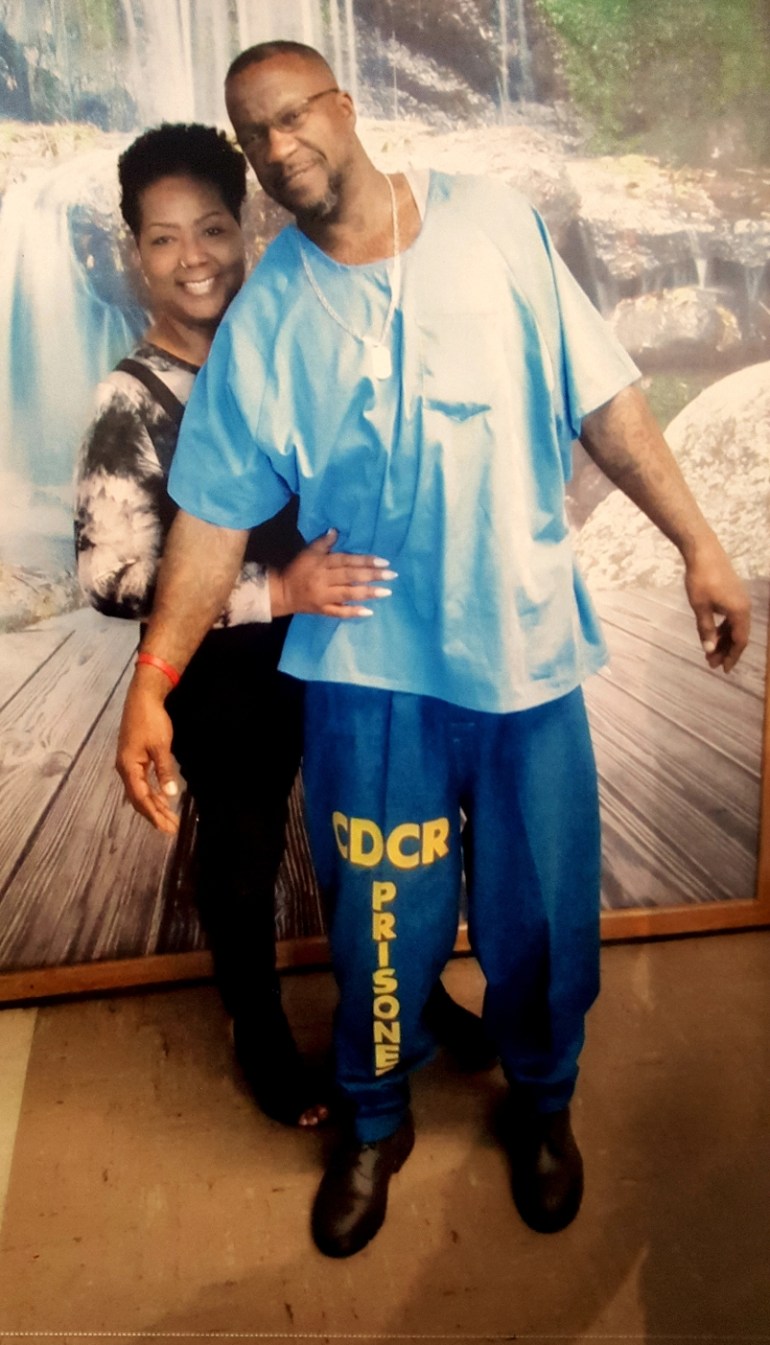
Another person imprisoned at San Quentin, who asked to remain anonymous because he was communicating with a contraband mobile phone, was taken into solitary. He was told he would spend 10 to 12 days in isolation but was kept there for two months.
“The first two weeks I was in the hole, no one from medical checked on me or even knew I was there,” he says. “After the first two weeks, I stopped a nurse walking by to ask when I would be returned to my regular cell. That’s when she asked who I was and said they had no record of me.”
In the chaos, he says, correctional officers simply forgot about him.
Lawyers and academic experts say that as COVID has spread, prisons have restricted the amount of information they release, including about the number of deaths and the use of solitary confinement.
Researchers “don’t have a good understanding of exactly how states are utilising solitary confinement,” explains Lauren Brinkley-Rubinstein, a professor at the University of North Carolina School of Medicine. “The collateral consequences of COVID are really severe, and we also don’t yet know how bad it actually is.”
Research has indicated that solitary confinement causes lasting damage. In the first year after their release, people placed in solitary confinement are 78 percent more likely to die from suicide than those who were not. Those kept in restrictive housing for any period were also 127 percent more likely to die of an opioid overdose in the first two weeks post-release. A recent report focused on New York state prisons found that the suicide rate in solitary confinement was more than five times greater than that of the general prison population.
For some of those already in solitary confinement, the conditions have deteriorated even further.
Kwame Shakur, 30, who has been in solitary confinement at Indiana’s Wabash Valley Correctional Facility for more than four years, and in the facility’s long-term segregation area for nearly two and a half years, says he was not allowed outside for a month and a half in late autumn and early winter.
Shakur says guards used to walk him, hands cuffed behind his back and attached to a dog leash, to a small recreation area once a day. Shortly before Thanksgiving, the prison went into a complete lockdown. Shakur lost his daily hour in the recreation yard, which he describes as being the size of a dog kennel, until early January.
Although Shakur lost his access to the recreation area while the prison locked down, he says correctional officers [COs] still interact with both COVID positive and COVID negative populations.
“The same three guards who bring us our food and take us to showers every day are the same COs that are dealing with these corona patients,” he says.
“IDOC [Indiana Department of Correction] follows the guidance of the CDC and ISDH [Indiana State Department of Health] in our facilities to address the risk of spreading COVID-19,” IDOC Chief Communications Officer Annie Goeller said in an email statement. “This has included, but not been limited to, staff screenings upon entry to the facility, dedicating staff to specific units whenever possible, requiring the use of PPE including masks by all staff, frequent sanitation within the facility and quarantining any staff who have had prolonged contact with someone who has tested positive for COVID-19.”
‘About to blow up’
The day after Christmas, family members of people being held in Richard J Donovan Correctional Facility gathered outside the Southern California institution to protest against the facility’s handling of COVID-19. Just over a dozen people, the majority of them women, attended the rally. One woman held a sign reading “Free my husband,” another poster said “COVID is a life sentence”.
Halfway through December, cases had exploded at the facility, with more than 700 people infected in a matter of weeks.

The rapid spread of COVID at Richard J Donovan had been modelled at prisons around the country for most of the year. Even as family visitations are stopped, guards and transfers of prisoners between facilities bring COVID; once inside overcrowded prisons where social distancing is impossible, the virus runs rampant. One-fifth of the people held in federal and state prisons had tested positive for COVID-19 as of December, and inconsistent testing means the number of prisoners who have contracted the virus is likely to be even higher. At least 2,419 prisoners have died.
The situation at Richard J Donovan had been predicted. In the spring, lawyers and staff voiced concern about inadequate safety precautions and overcrowding. Advocates urged the state to release prisoners. Then, as cases began climbing across the system in late autumn, Stephanie Johnson got a concerning call from her best friend.
“I think this place is about to blow up though, with f***ing COVID,” he says on a recording shared with Al Jazeera.
About a week later, a person infected with COVID was transported to a medical facility at Richard J Donovan, according to two inmates. During transit, the two prisoners said in recordings obtained by Al Jazeera, others were exposed.
“Richard J Donovan Correctional Facility (RJD) is following all proper protocols in its facility and during transit as outlined under CDCR/CCHCS Patient Movement Matrix and CCHCS guidance. Staff ensure all inmates that arrive at RJD maintain proper physical distancing, are quarantined for 14 days and are provided with proper testing immediately upon arrival back at the institution,” a CDCR spokesperson said in an email statement. “RJD responded to an increase in positive COVID-19 cases with robust coordinated efforts to increase the frequency of testing, conduct contact tracing and implement isolation and quarantine measures to mitigate spread of COVID-19.”
Johnson says her friend had tested positive on December 10. His phone time dropped to twice a week, and he used the time to call his family. Johnson did not hear from him for a month – a significant shift from the multiple calls per week they had before the pandemic.
While the cases have risen, family members of Richard J Donovan prisoners have been unable to reach their loved ones, and are left wondering if they are sick or in isolation.
“It’s the wildest response. In the regular world [a positive diagnosis] would be the moment that everyone starts calling,” says Bianca Tylek, the executive director of criminal justice advocacy organisation Worth Rises. “In the prison system, sometimes people’s families find out they have the virus because they haven’t heard [from] them.”
‘A big stress on families’
Even those who regularly receive phone calls and messages experience frequent problems.
Cammie Maturin, who co-founded a Louisiana organisation advocating for prison reform, regularly speaks with others whose family members are imprisoned. When she has tried to video chat with her fiance, an inmate at the Louisiana State Penitentiary in Angola, she has battled constant technical issues.
“It has been a big stress on families, not only emotionally, but financially,” she explains. “We’ve gone [from] talking two or three times a day to talking maybe once a week.”
The $1.4bn prison and jail telecommunications industry is largely controlled by just three companies. In 2019, a 15-minute call in Arkansas could cost $4.80, and $3.15 in Louisiana. Each message sent through JPay, one of the dominant electronics communications systems, costs anywhere between $.05 and $1.25, according to advocacy group Worth Rises. The costs add up quickly, with many facilities benefitting from monetary kickbacks built into the contracts.
“When the pandemic interrupted in-person visitation, Aventiv immediately began offering free communications and is proud to have provided 37.5 million free calls totaling 302.9 million minutes of free connection, 6.2 million free video connections, and 22.2 million free JPay Stamps for electronic messaging at hundreds of sites nationwide,” Jade Trombetta, a spokesperson for Aventiv, the parent company of JPay, wrote in a statement to Al Jazeera. “We will continue to work with our partners to continue to maintain connections between incarcerated Americans and their loved ones throughout the pandemic.”

Lockdowns have also increased the amount of items that prisoners need. With in-person education courses, vocational instruction and arts classes cancelled, family members send any entertainment they can afford.
Azzurra Crispino, the executive director of the advocacy group Prison Abolition Prisoner Support (PAPS), said she pays $28 and a $3 fee each month to provide her husband with streaming music. In the second half of December, she paid nearly $325 on phone minutes for her husband, who is imprisoned in Ohio’s Marion Correctional Institution.
“Getting the monthly music, which was something that before we maybe did as a treat, now has become a necessity. Sending him books, which before we did as a treat, now has become a necessity. Sending him more reading materials on JPay, also a necessity. Because he’s going more than a little nuts,” says Crispino, who last saw her husband on Valentine’s Day in 2020.
For “most of the pandemic”, she says, the prison provided fewer meals to her husband and other prisoners. She compensated by sending her husband food packages, purchased through a private company.
The Ohio Department of Rehabilitation and Correction (ODRC) said in an email statement that it did decrease the number of meals but raised the number of daily calories provided to prisoners from 2,500 to 2,725 calories.
“I am in a much better situation than most, and my car is held together by duct tape. If just calls were free, I could afford repairs or even a new car,” Crispino says. “We’re hearing from people who are saying I’m not paying on my electric bill to make sure that my child can talk to his father.”
Family members who spoke for this article said no amount of connection, at any cost, can ease the emotional strain of watching coronavirus tear through prisons. They worry about the masks their loved ones have used for months on end and the shared phones that are not adequately washed. They do not know when the next call will come. When they hear their loved ones are suffering, they wish they could help.
“He has been so down, and it scares me because he’s afraid he will die in prison, alone without his family,” says Patricia of her husband Rashiyd, who she married just five months before San Quentin shut down.
“This has been an agonising experience and some days it’s hard to even get up and work,” she adds. Even as she tries to buoy her husband’s spirits, she says, “this separation has caused me to sink into a deep depression, I’ve lost 40 pounds during this time due to stress. I have been to the [emergency room] multiple times, and after all types of testing I was advised that my symptoms were stress related.”

Vaccinations
As Christmas, the New Year and Valentine’s Day passed without visitations for the incarcerated, the COVID-19 vaccine has provided a glimmer of hope, though even that shred of optimism is tinged with distrust.
Margaret Breslau, the co-founder of the Virginia Prison Justice Network, says she hears from prisoners who do not want to take the vaccine.
“Many inmates either think that if they had COVID, they don’t need a vaccine, some think they should wait because they are afraid of secondary strains that would render this vaccine insufficient,” Breslau wrote in an email.
“The Department has a vaccine education campaign going and we’re trying to get as much information to both staff and inmates as we can,” Lisa Kinney, the Director of Communications for the Virginia Department of Corrections said in an email statement.
But in many states, those eager for the vaccine will have to wait. Although federal prisons across the country are distributing vaccines, some of the nation’s most populous state facilities, like those in Texas and Florida, are not inoculating inmates. After a lawsuit earlier in February, the New York corrections department said it was “preparing to vaccinate” prisoners aged 65 and older.
While the pandemic will likely leave a lasting scar on those outside prison walls, experts worry the damage will be deeper on those inside them.
“Our mind tends to hold on to the trauma in a way that even when we’re no longer in that setting of danger, our mind likes to sort of trick us into thinking we are. So even in safer settings, we still have those symptoms of PTSD and hypervigilance and being startled,” explains Kirandeep Kaur, a psychiatrist who has been evaluating undocumented immigrants held in ICE detention. “Those don’t go away unless there’s some sort of professional help.”

The Impact of COVID-19 in Jails and Prisons Across America
by | Oct 7, 2021 | Amicus , Criminal Justice , Human Rights , Policing and Law Enforcement |

Over the p ast 18 months, as the world has been ravaged by the COVID-19 pandemic, those detained in jails, prisons, and detention centers have been severely impacted due to lack of physical distancing, proper sanitation methods, and the failure to prioritize testing and vaccinations. Common conditions in jails and prisons have never been conducive to decent health for inmates – lack of access to proper medical care, food quality, and overcrowding have all been huge causes for concern for those advocating for prisoners’ rights since long before the pandemic. Throughout the pandemic, jails and prisons have not been isolated from outside communities. In fact, there are many documented stories of correctional staff and other officers contracting the virus outside of work and bringing it into prisons or jails, or bringing the virus to their communities from prisons and jails, resulting in large outbreaks. Thus, jails and prisons have been extremely conducive to the spread of the virus, resulting in a large number of infections and deaths.
Although jails throughout the country reported population reductions early in the pandemic due to the release of inmates, populations were rising again by November . Stories of overcrowding are abundant. For example, at a correctional institute in Ohio, inmates attempted to use bedsheets to separate themselves; however, four in five ended up infected. Although more attention has been drawn to conditions like these in jails and prisons, a lack of data reporting by carceral agencies has prevented the public from being able to understand the full impact of the pandemic on incarcerated persons. Organizations like the UCLA Law COVID-19 Behind Bars Data Project , The Marshall Project , and The COVID Prison Project have been working to collect data and information as there has been a lack of transparency from agencies in providing adequate or correct data on the number of cases, safety protocols, and deaths within their jails and prisons. Many states’ Departments of Corrections rolled back or stopped reporting their COVID-19 data altogether this past summer, despite the surges of cases across America due to the Delta variant.
For example, in Georgia, the Georgia Department of Corrections has not reported any new COVID deaths since March 14, 2021 , and recently they have halted all public reporting data. The GDC has the second-highest case fatality rate, or percent of those with reported infections who die, among all the correctional systems in the United States. In Florida, which along with Texas counts for 40 percent of new hospitalizations across the country, the Department of Corrections said reporting data was no longer “operationally necessary.” As of October 2021 , more than 542,000 incarcerated people and correctional staff members have tested positive for coronavirus and at least 2,700 have passed away. In December 2020, at the peak of the virus, more than 25,000 prisoners tested positive in a single week . Limited testing, as well as deaths that were not counted , point to the fact that these numbers are likely much higher. The New York Times noted that more than 50 men and women who died of COVID-19 in local jails were awaiting trial for charges they were not yet convicted of.
Although a number of federal, state, and local policymakers have taken steps in the forms of increasing releases, reducing admissions, and changing probation and parole requirements, these changes are scattered, with many counties and states not instituting changes. These inconsistent policies have left certain populations, especially those with underlying health conditions or of older age, at a high risk of complications.
As of October 5, BOP had administered 228,363 doses of the COVID-19 vaccine, and the vaccination rate is 70% for those incarcerated and 55% for staff members . For state jails and prisons, the numbers differ drastically depending on the state.
This is a critical time as infection rates decline in prisons and across America; however, this does not mean that state and federal correctional agencies can refrain from reporting data. The public must be informed in order to call on the relevant groups/governments to effectuate changes in America’s carceral system that have been necessary and demanded since long before the pandemic.
COVID-19 in Correctional and Detention Facilities — United States, February–April 2020
Weekly / May 15, 2020 / 69(19);587–590
On May 6, 2020, this report was posted online as an MMWR Early Release.
Please note: . This report has been corrected.
Megan Wallace, DrPH 1 ,2 *; Liesl Hagan, MPH 1 *; Kathryn G. Curran, PhD 1 ; Samantha P. Williams, PhD 1 ; Senad Handanagic, MD 1 ; Adam Bjork, PhD 1 ; Sherri L. Davidson, PhD 3 ; Robert T. Lawrence, MD 4 ; Joseph McLaughlin, MD 5 ; Marilee Butterfield 6 ; Allison E. James, DVM 2 ,7 ; Naveen Patil, MD 7 ; Kimberley Lucas, MPH 8 ; Justine Hutchinson, PhD 8 ; Lynn Sosa, MD 9 ; Amanda Jara, DVM 10 ; Phillip Griffin 11 ; Sean Simonson, MPH 12 ; Catherine M. Brown, DVM 13 ; Stephanie Smoyer 14 ; Meghan Weinberg, PhD 15 ; Brittany Pattee, MPH, MN 16 ; Molly Howell, MPH 17 ; Matthew Donahue, MD 2 ,18 ; Soliman Hesham, MD 19 ; Ellen Shelley, DNP 19 ; Grace Philips, JD 20 ; David Selvage, MHS 21 ; E. Michele Staley, MA 22 ; Anthony Lee 23 ; Mike Mannell, MPH 23 ; Orion McCotter 24 ; Raul Villalobos, MD 25 ; Linda Bell, MD 26 ; Abdoulaye Diedhiou, MD 26 ; Dustin Ortbahn, MPH 27 ; Joshua L. Clayton, PhD 27 ; Kelsey Sanders, MPH 28 ; Hannah Cranford, MPH 29 ; Bree Barbeau, MPH 30 ; Katherine G. McCombs, MPH 31 ; Caroline Holsinger, DrPH 31 ; Natalie A. Kwit, DVM 32 ; Julia C. Pringle, PhD 2 ,32 ; Sara Kariko, MD 33 ; Lara Strick, MD 33 ; Matt Allord, JD 34 ; Courtney Tillman, MPH 35 ; start highlight Andrea Morrison, PhD 36 ; Devin Rowe, MS 36 ; Mariel Marlow, PhD 1 ( View author affiliations )
What is already known about this topic?
Correctional and detention facilities face challenges in controlling the spread of infectious diseases because of crowded, shared environments and potential introductions by staff members and new intakes.
What is added by this report?
Among 37 jurisdictions reporting, 32 (86%) reported at least one confirmed COVID-19 case among incarcerated or detained persons or staff members, across 420 correctional and detention facilities. As of April 21, 2020, 4,893 cases and 88 deaths among incarcerated and detained persons and 2,778 cases and 15 deaths among staff members have been reported.
What are the implications for public health practice?
Prompt identification of persons with COVID-19 and consistent application of prevention measures within correctional and detention facilities are critical to protecting incarcerated or detained persons, staff members, and the communities to which they return.
Views: Views equals page views plus PDF downloads
- PDF pdf icon [196K]
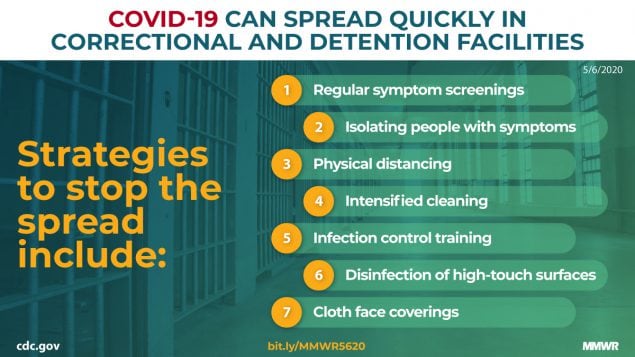
An estimated 2.1 million U.S. adults are housed within approximately 5,000 correctional and detention facilities † on any given day ( 1 ). Many facilities face significant challenges in controlling the spread of highly infectious pathogens such as SARS-CoV-2, the virus that causes coronavirus disease 2019 (COVID-19). Such challenges include crowded dormitories, shared lavatories, limited medical and isolation resources, daily entry and exit of staff members and visitors, continual introduction of newly incarcerated or detained persons, and transport of incarcerated or detained persons in multiperson vehicles for court-related, medical, or security reasons ( 2 , 3 ). During April 22–28, 2020, aggregate data on COVID-19 cases were reported to CDC by 37 of 54 state and territorial health department jurisdictions. Thirty-two (86%) jurisdictions reported at least one laboratory-confirmed case from a total of 420 correctional and detention facilities. Among these facilities, COVID-19 was diagnosed in 4,893 incarcerated or detained persons and 2,778 facility staff members, resulting in 88 deaths in incarcerated or detained persons and 15 deaths among staff members. Prompt identification of COVID-19 cases and consistent application of prevention measures, such as symptom screening and quarantine, are critical to protecting incarcerated and detained persons and staff members.
To estimate the prevalence of COVID-19 in U.S. correctional and detention facilities, CDC requested aggregate surveillance data from 54 state and territorial health department jurisdictions. Data were provided to CDC during April 22–28, 2020 and included laboratory-confirmed cases identified and reported to jurisdictions during January 21–April 21, 2020. Requested data elements included 1) the number of facilities that had reported at least one laboratory-confirmed COVID-19 case; 2) the cumulative number of incarcerated or detained persons and staff members with laboratory-confirmed COVID-19; and 3) the cumulative number of COVID-19–associated hospitalizations and deaths among incarcerated or detained persons and staff members. Jurisdictions were asked to include data for persons in the custody of or working for state and local corrections, U.S. Immigration and Customs Enforcement, U.S. Marshals Service, and Federal Bureau of Prisons. Data on the number tested or persons with negative test results were not requested.
Thirty-seven (69%) jurisdictions provided aggregate surveillance data; 32 (86%) of those reported at least one laboratory-confirmed COVID-19 case among incarcerated or detained persons or staff members. In those 32 jurisdictions, 420 facilities reported 4,893 COVID-19 cases among incarcerated or detained persons and 2,778 cases among staff members ( Table ). More than half (221; 53%) of the affected facilities reported cases only among staff members. Among COVID-19 cases in incarcerated or detained persons, 491 (10%) COVID-19–associated hospitalizations and 88 (2%) deaths were reported; among staff member cases, 79 (3%) hospitalizations and 15 (1%) deaths were reported. Among the 32 jurisdictions reporting cases, the median number of affected facilities was 10 (range = 1–59), the median number of cases in incarcerated or detained persons was 34 (range = 0–858), and the median number of cases in staff members was 26 (range = 1–756).
This analysis provides the first documentation of the number of reported laboratory-confirmed cases of COVID-19 in correctional and detention facilities in the United States, although information on the proportion of incarcerated and detained persons and staff members tested was not available. Approximately one half of facilities with COVID-19 cases reported them among staff members but not among incarcerated persons. Because staff members move between correctional facilities and their communities daily, they might be an important source of virus introduction into facilities. Regular symptom screening can help to reduce introduction of the virus from symptomatic persons, whether through staff members, new intakes, or incarcerated or detained persons who attend court-related or medical appointments in the community. Screening all incarcerated or detained persons quarantined as close contacts of a case twice daily and promptly isolating persons with symptoms can help identify persons infected as a result of transmission that occurred within the facility and control spread of disease.
Although symptom screening is important, an investigation of a COVID-19 outbreak in a skilled nursing facility found that approximately one half of cases identified through facility-wide testing were among asymptomatic and presymptomatic persons, who likely contributed to transmission ( 4 ). These data indicate that symptom screening alone is inadequate to promptly identify and isolate infected persons in congregate settings such as correctional and detention facilities. Additional strategies, including physical distancing, movement restrictions, use of cloth face coverings, intensified cleaning, infection control training for staff members, and disinfection of high-touch surfaces in shared spaces are recommended to prevent and manage spread within correctional and detention facilities ( Box ). Some jurisdictions have implemented decompression strategies to reduce crowding, such as reducing or eliminating bail and releasing persons to home confinement or community supervision. Testing might become an important strategy to include when it is more widely available and when facilities have developed plans for how the results can be used to inform operational strategies to reduce transmission risk.
The findings in this report are subject to at least six limitations, each of which could result in an underestimation of the number of COVID-19 cases in correctional facilities. First, only 69% of jurisdictions reported data; therefore, these results are not representative of the entire United States. Second, many facilities do not provide testing to staff members, making data completeness dependent on staff members self-reporting their diagnosis to their employer after being tested by their personal health care providers. Third, some jurisdictions received data only from state prisons and were missing data from local jails and federal or privately operated facilities. Fourth, data on the total number of facilities, the total number of incarcerated and detained persons, and the total number staff members were not available; thus, proportions of facilities and persons affected could not be determined. Fifth, one jurisdiction reported only collecting data on facility outbreaks (defined by the jurisdiction as >1 COVID-19 case per facility). Finally, data are not available to determine the extent to which variations in testing availability and testing practices across states influenced the number of COVID-19 cases reported among staff and incarcerated and detained persons.
Prompt identification of COVID-19 cases and consistent application of prevention measures are critical to protecting incarcerated and detained persons, correctional and detention facility staff members, and the communities to which they return ( 3 ). Additional data on COVID-19 in correctional and detention settings, particularly from facilities that have conducted broad-based testing, is needed to identify differences in disease risk based on demographic characteristics, underlying medical conditions, and type of correctional and detention setting, and to evaluate the effectiveness of mitigation measures. CDC recommends that facility administrators, with the support of local health departments and partners, prepare for potential SARS-CoV-2 transmission, implement prevention measures, and follow guidance for the management of suspected and confirmed COVID-19 cases to prevent further transmission, which is available at https://www.cdc.gov/coronavirus/2019-ncov/community/correction-detention/guidance-correctional-detention.html ( 3 ).
Acknowledgments
State, local, and territorial health departments and departments of corrections; affected facilities; Kathryn Arnold, Johnni Daniel, Bradley Goodwin, Sean M. Griffing, Diane M. Harris, Katherine Hendricks, Mary M. Jenkins, Kathleen H. Krause, Eva Leidman, Gary Lowry, Erin Parker, Dale Rose, Sharon Saydah, De’Lisa Simpson, CDC COVID-19 Emergency Response.
Corresponding author: Megan Wallace, [email protected] .
1 CDC COVID-19 Emergency Response; 2 Epidemic Intelligence Service, CDC; 3 Alabama Department of Public Health; 4 State of Alaska Department of Corrections; 5 Alaska Division of Public Health; 6 Arizona Department of Health Services; 7 Arkansas Department of Health; 8 California Department of Public Health; 9 Connecticut Department of Public Health; 10 Georgia Department of Public Health; 11 Kansas Department of Health and Environment; 12 Office of Public Health, Louisiana Department of Health; 13 Massachusetts Department of Public Health; 14 Michigan Department of Corrections; 15 Michigan Department of Health and Human Services; 16 Minnesota Department of Health; 17 North Dakota Department of Health; 18 Nebraska Department of Health and Human Services; 19 New Jersey Department of Corrections; 20 New Mexico Association of Counties; 21 New Mexico Department of Health; 22 New York State Department of Corrections and Community Supervision; 23 Oklahoma State Department of Health; 24 Oregon Health Authority; 25 Physician Correctional, San Juan, Puerto Rico; 26 South Carolina Department of Health and Environmental Control; 27 South Dakota Department of Health; 28 Texas Department of State Health Services; 29 U.S. Virgin Islands Department of Health; 30 Utah Department of Health; 31 Virginia Department of Health; 32 Vermont Department of Health; 33 Washington Department of Corrections; 34 Wisconsin Department of Corrections; 35 Wyoming Department of Health; start highlight 36 Florida Department of Health .
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
* These authors contributed equally.
† Correctional facilities refer to state and federal prisons, which incarcerate persons who have been tried for a crime, convicted, and sentenced for a duration >1 year. Those convicted of federal crimes are incarcerated in federal prisons; those convicted of state crimes are held in state prisons. Detention facilities refer to jails or detention centers, which temporarily detain persons awaiting sentencing or deportation, usually for a duration of <1 year.
- Bureau of Justice Statistics. Key statistic: total correctional population. Washington, DC: US Department of Justice, Bureau of Justice Statistics; 2018. https://www.bjs.gov/index.cfm?ty=kfdetail&iid=487 external icon
- Bick JA. Infection control in jails and prisons. Clin Infect Dis 2007;45:1047–55. CrossRef external icon PubMed external icon
- CDC. Interim guidance on management of coronavirus disease 2019 (COVID-19) in correctional and detention facilities. Atlanta, GA: US Department of Health and Human Services, CDC; 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/correction-detention/guidance-correctional-detention.html
- Arons MM, Hatfield KM, Reddy SC, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Eng J Med 2020. Epub April 24, 2020.
Abbreviation: COVID-19 = coronavirus disease 2019. * Jurisdictions reporting at least one laboratory-confirmed COVID-19 case among incarcerated or detained persons or staff members. † Data provided to CDC during April 22–28, 2020.
BOX. COVID-19 guidance for correctional and detention facilities
Prepare for COVID-19
- Update an emergency plan for COVID-19 response
- Coordinate with local public health department and other correctional and detention facilities
- Require that staff members and visitors stay home if ill, and consider suspending in-person visitation
- Ensure access to soap at no cost to encourage frequent handwashing
- Plan for how space will be used to medically isolate and care for ill persons and to quarantine close contacts
- Plan for potential staff member shortages
- Train staff members to safely use personal protective equipment
- Enhance facility cleaning and disinfection
Prevent introduction of COVID-19 into facilities from the community
- Limit nonmedical transfers into and out of the facility
- Screen all new entrants, staff members, and visitors for symptoms before they enter the facility
- Assign staff members to consistent locations to limit movement between facility areas
- Encourage daily use of cloth face coverings by incarcerated or detained persons and staff members
- Use multiple physical distancing strategies (e.g., sleep head to foot, stagger meals and showers, reduce the number of persons allowed in a common area at one time, suspend group gatherings*)
- Regularly communicate with staff members and incarcerated or detained persons about COVID-19 and how they can protect themselves and others
Manage COVID-19 in facilities
- Activate emergency plan and notify public health officials
- Medically isolate ill persons and quarantine close contacts
- Evaluate ill persons for underlying medical conditions that would increase their risk for severe illness from COVID-19, † and provide necessary care on-site or transfer to a health care facility
- Incorporate screening for COVID-19 symptoms into release planning §
- Continue activities from preparation and prevention phases
Abbreviation: COVID-19 = coronavirus disease 2019.
* Other suggestions available in full corrections guidance. https://www.cdc.gov/coronavirus/2019-ncov/community/correction-detention/guidance-correctional-detention.html .
† Asthma, chronic lung disease, diabetes, serious heart conditions, chronic kidney disease being treated with dialysis, severe obesity, age ≥65 years, immunocompromising conditions, and liver disease. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/groups-at-higher-risk.html .
§ Additional guidance on SARS-CoV-2 testing in correctional and detention facilities will be provided as testing becomes more widely available and strategies are developed to assist facilities in using test results to inform their operational efforts to reduce transmission risk.
Suggested citation for this article: Wallace M, Hagan L, Curran KG, et al. COVID-19 in Correctional and Detention Facilities — United States, February–April 2020. MMWR Morb Mortal Wkly Rep 2020;69:587–590. DOI: http://dx.doi.org/10.15585/mmwr.mm6919e1 external icon .
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services. Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services. References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of pages found at these sites. URL addresses listed in MMWR were current as of the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version ( https://www.cdc.gov/mmwr ) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
COVID-19 in Prisons and Jails in the United States
- 1 Cambridge Health Alliance, Cambridge, Massachusetts
- 2 Harvard Medical School, Boston, Massachusetts
- 3 Hunter College, City University of New York, New York, New York
- Research Letter COVID-19 Cases and Deaths in Federal and State Prisons Brendan Saloner, PhD; Kalind Parish, MA; Julie A. Ward, MN, RN; Grace DiLaura, JD; Sharon Dolovich, JD, PhD JAMA
- Viewpoint COVID-19, Decarceration–– A NASEM Report on the Role of Clinicians, Health Systems, and Payers Emily A. Wang, MD, MAS; Bruce Western, PhD; Donald M. Berwick, MD, MPP JAMA
- Research Letter COVID-19 Incidence and Mortality in Federal and State Prisons Compared With the US Population, April 5, 2020, to April 3, 2021 Neal Marquez, MPH; Julie A. Ward, MN, RN; Kalind Parish, MA; Brendan Saloner, PhD; Sharon Dolovich, JD, PhD JAMA
- In the News National Academies Report Urges Reducing Inmate Population to Curb COVID-19 in Prisons, Jails Joan Stephenson, PhD JAMA Health Forum
In mid-March 2020, the first case of novel coronavirus 2019 (COVID-19) was diagnosed at Riker’s Island, the main jail complex in New York City. Within 2 weeks, more than 200 cases were diagnosed within the facility, despite efforts to curb the spread. The situation at the Cook County jail in Chicago is similar, with about 350 incarcerated persons and staff members testing positive for the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus as of early April 2020. Many other jails and prisons have reported outbreaks of COVID-19 and related deaths.
Prior viral epidemics have wrought havoc in carceral settings. An account from San Quentin prison detailing the Spanish influenza of 1918 estimated that half of the 1900 inmates contracted the disease during the first wave of the epidemic; sick calls increased from 150 to 700 daily. Contrary to protocol, most of the ill were kept in the general prison population because the hospital ward was full. 1
At present, jails (which house individuals awaiting trial or serving short sentences) and prisons (which house individuals who have been convicted of crimes and are serving longer sentences) are usually crowded. When they are unable to adhere to measures needed to contain and mitigate a viral epidemic, incarcerated persons, staff, and the wider community are endangered.
The Challenge of Social Distancing in Prisons and Jails
At San Quentin, a single incoming prisoner initiated each wave of the 1918 epidemic. Once introduced, the disease spread rapidly as a result of the inmates’ close confinement and an inability to isolate the sick. The COVID-19 outbreak on the Diamond Princess cruise ship provides a contemporary analogy. With about 3700 passengers and crew held on board in separate but close quarters, about 700 people became infected and 12 died over a 4-week period. The rapid spread was attributed to a small number of kitchen workers housed together on Deck 3, who were responsible for feeding the quarantined passengers. 2 The infrastructure of most prisons and jails is similarly conducive to spreading disease. Moreover, people who are incarcerated will be at higher risk of exposure, as correctional officers and other staff frequently leave the facility and then return. In prisons and jails, social distancing is typically a physical impossibility.
Prisoners at High Risk for Severe Infection and Death
The elderly, and persons with underlying illnesses, are at high risk of severe illness and mortality from SARS-CoV-2 infection. As a result of longer sentences (mostly for non-violent offenses), the average age of the prison population has increased. In 2013, state prisons housed 131 500 persons older than 55 years, a 400% increase since 1993. Many incarcerated persons older than 55 years have chronic conditions, such as heart and lung diseases. 3 About half of the people incarcerated in state prisons have at least 1 chronic condition; 10% report heart conditions, and 15% report asthma, percentages far greater than those for the population at large, even when comparing similar age groups. 3
Effects on Prison Health Care Systems
Few US prisons have health care systems able to accommodate a surge in sick calls similar to the situation at San Quentin during the Spanish influenza epidemic. Crowding and clinical vulnerability compound the barriers to adequate health care inherent in carceral settings. Although the US Constitution guarantees a right to health care for people who are incarcerated, available medical care varies greatly with regard to both access and quality, and services have been challenged by the increased needs of the aging prison population. 4 Incarcerated persons may be charged co-payments that are high relative to their wages, and this will deter their seeking care, although little revenue is generated. Moreover, when incarcerated persons do seek care, they often face long wait times for visits. The costs of hospital care, which prison systems bear, is a disincentive to referrals; several states have been scrutinized for providing substandard hospital-level care within their correctional systems. 5
Solutions to Mitigate Harms
Even before COVID-19 cases were detected in prisons and jails, clinicians and advocates for incarcerated persons proposed measures to ameliorate the anticipated harms, such as the wide availability of protective equipment, testing and medical care, and the elimination of co-payments and other policies that may deter inmates from seeking care. Although these actions are essential, the most effective way to avoid an imminent outbreak, is, as others have argued, to drastically reduce the populations of jails and prisons. 6 Criminal justice systems can accomplish this by reducing unnecessary jail admissions and expediting prison release. Some prosecutors are already adjusting prosecutorial standards to reduce jail admissions and the length of stays. In Baltimore, prosecution of all drug possession and other minor crimes is being deferred. In San Francisco the district attorney has ordered the release of all persons in pretrial detention (who would be eligible for bail if they could afford it). 7 These steps may reduce crowding in some jails, but many other jails—and most prisons—are minimally affected.
Additional measures are required to reduce prison and jail populations. These include the release of those at high risk from COVID-19 owing to age or underlying conditions, those convicted of a nonviolent crime or incarcerated on a technical (crimeless) parole violation, and those with less than 2 years of their sentences remaining. In April 2020, US Attorney General William Barr ordered the release of many such persons incarcerated in federal prisons; it is unclear, however, how efficiently this order will be executed. 8
Criminology data suggest that these steps would pose little risk to public safety. Those older than 65 years are very unlikely to reoffend. Moreover, long sentences required by sentencing guidelines in accordance with state and federal laws have not been shown to enhance public safety; many prisoners nearing the end of their sentences have already served long periods of time.
Preparing for Release Into the Community
In the 2 weeks following release from incarceration, people are at increased risk of death, particularly from drug overdose and cardiovascular disease. 9 If more people are to leave prisons and jails, correctional officials and community members should take steps to mitigate these risks. Pharmacologic treatment for opioid use disorder is now available via telemedicine, and all prisoners who might benefit from such programs should be referred to them. Similarly, older prisoners and those with chronic health conditions should have pre-arranged primary care follow-up, and the means (eg, an appropriate computer or smartphone) to engage in telehealth visits.
Those who are released from prison and are at risk for homelessness require additional measures and resources. In Connecticut, a widespread effort to provide housing for the homeless in hotels has emptied shelters, which are high-risk environments for SARS-CoV-2 transmission. 10 Additionally, streamlining access to and broadening eligibility criteria for safety net programs including Medicaid and food stamps are important.
Addressing the COVID-19 pandemic requires bold policy changes throughout society. In the criminal justice system, aggressive and proactive measures are needed to minimize the catastrophe brewing in prisons and jails.
Corresponding Author: Laura Hawks, MD, Department of Medicine, Cambridge Health Alliance, 1493 Cambridge St, Cambridge, MA 02143 ( [email protected] ).
Published Online: April 28, 2020. doi:10.1001/jamainternmed.2020.1856
Conflict of Interest Disclosures: None reported.
See More About
Hawks L , Woolhandler S , McCormick D. COVID-19 in Prisons and Jails in the United States. JAMA Intern Med. 2020;180(8):1041–1042. doi:10.1001/jamainternmed.2020.1856
Manage citations:
© 2024
Artificial Intelligence Resource Center
Best of JAMA Network 2022
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Advertisement
Supported by
Federal Prisons Will Let Inmates Have Visitors During Pandemic
Some workers and families say they fear that the coronavirus will spread after the nation’s largest prison system allows visitors beginning on Saturday.
- Share full article

By Maura Turcotte and Libby Seline
Relatives and friends will be permitted once again to begin visiting inmates in federal prisons as of Saturday, six months after such visits were ended over concerns about the coronavirus pandemic.
Federal prisons officials said they were resuming family visits based on “the importance for inmates to maintain relationships with friends and family,” and some relatives of inmates lauded the decision.
“Their miserable circumstances need some relief,” Christy Balsiger, whose husband is in a federal prison in Texas, said, adding that family visits are vital for the psychological well-being of inmates.
But the coronavirus has hit prisons particularly hard, and some prison workers and families questioned whether outside visits — and the risk of further spread from inside and outside of facilities — were wise.
“I lost my mind when they said that,” said Aaron McGlothin, a warehouse foreman and union official at a federal prison in California. He said he feared that the resumption of visits would lead to more illness and death. “I was just like, ‘Are you kidding me?’”
There have been nearly 20,000 virus infections and 134 deaths among federal inmates and guards since the start of the pandemic, according to a New York Times database tracking infections in American prisons, jails and detention centers. The federal system currently has 1,813 active cases among inmates and 733 active cases among staff members, according to the authorities.
In a far broader array of correctional and detention facilities — federal, state and local — at least 226,320 inmates and guards have been infected and 1,321 have died, according to the Times database. Most state prison systems and local jails are continuing to bar family visits.
Under the federal prison system’s new rules , no physical contact with visitors — including children — will be permitted, and guards will check the temperatures of visitors before they are allowed to enter.
Inmates and visitors will be required to wear face coverings and to maintain distance, either by partitions or by spacing people at least six feet apart.
The federal prison system “is committed to protecting the health and welfare of those individuals entrusted to our care, as well as our staff, their families, and the communities where we live and work,” the agency said in a statement.
Inmates and prison officials have said the inability of inmates to see loved ones — combined with the fear of becoming sick and having been largely restricted to cells or crowded dormitories — had exacerbated existing mental illnesses.
But not everyone is pleased with the return of in-person visits.
Mr. McGlothin, the federal prison employee in California, said that when he went to officials with concerns about the risks of renewed visits, he was told that the new partitions would help and that the plan would be safe.
“I said, ‘Safe for who?’” Mr. McGlothin said.
Even some families were reluctant.
Nina Schunck said that she and her daughter, an inmate at a federal prison in West Virginia, had discussed a visit but ultimately decided against it.
“She does not want me to go because she is afraid of transmission,” Ms. Schunck said. “They just had their first positive case there. So she’s worried about that on both counts — that people will bring it in, or that people will get it while they’re there.”
She added: “The timing is just weird to me because it’s still continuing to spread. There’s no stop — every day, another prison.”
At Butner federal prison in North Carolina, Barry Taylor, an inmate, said fears about extending a remarkably deadly six-month stretch at the prison had led inmates and families to decide visits were too risky. If inmates become infected, they are typically placed in isolation units or grouped with other ill prisoners and have limited access to showers, phone calls, hot meals, fresh air and exercise.
The Butner prison has had 1,047 infections of inmates and guards and 27 deaths.
“We’re supposed to self-monitor and turn ourselves in to be quarantined if we feel sick,” Mr. Taylor wrote in an email. “Very few inmates will give up TV, commissary and rec for solitary confinement when we can treat ourselves with the same meds the BOP is providing in quarantine.”
Melissa Lynn McGee, an inmate at Carswell federal prison medical center in Texas, said she was recovering from the virus.
She said she feared that family visits would lead to widespread illness and plunge the facility back into the sort of desperation and chaos that marked the summer months. Six inmates have died at the prison and 547 have been infected.
“Even if the visitor doesn’t have a temperature doesn’t mean they haven’t been exposed in some way,” she said.
Reporting was contributed by Izzy Colón, Brendon Derr, Rebecca Griesbach , Danya Issawi , Ann Hinga Klein, K.B. Mensah and Timothy Williams
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 11, Issue 5
- Scoping review of mental health in prisons through the COVID-19 pandemic
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-5585-9512 Luke Johnson 1 ,
- Kerry Gutridge 2 ,
- Julie Parkes 1 ,
- Anjana Roy 3 ,
- Emma Plugge 1 , 3
- 1 Department of Primary Care, Population Sciences and Medical Education , University of Southampton Faculty of Medicine , Southampton , UK
- 2 Centre for Women’s Mental Health, Division of Psychology and Mental Health, School of Health Sciences , The University of Manchester Faculty of Biology Medicine and Health , Manchester , UK
- 3 Health and Justice Team, Alcohol, Drugs, Tobacco and Justice Division , Public Health England , London , UK
- Correspondence to Dr Luke Johnson; l.johnson{at}soton.ac.uk
Objective To examine the extent, nature and quality of literature on the impact of the COVID-19 pandemic on the mental health of imprisoned people and prison staff.
Design Scoping review.
Data sources PubMed, Embase, CINAHL, Global Health, Cochrane, PsycINFO, PsychExtra, Web of Science and Scopus were searched for any paper from 2019 onwards that focused on the mental health impact of COVID-19 on imprisoned people and prison staff. A grey literature search focused on international and government sources and professional bodies representing healthcare, public health and prison staff was also performed. We also performed hand searching of the reference lists of included studies.
Eligibility criteria for selection of studies All papers, regardless of study design, were included if they examined the mental health of imprisoned people or prison staff specifically during the COVID-19 pandemic. Imprisoned people could be of any age and from any countries. All languages were included. Two independent reviewers quality assessed appropriate papers.
Results Of 647 articles found, 83 were eligible for inclusion, the majority (58%) of which were opinion pieces. The articles focused on the challenges to prisoner mental health. Fear of COVID-19, the impact of isolation, discontinuation of prison visits and reduced mental health services were all likely to have an adverse effect on the mental well-being of imprisoned people. The limited research and poor quality of articles included mean that the findings are not conclusive. However, they suggest a significant adverse impact on the mental health and well-being of those who live and work in prisons.
Conclusions It is key to address the mental health impacts of the pandemic on people who live and work in prisons. These findings are discussed in terms of implications for getting the balance between infection control imperatives and the fundamental human rights of prison populations.
- mental health
- public health
- health policy
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study. All relevant review information in supplementary material. No primary data analysed.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2020-046547
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
The first scoping review of mental health in prisons during the COVID-19 pandemic.
We report our rigorous methodology in the format of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews to improve our review’s transparency, accuracy and completeness.
Our search strategy and inclusion criteria were broad, identifying comprehensively the relevant literature with clear implications for research and policy.
The review identified key challenges to mental health in prisons during the pandemic for further research.
The primary limitation of the study is the limited and low-quality research available within this review, which therefore means it is difficult to draw firm conclusions from the findings.
Introduction
In March 2020, the WHO declared a COVID-19 pandemic. 1 As of 31 March 2021, there have been more than 127 million confirmed infections worldwide with SARS-CoV-2, resulting in more than 2.5 million deaths. 2
There are over 11 million people imprisoned globally. 3 This population is particularly susceptible to COVID-19 because of overcrowded, poorly ventilated and often insanitary environments and suboptimal healthcare services. Frequent staff changeover and movement of imprisoned people in and out of and between prisons contribute to multiple entry points for COVID-19 and the potential for rapid spread once introduced. 4 5
Imprisoned people are at high risk for severe COVID-19 due to a high burden of chronic diseases, such as diabetes and hypertension. Also, people from black and minority ethnic groups are often over-represented, and such individuals have a poorer prognosis. 6 7 It is therefore clear that imprisoned people are at high risk for severe COVID-19, which is likely to result in significant stress and anxiety within this population. 8–12 This may be exacerbated further by the infection prevention and control measures in prisons, which focus on restricting prisoner access to each other and outside visitors. 13–16 Measures implemented include social distancing, cancelling all visits and limiting the time that prisoners spend outside their cell. This has resulted in imprisoned people being locked into cells for 23 hours or more each day. Comparisons could be drawn between this isolation and solitary confinement, 15 which has been shown to impact on mental health. 17 18 Furthermore, imprisoned people already have a high burden of mental health issues and substance use. 7 19 20 Prison staff also have a high burden of mental health conditions. 21 22 They face significant pressure from working in prisons, which is likely to be exacerbated by the pandemic. 9 23
We conducted a scoping review of literature related to COVID-19 and mental health in both prison staff and residents. The review aimed to examine the extent, nature and quality of literature on the impact of the COVID-19 pandemic on the mental well-being of imprisoned people and prison staff. We have also summarised and analysed the research findings and highlighted gaps in the evidence base.
Methodology
We conducted a scoping review using the methodology described by Arksey and O’Malley. 24 We adhered to the five stages of the scoping review process: (1) identifying the research question, (2) identifying relevant studies, (3) study selection, (4) charting the data and (5) collating, summarising and analysing the included literature. We have reported this review in accordance with the guidance in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews. 25
Identifying the research question
Our research question was ‘what is the extent, nature and quality of the literature on the impact of the COVID-19 pandemic on the mental health of imprisoned people and prison staff?’. We included substance misuse within the definition of mental health.
We used Ako et al ’s 26 definition of ‘prison’ as representing ‘detention facilities housing both on-remand and convicted people. These settings included prisons, police holding cells, pretrial detention, closed youth institutions and camps where drug users are forced into mandatory labour as means of rehabilitation’. We also included immigration detention centres.
Identifying relevant studies
We conducted a systematic literature search in nine databases (PubMed, Embase, CINAHL, Global Health, Cochrane, PsycINFO, PsychExtra, Web of Science and Scopus) from 2019 onwards, since this is when COVID-19 was identified. The search was carried out on 5 March 2021. These databases reflect the breadth of disciplines within this field. We kept search terms broad to maximise sensitivity (see online supplemental appendix 1 ). We also searched grey literature, focusing on official channels of information such as international and government sources and professional bodies representing healthcare, public health and prison staff. We hand-searched the reference lists of included studies.
Supplemental material
Study selection.
We screened articles by title and abstract for potentially eligible studies and obtained the full text. We included papers that met the eligibility criteria:
The article must examine the mental health of imprisoned people or prison staff, of any age and from any country in any language.
The article must look specifically at the mental health effects of the COVID-19 pandemic.
All study designs will be included.
Papers reporting research data were evaluated for research quality in line with scoping review adaptations suggested by Pham et al . 27 We used the relevant National Institutes of Health’s quality assessment tools. 28 Opinion pieces, case studies and grey literature were not quality assessed.
Charting, collating, summarising and analysing the data
We charted the data; key data were entered into a table with the following headings: author, month and year, title; study design; population described or studied; key findings; and recommendations (see online supplemental appendix 2 ). After familiarisation with the data, three authors (LJ, KG and EP) inductively identified six key themes from the data: fear of COVID-19, changes in movement and activities, changes in communication, changes in mental and substance health services, decarceration and continuity of care and the mental health of prison staff. 29 These themes were reviewed and finessed with the other authors.
Patient and public involvement
Discussions with experts with experience who had lived or worked in prisons highlighted the growing importance of mental well-being in prisons during the pandemic. However, they were not involved in the subsequent conduct of the review.
Our search returned a total of 1080 articles (see figure 1 ). After removal of duplicates and initial screening, we reviewed 280 articles in full. After reviewing these articles against our exclusion criteria, 83 papers were included (see online supplemental appendix 2 ).
- Download figure
- Open in new tab
- Download powerpoint
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart.
The majority of papers were opinion pieces, with the exception of 10 case studies, 30–39 seven guidelines, 13–16 40–42 six literature reviews, 43–48 five qualitative studies, 49–53 three cross-sectional studies, 54–56 three briefings, 57–59 three case studies 37 39 60 and one study protocol. 61 All assessed studies were found to be of poor quality (see online supplemental appendix 3 ). Of papers that were focused on a particular country, the countries included were the USA (27), the UK (8), Italy (5), Australia (5) and Canada (2) and then one from Brazil, China, Switzerland, Germany and Nigeria. One paper focused broadly on Africa and another on South America.
Many papers considered prison environments generally, but three examined juvenile correctional facilities (JCFs) in the USA, 62–64 seven looked at immigration and detention centres 8 44–46 60 65 66 and one described a mental health support programme for healthcare staff and attorneys working in prisons. 37
There was little primary data, and that which was identified was conflicting. One study found that recorded incidents of self-harm in 31 UK prisons had decreased by one-third when comparing February with April 2020. 67 However, three other studies documented higher levels of self-harm across UK prisons. 9 51 59
Fear of COVID-19
The pandemic has induced stress and anxiety in detainees over the risk to themselves and those they love contracting or dying from COVID-19. 12 39 64 68–71 This is exacerbated by awareness of their health vulnerabilities 9 and their unhygienic, overcrowded living conditions. 8 10 60 Those left after the pandemic could also experience survivor guilt and grief over loved ones who have died. 72
Changes in movement and activities
Movement of many imprisoned people has been severely restricted because of infection control measures. Those with symptoms and positive test results, new to the prison or vulnerable to severe infection are put into isolation, a practice that has negative connotations in prison for its perceived similarity to punitive solitary confinement. 35 43 47 70 73–78 Many were concerned that isolation may lead to exacerbations of mental health conditions, anger, depression, psychosis, self-harm and suicide. 39 46 56 66 72 74–76 79–84 There were also concerns that isolation in JCFs will affect young offenders’ neurological development. 63 74 85
In this context, it is important to clarify the difference between isolation and solitary confinement. 15 73–75 81 Solitary confinement refers to the confinement of prisoners for 22 hours or more a day without ‘meaningful human contact’. 86 It is used as a disciplinary sanction imposed by prison authorities but is also used as a preventative measure for the protection of the imprisoned person. Imprisoned people in isolation are removed from contact with other members of the prison, usually as an infection prevention and control measure. All prisoners should have resources to make it psychologically bearable—such as a ‘television, tablet, radio, reading materials and means of communicating with loved ones’ 73 85 87 —as well as access to health professionals and updates on the necessary length for isolation. 13 73 Unless the purpose of their isolation is well defined, prisoners may be reluctant to report symptoms. 9 73
Many prisons have significantly restricted prisoner movement regardless of COVID-19 status. 63 69 74 75 81 Together with social distancing measures, this can mean spending up to 23 hours isolated in an 8×6 foot cell each day. 59 63 74 75 This contrasts with Penal Reform International suggesting blanket isolation measures should be avoided or, if imposed, ‘only for the time required to undertake a more individualised and independent medical assessment’. 58
Many activities, including work, education and religious activities, have been stopped 59 69 75 and not substituted by recommended socially distant activities. 15 16 39 46 This is likely to have detrimental effects on mental health. 74 81 The lack of activities is a consequence of restricting staff numbers on site to minimise infection risk 63 and the logistical challenge for facilities such as gyms to clean shared equipment. 63 However, in-cell activities, including exercises, mindfulness, puzzles, videos, colouring and playing cards, offer alternatives. 9 75 88
Finally, imprisoned people are rarely attending appointments outside of prison, resulting in trials and court hearings being delayed, increased time spent on remand and likely additional distress. 39 75
Changes in communication
Many prisons have stopped visits, 11 12 39 59 62 69 74 75 89–92 which will likely negatively impact mental health. 10 12 62 69 74 81 87 89 91 Lack of contact could result in increased anxiety over the health of family members as well as prisoner’s own welfare. 69 The European Centre for Disease Prevention and Control calls for special considerations for deciding on visits when infants and children are involved. 14 However, in the USA, by early April 2020, all JCFs had suspended in-person visits, 62 and by May 2020, some women in UK prisons had not seen their children in 2 months. 59
One positive side effect of reduced visits is a reduction in drug availability and drug use in prisons as visits are a drug trafficking route. 36 57 67 Concurrently, demand for opioid substitution medication has increased, possibly to help with withdrawal symptoms. 36 57 Managing an increased number of withdrawing people has likely put additional strain on prison staff and healthcare workers.
Ensuring communication with family and friends is maintained is important. One key method by which this has happened is increased telephone access. 62 63 67 80 87 90 Additional methods include letter writing, video calls and a prison voicemail service. 10 14 62 63 69 75 81 87 88 90 However, these methods are not equally implemented or effective; different prisons have different policies and resources. 62 76 77 84 For example, secure phone handsets are only available in half of prisons in England and Wales. 75 Moreover, those with the greatest risk of self-harm and suicide are more likely to be alienated from support networks so least likely to benefit. 59 67
Communication between imprisoned people and staff is also a priority. Levels of education and health literacy are low among imprisoned people, and combined with a tight control of information within prisons, this can lead to the spread of misinformation and fear. 80 Emphasis must be placed on regular, clear communication to prisoners concerning changes in protocol. 31 43 69 87 The Royal College of General Practitioners emphasises good communication throughout their guidelines for managing COVID-19 in prisons. 40
Changes in mental and substance health services
Despite a prevailing belief that the mental health burden will increase, routine services have been deprioritised or withdrawn in many places due to infection risk. 9 54 59 62 72 93 94 This is contrary to the widespread belief that psychiatric and psychological care remains critical. 10 12 31 43 62 72 77 79 82 87 89 91 93 Adaptations include correctional staff providing psychological support, prisoner access to online counselling tools and telepsychiatry. 10 60 72 79 95 Telepsychiatry received particular note, 10 30 39 45 54 60 79 92 96 97 with recommendations for US states to waive license requirements to facilitate greater uptake. 10 98
With the reality of rationalised mental health services, articles emphasised the need to optimise triaging to ensure imprisoned people with the highest mental health risk are prioritised; suggested factors include pre-existing mental health condition, risk of harm to self or others, aggression and refusal to eat. 9 72 For the in-person mental health appointments that do take place, it is important that staff are risk-assessed and provided with personal protective equipment. 41 72 A number of articles reported how systems and processes had been modified and developed to ensure that imprisoned people were able to continue with drug treatment. 32 33 36 42 In one prison, depot buprenorphine had become first-line treatment for opioid agonist treatment (OAT). 36
Decarceration and continuity of care
Many recommended decarceration as a strategy to help reduce infection risk. 8 55 85 93 99–102 This has been implemented in several countries including Iran, Turkey, Afghanistan, France, Indonesia and Ethiopia. 92 103 104
However, there are important considerations for the mental health of those released. 75 90 105 First, they will be entering an unfamiliar environment with substantial societal changes, leading to increased stress. 68 75 Imprisoned people often have a lack of financial and social capital, lower educational attainment and higher rates of unemployment and regularly become homeless, all of which are more challenging with current restrictions. 68 98 99 105 Those who return to difficult family situations may be at risk of domestic violence, with restricted options to change living arrangements and challenges to seeking a police protective order if needed. 68 90 Second, many community services on which released prisoners often rely have been reduced, altered or discontinued, leading to challenges in accessing care. 39 68 75 90 101 One key area that needs careful planning is OAT. 15 32 40 61 99 105–107 In some areas, OAT services are now available via telemedicine, but these require prisoners to be equipped with technology and internet connection prior to release. 32 33 61 100 101
With these added complications and the rapid speed of decarceration, liaising with community services for follow-up is challenging. 16 68 75 90 105 Close attention must be paid to those released to ensure continuity of healthcare and social care. 68 75 99 101
The mental health of prison staff
The pandemic has affected the mental health of those who work in prisons. In England and Wales, prison staff absences have doubled. 75 Staff have been faced with fear of contracting the virus as well as burnout from operating with reduced numbers. 9 62 80 A diminished workforce will have implications on the mental health of imprisoned people too. 9 75 Fewer staff means less opportunity to support imprisoned people and less time to supervise those at high risk of self-harm or suicide. 75
In summary, the reported impacts on the mental health of imprisoned people are overwhelmingly negative, caused not just by fear of COVID-19, but mediated through the regime changes implemented to minimise infection risks. The key challenges can be summed up as social distancing and isolation, discontinuation of prison visits and reduced/discontinued mental health services. These impacts can be ameliorated by measures including the provision of individual and communal socially distant activities, clear communication with prisoners, decarceration, ensuring access to friends and family through telephones and video calls, effective risk assessment of the mental health of imprisoned people, telepsychiatry and socially distant in-person mental health appointments. This is summarised in figure 2 .
Summary of the challenges and solutions to prisoner mental health during COVID-19. OAT, opioid agonist treatment; PPE, personal protective equipment.
The review’s findings suggest that the pandemic has had a profound effect on the mental health of those living and working in prisons. Isolation is a huge challenge to mental health in prisons. The adverse psychological effects of solitary confinement are well documented 17 18 108 and include an increased risk of mortality 5 years after release. 108 Although the reasons for isolation are different, there are likely still negative consequences for mental health. Similarly, visitors have been shown to be positive for the well-being of imprisoned people and linked to reduced recidivism. 109 Preventing visits is therefore also likely to impact mental health. A rapid review of the psychological impact of quarantine in the wider community showed a detrimental effect on mental health in a wide-ranging and possibly long-lasting way. 110 Longer quarantine increases the severity of impact, and when a restriction to liberty is imposed rather than voluntary, it leads to more distress and greater long-term mental health complications. 110
Reduced access to health services is also likely to impact mental health. Since the pandemic started, health services in many countries have developed rapidly, with the widespread adoption of telemedicine. 111 There are, however, concerns over equity and lack of access to technology in prisons. Even in high-income countries such as the UK, at the start of the pandemic, 50 of 117 prison sites had connectivity too poor to enable video consultation. 112 With growing recognition that the pandemic is far from over, it is important to address mental health issues now. Prison riots have occurred in Brazil, Colombia, Italy and the USA, 10 12 79 which are linked to the challenges to mental health highlighted in figure 2 10 11 43 79 81 89 91 113 and demonstrate that solutions cannot wait.
The discussion around mental health in prisons throughout COVID-19 is lacking robust evidence. Considering the physical and mental health vulnerabilities of prisoners, 6 7 19 20 understanding the impact of COVID-19 and the implemented regime changes is an urgent need. Particularly in the context of mass decarceration, prisons are often places of transience, and the unaddressed mental health impact will have downstream consequences on wider society too. Currently, the prison service in England and Wales is evaluating feedback from prison residents and staff to improve management of safety and mental health as the pandemic continues. 66 67
This review has several key strengths. First, this is the first scoping review of the mental health in prisons during the pandemic. Also, through taking a systematic approach, it has identified comprehensively the relevant literature and gaps in evidence with clear implications for research and policy. However, the poor quality of articles included means that the findings are not conclusive.
More research is urgently needed not only to gain an in-depth understanding of the mental health impact in prisons but also to identify effective interventions. Research also needs to examine the impacts of decarceration. Recently released prisoners are at a high risk of mortality, particularly from drug-related deaths. 114 Given that drug-related sentences are one of the most common sentences being commuted, 68 104 it is important to examine how continuity of care is best maintained on release. The lack of research on prison staff and imprisoned women is notable and should also be addressed.
Prisons should consider the mental well-being of their residents and staff. There needs to be greater provision of in-cell activities and expansion of electronic communications to enable imprisoned people to communicate with health professionals and family and to enable courts to function remotely to prevent the backlog of trials. There must be clear communication with imprisoned people and staff about the public health measures taken so that they know what to expect. These measures, while enabling infection control, must be kept to a minimum to ensure the protection of prisoners’ human rights. Healthcare staff have an important role to play in identifying and monitoring the well-being of vulnerable people, maintaining services and responding to health needs. Releasing large numbers of people into the community creates problems for these individuals and requires adequate protections such as appropriate housing and links into health services. All these measures must be underpinned by strong leadership and collaborative working across prison systems, non-governmental organisations and healthcare and social care partners.
The impact of COVID-19 on the mental health of imprisoned people and prison staff is likely to be profound, related not only to fear of COVID-19 but also as a consequence of instituting infection prevention and control measures. Although essential, these must be kept to a minimum and mitigation strategies to maintain mental well-being implemented alongside them. In March 2020, the WHO noted, ‘People in prisons and other places of detention are not only likely to be more vulnerable to infection with COVID-19; they are also especially vulnerable to human rights violations’. Given the evidence of impact so far and the reality that this pandemic is far from over, there is an urgent need for action alongside further research to address the adverse mental health consequences of the pandemic on those who live and work in prisons.
Acknowledgments
We would like to thank Kelsey Johnson for helping develop the framework image (figure 2) for understanding mental health in imprisoned people throughout COVID-19, and Thiago Bento and Gracia Fellmeth for translations.
- World Health Organization
- World Prison Brief
- Wallace M ,
- Curran KG , et al
- Zou B , et al
- Baillargeon J
- Garcini LM ,
- Domenech Rodríguez MM ,
- Mercado A , et al
- Kothari R ,
- Forrester A ,
- Greenberg N , et al
- Robinson LK ,
- Heyman-Kantor R ,
- Angelotta C
- D'Angiolella G ,
- Gratteri S ,
- Sacco MA , et al
- Ministry of Justice and Public Health England
- European Centre for Disease Prevention and Control
- Centers for Disease Control and Prevention
- Arrigo BA ,
- Goldberg P ,
- Landre MF , et al
- Ferdik FV ,
- Clements AJ ,
- Tricco AC ,
- Zarin W , et al
- Mhlanga-Gunda R , et al
- Greig JD , et al
- National Institutes of Health
- Burton PRS ,
- Morris NP ,
- Hirschtritt ME
- di Giacomo E ,
- de Girolamo G ,
- Peschi G , et al
- Donelan CJ ,
- Potee RA , et al
- Sanders N ,
- Schiff M , et al
- Ruchman SG ,
- Katz CL , et al
- Roberts J ,
- Attalla D , et al
- Weingarten K ,
- Galván-Durán AR ,
- D'Urso S , et al
- Ogunwale A ,
- Majekodunmi OE ,
- Ajayi SO , et al
- Lancelevée C ,
- Eck M , et al
- Royal College of General Practitioners
- Royal College of Psychiatrists
- Keppler K ,
- Carvalho SGde ,
- Santos ABSD ,
- Chaimowitz GA ,
- Géa LP , et al
- Pedrosa AL ,
- Bitencourt L ,
- Fróes ACF , et al
- Stephenson T ,
- O'Moore Éamonn , et al
- Chevance A ,
- Gourion D ,
- Hoertel N , et al
- Gonçalves LC ,
- Weber M , et al
- Maycock M ,
- ↵ . CAPPTIVE: Covid-19 Action Prisons Project: Tracking Innovation, Valuing Experience. How prisons are responding to Covid-19 Briefing #2: Regimes, reactions to the pandemic, and progression . UK Prison Reform Trust ; 2021 .
- Testoni I ,
- Francioli G ,
- Biancalani G , et al
- ↵ . CAPPTIVE Covid-19 Action Prisons Project: Tracking Innovation, Valuing Experience. How prisons are responding to Covid-19. Briefing #3: The prison service’s response, precautions, routine health care, disabilities, well-being, mental health, self-harm, and what helped . UK Prison Reform Trust ; 2021 .
- Bandara S ,
- Kennedy-Hendricks A ,
- Merritt S , et al
- Marmolejo L ,
- Barberi D ,
- Bergman M , et al
- Novisky MA ,
- Narvey CS ,
- European Monitoring Centre for Drugs and Drug Addiction
- Penal Reform International UK
- HMP Chief Inspector of Prisons
- Stopka TJ ,
- Pivovarova E
- Hedrick K ,
- Borschmann R
- Pan L , et al
- Shepherd A , et al
- Sánchez A ,
- Diuana V , et al
- Barnert E ,
- Sabourin H ,
- Liebrenz M ,
- Augustine D , et al
- Dutheil F ,
- Bouillon-Minois J-B ,
- Clinchamps M
- Shepherd A ,
- Hard J , et al
- Distancing S
- Montoya-Barthelemy AG ,
- Cundiff DR , et al
- Stewart A ,
- Goncalves Junior J ,
- Mitchell SM ,
- La Rosa NL ,
- Eamranond PP
- United Nations Office on Drugs and Crime
- Brelje AB ,
- Pinals DA ,
- Shepherd S ,
- Wurcel AG ,
- Zaller N , et al
- Thibaut F ,
- Anosike UG ,
- Ogunwusi JF , et al
- Zielinski MJ ,
- Hinton KE ,
- Oladeru OT ,
- Al-Rousan T , et al
- Taylor PJ ,
- Forrester A , et al
- Robinson L ,
- Khalifa N , et al
- Crowley D ,
- O'Donnell P , et al
- Woolhandler S ,
- McCormick D
- Sivashanker K ,
- Rossman J ,
- Resnick A , et al
- Mukherjee TI ,
- El-Bassel N
- Wildeman C ,
- Andersen LH
- De Claire K ,
- Brooks SK ,
- Webster RK ,
- Smith LE , et al
- Hayward A ,
- Whitfield A , et al
- Pattavina A ,
- Palmieri MJ
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
- Data supplement 3
LJ and KG are joint first authors.
Contributors The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. LJ and EP conceived the study. LJ performed the search, and LJ and KG screened articles and assessed their quality. EP acted as coreviewer and quality assessor. All authors contributed substantially to the interpretation of the findings. LJ produced the first draft, and KG, EP, JP and AR revised critically the content. All authors approved the final manuscript. LJ is the overall content guarantor.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
The Impact of COVID-19 in US Prisons
By daniel mcgee.

On April 20, 2021, Commonwealth Honors College co-sponsored “The Pandemic behind Bars: COVID in the US Prison System.” Moderated by University of Massachusetts journalism professor Razvan Sibii, the event welcomed five panelists from across the United States to reflect upon the immense, disproportionate effects that the COVID-19 pandemic has had on prison institutions across the United States.
Before the panel discussion kicked off, event organizer Claire Healy ’21, a member of the UMass Prison Abolition Collective, reflected upon the guilty verdict of the Derek Chauvin trial and its potential to create reform.
“It is a decision that has been building up for a year and will continue to build with other decisions and implications,” Healy said. “The trial, in which we’ve seen the systemic racism of the US criminal justice system and entirety of police brutality tried, analyzed, and defended, has been painful and difficult, historical, traumatic, and deeply personal for so many people here and around the world.”
Professor Sibii then allowed each guest to introduce themselves and their work within the field. Panel members ranged from academics who study mass incarceration, to social activists and journalists, some of whom were formerly incarcerated.
Main themes of discussion focused on a lack of information given by prisons and the importance of advocacy from those on the outside. The recently freed panelists found common ground in a sense of survivor's guilt toward those still undergoing the unequal treatment of the incarceration system, especially during the pandemic.
Among the panelists was Eugene Youngblood, a member of the Black Prisoners’ Caucus and coordinator for The Freedom Project , who was recently commuted after serving nearly thirty years. Youngblood experienced COVID-19 in prison firsthand, contracting the disease along with over 300 others in his housing unit while still serving his sentence, just a month after he was granted clemency,
As a result, prisoners were put into “medical isolation.” The emotional toll of his experience nearly matched the physical battle his body went through.
“We’re sick and we were just placed in isolation,” Youngblood said. “I didn’t get any fresh air, wasn’t able to move around, the light was on twenty-four hours a day, so I couldn’t sleep. All these things exacerbated COVID. It got so bad, I had to go to the hospital and get oxygen treatment.”
Kathryn M. Nowotny, co-founder of the COVID Prison Project and an assistant professor of sociology at the University of Miami, brought a data-based, epidemiological approach to the discussion. Her work at the COVID Prison Project tracks and monitors coronavirus data in correctional facilities across the country.
According to Nowotny, at least 390,000 people in US prisons have been infected with COVID-19, representing 30 percent of the prison population. Of this number, at least 2,500 have died from COVID-19. Both numbers are likely an undercount due to inaccuracies within the system and a backlog of data reporting.
“All prison systems report data in very different ways; there’s no centralization or oversight in what they’re reporting,” Nowotny said. “In most states, the COVID-19 case rate in prisons dwarfs the case rate in the community.”
Page Dukes is a communications associate at the Southern Center for Human Rights and a core organizer for the online memorial service Mourning Our Losses , which memorializes those who have died of COVID-19 in prison. Dukes was previously incarcerated for ten years.
“We set up to name the people who are dying [of COVID-19 in prisons] to not be remembered as numbers on a dashboard,” Dukes said of Mourning Our Losses’ mission. “But as people with family members, loved ones, lives, and a right to exist just as much as anyone else.”
Panelists also emphasized the lack of vaccine information given to those incarcerated. This lack puts importance on the advocacy of outside organizations to represent and help those inside.
“Information is important, it is critical,” said Ernst Fenelon Jr., an author, public speaker, and program coordinator with the Prison Education Project , who was formerly incarcerated for over fourteen years. “Having informed choices, you’ll find the majority [of prisoners will take the vaccine]. And those that don’t, you can address them in a way that is effective and will respect their agency.”
During the pandemic, Fenelon Jr. helped community-based organizations donate PPE to prisons in the absence of state-provided help.
“It’s so important that [all the panelists] are here,” Fenelon Jr. said. “All of us are part of this experience and conversation to advocate for those who cannot advocate for themselves.”
Jesse Vasquez, who works at a community food distribution center, served as the editor-in-chief of San Quentin News while incarcerated for nineteen years. Vasquez, who was commuted, recently received a grant that gave housing to seventy formerly incarcerated individuals, which is often hard to find for those exiting the system.
“For me, it’s one of those things where I owe it to the guys who are inside to try and help their families,” Vasquez said. “Try to feed them, try to house them, try to contribute as much as I can to them.”
Panelists agreed that if anything positive came out of dealing with the pandemic, it's that society is more likely to recognize people’s humanity and question wrongdoings, such as systemic and institutional racism.
“If there’s any silver lining to the COVID pandemic, it’s the fact that society now has to look at this ugliness and say, ‘How do we address it?,'” Vasquez said. “How do we address systemic racism? How do we address institutional racism? How do we become a more humane society from a cultural perspective? You can change the institutions but racism isn’t going to go away.”
To view the full presentation, a recording is available on the Prison Abolition Collective's YouTube page.

Global footer
- ©2024 University of Massachusetts Amherst
- Site policies
- Non-discrimination notice
- Accessibility
- Terms of use
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Incarceration and COVID-19: Recommendations to Curb COVID-19 Disease Transmission in Prison Facilities and Surrounding Communities
Lauren jeanne natoli.
1 Public Health Division, AIDS Healthcare Foundation, Los Angeles, CA 90046, USA; [email protected] (A.C.S.-C.); [email protected] (W.E.-C.)
Kathy Linh Vu
Adam carl sukhija-cohen, whitney engeran-cordova, gabriel maldonado.
2 TruEvolution, Riverside, CA 92501, USA; gro.noituloveurt@mleirbag
Scott Galvin
3 City of North Miami City Council, Miami, FL 33161, USA; moc.vlagttocs@ttocs
William Arroyo
4 California Rehabilitation Oversight Commission, California Department of Corrections and Rehabilitation, Sacramento, CA 95811, USA; ten.llebcap@oyorramw
5 Department of Psychiatry and Behavioral Sciences, Keck School of Medicine, University of Southern California, Los Angeles, CA 90089, USA
Cynthia Davis
6 College of Medicine & College of Science and Health, Charles R. Drew University of Medicine and Science, Los Angeles, CA 90059, USA; ude.uwerdc@sivadaihtnyc
Overcrowding can increase the risk of disease transmission, such as that of SARS-CoV-2 (COVID-19), within United States prisons. The number of COVID-19 cases among prisoners is higher than that among the general public, and this disparity is further increased for prisoners of color. This report uses the example case of the COVID-19 pandemic to observe prison conditions and preventive efforts, address racial disparities for people of color, and guide structural improvements for sustaining inmate health during a pandemic in four select states: California, New York, Illinois, and Florida. To curb the further spread of COVID-19 among prisoners and their communities, safe public health practices must be implemented including providing personal protective equipment (PPE) and testing of staff and inmates, disseminating culturally and language appropriate information regarding the pandemic and preventive precautions, introducing social distancing measures, and ensuring adequate resources to safely reintegrate released prisoners into their communities.
1. Introduction
The media often highlights the dangers of SARS-CoV-2 (COVID-19) transmission in long-term care facilities and nursing homes; however, prisons are left out of the conversation despite having the most crowded living situations and limited protection measures compared to other facilities. Due to prison environments being filled beyond capacity and a constant influx of prisoners, prisons are highly susceptible to COVID-19 outbreaks when compared to the general population [ 1 ]. With the current COVID-19 pandemic, incarcerated individuals, correctional staff, and surrounding communities are particularly vulnerable to contracting and spreading this novel respiratory disease.
By mid-April 2020, rates of COVID-19 in prisons surpassed that of the United States (US) general population [ 2 ]. According to August 2020 data, the case rate among prisoners was 3251 cases per 100,000 population, 5.5 times higher than the general population (587 cases per 100,000), and the crude death rate in US prisons (39 deaths per 100,000 prisoners) was also higher compared to that of the general population (29 deaths per 100,000 people) [ 2 ]. By November 2020, COVID-19 cases in prisons continued to outpace the general public; confirmed case rates in prisons were 3.7 times the national rate, with 12 in 100 prisoners infected with COVID-19 as compared to three in 100 for the general public [ 3 ].
Overcrowding in prisons is the greatest factor contributing to the higher rates of COVID-19 transmission in prisons compared to the general public [ 4 ]. In 2018, about 20% of prisons in the US were operating at or above their maximum capacity [ 3 ]. Subsequently, there have been 322,769 confirmed cases of COVID-19 among US prisoners with 1846 deaths as of January 2021. For prison staff, there have been 70,658 cases with 113 deaths [ 3 ].
To combat COVID-19 transmission during a pandemic, a comprehensive and unified public health effort is desperately needed. This paper looks at the state of COVID-19 in prisons in four US states to report on the disparities and disadvantages experienced by inmates and makes recommendations to combat future COVID-19 outbreaks in prisons and surrounding communities where prisoners are released.
2. Materials and Methods
The authors reviewed multiple sources to accurately report on prison conditions, COVID-19 statistics, and recommended guidelines for disease transmission control. Sources included COVID-19 updates from correctional department websites, newspaper articles, first-hand accounts from prisoners, and academic sources. The correctional department websites posted a regularly updated count of tests, infections, recoveries, and deaths for inmates and staff, providing a much-needed level of transparency.
The authors also reviewed public health literature from the Centers for Disease Control and Prevention, the World Health Organization, the US Federal government, universities, and nongovernmental organizations for recommendations regarding COVID-19 mitigation in prisons. Additionally, press releases from local correctional authorities, news articles, and published manuscripts gave a timeline of which public health efforts were implemented and for how long, and the ever-changing understanding of COVID-19 as of December 2020 meant that methods were often altered as new information was learned. The information was organized to create a picture of the COVID-19 pandemic in America’s prison system and provide recommendations on how to curb the crisis behind bars.
3.1. COVID-19 Conditions within Prisons
It is important that the correctional systems have proper testing and treatment in place for people being released to prevent community spread of COVID-19. As reported in the Bureau of Justice’s Annual Survey of Jails, the weekly prisoner turnover rate was 54% in 2017 [ 5 ]. Of the 10,570,300 annual admissions in 2017, the estimated average time in jail was only 26 days. This fast turnover rate means significant movement of inmates without social distancing followed by release with missed opportunities to identify and treat COVID-19. Considering this high turnover rate along with the high numbers of prison transfers, prisoners may be exposed to COVID-19 and may not even know they are infected.
One prominent example is San Quentin State Prison. Among California’s 35 prisons, San Quentin had the largest outbreak and was reported as the third largest COVID-19 cluster in the US [ 6 ]. According to the state’s Office of the Inspector General, the transfer of infected prisoners from Chino caused the outbreak because these inmates were not tested prior to transfer [ 6 ]. In total, California has reported a high number of prison-related COVID-19 cases, leading to 139 COVID-19-related deaths among prisoners [ 7 ]. As of 4 January 2021, Los Angeles County alone has reported a total of 4025 symptomatic and asymptomatic COVID-19 cases among prisoners [ 8 ].
New York reported that 3109 prison staff, 3101 prisoners, and 170 parolees had confirmed cases of COVID-19, as of 5 January 2021 [ 9 ]. Six staff members, 24 inmates, and four parolees have died from COVID-19-related deaths in New York.
Despite precautions, there have been reports from prisoners claiming that they need to be “damn near dying” for the prison staff to provide any COVID-19-related assistance or medical care [ 10 ]. Prisoners interviewed about their conditions estimated that about two-thirds of their population have experienced symptoms of COVID-19, but that the staff is slow to provide testing. Furthermore, prisoners say that, while certain areas like the cafeteria are marked for social distancing, many places such as yards, workout areas, showers, and queues are impossible to social distance.
In Florida prisons, 17,537 prisoners and 4389 prison staffers have tested positive, and 191 prisoners have died from COVID-19, as of 5 January 2021 [ 11 ]. Florida’s Baker Correctional Facility reported 266 COVID-19 cases among inmates in early August, 42% of the 630 total cases of the entire county at that time [ 12 ]. While waiting for test results after the first wave of COVID-19 testing, officers scrambled to place over 1000 prisoners in quarantine, in addition to the 483 inmates already quarantined and 24 inmates already in medical quarantine [ 12 ].
The Illinois Department of Corrections reported 8652 total cases of COVID-19 among prisoners with 50 deaths, as of 5 January 2021 [ 13 , 14 ]. In comparison to the most common COVID-19 risks in Illinois—such as poverty, race, public transportation use, and population density—the most significant predictor of COVID-19 infection in Chicago is cycling through the prison system, which is associated with 16% of all documented cases of COVID-19 in the state of Illinois and 16% in the city of Chicago, as of 19 April 2020 [ 15 ]. Statistics regarding COVID-19 in all four states are depicted below in Table 1 .
COVID-19 in prisons as of 5 January 2021—select states.
* Approximate. Note: The number of prisoners, prisoner COVID-19 cases, and prisoner COVID-19 deaths were all taken from the respective states’ correctional facilities websites as of 5 January 2021. The staff cases and deaths were taken from the respective states’ correctional facilities websites, in addition to press releases and news articles.
3.2. Precautions Taken within Prisons
In response to the San Quentin State Prison COVID-19 outbreak in California, the prison installed a large, air-conditioned tent structure able to isolate and treat up to 164 prisoners [ 6 ]. This site has since been deactivated after a significant reduction in positive COVID-19 cases [ 6 ].
As cases in New York waned from their high in the late spring of 2020, new prison programs were reintroduced with the provision that staff and attendees wear masks at all times, including while in attendance during mental health programs and counseling programs, and while at the library [ 11 ]. Visitation resumed in August 2020; however, visiting rooms were configured to reduce capacity and facilitate adequate social distancing. Physical contact between prisoners and visitors is strictly prohibited.
While other states cut back on the number of prisoners, Florida instead opted to place over 14,000 prisoners into isolation for suspected COVID-19 infection [ 11 ]. Prison conditions in Florida lack basic precautionary measures against COVID-19, including ventilation, testing, and social distancing. It has been reported that prisoners are denied COVID-19 testing unless they specifically exhibit symptoms of a fever, which excludes the myriad other symptoms related to COVID-19 [ 10 ]. As for staff, reports from Florida prisons state that staff who have been exposed to COVID-19 have still been reporting to work despite a May 2020 memo which bars staff with pending COVID-19 test results from working [ 16 ]. The combination of poor ventilation, extreme heat, withholding prisoner releases, and low COVID-19 testing sets Florida apart from the other three states discussed in this report.
Despite alarming numbers in Illinois correctional facilities, there is a lack of sanitation and personal protection equipment (PPE; e.g., facemasks and gloves) given to Illinois prisoners. Two prisoners at Statesville Prison in Crest Hill described in letters how prison conditions were facilitating the spread of COVID-19 [ 17 ]. Social distancing is impossible with so many prisoners sharing a cell. Prisoners reported that there were no products available to wipe down shared spaces, such as communal phones, in between use [ 17 ]. Other reports say that prisoners are cleaning their cells with watered down bleach and dirty rags, while prison staff enter prisoners’ cells throughout the week to do regular shakedowns where the staff touch and potentially contaminate surfaces [ 17 ]. While prisoners have limited access to PPE and hand sanitizer, guards and officers are often fully equipped with these products, leaving prisoners feeling vulnerable and unprotected.
3.3. Early Release of Prisoners and Re-Entry Support
As of January 2021, California reduced the prison population by at least 10,000, due to the COVID-19 pandemic [ 18 ]. In Los Angeles County, prisoners meeting the following conditions are qualified for early release: low risk of reoffending, less than 180 days from the end of their sentence, not serving time for domestic violence or a violent crime, and not required to register as sex offenders [ 19 , 20 ]. While the Illinois Department of Corrections quickly released inmates in the spring of 2020, fewer prisoners are being released in late 2020 than they were pre-COVID-19 [ 21 ]. In addition, there are severe age and racial disparities among early release prisoners [ 21 ].
Resources dedicated to reintegrating prisoners into society are dwindling with the surplus of prisoners being released early [ 22 ]. Although some state and county officials are calling for prisons to release prisoners, there is no extra support provided to ensure safe reintegration into society. As a result, the reentry system is overburdened with sudden releases and is scrambling to find services such as food, transportation, medical care, and housing for released prisoners, many of whom have been exposed to COVID-19 [ 22 , 23 ]. Most jurisdictions partner with community-based organizations to help reintegrate released prisoners; however, these organizations are already overburdened due to the pandemic. One nonprofit organization estimates that it costs 650 USD to transport a single person to a housing facility, including mileage, a meal, PPE, clothing, and employee wages [ 22 ]. While it is important to direct more resources to ensure the safe reintegration of released prisoners through testing and healthcare access, local jurisdictions can also help curb the spread of COVID-19 in the local community by halting or drastically reducing admissions [ 23 ].
Implementing a unified, nationwide policy is necessary to prevent infected inmates and staff from slipping through the system undetected. Instead, in the cases of many COVID-19 policies, local authorities are left to create their own systems in an unprecedented time, leaving gaps for neglect.
3.4. Racial Disparities Regarding Incarceration and Early Release
Discrimination within the prison system leads to health disparities for prisoners of color. In the context of incarceration, people of color are also more likely to be imprisoned compared to White individuals [ 21 ]. For example, in 2018, the US Department of Justice’s reported that, within Californian prisons, Black individuals were incarcerated at a rate of 592 per 100,000 population, whereas White individuals were incarcerated at a rate of 187 per 100,000 population [ 23 ].
In March 2020, US Attorney General William Barr ordered the federal prison system to release some prisoners to relieve overcrowding in penitentiaries [ 19 ]. The planning system for determining who is safest to be released from prison found white-collar offenders generally safer to release. Only 7% of Black male prisoners and 16% of Latino male prisoners were eligible for release compared to 30% of White male prisoners. Furthermore, in Illinois, White prisoners account for only 32% of the prison population, yet they account for nearly half of all pandemic-related releases [ 21 ]. In contrast, Black individuals comprise 54% of Illinois prisoners, yet account for only 45% of early releases, and Latinx individuals represent 13% of the prisoner population, yet only account for 10% of the early releases. Furthermore, lawyers and families of prisoners have claimed that the selection process regarding who will be released has not been clear; prisoners who fulfill the guidelines for release are being denied or ignored [ 21 ].
4. Recommendations
This section summarizes public health recommendations regarding COVID-19 in prisons, which can improve the state of the pandemic in prisons as the virus continues. Prisons and public health officials can pick suitable courses of actions among the following recommendations to ensure that prison facilities initiate more effective primary prevention and mitigation measures to curb the spread of COVID-19 within prison facilities and ultimately in surrounding communities where prisoners are being released.
4.1. Enforce Health Precautions
- ▪ Screen prisoners, staff, and visitors entering and exiting prison facilities for temperature, symptoms, and exposure.
- ▪ Enforce mask wearing and social distancing.
- ▪ Encourage staff to stay home when they are feeling ill.
- ▪ Clean all high-touch areas with increased frequency.
- ▪ Reduce movement of inmates within institutions and between institutions to the greatest extent possible.
4.2. Create Hygienic Environments
- ▪ Post clear and simple signage throughout prison facilities in English and Spanish that describe proper hand hygiene instructions, PPE use, and social distancing guidelines.
- ▪ Educate prisoners on COVID-19 prevention in a way that is culturally and linguistically appropriate.
- ▪ Create proper ventilation and utilize air conditioning at correctional facilities.
- ▪ Provide prisoners and staff with no-cost soap, hand sanitizer, masks, and gloves.
- ▪ Increase hand sanitizing stations in prisons, as well as access to running water for handwashing.
- ▪ Install no-touch hand dryers and trash bins.
4.3. Reducing the Prison Population
- ▪ Release prisoners booked for nonviolent offenses who have served at least 75% of their time, elderly and medically vulnerable prisoners who are not a threat to the community, and prisoners booked on technicalities and minor violations.
- ▪ Reduce overall prison population size in order to minimize overcrowding and allow for social distancing.
- ▪ Reduce incarceration and unnecessary face-to-face contact for people on parole and probation.
4.4. Ensure Data Transparency
- ▪ Keep prisoners and staff regularly informed about the number of COVID-19 cases within the facility.
- ▪ All COVID-19 mitigation signage should be made of clear, simple wording in English and Spanish, with other languages available upon request.
4.5. Limitations
This report only focused on prisons in four states, California, Florida, Illinois, and New York, all providing a spectrum of responses and public health measures; however, this may provide a narrow view of the COVID-19 pandemic’s effects considering the spread of the virus in all states. For example, Arkansas, Delaware, Ohio, Oklahoma, and Oregon have reported COVID-19 deaths behind bars that are seven times the rate of the general public, and South Dakota, Arkansas, and Kansas have reported that more than 40% of their prisoner populations have been infected [ 24 ]. Furthermore, this paper collected data during the ongoing pandemic from 5 May 2020 to 5 January 2021; COVID-19 case reports and methods of data collection may already be outdated.
5. Conclusions
The current state of COVID-19 in the US prison system is abysmal and will only worsen if the public health community does not advocate for change. October and November 2020 reported some of the largest spikes across the US in all settings, signaling that the pandemic must continue to be rigorously addressed as it was in the first few months of the pandemic. The prison system lags on reform, as prisoners are often forgotten. Some of the most basic prevention tools are close to impossible to access in prison—PPE, hand sanitizer, and handwashing—and, with overcrowding, prisoners cannot remain six feet apart from other prisoners and staff. When prisoners are released back into communities, they are without services, programs, and shelter to self-isolate. Public health advocates must depend on local government officials to address the needs of prisoners if the US is going to be able to effectively curb the spread of COVID-19 in US prisons.
Although this report specifically looks at prison conditions under the COVID-19 pandemic, the recommendations and guidelines given can be extended to general disease control protocols. The COVID-19 pandemic has proven that the US prison system is unprepared at properly controlling the spread of a contagious virus; thus, there is a need to establish federal and state guidelines to ensure the future safety of prison inmates, staff, and the surrounding communities where prisoners are released. Furthermore, these federal and state guidelines would further benefit if researchers performed cost–benefit analyses on the precautions taken to curb disease transmission in prisons.
Author Contributions
Conceptualization, L.J.N., K.L.V., C.D. and W.E.-C.; methodology, A.C.S.-C.; formal analysis, L.J.N. and K.L.V.; resources, G.M., S.G. and W.A.; writing—original draft preparation, L.J.N., K.L.V. and A.C.S.-C.; writing—review and editing, W.E.-C., C.D., G.M., S.G. and W.A.; supervision, C.D. All authors read and agreed to the published version of the manuscript.
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Conflicts of interest.
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The impact of COVID-19 prison lockdowns on children with a parent in prison
In March 2020 prisons in the UK became subject to a restricted regime with no social visits allowed. This study explored the experiences of children whose parents were in prison during the period April - June 2020 and the implications of national lockdowns in 2020 and 2021
'The impact of COVID-19 prison lockdowns on children with a parent in prison'
In March 2020 prisons in the UK put in a place a restricted regime in order to mitigate against the risks of Covid-19 within prisons. Social visits were cancelled with immediate effect. The estimated 300,000 children who experience parental imprisonment each year in England and Wales suffer a number of harms during 'normal' times and therefore to experience parental imprisonment without the possibility of face to face visits in the midst of a pandemic during which children were also experiencing lockdown in their homes, seemed likely to amplify those harms and difficulties.
Participants
Although my focus is on child centric research it was not thought right to engage directly with children during lockdown, so instead adults caring for children with an imprisoned parents were invited to fill in an anonymous questionnaire and to take part in a video interview about the experiences of the child(ren) they looked after. In that way the study explored the experiences of more than 70 children whose parents were in prison across the UK during the first lockdown in 2020.
The report 'The impact of COVID-19 prison lockdowns on children with a parent in prison' is available here
The study found that children experienced confusing and complex emotions when face to face visits were stopped. Many children thought that their parent didn’t want to see them anymore, or maybe their parent no longer loved them. Children blamed themselves for this.
Many prisons did not have video call facilities in operation until early 2021 however video-calls and phone calls between children and parents were found to be inadequate in reinforcing the bond between parent and child. Physical contact between parent and child is of great importance to the development of relationships and both younger and older children missed hugs, touch, and seeing their parent.
In many establishments, prisoners were confined to their cells for up to 23 hours each day and they reported having to choose to use the time out of their cells to, for example, either have a shower or phone their child. Added to that the cost of calls from prison remains high and some families still found it hard to pay for sufficient phone time. Prior to the pandemic many prisoners were allowed out to work and had access to a mobile phone, but that ended with the lockdown.
“They think he doesn’t care about them because he can only ring for five minutes per day”
The study found that almost all participants reported that the children were experiencing sadness and grief related to the loss of contact with their parent. Children were suffering from depression and anxiety and there were incidences of self harm and the onset of eating disorders. Almost all participants were concerned about the difficulties families would face when the parent was released, as particularly for young children, the parent was a virtual stranger.
The report shares recommendations for change made by families including In cell telephony or secured mobile phones being made available to every prisoner to enable frequent phone contact, and that the Government should provide a clear and publicly communicated roadmap for the re-establishment of prison visits, and the lifting of restrictions within prisons, at the same time as announcements are made about the rest of the community. There are also recommendations that more use should be made of the early release scheme to allow parents to serve the end of their sentences at home, and for improvements to be made to the video call facilities within prisons.
Shona Minson
See all people
- State Profiles
- Advocacy Toolkit
- Fact Sheets
Stay Informed
Get the latest updates:
Can you make a tax-deductible gift to support our work?
COVID-19 in Prisons and Jails
America's response to the covid-19 pandemic in prisons and jails was a failure. this page provides a recap of our work during this tragic time..
April, 2023
With more than half a million infections behind bars and over 3,000 deaths, America’s response to COVID-19 in prisons and jails was a failure . Federal, state, and local governments ignored public health guidance, refused to implement even the most basic mitigation strategies, and failed to reduce their incarcerated populations to the level necessary to avoid these catastrophes.
10 must-read pieces about prisons, jails, and COVID-19:
Lessons for the next pandemic, reviews of state efforts to address COVID, how mass incarceration made the pandemic worse outside of the prison walls, and more.
- Lessons from COVID-19 can help prisons & jails prepare for the next pandemic
- The mitigation strategies prisons put in place (or failed to put in place) during the pandemic
- Prisons and jails in the first year of the pandemic: deaths were up and releases were down
- Untangling why prison and jail populations dropped early in the pandemic
- Large scale-scale prison releases have been done successfully before
- Parole doesn’t always mean release
- Compassionate release wasn’t designed to release large numbers of people
- States of Emergency: The Failure of Prison System Responses to COVID-19 — In this report, released in September 2021, We evaluated departments of corrections on their responses to the COVID-19 pandemic. Includes an appendix providing details about each state.
- Mass Incarceration, COVID-19, and Community Spread — This December 2020 report shows how, in the summer of 2020, over half a million cases of COVID-19 were attributable to the passage of the virus into, through, and out of crowded prisons and jails.
- Failing Grades: States’ Responses to COVID-19 in Jails & Prisons — In this report, which was released in June 2020, we worked with the ACLU to evaluate — and score — all 50 states’ criminal justice responses to the pandemic.
The COVID-19 national emergency may be over, but the ramifications of the nation's failed response to it will be felt for years.
Prison and jail crowding has deadly consequences
From the beginning of the pandemic, it was clear, the most effective way to mitigate the devastation of COVID-19 in prisons and jails is to reduce the number of people behind bars. The United States locks up a larger portion of its population than any other nation in the world . While it is true that the incarcerated population is lower than it was at the beginning of the pandemic, it is still far too high and trending back up.
America’s failed response to COVID-19 in prisons and jails:
- More than 3,000 incarcerated people have died from COVID-19
- In the first year of the pandemic, prisons released 10% fewer people than in the prior year
- Deaths in prisons were up by 46% in 2020, compared to 2019
When the pandemic struck, it was instantly obvious what needed to be done: take all actions possible to “ flatten the curve. ” This was especially urgent in prisons and jails, which are dense facilities where social distancing is impossible , sanitation is poor, and medical resources are limited. Public health experts warned that the consequences were dire: prisons and jails would become Petri dishes where, once inside, COVID-19 would spread rapidly and then boomerang back out to the surrounding communities with greater force than ever before. There were widespread calls for governments to decarcerate. Unfortunately, these calls went unanswered.
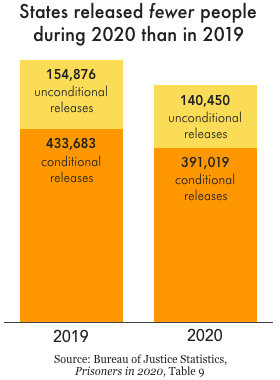
Despite initial hopes that leaders would respond to the pandemic by releasing people, on the whole prisons released almost no one. Only three states — New Jersey, California, and North Carolina — released a significant number of incarcerated people from prisons. Parole boards also approved fewer releases in the first year of the pandemic than the year before. The response of governments was so bad that, in total , 10% fewer people were released from prisons and jails in 2020 than in 2019. As a result, at the end of the first year of the pandemic, 19 state prisons systems were at 90% capacity or higher . Even states that reduced prison populations didn’t necessarily reach “safe” population levels (if any prison can be called “safe”). At the end of 2020, 1 in 5 state prison systems were at or above their design or rated capacity. And there is plenty of evidence that these numbers have gotten worse since then.
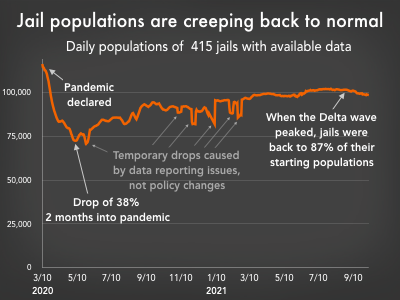
Jail populations dropped early in the pandemic, mostly due to reduced admissions. However, as the pandemic drug on, jail populations steadily climbed, nearly back to their pre-pandemic levels.
Jails were particularly ill-prepared to respond to the pandemic. People generally don’t stay in jails for extended periods. There is a constant churn of people entering and leaving, creating a significant public health threat to people on both sides of a jail’s walls. Much like prisons, jails also saw an initial decline in their populations due to reduced admissions. As the pandemic drug on, though, jails populations slowly approached their pre-pandemic levels.
So, if governments failed to undertake the large-scale releases necessary to confront a pandemic, how is it possible that the incarcerated population is lower now than it was in 2019?
Reductions in the number of people in our nation’s prisons were not the result of goodwill for incarcerated people, concern for their health and safety, or a concerted effort to end mass incarceration. Instead, they were primarily an unintended consequence of court delays and suspension of transfers from local jails early in the pandemic. Many of the same factors that snarled our nation’s supply chain and made it more difficult to get appointments for various services also slowed down the process of sending people to prison.
These delays were temporary, though. As governments adapted to the virus, they quickly returned to business as usual, and prison and jail populations began creeping back up.
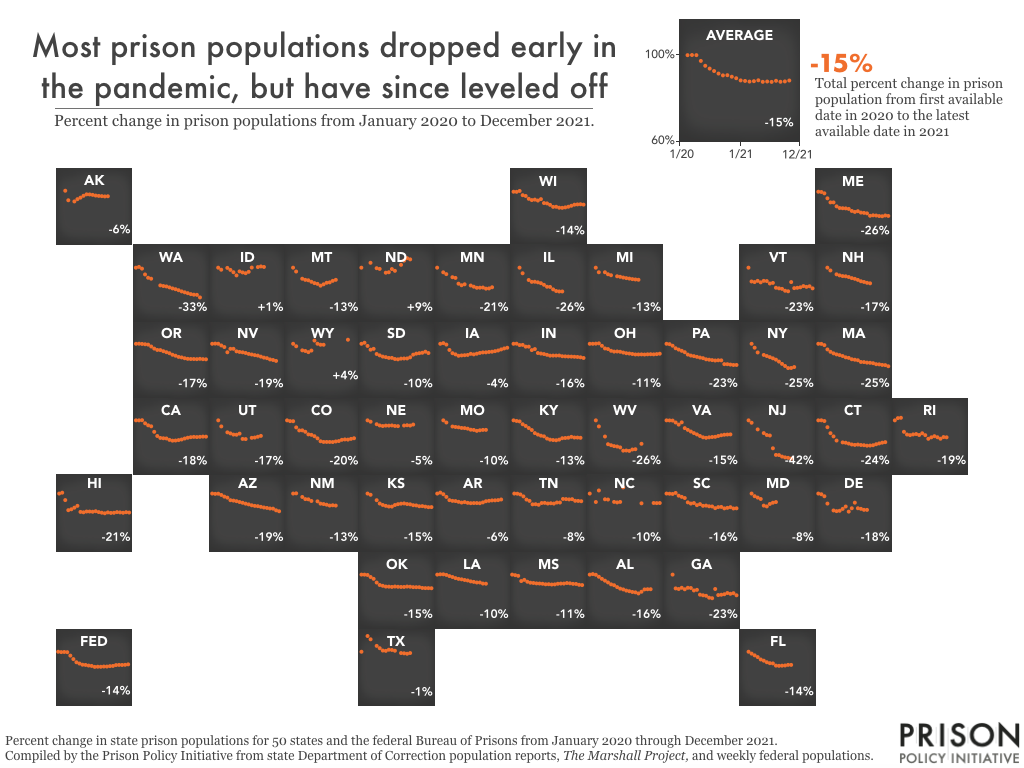
The failure to reduce incarcerated populations had ripple effects that worsened the pandemic far beyond the prison walls. At the onset of the pandemic, areas with higher incarceration rates experienced significantly higher COVID case rates. Our analysis showed that in the summer of 2020, mass incarceration resulted in half a million more cases nationwide . The study revealed that not only do prisons not improve public safety, but they also harm public health.
America also failed to effectively roll out vaccines in prisons. Despite the clear evidence that incarcerated people — like others living in close quarters — were at heightened risk from the virus, most states did not give people in prison the highest priority access to vaccines. In addition, states rarely took proactive steps to address vaccine-hesitancy behind bars . As a result of these two failures, vaccine updating in prisons — for both incarcerated people and corrections officers — consistently lagged behind the nation.
COVID-19 showed why our nation must abandon its addiction to mass incarceration. While the worst of the COVID pandemic appears to be over, the criminal legal system must change to ensure that a short stint in jail or prison does not become a de facto life sentence.
Our most important resources on prison and jail populations during COVID-19:
Correctional healthcare must change to respond to permanent covid-19.
The most important thing governments can do to stop the spread of COVID-19 is reduce the number of people behind bars. However, they must also take steps to ensure those they continue to incarcerate are safe. That will require dramatic improvements to health care protocols in prisons and jails.
Health care in prisons and jails is notoriously bad. It is plagued with poor care, inaccessible treatment, and mistrust. Recognizing that COVID-19 will be an ongoing threat, cities, states, and the federal government must address these deficiencies head-on. Here are a few ways they can do that.
- Ensure access to vaccinations and vaccine education Vaccinations are the single most effective tool to combat COVID-19. They reduce a person’s risk of being infected, and if they are infected, make it much less likely that they will become seriously ill or die. Unfortunately, in the initial vaccine rollout, far too few states prioritized incarcerated people to receive the shots, despite their increased risk. And in many states, vaccination rates among incarcerated people have consistently lagged behind the non-incarcerated population. Vaccination efforts should include an educational component that allows incarcerated people to get the information necessary to feel comfortable taking the vaccines. Information about the safety and efficacy of vaccines is limited for people behind bars. Additionally, the relationship between people in prisons and the medical staff of that prison is often defined by mistrust . Governments should bring in outside medical experts and community leaders that will have the trust of the people who are incarcerated and give them multiple opportunities to ask questions and voice their concerns. Now that vaccines are readily available in the United States, prisons should also give people the option to get the immunization of their choice. It is crucial to remember vaccination standards are likely to change over time. Data increasingly show that people will need to get periodic vaccinations to maintain ongoing protection from the virus. Prisons must ensure incarcerated people can maintain an up-to-date vaccination status.
Our research on the state of copays during the pandemic
- Establish metrics to identify outbreaks and protocols to respond to them Public health experts advise that endemic COVID-19 will be defined by waves of increased infections, often driven by new variants. Prison officials must recognize the threat posed by the virus could dramatically increase quickly. They should have established processes to monitor the threat the virus poses and, when appropriate, plans to impose more rigorous interventions — such as masking, increased testing, and enhanced hygiene practices — to stop its spread. Prison officials should recognize the importance of contact with loved ones outside of the prison’s walls and only suspend visits from family and friends as a last resort. They should also permanently eliminate fees to make phone and video calls; this is particularly important when incarcerated people are cut off physically from their loved ones.
The United States’ response to COVID-19 in prisons and jails was a failure. The refusal to reduce jail and prison populations resulted in unnecessary illness, suffering, and death, both inside and outside prison walls. Abysmal prison and jail medical systems failed to distribute vaccinations effectively and did little to detect and address outbreaks when they occurred.
The damage and death already caused by these failures cannot be undone, but as the world realigns its approach to COVID-19, government leaders have an opportunity to change course to prevent future death and suffering among incarcerated people.
Looking for something you saw on this page before? See an archived list of items that used to be on this page.
Recommended Reading:

COVID wasn't the first viral threat behind bars and won't be the last
We provide 12 steps prisons and jails can take today to prepare for the next inevitable viral outbreak.

States of Emergency: The Failure of Prison System Responses to COVID-19
We evaluated prison systems on population reduction, infection & mortality rates, vaccination, & more.
Tracking prison and jail populations during the pandemic
After modest declines early in the pandemic, prison and jail populations are growing again, despite more infections variants.

What information is available about COVID-19 vaccinations in prisons?
Vaccines are the most effective tool against COVID-19. Do people who are incarcerated have access to them?
- Open access
- Published: 10 April 2024
Implementation of COVID-19 vaccination services in prison in six European countries: translating emergency intervention into routine life-course vaccination
- Sara Mazzilli 1 , 2 na1 ,
- Nicola Cocco 3 na1 ,
- Davide Petri 1 ,
- Babak Moazen 4 , 5 ,
- Alicia Rosello 6 ,
- Jemima D’Arcy 6 ,
- Emma Plugge 7 ,
- Laura Baglietto 8 ,
- Eva Murauer 9 ,
- Heino Stöver 4 ,
- Tassos Trattonikolas 10 ,
- Iakovos Stylianou 10 ,
- Svetlana Doltu 11 ,
- Vladislav Busmachiu 12 ,
- Josefina Mavrou 13 ,
- Ioanna Yiasemi 13 ,
- Irina Barbiros 12 ,
- Filipa Alves da Costa 14 ,
- Fadi Meroueh 9 ,
- Roberto Ranieri 3 &
- Lara Tavoschi 1 na1
BMC Public Health volume 24 , Article number: 1001 ( 2024 ) Cite this article
Metrics details
Evidence has shown that the risk of transmission of SARS-CoV-2 is much higher in prisons than in the community. The release of the COVID-19 vaccine and the recommendation by WHO to include prisons among priority settings have led to the inclusion of prisons in national COVID-19 vaccination strategies. Evidence on prison health and healthcare services provision is limited and often focuses on a single country or institution due to the multiple challenges of conducting research in prison settings. The present study was done in the framework of the EU-founded project RISE-Vac. It aimed to analyse the best practices and challenges applied in implementing COVID-19 universal vaccination services during the pandemic to support future expansion of routine life course vaccination services for people living in prison (PLP).
Two online cross-sectional surveys were designed and piloted: survey1 on prison characteristics and (non-COVID-19) immunisation practices; survey2 on the implementation and coverage of COVID-19 vaccination with open-ended questions for thematic analysis. Each RISE-Vac project partner distributed the questionnaire to one or two prisons in their country. Answers were collected from eight European prisons’ directors or medical directors between November 2021-May 2022.
According to our findings, the implementation modalities of COVID-19 vaccination services in the surveyed prisons were effective in improving PLP vaccination coverage. Strategies for optimal management of the vaccination campaign included: periodic time slot for PLP vaccination; new staff recruitment and task shifting; distribution of informational material both to PLP and prison staff. Key challenges included continuity of care after release, immunisation information system, and vaccine hesitancy.
Conclusions
To the best of our knowledge, this is the first study describing the implementation of COVID-19 vaccination services in European prisons, suggesting that the expansion of vaccination provision in prison is possible. There is no unique solution that will fit every country but commonalities likely to be important in the design and implementation of future vaccination campaigns targeting PLP emerged. Increased availability of vaccination services in prison is not only possible, but feasible and highly desirable, and can contribute to the reduction of health inequalities.
Peer Review reports
According to most recent data, more than 1,4 million individuals are detained on any given day in the European region [ 1 ]. However, due to the high turnover, the number of people who navigate through European prisons each year is considerably higher. Individuals who experience incarceration often belong to socially marginalised and disadvantaged population groups. Regardless of the limited availability of data and differences between countries, there is overwhelming evidence that people living in prison (PLP) disproportionately experience complex, co-occurring health problems, including non-communicable, infectious diseases, mental illness, cognitive disability and substance dependence [ 2 , 3 ].
Despite the greater health needs experienced by PLP, these individuals often have suboptimal access to healthcare services in the community, including effective preventive services such as vaccination [ 4 , 5 ]. The available evidence, albeit scarce, indicates that individuals who enter the prison system are under-immunised, particularly against Hepatitis B Virus (HBV), influenza, measles mumps and rubella (MMR), and pneumococci [ 6 ]. However, the availability of vaccination services in European prisons is limited and usually focused on a few vaccines, such as HBV [ 7 , 8 ]. Routine data on vaccination coverage at entry and on vaccination uptake during incarceration episodes are largely unavailable, with direct implications on health needs, impact of services and for health planning purposes [ 6 , 8 ].
Furthermore, the provision of health services in prison is heterogeneous across Europe, more frequently under the responsibility of the Ministry of Justice (MoJ) alone or with shared responsibilities with the Ministry of Health (MoH). The diverse set-ups may have implications on the availability or organisation of infrastructures, human resources and medical commodities [ 3 , 9 ]. The COVID-19 emergency has uncovered some of the above-mentioned challenges, including within-country variability in policy measures adopted, highlighting important shortcomings of prison health provision and planning across the region [ 10 , 11 ].
Evidence has shown that the risk of transmission of SARS-CoV-2 is much higher in prisons and other closed settings [ 10 ]. Multiple large outbreaks of COVID-19 have been documented in detention facilities worldwide [ 11 , 12 ]. While non-pharmacological preventive measures have been implemented virtually in all prisons in Europe, the extent and continuity varied substantially across space and time [ 10 , 12 ]. The release of the COVID-19 vaccine in late 2020 and the recommendation by WHO [ 13 ] to include prisons among priority settings have led to the inclusion of prisons in the national COVID-19 vaccination strategy [ 13 , 14 ]. The implementation of universal vaccination services in prison settings has been unprecedented and such experience may provide solid ground for the much needed future expansion of vaccination offers for PLP [ 15 ]. In 2021 the project “RISE-Vac - Reaching the hard- to-reach: Increasing access and vaccine uptake among the prison population in Europe”, co-funded by the European Union, was launched to explore ways to promote vaccine offer and uptake in prisons in Europe, involving six countries across the region (Supplementary material, Table 1 . List of RISE-Vac partner institutions). RISE-Vac partners are in the consortium on the basis of their willingness to participate in the project and the availability of at least one prison in the country to carry out the research activities. With the present study, we aimed to analyse the best practices and challenges applied in implementing COVID-19 universal vaccination services during the pandemic in order to support future expansion of routine life course vaccination services for PLP.
Two online cross-sectional surveys were developed by researchers (SM, DP) using Survey Monkey ( https://it.surveymonkey.com ) and reviewed by experts participating in the RISE-Vac project. The surveys were piloted in the RISE-Vac project partner prisons and subsequently revised. Final surveys are available in the Supplemental material ( Annex1 , Annex2 ).
The first survey focused on prison characteristics (type of prison, prison population, capacity, etc.) and (non-COVID-19) immunisation practices for PLP. It included 10 categorical and open-ended questions. The second survey was developed to gather information on the implementation and coverage of COVID-19 vaccination in prison. The survey consisted of 20 categorical and open-ended questions covering: (i) COVID-19 vaccination service set-up; (ii) service implementation and assessment; (iii) barriers; (iv) COVID-19 vaccination coverage.
The six countries participating in the RISE-Vac project were included in this study: Cyprus, France, Germany, Italy, Republic of Moldova, the United Kingdom (UK). Each RISE-Vac project partner distributed the questionnaire to one or more prisons in their country. All participating prisons were selected using a convenience sampling method. Each RISE-Vac project partner distributed the questionnaire to one or more prisons in their country. All participating prisons were selected using a convenience sampling method. To investigate possible specific features or tailored arrangements in the implementation of COVID-19 vaccination services, one female prison and one therapeutic prison (organised around a group therapy programme, where PLPs participate in daily group meetings and activities) were included. In the countries where these prisons were selected (Germany for the female prison and UK for the therapeutic prison), another prison was also included.
In the eight participating prisons the online surveys were shared by email with the prison director (survey 1) or medical director (survey 2) of the prison health unit. Answers were collected from November 2021 through May 2022 for survey 1, and from February 2022 until 31 May 2022 for survey 2.
General population data sources
COVID-19 vaccination coverage among citizens over the age of 18 was obtained from a publicly accessible data set developed by the European Centre for Disease Prevention and Control and World Health Organization [ 16 ]. These data were available for France, Germany and Italy. COVID-19 vaccination coverage data for Cyprus, Moldova and UK were not available by age categories. The source used was: Our World in Data developed by the University of Oxford [ 17 ].
Data analysis
The data collected through the open-ended questions have been analyzed using thematic analysis. Inductive manual coding was applied in the analysis. The data have been coded according to the following emerging categories: COVID-19 vaccination set-up; COVID-19 vaccine implementation; barriers and facilitators; COVID-19 vaccination coverage. The preliminary categories and analysis were shared with RISE-Vac partners and agreed through a consensus building approach. The results have been presented using descriptive statistics, tables, and figures. We compared the vaccination coverage of PLP with the vaccination coverage in the general population.
Characteristics of included prison institutions
Eight prisons answered the questionnaires. The surveyed prisons’ general characteristics are presented in Table 1 . Six institutions hosted pre-trial and short-term sentences PLP. Three of these also hosted long-term sentenced PLP. Four prisons hosted juvenile PLP. Three hosted only males, one only females, while the rest hosted both. One institution was a therapeutic prison. The prisons in Cyprus, France and Italy reported overcrowding.
Vaccines for PLP were provided by the MoH for the prisons located in Cyprus, France, Italy, and UK, while the MoJ were responsible for vaccine provision in the German and Moldovan prisons. Immunisation status was always assessed upon entry into prison with the exception of one prison in Germany. In the Cypriot, Italian and Moldovan prisons the immunisation history was verified via medical records, in British prisons this is only true for part of the PLP. The alternative mode was patient history taking, also used in French and German prisons.
Figure 1 of the supplementary materials shows the vaccinations offered by each prison in the study. At the time of the study, Moldova had no active vaccination prevention service.
COVID-19 vaccination set-up
The answers to the questionnaire show that all six countries had a strategy for COVID-19 vaccination targeting PLP. Prison universal vaccination started in March 2021 in all prisons except prison 2 in Germany and the British prisons, where it started in December 2021. Responsibility for organising the vaccination campaign was assigned to the prison health unit in five prisons (France, Germany, Italy and UK), and to the national prison administration in two prisons (Cyprus and Moldova).
Six prisons (Cyprus, Germany, Italy, Moldova, and UK) reported individual protection and avoiding cases of serious illness as an objective of the prison vaccination campaign. Three prisons (France, Italy and UK) reported the achievement of herd immunity as one of the objectives, and two prisons (Moldova and UK) mentioned also ensuring access to vaccination for all, reducing health inequities.
COVID-19 vaccine implementation
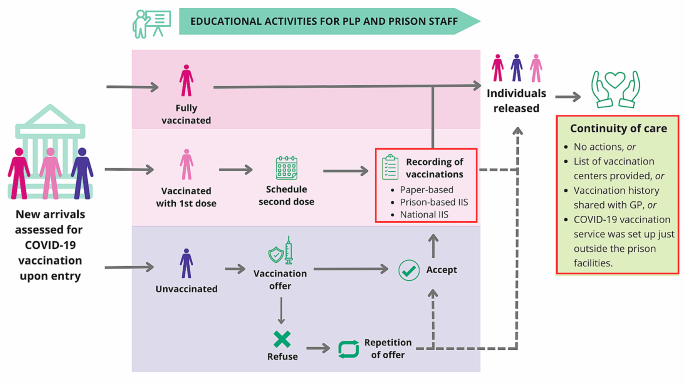
COVID-19 vaccination pathway implemented in European prisons in the study
Red boxes in the vaccination pathway correspond to steps of the COVID-19 vaccination services implemented differently in different prisons.
The COVID-19 vaccination pathway is summarised in Fig. 1 . In all prisons involved in the survey, COVID-19 vaccine immunisation status was assessed at prison entry (Table 1 ). The proportion of new arrivals in prison who received at least one dose of the COVID-19 vaccine before imprisonment ranged from 30% in France and in one prison in Germany to 90% in in Italy. In the French prison, individuals not immunised were offered the vaccine immediately at the first visit. Offer was repeated to those who refused. In all other prisons, administration of the vaccine was scheduled at the next available opportunity for individuals not immunised at entry. In the prisons in Cyprus, Italy, Germany and UK, regular vaccination clinics (i.e. once a week) were organised. In six institutions (Cyprus, France, Italy, Moldova, and UK) vaccination was administered by prison healthcare staff, whereas in the German prisons it was administered by external healthcare providers for the first six months of the vaccination campaign after which the prison health unit took over. To implement the vaccination campaign, additional human resources were hired in the Italian prison and task shifting occurred in the Italian and Moldovan institutions. In these prisons, the nurses held managerial and organisational roles and the custodial staff participated in the recall of PLP who needed to be vaccinated. Despite these differences, in all the institutions, mass COVID-19 vaccination took place within prison facilities and included education/training activities tailored for prison staff (Custodial and healthcare staff) and PLP. The educational activities implemented for health personnel were: face-to-face meetings, online information sessions and leaflet distribution. Regarding changes in the supply chain for the COVID-19 vaccine, the British prisons reported a simplification of the procedures to order vaccine doses, while the Italian prison reported a faster and more flexible delivery. In the Cyprus prison vaccinations administered were recorded in paper-based prison vaccination registries, in UK institutions in a prison-based digital information system and in the Moldovan and French prisons in the national digital information system. In the Italian prison, registration of vaccinations was initially paper-based, but the possibility of adding the information to the national digital information system was later introduced (Table 2 ).
In the French prison, PLP were given a list of vaccination centres where they could receive booster doses in the community. In the British prisons surveyed, in addition to providing the list of vaccination centres in the community, the vaccination history of the released individual was transferred to community-based GP (for individuals resident in the country of detention), while a COVID-19 vaccination service for released individuals was set-up within the Italian prison premises. There was no protocol in the Cypriot and Moldovan prisons to link to care subjects who were released before completing the COVID-19 vaccination schedule. The evaluation of the vaccination campaign was carried out by the Italian and British prisons. Continuous assessment of vaccination uptake rates among PLP was regularly performed and the findings were used to inform corrective actions such as repeated offers to all eligible individuals and review of information/communication material. At the time of the survey, the vaccination uptake of the complete series of COVID-19 vaccine among PLP in prison was between 50 and 75% in the France Moldovan and British prisons, and between 75 and 90% in Cypriot, German and Italian prisons (Fig. 2 ).
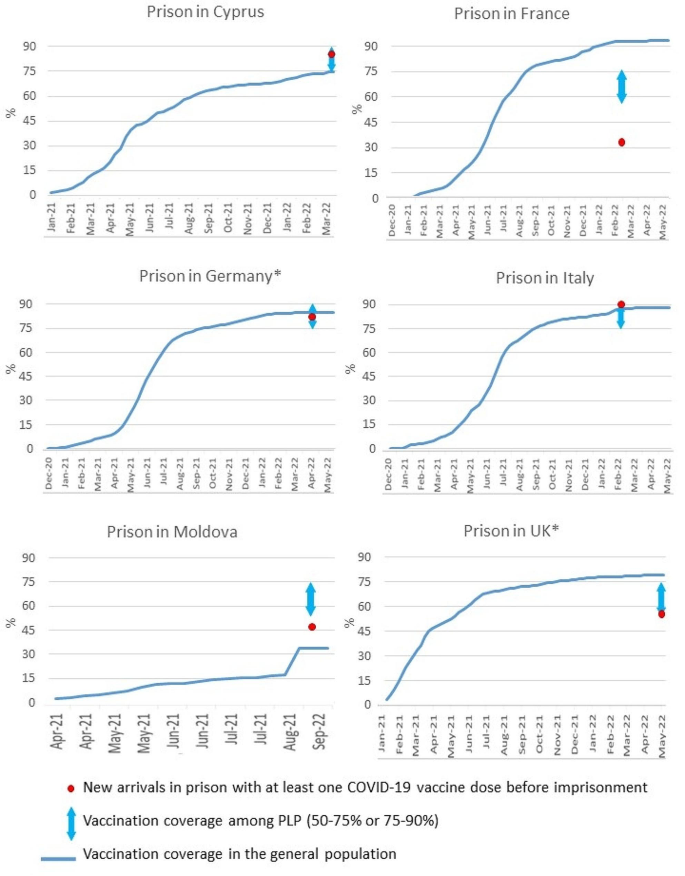
Vaccination coverage among new arrivals, PLP in the prisons surveyed and the general population (Feb-May 2022). *For Germany the data are shown for the prison with PLP of both sexes, for UK data from the non-therapeutic prison are shown
Barriers and facilitators
Common barriers encountered during the upscale of COVID-19 vaccination services were reported by all respondents. Identified barriers related mostly to infrastructural constraints, such as lack of human resources to deal with the surge of activity and lack of commodities such as adequate cold supply chain systems. These were addressed in different manners including task shifting, with lower cadres managing patients’ engagement and appointments, or implementation of pragmatic solutions such as dedicated immunisation days (Table 3 ).
Other important barriers related to recording the administration of vaccine doses in the absence of an interoperable immunisation information system between prison and community, or to the use of paper-based records exclusively. While this was successfully addressed in some cases (e.g. Italian prison) during the COVID-19 emergency, the solutions achieved were restricted to COVID-19 immunisation.
The post-release referral was also recognised as a barrier to the completion of the vaccination course. Solutions identified were common to other conditions requiring continuous access to care services (e.g. HIV treatment, opioid agonist treatment) [ 22 ] and included setting appointments in the most convenient healthcare service in the community (active referral) or providing the individual with a list of relevant services (passive referral). In one case (Italian prison), an ad hoc COVID-19 vaccination service accessible to released individuals was set up within prison premises. Released individuals were recalled and given appointments for booster dose/s. Low vaccination uptake has been reported as a limitation for achieving high vaccination coverage in PLP. The use of information material and the organisation of educational activities concerning vaccinations have been reported as facilitators to decrease vaccination hesitancy. All respondents reported that the implementation of COVID-19 vaccination services in prison was likely to impact future vaccination services for this population. In particular, respondents underlined the importance of sustaining and translating the good practices introduced with COVID-19 vaccination to other immunisation programmes relevant to PLP.
To the best of our knowledge, this is the first study describing the implementation of COVID-19 vaccination services in European prisons, showing that the expansion of vaccination provision in prison is possible, regardless of whether the health of PLP is the responsibility of the MoH or the MoJ. There is no unique solution that will fit every country’s prisons although these findings could inform the design and implementation of future vaccination campaigns targeting PLP.
One key element was the organization of a periodic (i.e. one day per week) time slot for PLP vaccination. This reduced the workload of prison healthcare staff compared to ad-hoc vaccination. Staff could accomplish vaccination-related activities in defined time slots, allowing more time for routine healthcare activities. This also addressed possible cold supply chain issues by streamlining vaccination delivery, stocking and administration in a single day. It is also likely to have decreased vaccine wastage [ 15 ].
With the exception of German prisons, respondents in the other five countries reported the exclusive involvement of healthcare staff working in prisons for COVID-19 vaccination of PLP. Despite this, all prisons recognised the need and implemented specific training activities tailored to healthcare professionals to equip them with the relevant skills for the administration of vaccines to PLP. This is in line with evidence from the literature related to both healthcare workers who administer vaccinations in other settings [ 18 , 19 ] and health workers who work in prison but address other health issues [ 20 , 21 ].
In response to staff shortages, task-shifting was implemented in two prisons involving other professionals for health and custodial staff. As already highlighted at global level for other primary health interventions and prevention tasks [ 22 , 23 ], this represents a useful organisational approach to improve coverage and timeliness of health prevention activities in limited resource settings.
Finally, high vaccination hesitancy was reported among PLP in several prisons, leading to low vaccination acceptance in some instances. Vaccine hesitancy is one of the most important reported barriers towards controlling vaccine-preventable diseases in prisons [ 24 ]. PLP may refuse vaccination due to various reasons including but not limited to concerns about side effects, low levels of perceived risk, distrust of authorities, vaccine, or vaccinator, or even fear of needles and injections [ 24 , 25 ]. To address this issue, in all responding prisons before or in parallel with the introduction of COVID-19 vaccination, efforts were made towards the development and dissemination of tailored information and educational resources.
There were different levels of information technology implementation within the prisons included in the study. Paper-based IIS was used in some cases as the main recording system. Electronic records were in use at most prisons, however interoperability with the national health information system was not always available. This is in line with what is reported in other prison institutions in Europe [ 26 ].
Continuity of care and completion of the vaccination cycle after release was identified as an issue in all prisons included. An ad hoc COVID-19 vaccination service, accessible to released persons, was set up within the Italian prison premises. Although effective in addressing pandemic emergency needs, this strategy is hardly sustainable. In the British prisons surveyed, vaccination history of released individuals was shared with the assigned community general practitioner where possible. Efforts to guarantee adequate continuity of care can be severely hampered if individuals’ medical records cannot reach healthcare services in the community upon release, or prison health services upon admission. Lack of accurate, updated and accessible data on previous immunisation, or other health interventions, may result in inadequate or untimely actions. This lack of seamless transfer of electronic information has been well documented for many other health conditions in people leaving prison in a number of countries [ 27 ].
Improvement in the prison-based health data collection is also pivotal to support the development of evidence-based approaches. Only two of the six prisons included in the questionnaire reported having a formal system to evaluate the effectiveness of the vaccination campaign.
Therefore, while the COVID-19 pandemic has catalysed some progress, improving the prison health information systems remain a major area for future investment. Ensuring interoperability of individuals’ and population (aggregated) health information system between prison and community is an essential requisite to guarantee continuity of care for people transitioning through the penal system, as well as to allow healthcare monitoring and planning activities to be performed at the same standard as in the community and using a data-driven approach, ultimately promoting health equity [ 5 ].
According to our findings, the implementation of COVID-19 vaccination in prison was effective in improving PLP vaccination coverage, including in countries such as Moldova, where vaccination services in prison were not available before the COVID-19 pandemic. Interestingly, this was achieved in prisons across countries with different governance arrangements with respect to prison healthcare provision [ 28 ]. There are various factors that may have impacted on the increase in coverage observed that are beyond the scope of this study but should nonetheless be mentioned. Namely, the adoption of national vaccination plans that directly refer to PLP, the mere acceptance that there is equivalence of care and thus PLP are included or, in contrast, the explicit exclusion of prisons from national policies. Coverage data presented in this manuscript is aligned with the scarce information available, namely from WHO, where in October 2021, Moldova reported having 36.8% of PLP fully vaccinated against COVID-19 [ 14 ]. Similarly, UK reported a higher vaccination coverage by June 2021 (66%). The speed of uptake in these two particular cases may be well related to the vaccination policies adopted, respectively omitting prison populations or explicitly acknowledging them as a group at higher risk.
This study has several limitations. First, the selection of prisons is convenience based. Second, the number of prisons interviewed is limited. Therefore, the results presented may not be transferable to all prisons in the countries studied. To increase representativeness the investigation of effective immunization programs implemented in prisons should be extended in future studies to a larger sample.
While this study captures the experience of only a few prison institutions within selected countries and a single vaccine, the COVID-19 emergency has shown the potential to exploit incarceration as a time window and prison as a place to offer targeted immunisation programs. This is particularly relevant, as our findings showed that availability of vaccines, beyond COVID-19, is limited in the surveyed prisons, confirming existing evidence, despite international guidelines extensively recommending vaccination for PLP [ 6 , 13 ].
Providing expanded, age-appropriate, free from coercion and tailored vaccination services to PLP will contribute to improving the health status of individuals in detention, while reducing within-prison transmission. Moreover, PLP transition to the community and therefore the health benefits resulting from vaccination accrue into the community [ 4 , 29 ]. The potential utility and desirability of expanded vaccination programmes in prison settings is even more evident when framed within regional and global initiatives such as the elimination of measles and rubella [ 30 ], the efforts to eliminate vaccine preventable cancer [ 31 ] and the achievement of universal health coverage, including access to safe, effective, quality and affordable vaccines for all is a component of UN Sustainable Development Goal 3.8 [ 32 ].
Life-course vaccination in prison should be part of an integrated healthcare system aimed at preventing and mitigating the burden of infectious diseases. As reported by the WHO, providing integrated services to combat multiple infectious diseases can synergistically strengthen the response, expand coverage and alleviate stigma and discrimination [ 33 ]. The implementation of life course vaccination programmes in prisons requires full integration of prison health into public health and is essential to upholding the principle of equity of care [ 34 ] and to guarantee the right to health for those deprived of liberty, leaving no one behind.
In conclusion, the COVID-19 pandemic has further confirmed how increased availability of vaccination services in prison is not only possible, but feasible and highly desirable, and can contribute to the reduction of health inequalities.
Data availability
The data used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
People living in prison
Hepatitis B Virus
Measles mumps and rubella
Ministry of Justice
Ministry of Health
The United Kingdom
Aebi MF, Tiago MM. Prison Population SPACE I– 2020. 2021.
European Monitoring Centre for Drugs and Drug Addiction. Prison and drugs in Europe: current and future challenges. Publ Off Eur Union, Luxemb [Internet]. 2022; Available from: https://www.emcdda.europa.eu/system/files/publications/13904/TDXD21001ENN.pdf .
World Health Organisation. 6th Prison Health Conference Prison health systems: the interface with wider national health systems. 2019. https://apps.who.int/iris/bitstream/handle/10665/347071/WHO-EURO-2019-3714-43473-61068
Gaskin GL, Glanz JM, Binswanger IA, Anoshiravani A. Immunization Coverage Among Juvenile Justice Detainees. J Correct Heal Care [Internet]. 2015;21(3):265–75. https://doi.org/10.1177/0885066615587790 .
Winkelman TNA, Dasrath KC, Young JT, Kinner SA. Universal health coverage and incarceration. Lancet Public Heal [Internet]. 2022;7(6):e569–72. https://doi.org/10.1016/S2468-2667(22)00113-X .
Vicente-Alcalde N, Ruescas-Escolano E, Harboe ZB, Tuells J. Vaccination coverage among prisoners: a systematic review. Int J Environ Res Public Health. 2020 Oct 19;17(20):7589. https://doi.org/10.3390/ijerph17207589 . PMID: 33086513; PMCID: PMC7589151.
Madeddu G, Vroling H, Oordt-Speets A, Babudieri S, O’Moore É, Noordegraaf MV et al. Vaccinations in prison settings: A systematic review to assess the situation in EU/EEA countries and in other high income countries. Vaccine [Internet]. 2019;37(35):4906–19. https://doi.org/10.1016/j.vaccine.2019.07.014 .
Nakitanda AO, Montanari L, Tavoschi L, Mozalevskis A, Duffell E. Hepatitis B virus infection in EU/EEA and United Kingdom prisons: a descriptive analysis. Epidemiol Infect. 2021 Jan 25;149:e59. https://doi.org/10.1017/S0950268821000169 . PMID: 33487201; PMCID: PMC8060813.
World Health Organization (WHO), United Nations Office on Drugs and Crime (UNODC). Good governance for prison health in the 21st century. A policy brief on the organization of prison health [Internet]. 2013. Available from: https://www.euro.who.int/__data/assets/pdf_file/0017/231506/Good-governance-for-prison-health-in-the-21st-century.pdf .
WHO COVID- Status report on prison health in the WHO European Region. Copenhagen WHO Reg Off Eur [Internet]. 2023; Available from: https://www.who.int/europe/publications/i/item/9789289058674 .
Neufeld M, Alves da Costa F, Ferreira-Borges C. Prisons need to be included in global and national vaccinations effort against COVID-19. Lancet Reg Heal - Eur [Internet]. 2021;4:100088. https://doi.org/10.1016/j.lanepe.2021.100088 .
Mazzilli S, Tavoschi L, Soria A, Fornili M, Cocca G, Sebastiani T, et al. COVID-19 infection among incarcerated individuals and prison staff in Lombardy, Italy, March 2020 to February 2021. JAMA Netw Open. 2022;5(March 2020):1–13.
Google Scholar
Why people living and working in detention facilities should be included in national COVID-19 vaccination plans. Copenhagen WHO Reg Off Eur [Internet]. 2021;1–14. Available from: https://www.who.int/europe/publications/i/item/WHO-EURO-2021-2569-42325-58577 .
Health in Prisons. – COVID-19 Minimum Dataset: Summary of data reported from May 2020 to October 2021. Copenhagen WHO Reg Off Eur. 2022;(October).
Ismail N, Tavoschi L, Moazen B, Roselló A, Plugge E. COVID-19 vaccine for people who live and work in prisons worldwide: a scoping review. PLoS ONE. 2022;17(9 September):1–19.
CAS Google Scholar
European Centre for Disease Prevention and Control, World Health Organization. Joint ECDC-WHO Regional Office for Europe Weekly COVID-19 Surveillance Bulletin [Internet]. 2022 [cited 2022 Dec 21]. Available from: https://worldhealthorg.shinyapps.io/euro-covid19/ .
Our World in Data. Coronavirus (COVID-19) Vaccinations [Internet]. 2022 [cited 2022 Dec 21]. Available from: https://ourworldindata.org/covid-vaccinations .
Biswas N, Mustapha T, Khubchandani J, Price JH. The Nature and Extent of COVID-19 Vaccination Hesitancy in Healthcare Workers. J Community Health [Internet]. 2021;46(6):1244–51. https://doi.org/10.1007/s10900-021-00984-3 .
Casey RM, Adrien N, Badiane O, Diallo A, Loko Roka J, Brennan T et al. National introduction of HPV vaccination in Senegal—Successes, challenges, and lessons learned. Vaccine [Internet]. 2022;40:A10–6. https://doi.org/10.1016/j.vaccine.2021.08.042 .
Bennett C, Perry J, Lapworth T, Davies J, Preece V. Supporting prison nurses: an action research approach to education. Br J Nurs. 2010;19(12):782–7.
Article PubMed Google Scholar
Perry AE, Waterman MG, House AO, Greenhalgh J. Implementation of a problem-solving training initiative to reduce self-harm in prisons: a qualitative perspective of prison staff, field researchers and prisoners at risk of self-harm. Heal Justice. 2019;7(1).
World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach—second edition. Vol. 5. 2016.
Oru E, Trickey A, Shirali R, Kanters S, Easterbrook P. Decentralisation, integration, and task-shifting in hepatitis C virus infection testing and treatment: a global systematic review and meta-analysis. Lancet Glob Heal [Internet]. 2021;9(4):e431–45. https://doi.org/10.1016/S2214-109X(20)30505-2 .
Allison M, Emerson A, Pickett ML, Ramaswamy M. Incarcerated adolescents’ attitudes toward Human Papillomavirus Vaccine: Report from a Juvenile Facility in Kansas. Glob Pediatr Heal. 2019;6.
Junghans C, Heffernan C, Valli A, Gibson K. Mass vaccination response to a measles outbreak is not always possible. Lessons from a London prison. Epidemiol Infect. 2018;146(13):1689–91.
Article CAS PubMed PubMed Central Google Scholar
World Health Organization. Organizational models of prison health. Considerations for better governance. 2020 Available from: https://apps.who.int/iris/bitstream/handle/10665/336214/WHO-EURO-2020-1268-41018-55685-eng .pdf?sequence=1&isAllowed=y.
Morris NP, Zisman-Ilani Y. Communication over incarceration: improving Care Coordination between Correctional and Community Mental Health Services. Psychiatr Serv. 2022;73(12):1409–11.
United Nations Office on Drugs and Crime (UNODC), World Health Organization. Regional Office for Europe. Good governance for prison health in the 21st century. A policy brief on the organization of prison health. 2013. Available from: https://apps.who.int/iris/bitstream/handle/10665/326388/9789289000505-eng.pdf?sequence=1&isAllowed=y
Palmateer NE, Goldberg DJ, Munro A, Taylor A, Yeung A, Wallace LA, et al. Association between universal hepatitis B prison vaccination, vaccine uptake and hepatitis B infection among people who inject drugs. Addiction. 2018;113(1):80–90.
World Health Organization (WHO). Immunization Agenda 2030: A Global Strategy to Leave No One Behind. 2020;(August):1–24. Available from: https://www.who.int/immunization/ia2030_Draft_One_English.pdf?ua=1 .
European Commission, EUROPE’S BEATING, CANCER PLAN Communication from the commission to the European Parliament and the Council. 2021; Available from: https://health.ec.europa.eu/system/files/2022-02/eu_cancer-plan_en_0.pdf .
United Nations (UN). The Sustainable Development Goals. [Internet]. New York: UN. Available from: https://sdgs.un.org/goals .
Cairo, WHO Regional Office for the Eastern Mediterranean. Consultation on integrated management of HIV, hepatitis, TB and STIs for key populations. 2019;(June 2019). Available from: https://www.who.int/europe/publications/i/item/9789289058674 .
UNODC. United Nations Standard Minimum Rules for the Treatment. Unodc [Internet]. 2015;16487(September):1–36. Available from: https://www.unodc.org/documents/justice-and-prison-reform/Nelson_Mandela_Rules-E-ebook.pdf .
Download references
RISE-Vac project is co-funded by the European Union’s 3rd Health Programme (2014–2020) under grant agreement No 101018353.
Author information
Sara Mazzilli and Nicola Cocco contributed equally to this paper.
Authors and Affiliations
Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, Pisa, Italy
Sara Mazzilli, Davide Petri & Lara Tavoschi
Scuola Normale Superiore, Pisa, Italy
Sara Mazzilli
Infectious Diseases Service, Penitentiary Health System, Azienda Socio-Sanitaria Territoriale Santi Paolo e Carlo, Milan, Italy
Nicola Cocco & Roberto Ranieri
Department of Health and Social Work, Institute of Addiction Research (ISFF), Frankfurt University of Applied Sciences, Frankfurt/Main, Germany
Babak Moazen & Heino Stöver
Heidelberg Institute of Global Health, Heidelberg University, Heidelberg, Federal Republic of Germany
Babak Moazen
UK Health Security Agency, London, UK
Alicia Rosello & Jemima D’Arcy
Primary Care, Population Sciences and Medical Education, Faculty of Medicine, University of Southampton, Southampton, UK
Emma Plugge
Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy
Laura Baglietto
Health Unit of the Villeneuve-les-Maguelone prison, University Hospital Centre Montpellier, Montpellier, France
Eva Murauer & Fadi Meroueh
Ministry of Justice and Public Order - Cyprus Prison Department, Nicosia, Cyprus
Tassos Trattonikolas & Iakovos Stylianou
Act For Involvement, Chișinău, Republic of Moldova
Svetlana Doltu
National Administration of Penitentiaries, Chișinău, Republic of Moldova
Vladislav Busmachiu & Irina Barbiros
Cyprus National Addictions Authority, Nicosia, Cyprus
Josefina Mavrou & Ioanna Yiasemi
Health in Prisons Programme, WHO Regional Office for Europe, Copenhagen, Denmark
Filipa Alves da Costa
You can also search for this author in PubMed Google Scholar
Contributions
LT, SM and NC conceptualised and designed the research. DP, BM, AR, JD, LB, EM, TT, IS, SD, VB, JM, IY, IB, FM, RR participated in the acquisition, analysis, or interpretation of data. SM, NC, LT and DP drafted of the manuscript. SM, NC, DP and LT analysed the data. SM and JD prepared the figure. EP, LB, HS, FAC, RR critically revised the manuscript for important intellectual content. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Lara Tavoschi .
Ethics declarations
Ethics approval and consent to participate.
The study protocol related to the RISE-Vac project has received approval from the Ethics Committee of the University of Pisa (n. 9/2022 - meeting 25th March 2022, protocol number 0049433/2022 on 12/04/2022). Respondents were recruited among RISE-Vac project consortium partners and allied entities. Verbal informed consent was obtained.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Filipa Alves da Costa is a consultant for WHO Regional Office for Europe. The author alone is responsible for the views expressed in this publication, and these do not necessarily represent the decisions or the stated policy of the World Health Organization.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mazzilli, S., Cocco, N., Petri, D. et al. Implementation of COVID-19 vaccination services in prison in six European countries: translating emergency intervention into routine life-course vaccination. BMC Public Health 24 , 1001 (2024). https://doi.org/10.1186/s12889-024-18063-2
Download citation
Received : 27 June 2023
Accepted : 10 February 2024
Published : 10 April 2024
DOI : https://doi.org/10.1186/s12889-024-18063-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Vaccination
- Health inequities
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
COMMENTS
On May 1, 2021, Massachusetts began to reopen visitation at three prisons, with more added in the following days. Personal visits were first suspended on March 13, 2020 and resumed with limits in July. On Nov. 14, 2020, the prisons again halted visits amid rising coronavirus cases. Legal visits were allowed.
We spoke with incarcerated people and their families, prison wardens, jailers, prosecutors, defense attorneys and civil rights groups. A year later, one in three inmates in state prisons are known ...
Captives Behind Plexiglass: How COVID Destroyed Prison Visits. "Parlour.". Painting by Julio Pomar (1926-2018) of Aljube Prison, Lisbon via Flickr. Every Saturday morning, private buses drop ...
The prison population declined by 157,500 persons during the first 6 months of the COVID-19 study period through the end of August 2020, and by 58,300 in the 6 months through the end of February 2021. Twenty-four states released a total of 37,700 persons from prison on an expedited basis (earlier than scheduled) during the COVID-19 study period.
Federal prisons saw a significant rise in deaths during the pandemic years, NPR found. Of those who died from COVID-19, nearly all were elderly or had health conditions, and many had tried to get out.
26 Feb 2021. In the days before Christmas, 44-year-old April Harris sat in her prison cell at the California Institution for Women for more than 23 hours a day. In the 20 minutes she was allowed ...
Over the p ast 18 months, as the world has been ravaged by the COVID-19 pandemic, those detained in jails, prisons, and detention centers have been severely impacted due to lack of physical distancing, proper sanitation methods, and the failure to prioritize testing and vaccinations. Common conditions in jails and prisons have never been conducive to decent health for inmates - lack of ...
During April 22-28, 2020, aggregate data on COVID-19 cases were reported to CDC by 37 of 54 state and territorial health department jurisdictions. Thirty-two (86%) jurisdictions reported at least one laboratory-confirmed case from a total of 420 correctional and detention facilities. Among these facilities, COVID-19 was diagnosed in 4,893 ...
An account from San Quentin prison detailing the Spanish influenza of 1918 estimated that half of the 1900 inmates contracted the disease during the first wave of the epidemic; sick calls increased from 150 to 700 daily. Contrary to protocol, most of the ill were kept in the general prison population because the hospital ward was full. 1
COVID-19 has been an unprecedented challenge in carceral facilities. As COVID-19 outbreaks spread in the US in early 2020, many jails, prisons, juvenile detention centers, and other carceral facili...
Key findings from Impact of COVID-19 on State and Federal Prisons, March 2020-February 2021:. Some prison systems significantly reduced the number of people entering prison, but a handful quickly returned to admitting large numbers of people, even more than the number admitted in January 2020, before the pandemic.
Oct. 1, 2020. Relatives and friends will be permitted once again to begin visiting inmates in federal prisons as of Saturday, six months after such visits were ended over concerns about the ...
Lessons from COVID-19 can help prisons & jails prepare for the next pandemic Prison Policy Initiative, April, 2023 "Without any serious change to our reliance on mass incarceration -- this population will continue to bear the disproportionate burden of public health crises.". COVID-19 amplified racial disparities in the US criminal legal ...
Results Of 647 articles found, 83 were eligible for inclusion, the majority (58%) of which were opinion pieces. The articles focused on the challenges to prisoner mental health. Fear of COVID-19, the impact of isolation, discontinuation of prison visits and reduced mental health services were all likely to have an adverse effect on the mental well-being of imprisoned people.
According to Nowotny, at least 390,000 people in US prisons have been infected with COVID-19, representing 30 percent of the prison population. Of this number, at least 2,500 have died from COVID-19. Both numbers are likely an undercount due to inaccuracies within the system and a backlog of data reporting. "All prison systems report data in ...
CORRECTIONAL STAFF ARE AT PARTICULARLY ELEVATED RISK. More than 500,000 correctional officers and correctional medical staff work in this environment. 12 They are essential personnel during the COVID-19 response, 1 and their professions bring them into direct contact with a high-risk population daily. They share all the risks of the physical environment as listed above but are additionally ...
The big picture that this policy tracker reveals is grim: Lawmakers have failed to reduce prison and jail populations enough to slow down the spread of the coronavirus, causing incarcerated people to get sick and die at a rate unparalleled in the general public.. However, some individual state and local policymakers have recognized the urgency of the situation, and taken actions that show how ...
Subsequently, there have been 322,769 confirmed cases of COVID-19 among US prisoners with 1846 deaths as of January 2021. For prison staff, there have been 70,658 cases with 113 deaths . To combat COVID-19 transmission during a pandemic, a comprehensive and unified public health effort is desperately needed.
"Between the start of the pandemic and August 31, 2020 — health insurance gaps were linked to an estimated 2.6 million COVID-19 cases and 58,000 COVID-19 deaths," the study notes. "Each 10% increase in the proportion of a county's residents who lacked health insurance was associated with a 70% increase in COVID-19 cases and a 48% ...
by There is still a prison pandemic, Kevin Walby, Abby Deshman March 7, 2022. By March 2021, it was clear that jails, prisons and penitentiaries across Canada were significant vectors of COVID-19 during the second wave of the pandemic, with infections among imprisoned people and staff increasing in unprecedented ways.
The report 'The impact of COVID-19 prison lockdowns on children with a parent in prison' is available here. The study found that children experienced confusing and complex emotions when face to face visits were stopped. Many children thought that their parent didn't want to see them anymore, or maybe their parent no longer loved them.
COVID-19 in Prisons and Jails America's response to the COVID-19 pandemic in prisons and jails was a failure. This page provides a recap of our work during this tragic time. April, 2023. With more than half a million infections behind bars and over 3,000 deaths, America's response to COVID-19 in prisons and jails was a failure. Federal, state ...
and prison staff, and at management of the prison population. We have held five oral evidence sessions specifically on Coronavirus (Covid-19): The Impact on prison, probation and court systems, and have taken evidence on the impact of Covid-19 during sessions related to other Justice Committee inquiries. We have received many written briefings
Background Evidence has shown that the risk of transmission of SARS-CoV-2 is much higher in prisons than in the community. The release of the COVID-19 vaccine and the recommendation by WHO to include prisons among priority settings have led to the inclusion of prisons in national COVID-19 vaccination strategies. Evidence on prison health and healthcare services provision is limited and often ...
បេក្ខជន ប្រធានាធិបតី សហរដ្ឋ អាមេរិក លោក Donald Trump ថា ច្បាប់ ...