- COVID-19 travel advice
Considering travel during the pandemic? Take precautions to protect yourself from COVID-19.
A coronavirus disease 2019 (COVID-19) vaccine can prevent you from getting COVID-19 or from becoming seriously ill due to COVID-19 . But even if you're vaccinated, it's still a good idea to take precautions to protect yourself and others while traveling during the COVID-19 pandemic.
If you've had all recommended COVID-19 vaccine doses, including boosters, you're less likely to become seriously ill or spread COVID-19 . You can then travel more safely within the U.S. and internationally. But international travel can still increase your risk of getting new COVID-19 variants.
The Centers for Disease Control and Prevention (CDC) recommends that you should avoid travel until you've had all recommended COVID-19 vaccine and booster doses.

Before you travel
As you think about making travel plans, consider these questions:
- Have you been vaccinated against COVID-19 ? If you haven't, get vaccinated. If the vaccine requires two doses, wait two weeks after getting your second vaccine dose to travel. If the vaccine requires one dose, wait two weeks after getting the vaccine to travel. It takes time for your body to build protection after any vaccination.
- Have you had any booster doses? Having all recommended COVID-19 vaccine doses, including boosters, increases your protection from serious illness.
- Are you at increased risk for severe illness? Anyone can get COVID-19 . But older adults and people of any age with certain medical conditions are at increased risk for severe illness from COVID-19 .
- Do you live with someone who's at increased risk for severe illness? If you get infected while traveling, you can spread the COVID-19 virus to the people you live with when you return, even if you don't have symptoms.
- Does your home or destination have requirements or restrictions for travelers? Even if you've had all recommended vaccine doses, you must follow local, state and federal testing and travel rules.
Check local requirements, restrictions and situations
Some state, local and territorial governments have requirements, such as requiring people to wear masks, get tested, be vaccinated or stay isolated for a period of time after arrival. Before you go, check for requirements at your destination and anywhere you might stop along the way.
Keep in mind these can change often and quickly depending on local conditions. It's also important to understand that the COVID-19 situation, such as the level of spread and presence of variants, varies in each country. Check back for updates as your trip gets closer.
Travel and testing
For vaccinated people.
If you have been fully vaccinated, the CDC states that you don't need to get tested before or after your trip within the U.S. or stay home (quarantine) after you return.
If you're planning to travel internationally outside the U.S., the CDC states you don't need to get tested before your trip unless it's required at your destination. Before arriving to the U.S., you need a negative test within the last day before your arrival or a record of recovery from COVID-19 in the last three months.
After you arrive in the U.S., the CDC recommends getting tested with a viral test 3 to 5 days after your trip. If you're traveling to the U.S. and you aren't a citizen, you need to be fully vaccinated and have proof of vaccination.
You don't need to quarantine when you arrive in the U.S. But check for any symptoms. Stay at home if you develop symptoms.
For unvaccinated people
Testing before and after travel can lower the risk of spreading the virus that causes COVID-19 . If you haven't been vaccinated, the CDC recommends getting a viral test within three days before your trip. Delay travel if you're waiting for test results. Keep a copy of your results with you when you travel.
Repeat the test 3 to 5 days after your trip. Stay home for five days after travel.
If at any point you test positive for the virus that causes COVID-19 , stay home. Stay at home and away from others if you develop symptoms. Follow public health recommendations.
Stay safe when you travel
In the U.S., you must wear a face mask on planes, buses, trains and other forms of public transportation. The mask must fit snugly and cover both your mouth and nose.
Follow these steps to protect yourself and others when you travel:
- Get vaccinated.
- Keep distance between yourself and others (within about 6 feet, or 2 meters) when you're in indoor public spaces if you're not fully vaccinated. This is especially important if you have a higher risk of serious illness.
- Avoid contact with anyone who is sick or has symptoms.
- Avoid crowds and indoor places that have poor air flow (ventilation).
- Don't touch frequently touched surfaces, such as handrails, elevator buttons and kiosks. If you must touch these surfaces, use hand sanitizer or wash your hands afterward.
- Wear a face mask in indoor public spaces. The CDC recommends wearing the most protective mask possible that you'll wear regularly and that fits. If you are in an area with a high number of new COVID-19 cases, wear a mask in indoor public places and outdoors in crowded areas or when you're in close contact with people who aren't vaccinated.
- Avoid touching your eyes, nose and mouth.
- Cover coughs and sneezes.
- Wash your hands often with soap and water for at least 20 seconds.
- If soap and water aren't available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub your hands together until they feel dry.
- Don't eat or drink on public transportation. That way you can keep your mask on the whole time.
Because of the high air flow and air filter efficiency on airplanes, most viruses such as the COVID-19 virus don't spread easily on flights. Wearing masks on planes has likely helped lower the risk of getting the COVID-19 virus on flights too.
However, air travel involves spending time in security lines and airport terminals, which can bring you in close contact with other people. Getting vaccinated and wearing a mask when traveling can help protect you from COVID-19 while traveling.
The Transportation Security Administration (TSA) has increased cleaning and disinfecting of surfaces and equipment, including bins, at screening checkpoints. TSA has also made changes to the screening process:
- Travelers must wear masks during screening. However, TSA employees may ask travelers to adjust masks for identification purposes.
- Travelers should keep a distance of 6 feet apart from other travelers when possible.
- Instead of handing boarding passes to TSA officers, travelers should place passes (paper or electronic) directly on the scanner and then hold them up for inspection.
- Each traveler may have one container of hand sanitizer up to 12 ounces (about 350 milliliters) in a carry-on bag. These containers will need to be taken out for screening.
- Personal items such as keys, wallets and phones should be placed in carry-on bags instead of bins. This reduces the handling of these items during screening.
- Food items should be carried in a plastic bag and placed in a bin for screening. Separating food from carry-on bags lessens the likelihood that screeners will need to open bags for inspection.
Be sure to wash your hands with soap and water for at least 20 seconds directly before and after going through screening.
Public transportation
If you travel by bus or train and you aren't vaccinated, be aware that sitting or standing within 6 feet (2 meters) of others for a long period can put you at higher risk of getting or spreading COVID-19 . Follow the precautions described above for protecting yourself during travel.
Even if you fly, you may need transportation once you arrive at your destination. You can search car rental options and their cleaning policies on the internet. If you plan to stay at a hotel, check into shuttle service availability.
If you'll be using public transportation and you aren't vaccinated, continue physical distancing and wearing a mask after reaching your destination.
Hotels and other lodging
The hotel industry knows that travelers are concerned about COVID-19 and safety. Check any major hotel's website for information about how it's protecting guests and staff. Some best practices include:
- Enhanced cleaning procedures
- Physical distancing recommendations indoors for people who aren't vaccinated
- Mask-wearing and regular hand-washing by staff
- Mask-wearing indoors for guests in public places in areas that have high cases of COVID-19
- Vaccine recommendations for staff
- Isolation and testing guidelines for staff who've been exposed to COVID-19
- Contactless payment
- Set of rules in case a guest becomes ill, such as closing the room for cleaning and disinfecting
- Indoor air quality measures, such as regular system and air filter maintenance, and suggestions to add air cleaners that can filter viruses and bacteria from the air
Vacation rentals, too, are enhancing their cleaning procedures. They're committed to following public health guidelines, such as using masks and gloves when cleaning, and building in a waiting period between guests.
Make a packing list
When it's time to pack for your trip, grab any medications you may need on your trip and these essential safe-travel supplies:
- Alcohol-based hand sanitizer (at least 60% alcohol)
- Disinfectant wipes (at least 70% alcohol)
- Thermometer
Considerations for people at increased risk
Anyone can get very ill from the virus that causes COVID-19 . But older adults and people of any age with certain medical conditions are at increased risk for severe illness. This may include people with cancer, serious heart problems and a weakened immune system. Getting the recommended COVID-19 vaccine and booster doses can help lower your risk of being severely ill from COVID-19 .
Travel increases your chance of getting and spreading COVID-19 . If you're unvaccinated, staying home is the best way to protect yourself and others from COVID-19 . If you must travel and aren't vaccinated, talk with your health care provider and ask about any additional precautions you may need to take.
Remember safety first
Even the most detailed and organized plans may need to be set aside when someone gets ill. Stay home if you or any of your travel companions:
- Have signs or symptoms, are sick or think you have COVID-19
- Are waiting for results of a COVID-19 test
- Have been diagnosed with COVID-19
- Have had close contact with someone with COVID-19 in the past five days and you're not up to date with your COVID-19 vaccines
If you've had close contact with someone with COVID-19 , get tested after at least five days. Wait to travel until you have a negative test. Wear a mask if you travel up to 10 days after you've had close contact with someone with COVID-19 .
- How to protect yourself and others. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html. Accessed Feb. 4, 2022.
- Domestic travel during COVID-19. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/travel-during-covid19.html. Accessed Feb. 4, 2022.
- Requirement for face masks on public transportation conveyances and at transportation hubs. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/face-masks-public-transportation.html. Accessed Feb. 4, 2022.
- International travel. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/international-travel/index.html. Accessed Feb. 4, 2022.
- U.S citizens, U.S. nationals, U.S. lawful permanent residents, and immigrants: Travel to and from the United States. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/international-travel-during-covid19.html. Accessed Feb. 4, 2022.
- Non-US. citizen, non-U.S. immigrants: Air travel to the United States. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/noncitizens-US-air-travel.html. Accessed Feb. 4, 2022.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed Feb. 4, 2022.
- Stay up to date with your vaccines. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html. Accessed Feb. 4, 2022.
- Pack smart. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/page/pack-smart. Accessed Feb. 4, 2022.
- Travel: Frequently asked questions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/faqs.html. Accessed Feb. 7, 2022.
- Coronavirus (COVID-19) information. Transportation Security Administration. https://www.tsa.gov/coronavirus. Accessed Feb. 7, 2022.
- WHO advice for international traffic in relation to the SARS-CoV-2 Omicron variant (B.1.1.529). World Health Organization. https://www.who.int/news-room/articles-detail/who-advice-for-international-traffic-in-relation-to-the-sars-cov-2-omicron-variant. Accessed Feb. 7, 2022.
- VRHP/VRMA Cleaning guidelines for COVID-19. Vacation Rental Management Association. https://www.vrma.org/page/vrhp/vrma-cleaning-guidelines-for-covid-19. Accessed Feb. 7, 2022.
- Safe stay. American Hotel & Lodging Association. https://www.ahla.com/safestay. Accessed Feb. 7, 2022.
- Khatib AN, et al. COVID-19 transmission and the safety of air travel during the pandemic: A scoping review. Current Opinion in Infectious Diseases. 2021; doi:10.1097/QCO.0000000000000771.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and coronavirus
- COVID-19 and pets
- COVID-19 and your mental health
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- COVID-19 drugs: Are there any that work?
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
U.S. travel resources
- Check CDC recommendations for travel within the U.S.
- Review testing requirements for travel to the U.S.
- Look up restrictions at your destination .
- Review airport security measures .
Related resources
Make twice the impact.
Your gift can go twice as far to advance cancer research and care!
Advertisement
Supported by
What to Know About the C.D.C. Guidelines on Vaccinated Travel
In updated recommendations, the federal health agency said both domestic and international travel was low risk for fully vaccinated Americans. But travel remains far from simple.
- Share full article

By Ceylan Yeginsu
The Centers for Disease Control and Prevention updated its guidance for fully vaccinated Americans in April, saying that traveling both domestically and internationally was low risk.
The long-awaited recommendations were issued by federal health officials after a series of studies found that vaccines administered in the United States were robustly effective in preventing infections in real-life conditions.
One is considered fully vaccinated two weeks after receiving the single dose of the Johnson & Johnson vaccine, or two weeks after receiving the second dose of the Pfizer-BioNTech or Moderna shots.
If you decide to travel, you might still have some questions. Here are the answers.
Will I still need to wear a mask and socially distance while traveling?
Yes. Under federal law, masks must be worn at airports in the United States, onboard domestic flights and in all transport hubs. The C.D.C. says that as long as coronavirus measures are taken in these scenarios, including mask wearing, fully vaccinated Americans can travel domestically without having to take a test or quarantine, although the agency warns that some states and territories may keep their local travel restrictions and recommendations in place.
For those wishing to travel internationally, a coronavirus test will not be required before departure from the United States unless mandated by the government of their destination. Vaccinated travelers are still required to get tested three days before travel by air into the United States, and are advised to take a test three to five days after their return, but will not need to self-quarantine.
Can I go abroad?
Yes, but only to countries that will have you.
More than half the world’s countries have reopened to tourists from the United States, including the countries of the European Union , which on June 18 added the United States to its “safe list” of countries, meaning that American travelers can now visit. While the European Union aims to take a coordinated approach to travel this summer, member states will be allowed to set their own requirements for travelers from individual countries based on their own epidemiological criteria, which means they may require testing or vaccination.
Some places like Turkey, Croatia and Montenegro had already been welcoming Americans with negative test results. Greece joined that growing list in May, ahead of most European countries, opening to fully vaccinated tourists and other foreigners with a negative test.
Many Caribbean nations have reopened to American tourists, but each has its own coronavirus protocols and entry requirements.
Here’s a full list of countries Americans can currently travel to.
What about domestic travel? Is it free and clear to cross state borders?
If you are fully vaccinated, the C.D.C. says you can travel freely within the United States and that you do not need to get tested, or self-quarantine, before or after traveling. But some states and local governments may choose to keep travel restrictions in place, including testing, quarantine and stay-at-home orders. Hawaii , for instance, still has travel restrictions in place.
Before you travel across state lines, check the current rules at your destination.
How are they going to check that I’m fully vaccinated?
Right now, the best way to prove that you have been vaccinated is to show your vaccine card .
Digital vaccine and health certificates showing that people have been vaccinated or tested are in various stages of development around the world and are expected, eventually, to be widely used to speed up travel.
The subject of “ vaccine passports ” is currently one of the most hotly debated topics within the travel industry, with questions over the equity of their use and concerns over health and data privacy.
In early April, Gov. Ron DeSantis of Florida issued an executive order that would ban local governments and state businesses from requiring proof of vaccination for services.
And in March, the European Union endorsed its own vaccine certificate , which some countries are already using, with more expected to adopt it by July 1.
But what about my kids? What’s the guidance on traveling with unvaccinated people?
The C.D.C. advises people against travel unless they have been vaccinated. If you must travel, the agency recommends testing one to three days before a trip and following all coronavirus guidance at your destination.
In May, the F.D.A. expanded its emergency use authorization of the Pfizer-BioNTech coronavirus vaccine to include adolescents between 12 and 15 years of age.
All air passengers aged two and older coming into the United States, including fully vaccinated people, are required to have a negative Covid-19 test result taken no more than three days before they board their flight.
What is my moral obligation to the places I visit where most people are not vaccinated?
The United States inoculation rollout has been among the fastest in the world, but there is a stark gap between its rapid rollout and the vaccination programs in different countries. Some nations have yet to report a single dose being administered.
Many countries are currently seeing a surge in new cases and are implementing strict coronavirus protocols, including mask mandates in public spaces, capacity limits at restaurants and tourist sites and other lockdown restrictions.
It is important to check coronavirus case rates, measures and medical infrastructure before traveling to your destination and not to let your guard down when you get there. Even though you are fully vaccinated, you may still be able to transmit the disease to local communities who have not yet been inoculated.
You can track coronavirus vaccination rollouts around the world here.
Follow New York Times Travel on Instagram , Twitter and Facebook . And sign up for our weekly Travel Dispatch newsletter to receive expert tips on traveling smarter and inspiration for your next vacation.
Ceylan Yeginsu is a London-based reporter. She joined The Times in 2013, and was previously a correspondent in Turkey covering politics, the migrant crisis, the Kurdish conflict, and the rise of Islamic State extremism in Syria and the region. More about Ceylan Yeginsu
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Traveler's Health
Related issues, see, play and learn.
- No links available
Clinical Trials
- Journal Articles
Find an Expert
Older adults, patient handouts.
Traveling can increase your chances of getting sick. A long flight can increase your risk for deep vein thrombosis. Once you arrive, it takes time to adjust to the water, food, and air in another place. Water in developing countries can contain viruses , bacteria , and parasites that cause stomach upset and diarrhea. Be safe by using only bottled or purified water for drinking, making ice cubes, and brushing your teeth. If you use tap water, boil it or use iodine tablets. Food poisoning can also be a risk. Eat only food that is fully cooked and served hot. Avoid unwashed or unpeeled raw fruits and vegetables.
If you are traveling out of the country, you might also need vaccinations or medicines to prevent specific illnesses. Which ones you need will depend on what part of the world you're visiting, the time of year, your age, overall health status, and previous vaccinations. See your doctor 4 to 6 weeks before your trip. Most vaccines take time to become effective.
Centers for Disease Control and Prevention
- International Travel: Tips for Staying Healthy (American Academy of Family Physicians) Also in Spanish
- Staying Healthy While You Travel (For Parents) (Nemours Foundation) Also in Spanish
- Travelers' Health (Centers for Disease Control and Prevention)
- Air Travel Health Tips (American Academy of Family Physicians) Also in Spanish
- Travelers' Health: Air Quality and Ionizing Radiation (Centers for Disease Control and Prevention)
- Travelers' Health: Cruise Ship Travel (Centers for Disease Control and Prevention)
- Travelers' Health: Extremes of Temperature (Centers for Disease Control and Prevention)
- Travelers' Health: Immunocompromised Travelers (Centers for Disease Control and Prevention)
- Travelers' Health: Injury and Trauma (Centers for Disease Control and Prevention)
- Travelers' Health: International Adoption (Centers for Disease Control and Prevention)
- Travelers' Health: Mosquitoes, Ticks, and Other Arthropods (Centers for Disease Control and Prevention)
- Travelers' Health: Travel Health Kits (Centers for Disease Control and Prevention)
- Travelers' Health: Zoonotic Exposures -- Bites, Stings, Scratches, and Other Hazards (Centers for Disease Control and Prevention)
- Your Health Abroad (Department of State, Bureau of Consular Affairs)
- Ears and Altitude (Barotrauma) (American Academy of Otolaryngology--Head and Neck Surgery)
- Foot Swelling during Air Travel: A Concern? (Mayo Foundation for Medical Education and Research) Also in Spanish
- Influenza Prevention: Information for Travelers (Centers for Disease Control and Prevention) Also in Spanish
- Jet Lag Disorder (Mayo Foundation for Medical Education and Research) Also in Spanish
- Motion Sickness: First Aid (Mayo Foundation for Medical Education and Research) Also in Spanish
- Protect against Mosquito Bites when Traveling (Centers for Disease Control and Prevention) - PDF Also in Spanish
- Rabies: What If I Receive Treatment Outside the United States? (Centers for Disease Control and Prevention)
- Traveler's Diarrhea (Centers for Disease Control and Prevention) Also in Spanish
- Travelers' Health: COVID-19 (Centers for Disease Control and Prevention)
- Travelers' Health: Destinations (Centers for Disease Control and Prevention)
- Visiting Friends or Relatives (Centers for Disease Control and Prevention)
- Zika Travel Information (Centers for Disease Control and Prevention) Also in Spanish
Journal Articles References and abstracts from MEDLINE/PubMed (National Library of Medicine)
- Article: A methodology for estimating SARS-CoV-2 importation risk by air travel into...
- Article: Risk perception about communicable and vector borne diseases among international travellers...
- Article: Perception, confidence, and willingness to respond to in-flight medical emergencies among...
- Traveler's Health -- see more articles
- Centers for Disease Control and Prevention Also in Spanish
- Flying and Your Child's Ears (Nemours Foundation) Also in Spanish
- Travelers' Health: Traveling Safely with Infants and Children (Centers for Disease Control and Prevention)
- Travelers' Health: Vaccine Recommendations for Infants and Children (Centers for Disease Control and Prevention)
- Travel during Pregnancy (American College of Obstetricians and Gynecologists)
- Travelers' Health: Travel and Breastfeeding (Centers for Disease Control and Prevention)
- Travelers' Health: Senior Citizens (Centers for Disease Control and Prevention)
- Jet lag prevention (Medical Encyclopedia) Also in Spanish
- Pregnancy and travel (Medical Encyclopedia) Also in Spanish
The information on this site should not be used as a substitute for professional medical care or advice. Contact a health care provider if you have questions about your health.
CDC Health Information for International Travel: Yellow Book
As unprecedented numbers of travelers cross international borders each day, the need for up-to-date, actionable information about the health challenges posed by this mass movement has never been greater. For both international travelers and the health professionals who care for them, CDC Health Information for International Travel (more commonly known as the Yellow Book ) is the definitive guide to staying healthy and safe anywhere in the world. The Yellow Book is produced biennially with input from hundreds of travel medicine experts and is published through a unique collaboration between CDC, the CDC Foundation and Oxford University Press.
The 2018 edition codifies the U.S. government’s most current health guidelines and information for international travelers, including pretravel vaccine recommendations, destination-specific advice, and easy-to-reference maps , tables and charts . The book also offers updated guidance for specific types of travel and travelers, including:
- Precautions for pregnant travelers, immunocompromised travelers and travelers with disabilities
- Special considerations for newly arrived adoptees , immigrants and refugees
- Practical tips for last-minute or resource-limited travelers
- Advice for air crews , humanitarian workers , missionaries and others who provide care and support overseas
The 2018 Yellow Book includes important travel medicine updates:
- The latest information about emerging infectious disease threats such as Zika , Ebola and MERS
- New cholera vaccine recommendations
- Updated guidance on the use of antibiotics in the treatment of travelers' diarrhea
- Special considerations for unique types of travel, such as wilderness expeditions , work-related travel and study abroad
- Destination-specific recommendations for popular itineraries, including new sections for travelers to Cuba and Burma
Written by a team of CDC experts on the forefront of travel medicine, the Yellow Book provides a user-friendly, vital resource for those in the business of keeping travelers healthy abroad. Order the 2018 edition online .

©David Snyder/CDC Foundation

NICHOLAS A. RATHJEN, DO, AND S. DAVID SHAHBODAGHI, MD, MPH
Am Fam Physician. 2023;108(4):396-403
Author disclosure: No relevant financial relationships.
Approximately 1.8 billion people will cross an international border by 2030, and 66% of travelers will develop a travel-related illness. Most travel-related illnesses are self-limiting and do not require significant intervention; others could cause significant morbidity or mortality. Physicians should begin with a thorough history and clinical examination to have the highest probability of making the correct diagnosis. Targeted questioning should focus on the type of trip taken, the travel itinerary, and a list of all geographic locations visited. Inquiries should also be made about pretravel preparations, such as chemoprophylactic medications, vaccinations, and any personal protective measures such as insect repellents or specialized clothing. Travelers visiting friends and relatives are at a higher risk of travel-related illnesses and more severe infections. The two most common vaccine-preventable illnesses in travelers are influenza and hepatitis A. Most travel-related illnesses become apparent soon after arriving at home because incubation periods are rarely longer than four to six weeks. The most common illnesses in travelers from resource-rich to resource-poor locations are travelers diarrhea and respiratory infections. Localizing symptoms such as fever with respiratory, gastrointestinal, or skin-related concerns may aid in identifying the underlying etiology.
Globally, it is estimated that 1.8 billion people will cross an international border by 2030. 1 Although Europe is the most common destination, tourism is increasing in developing regions of Asia, Africa, and Latin America. 2 Less than one-half of U.S. travelers seek pretravel medical advice. It is estimated that two-thirds of travelers will develop a travel-related illness; therefore, the ill returning traveler is not uncommon in primary care. 3 Although most of these illnesses are minor and relatively insignificant clinically, the potential exists for serious illness. The advent of modern and interconnected travel networks means that a rare illness or nonendemic infectious disease is never more than 24 hours away. 4 Travelers over the past 10 years have contributed to the increase of emerging infectious diseases such as chikungunya, Zika virus infection, COVID-19, mpox (monkeypox), and Ebola disease. 3
Although most travel-related illnesses are self-limiting and do not require medical evaluation, others could be life-threatening. 5 The challenge for the busy physician is successfully differentiating between the two. Physicians should begin with a thorough history and clinical examination to have the highest probability of making the correct diagnosis. Travelers at the highest risk are those visiting friends and relatives who stay in a country for more than 28 days or travel to Africa. Most travel-related illnesses become apparent soon after arriving home because incubation periods are rarely longer than four to six weeks. 3 , 6 The most common illnesses in travelers from resource-rich to resource-poor locations are travelers diarrhea and respiratory infections. 7 , 8 The incubation period of an illness relative to the onset of symptoms and the length of stay in the foreign destination can exclude infections in the differential diagnosis ( eTable A ) .
General questions should determine the patient’s pertinent medical history, focusing on any unique factors, such as immunocompromising illnesses or underlying risk factors for a travel-related medical concern. Targeted questioning should focus on the type of trip taken and the travel itinerary that includes accommodations, recreational activities, and a list of all geographic locations visited ( Table 1 3 , 6 , 9 and Table 2 3 , 6 ) . Patients should be asked about any medical treatments received in a foreign country. Modern travel itineraries often require multiple stopovers, and it is not uncommon for the casual traveler to visit several locations with different geographically linked illness patterns in a single trip abroad.
Travel History
Travelers visiting friends and relatives are at a higher risk of travel-related illnesses and more severe infections. 10 , 11 These travelers rarely seek pretravel consultation, are less likely to take chemoprophylaxis, and engage in more risky travel-related behaviors such as consuming food from local sources and traveling to more remote locations. 3 Overall, travelers visiting friends and relatives tend to have extended travel stays and are more likely to reside in non–climate-controlled dwellings.
During the clinical history, inquiries should be made about pretravel preparations, including chemoprophylactic medications, vaccinations, and personal protective measures such as insect repellents or specialized clothing. 12 , 13 Accurate knowledge of previous preventive strategies allows for appropriate risk stratification by physicians. Even when used thoroughly, these measures decrease the likelihood of certain illnesses but do not exclude them. 6 Adherence to dietary precautions and pretravel immunization against typhoid fever do not necessarily eliminate the risk of disease. Travelers often have no control over meals prepared in foreign food establishments, and the currently available typhoid vaccines are 60% to 80% effective. 14 Although all travel-related vaccines are important, the two most common vaccine-preventable illnesses in travelers are influenza and hepatitis A. 12 , 15
Travel duration is also an important but often overlooked component of the clinical history because the likelihood of illness increases directly with the length of stay abroad. The longer travelers stay in a non-native environment, the more likely they are to forego travel precautions and adherence to chemoprophylaxis. 3 The use of personal protective measures decreases gradually with the total amount of time in the host environment. 3 A thorough medical and sexual history should be obtained because data show that sexual contact during travel is common and often occurs without the use of barrier contraception. 16
Clinical Assessment
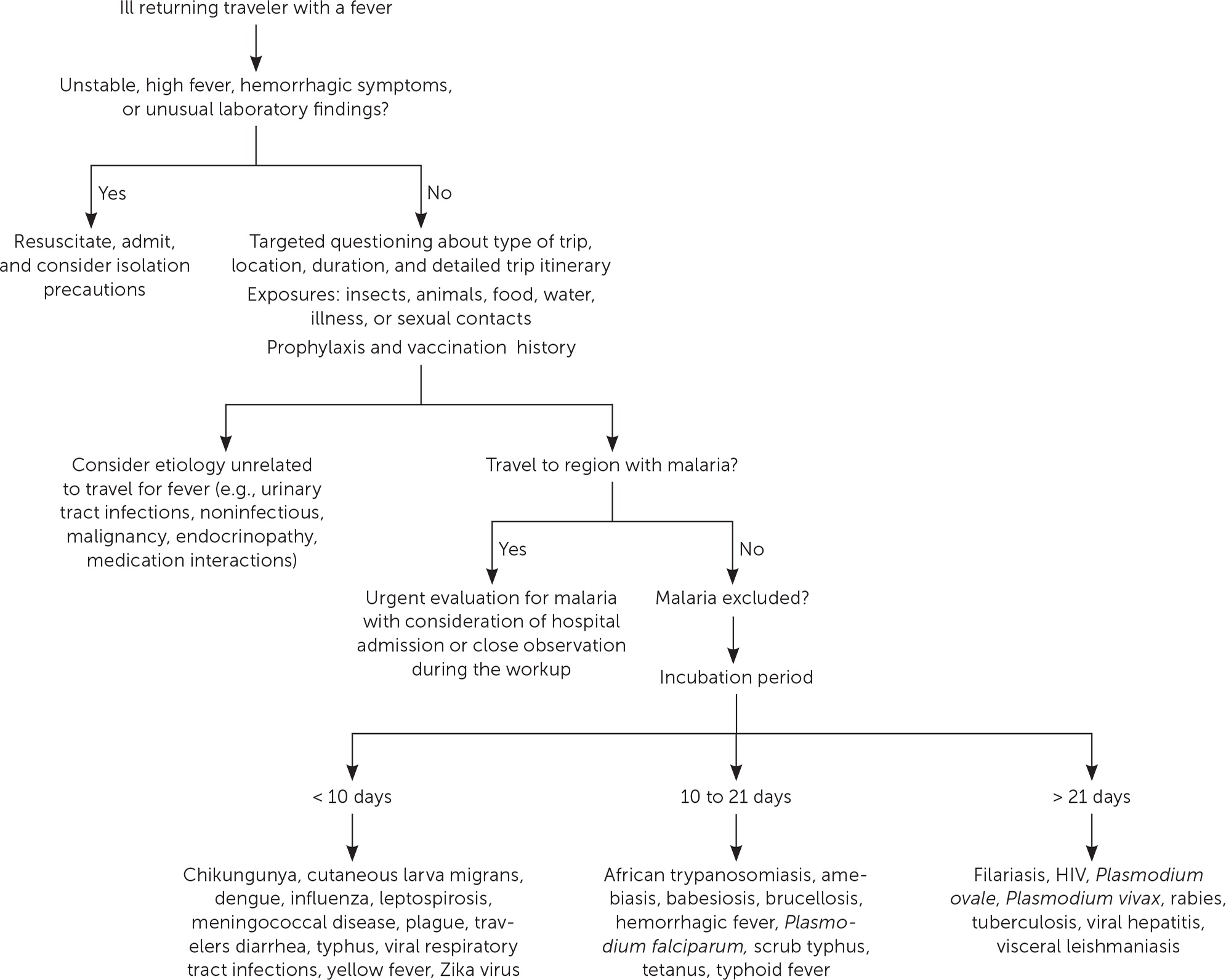
The severity of the illness helps determine if the patient should be admitted to the hospital while the evaluation is in progress. 3 Patients with high fevers, hemorrhagic symptoms, or abnormal laboratory findings should be hospitalized or placed in isolation ( Figure 1 ) . For patients with a higher severity of illness, consultation with an infectious disease or tropical/travel medicine physician is advised. 3 Patients with symptoms that suggest acute malaria (e.g., fever, altered mental status, chills, headaches, myalgias, malaise) should be admitted for observation while the evaluation is expeditiously completed. 13
Many tools can assist physicians in making an accurate diagnosis. The GeoSentinel is a worldwide data collection network for the surveillance and research of travel-related illnesses; however, this service requires a subscription. The network can guide physicians to the most likely illness based on geographic location and top diagnoses by geography. 4 For example, Plasmodium falciparum malaria is the most common serious febrile illness in travelers to sub-Saharan Africa. 17
Ill returning travelers should have a laboratory evaluation performed with a complete blood count, comprehensive metabolic panel, and C-reactive protein. Additional testing may include blood-based rapid molecular assays for malaria and arboviruses; blood, stool, and urine cultures; and thick and thin blood smears for malaria. 3 Emerging polymerase chain reaction technologies are becoming widely available across the United States. Multiplex and biofilm array polymerase chain reaction platforms for bacterial, viral, and protozoal pathogens are now available at most tertiary health care centers. 4 Multiplex and biofilm platforms include dedicated panels for respiratory and gastrointestinal illnesses and bloodborne pathogens. These tests allow for real-time or near real-time diagnosis of agents that were previously difficult to isolate outside of the reference laboratory setting.
Table 3 lists common tropical diseases and associated vectors. 3 , 6 , 18 Physicians should be aware of unique and emerging infections, such as viral hemorrhagic fevers, COVID-19, and novel respiratory pathogens, in addition to common illnesses. Testing for infections of public health importance can be performed with assistance from local public health authorities. 19 In cases of short-term travel, previously acquired non–travel-related conditions should be on any list of applicable differential diagnoses. References on infectious diseases endemic in many geographic locations are accessible online. The Centers for Disease Control and Prevention (CDC) Travelers’ Health website provides free resources for patients and health care professionals at https://www.cdc.gov/travel .
Febrile Illness
A fever typically accompanies serious illnesses in returning travelers. Patients with a fever should be treated as moderately ill. One barrier to an accurate and early diagnosis of travel-related infections is the nonspecific nature of the initial symptoms of illness. Often, these symptoms are vague and nonfocal. A febrile illness with a fever as the primary presenting symptom could represent a viral upper respiratory tract infection, acute influenza, or even malaria, typhoid, or dengue, which are the most life-threatening. According to GeoSentinel data, 91% of ill returning travelers with an acute, life-threatening illness present with a fever. 20 All travelers who are febrile and have recently returned from a malarious area should be urgently evaluated for the disease. 13 , 21 Travelers who have symptoms of malaria should seek medical attention, regardless of whether prophylaxis or preventive measures were used. Suspicion of P. falciparum malaria is a medical emergency. 13 Clinical deterioration or death can occur in a malaria-naive patient within 24 to 36 hours. 22 Dengue is an important cause of fever in travelers returning from tropical locations. An estimated 50 million to 100 million global cases of dengue are reported annually, with many more going undetected. 23 eTable B lists the most common causes of fever in the returning traveler.
Respiratory Illness
Respiratory infections are common in the United States and throughout the world. Ill returning travelers with respiratory concerns are statistically most likely to have a viral respiratory tract infection. 24 Influenza circulates year-round in tropical climates and is one of the most common vaccine-preventable illnesses in travelers. 3 , 12 Influenza A and B frequently present with a low-grade fever, cough, congestion, myalgia, and malaise. eTable C lists the most common causes of respiratory illnesses in the returning traveler.
Gastrointestinal Illness
Gastrointestinal symptoms account for approximately one-third of returning travelers who seek medical attention. 25 Most diarrhea in travelers is self-limiting, with travelers diarrhea being the most common travel-related illness. 7 Diarrhea linked to travel in resource-poor areas is usually caused by bacterial, viral, or protozoal pathogens.
The most often encountered diarrheal pathogens are enterotoxigenic Escherichia coli and enteroaggregative E. coli , which are easily treated with commonly available antibiotics. 26 Physicians should be aware of emerging antibiotic resistance patterns across the globe. The CDC offers up-to-date travel information in the CDC Yellow Book . 3 Although patients are often concerned about parasites, they should be reassured that helminths and other parasitic infections are rare in the casual traveler. 3
The disease of concern in the setting of gastrointestinal symptoms is typhoid fever. Physicians should be aware that typhoid fever and paratyphoid fever are clinically indistinguishable, with cardinal symptoms of fever and abdominal pain. 3 Typhoid fever should be considered in ill returning travelers who do not have diarrhea, because typhoid infection may not present with diarrheal symptoms. The likelihood of typhoid fever also correlates with travel to endemic regions and should be considered an alternative diagnosis in patients not responding to antimalarial medications. A diagnosis of enteric fever can be confirmed with blood or stool cultures. Although less common, community-acquired Clostridioides difficile should be considered in the differential diagnosis in the setting of recent travel and potential antimicrobial use abroad. 27
Another important travel-related pathogen is hepatitis A due to its widespread distribution in the developing world and the small pathogen dose necessary to cause illness. Hepatitis A is a more serious infection in adults; however, many U.S. adults have been vaccinated because the hepatitis A vaccine is included in the recommended childhood immunization schedule. 28 eTable D lists the most common causes of gastrointestinal illnesses in the returning traveler.
Dermatologic Concerns
Dermatologic concerns are common among returning travelers and include noninfectious causes such as sun overexposure, contact with new or unfamiliar hygiene products, and insect bites. The most common infections in returning travelers with dermatologic concerns include cutaneous larva migrans, infected insect bites, and skin abscesses. Cutaneous larva migrans typically presents with an intensely pruritic serpiginous rash on the feet or gluteal region. 3 Questions about bites and bite avoidance measures should be asked of patients with symptomatic skin concerns; however, physicians should remember that many bites go unnoticed. 29
Formerly common illnesses in the United States are common abroad, with measles, varicella-zoster virus infection, and rubella occurring in child and adult travelers. 3 Measles is considered one of the most contagious infectious diseases. More than one-third of child travelers from the United States have not completed the recommended course of measles, mumps, and rubella vaccines at the time of travel due to immunization scheduling. One-half of all measles importations into the United States comes from these international travelers. 30 Measles should always be considered in the differential because of the low or incomplete vaccination rates in travelers and high levels of exposure in some areas abroad. eTable E lists the most common infectious causes of dermatologic concern in the returning traveler.
Data Sources: A PubMed search was completed using the key words prevention, diagnosis, treatment, travel related illness, surveillance, travel medicine, chemoprophylaxis, and returning traveler treatment. The search was limited to English-language studies published since 2000. Secondary references from the key articles identified by the search were used as well. Also searched were the Centers for Disease Control and Prevention and Cochrane databases. Search dates: September 2022 to November 2022, March 2023, and August 2023.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the U.S. Army, the U.S. Department of Defense, or the U.S. government.
The World Tourism Organization. International tourists to hit 1.8 billion by 2030. October 11, 2011. Accessed March 2023. https://www.unwto.org/archive/global/press-release/2011-10-11/international-tourists-hit-18-billion-2030
- Angelo KM, Kozarsky PE, Ryan ET, et al. What proportion of international travellers acquire a travel-related illness? A review of the literature. J Travel Med. 2017;24(5):10.1093/jtm/tax046.
Centers for Disease Control and Prevention. CDC Yellow Book: Health Information for International Travel . Oxford University Press; 2023. Accessed August 26, 2023. https://wwwnc.cdc.gov/travel/yellowbook/2024/table-of-contents
Wu HM. Evaluation of the sick returned traveler. Semin Diagn Pathol. 2019;36(3):197-202.
Scaggs Huang FA, Schlaudecker E. Fever in the returning traveler. Infect Dis Clin North Am. 2018;32(1):163-188.
Feder HM, Mansilla-Rivera K. Fever in returning travelers: a case-based approach. Am Fam Physician. 2013;88(8):524-530.
Giddings SL, Stevens AM, Leung DT. Traveler's diarrhea. Med Clin North Am. 2016;100(2):317-330.
Harvey K, Esposito DH, Han P, et al.; Centers for Disease Control and Prevention. Surveillance for travel-related disease–GeoSentinel Surveillance System, United States, 1997–2011. MMWR Surveill Summ. 2013;62:1-23.
Sridhar S, Turbett SE, Harris JB, et al. Antimicrobial-resistant bacteria in international travelers. Curr Opin Infect Dis. 2021;34(5):423-431.
Matteelli A, Carvalho AC, Bigoni S. Visiting relatives and friends (VFR), pregnant, and other vulnerable travelers. Infect Dis Clin North Am. 2012;26(3):625-635.
Ladhani S, Aibara RJ, Riordan FA, et al. Imported malaria in children: a review of clinical studies. Lancet Infect Dis. 2007;7(5):349-357.
Sanford C, McConnell A, Osborn J. The pretravel consultation. Am Fam Physician. 2016;94(8):620-627.
Shahbodaghi SD, Rathjen NA. Malaria. Am Fam Physician. 2022;106(3):270-278.
Freedman DO, Chen LH, Kozarsky PE. Medical considerations before international travel. N Engl J Med. 2016;375(3):247-260.
- Marti F, Steffen R, Mutsch M. Influenza vaccine: a travelers' vaccine? Expert Rev Vaccines. 2008;7(5):679-687.
Vivancos R, Abubakar I, Hunter PR. Foreign travel, casual sex, and sexually transmitted infections: systematic review and meta-analysis. Int J Infect Dis. 2010;14(10):e842-e851.
Paquet D, Jung L, Trawinski H, et al. Fever in the returning traveler. Dtsch Arztebl Int. 2022;119(22):400-407.
Cantey PT, Montgomery SP, Straily A. Neglected parasitic infections: what family physicians need to know—a CDC update. Am Fam Physician. 2021;104(3):277-287.
Rathjen NA, Shahbodaghi SD. Bioterrorism. Am Fam Physician. 2021;104(4):376-385.
Jensenius M, Davis X, von Sonnenburg F, et al.; Geo-Sentinel Surveillance Network. Multicenter GeoSentinel analysis of rickettsial diseases in international travelers, 1996–2008. Emerg Infect Dis. 2009;15(11):1791-1798.
Tolle MA. Evaluating a sick child after travel to developing countries. J Am Board Fam Med. 2010;23(6):704-713.
Centers for Disease Control and Prevention. About malaria. February 2, 2022. Accessed August 21, 2022. https://www.cdc.gov/malaria/about/index.html
Wilder-Smith A, Schwartz E. Dengue in travelers. N Engl J Med. 2005;353(9):924-932.
Summer A, Stauffer WM. Evaluation of the sick child following travel to the tropics. Pediatr Ann. 2008;37(12):821-826.
Swaminathan A, Torresi J, Schlagenhauf P, et al.; GeoSentinel Network. A global study of pathogens and host risk factors associated with infectious gastrointestinal disease in returned international travellers. J Infect. 2009;59(1):19-27.
Shah N, DuPont HL, Ramsey DJ. Global etiology of travelers' diarrhea: systematic review from 1973 to the present. Am J Trop Med Hyg. 2009;80(4):609-614.
Michal Stevens A, Esposito DH, Stoney RJ, et al.; GeoSentinel Surveillance Network. Clostridium difficile infection in returning travellers. J Travel Med. 2017;24(3):1-6.
Mayer CA, Neilson AA. Hepatitis A - prevention in travellers. Aust Fam Physician. 2010;39(12):924-928.
Herness J, Snyder MJ, Newman RS. Arthropod bites and stings. Am Fam Physician. 2022;106(2):137-147.
Bangs AC, Gastañaduy P, Neilan AM, et al. The clinical and economic impact of measles-mumps-rubella vaccinations to prevent measles importations from U.S. pediatric travelers returning from abroad. J Pediatric Infect Dis Soc. 2022;11(6):257-266.
Continue Reading

More in AFP
More in pubmed.
Copyright © 2023 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
International Travel & Infectious Disease
- International Travel Home
- Guidance for Travelers
- Materials and Resources
- For Health Professionals
Related Topics
- Immunization Information for International Travelers
- International Travel Health Clinics Serving Minnesota Residents
- Coronavirus Disease 2019 (COVID-19)
- Mosquitoborne Diseases
- Measles (Rubeola)
Contact Info
International travel and infectious disease.
Traveling abroad can increase your exposure to infectious diseases caused by viruses, bacteria, or parasites. Some significant infectious health hazards for Americans traveling abroad are diarrhea, malaria, hepatitis A, and other emerging diseases.
- Guidance for Travelers Many diseases are just a plane ride away. Take care of yourself and others before you travel and when you return with this information.
- Materials and Resources Videos, posters, and other materials that you can share, view, or print.
- Guidance for Health Professionals Screening and triage information, clinical evaluation resources, infection control guidance, and other resources for health care providers.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

Management of Travel-Related Infectious Diseases in the Emergency Department
Laura throckmorton.
1 Center for Emergency Medicine, University Hospitals Cleveland Medical Center, 11100 Euclid Ave., Cleveland, OH 44106 USA
Jonathan Hancher
2 Department of Emergency Medicine, University of North Carolina Hospitals, University of North Carolina, Physician Office Building, 170 Manning Drive, CB# 7594, Chapel Hill, NC 27599-7594 USA
Purpose of Review
Emergency physicians generally have limited exposure to internationally acquired illnesses. However, travelers can present quite ill, and delays in recognition and treatment can lead to increased morbidity and mortality. This paper aims to summarize typical presentations of common international diseases and provide the emergency physician with a practical approach based on current guidelines.
Recent Findings
In the treatment of traveler’s diarrhea, azithromycin has become the treatment of choice due to the growing antibiotic resistance. Intravenous artesunate was approved in 2019 under investigational new drug protocol for the treatment of severe malaria, and artemisinin-based combination therapies (ACTs) have become the first-line treatment for most cases of uncomplicated malaria. Since the 2015 outbreak, Zika has become a concern to many travelers, but the current treatment is supportive.
Clinicians should be aware of a few noteworthy updates in the treatment of internationally acquired illnesses, but more importantly, they must recognize warning signs of severe illness and treat promptly. Future research on workup and disposition could help emergency physicians identify which patients need admission in well-appearing febrile travelers.
Introduction
While variable by practice setting, most emergency physicians in the USA have little regular exposure to internationally acquired illnesses. Therefore, their ability to recognize these illnesses can be limited. While basic practice guidelines are available, confirmatory diagnostic testing in the emergency department is limited, and some treatments might not be readily available. This article aims to assist the emergency physician identify internationally acquired illnesses based on travel history, signs, and symptoms and to help guide management based upon current guidelines and their practical applicability in the emergency department.
While the emergency physician is unlikely to be providing pre-travel care in the USA, many EM physicians travel internationally and therefore need to be aware of primary prevention strategies for themselves and patients they treat while abroad. Country-specific guidelines are published by the Centers for Disease Control (CDC), but general considerations include vaccination, prophylactic antibiotics, and protection from insect bites or infected water sources.
Mosquito-Borne Illnesses
- Bite prevention: Travelers to areas with malaria, Zika virus, and other mosquito-borne illnesses can minimize their risk by wearing long sleeves and pants, using bed netting, minimizing outdoor activities around dusk, and avoiding travel during the rainy season [ 1 ].
Table 1
Malaria chemoprophylaxis
Source: CDC [ 2 ]
- Standby emergency treatment (SBET): While chemoprophylaxis is the most efficacious in malaria prevention, SBET has also become an option for travelers who are traveling to low-risk areas who do not want to take chemoprophylaxis for the duration of their travel. Patients using this method should begin taking prescribed antimalarials if they develop a fever and seek a medical evaluation as soon as possible.
Vaccinations
- Second dose after 6 months for long-term immunity
- Particularly important due to rising antibiotic resistance of S. typhi
- Little to no efficacy against S. paratyphi
- Must be kept refrigerated and consumed 1 h prior to a meal
- Cannot be given to immunocompromised patients
- Booster needed every 5 years
- Booster needed every 2 years
- Increased risk of severe dengue with subsequent exposure if given to naïve patient
- Available through age 45 in many endemic countries
- Three doses spaced every 6 months
General Approach to the Febrile Traveler
When treating a febrile patient with a history of travel, important considerations include travel location, timing, sick contacts, weather, activities partaken while abroad, pregnancy, and medical comorbidities. Many infectious diseases acquired abroad can also take several weeks to manifest. Practitioners should remember to test for common local illness, particularly influenza during flu season, and cover for a broad range of illnesses in toxic-appearing patients.
Workup is dependent on location and timing of travel to help determine which diseases are most likely. For cases in which many pathogens seem possible, we would recommend lab workup to include complete blood count with differential, basic metabolic panel; liver function tests; coagulation screen; blood smear; CK level; pregnancy test; influenza swab; blood cultures; urinalysis; urine culture; and chest x-ray. While many findings are nonspecific, these tests will likely identify patients with warning signs of severe illness and might help guide the practitioner toward the most likely pathogen.
Many internationally acquired illnesses cannot be definitively diagnosed in the emergency department given the similar features of many diseases and the delay in diagnostic results. In determining disposition, clinicians should consider warning signs of severe disease for the most likely cause of illness, and if present, admit. Many febrile illnesses can be managed in the outpatient setting, but patients should be given strict return precautions and close follow-up. If the patient has a travel history which places him or her at risk of dengue, NSAIDs should be avoided until it has been definitively ruled out due to the risk of progression to dengue hemorrhagic fever.
Epidemiology and Transmission
Malaria is the most common febrile illness among travelers to endemic areas and is caused by the mosquito-borne parasites of the Plasmodium genus, primarily P. falciparum , P. vivax , P. ovale , and P. malariae . Cases in the USA have been increasing over the last few decades to over 2000 cases reported to the CDC in 2016. The majority of cases diagnosed in the USA are among travelers returning from Africa, particularly West Africa. P. falciparum has been identified in nearly 70% of infections with P. vivax being the second most common. Mortality in the USA is < 0.5% [ 6 •].

Signs and Symptoms
Symptoms of malaria include fever, headache, chills, diaphoresis, myalgias, diarrhea, vomiting, and cough. The onset of symptoms is dependent on the Plasmodium species with P. falciparum typically causing the most severe symptoms. In confirmed cases in 2016, over 90% of those with P. falciparum reported onset of symptoms within 1 month of returning to the USA [ 6 •]. However, nearly half of cases of P. vivax or P. ovale had onset of symptoms more than 1 month after returning to the USA likely due to reactivation of dormant liver parasites [ 6 •]. Febrile seizures can occur in children but should be considered a warning sign of cerebral malaria in any age group.
Severe malaria definitions vary between the CDC and the World Health Organization (WHO), but diagnosis can be made with any of the following signs and symptoms [ 7 , 8 , 55 ]:
- Seizures, altered mental status, or other neurologic manifestations
- Acute kidney injury
- Hemoglobin <7 g/dL
- Hypoglycemia (< 40 mg/dL)
- Liver failure or severe jaundice
- Hemodynamic instability
- > 5–10% parasitemia
Of confirmed US malaria cases reported in 2016, approximately 15% were classified as severe disease, and seven people died [ 6 •].
The diagnosis of malaria is typically by blood smear but can also be done by polymerase chain reaction. Additional laboratory abnormalities can include anemia, thrombocytopenia, elevated transaminases, mild coagulopathy, and elevated BUN and creatinine. Lumbar puncture has limited utility in cerebral malaria as results can be normal or show only mild elevations in total protein and cell counts with mildly depressed glucose [ 9 ]. If there is any concern for cerebral malaria, the patient should be treated empirically as mortality is high even with treatment.
Recommendations for treatment of malaria are dependent on the presence of any severe features, local resistance, and patient comorbidities. Access to antimalarials in the ED is likely to heavily influence treatment as even many large tertiary referral centers do not have most antimalarial drugs stocked. If the patient took prophylaxis while abroad, a different antimalarial should be selected for improved efficacy and reduced toxicity. The CDC does have a Malaria Hotline (770-488-7788) for treatment assistance with a staff member on call 24/7.
Based on CDC and WHO recommendations, we would recommend the following treatment for confirmed or suspected cases of malaria:
- WHO recommends ACTs as the first-line therapy due to highest cure rate.
- Chloroquine
- Hydroxychloroquine
- Atovaquone-proguanil
- Quinine + tetracycline, doxycycline, or clindamycin
- Second-line drug in first trimester due to limited safety data [ 11 ]
- Quinine + clindamycin
- Not accessible in the ED; must be shipped from CDC
- Quinidine: Production in the USA discontinued in 2017 [ 12 ]
- Interim treatment until IV Artesunate can be obtained from the CDC
- If unable to swallow pill, NG tube should be placed in ED
- Third line: atovaquone-proguanil or quinine.
- Intravenous clindamycin and doxycycline have been used in the past, but they are not recommended for the initial treatment of severe malaria as the onset of action is greater than 24 h [ 2 ].
Anyone with confirmed P. falciparum or species not yet known should be admitted to the hospital [ 10 ]. Patients with signs of severe malaria likely need admission to an intensive care unit. Those with no previous history of malaria, immunocompromised patients, children less than five, and pregnant women are at the highest risk for developing severe disease or rapid deterioration, and admission should be strongly considered [ 2 , 13 , 14 ].
Dengue is a febrile illness caused by a mosquito-borne flavivirus. It is endemic throughout the tropics and is estimated to cause symptoms in only one quarter of infections. According to the WHO, dengue is the second most common febrile illness in travelers returning from low- or middle-income countries [ 15 ]. There are four known serotypes (DEN1–4), and subsequent infection with a different serotype places the individual at higher risk of developing severe dengue.
Symptoms generally start 4–7 days following mosquito bite, and the disease consists of three phases [ 15 , 16 ]:
- 3–7 days
- High fevers (40C), severe headache, pain behind the eyes, myalgias, arthralgias, vomiting, lymphadenopathy, rash
- 24–48 h
- Defervescence, capillary leak, hypovolemia, potential development of severe dengue (dengue hemorrhagic fever [DHF] or dengue shock syndrome [DSS])
- Fatigue lasting days to weeks
Severe Dengue
Severe dengue (DHF/DSS) is rare and primarily seen in cases of secondary infection with a different serotype. Therefore, severe dengue is particularly uncommon in travelers and should only be expected in those with frequent travel to endemic areas. Nonetheless, severe dengue can be fatal, so awareness of certain features can help distinguish DHF and DSS from other severe febrile illnesses. These findings include pleural effusions, ascites, elevated hemoglobin in the setting of thrombocytopenia, low ESR, hepatomegaly, shock with narrow pulse pressure, petechiae/positive tourniquet test, mucosal bleeding, and DIC [ 15 – 17 ].
Within the first 7 days of illness, diagnosis is made by RT PCR or NS1 antigen testing. IgM antibodies can be detected 4–7 days after onset of symptoms but can cross-react with other flaviviruses including Zika, West Nile, Yellow Fever, and Japanese Encephalitis [ 17 ]. Other laboratory findings include hemoconcentration, thrombocytopenia, leukopenia, and elevated liver enzymes [ 15 , 16 ].
The treatment of dengue, including severe dengue, consists of supportive care, particularly fluid resuscitation, fever control, and management of bleeding. It is important to note that NSAIDS should not be used in the treatment of fever due to the increased risk of bleeding. Platelet transfusions are recommended for platelet counts < 10,000 in the setting of active bleeding. Prophylactic transfusions are not recommended [ 18 ].
Anyone developing warning signs of severe dengue including severe abdominal pain, persistent vomiting, hematemesis, mucosal bleeding, respiratory distress, restlessness, or severe fatigue within the critical phase should be admitted and watched closely [ 15 ]. Admission should also be considered in the settings of pregnancy, extremities of age, or significant comorbidities. Still, most cases of dengue can be managed in the outpatient setting. Patients should be educated on symptoms of severe dengue and told to return due to the risk of rapid progression [ 15 ].
Leptospirosis
Leptospirosis is an aerobic spirochete transmitted by contact with infected animal urine through abrasions, mucous membranes, or ingestion of contaminated food or water. Those affected typically have a history of freshwater exposure such as wading through flood waters or participating in water sports. In the USA, only 100–150 cases are identified each year, of which 50% are in Puerto Rico [ 19 ]. Cases have also been identified in Hawaii, the Pacific Coast, and the South. Internationally, leptospirosis can be acquired in most tropical regions with the highest risk in Southeast Asia [ 20 ].
Leptospirosis should be considered in patients with rapid onset fevers, myalgias, and headache with recent freshwater exposure or return from Southeast Asia. Incubation period is generally 5 to 14 days following exposure [ 21 ].
Leptospirosis consists of two phases [ 20 ]:
- May occur in 15–80% of cases and is highly specific [ 22 – 24 ]
- Other symptoms: Vomiting, diarrhea, hepatosplenomegaly, lymphadenopathy, pharyngitis, rash
- Pulmonary hemorrhage, ARDS, uveitis, optic neuritis, myocarditis, rhabdomyolysis, and Weil’s disease (jaundice and nonoliguric renal failure)
Diagnosis can be made from blood culture during phase one and urine culture during phase two [ 19 , 25 ]. Additional pathogen-specific testing is hospital dependent. Routine lab findings are nonspecific but can include thrombocytopenia, hypokalemia, hyponatremia, elevated amylase, transaminitis, and hyperbilirubinemia [ 20 , 21 ]. An elevated creatinine kinase can be useful in distinguishing leptospirosis from other diseases as it is elevated in up to 50% of patients [ 56 ]. CSF can show lymphocytic or neutrophilic pleocytosis, mildly elevated protein, and normal glucose. CSF culture is generally positive in the first 10 days of illness [ 20 ]. Chest x-ray should also be obtained for any respiratory symptoms due to risk of pulmonary hemorrhage and ARDS [ 20 ].
Most cases of leptospirosis are mild and can be managed outpatient with doxycycline (100 mg) or azithromycin (500 mg) [ 19 , 25 ]. Patients with pulmonary involvement, CNS infection, jaundice, renal failure, or age over 60 are at highest risk of death [ 25 , 26 ] and should be admitted and given IV doxycycline (100 mg), penicillin (1.5 million IUs), or a third-generation cephalosporin [ 19 , 25 ]. Until Rickettsia is ruled out, doxycycline is generally recommended as the initial treatment. In patients with severe disease, corticosteroids can be considered, but recent studies have conflicting data on their benefit [ 27 , 28 ].
Enteric (Typhoid) Fever
Enteric fever is a broader term encompassing both typhoid fever caused by Salmonella enterica serotype Typhi and Paratyphoid fever caused by Salmonella enterica serotypes Paratyphi A, B, or C. While S. typhi is more common, S. paratyphi is becoming more prevalent particularly in South Asia and is not covered by the typhoid vaccines. Enteric fever is contracted through ingestion of contaminated food or water, and the highest risk is from visits to areas of poor sanitation. The CDC estimates 400 cases per year in the USA with over 70% of cases occurring in travelers returning from India, Bangladesh, or Pakistan [ 29 •].
Enteric fever classically occurs in three stages:
- Week 1: Fever, chills, bacteremia
- Week 2: “Rose spots” and abdominal pain develop
- In those hospitalized with enteric fever, incidence of perforation can be as high as 10% [ 30 , 31 ].
Enteric fever should be considered in patients who have traveled to an endemic area within the preceding 3 weeks and who are presenting with gastrointestinal symptoms accompanied by 3 or more days of fever. While most patients will complain of abdominal pain, diarrhea is not always seen, and patients can instead present with constipation. Other common symptoms include headache, cough, arthralgias, and myalgias [ 32 ].
If enteric fever is suspected, workup should include complete blood count with differential, complete metabolic profile; coagulation screen; EKG; blood cultures; and stool culture. Findings that can help point to enteric fever include anemia, leukopenia with left shift (adults) or leukocytosis (children), elevated LFTs, high fever (> 40 °C), and bradycardia [ 32 ].
Definitive diagnosis is made by blood culture, but this test has low sensitivity and will not provide a diagnosis in the ED. Therefore, patients with suspected enteric fever should be treated empirically based on clinical suspicion [ 57 ].
- Second line: Fluoroquinolone if acquired in a region with low resistance
- Patients with altered mentation or signs of shock should also be given dexamethasone 3 mg/kg as this has been shown to dramatically reduce mortality [ 33 , 34 ].
- Ongoing outbreak of multidrug-resistant strain of S. typhi since 2016 [ 35 ]
Traveler’s Diarrhea
Traveler’s diarrhea is the most common illness seen in individuals traveling from developed to resource-limited regions [ 36 ], occurring in up to 40% of travelers [ 37 , 38 •]. Transmission is fecal-oral, most often by food and water in regions with suboptimal sanitation and hygienic practices [ 39 ]. The highest risk regions include South and Southeast Asia, Africa (excluding South Africa), South America, Central America, and Mexico. Food from street vendors and staying in “all-inclusive” lodgings are specific risk factors for developing the illness [ 40 ].
Most episodes occur between 4 and 14 days after arrival to a resource-limited region [ 41 ]. Acute illness is most frequently caused by bacteria but can also be caused by parasites or viruses. Worldwide, the most common cause is enterotoxigenic Escherichia coli (ETEC), followed by Salmonella , Campylobacter jejuni , and Shigella [ 39 ]. Practitioners should consider geographic variation, as Campylobacter species are more common than ETEC in Southeast Asia [ 42 ].
Classic traveler’s diarrhea is defined as three or more unformed stools in 24 h plus at least one of the following: nausea, vomiting, abdominal pain, fever, or blood in stool. Symptoms are variable and partially dependent on the causative agent [ 39 ].
ETEC classically consists of malaise, anorexia, abdominal cramps followed by sudden onset watery diarrhea with very frequent stools, typically without blood or purulence. Patients may have a fever, nausea, or vomiting. Campylobacter or Shigella cause inflammatory diarrhea, which can present with similar symptoms but may progress to fever, tenesmus, or bloody diarrhea [ 39 ].
Testing should include a basic metabolic panel to assess for dehydration or metabolic derangement. The determination of microbiologic agent is typically unnecessary as ETEC cannot be distinguished from nonpathogenic E. coli on routine stool cultures [ 43 ] . Whether or not to pursue further testing should be based on clinical judgment and will likely include a shared decision-making conversation with the patient. Stool testing in the ED is reasonable when patients present with severe diarrhea, bloody or mucoid stools, antibiotics in preceding 8–12 weeks, systemic illness, or symptom lasting longer than 10–14 days. Recommended tests include:
- Stool culture to evaluate for Campylobacter or Shigella .
- Hospital dependent tests for ETEC or Shiga toxin.
- Stool O&P for Giardia lamblia , Cyclosporidium , Isospora , and other parasites.
- If recent antibiotic history, test for Clostridioides (Clostridium) difficile
- If the patient appears systemically ill, send blood cultures to evaluate for bacteremia, most commonly seen from Salmonella species (Typhi).
Consider admission for those patients with laboratory evidence of severe dehydration, acute kidney injury, need for electrolyte replacement and inability to tolerate orals, or systemic illness.
The treatment is typically symptomatic and supportive, as the vast majority of episodes is self-limited and resolves within three to 5 days. Although antibiotic stewardship is important, it is very reasonable to fill a 3-day antibiotic prescription prior to travel and start the antibiotic within 1–2 days of symptoms [ 39 , 43 ]. Management includes the following:
- Fluid replacement, by mouth or intravenously.
- Antimotility agents such as loperamide or diphenoxylate can be helpful with those with frequent diarrhea.
- Good choice if traveled to Southeast Asia (quinolone-resistant C. jejuni )
- Falling out of favor due to greater awareness of side effects
- Poorly absorbed but remain alternatives for patients in whom fluoroquinolones or azithromycin are not appropriate.
Chikungunya
Chikungunya is an arthropod-borne Alphavirus primarily transmitted by mosquito bites [ 44 ]. Interestingly, the name is derived from an African dialect meaning “stooped walk” due to the disease hallmark: debilitating joint and back pains. Chikungunya often occurs in outbreaks during the rainy season and has been seen globally in Africa, Asia, Europe, the Pacific Islands, and in the Americas [ 45 ].
Viremia occurs within a few days of infection, and the virus has a propensity to invade synovium, tenosynovium, and muscles [ 45 ]. The virus may linger in the joints for up to 2 weeks. Chronic arthritis develops in up to 60% of infected individuals [ 46 ].
Typically, symptoms start with fever and malaise lasting 3–5 days which are followed by polyarthralgias and dermatologic symptoms lasting 7–10 days [ 45 ]. However, arthralgias can persist for weeks, months, or even years. The rash is typically macular but can be patchy, diffuse, or pruritic. It often starts on the limbs and trunk and may involve the face. Arthralgias are the hallmark of chikungunya. The joint pain is typically bilateral and symmetric, affecting distal joints. The axial skeleton is involved in 34–52% of cases [ 46 , 47 ]. Severe complications (respiratory failure, myocarditis, renal failure, hemorrhage, acute hepatitis, meningoencephalitis, acute flaccid paralysis, seizures) and death can occur, more often in elderly patients with medical comorbidities [ 44 ].
Diagnosis can be made with chikungunya viral RNA RT-PCR within the first week (sensitivity 100% and specificity 98%). If RT-PCR is negative or if the patient has had symptoms for 8 or more days, diagnosis is made by virus serology via ELISA or IFA. If testing for chikungunya, one should test for dengue virus and Zika virus as well [ 58 ]. Given the severe arthralgias associated with chikungunya, it may be prudent to rule out septic arthritis if significant effusion or asymmetry is present. Joint fluid analysis will be consistent with inflammatory arthritis [ 47 ].
Indications for admission include significant comorbidities or inability to ambulate. Treatment is primarily supportive with rest, fluids, and acetaminophen [ 59 ]. NSAIDs should not be used until dengue has been excluded [ 45 ].
Zika virus is an arthropod-borne flavivirus transmitted by mosquitoes. Transmission can also occur via the maternal-fetal route, sexual intercourse (vaginal, anal, oral), or direct exposure to blood [ 48 ]. Outbreaks have occurred in Africa, Southeast Asia, the Pacific Islands, the Americas, and the Caribbean, most notably during the 2016 Olympic Games in Brazil [ 49 , 50 ].
Approximately 20–25% of infected individuals have symptoms of infection, which are typically mild and last 2 to 7 days [ 51 ]. These include fever, pruritic rash, arthralgias, conjunctivitis, myalgias, headache, dysesthesia, and generalized weakness. Less commonly symptoms include abdominal pain, nausea, diarrhea, or mucous membrane ulcerations [ 52 ]. Zika has been implicated in serious neurologic complications such as congenital microcephaly, Guillain-Barré syndrome, myelitis, and meningoencephalitis [ 53 ].
Zika can be diagnosed by PCR and serology testing. However, cross-reactivity with other flaviviruses is common, and testing is generally not recommended from the ED [ 54 ]. If labs are sent, CBC may show thrombocytopenia. Treatment is supportive with fluids and acetaminophen. Generally, patients will be discharged, and we recommend education surrounding transmission and pregnancy prevention. If the patient is suffering from a severe neurologic complication, we recommend brain/spine imaging, lumbar puncture, and admission.
Conclusions
The differential diagnosis in a febrile international traveler is broad, and in many cases, definitive diagnosis will not be made in the ED. In addition, while the CDC and WHO have useful guidelines for diagnosis and management, these tests and treatment might not be available in the emergency department. Therefore, one must be aware of alternative treatments particularly for severely ill patients. In an otherwise undifferentiated febrile traveler, basic labs can be drawn to narrow the differential and screen for risk of development of severe disease. Recognition of development of severe disease is critical as these patients have high risk of complications and death.
Compliance with Ethical Standards
The authors declare that they have no conflict of interest.
This article does not contain any studies with human or animal subjects performed by any of the authors.
This article is part of the Topical Collection on Infectious Disease
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Laura Throckmorton, Email: moc.liamg@22kcorhTL .
Jonathan Hancher, Email: moc.liamg@rehcnahnahtanoj .
Papers of particular interest, published recently, have been highlighted as: • Of importance
Malaria and Travelers for U.S. Residents
Quick links.
- Prophylaxis Guidelines for Malaria in “Off-the-Radar” Areas
- Travel to West Africa? Don’t Neglect Malaria Prevention
- Mosquito Repellent Fact Sheet
- Prescribing Information for Malaria Prevention Drugs
- Yellow Book Malaria Section New!
- Blog: CDC Malaria Hotline—When the Caller is Ill Abroad
This information is intended for travelers who reside in the United States. Travelers from other countries may find this information helpful; however, because malaria prevention recommendations and the availability of antimalarial drugs vary, travelers from other countries should consult health care providers in their respective countries. For more health recommendations for international travel, visit the CDC Yellow Book .
Every year, millions of US residents travel to countries where malaria is present. About 2,000 cases of malaria are diagnosed in the United States annually, mostly in returned travelers.
Travelers to sub-Saharan Africa have the greatest risk of both getting malaria and dying from their infection. However, all travelers to countries where malaria is present may be at risk for infection.

Obtain a detailed itinerary including all possible destinations that may be encountered during the trip and check to see if malaria transmission occurs in these locations. The Malaria Information by Country Table provides detailed information about the specific parts of countries where malaria transmission does or does not occur. It also provides additional information including the species of malaria that occur there, the presence of drug resistance, and the specific medicines that CDC recommends for use for malaria prevention in each country where malaria transmission occurs on CDC’s Malaria maps.
Prevention of malaria involves a balance between ensuring that all people who will be at risk of infection use the appropriate prevention measures, while preventing adverse effects of those interventions among people using them unnecessarily. An individual risk assessment should be conducted for every traveler, taking into account not only the destination country, but also the detailed itinerary, including specific cities, types of accommodation, season, and style of travel. In addition, conditions such as pregnancy or the presence of antimalarial drug resistance at the destination may modify the risk assessment.
More on: Malaria Risk Assessment for Travelers
Based on the risk assessment, specific malaria prevention interventions should be used by the traveler. Often this includes avoiding mosquito bites through the use of repellents or insecticide treated bed nets, and specific medicines to prevent malaria.
More on: Preventing Mosquito Bites While Traveling
If malaria prevention medicines will be needed for the traveler, the Malaria Information by Country Table lists the CDC-recommended options. For many destinations, there are multiple options available. Factors to consider are the patient’s other medical conditions, medications being taken (to assess potential drug-drug interactions), the cost of the medicines, and the potential side effects.
More on: Tips on Choosing the Right Drug for an Individual Traveler
The Drugs for Malaria Prevention table provides prescription dosing information for both adults and children.
In some countries (including those with malaria risk), drugs may be sold that are counterfeit (“fake”) or substandard (not made according to United States standards). Such drugs may not be effective. Antimalarial drugs should always be purchased before traveling overseas!
For details and specific warnings, see Counterfeit and Substandard Antimalarial Drugs

This picture shows some things that travelers can use to protect themselves against malaria: malaria pills; insect repellent; long-sleeved clothing; bednet; and flying insect spray. (Not shown, but also protective: air conditioned or screened quarters.)
The interventions used to prevent malaria can be very effective when used properly, but none of them are 100% effective.
Malaria is always a serious disease and may be a deadly illness. Travelers who become ill with a fever or flu-like illness either while traveling in a malaria-risk area or after returning home (for up to 1 year) should seek immediate medical attention and should tell the physician their travel history.
Travelers who are assessed at being at high risk of developing malaria while traveling should consider carrying a full treatment course of malaria medicines with them. Providing this reliable supply of medicine (formerly referred to as standby or emergency self-treatment) will ensure that travelers have immediate access to an appropriate and high quality medicine if they are diagnosed with malaria while abroad. Depending on the medicine they are using for prevention, this could either be atovaquone/proguanil or artemether/lumefantrine.
More on: Malaria Treatment (United States)
Travelers are often surprised to learn that even if they adhered to all of the prevention advice and did not become sick with malaria, recent travel to a place where malaria transmission occurs is an exclusion criterion for blood donation.
More on: Prevention of Blood Transfusion-Associated Malaria
To receive email updates about this page, enter your email address:
New! Locally Acquired Cases of Malaria in Florida, Texas, Maryland, and Arkansas
New! Update to Guidance for use of Artemether-Lumefantrine (Coartem®) in Pregnancy for Uncomplicated Malaria New! Discontinuation of CDC’s Distribution of Intravenous Artesunate as Commercial Drug Guidance for Malaria Diagnosis in Patients Suspected of Ebola Infection in the United States -->
See all Malaria Notices
- New! Malaria is a Serious Disease
- New! La malaria (paludismo) es una enfermedad grave
- How to Report a Case of Malaria
- CDC Yellow Book
- Red Pages: Malaria-endemic areas by country
- Drugs for Prevention
- Choosing a Drug to Prevent Malaria
- Drugs for Treatment in the U.S.
- Frequently Asked Questions (FAQs)
- Blood Banks
Click here for contact information
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

Travel and Heart Disease

Travel precautions help people with heart disease
Traveling to a faraway place doesn’t need to be off limits because you have heart disease or are a caretaker of someone who has had a cardiac event like heart attack or stroke . A few simple precautions can help make your trip smooth.
Here are some travel tips:
- Keep medicines in their original, labeled containers. Ensure that they are clearly labeled with your full name, health care professional’s name, generic and brand name and exact dosage.
- Bring copies of all written prescriptions. Leave a copy of your prescriptions at home with a friend or relative in case you lose your copy or need an emergency refill. Download this medication chart (PDF) to keep track of your medicines.
- Ask your health care professional for a note if you use controlled substances, or injectable medicines, such as EpiPens and insulin. Tell your health care professional about your travel. Let your cardiologist or internist know where you’ll be. Your health care professional might know medical professionals or reputable heart institutes in the area you’re visiting if help is needed.
- Comprehensive travel insurance usually includes medical evacuation travel insurance. Coverage varies by plan, destination and duration of trip, so shop around. But the average cost is about $200, which is a small investment if it can cover tens of thousands dollars of potential medical expenses.
- Some health care professionals recommend taking a copy of your pertinent medical records with you while traveling.
High altitudes, exotic spots
Oxygen availability declines at higher altitudes, which can place unique stressors on the cardiovascular system. As such, patients who are at risk of or who have established cardiovascular disease may be at an increased risk of adverse events when staying at mountainous locations. However, these risks may be minimized by appropriate pretravel assessments and planning through shared decision‐making between patients and their managing health care professionals.
Talk to your health care team before your trip to understand what you should do to prepare. You may wish to gradually move up the mountain and acclimate at lower elevations before moving to the higher altitudes. People with coronary artery disease and angina should anticipate that reduced oxygen levels may increase angina. Your heart has to work harder, especially if you already have blockage. Watch out for shortness of breath or other symptoms that could indicate you’re tipping from a stable to an unstable state.
Be mindful of your fluid consumption and sodium (salt) intake if you have cardiomyopathy or a history of heart failure . A balanced fluid intake is important in these conditions.
If you’re traveling to a country where certain vaccines are needed to guard against disease, it’s not likely the immunization will affect your heart. The bigger concern may be consistent access to quality medical care.
Consider selecting destinations in parts of the world that both interest you and have many options for health care you may need while you are visiting.
Long distance precautions
Sitting immobile on long plane flights or car, train or bus rides can slightly increase a normal person’s risk of blood clots in the legs, but associated medical issues usually contribute to it. If someone has peripheral artery disease (PAD) or a history of heart failure, the clot risk increases. Recent surgery, older age and catheters in a large vein may also increase your risk of blood clots. Getting up and walking around when possible is recommended for long flights, just be sure the seatbelt light is not on when you do so. Stopping to take a quick break during long car rides may help as well.
Tell your health care professional about your travel plans to get the best advice on what precautions, if any, you may need to take. For example, some people might need compression stockings or additional oxygen. Others might need to watch fluids closely or avoid alcohol. And some may not be able to fly.
See our editorial policies and staff .
Last Reviewed: Jan 16, 2024

Travel Related Diseases & Prevention
It is important to prepare for the risks of travel related illnesses which may arise on your journey. Chat with Elle to learn what diseases may be prevalent at your destination and to receive tips on prevention.
Travel Vaccines
Cholera is a disease caused as a result of the bacteria Vibrio cholerae. It thrives in areas with poor sanitation and lack of access to safe drinking water. Any consumption of food or drink contaminated by the cholera bacteria can lead to the contraction of the disease. In a few cases, cholera can lead to death if the victim is dehydrated due to loss of fluids and electrolytes. Most international travelers do not get cholera because they do not visit areas with active cholera transmission and usually have good access to safe food and water. Cholera is found in countries around the world but is extremely rare in the United States and other industrialized nations.
Prevention:
A licensed cholera vaccine is available in the United States for adults 18-64 years old. It prevents severe diarrhea caused by the most common types of cholera-causing bacteria and should be administered at least 10 days prior to any potential cholera exposure. The vaccine is not 100% effective. In addition to vaccination, travelers should take steps to reduce their risk by:
- Only eat foods that are cooked and served hot
- Avoid food that has been sitting on a buffet
- Eat raw fruits and vegetables only if you have washed them in clean water or peeled them
- Only drink beverages from factory-sealed containers
- Avoid ice because it may have been made from unclean water
- Drink pasteurized milk
- Wash hands often with soap and water for 20 seconds, especially after using the bathroom and before eating
- If soap and water aren’t available, use an alcohol-based hand sanitizer that contains at least 60% alcohol
- Keep your hands away from your face and mouth
Centers for Disease Control and Prevention. Cholera Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/cholera.html . Reviewed October 30 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Cholera. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/cholera . Reviewed December 1 2020. Accessed April 20 2021.
Hepatitis A
Hepatitis A is a virus that often results in liver disease. Hepatitis A virus is found in the stool and the blood of infected individuals. It is a highly communicable disease. Symptoms appear quickly and could include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, diarrhea, clay-colored bowel movements, joint pain and jaundice (yellowing of the skin and eyes). You could be infected with hepatitis A if you engage in any of the following:
- Consumption of food or drink contaminated with hepatitis A
- Contact with objects contaminated by the virus followed by direct contact to mouth
- Direct and personal contact with infected individuals
- Sexual intercourse with infected individuals
Hepatitis A is a common disease in countries throughout the world. Anyone who has not been vaccinated or had hepatitis A infection before can get infected. Travelers are more likely to get infected with hepatitis A if they visit rural areas, trek in backcountry areas, or frequently eat or drink in settings of poor sanitation. However, even travelers who stay in urban areas, resorts, or luxury hotels, who wash their hands regularly, and who choose food and drinks carefully have been infected when visiting countries where hepatitis A is common.
The best way to prevent exposure and infection of the virus is to get vaccinated. The vaccine for hepatitis A is extremely effective and has been a routine childhood vaccine since 1996. It is recommended for travelers above the age of 6 months to countries where hepatitis A is prevalent. It is administered in 2 or 3 doses; with a minimum of 1 as soon as possible before you travel. Travelers allergic to a component or are below 6 months of age should be administered a single dosage of immune globulin which provides sufficient protection for up to 2 months depending on the dosage.
Centers for Disease Control and Prevention. Hepatitis A Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/hep-a.html . Reviewed July 28 2020. Accessed April 20 2021.
Centers for Disease Control and Prevention. Hepatitis A. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/hepatitis-a . Reviewed April 27 2020. Accessed April 20 2021.
Hepatitis B
Hepatitis B is a virus that causes liver disease. Hepatitis B virus is found in the blood and body fluids of infected people. People infected with hepatitis B can spread it to others. Early symptoms of hepatitis B can include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, clay-colored bowel movements, joint pain, and jaundice (yellow color in the skin or the eyes). Some infected individuals develop lifelong hepatitis B. The long-term health effects caused by chronic hepatitis B infection can cause people to die early from liver disease and liver cancer. You can be infected with hepatitis B virus if you:
- Have sexual intercourse with an infected partner
- Use of needles, syringes, or drug preparation equipment that are shared with an infected person
- Sharing of personal care items such as razors, toothbrushes, or medical equipment with an infected individual
- Acquire a wound with a sharp instrument or have a needlestick injury in a health care setting
- Direct contact the blood or open sores of an infected individual
Hepatitis B occurs in nearly every part of the world but is more common in some countries in Asia, Africa, South America and the Caribbean. This map shows the worldwide prevalence of hepatitis B virus infection . Although the risk to most travelers is low, medical tourists (people who travel for medical purposes) or people who need emergency medical care while traveling may be more likely to get infected.
Getting vaccinated is the best way to protect against hepatitis B. Hepatitis B is a routine vaccination that most people undergo during infancy in the US at birth. The vaccine has proved to be 90% effective at preventing contraction and has been recommended for infants since 1991. The vaccine is recommended for travelers of all ages with plans to travel to countries where hepatitis B is common.
Centers for Disease Control and Prevention. Hepatitis B – Chapter 4 – 2020 Yellow Book. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/hepatitis-b#5514 . Reviewed July 1 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Medical Tourism – Chapter 9 – 2020 Yellow Book. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-for-work-other-reasons/medical-tourism . Reviewed June 24 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Hepatitis B Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/hep-b.html . Reviewed April 5 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Hepatitis B. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/hepatitis-b . Reviewed April 28 2020. Accessed April 20 2021.
Japanese Encephalitis
Japanese encephalitis (JE) is a sickness spread through mosquito bites. Its symptoms usually take around 5-15 days to develop and could include fever, headache, vomiting, confusion, and difficulty moving. Symptoms that develop later include swelling around the brain and coma. JE is a serious disease that could be fatal. Travelers who go to Asia are at risk for getting Japanese encephalitis ( See map ). For most travelers the risk is extremely low but depends on where you are going, the time of year, your planned activities, and the length of the trip. You are at higher risk if you are traveling to rural areas, will be outside frequently, or will be traveling for a long period of time. In mild climates in northern Asia the risk for JE is greater in the summer and fall. In tropical and subtropical areas, there is a risk year-round.
In addition to bug bite prevention , travelers may choose to get vaccinated against JE. There is one JE vaccine available in the US. It is approved for use in individuals older than 2 months of age. The JE vaccine is administered in two doses, spaced 28 days apart. Individuals 18 to 65 years of age can shorten this buffer period to seven days and all must finish the last dose at least a week before travel. A third dose should ideally be taken if the person has taken the 2-dose primary vaccine a year or more as they risk re-exposure.
Centers for Disease Control and Prevention. Geographic Distribution of Japanese Encephalitis Virus. Centers for Disease Control and Prevention. https://www.cdc.gov/japaneseencephalitis/maps/index.html . Reviewed February 8 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Avoid Bug Bites. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/page/avoid-bug-bites . Reviewed January 3 2020. Accessed April 20 2021.
Centers for Disease Control and Prevention. Japanese Encephalitis Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/je-ixiaro.html . Reviewed August 15 2019. Accessed April 20 2021.
Malaria results from a parasite that is spread by mosquitoes. Symptoms appear between 7 to 3 days but in a few cases can take up to a year to display fully. These could include high fevers, chills and flu. If not treated, Malaria can result in severe illness or even death. The mosquitoes that spread malaria are found in Africa, Central and South America, parts of the Caribbean, Asia, Eastern Europe, and the South Pacific (See maps: Eastern Hemisphere and Western Hemisphere ). Travelers going to these countries may get bit by mosquitoes and get infected. About 2,000 cases of malaria are diagnosed in the United States annually, mostly among returned travelers.
There is no vaccine for malaria. Travelers can safeguard themselves by preventing mosquito bites and taking medication to protect against malaria. There are six different malaria medications available. The one that’s right for you depends on your trip and other factors. Depending on the medicine, individuals will have to start taking it several days before the trip as well as during and after. Consultation with a doctor is a must. If bitten by mosquitoes, avoid itching the bites and apply hydrocortisone cream to reduce irritation.
Centers for Disease Control and Prevention. Malaria – Chapter 4 – 2020 Yellow Book. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/malaria#5544 . Reviewed July 1 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Choosing a Drug to Prevent Malaria. Centers for Disease Control and Prevention. https://www.cdc.gov/malaria/travelers/drugs.html . Reviewed November 15 2018. Accessed April 20 2021.
Centers for Disease Control and Prevention. Malaria. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/malaria . Reviewed May 4 2020. Accessed April 20 2021.
Meningococcal Disease (Meningitis)
Meningococcal disease is a result of bacteria called Neisseria meningitidis. This disease is communicable through direct personal contact like kissing, sharing living spaces etc. Individuals with this disease require immediate medical attention and symptoms vary depending on the type of illness. Some common symptoms of meningococcal meningitis include headaches, sudden fever and a stiff neck as well as nausea, vomiting, confusion and heightened sensitivity to light. Symptoms may present differently in children and infants. The bacteria that cause this disease may also infect the blood and cause septicemia. The symptoms of this include chills, fatigue, vomiting, severe aches and pains, diarrhea, dark rash, and rushed breathing. This disease can also lead to death in a few cases in as little as a few hours. Anyone can get meningococcal disease, but people who live or travel to certain areas of the world are more likely to get it. The “meningitis belt” of sub-Saharan Africa has the highest rates of meningococcal disease in the world. The disease is more common in this part of Africa during the dry season (December through June). Travelers who spend a lot of time with local populations in the meningitis belt, especially during outbreaks of meningococcal disease, are more likely to get this disease. Participants in the Hajj or Umrah pilgrimages in Saudi Arabia are also more likely to get sick.
A vaccine is the best way to protect yourself from the meningococcal disease. There are two types of meningococcal vaccines available in the United States:
- Meningococcal ACWY (MenACWY) vaccine
- Serogroup B meningococcal (MenB) vaccine
- MenACWY is a routine vaccination administered to 11–12-year-olds followed up by a booster shot at 16. MenB is administered to teens and young adults at 16-18 years old. Depending on the travel plans, younger children and adults may also need a MenACWY and those vaccinated previously might require a booster shot. It takes a buffer period of 7-10 days after vaccination to enable maximum protection against the disease. Consult with a doctor to get your personalized recommendation.
Centers for Disease Control and Prevention. Signs and Symptoms of Meningococcal Disease. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/malari https://www.cdc.gov/meningococcal/about/symptoms.html#meningitis. Reviewed June 7 2017. Accessed April 20 2021.
Centers for Disease Control and Prevention. Meningococcal Disease – Chapter 4 – 2020 Yellow Book. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/meningococcal-disease#5559. Reviewed June 24 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Meningococcal ACWY Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/mening.html . Reviewed August 15 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Meningococcal B Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/mening-serogroup.html . Reviewed August 15 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Meningococcal Disease. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/meningococcal-disease . Reviewed May 1 2020. Accessed April 20 2021.
Rabies is a fatal disease caused by a virus that spreads through the saliva of infected animals. All mammals are susceptible to rabies. People typically get rabies from licks, bites, or scratches from infected dogs and other animals such as bats, foxes, raccoons, and mongooses. Rabies impacts the central nervous system, ultimately resulting in brain disease and death. Once symptoms of rabies make themselves known, the disease is nearly always fatal, making prevention paramount. Rabid dogs are a problem in many countries around the world, including most of Africa, Asia, and parts of Central and South America. Although any mammal can transmit rabies, dog bites are how most travelers get rabies. Factors that may increase a traveler’s chances of rabies infection include:
- Camping or exploring caves (spelunkers)
- Working with animals (veterinarians, animal handlers, field biologists, or laboratory workers handling animal specimens)
- Long-term travelers and expatriates
- Children are more likely to get infected because they often play with animals and may not report bites.
Rabies in dogs is rare in the United States, Australia, Canada, Japan, and most European countries.
In addition to practicing good animal safety , some travelers should get vaccinated against rabies. Rabies vaccine is administered to people at high risk of rabies to protect them should they be exposed. People at high risk of exposure to rabies should be offered a pre-exposure rabies vaccination. For pre-exposure protection, 3 doses of rabies vaccine are recommended. People who may be repeatedly susceptible to rabies virus should receive periodic testing for immunity, and booster doses may be necessary. Rabies vaccine can prevent rabies if given to a person after they have had an exposure, before symptoms appear. Anyone who has been bitten by an animal suspected to have rabies or has been exposed to it should clean the wound and visit a medical professional immediately regardless of vaccination status.
Centers for Disease Control and Prevention. Be Safe Around Animals. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/page/be-safe-around-animals . Reviewed October 31 2017. Accessed April 20 2021.
Centers for Disease Control and Prevention. Rabies Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/rabies.html . Reviewed January 8 2020. Accessed April 20 2021.
Centers for Disease Control and Prevention. Rabies. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/rabies . Reviewed January 28 2021. Accessed April 20 2021.
Tickborne Encephalitis
Tickborne encephalitis is a viral disease that affects the central nervous system. The virus is found across many parts of Europe and Asia and typically spreads to humans either through the bite of an infected tick or through consumption of unpasteurized dairy products from infected livestock (goats, sheep, or cows). The disease is not known to spread from person to person, except for an infected pregnant mother passing it to her fetus. Tickborne encephalitis infection is most common from April through November, when ticks are most active. Travelers whose plans include camping, hiking, and hunting are more likely to be exposed to the virus. Although most people who get infected with tickborne encephalitis do not get sick, symptoms can be serious and sometimes deadly. Possible symptoms include:
- Loss of appetite
- Nausea/vomiting
- Swelling of brain and/or spinal cord
- Confusion or sensory disturbances
Currently, the best way to protect against tickborne encephalitis is to prevent tick bites and avoid unpasteurized dairy products. Ticks are found in grassy, brushy, wooded areas, or on animals. Spending time in these kinds of areas can bring you in contact with ticks. If you do plan on being in areas where ticks are active, you can reduce the risk of being bitten by doing the following:
- Avoiding walking directly through tall grass and brush
- Use an EPA-registered insect repellent
- Treat clothing and gear with permethrin
- Check clothing and gear (and pets!) for ticks when returning indoors
- Shower right after being outdoors
Centers for Disease Control and Prevention. Tickborne Encephalitis. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/tickborne-encephalitis . Reviewed August 20 2021. Accessed January 25 2022.
Centers for Disease Control and Prevention. Tick-borne Encephalitis (TBE). Centers for Disease Control and Prevention. https://www.cdc.gov/vhf/tbe/index.html . Reviewed March 31 2014. Accessed January 25 2022.
Typhoid Fever
Typhoid fever and paratyphoid fever are similar diseases caused by the bacteria Salmonella Typhi. Salmonella Paratyphi bacteria cause paratyphoid fever. It is a communicable disease. It can be contracted when an infected person uses the bathroom and does not wash their hands. The bacteria can remain on their hands and subsequently contaminate everything that the person touches, including any food and drinks. In countries with poor sanitation, the water used to rinse and prepare food and beverages can also be contaminated with these bacteria. Travelers who consume foods or drinks contaminated with these bacteria are susceptible to the disease. Typhoid fever and paratyphoid fever cause similar symptoms. People with these diseases usually have a fever that may go as high as 103–104°F (39–40°C). They also may exhibit weakness, stomach pain, headache, diarrhea or constipation, cough, and loss of appetite. Some people have a rash of flat, rose-colored spots. Internal bleeding and death may occur but are rare.
Two typhoid vaccines are available in the US currently:
- Pill vaccine. People 6 years+ can take the pill vaccine. All four pills (1 pill every other day) must be taken at least a week before travel.
- Shot vaccine. People 2 years+ can receive the shot vaccine. One shot (or a booster shot) must be taken at least 2 weeks before travel.
Unfortunately, neither the typhoid pills nor shot can offer complete protection against infection (50%-80%) and both lose effectiveness over time. Also, there isn’t a vaccine that prevents paratyphoid fever. For these reasons, it is very important that you also take the following steps to prevent typhoid:
Choose food and drinks carefully
- Avoid food that has been sitting open on a buffet
- Eat raw fruits and vegetables only if they have been washed in clean water or peeled
- Only consume beverages from factory-sealed containers
- Avoid ice as it may have been made from unclean water
- Only consume pasteurized milk
Wash your hands
- Wash hands frequently with soap and water for 20 seconds, especially after using the bathroom and before eating
- If soap and water aren’t available, use an alcohol-based hand sanitizer that contains a minimum of 60% alcohol
Centers for Disease Control and Prevention. Typhoid Fever. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/typhoid . Reviewed December 1 2020. Accessed April 20 2021.
Yellow Fever
Yellow fever is a disease caused by a type of virus that is spread through mosquito bites. Symptoms take about 3–6 days to develop and include fever, chills, headache, backache, and muscle aches. Around 15% of people who contract yellow fever develop serious illnesses that could lead to bleeding, shock, organ failure, and sometimes even death. Travelers to certain parts of South America and Africa are at risk for yellow fever.
In addition to avoiding mosquito bites , travelers may be required or recommended the yellow fever vaccine . Yellow fever vaccine is a live vaccine containing a weakened, live yellow fever virus. It is administered as a single shot. A single dose provides lifelong protection for most people. Yellow fever vaccine is provided only at designated vaccination centers. After receiving the vaccine, you will be given an “International Certificate of Vaccination or Prophylaxis” (ICVP, also called the “yellow card”). You will need this card as proof of vaccination to be able to enter certain countries. If you don’t have it, you might be required to get yellow fever vaccine upon entering the country or be forced to wait for up to 6 days to ensure that you are not infected. Do not donate blood for 14 days after vaccination as there stands a risk of passing vaccine virus to others during that period.].
Centers for Disease Control and Prevention. Symptoms, Diagnosis, & Treatment. Centers for Disease Control and Prevention. https://www.cdc.gov/yellowfever/symptoms/index.html . Reviewed January 15 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Yellow Fever – Chapter 4 – 2020 Yellow Book. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/yellow-fever#4739. Reviewed April 9 2021. Accessed April 20 2021.
Centers for Disease Control and Prevention. Yellow Fever Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/yf.html . Reviewed April 1 2020. Accessed April 20 2021.
Centers for Disease Control and Prevention. Yellow Fever. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/yellow-fever . Reviewed November 30 2020. Accessed April 20 2021.
Routine Vaccines
Chickenpox is a highly contagious disease caused by the varicella-zoster virus (VZV). It can cause an itchy, blister-like rash. The rash first appears on the chest, back, and face, and then spreads over the entire body, causing between 250 and 500 itchy blisters. Chickenpox can be serious, especially in babies, adolescents, adults, pregnant women, and people with a weakened immune system. Anyone who has not had chickenpox or gotten the chickenpox vaccine can get the disease. Chickenpox illness usually lasts about 4 to 7 days. The classic symptom of chickenpox is a rash that turns into itchy, fluid-filled blisters that eventually turn into scabs. The rash may first show up on the chest, back, and face, and then spread over the entire body. It usually takes about one week for all of the blisters to become scabs. Other typical symptoms that may begin to appear 1-2 days before rash include:
The best way to prevent chickenpox is to get the chickenpox vaccine . Everyone – including children, adolescents, and adults – should get two doses of chickenpox vaccine if they have never had chickenpox or were never vaccinated. Children are routinely recommended to receive the first dose at age 12 through 15 months and the second dose at age 4 through 6 years. Chickenpox vaccine is very safe and effective at preventing the disease. Most people who get the vaccine will not get chickenpox. If a vaccinated person does get chickenpox, the symptoms are usually milder with fewer or no blisters (they may have just red spots) and mild or no fever. The chickenpox vaccine prevents almost all cases of severe illness. Since the varicella vaccination program began in the United States, there has been over 90% decrease in chickenpox cases, hospitalizations, and deaths.
Centers for Disease Control and Prevention. Chickenpox Vaccination: What Everyone Should Know. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/vpd/varicella/public/index.html#:~:text=CDC%20recommends%20two%20doses%20of,age%204%20through%206%20years . Reviewed August 7 2019. Accessed May 10 2021.
Influenza (Flu)
Flu is a contagious respiratory disease caused as a result of influenza viruses that create infections in the nose, throat, and sometimes the lungs. It can bring about mild to severe illnesses, and in a few cases could cause death. The best way to avoid the flu is by getting a flu vaccine annually. The risk for exposure to influenza during travel depends somewhat on the time of year and destination.
- In the Northern Hemisphere, the flu season can begin as early as October and can last as late as April or May.
- In the temperate regions of the Southern Hemisphere, influenza activity typically occurs during April – September.
- In the tropics, influenza activity occurs throughout the year.
- Travelers in the Northern and Southern Hemispheres can be exposed to influenza during months that fall outside of those listed above, especially when traveling as part of large tourist groups (e.g., on cruise ships) that include people from areas of the world where influenza viruses are circulating.
The CDC recommends that everyone 6 months and older get a flu vaccine yearly. There are several flu viruses that constantly change. New flu vaccines are developed annually to protect patients against 3 or 4 viruses most likely to cause diseases in upcoming flu seasons. Even if a vaccine does not match the virus, it still provides some degree of protection. The buffer period for the vaccine’s protection to develop is about 2 weeks. There are two types of flu vaccine:
- Inactivated influenza vaccine – standard flu shot.
- Live, attenuated influenza vaccine – administered as a nasal spray to non-pregnant people between the ages of 2 and 49.
Centers for Disease Control and Prevention. Key Facts about Seasonal Flu Vaccine. Centers for Disease Control and Prevention. https://www.cdc.gov/flu/prevent/keyfacts.htm . Reviewed December 16 2020. Accessed April 20 2021.
Centers for Disease Control and Prevention. Inactivated Influenza Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/flu.html . Reviewed August 15 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Live Intranasal Influenza Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/flulive.html . Reviewed August 15 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Flu (Influenza). Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/influenza-seasonal-zoonotic-and-pandemic . Reviewed October 21 2019. Accessed April 20 2021.
Measles-Mumps-Rubella (MMR)
Measles is an illness transmitted through a highly contagious virus. It is spread through air, commonly due to coughs, sneezes or even breathing. Symptoms include fever, rash, coughs, red eyes and a runny nose. Measles can also in a few cases lead to serious lung infections like pneumonia. In more serious cases, although rare, measles can lead to swelling of the brain and can be fatal. It is severe in infants and those who have weak immune systems or are malnourished.
Mumps is an illness caused by a virus. Individuals with mumps spread the virus when they:
- Cough, sneeze, or talk
- Share items that may have saliva and other bodily fluids on them like water bottles or cups
- Engage in close-contact activities with others such as playing sports, dancing, or kissing
Symptoms may include headache, fever, fatigue, muscle ache, appetite loss and swollen glands under ears or jaw (parotitis). Mumps can be recovered from fully but can create complications such as swelling of the brain, testicles, ovaries or breasts as well as temporary or permanent deafness.
Rubella is a virus that spreads through the air via coughs or sneezes. Symptoms are mild if there at all, a red rash being the first sign. Other symptoms may include headaches, fever, red eyes, coughs, runny nose, general discomfort and swollen and enlarged lymph nodes. It is dangerous in pregnant women as the baby could be born with birth defects or mental disabilities, organ damage, heart defects, deafness and cataracts.
Getting vaccinated is the best way to safeguard yourself against measles, mumps, and rubella. The combination vaccine MMR offers protection these three diseases. MMR is a routine vaccination that children in the US receive at 12-15 months of age. The vaccine is administered in 2 doses, with the second dose given a minimum of 28 days after the first dose. If you were born in or after 1957 and have never had measles, mumps, and rubella and have never been vaccinated against these diseases, you are susceptible. You should receive 2 doses of MMR vaccine before you travel, the second dose 28 days after the first. People born before 1957 are likely to have been exposed to measles, mumps, and rubella naturally, and usually do not require MMR vaccine. Infants 6 to 11 months old traveling internationally should receive 1 dose of the MMR vaccine prior to travel. This dose does not count as the first dose in the routine childhood vaccination series.
Pregnant women should NOT receive the MMR vaccine. A pregnant woman not vaccinated against rubella should not travel to countries where rubella is prevalent or areas with known rubella outbreaks, especially during the first 20 weeks of her pregnancy. A woman not vaccinated against rubella should be vaccinated against this disease immediately after her baby is born.
Centers for Disease Control and Prevention. Measles. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/measles . Reviewed May 1 2020. Accessed April 20 2021.
Centers for Disease Control and Prevention. Mumps. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/mumps . Reviewed April 30 2020. Accessed April 20 2021.
Centers for Disease Control and Prevention. Rubella. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/rubella . Reviewed May 4 2020. Accessed April 20 2021.
Centers for Disease Control and Prevention. MMR (Measles, Mumps, & Rubella) Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/mmr.html . Reviewed August 15 2019. Accessed April 20 2021.
Pneumococcal Disease (Pneumonia)
Pneumococcal disease is a result of bacteria called Streptococcus pneumoniae (pneumococcus). This virus is communicable through coughing and sneezing. Pneumococcus bacteria can create infections in many parts of the body depending on which symptoms present. Symptoms may include fever, cough, shortness of breath, chest pain, stiff neck, confusion, increased sensitivity to light, joint pain, chills, ear pain, sleeplessness, and irritability. In more severe cases, pneumococcal disease can lead to hearing loss, brain damage, and death. Pneumococcal disease occurs around the world but is more common in low- and middle-income countries where fewer people get pneumococcal vaccine. In more temperate climates, pneumococcal disease is more common during winter and early spring. In tropical climates with dry and rainy seasons, pneumococcal disease tends to occur more in the dry season. Travelers are more likely to get pneumococcal disease if they spend time in crowded settings or in close contact with children in countries where pneumococcal vaccine is not routinely used.
Getting vaccinated is the best way to protect against pneumococcal disease. Pneumococcal vaccines are routine in the United States. There are two types of pneumococcal vaccine:
- Adults 65 years or older
- Individuals aged 2 through 64 years old with certain medical conditions
- Adults aged 19 through 64 years old who are smokers
- All children below 2 years of age
- Individuals 2 years or older with certain medical conditions
- Adults 65 years or older dependent on consultation with medical professional
Some groups may require multiple doses or booster shots. It is important to consult you or your child’s clinician about what is best for your specific situation.
Centers for Disease Control and Prevention. Pneumococcal Polysaccharide Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/ppv.html . Reviewed October 30 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Pneumococcal Conjugate (PCV13) Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/pcv13.html . Reviewed October 30 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Pneumococcal Disease (Streptococcus pneumoniae). Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/pneumococcal-disease-streptococcus-pneumoniae . Reviewed May 4 2020. Accessed April 20 2021.
Polio is a disease caused by a virus that impacts the nervous system and is mainly spread through person-to-person contact. Polio can also be spread by eating raw or undercooked food or drinking liquids contaminated with the feces of an infected person. Symptoms aren’t usually prevalent and are typically minor, such as fever, tiredness, nausea, headache, nasal congestion, sore throat, cough, stiffness in the neck and back, and pain in the arms and legs. Most individuals impacted recover completely. In rare cases, polio infection can lead to the permanent loss of muscle function (paralysis) in the arms or legs (usually the legs); it can also be fatal if there is loss of function of the muscles used for breathing or infection of the brain. Polio has been eradicated from the United States but is still prevalent in other parts of the world. Travelers going to certain parts of Africa and Asia may be at risk for polio. Everyone should be up to date with their routine polio vaccination series . In addition, a one-time adult polio vaccine booster dose is recommended for previously vaccinated travelers to certain countries.
Children should usually be administered 4 doses of polio vaccine , at 2 months, 4 months, 6–18 months, and 4–6 years of age. Most adults do not need the polio vaccine if they were already vaccinated against polio as children. Some adults are at higher risk and should consider polio vaccination, such as people traveling to certain parts of the world, laboratory workers who might handle poliovirus, and health care workers who handle active cases of polio. The polio vaccine is available as both a stand-alone vaccine and as part of a combination vaccine. Polio vaccine may be given at the same time as other vaccines. In addition to vaccination, travelers can take steps to protect themselves by:
- Follow the Food and Water Safety tips to avoid exposure to any food and drinks that could be contaminated by the feces of a person infected with polio.
- Wash your hands often.
- If soap and water aren’t available, clean hands with hand sanitizer (containing at least 60% alcohol).
- Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.
- Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.
- Try to avoid close contact with other people, such as kissing, hugging, or sharing eating utensils or cups with people who are sick.
Centers for Disease Control and Prevention. Polio Vaccination. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/vpd/polio/index.html . Reviewed May 4 2018. Accessed April 20 2021.
Centers for Disease Control and Prevention. Polio Vaccine Information Statement. Centers for Disease Control and Prevention https://www.cdc.gov/vaccines/hcp/vis/vis-statements/ipv.html . Reviewed April 5 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Food and Water Safety. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/page/food-water-safety . Reviewed February 20 2020. Accessed April 20 2021.
Centers for Disease Control and Prevention. Polio. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/poliomyelitis . Reviewed September 10 2019. Accessed April 20 2021.
Shingles is caused by varicella zoster virus (VZV), the same virus that causes chickenpox. After a person recovers from chickenpox, the virus stays dormant (inactive) in their body. The virus can reactivate later, causing shingles, a painful rash that develops on one side of the face or body. The rash consists of blisters that typically scab over in 7 to 10 days and fully clears up within 2 to 4 weeks. Most people who develop shingles have only one episode during their lifetime. However, you can have shingles more than once. If you have shingles, direct contact with the fluid from your rash blisters can spread VZV to people who have never had chickenpox or never received the chickenpox vaccine. If they get infected, they will develop chickenpox, not shingles. They could then develop shingles later in life. In rare cases (usually in people with weakened immune systems), the rash may be more widespread on the body and look similar to a chickenpox rash. Other symptoms of shingles can include:
- Upset stomach
Shingles vaccination is the only way to protect against shingles and postherpetic neuralgia (PHN), the most common complication from shingles. CDC recommends that healthy adults 50 years and older get two doses of the shingles vaccine ̣recombinant zoster vaccine, separated by 2 to 6 months, to prevent shingles and the complications from the disease. Individuals who already had shingles (or are unsure if they had chickenpox) should still get the shingles vaccine. Your doctor or pharmacist can give you the vaccine as a shot in your upper arm. It provides strong protection against shingles and PHN. A two-dose series of shingles vaccine is more than 90% effective at preventing shingles and PHN. Protection stays above 85% for at least the first four years after you get vaccinated.
Centers for Disease Control and Prevention. Complications of Shingles. Centers for Disease Control and Prevention. https://www.cdc.gov/shingles/about/complications.html . Reviewed July 1 2019. Accessed April 20 2021.
Centers for Disease Control and Prevention. Shingles (Herpes Zoster). Centers for Disease Control and Prevention. https://www.cdc.gov/shingles/index.html . Reviewed October 5 2020. Accessed April 20 2021.
Tetanus-Diphtheria-Pertussis (Tdap)
Tetanus is a disease caused by a type of bacteria called Clostridium tetani. The bacteria are typically prevalent in soil, dust, and manure. These bacteria usually enter the body through breaks in skin, often cuts or wounds. It is not a communicable disease. A prominent feature of tetanus is when the jaw muscles tighten, preventing a sick person from opening their mouth. This is sometimes referred to as “lockjaw.” Other symptoms of tetanus could include muscle spasms, painful muscle stiffness, trouble swallowing, seizure, headaches, fever, sweating, difficulty breathing, and paralysis. Patients may also exhibit changes in blood pressure and heart rate. Even with intensive care, 10%–20% of individuals with tetanus die. Most people who contract tetanus will display symptoms within 14 days of infection.
Diphtheria is an infection brought about by bacteria called Corynebacterium Diphtheriae. These bacteria cause respiratory and skin contaminations. Individuals with Diphtheria can spread the bacteria to others when they wheeze or cough, or on the off chance that others come into contact with their contaminated injuries. Side effects of respiratory diphtheria incorporate weakness, fever, sore throat, and phlegm in the throat or nose. Swelling of glands in the neck is also possible.
Pertussis, or whooping cough, is a disease caused by bacteria called Bordetella pertussis. Individuals with whooping cough can spread the bacteria to others when they cough, sneeze, or share the same confined breathing spaces. Babies can be transmitted whooping cough from older siblings, parents, or caregivers who might be unaware that they have the disease. Early symptoms are usually mild and can include a cold, runny nose, low fever, and a mild cough. Later symptoms of the illness could include “fits” of many rapid coughs followed by a high-pitched “whoop,” vomiting, and fatigue. The coughing fits can continue for up to 10 weeks or more. In babies, the coughing can be minimal. Instead, babies could experience pauses in breathing also known as apnea. Whooping cough can cause serious and sometimes fatal complications in babies and young children. About half of babies younger than one year old who get the disease require hospitalization.
Staying up to date on Tdap vaccines is the best way to protect against tetanus, diphtheria, and pertussis. These vaccines are often known as DT, DTaP, Td, and Tdap . Babies require 3 shots of DTaP to build up high levels of protection against diphtheria, tetanus, and whooping cough. Then, young children require 2 booster shots to maintain that protection throughout their early childhood. Preteens should receive one shot of Tdap between the ages of 11-12 years to boost their immunity. Pregnant women should be administered Tdap during the early part of the 3rd trimester during every pregnancy. This can help protect her baby from whooping cough in the first few months of life. All adults who have never received one should be administered a shot of Tdap. This can be given at any time, regardless of when they last got Td. This should be followed by either a Td or Tdap shot every 10 years.
The Food and Drug Administration licensed 12 combination vaccines for use in the United States to help protect against diphtheria and tetanus. Nine of these vaccines also help protect against whooping cough. Some of the vaccines include protection against other diseases as well, including polio, Haemophilus influenzae type b disease, and hepatitis B.
- DT (generic) and Td provide protection against diphtheria and tetanus.
- DTaP provides protection against diphtheria, tetanus, and whooping cough.
- Upper-case letters in these abbreviations mean the vaccine has full-strength doses of that part of the vaccine. The lower-case “d” and “p” in Td and Tdap means these vaccines use smaller doses of diphtheria and whooping cough. The “a” in DTaP and Tdap stands for “acellular,” meaning that the whooping cough component contains only parts of the bacteria instead of the whole bacteria.
Centers for Disease Control and Prevention. Tetanus Vaccine Information Statement. Centers for Disease Control and Prevention https://wwwnc.cdc.gov/travel/diseases/tetanus . Reviewed May 4 2020. Accessed April 20 2021.
Centers for Disease Control and Prevention. Diphtheria Vaccine Information Statement. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/diphtheria . Reviewed May 1 2020. Accessed April 20 2021.
Centers for Disease Control and Prevention. Pertussis (Whooping Cough) Vaccine Information Statement. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/diseases/pertussis . Reviewed May 1 2020. Accessed April 20 2021.
Centers for Disease Control and Prevention. Diphtheria, Tetanus, and Whooping Cough Vaccination: What Everyone Should Know. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/vpd/dtap-tdap-td/public/index.html . Reviewed January 22 2020. Accessed April 20 2021.
Centers for Disease Control and Prevention. TD (Tetanus, Diphtheria) Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/td.html . Reviewed April 1 2020. Accessed April 20 2021.
Centers for Disease Control and Prevention. DTaP (Diphtheria, Tetanus, Pertussis) Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/dtap.html . Reviewed April 1 2020. Accessed April 20 2021.
Centers for Disease Control and Prevention. Tdap (Tetanus, Diphtheria, Pertussis) Vaccine Information Statement. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/tdap.html . Reviewed April 1 2020. Accessed April 20 2021.
- 150 College Rd W, Princeton, NJ 08540
- [email protected]
Stay Connected
- Terms of use
- Privacy Policy
AITC Immunization & Travel Clinic
We provide travel health visits, vaccinations, TB testing, and blood tests. Appointment only.
Attention! starting April 15, 2024
Our new website address is SF.GOV/AITC
AITC Services, Price, and Forms
Book an appointment on line and get clinic forms
See our services and prices
Donate to AITC
Welcome to AITC
AITC is a non-profit clinic that is part of the San Francisco Department of Public Health (SFDPH). As public health providers, our mission is to prevent disease and protect the health of all.
We are open to the public, and serve all members of the community, including:
- Teens and adults seeking recommended vaccinations
- School age children needing vaccines required for school
- Adults who need vaccines for work or school
- Immigrants to the US requiring vaccines for Change of Status
- Individuals and families planning international travel
Our services are by appointment only.
AITC is unable to accept insurance. Fees must be paid at the time of service. Low-cost or free services are available to those who qualify.
Message about our MPOX vaccine (JYNNEOS) supply
Mpox vaccine at AITC is still supplied free of charge by the government. Later in 2024 we may need to purchase the vaccine and charge a fee for it. We will post more information when it becomes available.
Getting here
Metered street parking or Civic Center Garage
Public transportation
Southwest corner, Civic Center Plaza Across from City Hall BART / MUNI : Civic Center Station
Make an appointment online by clicking the left link. It is highly recommended; it is simpler and faster.
If you need assistance, please call us.
AITC Immunization & Travel Clinic
Mon to Fri, 9:00 am to 4:00 pm Closed for lunch 12 pm - 1pm
We are closed weekends and holidays .
Find more information about how to get to our clinic .
Departments
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 3 - Travelers with Disabilities
- Section 3 - Highly Allergic Travelers
Travelers with Chronic Illnesses
Cdc yellow book 2024.
Author(s): Noreen Hynes
Although traveling abroad can be relaxing and rewarding, the physical demands of travel can be stressful, particularly for travelers with underlying chronic illnesses. With adequate preparation, however, these travelers can have safe and enjoyable trips. For more detailed information on assisting immunocompromised travelers , travelers with disabilities , highly allergic travelers , and travelers with substance use disorders prepare for international travel, see the respective chapters in this section.
Patients should see their established health care providers well in advance of travel to ensure that all chronic conditions are controlled, and management is optimized. Clinicians should encourage patients to seek pretravel consultation prior to paying for nonrefundable trips, and at least 4–6 weeks before departure to ensure adequate time to respond to immunizations, try new medications before travel, or redefine the itinerary based upon pretravel consultation recommendations.
General Approach
Advising travelers.
Adequate preparation for patients with chronic illnesses for international travel requires the active participation of both the traveler and the travel health provider. Box 3-03 includes a checklist of pretravel activities for travelers with chronic illnesses.
Box 3-03 A checklist for travelers with chronic illnesses preparing for international travel
☐ Carry copies of all prescriptions.
☐ Check with the foreign embassy or consulate for your destination country in the United States to clarify whether any medication restrictions exist. Some countries do not allow visitors to bring certain medications into the country, especially narcotics and psychotropic medications.
☐ Favor travel to destinations that have access to quality care for your condition (see Sec. 6, Ch. 2, Obtaining Health Care Abroad )
☐ Obtain an established provider letter. The letter should be on office letterhead stationery and outline existing medical conditions, medications prescribed (including generic names), and any equipment required to manage the condition. By law, some states do not permit a travel health specialist to furnish such a letter if the specialist is not also the primary care provider or established provider of record.
☐ Pack a travel health kit (see Sec. 2, Ch. 10, Travel Health Kits ). Take health kits on board as carry-on luggage, and bring all necessary medications and medical supplies (e.g., pouching for ostomies) in their original containers.
☐ Select a medical assistance company that allows you to store your medical history so it can be accessed worldwide.
☐ Sign up for the Smart Traveler Enrollment Program , a free service of the US Department of State to US citizens and permanent residents, to receive destination-specific travel and security updates. This service also allows the Department of State to contact international travelers during emergencies.
☐ Stay hydrated, wear loose-fitting clothing, and walk and stretch at regular intervals during long-distance travel (see Sec. 8, Ch. 3, Deep Vein Thrombosis & Pulmonary Embolism ).
☐ Wear a medical alert bracelet or carry medical information on your person. Various brands of jewelry or tags, even electronic ones, are available.
Health Care Provider Roles & Responsibilities
Health care providers play a critical role in helping patients with chronic underlying conditions travel safely. Ask patients about previous health-related issues encountered during travel (e.g., complications during air travel). In addition to sharing the advice found in Box 3-03 , ensure the traveler has sufficient medication (and proper storage conditions) for the entire trip, plus extra in case of unexpected delays. Because medications should be taken based on elapsed time and not time of day, offering travelers guidance on scheduling when to take medications during and after crossing time zones might be needed. Educate travelers on possible drug interactions (see Sec. 2, Ch. 4, Interactions Between Travel Vaccines & Drugs ). Some medications used to treat chronic medical illnesses (e.g., warfarin) can interact with prescribed self-treatment for travelers’ diarrhea or malaria chemoprophylaxis. Discuss all medications patients use, including medications taken daily, those taken on an as-needed basis, and dietary supplements or herbal products. In addition, discuss supplemental insurance options for travelers, including policies that cover trip cancellation in the event of illness, supplemental medical insurance, and medical evacuation insurance. Supplemental medical insurance can reimburse travelers for money paid for health care abroad; most medical insurance policies do not cover the cost of health care received in other countries. Medical evacuation insurance covers moving the person from the place of illness or injury to a place where they can receive definitive care. Travelers might need assistance to identify supplemental insurance plans that will cover costs for preexisting conditions (see Sec. 6, Ch. 1, Travel Insurance, Travel Health Insurance & Medical Evacuation Insurance ).
Help patients devise a Personal Travel Health Plan. This plan should give instructions for managing minor problems or exacerbations of underlying illnesses and should include information about medical facilities available in the destination country (see Sec. 6, Ch. 2, Obtaining Health Care Abroad ).
Specific Chronic Medical Conditions
Chronic illness or acute illness affecting underlying chronic disease might affect the recommendations clinicians make to a traveler after completing the risk assessment conducted as part of the pretravel consultation (see Sec. 2, Ch. 1, The Pretravel Consultation ). Some online resources for travelers who have ≥1 chronic medical conditions can be found in Table 3-05 (in Sec. 3, Ch. 2, Travelers with Disabilities ) and Table 3-07 .
Chronic conditions include those affecting the cardiovascular, endocrine, gastrointestinal, genitourinary, hematological, hepatic, neurologic, and respiratory systems. Table 3-08 addresses issues and recommendations related to specific chronic medical illnesses and should be used in conjunction with the other recommendations given throughout this book.
Travelers also might want to investigate international health care accreditation agencies to identify health care facilities at the travel destination that have received recognition or accreditation for high care standards and good patient safety records. If travelers or their health care providers have concerns about fitness for air travel or the need to obtain a medical certificate before travel, the medical unit affiliated with the specific airline is a valuable source for information.
Travelers who require service animals, including emotional support animals, should check with the airline and the destination country to ensure both the air carrier and the country will allow the animal; documentation and permits might also be required (see Sec. 7, Ch. 6, Traveling with Pets & Service Animals ). Travelers planning to use supplemental oxygen on the aircraft or needing other equipment (e.g., a wheelchair) must inform the airline far in advance of planned travel. The Transportation Security Administration (TSA) Cares Helpline (toll-free at 855-787-2227) or TSA Cares online assistance also can provide information on how to prepare for the airport security screening process for a particular disability or medical condition.
Table 3-07 Online resources for travelers with chronic illnesses: disease & condition-specific
DISEASE / CONDITION
ORGANIZATION / SOURCE
ANTICOAGULATION
Anticoagulation Forum
Centers of Excellence Resource Center
American Cancer Society
Eat Right and Stay Active while Traveling
CELIAC DISEASE
National Celiac Association
Eating GF when traveling abroad
CHRONIC PAIN
International Pain Foundation
Top Tips for Traveling Abroad with Chronic Pain
American Diabetes Association
Air Travel and Diabetes
Epilepsy Foundation
Travel and Holidays
Epilepsy Society (UK)
Travel and holidays for people with epilepsy
HEART CONDITIONS
American Heart Association
Healthy Travel
INFLAMMATORY BOWEL DISEASE
Crohn’s & Colitis Foundation
Traveling with IBD
KIDNEY DISEASE
American Association of Kidney Patients (AAKP)
International Travel while on Dialysis
National Kidney Foundation
Foreign Travel Tips for Dialysis Patients
Global Dialysis (UK)
Travel Advice
LUNGS & CHEST
American Lung Association
Traveling with Oxygen
MULTIPLE SCLEROSIS
Multiple Sclerosis Foundation
Tips for Traveling Abroad with MS
SLEEP APNEA
American Sleep Association
Travel: CPAP Machines
American Sleep Apnea Association
US Travel Tips for CPAP Users
Table 3-08 Special considerations for travelers with chronic illnesses
Abbreviations: AAKP, American Association of Kidney Patients; AICD, automatic implantable cardioverter defibrillator; CABG, coronary artery bypass graft; CHF, congestive heart failure; CKD, chronic kidney disease; CNS, central nervous system; COPD, chronic obstructive pulmonary disease; COVID-19, coronavirus disease; CrCl, creatinine clearance; CVA, cerebrovascular accident; DVT, deep vein thrombosis; ECG, electrocardiogram; FSBG, fingerstick blood glucose; GI, gastrointestinal; Hgb, hemoglobin; HIV, human immunodeficiency virus; IGRA, interferon-γ release assay; INR, international normalized ratio; PNS, peripheral nervous system; PPIs, proton-pump inhibitors; PTX, pneumothorax; TD, travelers’ diarrhea; TIA, transient ischemic attack; TNF, tumor necrosis factor; TST, tuberculin skin test; YF, yellow fever.
a There is a spectrum of airline travel–related risk that depends on the cardiovascular disorder, the defined risk group within the disorder, and the time since the acute event (if applicable). Evidence basis for recommendations is suboptimal, however.
b See Sec. 5, Part 3, Ch. 16, Malaria , for additional details.
The following authors contributed to the previous version of this chapter: Deborah Nicolls Barbeau, Gail A. Rosselot, Sue Ann McDevitt
Bibliography
Aisporna C, Erickson-Hurt C. End-of-life travel: A bucket list desire for patients with life limiting illnesses. J Hospice Pall Nursing. 2019;21(5):397–403.
Furuto Y, Kawamura M, Namikawa A, Takahashi H, Shibuya Y. Health risk of travel for chronic kidney disease patients. J Res Med Sci. 2020;25:22.
Heng S, Hughes B, Hibbert M, Khasraw M, Lwin Z. Traveling with cancer: A guide for oncologists in the modern world. J Glob Oncol. 2019;5:1–10.
International Air Transport Association. Medical manual, 12th edition; July 2020. Available from: www.iata.org/en/publications/medical-manual .
Josephs LK, Coker RK, Thomas M; British Thoracic Society Air Travel Working Group. Managing patients with stable respiratory disease planning air travel: a primary care summary of the British Thoracic Society recommendations. Prim Care Respir J. 2013;22(2):234–8.
McCarthy AE, Burchard GD. The travelers with pre-existing disease. In: Keystone JS, Kozarsky PE, Connor BA, Nothdurft HD, Mendelson M, Leder K, editors. Travel medicine, 4th edition. Philadelphia: Saunders Elsevier; 2018. pp. 263–6.
Pinsker JE, Becker E, Mahnke CB, Ching M, Larson NS, Roy D. Extensive clinical experience: a simple guide to basal insulin adjustments for long-distance travel. J Diabetes Metab Disord. 2013;12(1):59.
Ringwald J, Strobel J, Eckstein R. Travel and oral anticoagulation. J Travel Med. 2009;16(4):276–83.
Smith D, Toff W, Joy M, Dowdall N, Johnston R, Clark L, et al. Fitness to fly for passengers with cardiovascular disease. Heart. 2010;96(Suppl_2):ii1–16.
US Department of Justice. Exemption from import or export requirements for personal medical use. Title 21 CFR §1301.26. 2004 Sep 14. Available from: www.deadiversion.usdoj.gov/fed_regs/rules/2004/fr0914.htm .
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

IMAGES
VIDEO
COMMENTS
More. Learn about CDC's Traveler Genomic Surveillance Program that detects new COVID-19 variants entering the country. Sign up to get travel notices, clinical updates, & healthy travel tips. CDC Travelers' Health Branch provides updated travel information, notices, and vaccine requirements to inform international travelers and provide ...
Links with this icon indicate that you are leaving the CDC website.. The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website. Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
Don't travel while sick. If you have a weakened immune system or are at increased risk for severe disease talk to a healthcare professional before you decide to travel. If you travel, take multiple prevention steps to provide additional layers of protection from COVID-19, even if you are up to date with your COVID-19 vaccines.
Clean your hands often. Use soap and water or an alcohol-based cleanser to help prevent infection. Do not stand or swim in fresh-water rivers, streams, or lakes that have sewage or animal feces in them. This can lead to infection. Swimming in chlorinated pools is safe most of the time.
During 2020-2022, CDC used these authorities to restrict travel of people with COVID-19 and close contacts who were recommended to quarantine. These authorities were also used for mpox during 2022. Travel restrictions can also be used for other suspected or confirmed contagious diseases that could pose a public health threat during travel ...
You can then travel more safely within the U.S. and internationally. But international travel can still increase your risk of getting new COVID-19 variants. The Centers for Disease Control and Prevention (CDC) recommends that you should avoid travel until you've had all recommended COVID-19 vaccine and booster doses.
Before travel: contact a travel medicine centre or a physician, preferably 4-8 weeks before departure to receive any required vaccinations; read up on local diseases related to your destination; request information on malaria risk and prevention of mosquito bites.
Chang W. Lee/The New York Times. The Centers for Disease Control and Prevention updated its guidance for fully vaccinated Americans in April, saying that traveling both domestically and ...
Summary. Traveling can increase your chances of getting sick. A long flight can increase your risk for deep vein thrombosis. Once you arrive, it takes time to adjust to the water, food, and air in another place. Water in developing countries can contain viruses, bacteria, and parasites that cause stomach upset and diarrhea.
The Yellow Book is produced biennially with input from hundreds of travel medicine experts and is published through a unique collaboration between CDC, the CDC Foundation and Oxford University Press. The 2018 edition codifies the U.S. government's most current health guidelines and information for international travelers, including pretravel ...
The main infectious diseases to which travellers may be exposed, and precautions for each, are detailed in the Chapter 5 of the International travel and health situation publication.The most common infectious illness to affect travellers, namely travellers' diarrhoea, is covered in Chapter 3 of the International travel and health situation publication.
Protect your child and family when traveling in the United States or abroad by: Getting the shots required for all countries you and your family plan to visit during your trip. Making sure you and your family are up-to-date on all routine U.S. vaccines. Staying informed about travel notices and alerts and how they can affect your family's ...
Clean your hands often. Use soap and water or an alcohol-based cleanser to help prevent infection. Do not stand or swim in fresh-water rivers, streams, or lakes that have sewage or animal feces in them. This can lead to infection. Swimming in chlorinated pools is safe most of the time.
To identify travel-related diseases and facilitate rapid communication between clinicians and public health professionals globally, a surveillance system (e.g., GeoSentinel) is needed. Such connectivity can reduce the size of outbreaks while promoting the timely sharing of clinical insight regarding the diagnosis and treatment of patients.
Also searched were the Centers for Disease Control and Prevention and Cochrane databases. Search dates: September 2022 to November 2022, March 2023, and August 2023. ... Surveillance for travel ...
International Travel and Infectious Disease. Traveling abroad can increase your exposure to infectious diseases caused by viruses, bacteria, or parasites. Some significant infectious health hazards for Americans traveling abroad are diarrhea, malaria, hepatitis A, and other emerging diseases. Many diseases are just a plane ride away.
The Centers for Disease Control and Prevention (CDC) Travelers' Health website also has materials and an interactive web-tool to guide primary care physicians through a pretravel consultation. ... Hepatitis A is one of the most common vaccine-preventable diseases acquired during travel. Prevaccination serologic testing for hepatitis A ...
Malaria is the most common febrile illness among travelers to endemic areas and is caused by the mosquito-borne parasites of the Plasmodium genus, primarily P. falciparum, P. vivax, P. ovale, and P. malariae. Cases in the USA have been increasing over the last few decades to over 2000 cases reported to the CDC in 2016.
Malaria is always a serious disease and may be a deadly illness. Travelers who become ill with a fever or flu-like illness either while traveling in a malaria-risk area or after returning home (for up to 1 year) should seek immediate medical attention and should tell the physician their travel history. Travelers who are assessed at being at ...
Sitting immobile on long plane flights or car, train or bus rides can slightly increase a normal person's risk of blood clots in the legs, but associated medical issues usually contribute to it. If someone has peripheral artery disease (PAD) or a history of heart failure, the clot risk increases.
Typhoid fever and paratyphoid fever cause similar symptoms. People with these diseases usually have a fever that may go as high as 103-104°F (39-40°C). They also may exhibit weakness, stomach pain, headache, diarrhea or constipation, cough, and loss of appetite. Some people have a rash of flat, rose-colored spots.
AITC is a non-profit clinic that is part of the San Francisco Department of Public Health (SFDPH). As public health providers, our mission is to prevent disease and protect the health of all. We are open to the public, and serve all members of the community, including: Our services are by appointment only. AITC is unable to accept insurance.
CDC Yellow Book 2024. Although traveling abroad can be relaxing and rewarding, the physical demands of travel can be stressful, particularly for travelers with underlying chronic illnesses. With adequate preparation, however, these travelers can have safe and enjoyable trips. For more detailed information on assisting immunocompromised ...