

Popular Services
- Patient & Visitor Guide
Committed to improving health and wellness in our Ohio communities.
Health equity, healthy community, classes and events, the world is changing. medicine is changing. we're leading the way., featured initiatives, helpful resources.
- Refer a Patient
Dos and don’ts of visiting someone in the hospital
Author: Sean Ankrom, MD
- Health and Wellness

When a friend, family member or loved one is in the hospital, your first instinct is to visit them and show your respects, whether it be due to an illness, injury or accident. Stepping into the hospital environment can be intimidating and scary. Here are some things you should remember when visiting a hospital patient.
What are the most common things that hospital visitors do that they shouldn't?
It's very important to not overstay your welcome when visiting a hospitalized patient. Patients need rest during their stay, and hosting visitors for an extended period can be draining--both physically and emotionally. The length of the visit should be proportional to how well you know the patient, but I’d recommend limiting the visit to one hour or less. If a physician enters during your visit, it's polite to step outside of the room until the conversation is over.
When is the best time to visit someone in the hospital?
The best time to visit a hospitalized patient is in the early evening. The hospital is typically humming with activity throughout the day, when patients are often scheduled for tests, procedures and staff are frequently entering and exiting the room. Toward late afternoon, the hospital tends to slow down a bit. By visiting later in the day, you'll have a better chance of having an uninterrupted visit. Weekends are another great opportunity to visit, as the hospital is usually quieter.
What are a few important things visitors should do before/after visiting the hospital?
Before traveling to the hospital, call to check the visitation policy. Certain units have strict visiting hours and some have policies that restrict the number of visitors. It’s common for young children to be restricted from visiting. If you have any signs of illness, such as fever, runny nose, nasal congestion or cough, it’s recommended that you postpone your visit until you’re well. After arriving at the hospital, check in with the nurse before entering the room to see if any personal protective equipment is required to prevent communicable disease. Washing your hands or using hand sanitizer when you enter or exit a hospital room is one of the most important things you can do to prevent the spread of germs.
Is it OK to bring gifts?
Bringing gifts is a fantastic idea, but isn’t necessary. The presence of a familiar face is often the best present a patient can receive in the hospital. If you do choose to bring a gift, bear in mind that hospital rooms are often small and storage space is limited. A large bouquet of flowers or balloons may seem like a nice gesture, but it may end up making the room feel crowded. Before visiting, I recommend checking in with the patient or a family member to see if they have any gift requests. Maybe there’s a book they’ve been wanting to read, a new issue of a favorite magazine or newspaper, or a small item that reminds them of home that you can bring in. Coloring books, puzzle books and card games also make nice gifts. If you’re thinking about bringing in outside food, check with the nurse or physician first. Patients are often on specialized medical diets and may have certain dietary restrictions. Sean Ankrom is a hospitalist at The Ohio State University Wexner Medical Center.
- View our comprehensive guide to make your visit as a patient or visitor as effortless as possible. Learn more
More from Ohio State

Online price list gives you clarity for your health care
Online hospital charge lists can give you clarity for your healthcare costs, but like our medical care – we want to personalize it to you.

Sen. Brown tours COVID-19 testing site at CAS
Sen. Brown talks with members of the Ohio National Guard who’ve joined health care workers across the state on the front lines in the battle against COVID-19.

Decades of leadership experience prove vital in the state’s fight against COVID-19
Dr. Andrew Thomas and his decades of leadership experience at The Ohio State University Wexner Medical Center have been vital in the state’s fight against COVID-19.
Visit Ohio State Health & Discovery for more stories on health, wellness, innovation, research and science news from the experts at Ohio State.
Check out health.osu.edu
Subscribe. Get just the right amount of health and wellness in your inbox.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
How Hospital Visitation Policies Are Changing During COVID-19
Er Productions Limited / Getty Images
Key Takeaways:
- Since March, hospitals have implemented strict visitation policies, which have profoundly impacted patients and their families.
- Now, hospitals nationwide are slowly relaxing their protocols and seeking feasible ways to manage the emotional needs of patients while preventing the spread of COVID-19.
- Restrictive hospital visitation can leave patients without an advocate and physical support from their loved ones.
It was May 15 when Emily Schmitz's 78-year-old father was first admitted to the hospital for small bowel obstruction surgery. Despite her father testing negative for COVID-19, Schmitz says she and her siblings were not permitted to see him due to the hospital's strict visitation policies.
Schmitz, who owns a communications agency in Austin, Texas, tells Verywell that initially, her father was doing well, but he quickly deteriorated—showing signs of confusion—which concerned her and her siblings. Soon they were making countless phone calls to the hospital to ensure their father’s needs were met, including a request for water.
"[My sister] asked every day to see him, especially when his mental and physical state was deteriorating, and they still would not allow her to see him and advocate for better care for him," she says. Eventually, on May 21, the hospital allowed Schmitz's sister to visit their father, but only for the day.
Growing more concerned about her father's condition, Schmitz flew in from Texas, but upon arriving at the hospital, she was denied visitation. She decided to take matters into her hands. “I took it all the way to the hospital administrator and it took that to have someone listen to us,” Schmitz says. “It was pretty frustrating.”
On May 29, the hospital finally allowed Schmitz and her siblings to visit their father, who at that point, was in critical condition in the intensive care unit (ICU). They wore masks and gloves and were only allowed to visit for 10 minutes.
Their father passed away the next day—alone—not from the small bowel obstruction for which he was originally admitted, but from severe sepsis with septic shock.
“Families know their loved one and know when something is not right,” Schmitz says. “So, not being able to have somebody there for the patient is where hospital systems are falling really short.”
After months of restrictive visitation policies, patients and their families are speaking out about COVID-19's emotional toll. Now, hospitals nationwide are responding by slowly relaxing their protocols, and implementing new strategies to keep families connected.
What This Means For You
If you or your loved one needs to visit the hospital, check with your local hospital to review their updated COVID-19 visitation policies. Phone and video calls are good ways to stay connected, but your local hospital may have different resources to help families cope with the distance.
How Strict Are Visitation Policies Now?
At the beginning of the pandemic, most hospitals implemented strict no-visitor rules to curb the spread of COVID-19. A July study, published in The American Journal of Respiratory and Critical Care Medicine , found that out of 48 Michigan hospitals, 39% prohibited visitors without exception and 59% only allowed visitors under “certain exceptions.” These certain exceptions often meant end-of-life situations or the birth of a child. Hospital systems set their own individual policies, but federal organizations like the Centers for Disease Control and Prevention have released COVID-19 guidelines for healthcare facilities.
After several reports about the negative ways visitation policies have impacted patients and their families, some hospitals are beginning to loosen their restrictions, while still requiring visitors to take the necessary COVID-19 precautions like wearing masks. For example, for inpatient units, MedStar Health System, located in Maryland and Washington D.C., now allows patients one visitor per day, but only if that patient doesn't have COVID-19.
For Mothers and Babies
“Initially, we implemented a draconian approach, which was to almost completely shut down all visitors, except for the mother’s significant other,” Jorge E. Perez, MD , neonatologist and co-founder of Kidz Medical Services, tells Verywell.
According to Perez, who also serves as medical director of neonatal and newborn services at South Miami Hospital in Florida, the visitor would have to stay isolated in the mother’s room until the mother and baby were discharged. If the visitor left the hospital, they would be unable to return.
While the one visitor-per-patient rule remains in effect at South Miami Hospital, if that visitor leaves the hospital, they are now permitted to return.
Similar strict policies were common in other hospitals, especially during the height of the pandemic, when COVID-19’s impact on babies was relatively unknown. According to the Centers for Disease Control and Prevention (CDC), while most newborns who contract the virus have either mild or no symptoms, there have been reports of newborns who develop severe cases of COVID-19.
“We had to be creative to continue offering family-centered care," Perez says. The Kidz Medical team at his hospital communicated daily with the parents of patients in the NICU. In addition, they provided 24/7 viewing cameras so parents and extended family members could view infants in real-time and follow their progress.
“It’s known that women have better birth outcomes when stress levels are reduced and when they’re surrounded by support and advocacy," Talitha Phillips , a labor and postpartum doula in Los Angeles and CEO of Claris Health, tells Verywell. "This is especially critical for women of color who already face health disparities when it comes to labor and delivery.”
Phillips is no stranger to the emotional difficulties pregnant women face when forced to choose only one support person to accompany them in the hospital. She and her clients were devastated to learn about the restrictive visitation rules that went into effect this March.
“I will never forget sitting in an Uber, crying after I had to leave a mom and her husband at the entrance of a hospital," she says. "We’d labored together for 12 hours and in her most intense moments, I had to ‘abandon’ her.”
She explains that although the ability to provide her labor and postpartum doula services in-hospital is still limited, “in the last two weeks, two hospitals in LA have started allowing women to bring a partner and one support person with them.”
For ICU Patients
ICU visitation rules vary greatly by hospital and state. For example, the University of California San Francisco Health System now allows up to two visitors at a time in the ICU. Visitors may visit at any time and one visitor may stay overnight.
Studies show that visitation is highly important to patients in intensive care units, especially those who aren’t able to speak up for themselves. Researchers found that family presence at the bedside can help reduce delirium as well as help families make better decisions regarding their loved one’s care.
Schmitz and her family wish they could've been at her father's side during his hospitalization. Strict COVID-19 visitation rules made it difficult for her and her siblings to stand up for him, and keep track of the care he needed.
“The message I want to get across most urgently is the importance of having an advocate for your family member, speaking up, and taking it to the top if you have to," Schmitz says.
Valley T, Schutz A, Nagle M, et al. Changes to visitation policies and communication practices in michigan ICUs during the COVID-19 pandemic . Am J Respir Crit Care Med . 2020;202(6):883-885. doi:10.1164/rccm.202005-1706le
Centers for Disease Control and Prevention. Ten Ways Healthcare Systems Can Operate Effectively during the COVID-19 Pandemic .
MedStar Health. Temporary Visitor Restrictions and Guidance During COVID-19 .
Centers for Disease Control and Prevention (CDC). COVID-19 and Pregnancy .
UCSF Health. Visitor Restrictions at UCSF Due to the Coronavirus (COVID-19) .
By Kara-Marie Hall, RN, BSN, CCRN
- EXPLORE Random Article
How to Prepare Yourself for Visiting Someone in Hospital
Last Updated: February 16, 2022 References
This article was medically reviewed by Jonas DeMuro, MD . Dr. DeMuro is a board certified Pediatric Critical Care Surgeon in New York. He received his MD from Stony Brook University School of Medicine in 1996. He completed his fellowship in Surgical Critical Care at North Shore-Long Island Jewish Health System and was a previous American College of Surgeons (ACS) Fellow. There are 8 references cited in this article, which can be found at the bottom of the page. This article has been viewed 36,215 times.
If you're planning on visiting someone in the hospital, you may be feeling anxious, confused, or helpless about that individual's condition. You may even be fearful of seeing that person in a state of illness or incapacity. All of these feelings are normal and can be managed with proper planning. Learning how to manage your emotions and figure out the logistics of a hospital visit can help you be as prepared as possible for this potentially upsetting situation.
Figuring Out the Logistics

- Call ahead with the name of the patient you wish to visit to confirm the location of the patient and the visiting hours for that ward.

- Some patients may not be physically or mentally capable of having visitors. This could be for a variety of reasons, and it's important to be respectful of those reasons.
- The person may be on isolation precautions, meaning you will have to take special steps before entering the room. Speak to a nurse to find out if you need to wear a mask, protective gown, gloves, or other protective equipment. The nurse will be able to provide you with these items and instruct you on proper use. It's important you follow directions exactly, to protect both the patient and yourself.
- Call the hospital and ask to speak with a nurse working on your patient's floor. Ask the nurse whether it would be okay to visit, and provide a rough time frame you'd like to visit.

- Check in with the patient or her family to see if she wants visitors while staying in the hospital.
- If the patient does not want visitors, be respectful of her wishes. You can always send a card or get-well package through the mail or ask the patient's family to deliver it for you.

- If you're ill, you are better off staying out of the hospital for both yourself and the patient. Consider a phone call or video chat instead.
- Even if you're healthy, you should wash your hands before and after visiting the hospital, in particular when you enter and exit the patient’s room. You could accidentally introduce bacteria or viruses to patients inside the hospital, or you could inadvertently carry a serious pathogen home with you when you leave the hospital.
- When you wash your hands, use soap and clean, running water for a total of 20 seconds. [4] X Trustworthy Source Centers for Disease Control and Prevention Main public health institute for the US, run by the Dept. of Health and Human Services Go to source You may also wish to use an alcohol-based hand sanitizer instead of washing your hands.
Feeling Emotionally Prepared

- Start out by only reading credible medical articles. You can find a wealth of information on websites run by hospitals, medical schools, and medical care centers, such as the Mayo Clinic or Medline Plus .
- You can also find endless information in print form. Check your local library for medical textbooks and journals, then research the condition or illness for which your friend or relative is being treated.
- Once you've read some credible medical information, it may be comforting to read some personal accounts that talk about that condition/illness. Look for memoirs or even personal online blogs that discuss that condition or illness. Online forums specific to the illness often have good discussions and information.

- Remember that everyone deals with crisis situations differently. You may be able to maintain your composure and handle the situation, or you may grow anxious, frightened, or even angry.
- These feelings may change as the patient's health improves, declines, or alternates between improvement and decline.

- You can speak with family and friends about any concerns you have, especially if those friends or relatives are also close with the patient you're going to visit.
- If you have deeper-seated emotional concerns, you may want to consider speaking with a therapist or a clergy member (if you are religious).

- You can write anything you want in your journal. You don't have to show it to anyone, and you can even destroy the page when you're finished.
- Try to be consistent in your journaling. Since your feelings may change as the days or weeks go on, it can be helpful to make a daily habit of reflecting and writing.
- You can buy any type of journal you want, from a simple spiral-bound notebook to an elegant leather-bound book of blank pages; however, you may want to consider portability and ease of access when you're deciding on a notebook.
- It may be easier for you to journal on your phone or tablet. There are many apps that allow you to keep a journal on your devices.

- Exercise regularly. This can help you burn off some energy or stress and stay healthy. Even walking around the hospital can help.
- Make sure you're eating a healthy diet. While vending machines are convenient, they mostly contain junk food and you'll need proper nutrition, including a balanced diet with fresh fruits and vegetables.
- Get adequate rest. Remember that most adults need at least seven to nine hours of sleep each night, while some adults may need even more sleep. [7] X Research source
- Do things to help you relax and deal with your stress. Even if you can't leave the hospital, bring books, magazines, crafts, and other things to keep yourself busy and take your mind off of things.
Making a Successful Visit

- Try to base your gift on the individual's tastes.
- Choose a gift that will cheer up the individual. For example, if you know the person is an avid hiker and camper who is eager to get back on the trail, you may want to bring something that will make her think of hiking or camping.
- Consider bringing something that will help the person pass the time, such as a book of crossword puzzles, magazines, a book, or some other activity.
- If you know an image or object might upset the patient, you should avoid bringing anything that might be a reminder of that image or object. For example, if the individual will never be able to walk or ride a bike again, bringing reminders of these activities could be upsetting.

- Anticipate that the patient may be feeling a range of emotions. She may be feeling hopeful, fearful, angry, or she may even be in denial.
- Never tell the individual how she should feel. Simply accept the way she's feeling without criticism or interrogation.
- Ask the individual if she wants to talk about what she is going through. Don't unload your grief or fear on the patient, as she has enough to deal with on her own.
- Let the patient know that you're available to talk anytime. Even if she doesn't want to discuss what she's going through now, that may change with time. Make sure she has your contact information so she can reach you in case she wants to talk later.
- If the patient has a chronic illness/condition or will be going through a prolonged recovery period, be sure that you continue to offer support over the long-term. Many people will be there at first, but your friend or relative will need support down the line.

- Talk to other friends or family members of the patient to coordinate schedules. Let each other know when you're available and what shifts would work best.
- Once you've worked out a schedule, let the patient know who will be staying in the hospital and when. Having a schedule in mind may help give the patient some sense of normalcy.

- Going for a walk, getting yourself some food or coffee, or simply stepping outside to talk on the phone can help give you a mental break from the stress of being in the hospital.
- Let the individual know that you'll be back, and try to provide a rough time estimate. This can help put an anxious hospital patient a bit more at ease.

- Don't point out that the patient looks ill, injured, or otherwise unwell. Likewise, avoid talking about the procedure/surgery unless the patient wants to talk about it.
- Focus on the patient's treatment and recovery. Try to remain positive so that the patient can keep a healthy, positive attitude.
- If the patient is feeling sad or hopeless, try to lift her spirits. Talk about fun or humorous memories and try to get her to think about the fun times you'll have in the future once she is feeling better.
Expert Q&A
- Be aware of what you say to the patient. Never say something like, "Gosh, you gave us all a fright!" This can create feelings of guilt in the patient at a time when they should be focusing on recovery. Thanks Helpful 1 Not Helpful 0
- Try to see the positive things about a hospital stay. Many patients are having babies, getting long awaited life-changing surgery or having treatments that will make them better in the long term. Thanks Helpful 1 Not Helpful 0
- ↑ https://www.betterhealth.vic.gov.au/health/servicesandsupport/visitors-in-hospital#lp-h-3
- ↑ https://www.betterhealth.vic.gov.au/health/servicesandsupport/visitors-in-hospital#lp-h-1
- ↑ https://www.betterhealth.vic.gov.au/health/servicesandsupport/visitors-in-hospital#lp-h-2
- ↑ http://www.cdc.gov/features/handwashing/
- ↑ http://med.stanford.edu/cfcenter/services/SupportingLovedOnes.html
- ↑ http://www.healthtalk.org/peoples-experiences/intensive-care/intensive-care-experiences-family-friends/emotional-impact-relatives-friends-icu
- ↑ https://sleepfoundation.org/how-sleep-works/how-much-sleep-do-we-really-need
- ↑ https://www.betterhealth.vic.gov.au/health/servicesandsupport/visitors-in-hospital
About this article

Did this article help you?
You might also like.

- About wikiHow
- Terms of Use
- Privacy Policy
- Do Not Sell or Share My Info
- Not Selling Info
Patient and Visitor Guide

Patient & Visitor Guide
Your guide to getting care at mayo clinic, all about appointments.
From referrals to insurance. Here's what you need to know to request your first appointment.
Plan for your trip
Traveling for medical care isn't easy. Know what to expect and get practical tips to make your trip as easy and comfortable as possible.
- Preparing for your visit
While you're here
Hotels? Restaurants? Maps? We've compiled the travel resources you need for all three Mayo Clinic campuses.

Why choose Mayo Clinic?
We make sure patients get the personalized attention and expert care they need to heal faster.
Insurance, billing & financial support
Use these resources for insurance and billing questions. Or contact Patient Account Services for help.
- Billing & Insurance
- Cost Estimator Tool
- Charitable Care & Financial Assistance
International Services
Every year, patients from more than 140 countries travel to Mayo Clinic for care. International patients receive timely diagnosis and specialty care in a place designed to feel a little more like home.
Learn more about Mayo Clinic Patient Travel Services
Patient Travel Services makes planning for your appointment at Mayo Clinic seamless. From any location, worldwide, our dedicated team will guide you through your journey for the care you need.
Patient Online Services
Access your medical records and communicate with your care team from your favorite digital device.
- Create your Patient Online Services account
- Download the Mayo Clinic app
Join our online community
Share your experiences and find support from people like you. Get updates from Mayo Clinic doctors and other experts. You'll find groups focused on cancer, heart health, mental health and more.
Read Mayo Clinic stories
Sharing Mayo Clinic is a place for patients, families and Mayo Clinic staff to share their experiences. You might find inspiration in their triumphs and powerful stories.
Medical records and imaging request
Learn more about how to access and request your imaging and medical records.
Be a blood donor
Each whole blood donation might help save three lives.
Patient confidentiality, rights, responsibilities and privacy
Mayo Clinic is committed to protecting patient confidentiality and rights.
- Confidentiality at Mayo Clinic
- Patient rights, responsibilities and privacy
- Federal Civil Rights Postings in multiple languages
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Preventing infections when visiting someone in the hospital
Infections are illnesses that are caused by germs such as bacteria, fungi, parasites, and viruses. Patients in the hospital are already ill. Exposing them to these germs may make it harder for them to recover and go home.
If you are visiting a friend or loved one in the hospital, you need to take steps to prevent spreading germs.
The best way to stop the spread of germs is to:
- Wash your hands often
- Stay home if you are sick
- Use a face mask when directed or when infections may be transmitted through the air
- Keep your vaccines up to date
Hand Washing and Alcohol-based Hand Cleaners
Clean your hands:
- When you enter and leave a patient's room
- After using the bathroom
- After touching a patient
- Before and after using gloves
Remind family, friends, and health care providers to wash their hands when they enter a patient's room.
To wash your hands:
- Wet your hands and wrists, then apply soap.
- Rub your hands together for at least 20 seconds so the soap gets bubbly.
- Remove rings or scrub under them.
- If your fingernails are dirty, use a scrub brush.
- Rinse your hands clean with running water.
- Dry your hands with a clean paper towel.
- Do not touch the sink and faucets after you wash your hands. Use the paper towel to turn off the faucet and open the door.
You may also use alcohol-based hand cleaners (sanitizers) if your hands are not visibly soiled.
- Dispensers can be found in a patient's room and throughout a hospital or other health care facility.
- Apply a dime-sized amount of sanitizer in the palm of one hand.
- Rub your hands together, making sure all surfaces on both sides of your hands and between your fingers are covered.
- Rub until your hands are dry.
Stay Home If You are Sick
Staff and visitors should stay home if they feel sick or have a fever. This helps protect everyone in the hospital.
If you think you were exposed to COVID-19 , chickenpox, the flu, or any other infections, stay home.
Remember, what may seem like just a little cold to you can be a big problem for someone who is sick and in the hospital. If you are not sure if it is safe to visit, call your provider and ask them about your symptoms before you visit the hospital.
Anybody who visits a hospital patient who has an isolation sign outside their door should stop at the nurses' station before entering the patient's room.
Isolation precautions create barriers that help prevent the spread of germs in the hospital. They are needed to protect you and the patient you are visiting. The precautions are also needed to protect other patients in the hospital.
When a patient is in isolation, visitors may:
- Need to wear gloves, a gown, a mask, or some other covering
- Need to avoid touching the patient
- Not be allowed into a patient's room at all
Other Things You Can Do to Prevent Infections
Hospital patients who are very old, very young, or very ill are at the greatest risk for harm from infections such as colds and the flu. To prevent getting the flu and passing it to others, get a flu vaccine each year. To prevent getting COVID-19 and passing it to others, get COVID-19 vaccines according to current recommendations from the Centers for Disease Control. Ask your provider what other vaccines you need.
When you visit a patient in the hospital, keep your hands away from your face. Cough or sneeze into a tissue or into the crease of your elbow, not into the air.
Calfee DP. Prevention and control of health care-associated infections. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine . 27th ed. Philadelphia, PA: Elsevier; 2024:chap 261.
Centers for Disease Control and Prevention website. Infection control. www.cdc.gov/infectioncontrol/index.html . Updated November 18, 2022. Accessed October 20, 2023.
Review Date 10/13/2023
Updated by: Linda J. Vorvick, MD, Clinical Professor, Department of Family Medicine, UW Medicine, School of Medicine, University of Washington, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Health Facilities
- Infection Control
- Skip to main content
- Keyboard shortcuts for audio player
States pass laws to guarantee rights to visit patients, even during a pandemic

Stephanie Colombini
During the pandemic, nursing homes and hospitals often banned visitors, often for months. Although restrictions have eased, some states are passing "right to visit" laws for future pandemics.
AYESHA RASCOE, HOST:
Two years ago, hospitals and nursing homes banned visitors for months. As the pandemic continues, some facilities only allow visitors when COVID cases are low. A few states have now passed new laws to guarantee families a right to visit, even during a pandemic. And more states may follow suit. Stephanie Colombini of member station WUSF has this report.
STEPHANIE COLOMBINI, BYLINE: Jean White's mother has dementia. She moved her mom into a memory care facility near Tampa in early 2020, right before lockdowns began. The family tried video chats or just standing outside her window, but that upset her mom. Like many dementia patients, she couldn't grasp why she could hear familiar voices but not be with them in person. Finally, months later, the family was allowed in to see her. But White says the facility would keep shutting down any time a resident or staff member had the virus.
JEAN WHITE: What anxiety, loneliness and confusion she must have had. I think I would have rather her seen her family and taken the risk with COVID.
COLOMBINI: Restrictions on visitors helped protect residents from infection but may have harmed them in other ways. An investigation by the Associated Press found that for every two residents in long-term care who died from COVID, another resident died prematurely of other causes. The report came out in late 2020. It attributed some of those deaths to neglect. Others listed on death certificates as failure to thrive were tied to despair.
Mary Daniel of Jacksonville, Fla., is a patient advocate. When the pandemic began, she grew worried something like that would happen to her husband, Steve, who has Alzheimer's.
MARY DANIEL: I promised him when he was diagnosed that I would be by his side every step of the way. And for 114 days, I was not able to do that.
COLOMBINI: To get back inside, she decided to take a dishwasher job at her husband's assisted living facility just so she could see him during the first lockdown. She'd work in the kitchen two nights a week, then after her shift, go to his room. She'd help him change into his pajamas and then lay beside him, watching TV until he fell asleep.
DANIEL: That is really why I'm there, to be his wife, to hold his hand so he feels that love.
COLOMBINI: Daniel started pushing Florida to order long-term care facilities reopen to families that fall. She's been a champion for visitation rights ever since as leader of the group Caregivers for Compromise.
DANIEL: We understand that COVID kills, but we want to be sure that everybody understands that isolation kills, too.
COLOMBINI: At least eight states have now passed laws to allow visitation even during health emergencies. Some are specific to long-term care. Others include hospitals. To protect patients, these laws direct facilities to establish infection control measures that families must follow in order to visit. That could mean masks or health screenings. And they can ban visitors who don't follow the rules. That's fine with Daniel.
DANIEL: We want to protect their health. We want to be sure that everything is safe.
COLOMBINI: The federal government recently required nursing homes across the country to allow visitors at all times, with rare exceptions. But that doesn't apply to hospitals or assisted living. Veronica Catoe heads the Florida Assisted Living Association. She fears new state laws mandating visitation won't give facilities the flexibility they need to respond to crises.
VERONICA CATOE: These operators are trying to protect not only the loved one that wants to visit but also the loved one that doesn't want these outsiders coming in. And they both have resident rights.
COLOMBINI: Mary Mayhew is president of the Florida Hospital Association. She says patients go to hospitals because they're already sick or injured. That makes them vulnerable to infection.
MARY MAYHEW: There is significant risk of any of those patients getting exposed to, in this case, COVID, that might be brought in by a visitor.
COLOMBINI: Mayhew says families are vital to patient care. She says throughout the pandemic, hospitals have always tried to get relatives in, especially when people were dying, even during case surges and lockdowns. But for some families, that wasn't enough.
KEVIN RZESZUT: By the time we saw him, I mean, he was gone.
COLOMBINI: Kevin Rzeszut's father died from a bacterial infection in August, when Tampa hospitals were overwhelmed by the delta surge. Rzeszut couldn't visit his dad for nearly two weeks. Finally, doctors told the family to come say their goodbyes. His 11-year-old son went with him.
RZESZUT: And I think the worst part for me was that my son got to see him, you know, just hooked up to a bunch of machines and totally out of it. Like, that was it.
COLOMBINI: Rzeszut says his family continues to feel guilty that they couldn't visit his dad sooner. What he really wishes is that more people took COVID seriously so people didn't need a law to visit their loved ones.
For NPR News, I'm Stephanie Colombini in Tampa.
RASCOE: This story comes from NPR's partnership with WUSF and Kaiser Health News.
Copyright © 2022 NPR. All rights reserved. Visit our website terms of use and permissions pages at www.npr.org for further information.
NPR transcripts are created on a rush deadline by an NPR contractor. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of NPR’s programming is the audio record.
clock This article was published more than 2 years ago
Hospitals are still limiting visitors due to covid. Here’s what you need to know.

If nurse Joseph Falise could impart one tip to those with a loved one in the hospital nowadays, it would be to call ahead and confirm the visitation policy. Most hospitals still have tighter pandemic-related rules throughout their facilities, not just on covid wards. At University of Miami Hospital and Clinics, where Falise works, for example, only one visitor is permitted per day . When other family members or friends show up, he said, “It’s like a surprise attack when we say, ‘I’m really sorry, but you can’t come in.’”
Nearly two years into the pandemic, keeping up with visitor restrictions is one more stressor for already anxious friends and family of hospital patients. In addition to limiting visitors, some hospitals have shortened visiting hours, restricted visitors to one for a patient’s entire stay, and closed lobbies and other public places. (Some loosen certain restrictions if a patient is in hospice care.) Some hospitals also require all visitors to be vaccinated.
The University of Miami hospital’s policy has changed numerous times throughout the coronavirus pandemic, said Falise, the nurse manager in the cardiovascular and neuroscience ICUs. And “there’s a hospital across the street that's doing it differently than we are.”
There is no standardized visitation policy for hospitals in the United States. Restrictions on visitors are typically determined by the hospital’s administrators and patient family advisory council, said Robyn Begley , senior vice president of the American Hospital Association and CEO of the American Organization for Nursing Leadership. “The safety of the patient, safety for visitors and family members, and safety to the staff are always factors” that influence policies, she said.
“On top of that,” she added, “there’s local government mandates right now. So, there are safeguards that every hospital examines in the determination of what their visitation policy is, and it gets revisited depending on what’s happening regionally.”
What Black and Latina women need to know about dementia
Throughout the pandemic, some experts and patients have pushed for less restrictive visitation policies. A study published in April in the Patient Experience Journal found that quality of care suffers when hospital visits are limited. The researchers hypothesize that a lack of advocates might lead patients to feel less acknowledged in their care, and the lack of third-party observers could lead to less safe care.
“Families of patients serve two roles: emotional and as an advocate,” said Anthony C. Stanowski, a study co-author and president and CEO of the Commission on Accreditation of Healthcare Management Education. Visiting family members “are the best source of patient information and patient comfort, and have a vested interest in the well-being of the patient,” he said.
Falise said he has supported open visitation in the past, “because having your family members bedside has been proven to decrease mortality and increased patient satisfaction.” But, he added, “Hospitals are really good-intentioned on this. The reality is, we have to adjust to the times.”
Here are some tips for visitors dealing with covid-era hospitals rules and advice for being the best advocate possible — especially if that responsibility falls entirely on one person.
If it’s a planned admission, have a serious conversation ahead of time. Find out the hospital’s visitation policy by calling or checking its website, Falise said. You can then have a discussion about who will be the primary visitor and set expectations by letting other family members know. This is also a good time to find out “exactly who among the family the patient would want to have information shared with,” said Nancy Foster, AHA’s vice president of quality and patient safety policy, and whether they have an advanced directive that stipulates what type of medical measures they would want.
Expect to wait. All visitors need to be checked in, and it can take some time. If you come at the beginning of visiting hours you might find yourself in a long line outside the hospital.
Prepare in advance for talks with the doctor. Have questions written down, so you’re not caught off guard when a doctor comes in, said Kati Kleber , a nurse educator based in Urbana, Ill. and author of “ Admit One: What You Must Know When Going to the Hospital, But No One Actually Tells You .” Keep a running log of questions as they pop up; you could even store them in a Google doc accessible to family members who are unable to visit. If you want another person to also hear the doctor’s updates, “you can always call and put them on speakerphone,” Kleber said. “However, I recommend giving family members a heads-up to be near their phone and ready to answer if you call,” because provider schedules are unpredictable, and you won’t be able to plan a specific time.
How technology can help seniors beat loneliness and isolation
Some hospitals, such as University of Miami, have teams of nonclinical workers who act as a liaison between patients and their families, passing questions to the doctors and information to loved ones at home.
Ask about proxy access to the patient’s medical records. At Cleveland Clinic, a patient’s loved ones can be granted proxy access “so they can see what’s going on with test results,” said Stephanie Bayer, the hospital’s senior director of patient experience. “It’s the same point of view you would see if you were looking at your own record, and it helps keep people informed.” Ask a nurse to walk you through the options, and note that the patient will need to approve this access.
Get in touch with the hospital social worker. Advocating for a loved one in the hospital will almost definitely be confusing and overwhelming, said Ivelyse Andino , founder and CEO of Radical Health, which helps people with issues such as understanding health care rights. She suggests seeking out a social worker or patient navigator, who are professionals “provided by the hospital to help connect you with resources and support.” These folks can help you make sense of treatment options and prepare an at-home discharge plan, plus ensure you don’t burn out while caring for your loved one.
If you can’t visit, find other ways to show a patient you’re thinking about them. “There’s text, there’s FaceTime, there’s Zooming,” said George F. Blackall , a pediatric psychologist at Penn State Health Children’s Hospital in Hershey, Pa. “Offering to connect in that way is really helpful, particularly with adolescents.” Prioritize silly or lighthearted messages that might spark a patient’s first laugh of the day.
Gifts are almost always welcome, so long as there’s enough space in the room — just check first with whoever is spending time there. One idea: You could present the patient with a digital photo frame; “people just need the email address, and they can send photos that rotate on the display,” Kleber said. That can help brighten a patient’s days and remind them of those they’ll hopefully see soon.
If you’re visiting a senior, it’s especially important to advocate. You’re an essential part of your family member’s care team, said K. Andrew Crighton , an advisory board member at Family First , which offers caregiving benefit plans for employees. Let the doctors know if a patient has a hearing, visual or cognitive impairment, he said, in which case “your role becomes more critical.” (Sometimes visitation exceptions are made in those situations.)
Follow the rules. Whether it’s wearing a mask, practicing social distancing, leaving at a certain time, or not roaming the halls or loitering in the lobby, do what the hospital asks, Bayer said. Flouting the rules is not helpful to anyone. And don’t take out your frustration on the staffers who must implement a policy they did not draw up.
Be kind. Hospitals across the nation are dealing with staffing shortages. “This is a very challenging time for all our clinicians,” Begley said, calling for “a little extra patience.” Speaking of which: Say thank you. There’s no need to send the health-care team a gift, but “taking a minute to say, ‘I see you and appreciate the work you’re doing’” goes a long way, Bayer said. “It helps when people notice that we’re working hard.”
If you’re not able to visit, help out in other ways. During the pandemic, it’s likely that only one or two people are doing most of the visiting. You can help by doing grocery shopping, bringing them meals, offering to drive them to and from the hospital, and taking care of what needs to be done at the ill person’s house. “Things like walking their dogs, cleaning their house, doing laundry and paying for their parking can go a long way,” Kleber said.
Consider setting up a website to keep others informed. There are lots of “really great communication tools,” like CaringBridge , that allow friends and family to document a loved one’s health journey, Bayer said. These sites are typically so easy to use that they don’t add much stress to a patient advocate’s life, she notes — plus, someone other than the primary visitor could be designated to post updates.
Take care of yourself. Spending long days advocating for — and worrying about — your loved one will inevitably take a toll. “One of the things people forget to do is take care of themselves,” Bayer said. “So that means make sure you’re sleeping, make sure you’re eating. We need to keep ourselves resilient.” Many hospitals offer some form of spiritual care, she adds; seek it out if that would be helpful to you. And know that what you’re doing is important. “We recognize that family members are vital components of the patient’s healing,” Bayer said. “The love and support that patients get from their family and their visitors does help them and motivate them and keep them on the track of progress.”
Angela Haupt is a freelance writer and editor. Follow her on Twitter: @angelahaupt .
- Anti-aging ‘superfoods’ aren’t enough. Try one of these healthy overall eating plans. December 17, 2021 Anti-aging ‘superfoods’ aren’t enough. Try one of these healthy overall eating plans. December 17, 2021
- Thousands who ‘followed the rules’ are about to get covid. They shouldn’t be ashamed. December 22, 2021 Thousands who ‘followed the rules’ are about to get covid. They shouldn’t be ashamed. December 22, 2021
- Do dreams mean anything? Why do I feel like I’m falling? Or wake up paralyzed? We asked experts. December 30, 2021 Do dreams mean anything? Why do I feel like I’m falling? Or wake up paralyzed? We asked experts. December 30, 2021

UW Health recently identified and investigated a security incident regarding select patients’ information. Learn more
- Find a Doctor
- Conditions & Services
- Locations & Clinics
- Patients & Families
- Refer a Patient
- Refill a prescription
- Price transparency
- Obtain medical records
- Clinical Trials
- Order flowers and gifts
- Volunteering
- Send a greeting card
- Make a donation
- Find a class or support group
- Priority OrthoCare
- Emergency & Urgent care
University Hospital and East Madison Hospital : Patient and Visitors Guide
Preparing for your visit
We're honored to care for you
If you have any questions, compliments or concerns about your care or safety as a patient of UW Health, we encourage you to talk with your doctors and nurses. If you feel your concerns are not adequately addressed, please contact Patient Relations using our form or by calling (608) 263-8009 .
Patient guides
To view a pdf version of the patient guides, please select from the following:
University Hospital Patient and family guide (pdf)
Guía para los pacientes y sus familias (pdf)
East Madison Hospital Patient and family guide (pdf)
Additional patient guides
American Family Children's Hospital Patient and family guide (pdf)
SwedishAmerican Hospital
When you arrive
Preparing for your hospital stay or visit
University hospital, valet services and patient drop-off.
Valet services are open for golf cart parking assistance, Monday-Friday, 5:30 a.m.-5 p.m.
Patients can be dropped off and picked up at the front entrances, Monday-Friday, 6:30 a.m.-5 p.m.
Wheelchair assistance is available
East Madison Hospital
Patient drop-off.
Patients can be dropped off and picked up at the front entrance
Call Guest Services for any assistance: (608) 440-6242
Parking is available in parking ramps or parking lots.
Parking is available in front of the facility. Additional parking is available in the parking ramp on the east end of the facility.
Madison Metro Bus Service Route 26 might be operating reduced schedules. Please visit cityofmadison.com/metro/schedules
One primary visitor per patient receives complimentary parking. For assistance, please visit an information desk, 2nd floor (Main Street), 7:30 a.m. - 9 p.m.
RVs can park for free in Lot 131, located on University Bay Drive. Electricity is provided. To obtain an RV pass, please go to one of the information desks or call (608) 263-0315 .
During your stay
Services and amenities for a comfortable stay

A space to promote healing
A healing environment for rest and recovery
If you are feeling stressed by being in the unfamiliar environment of a hospital or by life events, please talk with your care team or check out online resources that are available.
If noise is a problem, please speak to your nurse about options to minimize sounds, such as requesting a sleep kit, wearing earplugs or listening to peaceful nature sounds on your television.
Pain control and comfort options
Preventing and managing pain can help you get well faster
This can help you enjoy greater comfort and improve results of your care. If you are feeling pain from lying in a hospital bed, please talk with your nurse or care team how to be more comfortable, such as:
Extra pillows for neck, knees, ankles
Fan or sound/white noise machine
Machine that stimulates nerves (TENS unit)
Warm pack/cold pack (heat/ice) or warm blanket

Passing the time
Things to do during your time with us
To help pass the time, you can watch mindfulness activities, games, movies or listen to music on MyChart Bedside.
Our gift shops can deliver these items to your room:
Books and magazines
Coloring books, notepad, pen
Crossword puzzles and Sudoku
Deck of cards

University Hospital's outdoor rooftop gardens and patios:
1st floor: Atrium Patio, located at J3/1
1st floor: Health Sciences Learning Center patio, located past the K elevators
3rd floor: Patio, located at C4/3
4th floor: Hilary Grace Healing Garden, located at E4/4

UW Health East Madison Hospital outdoor rooftop gardens and patios:
1st floor: East Wing Turf-side Patio
2nd floor, Bistro Rooftop Patio
Internet access, television and movies
UW Health facilities provide complementary internet access during your stay. Connect your smartphone, tablet or laptop to "UW Health Guest"
Watch movies, television shows or one of our relaxation channels. Our streaming movie service allows you the flexibility to start, pause or stop programming around your schedule. Please set your television volume at a comfortable hearing level so as not to disturb other patients. Most patient rooms have televisions equipped with closed captioning. If you require assistance, please ask your nurse.
Watch on your bedside tablet
On your MyChart Bedside tablet, open the MyChart Bedside app
Login to MyChart Bedside with your PIN
From the menu on the left, tap "Watch Movies"
Browse movies, television shows or other content and tap to start
Watch on your personal mobile device
Connect to "Free WiFi UW Health" on your smartphone, laptop or personal tablet
Download the "Swank Media Player" app from iTunes or Google Play store
Open your web browser (Chrome, Safari, Firefox, etc.), type swank.uwhealth.org in the URL text box and click enter
Watch on your television
Local and cable channels are listed on Channel 1.
Therapeutic and peaceful TV channels
To help you rest and recover, you might prefer to watch or listen to peaceful and comforting TV channels instead of regular TV programming.
View a listing of our channels (pdf)

Patient meals and room service
Providing a quality stay or visit

East Madison Hospital and University Hospital and American Family Children's Hospital room service dining menu features made-to-order, freshly prepared food, allowing for more personalized service.
Please check out the patient and family guides for the room service menus:
Every surface in your room has been thoroughly cleaned with hospital-grade cleaning products. We also use a UV disinfection robot to make sure your room is germ free — from top to bottom.
If your room needs cleaning, it is too hot or cold or if a feature of your room (television, bed, lights, etc.) does not work properly, please talk with your nurse or call:
East Madison Hospital: (608) 444-4055
University Hospital: (608) 263-1260
Information for visitors
Visits from family and loved ones
Visiting hours.
View our UW Health visitor guidelines for the latest updates including visiting hours.
Virtual visits
Family and loved ones provide emotional support and comfort to you. Even though we are limiting the number of visitors in the hospitals, we encourage you to stay in touch virtually with friends and loved ones. We are pleased to offer Webex Meet (Virtual Visitor) technology if you do not have a personal device or if you want a secure, private connection that allows your family to be involved in your care. You can access Webex Meet from your MyChart Bedside tablet. Please talk with your nurse.
We will provide your room number and phone number to people who call the hospital’s information desks. Please tell us if you do not want this information released.
Learn how to use a virtual visit with the Visitor Quick Reference Guide for Webex Meet (Viritual Visitor) (pdf) | Guía de referencia rápida para Webex Meet (Visita Virtual) (pdf) .
Your healthcare team
Working with your healthcare team
Our healthcare team members partner with you to achieve the best possible outcome for your care. We want you to feel informed and cared for during your hospital stay. If you have questions about the roles of your care team, or wonder why certain medicines, tests or therapies are being ordered, please ask us.
UW Health is a teaching hospital. Our faculty physicians provide patient care and often conduct leading-edge research to improve medical care. They also serve as teachers and mentors for medical students and residents to train the next generation of doctors.
Different care team members may ask you to answer many of the same questions. The information you provide is essential in helping us provide the best and safest care for you, and we thank you for your patience.
Your care team and their roles

You and your family
Your primary support person can be a family member, partner or friend, at least 18 years old, who provides you with significant emotional support.
Your nurse is your main caregiver and point of contact.
Nursing assistants work alongside your nurse to ensure you receive all of your care.
Your providers (doctor, nurse practitioner or physician assistant) partner together and provide care on your treatment plan with input of other care team members.
Health unit coordinators (HUCs) assist with communication between you and your healthcare team.
Hospitalists are physicians who specialize in internal medicine and the general medical care of hospitalized patients.
Medical interpreters
Nurse case managers assist your healthcare team to develop a discharge plan of care and arrange for home care, medical equipment or therapies outside of the hospital.
Social workers provide support to help you with the stresses associated with sudden and chronic illnesses and their impact on everyday life.
Patient care technicians are certified nursing assistants who work alongside your nurse to ensure you receive all of your care.
Pharmacists review your medicines and teach you how to take them properly so you get the best results.
Registered dietitians help you learn what foods and beverages promote healing and recovery as well as meet your nutritional needs based on your personal health concerns.
Therapists are skilled in specialized treatments help you develop skills to recover from illness or injury.
Various support services including environmental services, security, culinary, patient access, guest services, materials management and others also partner with your care team to ensure your stay meets your expectations.
Care team visits
Every day, your care team will discuss your goals, answer your questions and confirm next steps in your healthcare plan (tests, treatments and discharge plans). To limit the number of staff in the hospital and in your hospital room, your care team may meet virtually. Family can also be involved virtually in care team visits using Webex Meet technology. Please ask your nurse for assistance.
Please have your medication schedule available (see MyChart Bedside or ask for a printout), keep us aware of any sensitive issues and write down questions as you think of them so you can discuss them all with your care team.
You and your family members may be the first to notice a change in your condition. Please tell nursing staff if there is a change in your condition, such as high or low blood pressure, high or low heart rate, breathing problems, chest pain, facial droop, arm or leg weakness, problems speaking, new or increased confusion or inability to waken.
To ensure your safety, every time there is a change of shift, the off-going nurse will introduce you to the on-coming nurse. Together, both nurses will perform a safety check that includes a brief summary about your medical condition and a review of equipment and medications.
MyChart Bedside Gives you and your designated caregivers access to real-time information about your health, your care team, and what to expect during your hospital stay. Please talk with your nurse to request a tablet or if you need assistance.
UW Health MyChart
You may request copies of your UW Health medical records, radiology images and pathology reports and slides. Forms are available at check-in desks or at uwhealth.org/medical-records
Everyone is at risk for falling while in the hospital: Call, don't fall.
Before getting up, please check with your nurse first about assistance you may need.
Honoring your healthcare wishes
Completing advance care planning and an advance directive can give you and your loved ones the peace of mind that your current and future healthcare preferences are known and will be honored if you are not able to make decisions for yourself or not able to communicate your wishes. Advance directive forms are available online or staff can provide them for you.
Learn more about advance care planning
Email [email protected]
Call (608) 821-4144
Expressing gratitude
Some people find expressing gratitude to be emotionally healing as they reflect on challenging experiences.
Patients and families often ask how they can express their gratitude to our providers and staff. We appreciate your kindness and offer several ways that you can recognize members of our UW Health team.
If you wish to recognize: Physicians You may submit a message for a physician for National Doctors’ Day, which is celebrated annually on March 30.
You may submit a nomination for a DAISY award , which is presented monthly.
Nursing assistants
You may submit a nomination for a Sunshine award , which is presented monthly.
Medical assistants
The Sunflower award recognizes medical assistants for extraordinary care.
Respiratory therapists
You can nominate a respiratory therapist for a PHIL award for exceptional care.
UW Health staff or providers
You may submit a note of appreciation for our patient experience recognition program . This is a great way to recognize any provider or staff member year-round.
Thank you for taking the time to recognize our remarkable providers and staff – in your own words, which is especially meaningful.
To make a donation For those interested in making a philanthropic gift to support the care, research or services at UW Health, there are many ways to give .
Support services
Services to support your health and healing

A chaplain can provide a supportive, caring and compassionate presence to you and your family, especially during worrisome times of being in the hospital. We respect the spiritual beliefs and needs of everyone. Call (608) 263-8574 if you would like to talk with our chaplains or have us contact your faith leader.
You can find a wide array of gifts for all ages at our gifts shops. You can place orders for delivery of personal care items, such as phone chargers, reading glasses, toothbrushes, postage stamps and more. Visit the Flowers and Gifts main page for hours and information.
University Hospital: (608) 263-6472
East Madison Hospital: (608) 440-6244
Mendota Market is University Hospital's on-site convenience stories with groceries and convenience store items, prepared food, beverages, specialty teas and Starbucks, Barriques and Cadence Cold Brew coffee on Nitro Tap. The Mendota Market might have limited hours or be closed temporarily due to COVID-19; signs will be posted in any affected areas.
University Hospital, 1st floor, near the cafeteria, open overnight - hours could be altered due to COVID-19 safety measures.
We are pleased to offer a "patient and family rate" at the Best Western Plus InnTowner hotel near University Hospital and hotels close to UW Health at the American Center. Reservations must be made through UW Health Guest Services by calling:
University Hospital: (608) 263-0315
East Madison Hospital: (608) 440-6242
Medical bills from an unexpected accident, illness or hospitalization can cause financial stress. If you find yourself without a plan to pay medical expenses, our financial counselors will help you understand and manage your UW Health bills.
We can assist you with setting up payment plans, providing estimated costs for upcoming services, exploring other coverage options such as governmental programs or plans on the Healthcare Marketplace, and if applicable, applying for UW Health's Financial Assistance Program.
Please contact us if you have questions about your health insurance coverage, your medical bills, or if you would like to discuss payment options or financial assistance.
Billing and Insurance
Phone: (877) 565-0505
Mail: Please include the account number shown on your billing statement
University Hospital 600 Highland Ave. H6/220 Madison, WI 53792
- Skip to main content
- What are my care options and their costs?
Where to go for medical care
When you need medical attention, knowing where to go for health care can help you save time — and help assure you'll get the care you need. You may choose care from your primary care provider (PCP), a virtual visit (or telehealth), urgent care or emergency room, depending on your situation. Here are tips to help you choose where to go for care.
Consider your medical need
Where you go for care depends on what kind of medical care you'll need. Look at the examples in the chart below to get a sense of the options you may choose.
Tell your PCP about care you received
If you receive urgent or emergency care, It's important share information with your PCP, including diagnoses, treatments, prescriptions and therapy recommendations. This will help your PCP make the best possible decisions about your ongoing health and well-being. It will also help with coordinating care between other providers.

Do you get your health insurance through work?
If you have an employer-sponsored health plan, 1 your care choices may help you save both time and money. Let's take a look.
Learn how choosing some care options may help you save up to $2,400. 2
Find out about your 24/7 Virtual Visits benefit if you have a UnitedHealthcare plan through work.
Learn the details about Designated Diagnostic Provider benefits and how it may affect your coverage for outpatient lab and major imaging services.

Watch and learn more about where to go for care
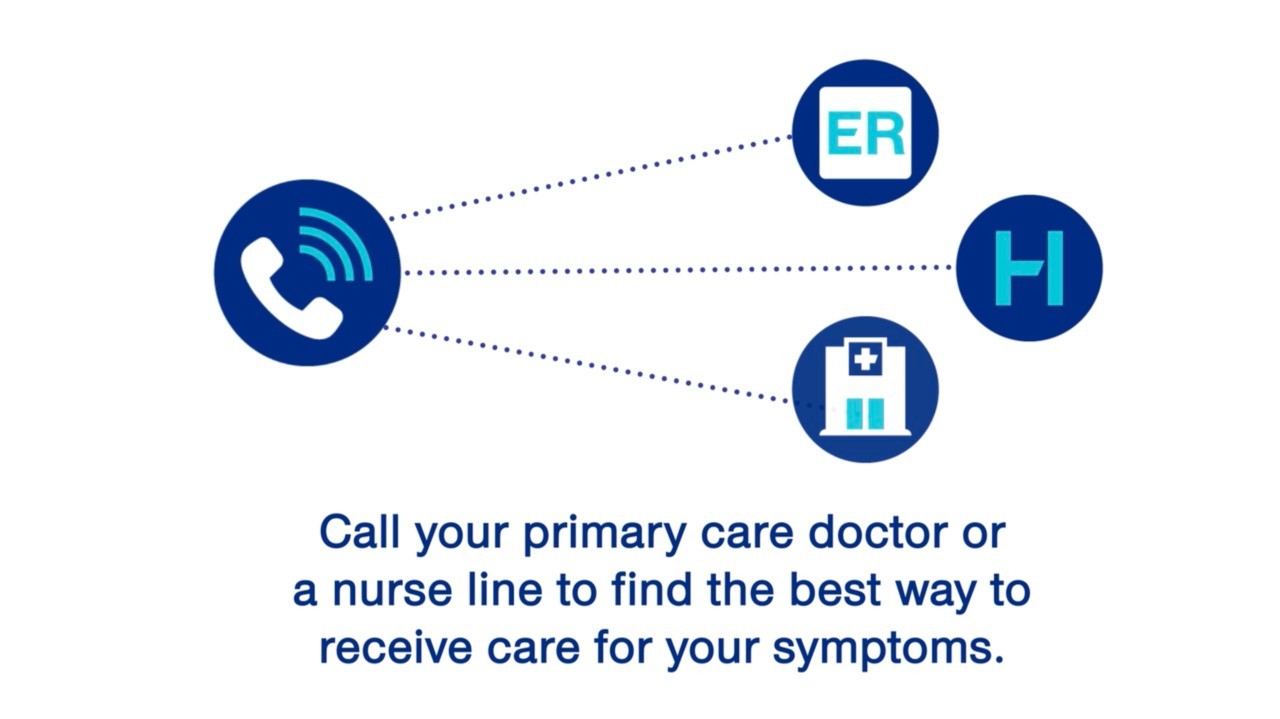
Whether you're walking home from work or sitting on the couch, feeling a sudden change in health can be upsetting. Some health conditions are serious, but it's important to keep calm and follow a plan. Watch this video to learn more about when to choose the ER vs another option.
How to choose where to get care
Video transcript
[ Video has no sound ]
Imagine you have a fever and need to see a doctor.
You could go to the emergency room, but you may find long wait times.
Also, you’ll meet with a doctor who doesn’t know your health history.
You can get the best quality care when your doctors work together.
Call your primary care doctor or a nurse line to find the best way to receive care for your symptoms.
You may even be able to chat with a doctor on your phone or computer for some basic prescriptions.
And see your primary care doctor to treat common health problems.
Call your health plan customer service to find a doctor or schedule a visit. The number is usually on the back of your card.
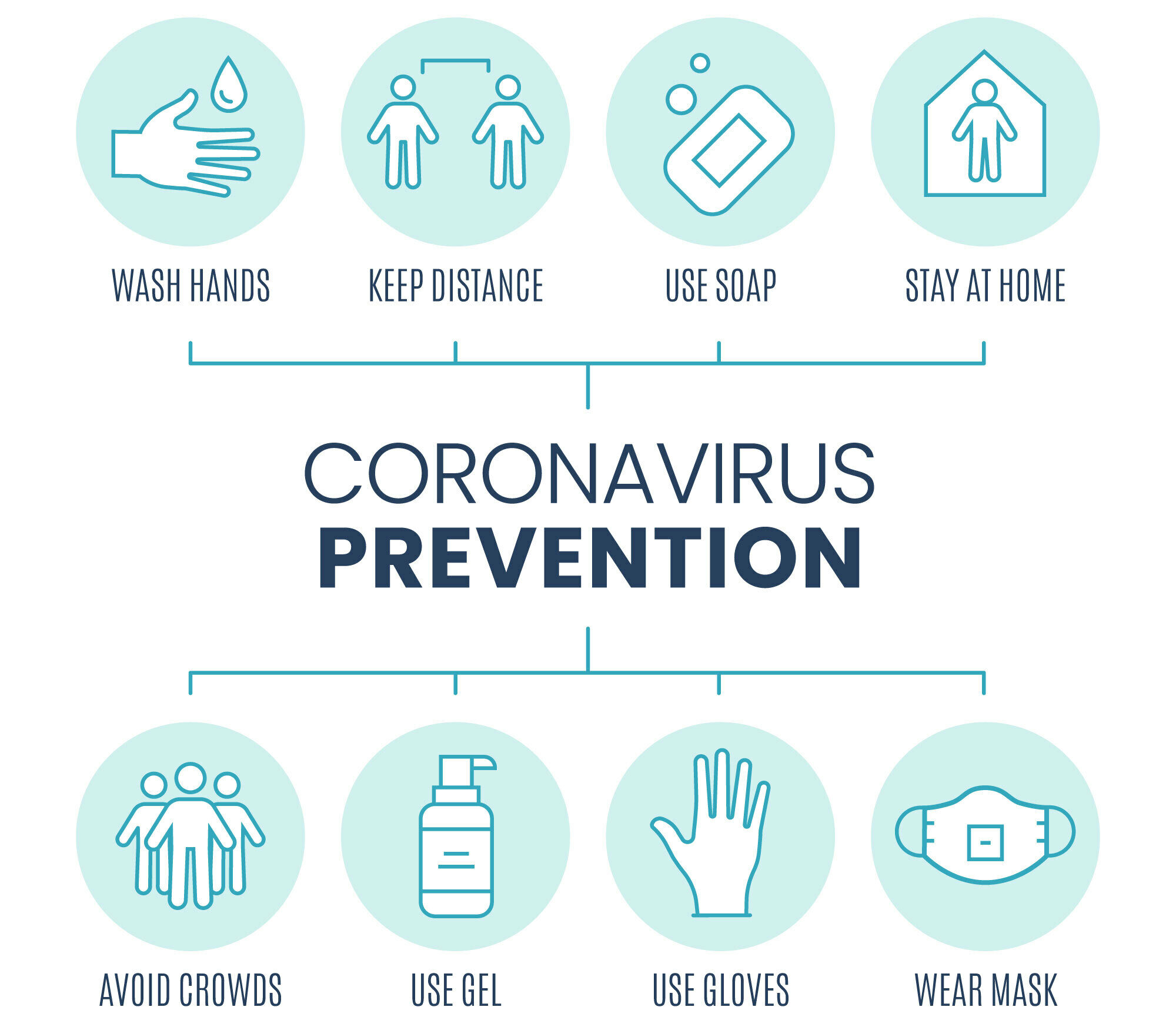
In light of COVID-19, remember to practice social distancing. Wash your hands often and wear a mask. Contact your care provider with questions about your visit.
UnitedHealthcare
ER Wait Time: 6 minutes | If you are having a medical emergency, call 9-1-1 .

Choose an option below for a customized menu.
- Healthcare Professional
- COVID-19 Information
- Find a Provider
- Medical Records
- MyChart - Patient Portal
- Job Opportunities
- Search Jobs
- Why Prime Healthcare?
- Volunteer Organization
COVID-19 Patient and Visitor Information
Your safety is our top priority.
Dear Patients, Families and our Community,
Thank you for choosing us for your health care needs. We are committed to providing a healthy and safe environment, and we recognize the important role that visitors and loved ones play in patient recovery. Our goal is to help patients’ rest and healing, while maintaining a safe environment for all.
Effective August 11, 2021, our visitor policy complies with the California Department of Public Health State Public Officer Order .
Per the Health Order, indoor visitors must show proof of vaccination or a negative COVID-19 test result.
Any one of the following may be used to show vaccination:
– COVID-19 Vaccination Record Card (issued by the Department of Health and Human Services Centers for Disease Control & Prevention or WHO Yellow Card – Photo of Vaccination Record Card as separate document – Photo of the visitor’s Vaccination Record Card stored on a phone or electronic device – Documentation of COVID-19 vaccination from a healthcare provider – Digital record that includes QR code that when scanned by a SMART Health Card reader displays the person’s name, date of birth, vaccine date(s) and vaccine type
* If partially vaccinated or unvaccinated, visitors must show a negative COVID-19 test result from within the past 72 hours. * All visitors are required to wear well-fitting, surgical or double cloth masks.
Patients whose visitors are exempt from this order: patients in critical condition or in end-of-life care, maternity patients in labor, pediatric patients age 17 and younger and patients with disabilities
Frequently asked questions for visitors (FAQ) can be viewed here.
We encourage everyone who is able to become fully vaccinated to ensure your safety, the safety of others and to help stop the spread of COVID-19. Vaccines are available at no cost and have undergone stringent testing and continue to undergo intense safety monitoring. Click here to find a vaccine near you .
Patient care requires teamwork; our staff works together with family and loved ones to help our patients heal in a safe, comfortable space. Thank you for your understanding and cooperation with these guidelines and helping us maintain a healthy, respectful and restful environment.
Please continue to check our website for updated visitor information.
You may be concerned about news of the novel coronavirus (COVID-19), and its implications for your health and those of your loved ones. Your safety and well-being are our top priority.
Please know that:
- We are taking all necessary measures and precautions to protect the safety of our patients and staff.
- We specialize in the care of patients with complex illnesses and have experience with managing and containing novel viruses.
- This is a rapidly evolving situation and we suggest you check out the latest updates on the CDC website as well as the website of your state health department .
- Our hospital has adopted and put in place California Crisis Care Continuum Guidelines that, together with our own hospital policies and operational plans, serve as a framework for emergency management planning during this COVID-19 pandemic. You may also download the guidelines here .
- Extenuating circumstances will be evaluated.
- Hospital entry points will be limited to enable the cease of visitors. Those who are able to visit due to extenuating circumstances, but who show any signs of illness, including mild symptoms, should not visit patients in the hospital or accompany patients to the emergency department.
- Please dial 714-827-3000 for any questions.
Visitation Guidelines
- Facility visiting hours are 8:00 AM to 8:00 PM, in all patient care areas
- Visitation will be limited to 2 visitors per patient
- Visitation will be suspended for COVID-19 patients
- Children under 13 years may visit at the discretion of the charge nurse
- The Subacute unit will continue to abide by CDPH patient visitation parameters for Skilled Nursing Facilities.
- All visitors must wear a face mask at all times
- Visitors will be screened prior to entrance
ER Visitation Guidelines
- Visitation will be suspended to COVID-19 patients
- ER visitors will be asked to remain in the designated waiting areas
- For cardiac events requiring invasive procedures, we ask that you wait in the waiting room. The Surgeon will contact you in that area
- Anyone entering the premises will be screened
Behavioral Health Services
Visiting Hours:
- Monday – Friday 12:00 p.m. – 2:00 p.m. and 6:00 p.m. – 8:00 p.m.
- Saturday & Sunday 12:00 p.m. – 2:00 p.m. and 4:00 p.m. – 8:00 p.m.
All visitors sign in and out upon arrival and departure and will agree to keep confidential the names and situations of other patients on the unit.
Frequently Asked Questions about the Novel Coronavirus
What is our hospital doing to protect patients?
- We are screening patients with symptoms of fever, cough or shortness of breath and with a history of travel within the past 14 days to communities with widespread or sustained community transmission of the coronavirus.
- If we have a confirmed or potential patient with COVID-19, we will institute standard infectious disease protocols, as well as additional measures, to prevent the potential spread of the virus. All healthcare providers who have contact with the patient will use appropriate personal protective equipment (PPE), following U.S. Centers for Disease Control and Prevention (CDC) guidelines.
How concerned should I be about the coronavirus?
- As of now, the seasonal flu remains a significant health risk.
- Coronaviruses can cause the common cold and pneumonia. Most people infected with the novel coronavirus have mild cold symptoms. A small fraction of people, however, may require more intensive care. We understand your concern about protecting yourself from respiratory diseases.
- We have launched an online self-checker for the novel coronavirus in the form of a bot nicknamed Robby. Robby walks users through symptoms and then gives recommendations if medical care is needed. Robby is not intended to be used for diagnosis or treatment purposes. Click the blue “Start Self-Check Assessment” button to launch the self-checker:
Start Self-Check Assessment
- Keep informed of the risk by checking the situation update on the CDC website.
What can I do to protect myself?
It is understandable to feel uncertain or anxious during a public health crisis, and we need to remember to avoid making assumptions about others’ perceived symptoms or any characteristics of identity.
Here are the current CDC recommendations to help prevent the spread of respiratory viruses:
COVID-19 vaccines are effective at protecting you from COVID-19, especially severe illness and death. COVID-19 vaccines reduce the risk of people spreading the virus that causes COVID-19. If you are fully vaccinated, you can resume activities that you did before the pandemic. Learn more about what you can do when you have been fully vaccinated.
- Take everyday preventive actions for respiratory infections, such as avoiding close contact with people who are sick, staying home when sick, and washing hands often.
- Avoid traveling to places with widespread or sustained community transmission of the coronavirus. A good place for reliable travel information can be found on the CDC’s travel advisory page .
Should I wear a mask?
CDC recommends wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain (e.g., grocery stores and pharmacies), especially in areas of significant community-based transmission.
Where can I learn more?
Concerned patients and family members should talk with their healthcare provider .
You can also find more information about the virus from these websites.
- CDC/Centers for Disease Control and Prevention . (updated daily with advice for the public)
- Find the latest on the CDC website as well as the website of your state health department .
- World Health Organization .
- U.S. Occupational Safety and Health Administration .
What is our COVID-19 Testing Cash Price?
The current cash price for Hospital COVID-19 Testing is $275.

- Prepare for Doctor Visits and Make a List of Questions
Prepare a list of questions and symptoms before you visit your doctor or go for a procedure or to the hospital. A doctor won’t be able to answer your questions if you don’t ask.
Bring a List of Questions
Do you ever get home from a doctor visit and suddenly think of a burning question you wish you’d asked during your visit an hour earlier? This is the case for a lot of people. It helps to think ahead of time about the reason for your visit and what you hope to get out of it. Talk it over with a friend or family member. You may find yourself with a list of questions. Bring them to your appointment and jot down the answers.
Learn more in this Take 5 podcast as Lisa DiBlasi Moorehead discusses why it’s important for a patient to play an active role in their care and be open and honest about symptoms, what to bring with to provider visits and what do to after a visit. Lisa DiBlasi Moorehead, EdD, MSN, RN, CENP is the Associate Nurse Executive in the division of Accreditation and Certification Operations at The Joint Commission.
Preparing for Virtual Visits
In today’s new normal, preparing for a doctor’s visit may look a little different and require additional preparation. As COVID-19 increases social distancing across the U.S., it’s no surprise that virtual medical appointments have seen a huge spike in popularity. Telemedicine isn’t new, but it’s been utilized more than ever during this stressful time of quarantine and self-isolation. Here are some ways to plan for a successful virtual visit.
In Person Visits
Health care facilities, such as hospitals, doctors’ offices, surgery centers and all sites of care are reopening as appropriate, and as state and local conditions allow. Precautions are being taken to ensure your care is safe and that you are protected. Patients should have confidence in seeking care, and trust that your health care providers are doing their best to keep you, your family, and your community safe. Therefore, you should not postpone necessary care or preventative care such as immunizations or cancer screening. Do not hesitate to reach out to your provider if you have any questions about when to seek treatment.
To prevent you from getting COVID-19, or giving it to others, you may be asked to do the following by your provider:
- Wear a face covering. This helps limit your risk of getting or spreading COVID-19.
- Avoid crowded waiting areas. Some practices may require patients to check in for their appointment from their car. You may be asked to wait in your car until your visit. Waiting rooms should have chairs spaced far apart to keep you and others safe.
- Limit visitors or people who go to your appointment with you. Be prepared that you may not be allowed to bring anyone with you and if you typically accompany an elderly family member, you may be asked to wait in the car. Limiting the number of people limits your exposure. Visitors should also wear a face covering.
- Screening before entering a facility. Your temperature may be taken, and you may be asked to use hand sanitizer and wear gloves. The office may call you a few days before your appointment to go over some screening questions. This means asking questions about your possible risk factors of having COVID-19. They may repeat these questions during your visit. You may also be asked additional information over the phone to reduce the amount of paperwork needed at the time of visit.
Discuss with your provider if you should get tested before going in for care. In some cases, such as before surgery, childbirth, or a procedure, it may be necessary to be tested for COVID-19.
Resources and Tools:
- Share symptoms with your doctor (STARS tool)
- Speak Up About Your Care
- Speak Up At the Doctor’s Office
- Visit the TakeCharge website
- Take 5: The TakeCHARGE Campaign’s 5 Steps to Safer Health Care – Preparing for Provider Visits
- Understand and Complete Your Advance Directives
- Keep a Record of Your Medical History and Current Medications
- Prevent Infections and Ask Caregivers to Wash Their Hands
- Use an Advocate or Be an Advocate for Others
- A- A+
The Gift of Presence: Tips for Visiting a Terminally Ill Family Member or Friend

You may think: “I don’t feel like I am doing anything.” … “The person is asleep, or falls asleep, during my visit. Should I wake them? Should I stay?” … “What should I be doing?” … “Am I helping?” or “What should I say to the person?”
Your presence does make a difference. It can be difficult to be with someone who is terminally ill; it isn’t always clear what to do, or say. Intention is everything. The person will sense your tone, pace of the visit and more. If your visit is intended to make the person feel encouraged, cared about, or put a smile on his or her face, the person will sense it.
Below are several helpful suggestions about how to prepare for a visit and ideas to guide you during the visit:
- It’s so important to make sure you are in a place of peace before the visit. If you don’t feel calm, peaceful and centered, take some time to quiet yourself before entering the person’s home or room.
- Always approach the person slowly and quietly so as not to startle them.
- Introduce yourself with a quiet voice. “Hi, it’s your niece, Jane. I would like to sit with you for a while.”
- If you want, hold the person’s hand. Start by telling the person what you are doing. “Mary, I am going to hold your hand now.” Another option is to put the person’s hand on top of yours. That way if the person does not like touch, they can pull away.
- If the person has a book or newspaper by their bed, read it aloud.
- If the person appears to be in and out of sleep, that is okay. They will know they are not alone.
Although it’s natural to be concerned about what you’re going to say, don’t worry so much about the words. The main thing is that your message comes from the heart. It’s also important to remember to stop talking at times and simply listen to the person if he or she is able to communicate.
Here are a couple of tips to help you keep the visit authentic:
- Do say – “It’s good to see you.” Let them know you have been thinking of them.
- At a loss for words – It’s OK to say, “Mary, I don’t know what to say or do, but I’m here and I care about you.”
- Listen – If the person talks about being anxious, listen quietly. Don’t try to change the subject or silence the person. When he or she is finished sharing concerns, encourage him or her by asking, “What do you want to achieve now?” Then you can gently shift the focus of the discussion to that goal rather than the prognosis or condition. For instance, if a person says she wants to live to see her grandbaby be born, ask her how they will celebrate when the baby arrives. Try to keep the conversation positive.
- Chatter is overrated – Be present without saying a word. You don’t have to fill every moment of your visit with conversation. Just make sure you are focused on the person and not thinking about your next appointment or task on the “to-do” list.
About Hospice of the Red River Valley In 1981, Hospice of the Red River Valley was founded on the belief that everyone deserves access to high-quality end-of-life care. We fulfill our nonprofit mission by providing medical, emotional, personal and spiritual care, as well as grief support to our patients, their families and caregivers during a tender time in life. Our staff helps those we serve experience more meaningful moments through exceptional hospice care, 24 hours a day, 365 days a year, wherever a patient calls home. The organization serves more than 40,000 square miles in North Dakota and Minnesota , including in and around Bismarck, Detroit Lakes, Devils Lake, Fargo, Fergus Falls, Grand Forks, Lisbon, Thief River Falls, Valley City and many more communities. Hospice of the Red River Valley offers round-the-clock availability via phone, prompt response times and same-day admissions, including evenings, weekends and holidays. Contact us anytime at 800-237-4629 or hrrv.org .
Return to the blog homepage →
Other Articles that May Interest You

When someone you care about or love has been told they only have a few…

by Sharon Dardis, guest blogger Many caregivers worry about what will happen to their loved…

With the support of Hospice of the Red River Valley, Bob and his daughters were…
Stay Connected
ENTER YOUR EMAIL ADDRESS
You can find additional stories, articles, tips and guides on our blog or in our resources section. Or, please contact us, anytime, with questions.

- Search Please fill out this field.
- Manage Your Subscription
- Give a Gift Subscription
- Newsletters
- Sweepstakes
Kate Beckinsale Shares New Photos from Hospital Bed as a Friend Visits Her
Beckinsale first revealed she was in the hospital in early March when she shared two teary-eyed pictures
:max_bytes(150000):strip_icc():format(webp)/Biopicture-7aed89e79c07468e879a00bb6ff007dc.jpg)
Kate Beckinsale/Instagram
Kate Beckinsale is sharing more snaps from the hospital.
On Thursday, April 4, the actress, 50, shared an update from her hospital stay as she posted a series of snaps with the caption, “🥜🥜🌈🌈🖕🏻😢🌈🌈🥜🥜."
Beckinsale has been posting photos from the hospital since early March, but she hasn't confirmed the reason for her being there.
In the first shot from the carousel, Beckinsale posed in a hospital bed in a pair of cat-print silk pajamas with her pal Jonathan Voluck, who was paying a visit to the star. The duo appeared to be wearing peanut headbands as they flashed a smile at the camera in the snap, while a collagen supplement could also be seen on the star's nightstand.
Beckinsale then shared a photo of a rainbow in the sky before posting a jar full of wooden words that featured the label, “F---s to give.”
In the fourth slide, Beckinsale revealed the book Grief Is For People by Sloane Crosley, before sharing another snap of a rainbow.
She then concluded the carousel post with another shot of herself and Voluck.
“The Clive pajamas! Sending love & healing 💖,” one person commented, while another added, “I saw the rainbow today too!! I hope you feel better soon!!! 🫰🏽💐.”
Fashion designer Ramona Agruma , who is also the fiancée of actress Rebel Wilson , also wrote, “Sending you lots of love 💗💗💗.”
Never miss a story — sign up for PEOPLE's free daily newsletter to stay up-to-date on the best of what PEOPLE has to offer, from juicy celebrity news to compelling human interest stories.
On March 19, Beckinsale remembered her late dad , Richard Beckinsale, with an emotional Instagram post, days after first revealing she was in the hospital. Richard died in 1979 of a heart attack at the age of 31. Her stepfather Roy Battersby also died at age 87 on Jan. 10.
While Beckinsale hasn't confirmed the reason behind her hospitalization, she has denied being treated for a ruptured cyst or endometriosis. Responding to one of her followers who said that her "ruptured cyst must have taken such a toll" on her, Beckinsale replied n the comments section, "I didn’t have a ruptured cyst since 2019. But thank you so much for your kind wishes x."
Beckinsale shared that she'd suffered a ruptured ovarian cyst in January 2019.
She first sparked concerns with her more recent hospital stay when she shared two teary-eyed photos of herself from the hospital and referred to being "sick” in an Instagram post on March 11.
"Happy birthday and UK Mother’s Day this last week to my incredible mother,” she wrote at the time. “Thank you to those that love us and support us when it’s s— and try to make sure there are some bits that aren’t. And for looking after our dogs when we can’t, and lead us to remember happy things when we can’t. And turn up when we are sick and sit with us . . And send balloons and check in and pull us out of wells with love.”
Meanwhile, the Farming star also marked her Easter holiday at the hospital by showing off a pair of festive-themed socks .
“Happy Easter 🐰🐇🐣,” her caption read as she shared two snaps of her black pajama pants and bunny socks from a hospital bed.
Related Articles

Gaza City Dispatch
Israeli Army Withdraws From Major Gaza Hospital, Leaving Behind a Wasteland
Al-Shifa Hospital as seen from an Israeli military position at a private clinic outside the hospital on Sunday in Gaza City. Credit...
Supported by
- Share full article
By Patrick Kingsley
Photographs by Avishag Shaar-Yashuv
The journalists were among a small group of international reporters brought by the Israeli army to Al-Shifa Hospital on Sunday. To join the tour, they agreed to stay with the Israeli forces at all times and not to photograph the faces of certain commandos.
- April 2, 2024
Al-Shifa Hospital in Gaza City, once the fulcrum of Gaza’s health system and now an emblem of its destruction, stood in ruins on Sunday, as if a tsunami had surged through it followed by a tornado.
The emergency department was a tidy, off-white building until Israeli troops returned there in March. Two weeks later, it was missing most of its facade, scorched with soot, and punctured with hundreds of bullets and shells.
The eastern floors of the surgery department were left open to the breeze, the walls blown off and the equipment buried under mounds of debris. The bridge connecting the two buildings was no longer there, and the plaza between them — formerly a circular driveway wrapping around a gazebo — had been churned by Israeli armored vehicles into a wasteland of uprooted trees, upturned cars and a half-crushed ambulance.
The hospital was the largest in Gaza, one of its biggest employers and a shelter for thousands of Gazans during war. I had visited its wards in calmer times, meeting Palestinians wounded in a previous conflict and doctors battling Covid-19. When I returned this week, the place was disfigured almost beyond recognition after a 12-day battle between Israeli soldiers and Gazan gunmen and an earlier raid by the Israeli military.
During a two-hour visit, I saw no Palestinians, but the Israeli soldiers who brought me there said there were still gunmen inside one building and a group of patients and doctors in another. Occasionally, we heard short bursts of gunfire. When the soldiers brought us to a vantage point overlooking the hospital, they told us not to linger long in the window in case a sniper saw us.

The symbolism of this hellscape differs according to the beholder, amid a deep divergence about how the conflict should be reported and explained.
To the Israelis who brought me to Al-Shifa on Sunday, the carnage is the result of Hamas’s decision to turn a civilian institution into a military stronghold, leaving Israel with no option but to enter it by force: Exhibit A in what they see as a war of necessity that they did not start.
“We had no alternative,” said Rear Adm. Daniel Hagari, Israel’s chief military spokesman, who led the visit. “We wanted to leave those places functional, but what happened was Hamas and Islamic Jihad were barricading and firing at our forces from the beginning.”
To the Palestinians who returned to Al-Shifa on Monday, searching for dead bodies after the Israelis withdrew, it was the embodiment of Israel’s perceived disregard for civilian life and infrastructure in its pursuit of Hamas: Exhibit A in what they see as a genocide of Gazans.
“As you see, this is Al-Shifa hospital after it was invaded and destroyed by the Israeli occupation forces,” said Motasem Dalloul, a Palestinian journalist, in a self-filmed video he sent from the wreckage on Monday.
“Or what was once Al-Shifa Hospital,” added Mr. Dalloul.
When we met before the war, Mr. Dalloul said that he is not a Hamas member but speaks regularly to its leaders and cadres; he has also acted as an interpreter for its officials.
Walking further through the compound, Mr. Dalloul encountered another man who blamed Israel for the destruction. “This occupation will die, Netanyahu will die, America will die — no matter how much they bomb us,” the unnamed man shouted. “No matter how much they bomb us and destroy Al-Shifa, the occupation will die,” he repeated.
Analysts have said that Israel’s return to Al-Shifa, more than four months after it was first captured, represents a strategic failure: It is the result of Israel’s unwillingness to set in motion any transition of power to forces independent of Hamas, creating a vacuum that has allowed Hamas to regroup.
The Israeli soldiers at Al-Shifa on Sunday portrayed the raid as a success. In one swoop, they said, they had killed about 200 fighters and captured 500 more — the majority, they said, of the remaining militants in northern Gaza. Gazan officials said hundreds of civilians were killed, a charge denied by Israel, and The New York Times could not independently verify either account.
In any case, the soldiers’ departure, hours later, means it will be possible for Hamas to return once again, unimpeded, raising the chances that Israel could return for a third raid in the future.
The Israeli military first captured the hospital site during a raid in November, exposing and destroying a subterranean tunnel network that Israel said was a Hamas command center.
After withdrawing from most of the city in January, the military returned to the hospital in March because it said remnants of Hamas’s military wing had regrouped in Israel’s absence, according to the officers who were escorting the international journalists, including two from The New York Times, to the site on Sunday.
To join the tour, we agreed not to photograph the faces of certain commandos and to stay with the Israeli forces at all times, but otherwise agreed to no other restrictions.
Israel’s naval commando unit, Shayetet 13, swept into the hospital compound early on March 18. By Israel’s account, the destruction began after Hamas gunmen refused to surrender and started shooting at the Israeli forces, prompting them to return fire.
A spokesman for Hamas, Basem Naim, declined to comment on the claim that Hamas was operating inside the hospital but denied that its fighters were there; Hamas’s armed wing has said that it fired on Israeli forces in the vicinity of Al-Shifa, but stopped short of saying that it fought inside the compound.
The Israeli military said that one of the first men killed on March 18 was a security chief, Faiq Mabhouh, whose death was later mourned in a statement from Hamas. A map supplied by the Israeli military said there were at least 13 gunfights that broke out across different parts of the campus over the following two weeks, as the soldiers searched for holdouts hiding throughout the site.
The military said the damage to the emergency and surgery departments was so great because the gunmen had entrenched themselves inside those buildings, one of them inside an elevator shaft, forcing the Israeli commandos to fire repeatedly at their positions. The military said that it found several weapons caches hidden inside the hospital.
The military said the fighting was compounded by Gazan armed groups located outside the compound who also fired at Israeli soldiers, leading to gun battles around its perimeter and the killing of two Israeli soldiers outside the hospital. Hamas said on its social media platforms that its snipers and mortar teams had fired at Israeli forces in the vicinity of the hospital.
To support its claim of Hamas’s presence at the hospital, the Israeli military displayed digital copies of documents, branded with the logo of Hamas’s military wing, that it said were found at the site and which purported to document a meeting of the group’s militants inside the hospital. The Times could not verify the authenticity of the documents.
The Hamas-run authorities in Gaza have accused Israel of killing patients and displaced people sheltering at the hospital, as well as detaining innocent people.
Yahia Al-Kayyali, a 58-year-old doctor, said he was detained by the Israeli Army during the raid while sheltering with his family at a building close to the hospital.
In a phone interview, Dr. Al-Kayyali said the soldiers forced him to strip, a common practice that Israel says is meant to ensure detainees do not conceal weapons, before beating him and his son, interrogating and blindfolding them, taking them to the roof and forcing them to sit on shattered glass for several hours.
They were later released after being made to walk south, he said.
“The soldiers treated us like animals,” he said.
The Israeli soldiers who escorted us on Sunday strongly denied any accusation of wrongdoing. They said they had evacuated more than half of the medics and patients to other health facilities, as well as allowing the vast majority of the 6,000 civilians who had sheltered at the hospital to move south. They said they had detained 900 people, 500 of whom they said were militants and about 400 others who were still being investigated. The numbers could not be independently verified.
“I’ve been here for 14 days,” said the Shayetet 13 commander, who asked to remain anonymous in line with military protocol. “It’s my soldiers. As far as I know, these accusations are a lie.”
According to both Israeli and Palestinian officials, more than 100 patients and medics were moved to a building on the western side of the compound, away from the worst of the fighting.
But there the narratives diverge. The Israeli military says that it did its best to provide food, water and medical care. The Gazan health ministry said in a statement that the remaining patients were left without enough medicine, clean water, food or sanitation, leaving some with septic wounds containing maggots.
“The situation as reported by many of the staff is horrific and inhumane,” the health ministry’s statement said.
Citing Palestinian medics, the World Health Organization said in a statement on Sunday that 21 patients had died since the raid began, and those remaining lacked diapers and bags for urine.
To Taysir al-Tanna, a surgeon who said he had worked for 25 years at Al-Shifa, the destruction of his hospital felt like a national tragedy.
He recounted by phone how the hospital — one of the largest employers in both Gaza and the Israeli-occupied West Bank — had formed “a central place in our country.”
“Now, it’s become a wasteland,” Dr. al-Tanna said. “Try to imagine what that feels like.”
Aaron Boxerman contributed reporting from Jerusalem, and Iyad Abuheweila from Istanbul.
Patrick Kingsley is the Jerusalem bureau chief, covering Israel and the occupied territories. He has reported from more than 40 countries, written two books and previously covered migration and the Middle East for The Guardian. More about Patrick Kingsley
Our Coverage of the Israel-Hamas War
News and Analysis
The Israeli military announced what it called a precise operation to kill members of Hamas in Gaza , a day after a strike there killed three sons of one of the most senior leaders of the group.
Hamas said that it did not have 40 living hostages in Gaza who met specific criteria for an exchange with Israel under a proposed cease-fire deal, raising fears that more hostages may be dead than previously believed.
There has been no apparent work done yet on increasing aid to Gaza by opening an additional border crossing from Israel and accepting shipments at a nearby Israeli port, but Israel said that both changes remain in the works.
Psychedelics and Trauma: Thousands of festival-goers were using mind-altering substances when Hamas-led fighters attacked on Oct 7. Now, scientists are studying the effects of such drugs at a moment of trauma .
Turmoil at J Street: The war in Gaza has raised serious concerns within the Jewish political advocacy group about its ability to hold a middle position without being pulled apart by forces on the right and the left.
Challenging Democratic Leaders: Protests over the Biden administration’s handling of the war in Gaza are disrupting the activities of Democratic officials, complicating their ability to campaign during a pivotal election year .
Germany’s Upended Arts Scene: Berlin, the home of boundary-pushing artists from around the world, has been turned upside down by debates about what can and can’t be said about Israel and the war in Gaza .
Advertisement
O.J. Simpson, NFL star whose murder trial gripped the nation, dies of cancer at 76
O.J. Simpson , the former NFL star who was acquitted of murdering his ex-wife and her friend in a televised trial that gripped the nation, has died of cancer, according to his family.
"He was surrounded by his children and grandchildren," the family said in a statement posted on X . "During this time of transition, his family asks that you please respect their wishes for privacy and grace."
Reports circulated in February that Simpson had been diagnosed with prostate cancer and was in hospice care as he underwent chemotherapy. He denied that he was in hospice in a video posted on X, but did not address whether he'd been diagnosed with cancer.
“Hospice? Hospice? You talking ‘bout hospice?” he said in the video with a laugh, adding that he doesn’t know who started the rumors.
Orenthal James Simpson played 11 seasons in the National Football League and was known as "The Juice" to his fans, but his sports legacy was tarnished forever in the 1990s after his ex-wife Nicole Brown Simpson and her friend Ronald Goldman were killed.
Brown Simpson, 35, and Goldman, 25, were found stabbed to death outside her Los Angeles home in 1994.
On June 13, 1994, Goldman was returning sunglasses that the mother of Brown Simpson had left at a restaurant where he worked. The two were stabbed and slashed dozens of times, and their bodies were found the next day.
When Los Angeles police officers went to Simpson's home to speak to him about the slayings, Simpson did not answer the door but officers noticed a trail of blood leading to his car, as well as blood on his car.
Once a revered athlete, Simpson went from a Hall of Fame icon to a murder suspect.
Days later, officials charged Simpson with the murders and he attempted to evade arrest, resulting in an infamous hourslong police chase along Southern California's highways in his white Ford Bronco .
Simpson's case went to trial in 1995 and was broadcast to millions of viewers across the nation. The court case was dubbed the "trial of the century" as it dragged on for months and transformed into a public spectacle.
Feelings over the trial have remained mixed over the years, with many accusing the Los Angeles Police Department of racism in its handling of the case. Others believe that Simpson's ability to retain high-powered attorneys allowed him to get away with murder.

The trial made prosecutors Christopher Darden and Marcia Clark household names, in addition to Simpson's defense attorneys Johnnie Cochran, Alan Dershowitz and Robert Kardashian.
He was acquitted of both murders in a controversial verdict. Two years later, he was found civilly liable for wrongful death in the double homicide case.
Despite his acquittal in the criminal trial, many still believed Simpson was guilty, a belief bolstered by a jury ordering him to pay $33 million to Goldman's family in the civil case — damages that were never paid in full.

Goldman's father, Fred Goldman, spoke to NBC News by phone Thursday and described Simpson's death as "no great loss."
“The only thing I have to say is it’s just further reminder of Ron being gone all these years," he said. "It’s no great loss to the world. It’s a further reminder of Ron’s being gone.”
In 2007, Simpson led an armed robbery attempt of a sports memorabilia dealer in Las Vegas. He argued in court that he was recovering his own stolen items, but his defense failed to sway the jury.

He was convicted and sentenced to 33 years in prison, of which he served only nine before he was released on parole .
Simpson spoke to The Associated Press by phone in 2019 , telling them that he was healthy and happy living in Las Vegas. He maintained that he believed his robbery conviction was unfair, but said: “I believe in the legal system and I honored it. I served my time.”
The Simpson murder trial was re-enacted and relitigated decades later in FX’s “The People v. O.J. Simpson,” an installment of the network’s popular “American Crime Story” series in 2016. Released that same year was the Academy Award-winning documentary "O.J.: Made in America," detailing Simpson's rise and fall.
Simpson was born in San Francisco and raised in public housing, going to a local community college before transferring to the University of Southern California. He was part of the school's national championship in 1967 and earned the Heisman Trophy the next year.
He was drafted by the Buffalo Bills in 1969 as a No. 1 overall pick.
According to NBC Sports , Simpson was the first player in the league to rush for 2,000 or more yards in a season and is considered the best running back of his era.
Simpson had three children from his first marriage to Marguerite Whitley, one of whom died in a drowning accident as a toddler.
He also shared two children with Brown Simpson.
Following her murder and his acquittal, Simpson won custody of their shared children and moved to Miami with them. His custody fight with his former-in-laws also drew headlines as the children's grandparents took him to court in a bitter legal battle.
Doha Madani is a senior breaking news reporter for NBC News. Pronouns: she/her.
latest in US News

Biden cancels another round of student debt for over 200,000 more...

TikTok star 'breathing on her own' two months after horrifying...

Historic hospital hits the market for just $10 — but potential...

Disturbing video shows white teen being viciously beaten in...

Afghan migrant on terror watchlist roams free in US after being...

16-year-old mugger arrested for shoving parishioner, 68, down...

Landscapers find possible Civil War cannonball buried in yard

Rite Aid to close 53 more stores across 9 states amid bankruptcy...
Breaking news, brazil-bound us travelers will need to show bank statements to visit country next year.
- View Author Archive
- Get author RSS feed
Thanks for contacting us. We've received your submission.
US travelers hoping to visit the beautiful beaches of Brazil will have to acquire a visa first beginning in 2025 — meaning they’ll have to share their bank statements with the South American country.
Beginning April 10, 2025, Brazil-bound travelers from the US, Canada and Australia need to be approved for a visa before their trip, CNN reported .
The application includes providing proof of income by either showing their last three checking or savings account statements or their previous six pay stubs, according to the Brazilian government’s website . Those who do not meet the threshold of $2,000 or more will need a sponsor.

Fortunately, the application process for an e-visa can be done online rather than at a consulate in person.
The visa fee is $80.90 with a 10-year validity and stays are limited to 90 days per year, the US Consulate in Brazil announced .
Additionally, Americans must provide a letter of intent outlining the duration and purpose of their trip and include information about where they will be staying.
They additionally must prove their US citizenship and show return tickets.
Brazil is reinstating the visa requirement for US tourists, who until 2019 had needed visas, according to CNN.
E-visas were introduced for just one year before the entire system was completely abolished.
Processing times for the Brazil visa system will be an average of five working days but officials “strongly recommend” applying two months before a trip.

The Brazilian Embassy and US State Department did not immediately respond to The Post’s request for comment.
For Brazilians planning to travel to the US, the process is much more complex, and visa systems between countries typically are established based on reciprocity, CNN reported.
Nearly all Brazilians must schedule an in-person visa appointment at their nearest embassy and prove they have the financial means to afford their planned trip. The visa costs $185.
Between January and September 2023, some 483,000 Americans visited Brazil — second only to its neighbor Argentina, according to TravelPulse.
Last year, the European Union decided to delay its controversial pre-travel program for American travelers, set to begin last May, until 2025 after several roadblocks.

The European Travel Information and Authorisation System , of ETIAS, will apply to visitors without visas from 60 countries, including the US, UK and Canada.
The program is needed to enter 30 European countries , including Spain, Germany, France and Greece.
Applicants must provide passport information, and personal info such as their place of birth and their parents’ first names, education level, current occupation, anticipated trip details and any criminal convictions.
It also entails an $8 fee.
ETIAS visas are valid for three years or until your passport expires. Visitors can enter European countries as often as they want for short-term stays — typically for up to 90 days in an 180-day period.
Share this article:

Advertisement

Mississippi Today
Pulitzer Prize-winning Nonprofit News
Mississippi hospital officials say marketplace insurance helps, but not as much as Medicaid

Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to email a link to a friend (Opens in new window)
- Click to print (Opens in new window)
Mississippi Senate leaders point to one component of the federal Affordable Care Act health care law as a reason not to expand Medicaid to provide health care coverage to the working poor.
The Senate has passed legislation to allow only those earning less than 100% of the federal poverty level (about $15,000 annually for an individual) and who are working to be covered by Medicaid.
A state House plan would provide Medicaid coverage to those earning up to 138% of the federal poverty level (about $20,000 annually) as is allowed under the Patient Protection and Affordable Care Act, also known as Obamacare.
House and Senate leaders are expected to begin negotiations in the coming days in an attempt to work out the differences between the two chambers.
One reason Senate leaders give for not expanding to provide Medicaid coverage to those earning between 100% and 138% of the federal poverty level is that people who fall into that income category can obtain private insurance through another component of the ACA – the Affordable Care Act Marketplace or “exchange.” People can receive private insurance through the exchange and receive federal help to pay for the policy.
“We want to keep more people on the exchange. The reimbursements (to health care providers) are better,” through the exchange than through Medicaid, said Senate Medicaid Chairman Kevin Blackwell, R-Southaven. “A lot of the argument for expansion has been to help the hospitals. Well, if you are going to take the people who currently have commercial insurance and put them on Medicaid, you just killed your hospitals.”
While the exchange policies assist people who otherwise would not have access to health care coverage, the problem, according to Mississippi hospital officials, is that they often lose money when treating low income people who have the marketplace coverage.
“The bottom line is that Medicaid reimburses at a higher rate,” said Lee McCall, chief executive officer of Neshoba General Hospital in Philadelphia. He said there are some private insurance policies that pay Mississippi hospitals a better reimbursement rate, but not the marketplace plans.
“Most of those marketplace plans, I kind of call catastrophic coverage … ,” McCall said. “For the most part the deductibles are so high many people cannot afford to pay them.”
Kim Hoover, interim chief executive officer of the Mississippi Hospital Association, said Medicaid actually pays state hospitals at the commercial rate – or at the same rate paid by private insurance companies.
Gov. Tate Reeves’ Division of Medicaid got approval from federal Medicaid officials to pay at that higher rate last year. The state’s hospitals agreed to pay the local matching funds needed to draw down the additional Medicaid dollars to pay at the commercial rate.
With the better rate the hospitals now receive from Medicaid, Hoover said, “The main difference between the two is the typically high deductibles for hospital services on the exchange plans. If the patient deductible isn’t paid, then the plan doesn’t pay the hospital the full payment. By comparison, Medicaid patients have no deductible.
“No deductible combined with the commercial rate means that Medicaid is typically better for providers and patients than the exchange plans,” Hoover continued.
Hoover cited an example of “a 54-year-old male in Hinds County making $17,000 a year could pay a monthly premium of $16.85 with a deductible of $6,350 for one of the exchange plans. In this case, the deductible is over 33% of the person’s pre-tax income. Recently, Mississippi led the nation in medical debt bankruptcies. Medicaid expansion would better protect these patients from medical debt.”
Granted, thanks to changes made to the exchange during the pandemic, low income people can get a policy better than what Hoover described. With federal help people between 100% and 138% of the federal poverty level can get a plan with little or no monthly premiums. But there are still out of pocket costs or deductibles for the policyholder on the marketplace plans, though currently less than the amount cited by Hoover.
For instance, on the federal HealthCare.gov website where Mississippians would go to obtain a marketplace plan, a 40-year-old earning $19,000 annually could obtain a plan with a monthly premium of less than $5. But there would be $1,650 out of pocket expenses for one plan.
In general, out of pocket expenses represent the most a person would pay in a year for in-network health care services.
The benefits offered by the marketplace plans have been enhanced through COVID-19 relief legislation passed during the President Joe Biden Administration. Because of that legislation, people pay lower monthly premiums and less in out of pocket expenses than they did previously.
Robin Rudowitz, director of Program on Medicaid and the Uninsured for KFF, said the “the enhanced coverage subsides” people currently are benefitting from are set to expire in 2025. After that, people will be paying more for premiums and more in deductibles and out of pocket expenses.
In addition, Rudowitz pointed out that according to a recent consumer survey, people with Medicaid, even though they generally have more serious health care issues and thus more opportunities for problems, rate their coverage through Medicaid higher than those on private marketplace plans rate their policies.
State Insurance Commissioner Mike Chaney was one of the first state officials to argue in favor of expanding Medicaid just to those earning less than 100% of the federal poverty level to ensure the people above that income level remained in the marketplace.
READ MORE: Negotiations begin: Where do House, Senate, governor stand on Medicaid expansion? Is there room for compromise?
Chaney said there are about 140,000 Mississippians between 100% and 138% of the federal poverty level who have insurance through the marketplace. Under the federal law, if those people are eligible for Medicaid expansion, through an expansion in their state, they no longer would receive the federal help with the private insurance option. With no federal financial assistance, low income people would not be able to afford the marketplace plans.
Moving those people to Medicaid “would destroy the exchange,” Blackwell said. But 40 other states have expanded Medicaid, and they still have exchange policies for those earning too much to qualify for Medicaid expansion.
Some states, such as Arkansas, have used Medicaid expansion funds to pay for private policies for those who would qualify for Medicaid expansion. The federal government allows those states to use their Medicaid expansion funds to pay for the costs of the private health insurance.
READ MORE : Speaker White on Medicaid expansion negotiations: ‘Come for the savings, stay for the compassion’
The federal government pays 90% of the health care costs for Medicaid expansion. But the federal government would not recognize the Senate plan as Medicaid expansion and thus would pay only 77% of the costs, thus costing the state more to cover fewer people, according to various studies. The federal government also will pay Mississippi an additional nearly $700 million over a two-year period as an incentive to expand Medicaid.
KFF, the national non profit that studies health care issues, “estimates that approximately 166,000 uninsured adults would be eligible for expansion – this includes 102,000 who currently fall into the coverage gap (earning less than 100% of the federal poverty level) and another 64,000 who have incomes between 100% and 138% and could be eligible for marketplace coverage but not enrolled.”
In addition there are 140,000 Mississippians who have private insurance through the exchange would have to drop their policy and sign up for Medicaid if expansion is approved by the Legislature.
Based on the experiences of hospital officials, replacing those private policies with Medicaid would not necessarily be a bad thing.
Republish This Story
Republish our articles for free, online or in print, under a Creative Commons license.
Republish this article

This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License .
- Look for the "Republish This Story" button underneath each story. To republish online, simply click the button, copy the html code and paste into your Content Management System (CMS).
- Editorial cartoons and photo essays are not included under the Creative Commons license and therefore do not have the "Republish This Story" button option. To learn more about our cartoon syndication services, click here .
- You can’t edit our stories, except to reflect relative changes in time, location and editorial style.
- You can’t sell or syndicate our stories.
- Any web site our stories appear on must include a contact for your organization.
- If you share our stories on social media, please tag us in your posts using @MSTODAYnews on Facebook and @MSTODAYnews on Twitter.
- You have to credit Mississippi Today. We prefer “Author Name, Mississippi Today” in the byline. If you’re not able to add the byline, please include a line at the top of the story that reads: “This story was originally published by Mississippi Today” and include our website, mississippitoday.org .
- You cannot republish our editorial cartoons, photographs, illustrations or graphics without specific permission (contact our managing editor Kayleigh Skinner for more information). To learn more about our cartoon syndication services, click here .
- Our stories may appear on pages with ads, but not ads specifically sold against our stories.
- You can only publish select stories individually — not as a collection.
by Bobby Harrison, Mississippi Today April 11, 2024
This <a target="_blank" href="https://mississippitoday.org/2024/04/11/mississippi-exchange-marketplace-medicaid-expansion-private-insurance-legislature/">article</a> first appeared on <a target="_blank" href="https://mississippitoday.org">Mississippi Today</a> and is republished here under a Creative Commons license.<img src="https://i0.wp.com/mississippitoday.org/wp-content/uploads/2024/01/MT_icon-logo-favicon-1.png?fit=134%2C150&ssl=1" style="width:1em;height:1em;margin-left:10px;"><img id="republication-tracker-tool-source" src="https://mississippitoday.org/?republication-pixel=true&post=1115014&ga4=G-VSX4B701MS" style="width:1px;height:1px;">
Bobby Harrison
Bobby Harrison, Mississippi Today’s senior capitol reporter, covers politics, government and the Mississippi State Legislature. He also writes a weekly news analysis which is co-published in newspapers statewide. A native of Laurel, Bobby joined our team June 2018 after working for the North Mississippi Daily Journal in Tupelo since 1984. He is president of the Mississippi Capitol Press Corps Association and works with the Mississippi State University Stennis Institute to organize press luncheons. Bobby has a bachelor's in American Studies from the University of Southern Mississippi and has received multiple awards from the Mississippi Press Association, including the Bill Minor Best Investigative/In-depth Reporting and Best Commentary Column.
Police investigate multiple Durham shootings; 1 leaves 16-year-old dead

DURHAM, N.C. (WTVD) -- Durham police are investigating after five people were shot, including a teenager who was killed, across the city on Thursday
Officers investigated at three different locations involving four victims. A fifth gunshot victim showed up at a hospital, but police haven't yet determined where that shooting happened.
The deadly shooting took place in the 1200 block of Truman Street just after 4 p.m. The Durham Police Department said officers found a 16-year-old boy who had been shot.
The teen was taken to a hospital where he later died.

Police have not released the teen's identity.
An active investigation is underway at the scene.
Anyone with information on this shooting is asked to call Investigator J. Berkstresser at (919) 560-4440 ext. 29538 or contact CrimeStoppers at (919) 683-1200 or online at www.durhamcrimestoppers.org .

Two more shootings reported
Durham Police confirmed that another shooting happened just after 6:15 p.m. in the 300 block of Pettigrew Street.
Officers responded to the scene after a report of shots fired. A short time later, a man with a gunshot arrived at the nearby bus terminal on foot.
He was taken to a hospital with what were believed to be serious but not life-threatening injuries.

A third shooting took place just before 5 p.m. in the 1300 block of Fayetteville Street at Linwood Avenue.

Officers didn't find anyone shot there, but a short time later, a man and a male juvenile who had both been shot arrived at a hospital in a private vehicle. Both victims sustained what were described as non-life-threatening injuries.
Fifth gunshot victim arrives at hospital
Yet another man with a gunshot wound also arrived at a hospital around the same time with what were believed to be non-life-threatening injuries.
Police do not yet know where this shooting took place.
DPD said it has not yet determined whether any of these shootings were related.
ABC11 spoke with Durham Mayor Leonardo Williams about the violence across the city.
"I just spoke about this in my state of the city. We have to take a holistic approach to, you know, just crime involving the youth," he said. "And the fact of the matter is, the people who are living in the zone where shots fired was, are the ones that are asking what is wrong with us as a council and where is ShotSpotter?"
Anyone with information about any of these shootings is asked to contact CrimeStoppers at (919) 683-1200 or online at www.durhamcrimestoppers.org . CrimeStoppers pays cash rewards of up to $2,000 for information leading to arrests in felony cases and callers never have to identify themselves.
Check back for updates.
Tracking crime and safety across Raleigh, Durham and your neighborhood
Related Topics
- FATAL SHOOTING
- GUN VIOLENCE
- TEEN KILLED
Top Stories

Durham County Sheriff to discuss efforts to reduce violent crime
- 40 minutes ago

NC 'rolling out the red carpet' for Japanese prime minister's visit

Knightdale woman struggles to get help with recalled car

Mark Robinson did not file federal income taxes for 5 years: Documents

Fujifilm vows $1.2B investment, 680 new jobs in NC
How OJ Simpson murder trial changed the news world
Strong wind damages auto shop; level 1 severe risk remains
ADL gives UNC an 'F' on campus antisemitism, Duke gets a 'B'

IMAGES
VIDEO
COMMENTS
Don'ts for Hospital Visitors. Don't enter the hospital if you have any symptoms that could be contagious. Neither the patient nor other hospital workers can afford to catch whatever you have. If you have symptoms like a cough, runny nose, rash or even diarrhea, don't visit. Make a phone call or send a card instead.
6. Keep conversations quiet. A hospital is not a quiet place. Between the constant beep and hum of machines and staff members' conversations, it can be next-to-impossible for hospitalized patients to get rest. Don't add to the noise by talking and laughing loudly; keep conversations quiet.
The system is in place at several entrances to The Johns Hopkins Hospital and the Children's Center. Patients, visitors and care partners will be required to register and present a valid photo ID when entering our hospital buildings. You will receive a printed badge that should be worn at all times while in the hospital.
Before traveling to the hospital, call to check the visitation policy. Certain units have strict visiting hours and some have policies that restrict the number of visitors. It's common for young children to be restricted from visiting. If you have any signs of illness, such as fever, runny nose, nasal congestion or cough, it's recommended ...
To contain the spread of COVID, hospitals and nursing homes barred visits, but the separation and isolation took a toll on patients and families. Now, some states are trying to ensure access.
At the beginning of the pandemic, most hospitals implemented strict no-visitor rules to curb the spread of COVID-19. A July study, published in The American Journal of Respiratory and Critical Care Medicine, found that out of 48 Michigan hospitals, 39% prohibited visitors without exception and 59% only allowed visitors under "certain ...
Choose the right time. Before you visit the hospital, you should check to see when visiting hours are at that facility. Most hospitals have evening hours to accommodate working visitors, but some hospitals or even some specialized departments or floors, such as the intensive care unit, may have restrictive schedules. Call ahead with the name of the patient you wish to visit to confirm the ...
These recommendations apply only to patients who test negative for SARS - CoV-2 or who are not suspected of having COVID-19. For those patients who are COVID Positive, additional considerations are needed to prevent transmission to the visitor and may preclude any visitation. Virtual visitation may be a way to connect the patient with their ...
Learn more about Mayo Clinic Patient Travel Services. Patient Travel Services makes planning for your appointment at Mayo Clinic seamless. From any location, worldwide, our dedicated team will guide you through your journey for the care you need. See how Patient Travel Services can help.
If you are visiting a friend or loved one in the hospital, you need to take steps to prevent spreading germs. The best way to stop the spread of germs is to: Wash your hands often. Stay home if you are sick. Use a face mask when directed or when infections may be transmitted through the air. Keep your vaccines up to date.
During the pandemic, nursing homes and hospitals often banned visitors, often for months. Although restrictions have eased, some states are passing "right to visit" laws for future pandemics.
Hospitals are still limiting visitors due to covid. Here's what you need to know. Some hospitals are allowing only one visitor per day; others are allowing only one visitor for a patient's ...
COVID-19 Patient Visitor Guidelines for Pennsylvania Hospital. Family caregivers are vital members of the care team. Penn Medicine seeks to maximize family caregiver presence while keeping our patients, caregivers and staff safe. Effective Tuesday May 2, 2023, visitation will be permitted at Pennsylvania Hospital under the following circumstances:
Care partners and parents/legal guardians are welcome 24/7. One care partner can stay overnight with the patient (up to two care partners for pediatric patients or patients with a disability). A visitor is anyone the patient/LAHD or parent/guardian chooses to have visit the patient. An adult patient, or parent/guardian of a pediatric patient ...
Patient and Visitors Guide. It is an honor to care for you and your family. We pride ourselves on providing patient- and family-centered care. We are also taking extra precautions to keep you and your loved ones safe and protected. Preparing for your visit We're honored to care for you Learn more. When you arrive Preparing for your hospital ...
What to Know About Hospitals. A hospital is a crucial part of the health system. It provides outpatient, inpatient, and emergency medical care for sick and injured people. You can visit a hospital ...
When you need medical attention, knowing where to go for health care can help you save time — and help assure you'll get the care you need. You may choose care from your primary care provider (PCP), a virtual visit (or telehealth), urgent care or emergency room, depending on your situation. Here are tips to help you choose where to go for care.
Hospital entry points will be limited to enable the cease of visitors. Those who are able to visit due to extenuating circumstances, but who show any signs of illness, including mild symptoms, should not visit patients in the hospital or accompany patients to the emergency department. Please dial 714-827-3000 for any questions.
The office may call you a few days before your appointment to go over some screening questions. This means asking questions about your possible risk factors of having COVID-19. They may repeat these questions during your visit. You may also be asked additional information over the phone to reduce the amount of paperwork needed at the time of visit.
Book Your Video Visit with the Best Doctors Online. Stay safe at home while receiving top-quality medical care: online video visits and phone appointments with certified physicians. It's safe, secure, and with all the same privacy as a physical visit. We know that finding the right doctor or provider is important to your health.
Intention is everything. The person will sense your tone, pace of the visit and more. If your visit is intended to make the person feel encouraged, cared about, or put a smile on his or her face, the person will sense it. Below are several helpful suggestions about how to prepare for a visit and ideas to guide you during the visit:
Visiting Hours are 8 am to 8 pm, 7 days a week with respect to the patient's wishes and needs, along with consideration of all patients on the unit. Two visitors at one time are permitted per patient. One visitor per patient is permitted in the Emergency Department. Children. Visitors must be 12 years of age in general areas of the hospital.
Scheduled Video Visits Scheduled video visits are appointments with your healthcare provider where you connect via your patient portal: The Christ Hospital Mobile App or MyChart for Desktop. You will be able to see, hear and speak to your provider, similar to the experience you have with friends or family using Facetime.
Kate Beckinsale shared a carousel post on April 4 featuring new photos of her hospital stay, including receiving a visit from a friend and her view of a rainbow.
The hospital was the largest in Gaza, one of its biggest employers and a shelter for thousands of Gazans during war. I had visited its wards in calmer times, meeting Palestinians wounded in a ...
When Los Angeles police officers went to Simpson's home to speak to him about the slayings, Simpson did not answer the door but officers noticed a trail of blood leading to his car, as well as ...
US travelers hoping to visit the beautiful beaches of Brazil will have to acquire a visa first beginning in 2025 — meaning they'll have to share their bank statements with the South American ...
Kim Hoover, interim chief executive officer of the Mississippi Hospital Association, said Medicaid actually pays state hospitals at the commercial rate - or at the same rate paid by private insurance companies. Gov. Tate Reeves' Division of Medicaid got approval from federal Medicaid officials to pay at that higher rate last year.
A fifth gunshot victim showed up at a hospital, but police haven't yet determined where that shooting happened. The deadly shooting took place in the 1200 block of Truman Street just after 4 p.m.