- Tools & Resources
- Find Your Local Chapter
- Use my current location

- News and Stories


Each Journey Is Unique
Your epilepsy story is powerful and can give people hope, empowerment, and safety. Join our community and share your story to talk about epilepsy, seizure safety, and the need to find cures. Make a difference and take action.
SHARE YOUR STORY
Type of Epilepsy or Syndrome
- Unknown Onset
- Temporal Lobe Epilepsy (TLE)
- Reflex Epilepsies
- Lennox Gastaut Syndrome LGS
- Landau Kleffner Syndrome
- Juvenile Myoclonic Epilepsy
- Infantile Spasms West Syndrome
- Generalized
- Epilepsy Generalized Tonic Clonic Seizures Alone
- Dravet Syndrome
- Childhood Epilepsy Centrotemporal Spikes (Benign Rolandic Epilepsy)
- Childhood Absence Epilepsy
Type of Seizure
- Tonic Seizures
- Tonic Clonic Seizures
- Myoclonic Seizures
- Focal Onset Impaired Awareness Seizures (Complex Partial Seizures)
- Focal Onset Aware Seizures (Simple Partial Seizures)
- Focal Bilateral Tonic Clonic Seizures (Secondarily Generalized Seizures)
- Febrile Seizures
- Epileptic or Infantile Spasms
- Drug-Resistant Seizures
- Clonic Seizures
- Atypical Absence Seizures
- Atonic Seizures
- Absence Seizures
- Non-epileptic seizures
Connection to Epilepsy
- Teen with Epilepsy
- Person with Epilepsy
- Parent of a Child with Epilepsy
- Lost a Loved One to Epilepsy
- Family of a Person with Epilepsy
- Child with Epilepsy
- Change Our Epilepsy Story
- Family/Friend
- Healthcare Professionals

Thursday, April 18, 2024
You Are Stronger Than You Know
Read More from Sophia Goldberg

Monday, April 15, 2024
Advocating for Healthy Living With Epilepsy
Read More from Tami Maier

Friday, April 05, 2024
Finding My Passion Despite a Challenging Journey
Read More from Emily Marzini

Tuesday, April 02, 2024
Listen to Your Body
Read More from Maya Wortman

Tuesday, March 26, 2024
There Is Hope
Read More from David Hayes
Friday, March 22, 2024
A Traumatic Brain Injury Caused My Seizures
Read More from María Sanfeliú

Tuesday, March 19, 2024
Honoring the Memory of Easton
Read More from Kim Plummer
Thursday, March 14, 2024
Supporting My Sister on Her Journey With Epilepsy
Read More from Lauren Evans

Friday, March 08, 2024
From Low Self-Esteem to Sharing My Story
Read More from Pasquale DeSavino

Tuesday, March 05, 2024
No Matter What Happens, I’ll Be Okay
Read More from Maddie Giles
Be inspired by our community and share your journey.
Sign up for emails.
Stay up to date with the latest epilepsy news, stories from the community, and more.
- Our Mission
- Become a Partner
- Our Partners
- Impact Reports
- Grants Awarded
- Epilepsy Genetics
- Infantile Spasms
- Post-Traumatic Epilepsy
- EEM / Jeavons Syndrome
- Epilepsy News
- CURE Epilepsy in the News
- Seizing Life Podcast
- Epilepsy Explained
- CURE EPILEPSY CARES
- Personal Stories
- UNITE to CURE Epilepsy 2023
- CURE Epilepsy’s 25th Anniversary Gala
- Attend an Event
- Host An Event
- How to donate
- Monthly giving
- Tribute gifts
- Major gifts
- Online giving
- Corporate giving
- Planned giving
- Stock donations
- Matching Gifts
- Workplace giving
- Say the Word #SayEpilepsy
- What is Epilepsy?
- What causes epilepsy?
- What is a Seizure?
- Seizure Classification
- Phases of Seizures
- Risks Associated with Epilepsy
- Diagnosis and Therapies
- Medication Access
- How is epilepsy diagnosed?
- Diagnostic Tests
- Other Diagnostic Tests
- Epilepsy Syndromes
- Adults and Pediatric Patients
- Epilepsy Medications
- Epilepsy Surgery
- Dietary Therapies
- Alternative Therapies
- Neurostimulation Devices
- Seizure Action Plan
- Clinical Trials
- Patient Opportunities
- COVID-19 and Epilepsy
- Epilepsy Centers
- Grants Program
- Research Resources
- CURE Epilepsy-Sponsored Conferences
- Researcher Updates
Episode #68 - Living and Thriving with Epilepsy featuring Jon Sadler
Living and thriving with epilepsy.

Seizing Life, a CURE Epilepsy podcast hosted by Kelly Cervantes, aims to inspire empathy & give hope as we search for a cure for epilepsy. Together, we can find a cure. We can seize life.
Living with epilepsy isn’t always easy. The physical, mental, and emotional effects of both seizures and the medications can take a daily toll on the person living with epilepsy, creating challenges that may not be visible to others. The lack of understanding around epilepsy within the general public adds yet another degree of difficulty for people living with epilepsy. Yet, a life lived with epilepsy can provide great rewards including defying the expectations of others, creating a rich and fulfilling life, and inspiring others with epilepsy to pursue their own goals and dreams.
On this week’s Seizing Life , epilepsy patient, counselor, and author Jon Sadler discusses his 50-year journey living with epilepsy. Jon’s experiences reflect many of the challenges and concerns of people with epilepsy including stigma, employment, family, dealing with changing treatments and side-effects, and undergoing life-changing brain surgery. Jon reflects on how his personal experiences have shaped his perspective on epilepsy and how this inspired him to become a counselor for fellow patients and caregivers. Jon’s story is a microcosm of what has been accomplished within the epilepsy community during the past 50 years, as well as a directive highlighting the work that still needs to be done.
Download Audio
Want to download this episode? Fill out the form below and enjoy the podcast any time you’d like!
First name*

#67 After SUDEP: A Journey of Grief and Hope

#69 Infantile Spasms: Awareness, Observation, and Intervention
Related episodes.

April 3, 2024
#136 one woman’s epilepsy journey through childhood, parenting, discrimination, and surgery.
This month on Seizing Life® author Laura Beretsky shares her decades-long journey with epilepsy chronicled in her recent memoir Seizing Control.

February 7, 2024
#134 artificial intelligence and epilepsy: the promise & pitfalls of ai in diagnosis and treatment.
Dr. Daniel Goldenholz of Beth Israel Deaconess Medical Center discusses the current and potential impacts of artificial intelligence on epilepsy care.

January 3, 2024
#133 best of seizing life 2023.
This week on Seizing Life®, we revisit several compelling conversations from the past year in our Best of Seizing Life 2023 compilation episode.
Download Transcript
Want to download this transcript? Fill out the form below and we’ll begin your PDF download.
Download audio: Living and Thriving with Epilepsy
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Creating an Epilepsy Treatment and Seizure Action Plan
Knowing What to Do If a Seizure Occurs
Treating Epilepsy
- Caring for a Loved One
- Need for Care Plan
- Creating an Action Plan
Frequently Asked Questions
An action plan can help a person who has epilepsy and other people around them know what to do in case a seizure happens. Everyone who is diagnosed with epilepsy would benefit from an action plan that includes the proper steps to take when an unexpected seizure occurs.
While some people with epilepsy have triggers that make the seizures more likely, seizures often occur without any predictability. Treatment with antiepileptic drugs (AEDs) and avoidance of triggers are important.
By taking medication, many people with epilepsy have very few seizures, but some may have frequent seizures even with medical treatment. The frequency can range from less than once a year to several per day.
This article will discuss how to create a seizure action plan, how epilepsy is treated, and caring for a loved one with epilepsy.
FG Trade / Getty Images
Epilepsy treatment involves medical care as well as lifestyle measures. Medication is the most common treatment used to prevent seizures. Still, some people also need surgical procedures or dietary changes if standard medication is ineffective or medication side effects are not tolerable.
Complementary and alternative medicine (CAM) treatments are often promoted for seizure control, but they are ineffective and might be unsafe for some people. Discuss any such remedies with your healthcare provider before using them.
Additionally, lifestyle measures to eliminate potential seizure triggers are highly valuable for people who have epilepsy. Illness, sleep deprivation, and alcohol can trigger seizures, including severe seizures.
Medical Treatment
Medical treatment for epilepsy usually involves taking daily, scheduled AEDs. This requires consistency and discipline. You need to take the medication even if you have not been having seizures. Lack of seizures is an indication that your medication is working. For most people with epilepsy, stopping the medication will trigger a seizure.
In addition to regular daily preventative medication, some people are also given a prescription for anti-epilepsy medication that is to be taken if a seizure occurs or if an aura occurs. An aura is a neurological change that causes symptoms prior to a seizure.
Most people will not benefit from taking medication that is given for an active seizure or an aura. You and your neurologist will have to determine whether you should have a prescription to take if you experience a seizure or an aura.
Other medical interventions involve surgery, and many people who have epilepsy surgery continue to need treatment with AEDs.
Most AEDs have side effects, and it can take some time to determine the ideal dose that controls your seizures with minimal side effects. Do not make changes in your AEDs on your own—discuss your dose, seizure control, and side effects with your neurologist.
Complementary Treatments
In general, complementary treatments are not effective in preventing seizures.
Some people with epilepsy are advised to try a ketogenic diet , which is a highly restrictive, low-carbohydrate, high-fat diet. This does not work for everyone, and you and your neurologist can discuss whether this would be a good option for you.
Identifying and Avoiding Seizure Triggers
If you have epilepsy, there are important lifestyle measures that you need to take, because certain things can trigger a seizure. Triggers include alcohol, sleep deprivation, lack of eating, extreme stress, and medical illness.
Some people also have photosensitive epilepsy , which is a type of epilepsy in which seizures are provoked by rapidly flashing lights. If you have photosensitive epilepsy, you need to take precautions to avoid exposure to this type of light, which can be present in video games and some entertainment.
Less often, people with epilepsy may experience seizures in response to certain smells or sounds. If you have noticed that you have an unusual trigger, be sure to discuss it with your neurologist, who might perform tests to determine exactly what your triggers are and advise you on how to avoid them.
Symptoms of a Seizure
Seizures can cause different symptoms, which may include:
- Staring into space
- Eye blinking or eye-rolling
- Unusual noises
- Stiffening of the whole body or part of the body
- Jerking movements
- Falling down
These symptoms can begin suddenly or may be preceded by dizziness, tiredness, or unusual sensations.
Caring for a Loved One With Epilepsy
If you care for a family member or other loved one with epilepsy, you must become familiar with their medication schedule. This includes knowing which medications they need to take daily for prevention and if there are any medications they need to take when they experience an aura or a seizure.
Most importantly, you must be prepared to take safety precautions if your loved one is having a seizure or it seems like they will have a seizure. Safety precautions involve keeping them away from water, fire, or any sharp objects or potential falls.
You should also have a plan for whom to call or where to take them if they have a prolonged seizure or experience an injury during a seizure.
Why Do You Need an Epilepsy Care Plan?
The key reason for having an epilepsy care plan is to avoid making an emergency decision unexpectedly.
Being prepared in advance also means having guidelines for your care from the neurologist who takes care of your seizures. This type of guidance is based on experience in terms of what works medically and how well people can implement the recommendations into daily life.
When your family, friends, or roommates are aware of the guidance you’ve received from your neurologist, they will be able to handle unexpected or emergency issues safely. And it will also help ease their stress or anxiety about your epilepsy, making them feel more comfortable about your condition.
Creating a Seizure Action Plan (SAP)
There are no widely established or endorsed seizure action plans. Each person can work with their neurologist to create one. This would include personalized instructions that you can use and share with others with whom you spend time or who would be in a position to take care of you if you have a seizure.
Research shows that having a seizure action plan is beneficial for people who have epilepsy and for their families.
Who Should Make an SAP?
Anyone who has epilepsy should have a SAP that is created with guidance from a neurologist, and with input and approval from the person who has epilepsy, as well as anyone taking care of them. This ensures that the SAP is medically sound and that it is practical and the people who are involved understand it and can handle it.
What to Include
Currently, there is no well-established uniform epilepsy care plan that’s used for people with epilepsy.
An expert panel meeting in 2021 established the importance of creating a seizure action plan. The panel recommend the following information be included:
- Circumstances specific to the person (type of seizures, where they are located, type of housing)
- Names and numbers of emergency contacts, including their healthcare provider, caregivers, and family
- A description of the individual's usual signs and symptoms of a seizure and any atypical ones
- How and when to administer seizure first aid to the person
- Information on the individual's prescribed treatment, including step-by-step instructions on how to give it
- When to start medication and when to contact emergency assistance
Where Is It Kept?
A person who has epilepsy should become familiar with their own epilepsy care plan. Epilepsy care plans should be shared with family members, friends, or roommates who live with a person who has epilepsy. The care plan should also be provided to a child’s teachers, school nurse, coaches, and chaperones for field trips or camps.
The student or parents should discuss the plan to help those individuals understand what needs to be done and answer any questions and address any concerns these individuals have.
Adults may need to share their epilepsy plan with certain people in the workplace who would be expected to call for help if a seizure occurs.
The key components of the care plan may be highlighted for specific individuals so that they can easily understand which parts of the care plan they need to take action on.
For some people with epilepsy, it can be beneficial to wear a bracelet or another identifying device so that emergency care workers will be able to quickly learn of the person's condition, as well as any allergies.
Some people have severe reactions to AEDs, and this should be made clear so that emergency healthcare providers will quickly know the information when a person who is having a seizure is unable to communicate.
If you or your child has epilepsy, it’s important to create a care plan that you and everybody who is involved in taking care of you or your child will be prepared in case a seizure occurs.
While there is no established format for an epilepsy care plan, there are some general principles that you and your neurologist can work on to create guidelines. These include having an understanding of what to do in case a seizure occurs, knowing when to call for help, and knowing if there is any medication that you should take if a seizure occurs.
Additionally, if there are allergies to any anti-seizure medication, this should be indicated on a bracelet or other obvious device in case emergency personnel are called and need to administer medication.
A Word From Verywell
Living with epilepsy requires planning. While the condition is manageable, sometimes unexpected emergencies occur. Therefore, it's always good to be prepared and to have a plan of action that guides you and others around you in case an emergency occurs.
You and your neurologist should discuss an emergency action plan for your epilepsy and determine periodically whether it needs to be updated or changed. The emergency action plan includes steps that you may need to take in case you have a seizure.
You will also need to share it with people whom you trust and who are responsible and could potentially put the plan into action in case you are unable to do so.
Warning signs can include eye fluttering, eye-rolling, making unusual grunting noises, jerking or stiffening, or falling to the ground. Sometimes people may have a seizure without having any of these warning signs.
Normally a seizure lasts for a few seconds, but if it lasts four minutes or more, it is a sign of a medical emergency that requires urgent medical attention.
Yes, you can stop a seizure after it starts, but most seizures end on their own before you would have time to take medication. It is not safe to swallow medication while you are having a seizure. If a seizure lasts for a long time, this usually requires medical intervention with intravenous medication.
In rare instances, people with epilepsy are given prescription medication to take during a seizure by intramuscular injection. This would have to be given by someone, such as a family member or healthcare provider.
If you are around someone who is having a seizure, help them avoid potential harm. This includes keeping them away from water, sharp objects, or anything that they could fall from.
If the seizure lasts for more than a few seconds, call for emergency help. Emergency responders are trained to assess whether a person needs urgent treatment for a seizure.
Centers for Disease Control and Prevention. Managing epilepsy well checklist .
National Institute of Neurological Disorders and Stroke. The epilepsies and seizures: hope through research .
Patel AD, Becker DA. Introduction to use of an acute seizure action plan for seizure clusters and guidance for implementation . Epilepsia. 2022;63 Suppl 1:S25-S33. doi:10.1111/epi.17344
Penovich P, Glauser T, Becker D, et al. Recommendations for development of acute seizure action plans (ASAPs) from an expert panel . Epilepsy Behav. 2021;123:108264. doi:10.1016/j.yebeh.2021.108264
Neville KL, McCaffery H, Baxter Z, Shellhaas RA, Fedak Romanowski EM. Implementation of a standardized seizure action plan to improve communication and parental education . Pediatr Neuro l. 2020;112:56-63. doi:10.1016/j.pediatrneurol.2020.04.005
By Heidi Moawad, MD Dr. Moawad is a neurologist and expert in brain health. She regularly writes and edits health content for medical books and publications.
- Search Menu
- Advance Articles
- Editor's Choice
- Supplements
- Patient Perspectives
- Methods Corner
- ESC Content Collections
- Author Guidelines
- Instructions for reviewers
- Submission Site
- Why publish with EJCN?
- Open Access Options
- Self-Archiving Policy
- Read & Publish
- About European Journal of Cardiovascular Nursing
- About ACNAP
- About European Society of Cardiology
- ESC Publications
- Editorial Board
- Advertising & Corporate Services
- War in Ukraine
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
Introduction, why patient journey mapping, how is patient journey mapping conducted, use of technology in patient journey mapping, future implications for patient journey mapping, conclusions, patient journey mapping: emerging methods for understanding and improving patient experiences of health systems and services.
Lemma N Bulto and Ellen Davies Shared first authorship.
Conflict of interest: none declared.
- Article contents
- Figures & tables
- Supplementary Data
Lemma N Bulto, Ellen Davies, Janet Kelly, Jeroen M Hendriks, Patient journey mapping: emerging methods for understanding and improving patient experiences of health systems and services, European Journal of Cardiovascular Nursing , 2024;, zvae012, https://doi.org/10.1093/eurjcn/zvae012
- Permissions Icon Permissions
Patient journey mapping is an emerging field of research that uses various methods to map and report evidence relating to patient experiences and interactions with healthcare providers, services, and systems. This research often involves the development of visual, narrative, and descriptive maps or tables, which describe patient journeys and transitions into, through, and out of health services. This methods corner paper presents an overview of how patient journey mapping has been conducted within the health sector, providing cardiovascular examples. It introduces six key steps for conducting patient journey mapping and describes the opportunities and benefits of using patient journey mapping and future implications of using this approach.
Acquire an understanding of patient journey mapping and the methods and steps employed.
Examine practical and clinical examples in which patient journey mapping has been adopted in cardiac care to explore the perspectives and experiences of patients, family members, and healthcare professionals.
Quality and safety guidelines in healthcare services are increasingly encouraging and mandating engagement of patients, clients, and consumers in partnerships. 1 The aim of many of these partnerships is to consider how health services can be improved, in relation to accessibility, service delivery, discharge, and referral. 2 , 3 Patient journey mapping is a research approach increasingly being adopted to explore these experiences in healthcare. 3
a patient-oriented project that has been undertaken to better understand barriers, facilitators, experiences, interactions with services and/or outcomes for individuals and/or their carers, and family members as they enter, navigate, experience and exit one or more services in a health system by documenting elements of the journey to produce a visual or descriptive map. 3
It is an emerging field with a clear patient-centred focus, as opposed to studies that track patient flow, demand, and movement. As a general principle, patient journey mapping projects will provide evidence of patient perspectives and highlight experiences through the patient and consumer lens.
Patient journey mapping can provide significant insights that enable responsive and context-specific strategies for improving patient healthcare experiences and outcomes to be designed and implemented. 3–6 These improvements can occur at the individual patient, model of care, and/or health system level. As with other emerging methodologies, questions have been raised regarding exactly how patient journey mapping projects can best be designed, conducted, and reported. 3
In this methods paper, we provide an overview of patient journey mapping as an emergent field of research, including reasons that mapping patient journeys might be considered, methods that can be adopted, the principles that can guide patient journey mapping data collection and analysis, and considerations for reporting findings and recognizing the implications of findings. We summarize and draw on five cardiovascular patient journey mapping projects, as examples.
One of the most appealing elements of the patient journey mapping field of research is its focus on illuminating the lived experiences of patients and/or their family members, and the health professionals caring for them, methodically and purposefully. Patient journey mapping has an ability to provide detailed information about patient experiences, gaps in health services, and barriers and facilitators for access to health services. This information can be used independently, or alongside information from larger data sets, to adapt and improve models of care relevant to the population that is being investigated. 3
To date, the most frequent reason for adopting this approach is to inform health service redesign and improvement. 3 , 7 , 8 Other reasons have included: (i) to develop a deeper understanding of a person’s entire journey through health systems; 3 (ii) to identify delays in diagnosis or treatment (often described as bottlenecks); 9 (iii) to identify gaps in care and unmet needs; (iv) to evaluate continuity of care across health services and regions; 10 (v) to understand and evaluate the comprehensiveness of care; 11 (vi) to understand how people are navigating health systems and services; and (vii) to compare patient experiences with practice guidelines and standards of care.
Patient journey mapping approaches frequently use six broad steps that help facilitate the preparation and execution of research projects. These are outlined in the Central illustration . We acknowledge that not all patient journey mapping approaches will follow the order outlined in the Central illustration , but all steps need to be considered at some point throughout each project to ensure that research is undertaken rigorously, appropriately, and in alignment with best practice research principles.
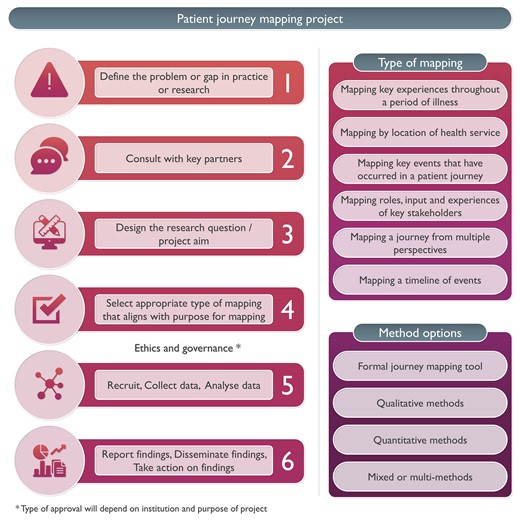
Steps for conducing patient journey mapping.
Five cardiovascular patient journey mapping research examples have been included in Figure 1 , 12–16 to provide specific context and illustrate these six steps. For each of these examples, the problem or gap in practice or research, consultation processes, research question or aim, type of mapping, methods, and reporting of findings have been extracted. Each of these steps is then discussed, using these cardiovascular examples.
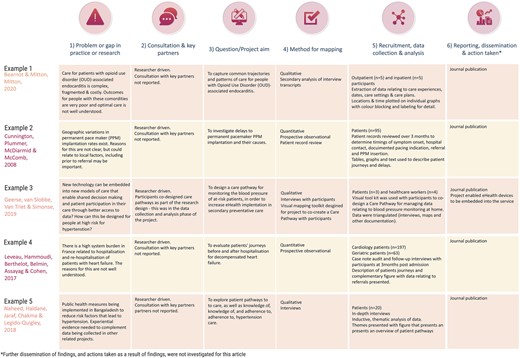
Examples of patient journey mapping projects.
Define the problem or gap in practice or research
Developing an understanding of a problem or gap in practice is essential for facilitating the design and development of quality research projects. In the examples outlined in Figure 1 , it is evident that clinical variation or system gaps have been explored using patient journey mapping. In the first two examples, populations known to have health vulnerabilities were explored—in Example 1, this related to comorbid substance use and physical illness, 13 and in Example 2, this related to geographical location. 13 Broader systems and societal gaps were explored in Examples 4 and 5, respectively, 15 , 16 and in Example 3, a new technologically driven solution for an existing model of care was tested for its ability to improve patient outcomes relating to hypertension. 14
Consultation, engagement, and partnership
Ideally, consultation with heathcare providers and/or patients would occur when the problem or gap in practice or research is being defined. This is a key principle of co-designed research. 17 Numerous existing frameworks for supporting patient involvement in research have been designed and were recently documented and explored in a systematic review by Greenhalgh et al . 18 While none of the five example studies included this step in the initial phase of the project, it is increasingly being undertaken in patient partnership projects internationally (e.g. in renal care). 17 If not in the project conceptualization phase, consultation may occur during the data collection or analysis phase, as demonstrated in Example 3, where a care pathway was co-created with participants. 14 We refer readers to Greenhalgh’s systematic review as a starting point for considering suitable frameworks for engaging participants in consultation, partnership, and co-design of patient journey mapping projects. 18
Design the research question/project aim
Conducting patient journey mapping research requires a thoughtful and systematic approach to adequately capture the complexity of the healthcare experience. First, the research objectives and questions should be clearly defined. Aspects of the patient journey that will be explored need to be identified. Then, a robust approach must be developed, taking into account whether qualitative, quantitative, or mixed methods are more appropriate for the objectives of the study.
For example, in the cardiac examples in Figure 1 , the broad aims included mapping existing pathways through health services where there were known problems 12 , 13 , 15 , 16 and documenting the co-creation of a new care pathway using quantitative, qualitative, or mixed methods. 14
In traditional studies, questions that might be addressed in the area of patient movement in health systems include data collected through the health systems databases, such as ‘What is the length of stay for x population’, or ‘What is the door to balloon time in this hospital?’ In contrast, patient mapping journey studies will approach asking questions about experiences that require data from patients and their family members, e.g. ‘What is the impact on you of your length of stay?’, ‘What was your experience in being assessed and undergoing treatment for your chest pain?’, ‘What was your experience supporting this patient during their cardiac admission and discharge?’
Select appropriate type of mapping
The methods chosen for mapping need to align with the identified purpose for mapping and the aim or question that was designed in Step 3. A range of research methods have been used in patient journey mapping projects involving various qualitative, quantitative, and mixed methods techniques and tools. 4 Some approaches use traditional forms of data collection, such as short-form and long-form patient interviews, focus groups, and direct patient observations. 18 , 19 Other approaches use patient journey mapping tools, designed and used with specific cultural groups, such as First Nations peoples using artwork, paintings, sand trays, and photovoice. 17 , 20 In the cardiovascular examples presented in Figure 1 , both qualitative and quantitative methods have been used, with interviews, patient record reviews, and observational techniques adopted to map patient journeys.
In a recent scoping review investigating patient journey mapping across all health care settings and specialities, six types of patient journey mapping were identified. 3 These included (i) mapping key experiences throughout a period of illness; (ii) mapping by location of health service; (iii) mapping by events that occurred throughout a period of illness; (iv) mapping roles, input, and experiences of key stakeholders throughout patient journeys; (v) mapping a journey from multiple perspectives; and (vi) mapping a timeline of events. 3 Combinations or variations of these may be used in cardiovascular settings in the future, depending on the research question, and the reasons mapping is being undertaken.
Recruit, collect data, and analyse data
The majority of health-focused patient journey mapping projects published to date have recruited <50 participants. 3 Projects with fewer participants tend to be qualitative in nature. In the cardiovascular examples provided in Figure 1 , participant numbers range from 7 14 to 260. 15 The 3 studies with <20 participants were qualitative, 12 , 14 , 16 and the 2 with 95 and 260 participants, respectively, were quantitative. 13 , 15 As seen in these and wider patient journey mapping examples, 3 participants may include patients, relatives, carers, healthcare professionals, or other stakeholders, as required, to meet the study objectives. These different participant perspectives may be analysed within each participant group and/or across the wider cohort to provide insights into experiences, and the contextual factors that shape these experiences.
The approach chosen for data collection and analysis will vary and depends on the research question. What differentiates data analysis in patient journey mapping studies from other qualitative or quantitative studies is the focus on describing, defining, or exploring the journey from a patient’s, rather than a health service, perspective. Dimensions that may, therefore, be highlighted in the analysis include timing of service access, duration of delays to service access, physical location of services relative to a patient’s home, comparison of care received vs. benchmarked care, placing focus on the patient perspective.
The mapping of individual patient journeys may take place during data collection with the use of mapping templates (tables, diagrams, and figures) and/or later in the analysis phase with the use of inductive or deductive analysis, mapping tables, or frameworks. These have been characterized and visually represented in a recent scoping review. 3 Representations of patient journeys can also be constructed through a secondary analysis of previously collected data. In these instances, qualitative data (i.e. interviews and focus group transcripts) have been re-analysed to understand whether a patient journey narrative can be extracted and reported. Undertaking these projects triggers a new research cycle involving the six steps outlined in the Central illustration . The difference in these instances is that the data are already collected for Step 5.
Report findings, disseminate findings, and take action on findings
A standardized, formal reporting guideline for patient journey mapping research does not currently exist. As argued in Davies et al ., 3 a dedicated reporting guide for patient journey mapping would be ill-advised, given the diversity of approaches and methods that have been adopted in this field. Our recommendation is for projects to be reported in accordance with formal guidelines that best align with the research methods that have been adopted. For example, COREQ may be used for patient journey mapping where qualitative methods have been used. 20 STROBE may be used for patient journey mapping where quantitative methods have been used. 21 Whichever methods have been adopted, reporting of projects should be transparent, rigorous, and contain enough detail to the extent that the principles of transparency, trustworthiness, and reproducibility are upheld. 3
Dissemination of research findings needs to include the research, healthcare, and broader communities. Dissemination methods may include academic publications, conference presentations, and communication with relevant stakeholders including healthcare professionals, policymakers, and patient advocacy groups. Based on the findings and identified insights, stakeholders can collaboratively design and implement interventions, programmes, or improvements in healthcare delivery that overcome the identified challenges directly and address and improve the overall patient experience. This cyclical process can hopefully produce research that not only informs but also leads to tangible improvements in healthcare practice and policy.
Patient journey mapping is typically a hands-on process, relying on surveys, interviews, and observational research. The technology that supports this research has, to date, included word processing software, and data analysis packages, such as NVivo, SPSS, and Stata. With the advent of more sophisticated technological tools, such as electronic health records, data analytics programmes, and patient tracking systems, healthcare providers and researchers can potentially use this technology to complement and enhance patient journey mapping research. 19 , 20 , 22 There are existing examples where technology has been harnessed in patient journey. Lee et al . used patient journey mapping to verify disease treatment data from the perspective of the patient, and then the authors developed a mobile prototype that organizes and visualizes personal health information according to the patient-centred journey map. They used a visualization approach for analysing medical information in personal health management and examined the medical information representation of seven mobile health apps that were used by patients and individuals. The apps provide easy access to patient health information; they primarily import data from the hospital database, without the need for patients to create their own medical records and information. 23
In another example, Wauben et al. 19 used radio frequency identification technology (a wireless system that is able to track a patient journey), as a component of their patient journey mapping project, to track surgical day care patients to increase patient flow, reduce wait times, and improve patient and staff satisfaction.
Patient journey mapping has emerged as a valuable research methodology in healthcare, providing a comprehensive and patient-centric approach to understanding the entire spectrum of a patient’s experience within the healthcare system. Future implications of this methodology are promising, particularly for transforming and redesigning healthcare delivery and improving patient outcomes. The impact may be most profound in the following key areas:
Personalized, patient-centred care : The methodology allows healthcare providers to gain deep insights into individual patient experiences. This information can be leveraged to deliver personalized, patient-centric care, based on the needs, values, and preferences of each patient, and aligned with guideline recommendations, healthcare professionals can tailor interventions and treatment plans to optimize patient and clinical outcomes.
Enhanced communication, collaboration, and co-design : Mapping patient interactions with health professionals and journeys within and across health services enables specific gaps in communication and collaboration to be highlighted and potentially informs responsive strategies for improvement. Ideally, these strategies would be co-designed with patients and health professionals, leading to improved care co-ordination and healthcare experience and outcomes.
Patient engagement and empowerment : When patients are invited to share their health journey experiences, and see visual or written representations of their journeys, they may come to understand their own health situation more deeply. Potentially, this may lead to increased health literacy, renewed adherence to treatment plans, and/or self-management of chronic conditions such as cardiovascular disease. Given these benefits, we recommend that patients be provided with the findings of research and quality improvement projects with which they are involved, to close the loop, and to ensure that the findings are appropriately disseminated.
Patient journey mapping is an emerging field of research. Methods used in patient journey mapping projects have varied quite significantly; however, there are common research processes that can be followed to produce high-quality, insightful, and valuable research outputs. Insights gained from patient journey mapping can facilitate the identification of areas for enhancement within healthcare systems and inform the design of patient-centric solutions that prioritize the quality of care and patient outcomes, and patient satisfaction. Using patient journey mapping research can enable healthcare providers to forge stronger patient–provider relationships and co-design improved health service quality, patient experiences, and outcomes.
None declared.
Farmer J , Bigby C , Davis H , Carlisle K , Kenny A , Huysmans R , et al. The state of health services partnering with consumers: evidence from an online survey of Australian health services . BMC Health Serv Res 2018 ; 18 : 628 .
Google Scholar
Kelly J , Dwyer J , Mackean T , O’Donnell K , Willis E . Coproducing Aboriginal patient journey mapping tools for improved quality and coordination of care . Aust J Prim Health 2017 ; 23 : 536 – 542 .
Davies EL , Bulto LN , Walsh A , Pollock D , Langton VM , Laing RE , et al. Reporting and conducting patient journey mapping research in healthcare: a scoping review . J Adv Nurs 2023 ; 79 : 83 – 100 .
Ly S , Runacres F , Poon P . Journey mapping as a novel approach to healthcare: a qualitative mixed methods study in palliative care . BMC Health Serv Res 2021 ; 21 : 915 .
Arias M , Rojas E , Aguirre S , Cornejo F , Munoz-Gama J , Sepúlveda M , et al. Mapping the patient’s journey in healthcare through process mining . Int J Environ Res Public Health 2020 ; 17 : 6586 .
Natale V , Pruette C , Gerohristodoulos K , Scheimann A , Allen L , Kim JM , et al. Journey mapping to improve patient-family experience and teamwork: applying a systems thinking tool to a pediatric ambulatory clinic . Qual Manag Health Care 2023 ; 32 : 61 – 64 .
Cherif E , Martin-Verdier E , Rochette C . Investigating the healthcare pathway through patients’ experience and profiles: implications for breast cancer healthcare providers . BMC Health Serv Res 2020 ; 20 : 735 .
Gilburt H , Drummond C , Sinclair J . Navigating the alcohol treatment pathway: a qualitative study from the service users’ perspective . Alcohol Alcohol 2015 ; 50 : 444 – 450 .
Gichuhi S , Kabiru J , M’Bongo Zindamoyen A , Rono H , Ollando E , Wachira J , et al. Delay along the care-seeking journey of patients with ocular surface squamous neoplasia in Kenya . BMC Health Serv Res 2017 ; 17 : 485 .
Borycki EM , Kushniruk AW , Wagner E , Kletke R . Patient journey mapping: integrating digital technologies into the journey . Knowl Manag E-Learn 2020 ; 12 : 521 – 535 .
Barton E , Freeman T , Baum F , Javanparast S , Lawless A . The feasibility and potential use of case-tracked client journeys in primary healthcare: a pilot study . BMJ Open 2019 ; 9 : e024419 .
Bearnot B , Mitton JA . “You’re always jumping through hoops”: journey mapping the care experiences of individuals with opioid use disorder-associated endocarditis . J Addict Med 2020 ; 14 : 494 – 501 .
Cunnington MS , Plummer CJ , McDiarmid AK , McComb JM . The patient journey from symptom onset to pacemaker implantation . QJM 2008 ; 101 : 955 – 960 .
Geerse C , van Slobbe C , van Triet E , Simonse L . Design of a care pathway for preventive blood pressure monitoring: qualitative study . JMIR Cardio 2019 ; 3 : e13048 .
Laveau F , Hammoudi N , Berthelot E , Belmin J , Assayag P , Cohen A , et al. Patient journey in decompensated heart failure: an analysis in departments of cardiology and geriatrics in the Greater Paris University Hospitals . Arch Cardiovasc Dis 2017 ; 110 : 42 – 50 .
Naheed A , Haldane V , Jafar TH , Chakma N , Legido-Quigley H . Patient pathways and perceptions of treatment, management, and control Bangladesh: a qualitative study . Patient Prefer Adherence 2018 ; 12 : 1437 – 1449 .
Bateman S , Arnold-Chamney M , Jesudason S , Lester R , McDonald S , O’Donnell K , et al. Real ways of working together: co-creating meaningful Aboriginal community consultations to advance kidney care . Aust N Z J Public Health 2022 ; 46 : 614 – 621 .
Greenhalgh T , Hinton L , Finlay T , Macfarlane A , Fahy N , Clyde B , et al. Frameworks for supporting patient and public involvement in research: systematic review and co-design pilot . Health Expect 2019 ; 22 : 785 – 801 .
Wauben LSGL , Guédon ACP , de Korne DF , van den Dobbelsteen JJ . Tracking surgical day care patients using RFID technology . BMJ Innov 2015 ; 1 : 59 – 66 .
Tong A , Sainsbury P , Craig J . Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups . Int J Qual Health Care 2007 ; 19 : 349 – 357 .
von Elm E , Altman DG , Egger M , Pocock SJ , Gøtzsche PC , Vandenbroucke JP , et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies . Lancet 2007 ; 370 (9596): 1453 – 1457 .
Wilson A , Mackean T , Withall L , Willis EM , Pearson O , Hayes C , et al. Protocols for an Aboriginal-led, multi-methods study of the role of Aboriginal and Torres Strait Islander health workers, practitioners and Liaison officers in quality acute health care . J Aust Indigenous HealthInfoNet 2022 ; 3 : 1 – 15 .
Lee B , Lee J , Cho Y , Shin Y , Oh C , Park H , et al. Visualisation of information using patient journey maps for a mobile health application . Appl Sci 2023 ; 13 : 6067 .
Author notes
Email alerts, citing articles via.
- Recommend to Your Librarian
- Advertising and Corporate Services
- Journals Career Network
Affiliations
- Online ISSN 1873-1953
- Print ISSN 1474-5151
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
ORIGINAL RESEARCH article
Unmet needs of people with epilepsy: a qualitative study exploring their journey from presentation to long-term management across five european countries.

- 1 OPEN Health Communications LLP, Marlow, Buckinghamshire, United Kingdom
- 2 Eisai Europe Ltd, Hatfield, United Kingdom
Introduction: Epilepsy is a neurological disease that can negatively impact a person’s physical, psychological, social, and emotional well-being. The aim of this study was to provide insights into the experiences of people with epilepsy on polytherapy (i.e., people on a combination of two or more anti-seizure medications [ASMs]), with an emphasis on their emotional journey.
Methods: Market research was conducted with 40 people with epilepsy from France, Germany, Italy, Spain, and the United Kingdom. Semi-structured interviews were analyzed using both a content and framework analysis approach. A content analysis of participants’ expressed emotions was used to illustrate the changes of emotions experienced by people with epilepsy from presentation through to monitoring and follow-up stages.
Results: In each stage of the journey, themes and subthemes were identified under the overarching headings: Stage 1: Presentation – Life is turned upside down; Stage 2: Diagnosis – Period of learning; Stage 3: Treatment – Aspirations and experimentation; and Stage 4: Monitoring and follow-up – Feeling “out on a limb”. The research identified key unmet needs and opportunities for people with epilepsy to improve their subjective experiences at different stages of their disease journey, namely: (1) establish and promote support networks from presentation through to monitoring and follow-up stages; (2) accelerate pathway to diagnosis; (3) provide opportunities to discuss the diagnosis with patients; (4) clarify treatment-change guidelines for patients; and (5) develop a shared treatment decision-making/empowerment tool.
Discussion: The research findings and recommendations have the potential to drive change at an individual level, as well as at a healthcare level.
1. Introduction
Epilepsy is one of the most common and debilitating neurological conditions, and it has been estimated to affect between 50 and 75 million people globally ( 1 , 2 ). The daily burden for people with epilepsy who experience epileptic seizures and accompanying symptoms remains high, despite advances in understanding pathophysiological disease mechanisms and treatment options ( 3 ). As well as the physical implications of epilepsy, such as disability, mortality, and comorbidities, the disease can also impact the psychological well-being and social aspects of peoples’ lives, including work, personal relationships, and quality of life (QoL) ( 4 ). Previous research has shown that emotions are closely related to the health and well-being of people with chronic disease ( 5 ), yet emotions are often overlooked in the literature reporting the subjective experience of people with epilepsy ( 6 ).
There are several qualitative and mixed-method research studies that have investigated patients’ subjective experiences (thoughts and feelings) of being diagnosed and living with epilepsy ( 7–17 ). The pathway to adjustment following a first seizure can trigger psychological concerns/issues, often stemming from the person’s perceived loss of control ( 16 ). Loss of control is an area of impact of living with epilepsy frequently reported in the qualitative literature. It impacted not only adults, but also children and adolescents, and was reported to be connected to fear of seizure recurrence, loss of control over their own bodies, as well as disruption to personal goals and plans ( 17 ). How quickly a person was able to adapt and re-establish perceived control following diagnosis could depend on their gender and clinical factors (e.g., presence of premorbid psychological disorder) ( 16 ). For example, people who were evaluated to have experienced a pervasive loss of control were thought to have a higher awareness of their own vulnerability and mortality, and have a higher fear of seizure recurrence and mood disturbances. They consequently needed to use more extensive strategies and external support to help them return to baseline levels of perceived control compared with those experiencing a limited loss of control following diagnosis ( 16 ).
Yennadiou and Wolverson ( 17 ), investigated how people of advanced age (more than 65 years) make sense of their epilepsy, and found that they appraised epilepsy as a powerful negative external force that is both threatening and unpredictable, yet perceived as separate from themselves. They also experienced loss of control, loss of independence, and difficulties dealing with stigma ( 17 ). Within this literature, social stigma is a common theme ( 10 , 11 , 17 ). Social stigma and persistent public misperceptions about epilepsy (e.g., the public perception that people with epilepsy are “possessed”), could have a disruptive effect on the person’s self-identity ( 10 ). Stigma could also impact a person’s self-esteem and social standing ( 10 ).
The findings illustrate the rich insights that qualitative accounts can provide, and how such techniques are invaluable when little is known about a particular issue or topic.
The current study was carried out as part of a wider program of research that aimed to provide a comprehensive, qualitative overview of the journey of living with epilepsy. The first step was a qualitative netnographic study of conversations posted on public social media sites relating to living with epilepsy ( 18 ). The analysis of these conversations identified key themes, namely: a lack of disease awareness among the public; the negative psychological and physical impact of seizures; the importance of ensuring appropriate sleep duration and quality; a tendency to understand disease burden through time (e.g., people with epilepsy were more likely to use the term “days” when describing negative experiences and “years” when describing positive experiences, especially when they were referring to treatment); the challenge of finding the right treatment and managing side effects; and the challenge of dealing with depression and anxiety ( 18 ). This was followed by a review of the published literature, reporting the emotional and clinical pathway of people with epilepsy and their carers (unpublished). This review identified themes relating to the impact of the relationship with a healthcare professional; stigma and how it can impact a person’s identity and self-esteem; the negative impact of epilepsy on everyday life/QoL; the experience and impact of seizures, symptoms, and treatment; a loss of independence; and mental health issues. Both pieces of research have highlighted that people with epilepsy have difficulties when first-line monotherapy treatment is not successful. This finding was supported by a recent published ethnographic study that explored the experiences of people who had either been diagnosed with drug-resistant epilepsy or had tried two or more anti-seizure medications (ASMs) without perceived success ( 19 ). The authors identified patient–provider gaps in both epilepsy and drug-resistant epilepsy treatment and management, and discovered that there was a negative impact of untimely disease management leading up to and after receiving a drug-resistant epilepsy diagnosis.
In this study, we recruited people for whom first-line monotherapy alone was not successful, and who were currently on a combination of two or more ASMs. Selecting this cohort of people with epilepsy, allowed us to not only identify the psychosocial consequences of epilepsy as they progressed through their clinical journey, but also to deep dive into the potential issues that can arise at the treatment and monitoring stages when monotherapy is not successful. To the best of our knowledge, the current study is the first to examine the experiential journey of people with epilepsy from the perspective of those on polytherapy, with a specific emphasis on their subjective experiences.
The aim of this study was to identify and raise awareness of the challenges and unmet needs faced by patients living with epilepsy on polytherapy in five European countries, and to identify opportunities to address those unmet needs.
The objectives were to:
a. Understand the subjective experiences of patients living with epilepsy and how these experiences may change over the duration of the patient journey from presentation through to ASM treatment, and ASM treatment monitoring and follow-up stages
b. Identify the impact these experiences have on patients’ everyday QoL (e.g., work life and relationships) and psychological well-being (e.g., emotions and mental health)
c. Identify patients’ unmet needs at each stage of the patient journey and recommend opportunities to address those.
2. Materials and methods
2.1. study design.
Semi-structured interviews were conducted to explore the participants’ subjective experiences; for example, emotions (mental states brought on by neurophysiological changes, variously associated with thoughts, feelings, behavioral responses, and a degree of pleasure or displeasure) ( 20 , 21 ), and feelings (a conscious experience created after the physical sensation or emotional experience) at each stage of the clinical journey ( 22 , 23 ). This study was conducted as market research; therefore, ethical approval was not required. Codes of conduct/guidance for the (pharmaceutical) market research industry, including the British Healthcare Business Intelligence Association and the European Pharmaceutical Market Research Association were strictly followed. A team of market researchers and health psychologists, who are experts in strategic patient innovation and engagement, worked in conjunction with senior staff from a pharmaceutical company to design the study and analyze the qualitative research.
2.2. Participants and sampling procedures
A third-party recruitment company was used to recruit participants within the predefined criteria as follows:
1. Live in France, Germany, Italy, Spain, or the United Kingdom (UK)
2. Aged more than 18 years old
3. Diagnosed with epilepsy
4. Currently on an ASM combination adjunctive therapy for their epilepsy (i.e., at least on two ASMs, regardless of the disease duration and number of ASMs used previously)
5. Comfortable to talk about their personal experiences of being diagnosed with epilepsy and living with the condition – particularly around the emotions felt at different stages
In the context of this research area, we have defined polytherapy to mean when first-line monotherapy alone was not successful.
2.3. Interview procedure
Participants were invited to take part in a market research study about their experiences of being diagnosed with epilepsy and living with the condition, with a focus on their emotional experiences.
The interview topic guide was developed in English by the research team, and all United Kingdom interviews were moderated by the same team of researchers. Interview topic guides were then translated into French, German, Italian, or Spanish by native speakers through a third-party contracted recruitment company, and interviews in each of the four non-English speaking countries were carried out by local language moderators. The third-party were also responsible for recruiting participants from all five countries according to the pre-established inclusion criteria. Interviews were conducted via a web-assisted platform (Microsoft Teams) and lasted 60 min on average. All 40 interviews were recorded with permission and transcribed. Microsoft Excel was used to store, manage, and carry out the analysis of interview transcripts. Before the interview commenced, participants were read an introduction to the study, which provided details of (1) the study procedure; (2) confidentiality; (3) the right to withdraw or to refuse to answer any questions; and (4) the need for reporting adverse events. The interview topic guide is described in Table 1 .
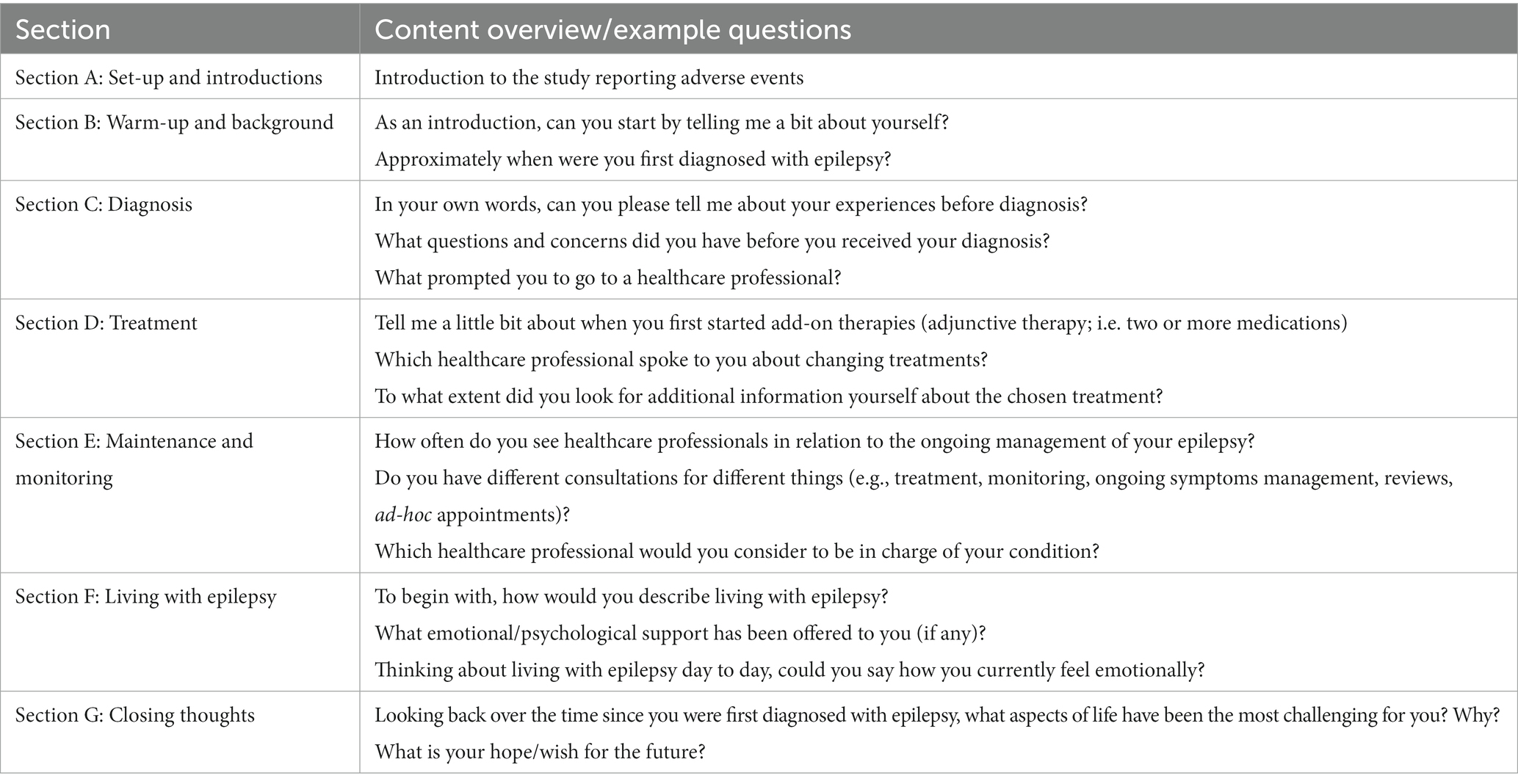
Table 1 . Interview structure and examples of questions from the topic guide.
2.4. Data extraction and analysis
We followed a combined framework and content analysis approach. Framework analysis is a comparative form of thematic analysis using a structure of inductively and deductively derived themes, and is a popular approach primarily used in applied research ( 24 ). It is particularly suitable when there are more than one researcher analyzing the data, as it sets out a systematic method to data analysis, and can be adapted for use with both an inductive and deductive type of qualitative analysis ( 25 ). The framework approach used in the current study incorporated three core steps: (1) deductive analysis (coding data into the stages of a predefined epilepsy clinical journey map, which was initially based on clinical guidelines for each of the included countries); (2) content analysis (to identify emotions within the patient journey); and (3) inductive analysis (an in-depth thematic analysis of the participants’ accounts within each stage of the patient journey).
2.4.1. Step 1: Identifying the clinical patient journey (deductive analysis)
The first step was the development of a map representing the distinct stages of a clinical journey in epilepsy, from presentation through to monitoring and follow-up stages. This was developed using insights derived from existing literature contained in clinical guidelines reporting the patient pathway within the five countries included in the research ( 26–30 ), as well as insights from the current research.
Quotes, extracted from the interview transcripts, were coded according to which stage of the clinical map they were evaluated to represent.
2.4.2. Step 2: Identifying emotions within the patient journey (content analysis)
Content analysis of emotional expressions used by participants (positive or negative) was conducted. Similar emotions or emotional impact that were described or mentioned by the patients using different words were extracted from the interviews and grouped together, and an overarching emotional label was assigned by three health psychologists by consensus. For example, words/terms such as “nervous,” “anxious,” “tense,” “worried,” “scared,” or “afraid” would be grouped under the emotional label “fear,” or words/terms such as “understanding,” “reassured,” or “trusting” would be grouped under the label “reassured.” All overarching emotional labels (e.g., those that were reported by one or more participants) within each clinical stage (Step 1) were positioned on the Y axis of the map in descending order, starting with what was assigned by the research team (by consensus) to be the most positive (i.e., acceptance) down to the emotional label evaluated to be the least positive (i.e., anxious). The overarching emotional labels for each clinical stage were then visually mapped onto the correct coordinates of the graph/map (e.g., where the two points between the clinical stage [X axis] and the emotional label [Y axis] meet [the origin]).
2.4.3. Step 3: Conducting an in-depth thematic analysis of patient experiences (inductive analysis)
Thematic analysis was used to explore participants’ experiences and to identify key emerging challenges and unmet needs ( 31 , 32 ). Extracted data (i.e., any patient quotes relating to the impact of epilepsy on everyday life or insights into the patients’ subjective experience of living with epilepsy and/or their mental health) were examined and sorted within each prespecified stage of the clinical journey (e.g., presentation, diagnosis, and treatment), to synthesize and identify emerging content themes. Initial theme labels (describing broad content themes), and where relevant, sub-theme labels (nested within content themes) were then generated for each cluster of similar data to express these shared experiences.
3.1. Participant characteristics
Forty participants were recruited in total, eight from each of the participating countries (France, Germany, Italy, Spain, and the United Kingdom). All participants were adults at the time of the interview, aged 18–65 years. Life stage of diagnosis varied, with some diagnosed in infancy/childhood and others in adulthood. Participants’ time of diagnosis spanned four decades from the 1980s up until the 2020s. Presentation also varied; participants reported experiencing several seizure types, including: absence, tonic–clonic, focal (aware and unaware), and myoclonic ( Table 2 ). All participants were on polytherapy.
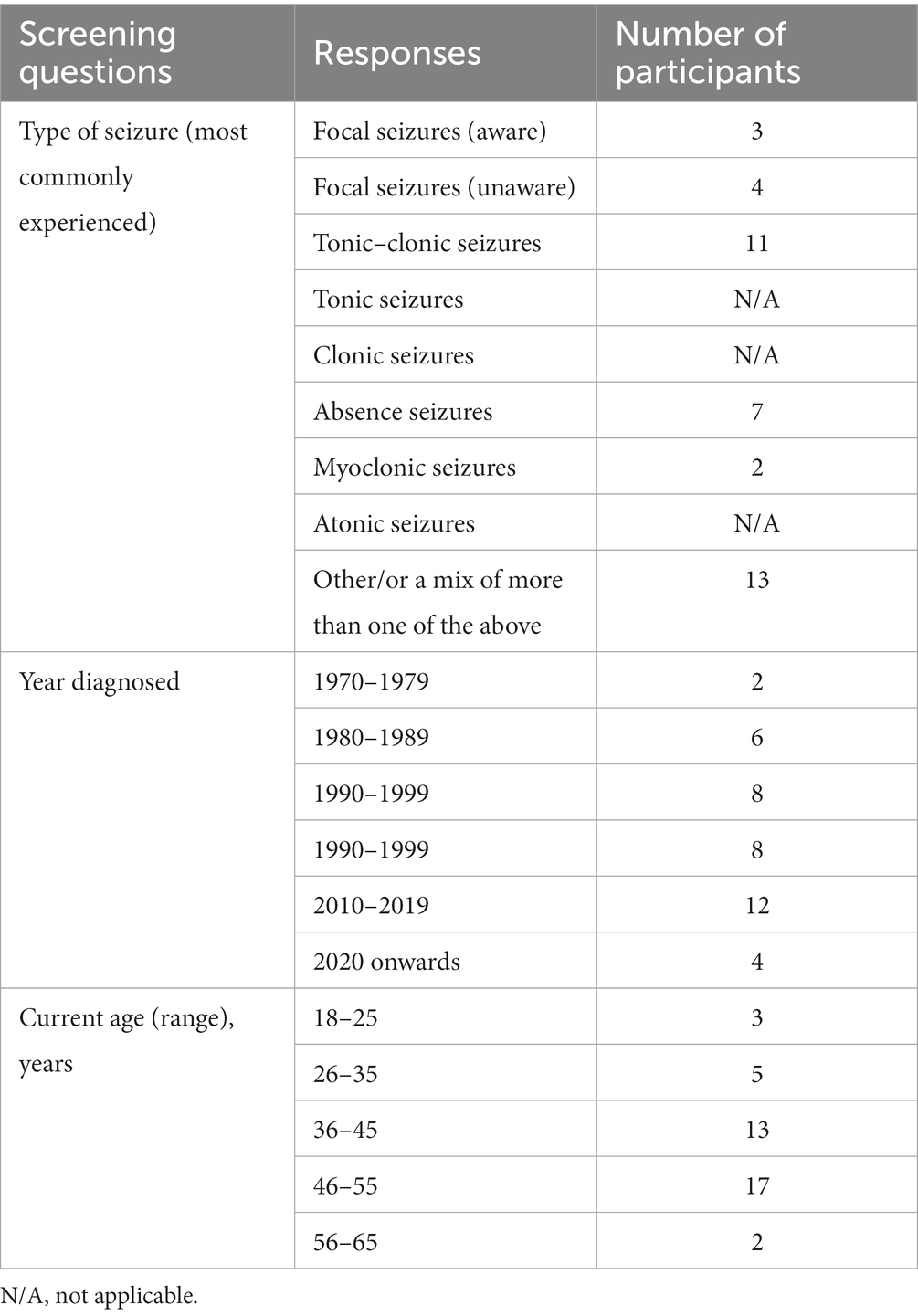
Table 2 . Participant characteristics.
3.2. Clinical patient journey map
Figure 1 displays the distinct clinical stages of the disease journey for people with epilepsy in Europe, from presentation through to monitoring and follow-up stages. The journey is not always a linear one; it can vary significantly between people with epilepsy, with some people not progressing through the different stages.
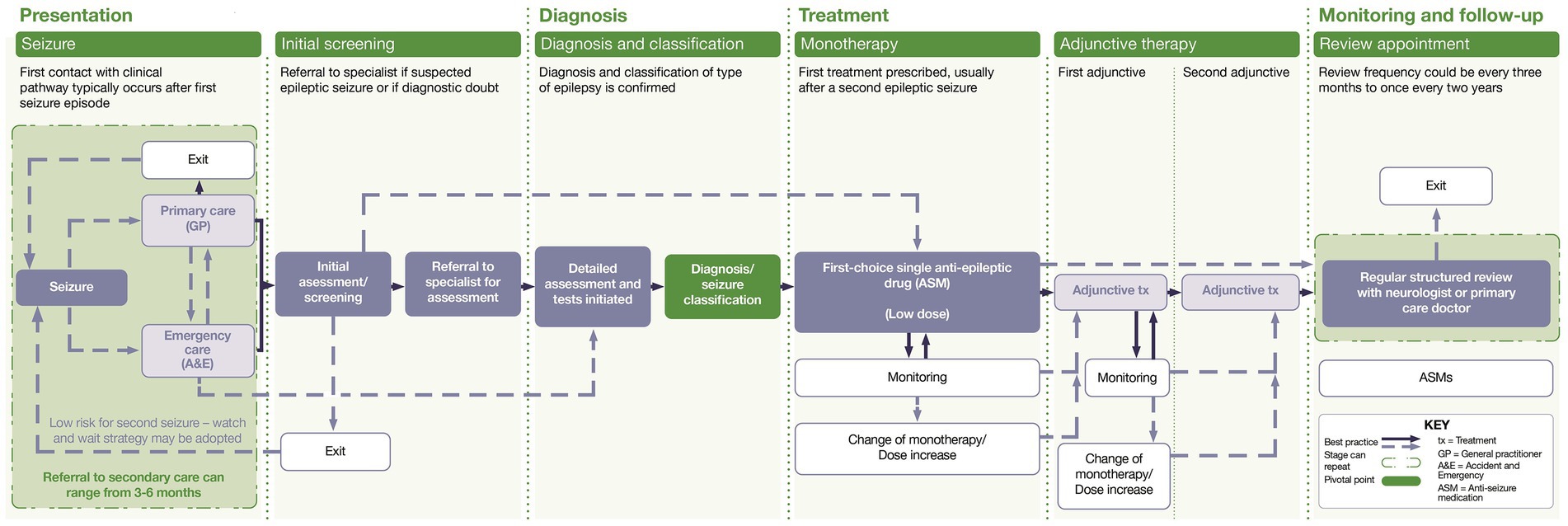
Figure 1 . Clinical journey map.
3.3. Emotional patient journey map
Figure 2 illustrates an aggregated emotional journey map developed from the participants’ reported emotions at each stage of the clinical journey. The lines that join the different emotions, do so only to illustrate the extent of the highs and lows of emotions that can be experienced. This emotional journey map is an aggregate of the emotional experiences of participants, and does not mean that all people with epilepsy experienced all these emotions, nor does it mean that these are the only emotions that each participant expressed or experienced. Furthermore, it does not mean that the emotions were experienced in a set order from one emotion to the next. However, it does illustrate how the participants may experience the same or similar emotions at different stages of the journey, or experience both positive emotions (e.g., gratitude) and negative emotions (e.g., frustration) within the same stage of the journey (e.g., treatment [first choice]). The emotional journey map therefore illustrates the emotional rollercoaster that people with epilepsy can experience.
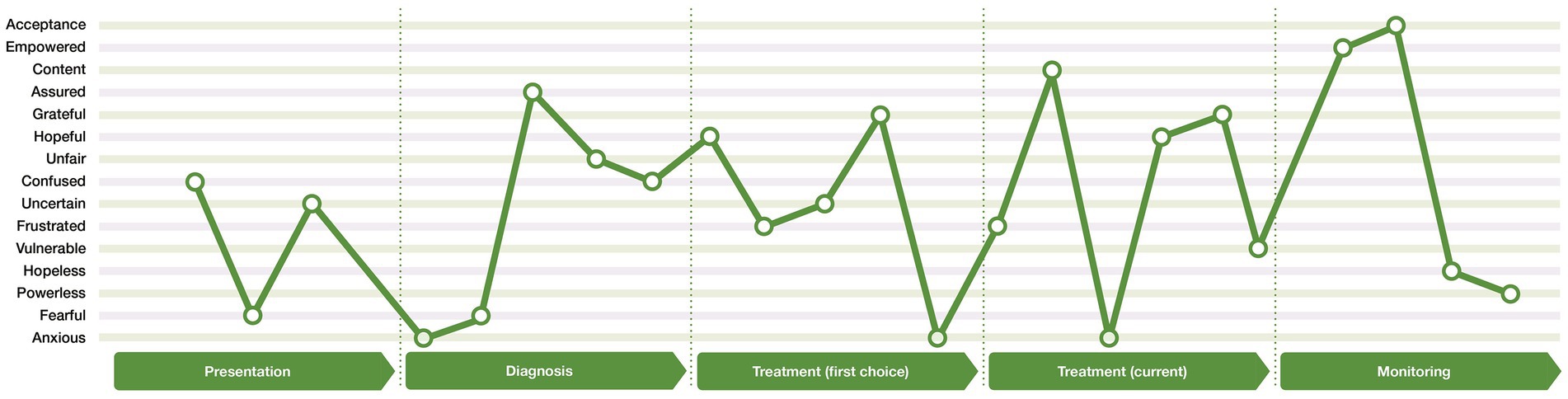
Figure 2 . Emotional journey map.
3.4. Thematic analysis within the journey stage
Data (e.g., patient quotes) from each of the 40 interviews were extracted and coded into the most relevant section within the clinical map framework ( Table 3 ). Due to analyzing the patient experience per journey stage, similar themes may occur in more than one stage (e.g., feelings of uncertainty or the impact of the doctor-patient relationship).
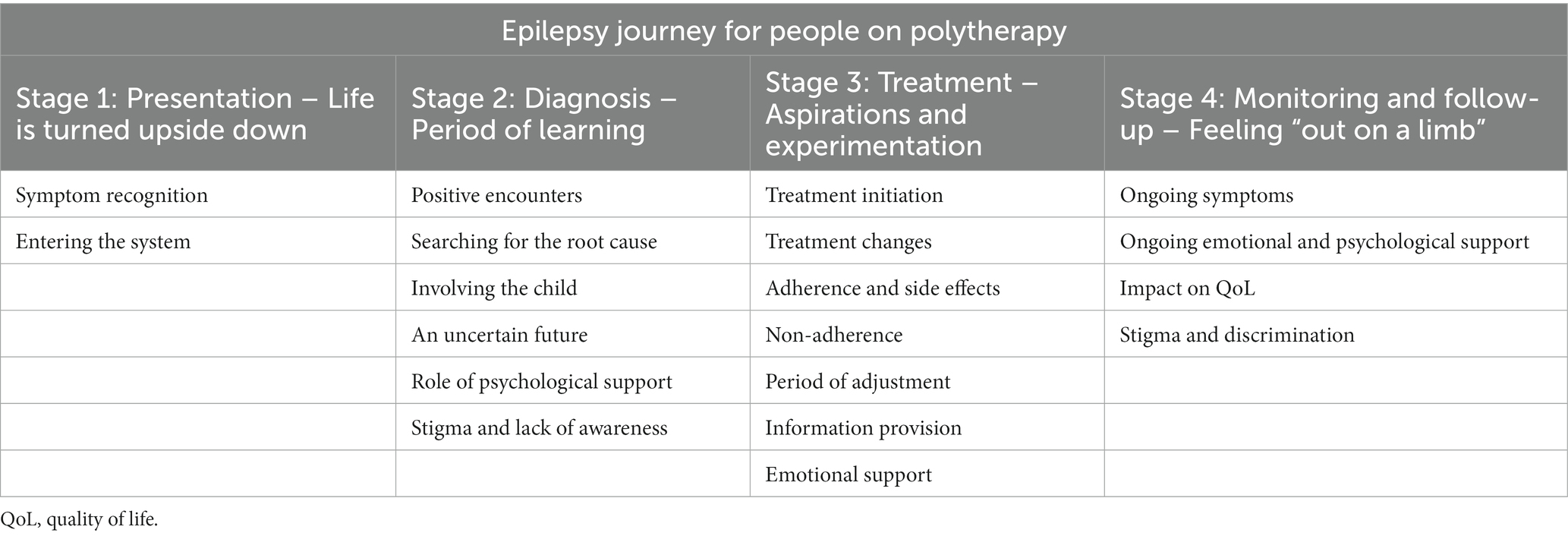
Table 3 . Themes and sub-themes within each of the four clinical stages of the epilepsy journey.
3.4.1. Stage 1: Presentation – Life is turned upside down
3.4.1.1. high variability of symptoms contributes to a lack of symptom recognition.
The unique symptomology of seizures meant that the way participants first presented varied from person to person. For many, their first seizure happened spontaneously, and occasionally, in a dangerous situation (e.g., in the bath). Others reported having symptoms before their first seizure, including fainting, headaches, sweating, jerks, and phantom odors and tastes.
There was a low awareness of the symptoms of epilepsy among many of the participants; for example, many had only heard of tonic–clonic seizures, and did not recognize the signs of other types of seizures. Seizures accompanied by loss of consciousness might have initially been attributed to fainting, stress, or low blood pressure, and were usually recognized as a symptom of epilepsy in hindsight, post diagnosis.
“It started with a shaking and twitching of My leg. I could Not control It. First, I thought it was because of overstraining. I did not think of epilepsy...” [participant 4.1, Germany]
3.4.1.2. Challenges of entering the system cause confusion and fear
Participants were either taken to the emergency department following a first seizure or to their family practitioner/general practitioner, dependent on presentation; for example, people who experienced absences and loss of consciousness, usually saw their primary care provider, whereas those with other types of seizures went to the hospital. The participants that were taken into the emergency department were often left confused about their possible diagnosis and feared the potential outcome.
“…very nervous, anxious, tense, and worried. I was an emotional wreck. I did not know what was happening, why I was hospitalized, what they were doing.” [Participant 3.3, Spain]
Most participants who were diagnosed as children could not remember their life experiences pre diagnosis, but remembered feeling sad, scared, and being unsure of the reason for their tests/scans. Many were concerned about being different from their peers, and anticipated peer rejection. Participants who were children at this stage, reported that they had missed school and experienced disruption in their social life because of initial testing and treatment.
Participants who were adults when they had their initial investigations, experienced anxiety in anticipation of the outcome of their diagnosis; for example, concerns were often related to their belief that they were experiencing a stroke or psychosis, or had a tumor or cancer. Delays in diagnosis left them with feelings of uncertainty and a lack of information about their seizures and their management.
At this stage, participants reported significant disruption to their lives. They had feelings of being “out of control” and being debilitated by the lack of certainty around their daily lives.
“…it came very suddenly; it was a drastic change, and shock, no longer able to drive, to continue ‘a normal life’.” [Participant 1.1, UK]
Furthermore, participants recalled being confused while in the hospital and unable to remember what the healthcare professional had explained.
“[I] didn’t understand what was happening to me, I felt like I was going crazy.” [Participant 2.3, Italy]
3.4.2. Stage 2: Diagnosis – Period of learning
3.4.2.1. positive encounters with healthcare professionals drive emotional well-being.
Positive diagnostic experiences were characterized by positive encounters with neurologists/epileptologists, highlighting the importance of this relationship. Participants who spent more time with their neurologist/epileptologist felt they had the information needed to understand their epilepsy. Participants generally had frequent appointments at this stage, and relied on and trusted their neurologist/epileptologist. Those who felt reassured and supported by their core healthcare professional, were able to adapt and adjust to their diagnosis.
“I did feel supported; I had a very quick appointment, didn't feel left on my own […] high confidence towards my neurologist.” [Participant 1.1, UK]
“She [my neurologist] explains things so that everyone can understand […], and she is also able to take away the fear and panic.” [Participant 4.4, Germany]
Participants highlighted that meeting others with epilepsy at diagnosis would have benefitted them, but they did not always get the opportunity. Participants who were able to meet others with epilepsy while in hospital felt less alone.
“ I would have appreciated meeting fellow patients to learn and know what living with epilepsy is like.” [Participant 3.5, Spain]
3.4.2.2. Difficulties understanding the epilepsy diagnosis
Participants wanted to know the cause of their epilepsy. Healthcare professionals’ explanations of the diagnosis were often complex and hard to understand, with many wanting the neurologist/epileptologist to “come down to their level.” They felt that a dedicated healthcare professional who could speak to them on a personal level, consider social aspects of their life, and spend time to reassure and discuss information with, would have been beneficial. Not understanding the cause and diagnosis triggered frustration.
“[…] but the main question is the real root cause of the epilepsy. I had it for 35 years and I would like to know the origins of it.” [Participant 5.5, France]
3.4.2.3. The importance of the caregiver
For participants diagnosed in childhood, parents and caregivers had been their main source of information. Involving the child in the diagnostic process by helping them in understanding their illness, was recommended as a strategy to reduce their confusion.
“It would be good to involve children directly or as early as possible, as their parents might not do it, as in my case.” [Participant 4.7, Germany]
3.4.2.4. Uncertainty about the future causes frustration and worry
There was little opportunity to explore what the diagnosis meant for the participants’ day-to-day life. Participants had questions about repeated seizures and the possibility of brain damage. Many felt that the discussions with healthcare professionals and information provided to them focused on what the person should avoid, instead of what they were still able to do, and some of the terminology used could be perceived as scary. Participants were unsure about their future ability to drive, have children, drink alcohol, and continue to work. This left them feeling overwhelmed, shocked, and with a sense of injustice, from epilepsy stripping them of future opportunities.
“It was all very overwhelming because it was a list of things I could not do, rather than reassuring.” [Participant 3.8, Spain]
“I was shocked when I was told that I could not continue my apprenticeship as a carpenter, as it involves the handling of machines.” [Participant 4.5, Germany]
“…before the diagnosis, I had a life full of sporting initiatives, of dreams to realize; all this collapsed after the diagnosis.” [Participant 2.7, Italy]
“I was told that I had a ‘mini storm’ in my mind, which I find extremely scary.” [Participant 5.2, France]
3.4.2.5. Role of psychological support
Experiencing mental health issues was common, as many of the participants expressed difficulty adjusting to their diagnosis, including panic attacks, anxiety, and depression. Those who were offered psychological tools and support by their healthcare professionals found it helpful, but others had to look for support from psychologists outside the hospital. Some deemed professional support unnecessary for them personally, however, retrospectively felt that they would have benefitted from support. Outside the healthcare setting, a strong family network could help people cope with mental health issues and their diagnosis.
“I had panic attacks, anxiety, depression, and all that was totally overlooked.” [Participant 3.5, Spain]
“It would have been nice to have it. Now looking back, I realize that they [healthcare professionals] take for granted that you are mature enough to digest everything they tell you. And I was not.” [Participant 3.8, Spain]
3.4.2.6. Stigma and lack of awareness
Stigma was reported to come from multiple sources, including healthcare professionals, friends, family, peers, and the public. Participants reported feeling fearful or embarrassed by public perceptions of epilepsy, and felt that there was a lack of awareness of the condition and its symptoms.
“Someone affected by epilepsy doesn’t only suffer from the condition itself, but also from the lack of education of everybody else around them.” [Participant 2.1, Italy]
3.4.3. Stage 3: Treatment – Aspirations and experimentation
3.4.3.1. treatment initiation is associated with hope and uncertainty.
Participants were generally initiated onto a single, low-dose ASM (monotherapy) following diagnosis. Treatment aims ranged from reducing the number and/or intensity of seizures to eliminating them entirely, with little to no medication side effects. Participants’ expectations were therefore often optimistic, and they were hopeful they would be able to resume life as before, or at least see an improvement in their QoL. This sense of hope and optimism was often accompanied by a sense of uncertainty about the future, as participants were aware there was no guarantee that their first-line monotherapy treatment would work or continue to work for them in the long term. Those with a good treatment response, on their current treatment, were able to return to their daily routine, and expressed gratitude that they had experienced respite from seizures.
“I hoped that this would have been the right one…” [Participant 1.6, UK]
“I hoped [with treatment] to have a normal life, be able to work again. Not be dependent on welfare.” [Participant 4.8, Germany]
“[…] they were very vague, saying that I could have a seizure tomorrow, next week, next year or never.” [Participant 3.3, Spain]
“I have not had a seizure in years… No longer on the verge of the cliff.” [Participant 3.1, Spain]

3.4.3.2. Treatment changes can cause confusion
Whether the participant remained on the prescribed treatment regimen, depended on the outcome of the regular review (clinical monitoring and an assessment of the impact of epilepsy and medication on the person’s daily life). If the frequency/intensity of seizures did not improve, there was a drop in effectiveness over time (e.g., months or years), or the person did not tolerate the treatment, then a trial-and-error approach was taken. This process, decided by the participant’s assigned neurologist/epileptologist, involved a gradual increase of the current ASM dose, a new single ASM, or an add-on therapy.
Treatment changes could cause confusion, however, when established on a new treatment regimen, participants felt hopeful that their treatment would be successful in stopping seizures and improving their QoL. They initially felt content in their new therapy, and expressed feeling safe, supported, and confident that they would be seizure free.
While some accepted that they might need to start and stop multiple treatments to reach and maintain control of their epilepsy, others were left with feelings of frustration, disappointment, and hopelessness regarding the possibility of continued treatment failures.
“… it was a bit done by trial and error.” [Participant 5.2, France]
“[I expected] a normal life [from the new treatment regimen]. I expected a better quality of life and not all the side effects.” [Participant 2.1, Italy]
“When I got the present combination, I felt it was a miracle, felt so happy, everything had gone back to normal […] very grateful for it, no negative impact.” [Participant 1.1, UK]
“Now I am so well adjusted that I hardly ever have a seizure, maybe once a year or twice at the most. I am content with my therapy, and I don’t want to switch to another drug.” [Participant 4.7, Germany]
“Every time they [added] a pill, it felt like they were improving the treatment, that I was being better taken care of, and that maybe, one day this will all end.” [Participant 3.3, Spain]
“It was a quite different treatment regimen. [If it were up to me, I would] just want to carry on with my life, free of all the treatments. It was [disappointing] to an extent, because I feel less […] hopeful regarding the treatment options.” [Participant 1.5, UK]
“…I felt unstable. I felt sad and angry… I didn’t feel optimistic because it was very difficult and challenging to move from one drug onto another. That’s because your whole body is [on] this treatment, and it can cause head-spinning episodes, eyesight problems, [anxiety], insomnia … Your whole body is all over the place.” [Participant 2.8, Italy]
3.4.3.3. Side effects impact on QoL
Participants reported experiencing a range of side effects. Those who perceived their medication as the key to controlling their seizures, tended to accept medication side effects as a “price worth paying,” yet others found the side effects hard to live with. Experiencing side effects could prompt the participant to discuss medication changes with their healthcare professional. However, healthcare professionals were not always sympathetic, in particular concerning side effects that were perceived to be less debilitating. Many who experienced medication side effects felt frustrated with the impact they had on their QoL, as well as worried about potential short-term negative consequences.
“It is difficult emotionally, as well as physically, with side effects and issues at the memory level, and the impact on work.” [Participant 1.6, UK]
“I was falling asleep everywhere. I felt I could be robbed.” [Participant 3.2, Spain]
3.4.3.4. Non-adherence caused by concerns and doubts about necessity for treatment
As a consequence of side effects perceived to be intolerable, some skipped doses, experimented with their dosage, or stopped taking their medication altogether to experience temporary relief without consulting their healthcare professional. This non-adherence resulted in hospitalizations for some participants.
Concerns about potential side effects of ASMs were frequent among participants, and with some potential side effects resembling symptoms of the illness itself (e.g., memory loss or fatigue), some participants may have misattributed epilepsy symptoms as side effects (“nocebo effect”). To avoid misattribution, one participant commented that they would not read the patient information leaflet in the medication box.
“The biggest challenge is exhaustion; it can put me in a bad mood, and sometimes I may skip one treatment. Sometimes I need a breather.” [Participant 1.5, UK]
“I stopped treatment for three days to see what the effects would be.” [Participant 5.1, France]
“At the beginning, it was really hard, and taking the treatment was an ordeal […], but I found it really hard to the point that I often just pretended not to have [epilepsy]… At some point, I stopped taking all drugs, until one day, I collapsed and ended up in hospital.” [Participant 2.3, Italy]
“Only months after receiving a new drug treatment, I would read the information leaflet. I did not want to read it prior, as I wanted to be open and not prejudiced.” [Participant 4.6, Germany]
3.4.3.5. Period of adjustment to medication changes
Participants often went through an expected period of adjustment when initiating a new medication regimen. Those that had a good relationship with their healthcare professional, were more likely to have trust or faith in the new medicine. However, if a person experienced a side effect while on a new medication regimen, it could lead to them feeling defeated, despite the quality of the relationship with their healthcare professional.
Add-on therapies could lead to participants experiencing practical medication challenges in their day-to-day lives, such as coping with the number of pills, remembering to take their medication, dealing with physical attributes of the medication (e.g., pill size), and having limited access to certain medications. However, participants often adjusted, and found strategies to help them cope.
“Going from one drug to two was not an issue. I have always trusted her and her decisions. If she said it was the right thing to do…” [Participant 3.1, Spain]
“Every new seizure brings you down…” [Participant 1.1, UK]
“I bought myself a weekly pill box because a couple of times I couldn’t remember whether I’d already taken the pill or not, and this can cause problems… So, I got organized with the weekly pill box.” [Participant 2.2, Italy]
3.4.3.6. Lack of information and conversations about treatment options
While some participants felt satisfied with the depth and quality of information and support they received from their healthcare professionals, others reported the opposite. They often did not receive written information about the current treatment to manage their expectations (i.e., risks and benefits), but instead, were provided with verbal information that they would later forget. Participants reported limited discussion with their neurologist/epileptologist about treatment changes. Although some felt that their opinion was taken into consideration, others did not feel part of the decision-making process, or decided to leave decisions entirely to the neurologist, as they did not feel equipped to contribute.
Participants reported looking for further information via the internet, including patient advisory group websites, patient forums, peer-reviewed journal articles, and drug company websites, to find the information about a specific treatment change. Participants were particularly interested in information about medication side effects and possible treatments for counteracting side effects.
“Very little [information] besides some [verbal] information during phone calls on potential side effects. In general, there is a lack of upfront information.” [Participant 1.2, UK]
“I was not offered options. Her words were ‘I am going to try this’ […] I have always been the kind that blindly follows what the doctor says. I sometimes do not even ask a single question.” [Participant 3.7, Spain]
3.4.3.7. Emotional support
Family members and close friends could be a helpful source of emotional and mental support while participants adjusted to a new medication regimen. For some, the idea of accepting support from outside the family was unthinkable, but most felt that it would have been beneficial to have additional support available from the healthcare system/hospital. Psychological support was rarely offered as part of a treatment package, sometimes resulting in the person feeling abandoned. When it was offered, it was often viewed as inadequate, due to long waiting lists, or it only being offered for a short period without continued support. Psychological support usually involved talking to a healthcare professional, either face to face or via the telephone, about their medication changes, to better manage their expectations and fears between consultations.
“They ask you if you need emotional support. You know, though, that there are no appointments with psychologists until one year later, unless you have something really urgent.” [Participant 4.8, Germany]
“… [I would have liked] having someone to talk to, even just a nurse to process the changes, the expectations, and having a bit [of] conversation.” [Participant 1.3, UK]
3.4.4. Stage 4: Monitoring and follow-up – Feeling “Out On a limb”
3.4.4.1. ongoing symptoms and support.
Fully establishing a satisfactory treatment regimen could take time. Therefore, despite receiving treatment, participants often still reported symptoms of epilepsy and side effects from their medication.
Although some participants felt that they continued to receive good support from their healthcare professionals, others felt neglected and abandoned at this stage due to fewer touchpoints with their specialist team. Those participants reported that their support network was made up mostly of close family and friends, and while some were satisfied with that level of support, others lacked a social support network.
“No support whatsoever. Epilepsy is not regarded as a long-term systemic disease, rather something [patients] ought to manage on their own.” [Participant 1.6, UK]
3.4.4.2. Impact of epilepsy on QoL
Participants reported that their epilepsy had a negative impact on all aspects of their QoL and psychological well-being at some point in their patient journey. All key areas of a participant’s life could be affected long term, including, but not limited to, socializing, sleep quality, working, using transport, and traveling. These functional limitations could leave the person with epilepsy feeling that they had lost their freedom, and depended on others for help and support. Those on a successful treatment regimen, however, reported learning to adapt and beginning to rebuild their lives.
“I would describe it like having a heavy stone on my back. Something heavy and attached to my back that I can’t get rid of, and the more I try to discard it, the more it hangs on to me.” [Participant 2.8, Italy]
“It’s been a huge journey and lots of work has been done. With Depakin®, I became more socially engaged, I studied more, I read more… I went out more often, and I learned to relate to other people again…” [Participant 2.1, Italy]
Personal relationships could be especially challenging, and participants’ social life could feel restricted in several ways. For example, participants reported avoiding to socialize, due to fearing they might get overtired or become exposed to flashing/strobe lights, which could trigger a seizure. Furthermore, they reported that friends did not always understand their condition, and they could no longer relate to their old friends, now that their lives had changed so much. An inability to be spontaneous was another reported barrier to socializing.
“I don’t feel confident enough to [be spontaneous]. For example, if a friend says […]: ‘Do you feel like going out for dinner tonight?’ I think: ‘Oh no, you did not have a nap, did not sleep for [enough hours], and what if you feel tired all of sudden and get a seizure?’. I wouldn't want to put anyone through that.” [Participant 4.8, Germany]
Sleep disorders were frequently reported (e.g., insomnia, sleep apnea, and restless leg syndrome), and lack of sleep could be a trigger for a seizure.
“I got to a point [where] I have to accept epilepsy as part of who I am. Tiredness is horrific, [particularly] with children. I try to sleep in the afternoon – a nap to be able to cope with epilepsy and avoid blackouts, or even seizures.” [Participant 1.5, UK]
Using transport and traveling could also be impacted. Participants who still experienced seizures, reported that they were not able to drive, and traveling far from home was complex and required detailed planning. Participants reported that they consequently often chose to stay closer to home than they used to prior to their epilepsy diagnosis.
Participants also reported that they had to stop working because of continued symptoms, or due to side effects of their ASMs (unemployment). Others reported only working part time on jobs below their skillset and capabilities (underemployment), or having to find alternative employment, especially if their previous work involved an element of driving or handling large machinery. For many, their job was important for their sense of self-worth and their limitations due to their epilepsy impacted their mental health and sense of self. Other participants did not feel that their jobs or careers had been hampered due to their epilepsy; however, they still experienced constant worry about having a seizure at their workplace.
“I am not able to drive; I have absences, lapses – it is nearly impossible for me to have a job, not only from the epilepsy, but [also] from the side effects of treatment.” [Participant 5.6, France]
3.4.4.3. Stigma and discrimination
As reported in earlier stages, participants could experience continued long-term stigma and discrimination in their everyday life, as there was little reported awareness of the illness among the public. Participants coped with the stigma by either talking about their condition openly, or not discussing it at all when they did not have to. Participants also reported experiencing discrimination in the workplace or in public places.
“It looks like you are drunk, and people would leave you in the middle of the street; they are not told about [this condition]. There should be more awareness campaigns.” [Participant 1.5, UK]
4. Discussion
Content and framework analysis of semi-structured interviews with 40 people with epilepsy on polytherapy, has identified their psychological and emotional journey ( Table 3 ), key insights along the disease journey ( Table 4 ) and unmet needs ( Table 5 ).
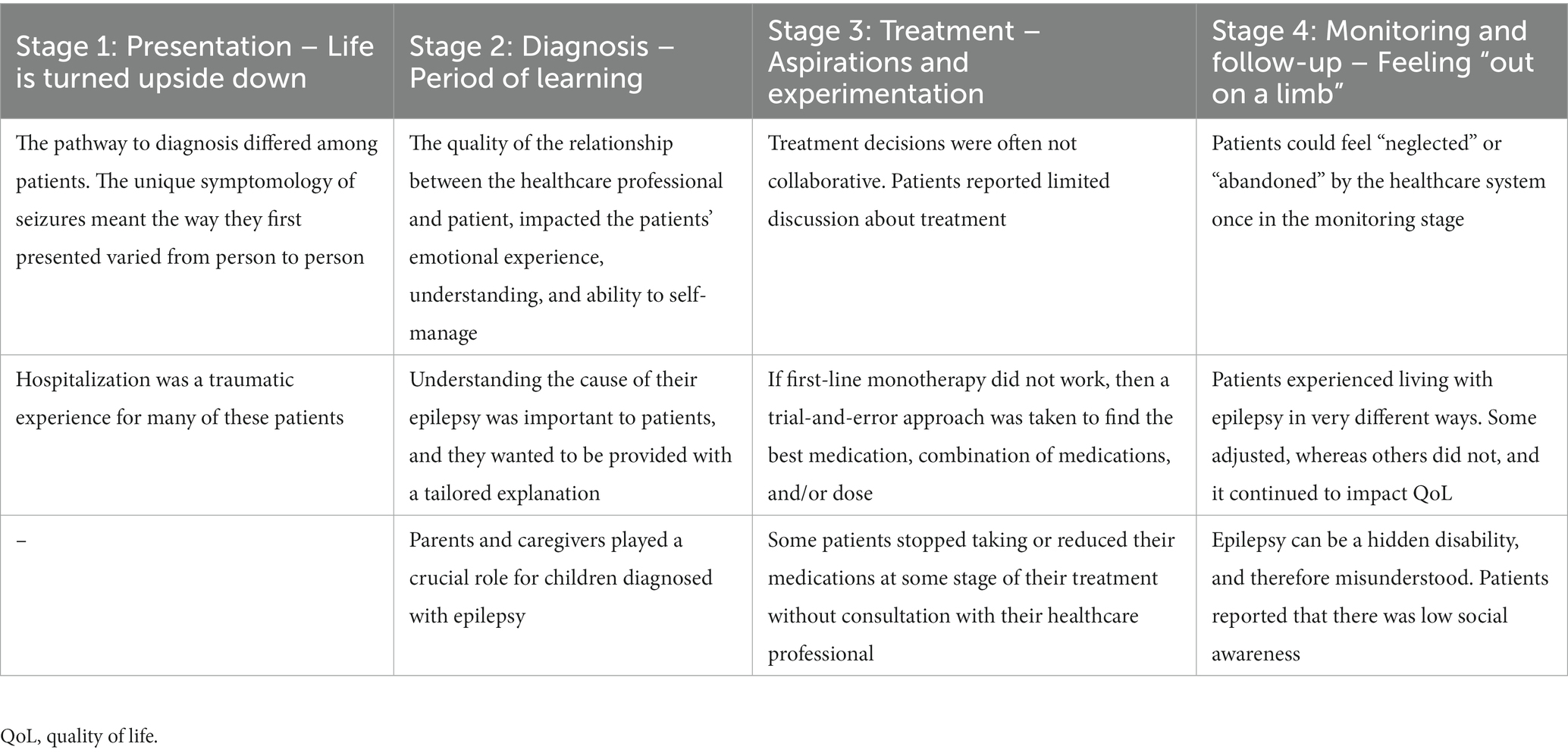
Table 4 . Key insights at each stage of the patient journey.
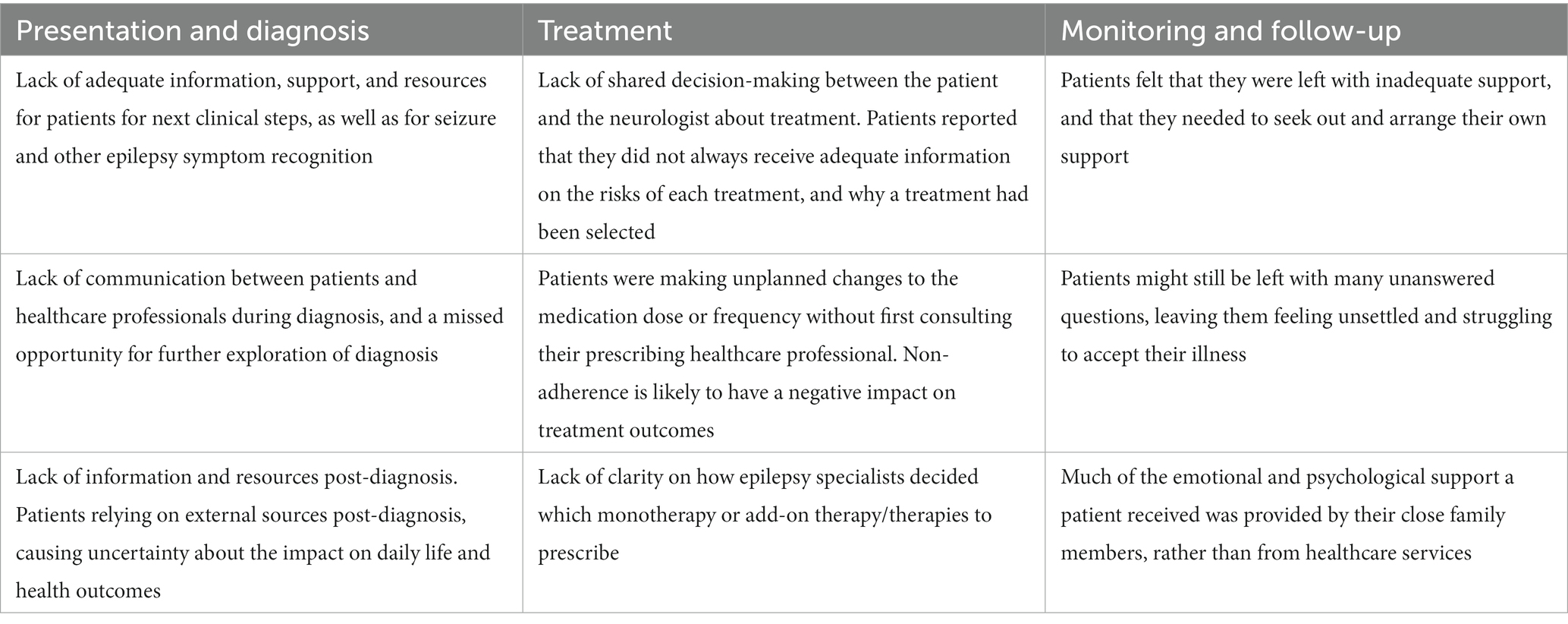
Table 5 . Key unmet needs at different stages of the epilepsy journey.
4.1. Implications for key stakeholders and the healthcare system
Thematic synthesis, within the four clinical stages, resulted in emergent themes that have helped to identify potential targets for future quality improvement interventions. Unmet needs were identified at multiple levels, including at the individual level (e.g., medication non-adherence); the healthcare professional level (e.g., lack of education provision about seizure care to the person with epilepsy); the healthcare system level (e.g., lack of prescribing guidelines for when first-line monotherapy therapy does not work); and the wider community level (e.g., low public awareness/lack of public awareness campaigns).
There are five overarching recommendations for future consideration, based on the unmet needs identified from the current study’s findings. It is important to note, that we do not claim that these are unique recommendations, and some or all, might already be under consideration or development within clinical practice or through patient organizations.
4.1.1. Establish and promote support networks from presentation through to monitoring and follow-up stages
This study highlighted the psychosocial burden of living with epilepsy. There is a need for consistent psychological support for people with epilepsy and caregivers at all stages of the patient journey, from presentation through to monitoring and follow-up stages. The call for support networks to be established in the epilepsy care pathway is echoed by other research ( 19 , 33 ). There is also an opportunity to develop and evaluate psychosocial interventions that support people who are experiencing difficult emotions that relate to living with epilepsy, in the same way that previous research has recommended in the case of sub-populations, such as the elderly ( 17 ) and those with a previous psychiatric history ( 16 ). Furthermore, in a paper by Kemp et al. ( 5 ), they argued that there is an opportunity not only to support patients with their distress, but also to encourage the use of positive psychology and cognitive behavioral therapy to promote mental health well-being in people living with chronic conditions ( 5 ).
4.1.2. Accelerate pathway to diagnosis
The findings from this study suggest that, at least from the patients’ perspective, there is a lack of clarity about what constitutes appropriate seizure care within the healthcare system, and this appears to have the potential to delay the pathway to diagnosis and treatment. Although there have been recent developments in the diagnosis of epilepsy using technological advancement ( 34 ), it would still be advantageous to provide patients entering the healthcare system with standardized education on: how to recognize seizures and other symptoms of epilepsy; seizure first aid; how to report any further seizures; and details of next steps. Furthermore, although not identified as an unmet need in the current study, Watson et al. ( 19 ), identified that there were practical barriers to access testing facilities, and they recommended the provision of at-home testing, dedicated travel assistance programs, and enhanced education on the importance of prompt testing, which would help to prevent treatment delays ( 19 ).
4.1.3. Provide opportunities to discuss the diagnosis with patients
When a person is diagnosed with epilepsy, it is essential that they are able to discuss their diagnosis with their neurologist/epileptologist. In our study, we found that participants were more likely to have a positive diagnostic experience, a better understanding of their condition, and a better ability to self-manage, if they felt that they had this opportunity. Fazekas et al. ( 18 ), argued that there may even be a lack of awareness or sensitivity among healthcare professionals, who may consequently underestimate the concerns of people with epilepsy, or not take sufficient time to discuss their needs ( 18 ). It is crucial that people are given ample time and space to discuss their diagnosis with their neurologist/epileptologist or other relevant healthcare professionals.
4.1.4. Clarify treatment change guidelines for patients
Although the participants in this study were on polytherapy at the time of their interviews, their experiences during presentation and diagnosis are likely to be similar to a person for whom first-line monotherapy treatment was successful. Differences in experiences would likely only occur during the treatment stage of the clinical journey, because of the additional burden of the trial-and-error approach to medication that patients perceive to take place in clinical practice. The analysis suggests that there is a lack of clarity, for patients, on how epilepsy specialists have reached a consensus on what monotherapies or add-on therapies to prescribe. Therefore, it is important to include the patient in the treatment choice process through shared decision-making and general engagement, such that the healthcare professional and their patient are involved in the co-creation of a care package. Further research to ascertain the impact of implementing shared decision-making and patient engagement tools in establishing the patient journey in epilepsy is warranted.
4.1.5. Development of a patient engagement and shared treatment decision-making tool
Treatment decisions are not always collaborative, and people with epilepsy can stop taking or reduce their medication without consulting with their healthcare professional. This might be due to misperceptions they may hold about their treatment (intentional), or as a consequence of practical/physical barriers to taking their prescribed medication (unintentional). Either way, it would be beneficial if healthcare professionals adapt their consultation style to the needs of the individual to address non-adherence in a non-judgmental way ( 35 ). We recommend raising shared decision-making and patient engagement awareness among healthcare professionals, and propose the development of a toolkit for healthcare professionals and people with epilepsy to prompt discussions about their treatment and epilepsy self-management, including add-on therapies, non-pharmacological treatments, and adherence. Empowering people with epilepsy to speak up, and not just passively receive their treatment regimens, is likely to improve patient–provider relationships, as well as their health outcomes, especially since non-adherence could be contributing to the deterioration in seizure control ( 36 ).
Within this decision-making and engagement tool, it would be imperative to educate patients about treatment options, processes, and managing expectations of ASMs. The treatment goal of an ASM is to achieve complete seizure freedom, or at least to reduce the frequency and/or intensity of seizures. In order to set the right expectations, it is essential to inform patients that there are other symptoms associated with epilepsy (comorbidities) that might require additional treatments, other than the ASM.
4.2. Limitations and recommendation for futures research
Limitations to this study should be acknowledged. First, there are limitations within the sample. Considering this was a qualitative interview study, we did access a relatively large sample of people living with epilepsy on polytherapy ( N = 40) in five European countries, yet due to the country spread, it was limited to eight participants per country, each with a mix of age of onset and seizure types. Although there is no specific reason to believe that the subjective experiences expressed by the current sample would differ significantly from other people’s experience within the same countries, it is possible there are differences across people with different clinical characteristics. For example, it is noteworthy that the greatest proportion of patients in this study reported having tonic–clonic seizures, and their experiences may differ to those who experience other types of seizures, such as absence seizures. Furthermore, it is possible that patients who had a psychiatric condition prior to diagnosis have more difficulties adjusting to their diagnosis compared with those that did not. This was touched on in a previous study that found that a higher proportion of patients with a previous psychiatric history described a pervasive loss of control, following diagnosis ( 16 ). However, we did not believe that the current study comprised sufficient individuals within any one category to merit our breaking down the analysis to identify any potential differences across participants. Second, qualitative analysis depends on researchers’ interpretations of textual data, and is therefore potentially open to bias and subjectivity; regular meetings between researchers to discuss and verify the ongoing coding, aimed to limit any confirmation bias. In addition, illustrative quotes have been presented throughout to demonstrate the validity of our analysis. Third, not all participants in this study experienced the same intensity of emotions throughout their journey, nor did all the participants experience the same emotions at the same stage. Not taking these differences into account would be misleading. The analysis offers only an overview of the potential emotional, psychological, and social experiences, and identifying disparities in such experiences across participants, was not an objective of this study. Patient demographics and clinical presentations varied, such as time since diagnosis and type of ASM. Future research could endeavor to investigate whether any differences in emotional, psychological, and social experiences identified in the current study, could reliability be associated with socio-demographic characteristics, such as gender, comorbidities, country of residence, type of epilepsy, or degree of social support.
4.3. Conclusion
Our research provides a comprehensive overview of the experiential journey that people with epilepsy on polytherapy can experience. The emotional mapping exercise specifically illustrates the emotional rollercoaster that many people with epilepsy experience. Our analysis has identified themes in each stage of the clinical journey, from presentation through to monitoring and follow-up stages, and provided actionable recommendations ranging from an individual level to a healthcare system level. Findings have the potential to drive change at the healthcare level, and stop the emotional rollercoaster from derailing.
Data availability statement
The datasets presented in this article are not readily available because of ethical and privacy restrictions. Requests to access the datasets should be directed to the corresponding author.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Author contributions
EG-R conducted the analysis and interpretation of the interview transcripts, as well as wrote the manuscript. CK contributed to the conceptualization of the study design, the management of the analysis and interpretation, as well as provided input into revising and editing of the manuscript. SR contributed to the conceptualization of the study design, as well as provided input into the interpretation of the data, and into editing of the manuscript. AA led the acquisition of patients and patient interviews. She also contributed to the conceptualization of the study design. LB contributed to the conceptualization of the study design, as well as provided input into revising and editing of the manuscript. RS-F contributed to the conceptualization of the study design, as well as provided input into revising and editing of the manuscript. BS was the principal investigator of the project. She contributed to the conceptualization of the study design, as well as provided senior input into all aspects of the study from conception to completion. All authors contributed to the article and approved the submitted version.
This study was supported by Eisai Europe Ltd.
Acknowledgments
The authors would like to thank all of the participants in the study. The third-party recruiters/interviewers that worked on the project. The wider project team at Eisai Europe Ltd. Georgina Charlton and Coralie Pelech. The wider project team at OPEN Health Communications LLP: Matt Maher. Jessica Proctor for her contributions to the early stages of the interview analysis at OPEN Health Communications LLP.
Conflict of interest
LB, RS-F, and BS were employed by Eisai Europe Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Thijs, RD, Surges, R, O'Brien, TJ, and Sander, JW. Epilepsy in adults. Lancet . (2019) 393:689–1. doi: 10.1016/S0140-6736(18)32596-0
CrossRef Full Text | Google Scholar
2. World Health Organization. Epilepsy key facts. (2022) Available at: https://www.who.int/news-room/fact-sheets/detail/epilepsy (Accessed 16 May, 2022).
Google Scholar
3. Moshé, SL, Perucca, E, Ryvlin, P, and Tomson, T. Epilepsy: new advances. Lancet . (2015) 385:884–8. doi: 10.1016/S0140-6736(14)60456-6
4. Hills, MD. The psychological and social impact of epilepsy. Neurology Asia . (2007) 12:10–2.
5. Kemp, AH, Tree, J, Gracey, F, and Fisher, Z. Editorial: improving wellbeing in patients with chronic conditions: theory, evidence, and opportunities. Front Psychol . (2022) 13:e868810. doi: 10.3389/fpsyg.2022.868810
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Räty, LK, Söderfeldt, BA, and Wilde Larsson, BM. Daily life in epilepsy: patients' experiences described by emotions. Epilepsy Behav . (2007) 10:389–6. doi: 10.1016/j.yebeh.2007.02.003
7. Chew, J, Carpenter, J, and Haase, AM. Young People's experiences of epilepsy: a scoping review of qualitative studies. Health Soc Work . (2017) 42:167–6. doi: 10.1093/hsw/hlx020
8. Chew, J, Carpenter, J, and Haase, AM. Living with epilepsy in adolescence-a qualitative study of young people's experiences in Singapore: peer socialization, autonomy, and self-esteem. Child Care Health Dev . (2019) 45:241–13. doi: 10.1111/cch.12648
9. Coleman, H, McIntosh, A, and Wilson, SJ. A patient-centered approach to understanding long-term psychosocial adjustment and meaning-making, 15 to 20 years after epilepsy surgery. Epilepsy Behav . (2020) 102:106656. doi: 10.1016/j.yebeh.2019.106656
10. Hosseini, N, Sharif, F, Ahmadi, F, and Zare, M. Patients' perception of epilepsy and threat to self-identity: a qualitative approach. Epilepsy Behav . (2013) 29:228–3. doi: 10.1016/j.yebeh.2013.06.003
11. Kerr, C, Nixon, A, and Angalakuditi, M. The impact of epilepsy on children and adult patients' lives: development of a conceptual model from qualitative literature. Seizure . (2011) 20:764–4. doi: 10.1016/j.seizure.2011.07.007
12. Ozanne, A, Graneheim, UH, Ekstedt, G, and Malmgren, K. Patients' expectations and experiences of epilepsy surgery--a population-based long-term qualitative study. Epilepsia . (2016) 57:605–1. doi: 10.1111/epi.13333
13. Rapport, F, Clement, C, Doel, MA, and Hutchings, HA. Qualitative research and its methods in epilepsy: contributing to an understanding of patients' lived experiences of the disease. Epilepsy Behav . (2015) 45:94–13. doi: 10.1016/j.yebeh.2015.01.040
14. Rawlings, GH, Brown, I, and Reuber, M. Narrative analysis of written accounts about living with epileptic or psychogenic nonepileptic seizures. Seizure . (2018) 62:59–65. doi: 10.1016/j.seizure.2018.09.022
15. Rawlings, GH, Brown, I, Stone, B, and Reuber, M. Written accounts of living with epilepsy: a thematic analysis. Epilepsy Behav . (2017) 72:63–70. doi: 10.1016/j.yebeh.2017.04.026
16. Velissaris, SL, Wilson, SJ, Saling, MM, Newton, MR, and Berkovic, SF. The psychological impact of a newly diagnosed seizure: losing and restoring perceived control. Epilepsy Behav . (2007) 10:223–3. doi: 10.1016/j.yebeh.2006.12.008
17. Yennadiou, H, and Wolverson, E. The experience of epilepsy in later life: a qualitative exploration of illness representations. Epilepsy Behav . (2017) 70:87–93. doi: 10.1016/j.yebeh.2017.01.033
18. Fazekas, B, Megaw, B, Eade, D, and Kronfeld, N. Insights into the real-life experiences of people living with epilepsy: a qualitative netnographic study. Epilepsy Behav . (2021) 116:107729. doi: 10.1016/j.yebeh.2020.107729
19. Watson, GDR, Afra, P, Bartolini, L, Graf, DA, Kothare, SV, McGoldrick, P, et al. A journey into the unknown: an ethnographic examination of drug-resistant epilepsy treatment and management in the United States. Epilepsy Behav . (2021) 124:108319. doi: 10.1016/j.yebeh.2021.108319
20. Damasio, AR. Emotion in the perspective of an integrated nervous system1Published on the world wide web on 27 January 1998.1. Brain Res Rev . (1998) 26:83–6. doi: 10.1016/S0165-0173(97)00064-7
21. Cabanac, M. What is emotion? Behav Process . (2002) 60:69–83. doi: 10.1016/S0376-6357(02)00078-5
22. Damasio, A. Descartes' error: Emotion, reason, and the human brian . London: Penguin Books (1994).
23. Damasio, A. The feeling of what happens body, emotion and the making of consciousness . San Diego: Harcourt Brace and Co. (1999).
24. Goldsmith, LJ. Using Framework Analysis in Applied Qualitative Research. Qual Res . (2021) 26. doi: 10.46743/2160-3715/2021.5011
25. Gale, NK, Heath, G, Cameron, E, Rashid, S, and Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol . (2013) 13:1–8. doi: 10.1186/1471-2288-13-117
26. National Institute for Health and Care Excellence. Epilepsies: diagnosis and management (2012) London: National Institute for Health and Care Excellence.
27. Elger, CE, and Berkenfeld, R. (geteilte Erstautorenschaft). S1-Leitlinie Erster epileptischer Anfall und Epilepsien im Erwachsenenalter . (2017). Deutsche Gesellschaft für Neurologie, Hrsg. Leitlinien für Diagnostik und Therapie in der Neurologie. Online: www.dgn.org/leitlinien
28. Mercadé Cerdá, JM, Toledo Argani, M, Mauri Llerda, JA, López Gonzalez, FJ, Salas Puig, X, and Sancho Rieger, J. The Spanish Society of Neurology's official clinical practice guidelines for epilepsy. Neurología (English Edition) . (2016) 31:121–9. doi: 10.1016/j.nrleng.2013.12.008
29. Haute Autorité de Santé, Épilepsies: Prise en charge des enfants et des adultes [Récommandation de bonne pratique] . (2020). Saint-Denis La Plaine: HAS.
30. Minicucci, F, Ferlisi, M, Brigo, F, Mecarelli, O, Meletti, S, Aguglia, U, et al. Management of status epilepticus in adults. Position paper of the Italian league against epilepsy. Epilepsy Behav . (2020) 102:106675. doi: 10.1016/j.yebeh.2019.106675
31. Ritchie, LS. Qualitative data analysis for applied policy research In: A Bryman, editor. Aanlyzing qualitative data . Lodon: Routledge (1994)
32. Spencer, L, Ritchie, J, O'Connor, W, Morrell, G, and Ormston, R. Analysis in practice, in qualitative research practice: A guide for social science students and researchers . Sage: Los Angeles, London: New Delhi, Singapore, Washington DC (2014).
33. Mahendran, M, Speechley, KN, and Widjaja, E. Systematic review of unmet healthcare needs in patients with epilepsy. Epilepsy Behav . (2017) 75:102–9. doi: 10.1016/j.yebeh.2017.02.034
34. Bandopadhyay, R, Singh, T, Ghoneim, MM, Alshehri, S, Angelopoulou, E, Paudel, YN, et al. Recent developments in diagnosis of epilepsy: scope of MicroRNA and technological advancements. Biology (Basel) . (2021) 10:1097. doi: 10.3390/biology10111097
35. NICE. Medicines adherence: Involving patients in decisions about prescribed medicines and supporting adherence, in Clincal guidelines . London: National Institude for Health and care Excellence (NICE) (2009).
36. Hovinga, CA, Asato, MR, Manjunath, R, Wheless, JW, Phelps, SJ, et al. Association of non-adherence to antiepileptic drugs and seizures, quality of life, and productivity: survey of patients with epilepsy and physicians. Epilepsy Behav . (2008) 13:316–2. doi: 10.1016/j.yebeh.2008.03.009
Keywords: epilepsy, patient journey, emotions, qualitative, market research, unmet needs
Citation: Graham-Rowe E, Katzer CB, Riaz S, Attwood A, Bates L, Sainz-Fuertes R and Swan B (2023) Unmet needs of people with epilepsy: A qualitative study exploring their journey from presentation to long-term management across five European countries. Front. Neurol . 14:1130817. doi: 10.3389/fneur.2023.1130817
Received: 23 December 2022; Accepted: 23 March 2023; Published: 14 April 2023.
Reviewed by:
Copyright © 2023 Graham-Rowe, Katzer, Riaz, Attwood, Bates, Sainz-Fuertes and Swan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Becky Swan, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Diseases & Diagnoses
Issue Index
- Case Reports
Newly Launched Epilepsy Care Management Company, Nile, Aims to Create a Predictable Patient Journey
UCB has announced the launch of a new company, Nile, that will offer a digital platform consisting of a patient app and a health care professional portal through which health care professionals and patients can interact. The formation of Nile is based on the observation that the intersections in epilepsy care, whether between patient and treatments, prescribers, monitoring services, and community supports are often limited to single points in time. The patient journey, however, is a continuum with no single intersection or relationship defining a person's quality of life or how they can get their epilepsy under control. The mission of Nile will not be to replace any current aspect of epilepsy care at those single points in time, but rather to bring them all closer together in a collaborative manner. For example, Nile aims to use that collaboration to eliminate some of the long waits between milestones in epilepsy care (eg, seeing an epileptologist, starting or changing treatments, monitoring seizures digitally, consulting neurosurgeons, or considering lifestyle changes).
Leo Petrossian, PhD, chief executive officer for Nile said, “The problem around epilepsy care management goes far, far beyond individual interactions, in part for the positive reason that there are hundreds of organizations working to improve pieces of the puzzle that is the epilepsy journey. We see the opportunity to accelerate the formation of relationships that occur along the journey of an epilepsy patient, interconnecting them as a way to unify improvement efforts. Among the challenges we hear over and over from patients is the uncertainty and isolation that can come from having epilepsy. Through this platform, we hope to create a predictable flow of patient care that eliminates some, if not all, of that uncertainty.”
Although the initial funding and values of Nile comes from UCB Pharma, Nile is a wholly independent company with overlap only at the governance level to avoid any potential conflicts of interest.
Nile has been created as a patient-centric organization that is building a foundational platform for epilepsy care management with the expectation that from this, solutions for epilepsy care that will be of value to health care organizations and payors will be developed into for-sale products. At this time, however, the core goal is to follow the UCB mantra of “inspired by patients, driven by science,” and use that to digitally coordinate and unify improvement efforts and develop a predictable flow of care for people with epilepsy.
Nile is currently testing the platform in usability studies with the Massachusetts General Hospital and Michigan State University Healthcare and expects to make the app and portal widely available later in 2021.
FDA Gives Clearance for the First 15-Minute Handheld Blood Test for Concussions
First Participant Treated in Phase 4 Study of Nusinersen Treatment After Prior Onasemnogene Treatment
This Month's Issue
Bénédicte Dansereau, MD, and Leo H. Wang, MD, PhD
Julia Greenberg, MD; Kaiulani Houston, MD, PhD; Kevin Spiegler, MD, PhD; Sujata Thawani, MD, MPH; Harold Weinberg, MD, PhD; and Ilya Kister, MD
Jill R. Baron, MD, and Jennifer Villwock, MD

Related Articles
Joyce H. Matsumoto, MD
Greg Grunberg
Sign up to receive new issue alerts and news updates from Practical Neurology®.
- Women's Health
- Health & Wellness

6 Learnings on My Journey from Medical Student to Epilepsy Attending
The road from medical student to attending is chock-full of critical decisions . The choices you make about location, institution and specialty will determine your career path and lay the foundation for your future.
No pressure, right?
Remember that your self-drive and motivation will guide you to earn a solid medical education, no matter the institution. So, if you focus your residency and fellowship search on finding the place that best fits you personally , you’ll be much more satisfied with your decisions long term.
It’s important to envision how you’ll balance the stress of a residency or fellowship with the kind of activities you enjoy. The location you choose for your residency and fellowship is just as important as the offerings of the institution:
- What will you do for fun when you’re not working?
- Will your family also enjoy the locale?
- Where can you make the most of your time and money?
I’d like to offer some guidance and reassurance to anyone in a transition phase who’s figuring out what to do next. Here’s a peek into my journey from med school student to epilepsy attending and how I found the perfect specialty—and training center—for my personality and lifestyle at UNM Health Sciences Center.
1. Be Open to Unfamiliar Locations
I grew up under the rainy skies of Washington and went to medical school surrounded by the plains of Nebraska. I didn’t see myself ending up in the Southwest because I simply didn't have any exposure to that part of the country. But when I started to get curious about New Mexico, I realized how well the locale complemented my interests.
I'm an avid skier and cyclist—I bike about 10 to 12 hours a week—so the Southwest clicked with my outdoor lifestyle. During winter weekends, it’s often sunny and 60 in Albuquerque but snowy up in the mountains, so recreational options are virtually limitless. Check out our Instagram to see how UNM HSC Neurology residents kick back and relax.
If you don’t factor in your life outside of the hospital, you run the risk of feeling lopsided and stressed out. It’s important to find a place where you can prioritize your wellness and establish a work-life balance. Though my neurology residency and fellowship were rigorous, UNM HSC offered a level of freedom in scheduling that allowed time for activities that benefited my health.
2. Find Your People
When you decide on an institution, you are choosing the department culture and the family you will be working with—because it really is a family of folks coming together to form that department. Find out if the other doctors have a similar practice style as you and if the members of the faculty desire to be mentors.
Let the people sway your decision, because it’s important that you feel you're an appreciated member of the team .
3. Connect with a Mission that Resonates
The medical school I attended is Jesuit-based, and a lot of their work involves give people with limited access the best health care and resources. The belief that every person deserves a high level of care resonates with me, and I found that UNM HSC has a very similar mission.
We serve people across the spectrum of access—from those with private insurance to those unable to work because of their disease. As a large health center, we have the privilege of serving patients all over the state—it’s fantastic the amount of outreach we get to provide.
4. Narrow It Down
When choosing your specialty, consider how narrow and deep you want to go with your education and experience. Start with what you’re good at and how you like to work. Some people are skilled at starting from scratch with a patient, building a differential diagnosis and managing a wide variety of cases. For them, becoming a specialist such as a neurologist is a great option.
For doctors like me who especially love the diagnostic aspect of neurology, a subspecialty like epilepsy is a perfect fit. You may start with a few vague neurological symptoms, but through your examination and detective-like problem-solving skills , you put together all the pieces of a complicated puzzle to discover what your patient needs.
The subspecialty of epilepsy offers a nice balance between reading EEGs and seeing patients in the clinic. That’s why I chose a two-year fellowship: a neurophysiology fellowship , which provided general exposure, followed by an epilepsy fellowship to learn a more refined approach to epilepsy.
Consider your academic curiosity. In neurology, there are a lot of gray areas, so you’ll really need to get to know your patients and stay on top of the most recent research.
5. Envision Your Future
Your choice of residency or fellowship program should be made with your long-term personal and professional goals in mind. I didn’t know when I started my residency here that I would be staying indefinitely, but I met my wife Lauren here, and she will soon be starting her epilepsy fellowship at UNM HSC. We can see ourselves raising a family here and making Albuquerque the hub of our extended family.
When I look forward to my career goals, I’m excited to take on more of an educational role as a junior faculty member. I hope to introduce neurology to new doctors that hadn't considered this incredible field , and I look forward to getting folks excited about the many areas in which they can specialize.
6. Choose Balance
It’s exciting to look back on how I've progressed through the stages of my medical education, some of which seemed pretty scary at the time:
- I was a medical student who was unsure of himself.
- A resident who fact-checked everything with his attending. A neurophysiology fellow who found his confidence and his niche.
- An epilepsy fellow who took the lead on patient rounds.
- And now, an attending in a leadership role that will help build the reputation of my department and UNM Health.
Deciding on a location for your residency or fellowship becomes easier when you zoom out and view the whole package. Find a place that lets you practice a high level of patient care alongside an outstanding group of people. And most importantly, decide where you’re personally going to be the happiest.
Exploring your neurology education options? Request an appointment with the enrollment team.
Explore Neurology Services Here .
- CONTACT US |
Resources on rare epilepsies
EpiCARE’s ePAG , the patient representatives, care to produce documents to help patient through their diagnosis, their communications with healthcare professionals and even with their close ones.
In collaboration with EpiCARE clinicians, they prepared two kinds of documents : patient leaflets and journeys. The leaflets are a informative document about a specific diseases, in 2 parts: one for the patients and their carers and families, and one for healthcare professionals. In each leaflet, you will be able to learn about the prevalence, diagnosis, treatment options… of rare and complex epilepsies. Secondly, patients journeys are also being developped. They illustrate the journey through the diagnosis, providing a kind of map from the perspective of those living with a rare and complex epilepsy.
Rare epilepsies leaflets
Patient and caregivers leaflets are developed to give precise and accessible informations on rare and complex epilepsies. With one part for healthcare profesionnals, and one part for patients and their families or carers , these documents detail comprehensively what to expect when facing a rare epilepsy, and how to manage care.
Unless mentioned otherwise, all leaflets are in english. We are working on translating them in as many languages as possible with the help of patients associations all over Europe, so check back regularly!

Read and download the following leaflets:
- Dravet Syndrome leaflet (EN) / Dravet versione italiana (IT) / Dravet Versiunea română (RO) / Dravet hrvatska verzija (HR) / Dravet deutsche Version (DE) / Dravet Norsk versjon (NO) / Dravet srpska verzija (RS) / Dravet Svensk version (SE)
- Hypothalamic Hamartoma leaflet / Hypothalamic Hamartoma Versiunea română (RO) / Hypothalamic Hamartoma Hrvatska verzija (HR)
- Ring Chromosome 20 leaflet / Ring Chromosome 20 Hrvatska verzija (HR) / R(20) ελληνική έκδοση (GR) / R(20) Lietuviška versija
- Alternating Hemiplegia of Childhood leaflet (EN) / AHC Hrvatska verzija (HR) / AHC Versione italiana (IT) / HAI Versión española / Version française (FR)
- GLUT1 Deficiency Syndrome leaflet (EN) / GLUT1 Hrvatska verzija (HR) / GLUT1 Versiunea română (RO) / Glut1 Deutsche Version (DE) / Glut1 versione italiana (IT)
- CDKL5 Deficiency Disorder leaflet (EN) / CDKL5 Versión española (ES) / CDKL5 Versão portuguesa (PO) / CDKL5 Hrvatska verzija (HR) / CDKL5 Versiunea română (RO)
- Lennox-Gastaut syndrome leaflet (EN) / Lennox-Gastaut syndrome Versiunea română (RO) / Lennox-Gastaut Hrvatska verzija (HR)
- SYNGAP1 leaflet (EN) / SYNGAP1 Versiunea română (RO) / SYNGAP1 Hrvatska verzija (HR)
- RETT Syndrome leaflet (EN) / RETT Hrvatska verzija (HR)
- Infantile Epileptic Spasms Syndrome leaflet (EN) / IESS Hrvatska verzija (HR)
- STXBP1 leaflet (EN) / STXBP1 Hrvatska verzija (HR)
These documents are being developed progressively. New ones should be added soon.
Patients journeys
Rare epilepsies patient’s journeys describe the specific needs and goals of a patient’s path for a rare or complex epilepsy. They describe the health-care pathway and provide a key perspective of those living with a rare disease. In consequence, they allow for a constructive discussion between clinicians and patients. The ePAG advocates made these journeys available by mapping the needs and expectations for each stage of the care pathway, for 4 rare and complex epilepsies so far.
Read and download the following patients journeys :
- Dravet Syndrome patient journey / Dansk version (DK) / Dravet Putovanje oboljelog (HR) / Dravet Percorso del paziente (IT) / Potovanje bolnika s sindromom Dravet (SI) / Dravetov sindrom –etape razvoja bolesti (RS) / Dravets Syndrom Pasientreise (NO)
- Hypothalamic Hamartoma patient journey / HH Putovanje oboljelog (HR) / HH Versiunea româna (RO)
- Alternating Hemiplegia of Childhood patient journey / AHC Putovanje oboljelog (HR) / AHC Percorso del paziente (IT) / HAI (AHC) Viaje del Paciente / AHC Parcours du patient (FR)
- KCNQ2 patient journey (EN) / KCNQ2 percorso del paziente (IT) / KCNQ2 Putovanje oboljelog (HR)
- GLUT1 patient journey / GLUT1 Putovanje oboljelog (HR) / Glut1 deutsche (DE) / GLUT1 percorso del paziente (IT)
- STXBP1 patient journey / STXPB1 Putovanje oboljelog (HR)
- SYNGAP1 patient journey
Please note that these documents are being developed progressively. We will add more regularly.
Emergency Protocols
- Emergency Protocol for Dravet syndrome – plateform built to help clinicians/carers to prepare a tailor-made emergency protocol for people affected by Dravet Syndrome
- Glut1 Deficiency syndrome emergency protocol – guidelines provided by BIMDG on behalf of Orphanet
- Tuberous Sclerosis ermergency guidelines – This document is a translation of the French recommendations drafted by Dr. M. Chipaux, reviewed and published by Orphanet in 2007.
Other resources
- Epilepsy & Pregnancy : A European Survey report published by the International Bureau for Epilepsy
- In spanish: Farmacos en camino para el sindrom de Dravet – resumen fin de 2021
- Speak up. Listen up. Follow up : a brief guide for rare disease patient organisations on how to listen to the community
- Patient journeys : A Tool to Raise Awareness on the Evolution, Common Needs and Critical Issues of Patients with Rare and Complex Epilepsies : poster presented at the IEC 2023 in Dublin by the ePAGs
- Alternating Hemiplegia of Childhood (AHC) Full Text Patient Journey
The medical team members of the European Reference Network EpiCARE, in collaboration with patient advocates, develop and deliver highly-specialized diagnostics and care to improve interventions and outcome in individuals with rare and complex epilepsies.
The ERN EpiCARE was created in 2017 and is co-funded by the European Union.
EpiCARE © 2021 all rights reserved | Privacy Policy | Webdesign : Marc Chaperon
Privacy Overview
- Future Leaders in Neurology
- ACTRIMS 2024
- Treating NMOSD: What's Next?

- Conferences
- Publications
Perspectives From the Journey of the Patient With Rare Epilepsy
Joseph E. Sullivan, MD; Kelly Knupp, MD; Mary Anne Meskis; and Tracy Dixon-Salazar, PhD, share insight into the patient and provider journey of LGS and Dravet syndrome, from diagnosis through treatment.

PATIENTS WITH RARE EPILEPSIES such as Dravet syndrome (DS) and Lennox-Gastaut syndrome (LGS) often experience difficulties from the disease that extend beyond the symptoms and biological effects that immediately come to mind. In addition to burdens on quality of life, there can also be delays in diagnosis and difficulties with treatment success.
Currently, DS affects an estimated 1 of every 15,7000 individuals, with approximately 80% to 90% of those having both an SCN1A mutation and a clinical diagnosis of DS. 1 LGS, on the other hand, is estimated to occur in roughly 0.1 to 0.28 of every 1000,000 individuals, accounting for roughly 1% to 4% of all childhood epilepsy cases. 2 Although these epilepsy disorders are rare, therapies are available to treat them, but many patients experience refractory disease, making the development of a treatment regimen a complex process. As the medical field moves toward more personalized and holistic care as a whole, the treatment process involves a much more in-depth conversation about the patient experience.
In a recent NeurologyLive ® Cure Connections ® series, a panel of experts in epilepsy care and advocacy came together to discuss how this landscape has shifted and to share their understanding of that patient experience from various angles. Moderated by JOSEPH E. SULLIVAN, MD, a professor of neurology at UCSF Weill Institute for Neurosciences, the conversation touched on a number of facets of the care paradigm.
Syndrome Overview
Dravet syndrome.
Panel member KELLY KNUPP, MD , a pediatric neurologist at Children’s Hospital Colorado, began the discussion with an overview of DS, noting that the developmental epileptic encephalopathy is often characterized by multiple seizure types provoked by temperature changes, as well as intellectual impairment. Notably, Knupp said, this impairment can become more apparent with age—a key change to look for diagnostically. DS can also be accompanied by progressive gait disorder and behavioral disorders, among other comorbidities.
“One of the characteristics of this syndrome is that it’s often associated with a pathogenic variant in a gene called SCN1A ,” Knupp explained. “The vast majority of children do have one of those genetic diagnoses, but not all children. That’s important to keep in mind, as well [as the fact] that there’s a clinical syndrome, but we may not find a genetic mutation that goes along with it. It is also important to know that there are some children who have a pathogenic variant in SCN1A who don’t actually have Dravet syndrome. It’s important to look for both of those things: the clinical syndrome as well as the gene mutation.”
DS was initially believed to be more uncommon than it is, and recent epidemiological data suggest that missed diagnoses were prevalent in clinical practice prior to current advances in genetic testing. This was driven largely by a lack of understanding of DS itself, and Sullivan explained that during his training, he saw very few children with a diagnosis of DS. “It’s almost embarrassing, but you can see how it happens. We are told as pediatricians that febrile seizures are common and many of these kids are told not to worry about it.”
Knupp explained that in her practice, any child who has had a prolonged febrile seizure, particularly hemiconvulsive seizure, raises a flag. “I’m on the fence about the children who have had 2 simple febrile seizures and otherwise are doing well because we know that about one-third of children who have a first febrile seizure will go on to have a second febrile seizure. But, if there’s something like a prolonged seizure or a focal nature to the seizure, we have to consider doing genetic testing,” she said.
Sullivan added, “Age is a factor, too. We’re told that febrile seizures occur at 6 months; if a patient has a simple febrile seizure at 6 months and then another simple febrile seizure at 7 months, that’s a worry to me.”
Lennox-Gastaut Syndrome
In LGS, the diagnostic process is similarly challenging for a variety of reasons, though much of it is driven by controversy surrounding the clinical definition of the syndrome. Although criteria do exist to make the diagnosis, Knupp explained that LGS has numerous etiologies and often evolves from another status, making it challenging to catch and properly diagnose.
“To have a diagnosis of Lennox-Gastaut most people would agree that you should have multiple seizure types, maybe just 2, but at least 1 of those should be tonic seizures. There are characteristic EEG [electroencephalogram] patterns that should be seen with slow spike and wave and then also paroxysmal fast activity which is most often seen during sleep,” she said.
Additionally, children with LGS have, almost universally, intellectual impairment, Knupp continued. This is often considered a requirement for the diagnosis and can be accompanied by a time point for presentation—sometimes prior to the age of 11 years. However, she said, there are reports of individuals who presented during adolescence or in early adulthood with these signs and symptoms.
“Because this is a syndrome that most children evolve into, what’s important is that when our families are starting to develop multiple seizure types, we do take another look and repeat their EEG [electroencephalography] and look for the electrographic findings of this,” Knupp said. “There are certain patient populations that we should probably always be very sensitive to and probably be looking for evolution into the syndrome. There are definitely some high-risk patients that we should be looking for this diagnosis in, but we also have to keep in mind that’s not all of them, and this can happen to any one of our children who presents with childhood epilepsy. We always have to be aware of that and making sure that we are clarifying what seizure types are [being seen], what’s happening at night, and thinking about getting an EEG particularly in a child who is having multiple seizure types and has developed mental delay or intellectual impairment.”
Knupp and Sullivan detailed the list of genetic disorders that are frequently associated with LGS, noting that infantile spasms have one of the highest risks of evolving into LGS, especially in patients with refractory spasms. But those with an epilepsy risk factor, such as neonatal stroke or developmental brain abnormality, are an important secondary group to evaluate as well.
“You don’t necessarily present with Lennox-Gastaut; you present with a few seizures and then it takes some time for the syndrome to evolve and declare itself,” Sullivan said. “It’s our job as epilepsy providers to be aware of that evolution, not only EEG-wise—we don’t look at any of these things in isolation—but how the whole picture fits together. Then there is a third group where there are no epilepsy risk factors, and maybe even normal development, but they have their first few seizures and then very quickly evolve into the Lennox-Gastaut picture. You can always get even more narrow and say specific genetic diagnosis.”
We still have to work to educate our adult providers about the importance of getting a diagnosis and making sure that they know this testing is available and is significantly less costly than it was in the past.
– MARY ANNE MESKIS
Patient Journey to Diagnosis
DS often presents during the first year of life, usually beginning with prolonged generalized tonic-clonic or hemiclonic seizures. Status epilepticus is also common among this population in the early stage of disease, and a variety of other seizures can occur prior to age 5 years. The disease itself is also often associated with hyperthermia, with the initial seizure often occurring alongside fever.
Recent advances in genetic testing have aided the diagnostic process, though many older patients previously experienced delays of several years prior to receiving an official diagnosis of DS. For one panel member, MARY ANNE MESKIS, executive director of the Dravet Syndrome Foundation, whose son is a patient with DS, the diagnostic delay was familiar.
“I think certainly in the last decade, we’ve really seen a change in the typical journey for patients and parents to get to diagnosis. Back then, my son, who is now 22, [did not receive a diagnosis] until age 4,” Meskis told the panel. “Early on, we kept being told that it was febrile seizures. Unfortunately, we still have some patients that follow that same diagnostic journey; if they’re not being seen by a health care professional that understands what they should be looking for and [one who] doesn’t order genetic testing, unfortunately it can still take several years until symptoms progress and until they find the right specialists that can help them get to diagnosis.”
For the physicians, though, the diagnosis can still be made without genetic testing. For experts in this realm of care, the key characteristics can be clear when a patient experiences an evolution from prolonged febrile seizures into multiple seizure types and temperature sensitivity. Additionally, in older patients, gait challenges can sometimes lead clinicians to the correct diagnosis. But as DS presents so early on, that time to see the evolution of seizures can be critical, and Sullivan noted that sometimes signs can be missed initially.
“The area where genetic testing has been really helpful has been with those very early seizures,” Knupp said. “It sometimes is challenging to tell the difference between a straightforward febrile seizure vs a febrile seizure associated with Dravet syndrome, particularly if it was not a hemiconvulsive seizure. But if I saw a patient whose first febrile seizure was a hemiconvulsive seizure on the right and their second febrile seizure was a hemiconvulsive seizure on the left, I would have felt really confident that it was Dravet syndrome, and that we should proceed as though that was the diagnosis.”
Sullivan added that without a proper childhood history of seizure evolution, oftentimes DS can be difficult to identify. Meskis echoed this sentiment, adding that as patients get older, unless the parent or guardian pushes for more answers, it can be particularly challenging to press for further inquiry into diagnosis, especially if the patient has improved otherwise.
“I have also heard from parents who kept pushing for testing, and after finally getting testing and a diagnosis, they might have had a child on a medication that was contraindicated for Dravet syndrome for many years,” Meskis said. “I think there’s a challenge and I think that we still have to work to educate our adult providers about the importance of getting a diagnosis and making sure that they know this testing is available and is significantly less costly than it was in the past, because that was a barrier for a long time for our families.”
Sullivan agreed, adding that the diagnosis also allows patients and families to experience a sense of community. Organizations such as the Dravet Syndrome Foundation and support groups provide a resource for these individuals living with similar day-to-day struggles. “I’ve just seen so much value in that,” he said.
In LGS, although the disease similarly presents early on in life, the situation can be less clear than with DS. This is mainly a result of the aforementioned lack of consensus about the clinical definition of LGS and the variety of underlying causes. Often, its cause goes completely unknown. For many, such as panelist TRACY DIXON-SALAZAR, PHD, executive director of the Lennox-Gastaut Syndrome Foundation, and whose daughter is a patient with LGS, the journey to diagnosis can take some time and can be characterized by numerous failed attempts at treatment.
This lag in diagnosis can lead to confusion for the parents and patients. Patients continue to experience seizures unexpectedly and without a discernable pattern, and all the while experiencing the consequences of these convulsive episodes without help from treatment. Over the past decade, though, the literature and understanding of LGS has improved drastically, which, in turn, has improved the diagnostic process for many. Cognitive changes in the setting of ongoing seizures, Knupp explained, are an immediate red flag to look into the possibility of LGS. Additionally, when it comes to disease management, a conversation about pairing nonpharmacologic interventions such as diet or stimulation devices can also provide some relief to patients.
“We are seeing a lot of families in our group that are coming in [for diagnosis at a] much younger [age]—1- or 1.5-year-olds, 2-year-olds that are getting in a lot earlier,” Dixon-Salazar said. “Our understanding is that there is this evolution and…that it is not the doctors who are failing you, it is the treatments. Science and medicine have not got to the point where they can help in a lot of ways, but you don’t want to stop trying. Families are supported now by other caregivers who have been there, done that, so I definitely think [the diagnostic journey] is faster and better.”
Dixon-Salazar added that part of the difficulty in the diagnostic process is that many patients with LGS are being treated in general neurology or family medicine practices, which may be unfamiliar with the rare epilepsy, marking the importance of getting referrals to epileptologists, such as Knupp or Sullivan. From there, Dixon- Salazar said, patients and their families can more easily find hope for their future care.
“That first visit is often trying to provide some education, understand what’s going on so far, and set reasonable expectations, which is part of our job to be able to move forward,” Knupp explained. “That first visit is usually assessing how many medications have been tried and having that conversation that if you have failed 2 or more medications, the likelihood of more medicine making you seizure free is pretty low.”
Nanopore Long-Read Sequencing Facilitates Diagnosis of Atypical Ataxia-Telangiectasia
Episode 113: Lessons Learned in Alzheimer Drug Development

Investigational Agent EDG-5506 Shows Promising 2-Year Data in Becker Muscular Dystrophy
Sleeping Around the Podcast × NeurologyLive: Candidate Biomarkers to Detect REM Sleep Behavior Disorder in Parkinson Disease

Understanding the Clinical Utility of Low-Contrast Letter Acuity and RAN Tasks in Alzheimer Disease

Researchers Identify Distinct Differences in Acute Optic Neuropathy of MOGAD vs Nonarterior Anterior Ischemic Optic Neuropathy
2 Commerce Drive Cranbury, NJ 08512
609-716-7777
- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram
Stanford Medicine-led study identifies novel target for epilepsy treatment
Researchers find that a little-understood part of the brain appears to be involved in starting seizures and keeping them going.
April 17, 2024 - By Kimberlee D'Ardenne

Stanford Medicine researchers and their colleagues found that removing or inhibiting the fasciola cinereum may help epilepsy patients who aren't helped by surgery. Tom - stock.adobe.com
Removing part of the brain’s temporal lobe is the only treatment available to the millions of people with a form of epilepsy that medications often don’t alleviate. But even that approach fails a third of the time.
A new study from Stanford Medicine researchers and their colleagues offers an explanation and suggests a more effective approach to treatment. They found that a previously overlooked region of the hippocampus, the fasciola cinereum, appears to be involved in instigating and propagating seizures. Removing or inhibiting the fasciola cinereum may help those patients who don’t find relief after surgery.
“The hippocampus is the best studied part of the brain by far, but there is shockingly little known about the fasciola cinereum,” said Ivan Soltesz , PhD, the James R. Doty Professor in Neurosurgery and Neurosciences and a senior author on the study. “This relatively small region was consistently involved in seizure activity in mice and in people undergoing pre-surgical electrical recordings. Our findings suggest that all patients with drug-resistant temporal lobe epilepsy should have depth electrodes placed in the fasciola cinereum as part of the surgery planning process.”
The work was published April 17 in Nature Medicine . Soltesz and Vivek Buch , MD, the Christina and Hamid Moghadam Faculty Scholar as well as the surgical director of the Stanford Comprehensive Epilepsy Center , are co-senior authors.
A tale of a tail
Worldwide, 65 million people live with epilepsy. Tens of millions have mesial temporal lobe epilepsy, with seizures originating, in part, from the amygdala, an almond-shaped structure involved in processing emotions, and the hippocampus, a region necessary for forming memories. When people with mesial temporal lobe epilepsy of just one hemisphere do not respond to anti-seizure drug therapies, the standard of care is surgery. In these procedures, the amygdala and most of the hippocampus in one hemisphere are either surgically removed or ablated, a technique that involves using a laser to heat up and destroy tissue. Because of the symmetry of the temporal lobe — both hemispheres of the brain have an amygdala and hippocampus — people who have these surgeries usually have minimal side effects, according to the researchers.

Ivan Soltesz
Before performing the surgery, physicians need to identify the brain tissue responsible for seizure activity. They do this by placing electrodes in areas of the brain suspected of starting or propagating seizures and taking recordings from the electrodes. This process, called stereoelectroencephalography, or sEEG, lets them map where in the brain seizure activity happens.
Though the amygdala and its next-door neighbor the hippocampus are common locations for sEEG recordings, the electrodes are typically placed in only the anterior and middle regions of the hippocampus. The human hippocampus, located deep in each hemisphere of the brain near the level of the ear, looks like a sea horse lying on its side, with its head pointing toward the front of the brain. sEEG electrodes are commonly placed in the anterior and medial regions, corresponding to the head, body and the beginnings of the tail of the sea horse.
The idea to record from the fasciola cinereum — the far tip of the sea horse’s tail — in patients with epilepsy undergoing sEEG for surgical planning first formed about three years ago, when Ryan Jamiolkowski , MD, PhD, co-lead author of the study and a resident in neurosurgery, joined the Soltesz lab.
At the time, Quynh-Anh Nguyen, PhD, co-lead author on the study and former postdoctoral scholar in the Soltesz lab who is now at Vanderbilt University, was screening for the hippocampal neurons that were active during seizures in mice. Unexpectedly, Nguyen discovered that neurons in a posterior region of the hippocampus, the fasciola cinereum, were involved in seizures.
Jamiolkowski and the research team used optogenetic techniques to test whether the fasciola cinereum could be a target for epilepsy interventions. The neurons in the fasciola cinereum were made to contain special proteins capable of shutting down neuronal activity when exposed to blue light. When electrical recordings from the hippocampus showed seizure activity, the researchers shined blue light onto the fasciola cinereum, shortening the duration of seizures in mice.
Recording from the human hippocampus tail
To understand the fasciola cinereum’s role in seizure activity in humans, Jamiolkowski and Buch recorded from the small region in six patients. All were undergoing sEEG to identify the source of their seizures in preparation for future surgeries to cure their epilepsy. The fasciola cinereum contributed recorded seizures in all six patients, including some episodes in which the head and body regions of the hippocampus were quiet.

Ryan Jamiolkowski
One of the patients with mesial temporal lobe epilepsy of the left hemisphere had already undergone laser ablation of the amygdala and anterior and middle regions of the hippocampus. The patient continued having seizures, and follow-up sEEG showed that the only part of the hippocampus that remained, the fasciola cinereum, was involved in all recorded seizures. The patient underwent a second surgical ablation that removed almost all of the fasciola cinereum, and the frequency of the seizures decreased by 83%, from one to two each month to once every three months.
The researchers said that patients whose seizures involve the fasciola cinereum may need to undergo two surgeries because of the shape of the hippocampus.
“The hippocampus curves like a banana, and the optical fiber used for laser ablation is a straight line. Reaching anterior and posterior regions requires different trajectories that are not currently feasible to combine into one procedure. The results of our study do not challenge the importance of ablating the amygdala and anterior hippocampus but suggest considering a second ablation targeting the posterior hippocampal tail for the patients whose seizures recur,” Jamiolkowski said.
Three of the patients had bilateral involvement of the mesial temporal lobe, which means the amygdala and hippocampus in both the right and left hemisphere showed seizure activity. Because new memories cannot be formed without at least one intact hippocampus, these patients instead received responsive neurostimulation from a device that detects and interrupts seizure activity. However, most responsive neurostimulation units can be configured to target only the anterior regions of the hippocampus on both sides of the brain. The findings from this study suggest that a more personalized approach that also allows the device to monitor and interrupt seizure activity in the posterior hippocampal tail region might be more beneficial to patients.
“Because one-third of patients — a high percentage — do not get seizure freedom from surgery, we should be putting sEEG electrodes in the fasciola cinereum in all temporal lobe epilepsy patients; seizure activity in this region could be a reason why these surgeries sometimes fail,” Jamiolkowski added. “Knowing which patients have seizures involving the fasciola cinereum would let us target it with either ablation or neurostimulation and help us treat patients better than a one-size-fits all approach.”
A researcher from Cambridge University contributed to the study.
Funding for this study was provided by the Stanford Maternal and Child Health Research Institute, the Tashia and John Morgridge Endowed Fellowship, the Lennox-Gastaut Syndrome Foundation Cure 365, the Stanford Neuroscience Scholars Program, and the National Institutes of Health (grants R25NS065741, K99NS121399, K99NS126725, NS121106 and P30AG066515).
- Kimberlee D'Ardenne Kimberlee D'Ardenne is a freelance writer.
About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Artificial intelligence
Exploring ways AI is applied to health care

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Artif Intell

Artificial intelligence assisted acute patient journey
Talha nazir.
1 Research Fellow, NeuroCare.AI Neuroscience Academy, Dallas, TX, United States
Muhammad Mushhood Ur Rehman
Muhammad roshan asghar, junaid s. kalia.
2 NeuroCare.AI, Dallas, TX, United States
3 Neurologypocketbook.com, Dallas, TX, United States
Artificial intelligence is taking the world by storm and soon will be aiding patients in their journey at the hospital. The trials and tribulations of the healthcare system during the COVID-19 pandemic have set the stage for shifting healthcare from a physical to a cyber-physical space. A physician can now remotely monitor a patient, admitting them only if they meet certain thresholds, thereby reducing the total number of admissions at the hospital. Coordination, communication, and resource management have been core issues for any industry. However, it is most accurate in healthcare. Both systems and providers are exhausted under the burden of increasing data and complexity of care delivery, increasing costs, and financial burden. Simultaneously, there is a digital transformation of healthcare in the making. This transformation provides an opportunity to create systems of care that are artificial intelligence-enabled. Healthcare resources can be utilized more justly. The wastage of financial and intellectual resources in an overcrowded healthcare system can be avoided by implementing IoT, telehealth, and AI/ML-based algorithms. It is imperative to consider the design principles of the patient's journey while simultaneously prioritizing a better user experience to alleviate physician concerns. This paper discusses the entire blueprint of the AI/ML-assisted patient journey and its impact on healthcare provision.
Introduction
Artificial intelligence is being used in the industry to leverage data for logistics. Previously, decisions were made at a human level to shelf individual products in a supermarket. Now we see that data enhances human decisions to find the right product and make seasonal recommendations. Similarly, AI will be helping in the complete journey of patients in terms of pre-hospital alert and in-hospital stay, and eventually, creating a pathway for post-hospital care. The healthcare industry is shifting its focus from decreasing readmissions to reducing admissions (Kang et al., 2020 ). Telehealth, health IoT, and other medical devices are being introduced every day. The FDA has recently published a general framework to streamline the integration of medical devices into the healthcare system (FDA, 2021 ).
Almost 25% of the US healthcare budget is being wasted due to multiple factors such as lack of coordination, over-treatment or low-value care, complex administrative procedures, and failure to provide care. Also, the healthcare system is getting crowded due to fewer human resources available (Shrank et al., 2019 ). We have observed the collapse of the healthcare system during the COVID-19 pandemic, and many patients with chronic diseases were left without a physician's consultation. We can improve healthcare provision by leveraging IoT, telehealth, and AI/ML-based algorithms with clinical decision support systems. AI/ML-based applications help apply the 4p model of healthcare (predictive, preventive, personalized, and participatory) (Briganti and Olivier, 2020 ).
Unfortunately, the current available solutions are isolated, and the true power of digital generation to create value in medicine comes from an ecosystem approach. Acute care is the most expensive portion of the United States healthcare system. This paper presents a narrative review of artificial intelligence technologies that can provide value to the community and insight to patients for better healthcare management. It aims to explain how a network of small digital solutions working together in coherence can impact healthcare provision throughout the patient's journey ( Figure 1 ). Furthermore, it provides a broader picture of what the digitization of healthcare means for the future.

Al-Assisted Acute Patient Journey Mapping.
AI/ML has made a significant contribution to a patient's journey from their homes to being released from the hospital. It can aid in gathering data from wearables and earlier health records and, in the end, ingeniously compile a patient's medical history. Furthermore, E-triage and smart clinical decision support systems can help in the allocation of resources more effectively, which in turn will aid in reducing healthcare spending without compromising the standard of care.
Digital tools are now ubiquitous in healthcare, whether in wearable devices or smart monitors in emergency rooms. While digital tools can help patients in a variety of ways, we have focused on the journey of acute patients and highlighted the impact of AI/ML tools on care delivery.
Pre-hospital
One of the critical issues is the identification of patients that require a higher level of care in the pre-hospital settings. There have been many systems based on statistical modeling to generate automated emergency alerts and predict the necessary levels of care, but they lack continuous learning and contextual reinforcement.
Automated emergency response/automated alert system
Automated alert systems may play an essential role in individualized emergency and disaster management. We have limited systems for acute emergencies with connected EMS systems (Pulsara, 2014 ). These systems need to be expanded, and more intelligent systems that link to wearable devices need to be developed.
The interest in applications such as fall and lost detection has risen over the past few years. Wang and the team reviewed the fall detection devices and concluded that these devices focus on offline analytics instead of automated healthcare monitoring. In addition, Apple has already implemented an emergency alert system and an automated fall detection system in the Apple Watch (Apple., 2022 ). We need to increase the sensitivity and specificity of fall detection and integrate it into our existing healthcare system to generate accurate and automated alerts. Furthermore, we can replicate the same process for other problems (Wang et al., 2020 ).
Healthcare data
We live in a digital world, and digital health as a reality relies on data. Machine learning (ML) modules require large amounts of high-quality data as training data to produce “ground truth.” We need to make high-quality real-time data collection a priority. This also creates a double-edged sword, opening the door to privacy and security concerns. Governance and management of data are central to creating secure data warehouses that provide access with differential privacy. Newly developed ML models like federated learning and swarm learning have brought new methods of decentralized learning. These models of decentralized learning will be crucial in healthcare as they provide privacy in learning, minimizing the need for a centralized data warehouse, and are more resourceful as they can push learning to the edge, decreasing cost and latency (Herresthal et al., 2021 ).
In these times of information explosion, it is difficult for healthcare workers to sift through a large amount of data to find pertinent information. AI-based applications are crucial to separating signal from noise. With modern data visualization techniques, these results, like pertinent labs, and imaging, can be presented in an interactive format. Physicians can rapidly identify and act on collected data with contextual information to make better-informed decisions (Stanfill and Marc, 2019 ). Additionally, by analyzing general population behavior and discovering new research avenues (Karan et al., 2022 ) through user-generated content (Saura et al., 2020 ) on social media, we can effectively fill any gaps in healthcare provision. This is the need of time to revolutionize the patient care paradigms and establish best practices to allocate financial resources, as the healthcare industry faces a heavy financial burden (Cai et al., 2020 ).
Wearable devices and eHealth integration
The adoption of wearables is increasing each year. More importantly, these are increasingly being integrated into healthcare. Important patient data like blood pressure, pulse, oxygen saturation, temperature, ambulatory ECG, seizure, and stroke alerts ( Figure 2 ) collected from various devices is being integrated using a software development kit (SDK) by Google Fit™ and Apple HealthKit™ (Henriksen et al., 2018 ). As an example of wearables in healthcare, Embrace 2 detects seizures and notifies users (Embrace, 2018 ). This provides an opportunity for a collaborative and participatory healthcare environment between the patient and provider. When linked to emergency response services, these systems can significantly decrease latency and cost of care. More importantly, it will enable clinical decision support tools for diagnosis and management (Dinh-Le et al., 2019 ).

Health Internet of Things (IoT).
Rather than functioning as a standalone entity, mobile healthcare applications should be integrated into the existing healthcare system. mHealth applications can assist us in deciphering data from wearables and other smart devices. The lack of a standard framework for innovators to work on these avenues is the main barrier to innovation. Labrique and the team proposed a common framework for health-based that addressed all the essential components of the healthcare system, starting with communication, data collection and going all the way to financial transactions and incentives (Labrique et al., 2013 ). In 2019, the FDA also announced the pre-certification program, establishing a framework for regulating digital health goods (FDA, 2019 ). The development of a common framework will incentivize the process of innovation in this field.
Electronic-triage and severity index
The capabilities and availability of an electronic triage system (ETS) are improving. Currently, it is only available for a limited number of diseases and in a limited number of facilities. The core problem is the accuracy of determining disease severity. The Emergency Severity Index (ESI) is a commonly used severity indexing system in the USA. However, most patients fall into level 3 on the ESI. Level 3 is a middle ground between high severity requiring extensive resources and low severity with a decreased resource requirement. This, in essence, does not guide physicians in terms of resource allocation. Levin et al. ( 2018 ) applied a machine learning model to improve the accuracy of level 3 on ESI. They applied the random forest model to the ESI level 3 patient triage data (65% of 172,726 ED visits). ETS tagged almost 22.9% as level 1, compared to 16.9% by ESI. Patients who were up-triaged to level 2 or 1 by ETS were prone to a critical outcome by almost five times and two times more likely to get hospitalized, and similarly decreased the risk of a critical event in patients who were down-triaged to level 4 or 5. Also, the study showed that the detection rate of secondary clinical outcomes was similar to or better than ESI (Levin et al., 2018 ).
Similarly, Kang et al. ( 2020 ) developed an AI algorithm to predict the need for critical care and compared it to existing triage systems. The combination of the AI algorithm and ESI outdid all other scoring systems (Kang et al., 2020 ). Integration of AI/ML-based tools into existing EMS can help streamline the care of patients in the ED.
Resource allocation
Machine learning can be used for appropriate resource allocation to alleviate the overcrowding of ERs. Predicting the length of stay in the ER can help streamline the workflow and prevent resource waste. Yousaf and the team have developed a novel algorithm to decrease the length of stay in ED. By combining a chaotic genetic algorithm and Adaboot (meta-learning), they managed to reduce the length of stay from 5.47 to 4.75 h in public testing at the emergency department of the Recoleta Tolentino Neves Hospital, Brazil. By actively monitoring vitals and labs remotely during the transfer and on-site, AI/ML algorithms can reduce ED resource usage by providing clinical decision support and appropriate allocation of resources (Yousefi et al., 2018 ).
Clinical decision support systems
AI-based clinical decision support system (AI-CDSS) is another avenue that needs to be explored. The poor integration of the existing clinical decision support system can lead to alarm fatigue and physician burnout. However, there are examples to follow in AI-CDSS implementation to improve patient care and provider satisfaction. The Canadian Association of Radiologists has explained in their recent paper that AI-based analysis of imaging will be more sophisticated and easier to integrate into our workflow. The diagnostic accuracy of lung nodules and congenital cataracts has been proven to be comparable to that of a trained physician (Stanfill and Marc, 2019 ).
Duke University Hospital has implemented a sepsis watch tool to detect early signs of sepsis in patients. Despite the lack of previous experience with integrating algorithms based on AI/ML, they could incorporate the tool into their workflow. An algorithm was trained to create an alert almost 12 h before the presentation. Early analysis showed that the median detection time was 5 h before the patient's deterioration, providing ample time for the physician to confirm the diagnosis and intervene (Sendak et al., 2020 ).
Clinical monitoring
Medical monitoring devices are based on the threshold alarming principle and do not contain analytical functions. AI/ML-based applications can help analyze large amounts of data and detect subtle clinical anomalies that humans may overlook (Rush et al., 2019 ). Remote clinical monitoring is vital in monitoring chronic diseases. COVID-19 pandemic has dramatically pushed the healthcare industry toward telehealth and remote monitoring devices. The remote monitoring of blood glucose levels, atrial fibrillation, epilepsy, BP, pulse, temperature, and oxygen saturation can significantly help physicians intervene timely. Also, patients per day visiting can be reduced by resolving minor problems with the help of telehealth and remote monitoring.
Clinical documentation
Documenting clinical journeys with contextual information is helpful for patient pathology accounts and is critical to maintaining quality standards. There is a significant burden for patients and allied health professionals (clinical coordinators, nurse educators, EMS responders) in terms of time to ensure proper time-stamped documentation. Several technologies have recently been introduced to create an ambient intelligence environment. These technologies can improve the quality of documentation while simultaneously reducing the burden on clinicians. (1) Automated Voice Transcription, (2) Digital Voice Assistant for providers, and (3) Voice assistant for patients. However, these technologies need to be incorporated and interoperable with deep integration at a system level to achieve accurate ambient intelligence (Microsoft, 2021 ).
Accurate clinical documentation leads to accurate medical coding, which is essential for (1) reimbursement, (2) quality improvement, and (3) future resource allocation planning. Implementing a common framework is a crucial requirement to allow the interoperability of AI/ML algorithms in the healthcare industry. This standardization and common framework will allow us to have resource planning at the level of a state, country, or even continents compared to county and hospital systems (Stanfill and Marc, 2019 ).
Automated EMR summary
The current EHR applications are hindering the provision of healthcare rather than helping it. The process of finding relevant information is usually manual. EHR systems can be improved by introducing customized EHR systems, using open-source software and customizing it, and incorporating AI/ML-driven applications. Some famous companies such as Epic, Allscripts, Cerner, and Athena are introducing AI/ML-based EHR tools and decision support systems to tackle the problem of data explosion. Many other startups and big names, such as Amazon Web Services and Google, have also introduced cutting-edge AI/ML-based tools (Davenport et al., 2018 ).
Rajkumar and the team published an article discussing the role of deep learning in developing predictive models and recommending that the Fast Healthcare Interoperability Resource (FHIR) be utilized. They have validated their hypothesis by using medical records from two hospitals. Results showed that the deep learning predictive model had outperformed the conventional prediction models in predicting mortality, prolonged length of stay, readmission, and discharge diagnosis. Deep learning predictive models can eliminate many variables that are the main hurdle in conventional predictive models. In addition to presenting relevant charts, history, and labs, to the physicians and paramedical staff, AI/ML integration can also help develop future learning aids (Rajkomar et al., 2018 ).
Disposition and continuity of care
As mentioned above, AI can be crucial for judicious, value-based resource allocation. However, it can be instrumental in automating patient continuity of care. One of the critical issues in mapping the patient journey is quickly moving the patient toward rehabilitation and a home environment. Patients with continuous monitoring will give us the data to make decisions over a longitudinal period compared to brief clinical visits by providers, even in an inpatient setting.
For better health outcomes, it is crucial to avoid unnecessary hospital stays and timely discharge of patients. AI/ML-based models can predict the patients who should be discharged based on their medical records and detect the barriers to discharge (Safavi et al., 2019 ). Mitigating those barriers can significantly reduce the anxiety of extended stays of patients on one hand while optimizing resource allocation and healthcare workers' efficiency on the other. As shown by a TEND Model study (van Walraven and Forster, 2018 ), AI models can predict the number of patients discharged per day. As data becomes more accessible, it will reduce costs and avoid repeating labs. Providing progressive summaries should be an integral part of the patient journey, and AI can aid providers. It can help transfer medical records along with patients without any loss of information.
As we noted above, we can use wearables not only to detect events but also to improve follow-up visitation frequency both in-person and via telehealth. Bian et al. ( 2020 ) conducted research at Peking Union Medical College Hospital. They concluded that AI-assisted follow-up of individual patients is comparable to manual follow-up by phone calls but in a much lesser time, i.e., 0 h compared to 9.3 h per 100 patients. Such interventions can be made sooner via notification. Physicians can provide care by telepresence or in person, depending on the patient's situation, rather than assigning arbitrary 2, 4, 6-week visits (Bian et al., 2020 ).
Health education
Education of the patient and the patient's family is essential to recovery, and many chronic conditions require a higher level of care. Relevant, just-in-time, and mixed media education can significantly improve patients' motivation, adherence, and compliance with medication and rehab therapy. Also, given the electronic nature and reproducibility, the patient can receive education about specific conditions, further increasing the chance of compliance.
Point-of-care education enhanced by AI/ML. Monitoring from various devices can be integrated into one application that can show notifications to educate patients according to their physical needs and current medical status. This kind of tailored education can improve the health outcomes of patients significantly.
Challenges and limitations
Though the advent of digital health tools will improve healthcare, it comes with challenges such as the reliability and validity of mHealth devices, access of the third party to patients' data, and lack of patient data management. Similarly, continuous monitoring might increase stress and raise concerns about patients' health (Volpato et al., 2021 ). Explainability is another critical challenge. Occasionally, the involved doctor may find it difficult or impossible to explain the algorithms responsible for the diagnosis to the patient (Davenport and Kalakota, 2019 ). Patients' privacy is another big concern as we propose more integration of healthcare data to produce wisdom through AI. More integrated systems are more vulnerable to cyberattacks and data theft.
There are substantial ethical challenges in AI implementation in healthcare. Accessibility and inequality have already profoundly impacted healthcare. AI can be expensive, and large portions of humanity may not have access to these tools because companies are charging premium prices for their services. Hence, it has the potential to deepen information inequality as well.
The bidirectional flow of information between healthcare providers and patients is crucial for continuously monitoring patients at risk for recurrent episodes of life-threatening disease. Therefore, it is critical to have a certain level of consistency among digital health tools in predicting the severity of symptoms in out-of-hospital patients. The significant challenges that hinder the implementation of these tools range from their reliability to their integration into existing health systems.
Digital healthcare, like digital banking, will be the future norm. We need to use a design process that enables intelligent communication, coordination, and resource management during the whole journey of acute patients instead of introducing isolated solutions. By integrating smart solutions into the healthcare system as a whole, we can save a tremendous amount of money and enhance healthcare delivery. This type of solution will not be limited to acute settings but can be implemented in outpatient, mobile clinics, and other touchpoints in a patient's journey. We will continue to see further convergence of technologies, enabling new experiences for both patients and providers.
Author contributions
TN had worked on literature research and writing the manuscript along with MM. MA was tasked on researching the literature and keep us updated regarding new modalities and publications and later on worked on limitations section. JK was our mentor who had supervised and helped us in formulating the table of content, editing, writing certain sections of manuscript etc. All authors contributed to the article and approved the submitted version.
JK personally paid for this research article.
Conflict of interest
Authors TN, MM and MA were employed by company NeuroCare.AI Neuroscience Academy. Author JK was employed by company NeuroCare.AI and Neurologypocketbook.com.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
- Apple. (2022). Use fall detection with Apple Watch. Apple Support . Available online at: https://support.apple.com/en-us/HT208944 (accessed August 2, 2022).
- Bian Y., Xiang Y., Tong B., Feng B., Weng X. (2020). Artificial intelligence-assisted system in postoperative follow-up of orthopedic patients: exploratory quantitative and qualitative study . J. Med. Internet Res. 22 :e16896. 10.2196/16896 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Briganti G., Olivier L. M. (2020). Artificial intelligence in medicine: today and tomorrow . Front. Med. 7 , 27–27. 10.3389/fmed.2020.00027 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cai C., Runte J., Ostrer I., Berry K., Ponce N., Rodriguez M., et al.. (2020). Projected costs of single-payer healthcare financing in the United States: a systematic review of economic analyses . PLoS Med. 17 :e1003013. 10.1371/journal.pmed.1003013 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Davenport T., Kalakota R. (2019). The potential for artificial intelligence in healthcare . Future Healthc. J. 6 , 94–98. 10.7861/futurehosp.6-2-94 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Davenport T. H., Hongsermeier T. M., Mc Cord K. A. (2018). Using AI to Improve Electronic Health Records . Available online at: https://hbr.org/2018/12/using-ai-to-improve-electronic-health-records (accessed March 16, 2022).
- Dinh-Le C., Chuang R., Chokshi S., Mann D. (2019). Wearable health technology and electronic health record integration: scoping review and future directions. JMIR Mhealth Uhealth 7 :e12861. 10.2196/12861 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Embrace W. (2018). Embrace2 Seizure Monitoring | Smarter Epilepsy Management | Embrace Watch | Empatica. Empatica . Available online at: https://www.empatica.com/embrace2/ (accessed April 5, 2022).
- FDA (2019). Developing a Software Pre-certification Program: A Working Model. U.S. Food Drug version 1.0 . Available online at: https://www.fda.gov/media/119722/download (accessed February 26, 2022).
- FDA (2021). Proposed Regulatory Framework for Modifications to Artificial Intelligence/Machine Learning (AI/ML)-Based Software as a Medical Device (SaMD). Discussion Paper and Request for Feedback . Available online at: https://www.fda.gov/news-events/press-announcements/fda-releases-artificial-intelligencemachine-learning-action-plan (accessed February 26, 2022).
- Henriksen A., Haugen Mikalsen M., Woldaregay A. Z., Muzny M., Hartvigsen G., Hopstock L. A., et al.. (2018). Using fitness trackers and smartwatches to measure physical activity in research: analysis of consumer wrist-worn wearables . J. Med. Internet Res. 20 :e110. 10.2196/jmir.9157 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Herresthal W. S., Schultze H., Shastry K. L., Manamohan S., Mukherjee S., Garg V., et al.. (2021). Swarm learning for decentralized and confidential clinical machine learning . Nature 594 , 265–270. 10.1038/s41586-021-03583-3 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kang D. Y., Cho K. J., Kwon O., Kwon J. M., Jeon K. H., Park H., et al.. (2020). Artificial intelligence algorithm to predict the need for critical care in prehospital emergency medical services . Scand. J. Trauma Resusc. Emerg. Med. 28 :17. 10.1186/s13049-020-0713-4 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Karan A., Mijwil M. M., Sonia Al-Mistarehi A-H., Safwan A., Gök M., Zein A. M. A., Safaa H. A. (2022). Has the future started? The current growth of artificial intelligence, machine learning, and deep learning . Iraqi J. Comput. Sci. Math. 3 , 115–123. 10.52866/ijcsm.2022.01.01.013 [ CrossRef ] [ Google Scholar ]
- Labrique A. B., Vasudevan L., Kochi E., Fabricant R., Mehl G. (2013). mHealth innovations as health system strengthening tools: 12 common applications and a visual framework . Glob. Health Sci. Pract. 1 , 160–171. 10.9745/GHSP-D-13-00031 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Levin S., Toerper M., Hamrock E., Hinson J. S., Barnes S., Gardner H., et al.. (2018). Machine-learning-based electronic triage more accurately differentiates patients with respect to clinical outcomes compared with the emergency severity index . Ann. Emerg. Med. 71 , 565–574.e562. 10.1016/j.annemergmed.2017.08.005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Microsoft (2021). Project EmpowerMD: Medical Conversations to Medical Intelligence. Microsoft Research . Available online at: https://www.microsoft.com/en-us/research/project/empowermd/ (accessed April 5, 2022).
- Pulsara (2014). Pulsara| Real-Time Team Communication Across Healthcare Entities . Available online at: https://www.pulsara.com/ (accessed April 5, 2022).
- Rajkomar A., Oren E., Chen K., Dai A. M., Hajaj N., Hardt M., et al.. (2018). Scalable and accurate deep learning with electronic health records . NPJ Digit. Med. 1 :18. 10.1038/s41746-018-0029-1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rush B., Celi L. A., Stone D. J. (2019). Applying machine learning to continuously monitored physiological data . J. Clin. Monit. Comput. 33 , 887–893. 10.1007/s10877-018-0219-z [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Safavi K. C., Khaniyev T., Copenhaver M., Seelen M., Zenteno Langle A. C., Zanger J., et al.. (2019). Development and validation of a machine learning model to aid discharge processes for inpatient surgical care . JAMA Netw. Open 2 :e1917221. 10.1001/jamanetworkopen.2019.17221 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Saura J. R., Reyes-Menendez A., Thomas S. B. (2020). Gaining a deeper understanding of nutrition using social networks and user-generated content . Internet Intervent. 20 :100312. 10.1016/j.invent.2020.100312 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sendak M. P., Ratliff W., Sarro D., Alderton E., Futoma J., Gao M., et al.. (2020). Real-world integration of a sepsis deep learning technology into routine clinical care: implementation study . JMIR Med. Inform. 8 :e15182. 10.2196/15182 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shrank W. H., Rogstad T. L., Parekh N. (2019). Waste in the US health care system: estimated costs and potential for savings . JAMA 322 , 1501–1509. 10.1001/jama.2019.13978 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stanfill M. H., Marc D. T. (2019). Health information management: implications of artificial intelligence on healthcare data and information management . Yearb. Med. Inform. 28 , 56–64. 10.1055/s-0039-1677913 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- van Walraven C., Forster A. J. (2018). The TEND (Tomorrow's Expected Number of Discharges) model accurately predicted the number of patients who were discharged from the hospital the next day . J. Hosp. Med. 13 , 158–163. 10.12788/jhm.2802 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Volpato L., Del Río Carral M., Senn N., Santiago Delefosse M. (2021). General practitioners' perceptions of the use of wearable electronic health monitoring devices: qualitative analysis of risks and benefits . JMIR Mhealth Uhealth 9 :e23896. 10.2196/23896 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wang X., Ellul J., Azzopardi G. (2020). Elderly fall detection systems: a literature survey . Front. Robot. AI 7 :71. 10.3389/frobt.2020.00071 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yousefi M., Yousefi M., Ferreira R. P. M., Kim J. H., Fogliatto F. S. (2018). Chaotic genetic algorithm and Adaboost ensemble metamodeling approach for optimum resource planning in emergency departments . Artif. Intell. Med. 84 , 23–33. 10.1016/j.artmed.2017.10.002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
'Taking care of our own': New TTUHSC dean shares goals, talks future of medical school

Traveling to the second floor of the Texas Tech University Health Sciences Center's original building, one will find the dean of the School of Medicine's office. It's a space that has a history of housing both deans and presidents of the university and now welcomes its newest occupant.
Having been named dean and executive vice president of the TTUHSC in February, Dr. John DeToledo's office sits bare except for a few knickknacks scattered throughout the space — a reflection of the humble and soft-spoken occupant.
Before being named to his new position, DeToledo's journey in medicine started decades ago, 5,359 miles south of Lubbock.
Journey from Brazil to Lubbock
DeToledo is a native of São Paulo, Brazil and comes from a long line of family physicians. He said it was only natural for him to attend São Paulo Medical School. He graduated in 1980 but didn't stay there for his residency training. Instead, he moved to Boston.
"I was an exchange student when I was 15 and I lived with a wonderful family in Michigan and I really enjoyed the experience," he said of his previous experience in the United States. "Specializing in this country would open doors for me ... I would not have that same kind of opportunity if I stayed in Brazil for my specialty training."
Gaining a spot at Columbia University for internal medicine, DeToledo crossed paths with his future predecessor — Dr. Steven Berk, who at the time was a doctor in Boston.
It was also during this time that DeToledo said he switched specialties from internal medicine to neurology.
"Neurology is rarely a love at first sight," he said. "Neurology, more often than not, is an acquired taste."
DeToledo said that 3% to 5% of a medical school students have an interest in neurology, which usually stems from undergraduate work done in the field. However, for him, it was different.
"There are some of us that they start in medicine and they find an affinity with the disease of the central nervous system and it's almost as if it clicks," he said. "It becomes effortless to make those connections."
Having switched fields, DeToledo gained additional training at Boston University and the Boston City Hospital and went on to complete his fellowship in epilepsy and neurophysiology at the Oregon Comprehensive Epilepsy Program.
Following his fellowship, DeToledo stayed as the Cornelia Wheeler division chief of Epilepsy until 1992, when his adventure took him to the nation's capital.
"I came to George Washington (University) as a junior professor," he said.
While in Washington, D.C., DeToledo ultimately became the chief of the Division of Epilepsy and Neurophysiology and the Neurology Residency Program Director at WGU, but his adventures were about to go abroad once more.
"I was invited to work in Saudi Arabia - in Riyadh - with King Faisal hospital," he said.
During his six-month stint there, DeToledo helped establish the Epilepsy Program at the King Faisal Specialist Hospital. He returned to the United States to serve as the co-director of the International Center for Epilepsy at the University of Miami in Florida.
That's where he met his wife, and the two would continue their journey together.
DeToledo moved to North Carolina to be Wake Forest University's chief of Epilepsy and Neurophysiology and the chief of the Magnetoencephalography Laboratory. That's when he received a call from an old friend — Dr. Berk - who was recruiting him to TTUHSC.
"When I received the invitation to come and visit, it was primarily because he was here that I came. I did not know much about Texas Tech or Lubbock," he said.
But after visiting Lubbock, DeToldeo said he and his wife agreed Lubbock was unique and appealing to them.
"The commitment of this community to support the university, to support the medical school — the pride that our people have in this school — really impressed me," DeToledo said. "I was invited to join a reception where there were some local people, and they were so proud of Texas Tech. I said, 'Wow, this is so different.'"
DeToledo joined TTUHSC as the Vernon & Elizabeth Haggerton chair of Neurology in 2009.
During his tenure, DeToledo went on to chair the Medical Practice Income Plan and serve as the Chief of Staff at the University Medical Center, along with serving in a position that helped prepare him to take the reins of the medical school.
"Dean Berk offered me the opportunity to become a vice dean for the School of Medicine," DeToledo said. "From that time on, I spent more time with him and being part of discussions about the vision, about the future, about the strategies for the medical school."
DeToledo went on to be named by the TTUHSC's President's Office as acting dean of the School of Medicine from December 2021 through February 2022 after Berk had suffered a medical emergency.
On May 26, 2023, Berk died suddenly after serving as the dean of the School of Medicine for 17 years. The search was on to find who would fill his shoes.
TTUHSC President Lori Rice-Spearman again looked to DeToledo and named him interim dean that same month.
After a nationwide search that resulted in nearly 25 candidates, TTUHSC announced in February 2024 that DeToldeo would be the new dean.
"We are fortunate to have Dr. DeToledo continue in this leadership role for the School of Medicine,” Rice-Spearman said at the time. “He has a great commitment and philosophy to academic medicine that reflects our TTUHSC values-based culture, and he brings a wealth of expertise to the table for an academic health institution as a clinician, clinic manager and physician-scientist.”
According to TTUHSC, DeToledo is tasked with leading faculty and staff in strategic planning, securing resources, and implementing and evaluating activities related to the academic, research, service and patient care operations.
“As an established educator, physician and chairman, Dr. DeToledo has a strong understanding of the School of Medicine and its clinical practice,” TTUHSC Provost and Chief Academic Officer Darrin D'Agostino said after DeToledo was named dean. “He is a respected leader committed to preparing the next generation of clinicians and providing exceptional health care for the communities we serve.”
The vision of the new dean
"The dean very often imparts part of his personality to the rest of the School of Medicine," DeToledo said.
As a regional medical school, DeToledo said he wants TTUHSC to attract students from around the nation but focus on reaching out to local students.
"This is home for them, to come to learn from us, and then to go back to our community and serve in the community," he said. "We pride ourselves in attracting a large number of first-generation physicians."
DeToledo said he will also champion the school's tradition of creating the best primary care physicians in the nation—an accomplishment that Ivy League schools have yet to achieve.
"Texas Tech ranked 19th in the country, in this in this field, and we are very proud of this," De Toledo said smiling.
Having a solid foundation in primary care allows physicians to expand their skills and knowledge to other specialties, DeToledo said. However, primary care is not the only thing TTUHSC wants to be known for.
"What we are now wanting to bring to West Texas is state-of-the-art cancer treatments," he said.
On Thursday, University Medical Center announced the groundbreaking of the new cancer center through a partnership between TTUHSC and the TLC2 Foundation to bring new treatments to West Texas and further cancer research.
More: UMC, TTUHSC break ground on new TLC2 Foundation Cancer Center in Lubbock
DeToledo said the field of medicine changes every five to eight years, with the principles of the field staying the same but the understanding of how the body operates changing.
"So a challenge that we all have is how to keep our are medical school curriculum relevant," he said. "We are committed to provide state of the art, up to date information to our learners so in order to prepare them to be successful when they graduate."
Asked what he wants to emphasize from his goals for the medical school, DeToledo's answer was simple — collaboration. He said he wants to ensure that everyone at TTUHSC works together to improve not only their learning experience but also patients' health and the healthcare field in general.
And one guiding philosophy and commitment will help DeToledo during his tenure as dean, he said.
"Texas Tech is entirely committed to this region, it's entirely committed to our people, it is entirely committed to improve the health of our own in urban areas and rural areas," DeToledo said. "We are laser-focused in taking care of our own, in giving back to our people, because they are so incredibly generous with us."

COMMENTS
Each Journey Is Unique. Your epilepsy story is powerful and can give people hope, empowerment, and safety. Join our community and share your story to talk about epilepsy, seizure safety, and the need to find cures. Make a difference and take action. SHARE YOUR STORY.
On this week's Seizing Life, epilepsy patient, counselor, and author Jon Sadler discusses his 50-year journey living with epilepsy.Jon's experiences reflect many of the challenges and concerns of people with epilepsy including stigma, employment, family, dealing with changing treatments and side-effects, and undergoing life-changing brain surgery.
Treating Epilepsy. Epilepsy treatment involves medical care as well as lifestyle measures. Medication is the most common treatment used to prevent seizures. Still, some people also need surgical procedures or dietary changes if standard medication is ineffective or medication side effects are not tolerable.
Patient journey mapping is an emerging field of research that uses various methods to map and report evidence relating to patient experiences and interactions with healthcare providers, services, and systems. This research often involves the development of visual, narrative, and descriptive maps or tables, which describe patient journeys and ...
Snapshot of Your Child's Epilepsy Journey. Your child's epilepsy care will be customized to their health and your family's needs. Here's a breakdown of common steps in the epilepsy care process: Comprehensive epilepsy evaluation. When we first meet you, our pediatric epilepsy experts (called epileptologists) fully evaluate your child ...
Keywords: epilepsy, patient journey, emotions, qualitative, market research, unmet needs. Citation: Graham-Rowe E, Katzer CB, Riaz S, Attwood A, Bates L, Sainz-Fuertes R and Swan B (2023) Unmet needs of people with epilepsy: A qualitative study exploring their journey from presentation to long-term management across five European countries. Front.
Similarly, Pieters et al. reported testimonies of epilepsy patient caretakers of the trials and tribulations of navigating the road to epilepsy surgery. These caretakers often found the journey to epilepsy surgery to be arduous, lonely, and distressing, especially considering the complexity of epilepsy and the need to make urgent decisions in ...
Epilepsy self-management extends beyond the clinic into the patient's home and community, and ultimately is a synergistic partnership between a patient and their provider. Chronic disease models demonstrate that effective self-management programs and supports can be implemented in clinical and community settings [ 1 , 6 , 9 , 63 - 65 ].
people with epilepsy and caregivers at all stages o f t he patient journey, from presentation thro ugh to monitoring and follo w-up stages. e call for support networks to be es tablished in the ...
The medical management of epilepsy predominantly involves seizure suppression with the long-term use of oral medication ( Table 4 and Table S2). Antiseizure medication is primarily indicated when ...
Epilepsy Brain Surgery in Childhood: What to Expect. We don't consider surgery for any child without lengthy discussions with families, often spanning months. Learn how we decide if surgery is the right epilepsy treatment for your child in our guide to the patient journey. Here's what you can expect before, during and after epilepsy surgery.
The patient journey, however, is a continuum with no single intersection or relationship defining a person's quality of life or how they can get their epilepsy under control. The mission of Nile will not be to replace any current aspect of epilepsy care at those single points in time, but rather to bring them all closer together in a ...
Here's a peek into my journey from med school student to epilepsy attending and how I found the perfect specialty—and training center—for my personality and lifestyle at UNM Health Sciences Center. ... you put together all the pieces of a complicated puzzle to discover what your patient needs. The subspecialty of epilepsy offers a nice ...
Download scientific diagram | The five stages of the 'patient-physician journey'. from publication: Measures for improving treatment outcomes for patients with epilepsy — Results from a ...
Patients journeys. Rare epilepsies patient's journeys describe the specific needs and goals of a patient's path for a rare or complex epilepsy. They describe the health-care pathway and provide a key perspective of those living with a rare disease. In consequence, they allow for a constructive discussion between clinicians and patients.
Perspectives From the Journey of the Patient With Rare Epilepsy. Joseph E. Sullivan, MD; Kelly Knupp, MD; Mary Anne Meskis; and Tracy Dixon-Salazar, PhD, share insight into the patient and provider journey of LGS and Dravet syndrome, from diagnosis through treatment. PATIENTS WITH RARE EPILEPSIES such as Dravet syndrome (DS) and Lennox-Gastaut ...
The Y-axis of the journey represents a patient's 'sense of control' over their epilepsy experience, with higher elevations representing more control both socially and emotionally.
Patient Journey: Children With Epilepsy; Epilepsy Surgery Evaluation Epilepsy Surgery Evaluation. Epilepsy can be caused by different things, such as a genetic disorder or a sudden head injury. Some types of epilepsy are harder to treat than others. If two or more medications haven't helped your child's seizure symptoms, your doctor may ...
The framework approach used in the current study incorporated three core steps: (1) deductive analysis (coding data into the stages of a predefined epilepsy clinical journey map, which was initially based on clinical guidelines for each of the included countries); (2) content analysis (to identify emotions within the patient journey); and (3 ...
The patient continued having seizures, and follow-up sEEG showed that the only part of the hippocampus that remained, the fasciola cinereum, was involved in all recorded seizures. The patient underwent a second surgical ablation that removed almost all of the fasciola cinereum, and the frequency of the seizures decreased by 83%, from one to two ...
Artificial intelligence is taking the world by storm and soon will be aiding patients in their journey at the hospital. The trials and tribulations of the healthcare system during the COVID-19 pandemic have set the stage for shifting healthcare from a physical to a cyber-physical space. A physician can now remotely monitor a patient, admitting ...
DeToledo went on to be named by the TTUHSC's President's Office as acting dean of the School of Medicine from December 2021 through February 2022 after Berk had suffered a medical emergency. On ...