Place of Service 12
Place of Service 12 in Medical Billing:
Place of Service 12 is also called as POS 12 in Medical billing. Place of Service 12 indicated when the patient receives the medical services in patients “Home”.

POS 12 Description:
POS 12 is a place other than a facility or hospital, where the patient receives health care services in a private residence.
Frequently asked questions on place of service 12 :
- When billing for medical services provided at place of service- patient’s home (POS 12), which address we need to report in block# 32? Do you put the patient’s home address or provider’s office address? Or is there a guideline that states that when you bill a service for patient’s home visit, you must have their home Address or patient address on the block# 32 on the claim form?
Answer: When you bill a home visit for a patient, then the claims need to be reported with place of service 12 in the block# 24B and provider’s office (practice) address at the bottom (Block# 32)
2) Patient’s exam for sleep concerns in the wellbeing of their home, which place of service needs to be reported?
Answer: If the Health Sleep Test device is shipped to the patient’s home, the place of service 12 needs to be reported.
3) When billing for Durable Medical Equipment, which place of service to be used?
Answer: Patients uses the Durable Medical Equipment at home (Either Rental or purchased items), place of service 12 is to be indicated on claim form when billing Durable Medical Equipment codes.
4) When billing the services provided at the patient’s home we use place of service 12. Do we need to use the patient’s home address at the bottom on HCFA Claim form?
Answer: Place of Service 12 indicates the services rendered at patient home. So the practice address to be mentioned at the bottom of HCFA Claim form, because place of service is enough for insurance to direct to the patient’s home address (Which will be on top of the HCFA claim form).
5) Does Insurance pay home visits claims billed with office visit E/M Codes 99201-99215 with place of service 12?
Answer: No.
Insurance will never pay the claim and they will deny the claim when office visit codes (99201-99215) billed with place of service 12.Because the services performed in home, but claim billed with an incorrect E/M office visit codes which is an incorrect.
Some providers even do fraudulent for getting paid, for example:
When insurance company will deny the claim submitted with place of service 12 and E/M office visit codes (99201 through 99215), some providers may even try to bill the home visit claim with place of service 11 for E/M office visit codes (99201-99215) in order to get paid. But this is totally fraudulent, because the services are performed in a home and billing the claim as an office visit is fraud.
According to me home visit E/M code should be billed with either new patient codes (99341-99345) or established codes (99347-99350) along with place of service 12.
- Place of Service 24
- Place of Service 31 and Place of Service 32

Place of Service Codes (CMS1500 box 24b)
List of place of service codes, other special considerations.
05-08 Special Considerations Medicare does not currently use the POS codes designated for these settings. Follow the instructions you have received regarding how to process claims for services rendered in IHS and Tribal 638 settings. If you receive claims with these codes, you must initially accept them in terms of HIPAA compliance. However, follow your "return as unprocessable" procedures after this initial compliance check. Follow your "return as unprocessable" procedures when you receive paper claims with these codes. (Note that while these codes became part of the National POS code set effective January 1, 2003, Medicare contractors received instructions regarding how to process claims with these codes effective October 1, 2003, so that Medicare could be HIPAA compliant by October 16, 2003).
When a physician/practitioner furnishes services to a registered inpatient, payment is made under the PFS at the facility rate. To that end, a physician/practitioner/supplier furnishing services to a patient who is a registered inpatient, shall, at a minimum, report the inpatient hospital POS code 21 irrespective of the setting where the patient actually receives the face-to-face encounter. In other words, reporting the inpatient hospital POS code 21 is a minimum requirement for purposes of triggering the facility payment under the PFS when services are provided to a registered inpatient. If the physician/practitioner is aware of the exact setting the beneficiary is a registered inpatient, the appropriate inpatient POS code may be reported consistent with the code list annotated in this section (instead of POS 21). For example, a physician/practitioner may use POS 31, for a patient in a SNF receiving inpatient skilled nursing care, POS 51, for a patient registered in a Psychiatric Inpatient Facility, and POS 61 for patients registered in a Comprehensive Inpatient Rehabilitation Facility.
When a physician/practitioner furnishes services to an outpatient of a hospital, payment is made under the PFS at the facility rate. Physicians/practitioners who furnish services to a hospital outpatient, including in a hospital outpatient department (including in a provider-based department of that hospital) or under arrangement to a hospital shall, at a minimum, report the outpatient hospital POS code 22 irrespective of the setting where the patient actually receives the face-to-face encounter. In other words, reporting the outpatient hospital POS code 22 is a minimum requirement for purposes of triggering the facility payment amount under the PFS when services are provided to a registered outpatient. If the physician/practitioner is aware of the exact setting the beneficiary is a registered hospital outpatient, the appropriate outpatient facility POS code may be reported consistent with the code list annotated in this section (instead of POS 22). For example, physicians/practitioners may use POS code 23 for services furnished to a patient registered in the emergency room, POS 24 for patients registered in an ambulatory surgical center, and POS 56 for patients registered in a psychiatric residential treatment center.
NOTE: Physicians/practitioners who perform services in a hospital outpatient department shall use, at a minimum, POS code 22 (Outpatient Hospital). Code 22 (or other appropriate outpatient department POS code as described above) shall be used unless the physician maintains separate office space in the hospital or on the hospital campus and that physician office space is not considered a provider-based department of the hospital as defined in 42. C.F.R. 413.65. Physicians shall use POS code 11 (office) when services are performed in a separately maintained physician office space in the hospital or on the hospital campus and that physician office space is not considered a provider-based department of the hospital. Use of POS code 11(office) in the hospital outpatient department or on hospital campus is subject to the physician self-referral provisions set forth in 42 C.F.R 411.353 through 411.357.
Thank you for choosing Find-A-Code, please Sign In to remove ads.


- Become a Member
- Everyday Coding Q&A
- Can I get paid
- Coding Guides
- Quick Reference Sheets
- E/M Services
- How Physician Services Are Paid
- Prevention & Screening
- Care Management & Remote Monitoring
- Surgery, Modifiers & Global
- Diagnosis Coding
- New & Newsworthy
- Practice Management
- E/M Rules Archive
April 25, 2024
Codes for Visits in Assisted Living
In 2023, how will we code for visits in assisted living?
January 1 st 2023, the codes for boarding home, rest home and domiciliary care are gone from the CPT® book. What are the codes for visits in assisted living in 2023 and beyond?
Home and residence services (99341—99345 for new patients) and (99347—99350 for established patients) are used for both settings. The definition of home includes a private residence, temporary lodging or short term accommodation, including hotel, campground, hostel or cruise ship. The codes are also used for people in “ assisted living facility, group home (that is not licensed as an intermediate care facility for individuals with intellectual disabilities), custodial care facility, or residential substance abuse treatment facility.”
A patient in assisted living is reported with these codes.
What about patients in continuing care facilities? These are facilities that include both private apartments, condos and homes and assisted living units with support. CPT® doesn’t talk about continuing care facilities, but these often include both completely independent living (home) and supportive care in assisted living. Since the same set of codes are used, does it matter?
Yes, because you still need to select the correct place of service. The place of service code for a home visit is 12. The place of service for assisted living is 13. Both are considered non-facility settings and Medicare pays claims in both settings at the non-facility rate.
Place of service codes
12 Home 13 Assisted living facility 14 Group home 16 Temporary lodging 33 Custodial care facility 55 Residential substance abuse treatment facility
Additional Resources
- Webinar – March 2024 – Home and Nursing Facility Category of Code Rules

E/M Expertise: Go Beyond the Basics | Course
Four module citation-based E/M course!
Non-Members $349
Non-members can take the course for a one-time fee.
Last revised April 8, 2024 - Betsy Nicoletti Tags: office and other E/M
CPT®️️ is a registered trademark of the American Medical Association. Copyright American Medical Association. All rights reserved.
All content on CodingIntel is copyright protected. Any resource shared within the permissions granted here may not be altered in any way, and should retain all copyright information and logos.
- What is CodingIntel
- Terms of Use
- Privacy Policy
Our mission is to provide up-to-date, simplified, citation driven resources that empower our members to gain confidence and authority in their coding role.
In 1988, CodingIntel.com founder Betsy Nicoletti started a Medical Services Organization for a rural hospital, supporting physician practice. She has been a self-employed consultant since 1998. She estimates that in the last 20 years her audience members number over 28,400 at in person events and webinars. She has had 2,500 meetings with clinical providers and reviewed over 43,000 medical notes. She knows what questions need answers and developed this resource to answer those questions.
Copyright © 2024, CodingIntel A division of Medical Practice Consulting, LLC Privacy Policy
An official website of the United States government
Here’s how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

U.S. Dept. of Health & Human Services
CMS Place of Service Code Set
Guidance for place of service codes and descriptions for professional claims.
Issued by: Centers for Medicare & Medicaid Services (CMS)
Issue Date: February 11, 2020
Place of Service Codes for Professional Claims
Database (updated september 2023).
Listed below are place of service codes and descriptions. These codes should be used on professional claims to specify the entity where service(s) were rendered. Check with individual payers (e.g., Medicare, Medicaid, other private insurance) for reimbursement policies regarding these codes.
NOTE : Please direct questions related to billing place of service codes to your Medicare Administrative Contractor (MAC) for assistance.
* Revised, effective April 1, 2004.
** Revised, effective October 1, 2005
HHS is committed to making its websites and documents accessible to the widest possible audience, including individuals with disabilities. We are in the process of retroactively making some documents accessible. If you need assistance accessing an accessible version of this document, please reach out to the [email protected] .
DISCLAIMER: The contents of this database lack the force and effect of law, except as authorized by law (including Medicare Advantage Rate Announcements and Advance Notices) or as specifically incorporated into a contract. The Department may not cite, use, or rely on any guidance that is not posted on the guidance repository, except to establish historical facts.

CAITLYN M. RERUCHA, MD, MSEd, RUBEN SALINAS, JR., MD, JACOB SHOOK, DO, AND MARGUERITE DUANE, MD, MHA
Am Fam Physician. 2020;102(4):211-220
Related Blog: Guest Post: Providing House Calls During the COVID-19 Pandemic
The demand for house calls is increasing because of the aging U.S. population, an increase in patients who are homebound, and the acknowledgment of the value of house calls by the public and health care industry. Literature from current U.S. home-based primary care programs describes health care cost savings and improved patient outcomes for older adults and other vulnerable populations. Common indications for house calls are management of acute or chronic illnesses, coordination of a post-hospitalization transition of care, health assessments, and end-of-life care. House calls may also include observation of activities of daily living, medication reconciliation, nutrition assessment, evaluation of primary caregiver stress, and the evaluation of patient safety in the home. Physicians can use the INHOMESSS mnemonic (impairments/immobility, nutrition, home environment, other people, medications, examination, safety, spiritual health, services) as a checklist for providing a comprehensive health assessment. This article reviews key considerations for family physicians when preparing for and conducting house calls or leading teams that provide home-based primary care services. House calls, with careful planning and scheduling, can be successfully and efficiently integrated into family medicine practices, including residency programs, direct primary care practices, and concierge medicine.
House calls, also referred to as home visits, are increasing in the United States. 1 Approximately 40% of patient visits in the 1930s were house calls. 1 , 2 By 1996, this decreased to 0.5% because insurance reimbursements for house calls decreased. 1 , 2 The pendulum in the United States is swinging again to house calls because of the need to develop care models for the growing aging population. 1 , 3 , 4 The proportion of house calls to outpatient clinic visits conducted by family physicians in the United States is unlikely to reach the 1930s levels; however, the number of house calls conducted from 1996 to 2016 doubled. 3 Medicare Part B billing and reimbursement for house calls are also increasing, with nearly 2.6 million house calls paid in 2015. 5
WHAT'S NEW ON THIS TOPIC
House Calls
There were more than 1,100 direct primary care practices in the United States in 2019, and 68% of these practices offered house calls, including eight practices that were completely mobile (i.e., had no actual office).
A systematic review of nine studies (N = 46,156) evaluating home-based primary care outcomes for homebound older adults reported fewer hospitalizations, hospital bed days of care, emergency department visits, long-term care admissions, and long-term bed days.
The increasing popularity of and call for home-based care have led to an increased need to study the outcomes and design of home-based primary care models in the United States. The two largest home-based primary care studies are the Centers for Medicare and Medicaid Services Independence at Home Demonstration and the U.S. Department of Veterans Affairs home-based primary care program. 6 , 7 The Independence at Home program demonstrated a 23% reduction in hospitalizations, a 27% decrease in 30-day readmissions, and a cost savings of $111 per beneficiary per month, which is a $70 million savings over three years. 7 – 10 Similarly, a large systematic review (N = 46,154; nine studies) evaluating home-based primary care outcomes for homebound older adults reported fewer hospitalizations, hospital bed days of care, emergency department visits, long-term care admissions, and long-term bed days of care. 11 The U.S. Department of Veterans Affairs home-based primary care study of chronically ill, frail adults (N = 179) in urban populations also found fewer hospital admissions and bed days of care, but no change in emergency department use. 12
House calls benefit patients post-hospitalization by reducing readmission rates, associated health care costs, and errors related to transitions of care. 13 , 14 There is an increased need for home-based care for the most vulnerable populations because of the recent shift in the United States toward value-based health care. 1 , 3 In 2011, there were 2 million homebound people in the United States, of which only 12% reported receiving home-based primary care. 15 This number is expected to increase to 4 million by 2030. 1
House calls also benefit patients with socioeconomic barriers to care, including pregnant patients and children who are at high risk of abuse. 16 Nurse- or social worker–led home visiting programs have reduced child maltreatment, decreased child health care overutilization, and improved cognitive skills of children born to a low income household with limited psychological resources. 16 – 18 Outcome data for physician-led house calls are limited for younger populations because most data are from studies on older adults. A meta-analysis of 51 studies of home-based family care reported small, statistically significant improvements in child cognitive outcomes, maternal life outcomes, and parental behaviors and skills. 19 Additionally, a Cochrane review of 11,000 newly postpartum patients receiving frequent in-home visits from interdisciplinary teams showed a decrease in infant health service utilization and an increase in maternal interest in exclusive breastfeeding. 20
Historically, family physicians have been the workforce that meets the critical needs of the United States' most vulnerable populations. Family physicians need to learn how to incorporate house calls into their practices. The Accreditation Council for Graduate Medical Education requires family medicine residents to conduct house calls. 21 Varying the type of calls and including patients with complex needs of all ages add training value that is consistent with the American Academy of Home Care Medicine clinical competencies. 22 House calls, with careful planning and scheduling, can be successfully integrated into a busy office-based practice or residency program. Portable technologies, including electronic health records, battery-powered examination equipment, and point-of-care diagnostic testing, enable health care teams to bring office capabilities to patients' homes. 1 This article provides tools for conducting house calls and reviews strategies for implementing house calls into a variety of outpatient practices, including residency programs, direct primary care (DPC), and concierge medicine models.
Conditions for the Initiation of House Calls
House calls may be needed for acute reasons because of a change in health status, serial visits for chronic conditions, or a one-time visit requested by caregivers or the physician to evaluate for a specific concern. The type of house call guides the goals and objectives for each patient encounter 18 ( Table 1 18 , 21 , 23 , 24 ) . For older adults, consider assessing for geriatric syndromes (e.g., recurrent falls, polypharmacy, frailty, memory loss). Evaluation for suspected elder abuse, neglect, or self-neglect may provide valuable information. Illness or injury prevention house calls for frail, older, homebound adults should focus on preventing functional loss and avoiding hospitalization. 18
A patient who is enrolled in Medicare must meet two criteria to be considered homebound ( Table 2 ) . 25 Most patients who are homebound have chronic medical conditions including heart failure, chronic obstructive pulmonary disease, renal failure, or advanced dementia. The goal of the house call for patients who have a chronic illness is to ensure safety at home, prevent exacerbation of symptoms, and evaluate caregiver burden and ability to care for the patient. 18 Patients enrolled in Medicare who do not meet homebound criteria for home health care may be eligible for home-based primary care services. These services include hospital-based, veterans affairs–based, or freestanding home-based primary care that provides acute and chronic management of medical conditions, polypharmacy management, improved access to durable medical equipment, community resources for the patient and caregivers, and symptom management in end-of-life care. 3 Medical necessity should be documented (i.e., frequently missed appointments, poor medication adherence, high use of emergency department services, or a need to assess function in the home environment). 3
For patients reaching the end of life, care focusing on comfort (rather than function or longevity) is a common reason for house calls. Most patients with terminal cancer want to die at home; therefore, home care is a valuable service that helps reduce the likelihood of death in the hospital. 18 , 26 – 28 House calls made by family physicians for patients who are dying are primarily to provide symptom management such as pain relief for patients not using hospice services, and to provide psychosocial support to the patient and caregivers before death, and to family members and caregivers after the patient's death. 29
Preparing for and Conducting House Calls
Previsit planning is essential to ensure the patient's maximum benefit from a house call. A member of the care team should call the patient in advance of arrival to verify the patient's availability and home address. Physicians should review the patient's medical record and medication list in advance, and bring a copy of the most recent information to the house for reconciliation during the visit. Once the physician is at the home, it is important to follow safety precautions ( Table 3 30 ) to prevent personal injury or infection. 18 , 30 Table 4 18 , 31 and Table 5 18 , 29 , 32 list recommended supplies for house calls.
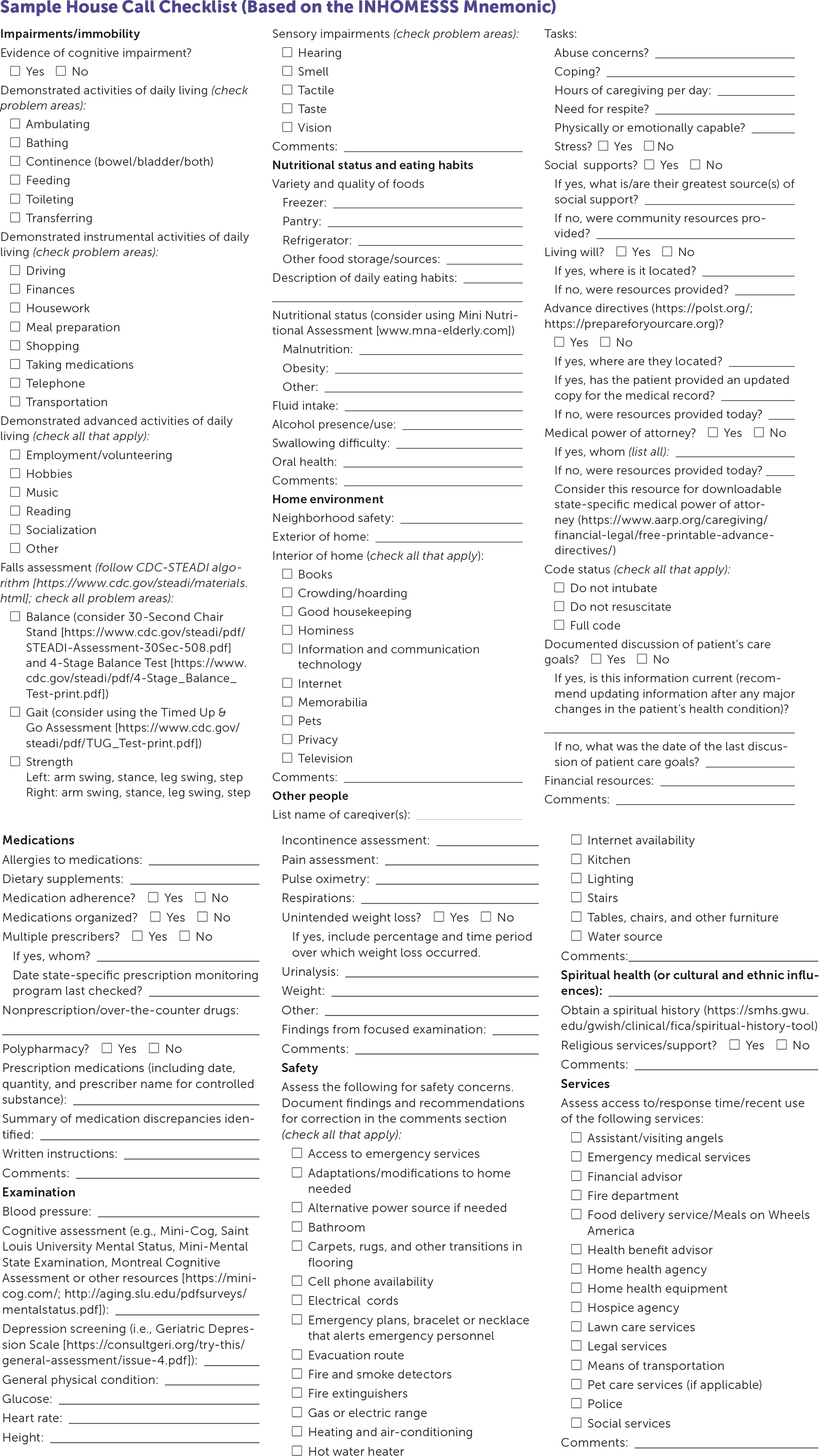
If needed, a house call checklist, such as the INHOMESSS mnemonic (impairments/immobility, nutrition, home environment, other people, medications, examination, safety, spiritual health, services; Figure 1 ), can be used as a guide for performing a complete geriatric assessment. 18 A typical approach begins with observing how the patient enters their home and evaluating for transitions of flooring in entryways and the need for extra grab handles, ramps, or rails. Once inside the home, begin by addressing any urgent patient concerns, then shift the conversation to focus on the items found on the checklist if time permits. This process typically takes 45 to 90 minutes, and frequent breaks are common.
Allocate time to review the patient's prescribed medications, herbs or supplements, and over-the-counter medications. The patient or caregiver should show the physician where these medications are kept and organized to provide further insight into medications that may not have been mentioned, issues with compliance, and identification of stockpiles of old or expired medications. Laying out the medications is recommended to perform true medication reconciliation, in addition to checking for drug-drug interactions.
While the patient is still seated, check vital signs, and perform a focused examination. Once that is completed, the physician should observe the patient as they stand and note if they have difficulty changing positions, need an assistive device to stand (e.g., chair with arms, cane), and how they move around the house (e.g., with a walker, cane, grasping onto furniture). Ask permission to follow the patient through the most frequented areas of the house while observing the patient's gait and noting any balance issues. Looking for transitions in flooring; stairwells; rug placement; pathway obstructions; height of chairs, bed, and toilet; type of showers (walk-in vs. tub); and location of smoke detectors, fire extinguishers, and firearms helps provide an understanding of the patient's functional status and identify potential patient safety and fall hazards ( Table 6 ) . 18
Provide written safety recommendations to the patient and caregiver addressing all urgent concerns and provide additional comments based on findings from the completed checklist. Some durable medical equipment recommendations, such as hospital beds, may be covered by insurance, including Medicare Part B; however, other equipment, such as grab bars or shower chairs, is not typically covered by insurance. The use of assessment tools ( Figure 1 18 ) can be incorporated into the house call based on the complexity of the patient's condition, the time allowed, and the purpose of the visit. Having an in-depth discussion of end-of-life care choices, guided by the patient's goals, may be appropriate, even if they have already been addressed in a clinic or hospital setting. End-of-life care choices should be confirmed or readdressed as the patient's health care situation changes. Providing prescriptions, supplies, handouts with helpful websites, or local resources communicates further support to the patient and caregivers.
Incorporating House Calls into Office-Based Practice
The benefits of house calls are substantial for physicians and their patients. Physicians experience a change of pace from typical clinic appointments, and house calls can provide additional important information about the patient, including insight into a patient's actual home situation, medication management, diet, and overall lifestyle. Patients report experiencing peace of mind, increased respect and trust in their physicians, and better access to care after a house call. 2 , 4 , 33
However, integrating house calls into office-based practice is challenging. Barriers include geography, travel time, and perceived loss of revenue. 18 Grouping house calls together within a half-day, grouping locations, and conducting the visits after the conclusion of a clinic day may minimize this barrier. A multidisciplinary strategy for house calls can help decrease physician burden and improve care. The care team commonly includes a customized combination of a physical therapist, occupational therapist, speech therapist, dietician, licensed social worker, clinical pharmacist, licensed practice/vocational nurse, registered nurse, psychiatric nurse, wound care nurse, and nurse practitioners or physician assistants. With a multidisciplinary team, improved tracking and scheduling of patients can optimize time management, allowing for greater spacing and efficiency of physician visits, and can decrease loss to follow-up.
A travel bag, dedicated house call vehicle, and a mobile office are tools that help keep house calls organized. Besides regular office equipment needed for a focused examination and gathering vitals, an emergency supply kit ( Table 5 18 , 29 , 32 ) may be useful. House calls for dying patients are unique because of the symptoms and treatment needs specific to that population. American Family Physician has previously published an article on managing common symptoms in end-of-life care. 29 Additional specialized equipment may be necessary based on the patient's needs ( Table 4 18 , 31 ) . It is important to have a good understanding of patients' individualized needs and commit to goals for the visit in advance. When applicable, physicians should provide educational materials, medication reconciliation forms, do-not-resuscitate and do-not-intubate forms, out-of-hospital resuscitation forms, home health forms, and hospice-required documents. 18
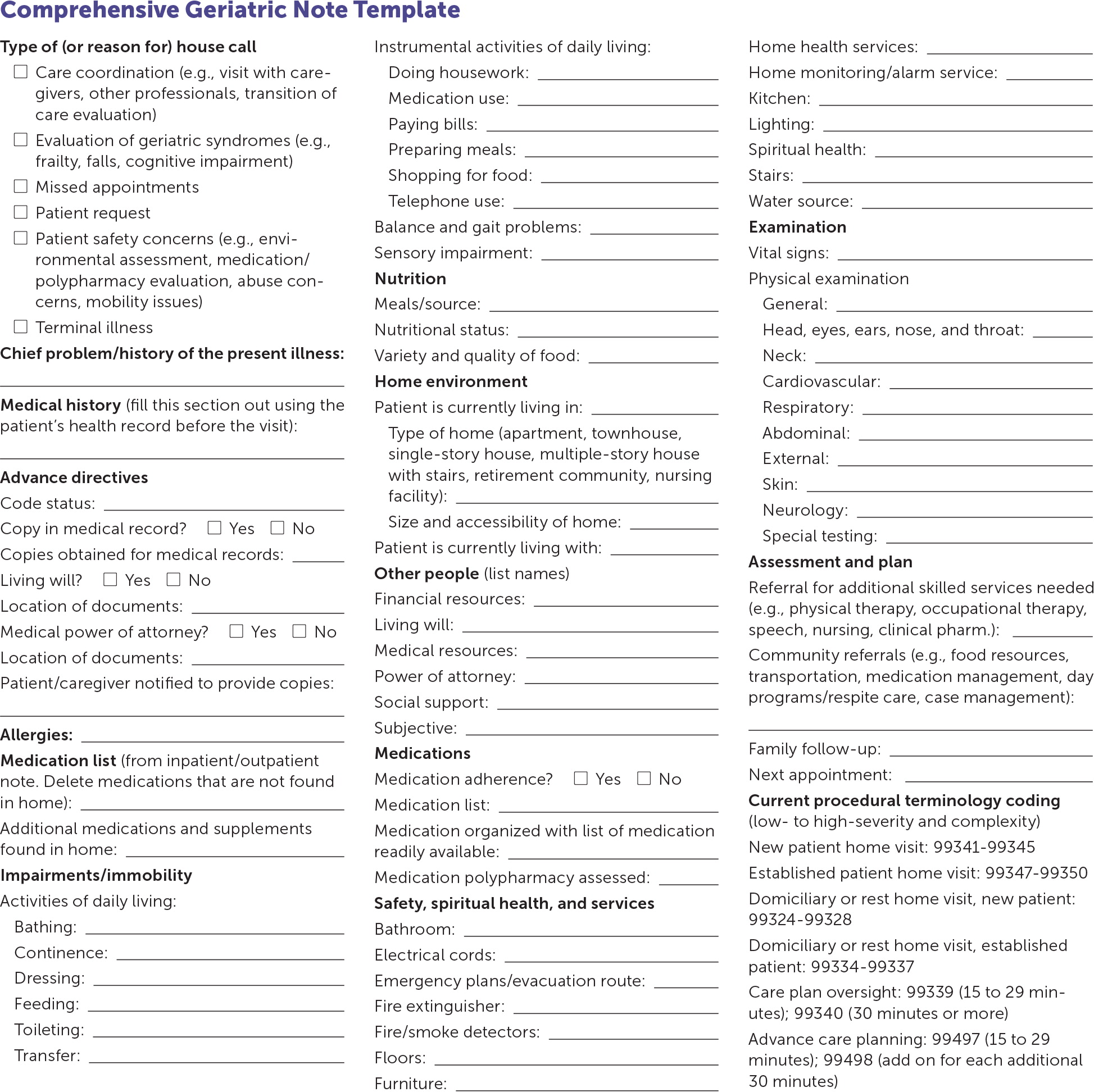
Documentation for a house call is similar to that for an office visit. A note template can help with consistent documentation and serve as a checklist ( eFigure A ) . Recommendations for continued care and changes to the care plan should be included in the documentation with proper coding and billing information ( eTable A ) .
Direct Primary Care and Concierge Medicine House Calls
DPC is an innovative practice model that offers patients a variety of primary care services for a low, periodic membership fee. 34 , 35 Integrating house calls into this type of practice may be easier because the DPC model enables physicians to spend more time with patients, and DPC physicians typically have smaller panel sizes. According to Phil Eskew, DO, founder of DPC Frontier, there were more than 1,100 DPC practices in the United States in 2019, and 68% of these practices offered house calls, including eight practices that were completely mobile (i.e., had no actual office). House calls may be included as part of the membership, or DPC physicians may charge a flat rate or a variable amount based on travel time or mileage. 36
Although DPC physicians often provide house calls to older adults and to patients who are disabled, terminally ill, and to patients who are homebound, some physicians may also offer newborn visits and well-child examinations. Additionally, house calls are commonly made for sick visits and postoperative care. Large families or families with young children may benefit from house calls because of the convenience and comfort of seeing multiple members at once in a familiar and safe environment. DPC physicians report that offering house calls is useful for recruiting new patients, and families appreciate the home-based service.
Concierge practices also routinely offer house calls but charge higher membership fees and may continue to bill insurance for covered services. 37 Concierge practices may also provide hotel calls for travelers seeking more personal, convenient care.
This article updates a previous article on this topic by Unwin and Tatum . 18
Data Sources: A PubMed search was conducted using the key terms home visits, house calls, home-based primary care, post-hospitalization visits, homebound, and direct primary care. The search included systematic and clinical reviews, meta-analyses, reviews of clinical trials and other primary sources, and evidence-based guidelines. Also searched was the Cochrane database. References from these sources were consulted to clarify the statements made in publications. Search dates: April 2019, August 2019, December 2019, and March 2020.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as the official policy or position of the Department of Defense or the U.S. government.
Cornwell T. House calls are reaching the tipping point—now we need the workforce. J Patient Cent Res Rev. 2019;6(3):188-191.
Meyer GS, Gibbons RV. House calls to the elderly—a vanishing practice among physicians. N Engl J Med. 1997;337(25):1815-1820.
Schuchman M, Fain M, Cornwell T. The resurgence of home-based primary care models in the United States. Geriatrics (Basel). 2018;3(3):E41.
Clair MCS, Sundberg G, Kram JJF. Incorporating home visits in a primary care residency clinic: the patient and physician experience. J Patient Cent Res Rev. 2019;6(3):203-209.
American Academy of Home Care Medicine. Number of house calls paid by Medicare Part B. Accessed April 14, 2019. https://www.aahcm.org/page/Number_house_calls
Hughes SL, Weaver FM, Giobbie-Hurder A, et al.; Department of Veterans Affairs Cooperative Study Group on Home-Based Primary Care. Effectiveness of team-managed home-based primary care: a randomized multicenter trial. JAMA. 2000;284(22):2877-2885.
U.S. Department of Health and Human Services. Independence at Home Demonstration performance year 3 results. Accessed May 21, 2019. https://innovation.cms.gov/Files/fact-sheet/iah-yr3-fs.pdf
U.S. Department of Health and Human Services. Report to congress: evaluation of the Independence at Home Demonstration. November 2018. Accessed April 14, 2019. https://innovation.cms.gov/Files/reports/iah-rtc.pdf
Edes T, Kinosian B, Vuckovic NH, et al. Better access, quality, and cost for clinically complex veterans with home-based primary care. J Am Geriatr Soc. 2014;62(10):1954-1961.
Rotenberg J, Kinosian B, Boling P, et al.; Independence at Home Learning Collaborative Writing Group. Home-based primary care: beyond extension of the Independence at Home Demonstration. J Am Geriatr Soc. 2018;66(4):812-817.
Stall N, Nowaczynski M, Sinha SK. Systematic review of outcomes from home-based primary care programs for homebound older adults. Jam Geriatr Soc. 2014;62(12):2243-2251.
Wajnberg A, Wang KH, Aniff M, et al. Hospitalizations and skilled nursing facility admissions before and after the implementation of a home-based primary care program. J Am Geriatr Soc. 2010;58(6):1144-1147.
Gardner R, Li Q, Baier RR, et al. Is implementation of the care transitions intervention associated with cost avoidance after hospital discharge?. J Gen Intern Med. 2014;29(6):878-884.
Coleman EA, Smith JD, Frank JC, et al. Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. J Am Geriatr Soc. 2004;52(11):1817-1825.
Ornstein KA, Leff B, Covinsky KE, et al. Epidemiology of the homebound population in the United States [published correction appears in JAMA Intern Med . 2015;175(8):1426]. JAMA Intern Med. 2015;175(7):1180-1186.
Kitzman H, Olds DL, Knudtson MD, et al. Prenatal and infancy nurse home visiting and 18-year outcomes of a randomized trial. Pediatrics. 2019;144(6):e20183976.
Easterbrooks MA, Kotake C, Fauth R. Recurrence of maltreatment after newborn home visiting: a randomized controlled trial. Am J Public Health. 2019;109(5):729-735.
Unwin BK, Tatum PE. House calls. Am Fam Physician. 2011;83(8):925-938. Accessed December 12, 2019. https://www.aafp.org/afp/2011/0415/p925.html
Filene JH, Kaminski JW, Valle LA, et al. Components associated with home visiting program outcomes: a meta-analysis. Pediatrics. 2013;132(suppl 2):S100-S109.
Yonemoto N, Dowswell T, Nagai S, et al. Schedules for home visits in the early postpartum period. Cochrane Database Syst Rev. 2017(8):CD009326.
Accreditation Council for Graduate Medical Education. Family medicine program requirements and FAQs. Accessed April 19, 2019. https://www.acgme.org/Specialties/Program-Requirements-and-FAQs-and-Applications/pfcatid/8/Family%20Medicine
American Academy of Home Care Medicine. Clinical competencies. Accessed December 20, 2019. https://cdn.ymaws.com/www.aahcm.org/resource/resmgr/homepage/homecaremedicinecomptencies_.pdf
Cauthen DB. The house call in current medical practice. J Fam Pract. 1981;13(2):209-213.
Scanameo AM, Fillit H. House calls: a practical guide to seeing the patient at home. Geriatrics. 1995;50(3):33-36.
Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 7 - Home health services. Accessed October 30, 2019. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c07.pdf
Waller A, Sanson-Fisher R, Zdenkowski N, et al. The right place at the right time: medical oncology outpatients' perceptions of location of end-of-life care. J Natl Compr Canc Netw. 2018;16(1):35-41.
Gomes B, Higginson IJ. Factors influencing death at home in terminally ill patients with cancer: systematic review [published correction appears in BMJ . 2006;332(7548):1012]. BMJ. 2006;332(7540):515-521.
Cohen J, Pivodic L, Miccinesi G, et al. International study of the place of death of people with cancer: a population-level comparison of 14 countries across 4 continents using death certificate data. Br J Cancer. 2015;113(9):1397-1404.
Albert RH. End-of-life care: managing common symptoms. Am Fam Physician. 2017;95(6):356-361. Accessed December 12, 2019. https://www.aafp.org/afp/2017/0315/p356.html
Henriksen K, Battles JB, Keyes MA, et al. Advances in patient safety: new directions and alternative approaches, Vol. 1. assessment. AHRQ Publication No. 08-0034-1. Agency for Healthcare Research and Quality. August 2008. Accessed December 12, 2019. https://bit.ly/3iZBhcO
Yang M, Thomas J, Zimmer R, et al. Ten things every geriatrician should know about house calls. J Am Geriatr Soc. 2019;67(1):139-144.
Giovino JM. House calls: taking the practice to the patient. Fam Pract Manag. 2000;7(6):49-54.Accessed July 14, 2020. https://www.aafp.org/fpm/2000/0600/p49.html
Hayashi J, Christmas C, Durso SC. Educational outcomes from a novel house call curriculum for internal medicine residents: report of a 3-year experience. J Am Geriatr Soc. 2011;59(7):1340-1349.
American Academy of Family Physicians. Direct primary care. Accessed December 19, 2019. https://www.aafp.org/about/policies/all/direct-primary.html
American Academy of Family Physicians. The direct primary care model: how it works. Accessed December 19, 2019. https://www.aafp.org/practice-management/payment/dpc.html
American Academy of Family Physicians. Direct Primary Care Member Interest Group. Poll of group members. Conducted on August 20, 2018, and June 21, 2019. Accessed July 14, 2020. https://www.aafp.org/membership/involve/mig/dpc.html
American Academy of Family Physicians Insurance Program. Direct primary care vs. concierge medicine: which is right for you? March 21, 2016. Accessed December 19, 2019. https://www.aafpins.com/2016/03/direct-primary-care-vs-concierge-medicine-which-is-right-for-you/
Continue Reading

More in AFP
More in pubmed.
Copyright © 2020 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- PBN Current Issue
- PBN User Tools
- PBN Benchmarks
- Ask a PBN Expert
- Part B News Archive
- NPP Report Archive
- PPP Archive
- Coding Resources
- Fee Schedules
- Medicare Transmittals
- Medicare Manual
- Editors' Blog
- Training & Events
Speed E/M coding with a place of service crosswalk

- CMS place of service code set: www.cms.gov/Medicare/Coding/place-of-service-codes/Place_of_Service_Code_Set
- CPT guidelines for 2023 E/M changes: www.ama-assn.org/system/files/2023-e-m-descriptors-guidelines.pdf
Subscribers to Part B News are purchasing access to an online service for a defined subscription period.
Each subscription is for one user. Log-ins and passwords cannot be shared. Multiple subscriptions can be purchased for one or many locations by calling an account representative at 1-800-865-9873. Enterprise wide licenses also are available.
Part B News is a service of DecisionHealth. While we strive to ensure that the information is accurate, we make no representation of its accuracy, completeness or appropriateness for a particular purpose. Therefore, the user assumes full liability for use of the information on this site, and understands and agrees that DecisionHealth is neither responsible nor liable for any claim, loss, or damage resulting from its use.
Copyright ©2010 DecisionHealth. All rights reserved. Do not duplicate or redistribute in any form. Users are granted the right to print out any article and/or newsletter found on the site for individual, personal use. This does not convey permission for commercial use or for making multiple copies for uses internal or external. Use of this web site evidences agreement with these restrictions.
The trademarks, service marks and logos of DecisionHealth, its product-specific brands, or others used on this are the property of DecisionHealth or its respective owners. You may not use any trademark displayed on the site without the written permission of DecisionHealth or its respective owners.
The Forum is temporarily unavailable.

- E&M Guidelines
- CCI Policy Manual

License for Use of "Physicians' Current Procedural Terminology", (CPT) Fourth Edition
End User/Point and Click Agreement: CPT codes, descriptions and other data only are copyright 2009 American Medical Association (AMA). All Rights Reserved (or such other date of publication of CPT). CPT is a trademark of the AMA.
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials including but not limited to CGS fee schedules, general communications, Medicare Bulletin , and related materials internally within your organization within the United States for the sole use by yourself, employees, and agents. Use is limited to use in Medicare, Medicaid, or other programs administered by the Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
This product includes CPT which is commercial technical data and/or computer data bases and/or commercial computer software and/or commercial computer software documentation, as applicable which were developed exclusively at private expense by the American Medical Association, 515 North State Street, Chicago, Illinois, 60610. U.S. Government rights to use, modify, reproduce, release, perform, display, or disclose these technical data and/or computer data bases and/or computer software and/or computer software documentation are subject to the limited rights restrictions of DFARS 252.227-7015(b)(2)(June 1995) and/or subject to the restrictions of DFARS 227.7202-1(a)(June 1995) and DFARS 227.7202-3(a)June 1995), as applicable for U.S. Department of Defense procurements and the limited rights restrictions of FAR 52.227-14 (June 1987) and/or subject to the restricted rights provisions of FAR 52.227-14 (June 1987) and FAR 52.227-19 (June 1987), as applicable, and any applicable agency FAR Supplements, for non-Department Federal procurements.
AMA Disclaimer of Warranties and Liabilities.
CPT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CGS or the CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
CMS Disclaimer
The scope of this license is determined by the AMA, the copyright holder. Any questions pertaining to the license or use of the CPT must be addressed to the AMA. End Users do not act for or on behalf of the CMS. CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CPT. CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL CONTAINED ON THIS PAGE. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material.
This license will terminate upon notice to you if you violate the terms of this license. The AMA is a third party beneficiary to this license.
POINT AND CLICK LICENSE FOR USE OF "CURRENT DENTAL TERMINOLOGY", ("CDT")
End User License Agreement
These materials contain Current Dental Terminology, Fourth Edition (CDT), copyright © 2002, 2004 American Dental Association (ADA). All rights reserved. CDT is a trademark of the ADA.
THE LICENSE GRANTED HEREIN IS EXPRESSLY CONDITIONED UPON YOUR ACCEPTANCE OF ALL TERMS AND CONDITIONS CONTAINED IN THIS AGREEMENT. BY CLICKING BELOW ON THE BUTTON LABELED "I ACCEPT", YOU HEREBY ACKNOWLEDGE THAT YOU HAVE READ, UNDERSTOOD AND AGREED TO ALL TERMS AND CONDITIONS SET FORTH IN THIS AGREEMENT.
IF YOU DO NOT AGREE WITH ALL TERMS AND CONDITIONS SET FORTH HEREIN, CLICK BELOW ON THE BUTTON LABELED "I DO NOT ACCEPT" AND EXIT FROM THIS COMPUTER SCREEN.
IF YOU ARE ACTING ON BEHALF OF AN ORGANIZATION, YOU REPRESENT THAT YOU ARE AUTHORIZED TO ACT ON BEHALF OF SUCH ORGANIZATION AND THAT YOUR ACCEPTANCE OF THE TERMS OF THIS AGREEMENT CREATES A LEGALLY ENFORCEABLE OBLIGATION OF THE ORGANIZATION. AS USED HEREIN, "YOU" AND "YOUR" REFER TO YOU AND ANY ORGANIZATION ON BEHALF OF WHICH YOU ARE ACTING.
- Subject to the terms and conditions contained in this Agreement, you, your employees, and agents are authorized to use CDT-4 only as contained in the following authorized materials and solely for internal use by yourself, employees and agents within your organization within the United States and its territories. Use of CDT-4 is limited to use in programs administered by Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to ensure that your employees and agents abide by the terms of this agreement. You acknowledge that the ADA holds all copyright, trademark and other rights in CDT-4. You shall not remove, alter, or obscure any ADA copyright notices or other proprietary rights notices included in the materials.
- Applicable Federal Acquisition Regulation Clauses (FARS)\Department of Defense Federal Acquisition Regulation Supplement (DFARS) Restrictions Apply to Government use. Please click here to see all U.S. Government Rights Provisions .
- ADA DISCLAIMER OF WARRANTIES AND LIABILITIES. CDT-4 is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values or related listings are included in CDT-4. The ADA does not directly or indirectly practice medicine or dispense dental services. The sole responsibility for the software, including any CDT-4 and other content contained therein, is with (insert name of applicable entity) or the CMS; and no endorsement by the ADA is intended or implied. The ADA expressly disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice to you if you violate the terms of this Agreement. The ADA is a third-party beneficiary to this Agreement.
- CMS DISCLAIMER. The scope of this license is determined by the ADA, the copyright holder. Any questions pertaining to the license or use of the CDT-4 should be addressed to the ADA. End users do not act for or on behalf of the CMS. CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CDT-4. CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL COVERED BY THIS LICENSE. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material.
The license granted herein is expressly conditioned upon your acceptance of all terms and conditions contained in this agreement. If the foregoing terms and conditions are acceptable to you, please indicate your agreement by clicking below on the button labeled "I ACCEPT". If you do not agree to the terms and conditions, you may not access or use the software. Instead, you must click below on the button labeled "I DO NOT ACCEPT" and exit from this computer screen.

Stay Connected
People With Medicare

Search This Blog
Evaluation and management (e/m) services - domiciliary or rest home environment, domiciliary, rest home, or custodial care services cpt codes 99324 - 99337.
These codes are also used to report E/M services in an assisted living facility. The facility’s services do not include a medical component.
A home or domiciliary visit includes a patient History, Physical Examination and Medical Decision Making in various levels depending upon a patient’s needs and diagnosis.
The visits may also be performed as counseling and/or coordination of car, when medically necessary outside the office environment and are an integral part of a continuous of the patient's care.
The patients seen may have chronic conditions, may be disabled, either physically or mentally, making access to a traditional office visit very difficult, or may have limited support systems.
The home or domiciliary visit in turn can lead to improved medical care by identification of unmet needs, coordination of treatment with appropriate referrals and potential reduction of acute exacerbation of medical conditions, resulting in less frequent trips to the Hospital or Emergency services.
The home-based health care is rapidly expanding and growth in hospital-based house call programs.
The Physicians and qualified non-physician practitioners (NPPs) are required to oversee or directly provide progressively more involving a great deal of worldly experience and knowledge of fashion and culture for home visits.
A Patients must understand the nature of a pre-arranged visit and consent to treatment in the home or domiciliary care facility. There is no requirement that the patient must be homebound.
If the service is provided to a patient for the first time, the patient, his/her delegate, or another medical provider managing the patient’s care, must request the service. The visiting provider may not directly solicit referrals.
- An example of inappropriate solicitation is knocking on residents’ doors or placing calls to residents on the telephone to offer medical care services when there has been no referral from another professional that is already involved in the case.
If laboratory and diagnostic tests are performed during the course of home or domiciliary care visits, they must be documented in the medically necessary reason. Medical reasons for repeat testing must be clearly documented.
Every page of the record must be legible and include appropriate patient identification information (e.g., complete name, dates of service[s]).
The documentation must include the legible signature of the physician or non-physician practitioner responsible for and providing the care to the patient.
Many elderly patients have chronic conditions, such as hypertension, diabetes, orthopedic conditions, and abnormalities of the toenails.
Required Criteria
- A home or domiciliary care visit must meet all of the following criteria.
- Chief complaint or a specific, reasonable, and medical necessity is required for each visit.
- A payable diagnosis alone does not support medical necessity of ANY service.
- Medical necessity must exist for each individual visit.
- Visit will be regarded as a social visit unless medical record clearly documents medical necessity for every visit.
- Service/visit must be medically reasonable and necessary and not for physician or qualified NPP convenience.
- Service must be of equal quality to a similar service provided in an office.
- Frequency of visits required to address any given clinical problem should be dictated by medical necessity rather than site of service.
- It is expected that frequency of visits for any given medical problem addressed in home setting will not exceed that of an office setting, except on rare occasion.
- Training of domiciliary staff is not considered medically necessary.
- The E/M service will not be considered medically necessary when it is performed only to provide supervision for a visiting nurse/home health agency visit(s).
Acceptable Location
Home based services are provided services which are performed in,.
- Private Residence - Home, apartment, town-home etc.
- Domiciliary Care Facility - A home providing mainly custodial and personal care for persons who do not require medical or nursing supervision, but may require assistance with activities of daily living because of a physical or mental disability. This may also be referred to as a sheltered living environment.
- Rest Home - A place where people live and are cared for when they cannot take care of themselves.
- Custodial Care Services - Custodial care is non-medical assistance, either at home or in a nursing or assisted-living facility with the activities of daily life (such as bathing, eating, dressing, using the toilet) for someone who's unable to fully perform those activities without help.
- Residential Substance Abuse Facility - A facility which provides treatment for substance (alcohol and drug) abuse to live-in residents.
Place of Service (POS) Codes
- 13 - Assisted Living Facility (adult living facility)
- 14 - Group Home
- 33 - Custodial Care Facility
- 55 - Residential Substance Abuse Facility
Domiciliary, Rest Home, or Custodial Care Services Listing -CPT 99324 to 99337
Cpt code description.
99324 Level 1 new patient domiciliary, rest home, or custodial care visit
99325 Level 2 new patient domiciliary, rest home, or custodial care visit
99326 Level 3 new patient domiciliary, rest home, or custodial care visit
99327 Level 4 new patient domiciliary, rest home, or custodial care visit
99328 Level 5 new patient domiciliary, rest home, or custodial care visit
99334 Level 1 established patient domiciliary, rest home, or custodial care visit
99335 Level 2 established patient domiciliary, rest home, or custodial care visit
99336 Level 3 established patient domiciliary, rest home, or custodial care visit
99337 Level 4 established patient domiciliary, rest home, or custodial care visit
Home Visits Listing - CPT codes 99341 - 99350
- The Home Services codes, are used to report E/M services furnished to a patient residing in his or her own private residence.
- The Private residence considered following, Private home, an apartment, or town home.
CPT Code Description
99341 Level 1 new patient home visit
99342 Level 2 new patient home visit
99343 Level 3 new patient home visit
99344 Level 4 new patient home visit
99345 Level 5 new patient home visit
99347 Level 1 established patient home visit
99348 Level 2 established patient home visit
99349 Level 3 established patient home visit
99350 Level 4 established patient home visit
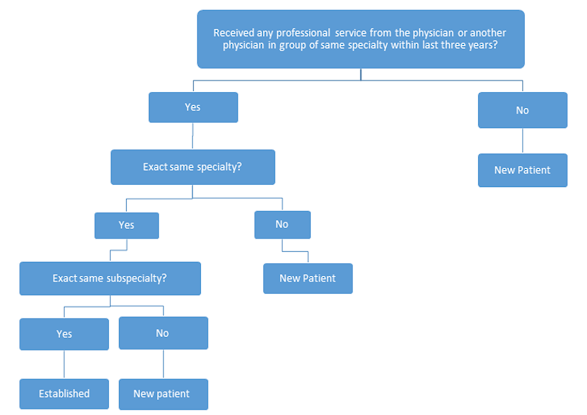
Refer New Patient vs. Established Guidelines
No comments:
Post a Comment
ICD 10 CM Updates
Guidelines for billing cpt g2211.
About CPT G2211 & Objectives Effective from January 1, 2024, the Centers for Medicare and Medicaid Services (CMS) began reimbursing for ...
- Usage of CPT Index - Instructions The alphabetic index is not a substitute for the main text of the CPT codebook. Even if only one code is present, the coder must refer to th...
- Additional Information About Modifiers Sequencing of modifiers How can that be if the modifiers used were accurate? There is an order to reporting modifiers and there are three ...

Free Inquiry (631) 652-3106 | Request a quote

Medical Billing Services for Home-Based Patients: POS 12 Explained
- Medical Billling Services
Touseef Riaz
February 6, 2024.

- ucontrolbilling
For healthcare professionals venturing into home-based care, deciphering the complexities of POS 12 medical billing services is paramount. It’s the key to accurate reimbursement, smooth patient care, and navigating the ever-evolving landscape of healthcare regulations. Worry not, fellow medical experts! This comprehensive guide is your ultimate tool to master the intricacies of POS 12 billing with confidence.
What is POS 12?
POS 12 stands for “Home Location,” signifying medical services rendered in a patient’s private residence, not a traditional healthcare facility. This encompasses a diverse spectrum of care, from routine check-ups and medication management to complex wound care and specialized procedures. Mastering POS 12 billing ensures proper claim coding, maximizes reimbursement, and minimizes the dreaded denials that can disrupt provider and patient workflows.
Why Does POS 12 Billing Matter?

Accurate POS 12 billing goes beyond mere paperwork. It’s about ensuring patients receive the vital care they need in the comfort of their own homes while simultaneously guaranteeing appropriate financial recognition for providers. Think of it as the bridge between delivering quality care and sustaining a thriving practice. Incorrect coding can lead to a cascade of issues, including:
- Claim denials: This translates to delayed or no reimbursement, impacting the provider’s financial stability and the patient’s access to crucial care.
- Administrative headaches: Dealing with denials and appeals consumes valuable time and resources that could be better directed towards patient care.
- Compliance concerns: Inaccurate coding can trigger audits and potential penalties, jeopardizing your reputation and practice.
Mastering the Maze: Key Pointers for POS 12 Billing Success
- Documentation is King: Detailed medical records are your shield against denials. Document the medical necessity for home-based care, including visit summaries, progress notes, and justifications for specific procedures.
- Eligibility Verification: Before embarking on any home visit, confirm the patient’s eligibility for home-based services through their insurance plan. This proactive step prevents wasted effort and potential claim denials.
- Modifier Magic: Remember to underestimate the power of modifiers! Utilize appropriate modifiers like “QW” for home visits to accurately portray the service location and ensure proper claim processing.
- Compliance Compass: Stay abreast of payer-specific rules and regulations regarding POS 12 billing. These guidelines evolve frequently, so regular updates are crucial to avoid compliance pitfalls.
Beyond the Basics: Advanced Strategies for POS 12 Billing Mastery
- Embrace Technology : Invest in robust billing software specifically designed to handle the complexities of POS 12 billing. These tools automate tasks, streamline processes, and minimize errors, freeing up your time for what matters most – patient care.
- Seek Expert Guidance: Consider partnering with specialized POS 12 billing services . Their in-depth knowledge and experience can provide comprehensive support, handle the heavy lifting of claim submissions and appeals, and offer invaluable peace of mind.
- Continuous Learning: The healthcare landscape is constantly shifting, and so should your knowledge. Remain informed about evolving regulations, coding updates, and best practices to optimize your POS 12 billing strategies and stay ahead of the curve.
- Stay Informed: Keep abreast of evolving regulations and coding updates to optimize your billing practices.
POS 12 Medical Billing Reimbursement: A SWOT Analysis
POS 12 medical billing reimbursement refers to the financial compensation healthcare providers receive for services rendered in a patient’s home. This encompasses a wide range of care, from routine check-ups to complex procedures, all delivered in the comfort of the patient’s private residence. To navigate this constantly evolving landscape efficiently, healthcare providers must comprehend the strengths, weaknesses, opportunities, and threats associated with POS 12 reimbursement.
- Increased access to care: POS 12 enables care for patients who may have difficulty travelling to traditional healthcare facilities due to mobility limitations, chronic illnesses, or geographical constraints. This expands access to essential medical services and improves patient outcomes.
- Enhanced patient satisfaction: Home-based care offers a personalized and convenient patient experience, leading to higher satisfaction and improved engagement with healthcare providers.
- Potential for higher reimbursement rates: Certain POS 12 services may qualify for higher reimbursement rates than traditional facility-based care, particularly for complex procedures or patients with chronic conditions requiring ongoing care.
- Providers can save money by eliminating physical infrastructure and overhead expenses.
Weaknesses:
- Complex coding and documentation requirements: Accurate POS 12 billing requires meticulous documentation and proper coding to ensure claim approvals and maximize reimbursement. Mastering the nuances of POS 12 coding can be challenging for some providers.
- Increased risk of claim denials: The intricacies of POS 12 billing can lead to a higher risk of claim denials if documentation or coding errors are present. This can result in financial losses and administrative headaches for providers.
- Limited payer coverage: Not all insurance plans offer comprehensive coverage for POS 12 services. Providers must stay updated on specific payer policies and eligibility requirements to avoid patient surprise bills and potential financial disputes.
- Dependence on patient cooperation: Successful POS 12 care hinges on patient cooperation and adherence to treatment plans. This can be more challenging than a controlled facility environment, potentially impacting outcomes and reimbursement if patients need help with medication adherence or appointment scheduling.
Opportunities:
- Technological advancements: Advancements in healthcare technology, such as telehealth and remote monitoring tools, can enhance the efficiency and effectiveness of POS 12 care, potentially expanding service offerings and attracting new patient populations.
- Growing ageing population: With the ageing population increasing globally, the demand for home-based care is expected to rise significantly. Providers who adapt and excel in POS 12 billing can capture this growing market and secure a thriving practice.
- Policy changes and advocacy: Ongoing efforts to advocate for improved POS 12 coverage and streamlined regulations can pave the way for better patient access to home-based care and increased provider financial stability.
- Collaboration and partnerships: Partnering with other healthcare organizations, community agencies, and technology companies can broaden access to POS 12 services, optimize care coordination, and enhance patient outcomes.
- Competitive landscape: The increasing popularity of POS 12 care attracts new providers entering the market, potentially intensifying competition and impacting reimbursement rates.
- Regulatory changes: Evolving regulations and coding requirements can pose challenges for providers needing to adapt their practices continuously. It is critical to comply with updated rules to avoid penalties and financial losses. It is important to remember that not taking necessary actions can adversely affect both individuals and organizations. It is essential to keep pace with the latest regulations and take all the steps required to comply.
- Economic pressures: Economic downturns and changes in reimbursement policies can negatively impact the financial viability of POS 12 services. Providers must be adaptable and explore alternative revenue streams to navigate potential economic challenges.
- Workforce challenges: Recruiting and retaining qualified healthcare professionals trained in POS 12 care can be a challenge, particularly in rural areas or for specialized services.
POS 11 in Medical Billing
In medical billing, POS 11 stands for Office location, which must not be a hospital, SNF, military treatment facility, community health centre, public health clinic, or ICF. It means the service was provided in a physician’s office, not the facilities above.
Here’s why POS 11 is necessary:
- Accurate claim processing: The correct POS code ensures that claims are submitted and processed correctly. This helps to ensure timely reimbursement and potential denial.
- Proper reimbursement rates: Different POS codes may have different reimbursement rates. Using POS 11 ensures the provider receives the correct reimbursement amount for services.
- Hey there! Did you know that healthcare providers must follow federal and state laws? It’s essential to ensure they comply with regulations to provide the best possible care to patients. Using the correct POS code is one way to ensure compliance.
- Data analysis: POS codes are used to track and analyze healthcare data. This data can be used to improve care quality, identify cost savings areas, and develop new healthcare programs.
Here are some additional things to keep in mind about POS 11:
- It is used for services provided in a physician’s office, but it can also be used in other outpatient settings, such as a clinic or laboratory.
- It is essential to document the location of the service in the medical record. This will help to ensure that the correct POS code is used when billing the claim.
- If you need help determining which POS code to use, contact your billing software provider or insurance company for clarification.
POS 22 in Medical Billing
POS 22 stands for “On-Campus Hospital Outpatient.” This means it signifies services provided within a hospital’s dedicated outpatient department on the same campus. Think of it as a separate clinic within the hospital walls, offering specialized care to non-admitted patients.
So, why is POS 22 necessary?
- Accuracy and Clarity: Using the correct code ensures your claims reach the right ears, avoiding confusion and unnecessary delays. By clearly stating “On-Campus Outpatient,” you prevent your services from being mistakenly billed as in-hospital procedures, which attract different reimbursement rates and regulations.
- Fair Reimbursement: Different settings, different notes! POS 22 ensures you receive the correct financial rhythm for your services in a dedicated outpatient department. Forget the hospital code’s lower melody; POS 22 plays the tune that rightly compensates for your expertise in this setting.
- Compliance Harmony: Just like an orchestra adheres to the conductor’s rules, healthcare providers must follow regulations. POS 22 acts as your compliance guide, demonstrating you’re playing by the hospital’s billing rules and reducing the risk of audits and fines.
- Data Symphony: Healthcare, like music, thrives on information. POS 22 joins the data chorus, adding its voice to track trends, understand resource allocation within the hospital, and inform future decisions about outpatient services.
Remember, POS 22 isn’t just a code; it’s a tool for:
- Efficient and accurate billing for your on-campus outpatient services.
- Securing fair reimbursement for your expertise in this specific setting.
- Maintaining compliance with hospital-specific regulations and avoiding administrative headaches.
- Contributing valuable data to the hospital’s overall understanding of resource allocation and service needs.
In medical billing, POS 99 is a catch-all code for “Other Place of Service.” This category encompasses any service location not specified by the other existing POS codes (ranging from 11 to 21 and beyond). It essentially signifies that the service was rendered in a setting that doesn’t have a dedicated code assigned to it.
POS 21 stands for “Inpatient Hospital.” This code indicates that the service was provided to a hospital inpatient. From routine check-ups to complex surgeries and specialized procedures, a wide range of services are provided within the hospital setting.
Why is POS 21 Important?
- Accurate Claim Processing: Using the correct code ensures your claims reach the right reimbursement pathway. For inpatient services, this means accessing the specific rates and regulations related to hospital admissions. An incorrect code, like an outpatient code for an inpatient stay, can lead to claim denials and financial losses.
- Proper Reimbursement Rates: Inpatient care generally attracts higher reimbursement rates than outpatient services. POS 21 ensures you receive the appropriate compensation for the intensive care and resources dedicated to hospitalized patients.
- Hey, do healthcare providers have to follow specific regulations regarding inpatient care? These regulations ensure patients receive the best care and treatment during their hospital stay. Healthcare professionals must stay up-to-date with these regulations to provide safe and effective patient care.POS 21 demonstrates adherence to these rules, reducing the risk of audits and fines.
In the digital era of healthcare, POS 02 might seem unassuming. Yet, within its two digits lies a powerful champion – Telehealth Provided Other than in Patient’s Home. This code unlocks a world of flexibility and convenience, enabling healthcare providers to deliver vital services beyond the traditional brick-and-mortar walls.
Conclusion:
POS 12 medical billing plays a crucial role in billing for home-based healthcare. U Control Billing understands the significance of accurate coding in medical billing. We help our clients navigate its intricacies. Our services ensure proper reimbursement and compliance and contribute to a growing healthcare model.
What is POS 12 on a claim?
POS 12 on a claim stands for “Home Location, other than a hospital or other facility.” It signifies that the service billed on the claim was provided to the patient in their private residence, not in a traditional healthcare setting like a hospital, clinic, or skilled nursing facility.
What is pos 13 in medical billing?
POS 13 stands for “Assisted Living Facility.” This code specifies that the service was provided to a patient in an assisted living facility (ALF).
What is POS in medical claims?
POS in medical claims stands for “Place of Service”. It’s a two-digit code used to indicate the location where the service billed on the claim was provided. This information is crucial for accurate claim processing, fair reimbursement, and compliance with healthcare regulations.
What is POS 22 on a medical claim?
This code specifies that the service billed on the claim was provided within a dedicated outpatient department located on the same campus as a hospital.
A couple of years ago, I executed the effective plan of creating a Medical billing and Coding company named U Control Billing. The company aims to bring revolutionary advancements to foster medical billing and coding revenues. As an official member of HIA-LI and MGMA, I feel honored in providing networking opportunities, problem-solving, and improving the revenue management cycle.
- Awards and Recognition
- Billing Specialist Duties
- Commercial Insurance
- Free Medical Billing
- Medical Billing
- Medical Billing and Coding Learning
- Medical Billing Software
- Medical Coding
- Telemedicine
- Uncategorized
Recent Posts
- How do you Bill a Broken Arm? What are the ICD Codes? April 23, 2024
- Medical Billing And Coding For Flu Vaccine April 18, 2024
- Understanding Medical Bills for Cirrhosis of Liver April 3, 2024
- Hospice Medical Billing and Coding Services March 27, 2024
- Allergy Medical Billing and Coding Services March 19, 2024
You May Also Like…

How do you Bill a Broken Arm? What are the ICD Codes?
by Touseef Riaz
When it comes to medical billing for a broken arm, healthcare...

Medical Billing And Coding For Flu Vaccine
In medical billing and coding, administering vaccines like the flu...

Understanding Medical Bills for Cirrhosis of Liver
Cirrhosis of the liver is a chronic, progressive disease. It is...
Ready To Get Started?
Pin it on pinterest.
- (888) 886-3GEN
- [email protected]
Billing Instructions For Home Or Residence Services
Starting with claims for services on January 1, 2023, the 2 E/M visit families titled “Domiciliary, Rest Home (e.g., Boarding Home), or Custodial Care Services” and “Home Services” are now 1 E/M code family. The new family is titled “Home or Residence Services.” Use the codes in this family to report E/M services you provide to a patient in:
- Their home or residence
- An assisted living facility
- Group home (that isn’t licensed as an intermediate care facility for individuals with intellectual disabilities)
- Custodial care facility
- Residential substance abuse treatment facility
There are no changes to the included care settings from each respective family, rather the current care settings for each of the current families are in the new, merged family.
This change deletes CPT codes 99324-99337. The following place of service (POS) codes for CPT codes 99341-99350 show the merger of the domiciliary visit codes with the home visit codes:
- Home (POS 12)
- Assisted Living Facility (POS 13)
- Group Home (POS 14)
- Custodial Care Facility (POS 33)
- Residential Substance Abuse Treatment Facility (POS 55)
Source: U.S. Centers for Medicare & Medicaid Services (CMS)
About 3Gen 3Gen Consulting has always been in the forefront when it comes to adding value. We always believe in setting our own standards. What sets us apart is the investment that we make in our people, processes and innovation to provide you with market leading healthcare revenue cycle management services. We work as an extension of our clients’ teams by focusing on their key challenges, aligning with their culture and delivering the best results.
If you’re interested in finding the right medical billing and coding services partner, contact us today .
Get In Touch!

Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps
Place of Service Codes
If your claims are being denied, it is important to make sure the information on your claims is correct. One of the billing issues identified by the government as problematic has to do with coding for the location where services have been provided. Recently, the Centers for Medicare and Medicaid Services (CMS) revised instructions for what Place of Service (POS) codes to use for your claims, and the changes went into effect on November 2016.
These instructions, issued as a result of a report published by the Office of Inspector General (OIG) on improper coding practices by clinicians, are designed to reduce errors in POS coding. Specifically, they help clinicians determine how to assign POS codes when interpreting diagnostic tests outside of the office setting.
POS codes must be assigned based on the setting in which the beneficiary receives the face-to-face service. Because most services include a face-to-face component, this rule applies to the overwhelming majority of services. Where there is no face-to-face requirement, such as where an interpretation of a diagnostic test is performed remotely, you should use the POS code for the setting in which the beneficiary received the test (also referred to as the technical component (TC)) of the test.
This determination is generally made easily when distinguishing between a hospital and physician’s office. However, it becomes much more complex when services are provided in the hospital because a determination will still need to be made as to whether the patient is being treated as an inpatient or outpatient. When reporting POS, CMS instructs providers to pay more attention to the patient’s general inpatient or outpatient hospital status, rather than the precise inpatient or outpatient code. That said, if you know that a determination has been made regarding inpatient or outpatient status, that is what should be reported.
Previously, CMS had instructed practitioners to use the two-digit POS code that described where they were physically located when rendering the service.
A beneficiary receives a myocardial imaging study (78491) at an outpatient department of a hospital near their home. The hospital submits a claim that would correspond to the TC portion of the myocardial imaging study. The physician furnishes the PC portion of the patient’s myocardial imaging study from their office location. POS code 22 (outpatient hospital) should be used on the physician’s claim for the PC to indicate that the beneficiary received the TC, face-to-face portion of the study, at the outpatient hospital.
Place of Service Code Set – Complete https://www.cms.gov/Medicare/Coding/place-of-service-codes/Place_of_Service_Code_Set.html For the complete list of Place-of-Service Codes for Professional Claims, see the current year Current Procedural Terminology (CPT) Book.
Chapter 12 - Physicians/Nonphysician Practitioners 20.4.2 - Site of Service Payment Differential http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf
Chapter 13 - Radiology Services and Other Diagnostic Procedures 150 - Place of Service (POS) Instructions for the Professional Component (PC or Interpretation) and the Technical Component (TC) of Diagnostic Tests https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c13.pdf
Chapter 26 - Completing and Processing Form CMS-1500 Data Set 10.4 - Items 14-33 - Provider of Service or Supplier Information 10.5 - Place of Service Codes (POS) and Definitions 10.6 - Carrier Instructions for Place of Service (POS) Codes http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf
CPT Book, Professional Edition https://catalog.ama-assn.org/Catalog/;jsessionid=B5YR30KIWYEFQCWBGOJVX5Q?_requestid=113916
MLN Matters: MM7631 http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM7631.pdf
OIG Report: http://oig.hhs.gov/oas/reports/region10/11000513.asp
Partial List of POS Codes
For the complete list of Place-of-Service Codes for Professional Claims, see the current year Current Procedural Terminology (CPT) Book.
Coding questions and comments may be sent to [email protected]
JACC Journals on ACC.org
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Email: [email protected]
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- ACC.org Quick Start Guide
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.

IMAGES
VIDEO
COMMENTS
Home and domiciliary visits are when a physician or qualified non-physician practitioners oversee or directly provide progressively more sophisticated E/M visits in a beneficiary's home. ... (POS) Codes. 12 - Home; 13 - Assisted Living Facility (adult living facility) ... (IOM), Publication 100-04, Medicare Claims Processing Manual Chapter 12 ...
Database (updated September 2023) Listed below are place of service codes and descriptions. These codes should be used on professional claims to specify the entity where service (s) were rendered. Check with individual payers (e.g., Medicare, Medicaid, other private insurance) for reimbursement policies regarding these codes.
Place of service codes. The chart below includes a list of approved place of service (POS) codes for use on the Part B CMS-1500 (02-12) claim form or its electronic equivalent. Pharmacy - A facility or location where drugs and other medically related items and services are sold, dispensed, or otherwise provided directly to patients. Telehealth ...
The E/M codes specific to domiciliary, rest home (e.g., boarding home), or custodial care (99324-99238, 99334-99337, 99339, and 99340) have been deleted, and the above codes should also be used in ...
Place of Service 12 indicated when the patient receives the medical services in patients "Home". POS 12 Description: ... According to me home visit E/M code should be billed with either new patient codes (99341-99345) or established codes (99347-99350) along with place of service 12.
However, the guideline for this code set has been revised or expanded to include assisted living facility and group home. Home visits services (CPT ® codes 99341-99350) may only be billed when services are provided in beneficiary's private residence (POS 12). To bill these codes, physician must be physically present in beneficiary's home.
CPT codes 99341 - 99350 show the merger of the domiciliary visit codes with the home visit codes: MLN Matters: MM13004 Related CR 13004 Page 2 of 2 • Home (POS 12) • Assisted Living Facility (POS 13) • Group Home (POS 14) ... "MLN Matters Article,MM13004,POS,home,residence" Created Date: 12/9/2022 4:23:12 AM ...
The provider sees an established patient for a home or residence visit involving evaluation and management (E/M). The visit involves low medical decision making or the provider spends at least 30 minutes of total time on the encounter on a single date. ... 99348 with POS 12. Paid by Noridian Medicare and supplement and second one I looked up is ...
CPT E/M Codes for New Home Visits New Patients: Requires all 3 components per level of service are met or time is met for counseling/ coordination of care visits; POS 12 (Home) New Patient. Typical Time. History . 95 Exam . MDM. 99341; 20; Problem Focused (1-3 HPI, No ROS, No PFSH) Problem Focused (1 body area or system) Straight. forward:
For services provided to a hospice beneficiary in an outpatient setting, such as the physician/nonphysician practitioner's office (POS 11); the beneficiary's home (POS 12), i.e., not operated by the hospice; or other outpatient setting (e.g., outpatient hospital (POS 22)), the patient's physician or nonphysician practitioner or hospice ...
Listed below are place of service codes and descriptions. These codes should be used on professional claims to specify the entity where service(s) were rendered. Check with individual payers (e.g., Medicare, Medicaid, other private insurance) for reimbursement policies regarding these codes. NOTE: Please direct questions related to billing ...
What are the codes for visits in assisted living in 2023 and beyond? Home and residence services (99341—99345 for new patients) and (99347—99350 for established patients) are used for both settings. The definition of home includes a private residence, temporary lodging or short term accommodation, including hotel, campground, hostel or ...
Database (updated September 2023) Listed below are place of service codes and descriptions. These codes should be used on professional claims to specify the entity where service (s) were rendered. Check with individual payers (e.g., Medicare, Medicaid, other private insurance) for reimbursement policies regarding these codes.
House calls, also referred to as home visits, are increasing in the United States. 1 Approximately 40% of patient visits in the 1930s were house calls. 1, 2 By 1996, ... (POS code 12). Home ...
Speed E/M coding with a place of service crosswalk. by: Julia Kyles, CPC Nov 22, 2022. Picking the right E/M family is straightforward when the treating practitioner goes to a nursing facility (POS 32) or the patient's home (POS 12). But it's not always clear when the visit takes place in a psychiatric residential treatment facility (POS 56 ...
Home Services CPT codes 99341 through 99350 should be used with POS code 12 (Home). Reference: Medicare Claims Processing Manual - 100-04. Chapter 12 - Physicians/Nonphysician Practitioners. Section 30.6.14.1 - Home Services (Codes 99341 - 99350) CGS identified an issue within our Kentucky Part B Region that allowed CPT Codes 99201 - 99215 ...
Place of Service (POS) Codes. 12 - Home; 13 - Assisted Living Facility (adult living facility) 14 - Group Home; 33 - Custodial Care Facility; 55 - Residential Substance Abuse Facility; ... Home Visits Listing - CPT codes 99341 - 99350. The Home Services codes, are used to report E/M services furnished to a patient residing in his or her own ...
POS 12 stands for "Home Location," signifying medical services rendered in a patient's private residence, not a traditional healthcare facility. This encompasses a diverse spectrum of care, from routine check-ups and medication management to complex wound care and specialized procedures. Mastering POS 12 billing ensures proper claim ...
The Medicare program uses a two-digit (11 for office) numeric place of service coding structure. The place of service identifies the location where the item was used or the service was performed. A place of service is required for all services and is reported in Item 24B of the CMS-1500 claim form or in the electronic equivalent. The following represents the current POS code set accepted by ...
937. Best answers. 1. Jan 26, 2024. #2. Hi there, you can only report G2211 with office/outpatient visit codes (99202-99215). Here is the full descriptor: Visit complexity inherent to evaluation and management associated with medical care services that serve as the continuing focal point for all needed health care services and/or with medical ...
The following place of service (POS) codes for CPT codes 99341-99350 show the merger of the domiciliary visit codes with the home visit codes: Home (POS 12) Assisted Living Facility (POS 13) Group Home (POS 14) Custodial Care Facility (POS 33) Residential Substance Abuse Treatment Facility (POS 55)
POS codes must be assigned based on the setting in which the beneficiary receives the face-to-face service. Because most services include a face-to-face component, this rule applies to the overwhelming majority of services. ... 12. Home. Location, other than a hospital or other facility, where the patient receives care in a private residence. 13.
A home visit : using codes 99341-99350 with POS 12 : cannot be billed by a physician unless the physician was actually present in the beneficiary's home. Section 10.1.1 in Chapter 1 of this manual provides additional information on billing with POS 12.
Page 1 of 6. MLN901705 February 2024. We pay for specific Medicare Part B services that a physician or practitioner provides via 2-way, interactive technology (or telehealth). Telehealth substitutes for an in-person visit, and generally involves 2-way, interactive technology that permits communication between the practitioner and patient.