Appointments at Mayo Clinic
- Pregnancy week by week

Prenatal care: 1st trimester visits
Pregnancy and prenatal care go hand in hand. During the first trimester, prenatal care includes blood tests, a physical exam, conversations about lifestyle and more.
Prenatal care is an important part of a healthy pregnancy. Whether you choose a family physician, obstetrician, midwife or group prenatal care, here's what to expect during the first few prenatal appointments.
The 1st visit
When you find out you're pregnant, make your first prenatal appointment. Set aside time for the first visit to go over your medical history and talk about any risk factors for pregnancy problems that you may have.
Medical history
Your health care provider might ask about:
- Your menstrual cycle, gynecological history and any past pregnancies
- Your personal and family medical history
- Exposure to anything that could be toxic
- Medications you take, including prescription and over-the-counter medications, vitamins or supplements
- Your lifestyle, including your use of tobacco, alcohol, caffeine and recreational drugs
- Travel to areas where malaria, tuberculosis, Zika virus, mpox — also called monkeypox — or other infectious diseases are common
Share information about sensitive issues, such as domestic abuse or past drug use, too. This will help your health care provider take the best care of you — and your baby.
Your due date is not a prediction of when you will have your baby. It's simply the date that you will be 40 weeks pregnant. Few people give birth on their due dates. Still, establishing your due date — or estimated date of delivery — is important. It allows your health care provider to monitor your baby's growth and the progress of your pregnancy. Your due date also helps with scheduling tests and procedures, so they are done at the right time.
To estimate your due date, your health care provider will use the date your last period started, add seven days and count back three months. The due date will be about 40 weeks from the first day of your last period. Your health care provider can use a fetal ultrasound to help confirm the date. Typically, if the due date calculated with your last period and the due date calculated with an early ultrasound differ by more than seven days, the ultrasound is used to set the due date.
Physical exam
To find out how much weight you need to gain for a healthy pregnancy, your health care provider will measure your weight and height and calculate your body mass index.
Your health care provider might do a physical exam, including a breast exam and a pelvic exam. You might need a Pap test, depending on how long it's been since your last Pap test. Depending on your situation, you may need exams of your heart, lungs and thyroid.
At your first prenatal visit, blood tests might be done to:
- Check your blood type. This includes your Rh status. Rh factor is an inherited trait that refers to a protein found on the surface of red blood cells. Your pregnancy might need special care if you're Rh negative and your baby's father is Rh positive.
- Measure your hemoglobin. Hemoglobin is an iron-rich protein found in red blood cells that allows the cells to carry oxygen from your lungs to other parts of your body. Hemoglobin also carries carbon dioxide from other parts of your body to your lungs so that it can be exhaled. Low hemoglobin or a low level of red blood cells is a sign of anemia. Anemia can make you feel very tired, and it may affect your pregnancy.
- Check immunity to certain infections. This typically includes rubella and chickenpox (varicella) — unless proof of vaccination or natural immunity is documented in your medical history.
- Detect exposure to other infections. Your health care provider will suggest blood tests to detect infections such as hepatitis B, syphilis, gonorrhea, chlamydia and HIV , the virus that causes AIDS . A urine sample might also be tested for signs of a bladder or urinary tract infection.
Tests for fetal concerns
Prenatal tests can provide valuable information about your baby's health. Your health care provider will typically offer a variety of prenatal genetic screening tests. They may include ultrasound or blood tests to check for certain fetal genetic problems, such as Down syndrome.
Lifestyle issues
Your health care provider might discuss the importance of nutrition and prenatal vitamins. Ask about exercise, sex, dental care, vaccinations and travel during pregnancy, as well as other lifestyle issues. You might also talk about your work environment and the use of medications during pregnancy. If you smoke, ask your health care provider for suggestions to help you quit.
Discomforts of pregnancy
You might notice changes in your body early in your pregnancy. Your breasts might be tender and swollen. Nausea with or without vomiting (morning sickness) is also common. Talk to your health care provider if your morning sickness is severe.
Other 1st trimester visits
Your next prenatal visits — often scheduled about every four weeks during the first trimester — might be shorter than the first. Near the end of the first trimester — by about 12 to 14 weeks of pregnancy — you might be able to hear your baby's heartbeat with a small device, called a Doppler, that bounces sound waves off your baby's heart. Your health care provider may offer a first trimester ultrasound, too.
Your prenatal appointments are an ideal time to discuss questions you have. During your first visit, find out how to reach your health care team between appointments in case concerns come up. Knowing help is available can offer peace of mind.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Lockwood CJ, et al. Prenatal care: Initial assessment. https://www.uptodate.com/contents/search. Accessed July 9, 2018.
- Prenatal care and tests. Office on Women's Health. https://www.womenshealth.gov/pregnancy/youre-pregnant-now-what/prenatal-care-and-tests. Accessed July 9, 2018.
- Cunningham FG, et al., eds. Prenatal care. In: Williams Obstetrics. 25th ed. New York, N.Y.: McGraw-Hill Education; 2018. https://www.accessmedicine.mhmedical.com. Accessed July 9, 2018.
- Lockwood CJ, et al. Prenatal care: Second and third trimesters. https://www.uptodate.com/contents/search. Accessed July 9, 2018.
- WHO recommendations on antenatal care for a positive pregnancy experience. World Health Organization. http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/anc-positive-pregnancy-experience/en/. Accessed July 9, 2018.
- Bastian LA, et al. Clinical manifestations and early diagnosis of pregnancy. https://www.uptodate.com/contents/search. Accessed July 9, 2018.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 1st trimester pregnancy
- Can birth control pills cause birth defects?
- Fetal development: The 1st trimester
- Implantation bleeding
- Nausea during pregnancy
- Pregnancy due date calculator
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Prenatal care 1st trimester visits
Make twice the impact
Your gift can go twice as far to advance cancer research and care!

- Pregnancy Classes

Your First Prenatal Visit
If you did not meet with your health care provider before you were pregnant, your first prenatal visit will generally be around 8 weeks after your LMP (last menstrual period ). If this applies to you, you should schedule a prenatal visit as soon as you know you are pregnant!
Even if you are not a first-time mother, prenatal visits are still important since every pregnancy is different. This initial visit will probably be one of the longest. It will be helpful if you arrive prepared with vital dates and information. This is also a good opportunity to bring a list of questions that you and your partner have about your pregnancy, prenatal care, and birth options.
What to Expect at Your First Pregnancy Appointment
Your doctor will ask for your medical history, including:.
- Medical and/or psychosocial problems
- Blood pressure, height, and weight
- Breast and cervical exam
- Date of your last menstrual period (an accurate LMP is helpful when determining gestational age and due date)
- Birth control methods
- History of abortions and/or miscarriages
- Hospitalizations
- Medications you are taking
- Medication allergies
- Your family’s medical history
Your healthcare provider will also perform a physical exam which will include a pap smear , cervical cultures, and possibly an ultrasound if there is a question about how far along you are or if you are experiencing any bleeding or cramping .
Blood will be drawn and several laboratory tests will also be done, including:
- Hemoglobin/ hematocrit
- Rh Factor and blood type (if Rh negative, rescreen at 26-28 weeks)
- Rubella screen
- Varicella or history of chickenpox, rubella, and hepatitis vaccine
- Cystic Fibrosis screen
- Hepatitis B surface antigen
- Tay Sach’s screen
- Sickle Cell prep screen
- Hemoglobin levels
- Hematocrit levels
- Specific tests depending on the patient, such as testing for tuberculosis and Hepatitis C
Your healthcare provider will probably want to discuss:
- Recommendations concerning dental care , cats, raw meat, fish, and gardening
- Fevers and medications
- Environmental hazards
- Travel limitations
- Miscarriage precautions
- Prenatal vitamins , supplements, herbs
- Diet , exercise , nutrition , weight gain
- Physician/ midwife rotation in the office
Possible questions to ask your provider during your prenatal appointment:
- Is there a nurse line that I can call if I have questions?
- If I experience bleeding or cramping, do I call you or your nurse?
- What do you consider an emergency?
- Will I need to change my habits regarding sex, exercise, nutrition?
- When will my next prenatal visit be scheduled?
- What type of testing do you recommend and when are they to be done? (In case you want to do research the tests to decide if you want them or not.)
If you have not yet discussed labor and delivery issues with your doctor, this is a good time. This helps reduce the chance of surprises when labor arrives. Some questions to ask include:
- What are your thoughts about natural childbirth ?
- What situations would warrant a Cesarean ?
- What situations would warrant an episiotomy ?
- How long past my expected due date will I be allowed to go before intervening?
- What is your policy on labor induction?
Want to Learn More?
- Sign up for our weekly email newsletter
- Bonding With Your Baby: Making the Most of the First Six Weeks
- 7 Common Discomforts of Pregnancy
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Leg Cramps During Pregnancy

Prenatal Vitamin Limits

Skin Changes During Pregnancy
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
- Copy/Paste Link Link Copied
What happens during prenatal visits?
What happens during prenatal visits varies depending on how far along you are in your pregnancy.
Schedule your first prenatal visit as soon as you think you are pregnant, even if you have confirmed your pregnancy with a home pregnancy test. Early and regular prenatal visits help your health care provider monitor your health and the growth of the fetus.
The First Visit
Your first prenatal visit will probably be scheduled sometime after your eighth week of pregnancy. Most health care providers won't schedule a visit any earlier unless you have a medical condition, have had problems with a pregnancy in the past, or have symptoms such as spotting or bleeding, stomach pain, or severe nausea and vomiting. 1
You've probably heard pregnancy discussed in terms of months and trimesters (units of about 3 months). Your health care provider and health information might use weeks instead. Here's a chart that can help you understand pregnancy stages in terms of trimesters, months, and weeks.
Because your first visit will be one of your longest, allow plenty of time.
During the visit, you can expect your health care provider to do the following: 1
- Answer your questions. This is a great time to ask questions and share any concerns you may have. Keep a running list for your visit.
- Check your urine sample for infection and to confirm your pregnancy.
- Check your blood pressure, weight, and height.
- Calculate your due date based on your last menstrual cycle and ultrasound exam.
- Ask about your health, including previous conditions, surgeries, or pregnancies.
- Ask about your family health and genetic history.
- Ask about your lifestyle, including whether you smoke, drink, or take drugs, and whether you exercise regularly.
- Ask about your stress level.
- Perform prenatal blood tests to do the following:
- Determine your blood type and Rh (Rhesus) factor. Rh factor refers to a protein found on red blood cells. If the mother is Rh negative (lacks the protein) and the father is Rh positive (has the protein), the pregnancy requires a special level of care. 2
- Do a blood count (e.g., hemoglobin, hematocrit).
- Test for hepatitis B, HIV, rubella, and syphilis.
- Do a complete physical exam, including a pelvic exam, and cultures for gonorrhea and chlamydia.
- Do a Pap test or test for human papillomavirus (HPV) or both to screen for cervical cancer and infection with HPV, which can increase risk for cervical cancer. The timing of these tests depends on the schedule recommended by your health care provider.
- Do an ultrasound test, depending on the week of pregnancy.
- Offer genetic testing: screening for Down syndrome and other chromosomal problems, cystic fibrosis, other specialized testing depending on history.
Prenatal Visit Schedule
If your pregnancy is healthy, your health care provider will set up a regular schedule for visits that will probably look about like this: 1
Later Prenatal Visits
As your pregnancy progresses, your prenatal visits will vary greatly. During most visits, you can expect your health care provider to do the following:
- Check your blood pressure.
- Measure your weight gain.
- Measure your abdomen to check your developing infant's growth—"fundal height" (once you begin to "show").
- Check the fetal heart rate.
- Check your hands and feet for swelling.
- Feel your abdomen to find the fetus's position (later in pregnancy).
- Do tests, such as blood tests or an ultrasound exam.
Talk to you about your questions or concerns. It's a good idea to write down your questions and bring them with you.
Several of these visits will include special tests to check for gestational diabetes (usually between 24 and 28 weeks) 3 and other conditions, depending on your age and family history.
In addition, the Centers for Disease Control and Prevention and the American Academy of Pediatrics released new vaccine guidelines for 2013 , including a recommendation for pregnant women to receive a booster of whooping cough (pertussis) vaccine. The guidelines recommend the shot be given between 27 and 36 weeks of pregnancy. 4
- Centers for Disease Control and Prevention. (2013). Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (TDAP) in pregnant women―Advisory Committee on Immunization Practices (ACIP), 2012. Retrieved September 20, 2013, from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6207a4.htm
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Prenatal visits: What to expect and how to prepare
Regular prenatal visits are an important part of your pregnancy care. Find out how often you'll see a healthcare provider, what to expect at each appointment, and smart ways to prepare.

When to schedule a prenatal visit
Prenatal visitation schedule, how should i prepare for a prenatal visit, what happens during prenatal visits, how can i make the most of my pregnancy appointments.
Make an appointment for your first prenatal visit once you're aware you are pregnant – when you receive a positive home pregnancy test, for example. Booking it around week 8 of pregnancy is typical.
You'll come back regularly in the weeks and months following that initial appointment. Most people have between 8 and 14 prenatal visits throughout the course of their pregnancy.
During this time, you'll see a lot of your healthcare practitioner. That's why it's so important to choose someone you like and trust. If you're not comfortable or satisfied with your provider after your first visit or visits, don't be afraid to find someone with whom you have a better connection.
Typically, a pregnant woman will visit their doctor, midwife , or nurse practitioner every four weeks during the first and second trimesters. In the third trimester, you'll be seen more often – usually every other week until 36 weeks, and then every week until the baby is born.
For more information on what happens at these visits, see:
Your first prenatal visit
Second trimester prenatal visits (14 weeks to 27 weeks)
Third trimester prenatal visits (28 weeks through the end of pregnancy)
The specific number of scheduled appointments you'll have depends on if your pregnancy is considered to be high-risk. This is determined by your medical history and whether you have any complications or conditions that warrant more frequent checkups, such as gestational diabetes , high blood pressure , or a history of preterm labor . If you've had any medical problems in the past or develop any new problems during this pregnancy, you may need more prenatal visits than the average pregnant woman.
In the weeks before each visit, jot down any questions or concerns in a notebook or a notes app on your smartphone. This way, you'll remember to ask your practitioner about them at your next appointment. You may be surprised by how many questions you have, so don't miss the opportunity to get some answers in person.
For example, before you drink an herbal tea or take a supplement or an over-the-counter medication , ask your provider about it. You can even bring the item itself – or a picture of the label – with you to your next appointment. Then, your doctor, midwife, or nurse practitioner can read the label and let you know whether it's okay to ingest.
Of course, if you have any pressing questions or worries, or develop any new, unusual, or severe symptoms , don't wait for your appointment – call your practitioner right away.
In addition to your list, you may want to bring a partner, friend, family member, or labor coach with you to some or all of your prenatal visits. They can comfort you, take notes, ask questions, and help you remember important information.
The goal of prenatal visits is to see how your pregnancy is proceeding and to provide you with information to help keep you and your baby healthy. It's important that you go to all of your prenatal appointments, even if you're feeling just fine and believe that everything is progressing perfectly.
Your practitioner will start by asking how you're feeling physically and emotionally, whether you have any complaints or worries, and what questions you may have. They'll also ask you about your baby's movements once you begin to feel them, typically during the second trimester. Your practitioner will have other questions as well, which will vary depending on how far along you are and whether there are specific concerns.
Your midwife, doctor, or nurse practitioner will also:
- Check your weight , blood pressure , and urine
- Check for swelling
- Measure your abdomen
- Check the position of your baby
- Listen to your baby's heartbeat
- Perform other exams and order tests, as appropriate
- Give you the appropriate vaccinations
- Closely monitor any complications you have or that you develop, and intervene if necessary
Near the end of your pregnancy, your provider may also do a pelvic exam to check for cervical changes. You will also discuss your delivery plan in more depth.
At the end of each visit, your practitioner will review their findings with you. They'll also explain the normal changes to expect before your next visit, warning signs to watch for, and the pros and cons of optional tests you may want to consider. Lifestyle issues will likely be a topic of discussion, as well. Expect to talk about the importance of good nutrition , sleep, oral health, stress management, wearing seatbelts, and avoiding tobacco , alcohol , and illicit drugs.
Many people look forward to their prenatal appointments but are disappointed to find that, with the exception of the first visit, they're in and out of the office in 10 minutes. A quick visit is typical and is usually a sign that everything is progressing normally. Still, you want to make sure your concerns are addressed – and that you and your baby are being well cared for.
Here are some things you can do to ensure that your prenatal visits are satisfying:
- Speak up. Your practitioner isn't a mind reader and won't be able to tell what you're thinking just by performing a physical exam. So, if anything is bothering you, say your piece. Are you having trouble controlling your heartburn ? Managing your constipation ? Suffering from headaches ? This is the time to ask for advice. Consult the notebook of questions you've been compiling. In addition to physical complaints, let your practitioner know if you have emotional concerns or fitness or nutrition questions.
- Ask the staff about the administrative stuff. Save your questions about things like insurance and directions to the hospital for the office staff so your practitioner has more time to answer your health-related questions. Go to the admin staff with any inquiries about payments, scheduling, office policies, and your contact information.
- Be open-minded. When talking with your doctor, midwife, or nurse practitioner, you should feel comfortable speaking freely. But remember to listen, too. Take notes if you find it helpful.
Keep in mind, too, that some days are busier than others. This is especially true during the COVID-19 pandemic. That doesn't mean your practitioner doesn't have to answer your questions, but sometimes a discussion can be continued at the next visit if it's a really busy day or if your practitioner needs to head to the hospital to deliver a baby.
At the same time, don't tolerate a healthcare practitioner who won't give you thorough answers, doesn't show reasonable compassion, or barely looks up from your chart. You and your baby deserve more than that.
Now that you know what to expect during all those prenatal visits, you might like a sneak peek at what else is in store. Here's an overview of the next nine months .
Learn more:
- The ultimate pregnancy to-do list: First trimester
- 12 steps to a healthy pregnancy
- When will my pregnancy start to show?
- Fetal development timeline
Was this article helpful?
What happens at second trimester prenatal appointments

What to expect at your first prenatal appointment

What to expect from third trimester prenatal appointments

Prenatal testing

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
MedlinePlus. (2021). Prenatal care in your first trimester. https://medlineplus.gov/ency/patientinstructions/000544.htm Opens a new window [Accessed September 21, 2021.]
March of Dimes. (2017). Prenatal Care Checkups. https://www.marchofdimes.org/pregnancy/prenatal-care-checkups.aspx Opens a new window [Accessed September 21, 2021.]
Office on Women’s Health. (2019). Prenatal Care and Tests. https://www.womenshealth.gov/pregnancy/youre-pregnant-now-what/prenatal-care-and-tests Opens a new window [Accessed September 21, 2021.]
NIH: Eunice Kennedy Shriver National Institute of Child Health and Human Development. (2017). What happens during prenatal visits? https://www.nichd.nih.gov/health/topics/preconceptioncare/conditioninfo/prenatal-visits Opens a new window [Accessed September 21, 2021.]
NIH: Eunice Kennedy Shriver National Institute of Child Health and Human Development. (2017). What is a high-risk pregnancy? https://www.nichd.nih.gov/health/topics/pregnancy/conditioninfo/high-risk Opens a new window [Accessed September 21, 2021.]
NIH: Eunice Kennedy Shriver National Institute of Child Health and Human Development. (2018). What are some factors that make a pregnancy high-risk? https://www.nichd.nih.gov/health/topics/high-risk/conditioninfo/factors Opens a new window [Accessed September 21, 2021.]
March of Dimes. (2020). Over-the-Counter Medicine, Supplements, and Herbal Products During Pregnancy. https://www.marchofdimes.org/pregnancy/over-the-counter-medicine-supplements-and-herbal-products.aspx Opens a new window [Accessed September 21, 2021.]
Associates in Women’s Healthcare (2021). Preparing for Your First Prenatal Visit. https://www.associatesinwomenshealthcare.net/blog/preparing-for-your-first-prenatal-visit/ Opens a new window [Accessed September 21, 2021.]
National Health Service (UK). (2018). Your baby’s movements. https://www.nhs.uk/pregnancy/keeping-well/your-babys-movements/ Opens a new window [Accessed September 21, 2021.]
MedlinePlus. (2021). Prenatal care in your third trimester. https://medlineplus.gov/ency/patientinstructions/000558.htm Opens a new window [Accessed September 21, 2021.]
UCLA Health. (2021). Schedule of prenatal care. https://www.uclahealth.org/obgyn/workfiles/Pregnancy/Schedule_of_Prenatal_Care.pdf Opens a new window [Accessed September 21, 2021.]
UCR Health. (2021). Healthy Pregnancy: The Importance of Prenatal Care. https://www.ucrhealth.org/2018/07/healthy-pregnancy-the-importance-of-prenatal-care/ Opens a new window [Accessed September 21, 2021.]
Mayo Clinic. (2020). Prenatal care: 1 st trimesters visits. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/prenatal-care/art-20044882 Opens a new window [Accessed September 21, 2021.]

Where to go next


- First Trimester
- OB-GYN & Prenatal Care
What to Expect at the First Prenatal Visit
You got a positive pregnancy test —congratulations are in order! Now it’s time to plan your first prenatal visit. You might be feeling nervous (or is that morning sickness already?!), and you probably have lots of questions, but not to worry—your provider will be there every step of the way. In the meantime, you might want to brush up on what to expect at your first pregnancy appointment. Ready for answers? We’ve consulted with ob-gyns on all the important info.
When Should You Schedule Your First Prenatal Visit?
After you get that positive test, you can take a day or two to soak in the news and celebrate, but it’s a good idea to book that first prenatal visit with your chosen ob-gyn or midwife pretty soon after. (If you haven’t picked a provider yet , you’ll want to get on that ASAP!)
Andrea Braden , MD, IBCLC, an ob-gyn and founder of the lactation company Lybbie , advises to “be on the safe side and give the office a call as soon as you find out you’re pregnant.”
When Will Your First Prenatal Visit Happen?
It’s ideal to schedule your first prenatal visit for when you’re around 7 to 8 weeks pregnant, says Braden. Doctors recommend this timing because that’s when an ultrasound can likely detect baby’s heartbeat . (The earliest a fetal heartbeat can be detected is around week 6, according to Cleveland Clinic .)
If you’ve had complications in an earlier pregnancy, you may want to go in earlier than 7 to 8 weeks. “Sometimes we want to watch these early pregnancies closer because with a history of complications, you have an increased risk of having complications in a subsequent pregnancy,” notes Braden.
On the other hand, if you miss the 7-to-8-week mark, Braden says the goal would be to get you in before 12 weeks, when the first trimester ends. “After that point, just get in as soon as you can because there will be some catching up to do!” she adds.
How Can You Prepare for Your First Pregnancy Appointment?
Want a handy checklist for your first prenatal appointment? Here’s what you need to prepare, according to the experts.
- The date of your last menstrual period (LMP). During your first pregnancy appointment, your ob-gyn will compare the LMP to an ultrasound to determine your due date , says Braden. “If the last period was irregular or unpredictable, sometimes you need to know the first day of the period before that one,” she adds.
- Your medications and medical history. Gather a list of medications and dosages to bring to your provider to discuss their safety during pregnancy, advises Michael Platt-Faulkner , DO, an ob-gyn at St. Elizabeth Physicians in Northern Kentucky. “Writing down any significant personal medical or surgical history and family history of genetic diseases is also helpful information for your visit,” he adds.
- Your pharmacy information. Your doc might prescribe prenatal vitamins or other medications, depending on your medical history, so make sure you have a convenient pharmacy in mind.
- Any questions about symptoms or other concerns. Those first-trimester symptoms—nausea, fatigue, peeing all the time—can cause anxiety. Plus, figuring out what to eat (and not to eat) and questions like “ Can I have coffee while pregnant? ” can be confusing. Platt-Faulker suggests writing all your questions and concerns down for your provider, so you don’t forget them in the heat of the moment.
- Somewhere to track the rest of your pregnancy appointments. “There will be a lot of information coming at you,” says Braden. “You want to have a place to write down future appointments and take any notes.”
What Happens at Your First Prenatal Visit?
What happens at your first prenatal visit can vary widely depending on your state and the type of practice you’re visiting, says Braden. In some practices, you get both an ultrasound and a consultation during your first pregnancy appointment, while other providers’ offices split up these to-dos.
Here’s generally what to expect at your first prenatal appointment.
Your provider may perform an ultrasound to confirm the pregnancy, help determine your due date, check baby’s heart rate and check for any complications, according to Cleveland Clinic . “Oftentimes, an early-pregnancy ultrasound may use a vaginal probe and can be mildly uncomfortable—which can be helpful to know in order to be best prepared for your visit,” says Platt-Faulkner. By about 12 to 14 weeks of pregnancy, your provider will be able to hear baby’s heartbeat with a small device called a Doppler ultrasound, according to Mayo Clinic .
Medical history
“Your provider will review your pregnancy, medical and surgical histories in detail,” says Platt-Faulkner. “Your ob-gyn will [also] review how any medical diagnoses, pregnancy complications or surgical history may affect your pregnancy.” Your provider will also take a look at your medication list and discuss any pregnancy-related safety concerns with the medications you’re taking. Omoikhefe Akhigbe , MD, an ob-gyn at Pediatrix Medical Group in Maryland, adds that your provider may also discuss whether there are any specialty doctors you should start seeing or continue to see.
Lifestyle discussion
Your provider will discuss the lifestyle choices you plan to make during pregnancy. (Remember that, for starters, that means no smoking or alcohol .) “You’ll learn about foods that are safe to eat in pregnancy and the way to keep yourself healthy,” says Braden. “They will answer questions about exercise, diet, nutrition, rest, common symptoms and how to treat them and what to do if you do have discomfort in pregnancy.”
Genetic testing
At your first pregnancy appointment, your provider might perform or discuss future genetic testing. “There are genetic tests that are time-sensitive and can be done as early as 10 weeks,” says Braden. “There are some that are done with an ultrasound around 12 or 13 weeks pregnant, and some that are done in the second trimester. Depending on your history and what you desire, that’ll likely be brought up.” There are some specific tests your provider may offer based on your age or family history too, she adds.
Blood testing
You’ll likely get blood drawn during your first prenatal visit. You’ll be tested for a variety of conditions, including anemia, hepatitis B, syphilis and HIV, as well as for your blood type and Rh factor .
Urine testing
For starters, your provider might test a urine sample to confirm your pregnancy, as well as to test kidney function and screen for the presence of protein, as noted by the Cleveland Clinic .
Physical exam
You can expect a full physical exam at your first prenatal visit, which may include a pelvic examination and a breast exam. “If you’re due for a pap smear and you’re over 21 years of age, then you can expect that you’ll have a pap smear screening test done for cervical cancer along with an HPV test if indicated,” says Braden. “Typically, we also test for sexually transmitted infections at the time of the first prenatal visit.”
Questions to Ask at Your First Prenatal Visit
You’re likely full of questions—and that’s completely normal! Make sure to write them down—and bring this list to your first prenatal appointment in case you feel like you’re forgetting something.
- Questions about symptoms. Of course, you should bring any questions about symptoms to your appointment. Akhigbe says it’s also important to ask “when and where to call for an urgent question, what constitutes an emergency, what is an urgent question and what is a routine question that could probably wait for normal business hours.”
- Questions about testing. Which tests will you need during pregnancy? What will your insurance pay for? “Ask about common resources to use and where you can find the evidence-based information about your pregnancy and guidelines and information about tests,” advises Braden. A lot of people also want to know when they’ll find out baby’s sex , she adds. (Spoiler alert: With non-invasive prenatal testing (NIPT) , you can find out as early as 10 weeks.)
- Questions about your ultrasound plan. How many ultrasounds will you get? “Sometimes it depends on insurance, sometimes it depends on your medical history and sometimes it depends on your provider. Do they do them in-house or at a different center?” says Braden.
- Questions about lifestyle choices. Your doctor will review information about how to eat a healthy pregnancy diet with you, but if you have any specific concerns—such as about drinking alcohol or eating sushi—be sure to let them know.
- Questions about logistics. You’ve got a long journey ahead of you! Your provider will likely “review their practice structure, visit schedule and confirm the hospital where you’ll deliver,” says Platt-Faulkner. But if they’ve missed anything, Akhigbe recommends asking follow-up logistical questions, like how many providers you’ll see and which doctor is most likely to deliver baby. (Remember, there are no guarantees!)
There’s a lot of information to take in at your first prenatal visit. It might seem overwhelming, so make sure to bring questions, take notes and do whatever else you need to feel comfortable. Bringing your partner or a good friend along for the ride can help ease some nerves too. “If you have a support person that will be going along this journey with you, it’s always great to bring them to this visit if that’s allowed,” says Braden.
While it might feel like a lot to take in, know that your provider is there to make sure you and baby are healthy during your first prenatal visit and throughout your whole pregnancy—and that you’re making a wonderful first step in your pregnancy journey.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
15 Early Signs of Pregnancy
Pregnancy Checklist: Your First Trimester To-Dos
When Do You Start Showing in Pregnancy?
Omoikhefe Akhigbe , MD, is an ob-gyn and medical director at Pediatrix Medical Group in Maryland. She earned her medical degree from Meharry Medical College School of Medicine in Nashville, Tennessee.
Andrea Braden , MD, IBCLC, is an ob-gyn, board-certified lactation consultant and founder of the lactation company Lybbie . She earned her medical degree from the University of South Alabama School of Medicine.
Michael Platt-Faulkner , DO, is an ob-gyn at St. Elizabeth Physicians in Northern Kentucky. He earned his medical degree from the Heritage College of Osteopathic Medicine at Ohio University.
Cleveland Clinic, Fetal Development , March 2023
Cleveland Clinic, Ultrasound in Pregnancy , September 2022
Mayo Clinic, Prenatal Care: 1st Trimester Visits , August 2022
Nemours KidsHealth, Prenatal Tests: First Trimester , July 2022
Cleveland Clinic, NIPT Test , October 2022
Cleveland Clinic, Your First Prenatal Appointment: What to Expect , December 2022
Learn how we ensure the accuracy of our content through our editorial and medical review process .
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.
Next on Your Reading List

MOM FOR THE LITTLES
Info and tips for all things bump, birth, breastfeeding and baby!
Pregnancy · July 8, 2023
First Prenatal Visit: What to Expect and How to Prepare
This post may contain affiliate links, which means I'll earn a commission, at no extra cost to you, if you make a purchase through those links. For more info, please read my affiliate disclosure. As an Amazon Associate, I earn from qualifying purchases. For the latest deals, visit my exclusive discount codes page.

Congrats on your pregnancy, mama! Did you already schedule your first prenatal visit?!
I know the wait between a positive pregnancy test and your first prenatal visit can feel like foreveeer …
And a bit surreal too.
Then you FINALLY get to go to your first prenatal appointment and BAM— the reality of your pregnancy really hits you!
After all, that’s when your pregnancy will be confirmed!
But in the meantime, while you’re waiting, you may be thinking a lot about your first pregnancy appointment.
What should I expect? How do I prepare? What should I wear? What questions should I ask?
So to shed some light on what may be the longest prenatal appointment you’ll ever have, let’s get into your first prenatal visit: what to expect and how to prepare !
In this post
When to make your first prenatal appointment
Before you call to make a prenatal appointment, make sure you have this info ready:, an example of what to say when scheduling your first prenatal appointment:, urine sample, confirmation of your pregnancy, calculation of your estimated due date, blood pressure check, weight check, review of you and your family’s medical history, surgical history, reproductive history, gynecological history, medication history, review of previous or current substance use, review of lifestyle habits, review of social and mental health history, assessment for domestic violence, full physical exam including pelvic exam and pap smear, fetal heart check, schedule next prenatal appointment, what is the normal schedule of routine prenatal care, how to prepare for your first prenatal visit, what questions to ask at your first prenatal visit, 7 tips and hacks to help you make the most of your prenatal appointments, now you’re totally ready for your first prenatal visit.
So when should you make your first prenatal appointment?
My BEST answer is to call to schedule a prenatal appointment as soon as you get a big fat positive (BFP) on your pregnancy test .
Even though you won’t get seen until you’re about about 8-10 weeks pregnant.
Why? Because prenatal appointments are booked pretty quickly. And the longer you wait, the further into the future your first prenatal appointment will be scheduled.
It’s bad enough that waiting for your first prenatal visit can feel like an eternity. So spare yourself those extra days (or weeks) of anxious waiting…
And call, like right now, if you haven’t already.
What to say when scheduling your first prenatal visit
I totally get it. This may be your first pregnancy, you might be nervous, shy or have social anxiety. It’s possible you never made a call to schedule an appointment before.
So I’m going to give you a script of what to say when scheduling your first prenatal appointment!
But before doing that, I want to give you some tips on how to prepare for the call. This is REALLY important!
- Name and date of birth (DOB): Yep, have your name and DOB ready LOL. Trust me, nervousness can make you forget your name, age, DOB, the reason why you’re calling in the first place, etc.
- First day of your LMP: They might ask, so they can get an idea of how far along you are in your pregnancy.
- Insurance cards: You’ll most likely be asked to provide your insurance name (e.g., Aetna) and your policy number (i.e., member ID number). Remember to ask about any co-payments!
- Your (& maybe your partner’s) schedule: Know when you’ll be free to make it to your appointment. You might be asked if you prefer an AM/PM time slot. If your partner is going, make sure you know his schedule and when he might be available to go with you.
- Calendar: Have a calendar in front of you. You can check your phone’s calendar, but you’ll have to put the call on speaker. So it might be better to have a physical calendar. This will help you see the day (e.g., Monday) a prospective appointment falls on and make it easier for you to schedule your appointment.
- Pen and paper/notebook: Have this in hand to write down any info you might be given (e.g., date, time, what you’re required to bring to your first appointment, any other specific instructions, etc.). I absolutely LOVE using pocket planners/calendars (like this ) to keep my scheduled appointments and other info all in one place. They usually have a notes section for you to write down any questions you may have .
Seriously, all of this preparation is 100% WORTHWHILE!
Okay, so now that you know how to prep for the call, here is…
“Hi, good [morning, afternoon]. My name is [your name]. I just found out I’m pregnant, so I’m calling to schedule my first prenatal appointment. Are you accepting new patients and do you take [name of your health insurance] insurance?”
Filled out version of the example above:
“Hi good morning. My name is Olivia Williams. I just found out I’m pregnant, so I’m calling to schedule my first prenatal appointment. Are you accepting new patients and do you take Aetna insurance?”
Note: If new patients are being accepted, the receptionist will ask for your name, DOB and health insurance information to register you into their system and set up your appointment.
What to expect at your first prenatal visit
Here is a quick glance at what to expect at your first pregnancy appointment:
- Review of previous and current substance use
Here’s a deeper look at what to expect at your first prenatal appointment:
One of the first things you’ll be asked to do is go to the bathroom to collect a urine sample.
You’ll be given a specimen bag with a specimen cup and a few packs of pre-moistened wipes to clean yourself beforehand.
Make sure to clean front to back and it’s better to collect a midstream catch (i.e., pee a little bit into the toilet then fill the cup with the rest of your urine).
If the outside of the cup gets soaked with pee, don’t panic. Just use some tissue to wipe the OUTSIDE of the cup dry and make sure you secure the top before placing into the specimen bag.
Give it to the nurse, or drop it off at the place you were directed to leave it.
Your urine will be checked for excess protein, sugar and other substances that may indicate an infection or pregnancy complication such as gestational diabetes.
Even though you got a positive home pregnancy test, your pregnancy still has to be confirmed at your first prenatal appointment.
They have to do their own pregnancy test so they can enter it into their system.
The urine sample you provided can be used to confirm your pregnancy, but it can also be confirmed with a blood test and/or ultrasound.
They will ask you for the first day of your last menstrual period. This helps them to give you an estimated due date by calculating 40 weeks from that date.
Don’t worry if you can’t remember the date of your LMP because an ultrasound can be done to predict your baby’s estimated due date (EDD).
Your EDD can also be calculated based on the date of your conception, if you happen to know it.
Your blood pressure will most likely be checked after you give them your urine sample.
It’s normal for your blood pressure to decrease when you’re pregnant due to the increase in blood volume, but sometimes it can be abnormally high.
Monitoring your blood pressure is an important part of prenatal care, so you’ll be checked at each prenatal visit.
Regular blood pressure checks are an easy way to detect and treat pregnancy complications like gestational hypertension (i.e., high blood pressure during pregnancy) early.
Your weight will be checked at every prenatal visit—starting with your first. This initial weigh-in will be used as a baseline for all future weigh-ins.
And based on your BMI, you’ll be expected to gain a certain amount of weight during your pregnancy.
Regular weigh-ins can check for sudden fluctuations in your weight and help your provider to see how your pregnancy is progressing.
You’ll be asked a lot of questions about you and your immediate family’s medical history (e.g., diabetes, high blood pressure, asthma, heart disease, allergies etc.).
You might also be asked about your partner’s medical history, as well as the medical history of your partner’s immediate family.
All of this information will help your provider to determine if you’re at risk for certain pregnancy complications and conditions.
If there are any concerns or an increased risk for genetic conditions, you’ll be given the opportunity to receive genetic counseling and genetic testing.
Any prior surgeries? They’ll want to know this because this info can shape your prenatal care.
For example, letting your provider know you’ve had a prior c-section can help them set up a TOLAC (trial of labor after c-section) if your goal is to have a VBAC (vaginal birth after c-section).
Any prior pregnancies, including miscarriages and abortions? They’ll need to know this too.
They will assess you for GTPAL to get a complete reproductive history:
- Gravida: Number of pregnancies you’ve had
- Term: Number of babies delivered after 37 weeks gestation
- Preterm: Number of babies delivered between 20- 36 weeks gestation
- Abortion/miscarriage: Number of losses before 20 weeks gestation
- Living: Number of living children you have
Your provider will want to know any current or past gynecological issues.
This is to determine if you have any potential or actual risks for birth defects and other pregnancy complications.
What’s your STD history? (e.g., herpes, HIV, chlamydia, gonorrhea, syphilis, genital warts, trichomoniasis and more).
It’s BEST to be honest here, so you and your partner can be treated if necessary!
Plus, untreated STDs during pregnancy can be really dangerous for your developing baby.
Your provider will want to know what medications you take (prescribed and over the counter) to assess whether or not it’s safe for you to take during pregnancy.
For any medications that aren’t safe, an alternative one may be provided. But usually the pros and cons of continuing that specific medication during pregnancy are weighed against each other. Meaning—do the benefits outweigh the risks? And vice-versa.
Your OB/midwife will also need to know if you’re allergic to any medications, so it can be entered into your patient record.
Your provider will want to know if you have any previous or current use of alcohol and/or drugs. This includes cigarettes, marijuana and other illicit drugs.
Being transparent can make it easier to get whatever help you may need.
For example: If you smoke cigarettes, but want to stop now that you’re pregnant, your provider can offer a smoking cessation program and other helpful resources to help you.
You will be asked about your lifestyle habits (e.g., exercise, diet, career, hobbies, etc.).
It’s important to be honest, so your provider can give you the best recommendations based on your situation.
Your provider can also let you know what things are safe vs unsafe for you to continue to do while you’re pregnant.
Tips may also be shared about how you can improve the health of your pregnancy.
You’ll be asked about your social history (e.g., emotional support system) and mental health history (e.g., depression, anxiety, prior mental health counseling, etc.).
These questions are asked to get a better idea of how your provider can best support you during your pregnancy.
Domestic violence tends to start or spike during pregnancy ( source ), so you’ll be asked if you’re experiencing any kind of abuse.
Studies have associated domestic violence (aka intimate partner violence) during pregnancy with:
- Poor maternal nutrition and inadequate weight gain
- A negative impact on a woman’s ability to receive regular prenatal care.
- Prenatal and postpartum depression
- A higher risk of substance use
- Adverse neonatal outcomes like low birth weight and premature birth
- An increased risk of miscarriage, stillborn death and induced abortion
If you’re experiencing abuse during pregnancy, your provider can give you all the resources and help that you need.
This includes connecting you with a domestic violence specialist to help you set up a safety plan .
You will also get the proper advice on how to get out of your abusive situation in the SAFEST way possible.
But, of course, you will NOT be forced or coerced to leave your situation if you don’t feel ready to.
You’ll get a full physical exam after you’re done answering questions and asking questions of your own . This usually involves a breast and pelvic exam.
A pap smear with cultures might also be done, especially if you’re due for one.
All of these exams check for infections, STDs and other abnormalities that may complicate your pregnancy.
Your provider will ask you to lie down and expose your abdomen, so a fetal doppler can be used to listen to your baby’s heartbeat.
Just so know, it’s not always possible to detect a fetal heart beat with a doppler in the very early weeks of pregnancy.
Your blood will be drawn at the end of your appointment to check for things like your blood type, Rh factor, blood count, HIV status and immunities.
Lastly, you’ll be told to make your next prenatal appointment.
This is usually done at the front desk, but your provider may set up your next appointment while you’re still in the exam room.
Here is the typical prenatal care schedule for a normal (i.e., uncomplicated) pregnancy:
- Weeks 4-28: every four weeks
- Weeks 28-36: every two weeks
- Weeks 36-birth: every week
The standard schedule is only a general guideline and might look different for you.
Your prenatal care schedule can increase in frequency if you:
- Have a medical history that requires extra monitoring
- Have a high risk pregnancy
- Experience a complication anytime during your pregnancy
The best way to prepare for your first prenatal visit is by gathering all the information you would need to answer all of their questions.
Before heading to your first prenatal visit, make sure you prepare all of the following information:
- Your insurance cards and ID: If a co-payment is required, make sure to have the money together.
- The first day of your last menstrual period: If you don’t know the first day of your LMP, you can give a rough estimate. Or let them know your conception date if you’ve been tracking your fertility. An ultrasound can be used to calculate an estimated due date.
- Your medical history: This includes your gynecological, reproductive, surgical and mental health history
- The medical history of you and your partner’s immediate family: It would be beneficial to have your partner with you, if possible.
- All of the medications you are currently taking: Including prescription, OTC, vitamins, supplements and herbal supplements (e.g., teas, pills, powders, liquids, patches, topical creams, etc) It’s BEST to put all of your medications into a large ziplock bag to bring with you. It will be easier for your provider to know what’s safe or unsafe for you to take during pregnancy.
- Previous or current substance use: This includes tobacco, cannabis, alcohol, vaping products and other illegal or recreational drugs.
- Social history and lifestyle habits: Your career, hobbies, diet, exercise, emotional support system, housing situation, domestic violence history, etc.
- Any questions you may have: Find out all the essential to ask at your first prenatal visit here .
There are 50+ questions you can ask at your first prenatal appointment , but here are a few to get you started:
- How often will I have my prenatal appointments?
- How much weight in total should I gain during my entire pregnancy? How much weight should I be gaining each week?
- How can I help support my baby’s development?
- What lifestyle changes do I need to make during my pregnancy?
- Is there a nurse line to call if I have questions or concerns?
- When should I go straight to the emergency room? (e.g., heavy bleeding, severe cramping, fainting, etc.)
- Are my prescribed and OTC medications safe for me to use during my pregnancy?
- What changes do I need to make to my diet during my pregnancy?
How to make the most of your prenatal appointments
Did you know that getting regular prenatal care from the start of your pregnancy increases health outcomes for you and your baby ( source )?
Prenatal care is SO IMPORTANT for managing the health of your pregnancy, reducing your risks for complications, early detection and treatment of complications and much more!
- Go to all of your prenatal visits: Don’t skip your appointments even if you have a normal, low-risk pregnancy. If you can’t make it to your appointment, call to reschedule but try your best to make it to each appointment.
- Prepare to give a urine sample at each appointment: I would drink water before each of my prenatal visits to make sure I had urine to collect.
- Prepare to have your blood pressure taken at each visit: You might be having your BP taken outside of the exam room, so wear something that will make it easy for you to expose your arm to get a proper BP measurement.
- Wear clothes that allow easy access to your belly: Fetal dopplers, fundal height measurements and checking for baby’s position all require easy access to your belly. I’d skip the maxi dresses, rompers, jumpers and go for T-shirts instead.
- Keep important info within easy reach: This includes your provider’s name and number, other emergency contact info, signs and symptoms to report ASAP and other helpful reminders on your fridge, mirror or anywhere else you think would be good for you
- Prepare your questions beforehand: Write down all of your questions, as they come up, in a notes app on your phone or in a notebook you won’t forget to put in your purse. That way you don’t leave your appointment to then realize you forgot to ask the question(s) you wanted to ask.
- Have your partner or support person go with you, if possible: Especially during the first prenatal visit when questions are being asked about past medical history and family medical history. If they can’t make it, ask if you are able to do a video call. Another tip: if your partner has to take off of work to make it to your prenatal visit, ask the receptionist for a letter for your partner to have proof for their employer. Also, the BIG VISITS to attend are the first prenatal visit, 12 week visit, 20 week anatomy scan (where you can find out the gender!) and one or two late pregnancy appointments nearing your due date.
- Have your insurance cards and ID ready to present to the receptionist when checking in to your appointment. And know beforehand if you have any co-pays to make because if you do, you’ll be expected to pay the day of your visit.
There you have it, mama! Now you know what to expect at your first prenatal visit, how to prepare, what questions to ask and how to make the most of your prenatal appointments. And then some!
I hope you found this post to be really helpful to you and, if so, I hope you share this post with all of your friends!
Seriously—knowing just what to expect, how to prepare and even what questions to ask at your first prenatal visit can really help to get rid of some of those jitters.
Your turn! When is your first prenatal visit and what have you been doing to prepare for it? What tips or info did you find the most surprising or helpful in this post? Let me know in the comments!
Enjoy your first prenatal visit, mama!

Pin to share!

- Alhusen, J. L., Ray, E., Sharps, P., & Bullock, L. (2015). Intimate partner violence during pregnancy: maternal and neonatal outcomes . Journal of women’s health (2002), 24(1), 100–106. https://doi.org/10.1089/jwh.2014.4872
- https://americanpregnancy.org/resources/pregnancy-calculator/
- https://www.thehotline.org/plan-for-safety/create-a-safety-plan/
- https://www.marchofdimes.org/find-support/topics/pregnancy/abuse-during-pregnancy
Related Posts

Hey! Love my content? Feel free to buy me a cup of coffee. And for a special thank you, I got you 20% off your first purchase of Purity Coffee (an organic, specialty-grade, antioxidant-rich coffee) with my code MOMFORTHELITTLES!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Amazon Affiliate
Mom For The Littles is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.com. As an Amazon Associate, I earn from qualifying purchases
- Affiliate Disclosure
- Privacy Policy
- Cookie Policy
- Disclaimer & Disclosure
- Terms & Conditions
- Accessibility Statement
Medical Disclaimer
This site is for informational and educational purposes only and is not intended to be a substitute for medical advice, diagnosis or treatment. Always seek the advice of your healthcare provider regarding any medical conditions and before trying anything recommended on this site.
Copyright © 2024 MOM FOR THE LITTLES · Theme by 17th Avenue
Privacy Overview
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
CALCULATORS
Related topics.
INTRODUCTION
This topic will discuss the initial prenatal assessment (which may require more than one visit) in the United States. Most of these issues are common to pregnancies worldwide. Preconception care, ongoing prenatal care after the initial prenatal assessment, and issues related to patient counseling are reviewed separately.
● (See "The preconception office visit" .)
● (See "Prenatal care: Second and third trimesters" .)
● (See "Prenatal care: Patient education, health promotion, and safety of commonly used drugs" .)
Your Guide to Prenatal Appointments
Medical review policy, latest update:.
Minor copy changes.
Typical prenatal appointment schedule
Read this next, what happens during a prenatal care appointment, what tests will i receive at my prenatal appointments, what will i talk about with my practitioner at prenatal care appointments , first trimester prenatal appointments: what to expect, second trimester prenatal appointments: what to expect, third trimester prenatal appointments: what to expect, questions to ask during prenatal appointments .
Prenatal care visits are chock-full of tests, measurements, questions and concerns, but know that throughout the process your and your baby’s wellbeing are the main focus. Keep your schedule organized so you don’t miss any appointments and jot down anything you want to discuss with your doctor and your prenatal experience should end up being both positive and rewarding.
What to Expect When You’re Expecting , 5th edition, Heidi Murkoff. American College of Obstetricians and Gynecologists, Having a Baby After Age 35: How Aging Affects Fertility and Pregnancy , 2020. American College of Obstetricians and Gynecologists, Routine Tests During Pregnancy , 2020. US Department of Health & Human Services, Office on Women’s Health, Prenatal Care and Tests , January 2019. Journal of Perinatology , Number of Prenatal Visits and Pregnancy Outcomes in Low-risk wWomen , June 2016. Mayo Clinic, Edema , October 2017. Mayo Clinic, Prenatal Care: 2nd Trimester Visits , August 2020. Mayo Clinic, Prenatal Care: 3rd Trimester Visits , August 2020. Jennifer Leighdon Wu, M.D., Women’s Health of Manhattan, New York, NY. WhatToExpect.com, Preeclampsia: Symptoms, Risk Factors and Treatment , April 2019. WhatToExpect.com, Prenatal Testing During Pregnancy , March 2019. WhatToExpect.com, Urine Tests During Pregnancy , May 2019. WhatToExpect.com, Fetal Heartbeat: The Development of Baby’s Circulatory System , April 2019. WhatToExpect.com, Amniocentesis , Mary 2019. WhatToExpect.com, Ultrasound During Pregnancy , April 2019. WhatToExpect.com, Rh Factor Testing , June 2019. WhatToExpect.com, Glucose Screening and Glucose Tolerance Test , April 2019. WhatToExpect.com, Nuchal Translucency Screening , April 2019. WhatToExpect.com, Group B Strep Testing During Pregnancy , August 2019. WhatToExpect.com, The Nonstress Test During Pregnancy , April 2019. WhatToExpect.com, Biophysical Profile (BPP) , May 2019. WhatToExpect.com, Noninvasive Prenatal Testing , (NIPT), April 2019. WhatToExpect.com, The Quad Screen , February 2019. WhatToExpect.com, Chorionic Villus Sampling (CVS) , February 2019. WhatToExpect.com, The First Prenatal Appointment , June 2019. WhatToExpect.com, Breech Birth: What it Means for You , September 2018.
Updates history
Jump to your week of pregnancy, trending on what to expect, signs of labor, pregnancy calculator, ⚠️ you can't see this cool content because you have ad block enabled., top 1,000 baby girl names in the u.s., top 1,000 baby boy names in the u.s., braxton hicks contractions and false labor.
What Happens at the First Prenatal Visit
Once you get a positive home pregnancy test, you should set up your first prenatal visit with a doctor or midwife .
Establishing care early on and attending regular prenatal visits helps keep you and your baby healthy.
Here’s what to plan for and what to expect at your first prenatal visit.
When to Schedule Your First Prenatal Visit
The first prenatal visit is typically scheduled for when you’re 7–10 weeks pregnant. This is counted from the first day of your last period.
This timing is important, as “it confirms a viable pregnancy and ideally gives the most accurate due date,” says Katy Orr , a certified registered nurse practitioner at the University of Alabama at Birmingham’s Department of Obstetrics and Gynecology.
If you’re further along in your pregnancy by the time you make that first appointment, don’t worry. Your doctor or midwife will get you in for a visit as soon as possible, says Jessica Salak, M.D. , board-certified ob-gyn at Tufts Medical Center in Boston.
It’s best to call as soon as you know you’re pregnant, since appointments can book up quickly. At your visit, the provider will check to make sure you’re healthy and your baby is developing as expected.
What Will Happen at Your First Prenatal Appointment
“The first visit is the longest visit of the entire pregnancy,” says Salak.
That’s because your doctor or midwife will complete the following assessments and tests:
- Measure your vital signs (height, weight, body temperature, and blood pressure)
- Collect a urine sample (the urine will be tested for kidney function/protein and look for any signs of infection)
- Do an ultrasound to confirm the pregnancy and provide an accurate due date
- Do a pap smear and breast exam (if you’re due for them)
- Draw blood to check your blood type and screen for potential concerns
- Offer genetic screening tests to screen for conditions such as Down syndrome
They’ll gather a lot of information from you too, says Salak. They will:
- Review your medical history, including any medications you take
- Discuss family health history (for both you and the baby’s other parent)
- Ask about tobacco, alcohol, and drug use , and recommend resources for quitting (if needed)
- Talk about your job to see if there are work-related risks to the pregnancy
- Ask about your relationships to be sure they’re healthy and safe
They may also offer some education around what to expect at each prenatal visit and throughout the pregnancy, says Salak. To do this, they will likely:
- Review healthy habits to follow during pregnancy
- Offer strategies to help pregnancy symptoms such as morning sickness
- Go over the schedule of prenatal visits
- Give you an opportunity to ask questions
What to Bring to Your First Prenatal Doctor’s Visit
Gather the right information and details before your first prenatal visit. Having these items can help make it go as smoothly as possible:
- Important health documents. Bring a valid ID and your health insurance card to your appointment. “And be prepared to discuss billing options,” says Orr.
- Date your last period began. This helps your provider assess how far along your pregnancy is, says Orr.
- Previous pregnancy history. Bring along any records you may have from past pregnancies, including delivery information. Also be sure to discuss any history of abortion, miscarriage, or fertility problems, says Orr.
- Personal medical history. Be sure to discuss any health conditions or issues you’re managing, such as high blood pressure. Tell the provider about any medications you’re currently taking and their exact dosages, Orr says. This is also a good time to mention any allergies you may have, adds Salak.
- Extended family medical history. “Talk to your family about any genetic disorders that may run in the family,” adds Salak. “Be prepared with your partner’s [or other parent’s] family history as well, because not everyone knows the details of that side’s family history.”
- Overall honesty. It's important to be honest when your provider asks you questions about habits like smoking, alcohol, or drug use, or if you’ve experienced any domestic violence, notes Salak. They can help you get the support you need to keep you and your growing baby safe.
Questions to Ask at Your First Prenatal Appointment
Take time before the appointment to gather your thoughts and concerns.
“Be ready with a list of questions written or typed in your phone so you don’t forget what you want to ask during the visit,” advises Orr.
Common questions to ask at the first prenatal visit include:
- How often do I need to come in for pregnancy-related visits?
- How many ultrasounds will I get during pregnancy?
- What types of prenatal screenings or tests do I need?
- Should I be making any changes to my diet?
- What prenatal vitamin do you recommend?
- Which exercises are safe for me during pregnancy?
- How much weight should I gain throughout the pregnancy?
- Where will I deliver the baby?
- What’s the best way to reach you with any questions or concerns?
And remember: No question you have is too silly, simple, or off the table. “We get all types of questions,” says Orr.

FAQ: If You Have a Partner, Should They Come to the First Prenatal Visit?
If you have a partner, they should be as involved in your prenatal care as possible. Attending the first prenatal visit is an important place to start. Consider involving the other parent even if you aren’t in a relationship.
“The first visit is usually more complex than most, with discussion about details of the pregnancy, the hospital or healthcare team, scheduling, billing, and expectations. This is also when the first ultrasound is usually done,” says Orr. “It helps to have both parents here for this, not just for support but also to help remember details, ask questions, take notes, and bring up concerns.”
You May Also Like:
- 6 Tips for Easier Prenatal Visits
- Your Guide to First-Trimester Tests and Screenings
- 8 Things to Consider When Choosing a Doctor for Your Pregnancy
Want to Read More?
Access all of Twill Care’s content, community, and experts for free!
Already a member? Login

15 Questions to Ask at First Prenatal Visit
Are you nervous and confused for questions to ask at first Prenatal visit?
The initial visit with your healthcare provider during pregnancy typically occurs between 8-10 weeks after conception and last about 30 minutes to 1 hour. This appointment is of utmost importance, as it often comprises a thorough physical examination and routine prenatal laboratory tests. If you missed out on your first prenatal check-up before hitting the 10-week mark, no worries! It’s never too late to book an appointment with your healthcare provider to make sure you’re all set for the remainder of your pregnancy.
Subsequent prenatal visits, in uncomplicated pregnancies, typically span around 15 minutes. While attending these appointments, ensure that your provider addresses all your queries. Even though a short appointment might seem alarming, it usually indicates that your pregnancy is progressing smoothly.
In the case of uncomplicated pregnancies, expectant mothers are advised to visit their healthcare provider every four weeks up until 28 weeks, every two weeks between 28 and 36 weeks, and weekly from 36 weeks until delivery. Each prenatal visit will encompass a weight check, blood pressure check, and an opportunity to listen to your baby’s heartbeat.
The initial prenatal visit is a crucial appointment that sets the foundation for your entire pregnancy. During this visit, your doctor will gather your medical history and assist you in devising a plan for your prenatal care. This is an excellent opportunity for you to ask any queries you may have.
In this article, we will guide you through some of the most important questions to ask at first prenatal visit to ensure that you derive maximum benefits.
Related: Schedule For Pregnancy Checkup For Healthy 9 Months
Table of Contents
Gather Important Medical Information Before You go
Prior to your appointment, it is essential to gather and educate yourself about your medical history. This encompasses more than just routine check-up information, so ensure that you have knowledge and documentation, when possible, of the following critical details.
It is important to note that your partner’s medical history can also affect the health of your baby. Therefore, if feasible, your partner should accompany you to the appointment. If you or your partner were adopted or used a donor egg or sperm, you may have limited genetic information. However, your doctor can assist you in interpreting the available information.
Here are the crucial pieces of information to include:
General Medical History
This includes any medical issues you have had or are currently experiencing. It is crucial to list the types, dates, and treatments, if applicable. If you suffer from health problems such as diabetes, cancer, kidney disease, epilepsy, or high blood pressure, your pregnancy may be classified as high-risk.
Family Medical History
If certain genetic disorders run in your family or your partner’s family, your baby may be at a higher risk of inheriting them. It is important to inquire with family members about genetic disorders and birth defect history. Depending on your family’s medical history, your ethnic background, and other factors, your provider may recommend different screenings or tests. For instance, people of Ashkenazi Jewish heritage have an increased risk of cystic fibrosis and Tay-Sachs Disease, while individuals of African descent have an increased risk of sickle cell disease.
Fertility History
Your menstrual history, including regular/irregular periods, history of cramping or PMS, and any medication you use to bring on a period, should be listed. Describe any fertility treatments you have undergone and their outcomes. Include your Pap smear history, any abnormalities detected, and treatments if applicable (i.e., colposcopy , cryosurgery , laser treatment , conization , LEEP procedure ).
Past Pregnancies
It is essential to include information about previous pregnancies, including live births, stillbirths, premature deliveries (less than 37 weeks), miscarriages (less than 20 weeks), ectopic/tubal pregnancies, and/or elective terminations (abortions).
Infection Exposure
List any sexually transmitted infections (STIs) you have had, such as chlamydia, gonorrhea, herpes, genital warts/HPV, syphilis, HIV/AIDS, and hepatitis.
Medications You’re Taking
Compile a list of all prescription and over-the-counter medications you are currently taking. Additionally, list any herbal medicines, vitamins, or health supplements you take. Be sure to note any medication allergies.
Dietary Habits
Your doctor will inquire about your caffeine, alcohol, and nicotine consumption. It is safe to consume a moderate amount of coffee during pregnancy, but no amount of nicotine, alcohol, or illicit drugs are considered safe. If you require assistance staying sober, reach out to your provider, and they will work with you to ensure a safe and healthy pregnancy.
Mental Health History
If you have a history of anxiety, depression, or other mental health conditions, let your doctor know. Your doctor will assist you in developing a treatment plan that considers both you and your baby’s well-being. In some cases, your doctor may recommend discontinuing a certain medication. However, in other cases, the risks of stopping a medication outweigh the potential benefits. Talk to your doctor to determine the most suitable plan for you.
Related: The Ultimate Guide: How to Tell Your Boss You’re Pregnant (Scripts Included)
Understanding What to Expect During Your Initial Prenatal Visit
The initial prenatal appointment is an essential aspect of pregnancy, and it’s important to know what to expect during the visit. Typically, your first prenatal check-up is the lengthiest one, but this may vary if you experience any pregnancy complications.
Standard Procedures
During this appointment, your healthcare provider will assess your medical history, record your weight and blood pressure, and conduct a blood test. The blood test will examine your blood type, Rh factor, exposure to hepatitis and syphilis, and immunity to German measles.
Additional Procedures
Your healthcare provider might want to run some extra tests if they feel it’s necessary, but don’t stress, it’s not always the case. During your first prenatal check-up, they may suggest additional testing, which could include genetic carrier screening, blood sugar test, non-invasive prenatal genetic screening.
Fetal Heartbeat
You may have the opportunity to listen to your baby’s heartbeat during the appointment. However, if your prenatal visit is scheduled earlier in your pregnancy, you may have to wait to hear your baby’s heartbeat. Generally, the fetal heartbeat becomes detectable between the 12th and 14th weeks.
HIV Screening
It is advisable to have an HIV test during the initial stages of your pregnancy. Anyone who is sexually active is potentially at risk of contracting HIV. Many individuals who test positive for HIV do not necessarily belong to a particular high-risk group, such as drug users.
HIV during pregnancy can have significant consequences for both the mother and the baby. We can offer medications during pregnancy to help prevent the transmission of the virus to the baby, but this can only happen if we know your HIV status. Fortunately, most women receive a normal or negative result, which provides them with relief. If you test positive for HIV, we can assist you in receiving specialized care for yourself and your baby.
Prenatal Care Plan
Lastly, your healthcare provider will discuss recommendations for your prenatal care, including diet, exercise, sexual activity, travel, and work. You will review your appointment schedule throughout your pregnancy and also plan for your overall health. You may need to visit your doctor more frequently than usual during your pregnancy, but it’s crucial not to neglect other regular procedures, such as your dental check-up.
Related: Say Goodbye to Pregnancy Headaches
Questions Your Doctor May Ask You
Your doctor will ask several questions to assess your pregnancy’s status and to determine the appropriate prenatal care for you. These questions include:
- What was the start date of your last menstrual period to determine your gestational age?
- Did you experience any symptoms during early pregnancy?
- Are you currently taking any medications?
- What birth control methods have you used in the past?
- Have you experienced any miscarriages or preterm births?
- Are you allergic to any medications or substances?
- Do you have any diseases or conditions?
- What is your physical and mental medical history?
- Do you or your partner’s family have a history of genetic disorders or pregnancy complications?
- Did you take prenatal supplements while trying to conceive, or are you taking them now?
- Have you been exposed to any environmental or work-related hazards?
- What is your usual diet and nutritional habits?
By answering these questions accurately, your healthcare team can provide you with the best possible prenatal care.
Your doctor may also request historical documents to help them assess your pregnancy’s status and risks. These documents include:
- Medical records
- Previous Pap smear results
- Previous blood test results
- Ultrasounds
- Previous delivery records
Related: Making Love, Not War: 10 Comfortable Pregnancy Sex Positions
List of 15 Questions to Ask at First Prenatal Visit
As a pregnant woman, you may have various concerns about your health and the well-being of your baby. It’s essential to be prepared with a list of questions to ask your doctor during your initial prenatal visit. The following are the top 15 questions to ask at first prenatal visit:
What is Your Expected Due Date?
While you may feel confident about your anticipated due date , having tracked your menstrual cycles, ovulation, and timed intercourse (or perhaps you have no idea), it is prudent to confirm this information with your obstetrician-gynecologist. It’s possible that your due date may shift based on when ovulation and implantation occurred.
What Pregnancy Symptoms Can You Expect Each Trimester?
As you progress through each trimester of your pregnancy, your body will undergo significant changes, which can manifest in various symptoms. It’s essential to understand what to expect during each phase, and your obstetrician/gynecologist (OBGYN) can provide valuable insights to help you navigate these changes.
What Dietary Changes Should I Make During Pregnancy?
Your doctor can provide you with specific dietary recommendations that are suitable for your pregnancy. Consuming a variety of healthy foods, including lean meats, whole grains, fruits, vegetables, and unsaturated fats, is crucial. Prenatal vitamins can also be beneficial, so be sure to ask your doctor about them.
What Foods Should I Avoid During Pregnancy?
Certain foods, such as raw or undercooked seafood and unwashed fruits or vegetables, should be avoided to prevent congenital toxoplasmosis. Your doctor can also guide you on other foods that may pose a risk to your baby.
What Amount of Caffeine is Safe to Consume?
The answer varies from person to person, and it depends on a lot of factors. But one thing is for sure, when you’re pregnant, you’re not just drinking for two, you’re also caffeinating for two. So it’s best to consult with your doctor to ensure you’re not overdoing it with the caffeine. Remember, a little buzz is fine, but you don’t want to brew up any regrets later on.
How Much Weight Should I Expect to Gain During Pregnancy?
Your pre-pregnancy BMI will determine your healthy weight gain range, and your doctor can help you set achievable weight gain goals.
How Much Exercise Should I be Doing?
Regular exercise can have numerous benefits during pregnancy, such as reducing back pain, preventing excessive weight gain, and lowering the risk of gestational diabetes and high blood pressure. However, it’s crucial to avoid activities that could cause a fall or abdominal trauma, exercise at high altitudes, and scuba diving. Consult with your doctor about specific exercises that are safe for you.
Can I Travel While Pregnant?
Many women drive and fly during pregnancy , and most airlines permit travel until 37 weeks gestation. Your doctor can advise you on safety measures to take when traveling.
Can I Continue Working During Pregnancy?
Women can typically continue working throughout their pregnancy with some adjustments to their work style. Speak to your doctor about strategies to remain comfortable at work and any special accommodations you may require.
Can I Keep Taking My Current Medications?
While few medications have been approved for use during pregnancy, some medications have not been linked to adverse pregnancy outcomes or birth defects. However, it’s essential to weigh the severity of your symptoms against the possible risks to your baby before taking any medication during pregnancy. Consult with your doctor for more information about specific medications.
When is My Next Appointment?
For an uncomplicated pregnancy, most women should see their healthcare provider every four weeks up to 28 weeks, every two weeks between 28 and 36 weeks, and weekly from 36 weeks until delivery. If you have a high-risk pregnancy, your doctor may wish to see you more frequently. Discuss your prenatal care plan with your doctor during your first appointment.
Do You Recommend any Prenatal Screening or Testing?
Depending on your family medical history and ethnic background, your doctor may recommend prenatal screening or testing. The decision to pursue these tests is personal, and your doctor can help you make an informed decision.
Do You Recommend any Prenatal Classes?
Taking a prenatal class can help prepare you for delivery. With various options available, it’s crucial to choose a class that suits your needs. Speak to your doctor about finding the right class for you.
How Often You’ll need to Attend Your Prenatal Appointments?
For uncomplicated pregnancies, you can expect to attend appointments every four weeks for the first 28 weeks. After that, the frequency of appointments increases to every two weeks until you reach 36 weeks, at which point you’ll attend weekly appointments until delivery. To ensure you don’t miss any important appointments, it’s advisable to schedule them in advance, as OB/GYN schedules can fill up quickly.
Who will be Delivering Your Baby?
This can vary depending on the clinic you choose, so it’s important to have a discussion with your healthcare provider. Previously, many OB/GYNs worked in solo or dual practices, which meant that your own physician would almost certainly be the one to deliver your baby. However, due to the grueling nature of the job, many practices now have multiple OB/GYNs who rotate in a call pool for delivery.
While you will primarily be managed by the OB/GYN you choose, you may also see other doctors in their group, giving you the opportunity to get to know several of them in case one of them ends up delivering your baby. If knowing who will be delivering your baby is of utmost importance to you, it may affect your decision on which OB/GYN to ultimately choose.
Related: Cervical Changes: Early Pregnancy vs. Pre-period
It’s crucial to remember that each pregnancy is unique, and your doctor is there to guide and support you throughout your journey. Now, you are having a list of 15 questions to ask at first prenatal visit and maintaining open and honest communication with your healthcare provider and greatly contribute to ensuring a healthy pregnancy and a healthy baby.
Related: Is Morning Sickness a Good Sign of Pregnancy?
Frequently Asked Questions
When should i schedule my first prenatal visit.
Most healthcare providers recommend scheduling your first prenatal visit between 8 and 10 weeks of pregnancy.
What Should I Bring to My First Prenatal Visit?
Bring your medical history, any medications you’re currently taking, and a list of questions to ask at first prenatal visit for your healthcare provider.
Can I Bring My Partner or Support Person to My First Prenatal Visit?
Absolutely. Many healthcare providers encourage partners or support persons to attend prenatal visits to offer emotional support and ask questions.
What if I Don’t Have a Healthcare Provider Yet?
If you don’t have a healthcare provider yet, you can start by contacting your insurance provider or local hospital to get a referral or list of providers in your area.
Related posts:
- Should I Avoid Caffeine In Pregnancy?
- Symptoms and Management of HPV During Pregnancy
- Symptoms and Treatment of Partial Molar Pregnancy
- Thoughtful Advice To Help You Through Your Pregnancy
Hi, I'm Sushil Singh, a devoted dad and guiding voice in the transformative journey of parenting, based in Mumbai. Drawing from a decade of firsthand experience and extensive research, I offer authentic insights into prepartum, pregnancy, and postpartum stages at Pregnancy Boss. From joyous milestones to challenging uncertainties, my mission is to provide reliable support and practical advice, helping you navigate this profound journey with confidence. Let's embrace the beauty and complexities of parenthood together. Connect for guidance or shared stories. Cheers to our shared path! 🥂 Social Medial Profiles: Quora Pinterest Twitter Facebook
Leave a Comment Cancel reply
You must be logged in to post a comment.
Shop for Plans
Shop for your own coverage, plans through your employer.
Learn about the medical, dental, pharmacy, behavioral, and voluntary benefits your employer may offer.
Looking for Medicare coverage?
Pregnancy: first prenatal visit.
Your first prenatal visit will probably be the longest visit you'll have. Your doctor or midwife will take your medical history and do a complete physical exam. You may also have some tests. This will provide information that can be used to check for any problems as your pregnancy progresses.
Medical history
Your doctor or midwife will ask about your medical history. This helps your care provider plan the best possible care for your pregnancy and childbirth. Things you'll be asked about include:
- Your menstrual history. This will include your age when you had your first period, whether your cycles are regular, and the date of your last period. Information about your last period is used to estimate your due date .
- Any previous pregnancies, abortions, miscarriages, or stillbirths.
- Problems with previous pregnancies.
- Any problems with your reproductive organs .
- Health problems in your family, such as heart disease or genetic conditions .
- Your general health. This includes vaccinations, surgeries, and serious illnesses you have had. It also includes any current or past mental health issues, such as depression.
- Any medicines you take regularly. This includes prescription and over-the-counter medicines, vitamins, and supplements.
- Any habits that could affect your pregnancy, such as tobacco, alcohol, or drug use.
Physical exam
A complete physical exam may include:
- Checking your weight and blood pressure.
- A pelvic exam .
- A Pap test (if you haven't had one recently).
- A breast exam.
This may be used to confirm your pregnancy and to:
- Estimate the due date.
- Make sure the pregnancy is located in your uterus.
- Check the number of embryos in your uterus.
A urine test may be done to check for:
- Sugar in your urine. This is a sign of gestational diabetes.
- Protein in your urine. This may be a sign of kidney disease.
- Bacteria in your urine. This is a sign of a urinary tract infection (UTI). UTIs are common during pregnancy, and they may not cause symptoms. If not treated, a UTI may lead to a kidney infection.
Blood tests
You may have blood tests to check for:
- Blood type . If your blood is Rh-negative and the father's blood is Rh-positive, the fetus may have Rh-positive blood. That can lead to problems with Rh sensitization.
- Iron deficiency anemia.
- Immunity to German measles (rubella).
- HIV infection.
- Hepatitis B infection. If you are infected, your baby will be treated within 12 hours of birth. You may also be tested for hepatitis C infection.
- Gestational diabetes.
Other tests
You may have other tests to look for some conditions, such as:
- Genetic conditions that can be passed down through families. These include cystic fibrosis, sickle cell disease, and Tay-Sachs disease.
- Sexually transmitted infections (STIs) such as gonorrhea and chlamydia. STIs during pregnancy have been linked to serious problems, including miscarriage and premature birth.
- Thyroid disease. You may have thyroid tests if you have a personal or family history of thyroid problems.
- Diabetes. You may have an early blood sugar test (glucose tolerance test) if you have risk factors for having gestational diabetes.
Current as of: July 10, 2023
Author: Healthwise Staff
Clinical Review Board All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use . Learn how we develop our content .
To learn more about Healthwise, visit Healthwise.org .
© 1995-2024 Healthwise, Incorporated. Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Healthwise, Incorporated.
Related Links
Page footer, i want to..., secure member sites, the cigna group information.
Cigna. All rights reserved.
Individual and family medical and dental insurance plans are insured by Cigna Health and Life Insurance Company (CHLIC), Cigna HealthCare of Arizona, Inc., Cigna HealthCare of Illinois, Inc., Cigna HealthCare of Georgia, Inc., Cigna HealthCare of North Carolina, Inc., Cigna HealthCare of South Carolina, Inc., and Cigna HealthCare of Texas, Inc. Group health insurance and health benefit plans are insured or administered by CHLIC, Connecticut General Life Insurance Company (CGLIC), or their affiliates (see a listing of the legal entities that insure or administer group HMO, dental HMO, and other products or services in your state). Accidental Injury, Critical Illness, and Hospital Care plans or insurance policies are distributed exclusively by or through operating subsidiaries of Cigna Corporation, are administered by Cigna Health and Life Insurance Company, and are insured by either (i) Cigna Health and Life Insurance Company (Bloomfield, CT); (ii) Life Insurance Company of North America (“LINA”) (Philadelphia, PA); or (iii) New York Life Group Insurance Company of NY (“NYLGICNY”) (New York, NY), formerly known as Cigna Life Insurance Company of New York. The Cigna name, logo, and other Cigna marks are owned by Cigna Intellectual Property, Inc. LINA and NYLGICNY are not affiliates of Cigna.
All insurance policies and group benefit plans contain exclusions and limitations. For availability, costs and complete details of coverage, contact a licensed agent or Cigna sales representative. This website is not intended for residents of New Mexico.
Selecting these links will take you away from Cigna.com to another website, which may be a non-Cigna website. Cigna may not control the content or links of non-Cigna websites. Details
Amid syphilis surge, doctors call for more testing during pregnancy

The nation’s largest coalition of obstetricians issued an urgent warning Thursday calling on doctors to expand testing for syphilis during pregnancy amid a surge of cases in recent years.
The American College of Obstetricians and Gynecologists updated its recommendations, advising a routine blood screening at the first prenatal visit and screenings in the third trimester of pregnancy and at birth. This contrasts with previous recommendations, which called for testing in the third trimester exclusively for individuals living in communities with high syphilis rates and for those at risk of syphilis exposure during pregnancy.
“We’re always trying to create healthier families, and some of the diseases that we can easily diagnose and treat are things that we should prioritize, especially when they can be devastating to a baby,” said Laura E. Riley, chair of the obstetrician coalition’s immunization work group. Riley helped write the guidance.
“Sometimes, it’s difficult to know that you’ve been exposed to syphilis, and it’s not like you can raise your hand and say, ‘I have this, please give me treatment,’ because you may not even know you have it,” said Riley, chair of obstetrics and gynecology at Weill Cornell Medicine in New York.
Rates of syphilis have been skyrocketing, with cases hitting their highest level since the 1950s. Reported syphilis cases increased 80 percent from 2018 to 2022 in the United States, soaring from about 115,000 cases to more than 207,000, according to the Centers for Disease Control and Prevention .
In 2022, more than 3,700 babies were born with syphilis, with 231 stillbirths and 51 infant deaths attributed to transmission of syphilis from pregnant people to their babies.
Experts say these rising numbers reflect decreased condom use and an uptick in substance use, The Washington Post reported.
Syphilis is a sexually transmitted infection caused by the bacterium Treponema pallidum. When a pregnant person is infected with syphilis, the infection can pose severe consequences for the pregnant individual and the unborn baby. Left untreated, syphilis can progress to advanced stages and damage organs and nerves.
It can also be transmitted to the fetus during pregnancy or at childbirth, resulting in congenital syphilis, which can lead to severe health problems for the baby, including premature birth, low birth weight, stillbirth, developmental delays and other complications.
Nicole Smith, medical director of maternal-fetal medicine at Brigham and Women’s Hospital in Boston, said that by calling for routine syphilis testing, the guidelines should prove to be a useful tool for physicians, especially when stigma surrounding sexually transmitted infections persists.
“Some populations are less likely to be either screened or treated … due to the locations where they’re receiving care or because there’s a concern among that population that they’re being stigmatized because they’re being tested,” Smith said.
“So if we say, ‘No, this is nothing about you in particular, this is something that we’re doing for every single pregnant person in this country … we’re treating everyone the same way,’ and therefore some of the barriers to appropriate treatment should be diminished or ideally removed,” she said.
A single injection of a long-acting dose of penicillin can cure early-stage syphilis.
If a person has late-latent syphilis or does not know how long they had the infection, the CDC suggests three doses of long-acting benzathine penicillin G, given weekly. While the treatment can eliminate the infection and stop more harm, it can’t undo damage that has already occurred.
Hurdles exist for syphilis patients, including getting access to testing and medication. Drug shortages — a long-standing issue for many medications — have contributed to rising syphilis cases, experts say.
In April 2023, the Food and Drug Administration announced a shortage of penicillin in the United States attributed to increased demand.
To combat the ongoing shortages, the FDA granted temporary approval for a French drug, Extencilline, which is used for syphilis treatment but is not FDA-approved. While the Food, Drug, and Cosmetic Act prohibits importing unapproved drugs into the United States, the secretary of Health and Human Services can authorize temporary importation and distribution of such drugs to address shortages until domestic production returns to normal levels.
Riley said the updated guidance from the obstetricians group is essential because it makes physicians aware of the alternative treatment for syphilis amid the shortage.
In June 2023, the maker of penicillin, Pfizer, said it would prioritize making the drug available, with the shortage expected to be relieved within the next few months of this year.

- Study Protocol
- Open access
- Published: 22 April 2024
Implementation and early effects of medicaid policy interventions to promote racial equity in pregnancy and early childhood outcomes in Pennsylvania: protocol for a mixed methods study
- Marian Jarlenski 1 ,
- Evan Cole 1 ,
- Christine McClure 1 ,
- Sarah Sanders 2 ,
- Marquita Smalls 2 &
- Dara D Méndez 2
BMC Health Services Research volume 24 , Article number: 498 ( 2024 ) Cite this article
115 Accesses
Metrics details
There are large racial inequities in pregnancy and early childhood health within state Medicaid programs in the United States. To date, few Medicaid policy interventions have explicitly focused on improving health in Black populations. Pennsylvania Medicaid has adopted two policy interventions to incentivize racial health equity in managed care (equity payment program) and obstetric service delivery (equity focused obstetric bundle). Our research team will conduct a mixed-methods study to investigate the implementation and early effects of these two policy interventions on pregnancy and infant health equity.
Qualitative interviews will be conducted with Medicaid managed care administrators and obstetric and pediatric providers, and focus groups will be conducted among Medicaid beneficiaries. Quantitative data on healthcare utilization, healthcare quality, and health outcomes among pregnant and parenting people will be extracted from administrative Medicaid healthcare data. Primary outcomes are stakeholder perspectives on policy intervention implementation (qualitative) and timely prenatal care, pregnancy and birth outcomes, and well-child visits (quantitative). Template analysis methods will be applied to qualitative data. Quantitative analyses will use an interrupted time series design to examine changes over time in outcomes among Black people, relative to people of other races, before and after adoption of the Pennsylvania Medicaid equity-focused policy interventions.
Findings from this study are expected to advance knowledge about how Medicaid programs can best implement policy interventions to promote racial equity in pregnancy and early childhood health.
Peer Review reports
Rates of maternal and infant morbidity and mortality in the United States far exceed those of comparable nations [ 1 ]. The burdens of racist policies have produced vastly worse outcomes for Black and Native, relative to White, populations [ 2 ]. For example, Black and Native birthing people are more than three times as likely to experience pregnancy-related mortality compared to white birthing people [ 3 ]. For every pregnancy-related death, there are thousands of birthing people who experience severe morbidity; including stark racial disparities where Black populations are more likely to experience stroke or serious cardiovascular events sending them on a trajectory of adverse health outcomes beyond pregnancy [ 4 , 5 ]. We also see similar racial inequities for infant mortality and morbidity. These racial inequities are not adequately explained by individual behaviors or other socio-economic factors, but are a complex intersection of factors shaped by structural and social determinants [ 2 , 6 ], policies and institutions carrying out such policies [ 7 ]. There is a long history of structural racism that has resulted in practices and policies that have had a detrimental impact on Black and Indigenous populations in the United States [ 8 ].
State Medicaid programs are the largest single payer for pregnancy and birth in the US, covering 68% of births to Black people [ 9 ]. As such, Medicaid programs have great potential to implement structural interventions to advance racial equity in healthcare and health outcomes during pregnancy and postpartum [ 10 ]. Historically, Medicaid policies have promoted equality, that is, providing equal benefits to all regardless of the distribution of need [ 11 ]. An equity-focused policy approach, however, will direct resources toward improving health and well-being among those with the greatest need [ 12 ]. Unfortunately, a vast body of research conducted among Medicaid-enrolled populations shows that healthcare systems do not provide the same quality of obstetric care to Black people and other people of color, relative to white people [ 13 , 14 , 15 , 16 , 17 , 18 ].
Pennsylvania’s Medicaid program is the fourth-largest in the United States, with 3.5 million people enrolled and expenditures of $35.1 billion [ 19 , 20 ]. Past research in the Pennsylvania Medicaid program has demonstrated Black people were less able to access prenatal and postpartum care relative to those in other race groups [ 15 ]. Reporting from the Pennsylvania Maternal Mortality Commission shows that in more than half of the cases of pregnancy-associated deaths, the decadents were enrolled in Medicaid [ 21 ]. Similar to national figures, pregnancy-associated death was far more common among Black people vs. those of other races ( [ 21 ].
To ameliorate these racial disparities, Pennsylvania Medicaid is currently implementing two novel policies with the goal to advance racial equity in pregnancy and child health. The first, the equity incentive payment program, was initiated in 2020. The equity incentive payment program makes available approximately $26 million in Medicaid managed care organization (MCO) payments each year to plans that improve access to timely prenatal care and well-child visits among Black beneficiaries. The second is the maternity care bundled payment model, initiated in 2021, designed to provide incentives to obstetric providers across a wide range of pregnancy health outcomes and specifically incentivizes improvements among Black beneficiaries.
Although these policy approaches are unique, it is possible that other state Medicaid programs or other health insurers could learn from the policies and adapt or expand these approaches. Our research team will conduct a mixed-methods study to investigate the implementation and early effects of the two aforementioned policy changes on pregnancy and infant health equity. Our research aims are to: (1) evaluate implementation and early effects of the equity incentive payment program prenatal and early childhood healthcare outcomes and experiences among Black Medicaid beneficiaries; and (2) determine the extent to which an equity-focused maternity care bundled payment model affects racial equity in obstetric care and pregnancy health outcomes. To achieve these aims, we will draw on established partnerships between university researchers, community organizations, and policymakers to collect and analyze data. First, we will collect qualitative data with diverse stakeholders including Medicaid beneficiaries, MCO plan representatives, and pediatric and obstetric care clinicians to study implementation of these equity-focused policy changes. Second, we will use a community-partnered approach to develop a quantitative analysis plan of Medicaid administrative data for an estimated 167,000 birthing person-child dyads to estimate early effects of these policies. Our cross-disciplinary, community-engaged partnerships will enable us to triangulate how the healthcare policy structures of state Medicaid programs can be changed to promote racial equity in health.
Theoretical framework
The proposed research seeks to advance knowledge about the causes of, and structural interventions to improve, health and well-being among Black pregnant and parenting persons and their children in Medicaid. The theoretical model underlying this work is informed by foundational literature from a range of disciplines. First, it incorporates Critical Race Theory and Public Health Critical Race Praxis, which posit structural determinants, such as racism and other forms of oppression (e.g., sexism, classism, poverty), as fundamental causes of adverse social environments that interact to make certain populations more susceptible to illness and resulting in suboptimal health [ 22 , 23 , 24 , 25 , 26 ]. Second, it incorporates political science theory that dominant social definitions of populations shape group empowerment and resulting health policies and material benefits [ 27 ]. Third, it draws on new scholarship suggesting the necessity of studying social welfare policies with a critical race lens centering the beneficiaries’ lived experiences [ 11 , 28 , 29 ].
As depicted in Fig. 1 , our research project identifies both the Medicaid policy environment as well as the beneficiary experiences of the policy environment as upstream factors that influence healthcare organization and beneficiaries’ interaction with healthcare systems. In particular, we aim to facilitate and further enhance the connection between beneficiaries’ lived experiences and policy decision-makers through our collaboration with community partners. This connection can influence the policymaking process that shapes how care is delivered both at the managed care and healthcare provider levels. Healthcare utilization and quality are conceptualized as intermediate outcomes which may influence pregnancy and birth outcomes.
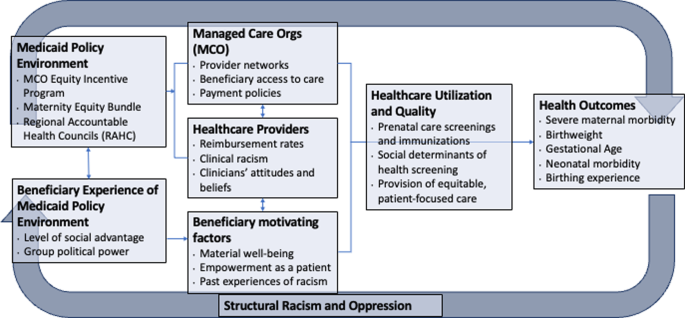
Conceptual model of the evaluation of structural interventions in Medicaid to promote racial equity in pregnancy and child health
Medicaid policy interventions
Nearly all Medicaid beneficiaries in Pennsylvania are enrolled in 1 of 8 Medicaid managed care plans, which manage the physical health care of enrollees and are subject to pay-for-performance requirements for healthcare quality measures. Currently, the Pennsylvania Medicaid program makes available 2% of total payments to MCO plans, contingent on MCO plan performance on 13 different healthcare quality metrics. An equity incentive payment program was added to this reimbursement scheme for two metrics in 2020: timely prenatal care and well-child visit utilization in the first 15 months of life (Fig. 2 ). Specifically, 2/13 (or 0.15%) of total payments are withheld for these two equity-focused metrics. MCO plans are assessed on overall performance and subsequently on the annual improvement on these measures among Black beneficiaries. MCO plans can be penalized (up to -0.12% of total payments) or rewarded (up to + 0.35% of total payments) for their performance on each of these two metrics.
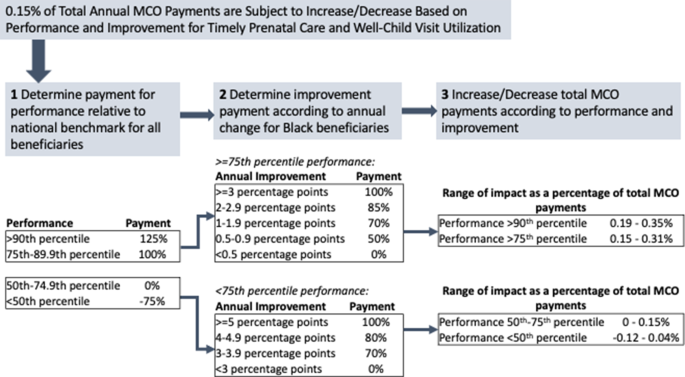
Pennsylvania Medicaid’s health equity incentive payment program will condition payments to managed care organizations based on overall performance as well as improvement among Black beneficiaries
Second, Pennsylvania Medicaid implemented a maternity care bundled payment model in 2021 that considers outcomes among Black beneficiaries (Fig. 3 ). Under maternity care bundled payment models, obstetric providers are incentivized to meet a total cost threshold and quality metrics for prenatal and delivery care [ 30 ]. Specifically, providers and payers agree on a target cost for low- or average-risk perinatal care, including pregnancy, delivery, and postpartum care. If total payments to providers are lower than the target cost while maintaining certain quality metrics, providers and payers share those savings. Under Pennsylvania’s new model, providers are able to achieve shared savings based on quality metric performance, as well as a health equity score reflecting performance on those metrics among Black beneficiaries.
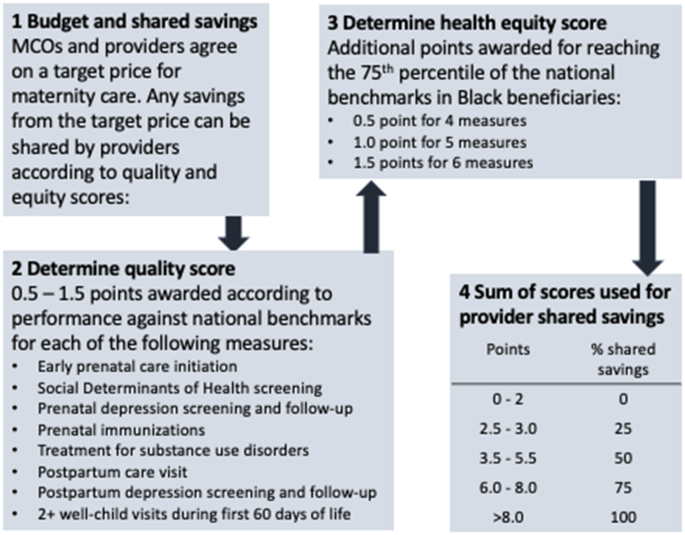
Pennsylvania Medicaid’s equity-focused maternity bundled payment model will allow for shared savings between obstetric care providers and managed care organizations, allowing for extra shared savings among providers whose Black patients experience better outcomes
Qualitative data Collection
To understand the interventions and responses to these policies, as well as related implementation barriers and facilitators, we will conduct interviews with each at least two representatives from each MCO ( n = 18). We will partner with colleagues from the Department of Human Services (DHS) to identify relevant MCO representatives. Interviews will elucidate MCOs’ perspectives, processes used by MCOs to design their interventions (e.g., review of existing evidence, input from community members or providers who serve them), anticipated effects, and sustainability of these payment policy changes. The goal is for some of the results of these interviews to inform our understanding of the implementation process which will be further explored in the interviews and focus groups with clinicians and Medicaid recipients.
In collaboration with the Community Health Advocates (CHA) program led by Healthy Start Pittsburgh, as well as other community and organizational partners across the state, we will recruit current and former Medicaid beneficiaries for focus group participation. We aim to recruit ∼ 50 community participants and will purposively oversample Black participants and will aim to recruit people of all ethnicities who identify as Black and multi-racial in order to achieve our aims of elucidating the experiences of Black parenting and pregnant people in Medicaid. Inclusion criteria are: current pregnancy or pregnant within the past 2 years; current or former enrollment in Pennsylvania Medicaid and/or Healthy Start; and ability to complete the interview in English.
Finally, we will partner with colleagues from DHS to identify pediatric and obstetric health professionals for interviews regarding the maternity bundled payment program and key outcomes related to the equity incentive payment. We will also use Medicaid administrative data to identify providers who serve Black beneficiaries and invite them to participate. We will aim to interview at least 20 obstetric and pediatric healthcare professionals to elucidate their perspectives on how structural racism in medicine affects patient outcomes, and the types of Medicaid policy changes that should be implemented.
We developed separate focus group/interview guides for community members, MCO leaders, and healthcare professionals. Each interview guide consists of open-ended questions to elucidate participants’ experiences with Medicaid; desired policy changes in Medicaid (among beneficiary participants); perceived steps that would be useful to combat anti-Black racism in healthcare and social services (especially among Black participants); and perspectives about the new Medicaid policies. Additionally, the interview guides ask demographic questions regarding gender identity, race, and ethnicity. We will first pilot-test the guide with our research partners and Healthy Start CHAs for clarity of question wording. All interviews will take place in-person in a private office space, or over the phone or videoconference, according to participants’ preferences and COVID-19 protocols. The interviewer will describe study objectives to each participant, obtain consent, and each interview will be audio-recorded and the interviewer will take notes throughout. Interview audio recordings will be transcribed verbatim, and transcripts spot-checked against the audio recordings for accuracy. The audio recording files will then be deleted to protect confidentiality of participants.
Qualitative data analysis
Study data will be analyzed and reported using the Consolidated Criteria for Reporting Qualitative Research (COREQ) Framework [ 31 ]. To analyze data, we will use template analysis, which combines features of deductive content analysis and inductive grounded theory, thereby allowing us to obtain specific information while also capturing any new or unanticipated themes [ 32 ]. Two coders will separately code the first 3 interview transcripts, meet to compare codes, discuss inconsistency in coding approaches, and then alter or add codes. This iterative process will be repeated until the coding scheme is fully developed. The coders will independently code all transcripts, and any coding discrepancies will be resolved via discussion. Once coding is complete, synthesis of content will begin by organizing codes under broader domains (meta-codes) as well as sub-codes. The primary analysis will be to convey qualitative data, including the use of illustrative quotes.
Quantitative healthcare data and analysis
Administrative healthcare data from the Pennsylvania Medicaid program, with linked birthing person-child dyads, will be used to create our quantitative analytic data. Medicaid data include a census of enrollment, hospital, outpatient/professional, pharmaceutical, and provider data for all beneficiaries in the Pennsylvania Medicaid program. Importantly, data contain self-reported race and ethnicity that is provided at the time of Medicaid enrollment (< 2% missing); as well as time-varying data on 9-digit ZIP code of residence. Data also include the amounts paid from Medicaid MCOs to healthcare providers for all medical services. Table 1 shows baseline data from Pennsylvania Medicaid-enrolled persons with a livebirth delivery in 2019, overall and stratified by race of the birthing person. We will also conduct sensitivity analyses to examine dyads that are multi-racial.
We will employ a comparative interrupted time series (ITS) analyses with a nonequivalent comparison group to estimate policy effects. Specifically, we will evaluate: (1) the extent to which the equity incentive payment program improved timely prenatal care and well-child visits among Black beneficiaries, relative to those of other races; and (2) the extent to which healthcare provider participation in the equity-focused maternity bundled payment model improved healthcare and health outcomes among Black beneficiaries, relative to those of other races.
For Aim 1, outcomes include binary measures of initiating prenatal care in the first trimester, and children receiving at least 6 well-child visits in the first six months of life. We will compare outcomes among Black beneficiaries relative to those of other racial groups, post- relative to pre- implementation of the equity incentive payment program. For Aim 2, outcomes include a composite of prenatal care quality measures (social determinants of health screening, prenatal and postpartum depression screening and follow-up, immunization, screening and treatment for substance use disorders, postpartum visit attendance), gestational age and birthweight, and severe maternal morbidity [ 33 ]. For both aims, multivariable regression models will control for maternal age, ethnicity, parity, ZIP code of residence, MCO plan enrollment, Medicaid eligibility category (expansion, pregnancy, disability, or others), and indices of obstetric and pediatric clinical comorbidities [ 34 , 35 ].
Sensitivity analyses
Analyses are designed to estimate early effects of the policies and should be interpreted alongside the qualitative results regarding policy implementation and beneficiary experiences. One assumption of ITS analyses is that our comparison groups approximate a counterfactual scenario for the intervention groups [ 36 , 37 , 38 ]. Although trends in Black-White inequities in pregnancy and child outcomes have, unfortunately, persisted over time [ 39 ], the COVID-19 pandemic has differentially burdened Black and Latina/x people relative to other race and ethnic groups [ 40 , 41 ]. Effects of the pandemic on pregnancy outcomes are only just beginning of what is to be explored [ 42 ]. It is therefore possible that we will not be able to disentangle policy effects from effects of COVID-19. To address this limitation, we will employ area-level rates of COVID-19 infection as control variables and for Aim 1 (equity incentive payment) we will conduct a sub-analysis investigating trends in 2021 vs. 2020. We chose to evaluate outcomes for Aim 2 (maternity care bundled payment) only in 2021, comparing the statistical intervention of race*provider. Finally, our qualitative analyses will provide context on differential impacts of COVID-19, which will inform interpretation of the quantitative results.
This study was approved by the University of Pittsburgh Institutional Review Board (Study # 23090108).
This mixed-methods research will investigate the extent to which changes in the Pennsylvania Medicaid program are associated with improvements in access to medical care and health outcomes among Black pregnant and birthing persons and their children. Our past research found that Black childbearing people in Pennsylvania Medicaid consistently experienced worse healthcare and health outcomes, compared to those of other racial and ethnic groups [ 43 , 44 ]. Racism in healthcare and other systems manifests in systematically worse access to and quality of care and other services for Black childbearing people [ 8 ]. In addition to suboptimal healthcare experiences, historical policies and practices such as residential redlining and segregation have resulted in lower wealth attainment in Black communities resulting in inequities in neighborhood factors and perinatal health [ 45 , 46 , 47 ].
The policies under study involve modifying common Medicaid reimbursement arrangements– namely, pay-for-performance programs and maternity care bundled payments. The policies are modified to embed financial incentives for Medicaid health plans and healthcare providers to improve the quality of care and health outcomes for Black pregnant and parenting persons and their children. These are the first such payment policies, to our knowledge, that explicitly aim to promote racial health equity with an explicit focus on addressing inequities that affect Black and Indigenous populations in Pennsylvania.
Interest from policymakers in payment reforms to improve health equity has increased recently; however, information on the implementation and effects of such models is sparse [ 48 , 49 ]. Although several state Medicaid programs have adopted maternity care bundled payment models, prior models have not considered racial inequities in pregnancy outcomes [ 30 , 50 ]. In 2012, Oregon adopted regional health equity coalitions as part of the state Medicaid program’s transition to Coordinated Care Organizations (CCOs). CCOs were required and given support to develop strategies that would address racial health disparities within the Medicaid population, and the regional health equity coalitions included underrepresented stakeholders to guide CCOs in the development of these interventions. While CCOs did reduce Black-white differences in primary care utilization and access to care within 3 years of policy implementation, it did not impact disparities in emergency department utilization [ 51 ]. The current research project will add to the extant evidence on how Medicaid programs can use policy to promote racial health equity.
Our study is limited in investigating the direct effects of the pandemic on racial inequities in perinatal and infant health and the intersections between the effects of the pandemic and the effects of the aforementioned Medicaid policies. However, we will have the ability to look at changes in outcomes over time. Additionally, these payment reform interventions focus largely on transforming the financing and delivery of healthcare, drawing attention to the structural and social determinants of health in the healthcare system. It is estimated that medical care contributes 10–20% to health outcomes; health and well-being are also shaped by factors such as environmental and socioeconomic conditions [ 52 ].
This study will contribute to the current body of knowledge about the recent interventions in Medicaid focused on racial equity. Specifically, findings will shed light on how the equity-focused obstetric care policies are being implemented and provide an evaluation of effects on health outcomes. These results can be used for future adaptions of the policy interventions or to inform the adoption of such equity-focused policies in different geographic regions of the United States.
Data availability
No datasets were generated or analysed during the current protocol study.
Abbreviations
Managed Care Organization
Community Health Advocate
Coordinated Care Organization
Alkema L, Chou D, Hogan D, Zhang S, Moller AB, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-agency Group. Lancet. 2016;387(10017):462–74.
Article PubMed Google Scholar
Wang E, Glazer KB, Howell EA, Janevic TM. Social determinants of pregnancy-related mortality and morbidity in the United States: a systematic review. Obstet Gynecol. 2020;135(4):896–915.
Article PubMed PubMed Central Google Scholar
Hoyert D. Maternal mortality rates in the United States, 2020. NCHS Health E-Stats; 2022.
Fingar K, Hambrick MM, Heslin KC, Moore JE. Trends and Disparities in Delivery Hospitalizations Involving Severe Maternal Morbidity, 2006–2015. Rockville, MD. 2018.
Thomas SB, Quinn SC, Butler J, Fryer CS, Garza MA. Toward a fourth generation of disparities research to achieve health equity. Annu Rev Public Health. 2011;32:399–416.
Crear-Perry J, Correa-de-Araujo R, Lewis Johnson T, McLemore MR, Neilson E, Wallace M. Social and Structural Determinants of Health Inequities in maternal health. J Womens Health (Larchmt). 2021;30(2):230–5.
Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90(8):1212–5.
Article CAS PubMed PubMed Central Google Scholar
Prather C, Fuller TR, Jeffries WLt, Marshall KJ, Howell AV, Belyue-Umole A, et al. Racism, African American Women, and their sexual and Reproductive Health: a review of historical and Contemporary Evidence and Implications for Health Equity. Health Equity. 2018;2(1):249–59.
Markus AR, Andres E, West KD, Garro N, Pellegrini C. Medicaid covered births, 2008 through 2010, in the context of the implementation of health reform. Womens Health Issues. 2013;23(5):e273–80.
Headen IE, Elovitz MA, Battarbee AN, Lo JO, Debbink MP. Racism and perinatal health inequities research: where we have been and where we should go. Am J Obstet Gynecol. 2022.
Michener JSM, Thurston C. From the Margins to the Center: A Bottom- Up Approach to Welfare State Scholarship. Perspectives on Politics. 2020:1–16.
Braveman PAE, Orleans T, Proctor D, Plough A. What is health equity? And what difference does a definition make? Princeton, NJ: Robert Wood Johnson Foundation; 2017.
Google Scholar
Thiel de Bocanegra H, Braughton M, Bradsberry M, Howell M, Logan J, Schwarz EB. Racial and ethnic disparities in postpartum care and contraception in California’s Medicaid program. Am J Obstet Gynecol. 2017;217(1):47. e1- e7.
Article Google Scholar
Gao YA, Drake C, Krans EE, Chen Q, Jarlenski MP. Explaining racial-ethnic disparities in the receipt of medication for opioid use disorder during pregnancy. J Addict Med. 2022.
Parekh N, Jarlenski M, Kelley D. Prenatal and Postpartum Care Disparities in a large Medicaid Program. Matern Child Health J. 2018;22(3):429–37.
Gavin NI, Adams EK, Hartmann KE, Benedict MB, Chireau M. Racial and ethnic disparities in the use of pregnancy-related health care among Medicaid pregnant women. Matern Child Health J. 2004;8(3):113–26.
Aseltine RH Jr., Yan J, Fleischman S, Katz M, DeFrancesco M. Racial and ethnic disparities in Hospital readmissions after Delivery. Obstet Gynecol. 2015;126(5):1040–7.
Wagner JL, White RS, Tangel V, Gupta S, Pick JS. Socioeconomic, racial, and ethnic disparities in Postpartum readmissions in patients with Preeclampsia: a multi-state analysis, 2007–2014. J Racial Ethn Health Disparities. 2019;6(4):806–20.
Kaiser Family Foundation. Total Monthly Medicaid/CHIP Enrollment and Pre-ACA Enrollment: Kaiser Family Foundation; 2022 [ https://www.kff.org/health-reform/state-indicator/total-monthly-medicaid-and-chip-enrollment/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D .
Kaiser Family Foundation, Total Medicaid Spending. FY 2020 2022 [ https://www.kff.org/medicaid/state-indicator/total-medicaid-spending/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D .
Pennsylvania Department of Health. Pregnancy-Associated Deaths in Pennsylvania, 2013–2018. Harrisburg, PA. 2020 December 2020.
Geronimus AT, Hicken MT, Pearson JA, Seashols SJ, Brown KL, Cruz TD. Do US Black women experience stress-related Accelerated Biological Aging? A Novel Theory and First Population-based test of black-white differences in telomere length. Hum Nat. 2010;21(1):19–38.
Marmot M. Health in an unequal world. Lancet. 2006;368(9552):2081–94.
Ekeke P, Mendez DD, Yanowitz TD, Catov JM. Racial differences in the biochemical effects of stress in pregnancy. Int J Environ Res Public Health. 2020;17:19.
Ford CL, Airhihenbuwa CO. Critical race theory, race equity, and public health: toward antiracism praxis. Am J Public Health. 2010;100(Suppl 1):S30–5.
Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–63.
Schneider AIH. Social Construction of Target populations: implications for politics and policy. Am Polit Sci Rev. 1993;87(2):334–47.
Michener J. Fragmented democracy: medicaid, federalism, and unequal politics. Cambridge, United Kingdom; New York, NY, USA: Cambridge University Press; 2018. xii, 226 pages p.
Ford CL, Airhihenbuwa CO. The public health critical race methodology: praxis for antiracism research. Soc Sci Med. 2010;71(8):1390–8.
Carroll C, Chernew M, Fendrick AM, Thompson J, Rose S. Effects of episode-based payment on health care spending and utilization: evidence from perinatal care in Arkansas. J Health Econ. 2018;61:47–62.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Centers for Disease Control and Prevention. Severe Maternal Morbidity in the United States 2021 [ http://www.cdc.gov/reproductivehealth/maternalinfanthealth/severematernalmorbidity.html .
Bateman BT, Mhyre JM, Hernandez-Diaz S, Huybrechts KF, Fischer MA, Creanga AA, et al. Development of a comorbidity index for use in obstetric patients. Obstet Gynecol. 2013;122(5):957–65.
Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14:199.
Ashenfelter OCD. Using the longitudinal structure of earnings to estimate the effect of training programs. Rev Econ Stat. 1985;67:648–60.
Donald SGLK. Inference with difference-in-differences and other panel data. Rev Econ Stat. 2007;89(2):221–33.
Imbens GWJ. Recent developments in the econometrics of program evaluation. J Econ Lit. 2009;47(1):5–86.
Goldfarb SS, Houser K, Wells BA, Brown Speights JS, Beitsch L, Rust G. Pockets of progress amidst persistent racial disparities in low birthweight rates. PLoS ONE. 2018;13(7):e0201658.
Prasannan L, Rochelson B, Shan W, Nicholson K, Solmonovich R, Kulkarni A et al. Social Determinants of Health and Coronavirus Disease 2019 in pregnancy: condensation: social determinants of health, including neighborhood characteristics such as household income and educational attainment, are associated with SARS-CoV-2 infection and severity of COVID-19 in pregnancy. Am J Obstet Gynecol MFM. 2021:100349.
Flores LE, Frontera WR, Andrasik MP, Del Rio C, Mondriguez-Gonzalez A, Price SA, et al. Assessment of the Inclusion of Racial/Ethnic Minority, female, and older individuals in Vaccine clinical trials. JAMA Netw Open. 2021;4(2):e2037640.
Janevic T, Glazer KB, Vieira L, Weber E, Stone J, Stern T, et al. Racial/Ethnic disparities in very Preterm Birth and Preterm Birth before and during the COVID-19 pandemic. JAMA Netw Open. 2021;4(3):e211816.
Krans EE, Kim JY, James AE 3rd, Kelley D, Jarlenski MP. Medication-assisted treatment use among pregnant women with opioid Use Disorder. Obstet Gynecol. 2019;133(5):943–51.
Parekh NJM, Kelley D. Disparities in access to care and emergency department utilization in a large Medicaid program. J Health Dispar Res Pract. 2018;11(4):1–13.
Assibey-Mensah V, Fabio A, Mendez DD, Lee PC, Roberts JM, Catov JM. Neighbourhood assets and early pregnancy cardiometabolic risk factors. Paediatr Perinat Epidemiol. 2019;33(1):79–87.
Mendez DD, Hogan VK, Culhane JF. Institutional racism, neighborhood factors, stress, and preterm birth. Ethn Health. 2014;19(5):479–99.
Mendez DD, Hogan VK, Culhane J. Institutional racism and pregnancy health: using Home Mortgage Disclosure act data to develop an index for mortgage discrimination at the community level. Public Health Rep. 2011;126(Suppl 3):102–14.
Huffstetler AN, Phillips RL. Jr. Payment structures that support Social Care Integration with Clinical Care: Social Deprivation indices and Novel Payment models. Am J Prev Med. 2019;57(6 Suppl 1):S82–8.
Anderson AC, O’Rourke E, Chin MH, Ponce NA, Bernheim SM, Burstin H. Promoting Health Equity and eliminating disparities through performance measurement and payment. Health Aff (Millwood). 2018;37(3):371–7.
Jarlenski M, Borrero S, La Charite T, Zite NB. Episode-based payment for Perinatal Care in Medicaid: implications for practice and policy. Obstet Gynecol. 2016;127(6):1080–4.
McConnell KJ, Charlesworth CJ, Meath THA, George RM, Kim H. Oregon’s emphasis on Equity Shows Signs of Early Success for Black and American Indian Medicaid Enrollees. Health Aff (Millwood). 2018;37(3):386–93.
Hood CM, Gennuso KP, Swain GR, Catlin BB. County Health rankings: relationships between determinant factors and Health outcomes. Am J Prev Med. 2016;50(2):129–35.
Download references
This study received funding from the National Institute of Nursing Research under award R01NR020670. The funder had no role in the study design, data collection or analysis, or decision to publish the study.
Author information
Authors and affiliations.
Department of Health Policy and Management, University of Pittsburgh School of Public Health, 130 DeSoto St, A619, 15261, Pittsburgh, PA, USA
Marian Jarlenski, Evan Cole & Christine McClure
Department of Epidemiology, University of Pittsburgh School of Public Health, Pittsburgh, PA, USA
Sarah Sanders, Marquita Smalls & Dara D Méndez
You can also search for this author in PubMed Google Scholar
Contributions
Jarlenski: Conceptualization; funding acquisition; investigation; methodology; supervision; writing-original draftCole: Conceptualization; data curation; investigation; resources; writing-reviewing and editingMcClure: Investigation; project administration; supervision; writing-reviewing and editingSanders: Investigation; methodology; visualization; writing-reviewing and editingSmalls: Investigation; project administration; visualization; writing-reviewing and editingMendez: Conceptualization; funding acquisition; investigation; validation; supervision; writing-original draft.
Corresponding author
Correspondence to Marian Jarlenski .
Ethics declarations
Ethical approval, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jarlenski, M., Cole, E., McClure, C. et al. Implementation and early effects of medicaid policy interventions to promote racial equity in pregnancy and early childhood outcomes in Pennsylvania: protocol for a mixed methods study. BMC Health Serv Res 24 , 498 (2024). https://doi.org/10.1186/s12913-024-10982-5
Download citation
Received : 12 December 2023
Accepted : 10 April 2024
Published : 22 April 2024
DOI : https://doi.org/10.1186/s12913-024-10982-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Well-child visits
- Prenatal care
- Health policy
- Health equity
- Mixed methods
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Surrogacy 'unicorn' is pregnant with baby No. 11 and would do it again 'in a heartbeat'

April 21-27 is National Infertility Awareness Week. All week, TODAY will be sharing stories to raise awareness of what it is like to experience infertility.
In the last 13 years, 37-year-old Emily Westerfield has delivered 10 healthy babies. Three were her own biological children. She acted as a gestational carrier for families of the others. Twice, she carried twins.
She is now 28 weeks pregnant with baby No. 11.
“I’m probably the unicorn in this industry,” Westerfield tells TODAY.com.
Her incredible success in navigating the surrogacy experience led her to give birth to Carrying Dreams , her own full-service agency designed to help egg donors, surrogates and intended parents on their parenting journeys in a way that works best for them.
So, would Westerfield consider having baby No. 12?
“In a heartbeat,” she says.
Planting the seed for surrogacy
Westerfield and her husband, Max, live in Celina, Ohio, with their three biological children: Mckenna, 13, Jack, 11, and Charlie, 10.
In 2010, Westerfield spent a lot of time bonding with Max’s cousin, who had been having trouble sustaining a pregnancy for years. She was suffering from secondary infertility and struggled to bring a pregnancy to term.
“She just continuously kept having loss after loss , and it was heartbreaking,” she says.
Westerfield was able to conceive and deliver her three biological children with relative ease, making her feel “guilty” every time she shared the news with her husband’s cousin. Without knowing much about the process of surrogacy, Westerfield offered to be a gestational carrier for the cousin’s embryo.

“They did not feel that surrogacy was the path that they wanted to take,” she explains, “but I knew that there were probably so many other people in the world who needed help in a very similar way. Maybe I could help.”Even while she was pregnant with her third (and last) biological child, Westerfield mentioned to her husband that she was interested in becoming a gestational carrier.
“I was shot down by him so many times,” Westerfield says with a laugh. “The more and more I shared to educate him, I think the more and more he felt comfortable with it. Or he just got sick of me nagging.”
The first surrogacy journey
After her son Charlie completed their family, Westerfield activated her search to find another family to assist via surrogacy in earnest. She joined an online forum that no longer exists. “It was almost like a Craigslist of everybody in the infertility community,” she says. Surrogates, egg donors, sperm donors and intended parents used the site to help create families.
“I created a profile and just put myself out there,” says Westerfield. “I was overwhelmed with the response and just inundated with emails and queries. The more and more that I got into this, the more I realized there’s so many more people out there that need the help than the people that are willing to help.”
Westerfield had initial conversations with a handful of hopeful parents and ultimately chose a couple that seemed like a good match in terms of personality, age and location. They were an easy three-hour drive away.
But the decision wasn’t easy. Each story was more heartbreaking than the one before. The family that Westerfield ultimately decided to help already had two children. During the second birth, the mother needed an emergency hysterectomy, leaving her unable to complete their family with the third child they so desperately wanted.
Calling to tell the couple the good news “was so emotionally overwhelming and exciting and nerve-wracking, all at the same time.” Using the embryos the couple had already created, Westerfield delivered their third child, a girl, in December 2015.
“And that’s when everything started,” Westerfield says.

Westerfield says, “I noticed that as soon as I had the first one, I wanted to do this again. It was almost just like, ‘Now who else can I help?’”
She delivered healthy babies in 2011, 2013, 2014, 2015, 2017, 2018, 2021 and 2022. She is currently pregnant and due in July.
“I’ve been able to completely just have wonderful pregnancies,” she says. Even so, at age 37, she knows that she may have a limited window in which to continue.
The process of being a gestational carrier is markedly different than being pregnant with your own child, according to Westerfield. For instance, there are screenings and contracts and psychological evaluations. Her husband did not accompany her to appointments. She keeps in mind that the end goal is to deliver a healthy child so that another couple can “start, build or complete their family.”
Wondering if it’s ever hard to let go of a baby you have physically carried for nine months? Westerfield says it’s not.
“I get attached like a loving aunt,” she explains. Knowing the heartbreak that the couple has gone through in the past, “you want to hand that baby over when you get to the end of this.”
Westerfield started her own surrogacy agency in August 2023 in part to help educate and provide resources for both potential surrogates and intended families.
“I feel like there’s so much information out there that it’s overwhelming,” Westerfield says. “And a lot of it is outdated or incorrect, and I want to be able to speak from personal experience going through this process.”

She also helps match families with gestational carriers and helps hold their hand through a stressful process, making sure they are on the same page for important topics like physical or chromosomal abnormalities, geographic location, contact preferences after birth and even vaccination status.It’s difficult to find gestational carriers who are willing and fit all of the qualifications. Westerfield also thinks it’s essential for gestational carriers to have completed their own families before helping others grow theirs. She has about six prospective couples for every one potential surrogate.
Westerfield takes a lot of pride in helping families grow, especially those she has carried children for. She stays in touch with each family in some capacity via text or social media, and she tries to remember to send birthday gifts.
“I am so proud to be able to do this for other people. I know my time is very limited as we’re getting closer and closer to how many people I’m able to help, but still I’m young enough and I’m healthy enough to be able to do so,” Westerfield says. “And I’ll continue to help as long as my body and my family allows me to.”
Rosie Colosi is a reporter for TODAY Parents.

IMAGES
VIDEO
COMMENTS
Your next prenatal visits — often scheduled about every four weeks during the first trimester — might be shorter than the first. Near the end of the first trimester — by about 12 to 14 weeks of pregnancy — you might be able to hear your baby's heartbeat with a small device, called a Doppler, that bounces sound waves off your baby's ...
If your first prenatal appointment comes later in your pregnancy, around 10 or 12 weeks or later, your provider may use a traditional ultrasound or Doppler to check the fetal heartbeat. Earlier ...
The most common tests at your first prenatal visit will likely include: [3] Urine test. Your urine may be checked for protein, glucose (sugar), white blood cells, blood and bacteria. Bloodwork. A sample of your blood will be used to determine blood type and Rh status and check for anemia. Trusted Source Mayo Clinic Rh factor blood test See All ...
If you did not meet with your health care provider before you were pregnant, your first prenatal visit will generally be around 8 weeks after your LMP (last menstrual period ). If this applies to you, you should schedule a prenatal visit as soon as you know you are pregnant! Even if you are not a first-time mother, prenatal visits are still ...
When to schedule your first prenatal visit. As soon as you get a positive result on a home pregnancy test, book an appointment with an obstetrician, family physician, or midwife.Depending on the practice, it's normal for another provider in the office, like a nurse practitioner or physician assistant, to handle your first visit.
The first ultrasound. Many people look forward to their first ultrasound, which usually happens at the initial prenatal visit. This ultrasound gives you the opportunity to hear your baby's heartbeat. It'll be fast — about 100 to 160 beats per minute! An ultrasound gives your clinician a better idea about your due date.
1st Trimester: 1st Prenatal Visit. It's the first doctor visit of your pregnancy. Congratulations! During this visit, your doctor will check your overall health and determine your due date. They ...
Your first prenatal visit will probably be scheduled sometime after your eighth week of pregnancy. Most health care providers won't schedule a visit any earlier unless you have a medical condition, have had problems with a pregnancy in the past, or have symptoms such as spotting or bleeding, stomach pain, or severe nausea and vomiting. 1 You've probably heard pregnancy discussed in terms of ...
The first prenatal visit can be exciting yet stressful. With all the poking and prodding and the uncertainty of test results, it is bound to get any mom-to-be nervous.
During prenatal care visits, your doctor, nurse, or midwife may: update your medical history. check your urine. check your weight and blood pressure. check for swelling. feel your belly to check the position of your fetus. measure the growth of your belly. listen to the fetal heartbeat. give you any genetic testing you decide to do.
The first prenatal check-up is usually scheduled around week eight of pregnancy, or, at least, ideally before week 10. It's a good idea to schedule your first prenatal appointment once you get a positive pregnancy test. The first prenatal visit is significant because getting prenatal care on time is a vital step in a healthy pregnancy.
Typically, the first thing your ob-gyn will do is confirm your pregnancy with a urine or blood test. You'll also have a physical exam. 1,8 A nurse or ob-gyn will check your height, weight and blood pressure. You'll then have a thorough health screening, checking everything from your thyroid, heart and lungs to your breasts, abdomen and skin.
Make an appointment for your first prenatal visit once you're aware you are pregnant - when you receive a positive home pregnancy test, for example. Booking it around week 8 of pregnancy is typical. You'll come back regularly in the weeks and months following that initial appointment. Most people have between 8 and 14 prenatal visits ...
At your first pregnancy appointment, your provider might perform or discuss future genetic testing. "There are genetic tests that are time-sensitive and can be done as early as 10 weeks," says Braden. "There are some that are done with an ultrasound around 12 or 13 weeks pregnant, and some that are done in the second trimester.
Also, the BIG VISITS to attend are the first prenatal visit, 12 week visit, 20 week anatomy scan (where you can find out the gender!) and one or two late pregnancy appointments nearing your due date. Have your insurance cards and ID ready to present to the receptionist when checking in to your appointment.
Complications of pregnancy and childbirth are the leading cause of morbidity and mortality in females of reproductive age globally . This topic will discuss the initial prenatal assessment (which may require more than one visit) in the United States. Most of these issues are common to pregnancies worldwide.
Your first prenatal visit will likely be your longest visit. Your care team will ask about your medical history (menstrual cycle, birth control, past pregnancies, previous surgeries, family history and medications). They will also perform a physical exam and order routine lab tests. Your care team will let you know what your expected due date ...
Overview. Your first prenatal visit will probably be the longest visit you'll have. Your doctor or midwife will take your medical history and do a complete physical exam. You may also have some tests. This will provide information that can be used to check for any problems as your pregnancy progresses.
Typical prenatal appointment schedule. The number of visits you'll have in a typical pregnancy usually total about 10 to 15, depending on when you find out you're expecting and the timing of your first checkup. In most complication-free pregnancies, you can expect to have a prenatal appointment with the following frequency: Weeks 4 to 28 ...
The first prenatal visit is typically scheduled for when you're 7-10 weeks pregnant. This is counted from the first day of your last period. This timing is important, as "it confirms a viable pregnancy and ideally gives the most accurate due date," says Katy Orr, a certified registered nurse practitioner at the University of Alabama at ...
The initial visit with your healthcare provider during pregnancy typically occurs between 8-10 weeks after conception and last about 30 minutes to 1 hour. This appointment is of utmost importance, as it often comprises a thorough physical examination and routine prenatal laboratory tests. If you missed out on your first prenatal check-up before ...
Your first prenatal visit will probably be the longest visit you'll have. Your doctor or midwife will take your medical history and do a complete physical exam. You may also have some tests. This will provide information that can be used to check for any problems as your pregnancy progresses. Medical history
The American College of Obstetricians and Gynecologists updated its recommendations, advising a routine blood screening at the first prenatal visit and screenings in the third trimester of ...
For Aim 1, outcomes include binary measures of initiating prenatal care in the first trimester, and children receiving at least 6 well-child visits in the first six months of life. We will compare outcomes among Black beneficiaries relative to those of other racial groups, post- relative to pre- implementation of the equity incentive payment ...
Westerfield says, "I noticed that as soon as I had the first one, I wanted to do this again. It was almost just like, 'Now who else can I help?'" She delivered healthy babies in 2011, 2013 ...