
Are doctors spending less time with patients?

Patient visits are changing. In 2020, COVID-19 ushered in telehealth . And in just the past decade, nearly every physician started using electronic health records. This infusion of health IT into clinical encounters means physicians have changed their documentation workflows and are approaching patient visits differently. Amidst these changes, are doctors spending less time with patients?
The short answer is “no.” While it’s hard to pin down a meaningful average for something like patient visit times, studies indicate that doctors have spent roughly 13 to 24 minutes with patients for at least the past three decades.
Data from the 1990s reveal some debates about the average time physicians spend with patients. Surveys from those years placed the average around 17 minutes, but competing studies claimed the real number was closer to 10 minutes. Other research found that physicians and their staff tend to overreport patient visit times by about 4 minutes, on average.
Research published in 2021 used time-stamped EHR data from over 21 million primary care visits to estimate average exam length. The authors conclude that the average primary care exam lasts 18 minutes, which is consistent with estimates derived from more common methods like retrospective surveys.
A review of 2018 data suggests that most U.S. physicians spend between 13 and 24 minutes with patients. About 1 in 4 spend less than 12 minutes, and roughly 1 in 10 spend more than 25 minutes. All in all, it seems like doctor-patient time isn’t changing substantially.
While about half of physicians did report experiencing a permanent reduction in patient volume due to COVID-19, for most the impact has been marginal. The weekly average number of patients doctors see dropped from 76 to 71 after the pandemic, which predictable variation across specialties. This reduction may affect visit times, but there is not yet reliable data to confirm either way.

Have EHRs changed the length of patient visits?
Much of the U.S. survey data come from Medscape’s annual Physician Compensation Report , which surveys roughly 18,000 doctors about things like their salary, hours worked, and time spent with patients. Presumably their survey would register any notable changes to how long doctors are spending with patients in each visit.
Contrary to what you might expect, physician-patient time has remained pretty constant since the adoption of EHRs. In the 2018 survey, when time spent with patients was last reported, 61 percent of physicians reporrted spending 1 3-24 minutes with patients . In 2016 that number was 60 percent. Responses look similar in Medscape’s annual surveys going back to 2011.
The reason visit times haven’t dropped is probably that physicians enjoy interacting with patients. Gratitude and relationships with patients is the aspect their job that doctors say is most rewarding (in 2021 this was matched by “knowing that I’m making the world a better place”).
Research shows that when limits are put on time with patients, physicians experience less job satisfaction . Longer visits are also connected to positive patient outcomes . When patients get more time with doctors, they tend to be more satisfied with their care, experience reduced rates of medication prescriptions, and be less likely to file malpractice claims.
So what’s the problem?
So why are so many physicians struggling in medicine or leaving the field? Physician burnout is skyrocketing . It seems like more and more doctors are seeing a gap between the values that brought them to medicine and their day to day reality. But what’s causing the disconnect?
Patient visit times are about as long as they’ve always been. It’s the rest of physicians’ work days that’s changing. Doctors are spending more time than ever on documentation and administrative tasks, leading to dissatisfaction and professional burnout.
Here’s the number that’s shocking: in 2021 doctors reported spending on average 15.6 hours per week on paperwork and other administrative tasks. This reflects a trend that’s emerged in the last decade. In 2018, 70 percent of physicians said they spend over 10 hours per week on paperwork and administrative tasks. In 2017, that number was 57 percent . But just one-third of physicians reported the same experience in 2014.
Most physicians’ would tell you that their experience of practicing medicine is different than it was a decade ago. But when we look at the numbers, it’s not patient visit times that are changing. It’s everything else.
- Mobius Conveyor
- Conveyor QR
- Conveyor USB
Athenahealth-Specific
- Mobius Clinic
- Mobius Scribe
- Mobius Desktop Scribe
- Mobius Capture
Recent Posts
- Medical transcription: a brief history
- Manage your EHR inbox more effectively with these tips
- Use your smartphone for instant medical dictation
- Do AI medical scribes work?
- Which medical dictation workflow is best for you?
- Privacy & Terms
How Much Time Does A Doctor Visit Really Take?
July 4, 2022
First Stop Health
When you or a family member is not feeling well or hurt, finding quick care can be challenging. Doctor’s offices, urgent care centers and emergency rooms are three traditional options for care that are not time-friendly or convenient. Whether it’s travel time, transportation, taking time off work, cost or arranging for childcare, there are many personal factors to consider when seeking care at these institutions.
Transportation is one of the biggest barriers to accessing healthcare. 1 In fact, “Americans spend an average of 34 minutes on the road to a doctor’s office or other medical entity,” totaling more than an hour of travel time to and from an in-person visit. 2 This statistic excludes the time it takes with public transportation. Shockingly, 45% of Americans do not have access to public transportation and 3.6 million people do not get care annually due to limited transportation access. 3, 4
Another personal factor to consider is childcare. The average cost for childcare is $15 and $23 per hour and accessing childcare may not be easy. 5 Due to COVID-19, childcare centers across the U.S. are in short supply. 6
Now that we’ve broken down some personal factors, let’s look at the time it actually takes at a doctor’s office, urgent care center and emergency room.
A Doctor’s Office Visit
While having routine checkups with a primary care physician (PCP) is essential for overall physical and mental health, for non-emergent issues such as a sinus infection, rash or urinary tract infection, the time it takes to get an appointment with a PCP isn’t helpful. On average, Americans wait 24 days to see a PCP in-person. 7
Once in the office, patients wait almost 20 minutes to be seen, even with an appointment. 8 These wait times are sometimes longer and are another deterrent for seeking care. A recent study revealed 30% of patients left their doctor’s office due to long wait times. 8
After the time it takes to get to the doctor’s office and the time spent waiting, 1 in 4 doctors spend just 9-12 mins with a patient. 9 This is an inadequate amount of time for a PCP to cover symptoms and the patient’s history. Rushed appointments strain the doctor-patient relationship, diminishing trust and value-based care. The 15-minute care model is not beneficial to the patient. 10
If an illness emerges during a doctor’s office off-hours, there is typically no way to access care. U.S. adults are the least likely of high-income countries to have a primary doctor to seek care from and are the least likely to have access to care during off-business hours, leading them to seek care at an urgent care center or emergency room. 11 This makes the time to get care even longer.
The end result = 1 doctor’s visit is 2 hours (if you can get in to see a doctor before the average 24-day wait period)
An Urgent Care Center Visit
Much like a visit to a PCP, a trip to an urgent care center will take about two hours or more. But depending on the severity of your illness or injury and the number of other patients (and the severity of their illnesses or injuries), wait times can be much longer. Wait times in an urgent care center can range from 20 minutes to 90 minutes. 12
Unlike a visit with a PCP, urgent care center visits are much more expensive. The average cost of urgent care center visits range from $100 to $150 and costs can be higher or lower depending on insurance coverage, annual deductibles and copays. 13
The end result = 1 urgent care visit is 2-4 hours and costs can be confusing based on insurance coverage
An Emergency Room Visit
Higher-severity cases might bump a minor injury down the list, and emergencies aren’t scheduled. On average, the entirety of an emergency room visit is 2+ hours and costs more than $1,300. 14
Almost 60% of emergency room visits come outside of business hours. 14 So, after enduring the wait time and exam, the wait times roll over to the next day to see the referred doctor or to visit a pharmacy during regular hours.
A doctor should be someone a patient can trust. According to a recent study, 70% of providers told patients to go to an emergency room instead of an urgent care center, even though the patient indicated they would seek care at an urgent care center. 15 In turn, 56% of emergency room visits are completely avoidable and could save a patient thousands of dollars in out-of-pocket expenses. 14
The end result = 1 emergency room visit is 4+ hours, expensive and likely avoidable
Summary
Whether it’s an emergency or a routine trip to your PCP for a simple sinus infection, a doctor’s visit takes much more time than we anticipate. It’s never as quick or affordable as we hope. Plus, a patient must also take into consideration pharmacy wait times and travel times if a medication is prescribed.
As an alternative, First Stop Health Telemedicine and Virtual Primary Care provide fast, convenient solutions to a daunting necessity. You can’t just skip unavoidable medical care, but you can skip worrying about transportation, wait times, co-pays and time off work. First Stop Health members have 24/7 access to free, quality and convenient healthcare. Members can connect to doctors in under 6 minutes for Telemedicine and within 3 days for Virtual Primary Care. Our virtual doctors are board certified in their field of medicine, can treat patients in all 50 states and Washington DC, and have 10 years of post-residency experience, on average.

- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4265215/
- https://www.naplesnews.com/story/news/health/2019/03/03/americans-average-34-minutes-road-see-doctor-study-shows/3020326002/
- https://www.apta.com/news-publications/public-transportation-facts/
- https://www.aha.org/ahahret-guides/2017-11-15-social-determinants-health-series-transportation-and-role-hospitals
- https://www.valuepenguin.com/average-cost-child-care#:~:text=Parents%20in%20U.S.%20cities%20generally,typically%20pay%20more%20per%20hour
- https://www.americanprogress.org/article/costly-unavailable-america-lacks-sufficient-child-care-supply-infants-toddlers/
- https://medcitynews.com/2017/12/patients-waiting/
- https://www.fiercehealthcare.com/practices/ppatients-switched-doctors-long-wait-times-vitals#:~:text=Across%20specialties%2C%20the%20average%20wait,patient%20waits%20depending%20on%20location .
- https://www.statista.com/statistics/250219/us-physicians-opinion-about-their-compensation/
- https://khn.org/news/15-minute-doctor-visits/
- https://www.commonwealthfund.org/publications/issue-briefs/2022/mar/primary-care-high-income-countries-how-united-states-compares
- https://www.advisory.com/daily-briefing/2012/12/04/member-asks#:~:text=The%20Urgent%20Care%20Association%20of,as%20long%20as%2090%20minutes .
- https://www.debt.org/medical/emergency-room-urgent-care-costs/
- https://journals.sagepub.com/doi/10.1177/1062860617700721
Originally published Jul 4, 2022 2:00:00 PM.
Related Posts
The state of primary care .
August 30, 2022
3 Reasons to Offer Virtual Primary Care to Employees
November 8, 2022
The Evolution of Primary Care
July 18, 2022
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
December 15, 2020
How long do doctor visits last? Electronic health records provide new data on time with patients
by Wolters Kluwer Health

How much time do primary care physicians actually spend one-on-one with patients? Analysis of timestamp data from electronic health records (EHRs) provides useful insights on exam length and other factors related to doctors' use of time, reports a study in the January issue of Medical Care . The journal is published in the Lippincott portfolio by Wolters Kluwer.
"By using timestamps recorded when information is accessed or entered, EHR data allow for potentially more objective and reliable measurement of how much time physicians spend with their patients," according to the new research by Hannah T. Neprash, Ph.D., of University of Minnesota School of Public Health and colleagues. That may help to make appointment scheduling and other processes more efficient, optimizing use of doctors' time.
More precise estimates of primary care visit times
Using a national source of EHR data for primary care practices, the researchers analyzed exam lengths for more than 21 million doctor visits in 2017. The study focused on exam lengths and discrepancies between scheduled and actual visit times.
Based on EHR timestamps, the mean exam time was 18 minutes, with a median of 15 minutes. "The mean exam lasted 1.2 minutes longer than scheduled, while the median exam ran 1 minute short of its scheduled duration," Dr. Neprash and coauthors write. The longer the scheduled visit, the longer the exam time.
"However, shorter scheduled appointments tended to run over while longer appointments often ended early," the researchers add. Scheduled 10-minute visits ran over by an average of 5 minutes; in contrast, scheduled 30-minute visits averaged less than 24 minutes.
More than two-thirds of visits deviated from the schedule for 5 minutes or more. About 38 percent of scheduled 10-minute visits lasted more than 5 minutes, while 60 percent of scheduled 30-minute visits lasted less than 25 minutes.
The findings suggest "scheduling inefficiencies in both directions," according to the authors. "Primary care offices' overuse of brief appointment slots may lead to appointment overrun, increasing wait time for patients and overburdening providers." In contrast, "longer appointments are critical for clinically complex patients, but misallocation of these extended visits represents potentially inefficient use of clinical capacity."
The time doctors spend with patients has a major impact on care. Average visit times seem to have increased over the years—yet physicians may still feel pressed to do more in the available time, including documentation, patient monitoring, and prevention/screening steps.
Estimates of medical visit times have been largely based on national surveys, which rely on information reported by office-based practices. For several reasons, these estimates may not accurately reflect the actual time doctors spend with patients in the examination room.
Routine data collected by EHRs provide a new way to measure length of physician visits, Dr. Neprash and colleagues write. Their method excluded visits where EHR data didn't seem to be recorded in real time and accounted for overlapping visits due to "double-booking."
Health systems could use EHR data to track discrepancies between schedules and actual visit lengths, enabling more efficient scheduling for patients with different needs. While acknowledging some limitations and challenges of this approach, the researchers believe their findings "support the development of a scalable approach to measure exam length using EHR data."
Explore further
Feedback to editors

Specific nasal cells found to protect against COVID-19 in children
54 minutes ago

Human muscle map reveals how we try to fight effects of aging at cellular and molecular levels

Are Americans feeling like they get enough sleep? Dream on, a new Gallup poll says

Physical activity lowers cardiovascular disease risk by reducing stress-related brain activity, study finds
3 hours ago

Carbon beads help restore healthy gut microbiome and reduce liver disease progression, researchers find
10 hours ago

Untangling dreams and our waking lives: Latest findings in cognitive neuroscience
16 hours ago

Researchers demonstrate miniature brain stimulator in humans
Apr 13, 2024

Study reveals potential to reverse lung fibrosis using the body's own healing technique
Apr 12, 2024

Researchers discover cell 'crosstalk' that triggers cancer cachexia

Study improves understanding of effects of household air pollution during pregnancy
Related stories.

Extra visit time with patients may explain wage gap for female physicians
Sep 30, 2020

Virtual follow-up care is more convenient and just as beneficial to surgical patients
Oct 4, 2020

Outpatient wait times are longer for Medicaid recipients
May 11, 2017

Four tips for maximizing virtual healthcare visits
May 12, 2020

Telemedicine reduces cancellations for care during COVID in large Ohio heath center
Nov 6, 2020

Patients find video primary care visits convenient
Apr 30, 2019
Recommended for you

Scientists uncover a missing link between poor diet and higher cancer risk

PFAS exposure from high-seafood diets may be underestimated, finds study

Pandemic drinking hit middle-aged women hardest, study finds

First national study of Dobbs ruling's effect on permanent contraception among young adults
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Gen Intern Med
- v.30(11); 2015 Nov

The End of the 15–20 Minute Primary Care Visit
Mark linzer.
Division of General Internal Medicine, Hennepin County Medical Center, 701 Park Ave S (P7), Minneapolis, MN 55415 USA
University of Minnesota, Minneapolis, MN USA
Asaf Bitton
Harvard Medical School, Boston, MA USA
Shin-Ping Tu
Virginia Commonwealth University, Richmond, VA USA
Margaret Plews-Ogan
University of Virginia, Charlottesville, VA USA
Karen R. Horowitz
Louis Stokes Cleveland VAMC, Cleveland, OH USA
Case Western Reserve University School of Medicine, Cleveland, OH USA
Mark D. Schwartz
New York University School of Medicine, New York, NY USA
Sign on a print shop door:
“We can do it fast, we can do it well, we can do it cheap. Pick two.”
A 78-year-old widow with hypertension, osteoarthritis, a recent stroke, elevated cholesterol, and a 50-pack-year smoking history comes to her primary care provider for a mild cough and weight loss. She lives alone and loves to chat with her doctor. The physical examination is unrevealing. Chest x-ray shows a lung nodule. A CT scan is ordered. A long discussion ensues about what would happen if the CT scan shows cancer: how would she undergo evaluation and treatment with her family far away? For what became a 40-min visit, only 15 min had been allotted. Now the doctor is behind schedule. She feels guilty and gives more time to each patient, thus falling further behind. Screening issues are postponed and personal interactions are diminished. A walk-in patient is added. One waiting patient leaves angrily. At the end of the day, facing a large pile of forms and documentation needs, the doctor feels drained and questions the quality of care she provided.
The Time Crunch
While Mechanic demonstrated that routine primary care visits (averaging 15–20 min) were 1 to 2 min longer than before, 1 the complexity of clinical issues addressed during these visits has increased. In 2010, the CDC reported that one-third of elderly patients had three or more chronic medical conditions, with 40 % of patients taking three or more medications. Providers may respond by cutting corners on the history and physical examination and by ordering more tests, which lead to a cascade of follow-up tests. Providers describe behind-the-scenes burdens of documentation, phone calls, emails, refills, consultations, and lab reports, while careful calculations show that guideline-driven preventive care would add 7 h to each primary care clinician’s workday. 2 The work of primary care simply cannot be completed in the time allotted.
Consequences for Patients
Increased work during short (<20 min) visits means appointments in which fewer health care issues are addressed and the depth of understanding is diminished. Time-consuming psychosocial determinants of health are left unaddressed. These consequences translate to decreased patient satisfaction, excess emergency room usage and non-adherence to treatment plans. 3
Consequences for Providers
Fifty-three percent of primary care providers report time pressure in the clinical encounter. 4 Many providers describe emotional exhaustion and the fear of making clinical errors. Students observe harried primary care providers and choose alternative career paths.
Root Causes
In the early 1990s, Medicare adopted the relative value unit (RVU) payment model. In a budget-neutral system, the introduction of new procedures at substantially higher RVU levels has resulted in the devaluing of cognitive care such as evaluation and management services. When private insurers and managed care contracts reduced compensation, providers increased daily volumes to maintain stable incomes. Health systems followed with daily visit targets. This fee-for-service (FFS) system, poorly constructed for the delivery of comprehensive primary care, has left primary care providers feeling like they are on an assembly line rather than engaged in a mission to heal the sick and prevent serious illness.
Brief visits would suffice if the tasks of primary care had decreased, or if sharing this work with other team members had increased. But this has not been the case. Scientific advances have increased the complexity of diagnostic testing and prescribing, the frequency of care coordination between generalists and subspecialists, and the post-visit workload. Computer work has spiraled, along with an expanded number of reportable performance measures. Electronic medical records (EMRs) have decreased face-to-face time with patients, while “meaningful use” EMR requirements have set forth worthy but time-consuming tasks. To provide patients with the personalized care they seek, a new system is needed.
Suggestions for Broad System Changes
Having flexible encounter times in primary care to meet patient needs will require shifts in both workflow and compensation. We recommend that the routine care of complex primary care patients requires a visit time to meet patient needs, and may be 30 min or longer . Models should include fees for care management and provide resources for team-based care by nurses, medical assistants, and pharmacists. While alternative payment models are emerging in both public and private sectors, 5 what is lacking is a systematic approach for providers to respond to these new incentives with strategies that improve outcomes with lower spending. These strategies should include the means to allow sufficient time for patients to feel heard and for providers to deliver high-quality care.
To account for the increasing complexity of primary care, there will need to be a recalibration of the value of cognitive care codes , by both the Relative Value Scale Update Committee, or RUC (who provides the recommendations), and by CMS (who implements them). Updating RVUs for evaluation and management services to give them greater weight would help redirect revenue to primary care, as most alternative payment models, such as patient-centered medical homes and accountable care organizations (ACOs), are still built upon an FFS base.
New payment systems to support longer primary care visits face uphill challenges. First, inadequate care management fees (with extensive time requirements for documentation) often leave practices adrift between the promise of team-based care and the reality of an FFS system (a “foot in two canoes”). Second, due to Medicare Part B’s 20 % co-pay mandate, adoption of CMS’ care management fees may lead to increased patient co-pays for beneficiaries without supplemental insurance covering this newly reimbursed service. Finally, it will take time and perseverance to change a culture in which practice leaders are accustomed to thinking of fewer visits as a sign of clinicians not working hard.
We believe there are several ways to get from here to there. For one, health care organizations should acknowledge differing care models (FFS versus “total cost of care”) operating within the same health system. For example, “ambulatory ICUs” or “intensive primary care” settings have become a popular means to reduce excess utilization. In these models, increased visit time and upfront investments in personnel and resources improve the ability of providers to manage the social and medical needs of high-utilizing patients. These systems are sustainable when integrated business models track dollars spent in the new care model (e.g., on additional team members) and include credits for savings from reduced emergency department and inpatient utilization. Otherwise, providers with low RVU production are penalized for “not working hard enough.” These integrated business models will reflect overall cost savings for the institution and will remove “intensive primary care” providers from being evaluated through an FFS lens. Second, alternative payment models could be expanded with new mechanisms to change the basis for clinician payments, such as through the SGR [Sustainable Growth Rate] Repeal and Provider Payment Modernization Act. Third, ACOs, which manage the full continuum of care while being held accountable for costs and quality, may negotiate contracts with additional primary care funding based upon risk adjustment for social and medical characteristics of their populations.
How can practices traverse the change to appropriately timed visits while unbundling activities that could be performed by others? Management approaches, such as LEAN methodology, could be used to streamline primary care visit. These practice transformations will first require evaluating an organization’s “capacity for development,” or readiness to change, and resources will be needed to reshape the practice’s operations and values. While we await these transformations, the provision of primary care will require more time than is currently allotted.
Innovative processes to improve access to care, including patient portals, e-visits, nurse visits, and community health worker (CHW) contacts, are all in development. Providing efficient care to patients during longer visits could avoid short-changing patient needs, lead to better outcomes, and preserve access by reducing the need for early return appointments.
We anticipate real benefits of allowing sufficient time for primary care, including lower emergency room and hospital utilization, fewer unnecessary referrals, less ill-advised diagnostic testing, and improved patient satisfaction. Better interpersonal communication will also improve clinician satisfaction and well-being, critical components in addressing the current crisis in the shrinking primary care workforce.
In a new model, the same 78-year-old patient would have had a CHW and a provider with flexible visit times. In this scenario, the CHW had spoken with the patient and reported her cough and weight loss to the doctor. The chest x-ray performed prior to the visit showed a large nodule. In the 30 min allotted, the doctor had time to empathically discuss the findings with the patient, order a CT scan, and collaboratively decide upon a follow-up plan. The doctor did not fall behind in her work day, and other patients were not inconvenienced. It was still a hard day, but it was also rewarding. The medical student working with her was impressed with the compassionate, multidisciplinary care, and decided that this was a career worth pursuing.
Primary care cannot be done fast, well, and cheap. Let’s find the ways to appropriately structure it, pay for it, and do it right.
Acknowledgments
We are grateful to Dr. Christine Sinsky for her inspiring comments on a draft of this manuscript. We also thank the editors for their support and insights in developing this final version.
Conflicts of Interest
Dr. Bitton is senior adviser for the Comprehensive Primary Care Initiative at the Center for Medicare and Medicaid Innovation (CMMI). (The views expressed do not reflect the official views of CMS or CMMI). There are no other conflicts of interest among the authors.
* ACLGIM Writing Group Members (in addition to those listed above) include: Sara Poplau, BA, Minneapolis Medical Research Foundation, Minneapolis, MN; Anuradha Paranjape, MD, MPH, Temple University School of Medicine, Philadelphia, PA; Michael Landry, MD, MSc, New Orleans VAMC and Tulane University, New Orleans, LA; Stewart Babbott, MD, University of Kansas, Kansas City, KS; Tracie Collins, MD, MPH, Department of Preventive Medicine and Public Health, University of Kansas, Wichita, KS; T. Shawn Caudill, MD, MSPH, University of Kentucky, Lexington, KY; Arti Prasad, MD, and Allen Adolphe, MD, PhD, University of New Mexico, Albuquerque, NM; David E. Kern, MD, MPH, Johns Hopkins University School of Medicine, Baltimore, MD; KoKo Aung, MD, MPH, University of Texas Health Science Center at San Antonio, San Antonio, TX; Katherine Bensching, MD, Oregon Health Sciences University, Portland, OR; Kathleen Fairfield, MD, MPH, DrPH, Maine Medical Center, Portland, ME, and the Association of Chiefs and Leaders in General Internal Medicine (ACLGIM), Alexandria, VA.
- Open access
- Published: 06 March 2022
Association between primary care appointment lengths and subsequent ambulatory reassessment, emergency department care, and hospitalization: a cohort study
- Kristi M. Swanson 1 na1 ,
- John C. Matulis III 2 na1 &
- Rozalina G. McCoy 2 , 3
BMC Primary Care volume 23 , Article number: 39 ( 2022 ) Cite this article
4257 Accesses
2 Citations
11 Altmetric
Metrics details
To meet increasing demand, healthcare systems may leverage shorter appointment lengths to compensate for a limited supply of primary care providers (PCPs). Limiting the time spent with patients when evaluating acute health needs may adversely affect quality of care and increase subsequent healthcare utilization; however, the impact of brief duration appointments on healthcare utilization in the United States has not been examined. This study aimed to assess for potential inferiority of shorter (15-min) primary care appointments compare to longer (≥ 30-min appointments) with respect to downstream healthcare utilization within 7 days of the initial appointment.
We performed a retrospective cohort study using electronic health record (EHR), billing, and administrative scheduling data from five primary care practices in Midwest United States. Adult patients seen for acute Evaluation & Management visits between 10/1/2015 and 9/30/2017 were included. Patients scheduled for 15-min appointments were propensity score matched to those scheduled for ≥ 30-min. Multivariate regression models examined the effects of appointment length on repeat primary care visits, emergency department (ED) visits, hospitalizations, and diagnostic services within 7 days following the visit. Models were adjusted for baseline patient, visit, and provider characteristics. A non-inferiority approach was employed.
We identified 173,758 total index visits (6.5% 15-min, 93.5% ≥ 30-min). 11,222 15-min appointments were matched to a comparable ≥ 30-min visit. Longer appointments were more frequent among trainee physicians, patients with limited English proficiency, and patients with more comorbidities. There was no significant effect of scheduled appointment length on the incidence of repeat primary care visits (OR = 0.983, CI: 0.873, 1.106) or ED visits (OR = 0.856, CI: 0.700, 1.047). Shorter appointments were associated with lower rates of subsequent hospitalizations (OR = 0.689, CI: 0.504, 0.941), laboratory services (OR = 0.682, CI: 0.643, 0.724), and diagnostic imaging services (OR = 0.499, CI: 0.466, 0.534). None of the non-inferiority thresholds were exceeded.
Conclusions
For select indications and select low risk patients, shorter duration appointments may be a non-inferior option for scheduling of patient care that will not result in greater downstream healthcare utilization. These findings can help inform healthcare delivery models and triage processes as health systems and payers re-examine how to best deliver care to growing patient populations.
Peer Review reports
A robust primary care infrastructure is foundational for individual and population health [ 1 ]. The growing shortage of primary care providers (PCPs) impedes timely and effective management of acute and chronic health conditions, delivery of essential preventive services, and careful stewardship of healthcare resources [ 1 , 2 ]. It also threatens future progress in caring for an aging population [ 3 , 4 , 5 ]. This shortage is driven, in part, by increasing demands for PCP services, fueled by population growth, increasing prevalence of chronic health conditions, and falling rates of the uninsured [ 6 , 7 , 8 ]. Furthermore, alternative payment models place greater responsibility on primary care practices to complete work outside the traditional purview of primary care, including population health management and care coordination [ 9 , 10 ].
To improve healthcare access for growing patient populations and maximize revenue generation in a fee-for-service environment, many healthcare systems have introduced shorter appointment lengths (e.g., 15-min in duration) into scheduling templates, seeking to maximize the number of patients seen on a given day [ 11 , 12 ]. While shorter appointment lengths do allow more patients to be seen in a given day, allocating valuable clinician time in standardized, brief increments may not effectively meet patient needs, resulting in incomplete or incorrect diagnostic evaluations, poor patient experience, and potentially avoidable downstream healthcare utilization [ 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 ]. Despite scheduled appointment lengths getting shorter, the time required to care for increasingly complex patients and comply with growing regulatory and documentation requirements has been increasing. A National Ambulatory medical survey suggested that physician reported time spent directly with patients had lengthened by an average of 2.4 min between 2008 and 2015, raising the question of what amount of time is needed for clinicians to provide satisfactory care [ 12 , 21 ].
Although there is no consensus on what constitutes “adequate time” with a clinician, shorter visits may be inadequate to effectively address patient concerns and also manage chronic health conditions, deliver necessary preventive services, and interact with the electronic health record (EHR) [ 13 , 14 , 22 , 23 , 24 , 25 , 26 , 27 ]. Prior work in evaluating the effects of appointment length on healthcare utilization is sparse, often conflicting, and dated [ 28 , 29 , 30 , 31 , 32 , 33 ]. When shorter duration visits are employed, the quality of care rendered is uncertain and rarely rigorously evaluated in the primary care setting. Wilson et al. performed two separate systematic reviews, noting that shorter appointment lengths were associated with missing patient care elements among British General Practitioners [ 29 , 32 ]. The impact of shorter duration primary care office visits on subsequent healthcare utilization in the United States has not been examined.
A more nuanced assessment of the value of different duration appointment lengths in primary care is needed as health systems and payers re-examine how to best deliver care to complex patient populations. Using data from an integrated healthcare delivery system in the Midwestern United States, we aimed to assess for potential inferiority of short (15-min) appointment lengths in the primary care setting compared to longer (≥ 30-min or greater) appointments by examining downstream healthcare utilization including return office visits, emergency department and hospital utilization and diagnostic testing in the 7 days following the initial appointment. Results of this study will help inform healthcare delivery models and the appropriateness of using shorter appointment slots in the primary care setting.
Study design & setting
We performed a retrospective cohort study using EHR, billing, and administrative scheduling data from Mayo Clinic, Rochester, Minnesota, U.S.A. Mayo Clinic is an integrated healthcare delivery system that serves local, regional, national, and international patients. The five primary care practices of Mayo Clinic Rochester reside in both urban and rural areas and are comprised of family medicine, internal medicine, and pediatrics specialties that care for over 150,000 local residents, Mayo Clinic employees, and their dependents. PCPs in these practices include attending physicians, trainees in medical education programs (residents and fellows), nurse practitioners (NPs), and physician assistants (PAs). This study was approved by Mayo Clinic’s Institutional Review Board.
Study population
We identified acute outpatient office (“index”) visits among adults (age ≥ 18 years) in the community internal medicine (CIM) and family medicine (FM) practices of Mayo Clinic, Rochester between 10/1/2015 and 9/30/2017. Patients were required to be empaneled to a Mayo Clinic PCP for at least one year prior to the index visit and for 30 days following (to allow for ascertainment of baseline characteristics and utilization outcomes). Index visits were first identified using Current Procedural Terminology (CPT) codes for office or other outpatient evaluation and management (E&M) visits (99201–99215, 99241–99245) and did not include preventive medicine, case or care management services, special evaluations, advanced care planning, or services performed outside the office setting. Index visits were then merged with administrative scheduling data to determine the allotted appointment time.
To ensure visits were for a new chief complaint, we excluded visits that were preceded by another eligible E&M visit in primary care within the previous two weeks. Visits for preventive services only or with non-PCP providers (e.g., nurse, dietician, social worker, etc.) were excluded from analyses, as were visits where the scheduled appointment length could not be determined. Patients who did not provide research authorization were excluded in accordance with Minnesota state law [ 34 ].
Explanatory variable
The exposure of interest was the scheduled appointment length of the index visit. Appointment lengths were ascertained from administrative scheduling data and categorized as 15-min versus ≥ 30-min. Appointment lengths are determined by centralized scheduling staff members using standardized templates based on the patient’s stated health concern and patient characteristics (see Additional file 1 ); the vast majority of appointments are either 15 or 30 min, but 45-min appointments are available for patients new to the practice and those requiring interpreter services. Because only 2.3% of longer appointments were 45 min long, they were grouped together with the 30-min appointments. Schedulers may substitute their own judgement and schedule 15-min concerns into longer appointment slots. Additionally, providers can request that concerns normally scheduled in a longer appointment be placed into a 15-min slot based on their calendar availability. As such, there is substantial overlap of clinical conditions and contexts that may be seen in either 15-min or 30-min time slots.
Independent variables
Covariates of interest included patient, visit, and provider level characteristics. Patient characteristics were extracted from the EHR and included age, ethnicity, race, gender, marital status, and geographic location. Marital status was included as a proxy for social support. Limited English proficiency was identified using the language preference recorded in the patient’s registration data. The Deyo adaptation of the Charlson comorbidity index with incorporated severity weighting was calculated using ICD-9/ICD-10 diagnosis codes from billing data [ 35 , 36 , 37 ]. Prior healthcare utilization, measured by the number of emergency department (ED) visits and hospitalizations in the prior year, was also obtained for each index visit.
Visit and provider information included the specialty area of the appointment (FM vs. CIM), the type of provider seen (physician, NP/PA, or trainee physician), and the specific clinic site where care was sought. The chief complaint for the visit was obtained using the primary diagnosis from billing data and was summarized using the clinical classification software refined (CCSR) multi-level categories [ 38 ].
Outcomes of interest were assessed within 7 days following the index visit and included outpatient office visits in primary care (referred to as repeat visits), ED visits, hospitalizations, laboratory services, and diagnostic imaging services. Repeat visits were identified using similar methodology to that of the index visit, but without examination of the two weeks prior. ED visits were identified using CPT codes (99281–99288). Laboratory and diagnostic imaging services were identified using revenue center codes (i.e., codes used to identify accommodation or ancillary services), and in some instances, a combination of revenue center and CPT codes (see Additional file 2 ). To account for the fact that diagnostic services may, in some instances, be ordered and conducted ahead of the scheduled appointment, we performed a sensitivity analysis excluding laboratory or imaging services rendered on the same day as the index appointment.

Adjustment for differences between groups
We anticipated that certain factors would be influential in determining whether a patient gets scheduled for a 15-min versus ≥ 30-min appointment. These would include patient level factors (medical complexity, social support, utilization patterns) and system factors (triage factors, access to care). For this reason, we implemented propensity score matching to account for potential selection bias in the exposure of interest. Full details regarding the propensity score matching approach used are provided in Additional file 3 .
Statistical analysis
Patient, visit, and provider characteristics were compared using standardized differences as opposed to p-values, as examination of standardized differences is a more appropriate method for determining balance across matched groups that is not influenced by reductions in sample size due to matching [ 39 ]. Crude outcome rates were compared within our matched population using McNemar’s test for paired data.
Multivariate regression models were used to examine the effects of appointment length on each of the outcomes of interest, while adjusting for important confounding variables not used as part of the matching process. We used conditional logistic regression methods to account for the matched nature of the data. Confounding factors included the ethnicity, race, gender, and marital status of the patient, as well as prior healthcare utilization. We reported multivariate regression results in the form of odds ratios and 95% confidence intervals.
To assess non-inferiority of shorter appointment lengths, we a priori defined a non-inferiority threshold of 10% increased likelihood (Odds Ratio [OR] of 1.1) of subsequent ED and hospital visits and a threshold of 20% (OR of 1.2) increased likelihood of repeat visits, laboratory services, and diagnostic imaging services. In essence, we are willing to accept a higher likelihood of subsequent utilization for those with shorter appointments so long as the increased rate does not exceed our defined non-inferiority threshold. We used the upper limits of the 95% confidence intervals as a boundary for assessing non-inferiority and compared this value to the corresponding non-inferiority threshold. All data management and analyses were carried out using SAS 9.4 (SAS Institute Inc. Cary, NC).
We identified 173,758 eligible acute care visits to primary care during the study period. Shorter (15-min) appointments accounted for 6.5% ( N = 11,222) of the visits, while appointments scheduled for ≥ 30-min comprised 93.5% ( N = 162,536). Prior to matching, the majority (63.8%) of 15-min appointments were scheduled in the FM practice, while longer appointments were more evenly distributed between the practice areas (52.1% in FM and 47.9% in CIM) (Table 1 ). Longer appointments were more frequently scheduled with trainee physicians and for patients with limited English proficiency and a higher number of comorbidities. Visits with chief complaints related to congenital anomalies, mental illness, blood diseases, the circulatory system, digestive system, or musculoskeletal system, as well as endocrine or metabolic diseases, immunity disorders, injuries, and ill-defined conditions were more likely to have a longer appointment scheduled.
We matched 11,222 15-min appointments to a comparable ≥ 30-min appointment visit, resulting in a final matched cohort of N = 22,444 visits. After performing one-to-one propensity score matching, substantial balance was achieved between the two groups, with all match characteristics having a standardized difference below 5% (Table 1 ). Differences in additional baseline demographic characteristics not used as part of the matching process also substantially improved after matching.
There were no significant differences in the crude rates of repeat acute care visits between the appointment length groups (Table 2 ). Shorter appointment lengths had a lower rate of 7-day ED visits (1.8% vs. 2.2%, p = 0.03) and hospitalizations (0.7% vs. 1.0%, p < 0.01) compared to longer appointment lengths. Longer appointments were also followed by higher rates of laboratory (38.3% vs. 30.5%, p < 0.001) and diagnostic imaging services (28.2% vs. 17.2%, p < 0.001). These findings held true when excluding same day diagnostic services as part of our sensitivity analyses (see Additional file 4 , Tables D5 and D7).
Multivariate analyses showed no significant effect of scheduled appointment length on repeat visits (OR = 0.983, CI: 0.873,1.106) or ED visits (OR = 0.856, CI: 0.700, 1.047) (Fig. 1 ). Indeed, the strongest risk factor for repeat visits and subsequent ED visits was a history of greater ED utilization in the 6 months prior to the index visit (see Additional File 4 , Tables D1-D2). Shorter appointment lengths were associated with a lower likelihood of subsequent hospitalizations (OR = 0.689, CI: 0.504, 0.941), laboratory services (OR = 0.682, CI: 0.643, 0.724), and diagnostic imaging services (OR = 0.499, CI: 0.466, 0.534) compared to longer appointment lengths (Fig. 2 ). Female patients were more likely to have subsequent laboratory services compared to male patients (OR = 1.296, CI: 1.184, 1.419) (see Additional file 4 , Tables D3-D7). No other measures were significantly associated with our outcomes of interest.
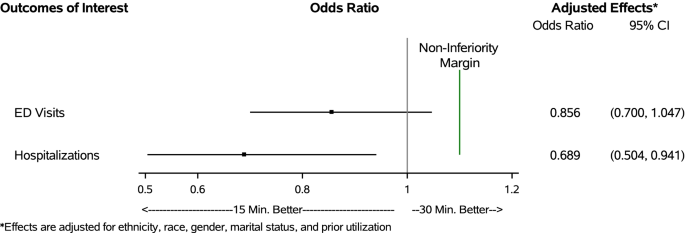
Effect of primary care appointment length on ED visits and hospitalizations within 7 days of the index appointment
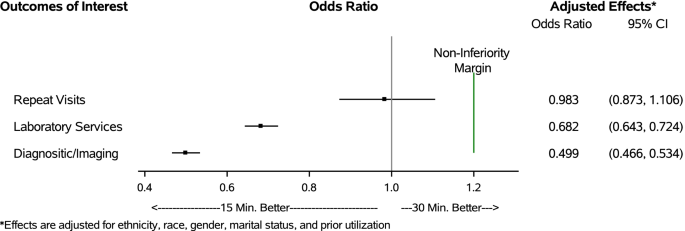
Effect of primary care appointment length on repeat visits, diagnostic laboratory, and imaging services obtained within 7 days of the index appointment
None of the upper confidence limits for repeat visits (UCL = 1.106), laboratory services (UCL = 0.724), and diagnostic imaging services (UCL = 0.534) exceeded the non-inferiority threshold of an OR of 1.2 (i.e., 20% higher likelihood) (Fig. 2 ). Similarly, the upper confidence limits for subsequent ED visits (UCL = 1.047) and hospitalizations (UCL = 0.941) fell below the non-inferiority threshold of an OR of 1.1 (i.e., 10% higher likelihood) (Fig. 1 ). These findings indicate that shorter scheduled appointments are non-inferior to longer scheduled appointments for all primary study outcomes.
Real-time evaluation of practice changes to assess for unanticipated and undesired outcomes is necessary to ensure that care delivery is safe, timely, effective, equitable, efficient and patient-centered [ 40 ]. Our study aimed to fill a critical knowledge gap by assessing whether 15-min primary care appointments represent a non-inferior option to traditional 30-min or longer appointments with respect to need for repeat primary care visits, ancillary diagnostic studies (laboratory and imaging tests), and ED visits and hospitalizations. We found that when propensity score matched on important patient and visit characteristics, patients seen for 15-min appointments did not incur greater healthcare utilization within seven days of the index visit, demonstrating that shorter appointments may provide a non-inferior option for scheduling when used for carefully selected patient populations.
Ideally, primary care appointments would allow for enough time to successfully complete all necessary clinical and ancillary tasks without shifting care to later appointments or generating unnecessary diagnostic testing or referrals. While the time required to complete all tasks associated with a comprehensive primary care appointment is increasing, healthcare organizations may be pressured to limit appointment durations to maximize access and reimbursement. Our findings suggest that for carefully selected patients with low-risk visit indications—the situations where these appointments were being used—shorter appointment lengths do not result in greater down-stream healthcare utilization. However, as only a small number of total primary care appointments in our study period were of shorter length and were focused on simpler chief complaints and lower risk patients, our findings should not be generalized to higher risk patients or chief complaints that were excluded from the comparisons during matching. Thus, changes to scheduling standards should be considered with caution to avoid potential oversaturation of shorter appointments within provider calendars, which could limit their ability to effectively manage patients scheduled on a given day.
Prior work in evaluating appointment lengths has found an association between increasing appointment lengths and improved quality of care indicators, better counseling or screening, higher patient satisfaction, and lower risk of malpractice suits, as longer appointments allow adequate time to perform comprehensive services [ 11 , 20 ]. Similarly, other retrospective work found that shorter appointment lengths are associated with incomplete visit tasks and higher medication prescribing, serving as a surrogate for lower value care, albeit much of this work was completed outside of the United States [ 30 , 32 , 41 , 42 ]. Our study built on these findings to offer reassurance that for select lower risk conditions and patients, shorter appointment lengths do not necessarily translate to greater total healthcare utilization secondary to incomplete or incorrect diagnostic evaluations. However, we did not consider whether longer appointments were more conducive to addressing health maintenance and preventive health needs; while this is not indicative of suboptimal care for the acute condition serving as the chief complaint, it nevertheless reflects missed opportunities to deliver care and improve long-term health outcomes.
To our knowledge, this is the first contemporary study to examine the impact of scheduled appointment lengths on subsequent healthcare utilization in the general primary care population in the United States. It was made uniquely possible by linking EHR data, which spans the outpatient and inpatient settings, to administrative scheduling data, which allowed us to examine healthcare utilization and outcomes for a diverse population of primary care patients. Our analyses are further enhanced by the use of administrative scheduling data, which includes the actual durations allotted to specific appointments, rather than CPT codes, which are imperfect surrogates of time spent on patient care and do not necessarily reflect the time allotted for the care that was performed. As part of a regionally dominant, integrated healthcare system we suspect there is very little leakage of down-stream care to other healthcare systems unable to be captured in our data. The five included clinics represented both urban and rural settings, patients were seen in teaching and non-teaching clinics, and a variety of practice styles and clinic level resources were available across the different sites, increasing the generalizability of our findings.
While informative, this study is subject to some limitations. Because this is an observational study using secondary data analysis approaches, we are limited to describing associations present in the data and cannot make causal inferences. To minimize the impact of this limitation, we utilized propensity score matching, which is a common approach to address underlying confounding and selection bias to estimate causal effects. However, because propensity score matching relies on observable data and administrative data alone cannot fully capture patient and care complexity and key social determinants of health, there may be residual bias in our study, resulting in some populations not being matched and included in our outcomes assessments. Thus, there may be important subgroups of patients, particularly those with multiple chronic conditions, patients with limited English proficiency who require interpreter services, patients with psychosocial barriers to health and healthcare, and those seen by trainee clinicians, for whom longer appointments may remain the superior option for scheduling. Additionally, care managed through email, phone calls, patient portals, and telemedicine is not represented in our study. Therefore, inferences of this study are only generalizable to face-to-face visits with the potential to be scheduled at a 15-min interval.
Further research in this area is needed to comprehensively understand how appointment scheduling approaches impact the clinical experience. While we showed non-inferiority of shorter appointments in this population as it relates to subsequent healthcare utilization, the association of appointment lengths with patient satisfaction, chronic disease outcomes, and measures of physician burnout are less clear [ 20 ]. Investigation into the value of using more patient and physician centered scheduling templates may represent another research area of opportunity.
Understanding how primary care appointment lengths impact downstream care and utilization may be of significant value to clinicians, practice administrators, quality improvement professionals, payers, and health policy experts. This study investigated the association of scheduled appointment length on repeat visits and diagnostic testing services rendered within the 7 days following the appointment and demonstrated that under the specific circumstances being considered, shorter appointment lengths, in carefully selected patients and carefully selected conditions may be adequate to meet patient needs. These findings can be used to improve healthcare delivery models and triage processes to provide higher quality and more efficient care, while aiming to reduce low-value healthcare utilization.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to inclusion of protected health information but can be made available subsequent to de-identification upon reasonable request.
Abbreviations
Primary care providers
Electronic health record
Nurse practitioners
Physician assistant
Community internal medicine
Family medicine
Current procedural terminology
Evaluation and management
Emergency department
Clinical classification software refined
Upper confidence limit
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Implementing High-Quality Primary Care. Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care. Robinson SK, Meisnere M, Phillips RL Jr, McCauley L, editors. Washington (DC): National Academies Press (US); 2021.
Association of American Medical Colleges. The Complexities of Physician Supply and Deman: Projections From 2019 to 2034. Washington, DC: AAMC; 2021.
Google Scholar
Zhang X, Lin D, Pforsich H, Lin VW. Physician workforce in the United States of America: forecasting nationwide shortages. Hum Resour Health. 2020;18(1):8.
Article Google Scholar
Bodenheimer T, Chen E, Bennett HD. Confronting the growing burden of chronic disease: can the US health care workforce do the job? Health Aff. 2009;28(1):64–74.
Colwill JM, Cultice JM, Kruse RL. Will generalist physician supply meet demands of an increasing and aging population? Health Aff (Millwood). 2008;27(3):w232–41.
Linda A, Jacobsen, et al. “America’s Aging Population,” Population Bulletin. 2011;66(1).
Vincent GK, Velkoff VA. The next four decades: the older population in the United States: 2010 to 2050. Washington: Census Bureau(Current Population Report); 2010.
Truglio J, Graziano M, Vedanthan R, Hahn S, Rios C, Hendel-Paterson B, et al. Global health and primary care: increasing burden of chronic diseases and need for integrated training. Mount Sinai Journal of Medicine: A Journal of Translational and Personalized Medicine. 2012;79(4):464–74.
Collins S, Piper KB, Owens G. The opportunity for health plans to improve quality and reduce costs by embracing primary care medical homes. Am Health Drug Benefits. 2013;6(1):30–8.
PubMed PubMed Central Google Scholar
Rittenhouse DR, Shortell SM, Fisher ES. Primary care and accountable care–two essential elements of delivery-system reform. N Engl J Med. 2009;361(24):2301–3.
Article CAS Google Scholar
Chen LM, Farwell WR, Jha AK. Primary care visit duration and quality: does good care take longer? Arch Intern Med. 2009;169(20):1866–72.
Mechanic D, McAlpine DD, Rosenthal M. Are patients’ office visits with physicians getting shorter? N Engl J Med. 2001;344(3):198–204.
Linzer M, Poplau S, Babbott S, Collins T, Guzman-Corrales L, Menk J, et al. Worklife and wellness in academic general internal medicine: results from a national survey. J Gen Intern Med. 2016;31(9):1004–10.
Linzer M, Bitton A, Tu SP, Plews-Ogan M, Horowitz KR, Schwartz MD, et al. The end of the 15-20 minute primary care visit. J Gen Intern Med. 2015;30(11):1584–6.
Erickson SM, Rockwern B, Koltov M, McLean RM. Putting patients first by reducing administrative tasks in health care: a position paper of the American College of Physicians. Ann Intern Med. 2017;166(9):659–61.
Bodenheimer T, Pham HH. Primary care: current problems and proposed solutions. Health Aff. 2010;29(5):799–805.
Rabin RC. 15-Minute doctor visits take a toll on patient-physician relationships. https://www.pbs.org/newshour/health/need-15-minutes-doctors-time .Published April 21, 2014.
DiMatteo MR. The physician-patient relationship: effects on the quality of health care. Clin Obstet Gynecol. 1994;37(1):149–61.
Pronovost P. How the 15-minute Doctor's Appointment Hurts Health Care.: The Wall Street Journal; 2016 [Available from: https://blogs.wsj.com/experts/2016/04/15/how-the-15-minute-doctors-appointment-hurts-health-care/ .
Dugdale DC, Epstein R, Pantilat SZ. Time and the patient-physician relationship. J Gen Intern Med. 1999;14(Suppl 1):S34-40.
Rao A, Shi Z, Ray KN, Mehrotra A, Ganguli I. National Trends in Primary Care Visit Use and Practice Capabilities, 2008–2015. The Annals of Family Medicine. 2019;17(6):538–44.
Berra K, Hughes S. Counseling patients for lifestyle change: making a 15-minute office visit work. Menopause. 2015;22(4):453–5.
Fiscella K, Epstein RM. So much to do, so little time: care for the socially disadvantaged and the 15-minute visit. Arch Intern Med. 2008;168(17):1843–52.
Yarnall KS, Pollak KI, Østbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003;93(4):635–41.
Geraghty EM, Franks P, Kravitz RL. Primary care visit length, quality, and satisfaction for standardized patients with depression. J Gen Intern Med. 2007;22(12):1641–7.
Bodenheimer T. Coordinating care--a perilous journey through the health care system. N Engl J Med. 2008;358(10):1064-71.
Arndt BG, Beasley JW, Watkinson MD, Temte JL, Tuan W-J, Sinsky CA, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. The Annals of Family Medicine. 2017;15(5):419–26.
Elmore N, Burt J, Abel G, Maratos FA, Montague J, Campbell J, et al. Investigating the relationship between consultation length and patient experience: a cross-sectional study in primary care. Br J Gen Pract. 2016;66(653):e896–903.
Wilson A, Childs S. The relationship between consultation length, process and outcomes in general practice: a systematic review. Br J Gen Pract. 2002;52(485):1012–20.
Cape J. Consultation length, patient-estimated consultation length, and satisfaction with the consultation. Br J Gen Pract. 2002;52(485):1004–6.
Wilson A. Extending appointment length–the effect in one practice. J R Coll Gen Pract. 1989;39(318):24–5.
CAS PubMed PubMed Central Google Scholar
Wilson A, Childs S. The effect of interventions to alter the consultation length of family physicians: a systematic review. Br J Gen Pract. 2006;56(532):876–82.
Carr-Hill R, Jenkins-Clarke S, Dixon P, Pringle M. Do minutes count? Consultation lengths in general practice. J Health Serv Res Policy. 1998;3(4):207–13.
Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ 3rd. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87(12):1202–13.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Clinical Classifications Software Refined (CCSR). Healthcare Cost and Utilization Project (HCUP). October 2021. Agency for Healthcare Research and Quality, Rockville, MD. www.hcupus.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp .
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–107.
Institute of Medicine (US) Committee on Quality of Health Care in America. rossing the Quality Chasm: A New Health System for the 21st Century. Washington: National Academies Press (US); 2001.
Deveugele M, Derese A, van den Brink-Muinen A, Bensing J, De Maeseneer J. Consultation length in general practice: cross sectional study in six European countries. BMJ. 2002;325(7362):472.
Jin G, Zhao Y, Chen C, Wang W, Du J, Lu X. The length and content of general practice consultation in two urban districts of Beijing: A preliminary observation study. PLoS ONE. 2015;10(8):e0135121.
Download references
Acknowledgements
Not applicable
This effort was funded in part by the National Institute of Health (NIH) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grant number K23DK114497 and a Mayo Clinic Division of Community Internal Medicine Time for Scholarly Activity Award.
Author information
Kristi M. Swanson and John C. Matulis III contributed equally to this work.
Authors and Affiliations
Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery, Mayo Clinic, Rochester, USA
Kristi M. Swanson
Division of Community Internal Medicine, Department of Medicine, Mayo Clinic, Rochester, USA
John C. Matulis III & Rozalina G. McCoy
Division of Health Care Delivery Research, Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery, Mayo Clinic, Rochester, USA
Rozalina G. McCoy
You can also search for this author in PubMed Google Scholar
Contributions
R.G.M. and K.M.S. conceived of the idea and developed the study design. R.G.M. supervised the project. J.C.M. provided critical clinical practice expertise. K.M.S. was responsible for data acquisition and analysis. R.G.M. and K.M.S. interpreted the data. K.M.S. and J.C.M. wrote the manuscript with critical revisions/editing from R.G.M. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Kristi M. Swanson .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was obtained from the Mayo Clinic Institutional Review Board. The Mayo Clinic Institutional Review Board granted a waiver of informed consent as the study involved no more than minimal risk to study subjects, there was no planned intervention or direct contact/communication with study participants, as such the waiver did not adversely affect the rights and welfare of the subjects, and the study only included patients who provided authorization for their medical records to be used for research purposes. All research methods used to conduct this study were performed in accordance with the guidelines of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
In the last 36 months, Dr. McCoy also received support from NIDDK (R03DK127010; P30DK111024) and AARP® (Quality Measure Innovation Grant), as well as served as a Data Safety and Monitoring Board member (Entolimod Study CBLB502; study PI: Robert Pignolo, MD, PhD [Mayo Clinic]). Dr. Matulis and Mrs. Swanson declare that they have no other conflicts of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Scheduling Template . Standardized scheduling template used by centralized scheduling staff members when assigning appointment lengths.
Additional file 2.
Billing Codes Used to Define Outcomes of Interest . Billing code rules used to identify laboratory and diagnostic imaging services outcomes.
Additional file 3.
Technical Appendix – Propensity Score Matching. A detailed summary of the methods used to carry out the propensity score matching approach.
Additional file 4.
Full Regression Model Results . A full summary of regression model estimates for each of the outcomes of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Swanson, K.M., Matulis, J.C. & McCoy, R.G. Association between primary care appointment lengths and subsequent ambulatory reassessment, emergency department care, and hospitalization: a cohort study. BMC Prim. Care 23 , 39 (2022). https://doi.org/10.1186/s12875-022-01644-8
Download citation
Received : 24 August 2021
Accepted : 08 February 2022
Published : 06 March 2022
DOI : https://doi.org/10.1186/s12875-022-01644-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Schedules and Appointments
- Primary Care
- Practice Patterns
- Healthcare Utilization
- Quality of Healthcare
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
- Article Information
Adult primary care visit duration (1997-2005). For all visits, P < .001 for trend. For general medical examination visits, P = .02 for trend.
Visit duration for 4 common primary diagnoses (1997-2005). P values for trend were P = .002 for diabetes, P < .001 for essential hypertension, P < .001 for arthropathies, and P = .05 for spinal disorders. Arthropathies include most visits for joint discomfort such as those for gout, osteoarthritis, and rheumatoid arthritis. Spinal disorders primarily include visits for low back pain.
Comparison of the early period (1997-2001) vs the late period (2002-2005). A, Change in medication quality indicator performance over time. P > .05 for all medication indicators except angiotensin-converting enzyme inhibitor or angiotensin receptor blocker for congestive heart failure (ACEI/ARB for CHF) ( P = .04), treatment for atrial fibrillation (Rx for Afib) ( P = .002), β-blocker (BB) or diuretic for hypertension (HTN) ( P < .001), and BB for coronary artery disease (CAD) ( P = .006). B, Change in counseling or screening quality indicator performance over time. P > .05 for all counseling or screening quality indicators except blood pressure check ( P < .001).
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Chen LM , Farwell WR , Jha AK. Primary Care Visit Duration and Quality : Does Good Care Take Longer? Arch Intern Med. 2009;169(20):1866–1872. doi:10.1001/archinternmed.2009.341
Manage citations:
© 2024
- Permissions
Primary Care Visit Duration and Quality : Does Good Care Take Longer?
Author Affiliations: Massachusetts Veterans Epidemiology Research and Information Center, Veterans Affairs Boston Healthcare System (Drs Chen, Farwell, and Jha), and Divisions of Aging (Dr Farwell) and General Internal Medicine (Dr Jha), Brigham and Women's Hospital and Harvard Medical School, and Department of Health Policy and Management, Harvard School of Public Health (Dr Jha), Harvard University, Boston, Massachusetts. Dr Chen is now with the Division of General Medicine, University of Michigan Health System, Ann Arbor.
Background It is unclear if increasing pressure on primary care physicians to be more efficient has affected visit duration or quality of care. We sought to describe changes in the duration of adult primary care visits and in the quality of care provided during these visits and to determine whether quality of care is associated with visit duration.
Methods We conducted a retrospective analysis of visits by adults 18 years or older to a nationally representative sample of office-based primary care physicians in the United States.
Results Between 1997 and 2005, US adult primary care visits to physicians increased from 273 million to 338 million annually, or 10% on a per capita basis. The mean visit duration increased from 18.0 to 20.8 minutes ( P < .001 for trend). Visit duration increased by 3.4 minutes for general medical examinations and for the 3 most common primary diagnoses of diabetes mellitus (4.2 minutes, P = .002 for trend), essential hypertension (3.7 minutes, P < .001 for trend), and arthropathies (5.9 minutes, P < .001 for trend). Comparing the early period (1997-2001) with the late period (2002-2005), quality of care improved for 1 of 3 counseling or screening indicators and for 4 of 6 medication indicators. Providing appropriate counseling or screening generally took 2.6 to 4.2 minutes. Providing appropriate medication therapy was not associated with longer visit duration.
Conclusions Adult primary care visit frequency, quality, and duration increased between 1997 and 2005. Modest relationships were noted between visit duration and quality of care. Providing counseling or screening required additional physician time, but ensuring that patients were taking appropriate medications seemed to be independent of visit duration.
Two of the most pressing goals for the US health care system are to deliver higher-quality care and to lower costs. 1 Primary care physicians (through care provided during ambulatory care visits) have been charged with meeting both of these goals even as their patient population has grown older and more complex. Furthermore, after adjusting for inflation, net income for primary care physicians dropped by 10.2% between 1995 and 2003. 2 Given the reimbursement environment and the pressures to improve efficiency, one might worry that primary care physicians would respond by spending less time with each patient to see more patients, improve their efficiency, and boost their incomes. Such practices could potentially adversely affect the quality of care provided.
Past work suggests that significant investments of primary care physician time may be required to deliver high-quality care. Results of previous studies suggest that it would take at least 7.4 to 10.6 hours per workday to deliver recommended care to a typical panel of primary care patients 3 , 4 and that greater patient satisfaction is associated with perceived and actual visit duration. 5 , 6 Other investigators have shown that a poor provider relationship may lead to greater medication nonadherence, 7 which is likely to require provider time to remedy. Together, findings from these studies raise questions about whether efforts to improve efficiency might have a detrimental effect on quality of care at the visit level.
At the visit level nationwide, we know little about whether primary care physicians are spending more or less time with patients than they were in the past and about whether visits that provide evidence-based care take more time. Therefore, we sought to answer the following 3 questions: (1) Has the duration of adult primary care office visits in the United States decreased over the last decade? (2) Which patient or physician characteristics are associated with shorter or longer office visits? (3) Is visit duration associated with the quality of care provided during ambulatory care visits to primary care physicians in the United States?
We used the National Ambulatory Medical Care Survey (NAMCS), a US representative survey administered by the National Center for Health Statistics. We supplemented these data with population estimates from the US Census Bureau. 8 , 9 The NAMCS uses a 3-stage sampling design to collect information on visits to non–federally funded office-based physicians throughout the United States. The sampling is based on geographic location, physician practices by specialty in specified geographic regions, and visits within individual physician practices. The National Center for Health Statistics weights each visit to account for (1) probability of selection, (2) nonresponders, (3) number of physicians in each specialty, and (4) extreme values. The weighting permits extrapolation to national estimates.
Patient, physician, and clinical information is recorded by participating physicians, office staff, or US Census Bureau representatives. Clinical characteristics include the following: (1) up to 3 reasons for the visit (coded using the reason-for-visit classification), (2) 3 diagnoses coded using the International Classification of Diseases, Ninth Revision, Clinical Modification ( ICD-9-CM ), and (3) since 2003 up to 8 drugs (≤6 drugs for 1995-2002) coded using a unique National Center for Health Statistics–assigned 5-digit code. These include prescription and over-the-counter drugs, and they must be ordered, supplied, administered, or continued during the visit. Duration of the office visit is reported by physicians, office staff, or US Census Bureau representatives and is defined as the time spent by the patient with the physician. A complete description of the visit duration variable is included in an appendix that is available from the author.
We excluded visits by patients younger than 18 years and visits that did not include time with a provider (5% of all adult visits to primary care providers). We included only visits to general practitioners, family practitioners, or general internists. We created a 9-year sample beginning in 2005 and included the previous 8 years of NAMCS data. We chose this period because it was the length of time for which survey questions about practice ownership and size remained unchanged.
We identified visits that were eligible for at least 1 of 9 validated quality indicators used in previous studies 10 , 11 evaluating NAMCS data. The indicators were placed into 2 categories, namely, medication quality indicators and counseling or screening quality indicators. A complete list of the quality indicators, their eligibility criteria, and clinical actions that allow the indicators to be met 10 , 11 are available in an appendix from the corresponding author.
We calculated the per capita number of adult primary care visits using adult primary care visits as the numerator and using annual US Census population estimates for adults as the denominator. We next examined trends in office visit duration for general medical examination (GME) visits and for all visits from December 30, 1996, through December 25, 2005, using simple linear regression analysis. General medical examination visits were defined as visits with the following: (1) ICD-9-CM code V70.0X or V70.9X (or both), (2) reason-for-visit classification code 31000, or (3) a preventive or non–illness care code as the NAMCS major reason for the visit. As we were concerned that visit duration might have changed over time because of the changing composition of visits, we also chose the 4 most common primary diagnoses for all adult office visits and examined visit duration for these individual conditions over time. The 4 conditions were essential hypertension ( ICD-9-CM code 401), diabetes mellitus ( ICD-9-CM code 250), spinal disorders ( ICD-9-CM codes 720-724), and arthropathies and related disorders ( ICD-9-CM codes 710-719).
To examine whether certain patient or physician characteristics were associated with longer visit duration, we pooled visits across all 9 years of the study period. We used bivariate techniques and multiple linear regression analysis to estimate patient, practice, and physician characteristics associated with visit duration. Our primary outcome was visit duration. Covariates in the multivariate model included patient factors such as sex, new patient (yes or no), visit type (GME or other), insurance (Medicare, private insurance, or other), age (18-35, 36-49, 50-64, 65-75, or ≥76 years), and race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, or other). We also included physician factors such as whether the visit was to a general practitioner or family practitioner or to a general internist, whether the physician practiced solo or was part of a group practice, what US Census region the visit occurred in (Northeast, Midwest, South, or West), whether the metropolitan area of the visit was urban or rural, and whether the practice was physician owned or not. Finally, we included visit year as an indicator variable.
Because of the heterogeneous reasons for the office visits and the high likelihood that the underlying reasons varied by the characteristics enumerated in the previous paragraph, we also examined just GME visits. We built multiple linear regression models and adjusted for each of the characteristics (except whether the visit was for a GME visit or not) to identify independent predictors of longer GME visits.
We next pooled quality performance into 2 periods representing similar total numbers of visits, namely, the early period (1997-2001) and the late period (2002-2005). We used χ 2 tests to determine whether quality of care changed over time.
Finally, to test our hypothesis that providing high-quality care should take more time, we examined the relationship between quality of care and visit duration using bivariate techniques. We then built multiple linear regression models (1 for each quality indicator) in which meeting the quality indicator (yes or no) was the primary predictor and visit duration was the outcome. We included all covariates from the characteristics enumerated, but we modeled age as a continuous predictor and did not include GME visit as a predictor for counseling or screening models. Although we hypothesized that age, sex, race/ethnicity, and new patient status might interact with quality indicator performance, we found little evidence to support these hypotheses. Therefore, we excluded interaction terms in our final models. To account for the probability of a type I error due to multiple testing, we used a Bonferroni-corrected P value (.05/ n , where n indicates 9 quality indicators) to test for significance.
All analyses were performed using commercially available software (SAS version 9.1.3; SAS Institute Inc, Cary, North Carolina; and SAS-callable SUDAAN version 10.0.0; Research Triangle Institute, Research Triangle Park, North Carolina). All P values were 2-tailed, and P < .05 was considered statistically significant (except in the case of multiple comparisons, in which P < .0056 was considered statistically significant).
After excluding visits without physician contact, there were 46 250 adult visits to primary care physicians in the NAMCS database, representing a total of 2.6 billion primary care visits in the United States between 1997 and 2005. The number of annual visits increased from 273 million visits in 1997 to 338 million visits in 2005. Between 1997 and 2005, per capita adult primary care visits increased from 1.4 to 1.5 visits per year. Over the 9-year period, the mean visit duration was 18.9 minutes, and the median visit duration was 15 minutes. Overall sample variability was modest (available in the appendix from the author).
Between 1997 and 2005, the mean duration of an adult primary care visit increased by 16% ( Figure 1 ) from 18.0 to 20.8 minutes ( P < .001 for trend). Visit duration increased comparably across age groups (available in the appendix from the author). The duration of GME visits increased from 21.7 to 25.1 minutes ( P = .02 for trend). Visits also lengthened for patients with the 3 most common primary diagnoses of diabetes mellitus (4.2 minutes, P = .002 for trend), essential hypertension (3.7 minutes, P < .001 for trend), and arthropathies (5.9 minutes, P < .002 for trend) ( Figure 2 ). However, there was substantial variation across years.
Patients seen by general internists had visits that were 1.7 minutes longer than those of patients seen by general practitioners or family practitioners ( Table 1 ). Older patients, new patients, and those in certain regions of the country also had longer visits. Non-Hispanic blacks and Hispanics spent less time with primary care physicians, although this difference reached statistical significance only for GME visits ( P = .01) ( Table 2 ).
Between 1997 and 2005, there were improvements in the proportion of eligible visits meeting 4 of 6 medication quality indicators and meeting 1 of 3 counseling or screening quality indicators ( Figure 3 ). Results were similar when adjusting for differences in demographic characteristics (sex, age, and race/ethnicity) between the 2 periods (early period vs late period). Even in 2002 through 2005, rates of adherence to simple quality metrics were low, with performance below 70% on 7 of 9 measures. Estimates of annual changes in quality indicator performance are available in the appendix from the author.
One of 6 medication quality indicators and all 3 counseling or screening quality indicators were associated with longer visits ( Table 3 ). Appropriately prescribing a β-blocker or diuretic for hypertension was associated with a visit that was 0.7 minutes longer ( P = .03), but this did not meet the Bonferroni-corrected threshold of significance ( P < .0056). Visits that met any of 3 counseling or screening quality indicators were 2.6 to 4.2 minutes longer than eligible visits in which patients did not receive these services ( P < .001 for all).
We found no evidence that primary care physicians, despite decreasing income and increasing pressures for greater efficiency, have responded by shortening the time they spend with their patients. In fact, primary care physicians spent 16% more time during a typical office visit in 2005 compared with 1997. Not surprisingly, older patients or those making their first visit spent more time with the physician. In contrast, primary care physicians spent less time with patients of racial/ethnic minority groups, especially during GME visits. Although quality of care increased concomitantly during this period, we found little evidence that longer visits were associated with better care for medication quality indicators. However, primary care visits in which physicians provided appropriate counseling or screening took longer than visits in which they did not.
It may be surprising that primary care physicians are spending more time with patients. Although it is possible that physicians have become less efficient over time, it is far more likely that visit duration has increased because it takes more resources or time to care for an older and sicker population. 12 - 14 We found that the fraction of older patients increased during this period. However, when we adjusted for changes in demographics, primary care physicians still spent more time with their patients in 2005 than they did in 1997. Other factors such as complexity of illness or a growing emphasis on patient participation in clinical decision making 15 - 17 might have contributed to these increases.
We expected to find that certain factors such as older age or new patient status would be associated with longer visits. However, we were surprised to find that physicians spent less time with black and Hispanic patients than they did with white patients, at least during GME visits. Despite the limitations of our data set to better understand the factors associated with racial/ethnic differences, our findings may explain why patients of minority groups do not always receive care that is comparable to that provided to white patients. 18 Further work to delineate why these differences exist would be helpful.
We found only modest improvements overall in the quality of care that Americans received over this period. Our findings are consistent with those seen in the National Healthcare Quality Report and other national examinations of quality of care. 19 Furthermore, we found no improvements in rates of diet and exercise counseling during the study period, despite evidence of the benefits of these interventions among high-risk patients. Accelerating the pace of improvement may require changes in the way care is provided, including the implementation of systems such as electronic health records with robust clinical decision support, 20 although the adoption of such systems has been slow 21 and evidence is mixed on whether such systems save physician time. 22 - 24
Our findings suggest that the relationship between quality of care and physician visit duration depends on the type of quality indicator being measured, namely, medication quality indicators vs counseling or screening quality indicators. In general, our results support the notion that ensuring that patients are prescribed the appropriate medications need not take more time than allowing their continued use of the wrong medication or ignoring key conditions altogether. Not surprisingly, however, we found a clear and consistent relationship between visit duration and provision of counseling and screening–based care. Providing higher-quality preventive care may require greater reimbursement to account for the additional time spent, for more routine use of alternative strategies such as combining efforts of physician and nonphysician caregivers to maximize the effect of advice, 25 or for the use of Internet-based behavioral counseling and education to modify behavior. 26
Although other investigators have examined visit duration trends 27 in earlier periods and changes in quality of care, 10 we are unaware of other studies that have examined how these 2 pieces fit together for multiple quality indicators in the ambulatory setting. Mechanic et al 27 found that primary care visit duration increased between 1989 and 1998, and Blumenthal et al 12 found that certain characteristics such as age and number of diagnostic tests were associated with longer visits. Ma and Stafford 10 created ambulatory quality indicators using NAMCS data and focused on trends in quality of care through 2002. Our work analyzes more recent data and examines the relationship between the quality of provided care and the time taken to provide that care. In addition, although prior work has documented that it takes time to provide recommended 28 and effective 25 , 29 , 30 counseling, we examined a much broader set of measures through a more contemporary period and linked quality of care to recorded visit duration in a nationally representative data set.
Our study has several limitations. Duration of the outpatient visit was not directly observed but was self-reported by physicians, office staff, or NAMCS field staff. Although a study 31 found that physicians may overestimate the face-to-face time they spend with patients, other factors such as the time physicians spend on other patient-related work may explain some of the gap. 32 Moreover, other investigators have used the NAMCS data to examine national trends in visit duration, 27 and they found that trends in the NAMCS data mirror those in other data sources. Finally, there is no evidence that overestimation of visit duration, if any, has worsened over time. Another limitation is that NAMCS data may inadequately capture patients' complexity and the severity of their illnesses. In sensitivity analyses, we adjusted our results for the number of diagnoses and the number of quality indicators for which patients were eligible and found that our results were qualitatively similar. In addition, our quality measures were limited given that these are visit-based survey data. For example, reporting of over-the-counter medications may be underreported, potentially leading to an underestimate of performance on the quality indicator of antithrombotic treatment for atrial fibrillation (given that aspirin is an effective therapy that may not be captured by NAMCS data). However, these measures have been previously validated 10 and used, 11 and the visits are representative of the care that Americans receive in the ambulatory setting. Finally, we were unable to adjust for 3 factors that might affect our estimates of the association between quality of care and visit duration. First, past work has found that NAMCS data underreport behavioral counseling 31 ; such visit misclassification would lead to an underestimate of the association between visit duration and performance on counseling or screening quality indicators. Second, the most difficult patients tend to take more time than the average patient, 33 and preventive care may get overlooked during these visits. We could not adjust for such patient factors, again potentially biasing our results toward an underestimate of the time that it takes to provide high-quality care. Third, we did not have information about the strength of the patient-physician relationship, potentially leading to an underestimate of the amount of time that it takes to deliver counseling or screening, as familiarity between a patient and physician may increase the likelihood of meeting quality indicators and may shorten the mean visit duration.
In summary, there was a surprising scarcity of recent data on how much time primary care physicians spend with their patients and how this has changed over time. In our study, we found no evidence for the commonly held belief that physicians are spending less time with their patients or that quality of care has diminished. In fact, patients spent more time with their primary care physicians during office visits in 2005 than they did almost a decade earlier, and overall they received better care. On average, older patients, patients of white race/ethnicity, and patients who visited general internists spent more time with their physicians than younger patients, patients of racial/ethnic minority groups, and patients who visited general practitioners or family practitioners. Overall performance on clinical quality metrics was poor. Better performance on medication quality measures did not seem to require extra physician time, while better performance on counseling or screening indicators was associated with longer visit duration. Improvements in quality of care will likely require a combination of investments in systems such as electronic health records, greater use of other professionals such as nurse practitioners, and better reimbursement to primary care physicians for the extra time spent.
Correspondence: Lena M. Chen, MD, MS, Division of General Medicine, University of Michigan Health System, 300 N Ingalls St, Room 7C17, Ann Arbor, MI 48109 ( [email protected] ).
Accepted for Publication: July 23, 2009.
Author Contributions: Dr Chen had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design : Chen and Jha. Acquisition of data : Chen and Farwell. Drafting of the manuscript : Chen and Jha. Critical revision of the manuscript for important intellectual content : Chen, Farwell, and Jha. Statistical analysis : Chen, Farwell, and Jha. Study supervision : Jha.
Financial Disclosure: None reported.
Funding/Support: This study was supported by the Massachusetts Veterans Epidemiology Research and Information Center, Veterans Affairs Boston Healthcare System.
Previous Presentations: This study was presented as an abstract at the New England Society of General Internal Medicine Annual Meeting; March 14, 2008; Worcester, Massachusetts; at the National Society of General Internal Medicine 31st Annual Meeting; April 11, 2008; Pittsburgh, Pennsylvania; and at the AcademyHealth 25th Annual Research Meeting; June 10, 2008; Washington, DC.
Additional Contributions: David W. Bates, MD, MSc, provided insightful comments on an early version of the manuscript.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
It's not just you: Americans everywhere are waiting longer to see a doctor
- A survey of average wait times for doctor's appointments looked at 15 large metropolitan US cities.
- The average doctor's appointment wait time in 2022 was 26 days, 24% higher than it was in 2004.
- The physician-to-population ratios for the surveyed cities are some of the highest in the country.

People are waiting longer to see a doctor now, a survey from AMN Healthcare and its physician-recruiting division, Merritt Hawkins, found.
Researchers at AMN/Merritt Hawkins called doctor's offices in 15 large metropolitan US cities to schedule an appointment as a new patient to see how long they would have to wait for the next availability, or used an online scheduling system to check. The doctor's offices focused on different specialties: cardiology, dermatology, obstetrics-gynecology, orthopedic surgery, and family medicine, according to the survey.
The average appointment wait time for a doctor's visit has increased 8% since the survey was last conducted in 2017. In 2022, the average appointment wait time in the 15 cities is 26 days, up from 24.1 days in 2017. The survey noted that the researchers did not ask for appointments regarding urgent or emergency medical needs, so these wait times are not included.
Compared with 2004 when the survey was first conducted, the average wait time has increased by 24%, from 20.9 days. The survey was conducted between March and mid-May, and covered 1,034 offices.
Portland, Oregon, had the highest average wait time – 45.6 days. New York City had the lowest average wait time at 17.4 days.
Related stories
The specialty with the highest average appointment wait time is dermatology, which has an average wait time of 34.5 days. The average wait time to see a dermatologist in Minneapolis was the highest, at 72 days, while Philadelphia had the lowest average wait time, nine days.
The lowest average appointment wait time was 16.9 days to see an orthopedic surgeon. San Diego had the highest average wait time of 55 days to see an orthopedic surgeon, while Washington, DC, had an average appointment wait time of 5 days.
Historically, the doctor-to-population ratios in the 15 surveyed cities are some of the highest in the US, the survey noted.
"If access to physicians in metropolitan areas with a large number of physicians per capita is limited, it may be reasonable to infer that physician access could be more problematic in areas with fewer physicians per capita," the survey said.
During the coronavirus pandemic, hospitals have struggled financially from having to hire temporary clinical staff when hospital staff is out with COVID-19. For example, a Dallas-based chain of hospitals, surgery centers, and clinics reported lower revenue and earnings in its third quarter than it did in 2021. Tenet Health had to spend money on temporary staff while almost 10% of its clinical staffers were sick in July.
Longer wait times ahead?
The survey listed other factors that can make wait times even longer in the future. The US could have a deficit of between 37,800 and 124,000 doctors by 2034, according to the Association of American Medical Colleges. One of the reasons for that is a growing US population. The US Census Bureau estimates that the population will grow to 423 million by 2050.
Doctors are also aging, with over 30% of the active workforce being 60 or older, AMN/Merritt Hawkins found based on AMA data. A c ap on federal funding for graduate medical education , which Congress implemented in 1997, limited how many doctors could enter practice each year, but was lifted in 2021. Despite the lift, only 1,000 training positions are being funded, "far short of what is needed," the survey said.
- Main content
We're looking for more great physicians to join our team! Explore more here.
- For Individuals & Families
- For Employers & Employees
- For Physicians
- Patient Portal
- For Prospective Physicians
- Cost of PartnerMD
- Find a Doctor
- Find a Location
- Learning Center
- Explore Membership
- Health Insurance
« View All Posts
Why Do You Wait So Long at Doctor's Offices?
March 6th, 2023 | 4 min. read
By Melissa Gifford

It’s the day of your doctor’s appointment. It may have taken you a while to get an appointment , but it’s here.
You drive to the office and walk into the lobby or waiting room. You’re ready to see your primary care physician.
You head to the front desk to check in. The receptionist notes your arrival and directs you to a chair. You sit down. Maybe you grab a magazine to flip through.
And that’s when the waiting begins.
What is the average wait time in doctor’s offices?
A 2018 study by Vitals determined patients wait for an average of 18 minutes and 13 seconds for a physician. While there hasn’t been an updated figure since then, a quick search of the Twittersphere reveals it’s still a common problem with the traditional primary care model.
I hate waiting at doctors offices. — akaMatisse (@akaMatisse) April 29, 2022
still waiting at doctors office like can i please leave if u guys aren’t gonna talk to me. — nine inch tails (@razrluvr) April 19, 2022
Because the average length of an actual appointment is usually between 10-15 minutes, patients often spend more time waiting than they do actually talking to their doctor.
So it begs the question: why do doctors make you wait so long?
Because of an unfortunate combination of not enough primary care physicians, too many patients, and the health insurance reimbursement model.
/line-of-people-at-vaccination-center-picture-id1308661598%20(1).jpg?width=1024&name=line-of-people-at-vaccination-center-picture-id1308661598%20(1).jpg)
1. There aren’t enough primary care physicians.
The United States is in the midst of a physician shortage, particularly among primary care physicians. A report from the Association of American Medical Colleges (AAMC) projects a shortage of between 17,800 and 48,000 primary care physicians by 2034.
Why aren’t there more primary care physicians? It’s complicated, but it can be boiled down to three reasons:
- More and more PCPs are approaching retirement age. The AAMC projected that 40% of physicians in the U.S. will be 65 or older within the next decade.
- Fewer medical school students select primary care as their specialty , in part because it pays significantly less than other specialties. For instance, the average salary of a cardiologist is $490,000, per the 2022 Medscape Physician Compensation report . The average salary of a PCP is $260,000. Given the debt medical students rack up during their education, it’s not surprising more are choosing the more lucrative fields.
- The model of traditional primary care relying on health insurance reimbursements for their revenue is broken . PCP practices rely heavily on these reimbursements for medical services to generate revenue for their practice. And that leads us to the next reason why doctors make you wait so long.
2. Doctors have too many patients.
When your primary source of revenue as a business is through health insurance reimbursements, there’s one easy way to increase revenue – see more patients.
It’s a flawed incentive arrangement that prioritizes the need to see as many patients as possible, instead of the right number required to provide high-quality care for every patient. If you want to keep the business running, you’ve got to see more and more patients.
For doctors running their own practices or as part of a larger hospital system, the pressure of keeping the business running looms, and forces them to grow their panel size to exorbitant sizes.
Today, it’s estimated the average panel size of a traditional primary care physician is north of 2,000 patients.
The result? Packed schedules (sometimes double booked) and not enough time in the day.
With that many patients to take care of, a primary care physician’s schedule can be booked weeks in advance. You probably just experienced that trying to get an appointment .
And because doctor’s offices, like most businesses, typically operate from 8 a.m. to 5 p.m., with an hour for lunch, they churn through dozens of appointments each day, often 20-35. It’s their only option if they want to provide care to thousands.
There just is not enough time in the day to squeeze in everyone effectively.
That means they are booked back-to-back-to-back with patient appointments, and if they spend extra time with one patient, it just makes them late for the next one, and it snowballs from there. Some physicians even double-book appointment slots to provide as much care as possible.
That’s why doctors make you wait so long in a waiting room, lobby, or exam room. They’re trying to keep up with a slammed schedule every day, and that’s just not sustainable.
/female-senior-doctor-welcoming-greeting-mother-and-daughter-at-picture-id1198823252%20(1).jpg?width=1024&name=female-senior-doctor-welcoming-greeting-mother-and-daughter-at-picture-id1198823252%20(1).jpg)
One solution to waiting at doctors’ offices? Concierge medicine.
Let’s be clear: this is not the fault of the physician. It’s the hand they are dealt in the traditional primary care model .
Unfortunately, unless medical schools suddenly increase the rate at which they produce PCPs and health insurance reimbursements change, it’s a system that is unlikely to change, leaving you still waiting at the doctor’s office.
And that’s one of the reasons the concierge medicine model has grown significantly since it was first used in the late 1990s.
Concierge doctors charge a membership fee for patients to be part of the practice. They then reduce the size of their panels from 2,000+ to somewhere between 400-600 patients.
By reducing the size of their panel, they see fewer patients per day and spend more time with each patient (often 30 minutes).
With fewer appointments on the daily schedule and more than enough time with each patient, concierge medicine practices can guarantee little to no waiting. At PartnerMD, we’ll get you back in five minutes or less, often immediately upon your arrival.
If you’re just sick of the waiting that is common at the doctor’s office and want a better experience, it may be time to consider concierge medicine .
As a concierge medicine patient, you can expect your appointment to start on time, and shortly after checking in, you’ll be taken back to the exam room to begin your appointment.
It’s one of the ways concierge medicine removes the hassles of the traditional primary care experience .
Want to learn more about concierge medicine? Download our Understanding Concierge Medicine ebook.
Melissa Gifford
Don't forget to share this post:
Related Articles
5 pros and cons of concierge medicine for patients.
December 12th, 2023 | 4 min. read
Comparing Concierge Medicine in Greenville, SC
November 20th, 2023 | 4 min. read
Top 5 Reasons Why Patients Switch to a Concierge Doctor
November 6th, 2023 | 3 min. read
Inova VIP 360 vs. PartnerMD: A Concierge Medicine Comparison
November 6th, 2023 | 4 min. read
How Does 24/7 Access to Concierge Care Work at PartnerMD?
October 24th, 2023 | 4 min. read
5 Questions To Ask If Your Primary Care Doctor Is Retiring
October 23rd, 2023 | 3 min. read
Comparing Concierge Medicine Practices in Atlanta, GA
October 10th, 2023 | 6 min. read
Holistic Doctor vs. Naturopathic Doctor: Understanding the Difference
October 4th, 2023 | 2 min. read
Concierge Doctors vs. Primary Care Doctors: What's the Difference?
September 25th, 2023 | 4 min. read
Considering Concierge Medicine? Avoid the Top 5 Mistakes Patients Make
September 14th, 2023 | 5 min. read
5 Biggest Challenges with Concierge Medicine
September 5th, 2023 | 4 min. read
4 Newer Primary Care Practice Models for Patients
August 21st, 2023 | 4 min. read
3 Myths About Concierge Medicine Practices for Patients
August 21st, 2023 | 2 min. read
Why Do Doctors Stop Accepting New Patients?
August 14th, 2023 | 2 min. read
4 Things to Do If You Haven’t Been to the Doctor in Years
August 14th, 2023 | 4 min. read
Concierge Medicine for Kids: Doctors, Age Limits, Cost, and More
August 7th, 2023 | 4 min. read
Caring for Elderly Parents: 4 Ways Concierge Medicine Helps Caregivers
July 28th, 2023 | 4 min. read
Is Concierge Medicine Worth It?
July 24th, 2023 | 3 min. read
6 Ways Concierge Medicine Helps Busy Professionals
July 24th, 2023 | 5 min. read
Primary Care for Kids: 7 Reasons to Consider Concierge Medicine
July 18th, 2023 | 5 min. read
What Are the Benefits of a Concierge Doctor If You're Healthy?
July 17th, 2023 | 4 min. read
4 Ways Concierge Medicine Helps Moms Manage Time Better
June 30th, 2023 | 4 min. read
6 Types of Concierge Medicine Fees
June 28th, 2023 | 3 min. read
How Does Coordination of Specialist Care Work at PartnerMD?
June 20th, 2023 | 5 min. read
Concierge Medicine vs. Direct Pay Primary Care vs. VIP Medicine
June 20th, 2023 | 4 min. read

IMAGES
VIDEO
COMMENTS
Results—During 2019, an estimated 1.0 billion office-based physician visits occurred in the United States, an overall rate of 320.7 visits per 100 people. The visit rate among females was higher than for males, and the rates for both infants and older adults were higher than the rates for those aged 1-64.
Previous Medscape studies have suggested that female doctors spend more time per patient, on average, than their male counterparts, and this study shows the same pattern, with 49% of female ...
The short answer is "no.". While it's hard to pin down a meaningful average for something like patient visit times, studies indicate that doctors have spent roughly 13 to 24 minutes with patients for at least the past three decades. Data from the 1990s reveal some debates about the average time physicians spend with patients.
The average cost of urgent care center visits range from $100 to $150 and costs can be higher or lower depending on insurance coverage, annual deductibles and copays.13. The end result = 1 urgent care visit is 2-4 hours and costs can be confusing based on insurance coverage. An Emergency Room Visit.
What doctors want: more time with patients. athenahealth; October 18, 2017. Accessed May 18, 2020. ... Time is a scarce and valuable resource in primary care, with the average visit lasting 18 minutes. 1 By a recent estimate, primary care clinicians would require 27 hours per day to provide all guideline-recommended preventive, ...
The number of primary care physicians per 100,000 population varies significantly by state (Figure 5). Mississippi has the lowest, with 49.1, and Vermont the highest, with 103.9 primary care physicians per 100,000 people. The District of Columbia has an even higher physician-to-population ratio of 130.7.
Between 1989 and 1998, the average number of office hours held by office-based physicians increased nonsignificantly, by 0.1 hour (95 percent confidence interval, -0.7 to 0.9). The small ...
The number of primary care visits decreased from 336 million to 299 million per year. Per capita visit rates declined from 1.5 visits per person in 2008 to 1.2 visits per person in 2015: a 20% decline over the study period (−0.25 visits per person, 95% CI, -0.32 to -0.19) ( Table 1 ).
PURPOSE Recent evidence shows a national decline in primary care visit rates over the last decade. It is unclear how changes in practice—including the use and content of primary care visits—may have contributed. METHODS We analyzed nationally representative data of adult visits to primary care physicians (PCPs) and physician practice characteristics from 2007-2016 (National Ambulatory ...
Average length of visits was 17.4 minutes. The median length of visits was 15.7 minutes. The median talk time by patient was 5.3 minutes, and physician, 5.2 minutes. The median time during which neither part spoke was 55 seconds. (Note: unlike the case of the mean, the sum of the medians is not the median of the sum.)
The time doctors spend with patients has a major impact on care. Average visit times seem to have increased over the years—yet physicians may still feel pressed to do more in the available time ...
The Time Crunch. While Mechanic demonstrated that routine primary care visits (averaging 15-20 min) were 1 to 2 min longer than before, 1 the complexity of clinical issues addressed during these visits has increased. In 2010, the CDC reported that one-third of elderly patients had three or more chronic medical conditions, with 40 % of patients taking three or more medications.
A National Ambulatory medical survey suggested that physician reported time spent directly with patients had lengthened by an average of 2.4 min between 2008 and 2015, raising the question of what amount of time is needed for clinicians to provide satisfactory care [12, 21].
In fact, primary care physicians spent 16% more time during a typical office visit in 2005 compared with 1997. Not surprisingly, older patients or those making their first visit spent more time with the physician. In contrast, primary care physicians spent less time with patients of racial/ethnic minority groups, especially during GME visits.
Average Time Doctors Spend with Patients by Specialty. The Medscape Physician Compensation Report 2017 found overall that: ... Their average patient visit lasts 26 minutes, including time with the medical assistant. Olden also suggested allowing team members to provide more of the services. Then the physician can spend time after the visit ...
Exams, on average, ran 1.2 minutes later than their scheduled duration (standard deviation, 13.5 minutes). More than two-thirds of visits deviated from the schedule by five minutes or more. Compared with visits scheduled for 20 or 30 minutes, visits scheduled for 10 or 15 minutes were more likely to exceed their allotted time.
The average appointment wait time for a doctor's visit has increased 8% since the survey was last conducted in 2017. In 2022, the average appointment wait time in the 15 cities is 26 days, up from ...
Across all specialties in this poll, approximately 45% of men surveyed report spending 16 minutes or more on average with their patients, while 57% of women report spending 16 minutes or more with their patients. Similarly, a NEJM study found that amongst PCPs, women spent 15.7% more time with a patient per visit than men.
still waiting at doctors office like can i please leave if u guys aren't gonna talk to me. — nine inch tails (@razrluvr) April 19, 2022. Because the average length of an actual appointment is usually between 10-15 minutes, patients often spend more time waiting than they do actually talking to their doctor.
Understanding the cost of your doctor visit. In the fourth installment of this 4-part series on health care costs, we look at the different types of care to help you better understand what you'll need to pay. Understanding your health plan costs can help you choose the right coverage and budget for your health care spending.