
Ultrasound has head-to-toe applications for primary care, and the newest machines are portable and affordable enough to fit into almost any practice.
JOY SHEN-WAGNER, MD, FAAFP, AND MARK DEUTCHMAN, MD, FAAFP
Fam Pract Manag. 2020;27(6):33-40
Author disclosures: Dr. Deutchman is on the medical advisory board of EchoNous, a point-of-care ultrasound device manufacturer. It is an unpaid position. He also owns stock in the company. No other relevant financial affiliations disclosed.
Related article from American Family Physician : " Point-of-Care Ultrasonography ."
Family physicians can order a wide range of imaging services for patients. But barriers such as time, money, and physical distance sometimes prevent patients from accessing those services, causing gaps in care. Incorporating point-of-care ultrasound (POCUS) into clinical practice is one way to bridge those gaps.
Technological advancements have allowed more physicians to bring ultrasound services to the office visit or bedside, and to make POCUS an integral part of practice. I [Dr. Deutchman] was an early adopter, adding ultrasound to my rural practice in 1980 after delivering a surprise set of twins in the wee hours of the morning. I have never since been surprised by twins, nor missed an ectopic pregnancy. In addition, I [Dr. Shen-Wagner] first used POCUS during residency in 2011, after a patient complained that it felt like her intrauterine device (IUD) had moved. Everything looked normal on the pelvic exam, but a hand-me-down ultrasound machine from the clinic's obstetrics department revealed the unmistakable flutter of a tiny heartbeat. The patient was pregnant, despite having an IUD for three years.
These are just two examples of the many ways POCUS can benefit doctors and patients. There is robust evidence that POCUS improves care in critically ill patients and improves the efficiency and safety of many invasive ambulatory surgeries that are otherwise performed blindly or by anatomic landmarks. 1 There is also preliminary but growing evidence that POCUS can improve diagnostic capabilities, expedite patient care, and inform bedside treatment and management. 2 , 3 Most recently, POCUS has proven to be a valuable tool for confirming COVID-19 diagnoses, as well as monitoring some symptoms of the disease. 4
The hands-on, “showing while telling” nature of POCUS advances physical diagnosis skills, fosters doctor-patient communication, and increases patient satisfaction. 5 This article outlines some common uses for POCUS and explains how to add it to a practice.
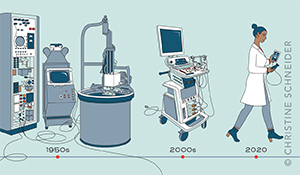
Advances in technology have made ultrasound machines more portable and affordable, increasing their accessibility for primary care clinicians.
Point-of-care ultrasound beginners should start with impactful procedures that are easy to perform, simple to interpret, and relatively low liability for both patient and physician. Move on to more complex uses only after those are learned.
Pocket-sized ultrasound machines cost $2,000 to $10,000, plus the costs of gel, probe covers, and cleaning supplies. But several high-yield ultrasound codes can help recoup those expenses.

WHAT IS POCUS AND WHAT IS IT GOOD FOR?
POCUS is a quick, abbreviated study performed and interpreted immediately by the evaluating and treating clinician to help answer clinically impactful questions.
Ultrasound uses have evolved with the technology. The first widely used diagnostic ultrasounds were large, stationary machines that produced grainy still images in the 1960s. Ultrasound in that era was a snapshot in time, performed by a sonographer and interpreted by a radiologist with limited context.
Through decades of advancements those ponderous machines have become pocket-sized devices, capable of pairing with tablets and smartphones to create high-resolution, real-time images, which allows for innovative primary care applications. 6 In the hands of a family physician who is familiar with the patient, these applications can expand beyond diagnostics to procedures like endometrial biopsy or IUD placement, among others. POCUS is now being investigated for home visits to extend services beyond the clinic walls. 7
For physical exams, POCUS supplements palpation, providing greater sensitivity and specificity. 8 It can help identify the best place to insert a needle, especially when traditional landmarks are unreliable because of obesity, or if safety is a concern (e.g., amniocentesis, central line, and paracentesis). For complex questions about a patient's hemodynamics, POCUS can provide multi-organ views pieced together to form an assessment, whereas traditional approaches might require a combination of different types of imaging (e.g., echocardiogram, X-ray, and computerized tomography scan) to arrive at a similar conclusion. (See “ Point-of-care ultrasound uses .”)
POCUS, in fact, has “head-to-toe” primary care applications, from ocular ultrasounds to assess elevated intracranial pressure to ultrasounds looking for gout in the big toe. It can examine a specific, limited structure like soft tissue to evaluate lumps and bumps, or provide multi-organ views for undifferentiated complaints such as dyspnea. 9
With such a wide range of uses, it can be hard to know where to start. But we recommend beginners start with applications that are easy to perform, simple to interpret clinically, low liability to the physician and the patient, and still clinically useful. (See “ POCUS for beginners .”) For example, physicians new to POCUS should not start by scanning for deep vein thrombosis (DVT). The technique is not easy (it requires multi-point compression in specific locations along the affected leg), the interpretation is not simple (it requires knowing anatomical variations and the patient's pretest probability and clinical context), and the liability is high (because there are grave consequences to missing a DVT). It should be left to an experienced ultrasound user.
On the other hand, scanning to determine if cellulitic skin has formed an abscess is a great POCUS starting point. It is impactful (it informs the need for bedside incision and drainage), easy to perform (it only requires one or two views), simple to interpret (it involves simple anatomy and limited diagnostic endpoints — either there is a fluid pocket or there is no pocket), and low risk for harm (after learning basic rules to differentiate from a lymph node or vascular structure).
Physicians can then add more complex applications as they gain experience. (See “ POCUS multi-organ scans .”)
COMPETENCY, CREDENTIALING AND CERTIFICATION
POCUS does not belong to any one specialty or field. The American Medical Association affirmed in 1999 — and reaffirmed in 2020 — that “ultrasound imaging is within the scope of practice of appropriately trained physicians.” 10 The guidelines for determining whether physicians are “appropriately trained” generally fall under the “three Cs”: competency, credentialing, and certification.
Competency is physicians' ability based on their education and demonstrated experience, and is the key factor in determining if family physicians can perform point-of-care ultrasound. Physicians should only begin billing for POCUS after they achieve competency and establish billing and documentation infrastructure. The American Academy of Family Physicians (AAFP) has endorsed recommended POCUS curriculum guidelines for family medicine residents, and as more residency programs begin to incorporate POCUS in their curriculum, it may become a core competency like it is in emergency medicine residency. 11 In the meantime, hands-on ultrasound training is increasingly available throughout the year, including sessions geared towards primary care physicians offered by the AAFP, American Institute of Ultrasound in Medicine (AIUM), and American College of Physicians (ACP). There are a handful of primary care ultrasound fellowships (and some emergency medicine fellowships that accept general medicine applicants) across the U.S. that can jumpstart training. There are also free online resources available to supplement hands-on education.
Learners should keep a log of completed scans, but requiring a specific number of scans for competency is controversial because the number varies by physician and by the complexity of the application.
Credentialing is determined by the credentialing body at the physician's local hospital and is often undefined for family physicians. If you are an early adopter at your institution, you may have to self-advocate and carve out a pathway. Reach out to your counterparts in emergency medicine, internal medicine, and critical care to network and support each other in credentialing.
Certification is offered by several national institutions and can streamline the credentialing process, depending on local politics. However, certification can be costly and time-consuming, and should not be viewed as an absolute requirement for using POCUS within family medicine.
PUTTING POCUS INTO PRACTICE
Placing the ultrasound probe on the patient and getting the image is fun and rewarding, which makes it tempting to skip the administrative tasks and jump right in. But long-term success requires a consistent billing and documentation routine. Ignoring ultrasound administrative tasks could mean lost revenue, lack of justification for new equipment, and legal vulnerability for missing documentation. Some ultrasound scans could be non-billable “quick looks,” such as scanning to monitor therapy, or educational scans by trainees. But most scans should aim to be billable, with documentation in the medical record, independent image reports, and archived representative images, depending on the CPT code. Establishing a good system is therefore key for sustainable scanning.
POCUS documentation . To meet billing requirements, an independent report needs to include these components: two patient identifiers or demographics (e.g., patient name, facility name, date and time of exam, etc.), indication for the ultrasound, adequacy of the scan, description of the findings, and interpretation. 12 Documentation and reporting templates can be found in the American College of Emergency Physicians (ACEP) ultrasound standard reporting guidelines. 13 , 14
Documentation should reflect the level of training or stage of ultrasound learning maturation. During the learner stage (whether you are a medical student or a seasoned clinician adopting ultrasound as a new skill), document that you performed an educational ultrasound with the patient's verbal consent and that the purpose of the imaging was strictly educational and not meant to replace clinical judgment or a formal study. If there was a clinical finding, document that you discussed the finding with the patient and document any additional steps taken or studies ordered.
Image archival . Billable scans require images that can be retrieved for audits, to substantiate insurance claims, or for comparison and review down the road. Medicare requires billers to retain images for at least five years, but states may have different rules. 15 Though images have to be retrievable, they do not have to be stored within the EHR. There are three ways to store images, each with its own pros and cons.
Device storage: This is a temporary stop for images and needs to be regularly reviewed, backed up, and cleared. This is the easiest option to achieve, but also the riskiest.
Hard drive storage: This is where images can be regularly saved. It needs to have encryption, be checked regularly and backed up, and be stored in a secure location. This is cost effective but labor intensive.
Cloud storage: Images are stored using “middleware” (software that acts as a bridge between a device and an operating system), and then uploaded securely to a server. It's the most secure, but most expensive option.
Image capturing requirements differ for each application. For example, billing for procedural guidance typically requires just one still image of the structure of interest (e.g., the effusion in a knee aspiration). CPT codes for limited scans are generally well-suited to POCUS because they are narrower in scope and require only a few representative images. Complete studies require more documentation. For example, an abdominal aortic aneurysm screening requires captured images and measurements of three segments of the aorta in two planes. Common requirements can be found in the ACEP reporting guidelines and AIUM practice parameters. 12 , 13 Different insurance companies may have slight variations in requirements.
Cleaning and disinfection . Ultrasound cleaning protocols generally follow Centers for Disease Control and Prevention or AIUM recommendations for disinfection of medical equipment. 16 , 17
After performing an ultrasound, your first disinfection step should be wiping away any gel left on the ultrasound transducers with a soft clean cloth. Sterile ultrasound gel is recommended, but it can still harbor organisms and, if it is allowed to dry, can make disinfection less effective. Infection risk can be further mitigated with single-use probe covers, which should be discarded promptly after use.
The rest of the ultrasound cleaning and disinfection protocols fall into two categories: lower risk scans (or “non-critical” based on the Spaulding criteria for sterilization of medical devices), which require low-level disinfection (LLD), and higher risk scans (“semi-critical,” per Spaulding), which require high-level disinfection (HLD).
Ultrasound applications that involve scanning intact skin and no mucous membranes require only LLD. Multiple passes with a commercial disinfecting wipe readies the equipment for the next use. Commercial wipes and sprays have varying wet contact times to be effective, which should be listed on the packaging. Ultrasound manufacturers can recommend cleaning agents that won't corrode equipment. If disinfecting wipes are not available, soap and water is acceptable. The ultrasound can also be sufficiently cleaned in this manner after certain percutaneous procedures and needle guidance, if you use a disposable probe cover and sterile gel.
Ultrasound applications that include contact with mucous membranes (vaginal or rectal mucosa) or non-intact skin (such as burns or stasis ulcers) require HLD. In addition to using probe covers and an appropriate commercial disinfectant wipe, the user should also put the equipment through a series of chemical washes made specifically for medical products (e.g., Cidex or MetriCide) or in an aerosolized hydrogen peroxide misting machine (e.g., Nanosonics' trophon).
In the era of COVID-19, physicians should pay special attention to disinfection before and after scanning. Most commercial wipes are effective against the novel coronavirus, with variations in contact time that can be confirmed on the Environmental Protection Agency's website. 18
ECONOMIC CONSIDERATIONS IN IMPLEMENTING POCUS
A variety of entry-level ultrasound units are now affordable for individual physicians, and some companies allow physicians to rent equipment as well as buy it. (See “ Pocket-sized ultrasound models .”)
Make sure any device you purchase has Food and Drug Administration approval before using it on patients. If you are employed by a hospital system, your employer may require institutional approval before you can use ultrasound in patient care (outside of educational scans). Reimbursements are determined by the type of scan performed and the practice setting (e.g., hospital-employed physicians will need to use modifier -26 to bill only the professional component).
Entry-level ultrasound devices cost between $2,000 and $10,000. Some offer annual subscriptions for features like HIPAA-compliant cloud storage, tutorials, and advanced imaging presets. Those are the startup costs. There are also per-procedure costs. When bought in bulk, single-use packets of sterile gel generally cost $1–$2, and disposable probe covers cost about $0.25 each. LLD cleaning products are generally less than $0.25 per use, and HLD chemical washes cost about $50 per gallon.
Family physicians can perform a number of POCUS procedures that yield Medicare reimbursements of $50–$125 (see “ POCUS coding ”). These far outweigh the per-procedure costs, allowing physicians to recoup startup expenses within a reasonable timeframe, although a warranty to hedge against breakdowns of the ultrasound device may be considered, depending on the cost. That's just one of many things to consider when adding ultrasound to a practice. However, there have never been more free resources and hands-on CME workshops to help family physicians do it. Technological advancements have brought more user-friendly interfaces, increased portability, and lower costs. The latest POCUS models even include telemedicine capabilities to interact with experts remotely, and artificial intelligence to increase diagnostic support, making interpretation easier. 19 With time, effort, and practice, any motivated physician can incorporate ultrasound into clinical practice.
Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical landmarks for internal jugular vein catheterization. Cochrane Database Syst Rev . 2015;1(1):CD006962.
Wagner M, Shen-Wagner J, Zhang KX, Flynn T, Bergman K. Point-of-care ultrasound applications in the outpatient clinic. South Med J . 2018;111(7):404-410.
Arnold MJ, Jonas CE, Carter RE. Point-of-care ultrasonography. Am Fam Physician . 2020;101(5):275-285.
Mathews BK, Koenig S, Kurian L, et al.; Clinical progress note: point-of-care ultrasound applications in COVID-19. J Hosp Med . 2020;15(6):353-355.
Howard ZD, Noble VE, Marill KA, et al.; Bedside ultrasound maximizes patient satisfaction. J Emerg Med . 2014;46(1):46-53.
Bornemann P, Jayasekera N, Bergman K, Ramos M, Gerhart J. Point-of-care ultrasound: Coming soon to primary care?. J Fam Pract . 2018;67(2):70-80.
Bonnel AR, Baston CM, Wallace P, Panebianco N, Kinosian B. Using point-of-care ultrasound on home visits: the home-oriented ultrasound examination (HOUSE). Letter. J Am Geriatr Soc . 2019;67(12):2662-2663.
Adhikari S, Blaivas M. Sonography first for subcutaneous abscess and cellulitis evaluation. J Ultrasound Med . 2012;31(10):1509-1512.
Mantuani D, Frazee BW, Fahimi J, Nagdev A. Point-of-care multi-organ ultrasound improves diagnostic accuracy in adults presenting to the emergency department with acute dyspnea. West J Emerg Med . 2016;17(1):46-53.
Privileging for ultrasound imaging H-230.960. American Medical Association Council on Medical Service. 2020. Accessed Sept. 3, 2020. https://policyse-arch.ama-assn.org/policyfinder/detail/Ultrasound%20imaging?uri=%2FAMADoc%2FHOD.xml-0-1591.xml
Recommended curriculum guidelines for family medicine residents: point of care ultrasound (AAFP reprint No. 290D). American Academy of Family Physicians. Accessed Sept. 3, 2020. https://www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint290D_POCUS.pdf
American Institute of Ultrasound in Medicine; AIUM practice parameter for documentation of an ultrasound examination. J Ultrasound Med . 2020;39(1):E1-E4.
Standard reporting guidelines: ultrasound for procedure guidance. American College of Emergency Physicians. May 2015. Accessed Sept. 3, 2020. https://www.acep.org/globalassets/uploads/uploaded-files/acep/by-medical-focus/ultrasound/eus-srg-proc-guidmay2015_final.pdf
Liu RB, Blaivas M, Moore C, et al. Emergency ultrasound standard reporting guidelines. American College of Emergency Physicians. June 2018. Accessed Sept. 3, 2020. https://www.acep.org/globalassets/uploads/uploaded-files/acep/clinical-and-practice-management/policy-statements/information-papers/emergency-ultrasound-standard-reporting-guidelines---2018.pdf
Digest of council actions 2019–2020 (appendix E). American College of Radiology. Accessed Sept. 3, 2020. https://www.acr.org/-/media/ACR/Files/Governance/Digest-of-Council-Actions.pdf
A rational approach to disinfection and sterilization. Centers for Disease Control and Prevention. Sept. 18, 2016. Accessed Sept. 3, 2020. https://www.cdc.gov/infectioncontrol/guidelines/disinfection/rational-approach.html
Guidelines for cleaning and preparing external- and internal-use ultrasound transducers and equipment between patients as well as safe handling and use of ultrasound coupling gel. American Institute of Ultrasound in Medicine. March 27, 2020. Accessed Sept. 3, 2020. https://www.aium.org/officialStatements/57
List N: disinfectants for Coronavirus (COVID-19). United States Environmental Protection Agency. Updated Oct.5, 2020. Accessed Oct. 8, 2020. https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2
Akkus Z, Cai J, Boonrod A, et al.; A survey of deep-learning applications in ultrasound: Artificial intelligence-powered ultrasound for improving clinical workflow. J Am Coll Radiol . 2019;16(9 Pt B):1318-1328.
Continue Reading
More in FPM
More in pubmed.
Copyright © 2020 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Scientific Reports

Novice-performed point-of-care ultrasound for home-based imaging
Nicole m. duggan.
1 Department of Emergency Medicine, Brigham and Women’s Hospital, 75 Francis Street, NH-2, Boston, MA 02115 USA
Nick Jowkar
2 Department of Radiology, Brigham and Women’s Hospital, Boston, USA
Irene W. Y. Ma
3 Division of General Internal Medicine, University of Calgary, Calgary, Canada
Sara Schulwolf
4 University of Connecticut School of Medicine, Farmington, USA
Lauren A. Selame
Chanel e. fischetti, andrew j. goldsmith, associated data.
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Patient-performed point-of-care ultrasound (POCUS) may be feasible for use in home-based healthcare. We investigated whether novice users can obtain lung ultrasound (LUS) images via self-scanning with similar interpretability and quality as experts. Adult participants with no prior medical or POCUS training, who were capable of viewing PowerPoint slides in their home and who could hold a probe to their chest were recruited. After training, volunteers self-performed 8-zone LUS and saved images using a hand-held POCUS device in their own home. Each 8-zone LUS scan was repeated by POCUS experts. Clips were independently viewed and scored by POCUS experts blinded to performing sonographers. Quality and interpretability scores of novice- and expert-obtained LUS images were compared. Thirty volunteers with average age of 42.8 years (Standard Deviation (SD) 15.8), and average body mass index of 23.7 (SD 3.1) were recruited. Quality of novice and expert scans did not differ (median score 2.6, interquartile range (IQR) 2.3–2.9 vs. 2.8, IQR 2.3–3.0, respectively p = 0.09). Individual zone quality also did not differ (P > 0.05). Interpretability of LUS was similar between expert and novice scanners (median 7 zones interpretable, IQR 6–8, for both groups, p = 0.42). Interpretability of novice-obtained scans did not differ from expert scans (median 7 out of 8 zones, IQR 6–8, p = 0.42). Novice-users can self-obtain interpretable, expert-quality LUS clips with minimal training. Patient-performed LUS may be feasible for outpatient home monitoring.
Introduction
Since early 2020, the Coronavirus disease 2019 (COVID-19) pandemic has placed unparalleled stress on healthcare resources worldwide. In response, and in conjunction with support from both private payers and government entities such as the Centers for Medicare and Medicaid Services, home-based health services and telemonitoring systems are rapidly expanding 1 . By mid-2021, telehealth use had surged to 38-fold higher than pre-pandemic levels, and a further 29% increase in telehealth visits for medical evaluation and management is anticipated by 2029 2 , 3 . As home-based initiatives evolve into a pillar of healthcare delivery, portable tools to facilitate diagnostics and therapeutics in alternative care settings such as patient homes must be explored.
Point-of-care ultrasound (POCUS) is a low-cost, radiation-free imaging modality that offers real-time data to aid medical care. Lung ultrasound (LUS) in particular demonstrates higher sensitivity than chest x-ray or computed tomography in detecting pulmonary pathologies such as pleural effusion, alveolar interstitial syndrome, pneumothorax, pneumonia, and acute decompensated heart failure 4 – 7 . For patients with heart failure, LUS findings over the course of treatment can predict adverse events and can correlate with both short- and long-term outcomes as well as patient mortality 8 – 11 . Expert consensus statements outlining the use of LUS to monitor known or suspected COVID-19 infection have also been proposed 12 , 13 . Over the last decade, POCUS has become even more portable with the development of hand-held transducers that collect and transmit images from smartphones or tablet devices. The versatility and increasing portability of POCUS makes this an ideal technology to deploy in alternative care settings.
The potential for patients to self-perform POCUS scans and obtain interpretable images to aid in real-time medical decision-making could transform home-hospital care. Traditionally POCUS experts undergo extensive training to learn to accurately acquire and interpret images 14 . Recent case reports have described healthcare providers who are infected with COVID-19 and on home isolation successfully performing daily self LUS to monitor disease progression 15 , 16 . However, these patients did have prior POCUS training, thus the ability for a typical home hospital patient with no prior POCUS experience to perform and obtain interpretable images remains unclear.
Aim of the study
The goal of this work was to assess the ability of novice POCUS users to self-acquire interpretable LUS images using a hand-held device. We hypothesized that with minimal training, novice users would be able to self-obtain LUS images that were sufficient for diagnostic purposes, and which would have minor variation from the quality of expert-obtained scans.
Study design and setting
This prospective study was performed in participant homes outside of the healthcare setting. All patients provided informed consent for study participation and to publish their information. This work was performed in accordance with all local guidelines and regulations and was approved by the Mass General Brigham Institutional Review Board.
Selection of participants
Healthy adult volunteers aged 18 years or older with no prior medical training were recruited. Individuals who met these criteria were referred to study personnel by colleagues and were recruited via telephone contact. Participants were deemed eligible for inclusion if they had access to a computer, email address, and internet to preview a slide show-based presentation which was electronically sent to them ahead of the study period, and were physically able to hold a probe on their chest as self-determined by participants. Live and/or continuous internet access during the study period was not required. Patients with prior medical or imaging training or prior experience performing POCUS were excluded from this study. Patients provided demographic information including age, height, weight, and highest level of formal education achieved.
Novice training and LUS scanning protocol
A 28-slide tutorial slideshow with instructions on how to perform self-ultrasound was electronically mailed to participants to review on their own before initiating the study. The slideshow consisted of a combination of text and images including an introduction to POCUS, depicting use of the portable POCUS device and software, as well as desired LUS scanning technique and locations. Key anatomical structures necessary for obtaining interpretable images including rib shadows, pleural line, and A-lines as illustrated by the BLUE protocol and the American College of Emergency Physicians Emergency Ultrasound imaging criteria were described and depicted in the tutorial slideshow 17 , 18 . Training slides did not include information about pulmonary pathology identifiable on POCUS as the purposes of this study was to assess image acquisition alone and not image interpretation. Participants were allowed to review the slide show as many times as they needed to feel comfortable with the content prior to scanning, and were allowed to review the slides while scanning as needed. Study personnel did not assist or participate in patient-performed scans.
LUS scans were performed in participant homes using a hand-held ultrasound probe (Butterfly iQ, Butterfly Network Inc, Guilford CT, USA) connected to an iOS-capable device (Apple, Cupertino CA, USA). After reviewing the tutorial, participants were asked to perform an 8-zone LUS on themselves with instruction to try to obtain as interpretable images as possible as described in the tutorial (Fig. 1 A). Lung zones included two anterior zones and two lateral zones on each side of the thorax (Fig. 1 B). While international standards for performing LUS have recently been proposed using 14-zone scans, these scanning protocols include 6 posterior lung zones which are not accessible to individuals performing self-scans, thus an 8-zone scanning protocol was used 13 . Participants were instructed to obtain the most interpretable clips possible for each zone following interpretability rules as described in the training slideshow. POCUS experts observed all novice-scans but did not offer instruction or intervene in the scanning in any way. Emergency medicine faculty with fellowship training in emergency ultrasound then repeated the same 8-zone LUS on each participant using the same ultrasound device. Six-second clips of each zone for both novice and expert scans were saved to the iOS device and subsequently uploaded to the cloud.

Novice-performed lung ultrasound scanning protocol. ( A ) A novice self-performs a LUS using a hand-held ultrasound probe attached to an iOS device. ( B ) 8-zone scanning protocol performed by both novices- and expert-sonographers.
LUS scoring and rater training
All LUS clips were deidentified and presented in random order to two POCUS experts (emergency medicine faculty with fellowship training in emergency POCUS, NMD and AJG). All images were blinded and randomized as to who acquired each clip (novice vs expert), and to lung zone scanned.
Clips were individually scored by each POCUS expert using a previously described scoring system as follows: 0 indicates no identifiable structures are visualized over an entirety of the clip, 1 indicates the pleural line is partially visualized but the clip is of non-diagnostic quality, 2 indicates that the pleural line is partially visualized but the image is sufficient for diagnostic purposes, and 3 indicates an ideal image with the pleural line easily visualized 15 . Scores of 0 and 1 were considered non-diagnostic whereas scores of 2 and 3 were considered to be sufficient quality for diagnostic assessment (e.g. interpretable, Fig. 2 ).

Scoring system used for grading novice- and expert-performed lung ultrasounds.
Prior to scoring study clips, for training purposes, two expert raters scored together a separate training dataset of LUS clips, discussing and resolving any rating discrepancies. The two raters then scored an additional dataset of 16 LUS clips independently to ensure acceptable inter-rater reliability. Post-training inter-rater reliability of quality scores was excellent (intraclass correlation coefficient 0.97, 95% CI 0.90–0.99). Agreement of image interpretability between the two raters was moderate (kappa = 0.64), with only one disagreement in interpretability. This disagreement occurred on a clip that was given a rating of 1 (pleural line is partially visualized in the clip but the clip is non-diagnostic in quality) by one expert, and a score of 2 (pleural line is partially visualized in the clip however the clip is diagnostic in quality) by the second expert.
Statistical analyses
Data were analyzed using standard parametric and non-parametric techniques. The number of interpretable zones and quality scores of novice-obtained scans were compared with expert-obtained scans using Wilcoxon signed rank sum tests. Proportions of interpretable scans between groups were compared using Chi-square tests. To account for multiple comparisons, we used Bonferroni-adjustments. Agreement in ratings between the two trained raters on quality scores and interpretability of scans was assessed using intraclass correlation coefficients and Kappa statistics, respectively. All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) and SPSS, version 28 (IBM Corporation, Armonk, NY, USA).
Characteristics of study subjects
In total, 30 participants were recruited for this study. Participants had an average age of 42.8 years [standard deviation (SD) 15.8], an average body mass index of 23.7 kg/m 2 (SD 3.1), and 67% of participants (n = 20) were male (Table (Table1). 1 ). Among participants 3% were high school graduates (n = 1), 3% received some college credit but no degree (n = 1), 27% held a Bachelor’s degree (n = 8), 23% held a Master’s degree (n = 23), 13% held a Professional degree, and 13% held a Doctoral degree (n = 9).
Participant demographics.
Main results
A total of 480 LUS clips were obtained from both novice and expert POCUS scanners. Overall, 84% (n = 201) of novice-obtained clips were considered interpretable, which was not different compared to 87% expert-obtained clips being interpretable (n = 209), p = 0.30. Quality scores of novice and expert scans did not differ (median 2.6, interquartile range (IQR) 2.3–2.9 for novices, median 2.8, IQR 2.3–3.0, p = 0.09 for experts) (Table (Table2). 2 ). Quality scores in the eight individual zones also did not differ (P > 0.05 for all). Overall, a median of 7 out of 8 zones were deemed interpretable for novice-obtained scans (IQR 6–8). Interpretability of novice- and expert-obtained scans did not differ, compared to expert-obtained scans (median 7 out of 8 zones, IQR 6–8, p = 0.42). When adjusted for multiple comparisons, interpretability of LUS for each zone did not differ between expert-obtained scans and novice-obtained scans (Table (Table2 2 ).
Novice- vs expert-obtained clip quality score reported at median average scores (interquartile range).
*This score references the gold standard score which is the average of the expert raters’ scores.
**Wilcoxon signed rank sum test.
Inter-rater reliability between the two raters was high. Agreement was excellent for quality scores between the two raters (ICC 0.99, 95% 0.97–0.99 for both novice and expert-obtained scans) (Table (Table3). 3 ). Agreement was also almost perfect for both novice and expert-obtained scans in the determination of interpretability [kappa for novice scans = 1.00 (CI 1.00–1.00); kappa for expert scans = 0.98 (CI 0.94–1.00)] (Table (Table3 3 ).
Inter-rater reliability for scores of novice- and expert-obtained clips.
Kappa values are reported for comparing clips rated as interpretable.
CI confidence interval.
In this study we assessed whether healthy volunteers with no prior medical experience or POCUS training could accurately perform LUS using a hand-held POCUS in their home setting. Overall, quality and diagnostic capabilities of LUS scans did not differ between novice- and expert-obtained scans. This work supports the emerging body of literature which suggests that non-physician novice POCUS users are able to self-perform LUS with minimal prior training and without the need for live expert guidance 11 , 15 , 19 .
Our data demonstrate that novice POCUS users can obtain LUS images of both anterior and lateral lung zones independently without need for expert assistance. This work supports the recent report by Kirkpatrick et al. in which novice users guided by experts on live tele-ultrasound were able to self-obtain images of the anterior and lateral lung zones in 100% of attempts with 99.8% of images being read as interpretable by experts 20 . However in this prior work only 66% of attempts to self-obtain images of posterior lung zones were successful. Our goal with this work was to create a LUS scanning protocol which is easy and feasible for novice users to successfully self-perform at home. However, for some pathological processes, important findings may be missed by not imaging posterior fields. Further work is needed to assess whether interpretable posterior lung zone clips are obtainable in remote patient self-assessment.
In recent years, healthcare initiatives focusing on expanding home-based care services have been rapidly expanding world-wide 1 – 3 . These initiatives which explore a variety of services such as monitoring post-hospital discharge, providing primary hospital services, and outpatient telehealth visits all provided remotely to patients in their own homes have shown promise in both clinical outcomes and patient satisfaction 21 – 25 . With the entry of portable, hand-held POCUS devices into the market, availability of POCUS for use outside of traditional acute care settings is now feasible. This includes settings where point-of-care imagine was not historically available such as in primary care offices, rural health clinics, and even in patient homes. As home-based healthcare services become more widely available, advanced methods for patient evaluation and monitoring must be explored.
This work helps to demonstrate that POCUS may be a viable approach to patient-centered monitoring and diagnostic evaluation for conditions which are increasingly being managed outside of traditional clinical spaces such as heart failure. Currently, patients with heart failure are asked to monitor their weight and blood pressure at home daily to help guide outpatient medical management. LUS also has a demonstrated role in assessing acute heart failure exacerbations and the presence of B-lines on LUS has been correlated with increased morbidity and mortality in this population 9 , 10 . Thus, programs which incorporate tools such as LUS into home-based monitoring programs may improve disease management by providing more objective data for monitoring purposes. A suggested workflow to incorporate LUS into home-based monitoring for conditions such as heart failure can be seen in Fig. 3 . While performing self-scans may be challenging in acutely ill patients, this may represent a viable tool for home monitoring patients with chronic illness or acute-on-chronic disease. Future studies examining clinical outcomes of such a program would provide invaluable information both for clinicians and private companies examining new technology related to remote or home-based healthcare.

Proposed workflow for integrating patient-performed self-lung ultrasound into clinical care.
Limitations
This was a small, single center study which limits the generalizability of our findings. Subjects were recruited via referral from colleagues to study personnel, thus this may have led to selection bias in our study population. Our population had a fairly high level of baseline education which may have impacted their comfort with using and adjusting to new technology. Further, the average BMI of our participants was fairly low compared to the national averages of 29.5 for adult males and 30.1 for adult females 26 . Patients with a low BMI may have more flexibility in reaching each lung zone, or have less soft tissue to scan through thereby improving ease of obtaining interpretable images 27 .
Subjects enrolled in the study were assessed only once in their LUS self-exam and as a result we did not assess their ability to reliably perform the exam over time. As prior studies have shown that patients can reliably perform repeat self-medical evaluations such as blood pressure and/or blood glucose at home reliably, further longitudinal studies are needed to determine whether patients can reliably perform self- LUS and obtain interpretable scans over time.
Conclusions
As healthcare increasingly evolves towards providing care in alternative settings such as virtual telehealth visits or in patients’ homes with home hospital programs, portable tools that offer rapid, accurate data and can be self-implemented by patients will be needed. Here, we demonstrate that LUS when performed by healthy volunteers is not only feasible, but provides interpretable and diagnostic images. The applicability of these images to guiding clinical decision-making in home-based care should be explored.
Supplementary Information
Acknowledgements.
The authors would like to thank volunteer participants in this work for their partnership. This work is financially supported by the National Institute of Biomedical Imaging and Bioengineering Protocol Number R01EB027134 (Supplement). This work has not been previously presented at any conference or other proceedings.
Abbreviations
Author contributions.
A.J.G., T.K., and N.M.D. developed the concept for this work. S.S., L.A.S., and C.F. recruited volunteers and performed expert-level LUS. N.M.D. and A.J.G. performed blinded expert-review of novice-obtained and expert-obtained LUS scans. N.J. served as research assistant, managed and de-identified all data. I.W.Y.M. and N.M.D. performed statistical analyses and assisted with table and figure production. N.M.D. drafted the manuscript. All authors contributed to manuscript review and editing.
Data availability
Competing interests.
NMD reports no conflicts of interest. NJ reports no conflicts of interest. IMA supervises a trainee who receives financial support from Mitacs Business Strategy Internship grant. IMA is also the 3rd vice president and board of governor for the American Institute of Ultrasound in Medicine, and is the Governor-elect of the Alberta Chapter of the American College of Physicians. SS reports no conflicts of interest. LAS reports no conflicts of interest. CEF engages in consulting with Level Ex, is the former Chief Medical Officer of Centaur Labs, Inc, and currently owns equity in Centaur Labs, Inc. TK reports no conflicts of interest. AJG engages with consulting with Exo.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The online version contains supplementary material available at 10.1038/s41598-022-24513-x.

- Order Lab Tests
- Wellness Clinic
- All Radiology Services
- Schedule Home Imaging
- Schedule X-Ray
- Schedule MRI
- Schedule CT-Scan
- Schedule Ultrasound
Find A Doctor
- In-office consultation
- Online Consultation
- All Services
- Corporate Solutions
Patient Resource
- DPC Directory
- Medical Conditions
- How to order services
- Home Diagnostics
- Online Pharmacy
- Medical Procedure
- Wellness Plans
Wellness Programs
- Sleep Program
- Pharmacy Card
- Clinical Review Team
- Login Sign Up
Home Imaging Request
Patient information, home ultrasound.
Portable medical equipment has made ultrasound imaging more accessible and affordable than standard ultrasounds, allowing doctors to diagnose and treat patients more quickly and with greater ease and convenience. Using home ultrasound service has several advantages that have helped both patients and doctors.
Benefits of using home ultrasound service
- Accurate & Instant diagnosis
- Reduced wait times
- Accessible & cost-efficient
- Reduced hospital trips
- Comfortable & convenient
- Reduced risks of infection
Home Ultrasound Basics
What is an ultrasound, when are home ultrasounds used.
- Examining the uterus and ovaries to monitor the baby's development and health during pregnancy.
- Determining gallbladder disease.
- Evaluation of blood flow in blood vessels.
- Guiding procedures such as needle biopsy.
- Examining a lump in the breast.
- Detecting problems with the genitalia and prostate.
- Examining the inflammation in joints (synovitis).
- Determining metabolic bone disease
- Examining other abdominal organs, skin, and muscles.
How do Home Ultrasound scans work?
How to prepare for a home ultrasound scan.
Most ultrasound scans do not require any prior preparation. You may be asked to follow certain instructions before having some types of ultrasound scans to help improve the quality of the images produced.
For instance, you might be told to:
- Drink water and wait until after the scan to go to the bathroom - this may be required before a scan of your unborn baby or pelvic area.
- Avoid eating or drinking for several hours before the scan if your digestive system, including the liver and gallbladder, is being scanned.
You may be asked to remove some clothing and wear a gown depending on the area of your body being examined.
What happens during an ultrasound scan?
Ultrasound scans usually last 15 to 45 minutes. They are usually conducted by a doctor, a radiographer, or a sonographer. Depending on which body area is being scanned, several types of ultrasound scans are available. The main types are:
External Ultrasound scan: External ultrasound scans are most commonly used to examine the heart or a developing baby in the womb. It can also be used to examine the liver, kidneys, and other organs in the abdomen and pelvis and any other organs or tissues that can be seen through the skin, like muscles and joints. A small portable probe (transducer) is put on your skin and moved over the area to be examined. A lubricating gel is applied to your skin to allow the probe to glide smoothly. This also ensures that the probe is in constant contact with the skin. You shouldn't feel anything on your skin except the sensor and the gel (which is often cold). If you're having a womb or pelvic scan, you may have a full bladder, which causes little discomfort. Once the scan is completed, you may empty your bladder.
Doppler ultrasound: Doppler ultrasound is a type of ultrasound that evaluates the movement of materials in the body. It enables the doctor to examine and assess blood flow through the body's arteries and veins. Some Doppler ultrasounds include Color Doppler, Power Doppler, and Spectral Doppler.
Internal ultrasound scan Ultrasounds are sometimes performed inside the body. An internal examination allows a doctor to see within the body at organs such as the prostate gland, ovaries, or womb in greater detail. The transducer is connected to a probe that is inserted into a natural opening in your body in this case. Here are some examples.
Transvaginal Ultrasound: The term "transvaginal" refers to an ultrasound that is performed through the vagina. You'll be asked to lie on your back or side with your legs raised to your chest during the procedure. After that, a small ultrasound probe with a sterile cover is gently inserted into the vagina, and images are transmitted to a monitor. Internal examinations can be uncomfortable, but they usually aren't painful and don't take long.
Transrectal ultrasound: This test uses a special transducer inserted into the rectum to create images of the prostate.
Transesophageal echocardiogram: The doctor inserts the probe into the esophagus to obtain images of the heart.
Endoscopic Ultrasound An endoscope is inserted into your body, usually through your mouth, to examine areas such as your stomach or food pipe (esophagus) during an endoscopic ultrasound scan. The endoscope will be carefully pushed down towards your stomach while you lie on your side. On the end of the endoscope is a light and an ultrasound device. Sound waves are used to create images in the same way as an external ultrasound once inserted into the body. Because an endoscopic ultrasound scan might be uncomfortable and make you feel nauseous, you'll normally be given a sedative to keep you calm and a local anesthetic spray to numb your throat.
What happens after an ultrasound scan??
There are usually no side effects, and if no sedative was used, you can immediately drive, eat, drink, and resume your daily activities after the scan is completed.
If you had an endoscopic ultrasound and were given a sedative to help you rest, you should stay in the hospital for a few hours until the medication wears off. You should not drive, drink alcohol, or operate any machinery during this period.
The results of your scan may be given to you shortly after it is completed, but in most cases, the images will need to be analyzed before a report is provided to the doctor who referred you for the scan. They'll discuss the results at your next scheduled visit if one has been set up.
Are there any risks or side effects?
Home imaging form.

Thank you for requesting home imaging service. Our team will get back to you within 16-24 hours
Quick links
- Lipid Profile
- Creatinine, Serum
- Covid-19 Antibody Test
- Liver Function Test
- Basic Metabolic Panel
- Complete Blood Count (CBC)
- Comprehensive Metabolic Panel
For Patients
- Find a doctor
- Order Radiology
- Get a Wellness Check
- Schedule Procedure
- Order Home Testing Kits
- DPC Practices near me
- Patient Education
For Physicians
- Refer a patient to a specialist
- Order labs for patients
- Order radiology for patients
- Order At-Home Services
- Get your practice listed
For Companies
- CURA4U corporate plans
- Advertise With Us
- Terms & Conditions
- Privacy Policy
Returning Customer
New customer, select location.
Has been successfully added in your current order.
Physician's Order Request Policy
Please note that these services are not intended for any emergency medical situations. If you are having a life-threatening or serious condition that may require hospitalization, including, but not limited to, high-grade fever; low or high blood pressure; active serious infection, including, but not limited to, COVID; chest pain; shortness of breath; severe pain; or stroke-like symptoms, please call 911 immediately or go to a nearby emergency center as quickly as possible.
If you do not have a physician's order for labs or non-invasive radiology services, you may request it through our network of affiliated physicians/providers in selected states for an additional non-refundable fee, as listed (asynchronous consultation). Please note that an asynchronous consultation or physician-order service for diagnostics is not available for radiology tests requiring IV contrast. Patients needing a diagnostic study with IV contrast must complete an online visit with our physician first and, likely, will also need to have a lab test for their kidney function before a diagnostic study with IV contrast can be scheduled.
Once you request our provider or physician's order service, you will receive an email from us inquiring more details about your medical history. Based on the information you provide, one of our affiliated physicians or providers will make a determination about processing the order for the requested service. In some cases, as determined by our affiliated medical team, you may be required to provide additional clinical information or may be asked to have a more detailed online visit (an additional fee may apply) before your order can be processed. Please note that in some situations, or based on available clinical information, our team may even decide not to process the requested diagnostic order service and rather may recommend you to seek immediate medical attention in person or go to the nearest urgent care or ER. In that case, any advanced payment for the diagnostic service(s) will be refunded, but the physician's consultation or order request fee will remain non-refundable.
Please also note that any post-diagnostic service follow-up visit(s) or treatment(s) is not covered in this service fee and the ordering physician is not responsible to provide any continued care unless you sign-up for that service separately. Depending on your situation or test results, you may be advised to seek consultation with either primary care or a specialist physician (local or online) for further work-up and treatment. If you are unsure or have any questions, please call our customer support service before placing an order.
By clicking " Continue ", you agree to the policy, terms, and conditions.
Book Through Us
Detail form.

- Center on Health Equity and Access
- Health Care Cost
- Health Care Delivery
- Value-Based Care
How Point‐of‐Care Ultrasound May Improve At-Home Hospital Care
A recent review suggests point-of-care ultrasound can help home hospital care providers assess, diagnose, and monitor a range of conditions with relatively little additional training.
Throughout the COVID-19 pandemic, hospitals have been under severe stress and seen unprecedented strain placed on providers as well as the health care system overall. One way to mitigate this issue is hospital at home (HAH) programs, which facilitate care in eligible patients’ homes rather than the hospital. An article published in the Journal of Hospital Medicine explored the potential of point‐of‐care ultrasound (POCUS) to supplement care in HAH settings.
The number of HAH programs in the United States has grown to include 192 hospitals in 34 states with programs differing from hospital to hospital as well as patient needs. Overall, HAH programs have garnered positive patient and caregiver feedback and have not demonstrated negative effects on mortality or readmission thus far.
“As the house call's next iteration, HAH programs provide an exciting opportunity for hospitalists to enter our patients’ homes and lives,” the authors wrote. “Additional skills will be necessary for the competent home hospitalist—an expansion of purview without sacrificing the quality of care provided.”
POCUS, which is done at the bedside by health care professionals, has also become increasingly common in recent years. It provides a portable alternative to consultative imaging, and a recent survey conducted at large urban medical centers found that 93% of hospitalists considered POCUS a tool that can serve an important diagnostic purpose. In particular, the authors note that POCUS can assist with cardiopulmonary examination and diagnosis, which is commonly needed for HAH patients, in a relatively cost-effective way.
Working as a home hospitalist comes with unique challenges and requires skills to deal with the limitations of home care versus in-hospital care, and POCUS proficiency could be a very useful special skill in this setting. Advanced practice providers and nurses can perform POCUS exams, and the authors suggest that even patients may be capable of performing simple POCUS exams on themselves in the context of virtual HAH programs. One study cited in the article found that patients had a high success rate performing basic 4-zone lung ultrasounds on themselves in the context of titrating diuretic therapy—175 total lung zones were scanned, and 150 were interpretable with nearly 90% expert agreement.
Worsening heart failure is a common reason for home hospitalization, and POCUS can supplement examinations of patients presenting with dyspnea that is potentially related to heart failure. Lung ultrasound for diuretic effectiveness, inferior vena cava examination, and estimated jugular vena cava pulse validation are all strategies that providers proficient in POCUS could use to assist diagnosis in HAH settings. Nurses or patients could also be trained to perform relevant scans if an HAH program is largely virtual.
For post-surgical patients or those with inflammatory conditions, POCUS can help identify venous thrombosis and embolism. Detecting superficial thrombophlebitis in HAH settings via POCUS can spare patients with malfunctioning venous catheters visits to the hospital for the diagnostic ultrasound or line troubleshooting that a vascular access team would do within the institution. Kidney and bladder assessment with POCUS has been shown effective in identifying urinary retention and hydronephrosis, which elderly patients in HAH programs can be prone to.
“POCUS improves diagnostic accuracy over standard evaluation in the assessment of the acutely decompensating patient. This can crucially expedite management in resource‐limited settings where typical decision‐making supplements like blood tests and radiographs are not as readily available,” the authors wrote. “It may even allow the provider to identify a readily reversible cause that would have otherwise prompted transfer back to a brick‐and‐mortar institution.”
The authors concluded that POCUS can play an important role in HAH care and help providers assess, diagnose, and monitor a range of conditions with relatively little additional training. This could help minimize transfers to in-hospital care and maintain patient health and satisfaction within HAH programs. Additional research is warranted to quantify the effects of POCUS implementation on the rate of transfer to in-hospital care, the length of hospital stays, and costs.
Biggerstaff S, Restrepo D, Thompson R. POCUS at home: Point‐of‐care ultrasound for the home hospitalist. J Hosp Med. Published online August 28, 2022. doi:10.1002/jhm.12949

Health Equity and Access Weekly Roundup: April 27, 2024
Racial disparities in end-of-life care, the role of wellness and faith in minority health, award-winning research on health disparities, societal factors impacting cardiometabolic health, and rising mental health challenges among US youth are all covered this week in the Center on Health Equity and Access.

Updates on Adagrasib in CRC and the Importance of Genomic Testing With Dr Jun Gong
Jun Gong, MD, of Cedars-Sinai Medical Center, discusses the latest data on adagrasib in colorectal cancer, the importance of conducting genomic testing, and more.
What We’re Reading: Kaiser Permanente Data Breach; GSK Sues Pfizer, BioNTech; HIV Infections via Cosmetic Injections
Kaiser Permanente was hit by a data breach in mid-April, impacting 13.4 million health plan members; GlaxoSmithKline (GSK) sued Pfizer and BioNTech for allegedly infringing on its messenger RNA technology patents in the companies’ COVID-19 vaccines; the CDC announced the first-known HIV cases transmitted via cosmetic injections.
Managed Care Cast Presents: Insights Into Precision Medicine in NSCLC
In this podcast, a trio of experts discuss precision medicine in non–small cell lung cancer (NSCLC), current immunotherapies, and more.

Mental Health Diagnoses, Care Challenges Rise Among US Youth, Report Finds
While behavioral health care utilization has been rising, the treatment landscape has been worsening. New findings show that 20% of youths did not receive any form of treatment within 3 months of their initial behavioral health diagnosis.

Patients With DMD Receiving Eteplirsen Show Prolonged Survival, Study Finds
The study provides evidence of survival benefits among patients with Duchenne muscular dystrophy (DMD) receiving eteplirsen compared with the natural history of the condition.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777
Using Point-of-Care Ultrasound on Home Visits: The Home-Oriented Ultrasound Examination (HOUSE)
Affiliations.
- 1 Department of Emergency Medicine, University of Pennsylvania, Philadelphia, Pennsylvania.
- 2 Department of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania.
- PMID: 31587264
- DOI: 10.1111/jgs.16188
Publication types
- Diagnostic Imaging
- Home Care Services / trends*
- House Calls*
- Pilot Projects
- Point-of-Care Systems*
- Ultrasonography / instrumentation*
FindYourMomTribe » Parenting » Pregnancy
6 Things To Consider Before Getting A Private Ultrasound Scan
By Author Emma Martinez
Posted on Last updated: March 5, 2021

Should you get a private ultrasound scan? Is multiple scanning dangerous for your unborn child?
These questions and many others can be overwhelming with this new chapter in your life! But, that’s what I am here for – for answers to these and many other questions, keep reading!
If you’re expectant parents, I know just how excited you are about seeing your baby!
And of course, it would be awesome if you could see your little one in a more lifelike form than the one provided by the 2-D ultrasound from your doctor’s office.
That is one of the main reasons why private ultrasound scans have become extremely popular among parents, but before getting one (or a few), there are some things that need to be considered!
You probably already know that there is a wide array of private ultrasound facilities offering 3-D ultrasound and 4-D ultrasound services across the globe.
A quick Google search on “private ultrasound near me” provided so many options that I’d need a day just to make a decision about which one to choose.
But, despite the availability and popularity of these fetal keepsake images and videos, there are many warnings about the potential dangers of them.
From unregulated ultrasound scan providers to potential pregnancy complications due to multiple scanning, here is everything you need know before deciding to go for a private scan (or scans):
1. The Difference Between 2-D, 3-D, 4-D, And HD Ultrasounds
Ultrasound works on the principle of using sound waves to create an image of your little one in the womb. From 2-D to HD, different ultrasounds provide individual experiences:
2-D ultrasound

A 2-D ultrasound is the traditional black and white ultrasound image representing a flat cross-sectional view of your little one.
This type of ultrasound is typically done at a doctor’s office. With 2-D ultrasounds, you can see through the baby and her organs, as well as visualize their skeletal system.
This can help you to acquire information about your baby’s heart rate, and growth measurements, as well as to detect any potential irregularities.
3-D / 4-D ultrasound
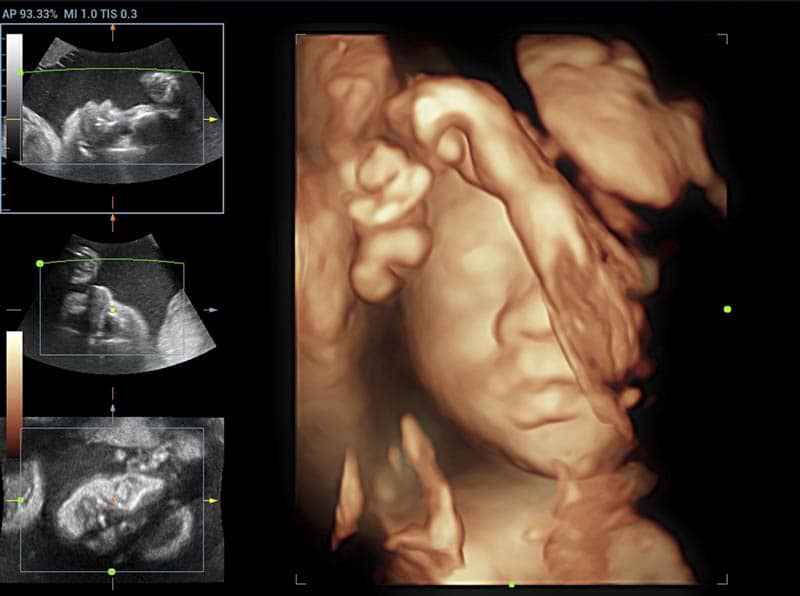
3-D ultrasounds use multiple 2-D images that are taken from different angles and then puts them together to create a 3-D (three-dimensional) image. 3-D ultrasound images allow you to see your little one’s outer appearance.
Now, do you know what happens when you combine a 3-D image with time? 4-D movements happen!
Yes, 4-D ultrasound is more advanced and it shows the baby’s movement in real-life motion (opening and closing of eyes, kicking, etc).
You can also see your baby’s facial expressions such as sucking the thumb or toe, yawning, and more!
Now you’re probably wondering why people don’t use 3-D and 4-D as a standard ultrasound session, right? The answer is simple.
While 3-D can allow you to see your baby’s external appearance, 2-D is the standard (developed by experts) for uncovering any irregularities and for tracking your little one’s development.
Still, there are some things that can’t be seen on 2-D ultrasounds and that’s when 3-D and 4-D come in handy. For example, if your baby has a cleft lip, this can only be seen in 3-D and 4-D ultrasound scans.
Given that such scans provide better visualization, they are also helpful when doctors and sonographers need to describe and explain any abnormality to parents.
HD ultrasound
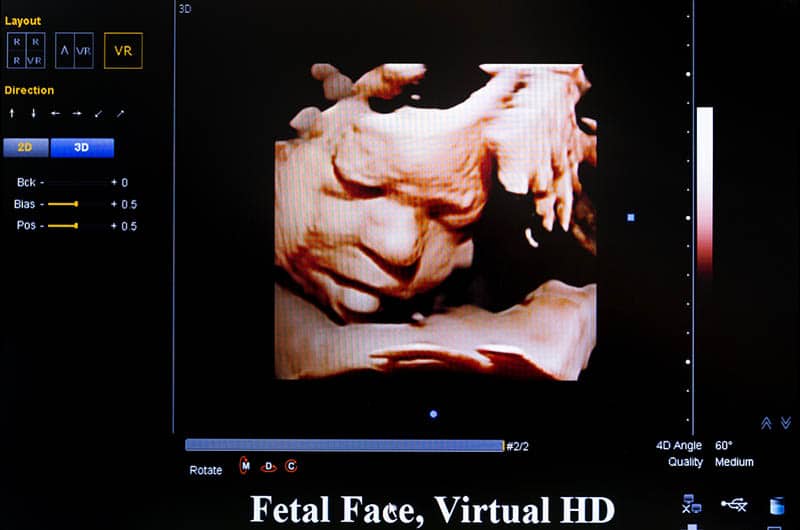
HD (High Definition) is the newest technology in the realm of ultrasounds. HD ultrasound imaging allows you to see the real skin tone and the baby’s face as if they were right in front of you.
Due to the light source that is adjustable, the HD live system allows the operator to play with shadowing and lighting effects creating a genuine display of your baby’s face.
Such images are smoother and more realistic than the ones in 2-D, 3-D, or 4-D.
Best of all is that you can also see your baby’s facial expressions such as smiling or when they’re yawning.
Yes, you can also see that in 3-D and 4-D, but the new HD ultrasound technology provides a more realistic experience.
HD live ultrasound allows you to share a real-time video of the baby with your family and friends. In case you’re wondering whether private ultrasound facilities offer different types of ultrasounds, the answer is: Yes.
Most private ultrasound facilities offer 3D/4D/HD ultrasound experiences.
2. Are Ultrasounds Safe For Your Little One?

Given that ultrasound uses sound waves that create an image of your little one in the womb, the process exposes the baby to the energy found in the form of heat. Sometimes (and under specific circumstances), this heat can cause birth defects.
Because of this, when performing ultrasounds, it is advisable to use an amount of power that is as low as possible and necessary.
Also, limiting the amount of time that is needed to obtain ultrasound images will prevent the baby from being overly exposed to this energy.
This principle is known as ALARA meaning “as low as reasonably achievable.”
ACOG (American College of Obstetricians and Gynecologists) endorsed the following statement from the American Institute of Ultrasound in Medicine:
“Although there are no confirmed biological effects on patients caused by exposures from present diagnostic ultrasound instruments, the possibility exists that such biological effects may be identified in the future. Thus ultrasound should be used in a prudent manner to provide medical benefit to the patient.”
There are two reasons why parents would want to get an ultrasound.
Some parents feel overly anxious about their little one (this is known as ‘scanxiety’), while others just want to check their baby without any medical reason or purpose.
If you’re getting an ultrasound scan for the purpose of managing the pregnancy by trained health care professionals, there’s nothing you should worry about.

3. Qualifications Of The Ultrasound Provider

If you’re interested in getting a 3-D or 4-D keepsake ultrasound scan (and not for the purpose of managing the pregnancy – medical scan), know that the provider of such ultrasounds will be primarily focused on creating a great photo or video for you.
They will not assess your baby’s development and health.
Unlike certified ultrasound facilities, sonographers at private ultrasound centers may not have the same experience and training.
If they notice some abnormalities or something similar, they may not feel comfortable sharing it with you or explaining the situation (or, as untrained professionals, they may not even notice it in the first place).
If something like that happens to you, then you need to visit your doctor and get another ultrasound scan, but this time the medical one.
Keep in mind that keepsake ultrasounds (known as commercial ultrasounds) can be falsely reassuring.
If the ultrasound provider is not a trained health care professional, they will not be able to tell you if something’s not right with the baby’s development.
Also, some parents tend to come to conclusions of their own, thinking that a nice photo of the baby’s appearance means a healthy baby.
I’m not trying to be a party pooper, but the only way to make sure that your baby is healthy is by getting a medical ultrasound.
Some unregistered private ultrasound centers don’t offer that. It is important that you always seek an OB/GYN that is a certified and registered diagnostic medical sonographer.
Most private ultrasound providers do acknowledge on their site that they don’t perform medical ultrasounds.
They also require expectant mothers to have a diagnostic ultrasound and documentation of their prenatal care.

The number one concern when it comes to safety when getting an ultrasound at a private ultrasound clinic is that the sonographer will not remember (or won’t care enough) to lower the power settings on the ultrasound machine or monitor for how long the baby is being exposed to this energy.
It’s important that the ultrasound equipment comes from the manufacturer who is responsible and knowledgeable about its proper usage so that they can pass this knowledge on to ultrasound providers.
Of course, the equipment needs to be properly inspected and serviced regularly for maximum safety.
Needless to say that some ultrasound providers don’t bother meeting those standards but rather opt to set up the ultrasound machine on their own without proper guidance or knowledge.
Not to mention improper isolation of the equipment that may lead to electric shocks.

For a pregnant woman / expectant parents having so many expenses from crib mattresses to finding the best travel high chair , 3-D and 4-D ultrasound keepsakes are definitely not cheap.
There are plenty of ultrasound packages, weekday specials, and other offers by the private ultrasound providers promising to give you a sneak peek into the magical world of your baby.
But, sometimes this sneak peek can literally break the bank (especially if done several times).
You should never skip a medical ultrasound provided by your doctor just because you’ve already got a non-medical (keepsake) ultrasound and now you’re convinced that your baby is perfectly healthy.
Don’t fall for this commercial trap, but rather make an investment in organic diapers or other things that will be necessary to you once your baby comes into the world.
As always, the choice is yours! (But, make sure that you don’t put your baby at risk due to an inadequate or multiple ultrasound scanning).
6. Your Expectations

Remember all those ultrasound images you’ve seen in different magazines? Or those magnificent ultrasound photos of your friends that you’re secretly jealous of?
Well, there are some valid reasons for those perfect images.
First of all, for an ultrasound image to look perfect (according to your standards of perfect), the baby needs to be surrounded by plenty of fluids and be in a good position.
To get a great ultrasound image, you may be required to do it multiple times, but keep in mind that this will increase the amount of energy to which your little one is exposed.
However, multiple images are still not a guarantee that you will be one hundred percent delighted with the photos and that they will be exactly what you expected and imagined.
We all know that we rarely get exactly what we desire, right? Right.
You’ve probably seen some scary ultrasound photos yourself and instantly got worried that something was wrong with the child in the photo because it looks weird.
Well, some 3-D images do look creepy but you shouldn’t immediately think that your baby is sick or something similar.
Here’s the secret to getting perfect ultrasound images:
Get a keepsake ultrasound between 24 and 28 weeks. The reason why you should do so is that at that period your baby won’t look so bony, but will be nicely filled out.
Also, there will be the right amount of fluid around your little one which will help make the photo look just perfect.
Perhaps the best bet would be to ask your doctor if they can do a 3-D or 4-D ultrasound after they’ve done a 2-D ultrasound.
They may be willing to do so, of course, assuming they have enough time and the required technology at their disposal.
Digital video or images of an ultrasound session provide a bonding experience for both parents and the baby.
Listening to your baby’s heartbeat for the first time is one of the most beautiful things in the world. Sharing videos and images of your unborn baby with your family and friends is also fulfilling.
But, still, you should avoid inadequate and multiple scanning. Expectant mothers should avoid elective ultrasounds (non-medical scans) and limit them to medical purposes.
Ultrasound scans should be performed by certified and trained health care professionals.
If you decide to get a private ultrasound scan, make sure that the ultrasound imaging facility has certified radiologists and sonographers in Obstetrics and Gynecology. Whatever you decide, good luck and I wish you happy parenting !
References:
• American Institute of Ultrasound in Medicine. (2005, September 12). “Beyond Tom Cruise – The Bigger Ultrasound Picture”.
READ NEXT: Get Prepped: The 36 Best Baby Things To Buy Before Birth
Like this post? Please share or pin it for later. You can also stay in the loop and follow us on Facebook , Instagram and Pinterest .
This post contains affiliate links. Please see our full disclosure for more info.
- Patient Care & Health Information
- Tests & Procedures
Diagnostic ultrasound, also called sonography or diagnostic medical sonography, is an imaging method that uses sound waves to produce images of structures within your body. The images can provide valuable information for diagnosing and directing treatment for a variety of diseases and conditions.
Most ultrasound examinations are done using an ultrasound device outside your body, though some involve placing a small device inside your body.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Assortment of Products for Daily Living from Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Ultrasound is used for many reasons, including to:
- View the uterus and ovaries during pregnancy and monitor the developing baby's health
- Diagnose gallbladder disease
- Evaluate blood flow
- Guide a needle for biopsy or tumor treatment
- Examine a breast lump
- Check the thyroid gland
- Find genital and prostate problems
- Assess joint inflammation (synovitis)
- Evaluate metabolic bone disease
More Information
- Abdominal aortic aneurysm
- Acute kidney failure
- Acute liver failure
- Acute lymphocytic leukemia
- Adenomyosis
- Adult Still disease
- Alcoholic hepatitis
- Ambiguous genitalia
- Anal cancer
- Appendicitis
- Arteriosclerosis / atherosclerosis
- Arteriovenous fistula
- Atelectasis
- Autonomic neuropathy
- Bladder stones
- Blood in urine (hematuria)
- Breast cancer
- Breast pain
- Carotid artery disease
- Cerebral palsy
- Cholestasis of pregnancy
- Chronic exertional compartment syndrome
- Chronic kidney disease
- Cleft lip and cleft palate
- Congenital adrenal hyperplasia
- Conjoined twins
- Deep vein thrombosis (DVT)
- Double uterus
- Down syndrome
- Ductal carcinoma in situ (DCIS)
- Endometrial cancer
- Endometriosis
- Enlarged breasts in men (gynecomastia)
- Enlarged liver
- Epididymitis
- Erectile dysfunction
- Eye melanoma
- Fibroadenoma
- Fibrocystic breasts
- Galactorrhea
- Ganglion cyst
- Glomerulonephritis
- Growth plate fractures
- Hamstring injury
- High blood pressure in children
- Hurthle cell cancer
- Incompetent cervix
- Infant reflux
- Inflammatory breast cancer
- Intussusception
- Invasive lobular carcinoma
- Iron deficiency anemia
- Ischemic colitis
- Kidney cancer
- Knee bursitis
- Liver cancer
- Liver disease
- Liver hemangioma
- Male breast cancer
- Mammary duct ectasia
- Median arcuate ligament syndrome (MALS)
- Menstrual cramps
- Miscarriage
- Morning sickness
- Morton's neuroma
- Multisystem inflammatory syndrome in children (MIS-C)
- Muscle strains
- Muscular dystrophy
- Myelofibrosis
- Neuroblastoma
- Nonalcoholic fatty liver disease
- Osteoporosis
- Ovarian cancer
- Ovarian cysts
- Painful intercourse (dyspareunia)
- Pancreatic cancer
- Patellar tendinitis
- Pelvic inflammatory disease (PID)
- Peripheral artery disease (PAD)
- Peyronie disease
- Placenta previa
- Placental abruption
- Polycystic kidney disease
- Polymyalgia rheumatica
- Post-vasectomy pain syndrome
- Precocious puberty
- Premature birth
- Preterm labor
- Prostate cancer
- Pulmonary embolism
- Pyloric stenosis
- Recurrent breast cancer
- Residual limb pain
- Retinal detachment
- Retinoblastoma
- Rotator cuff injury
- Sacral dimple
- Sacroiliitis
- Scrotal masses
- Secondary hypertension
- Solitary rectal ulcer syndrome
- Spermatocele
- Spina bifida
- Swollen knee
- Takayasu's arteritis
- Tapeworm infection
- Testicular cancer
- Thrombophlebitis
- Thyroid cancer
- Thyroid nodules
- Torn meniscus
- Toxic hepatitis
- Toxoplasmosis
- Tricuspid atresia
- Tuberous sclerosis
- Uterine fibroids
- Uterine prolapse
- Wilms tumor
- Zollinger-Ellison syndrome
Diagnostic ultrasound is a safe procedure that uses low-power sound waves. There are no known risks.
Ultrasound is a valuable tool, but it has limitations. Sound waves don't travel well through air or bone, so ultrasound isn't effective at imaging body parts that have gas in them or are hidden by bone, such as the lungs or head. Ultrasound may also be unable to see objects that are located very deep in the human body. To view these areas, your health care provider may order other imaging tests, such as CT or MRI scans or X-rays.
How you prepare
Most ultrasound exams require no preparation. However, there are a few exceptions:
- For some scans, such as a gallbladder ultrasound, your care provider may ask that you not eat or drink for a certain period of time before the exam.
- Others, such as a pelvic ultrasound, may require a full bladder. Your doctor will let you know how much water you need to drink before the exam. Do not urinate until the exam is done.
- Young children may need additional preparation. When scheduling an ultrasound for yourself or your child, ask your doctor if there are any specific instructions you'll need to follow.
Clothing and personal items
Wear loose clothing to your ultrasound appointment. You may be asked to remove jewelry during your ultrasound, so it's a good idea to leave any valuables at home.
What you can expect
Before the procedure.
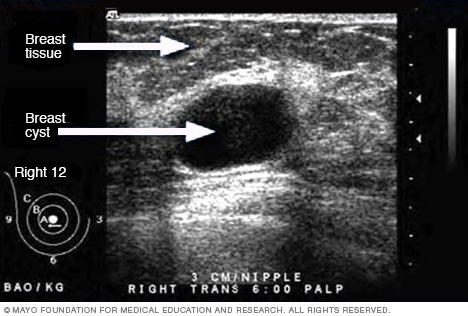
- Ultrasound of breast cyst
This ultrasound shows a breast cyst.
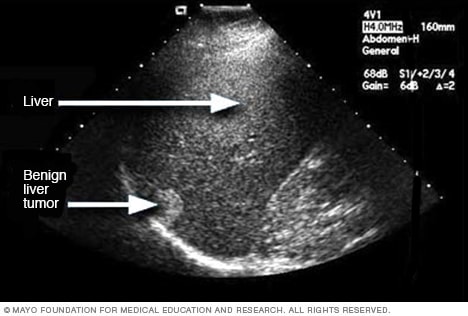
- Liver ultrasound
An ultrasound uses sound waves to make an image. This ultrasound shows a liver tumor that isn't cancer, called benign.

- Ultrasound of gallstones
This ultrasound shows gallstones in the gallbladder.
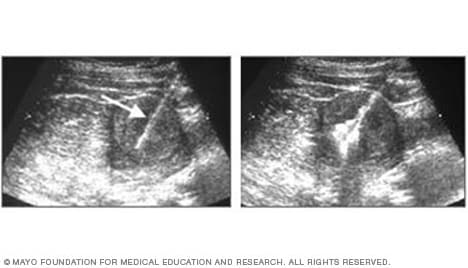
- Ultrasound of needle-guided procedure
These images show how ultrasound can help guide a needle into a tumor (left), where material is injected (right) to destroy tumor cells.
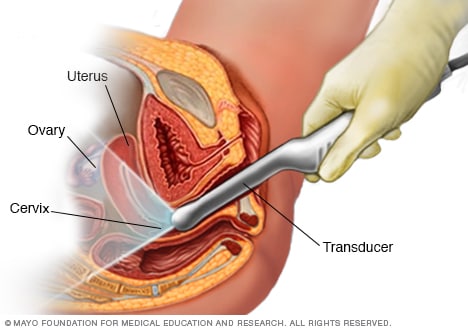
- Transvaginal ultrasound
During a transvaginal ultrasound, you lie on an exam table while a doctor or a medical technician puts a wandlike device, known as a transducer, into the vagina. Sound waves from the transducer create images of the uterus, ovaries and fallopian tubes.
Before your ultrasound begins, you may be asked to do the following:
- Remove any jewelry from the area being examined.
- Remove or reposition some or all of your clothing.
- Change into a gown.
You'll be asked to lie on an examination table.
During the procedure
Gel is applied to your skin over the area being examined. It helps prevent air pockets, which can block the sound waves that create the images. This safe, water-based gel is easy to remove from skin and, if needed, clothing.
A trained technician (sonographer) presses a small, hand-held device (transducer) against the area being studied and moves it as needed to capture the images. The transducer sends sound waves into your body, collects the ones that bounce back and sends them to a computer, which creates the images.
Sometimes, ultrasounds are done inside your body. In this case, the transducer is attached to a probe that's inserted into a natural opening in your body. Examples include:
- Transesophageal echocardiogram. A transducer, inserted into the esophagus, obtains heart images. It's usually done while under sedation.
- Transrectal ultrasound. This test creates images of the prostate by placing a special transducer into the rectum.
- Transvaginal ultrasound. A special transducer is gently inserted into the vagina to look at the uterus and ovaries.
Ultrasound is usually painless. However, you may experience mild discomfort as the sonographer guides the transducer over your body, especially if you're required to have a full bladder, or inserts it into your body.
A typical ultrasound exam takes from 30 minutes to an hour.
When your exam is complete, a doctor trained to interpret imaging studies (radiologist) analyzes the images and sends a report to your doctor. Your doctor will share the results with you.
You should be able to return to normal activities immediately after an ultrasound.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
- Andreas A, et al., eds. Grainger & Allison's Diagnostic Radiology: A Textbook of Medical Imaging. 7th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed Jan. 28, 2022.
- General ultrasound. RadiologyInfo.org. https://www.radiologyinfo.org/en/info/genus. Accessed Jan. 28, 2022.
- McKenzie GA (expert opinion). Mayo Clinic. Feb. 1, 2022.
- Chronic pelvic pain
- Ectopic pregnancy
- Fetal macrosomia
- Heavy menstrual bleeding
- Kidney stones
- Molar pregnancy
- Peritonitis
- Rheumatoid arthritis
- Soft tissue sarcoma
- Undescended testicle
- Urinary incontinence
News from Mayo Clinic
- Advancing ultrasound microvessel imaging and AI to improve cancer detection Oct. 13, 2023, 02:01 p.m. CDT
- Doctors & Departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
USG at home
Easy, comprehensive in-home usg services.
Sonography scans without hospital visits; ideal for bedridden patients.
Tikotra’s ultrasonography professionals can provide high-quality scans in the comfort of home. This service includes:
Expert-level scans just like in a hospital.
When you use our USG at home service, you’re still benefiting from hospital-grade treatment
Practised technicians for high-quality scans.
Our Sonologists have a wide range of experience offering in-home USG support
Same-day reporting for fast results.
Don’t wait weeks for your scans to come back. Recuperating or bedridden patients enjoy sonography/ultrasonography reports that day
Private appointments in the comfort of home.
Have your USG appointment in complete privacy, at your bedside
Time-saving scheduling with planned visits.
No waiting rooms, Your sonography/ultrasonography technician will visit your home on the booking date
Blood clot scans to detect issues early.
Easily check for blood clots via a carotid Doppler test or carotid ultrasound, blood flow meter, Limb Arterial or Venous Doppler test at home
Body cavity scans to aid in diagnosis.
Book a high-quality abdominal or pelvic ultrasound, renal or KUB USG at home
Routine check-ups for your peace of mind.
Even if you’re bedridden, book your USG scan at home to stick to your preventive care plans
Specialist reviews are available if needed.
Should your USG report contain anything concerning, a specialist doctor can offer interpretation online without delay
Get your USG done at home for a change
Our healthcare team is ready to serve you. Let us know your requirements in the live chat.
Testimonials
Dear Ms. Nathiya,... Show More ...Thanks for all the support extended to us in scheduling the doctor for my mother From picking up our call late in the night and follow up to check till the doctor visited us, you had been very professional and helpful. The doctor patiently examined and suggested remedies for my mother Regards, Vijaylaksmi Mrs. Vijaylaksmi
Hi Team,... Show More ... I have taken ECG for my mother-in-law Excellent patient service with good guidelines. Thank you so much Josiwin Wonderful support Thanks and Regards Mrs. Kalpana
This I have to give special note that, when I was in trouble regarding my husband’s health condition... Show More ... The timely help rendered by you can’t be forgettable Guru Nathan Mr. Gurunathan
I got to know about Tikotra through Google.... Show More ... They provide home services for various diagnostic tests. I got my ultrasound abdomen done and overall it was real smooth and comfortable experience for me. The Dr who did my scan, Dr Selvi is an excellent doctor and a very nice person as well. The test went on smoothly and I was very comfortable doing the test at my own home and in my comfort. Joswin mam from Tikotra had organized the home test for me. She is a really nice and professional person. She has been very patient and kind towards me. Thank you Tikotra for providing such excellent service at my home. A special thank you to Dr Azaku Tamil Selvi and Josiwin mam. I highly recommend Tikotra to anyone who is looking for healthcare services at home. By, A very satisfied and happy customer of Tikotra :) Ms. Chopra
Why Tikotra?
Packages for all requirements
Same Day Service
For most locations and services
Comprehensive Service
Full suite of healthcare services at home
Hospital Grade
Highest quality care at home

- Mission, Vision, Values
- Our Leadership
- No Surprises Act
- Medical Records
- At Home Patients & Programs
- Commercial Markets
- Government Agencies
- Correctional Institutions
- Digital X-ray
- Ultrasound and EKG
- Laboratory Services
- Lab Outreach Services
- Vascular Access
- Get TridentCare Services
- In The News
At Home Services

TridentCare Account Request
Exam Request Form for TridentCare Imaging At Home Orders
For specific questions related to TridentCare At Home, please email us directly:
[email protected]
Exclusively designed for patients in the comfort of home.
TridentCare At Home has been providing comprehensive, high-quality mobile diagnostic imaging services for more than thirty-five years. Our team of dedicated medical professionals are focused on delivery the highest levels of patient care in a variety of settings.
We proudly partner with physician groups, hospital-at-home programs, home health and hospice care organizations to quickly and accurately complete the diagnostic imaging exams requested, in the privacy and comfort of the patient’s home. Private insurance and Medicare Advantage plans accepted.

Digital X-ray Services
Hospital-quality images at home
Images transmitted to reading radiologist from patient’s home
Technologists certified by ARRT
Dedicated, Caring TridentCare At Home Team
Professionally-trained to serve patients at home
Federal and state background and security checks
Same day service availability
Ultrasound Services
Including vascular, arterial, cardiac, and general studies
Sonographers ARDMS-certified
Interpreted by radiologist and cardiologist
Fast online ordering and results
Order exams through Trident Connect
Easy online access to patient history and results
HIPAA-compliant security
Visit www.tridentconnect.com for more info

Streamlined operations
TridentCare At Home brings the most advanced imaging services in the comfort and safety of your patients’ homes. Our electronic ordering and reporting system is fast, easy, and accurate. TridentCare offers secure Web access, allowing your medical team to quickly and efficiently access information – including digital images and results – whenever needed. Our paperless system saves time, reduces errors and offers rapid turnaround time in receiving results. Access to images and results is available 24/7 to you as the provider from your smartphone, laptop, tablet or PC.

What Is Home Visiting?
Early childhood home visiting is a service delivery strategy that matches expectant parents and caregivers of young children with a designated support person—typically a trained nurse, social worker, or early childhood specialist—who guides them through the early stages of raising a family. Services are voluntary, may include caregiver coaching or connecting families to needed services, and provided in the family's home or another location of the family's choice.
Home visiting is a holistic, two-generation approach.
Home visiting views child and family development from a holistic perspective that encompasses child health and well-being, child development and school readiness, positive parent-child relationships, parent health and well-being, family economic self-sufficiency, and family functioning. A two-generation approach with a lengthy history , home visiting delivers both parent- and child-oriented services to help the whole family thrive. Although services differ across models, home visitors typically—
Gather Family Information to Tailor Services
- Screen caregivers for issues like postpartum depression, substance use, and domestic violence
- Screen children for developmental delays
Provide Direct Education and Support
- Provide knowledge and training to make homes safer
- Promote safe sleep practices
- Offer information about child development
Make Referrals and Coordinate Services
- Help pregnant women access prenatal care
- Check to make sure children attend well-child visits
- Connect caregivers with job training and education programs
- Refer caregivers as needed to mental health or domestic violence resources
Discover more in our Primer and At a Glance resources.
Home visiting outcomes are supported by research.
Research shows that voluntary home visiting programs help improve infant and maternal health, develop safe homes and nurturing relationships to prevent prevent child abuse and injury or mortality, support early learning and long-term academic achievement, and make referrals and coordinate services. Studies have found a return on investment of $1.80 to $5.70 for every dollar spent. This strong return on investment is consistent with established research on other types of early childhood interventions.
Learn more about the benefits .
Many models are evidence based or on the path to becoming so.
Programs choose from a variety of models to implement with families, each suited to differing community needs, target obstacles, and available resources. The Home Visiting Evidence of Effectiveness (HomVEE) project administered by the U.S. Department of Health and Human Services has issued a set of criteria for evidence of model effectiveness. Models that meet criteria are deemed evidence based. NHVRC surveys evidence-based and emerging models at the national, state/local, and tribal levels annually to provide a comprehensive assessment of the landscape in our Yearbook .
Visit our model profiles for details on individual models.
Home Visiting Primer READ

Stay up to date on the latest home visiting information.
- 24/7 service available 847-543-0045
- see our brochures download now

Home Visiting Physicians
Be seen right at your home and start the care you need..
Your health is our priority! Your course of treatment will never be just about diagnosis, test results, and medications; it will also be about helping you reach the highest quality of life. We do this by actively listening and understanding your personal goals so we can tailor a plan-of-care that will be created with you in mind.
Where can we come?
These services can be utilized wherever the patient resides – whether that be in their home or in a facility.
Contact Us Today
What we offer
A primary care home visit by one of our board certified and caring medical providers. A visit may be for acute concerns, regular follow-up, and annual physicals.
Comprehensive medical exam in the comfort of your home; which may include orders for blood test, urine test, radiological imaging, medication prescription, and/or specialty referral.
The ability to directly reach your medical provider for any questions or concerns over the phone or email.
New prescription and renewals sent electronically to your pharmacy of choice within 24-hours
We are here to help when you need us
Free download resources.
Meridian Health Care is proud to offer the following resources for you.
- Home Health Care
- Hospice Care
- Palliative Care
- Our Mission & Vision
- Our Leadership
- Our Proud History
2018 Primetime Emmy & James Beard Award Winner
R&K Insider
Join our newsletter to get exclusives on where our correspondents travel, what they eat, where they stay. Free to sign up.
A History of Moscow in 13 Dishes
Featured city guides.
Related Guides:
Moscow Neighbourhoods, Locations and Districts
(moscow, central federal district, russia), city centre, tverskoy district, arbat district, barrikadnaya. district, khamovniki district, chistye prudy district, zamoskvorechie district, zayauzie district.
© Copyright TravelSmart Ltd
I'm looking for:
Hotel Search
- Travel Guide
- Information and Tourism
- Maps and Orientation
- Transport and Car Rental
- SVO Airport Information
- History Facts
- Weather and Climate
- Life and Travel Tips
- Accommodation
- Hotels and Accommodation
- Property and Real Estate
- Popular Attractions
- Tourist Attractions
- Landmarks and Monuments
- Art Galleries
- Attractions Nearby
- Parks and Gardens
- Golf Courses
- Things to Do
- Events and Festivals
- Restaurants and Dining
- Your Reviews of Moscow
- Russia World Guide
- Guide Disclaimer
- Privacy Policy / Disclaimer

IMAGES
VIDEO
COMMENTS
To our knowledge, this is the first report on the use of this technology with the home visit population. METHODS. A geriatrician with an established home visit practice in a large US city and an internal medicine physician participating in a dedicated point-of-care ultrasound (POCUS) fellowship 5 identified visits that would be ideal for this ...
See the Future. The first and only home ultrasound. for remote and reliable professional care. Pulsenmore (TASE:PULS) is a world leader in self-scan ultrasound devices for remote clinical diagnosis and screening. Our home ultrasound solutions improve access and continuity of care, providing efficiency that benefits clinicians and patients alike.
Limited ultrasound exam of arm/leg joint, tendon, or muscle: 76882: $58.10: Ultrasound-guided needle placement for abscess aspiration: 76942: Bill separately for the incision and drainage (10160 ...
As home-based initiatives evolve into a pillar of healthcare delivery, portable tools to facilitate diagnostics and therapeutics in alternative care settings such as patient homes must be explored. Point-of-care ultrasound (POCUS) is a low-cost, radiation-free imaging modality that offers real-time data to aid medical care.
Home Ultrasound is commonly used to monitor the growth and development of the fetus during pregnancy. The exam, however, has a wide range of applications. +1-888-360-0001 8:00AM to 6:00PM EST For Physicians ... Please also note that any post-diagnostic service follow-up visit(s) or treatment(s) is not covered in this service fee and the ...
Biggerstaff S, Restrepo D, Thompson R. POCUS at home: Point‐of‐care ultrasound for the home hospitalist. J Hosp Med. Published online August 28, 2022. doi:10.1002/jhm.12949 Related Videos
Using Point-of-Care Ultrasound on Home Visits: The Home-Oriented Ultrasound Examination (HOUSE) J Am Geriatr Soc . 2019 Dec;67(12):2662-2663. doi: 10.1111/jgs.16188.
From unregulated ultrasound scan providers to potential pregnancy complications due to multiple scanning, here is everything you need know before deciding to go for a private scan (or scans): 1. The Difference Between 2-D, 3-D, 4-D, And HD Ultrasounds. Ultrasound works on the principle of using sound waves to create an image of your little one ...
Overview. Diagnostic ultrasound, also called sonography or diagnostic medical sonography, is an imaging method that uses sound waves to produce images of structures within your body. The images can provide valuable information for diagnosing and directing treatment for a variety of diseases and conditions. Most ultrasound examinations are done ...
Easy, comprehensive in-home USG services. Sonography scans without hospital visits; ideal for bedridden patients. Chat with us Call 1800-313-1883. Tikotra's ultrasonography professionals can provide high-quality scans in the comfort of home. This service includes:
TridentCare At Home has been providing comprehensive, high-quality mobile diagnostic imaging services for more than thirty-five years. Our team of dedicated medical professionals are focused on delivery the highest levels of patient care in a variety of settings. We proudly partner with physician groups, hospital-at-home programs, home health ...
1 They raise several opportunities for additional point-of-care ultrasound (POCUS) modalities as useful in the home visit including examinations of soft tissue, the musculoskeletal system, and the ...
All of this means fewer in-person appointments and that some non-urgent ones will be done over phone or video chat instead. For example, at Michigan Medicine, they're typically only seeing pregnant women 5 times before birth: Initial prenatal visit. Anatomy ultrasound. 28-week check-up. 36-week check-up. 39-week check-up.
This digital home visit checklist covers the patient's immobility, nutrition, home environment, other people, medications, examination, safety, spiritual health, and other services needed (INHOMESSS). Used with SafetyCulture (formerly iAuditor) on a mobile device, this home visit checklist allows you to: Make notes on corresponding areas of ...
CLARIUS L7 HD3. Price: $4,190. 192e. Android, and iOS compatible. Clarius is a big name in the ultrasound scanning industry. Clarius has proved them over and over in their respective field. Their L7 HD3 design is one of the best inventions. This ultrasound scanner works fantastic for home and professional use.
Early childhood home visiting is a service delivery strategy that matches expectant parents and caregivers of young children with a designated support person—typically a trained nurse, social worker, or early childhood specialist—who guides them through the early stages of raising a family. Services are voluntary, may include caregiver ...
Walking tour around Moscow-City.Thanks for watching!MY GEAR THAT I USEMinimalist Handheld SetupiPhone 11 128GB https://amzn.to/3zfqbboMic for Street https://...
What we offer. A primary care home visit by one of our board certified and caring medical providers. A visit may be for acute concerns, regular follow-up, and annual physicals. Comprehensive medical exam in the comfort of your home; which may include orders for blood test, urine test, radiological imaging, medication prescription, and/or ...
HOME SONOGRAPHY
The safety of you and your household always comes first. There's also a video option if you choose to have your visit via smartphone, tablet, or computer. Call to schedule your no-cost, In-Home Visit now. And stay healthy and safe. 1-844-226-8216. Disclaimer. Blue Cross Blue Shield of Michigan offers home visit benefits to UAW Trust members.
1: Off-kilter genius at Delicatessen: Brain pâté with kefir butter and young radishes served mezze-style, and the caviar and tartare pizza. Head for Food City. You might think that calling Food City (Фуд Сити), an agriculture depot on the outskirts of Moscow, a "city" would be some kind of hyperbole. It is not.
Edged by the streets of Lubyansky, Mokhovaya, Okhotny and Teatralny, Moscow city centre is where it all happens and is home to many of the city's most famous landmarks. Red Square (Krasnaya Ploshchad) is situated directly alongside the north-eastern side of the Kremlin itself and is dominated on its southerly side by the iconic 16th-century St ...