

Navigating Vertigo After Dental Work: Understanding Causes and Solutions
Introduction:.
Experiencing vertigo after dental work can be disconcerting and raise questions about its underlying causes and management. In this comprehensive guide, we’ll address common queries and concerns surrounding vertigo following dental procedures, offering insights into potential triggers and strategies for symptom relief.
FAQs on Vertigo After Dental Work:
Can a bad tooth cause vertigo.
- Yes. Dental issues such as infections or abscesses can potentially lead to vertigo. The inner ear’s proximity to the oral cavity means that inflammation or infection in the teeth or gums can affect the vestibular system, triggering vertigo symptoms
How Long Does Dizziness Last After Tooth Extraction?
- Dizziness following tooth extraction can vary from person to person. Typically, it may last for a few hours to a couple of days post-procedure. However, if dizziness persists or worsens, it’s essential to consult your dentist or healthcare provider for further evaluation.
Can Dental Work Cause Inner Ear Problems?
- Yes. Certain dental procedures, especially those involving the lower jaw or proximity to the inner ear, can potentially lead to inner ear disturbances and vertigo. This is often due to the manipulation of the jawbone or pressure exerted on nearby structures during dental interventions.
How to Avoid Vertigo at the Dentist?
- Communicate any history of vertigo or vestibular issues with your dentist before undergoing any procedures. Additionally, consider using relaxation techniques or sedation options if anxiety exacerbates vertigo symptoms during dental visits.
What Causes Dizziness After Tooth Extraction?
- Dizziness following tooth extraction can stem from various factors, including changes in blood pressure, pain medication side effects, or positional changes during the procedure. It’s crucial to follow post-operative care instructions provided by your dentist to minimize discomfort and dizziness.
Can a Wisdom Tooth Cause Vertigo?
- Yes. Impacted wisdom teeth or complications arising from their extraction can potentially lead to vertigo. Wisdom teeth removal procedures may involve manipulation near the temporomandibular joint (TMJ) or adjacent structures, potentially affecting vestibular function.
Can a Cavity Cause Dizziness?
- While cavities themselves may not directly cause dizziness, untreated dental issues such as infections or abscesses can lead to systemic inflammation and potential vestibular disturbances, contributing to dizziness or vertigo.
Dizziness After Root Canal: Is It Normal?
- It’s not uncommon to experience mild dizziness or lightheadedness following a root canal procedure due to factors such as stress, changes in blood pressure, or medication effects. However, persistent or severe dizziness warrants further evaluation by your dentist or healthcare provider.
Can Braces Cause Dizziness?
- Braces themselves typically do not cause dizziness. However, the initial adjustment period or discomfort associated with orthodontic treatment may lead to transient feelings of lightheadedness in some individuals.
Can Dental Problems Cause Dizziness?
Yes. Dental problems such as infections, abscesses, or temporomandibular joint (TMJ) disorders can potentially cause dizziness or vertigo. It’s essential to address underlying dental issues promptly to minimize associated symptoms and complications.
Can Novocaine Make You Dizzy?
While rare, some individuals may experience dizziness or lightheadedness as a side effect of local anesthetics such as Novocaine used during dental procedures. If you experience significant dizziness or other adverse reactions, inform your dentist immediately for appropriate management.
Conclusion: Navigating vertigo after dental work requires a nuanced understanding of potential triggers and effective management strategies. By addressing common queries and concerns surrounding vertigo following dental procedures, individuals can proactively alleviate discomfort and enhance their dental care experience. Remember to communicate any pre-existing vestibular issues with your dentist and seek timely medical attention if dizziness persists or worsens post-treatment. With informed decision-making and proactive symptom management, you can navigate dental visits with confidence and ease.
Addressing Vertigo Naturally with DiVertigo:
In addition to understanding the potential causes and management strategies for vertigo after dental work, it’s essential to explore natural remedies that can complement traditional approaches. DiVertigo offers a natural, drug-free solution for alleviating vertigo symptoms and promoting vestibular health.
How DiVertigo Works: DiVertigo harnesses the power of natural essential oils, including Lavender, Peppermint, and Frankincense, to provide fast-acting relief from vertigo and motion sickness. By inhaling the soothing aroma of these botanical extracts, individuals experiencing vertigo can experience a sense of calm and balance, helping to mitigate discomfort and regain equilibrium.
Benefits of DiVertigo:
Fast-Acting Relief: DiVertigo offers rapid relief from vertigo symptoms, providing comfort and reassurance during episodes of dizziness or imbalance. Drug-Free Solution: Unlike traditional medications that may carry side effects or interactions, DiVertigo offers a natural, non-pharmaceutical alternative for managing vertigo safely and effectively. Convenient Application: DiVertigo’s compact size and easy application make it ideal for on-the-go use, ensuring relief is readily accessible whenever and wherever vertigo strikes. Experience Relief Today: Whether you’re navigating vertigo after dental work or managing symptoms in daily life, DiVertigo offers a natural way to find relief and regain control over your vestibular health. Discover the soothing benefits of DiVertigo and take proactive steps towards a more balanced, symptom-free lifestyle.
By incorporating information about DiVertigo as a natural remedy for vertigo, readers can explore additional options for managing their symptoms and enhancing their overall well-being.

View all posts
Previous Post Will Benign Paroxysmal Positional Vertigo (BPPV) Go Away on Its Own?
Next post can benign paroxysmal positional vertigo (bppv) cause headaches, recommended for you, essential oils for vertigo.

I have Vertigo. Could it be Multiple Sclerosis Vertigo?
Types of vertigo.
Comments are closed.
Sign Up For Our Newsletter
Email address:
Statements on this website have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
© 2024 DiVertigo. All Rights Reserved | 100% money-back guarantee | 727-842-7544 | 1-888-212-5503
- Product Info
- Testimonials

Dental Vertigo: What Causes It?
by Dr. Kim Bell, DPT | Dec 30, 2021 | Blogs , BPPV , Clinical Practice , Dizziness , Dizziness Lying Down , Dizziness Rolling Over , FAQs , Kimberley Bell, DPT , Physical Therapy , Preventing Falls , The Bell Method , Vertigo , Vestibular Rehabilitation , Walking Stability

Vertigo from dental treatment is a common complaint among my patients. Many of my patients experienced vertigo at or after the dentist. In this article, I will share five possible causes of dental vertigo.
Causes of Dental Vertigo
1. vertigo from neck strain.
When you are reclined in the dental chair with your head turned to the side, that is a very awkward position for your neck. If you remain that way for more than a few minutes, your neck can come out of alignment. This especially affects the first and second cervical vertebrae, the C1 atlas bone and C2 axis bone.
If you notice that your neck is making crunching, popping, grinding, clicking, or clunking sounds when you turn your head from side to side, then you may have cervical vertigo. To learn more about this root cause, click here .
2. Vertigo from TMJ
Very close to the neck is the temporomandibular joint. This jaw joint is also known as TMJ. Some TMJ issues after dental work include a TMJ sprain, inflammation of the TMJ, or TMJ alignment issues.
Opening your mouth extremely wide as you might do at the dentist can cause a sprain to the TMJ. Other activities that can sprain the TMJ include yawning extremely wide or taking a bite out of a really big sandwich. TMJ sprain as a cause of dental vertigo is more likely if you have to open your mouth really wide.
Another risk factor for TMJ as a cause of dental vertigo is having force or pressure applied to your lower teeth or lower jaw. This may occur during dental surgery or more extensive procedures involving the lower teeth.
3. Vertigo from BPPV
BPPV is the most common inner ear cause of vertigo. If you already have BPPV, then reclining in the dental chair may trigger a spin for you. The spin should hopefully only last for a minute or two, but maybe quite intense. You may spin again or your spin may get worse when you tilt your head to the side while reclined. If you have BPPV, you may also spin again for a minute or two when you stand up after you finish.
If you do not already have BPPV, certainly the drilling involved with some dental surgeries can cause a new onset of BPPV. The crystals in your inner ear can get shaken loose from the vibration of drilling.
If you have a new onset of BPPV from dental care, you may feel weird after the dental work. Your strange feelings may get better over time, but may not resolve completely until you have the BPPV successfully treated.
Someone may experience dental vertigo due to a current case of BPPV, or new onset of BPPV. In either case, BPPV treatment is the best next step.
4. Vertigo from Viral Attacks
If you have a history of cold sores (or fever blisters) around your mouth or lips, then dental work can trigger an oral herpes outbreak. This can happen even if you have not experienced any cold sores for many years.
This viral attack triggered by dental work can cause cold sores to show up on your lips. The oral herpes virus may even travel down your vestibular nerve to attack your inner ear. That causes the second most common inner ear cause of vertigo, vestibular neuritis .
In this case, vestibular neuritis is caused by a virus. This type of vertigo usually starts a day or more after the dental procedure and is intense.
Antiviral medication can treat or help prevent viral vestibular neuritis. If you are prone to viral attacks after dental procedures, you may want to discuss pre-medicating with your doctor or dentist.
5. Vertigo from Bacterial Infection or Abscess in upper molar
If you end up getting a bacterial infection or abscess, especially in your upper molar, that can cause dental vertigo. Similar to the viral attack, the bacterial infection or abscess may not occur right away. Bacterial infections may build up a day or more after the dental procedure.
In that case, antibiotics would likely be prescribed by your dentist or oral surgeon to address the bacterial infection. However, some antibiotics are ototoxic. This means that certain medications used to treat bacterial infections may cause temporary or permanent damage to your ears and vestibular system.
Also in some cases, the bacterial infection can spread out and affect your vestibular system, which is located near your upper molars. Vestibular neuritis caused by a bacterial infection is a complication to dental work that does affect some unfortunate people. Not everyone who gets a bacterial infection or abscess after dental work will get a bacterial case of vestibular neuritis.
I recommend you always read up on medication side effects when you get a new prescription filled. Sometimes your doctor can recommend another antibiotic medication that is not ototoxic. Other times, your doctor may decide that the benefit of the medication to fight the infection is worth the potential risk of damaging your ears.
I hope this summary of some of the causes of dental vertigo is helpful. If you would like to learn more about how I help people with dental vertigo and/or dizziness, schedule a consultation today !
To learn more about the connection between teeth and vertigo, visit this page .
For tips, if you get dizzy at the dentist, check out this article .
This blog is provided for informational purposes only. The content and any comments by Dr. Kim Bell, DPT are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. The details of any case mentioned in this post represent a typical patient that Dr. Bell might see and do not describe the circumstances of a specific individual.
Hello I would like to set a consultation up I’m currently dealing with off balance issues after having veneers put on they cracked a tooth and I been suffering since
Hi Roberta,
I am sorry to hear about this!
Please click here to learn how to Request a Consultation.
Kim Bell, DPT
Hello Dr Bell 3months ago I had crowns put on my upper central incisors, I was in the chair for 1 hr without a pillow. I have a small mouth 33mm and it was stretched open wide. I have no history of ENT nor TMJ issues. The next day I woke up with extreme dizziness which lasted for 4 days with tinnitus. I took a 1 hr flight and my symptoms got worse, clicking, blocked ears, fullness. I was diagnosed with Eustachian Tube Dysfunction and I’m on steroid nasal drops. The tubes still aren’t opening and closing properly. It’s very frustrating. Can you tell me what you think might have caused the acute onset of ETD?
I am sorry to hear what you are going through!
I cannot speculate on what might have caused the acute onset of ETD, since I do not know you or the details of your case.
However, I suggest that you consult and OtoNeurologist or Neurotologist or Otologist. You can search for a provider at Vestibular.org .
I hope that you find answers and relief soon!
Hi Jane I had the same thing happen 7 days ago. I’m still dizzy.
What did you do to make it better?
I had a root canal started the other day and woke up the next day dizzy and nauseous. My theory is that vertigo may have been simmering and the position and vibration shook things loose. Needless to say I am worried about finishing the procedure. The dental field seems very j educated about this. I wonder if taking a meclizine before the procedure would cut down on the possibility of it happening again.
I had a dental implant two years ago. Due to the fact that my bone density in my upper right cheek was shrinking I needed to have the back two teeth made into an implant. I had to have artificial bone put in and my sinus lifted. The whole thing took about five months. After the procedure was completed I woke up next day not being able to get out of bed. I was nauseous and had to be helped out of bed. Luckily I had a PT appointment that day and she did the epley maneuver. I felt like I was having a seizure. This alleviated the worse of it. But the dizziness never completely went away. I’ve seen just about all the doctors and have had just about every test. My latest procedure is Botox. Do you have any suggestion?
You may be interested in this article that I wrote on the connection between Teeth & Vertigo.
You may want to find a vestibular physical therapist to assess you. You may require different types of maneuvers or exercises to recover from this incident.
I wrote this article discussing five reasons why the Epley maneuver may not help.
You can also talk to your primary care provider to find out if medication would be appropriate for your current situation.
I hope you feel better soon!
Submit a Comment Cancel reply
All blog comments submitted using this form are subject to editorial review. Comments may be edited before publication, or may not be published at all, based on our review of the content. If you submit a comment on this blog, please note that it may become public information. Do not include any information you do not want disclosed or associated with your name. If your comment is published, your email address will not be published. Blog content is provided for informational purposes only. This website is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Have You Seen? Over 3 Million views!

Recent Posts
- What Is Viral Vertigo?
- What Is Horizontal Canal BPPV?
- Can Your Posture Cause Dizziness?
- Clinical Practice (79)
- Dizziness (85)
- Dizziness Lying Down (47)
- Dizziness Rolling Over (47)
- Fear of Falling (25)
- Foot Neuropathy (5)
- Geriatric Fall Prevention (46)
- Incontinence (5)
- Kimberley Bell, DPT (70)
- Laughter (1)
- Migraines (26)
- My Healing Journey (28)
- Normal Aging (30)
- Nystagmus (7)
- Physical Therapy (71)
- Preventing Falls (46)
- San Diego (41)
- Shuffling Feet (8)
- The Bell Method (87)
- Tinnitus (4)
- Travel Tips for People with Dizziness (4)
- Vertigo (73)
- Vestibular Rehabilitation (74)
- Walking Stability (50)
Walk with Me
Subscribe to our blog.
Enter your email to subscribe and receive notifications of new posts and helpful information from Dr. Kim Bell, DPT.
Accessibility Toolbar
- Powered with favorite Love by Codenroll
Pin It on Pinterest
Share this post with your friends!
- Patient Care & Health Information
- Diseases & Conditions
- Benign paroxysmal positional vertigo (BPPV)
Benign paroxysmal positional vertigo (BPPV) is one of the most common causes of vertigo — the sudden sensation that you're spinning or that the inside of your head is spinning.
BPPV causes brief episodes of mild to intense dizziness. It is usually triggered by specific changes in your head's position. This might occur when you tip your head up or down, when you lie down, or when you turn over or sit up in bed.
Although BPPV can be bothersome, it's rarely serious except when it increases the chance of falls. You can receive effective treatment for BPPV during a doctor's office visit.
Products & Services
- A Book: Mayo Clinic on Hearing and Balance
The signs and symptoms of benign paroxysmal positional vertigo (BPPV) may include:
- A sense that you or your surroundings are spinning or moving (vertigo)
- A loss of balance or unsteadiness
The signs and symptoms of BPPV can come and go and commonly last less than one minute. Episodes of BPPV can disappear for some time and then recur.
Activities that bring about the signs and symptoms of BPPV can vary from person to person, but are almost always brought on by a change in head position. Some people also feel out of balance when standing or walking.
Abnormal rhythmic eye movements usually accompany the symptoms of benign paroxysmal positional vertigo.
When to see a doctor
Generally, see your doctor if you experience any recurrent, sudden, severe, or prolonged and unexplained dizziness or vertigo.
Seek emergency care
Although it's uncommon for dizziness to signal a serious illness, see your doctor immediately if you experience dizziness or vertigo along with any of the following:
- A new, different or severe headache
- Double vision or loss of vision
- Hearing loss
- Trouble speaking
- Leg or arm weakness
- Loss of consciousness
- Falling or difficulty walking
- Numbness or tingling
The signs and symptoms listed above may signal a more serious problem.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
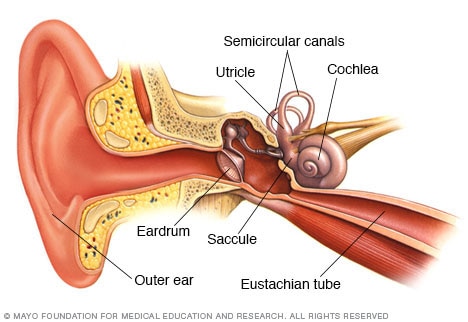
Inner ear and balance
Semicircular canals and otolith organs — called the utricle and saccule — in your inner ear contain fluid and fine, hairlike sensors. These sensory hair cells help you keep your eyes focused on a target when your head is in motion. They also help you keep your balance.
Often, there's no known cause for BPPV . This is called idiopathic BPPV .
When there is a known cause, BPPV is often associated with a minor to severe blow to your head. Less common causes of BPPV include disorders that damage your inner ear or, rarely, damage that occurs during ear surgery or long periods positioned on your back, such as in a dentist chair. BPPV also has been associated with migraines.
The ear's role
Inside your ear is a tiny organ called the vestibular labyrinth. It includes three loop-shaped structures (semicircular canals) that contain fluid and fine, hairlike sensors that monitor your head's rotation.
Other structures (otolith organs) in your ear monitor your head's movements — up and down, right and left, back and forth — and your head's position related to gravity. These otolith organs contain crystals that make you sensitive to gravity.
For many reasons, these crystals can become dislodged. When they become dislodged, they can move into one of the semicircular canals — especially while you're lying down. This causes the semicircular canal to become sensitive to head position changes it would normally not respond to, which is what makes you feel dizzy.
Risk factors
Benign paroxysmal positional vertigo occurs most often in people age 50 and older, but can occur at any age. BPPV is also more common in women than in men. A head injury or any other disorder of the balance organs of your ear may make you more susceptible to BPPV .
Complications
Although BPPV is uncomfortable, it rarely causes complications. The dizziness of BPPV can make you unsteady, which may put you at greater risk of falling.
- Barton JJS, et al. Benign paroxysmal positional vertigo. https://www.uptodate.com/contents/search. Accessed July 17, 2020.
- Elsevier Point of Care. Clinical Overview: Benign paroxysmal positional vertigo. https://www.clinicalkey.com. Accessed July 17, 2020.
- Ferri FF. Benign paroxysmal positional vertigo. In: Ferri's Clinical Advisor 2021. Elsevier; 2021. https://www.clinicalkey.com. Accessed July 17, 2020.
- Lalwani AK. Benign paroxysmal positional vertigo In: Current Diagnosis & Treatment Otolaryngology — Head & Neck Surgery. 4th ed. McGraw-Hill Education; 2020. https://accessmedicine.mhmedical.com. Accessed July 17, 2020.
- AskMayoExpert. Vertigo and vestibular disorders (adult). Mayo Clinic; 2020.
- Furman JM. Causes of vertigo. https://www.uptodate.com/contents/search. Accessed July 17, 2020.
- Libi SE (expert opinion). Mayo Clinic. Aug. 6, 2020.
Associated Procedures
- Canalith repositioning procedure
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
Dental work and Vertigo
Timothy c. hain, md • most recent update: april 3, 2023.
There is a modest literature concerning dental work and vertigo. For students -- a good topic for research ? Nevertheless, as a result, the content of this page is based on a combination of consideration of mechanisms and clinical material from the author's dizziness practice in Chicago Illinois. There is also a modest literature concerning dental work and hearing loss. See our dental hearing loss pages for more.
General categories of disorders where dizziness might be associated with or provoked by dentistry include:
- Positional vertigo -- vertigo triggered by changing of head movement with respect to gravity. BPPV is by far the most common cause.
- Cardiac conditions -- arrhythmia associated with the adrenalin often accompanying dental work
- Migraine -- dental work can hurt and trigger migraine associated dizziness.
- Hyperventilation induced dizziness
- Psychiatric conditions
- TMJ/TMD disorders
Clinical observations and commentary on dizziness associated with dentistry

BPPV is by far the most common cause of dizziness reported to be associated with dentistry ( Brauer, 2009), see also our post-surgery page . For the most part, reports are associated with blows to the jaw -- such as use of the "osteotome". It would also seem very logical that vibration associated with dental area drilling might cause BPPV. Another source, much more rarely reported, is when positional vertigo triggered in the person who is supine or head turned on the side during the dental encounter. The illustrations above shows positions that typically trigger vertigo. Positions where the body is supine and head turned to either side are equally provocative. This situation nearly always is due to a very common ear condition -- benign paroxysmal positional vertigo ( BPPV ), which fortunately is generally easily treated. Cardiac conditions -- do not seem to be a common cause of dizziness during dentistry. We suspect that this is due to a tendency for participants to accept as normal a rapid heart beat. We have never encountered anyone who has indicated that dizziness was accompanied by angina pain or an event that could be interpreted as being due to low blood pressure, in the course of dentistry. So to summarize, this seems very unlikely.
Migraine - similarly, migraine associated dizziness does not seem to greatly interfere with dentistry.
Hyperventilation -- Clinically this is not a substantial problem. We think that this is due to the fact that HVT induced dizziness is usually transient, minor and fairly easily ignored.
Psychiatric condtions - - dentistry can be painful and anxiety provoking. It is not surprising that dizziness can be a consequence. We know of no papers published on this assocation.
TMJ and TMD (temporomandibular joint or temporomandibular dysfunction) :
According to literature published by the dental community (e.g. Tuz, Onder, et al. 2003; Lam et al. 2001), ear (otologic) complaints are common in persons with TMJ/TMD. Typical reports (including ear pain) have prevalence much greater than 50%. It is our position that TMJ or TMD and vertigo are both common medical conditions, but there is almost never a causual relation. TMJ disorders are essentially a type of arthritis. While the joint is close to the ear, it does not have any direct connection to the inner ear. Accordingly, the hypothesis that TMJ "causes" vertigo is very implausible. As another example, although the heart is just underneath the ribcage, it would be implausible to attribute heart-attacks to arthritis of the ribs. Neverthless, there are numerous examples of individuals with the opposite opinion -- suggesting, for example, that Meniere's disease might respond to treatment of the TMJ( Bjorne and Ajersberg, 2003). In our opinion, these papers are simply mistaken. Salvetti et al. (2006) pointed out that that the methodological problems with studies of this nature are common. There are several logical places for mistakes in papers published by the dental community in regard to TMJ/TMD are mistaking dizziness provoked by their procedures (i.e. positioning) as being caused by the disease that they are treating, and certainly attributing pain associated with TMJ/TMD to an inner ear source. We are especially dubious about small, uncontrolled studies. There are also reports of hearing disturbances in TMJ/TMD. This is interesting, but we would like to see confirmation using a more objective methodology than subjective audiograms. It would seem reasonable that tinnitus could be associated with TMJ/TMD. The ear is close to the TMJ, and there is a reasonable scientific basis for "somatic tinnitus". Some simply report that vertigo or tinnitus improves after treatment for TMJ, e.g. (Wright, 2007). This is a less aggressive claim. It does seem possible to us that reduction of discomfort in one part of the body might provide more cognitive resources to deal with discomfort in another part of the body.
Diagnosis of Dizziness associated with Dentistry
As is the usual situation with dizziness, the first step to sort out the condition.
- Dix-Hallpike testing (for BPPV)
- Hyperventilation
- Ambulatory event monitoring for cardiac arrhythmia
A careful history is the beginning. While it has not been our experience that many patients will report dizziness associated with dentistry, they will nevertheless commonly report dizziness associated with particular head positions or exercise.
Office(bedside) testing is the next step. One should also attempt to reproduce positioning of the head (Dix-Hallpike testing), as well as have the patient strain and hyperventilate, while monitoring eye movements with a video frenzel goggle system. Persons who have psychological disturbances (i.e. anxiety or malingering), should have no substantial exam findings, or might refuse office testing -- usually claiming that the vertigo is so severe that a diagnostic evaluation is impossible. This is highly unlikely as with appropriate medication, any patient can be examined successfully.
Laboratory testing is not always needed -- if a person has BPPV, one can simply proceed on to treatment. However, in situations where the diagnosis is not so clear, the tests above should be considered.
Audiometry seems very reasonable. According to Pekkan, G., S. Aksoy, et al. (2010). TMD patients with otological complaints have hearing impairment at low frequencies and also perhaps, at high frequencies. As audiometry is a subjective test, and because this conclusion is illogical (see discussion above) we would like to see the results of an objective test such as OAE.
Treatment of dizziness associated with dentistry
As there are several causes of dizziness associated with dentistry, it follows that there are also many approaches to treatment. In most cases, and especially with positional vertigo, one can correct the underlying inner ear dysfunction and allow the person to go about life normally. Occasionally of course, individuals will instead find ways to modify the way that they go about their activity. In this case, it is still very helpful to know what triggers the vertigo, how long it lasts, and what can be done to mitigate it's effects.
Medication can be useful, especially vestibular sedatives. Particular useful medications are listed below:
- Meclizine (antivert)
- Ondansetron (Zofran)
References:
- Brauer, H. U. (2009). "Unusual complications associated with third molar surgery: a systematic review." Quintessence Int 40 (7): 565-572.
- Bjorne, A. and G. Agerberg (2003). "Symptom relief after treatment of temporomandibular and cervical spine disorders in patients with Meniere's disease: a three-year follow-up." Cranio 21 (1): 50-60.
- Chiarella, G., G. Leopardi, et al. (2007). "Iatrogenic benign paroxysmal positional vertigo: review and personal experience in dental and maxillo-facial surgery." Acta Otorhinolaryngol Ital 27 (3): 126-128.
- Chiarella, G., G. Leopardi, et al. (2008). "Benign paroxysmal positional vertigo after dental surgery." Eur Arch Otorhinolaryngol 265 (1): 119-122.
- D'Ascanio, L., F. Salvinelli, et al. (2007). "Benign paroxysmal positional vertigo: an unusual complication of molar teeth extraction." Br J Oral Maxillofac Surg 45 (2): 176-177.
- Di Girolamo, M., B. Napolitano, et al. (2005). "Paroxysmal positional vertigo as a complication of osteotome sinus floor elevation." Eur Arch Otorhinolaryngol 262 (8): 631-633.
- Flanagan, D. (2004). "Labyrinthine concussion and positional vertigo after osteotome site preparation." Implant Dent 13 (2): 129-132. Galli, M., T. Petracca, et al. (2004). "Complications in implant surgery by Summer's technique: benign paroxysmal positional vertigo (BPPV)." Minerva Stomatol 53 (9): 535-541.
- Kaplan, D. M., U. Attal, et al. (2003). "Bilateral benign paroxysmal positional vertigo following a tooth implantation." J Laryngol Otol 117 (4): 312-313.
- Klewansky, P., E. Benarroch, et al. (1969). "[Anatomic-clinical study of jaw fractures treated at the Maxillofacial Center of the Dental Institute of Strasbourg during the last 10 years]." Rev Fr Odontostomatol 16 (8): 1065-1102.
- Lam, D. K., H. P. Lawrence, et al. (2001). "Aural symptoms in temporomandibular disorder patients attending a craniofacial pain unit." J Orofac Pain 15 (2): 146-157
- Pekkan, G., S. Aksoy, et al. (2010). "Comparative audiometric evaluation of temporomandibular disorder patients with otological symptoms." J Craniomaxillofac Surg 38 (3): 231-234.
- Penarrocha-Diago, M., J. Rambla-Ferrer, et al. (2008). "Benign paroxysmal vertigo secondary to placement of maxillary implants using the alveolar expansion technique with osteotomes: a study of 4 cases." Int J Oral Maxillofac Implants 23 (1): 129-132. Penarrocha, M. and A. Garcia (2006). "Benign paroxysmal positional vertigo as a complication of interventions with osteotome and mallet." J Oral Maxillofac Surg 64 (8): 1324; author reply 1324.
- Penarrocha, M., H. Perez, et al. (2001). "Benign paroxysmal positional vertigo as a complication of osteotome expansion of the maxillary alveolar ridge." J Oral Maxillofac Surg 59 (1): 106-107.
- Perez Garrigues, H., M. Mateos Fernandez, et al. (2001). "[Benign paroxysmal positional vertigo secondary to surgical maneuvers on superior maxilla]." Acta Otorrinolaringol Esp 52 (4): 343-346.
- Rodriguez Gutierrez, C. and E. Rodriguez Gomez (2007). "Positional vertigo afterwards maxillary dental implant surgery with bone regeneration." Med Oral Patol Oral Cir Bucal 12 (2): E151-153.
- Saker, M. and O. Ogle (2005). "Benign paroxysmal positional vertigo subsequent to sinus lift via closed technique." J Oral Maxillofac Surg 63 (9): 1385-1387.
- Salvetti, G., D. Manfredini, et al. (2006). "Otologic symptoms in temporomandibular disorders patients: is there evidence of an association-relationship?" Minerva Stomatol 55 (11-12): 627-637.
- Tuz, H. H., E. M. Onder, et al. (2003). "Prevalence of otologic complaints in patients with temporomandibular disorder." Am J Orthod Dentofacial Orthop 123 (6): 620-623.
- Wright, E. F. (2007). "Otologic symptom improvement through TMD therapy." Quintessence Int 38 (9): e564-571.
- Free TMJ eBook
- Testimonials
- Patient Referrals
- Out Of Town Patients
Benign Paroxysmal Positional Vertigo (BPPV) After Dental Procedures
by Dr. Shapira | Apr 5, 2016
Dental Treatment appears to be a major Risk Factor for Benign Paroxysmal Positional Vertigo according to a new article (abstract below).
The statistical connection is not yet shown to be a cause and effect relationship but there is a major correlation. The study showed over 9% of BPPV patients had had dental work in the month prior to diagnosis.
The definition of BPPV according to Mayo Clinic Staff is: “Benign paroxysmal positional vertigo (BPPV) is one of the most common causes of vertigo — the sudden sensation that you’re spinning or that the inside of your head is spinning.
Benign paroxysmal positional vertigo causes brief episodes of mild to intense dizziness. Benign paroxysmal positional vertigo is usually triggered by specific changes in the position of your head. This might occur when you tip your head up or down, when you lie down, or when you turn over or sit up in bed.
Although benign paroxysmal positional vertigo can be a bothersome problem, it’s rarely serious except when it increases the chance of falls. You can receive effective treatment for benign paroxysmal positional vertigo during a doctor’s office visit.”
Patients with BPPV often do well with Physiologic Dental Treatment. Patients should be evaluated by their physicians following onset of sudden new symptoms.
PLoS One. 2016 Apr 4;11(4):e0153092. doi: 10.1371/journal.pone.0153092. Benign Paroxysmal Positional Vertigo after Dental Procedures: A Population-Based Case-Control Study. Chang TP1,2, Lin YW3, Sung PY4, Chuang HY5, Chung HY6, Liao WL4. Author information Abstract BACKGROUND: Benign paroxysmal positional vertigo (BPPV), the most common type of vertigo in the general population, is thought to be caused by dislodgement of otoliths from otolithic organs into the semicircular canals. In most cases, however, the cause behind the otolith dislodgement is unknown. Dental procedures, one of the most common medical treatments, are considered to be a possible cause of BPPV, although this has yet to be proven. This study is the first nationwide population-based case-control study conducted to investigate the correlation between BPPV and dental manipulation. METHODS: Patients diagnosed with BPPV between January 1, 2007 and December 31, 2012 were recruited from the National Health Insurance Research Database in Taiwan. We further identified those who had undergone dental procedures within 1 month and within 3 months before the first diagnosis date of BPPV. We also identified the comorbidities of the patients with BPPV, including head trauma, osteoporosis, migraine, hypertension, diabetes, hyperlipidemia and stroke. These variables were then compared to those in age- and gender-matched controls. RESULTS: In total, 768 patients with BPPV and 1536 age- and gender-matched controls were recruited. In the BPPV group, 9.2% of the patients had undergone dental procedures within 1 month before the diagnosis of BPPV. In contrast, only 5.5% of the controls had undergone dental treatment within 1 month before the date at which they were identified (P = 0.001). After adjustments for demographic factors and comorbidities, recent exposure to dental procedures was positively associated with BPPV (adjusted odds ratio 1.77; 95% confidence interval 1.27-2.47). This association was still significant if we expanded the time period from 1 month to 3 months (adjusted odds ratio 1.77; 95% confidence interval 1.39-2.26). CONCLUSIONS: Our results demonstrated a correlation between dental procedures and BPPV. The specialists who treat patients with BPPV should consider dental procedures to be a risk factor, and dentists should recognize BPPV as a possible complication of dental treatment. PMID: 27044009 [PubMed – as supplied by publisher] Share on FacebookShare on TwitterShare on Google+
It happened to me recently. I wish I knew this information before as I become so relieved after reading this information
The morning after having a temporay crown was put on, I went to get out of bed and almost fell down because I was so dizzy. It has been 2 weeks and I still have it every morning. Also have it if I bend down to pick something up. No sudden movements for me. Hopefully it will go away soon.
This may or may not be related to the temporary crown. Often extended mouth opening can cause issues. See a neuromuscular dentist who utilizes ULF_TENS and neuromuscular orthotics if it does not resolve. Immediately see dentist and have them check the bite on the temporary.
Find It Fast

Recent Blogs
- TMJ Chicago: Severe Disabling Pain to Pain Free, Long-Term Gold Orthotic after 35 years of TMD December 20, 2023
- Severe TMJ Disorder Relieved….23 year Follow up Doing Great! December 20, 2023
- Vivos Therapeutics Receives First Ever FDA 510(k) Clearance for Oral Device Treatment of Severe Obstructive Sleep Apnea November 29, 2023
- Highland Park Dentist Steps Down As Editor In Chief of CRANIO Journal to Spend More Time Treating TMJ Disorders, Headaches, Migraines and Facial Pain Patients. This is good news for patients in pain November 11, 2023
- THE ART AND SCIENCE OF MUSCULOSKELETAL DENTISTRY. What is a Muscular Skeletal Dentist July 29, 2021
Explore Our Blog Topics
Benign Paroxysmal Positional Vertigo after Dental Procedures: A Population-Based Case-Control Study
Affiliations.
- 1 Department of Neurology/Neuro-Medical Scientific Center, Taichung Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Taichung, Taiwan.
- 2 School of Medicine, Tzu Chi University, Hualien, Taiwan.
- 3 Department of Dentistry, Taipei Medical University Hospital, Taipei, Taiwan.
- 4 Department of Physical Medicine and Rehabilitation, Taichung Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Taichung, Taiwan.
- 5 Department of research, Taichung Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Taichung, Taiwan.
- 6 Department of Dentistry, Taichung Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Taichung, Taiwan.
- PMID: 27044009
- PMCID: PMC4820237
- DOI: 10.1371/journal.pone.0153092
Background: Benign paroxysmal positional vertigo (BPPV), the most common type of vertigo in the general population, is thought to be caused by dislodgement of otoliths from otolithic organs into the semicircular canals. In most cases, however, the cause behind the otolith dislodgement is unknown. Dental procedures, one of the most common medical treatments, are considered to be a possible cause of BPPV, although this has yet to be proven. This study is the first nationwide population-based case-control study conducted to investigate the correlation between BPPV and dental manipulation.
Methods: Patients diagnosed with BPPV between January 1, 2007 and December 31, 2012 were recruited from the National Health Insurance Research Database in Taiwan. We further identified those who had undergone dental procedures within 1 month and within 3 months before the first diagnosis date of BPPV. We also identified the comorbidities of the patients with BPPV, including head trauma, osteoporosis, migraine, hypertension, diabetes, hyperlipidemia and stroke. These variables were then compared to those in age- and gender-matched controls.
Results: In total, 768 patients with BPPV and 1536 age- and gender-matched controls were recruited. In the BPPV group, 9.2% of the patients had undergone dental procedures within 1 month before the diagnosis of BPPV. In contrast, only 5.5% of the controls had undergone dental treatment within 1 month before the date at which they were identified (P = 0.001). After adjustments for demographic factors and comorbidities, recent exposure to dental procedures was positively associated with BPPV (adjusted odds ratio 1.77; 95% confidence interval 1.27-2.47). This association was still significant if we expanded the time period from 1 month to 3 months (adjusted odds ratio 1.77; 95% confidence interval 1.39-2.26).
Conclusions: Our results demonstrated a correlation between dental procedures and BPPV. The specialists who treat patients with BPPV should consider dental procedures to be a risk factor, and dentists should recognize BPPV as a possible complication of dental treatment.
Publication types
- Research Support, Non-U.S. Gov't
- Benign Paroxysmal Positional Vertigo / epidemiology*
- Benign Paroxysmal Positional Vertigo / etiology*
- Case-Control Studies
- Comorbidity
- Middle Aged
- Population Surveillance*
- Prosthodontics*
- Risk Factors
- Taiwan / epidemiology
Grants and funding
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Maxillofac Oral Surg
- v.19(4); 2020 Dec

Benign Paroxysmal Positional Vertigo After Oral and Maxillofacial Surgery: Our Experience and Review of Literature
Marzia petrocelli.
1 Otolaryngology Unit, Department of Medicine, Surgery and Odontoiatrics, University of Salerno, Via Giovanni Paolo II 132, 84084 Fisciano, Salerno Italy
Carolina Sbordone
2 Maxillofacial Surgery Unit, Department of Neurosciences, Reproductive and Odontostomatological Sciences, University Federico II, Via Pansini 9, 80100 Naples, Italy
Giovanni Salzano
Giovanni dell’aversana orabona, francesco maria cassandro.
3 Dentistry Unit, Department of Neurosciences, Reproductive and Odontostomatological Sciences, University Federico II, Via Pansini 9, 80100 Naples, Italy
Alfonso Scarpa
Luca ramaglia, giorgio iaconetta.
4 Neurosurgery Unit, Department of Medicine, Surgery and Odontoiatrics, University of Salerno, Via Giovanni Paolo II 132, 84084 Fisciano, Salerno Italy
Luigi Califano
Ettore cassandro.
The aim of our study is to evaluate the influence of patient risk factors and the length of surgical time on the onset of BPPV (benign paroxysmal positional vertigo) and suggest surgical and clinical strategies to prevent this rare complication.
Our retrospective study analyzes that, in 2 years, 281 patients, divided into three groups, underwent wisdom teeth extraction, sinus lift elevation and orthognathic surgery, at the Oral and Maxillofacial Department of the University of Naples “Federico II.”
Twenty-one patients presented postoperative BPPV. Some comorbidities, like dyslipidemia, high cholesterol levels, vascular problems, endocrinological disorders, perimenopausal age, female gender, cranial trauma, neurologic disorders, migraine, hypovitaminosis D, autoimmune disease, flogosis of inner ear, can be risk factors to the occurrence of postoperative vertigo.
Our statistical analysis revealed a relationship between surgical time and comorbidity and onset of vertigo for each group of patients.
Introduction
Positional vertigo is a feeling of spinning when the patient turns the head in a particular manner or assumes a certain position [ 1 ].
The etiology of benign paroxysmal positional vertigo (BPPV) is unknown. About 20% of cases have been associated with minor and major head and neck traumas; few cases were associated with oral or maxillofacial procedures [ 2 ].
Preparation of implant beds or sinus floor elevation procedures, impacted wisdom teeth extraction, osteotomies during orthognathic surgery with the aid of osteotomes and surgical mallets transmits percussive and vibratory forces capable of detaching the otoliths, causing them to float around in the endolymph producing BPPV [ 3 ].
BPPV is usually unilateral; episodes associated with head trauma are bilateral as well as some cases of bilateral vertigo after orthognathic surgery [ 4 ].
The common postoperative complications of extraction of wisdom teeth, orthognathic surgery and sinus floor lift are: infection, injury to neighboring vessels, nerve injuries, bad fractures, acute or chronic sinusitis, implant failure, Schneiderian membrane perforation and so on [ 5 – 8 ].
The postoperative BPPV is a less common complication less described in the scientific literature; however, oral and maxillofacial surgeons should consider it.
The aim of our study is to evaluate the influence of specific comorbidities on the onset of BPPV and the relation between the length of surgical time and the onset of BPPV. Furthermore, we propose some surgical and/or clinical strategies to prevent this complication.
Materials and Methods
From January 2015 to December 2016, 301 patients underwent wisdom teeth extraction, sinus lift elevation and orthognathic surgery, at the Oral and Maxillo Facial Department of University of Naples “Federico II.”
Patients lost during follow-up or BPPV sintomatology for over 15 days from surgery, or previous surgical treatment for facial traumas, or previous BPPV or previous labyrinth disorders were excluded (20 patients).
For this retrospective analysis, 281 subjects (180 males and 101 females, average age of 41.5) were enrolled; of these, 21 patients presented postoperative BPPV.
All surgical procedures required osteotomes and/or mallets and/or rotating tools.
Features of selected patients are outlined in Table 1 . All patients were divided into three groups: 95 patients (67 males and 28 females) underwent bimaxillary surgery for dentoscheletric malocclusion (Group I); 160 patients (97 males and 63 females) underwent extraction of impacted teeth of 3.8 and 4.8 through the erosion of the incarcerating bony wall (Group II); and 26 patients (16 males and 10 females) underwent preparation of implants bed with elevation of sinus floor (Group III) (Fig. 1 ).
Table 1
Clinical data of patients enrolled for the study

Surgical techniques performed on enrolled patients
All patients were subjected to bed-side examination, posterior nystagmus was evaluated, and cases of BPPV were identified through the involvement of vertical or lateral channels.
The diagnosis of postoperative BPPV was made, under Frenzel glasses or videoculoscopy control, using the typical positioning maneuvers of Hallpike for the posterior semicircular canal (PSc) and Pagnini [ 9 ] and Mc Clure’s maneuvers [ 10 ] (slow positioning on the sides) for the lateral semicircular canal (lSc).
The canalith repositioning procedure (CRP) through Epley maneuver [ 11 ] was performed for all patients with postoperative BPPV.
Patients’ follow-up was scheduled for 3, 6 and 12 months after Epley maneuver.
Data were aggregated with Microsoft Excel ® spreadsheet, and statistical analysis was performed using statistical packages software system 14.0 (SPSS Inc., Chicago, USA). Fisher double-tailed test has been used to evaluate statistical relationship between surgical time with comorbidity and onset of vertigo.
Vestibular pathology has been recorded on the side submitted to surgical treatment in 6 cases: 2 males and 1 female underwent extraction of impacted teeth, and 1 male and 2 females underwent preparation of implants bed with unilateral elevation of sinus floor. There was evidence of bilateral pathology with simultaneous involvement of multiple semicircular canals in 15 cases: 2 females and 2 males underwent bimaxillary surgery, and 7 males and 4 females underwent extraction of impacted teeth (3.8 and 4.8).
The mean onset time of postoperative BPPV was 3.61 days. The most rapid onset was reported in a 60-year-old female, 8 h after extraction of 1.8 and 4.8 impacted teeth. The most remote onset was reported in a 68-year-old female 7 days after extraction of 4.8 impacted teeth.
Fisher test conducted for each group of patients revealed a statistical dependence as shown in Tables 2 , ,3 3 and and4 4 .
Table 2
Analysis of risk factors associated with the onset of BPPV for patients that underwent orthognathic surgery (Group 1) (Fisher exact test both tails for p = 0.05)
Table 3
Analysis of risk factors associated with the onset of BPPV for patients that underwent third molar avulsion (Group 2) (Fisher exact test both tails for p = 0.05)
Table 4
Analysis of risk factors associated with the onset of BPPV for patients that underwent sinus lift (Group 3) (Fisher exact test both tails for p = 0.05)
After Epley maneuver, a negative clinical pattern was confirmed in all cases at 3-, 6- and 12-month follow-up.
The inner ear is formed by the osseous labyrinth and the membranous labyrinth. The osseous labyrinth is contained in the petrous portion of the temporal bone; it is formed by the vestibule, semicircular canals and the cochlea. These bone cavities are lined with a very thin fibroserous membrane filled with the perilymph. The semicircular canals and vestibule contain equilibrium receptors. Receptors in the semicircular canals respond to alterations in direction of head movement. During head rotation, the endolymph in the semicircular canals slows down and then moves in the opposite direction to the head’s movement causing stimulation of hair cells that send an impulse to the cerebellum through the vestibular nerve. The vestibule contains macula receptors that sense the body’s static equilibrium. Otoliths move with head position and stimulate the hair cells that in turn transmit a signal to the brain to sense balance in the vestibule [ 1 , 2 ].
The BPPV is an attack of rotatory vertigo, induced by changes in the head position relative to gravity. Typical signs of BPPV are a paroxysmal nystagmus, torsional and directed upwards, for the PSc, horizontal and geotropic or apogeotropic for lSc. 1 The criteria used for the diagnosis were: a paroxysmal nystagmus with brief latency, accompanied by exhaustible, repeatable and fatigable vertigo. Each vertigo episode appears with short latency, lasts for less than a minute and is characterized by an increase followed by a decrease in its intensity. The vertigo is associated with neurovegetative symptoms such as nausea, vomiting, tachycardia and anxiety, without any cochlear symptoms such as hearing loss, tinnitus or ear fullness [ 2 ].
The etiology of benign paroxysmal positional vertigo (BPPV) is unknown; 15–20% of cases have been associated with minor and major head trauma; few cases were associated with oral or maxillofacial procedures. Sinus floor elevation procedures, wisdom teeth avulsion, maxillary and mandibular osteotomies performed with osteotomes and surgical mallets transmit percussive and vibratory forces capable of detaching the otoliths, causing them to float around in the endolymph, hence determining BPPV [ 1 – 5 , 12 – 14 ]. The BPPV is usually unilateral; the episodes associated with head trauma and orthognathic surgery are bilateral [ 15 ], as in our sample.
In our sample, for patients that underwent orthognathic surgery and third molar extraction (Group 1 and Group 2) emerges a statistical correlation between the length of surgical time and the onset of BPPV (Table 2 , p = 0.007, Table 3 , p = 0.014).
The patient’s surgical head position, with hyperextended head, the length of surgical time with a repeated percussive and vibratory stress help the displacement of these free-floating particles into the posterior semicircular canal; when the patient later adopts a seated position, the otoconia descend into the ampullary crest, triggering an anomalous stimulus causing vertigo (BPPV). The postoperative BPPV is characterized by short-term recurrent episodes of vertigo associated with intense nystagmus, due to the anatomical features of the district involved. BPPV risk factors (comorbidities), like dyslipidemia, high cholesterol levels, vascular problems, endocrinological disorders, perimenopausal age (50–60 years), sex (female gender), cranial trauma, neurologic disorders, migraine, hypovitaminosis D, autoimmune disease, flogosis of inner ear, may promote the occurrence of postoperative vertigo [ 16 – 23 ].
In our sample, for patients that underwent preparation of bed implant through sinus floor lift (Group 3) emerges a statistical correlation between the presence of comorbidities and the onset of BPPV (Table 4 , p = 0.046).
The criteria commonly approved for the diagnosis of BPPV are a paroxysmal nystagmus with brief latency, accompanied by exhaustible, repeatable and fatigable vertigo. The diagnosis is made, under Frenzel glasses or videoculoscopy control, using the typical positioning maneuvers of Hallpike and Pagnini and Mc Clure’s maneuvers (slow positioning on the sides) for the lateral semicircular canal (lSc).
Specifically, in posterior canal type of BPPV, a torsional nystagmus is present, with additional vertical upward component, in which the upper pole of the eye rotates toward the affected ear. Such nystagmus is induced by the Dix–Hallpike maneuver [ 24 ], while in lateral canal type of BPPV, geotropic nystagmus is present, induced by the supine roll test. The rightward horizontal nystagmus is induced by the right-ear-down head position, while leftward horizontal nystagmus is induced by the left-ear-down head position, with the patient supine in the geotropic variant and leftward horizontal nystagmus induced by the right-ear-down head position and rightward horizontal nystagmus induced by the left-ear-down head position in apogeotropic variant [ 25 ]. There are several reports of BPPV following osteotome sinus floor elevation [ 14 , 3 , 13 , 26 , 10 , 27 , 28 ].
Di Girolamo et al. [ 3 ] analyzed 146 patients who underwent osteotome sinus floor elevation; 4 patients of 146 developed BPPV 1 or 2 days after the surgical procedure, which was solved with the Epley repositioning maneuver.
Sammartino et al. [ 28 ] showed that 3 of 98 patients who underwent sinus floor elevation with osteotome and mallet developed BPPV but none of the 98 patients who underwent sinus floor elevation without the use of a mallet.
Moreover, Chiarella et al. [ 2 ] showed that dentoalveolar surgery with a rotating bur for removal of impacted teeth and cysts could lead to BPPV.
Furthermore, Beshkar et al. [ 1 ] analyzed 50 patients who underwent orthognathic surgery and showed 1 case of BPPV positive on Dix–Hallpike test subsequently treated by a neurologist.
Vannucchi et al. [ 29 ] explained that the treatment for BPPV is expected by the canalith repositioning procedure (CRP), such as modified Epley maneuver for the treatment of the posterior canal type of BPPV, in which the specific sequential head movements cause otoconial debris to move from the posterior semicircular canal to the utricle. Specifically, after rotating the head to the affected ear, the patient is moved from the sitting position to supine position, with their head tilted back of about 45°. Subsequently, after 30 s, the head is moved to the other side and then the patient’s trunk is turned in the opposite direction to the affected ear. Then, after additional 30 s, the patient is placed in sitting position.
The postoperative BPPV is a less common complication that should be considered by oral and maxillofacial surgeons.
We propose, in the treatment of patients with risk factors to the postoperative BPPV, some surgical and/or clinical strategies to prevent this complication:
- Use piezoelectric and endoscopic aid to reduce vibration and percussion stress in long and complicated surgery;
- Limit the hyperextension of the head during surgery;
- Advise on a semi-deployed (double pillow use) position, during postoperative times, even during night rest.
Finally, patients should always be informed about the possible BPPV postoperative complication in order to prevent legal disputes.
In further studies, with an enlargement of the sample, it would be appropriate to evaluate the ocular vemps (vestibular evoked myogenic potentials) and the cervical vemps through the video head impulse test. The possible irreversible saccular and utricular otolithic dysfunction caused by the surgical insult could be related to the clinical substrate (comorbidity).
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Compliance with Ethical Standards
The authors declare that they have no conflict of interest.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rathke Family Dentistry
Restorative & cosmetic dentistry, can dental work cause vertigo.

Have you ever stood up too fast and caused yourself to be dizzy? As a child, do you remember the feeling of spinning fast on a merry-go-round and suddenly stopping, but the world around you continued to spin?
Now, imagine you are standing still, not moving, and the room starts spinning around you. Although your body is still, you feel you’re losing your balance. Suddenly you feel nauseated because you can’t get the room to stop spinning. Finally, think of how it would feel if this sensation lasts for several hours.
This is how many people feel with various forms of vertigo.
I recently had a patient for a moderately long dental appointment, probably about 2.5 hours. When we were finished, the patient said they felt well, thanked us for our service, and left in a stable and ambulatory state. The next day the patient’s spouse called our office and reported the patient was experiencing dizziness if they tried to get up and walk. Furthermore, the dizziness was inducing some significant nausea. These symptoms slowly got better throughout the day, and by noon the following day the patient was fine.
This patient had experienced a significant vertigo episode shortly following her dental appointment. They had never experienced vertigo problems like this before. This begs the question: can dental work cause vertigo? This post will explore the relationship of vertigo and dental visits.
What is Vertigo?
As described above, vertigo is a sensation of dizziness or lack of balance. Patients often report they feel the room is spinning, even though they are standing still. Obviously this can be quite a disconcerting experience!
There are several different types of vertigo, but the one appearing to be most associated with dental work is benign paroxysmal positional vertigo (BPPV). It is the most common type of vertigo observed in the general population.
Most causes of BPPV are unknown, but some inner ear disorders and trauma to the head have been known to cause it. Several risk factors have been identified which include bed rest, osteoporosis, migraines, and some vascular factors.
It is believed BPPV is induced by small calcifications in the ear that dislodge and collect in the vestibular canals. The vestibular canals are the part of the inner ear that affect your sensation of balance from your head position relative to gravity.
Many times, patients with BPPV will experience symptoms on and off for a few days, sometimes even weeks. The symptoms may disappear for weeks or months, then return again.
A Look at the Literature
There have been a number of case reports that document the onset of vertigo symptoms following dental visits. Until 2016, no major population-based studies had been published. This study by Tzu-Pu Chang, et al . explores onset of BPPV in the general population in Taiwan. It pays particular focus to those who had recent dental work.
The study found a correlation between recent dental work and onset of BPPV symptoms. It took note of patients with BPPV onset within 1 month following dental work and those with BPPV onset within 3 months. They documented a statistically significant difference between those receiving recent dental work and the control groups.
The study also explored the types of dental procedures performed to explore their relationship to BPPV onset. However these were reported as very broad fields. For instance, one of the procedures reported was “prosthodontics”. Prosthodontics is an extremely broad field of dentistry that is further divided into “fixed” and “removable” sub-fields. Techniques and procedures for fixed prosthodontics are totally different than those of removable prosthodontics.
I didn’t put much stock into this section. The procedures explored were far to broad and non-specific. Instead, I would like to have seen a focus on appointment length and chair position rather than the very broad types of dentistry performed.
Based on the available evidence, it is difficult to conclude that dental work is a direct cause of BPPV.
Onset of BPPV symptoms seemed to correlate with recent dental visits in the Taiwan study. However, it is still not clear if these patients already had BPPV and dental work merely induced the first onset of symptoms.
I would say it is a possibility that should not be ignored. Furthermore we still do not know why dental work would cause onset of BPPV symptoms. I have a few educated guesses on the matter.
First, patients often need to turn their heads left and right during dental procedures to provide the caregiver access to different parts of the mouth. It is known that turning of the head in this manner can bring about BPPV symptoms.
Another possibility is the length of time the patient is supine (laying on their back) in the chair. Many patients sleep with multiple pillows at home and do not sleep in a totally supine position. The length of time spent supine while turning the head left and right could also be an inducing factor for BPPV symptoms.
Finally, another possibility could be related to the micro-vibrations experienced with the dental handpiece (or “drill”). These micro-vibrations could cause calcifications already deposited in the vestibular canals to circulate. This would send confusing signals to the brain related to balance and head position.
The bottom line I draw from all of this is: It’s difficult to conclude that dental work directly causes BPPV, however the correlation between the two cannot be ignored.
Treatment for Benign Paroxysmal Positional Vertigo
There are several different ways to treat BPPV. Several in-office remedies exist that can be performed to alleviate symptoms, or in some cases cure BPPV altogether. There are also reported home remedies and surgical interventions. This article goes into some detail about the treatments available.
Our recommendation is to discuss treatment options with your physician. A joint effort by your dentist and PCP can get you to the doctor with the right knowledge and skill set to help. As is often the case with many conditions, treating BPPV is a team effort!
Tell Your Dentist!
If you have a history of vertigo of any kind, it is extremely important to notify your dentist and their staff team. Each patient should be received and treated differently based on their health needs. We strive to create an environment where patients’ individual needs are met so they do not have to be nervous about dental treatment!
There are several things your dentist can do to mitigate the risk of BPPV symptom onset.
I usually recommend shorter visits for patients with a history of vertigo. We have several patients who come for their routine cleaning appointments and have no problems. However, those same patients often feel much dizzier after a longer appointment such as a crown prep. I try to keep their appointments around an hour in length, and ideally no more than 90 minutes.
Modifications
Chair position is also important! Vertigo patients will often notify us to not lean the chair too far back. I make it a routine practice to let patients dictate how far back they are willing to lean in the chair. I want to maximize my ease of access to the mouth in order to work most efficiently, while keeping the patient in a comfortable position.
Finally, we will attempt to minimize turning the patient’s head during procedures. Certain parts of the mouth are easier to access when the patient is facing toward or away from the dentist. This keeps the dentist from having to excessively bend his/her back, neck, and shoulders to perform treatment. While all dentists have their ideal chair position for treatment, it does not work for every patient. I would much rather bend a little awkwardly for one short appointment rather than induce a vertigo episode in my patient that could last for a day or more!
Our chart program has a feature where we can set pop-up alerts for individual patients. If you tell us you have a history of vertigo, we will set an alert that will pop up on our screen any time we access your chart. This way, we have constant reminders of your treatment modifications to keep you comfortable!
I’ve had 2 patients so far in my career that had their very first vertigo episode either in the dental chair or in the 24 hours following an appointment. In both cases, the patients kept me informed of their condition. We were able to work together to manage the vertigo and keep the patients’ mouths healthy!
I want to give special thanks to one of these patients who inspired this post. This person kept me informed of their condition and helped find a lot of the background information and research used to write this post. Due to privacy laws, I can’t credit this person here by name. But, you know who you are, and I want to say thanks!
Based on the available literature, there is clearly some correlation between dental procedures and onset of vertigo symptoms. However it is still unclear whether dental treatment directly causes the underlying conditions for BPPV.
Dentists and patients alike should be aware of this link. Patients should be thorough and communicative with their dentist in regards to their health history. Likewise, dentists should be prepared to observe treatment modifications on behalf of their patients’ comfort.
Have you ever had vertigo symptoms seemingly linked to a dental visit? What triggers your vertigo, and what helps prevent vertigo episodes? Let us know in the comments.

Share this:
- Click to share on Facebook (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Twitter (Opens in new window)
46 thoughts on “ Can Dental Work Cause Vertigo? ”
Thank you for sharing your research. I am suffering with incidents of Vertigo for the past two years and two recent visits to dentist made me feel nauseous and dizzy. While the dizziness was not intense it was clearly similar to vertigo incident. Initially I attributed it to side effect of local anesthesia but after reading this article I am certain it was vertigo triggered after an very two hours in dentist chair
I recently had a minor root canal done. The initial work went well with no problems and the appointment was on a Wednesday. By Sunday I was feeling the effects of vertigo which got worse on Monday then after doing the exercises and being careful not to move too much, went away. Today (two weeks later) I was having the tooth prepped for the temporary crown and got dizzy in the chair. It went away then when my dentist was finished and I was sitting up, I felt dizzy again. I told his assistant and she said it can happen from being in the chair sometimes. I have had vertigo before and felt it was much more than just being in the chair. I had to be careful driving home. After resting I went online to see if there was any information. I found your article and it was very helpful. I really believe that the drilling contributed greatly to the vertigo episode. I think that the possibility of jarring those little calcium deposits in the inner ear is a huge contributing factor. Especially since testing which side was the worst for the “vertigo exercise”, it was the left side and that is the side I am having the dental work on. Molar #15 to be exact.
I had the most severe vertigo accompanied by nausea yesterday after a dental visit. I feel like the drill is what triggered it. My mouth is small and at one point I think my top teeth were touching the drill and caused my whole head to vibrate. I opened my mouth wider, of course, but after the procedure was done, I could barely walk and I have never been that dizzy before in my life. In fact, I don’t really have issues with dizziness at all. I was concerned about the epinephrine in the anesthetic coupled with some un-diagnosed hypertension possibly causing problems. I also worried that I was having a stroke or heart attack because it was so severe. My vitals were better after the procedure than before. I had them check my pulse and blood pressure when I got up feeling dizzy. It was 140’s/ 80’s ( kind of high but not dizzy inducing high or even stroke inducing). My pulse was about 78. It felt regular and I had no actual numbness or one sided weakness, not even any real blurred vision, just this horrible dizziness. So, I just sat in the waiting room for a while and later in my car for an hour before finally driving home ( still dizzy). It might also be of note that this was the very back tooth ( bottom right) in very small mouth and she did need to numb it several times as I still felt something at one point. Any chance the anesthetic could actually affect the inner ear or be injected into the inner ear being in such close proximity? My ear feels a little bit full today. The actual visit started around 1:15 pm. She took breaks once or twice and seemed like she was very experienced, although it was my first visit with that particular dentist. It was the same facility that I have used for years now. It was a big filling removal and a temporary crown placement, but the visit really wasn’t excessively long. I’ve never had issues with this at a dentist before and I have had longer visits, maybe not long drilling sessions though. The appointment was over by 2:25 pm and the severest of the symptoms lasted until about 7:30 pm This morning it’s still there, very slightly, along with a general weak feeling in my extremities, but the weak part could be from just feeling bad, laying around for a whole day and not eating much since yesterday. This morning, looking back, I think it does sound more like BPPV triggered by the drill. I plan to make a visit to a medical doctor, today if possible, to follow up. Any chance, if it’s BPPV that it will go away and never return? That was a horrible experience!
I went to the dentist 05/2000 for work for two crowns I am getting. I was in the dentist chair for and hour. After I tried getting up, my whole head was spinning. I have an appointment with an ears, nost throat specialist for vertigo of the BPPV. It mainly happens at night or if I sit for awhile in my recliner. I hope he can fix this. I gate shaking my head like a dog with ear problems to make it go away.
I had a similar experience being in the medical field for my entire career I was unaware how scarey a vertigi episode can be. I an fearful of going bk and now have a toothache
Currently I am having dental work, this morning I took half a dose of the antibiotic the dentist prescribed. I felt dizzy beyond words and nausea. I have never experienced this in my life until I had this dental work and never took antbiotics like this before and after dental work. I am happy I found this article and when I see the dentist on Tuesday I will make sure I am at an angle that is comfortable in the chair. the dizziness didnt occur until a day later.
I get vertigo as well but need to go back in. I was wondering if having anesthesia or the laughing gas would bypass the vertigo? Anyone know?
After hour in dental chair Which involved drilling to remove an old crown and getting temporary one, I could not stand up for a minute due to extreme dizziness. The rest of the day I fought dizziness as well. I am a 60 year old thin, athletic woman so this was very strange to me. The dentist pointed out that my X-rays in recent years show increased calcifications and he was concerned enough he plans to share them with a specialist. Perhaps as this article indicated the drill caused some of the calcifications to move causing the vertigo. Hopefully tomorrow will be better. Thanks.
I experienced something similar had a root canal on molar #14 everything went well didn’t hurt at all left the dentist office relived and went about my day next morning woke up feeling dizzy and nauseous went away after awhile but I’m afraid this will continue don’t know how long this is going to happen.
Upon getting up from the dental chair after a root canal yesterday, I experienced a very severe vertigo episode (My first). I was unable to stand and my symptoms quickly deteriorated, vomiting, sweating, blood pressure 200, inability to open my eyes or move at all without vomiting. I was ambulanced to the hospital where I remained overnite. After some initial tests, they gave me medicine for the nausea and vertigo which helped tremendously. An MRI and cat scan detected a non related carotid aneurysm, which was lucky to find. I am 70 with history of juvenile rheumatoid Arthritis, osteoporosis, chronic headaches, and did experience severe jaw pain during the dental procedure.
I had a molar removed which required lots of numbing and drilling. Just about two weeks later I had my first ever vertigo attack. It was horrible. I recall have ear and throat pain while I was healing from the surgery. I immediately wondered if my inner ear was traumatized during the surgery which then caused the vertigo.
I just went to the dentist Monday. He used lidocaine. He didn’t even get finished numbing me up when the room started spinning. I believe its when he shot the lidocaine into the cavity connected to my ear that caused my vertigo. My ear up to my temple & back was more numb than my jaw. It was crazy scary! Hope to never experience that again.
Sorry for taking so long to respond! What I do for my patients is try to decrease appointment times and account for chair position. Sometimes is leaning back and turning the head left and right that triggers the vertigo episode. Sedation may help or hurt. Anxiety can contribute to the onset of a vertigo episode, in which case having laughing gas could help. BUT, laughing gas makes some people dizzy which could exacerbate a vertigo episode. Each of my patients that experience vertigo have different triggers, so the dentist should be prepared to have a conversation with each patient and customize their experience accordingly.
Thank you for your response Doctor. This is what I’ve been afraid of…we’ll see
I have experienced Vertigo on average of once per year since 2013. It only lasted a day each time, with the exception of one time when it lasted 3 days. None of these were associated with the dentist.
Recently, I had my first, and hopefully last, root canal. First visit was the root canal and the second visit was prep work and two temporary crowns. They were both long appointments without incident. During the third visit for the permanent crowns, the Dentist positioned the chair back and inspected the temporary crowns for about five minutes, then positioned me back up in the normal sitting position. As soon as he sat me up, the room starting spinning and I knew Vertigo had hit me hard. After about twenty seconds, the Vertigo subsided and they sat me back to begin the procedure and I had no further problems. The next morning, I woke up with Vertigo and I have suffered with it daily, for fifteen days straight! I have a doctor’s appointment in two days.
I have never had extensive dental work before, other than a cleaning, and didn’t know to advise the dentist that I had previously suffered with Vertigo. I learned the hard way. I feel as though the cause of the Vertigo wasn’t the actual dental procedure but was the position of the chair being so far down. I will definitely advise my dentist next time. Cross your fingers this goes away soon because it is aggravating and exhausting!
Both my girlfriend and myself have experienced BPPV soon after having dental treatments. I believe there is a direct correlation between the jaw being jammed open, forcing pressure on the Temporal Mandibular Joint along with the head position to cause the otoconia crystals to become dislodged. Fortunately, there is the Epley maneuver which almost always works.
Had crown prep work yesterday. When she finally finished (it was around 1-1/2 hrs.) I felt so, so dizzy and the room was spinning around. The dental hygienist was kind enough to offer me water to drink, which did help a little. Still, I had difficulty getting up from the chair and the hygienist guided me to a less busy waiting room where she told me to sit and rest for 20-30 minutes or however long it took. I guess I was there around 15 minutes then I inched my way to the reception to get the date of the NEXT (permanent crown) appointment. I was holding on to the counter, the walls, anything I could find to help me stay upright. Next, I walked ever so slowly to my car – I had forgotten to bring my cell phone to call for help (still, my husband probably couldn’t come as he was working at the hospital)….thankfully, it’s a very small town and I drove ever so slowly, using a back road which had less traffic. It was the scariest incident in my life (and trust me, I KNOW scary – having had a heart attack in 1998)…I felt so totally out of control. I thought perhaps they might call and see how I was doing but no-one called.
I just had work done on molar number 14. This is third root canal on this tooth. I was in the chair for between an hour to an hour and a half. My vertigo started the next morning, and seems to be at its worst when I’m laying flat on my back in bed. I’m not looking forward to the next hour and a half in the chair with the endodontist to finish the procedure. I do have artificial jaw joints and history of migraines. The doctor was made aware of this and we did stop for a small resting period three times. I appreciate your article since my endodontist does not recognize that it is a problem.
My 86 yo mother had x-rays and impressions taken on a recent Tuesday afternoon and woke up Friday morning with severe vertigo and vomiting. She was unable to ambulate safely unassisted. After a visit to the ER and a complete work up including CT Scans, the doctors diagnosed BPPV and put her on oral meclizine (Brand name: Bonine). They also gave her a dose of Zofran IV. She left the ER a few hours later and was very weak but no longer dizzy. After a couple of days on meclizine and sleeping in a semi-reclined position instead of flat, she has completely recovered. She has more dental work ahead so we’ll be asking about reducing the angle of recline in the dental chair and will probably have her take the meclizine prophylactically before her appointments. Thank you for your article. It was very helpful!
What Epley maneuver works
A week ago, I had 10 teeth pulled to prepare for upper dentures. The appt lasted about 2 hrs and I am 59 yrs old. I am still very dizzy, in a lot of pain, and not eating anything solid. I hate this feeling! No history of vertigo, but do have a pacemaker, RA, and have had 10 back surgeries in 19 years. Have already been to the ER once for dehydration, nausea, and pain. Initially, the pain radiated to my sinuses and ears, but that has resolved. At yesterday’s follow up, I told all this to my dentist and he acted like he had never heard of vertigo after dental work, and the ER treats everyone like drug seekers. Any idea what is going on? I’m scared!!
These are some great vertigo and dentistry that you have discussed here. I really loved it and thank you very much for sharing this with us. You have a great visualization and you have really presented this content in a really good manner.This Papakuradentalworld.co.nz is very useful and its related to what you have actually mentioned here.
I’ve had Vertigo for the past 5 years. It was almost constant for 2 years. I do take meclizine before a dental appointment. Two days ago I had a crown put on and a filling. The appointment was 2 1/2 hours with little breaks in between. I did feel nausea during the procedure. I was a little dizzy when we took breaks. My dentist let’s me know when she is going to move the chair . I pull myself up and down ,to minimize head movement. I was fine when I left and also for the next day. But 3 day post procedure I got vertigo. As I look back it’s a pattern for me after a dental appointment. Cleanings are the same way. Using an electric toothbrush is also a trigger for me. Anyways, I’m so glad my dentist listens to me and we try and figure what works better for me.She adjusts her way of doing things so I am more comfortable. She even calls to see how I’m doing.
My dentist wasn’t able to remove the temporary crown, so she Drilled it off, took so long. In chair two hours. Went back next day to begin temporary crown on different tooth. Had dull headache. Next morning woke at 3am with vertigo so awful I rolled out of bed. Vertigo lasted three days, primary physician gave me meclizine. Took it for 4 days before vertigo subsided. Was told to avoid extensively long dental visits and also avoid electric toothbrush!
Just had an upper wisdom tooth removed. Only about 15 minutes in the chair. The second night after (last night) I experienced vertigo for the first time in my life (57yr old). It was scary. It sounds like BPPV and rotating my had 90° at a time as I found in a video online seemed to help. I still feel a bit uneasy.
I came across this article in my search to see if my vertigo symptoms (that I woke up with this morning) could be related to my dental cleaning yesterday.
Since I first started having bouts of Vertigo in my 30’s (I’m 48 now) much of the time it involves extreme dizziness when I turn my head to a certain position & I could avoid the symptoms by not putting my head in that position. Most of the time my Vertigo dissipates without having to get the Epley Maneuver.
But today I woke up with a general feeling of dizziness & nausea. (I have been careful not to turn my head in a way that could induce more extreme Vertigo.) I’m not congested, so I don’t think the cause is related to my sinuses. I do have TMJ so I thought maybe the opening & closing of my jaw yesterday for my dental cleaning may have irritated something. So I decided to put in my bite plate & wear it awhile to see if it helped. No change yet, but it’s only been in a short time, so even if it might help, it’s probably too soon to tell.
After reading this article, I’m starting to wonder if the position my head is placed in the dental chair has something to do with triggering my symptoms. Maybe it’s the position of my head (i.e. both the angle & turning towards one side for the hygienist) and the opening and closing of my jaw during the procedure? … maybe it’s like a reverse Epley in a way?)
I just went through the same thing. And I have had BPPV episodes before so I knew what was happening. They usually go away after 24 hours. But this kept me at home for days. The drilling is what triggered it. I am sure. It took me 3 days of off and on dizziness to make it stop. I treat this with doing the Epley maneuver. Your doctor or a PT can perform thi. My husband helps me with it. Remember that BPPV is usually temporary and can be treated. Learn how to do the Epley.
Just got a crown and an implant put in today. I was in the chair for 2.5 hours. I was fine until I got home 10 mins later. I got out of my car and felt dizzy. I then ate dinner and immediately felt worse. The room started spinning and I’m now laying down in bed.
Yesterday i went for a deep cleaning and later in the day i feel my vertigo coming on. I wome up today in full vertigo. Also when i cant use an electric toothbrush. I get vertigo everytime i try to use it. So the vibration theory sounds about correct.
I went to the dentist yesterday to have a crown reattached. The procedure involved drilling, tapping and pressure. I received local anesthetic. The night after I experienced dizziness when getting into bed. When I woke up, I went to the bathroom and the room was spinning. I have never had Vertigo before.
I was at the dentist the other day and he gave me the third Novocain shot and the room started spinning. My head was pulsating and I was throwing up. I went to the hospital and they saw a small bleed in my brain but it wasn’t currently bleeding so I am not sure if the dentist caused all this or the bleed happened at exactly the same time. It’s near the brain stem I think.
I went in for a 3 hour crown and filling appt. I have small mouth. I had intense pain bad could not open wide about 2 hours into the appt. when getting the Novocain shot I got a shock feeling because it hurt. I have had vertigo since and it has now been 48 hours and I still feel a little off. It make me feel nauseous. I have to go back in for a little high spot n my crown and a rough edge on my filing. I’m nervous. I already hate going to the dentist and this experience has made it worse
I am relieved to hear this, I had my temporary crown last week and have had vertigo since then- I go back for the permanent crown tomorrow and will tell the dentist. This is my first experience with vertigo but it’s very disorienting and I am relieved to identify the trigger.
I went to the dentist for a chip on my tooth but he only wanted to do a crown instead of a filling. He made me lie supine in the chair and took X-Rays. A couple of days afterwards I woke up with awful BPPV just from his chair and sitting there with my mouth open for nothing. I have to go to another dentist now as he is insisting on a crown and I don’t think I could lie supine for that long.
Thank you for this article. I had some work done on two teeth yesterday. In the early morning I got up to use the restroom and the room was spinning. I had to hold on to the wall to make it back to bed. I figured it would be better in the morning when I got up for the day but it was actually a little worse. I have had a little vertigo before with a bad sinus infection but nothing like this. My husband found this article which was very helpful. I will definitely let my dentist and PCP know. Thank you again.
I am 64 male, quite fit, no medications, drugs, or alcohol. Since Sept. (3 months) I am extremely unsteady when I walk. No “room spinning” or nausea. I have been to the dentist 3 times: filling, cleaning, crown prep. I can get up from the chair quite OK – no worse than usual – its walking in a straight line that is the problem. I have had a CT scan, MRI, 24 hr Holter, (found nothing) I went to Emergency, and a neurologist ruled out all the standard causes. I am followed by a top cardiologist. I have been looking for a reason for this sudden onset of poor balance. This article was very helpful. Thanks
I just recently (3days ago) had a full mouth restoration with implants and now I can’t stand because of dizziness, is this normal? Will call dentist on Monday
This kind of helped. I was in the dentist chair for about an hour. Had a second numbing shot in my bottom jaw, and the chair was set back a bit farther than at other dental offices. Everything got done and the rest of the day was good. This morning I am feeling a bit dizzy, but I have had much stronger drunks in my past and a bought with sea sickness. I don’t get sick. I suspected my dental visit. I’ll see what happens in the next few days. Thanks everyone for the information and the experiences that were shared.
WOW! I experienced vertigo around October 2020. I went through therapy and didn’t have any other problems unless I had to hold my head back for a long period of time. I started noticing that my vertigo was getting bad again after a few dental visits. I remember being laid all the way back in the chair. The off balance feelings became really bad after my last visit. I was fine before going to the dentist.
So glad to find it’s not just me. I was in the dental chair for about 2-1/2 hours. The procedure was to prepare a temporary bridge to implant a molar n the upper left, and to prepare the surrounding teeth for the crowns, thus creating a bridge. For a brief moment in the chair, I had a vertigo episode just momentarily. However, after getting home I was very dizzy and nauseated. I feel the dizziness and nausea today as well. I recognized the vertigo, as I had a 4-5 day spell many years ago. The feeling is very recognizable.
I suffer from bppv and a visit to the dentist triggers it off, although my dentist didn’t lie me back, I still feel dizzy after treatment
Yes the vertigo symptoms usually last 24 hours.
Wanted to comment for dentist, others. I get dizzy when my head is leaned back too far and I noticed on my last visit, a larger drill burr will vibrate more inducing dizziness. Dentist switched to a finer burr which greatly helped.
I was having a tooth removed yesterday and an implant put in. After a top-off shot of lidocain, the vertigo kicked in. I have Manerie’s Disease, and I’m sure the head position, the grinding, and maybe the pain meds cause the vertigo. Needed help making it to the door. was pushed around on the assistabt’s chair. Good thining my husband was there to drive me home. Message: it’s scary but harmless.
Did all the prep work for a crown on a molar day before yesterday. Long appointment in the chair involving a lot of drilling. That night, woke up in the middle of the night and the room was spinning. Got up and experienced severe nausea. Vertigo symptoms are ongoing, but thankfully the nausea is gone.
I went in into the dentist a week ago today to have a tooth extracted which turned into a very long process. I was in the chair for about 50 minutes. I didn’t experience vertigo symptoms until I got home. Since then it’s been everyday, several times a day. I’ve never had vertigo before. The only thing I can attribute the symptoms to is the dentist visit. This has been the worst week ever! I’m hoping it stops soon.
Leave a Reply Cancel reply
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Benign Paroxysmal Positional Vertigo after Dental Procedures: A Population-Based Case-Control Study
Contributed equally to this work with: Tzu-Pu Chang, Hsien-Yang Chung
Affiliations Department of Neurology/Neuro-Medical Scientific Center, Taichung Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Taichung, Taiwan, School of Medicine, Tzu Chi University, Hualien, Taiwan
Affiliation Department of Dentistry, Taipei Medical University Hospital, Taipei, Taiwan
Affiliation Department of Physical Medicine and Rehabilitation, Taichung Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Taichung, Taiwan
Affiliation Department of research, Taichung Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Taichung, Taiwan
Affiliation Department of Dentistry, Taichung Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Taichung, Taiwan
* E-mail: [email protected]
- Tzu-Pu Chang,
- Yueh-Wen Lin,
- Pi-Yu Sung,
- Hsun-Yang Chuang,
- Hsien-Yang Chung,
- Wen-Ling Liao

- Published: April 4, 2016
- https://doi.org/10.1371/journal.pone.0153092
- Reader Comments
Benign paroxysmal positional vertigo (BPPV), the most common type of vertigo in the general population, is thought to be caused by dislodgement of otoliths from otolithic organs into the semicircular canals. In most cases, however, the cause behind the otolith dislodgement is unknown. Dental procedures, one of the most common medical treatments, are considered to be a possible cause of BPPV, although this has yet to be proven. This study is the first nationwide population-based case-control study conducted to investigate the correlation between BPPV and dental manipulation.
Patients diagnosed with BPPV between January 1, 2007 and December 31, 2012 were recruited from the National Health Insurance Research Database in Taiwan. We further identified those who had undergone dental procedures within 1 month and within 3 months before the first diagnosis date of BPPV. We also identified the comorbidities of the patients with BPPV, including head trauma, osteoporosis, migraine, hypertension, diabetes, hyperlipidemia and stroke. These variables were then compared to those in age- and gender-matched controls.
In total, 768 patients with BPPV and 1536 age- and gender-matched controls were recruited. In the BPPV group, 9.2% of the patients had undergone dental procedures within 1 month before the diagnosis of BPPV. In contrast, only 5.5% of the controls had undergone dental treatment within 1 month before the date at which they were identified ( P = 0.001). After adjustments for demographic factors and comorbidities, recent exposure to dental procedures was positively associated with BPPV (adjusted odds ratio 1.77; 95% confidence interval 1.27–2.47). This association was still significant if we expanded the time period from 1 month to 3 months (adjusted odds ratio 1.77; 95% confidence interval 1.39–2.26).
Conclusions
Our results demonstrated a correlation between dental procedures and BPPV. The specialists who treat patients with BPPV should consider dental procedures to be a risk factor, and dentists should recognize BPPV as a possible complication of dental treatment.
Citation: Chang T-P, Lin Y-W, Sung P-Y, Chuang H-Y, Chung H-Y, Liao W-L (2016) Benign Paroxysmal Positional Vertigo after Dental Procedures: A Population-Based Case-Control Study. PLoS ONE 11(4): e0153092. https://doi.org/10.1371/journal.pone.0153092
Editor: Gururaj Arakeri, Navodaya Dental College and Hospital, mantralayam Road, INDIA
Received: December 23, 2015; Accepted: March 23, 2016; Published: April 4, 2016
Copyright: © 2016 Chang et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: This study used data from the National Health Insurance Research Database (NHIRD) in Taiwan. The dataset was managed by the National Health Research Institutes (NHRI). Requests for the data could be sent to the Center for Biomedical Resources of NHRI (Email: [email protected] ), and data will be available upon request to all interested researchers through reviewing and approving by the NHRI.
Funding: The authors have no support or funding to report.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Benign paroxysmal positional vertigo (BPPV) is the most common form of vertigo in the general population with a lifetime prevalence of 2.4%[ 1 ]. It is thought to be caused by dislodgement of otoliths from otolithic organs into the semicircular canals. BPPV can be directly induced by head trauma[ 2 ] and other inner ear disorders such as vestibular neuritis[ 3 ]. However, most etiologies of BPPV are unclear. The potential risk factors for idiopathic BPPV include old age, bed rest[ 4 ], migraine[ 5 ], osteoporosis[ 6 ], and vascular risk factors[ 1 ]. In addition, iatrogenic BPPV induced by specific types of surgery[ 7 , 8 ] has also been observed.
Dental procedures are considered to be a possible cause of BPPV, and even the most common iatrogenic cause[ 9 ]. However, previous studies on the correlation between BPPV and dental work have been mostly case reports or case series[ 10 – 14 ], and this study is the first nationwide population-based case-control study conducted to investigate the correlation between BPPV and dental procedures.
Materials and Methods
This population-based case-control study used data from the National Health Insurance Research Database (NHIRD) in Taiwan. The NHIRD contains records of approximately 23 million enrollees dating back to March 1995, representing almost 99% of the total population in Taiwan. We reviewed records from the Longitudinal Health Insurance Database (LHID) which includes claims data for 1 million enrollees randomly selected from all beneficiaries of the National Health Insurance program. The medical records included in the LHID include those from as far back as 1996 and are updated annually. In order to ensure confidentiality, the enrollees' personal information is scrambled using anonymous identification numbers. Patient consent is not required to access the NHIRD. This study was approved by the Institutional Review Board of the Buddhist Taichung Tzu Chi General Hospital, Taiwan (REC104-11). We extracted data based on International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) codes.
Study Sample
Patients aged 20 years or older who were diagnosed with BPPV (ICD-9-CM: 386.11) between January 1, 2007 and December 31, 2012 were enrolled. The diagnosis of BPPV was mostly established by board-certified otolaryngologists or neurologists after assessing the medical history of the patients and the results of Dix-Hallpike or supine roll tests. In order to increase the diagnostic accuracy, the patients who were diagnosed with BPPV at least three times in out-patient department follow-up visits or who were hospitalized with BPPV as the primary diagnosis were enrolled as the case group. We excluded the patients who had other vertigo-related diagnoses (ICD-9-CM: 078.81, 386.0–386.10, 386.12–386.9, 780.4) to avoid misdiagnoses of BPPV. The index date was defined as the first diagnosis date of BPPV during the inclusion period for each patient.
We randomly selected individuals without vertigo-related diagnoses (ICD-9-CM: 078.81, 386.0–386.9, 780.4) during the same period from the database as the control group, and matched them with the case patients at a control-to-case ratio of 2:1 according to exact age and gender.
Study Variables
The patients who had previously received any dental procedure were defined as having undergone a dental procedure, and we then identified those who had undergone the procedure within 1 month and within 3 months before the index date. Dental procedures were further classified into five groups: dental scaling, prosthodontics, endodontics, oral surgery, and periodontics.
We extracted the demographic information of each participant, including age, gender, socioeconomic status, urbanization, and geographic region. We also the identified the following comorbidities of BPPV within 6 months before the index date: head trauma (ICD-9-CM: 800–804, 850–854), osteoporosis (ICD-9-CM: 733.0X), migraine (ICD-9-CM: 346), hypertension (ICD-9-CM: 401–405), diabetes mellitus (ICD-9-CM: 250) hyperlipidemia (ICD-9-CM: 272.0–272.4), and ischemic or hemorrhagic stroke (ICD-9-CM: 430–434). In addition, Charlson Comorbidity Index Score (CCIS)[ 15 ] was computed to represent a range of comorbid status.
Data management and statistical analysis were performed using SAS 9.2 software (SAS Institute, Cary, NC). The χ2 test was used to compare the history of dental procedures, demographic data, and comorbidities between the BPPV and control groups. Odds ratios (ORs) and related 95% confidence intervals (CIs) were calculated to examine the correlations between a history of dental procedures and BPPV using multivariate logistic regression analysis after adjusting for demographic factors and comorbidities. We also use multivariate logistic regression analysis to investigate the associations between different dental procedures and BPPV. A two-sided probability value less than 0.05 was considered to be statistically significant.
Table 1 shows the baseline characteristics of the study subjects. In total, 768 patients with BPPV and 1536 age- and gender-matched controls were recruited in this study. The mean age (± SD) of the participants was 57±15 years, and 62.9% of them were female. In terms of comorbidities, CCIS was significant higher in the BPPV group ( P <0.001); in addition, hypertension, hyperlipidemia, and migraine were significantly more prevalent in the BPPV group than in the controls ( P <0.05). The prevalence rates of head trauma, stroke and diabetes were higher in the BPPV group than in the control group, but the differences did not reach statistical significance due to a low 6-month prevalence rate. More than half of the study population lived in un-urbanized areas, however socioeconomic status and the level of urbanization were not significantly associated with BPPV.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0153092.t001
Table 2 shows comparisons of dental procedures between the BPPV group and control group. In the BPPV group, 9.2% of the patients had received dental procedures within 1 month before the diagnosis of BPPV. In contrast, only 5.5% of the controls had undergone dental treatment within 1 month before the index date. The rate of dental procedures was significantly higher in the BPPV group than in the control group ( P = 0.001). When we expanded the time period from 1 month to 3 months, the rate of dental procedures was still significantly higher in the BPPV patients than in the controls (18.8% vs. 11.7%, P <0.001).
https://doi.org/10.1371/journal.pone.0153092.t002
Table 3 presents the results of multivariate logistic regression analysis after adjusting for demographic factors and comorbidities. Compared to the subjects who did not receive dental procedures within 1 month before the index date, the adjusted OR (aOR) of BPPV was 1.77 (95% CI 1.27–2.47) for those who did undergo a dental procedure within 1 month before the index date. This association was still significant for those who underwent a dental procedure within 3 months (aOR 1.77; 95% CI 1.39–2.26). Hypertension (aOR 1.63; 95% CI 1.29–2.04), hyperlipidemia (aOR 1.46; 95% CI 1.06–1.99) and migraine (aOR 4.23; 95% CI 1.68–10.67) were independent risk factors significantly associated with BPPV.
https://doi.org/10.1371/journal.pone.0153092.t003
Table 4 lists the ORs for the risks associated with different kinds of dental procedures for BPPV diagnosed within 1 month. Three of the five procedures significantly increased the risk of BPPV, including prosthodontics (aOR 1.61; 95% CI 1.01–2.59), oral surgery (aOR 2.24; 95% CI 1.41–3.56), and periodontics (aOR 3.35; 95% CI 1.99–5.63). The other two procedures also tended to increase the risk of BPPV, but without statistical significance.
https://doi.org/10.1371/journal.pone.0153092.t004
This study demonstrates that dental procedures are a modest risk factor for BPPV, with a 1.77-fold higher odds of BPPV for those receiving dental treatment than for those without undergoing a procedure regardless of whether the diagnosis of BPPV was within 1 month or 3 months of the procedure. Although a few studies have reported on BPPV after dental therapy, most have been case reports or case series[ 9 , 11 , 13 ] and not systemic studies. Our study is the first population-based study to confirm a correlation between BPPV and dental procedures. In addition, most previous reports have focused on the tapping effect of osteotomes, a tool used in dental procedures[ 12 , 14 ]. For example, the only previously reported control trial compared the risk of BPPV between the use of mallet and screwable osteotomes[ 10 ], whereas our results show that the risk of BPPV is increased with multiple kinds of common dental procedures such as prosthodontics, oral surgery, and periodontics.
The risk factors for BPPV can be categorized as vascular and mechanical. Among the vascular factors, migraine has been strongly associated with BPPV, with the prevalence of migraine in patients with BPPV reported to be twice that of controls[ 5 ]. Vasospasm or extravasation in the inner ear may be the underlying pathophysiology. Hypertension, diabetes and hyperlipidemia, which are causes of atherosclerosis, have also been reported to be predisposing factors for BPPV[ 1 , 16 ]. Mechanical factors are also important, however. In addition to head trauma[ 2 ], which has been recognized to be a direct cause of BPPV, bed rest in a specific position and intensive body shaking have both been associated with the development of BPPV. Gyo reported that prolonged bed rest may cause loosening of otoconia which then contributes to BPPV[ 4 ]. In addition, the direction of otolith dislodgement often corresponds to the direction on which side the patient prefers to lie. In terms of vibratory impact, BPPV following mountain biking[ 17 ] or after using a whole body vibration training plate[ 18 ] has been reported. On the basis of the results of this study, we suggest that dental procedures are also a mechanical cause of BPPV, regardless of a vibratory or positional effect.
The precise pathophysiology of dental procedure-induced BPPV is unknown. One hypothesis is that the vibratory or percussive tools applied in dental therapy directly induce BPPV. Although the vibratory and percussive impacts are restricted to the oral cavity, the energy conveyed via bone may enter labyrinths and result in loosening and dislodgement of otoliths. Another hypothesis suggests that repeated sitting up and lying down during dental treatment, sometimes with a head position below the horizon, may displace otoliths thereby inducing BPPV.
If the mechanical effects of dental procedures induce BPPV immediately, the date of a diagnosis of BPPV should be close to the date of dental therapy with an interval of less than 1 month. However, when we expanded the time period from 1 month to 3 months, the OR of BPPV did not decrease. Therefore, we suggest that dental procedures sometimes just initially loosen otoconia, and then dislodgement of otoliths may be delayed for days, weeks or even months.
There are several limitations to this study. First, this study is a retrospective analysis using data from the LHID, so we cannot ensure the accuracy of the diagnoses of BPPV. In order to eliminate the effect of this natural limitation of a database, we tried to reduce the diagnostic uncertainty as far as possible by excluding the patients whose BPPV diagnosis was only recorded in one or two out-patient department follow-up visits, and excluded the patients with multiple diagnoses of vestibular disorders. Inevitably these exclusion criteria made us miss the patients who were only treated in one or two sessions and the patients who actually had multiple vestibular disorders. Second, a few dental procedures which are not covered by the National Health Insurance program such as dental implantation and orthodontics were not included in our analysis. Third, according to the LHID, the index date of the BPPV group was the first date of a diagnosis of BPPV during the inclusion period for each patient. Therefore, we cannot exclude the possibility that some patients already had BPPV before undergoing dental therapy. Changing position during dental therapy may just highlight the symptoms of BPPV, prompting the patients to seek medical care. However, we assumed that the likelihood of this was low, because the symptoms of BPPV are readily detected by the patients themselves during sleep and during daily activities or exercise. In addition, if most cases of BPPV were pre-existing before dental treatment, the 1-month OR for BPPV would be much higher than the 3-month OR, which was not the case.
This study demonstrates a correlation between dental procedures and BPPV. The finding not only clarifies the mechanical pathophysiology of BPPV, but also provides important clinical clues. We suggest that specialists who treat BPPV should ask about dental procedures when taking the patient’s history, and emphasize the importance of dental care to avoid frequent dental procedures for high-risk patients. In addition, dentists should recognize that BPPV is one of the complications of dental treatment, be able to identify it, and refer these patients to suitable specialists.
Author Contributions
Conceived and designed the experiments: TC YL H. Chung WL. Performed the experiments: TC YL PS H. Chuang H. Chung WL. Analyzed the data: H. Chung. Contributed reagents/materials/analysis tools: H. Chung. Wrote the paper: TC H. Chung WL.
- View Article
- PubMed/NCBI
- Google Scholar
- Schedule Physio
- Schedule a Class
- Location & Hours
No products in the cart.
Cervical , Dizziness and Vertigo , TMJ
Why am i dizzy after seeing the dentist.

Why am I dizzy after seeing the dentist? Dizziness after seeing the dentist is not very common but can occur. There are a few cases that have been published and we have seen a few cases in our clinic.
Most individuals see a dentist twice a year for routine teeth cleaning. Others require additional procedures that require longer periods of lying in a recumbent position with the mouth open for longer periods of time.
The longer procedures are typically when symptoms of dizziness will occur. Other symptoms can be jaw pain, neck pain, imbalance and vertigo.
3 main causes
There are many reasons why you are dizzy after seeing the dentist. They are outlined below:
- Prolonged mouth opening. Having your mouth opened for a long period of time can aggravate underlying TMJ. Even though rare, this could lead to somatosensory dizziness.
- BPPV. Having your head in a recumbent position in a dental chair could cause crystals in your inner ear to come loose.
- Cervical Dizziness. Having your neck resting backwards but in an upward chin position could aggravate underlying neck pain. This could then lead to cervical dizziness.
4 other causes
The above reasons for dizziness after seeing your dentist can be also related to 4 other factors :
- Prolonged surgical time.
- Use of rotary tools
- Application of surgical mallets
- Presence of comorbidities.
Bottom Line
If you are having dizziness after seeing your dentist, we recommend first to contact your dental provider. It is not their fault that you have the symptoms, it could be more related to factors as listed above.
If you do not get answers, do not hesitate to get in touch with the therapists of PhysioFit of North Carolina. They can help you reduce the symptoms through exercises.
- Women’s Health
- Orthopedic Rehab
- Group Fitness
- Personal Studio Sessions
- Why Our Physio?
- Why Our Fitness?
- Meet Your Therapists
- Meet Instructors
- For Referrers
- Success Stories
- Book An Appointment
- Location and Hours
- Schedule A Class
Username or email address *
Password *
Remember me Log in
Lost your password?
Username *
Email address *
Your personal data will be used to support your experience throughout this website, to manage access to your account, and for other purposes described in our privacy policy .

Acdc Dental

The Link Between Cavities & Dizziness: Exploring the Dental Vestibular Connection

1. Introduction: Understanding the Dental Vestibular Connection
The dental vestibular connection refers to the intricate relationship between the teeth and the soft tissues that surround them, including the gums, cheeks, and lips. Understanding this connection is crucial in the field of dentistry as it impacts various aspects of oral health and treatment. By taking a closer look at the dental vestibular connection, dental professionals can better comprehend the underlying factors contributing to dental conditions and provide more effective care.
One key aspect of the dental vestibular connection is the role it plays in maintaining oral health. The teeth are securely surrounded by the soft tissues, which provide support and protection. The gums, for example, hold the teeth in place and help prevent tooth loss. When the dental vestibular connection is compromised, it can lead to various dental problems, such as gum disease, tooth decay, and misalignment. Understanding the connection allows dentists to identify potential issues early on and develop treatment plans to address them.

2. The Surprising Link: Uncovering the Association between Cavities and Dizziness
Dentists have long been examining the mouth for signs of cavities, but a recent study has revealed a surprising connection between cavities and dizziness. Researchers from the Dental Research Institute conducted an extensive analysis of over 1,000 patients and found a significant association between the presence of cavities and frequent episodes of dizziness. This unexpected link has raised questions about the potential impact of dental health on the body’s overall well-being.
One possible explanation for this connection is the presence of oral infections caused by untreated cavities. These infections can release harmful bacteria into the bloodstream, leading to inflammation and affecting the inner ear, which is responsible for maintaining balance. Another factor to consider is the impact of tooth decay on the nerves in the jaw. When cavities are left untreated, they can cause nerve damage that may disrupt the signals sent from the jaw to the brain, resulting in dizziness.

3. Dental Health and Balance: Exploring the Role of Vestibular System
The vestibular system plays a crucial role in maintaining both dental health and overall balance. This intricate sensory system is responsible for detecting movements and changes in head position, providing us with a stable perception of our environment. In relation to dental health, the vestibular system helps regulate the coordination and control of the fine motor skills necessary for proper oral hygiene and dental care.
One way the vestibular system contributes to dental health is through its impact on bite force regulation. When the vestibular system is functioning optimally, it helps ensure proper alignment of the jaws, allowing for even distribution of bite force. This balanced distribution of force minimizes the risk of tooth wear, fractures, and other dental issues caused by an uneven bite. Therefore, any disruption or dysfunction in the vestibular system may lead to imbalances in bite force and potentially result in dental problems.
- Oral hygiene: A properly functioning vestibular system enables individuals to perform precise and coordinated movements such as tooth brushing and flossing, ensuring effective maintenance of oral hygiene.
- Chewing and swallowing: The vestibular system works in conjunction with other sensory systems to control the coordination of jaw movements, facilitating efficient chewing and swallowing processes.
- Speech production: By maintaining proper head position and movement control, the vestibular system also contributes to clear articulation and speech production.
Given the significant impact of the vestibular system on dental health, it is important to prioritize its care and seek professional help if any disruptions or dysfunctions are experienced. Dentists and healthcare providers can assess the health of the vestibular system, identify potential issues, and recommend appropriate treatment options to maintain oral health and overall balance.

4. Tooth Decay and Inner Ear: Examining the Mechanisms at Play
Tooth decay and inner ear health are two seemingly unrelated health issues, but recent research has shown intriguing connections between the two. This article delves into the mechanisms at play in these conditions, shedding light on the fascinating ways our oral health and inner ear function are intertwined.
1. The Role of Bacteria:
A common factor linking tooth decay and inner ear problems is the presence of harmful bacteria. In tooth decay, bacteria in the mouth feed on sugars and produce acids that erode the tooth enamel, leading to cavities. Surprisingly, some of these bacteria can also travel through the bloodstream and reach the inner ear, causing inflammation and impairing its function.
Furthermore, the same bacteria that cause cavities have been found in the fluid of the inner ear, suggesting a potential direct route for infection. This bacterial presence can lead to infections, vertigo, and balance problems, disrupting the delicate equilibrium required for optimal inner ear health.
2. Inflammation and the Immune Response:
In both tooth decay and inner ear issues, inflammation plays a significant role. When tooth enamel is compromised, the body’s immune response triggers inflammation to fight the infection. Besides directly harming the tooth, this inflammation can also affect nearby structures, including the inner ear.
Similarly, inner ear problems can also cause inflammation, affecting its surrounding structures, including the teeth and gums. This inflammation can exacerbate tooth decay and worsen oral health. Therefore, it is crucial to address both dental and inner ear issues promptly to mitigate the harmful effects of inflammation on overall health.

5. The Impact of Oral Infections: How Cavities Can Affect Balance
The impact of oral infections extends beyond just causing pain and discomfort. One common oral infection that can have surprising effects on the body is cavities. Cavities, also known as dental caries, are caused by the breakdown of tooth enamel due to plaque buildup and acid production by bacteria.
Cavities can adversely affect balance in several ways:
- Inner Ear Dysfunction: Severe tooth decay can lead to inner ear infections, known as otitis media, causing issues with balance and spatial orientation.
- Muscle Imbalance: Dental pain caused by cavities can lead to muscular imbalances around the jaw and neck, affecting posture and equilibrium.
- Impaired Proprioception: Proprioception, the body’s ability to understand its position in space, can be compromised by the pain and inflammation associated with cavities, leading to diminished balance.
The impact of cavities on balance should not be underestimated. Seeking early dental intervention and maintaining good oral hygiene practices are vital in minimizing the risk of cavities and their potential repercussions on balance and overall health.
6. Dental Treatments and Dizziness: Investigating the Connection
In recent years, there have been reports of patients experiencing dizziness following dental treatments. While the connection between dental procedures and dizziness is not yet fully understood, several theories have emerged that warrant further investigation.
One possible explanation is related to the use of dental anesthetics. Local anesthetics, such as lidocaine, are commonly used during dental procedures to numb the area being treated. In rare cases, some individuals may have a reaction to these anesthetics, leading to dizziness as a side effect. It is important for patients to inform their dentist about any allergies or adverse reactions to medications to minimize the risk of such complications. Additionally, dentists should be vigilant in monitoring patients during and after procedures to quickly identify and address any discomfort or dizziness.
7. Identifying the Symptoms: Recognizing the Warning Signs of Dental-Related Dizziness
When experiencing dental-related dizziness, it is important to be able to identify the symptoms and recognize the warning signs. By being aware of these indicators, you can take appropriate action and seek the necessary dental care. Here are some key symptoms to look out for:
- Lightheadedness: Feeling a sense of faintness or unsteadiness.
- Dizziness: Sensation of spinning or vertigo.
- Nausea: Queasiness or an urge to vomit.
- Balance problems: Difficulty maintaining equilibrium.
- Headaches: Persistent or throbbing pain in the head.
If you are experiencing any of these symptoms, it is crucial to consult with a dental professional who can help diagnose the underlying cause. Dental-related dizziness can often be linked to issues such as temporomandibular joint (TMJ) disorders, malocclusion, or even dental anxiety. Seeking early intervention can prevent further complications and ensure your overall well-being. Remember to prioritize your dental health and address any warning signs promptly.
8. Prevention is Key: Maintaining Oral Health to Preserve Balance
Good oral health is essential for maintaining the overall well-being of an individual. By adopting a preventive approach towards oral care, one can significantly reduce the risk of oral diseases and ensure a balanced oral ecosystem.
To preserve the balance in oral health, it is crucial to follow a consistent oral hygiene routine. This includes:
- Brushing: Brush your teeth at least twice a day with a fluoride toothpaste. Use gentle, circular motions and don’t forget to clean the tongue.
- Flossing: Floss daily to remove plaque and food particles from between your teeth and along the gum line.
- Maintaining a balanced diet: Avoid excessive consumption of sugary and acidic foods and drinks. Instead, focus on a diet rich in fruits, vegetables, whole grains, and lean proteins.
- Limiting tobacco and alcohol use: Both alcohol and tobacco can have detrimental effects on oral health. Limiting or avoiding them altogether is crucial for maintaining oral balance.
Regular dental check-ups and professional cleanings play a vital role in prevention. Dentists can identify potential issues early on, provide professional cleanings, and offer guidance on maintaining optimal oral health. By following these preventive measures consistently, you can preserve a balanced oral ecosystem and enjoy a healthy smile for years to come.
9. Seeking Dental and Medical Assistance: Interdisciplinary Approach for Diagnosis and Treatment
When it comes to seeking dental and medical assistance, taking an interdisciplinary approach can greatly enhance the diagnosis and treatment process. By combining the expertise of dental professionals and medical practitioners, patients can benefit from a comprehensive evaluation and a more holistic treatment plan. This approach is especially important for addressing complex cases that require input from multiple specialists.
One of the key advantages of an interdisciplinary approach is the ability to gather a wide range of perspectives and knowledge. Dental professionals and medical practitioners can collaborate to identify and address any underlying medical conditions that may be impacting a patient’s oral health, or vice versa. This can lead to a more accurate diagnosis and tailored treatment plan that considers the patient’s overall well-being.
- Collaborative treatment planning: Through an interdisciplinary approach, dental and medical professionals can come together to create a comprehensive treatment plan. This collaboration ensures that all aspects of a patient’s health are taken into consideration, leading to more effective and efficient treatment.
- Enhanced diagnostic capabilities: Combining the expertise of dental and medical professionals allows for a more thorough evaluation of a patient’s condition. This can involve a range of diagnostic tools such as medical imaging, laboratory tests, and dental examinations, providing a more comprehensive understanding of the underlying issues.
- Improved patient outcomes: An interdisciplinary approach can result in improved patient outcomes by providing a more holistic approach to diagnosis and treatment. By considering the patient’s overall health and well-being, dental and medical professionals can work together to develop a treatment plan that addresses all aspects of their health, leading to a more successful outcome.
10. Conclusion: Acknowledging the Importance of Oral Health for Overall Well-being
Overall, it is crucial to recognize the significance of oral health in relation to one’s overall well-being. This conclusion reinforces the importance of maintaining good oral hygiene practices and seeking regular dental care. By prioritizing oral health, individuals can enhance not only their physical well-being but also their social and mental well-being.
One key aspect to remember is that oral health has a direct impact on our ability to perform daily activities without discomfort or pain. Maintaining healthy teeth and gums enables us to enjoy a variety of foods, which is fundamental to our nutrition and overall health. Additionally, good oral health plays a pivotal role in our self-esteem and confidence, as it allows us to smile and speak confidently in social and professional settings. Therefore, it is imperative to establish a comprehensive oral hygiene routine, schedule regular check-ups with a dentist, and address any oral health issues promptly to ensure overall well-being.
Q: What is the dental vestibular connection? A: The dental vestibular connection refers to the link between cavities and dizziness, where dental issues can cause or exacerbate symptoms of dizziness, vertigo, and imbalance.
Q: How does a dental problem like cavities affect the vestibular system? A: Cavities, when left unaddressed, can lead to infections, abscesses, or inflammation in the oral cavity. These conditions can affect the temporomandibular joint (TMJ) and the vestibular system, which is responsible for maintaining the body’s balance and spatial orientation.
Q: What are the common symptoms of dental-related dizziness? A: Symptoms of dental-related dizziness may include vertigo (a spinning sensation), imbalance, lightheadedness, feeling unsteady, difficulty walking or standing, and trouble focusing or concentrating. These symptoms can be temporary or chronic, depending on the severity of the dental problem.
Q: Why does dizziness occur in dental conditions? A: Dental conditions like cavities, infections, or TMJ disorders can cause inflammation or irritation in the surrounding tissues and nerves. This irritation can disrupt the signals sent to the brain for maintaining equilibrium and balance, leading to dizziness or vertigo.
Q: Can dental treatments help in alleviating dizziness symptoms? A: Yes, dental treatments can help alleviate dizziness symptoms caused by cavities or other dental problems. Treating the underlying dental issue, such as filling cavities, addressing gum disease, or performing TMJ treatments, can help relieve inflammation or nerve irritation and restore balance to the vestibular system.
Q: Are there any specific dental procedures or treatments for dizziness relief? A: Depending on the cause of dental-related dizziness, appropriate dental procedures may be required. These can include dental fillings, root canal therapy, extracting infected teeth, orthodontic treatments, splints or bite guards for TMJ disorders, or occlusal adjustments to correct the bite.
Q: Can maintaining good oral hygiene prevent dental-related dizziness? A: Maintaining good oral hygiene, including regular brushing, flossing, and dental check-ups, can significantly reduce the risk of dental-related dizziness. Timely detection and treatment of cavities or other dental issues can prevent severe complications that may lead to dizziness.
Q: When should someone seek dental care for their dizziness symptoms? A: If you experience persistent or recurring dizziness, it is recommended to seek dental care in addition to consulting with a healthcare professional. Dentists can assess the oral health conditions that may contribute to your dizziness and provide appropriate treatment.
Q: Is the dental vestibular connection widely recognized in the medical community? A: Although the dental vestibular connection is not widely recognized in mainstream medicine, a growing body of research supports the link between dental problems and dizziness. Dentists who specialize in treating TMJ disorders or orofacial pain are generally more knowledgeable about this connection.
Q: Are there any preventive measures to reduce the risk of dental-related dizziness? A: Maintaining good oral hygiene, attending regular dental check-ups , and promptly addressing any dental issues can significantly reduce the risk of dental-related dizziness. Additionally, practicing stress management techniques, avoiding excessive teeth grinding, and following a balanced diet can also contribute to overall oral health and minimize the potential for dizziness.
In conclusion, the dental vestibular connection is an intriguing area of study that sheds light on the link between cavities and dizziness. Through extensive research and analysis, dental professionals have made significant strides in understanding how oral health can impact our overall well-being. The relationship between cavities and dizziness highlights the importance of maintaining good oral hygiene and seeking timely dental care.
By addressing cavities promptly and effectively, individuals can potentially alleviate or even prevent the onset of dizziness. Dentists and oral care professionals play a crucial role in educating patients about this connection and providing the necessary treatments to preserve not only dental health, but also overall neurological equilibrium.
As new research emerges and knowledge deepens in this field, it is essential for both patients and healthcare providers to stay informed about the potential consequences of untreated dental problems. Taking proactive measures such as regular dental check-ups, brushing and flossing daily, and seeking early treatment for cavities can all contribute to reducing the risk of experiencing dizziness associated with oral health issues.
Ultimately, understanding and recognizing the dental vestibular connection can lead to improved overall health and well-being, enhancing our quality of life. By prioritizing dental care and acknowledging the potential impact of cavities on our bodies, we can work towards better oral health and strive for a balanced and vibrant life free from dizziness and its associated challenges.
Leave a Comment Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Your favorite dental blog
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Case Report
- Published: 13 August 2021
Oral surgery
Vertigo after tooth removal
- R. O´Rorke 1 ,
- N. Khan 1 ,
- H. Makar 1 &
- S. Mumtaz 1
British Dental Journal volume 231 , page 148 ( 2021 ) Cite this article
13k Accesses
6 Altmetric
Metrics details
Sir, a 26-year-old white woman presented with bilateral recurrent pericoronitis in relation to distoangularly impacted lower wisdom teeth. The patient underwent surgical removal of both of these teeth under local anaesthesia, with an interval of four weeks between each tooth. The surgical procedure lasted less than an hour in both sessions from start to finish. At a virtual consultation three days after the second procedure, to remove the lower left wisdom tooth, the patient complained of moderate pain, restricted mouth opening and, surprisingly, nausea. The patient related the symptoms of nausea to taking analgesia on an empty stomach. She was reassured and was advised to maintain good oral hygiene.
Subsequently, the patient then noted new-onset dizziness and worsening nausea, exacerbated with movement and imbalance. She denied any previous history of otological symptoms and treatment nor any recent history of trauma. She was brought in to the emergency department and admitted for 24 hours, where she was monitored and administered prochlorperazine. Her balance improved and she was discharged with an oral course of antiemetics, which she discontinued due to spontaneous improvement.
Our literature review revealed only four publications which have reported vertigo after isolated dental extractions. 1 , 2 , 3 , 4 Few other reports have noted post-operative vertigo in patients who have had maxillary surgery and dental implant placements. 5 , 6 Some of the factors considered by these authors to be causative include prolonged surgical time, use of rotary tools, application of osteotomes/surgical mallets and presence of comorbidities. In the case described, a surgical drill was used to remove bone. Prolonged mouth opening during dental procedures is a well-known risk factor for temporomandibular disorders which can present with otological symptoms. Finally, we haven't ruled out the possibility of coincidence in presentation of these symptoms, although this does not explain or help the patient's debilitation. We found this case interesting and worth discussing to understand the pathophysiology of this odd relationship.
D'Ascanio L, Salvinelli F, Martinelli M. Benign paroxysmal positional vertigo: an unusual complication of molar teeth extraction. Br J Oral Maxillofac Surg 2007; 45: 176-177.
Yilmaz H B, Erdogan R B, Paksoy M, Sanli A. Sudden hearing loss and vertigo after tooth extraction successfully treated with combined therapy including HBO2: a case report. Undersea Hyperb Med 2015; 42: 603-606.
Chiarella G, Leopardi G, De Fazio L, Chiarella R, Cassandro E. Benign paroxysmal positional vertigo after dental surgery. Eur Arch Otorhinolaryngol 2008; 265: 119-122.
Petrocelli M, Sbordone C, Salzano G et al. Benign paroxysmal positional vertigo after oral and maxillofacial surgery: our experience and review of literature. J Maxillofac Oral Surg 2020; 19: 527-531.
Perez Garrigues H, Mateos Fernandez M, Penarrocha M. Benign paroxysmal positional vertigo secondary to surgical maneuvers on superior maxilla. Acta Otorhinolaryngol Esp 2001; 52: 343-346.
Kaplan D M, Attal U, Kraus M. Bilateral benign paroxysmal positional vertigo following a tooth implantation. J Laryngol Otol 2003; 117: 312-313.
Download references
Author information
Authors and affiliations.
By email, London, UK
R. O´Rorke, N. Khan, H. Makar & S. Mumtaz
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
About this article
Cite this article.
O´Rorke, R., Khan, N., Makar, H. et al. Vertigo after tooth removal. Br Dent J 231 , 148 (2021). https://doi.org/10.1038/s41415-021-3343-y
Download citation
Published : 13 August 2021
Issue Date : August 2021
DOI : https://doi.org/10.1038/s41415-021-3343-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Live CE Event – June 1, 2024
- Self-Study CE Courses
- Live Event CE Certificates
- Dental Quizzes
- Dental Hygiene
- Dental Research
- Patient Care
- Life at Work
- Infection Control
- Students & New Grads
- Ask Kara RDH
- Curiosity Killed the Plaque
- Videos & Hygiene Chats
- Hygiene Chats: Kara & Emily
- Hygienist Spotlight
- Today’s RDH Honor Awards
- Submissions
- June 1st Live CE Event

Spinning Rooms: Dental Practice Considerations Can Help Patients with Vertigo

Vertigo is an umbrella term for a person who has a sensation of motion when they are not moving, and inner ear problems often cause it. Vertigo can also be caused by migraines and some medications, including those to treat high blood pressure, anxiety, or infections.
Dental providers who stay alert about patients’ health histories can help our clients with vertigo. Some steps dental practice personnel can consider for patients with vertigo are listed below.
A reduction in balance from inner ear function may be caused by normal aging, infection, or diminished blood flow to specialized nerve cells in the inner ear. Labyrinthitis is an infection or inflammation of the inner ear that causes severe vertigo lasting one to two days. Labyrinthitis can induce hearing loss. Neuronitis causes episodes of vertigo in a similar manner, but it does not affect hearing.
Both conditions could be triggered by an upper respiratory infection, virus or flu, or can have no obvious cause. Some medications, such as antibiotics and chemotherapy drugs, damage the inner ear, causing temporary or permanent hearing loss, impaired balance, and trouble seeing.
Benign Paroxysmal Positional Vertigo
Half of the people over the age of 65 will suffer an episode of benign paroxysmal positional vertigo (BPPV). According to the Cleveland and Mayo Clinic, women are most prone. 1 The experience may include lightheadedness, disrupted balance, nausea, and perhaps vomiting. It occurs when tiny calcium carbonate crystals that are normally in an inner-ear organ called the utricle break loose and travel into the inner ear’s canals.
Even a bump on the head can dislodge those crystals causing BPPV. Yet again, another reason to always wear a helmet. BPPV is positionally triggered. When you move your head a certain way, such as dropping it forward to pick something up off the floor or attempting a downward-facing dog, you can cause these crystals to move and bring on an attack. It may also be triggered when you’re lying down and happen to roll towards your bad ear to get out of bed in the morning, and, bam, you get hit.
The dizzy spells typically last for less than a minute but can return anytime you pitch your head, triggering another brief, brisk spin. It can be annoying and debilitating (even dangerously) to make people feel off-balance and put them at risk for falls. BPPV can go away on its own though it can last for months and even years.
A treatment called the Epley maneuver is typically performed by a vestibular rehabilitation therapist, occupational therapist, audiologist, or doctor. It involves moving the head in a certain series of precise positions that allow the crystals to migrate out of the semicircular canals back to the original vestibular organ they came from in the utricle.
If this is a treatment choice, make sure to be treated by a skilled practitioner. Some providers may use the wrong technique and treat the wrong ear or even the wrong canal. The Epley maneuver is designed for the posterior canal. There is also a possibility that the crystals are stuck; it’s not common, but it may happen.
Ménière’s Disease
BPPV and Ménière’s disease (endolymphatic hydrops) have similar symptoms. However, BPPV is usually triggered by specific head movements, while the attacks in Ménière’s can occur without warning and is characterized by vertigo, spinning sensation, headaches, loss of balance, hearing problems, and a ringing sound. Ménière’s comes from abnormal fluctuations in the fluid called endolymph which fills the hearing and balance structures of the inner ear. Usually, this involves only one ear.
Prosper Ménière, a French physician, hypothesized in 1861 that the symptoms of vertigo were not from the brain but instead the inner ear. Although Ménière’s is a relatively rare disorder, it can be debilitating for those who have it.
The potential triggers may include a head injury, ear infections, allergies, stress, smoking, alcohol, and certain medications. The exact cause is not known. Some people with Ménière’s find that certain events and situations such as smells, foods, and even lighting can be a trigger and set off an attack. Oncoming attacks are often preceded by an “aura” or a specific set of warning symptoms. They can be balance disturbance, dizziness, lightheadedness, headache, increased ear pressure, hearing loss or tinnitus, increased sound sensitivity, and a vague feeling of uneasiness.
As health care providers, it is important that we pay attention to our patients who battle with Ménière’s and look for the early onset of the attacks. These attacks can last 20 minutes to 24 hours.
Patients with Ménière’s are often encouraged to adopt lifestyle changes such as quitting smoking, as well as limiting or excluding salt, MSG, caffeine, and alcohol from diets. Ménière’s is treated with medications that are used for motion sickness, antiemetics, and/or diuretics. An injected drug, gentamicin, is deemed safe by many for a treatment protocol. 2
Dental Practice Considerations
A study by Tzu-Pu Chang et al. found a correlation between dental procedures and BPPV. 3 The study concluded that dentists should recognize BPPV as a possible complication of dental treatment. The odds ratio was different depending upon the procedures. Periodontics was highest, followed by oral surgery, endodontics, prosthodontics, and finally dental scaling. Looking at all the available evidence, it’s hard to conclude that dental work is a direct cause of BPPV. In that Taiwan study, it’s still not clear if the patients already had BPPV, and dental work merely induced the first onset of symptoms.
During dental treatment, patients need to turn their heads to the left or to the right for providers to access different parts of the mouth. Could that bring on BPPV symptoms? Is it perhaps the length of time a patient is lying back in the chair? Could it be related to the micro-vibrations that they experience with the dental handpiece or ultrasonic scaler, and those micro-vibrations cause calcifications already deposited in the vestibular canals to circulate?
While it is difficult to conclude that the dental work directly causes BPPV, the correlation between the two cannot be ignored, and we need to be alert to the possibilities. An investigation into the relationship between dental and maxillofacial surgery and BPPV was reported following surgical trauma from different surgical interventions. 4 The indirect trauma by using either rotating tools or hammer and scalpel on the maxilla as well as on bone structures on the posterior labyrinth seems to be the origination of BPPV. Even mild trauma during surgery caused by vibrations can cause damage. They concluded that dental surgery is a risk factor for BPPV.
The first action providers should be paying attention to is the health history and be hopeful that patients notify us of their history of vertigo. An addition to our standard medical histories may need to include vertigo.
Should we consider doing shorter visits? Do we modify how we treat such as changing chair position? We all know how difficult it is when a patient doesn’t want to lean all the way back, but we do have to be cognizant of their health challenges and their comfort. Provide a neck pillow, check the noise level, and reduce lighting by offering dark safety glasses.
If a patient has a history of vertigo, we should pay attention to prevent them from excessively bending the back of their neck or shoulders to perform treatment. The Vestibular Disorders Association (VeDA) published a dentist’s guide for the dizzy patient, and the following list is from the association’s website: 5
- Schedule dizziness patients at their best time of day.
- Symptoms can come on suddenly, resulting in possible last-minute scheduling changes.
- Offer an arm for the patient to hold while walking, as hallways and busy pattern flooring exacerbate disequilibrium.
- Accommodate a friend or family member who may accompany the patient.
- Communicate while sitting knee-to-knee and in front of the patient as much as possible. Politeness eases tension, and the closeness will aid those with hearing loss and/or tinnitus.
- Speak slowly while keeping your head and arms still. Be patient as these patients tend to behave anxiously due to their physical symptoms.
- Do not move the dental chair without discussing it with the patient first. Some patients will want to sit forward while the chair reclines.
- Ask the patient for positioning feedback and always keep their head above their feet.
- Empower the patient by allowing them to take breaks, if needed, by raising their hand.
- During the procedure, inform the patient when to anticipate vibration and check on their wellbeing.
- Conversation should pertain to the patient. Do not engage in side-talk, which can be distracting and cause anxiety, unless the patient initiates it to relieve tension.
- Move your operator chair and change your position to accommodate patients who cannot lie supine and/or turn their heads.
Our baby boomers are aging, and the propensity for BPPV will be growing. The population of our practices that may have any cause of vertigo is an area that we should all be well versed in. Compassion for this subgroup of patients from the front staff to the back staff would be welcomed. As Aesop noted, “No act of kindness, no matter how small, is ever wasted.”
Now Check Out the Peer-Reviewed, Self-Study CE Courses from Today’s RDH!
Listen to the today’s rdh dental hygiene podcast below:.
- Benign Paroxysmal Positional Vertigo (BPPV). (2020, August 18). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/vertigo/symptoms-causes/syc-20370055
- Scarpa, A., Ralli, M., Cassandro, C., et al. Low-dose Intratympanic Gentamicin Administration for Unilateral Meniere’s Disease Using a Method Based on Clinical Symptomatology: Preliminary Results. Am J Otolaryngol . 2019; 40(6): 102289. doi:10.1016/j.amjoto.2019.102289. https://pubmed.ncbi.nlm.nih.gov/31537428/
- Chang, T.P., Lin, Y.W., Sung, P.Y., et al. Benign Paroxysmal Positional Vertigo after Dental Procedures: A Population-Based Case-control Study. PLoS One. 04 April 2016; 11(4): e0153092. doi:10.1371/journal.pone.0153092. https://europepmc.org/article/PMC/4820237
- Chiarella, G., Leopardi, G., De Fazio, L., et al. Benign Paroxysmal Positional Vertigo after Dental Surgery. Eur Arch Otorhinolaryngol. 2008; 265(1): 119-122. doi:10.1007/s00405-007-0397-7. https://pubmed.ncbi.nlm.nih.gov/17647006/
- Hughes, T. (2022). Dentist’s Guide to The Dizzy Patient. Vestibular Disorder Association. https://vestibular.org/article/coping-support/living-with-a-vestibular-disorder/dentists-guide-to-the-dizzy-patient/
RELATED ARTICLES MORE FROM AUTHOR

Kiss and Tell: Variations of Normal and Pathology of the Lips

How Hygienists Can Be the First Line of Defense Against Oral Cancer
Oral Cancer: Why the Biopsy is Still the Most Important Treatment to Recommend
Trending now.

Caviar Tongue: Are Dental Hygiene Patients Displaying Signs of “Aging?”
4 Simple Tips for Newly Graduated Dental Hygienists

Dental Radiology: New Recommendations for Patient Lead Shielding
- Dental Hygiene 592
- Patient Care 319
- Dental Research 262
- Hygiene Chats & Videos 138
- Life at Work 121
- Healthy Smiles, Healthy Practices 86
- Students & New Grads 56
- COVID-19 53
- Hygienist Spotlight 48
Most Recent

A Hygienist’s Guide to Succeeding at Dental Conferences

Does Referring to Appointments as a “Cleaning” Undervalue Dental Hygienists and...

Researchers Find the Mechanism Behind Potential Anticancer Properties in Lidocaine
Don't miss.

D4346: The Who, What, When, Where, and Why of Gingivitis Treatment

Debunking the Dental Hygiene Diagnosis

How the Pandemic Strengthens the Case for Teledentistry and Dental Hygienists

6 Surefire Ways to Get a Raise… But Only if You...
Headache After the Dentist? Here's What Your Body's Trying to Tell You

Nagging dental problems can be a headache. But sometimes, a trip to your dentist can make your head throb, too.
Advertisement
While hard stats on dentist-induced headaches are hard to come by, "getting a headache after dental work or a dental cleaning is not uncommon," says Alla Al-Habib, MD , a neurologist with Texas Health Presbyterian Hospital Plano.
Video of the Day
While this head pain can be annoying, it likely isn't anything serious.
Here are some of the most common reasons why you get a headache after dental work and what you can do to feel better.
If you consistently get headaches or migraines after dental work, let your dentist know the next time you see them. They can make adjustments to your treatment or offer advice on how to avoid this issue.
1. Dental Visits Make You Anxious
Many people have anxiety about going to the dentist . In fact, about 36 percent of people in the U.S. have a fear of dental treatment, per the Cleveland Clinic .
This anxiety alone can leave your head throbbing in pain. "Stress and anxiety associated with dental visits can cause tension headaches," Dr. Al-Habib says.
Poor sleep could come into play, too. If anxiety keeps you awake the night before your dentist appointment, that could lead to a tension headache later in the day, according to the National Institute of Neurological Disorders and Stroke .
Anxiety and lack of sleep can also trigger migraines for some people, per the NIH.
First, give yourself a pat on the back for keeping up with your oral health despite your fears.
To help make your next appointment more comfortable, share your fears with your dentist. They may be able to adjust your treatment or the speed that they work.
You can also bring headphones and listen to music in the dental chair, which has been proven to soothe nerves, per a January 2022 study in Acta Biomedica .
2. You Were Clenching Your Teeth
If you're feeling stressed or anxious during your visit, you may clench your teeth , sometimes without realizing it, per the Mayo Clinic .
You may do it while in the waiting room, before the hygienist does your cleaning or once your cleaning or procedure is over.
This can "strain your jaw muscles, resulting in a headache," Dr. Al-Habib says.
Again, talk to your dentist or hygienist about your nerves to see if they can make any adjustments to your treatment.
You can also try other stress-relief techniques at your next appointment, like squeezing a stress ball or visualizing yourself in a happy place to take the edge off, per the American Dental Association .
3. Your Jaw Is Strained
When you're at the dentist, you often have to keep your mouth open wide for long periods of time.
But holding this position for a while can strain your jaw and cause the surrounding muscles to spasm, leading to a headache.
"The temporomandibular joint (TMJ) connects your jawbone to your skull, and excessive strain on this joint can cause tension headaches," Dr. Al-Habib says.
These headaches often feel like a tight band squeezing around your head, and you might also notice your jaw feels sore or fatigued.
Apply a warm compress to your achy jaw for 15 to 20 minutes. "This can help relax your muscles and reduce inflammation," to help ease tension headache pain, Dr. Al-Habib says.
Gently massaging the area with your fingertips can also help relieve tension by increasing circulation, she adds. Or, try some jaw exercises to loosen those muscles.
4. The Numbing Meds Gave You a Headache
In rare cases, the numbing medicine dentists use on your mouth before a filling, crown application or other procedure can cause a headache.
Around 2 percent of people get a headache after receiving an oral numbing medicine for dental work, according to a December 2021 review in the Journal of Dental Anesthesia and Pain Medicine .
These medicines often have ingredients like norepinephrine, which can cause a temporary spike in blood pressure that can cause a headache, Dr. Al-Habib says.
Headaches from oral numbing shots are usually short-lived and will go away on their own, Dr. Al-Habib says.
You can speed the process along by drinking plenty of water and resting in a dark, quiet room to minimize sensory stimulation, she adds.
When to See a Doctor About a Headache After Dental Work
You likely don't need to worry about a brief or mild headache after seeing the dentist.
In fact, for some people, even a rough cleaning (like to scrape tartar off your teeth ) can cause your gums to hurt , resulting in jaw and head pain.
But if your headache lasts a week after dental work (or even just 48 hours), is accompanied by pain, dizziness or vision changes or is interfering with daily activities, Dr. Al-Habib suggests you call your doctor. You may have another issue that needs to be treated.

6 Things Dentists Do Every Day to Protect Their Teeth

7 Things Dentists Wish You'd Stop Doing at Your Checkups

8 Reasons Your Teeth Hurt All of a Sudden
- Acta Biomedica: "The Effect of Music Therapy in Reducing Dental Anxiety and Lowering Physiological Stressors"
- Mayo Clinic: "Bruxism"
- American Dental Association: "Anxiety: 3 Ways to Stop Fearing the Dentist"
- Journal of Dental Anesthesia and Pain Medicine: "Adverse effects following dental local anesthesia: a literature review"
- Texas Neurology and Stroke Center: "Alla Al-Habib, MD"
- Cleveland Clinic: "Dentophobia"
- National Institute of Neurological Disorders and Stroke: "Headache"
Is this an emergency? If you are experiencing serious medical symptoms, please see the National Library of Medicine’s list of signs you need emergency medical attention or call 911.
Report an Issue
Screenshot loading...
Bridge Creek Dental
Why Do I Feel Sick After Dental Cleaning?
February 24, 2022 By Bridge Creek Dental Leave a Comment

Although a trip to the dentist is harmless, there are often plenty of other activities on your to-do list that you prefer to do. In most cases, you’ll be in and out of your annual cleaning appointment in no time, ready to take on the rest of the day.
But sometimes, you may find yourself experiencing flu-like symptoms after dental work, especially if you have a weak immune system.
A patient may feel sick after a dental cleaning or dental work if the dentist uncovered or treated an infection in the mouth. As a result, the individual may experience bleeding, swelling, discomfort, or fever, all of which can be reminiscent of the flu. If you feel sick following a dental appointment, reach out to your dentist.
Not sure if the symptoms you’re experiencing are a cold or a result of a dental cleaning?
Bridge Creek Dental is here to walk you through the flu-like symptoms you may experience post-procedure.
Flu-like symptoms after a dental appointment
If you think you picked up a cold at your dentist’s office, think again. You may be experiencing flu-like symptoms as your body’s reaction to a dental cleaning or procedure. This often occurs due to the patient having a weakened immune system or underlying health conditions.
If you’re not feeling well, be on the lookout for the following symptoms that may occur after dental work:
- Ear pain – Ear pain is no joke. Not only can it make it difficult to hear conversations or sounds around you, but it can leave you with a splitting headache. You may experience ear pain because of muscle strain, an infection, misaligned teeth, or an allergy to a medication or a dental instrument.
- Pressure – There are few things more annoying than the feeling of pressure or buildup in your head, leaving you feeling groggy and under the weather. If your dentist treated an infected tooth, you might feel pressure or tooth sensitivity from the procedure. Over time, the pressure should subside, but if it lasts longer than a week, your dentist should be contacted.
- Sore throat – One of the first tell-tale warning signs of a cold is a sore throat. You may experience a scratchy or sore throat following dental work because your body is a bit dehydrated from your mouth staying open throughout the procedure. Make sure you drink plenty of fluids following your dental work to rehydrate your body and relieve the sore throat.
- Nausea – If your dental procedure requires anesthetics and medication, it won’t be uncommon for you to experience nausea or dizziness as the medication begins to wear off. Depending on how much medicine you were given, you can expect nausea or dizziness to lessen over the next few days. If the feeling persists longer than a week, reach out to your dentist.
- Jaw pain – A sore jaw is a common cold symptom that can make it uncomfortable to chew. You may experience jaw pain following a dental appointment due to keeping your mouth open for an extended period. As a result, the muscles in your jaw stiffen and feel sore for a few days after. Using a warm compress can help reduce the discomfort.
If you have noticed flu-like symptoms following your appointment, there’s no need to stress out. Should the symptoms persist longer than a week, your dentist will be able to determine a plan of action to reduce the symptoms. You can also reduce the chances of feeling sick post-appointment by strengthening your immune system before any upcoming dental appointments.
Call Bridge Creek Dental for preventative dental care
Keeping your teeth healthy can help you avoid unwanted dental work. Scheduling a preventative dental care visit is the most effective way to catch minor oral health issues before they turn into larger problems down the line.
During the dental cleaning, the team at Bridge Creek Dental will treat any troublesome areas to help prevent major health concerns such as gum disease and tooth loss. Instead of letting any oral hygiene issues fester, our top-rated preventative dental care helps you maintain a beautiful, clean smile.
Here at Bridge Creek Dental, we specialize in providing preventive dental care for your entire family. If you or your loved ones are experiencing dental issues, give our team a call to schedule an appointment in Billings, MT.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

Insurance We Accept

Financing Options

- Dr. Kyle B. Wassmer, DDS
- Dr. Jacob M. Taylor, DMD
- New Patients
- Patient Login
- Bridge Creek Rock
- Billings Christmas Light Map
- Tour Our Office
Opening Hours
Monday 8am to 5pm Tuesday 7am to 5pm Wednesday 7am to 5pm Thursday 7am to 5pm Friday 7am to 3pm
- About Our Team
- Dr Oliver Swensen
- Dr. Michael J. McCarthy, DDS (Retired)
- Dr. Gayle A. Roset, DDS (Retired)
- Cosmetic Dentistry
- Emergency Dentistry
- Root Canals
- Sedation Dentistry
- Teeth Whitening
- Dental Hygiene
- Crowns Gallery
- Veneers Gallery
- Filllings Gallery
- Bonding Gallery
- Dentures Gallery
- Root Canal Gallery
- Whitening Gallery
- Implant Gallery
- Periodontal Gallery

IMAGES
VIDEO
COMMENTS
Conclusion: Navigating vertigo after dental work requires a nuanced understanding of potential triggers and effective management strategies. By addressing common queries and concerns surrounding vertigo following dental procedures, individuals can proactively alleviate discomfort and enhance their dental care experience.
The other link that I have observed with vertigo and teeth is that vertigo can occur during or after a visit to the dentist. Vertigo that occurs when the head is reclined back in the dentist's chair could be from the neck circulation - or blood flow to the brain, or it could indicate BPPV. One way to tell the difference is to place a pillow ...
Offer a neck pillow and blanket. Avoid scents such candles, perfume, cologne, and air fresheners. Check with the patient about the noise level. Some patients with dizziness find background music disorienting. Do not wear print scrubs or patterned clothing, as busy visual environments cause discomfort for people with vestibular disorders. 5.
In contrast, only 5.5% of the controls had undergone dental treatment within 1 month before the date at which they were identified (P = 0.001). After adjustments for demographic factors and comorbidities, recent exposure to dental procedures was positively associated with BPPV (adjusted odds ratio 1.77; 95% confidence interval 1.27-2.47).
This viral attack triggered by dental work can cause cold sores to show up on your lips. The oral herpes virus may even travel down your vestibular nerve to attack your inner ear. That causes the second most common inner ear cause of vertigo, vestibular neuritis. In this case, vestibular neuritis is caused by a virus.
The signs and symptoms of benign paroxysmal positional vertigo (BPPV) may include: Dizziness. A sense that you or your surroundings are spinning or moving (vertigo) A loss of balance or unsteadiness. Nausea. Vomiting. The signs and symptoms of BPPV can come and go and commonly last less than one minute. Episodes of BPPV can disappear for some ...
General categories of disorders where dizziness might be associated with or provoked by dentistry include: Positional vertigo -- vertigo triggered by changing of head movement with respect to gravity. BPPV is by far the most common cause. Cardiac conditions -- arrhythmia associated with the adrenalin often accompanying dental work.
You can receive effective treatment for benign paroxysmal positional vertigo during a doctor's office visit." ... PLoS One. 2016 Apr 4;11(4):e0153092. doi: 10.1371/journal.pone.0153092. Benign Paroxysmal Positional Vertigo after Dental Procedures: A Population-Based Case-Control Study. Chang TP1,2, Lin YW3, Sung PY4, Chuang HY5, Chung HY6 ...
Dental visits are especially challenging for patients with dizziness and vertigo because dental chair positioning, equipment, and instruments can worsen their condition. Fortunately, dental office personnel can minimize patient symptoms and agitation by implementing the following protocols: COPING 5018 NE 15th Ave. Portland, OR 97211 1-800-837-8428
People with BPPV can experience a spinning sensation — vertigo — any time there is a change in the position of the head. The symptoms can be very distressing. People can fall out of bed or lose their balance when they get up from bed and try to walk. If they tilt their head back or forward while walking, they may even fall, risking injury.
Abstract. Background: Benign paroxysmal positional vertigo (BPPV), the most common type of vertigo in the general population, is thought to be caused by dislodgement of otoliths from otolithic organs into the semicircular canals. In most cases, however, the cause behind the otolith dislodgement is unknown. Dental procedures, one of the most ...
The vertigo is associated with neurovegetative symptoms such as nausea, vomiting, tachycardia and anxiety, without any cochlear symptoms such as hearing loss, tinnitus or ear fullness . The etiology of benign paroxysmal positional vertigo (BPPV) is unknown; 15-20% of cases have been associated with minor and major head trauma; few cases were ...
There are several different types of vertigo, but the one appearing to be most associated with dental work is benign paroxysmal positional vertigo (BPPV). It is the most common type of vertigo observed in the general population. Most causes of BPPV are unknown, but some inner ear disorders and trauma to the head have been known to cause it.
Background Benign paroxysmal positional vertigo (BPPV), the most common type of vertigo in the general population, is thought to be caused by dislodgement of otoliths from otolithic organs into the semicircular canals. In most cases, however, the cause behind the otolith dislodgement is unknown. Dental procedures, one of the most common medical treatments, are considered to be a possible cause ...
Dizziness is a generalized phenomenon resulting from medication, motion, disease, or balance issues. Vertigo is the sensory sensation of oneself or one's surroundings being in motion. 1 Vertigo is often triggered by a change in head position with patients complaining of: Spinning/tilting. Swaying.
The longer procedures are typically when symptoms of dizziness will occur. Other symptoms can be jaw pain, neck pain, imbalance and vertigo. 3 main causes. There are many reasons why you are dizzy after seeing the dentist. They are outlined below: Prolonged mouth opening. Having your mouth opened for a long period of time can aggravate ...
When cavities are left untreated, they can cause nerve damage that may disrupt the signals sent from the jaw to the brain, resulting in dizziness. 3. Dental Health and Balance: Exploring the Role of Vestibular System. The vestibular system plays a crucial role in maintaining both dental health and overall balance.
Ask for a pillow or neck support. There are a few reasons why people feel dizzy at the dentist. Many of those reasons have to do with reclining back in the chair. You can ask the dentist for a pillow or neck support. Then you will not be leaning so far back. You can also bring your own neck support or small pillow if you have one that works well.
For some, this feeling can be immediate, and for others it can continue for the remainder of the day. Dizziness can be caused by your reaction to the local anesthesia, sudden changes to your blood pressure and lying back in the dental chair for prolonged periods of time. If you are feeling dizzy, get rest, move slowly and take plenty of fluids.
Vertigo after tooth removal. British Dental Journal 231 , 148 ( 2021) Cite this article. Sir, a 26-year-old white woman presented with bilateral recurrent pericoronitis in relation to ...
March 9, 2022. Vertigo is an umbrella term for a person who has a sensation of motion when they are not moving, and inner ear problems often cause it. Vertigo can also be caused by migraines and some medications, including those to treat high blood pressure, anxiety, or infections. Dental providers who stay alert about patients' health ...
Apply a warm compress to your achy jaw for 15 to 20 minutes. "This can help relax your muscles and reduce inflammation," to help ease tension headache pain, Dr. Al-Habib says. Gently massaging the area with your fingertips can also help relieve tension by increasing circulation, she adds.
But sometimes, you may find yourself experiencing flu-like symptoms after dental work, especially if you have a weak immune system. A patient may feel sick after a dental cleaning or dental work if the dentist uncovered or treated an infection in the mouth. As a result, the individual may experience bleeding, swelling, discomfort, or fever, all ...