- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

Guidelines for Flying With Heart Disease
Air travel is generally safe for heart patients, with appropriate precautions
- Pre-Flight Evaluation
Planning and Prevention
During your flight.
If you have heart disease, you can fly safely as a passenger on an airplane, but you need to be aware of your risks and take necessary precautions.
Heart conditions that can lead to health emergencies when flying include coronary artery disease (CAD) , cardiac arrhythmia (irregular heart rate), recent heart surgery, an implanted heart device, heart failure , and pulmonary arterial disease.
When planning air travel, anxiety about the prevention and treatment of a heart attack on a plane or worrying about questions such as "can flying cause heart attacks" may give you the jitters. You can shrink your concern about things like fear of having a heart attack after flying by planning ahead.
Air travel does not pose major risks to most people with heart disease. But there are some aspects of flying that can be problematic when you have certain heart conditions.
When you have heart disease, air flight can lead to problems due to the confined space, low oxygen concentration, dehydration, air pressure, high altitude, and the potential for increased stress. Keep in mind some of these issues compound each other's effects on your health.
Confined Space
The prolonged lack of physical movement and dehydration on an airplane may increase your risk of blood clots, including deep vein thrombosis (DVT) or pulmonary embolism (PE) . One of the biggest risks for people with heart disease who are flying is developing venous thrombosis.
These risks are higher if you have CAD or an implanted heart device, such as an artificial heart valve or a coronary stent. And if you have an arrhythmia, a blood clot in your heart can lead to a stroke.
One of the biggest risks for people with heart disease who are flying is developing an arterial blood clot or venous thrombosis.
Low Oxygen and Air Pressure
The partial pressure of oxygen is slightly lower at high altitudes than at ground level. And, while this discrepancy on an airplane is typically inconsequential, the reduced oxygen pressure in airplane cabins can lead to less-than-optimal oxygen concentration in your body if you have heart disease.
This exacerbates the effects of pre-existing heart diseases such as CAD and pulmonary hypertension .
The changes in gas pressure in an airplane cabin can translate to changes in gas volume in the body. For some people, airplane cabin pressure causes air expansion in the lungs. This can lead to serious lung or heart damage if you are recovering from recent heart surgery.
Dehydration
Dehydration due to cabin pressure at high altitude can affect your blood pressure, causing exacerbation of heart disease. This is especially problematic if you have heart failure, CAD, or an arrhythmia.
If you experience stress due to generalized anxiety about traveling or sudden turbulence on your flight, you could have an exacerbation of your hypertension or CAD.
Pre-Flight Health Evaluation
Before you fly, talk to your healthcare provider about whether you need any pre-flight tests or medication adjustments. If your heart disease is stable and well-controlled, it is considered safe for you to travel on an airplane.
But, if you're very concerned about your health due to recent symptoms, it might be better for you to confirm that it's safe with your healthcare provider first before you book a ticket that you may have to cancel.
Indications that your heart condition is unstable include:
- Heart surgery within three months
- Chest pain or a heart attack within three months
- A stroke within six months
- Uncontrolled hypertension
- Very low blood pressure
- An irregular heart rhythm that isn't controlled
If you've had a recent heart attack, a cardiologist may suggest a stress test prior to flying.
Your healthcare provider might also check your oxygen blood saturation. Heart disease with lower than 91% O2 saturation may be associated with an increased risk of flying.
Unstable heart disease is associated with a higher risk of adverse events due to flying, and you may need to avoid flying, at least temporarily, until your condition is well controlled.
People with pacemakers or implantable defibrillators can fly safely.
As you plan your flight, you need to make sure that you do so with your heart condition in mind so you can pre-emptively minimize problems.
While it's safe for you to fly with a pacemaker or defibrillator, security equipment might interfere with your device function. Ask your healthcare provider or check with the manufacturer to see if it's safe for you to go through security.
If you need to carry any liquid medications or supplemental oxygen through security, ask your healthcare provider or pharmacist for a document explaining that you need to carry it on the plane with you.
Carry a copy of your medication list, allergies, your healthcare providers' contact information, and family members' contact information in case you have a health emergency.
To avoid unnecessary anxiety, get to the airport in plenty of time to avoid stressful rushing.
As you plan your time in-flight, be sure to take the following steps:
- Request an aisle seat if you tend to need to make frequent trips to the bathroom (a common effect of congestive heart failure ) and so you can get up and walk around periodically.
- Make sure you pack all your prescriptions within reach so you won't miss any of your scheduled doses, even if there's a delay in your flight or connections.
- Consider wearing compression socks, especially on a long trip, to help prevent blood clots in your legs.
If you have been cleared by your healthcare provider to fly, rest assured that you are at very low risk of developing a problem. You can relax and do whatever you like to do on flights—snack, read, rest, or enjoy entertainment or games.
Stay hydrated and avoid excessive alcohol and caffeine, which are both dehydrating. And, if possible, get up and walk for a few minutes every two hours on a long flight, or do leg exercises, such as pumping your calves up and down, to prevent DVT.
If you develop any concerning issues while flying, let your flight attendant know right away.
People with heart disease are at higher risk for developing severe complications from COVID-19, so it's especially important for those with heart disease to wear a mask and practice social distancing while traveling.
Warning Signs
Complications can manifest with a variety of symptoms. Many of these might not turn out to be dangerous, but getting prompt medical attention can prevent serious consequences.
Symptoms to watch for:
- Lightheadedness
- Dyspnea (shortness of breath)
- Angina (chest pain)
- Palpitations (rapid heart rate)
- Tachypnea (rapid breathing)
To prepare for health emergencies, the U.S. Federal Aviation Administration mandates that supplemental oxygen and an automated external defibrillator (AED) is on board for passenger airplanes that carry 30 passengers or more. Flight crews receive training in the management of in-flight medical emergencies and there are protocols in place for flight diversions if necessary.
A Word From Verywell
For most people who have heart disease , it is possible to fly safely as long as precautions are taken. Only 8% percent of medical emergencies in the air are cardiac events, but cardiac events are the most common in-flight medical cause of death.
This means that you don't need to avoid air travel if you have stable heart disease, but you do need to take precautions and be aware of warning signs so you can get prompt attention if you start to develop any trouble.
Hammadah M, Kindya BR, Allard‐Ratick MP, et al. Navigating air travel and cardiovascular concerns: Is the sky the limit? Clinical Cardiology . 2017;40(9):660-666. doi:10.1002/clc.22741.
Greenleaf JE, Rehrer NJ, Mohler SR, Quach DT, Evans DG. Airline chair-rest deconditioning: induction of immobilisation thromboemboli? . Sports Med. 2004;34(11):705-25.doi:10.2165/00007256-200434110-00002
American Heart Association. Travel and heart disease .
Ruskin KJ, Hernandez KA, Barash PG. Management of in-flight medical emergencies . Anesthesiology. 2008;108(4):749-55.doi:10.1097/ALN.0b013e31816725bc
Naqvi N, Doughty VL, Starling L, et al. Hypoxic challenge testing (fitness to fly) in children with complex congenital heart disease . Heart. 2018;104(16):1333-1338.doi:10.1136/heartjnl-2017-312753
By Richard N. Fogoros, MD Richard N. Fogoros, MD, is a retired professor of medicine and board-certified in internal medicine, clinical cardiology, and clinical electrophysiology.

NICOLE POWELL-DUNFORD, MD, MPH, JOSEPH R. ADAMS, DO, MPH, AND CHRISTOPHER GRACE, DO, MPH
Am Fam Physician. 2021;104(4):403-410
Related Letter to the Editor: Helping Adults With Dementia Travel by Air
Author disclosure: No relevant financial affiliations.
Air travel is generally safe, but the flight environment poses unique physiologic challenges such as relative hypoxia that may trigger adverse myocardial or pulmonary outcomes. To optimize health outcomes, communication must take place between the traveler, family physician, and airline carrier when there is any doubt about fitness for air travel. Travelers should carry current medications in their original containers and a list of their medical conditions and allergies; they should adjust timing of medications as needed based on time zone changes. The Hypoxia Altitude Simulation Test can be used to determine specific in-flight oxygen requirements for patients who have pulmonary complications or for those for whom safe air travel remains in doubt. Patients with pulmonary conditions who are unable to walk 50 m or for those whose usual oxygen requirements exceed 4 L per minute should be advised not to fly. Trapped gases that expand at high altitude can cause problems for travelers with recent surgery; casting; ear, nose, and throat issues; or dental issues. Insulin requirements may change based on duration and direction of travel. Travelers can minimize risk for deep venous thrombosis by adequately hydrating, avoiding alcohol, walking for 10 to 15 minutes every two hours of travel time, and performing seated isometric exercises. Wearing compression stockings can prevent asymptomatic deep venous thrombosis and superficial venous thrombosis for flights five hours or longer in duration. Physicians and travelers can review relevant pretravel health information, including required and recommended immunizations, health concerns, and other travel resources appropriate for any destination worldwide on the Centers for Disease Control and Prevention travel website.
Air travel has become increasingly popular over time, despite decreases during the COVID-19 pandemic, with 1.1 billion total passengers in 2019 and most Americans having flown at least once in the past three years. 1 Air travel is generally safe, but especially for the aging U.S. population, the flight environment poses unique physiologic challenges, particularly relative hypoxia, which may trigger adverse myocardial or pulmonary outcomes. To optimize health outcomes, communication must take place between the traveler, family physician, and airline carrier when any doubt occurs about fitness for air travel. Travelers should carry current medications in their original containers as well as a list of their medical conditions and allergies and should adjust timing of medications as needed based on time zone changes. Travelers should also consider available medical resources at their travel destinations and layover locations. Family physicians and travelers can review relevant pretravel health information, including required and recommended immunizations, health concerns, and other travel resources appropriate for any destination worldwide at https://wwwnc.cdc.gov/travel/destinations/list .
Pulmonary Conditions
By law, U.S. commercial aircraft cannot exceed a relative cabin altitude of 8,000 feet (2,438 m) because of the potential for significant hypoxia above this altitude. 2 Most passengers exposed to this environment will have a partial pressure of arterial oxygen (Pao 2 ) of 60 to 65 mm Hg (7.98 to 8.64 kPa), corresponding to 89% to 94% peripheral oxygen saturation (Spo 2 ), which may compromise cardiovascular or pulmonary disease in affected travelers. 3 Neither reassuring pulse oximetry nor reassuring forced expiratory volume in one second has been found to predict hypoxemia or in-flight events for patients with pulmonary conditions. 3
The nonstandardized Hypoxia Altitude Simulation Test, administered and interpreted by pulmonologists, can be used to determine specific in-flight oxygen requirements for patients with pulmonary complications or those for whom safe air travel remains in doubt. Typically, the Hypoxia Altitude Simulation Test comprises breathing 15% fraction of inspired oxygen for 20 minutes, with pulse oximeter and blood gas measurements taken before and after testing. 4 – 6 Patients with a Hypoxia Altitude Simulation Test Pao 2 less than 50 mm Hg (6.65 kPa) at any point during the test require supplemental oxygen in flight, whereas those with a Pao 2 greater than 55 mm Hg (7.32 kPa) do not. Pao 2 measurements falling between 50 and 55 mm Hg are considered borderline and may necessitate further testing with activity. 5 Given that the test itself incurs some risk and may not be available to all travelers, family physicians can counsel patients who are unable to walk 50 m (164 ft) or those whose usual oxygen requirements exceed 4 L per minute not to fly. 3 , 4 , 7 , 8
Patients with oxygen requirements less than 4 L per minute can be counseled to double their usual flow rate while flying. 8
Commercial airline carriers usually permit the use of personal Federal Aviation Administration–approved portable oxygen compressors, but carriers require travelers to give from 48 hours to one month's notice before flight when they are requesting the use of compressed oxygen. 9
Table 1 lists indications for which further assessment (e.g., Hypoxia Altitude Simulation Test, ability to walk 50 m) is warranted, including previous respiratory difficulties while flying, severe lung disease, recent or active lung infections, any preexisting oxygen requirements or ventilatory support, or if less than six weeks have passed since hospital discharge for acute respiratory illness. 3 Patients who have undergone an open-chest lung procedure should defer travel for two to three weeks, must not have any recent or residual pneumothorax, and should be assessed for supplemental oxygen needs. 10
Cardiac Conditions
Travelers with underlying cardiac conditions should use airport assistance services such as wheelchairs and baggage trolleys to decrease myocardial oxygen demand. 9 Although most cardiac conditions are safe for flight, some require additional consideration. Travelers with minimally symptomatic, stable heart failure may safely fly, but medication adherence is critical. 9 , 11 Patients with stable angina should be assessed for oxygen needs if they become short of breath after walking 50 m , and they should not fly following any recent medication changes that have not demonstrated clinical stability beyond that medication's half-life. 7 , 11
Patients with unstable angina, new cardiac or pulmonary symptoms, or recent changes in medication without appropriate follow-up should not fly until stable, particularly for medication changes that could impact blood pressure or coronary reserve. 11 Travelers with recent myocardial infarction at low risk should defer air travel for three to 10 days postevent 11 – 15 ( Table 2 11 ) . Low-risk patients who required percutaneous transluminal coronary angioplasty may fly after three days as long as they are asymptomatic. 9 Travelers who have had coronary artery bypass grafting or an uncomplicated open-chest procedure should wait to fly until they are 10 days postprocedure. 7 , 11
Many implantable-cardioverter defibrillators are compatible with standard airport security. 9 The Transportation Security Administration recommends that travelers with pacemakers, defibrillators, or any other implanted metal device request pat-down screening instead of using a walk-through metal detector. 16 For travelers with pacemakers and implantable-cardioverter defibrillators, a two-day flight restriction following uncomplicated placement is appropriate. 11 It is prudent for all cardiac patients to travel with a copy of their most recent electrocardiography results and a preflight graded exercise test, which may aid in assessment and management in case of an event during flight. 9 In patients with hypertension, medication compliance is especially important because aircraft noise and other travel-related stress may provoke blood pressure elevations. 17 Travel in patients with moderately controlled hypertension is not a contraindication, but airline travel for those with uncontrolled hypertension requires shared decision-making and clinical judgment.
Ear, Nose, and Throat Conditions
Trapped gases and sinus air-fluid levels can cause significant pain for the patient with ear, nose, and/or throat conditions. Adult patients with symptomatic rhinosinusitis or allergic rhinitis may benefit from oxymetazoline (Afrin) and/or pseudoephedrine to prevent ear blockage during descent. 18 No evidence suggests that antihistamines or decongestants are beneficial in children with sinusitis, 19 and these medications should not be used to hasten an early clearance for flight in any age group. Flight within 36 hours of otitis media resolution is generally safe. 20 Equalizing pressure on descent can also be accomplished in adults with frequent swallowing, chewing gum or food, or by generating pressure against a closed mouth and glottis. In young children and infants, upright bottle feeding or pacifier use can achieve similar effects. 21
Patients who have undergone jaw fracture repair should defer flying for at least one to two weeks, and jaw wiring should be temporarily replaced with elastic bands in case of emesis. 18 Transdermal scopolamine is effective in preventing air sickness , 22 and alternatives such as first-generation antihistamines may also be useful. Patients who elect to take scopolamine should be counseled on adverse effects of drowsiness, blurry vision, dry mouth, or dizziness. 22 Individuals who are prone to air sickness should refrain from alcohol use during flight and in preflight and should eat smaller, lighter meals. 18 The expansion of trapped gas at altitude may cause severe tooth pain in patients with caries beneath fixed restorations. Travelers with hearing aids should bring extra batteries and all accessories and may need to adjust their volume levels to offset background noise.
Diabetes Mellitus
In addition to carrying all medications, travelers with diabetes requiring insulin should request appropriate meals and consider checking blood glucose levels at intervals during longer flights. 23 Bringing snacks or other food can assist those with tenuous diabetes management in the event of layovers or delays. Insulin requirements may change based on the direction of travel and crossing time zones, which may entail lost or gained hours. Even if it is not part of the patient's normal regimen, fast-acting insulin, ideally with a pen device, should be considered for all travelers during flight due to its flexibility and responsiveness. 23 When traveling east, if the day is shortened by two or more hours, it may be necessary to give less insulin on the first day at the destination. When traveling west, if the day is extended by two or more hours, it may be necessary to give more insulin on the first day at the destination. Blood glucose should be checked at least 10 hours after the first-day dose to allow for further adjustments. Travelers can return to their normal insulin regimen on day 2 at their destination. A comprehensive public access resource for medical professionals addressing insulin adjustment for the air traveler is available through the Aerospace Medical Association. 23
Gastrointestinal Conditions
For travelers with recent intra-abdominal procedures, trapped gas expansion could disrupt sutures and cause rebleeding. Travelers should wait until 24 hours have passed and any bloating has resolved following laparoscopic abdominal procedures or colonoscopy. 7 , 10 Travelers should wait one to two weeks after open abdominal surgery. 10 Patients with active gastrointestinal problems, including hematemesis, melena, or obstruction, should not fly. 24
Hematologic Conditions
A baseline anemia may predispose travelers to syncope given the relative hypoxia of the flight environment. Caution should be exercised for travelers with a hemoglobin level below 8.5 g per dL (85 g per L), and some authorities recommend not advising flight for any travelers with levels below 7.5 g per dL (75 g per L). 7 Young, otherwise healthy patients with chronic anemia may be more tolerant of relative hypoxia, especially if their hemoglobin level is greater than 7.5 g per dL. 24 For the traveler with sickle cell anemia, sickling crisis during flight is unlikely 24 ; however, flight should be delayed for 10 days following an acute crisis, and patients with sickle cell anemia who have received a recent transfusion should not fly if hemoglobin levels are less than 7.5 g per dL. 24
Although deep venous thrombosis (DVT) is not caused by the flight environment itself, DVT is a concern for people who sit for extended periods or have risk factors. 25 Incidence of DVT reaches up to 5.4% in high-risk groups flying an average of 12.4 hours. 26 Compression stockings can prevent asymptomatic DVT and superficial venous thrombosis in flights lasting five hours or longer. 27 Table 3 lists recommendations for DVT prophylaxis for travelers who are at low, moderate, and high risk for DVT. 11 The baseline recommendations for each group include staying hydrated, avoiding alcohol to prevent dehydration, walking at least 10 to 15 minutes in each two hours of travel time, and performing isometric exercises while seated. 11 When indicated for high-risk travelers, including those with reduced mobility, low-molecular-weight heparin (e.g., 40 mg of subcutaneous enoxaparin [Lovenox]) on the day of and day after travel is appropriate for anticoagulation. 28
Psychiatric and Intellectual Disability Conditions
Passengers with mental or intellectual disabilities often benefit from a traveling companion because physiologic stresses of flight and the chaotic nature of busy airports may be especially challenging aspects of travel for these groups. 9 Prescription anxiolytics may alleviate travel anxiety, but a test dose is highly encouraged before flight. 9 Service or emotional support animals can be used for a variety of mental health conditions; an article in American Family Physician provides information about considerations for documentation for emotional support animals. 29 See the U.S. Department of Transportation website for current guidelines regarding the use of these animals during air travel. 30
Neurologic Conditions
Passengers predisposed to stress-related headaches and severe migraines should always carry abortive medications. Travelers with uncontrolled vertigo are not good candidates for flight. Patients prone to syncope should remain well-hydrated and be cautioned to avoid alcohol or quickly standing from a seated position. One small study suggests that people who have epilepsy with a history of flight-related seizures and a high baseline seizure frequency are likely to have a seizure after flying. 31 The Aerospace Medical Association recommends that patients with uncontrolled or poorly controlled seizures should not fly. 32 A safe amount of time permitted before flight following a seizure has not been established, but clinical judgment and the presence of a knowledgeable chaperone should factor into any medical recommendation. Although some airline carriers allow patients to fly 72 hours after a stroke, 7 the Aerospace Medical Association recommends waiting one to two weeks. 32
Obstetric Conditions
Background radiation associated with the flight environment does not pose a special hazard for most pregnant air travelers; however, the Federal Aviation Administration recommends informing aircrew or frequent flyers about health risks of radiation exposure. 33 Because a lack of in-flight medical resources may jeopardize safety of the mother and neonate, patients with an uncomplicated singleton pregnancy should generally not fly beyond 36 weeks of estimated gestational age 7 , 24 , 33 , 34 and those with a multiple gestation not beyond 32 weeks . 7 , 34 Body imaging scanners are safe for security screening during pregnancy. 34 , 35 Postpartum travelers are at moderate risk for DVT and should wear compression stockings and perform isometric exercises during flight. 11 Travelers who have undergone an uncomplicated cesarean delivery are generally safe for flight within one to two weeks. 10
Ophthalmologic Conditions
Passengers with severe visual impairment may benefit from having a traveling companion. Xerophthalmia may be exacerbated in the low humidity of the airplane cabin, and lubricating eye drops are advisable. Cataracts and clinically stable glaucoma are not contraindications to flight; however, any retinal detachment interventions should restrict flight for at least two weeks. 36 Open-globe eye surgery should delay air travel for up to six weeks, and travel recommendations should be made in conjunction with an ophthalmologist. 36
Orthopedic Conditions
Because of expansion of trapped air at altitude, all fixed casts should be bivalved. 7 , 37 Some airlines do not permit air casts of any kind, but if they are used, a small amount of air should be released to prevent any limb compression that occurs as a result of trapped gas expansion. Elastic bandages can be added to a bivalved cast and can be loosened as tolerated. The Transportation Security Administration recommends that passengers with prosthetic limbs should avoid metal detector screening and should be screened with alternative measures. 16 Individuals with significantly decreased mobility should consider wheelchairs and the use of travel companions. Passengers with low back pain and other mobility-limiting conditions can request seating near the front to reduce walking; however, business and first-class seating is an additional cost.
Urologic Conditions
Foley catheters and other inflatable balloons are compatible with flight; however, they should be filled with liquid for air travel, given the previously described expansion of trapped gas at altitude.
Special Considerations for Children
Healthy, term neonates should not fly for at least 48 hours after birth but preferably one to two weeks. 21 Infants younger than one year with a history of chronic respiratory problems since birth should be evaluated by a pulmonologist before air travel. 3
Other Air Travel Considerations
Jet lag occurs as a result of desynchronization between an individual's internal circadian rhythm and the external environment's time zone. 38 , 39 Jet lag is worse for eastward rather than westward travel. 40 Measures for prevention include ensuring enough sleep before travel, timing light exposure using sunglasses, avoiding alcohol, and eating at appropriate times after arriving at the destination. Timed melatonin is highly effective at treating jet lag, 41 and prescription hypnotic-sedative medications may also work in controlling sleep loss. 38
Self-contained underwater breathing apparatus (SCUBA) divers should not fly within 12 hours of a dive because of the concern for decompression sickness or life-threatening arterial gas embolism. 42
The airplane cabin does not inherently pose greater risk for infection than any other close contact, but respiratory viral pathogens are the most commonly transmitted infections. 43 Because of the ongoing COVID-19 pandemic, the Centers for Disease Control and Prevention (CDC) recommends delaying travel until the individual is fully vaccinated because traveling increases the chance of getting and spreading COVID-19. For patients not fully vaccinated who must travel, it is important to follow the CDC's recommendations for unvaccinated people. Check for evolving guidelines on the CDC's website. 44
Patients with breast cancer who have had surgery may fly without risking new or worsening lymphadenopathy. 45
A comprehensive discussion of in-flight emergencies is beyond the scope of this article. See the American Family Physician article on in-flight emergencies for more details. 46
This article updates a previous article on this topic by Bettes and McKenas . 37
Data Sources: A PubMed, Cochrane database, Essential Evidence Plus, ACCESSSS, and ECRI search occurred in April and May 2020 and April and May 2021 using search terms aviation medicine, travel medicine, commercial flight, air travel, and fitness to fly. The Aerospace Medical Association's website resource, Medical Considerations for Airline Travel, was searched in its entirety. The Handbook of Aviation and Space Medicine, Fundamentals of Aerospace Medicine, and Aviation and Space Medicine were reviewed for clinically relevant chapters.
The authors acknowledge Rachel Kinsler, USAARL Research Engineer, for her thoughtful review of this manuscript.
The views, opinions, and/or findings contained in this report are those of the authors and should not be construed as an official Department of the Army position, policy, or decision, unless so designated by other official documentation. Citation of trade names in this report does not constitute an official Department of the Army endorsement or approval of the use of such commercial items.
Airlines for America. Air travelers in America: annual survey. Accessed May 1, 2021. https://www.airlines.org/dataset/air-travelers-in-america-annual-survey/#
14 Code of Federal Regulations §25.841—pressurized cabins. Accessed May 1, 2021. https://www.govinfo.gov/app/details/CFR-2012-title14-vol1/CFR-2012-title14-vol1-sec25-841
- Ahmedzai S, Balfour-Lynn IM, Bewick T, et al.; British Thoracic Society Standards of Care Committee. Managing passengers with stable respiratory disease planning air travel. Thorax. 2011;66(suppl 1):i1-i30.
Respiratory disease. In: Green N, Gaydos S, Hutchinson E, et al., eds. Handbook of Aviation and Space Medicine . CRC Press; 2019:329–333.
Dine CJ, Kreider ME. Hypoxia altitude simulation test. Chest. 2008;133(4):1002-1005.
- Matthys H. Fit for high altitude: are hypoxic challenge tests useful? Multidiscip Respir Med. 2011;6(1):38-46.
Bagshaw M. Commercial passenger fitness to fly. In: Gradwell DP, Rainford DJ, eds. Ernsting's Aviation and Space Medicine . 5th ed. CRC Press; 2016:631–640.
Josephs LK, Coker RK, Thomas M; BTS Air Travel Working Group; British Thoracic Society; Managing patients with stable respiratory disease planning air travel. Prim Care Respir J. 2013;22(2):234-238.
Rayman RB, Williams KA. The passenger and the patient inflight. In: DeHart RL, Davis JR, eds. Fundamentals of Aerospace Medicine . 3rd ed. Lippincott Williams & Wilkins; 2002:453–469.
Aerospace Medical Association. Surgical conditions. May 2003. Accessed May 1, 2021. http://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Surgical-Conditions.pdf
- Smith D, Toff W, Joy M, et al. Fitness to fly for passengers with cardiovascular disease. Heart. 2010;96(suppl 2):ii1-ii16.
- Thomas MD, Hinds R, Walker C, et al. Safety of aeromedical repatriation after myocardial infarction: a retrospective study. Heart. 2006;92(12):1864-1865.
Roby H, Lee A, Hopkins A. Safety of air travel following acute myocardial infarction. Aviat Space Environ Med. 2002;73(2):91-96.
- Zahger D, Leibowitz D, Tabb IK, et al. Long-distance air travel soon after an acute coronary syndrome: a prospective evaluation of a triage protocol. Am Heart J. 2000;140(2):241-242.
- Cox GR, Peterson J, Bouchel L, et al. Safety of commercial air travel following myocardial infarction. Aviat Space Environ Med. 1996;67(10):976-982.
Transportation Security Administration. Frequently asked questions. Accessed May 1, 2021. https://tsa.gov/travel/frequently-asked-questions
- Steven S, Frenis K, Kalinovic S, et al. Exacerbation of adverse cardiovascular effects of aircraft noise in an animal model of arterial hypertension. Redox Biol. 2020;34:101515.
Aerospace Medical Association. Ear, nose, and throat. May 2003. Accessed May 1, 2021. https://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Ear-Nose-and-Throat.pdf
Shaikh N, Wald ER, Pi M. Decongestants, antihistamines and nasal irrigation for acute sinusitis in children. Cochrane Database Syst Rev. 2014;(10):CD007909.
- Pinto JA, Dos Santos Sobreira Nunes H, Soeli Dos Santos R, et al. Otitis media with effusion in aircrew members. Aerosp Med Hum Perform. 2019;90(5):462-465.
Aerospace Medical Association. Travel with children. May 2003. Accessed May 1, 2021. https://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Travel-With-Children.pdf
Spinks A, Wasiak J. Scopolamine (hyoscine) for preventing and treating motion sickness. Cochrane Database Syst Rev. 2011;(6):CD002851.
Aerospace Medical Association. Diabetes. May 2003. Accessed May 1, 2021. http://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Diabetes.pdf
Passenger fitness to fly. In: Green N, Gaydos S, Hutchinson E, et al., eds. Handbook of Aviation and Space Medicine . CRC Press; 2019:263–266.
Watson HG, Baglin TP. Guidelines on travel-related venous thrombosis. Br J Haematol. 2011;152(1):31-34.
Possick SE, Barry M. Evaluation and management of the cardiovascular patient embarking on air travel. Ann Intern Med. 2004;141(2):148-154.
- Clarke MJ, Broderick C, Hopewell S, et al. Compression stockings for preventing deep vein thrombosis in airline passengers. Cochrane Database Syst Rev. 2021;(4):CD004002.
Gavish I, Brenner B. Air travel and the risk of thromboembolism. Intern Emerg Med. 2011;6(2):113-116.
Tin AH, Rabinowitz P, Fowler H. Emotional support animals: considerations for documentation. Am Fam Physician. 2020;101(5):302-304. Accessed May 1, 2021. https://www.aafp.org/afp/2020/0301/p302.html
U.S. Department of Transportation. U.S. Department of Transportation announces final rule on traveling by air with service animals. December 2, 2020. Accessed May 1, 2021. https://www.transportation.gov/briefing-room/us-department-transportation-announces-final-rule-traveling-air-service-animals
Trevorrow T. Air travel and seizure frequency for individuals with epilepsy. Seizure. 2006;15(5):320-327.
Hastings, JD; Aerospace Medical Association. Medical guidelines for airline travel: air travel for passengers with neurological conditions. September 2014. Accessed May 1, 2021. http://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Neurology-Sep-2014.pdf
ACOG Committee opinion no. 746: air travel during pregnancy. Obstet Gynecol. 2018;132(2):e64-e66.
Royal College of Obstetricians and Gynaecologists. Air travel and pregnancy: scientific impact paper no. 1. May 2013. Accessed May 1, 2021. http://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/RCOG-Pregnancy-and-Air-Travel-Scientific-Impact-Paper.pdf
Harvard Medical School. Are full-body airport scanners safe? June 2011. Accessed May 1, 2021. https://www.health.harvard.edu/diseases-and-conditions/are-full-body-airport-scanners-safe#:~:text=he%20authors%20begin%20with%20an,the%20biological%20effects%20of%20radiation
Aerospace Medical Association. Ophthalmological conditions. May 2003. Accessed May 1, 2021. http://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Ophthalmological-Conditions.pdf
Bettes TN, McKenas DK. Medical advice for commercial air travelers. Am Fam Physician. 1999;60(3):801-808. Accessed May 1, 2021. https://www.aafp.org/afp/1999/0901/p801.html
Aerospace Medical Association. Jet lag. May 2003. Accessed May 1, 2021. https://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Jet-Lag.pdf
Choy M, Salbu RL. Jet lag: current and potential therapies. PT. 2011;36(4):221-231.
- Waterhouse J, Reilly T, Atkinson G, et al. Jet lag: trends and coping strategies. Lancet. 2007;369(9567):1117-1129.
Herxheimer A, Petrie KJ. Melatonin for the prevention and treatment of jet lag. Cochrane Database Syst Rev. 2002;(2):CD001520.
Divers Alert Network. February 1, 2017. Accessed May 11, 2021. https://dan.org/alert-diver/article/flying-after-pool-diving-2/
Mitchell GW, Martin GJ. Chapter 19 Infectious diseases. In: Davis JR, Johnson R, Stepanek J, et al. Fundamentals of Aerospace Medicine . 4th ed. Lippincott Williams & Wilkins; 2008:432–446.
Centers for Disease Control and Prevention. Domestic travel during COVID-19. Updated April 27, 2021. Accessed April 30, 2021. https://www.cdc.gov/coronavirus/2019-ncov/travelers/travel-during-covid19.html
Co M, Ng J, Kwong A. Air travel and postoperative lymph-edema—a systematic review. Clin Breast Cancer. 2018;18(1):e151-e155.
Hu JS, Smith JK. In-flight medical emergencies. Am Fam Physician. 2021;103(9):547-552. Accessed April 30, 2021. https://www.aafp.org/afp/2021/0501/p547.html
Continue Reading

More in AFP
More in pubmed.
Copyright © 2021 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Can You Fly With High Blood Pressure? What You Need To Know

Traveling is a fantastic way to escape the daily routine, experience new cultures, and create unforgettable memories. However, traveling can be challenging if you have certain health conditions, such as:
- High blood pressure
- Asthma & allergies
However, living with health conditions shouldn’t stop you from exploring the world. With adequate preparation and the right precautions, you can have a safe and enjoyable trip.
In today’s post, we’ll share everything you need to know about traveling with high blood pressure, including:
- What hypertension is
- Risks of traveling with high blood pressure
- What to consider when planning your trip
- Some tips on high blood pressure and flying
Without further ado, let’s begin.
What is Hypertension? (aka High Blood Pressure)
For most people, hypertension is defined as a blood pressure reading over 140/90 mm Hg. According to WHO, approximately 1.28 billion adults aged 30 to 79 suffer from hypertension worldwide, and 46% are unaware of it. Besides, only 1 in 5 people (21%) has it under control.
High blood pressure is a leading cause of death or a contributing factor. Sadly, hypertension doesn’t show evident symptoms.
Severe high blood pressure cases (usually 180/120 or higher) may experience the following symptoms:
- Severe headaches
- Difficulty breathing
- Blurred vision
- Abnormal heart rhythm
All in all, high blood pressure is a common condition but it can be serious if it’s not treated. Typically, you can reduce your blood pressure by adopting a healthier lifestyle with practices like:
- Exercising regularly
- Keeping a healthy diet
- Quitting smoking
- Avoiding excessive alcohol and caffeine consumption
- Monitoring blood pressure at home or your local pharmacy
- Reducing stress
- Minimizing salt consumption
Nonetheless, some people may need to take medications.
High Blood Pressure and Flying: What Are The Risks?
Overall, high blood pressure patients who take medication don’t have an increased risk of health problems at higher altitudes. Nevertheless, poorly controlled or severe hypertension does increase this risk.
The effects of occasional flying on heart health are relatively unstudied. Yet, according to a recent study , even men in good health have an increased blood pressure of 6% during commercial flights.
According to the CDC , about 1 in 600 flights experience a medical emergency, such as:
- Heart problems
- Nausea or vomiting
And blood pressure may be a contributing factor to some of these emergencies.
What to Consider When Planning Your Trip
Traveling to high altitudes (5,000 to 11,500 feet) can increase blood pressure. Why? At these heights, your blood works harder to deliver oxygen, causing blood pressure to rise.
Therefore, when planning your trip, you may want to avoid destinations like:
However, if you already booked your trip, don’t panic: managing your blood pressure at high altitudes is possible. Experts recommend:
- Light physical activity
- Avoid climbing more than 300 meters per day
Be extra mindful of these tips when staying in mountainous areas, like the Alps or the Andes.
Overall, traveling at high altitudes shouldn’t be a problem as long as your blood pressure is controlled and you take some precautions. Here are some tips you may want to consider:
- Consult your doctor 8 weeks before your trip to discuss your travel plans.
- Get your medication ready , and make sure to bring enough to cover your whole trip. Besides, bringing a bit extra may be a good idea in case your return flight gets rescheduled.
- Keep your alcohol and caffeine consumption to a minimum during your flight to avoid dehydration.
- Be careful with airline food, it might have high sodium levels , which can raise your blood pressure.
- Taking Dramamine to avoid motion sickness doesn’t interfere with blood pressure medications.
- Avoid using sedative and hypnotic medications before and during flight.
- Promote circulation by moving around during your flight with walks every two hours and by moving in your seat.
Key Takeaways
Ultimately, traveling with high blood pressure doesn’t have to limit your travel plans. With proper planning, taking necessary precautions, and consulting your doctor, you can enjoy your trip confidently and safely.
Remember to:
- Monitor your blood pressure
- Make wise choices regarding food and drink
- Stay active during your journey
Want to get tested for COVID before your next trip? No matter where you are, or what type of test you need, find testing locations near you with our international directory .
Have Travel Questions?
Join our Facebook community full of travelers like you
Recent posts

COVID Testing in San Antonio

Best Foods for COVID Recovery

COVID Testing in Spanish: What to Know and Who to Ask

COVID Pandemic Effects: Social Impact, Mental Health, Worklife, and more
Share this article.
- Skip to primary navigation
- Skip to main content
- Skip to footer
Your Blood Pressure Specialist
Can You Fly With High Blood Pressure?
Michael Rotman, MD, FRCPC, PhD | Medically reviewed by Robin Backlund, BHSc Last update: December 1, 2023
Do you have upcoming travel plans requiring flying with high blood pressure? Read our guide to learn about the risks involved and how to prevent them.
Quick Summary
- High blood pressure or hypertension can be a concern when traveling by air due to the medical risks involved.
- Cabin pressurization aims to reduce the chance of symptoms; however, it is not always effective at preventing ailments like hypoxia.
- Certain precautions can make flying with blood pressure safer while preventing issues during your journey.
Fear of flying extends beyond the bumps and jolts of air turbulence. For a significant number of people, it’s underlying health issues like high blood pressure that turn the boarding gate into a gateway of apprehension.
High blood pressure, also known as hypertension, is a medical condition where the force of blood against your artery walls is consistently too high. Symptoms might be elusive but can include headaches, shortness of breath, and nosebleeds. Left unmanaged, hypertension can lead to severe health problems like heart disease.
The aviation environment can exacerbate these concerns. Air travel exposes your body to altitude changes, triggering symptoms like headaches and nausea. Add in the stress of travel, and you’ve got a recipe for increased blood pressure levels.
Though modern airplanes employ cabin pressurization to mitigate health risks, it’s essential to heed expert advice. As specialists point out:
“Flying at high altitudes can be particularly hazardous for those with pulmonary hypertension.”
So, if you’re one of the millions dealing with hypertension and contemplating a trip up in the clouds, consider this article your guidebook. It aims to arm you with all the information needed for a healthier, more comfortable flying experience.
Is this takeoff-ready? Shall we move on?
Why Is High Blood Pressure A Concern During Air Travel?
When you have high blood pressure, flying isn’t just about securing the best window seat. It’s a health consideration, too. As the airplane ascends, changes in altitude exert pressure on your body.
The air up there is less dense, meaning your body has to work harder for oxygen. This can spike your blood pressure even if it’s generally well-controlled at ground level.
Studies shed light on this. They show a notable increase in blood pressure levels at higher altitudes, even among otherwise healthy individuals.
Lack of oxygen, also known as hypoxia, poses an additional threat. Especially when coupled with existing conditions like heart disease, the stakes get higher. Medical emergencies like hypoxia can be more frequent and severe.
So, it’s not just the dizzying heights that are concerning. It’s what those heights can do to your circulatory system that warrants attention.
How Does Cabin Pressure Affect Your Blood Pressure?
Ever wonder why you can breathe easily on a plane cruising at 35,000 feet? Thank cabin pressure for that. Simply put, cabin pressure is the regulated air pressure inside the airplane that mimics conditions closer to sea level.
Aircraft have pressure control systems that work diligently to maintain this environment. These systems pump in compressed air, mostly harvested from the plane’s engines, into the cabin. It’s a fine balancing act to keep passengers comfortable and safe.
However, even with these mechanisms, the cabin pressure usually simulates an altitude of around 6,000 to 8,000 feet. It’s not quite the same as being on the ground.
For people with high blood pressure, this can be a point of concern. Although cabin pressure alleviates many issues related to altitude, it’s not a perfect substitute for the sea-level conditions our bodies are accustomed to.
Your body still has to work a bit harder for oxygen, and your blood pressure can be elevated as a result.
At the aforementioned altitudes, the barometric pressure drops from 760 mm Hg at sea level to 560 mm Hg. As a result of this pressure change, arterial oxygen tension decreases, which can cause ischemia and arrhythmias in susceptible individuals. The inspired PO2 falls by 4 mm Hg per 1,000 feet above sea level.
As a result, patients with concomitant pulmonary diseases such as chronic obstructive pulmonary disease and pulmonary hypertension may require supplemental oxygen during travel. Additionally, patients with chronic cardiovascular diseases, including severe left and/or right ventricular dysfunction and congenital heart disease, can be more sensitive to changes in arterial oxygen saturation.
In a recent study, published in the Anatolian Journal of Cardiology, 12 men without any known cardiovascular disease or coronary risk factors were monitored on commercial flights. They reported 24% elevated heart rate, 6% increase in blood pressure, and reduced parameters of heart rate variability.
While this may not present any risks for individuals in good health, the situation differs for individuals diagnosed with uncontrolled high blood pressure. We strongly encourage individuals in such circumstances to take preventive measures.
Plus, the relatively lower pressure can cause existing blood clots to expand, posing a risk for complications like deep vein thrombosis (DVT).
According to a study published in the British Medical Journal, tracking 5,408 individuals hospitalized with venous thromboembolism, it was discovered that the risk of this condition is elevated specifically within a two-week period following a long-haul flight. Afterward, the risk subsides and returns to its usual levels.
Can Dehydration Affect My Blood Pressure While Flying?
Hydration is more than just a wellness trend; it’s critical when flying, particularly for those with high blood pressure. Air travel is notoriously dehydrating. Ever notice how parched you feel during a flight? That’s not a coincidence.
Airplane cabins have incredibly low humidity levels, often ranging between 10-20%. To put it in perspective, most homes have a humidity level of around 30-60%. This dry air can zap moisture from your skin and respiratory system at an accelerated rate.
According to a study published in the Journal of Environmental and Public Health, the average person loses up to 8 percent of their body weight in water during a flight or about 8 ounces (0,25 liters) of water per hour, enough to cause a 10 mmHg increase in blood pressure.
But here’s the kicker: dehydration can also elevate your blood pressure . When you’re dehydrated, your blood volume decreases. This means your heart has to work harder to pump blood, which can result in a surge in blood pressure levels.
Combine the arid conditions inside an airplane with the body’s natural tendency to become dehydrated, and you’ve got a situation that can escalate your blood pressure.
This is why sipping water throughout the flight isn’t just refreshing, it’s a health imperative. And while it might be tempting to pass the time with coffee or a cocktail, keep in mind that caffeine and alcohol can worsen dehydration.
So, staying hydrated is not just about quenching your thirst; it’s a crucial step in managing your blood pressure while flying.
What Types of Medications Should I Consider When Flying With Hypertension?
If you’re flying with high blood pressure, medications are likely part of your travel checklist. Common medications for hypertension include beta blockers, ACE inhibitors, and diuretics. Each has its own set of instructions, so it’s crucial to consult your healthcare provider before you take off.
Timing is key when it comes to medication. Long-haul flights can mess with your regular schedule, potentially impacting your medication routine. Missing a dose or taking it late can lead to unstable blood pressure levels.
Many travelers wonder if they can pack their pills in checked baggage. The answer is a resounding no. Always carry medications in your hand luggage and keep prescriptions in their original packaging. This ensures you have access to them throughout the flight and during layovers.
Something else to consider is that airplanes are not the best places for medication storage. Extreme temperatures can compromise medication efficacy. So, a simple trick is to keep them in a sealed bag and place them in a more temperate location in your carry-on.
What Steps Should I Take F or Pre-Flight Checkups?
Planning a flight when you have hypertension ? A visit to your healthcare provider should be on your pre-flight to-do list. Think of it as your medical pre-check, a critical step to ensure you’re fit for air travel.
During this checkup, your healthcare provider will likely assess your blood pressure levels, review your medication, and discuss any symptoms you’ve been experiencing. They might also run some basic tests like blood work or an EKG to evaluate your heart’s condition.
Why is this pre-flight medical visit so crucial? Well, it’s all about risk assessment. If your blood pressure isn’t well-controlled or you’ve recently had cardiovascular issues, your provider might suggest delaying travel or making specific accommodations for your journey.
Often, a checkup could lead to medication adjustments tailored for travel. For instance, if your flight crosses multiple time zones, your healthcare provider may advise altering your medication timing to align with your destination’s local time.
How Can I Avoid Deep Vein Thrombosis (DVT) During My Flight?
The term “Deep Vein Thrombosis” or DVT might sound like something out of a medical thriller, but it’s a real concern for flyers, particularly those with hypertension. Simply put, DVT is the formation of a blood clot in a deep vein, often in the legs. Long periods of immobility, like during a flight, can elevate this risk.
The scenario is pretty straightforward: when you’re seated for an extended time, blood flow in the legs can become sluggish. For someone with high blood pressure, this reduced circulation could lead to clot formation. And if that clot breaks free, it can travel to the lungs, causing a life-threatening condition called pulmonary embolism.
So, how can you dodge this risk? First, stay active. You don’t need to do in-seat aerobics, but simple exercises can help. Rotate your ankles, flex your feet, and take short strolls down the aisle when it’s safe to do so.
You could even massage your calves if the space allows. In a study published by the Japanese Society of Physical Therapy, involving 165 patients who underwent primary unilateral total knee arthroplasty, half of whom relied solely on self-calf massage as a preventive measure for deep vein thrombosis, it was discovered that the incidence of this condition decreased significantly.
Specifically, the occurrence rate decreased from 6.5% to 0.8% after implementing this massage technique. Therefore, we urge people at risk to use this method to prevent DVT during a flight.
Compression socks are also a good idea. These special stockings apply pressure to your lower legs, helping to maintain blood flow and reduce the risk of DVT. Just make sure to choose the right size and compression level, usually with guidance from a healthcare provider.
Actually, according to a newer study from 2021 published in the Cochrane Library, that involved 2637 participants, the odds of developing symptomless DVT were significantly lower in participants who wore stockings compared to those who did not.
Additionally, no cases of symptomatic DVT, pulmonary emboli, or deaths were reported. The evidence also suggests a potential reduction in superficial vein thrombosis with the use of stockings, although the difference was not statistically significant.
Wearing stockings also had a notable impact in reducing edema, as supported by multiple trials. Overall, no significant adverse effects were reported. These findings highlight the efficacy and safety of wearing compression stockings as a preventive measure for DVT and associated symptoms.
How Does Jet Lag Impact High Blood Pressure?
Jet lag isn’t just a nuisance that throws off your sleep schedule; it can have palpable effects on your blood pressure. This disruption stems from your body’s internal clock, or circadian rhythm, getting out of sync with the time zone you’ve traveled to.
Here’s the deal: jet lag can lead to erratic sleeping and eating patterns. Your body is essentially playing catch-up, trying to align its internal clock with a new day-night cycle. These changes can stress your body and, yes, lead to spikes in your blood pressure.
A study published in the American Journal of Hypertension investigated the impact of acute sleep deprivation on 24-hour blood pressure monitoring (ABPM) in 36 previously untreated patients with mild to moderate hypertension. Using a crossover design, the participants were randomly assigned to experience either sleep deprivation or a full night’s sleep, with a one-week interval between the two conditions. ABPM was conducted during both sessions.
Results showed that during the sleep-deprivation period, the average 24-hour blood pressure and heart rate were higher compared to measurements taken on a regular workday.
This difference was particularly pronounced during the nighttime. Additionally, the morning following a sleep-insufficient night, both blood pressure and heart rate exhibited a significant increase.
In summary, the study demonstrated that acute sleep deprivation, especially during the first part of the night, had a detrimental effect on 24-hour blood pressure and heart rate. These findings highlight the importance of adequate sleep in maintaining optimal cardiovascular health, particularly for individuals with hypertension.
So, what can you do to mitigate this? First, consider adjusting to your new time zone a few days before your flight. Gradually shift your sleeping and eating schedules to match the destination’s local time. Doing this can help ease your body into the new rhythm, reducing stress and its impact on your blood pressure .
Hydration also plays a role here. We’ve already touched on the dehydrating aspects of flying, but when it comes to jet lag, staying hydrated can be particularly helpful. Dehydration can exacerbate the effects of jet lag, further complicating your body’s adjustment efforts.
Melatonin supplements could be another avenue to explore. They can help reset your internal clock but consult your healthcare provider before taking them, especially if you’re on blood pressure medications.
What Should Be In My High Blood Pressure Travel Kit?
Traveling with high blood pressure requires some extra prep, and a well-stocked travel kit can be your best ally. Think of it as your personalized, on-the-go health station.
- First and foremost, medication. Pack enough to last the entire trip, plus some extra in case of delays. As mentioned earlier, keep these medications in your carry-on bag and always in their original packaging. Don’t forget to include a copy of your prescription as well; it’s your golden ticket in case you need a refill or have to explain your meds to security personnel.
- Next, hydration. A refillable water bottle is a must-have. Airports and planes are dry environments that can contribute to dehydration, a factor that can exacerbate high blood pressure. A reusable bottle can be filled after airport security and ensures you stay hydrated throughout the flight.
- Let’s talk snacks. Salty airplane food won’t do you any favors if you’re watching your blood pressure. Pack your own low-sodium, nutrient-rich snacks like unsalted nuts, fruits, or whole-grain crackers. They’ll not only keep your hunger at bay but also help maintain a steady blood pressure.
- Also, consider adding a portable blood pressure monitor to your kit. These handy devices are compact and can give you peace of mind by allowing you to check your levels during the journey. However, make sure to consult your healthcare provider on the best way to interpret and act on the readings you get while in transit.
What Are Some Dietary Precautions To Take When Flying With High Blood Pressure?
If you’re flying with high blood pressure, your diet shouldn’t take a backseat. In fact, what you consume before and during your flight can have a direct impact on your blood pressure levels.
- Let’s start with the big offender: salt . Airlines aren’t exactly known for their low-sodium culinary offerings. High salt intake can send your blood pressure soaring, making the already stressful environment of an airplane even less welcoming. The solution? Opt for low-sodium snacks like fruits or whole-grain crackers, as mentioned earlier.
- Now, about alcohol. A glass of wine or a beer might seem tempting, especially if it’s free. But alcohol can dehydrate you and lead to a spike in your blood pressure. It can also interfere with any medications you’re taking. Best to steer clear and stick with water or herbal teas.
- And don’t forget caffeine. That cup of coffee before boarding might wake you up, but it can also wake up your blood pressure. Like alcohol, caffeine can have diuretic effects, meaning it can dehydrate you. If you can’t do without, try limiting yourself to just one cup several hours before your flight.
So, what should be on your food radar? Low-sodium and potassium-rich foods can help balance your blood pressure. Opt for fresh fruits like bananas and oranges, and consider whole-grain foods like brown rice or whole-wheat bread.
What About Anxiety A nd Stress During Air Travel?
When flying, the term “turbulence” can apply to more than just air pockets. Anxiety and stress are common travel companions, and for those with high blood pressure, they’re passengers you’d rather not have on board.
Let’s get this straight: stress and anxiety can be like adding fuel to the fire when it comes to high blood pressure. These emotional states trigger your body’s “fight-or-flight” response, leading to temporary spikes in blood pressure. Over time, these short-lived increases can add up, presenting additional risks during travel.
So how do you keep your cool? One proven method is deep breathing exercises . By focusing on your breath, you activate your body’s relaxation response, effectively countering the stress-induced increases in blood pressure. Just a few minutes of deep breathing can go a long way.
Another tool in your anti-anxiety toolkit could be meditation or mindfulness techniques. These practices encourage you to be present, helping you tackle stressors as they come rather than dwelling on “what-ifs.” There are even meditation apps specifically designed for travel that can guide you through quick, effective sessions.
And don’t underestimate the power of distraction. Whether it’s a gripping novel, a playlist of your favorite calming tunes, or even a simple game on your phone, distractions can pull your mind away from stressors, keeping your blood pressure more stable.
How Do Airlines Handle Passengers With Medical Conditions Like Hypertension?
Navigating the airport and plane can be a maze of protocols and procedures. But what happens when you throw a medical condition like hypertension into the mix? Let’s unpack how airlines typically handle passengers with high blood pressure.
First off, airlines are equipped to handle a variety of medical conditions, including high blood pressure. Most carriers have standard procedures to ensure the safety and comfort of passengers with health issues. But it’s essential to be proactive. Inform the airline about your condition when booking your ticket or at least a few days before your departure.
Why does this matter? Early notification gives the airline time to make necessary accommodations. These can range from priority boarding to quick access to medical aid in case of an emergency. Some airlines even provide the option to request a briefing with the cabin crew about your specific needs.
Now, let’s talk clearances. In most cases, if your high blood pressure is well-managed, you won’t need a medical clearance to fly. However, if you’ve recently had surgery or experienced significant changes in your condition, a clearance from your healthcare provider might be necessary. This usually involves filling out a medical form provided by the airline and having it signed by your doctor.
Do I Need Special Travel Insurance For High Blood Pressure?
Insurance might seem like a dreary subject, but when you’re flying with high blood pressure, it becomes essential. It’s that safety net that can turn a potential calamity into a manageable situation.
First things first, many standard travel insurance policies cover medical emergencies. However, “standard” often excludes pre-existing conditions like hypertension. This is where specialized travel insurance comes into play. These policies specifically cover health conditions you already have, making sure you’re not left in a lurch if something goes awry.
Why is this so crucial? Medical care can be expensive, especially if you’re abroad. We’re talking not just about doctor visits, but also any unexpected hospital stays or procedures. With the right insurance, these potential financial burdens become less daunting.
Picking the right policy requires some homework. Look for coverage that includes emergency medical services, hospitalization, and even emergency evacuation if you’re traveling to remote places. It’s also wise to check if the policy requires you to inform them of any medication changes or hospital visits prior to your trip.
What Should Frequent Flyers With High Blood Pressure Know?
For some, flying is a rare adventure. But what if you’re someone whose job or lifestyle makes you a frequent visitor to the skies? When you have high blood pressure, that frequent-flyer status comes with its own set of considerations.
- First up, consistency is key. If you’re regularly flying, keeping a constant medication schedule becomes even more critical. Changes in time zones can mess with your internal clock, potentially disrupting your medication timing. Always keep a watch or set phone reminders to make sure you’re taking your medication as prescribed.
- Speaking of medication, always pack extra. Delays and cancellations are part and parcel of air travel. Having a surplus ensures you won’t run out if your travel plans go awry. Keep these meds in your carry-on; you don’t want them trapped in a checked bag that might go missing.
- You’ll also want to get familiar with airport layouts . Why? The less time you spend rushing to your gate, the less stress you’ll experience. Many airports offer maps and apps to help you navigate your way swiftly and calmly.
- Airline loyalty can be a boon. Sticking with one airline can net you benefits like priority boarding and extra legroom. These small perks can reduce stress, making for a more comfortable and blood pressure-friendly journey.
- Last but not least, develop a pre-flight routine. Whether it’s a quick session of deep breathing or a favorite playlist, having a go-to ritual can help your body relax and prepare for the flight, contributing to more stable blood pressure levels.
How Important Is Consultation With A Cardiologist or Primary Care Doctor?
Sure, the internet is a treasure trove of information. But when it comes to health, nothing replaces the expertise of a healthcare provider, especially if you’re planning to fly with high blood pressure. So, how vital is that visit to a cardiologist or primary care doctor?
To put it simply: very. Consulting a healthcare provider is your first line of defense. They’ll assess your condition, review your medications, and offer tailored advice on how to manage blood pressure while flying. It’s like having a personalized travel guide, but for your health.
Why is this so crucial? Well, uncontrolled high blood pressure can turn a routine flight into a medical emergency. A healthcare provider can tell you if you’re fit to fly, and if any medication adjustments are needed. You wouldn’t fly a plane without a pre-flight check, so consider this your personal health check before takeoff.
Your healthcare provider can also offer travel tips you might not have considered. Simple advice like staying hydrated or doing in-seat exercises can go a long way in keeping your blood pressure stable mid-air.
A common part of these consultations is a blood pressure check, often done in both arms. This gives a baseline, providing something to compare against should you experience issues during your trip.
So, yes, before you buckle that seatbelt and recline that chair, consult your healthcare provider. It’s a simple step that can set the stage for a smoother, safer journey.
We’ve covered a lot of sky today, from the science of cabin pressure to the nitty-gritty of medication schedules. If you’re planning to fly with high blood pressure, taking these factors into account can make your journey as smooth as a well-piloted plane.
Firstly, don’t overlook the importance of a healthcare consultation. Whether it’s your cardiologist or primary care doctor, their advice is your roadmap for a safe trip. And while you’re at it, consider specialized travel insurance that covers hypertension-related incidents. It’s your financial safety net in the sky.
For the frequent flyers among you, remember, consistency is your best companion. A stable medication schedule and familiar airport layouts can drastically reduce stress levels. If you’re flying often, stick with an airline to enjoy perks that make your journey more comfortable.
Don’t underestimate the little things either. Hydration is crucial, as is having a well-stocked travel kit filled with your medications and other essentials. To fend off complications like Deep Vein Thrombosis, simple exercises can do wonders.
As for food, steer clear of salty snacks and alcohol. Opt instead for healthier alternatives like fruits or whole-grain bars. Add in some deep breathing or a calming playlist, and you’ve got yourself a stress-reducing, blood pressure-friendly flight routine.
So go ahead, book that ticket. With these tips in your arsenal, the sky is not the limit, but your next adventure. Safe travels!
Have we landed smoothly? Ready for takeoff?
Effect of self-calf massage on the prevention of deep vein thrombosis after total knee arthroplasty: A randomized clinical trial. 2020. Oka T, Wada O, Nitta S, Maruno H, Mizuno K. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7344361/
Assessment of Hydration Status and Blood Pressure in a Tertiary Care Hospital at Al-Khobar. 2022. Mohammedin AS, AlSaid AH, Almalki AM, Alsaiari AR, Alghamdi FN, Jalalah AA, Alghamdi AF, Jatoi NA. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9441182/
Compression stockings for preventing deep vein thrombosis in airline passengers. 2021. Clarke MJ, Broderick C, Hopewell S, Juszczak E, Eisinga A. https://pubmed.ncbi.nlm.nih.gov/33878207/
Effects of insufficient sleep on blood pressure in hypertensive patients: a 24-h study. 1999. Lusardi P, Zoppi A, Preti P, Pesce RM, Piazza E, Fogari R. https://pubmed.ncbi.nlm.nih.gov/10075386/
Systemic arterial hypertension and flight. 2021. Okyay K. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8412044/
Was this helpful?


Michael Rotman, MD, FRCPC, PhD
Michael Rotman is a Structural Heart Specialist, Interventional Cardiologist and Scientist. He has more than a decade of experience in treating heart related desease, as well as authoring and reviewing health and wellness-related content. Currently work for a St. Michael’s Hospital in Toronto.
Email | Instagram | Twitter
You May Also Like

DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
TheEMTSpot adheres to rigorous sourcing guidelines and relies solely on peer-reviewed studies, scholarly research institutions, and medical journals and associations for information. We steer clear of using tertiary references. We embed primary sources — encompassing studies, scientific references, and statistics — within each article and additionally list them in the resources section at the end of our articles. You can learn more about how we safeguard the accuracy and timeliness of our content by reviewing our editorial policy .
Site Navigation
Useful Links
[email protected]
Switch language

All TheEMTSpot’s content is medically reviewed or fact checked to ensure that it is as accurate as possible.
We have strict sourcing guidelines and only link to other reputable media sites, educational institutions, and, whenever possible, peer-reviewed studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please contact us .

Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
High altitude provides a unique physiologic challenge to the cardiovascular system. The cardiovascular response in both healthy individuals and in patients with cardiovascular disease will be reviewed here. Insights surrounding high-altitude disease will also be included to provide a comprehensive understanding. (See "High-altitude illness: Physiology, risk factors, and general prevention" .)
Most importantly, this topic will discuss the impact of high altitude on the heart and the associated hemodynamic changes. Altitude exposure can also lead to a variety of well-described clinical syndromes including some not directly involving the cardiovascular system, such as acute mountain sickness (AMS), high-altitude pulmonary edema, high-altitude cerebral edema, and high-altitude retinal hemorrhage. These conditions are discussed separately. (See "High-altitude pulmonary edema" and "Acute mountain sickness and high-altitude cerebral edema" and "High-altitude illness: Physiology, risk factors, and general prevention", section on 'Other altitude-related illnesses' .)
BAROMETRIC PRESSURE AND PIO2
Although altitude is the most obvious determinant of barometric pressure and its resulting physiologic stress, other factors can contribute to a reduction in barometric pressure including a decrease in temperature, deteriorating weather (ie, blizzards, hail, or extreme winds), and distance from the equator.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Anatol J Cardiol
- v.25(Suppl 1); 2021

Can a patient with pulmonary hypertension travel safely by plane?
Air travel is known as the safest way of transportation. Therefore, patients with health problems prefer to travel by air; however, those with heart or lung issues, who do not have any problems under normal conditions, may experience some problems in high altitude and different environmental conditions. In this review, we have described the points to be considered during air travel in patients with pulmonary hypertension.
Introduction
Airline transportation, which is the fastest and safest form of travel, is preferred frequently nowadays with the advancement of technology. Over a billion people worldwide travel on commercial aircrafts every year, and there are a reported 0.31 in-flight deaths per million passengers carried. Cardiovascular events represent the main cause of death during a flight. Owing to engineering and financial constraints, the pressure inside the cabin is kept at a maximum altitude of 2,438 m. This reduction in cabin pressure is equivalent to 15% breathable oxygen compared with 21% at sea level ( 1 , 2 ).
In patients with a diagnosis of pulmonary hypertension (PH), the hypobaric environment during air travel leads to a general hypoxic vasoconstriction in the pulmonary circulation, which exacerbates pulmonary vascular resistance and right ventricular afterload and may lead to acute right-heart failure. Therefore, in addition to the typical flight-related risks, such as deep vein thrombosis, pulmonary thromboembolism, and changes in fluid balance, people with cardiovascular and pulmonary diseases also have an increased risk of worsening hemodynamics during a flight ( 3 ).
Air travel can cause significant respiratory problems in a patient with severe pulmonary arterial hypertension (PAH) because of high-altitude hypoxemia. Despite the risks of physiological compromise, there are limited data on the effects of air travel in patients with PAH in the literature. It is known that air travel activates certain elements of human response to hypoxia, including increased ventilation and erythropoietin secretion ( 4 ). Another classic response, hypoxic pulmonary vasoconstriction, may be more clinically relevant. Therefore, hypoxia can cause increased pulmonary artery pressure that may lead to PH and ultimately right heart failure, such as in hypoxic lung disease and at high altitude. Such an effect may be important for some sensitive passengers. Hypoxic pulmonary vasoreactivity varies greatly among individuals, and high reactivity could lead to hypoxia-related diseases such as high-altitude pulmonary edema. Susceptible passengers may similarly be at risk of hypoxia-induced PH and its sequelae during a flight ( 5 , 6 ).
Hypoxemia is common among patients with PAH traveling by air. Hypoxemia is mostly associated with ambulation during flight, lower cabin pressures, failure to use O 2 in people with home oxygen (predominantly nighttime-only users), and longer flight duration. Patients with PAH traveling on long-duration flights or who have a history of oxygen supply should be evaluated for supplemental in-flight oxygen ( 7 ).
There are no studies using flight simulation to determine the need for oxygen supply during prolonged air travel in patients with PAH. The European Society of Cardiology and the European Respiratory Society (ERS) (2015) guidelines recommend that oxygen supplementation should be considered in patients with World Health Organization functional class III and IV and arterial blood O 2 pressure continuously <8 kPa (60 mm Hg). Oxygen support inspired by 2 L/min increases partial pressure of oxygen to values seen at sea level. Similarly, these patients should avoid going to altitudes higher than 1,500–2,000 m without additional oxygen support. The patients should be warned to travel with written information about their PAH and to get in close contact with the local PH clinics ( 8 ). Guidelines for PH by the American College of Cardiology/American Heart Association suggest that supplemental oxygen be made available on commercial aircraft for patients with a pre-flight pulse oximetry oxygen saturation <92% ( 9 ). For patients with chronic pulmonary disease who are planning to travel by air, ERS advises a minimum pulmonary vital capacity of 3 L, a forced expiratory volume in 1 second (FEV 1 ) >70% of reference, a minimum oxygen saturation of 85%, and a minimum arterial partial oxygen pressure of 70 mm Hg, as well as a stable state of vital signs ( 3 , 10 ).
The hypoxia altitude simulation test (HAST) is a standardized and well-known pre-flight assessment tool that has increasingly been used in patients with chronic obstructive pulmonary disease recently. The patient breathes a mixture of hypoxic gases of 15.1% oxygen, mimicking the effects of an altitude of 8,000 feet (2,438 m), and changes in oxygen saturation and arterial blood gases are used to estimate the severity of hypoxemia during flight. The patient is also monitored for symptoms and myocardial ischemia or arrhythmias, and the overall goal is to reduce morbidity and mortality during a flight. The pre-flight aeromedical assessment of patients with sensitive respiratory systems can be performed by combining echocardiography with a standard HAST, by inhaling the mild hypoxic gas mixture, and predicting responses during flight. At sea level, this gas mixture replicates the in-flight partial inspired oxygen pressure of at the maximum allowed altitude of 8,000 feet. HAST-echo can lead to predicting in-flight changes of pulmonary hemodynamics, prescribing in-flight complementary oxygen, and ultimately deciding on suitability for flight ( 11 , 12 ).
Employment as aircraft crew or cabin crew may not be safe for people who are prone to flight-induced PH, even in the absence of symptoms. Patients in whom exaggerated hypoxic pulmonary vasoreactivity can be predicted, such as those diagnosed with Chuvash polycythemia or with a history of high-altitude pulmonary edema, pre-employment screening with HAST-echo may be recommended ( 13 ).
Considering the potential health risks of air travel in patients with PH, all patients with PH should consult their physician prior to flying. Patients with sensitive respiratory systems should be warned by their physicians in terms of the risks that may occur during the flight and the necessary precautions to be taken before air travel. Large-scale studies are needed for more information on this issue.
Conflict of interest: None declared.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 06 January 2022
Travelling with heart failure: risk assessment and practical recommendations
- Stephan von Haehling 1 , 2 ,
- Christoph Birner 3 , 4 ,
- Elke Dworatzek 5 , 6 ,
- Stefan Frantz 7 ,
- Kristian Hellenkamp 1 ,
- Carsten W. Israel 8 ,
- Tibor Kempf 9 ,
- Hermann H. Klein 10 ,
- Christoph Knosalla ORCID: orcid.org/0000-0002-8127-5019 6 , 11 , 12 ,
- Ulrich Laufs ORCID: orcid.org/0000-0003-2620-9323 13 ,
- Philip Raake 14 , 15 ,
- Rolf Wachter 1 , 2 , 13 &
- Gerd Hasenfuss 1 , 2
Nature Reviews Cardiology volume 19 , pages 302–313 ( 2022 ) Cite this article
39k Accesses
6 Citations
164 Altmetric
Metrics details
- Heart failure
- Patient education
Patients with heart failure are at a higher risk of cardiovascular events compared with the general population, particularly during domestic or international travel. Patients with heart failure should adhere to specific recommendations during travel to lower their risk of developing heart failure symptoms. In this Review, we aim to provide clinicians with a set of guidelines for patients with heart failure embarking on national or international travel. Considerations when choosing a travel destination include travel distance and time, the season upon arrival, air pollution levels, jet lag and altitude level because all these factors can increase the risk of symptom development in patients with heart failure. In particular, volume depletion is of major concern while travelling given that it can contribute to worsening heart failure symptoms. Pre-travel risk assessment should be performed by a clinician 4–6 weeks before departure, and patients should receive advice on potential travel-related illness and on strategies to prevent volume depletion. Oxygen supplementation might be useful for patients who are very symptomatic. Upon arrival at the destination, potential drug-induced photosensitivity (particularly in tropical destinations) and risks associated with the local cuisine require consideration. Special recommendations are needed for patients with cardiac implantable electronic devices or left ventricular assist devices as well as for those who have undergone major cardiac surgery.
Patients with heart failure (HF) are recommended to schedule a specialist consultation for pre-travel risk assessment 4–6 weeks before departure.
Preparation for travel requires special considerations in patients with HF, including the choice of destination, availability of medical resources and strategies to prevent volume depletion.
Most patients with HF can travel when medically stable; patients with a ground-level oxygen saturation ≤90% or those in NYHA class III–IV might need an on-board medical oxygen supply.
All medication and important documents should be stored in carry-on luggage.
Volume depletion and dehydration are important considerations requiring meticulous attention with regards to medication adjustment and fluid intake.
Patients with implantable cardiac devices might require extra time at security checkpoints and additional documents; for some patients, remote monitoring of implantable cardiac devices might be useful.
Similar content being viewed by others

Diagnosis and management of Guillain–Barré syndrome in ten steps
Sonja E. Leonhard, Melissa R. Mandarakas, … Bart C. Jacobs

Key recommendations for primary care from the 2022 Global Initiative for Asthma (GINA) update
Mark L. Levy, Leonard B. Bacharier, … Helen K. Reddel

Burn injury
Marc G. Jeschke, Margriet E. van Baar, … Sarvesh Logsetty
Introduction
Domestic and international travel are associated with increased health risks, with 20–70% of individuals reporting health issues during their travels 1 . During international travel, 1–5% of individuals seek medical attention and the rate of death among travellers is 1 in 100,000, with cardiovascular disease being the most frequent cause of death 1 . Trauma, particularly from motor vehicle accidents, is another major cause of death while travelling 1 . Health-care providers are frequently approached by patients for advice on how to prepare for travel or to determine whether travelling is advisable at all. General practitioners can provide information to healthy individuals but specialist consultation is of benefit for patients with underlying illnesses such heart failure (HF) 2 . Indeed, many patients with HF intend to travel for business or leisure. Although some guidance has been published 3 , a systematic overview of recommendations for patients with HF planning to travel is not yet available. In this Review, we aim to provide clinicians with recommendations for preparatory measures before travel to inform and educate patients with HF. We discuss factors that might increase the risk of HF symptom development, such as local climate, air pollution levels and altitude levels, and provide specific guidance for patients with a cardiac implantable device and those who have undergone major surgery.
Which patients with HF can travel safely?
To date, guidance on travel recommendations for patients with HF is limited. In general, patients with NYHA class I–III HF who are stable should be able to travel safely 4 . However, patients with NYHA class III HF who are planning to travel by air should be advised to consider on-board medical oxygen support. Patients with NYHA class IV should not travel; however, if travel is unavoidable, on-board oxygen and medical assistance should be requested. A patient with an oxygen saturation rate >90% at ground level usually will not require medical oxygen during flight 5 . An overview of whether travelling is advisable for different classes of HF 6 , 7 is provided in Box 1 . An overview of contraindications for air travel in patients with cardiovascular diseases is provided in Box 2 .
Box 1 Travel recommendations for patients with heart failure
Chronic stable heart failure
NYHA class I–II: travel advisable, if patient is stable
NYHA class III: travel advisable, if patient is stable; consider use of on-board medical oxygen during air travel
NYHA class IV: travel not advisable; if travel is unavoidable, on-board oyxgen and medical assistance are required
Acute heart failure decompensation
Travel not advisable until at least 6 weeks after discharge and rehabilitation, if patient is stable
Ventricular assist device implantation
Travel advisable after hospital discharge and rehabilitation, if patient is stable
Heart transplantation
Not advisable until at least 1 year after transplantation surgery, if patient is stable
Implantable cardioverter–defibrillator or cardiac resynchronization therapy implantation
Not advisable until at least 2 weeks after discharge, if patient is stable
Box 2 Contraindications for air travel in patients with cardiovascular disease
Myocardial infarction (ST-elevation or non-ST-elevation myocardial infarction) within the previous 2 weeks
Unstable angina without further diagnostics and treatment
Percutaneous coronary angioplasty within the previous 2 weeks; in patients who have undergone uncomplicated percutaneous coronary intervention, shorter time frames might be acceptable
Cardiac surgery or interventional valve therapy within the previous 3 weeks
NYHA class IV heart failure or any decompensated heart failure
Untreated arrhythmias (ventricular or supraventricular)
Eisenmenger syndrome
Uncontrolled pulmonary artery hypertension
Pneumothorax (such as after major cardiac surgery)
Choice of destination
The choice of destination for travel can have important health implications for patients with HF, particularly when travelling abroad. Considerations include the local climate, air pollution levels, altitude levels, the season upon arrival, the distance and time for travelling, jet lag, and vaccines required.
Effects of transitioning climates on HF
Individuals who transition through climates different to the one they reside in (such as someone living in the arctic travelling to a tropical island) are at an increased health risk. In general, people living in warmer regions tend to be most vulnerable to cold weather and, conversely, those residing in a cold climate are most sensitive to heat 8 . Exposure to extreme heat has been associated with increased morbidity and mortality from heat exhaustion and heat stroke 9 , 10 . Maintenance of homeostasis during hot weather requires an increase in cardiac output; heat tolerance is impaired when cardiac output cannot be increased to meet the requirements of heat loss. Numerous medications that are frequently prescribed for individuals with HF can also increase susceptibility to heat stroke, including loop diuretics, serotonic antidepressants, angiotensin-converting enzyme inhibitors and proton-pump inhibitors 11 , 12 , 13 . Colder temperatures are less likely to have effects on cardiovascular health but have been associated with increased morbidity among patients with respiratory disease 14 . Patients with HF should be advised to choose either spring or autumn for international travel to avoid travelling during extremities in weather and to adjust medications that can contribute to volume depletion. Appropriate clothing is required for the site of departure, the destination and for the journey itself. Given the challenges in contacting a patient’s primary care physician if the patient is in a different country or continent, distant travel destinations might only be advisable for patients who are well-informed about their medication regimen, dietary restrictions and exercise limitations.
Endemic diseases
The need for immunization for travel depends on the destination. In general, the status of routine vaccinations, such as the diphtheria, measles–mumps–rubella, pertussis, tetanus and varicella vaccines, should be checked before travelling abroad. For all patients with HF, vaccines are required for pneumococcal disease, influenza and coronavirus disease 2019 (COVID-19). Other destination-dependent vaccines are provided in Table 1 .
Air pollution and HF
Air pollution can be measured by the air quality index, which integrates measures for the five main air pollutants: ground-level ozone, particulate matter, carbon monoxide, sulfur dioxide and nitrogen dioxide. An air quality index value of 0–50 indicates good air quality, 51–100 indicates moderately polluted air, >100 indicates an unhealthy level of air pollution and >300 designates a hazardous environment 15 . Particulate matter (PM) of ≤10 µm (PM 10 ) or ≤2.5 µm (PM 2.5 ) in diameter are linked with increased cardiopulmonary mortality 16 , 17 as well as with an increased risk of hospitalization for HF 18 and death 19 . The pathophysiological mechanisms underlying this increased risk remain elusive. Accumulating evidence points towards a crucial role of PM-induced systemic oxidative stress 20 and endothelial dysfunction 21 in the development of arterial vasoconstriction and elevated systemic blood pressure 22 . In addition, PM-induced pulmonary vasoconstriction results from increases in pulmonary and right ventricular diastolic filling pressures, which affect right ventricular performance 22 . Given that the effects of air pollutants on cardiovascular performance and outcomes can occur within hours or days of exposure 23 , patients with HF should be advised to avoid travelling to locations with high levels of air pollution.
Altitude-induced hypoxia and HF
Patients with HF are more susceptible to the physiological changes induced by high altitude exposure than the general population 24 . During air travel, cabin pressure is required to be no less than the barometric pressure at an altitude of 2,438 m (8,000 ft), which is classified as an intermediate altitude 25 (Fig. 1a ). Cabin pressures usually remain higher than this altitude, particularly during long-haul flights 26 . Travel to high altitude locations that are >2,500 m above sea level triggers physiological acclimatization processes within the cardiocirculatory and pulmonary systems 27 , 28 (Fig. 1b ). These processes are initiated by a gradual decrease in barometric pressure, which in turn lowers the partial pressure of oxygen in inspired air. Hypobaric hypoxia leads to a fast increase in respiratory rate and tidal volume 29 , which leads to respiratory alkalosis and hypoxic diuresis 30 . Hypoxia induces pulmonary vasoconstriction and eventual pulmonary hypertension, an important trigger for high altitude pulmonary oedema 31 . To compensate for the lower arterial oxygen content, heart rate and stroke volume are increased via activation of the sympathetic nervous system 26 , 32 , 33 , 34 . Together, these physiological adaptations limit the exercise capacity of patients with HF and make them prone to cardiac decompensation. However, studies that assessed simulated altitude-induced hypoxia in patients with NYHA class III–IV HF showed that high altitude was not associated with angina, arrhythmia, or ischaemia 35 , 36 and that the degree of the reduction of maximum work capacity was dependent on the individual’s exercise tolerance at sea level 35 . The ESC and other professional societies recommend that the assessment of safety of high altitude exposure for patients with HF should depend on their functional capacity (that is, NYHA class) at sea level 35 , 37 . Furthermore, certain drugs that are prescribed to patients with HF can further interfere with the physiological adaptation processes at high altitudes. For example, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers can reduce renal erythropoietin production, thereby hampering the compensatory rise in haematocrit mediated by altitude-induced hypoxia 38 . Therefore, diuretic therapy should be tailored to the individual to account for clinical signs of dehydration (such as through hypoxic diuresis) or fluid gain 39 . Finally, anaemia reduces oxygen delivery, and muscle loss (present in patients with sarcopenia or cachexia) reduces maximal physical workload and time to fatigue; patients with these conditions in addition to HF need to have special considerations when planning to travel to high altitude locations. To summarize, travel to destinations at an intermediate altitude (~2,000 m) is safe for patients with HF who have good exercise tolerance at sea level.
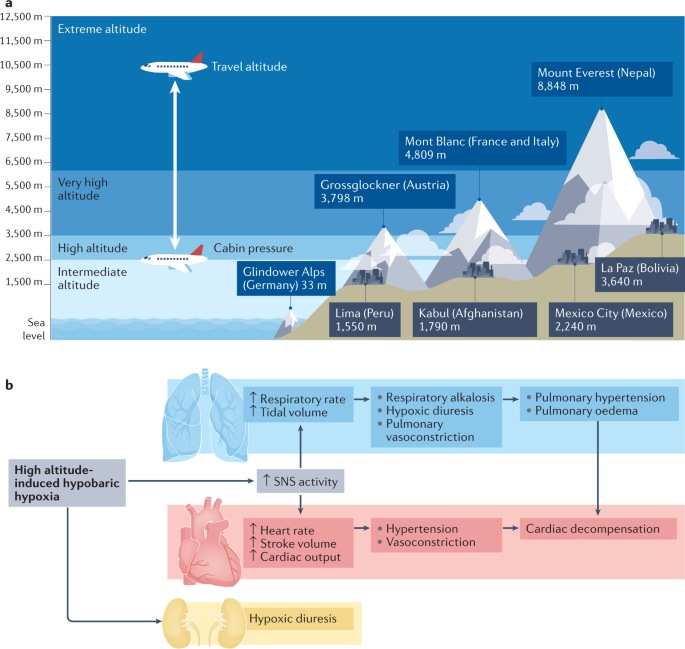
a | Definitions of height and examples of mountains and cities at different altitudes. Most aircraft fly at approximately 10,000–12,000 m (33,000–42,000 ft) above sea level, with the cabin pressurized to an equivalent of 2,438 m (8,000 ft). b | High altitude-induced hypobaric hypoxia leads to an increase in respiratory rate and tidal volume, which promotes respiratory alkalosis, hypoxic diuresis, pulmonary vasoconstriction and, ultimately, pulmonary hypertension and pulmonary oedema. Compensatory mechanisms of this hypoxia include increases in heart rate and stroke volume via activation of the sympathetic nervous system (SNS). Together, these changes can limit exercise capacity and promote cardiac decompensation.
Seasonal variations and HF
Hospitalizations owing to worsening HF show intriguing seasonality, with a substantial decline during warmer periods and an increase during colder periods 18 , 40 , especially in older patients 41 . Temperature had the greatest (inverse) correlation with hospitalizations for HF among other causative environmental factors such as humidity, precipitation or irradiation 16 . Skin cooling has been shown to increase vascular resistance 42 and plasma noradrenaline concentration 43 , which might lead to HF decompensation. Beyond neurohumoural activation and haemodynamic stress, respiratory infections, which peak during the colder months, can precipitate and aggravate HF symptoms 41 . Furthermore, vitamin D insufficiency during winter has also been linked to worsening HF 44 . Interestingly, the effect of seasonal variability on health is more prominent in elderly people and winter hospitalization is associated with both poorer short-term and long-term prognosis 41 . These observations suggest that patients with more severe HF (and worse prognosis) are prone to decompensation during winter and that these patients and older patients with more advanced disease should be advised to avoid travelling to colder regions. Of note, a study from Norway reported that the Christmas winter period was associated with the highest rates of excess all-cause and cardiovascular deaths 45 . Overall, appropriate clothing and heating strategies need to be carefully selected for optimal stabilization of body core temperatures, vitamin D levels should be measured before departure and supplemented if required, and vaccines against influenza and pneunococcal disease should be administered 40 (Table 1 ).
Preparing to travel
Any patient with a history of HF should seek medical consultation before departure, particularly when travelling overseas or when leaving for a long period. Women are generally more likely to seek pre-travel medical advice than men 46 and are also more likely to have travel-related worries 47 . A cross-sectional national survey found that a low perceived need was among the main causes for avoiding medical care, often because patients expected their illness or symptoms to improve over time 48 . For patients with HF, travel preparation should include a specialist consultation approximately 4–6 weeks before departure. This consultation should follow a structured and sequenced approach, which should involve risk assessment (including an evaluation of medical history and travel itinerary), interventions required before departure (including physical examination or setting up of remote monitoring for cardiac implantable devices) and focused education on topics such as medications and factors that can lead to volume depletion. For example, the presence of anaemia might cause lightheadedness, angina or loss of consciousness, particularly during flights 49 , 50 . Medication regimens should be optimized before departure and patients with iron deficiency should be considered for repletion therapy. Suggestions for topics to cover during this consultation are summarized in Box 3 .
Box 3 Recommendations for pre-travel assessment
Risk assessment
Full medical history (current medications, immunization history, history of surgeries or device implantation, immune status, allergies, pregnancy or breast feeding)
Previous travel experience (particularly to the same destination) or risk tolerance
Travel itinerary (destination, mode of travel, travel distance, season, air pollution levels, potential jet lag, clothing required and altitude)
Activities planned (such as adventure sports or hiking, mass gatherings)
Type of accommodation
In-office interventions
Physical examination, electrocardiogram tracing, biochemistry analysis (plasma levels of creatinine, ferritin, glucose, glycated haemoglobin, N-terminal pro-B-type natriuretic peptide, potassium, sodium, transferrin saturation, thyroid-stimulating hormone, vitamin D and urea, estimated glomerular filtration rate, and lipid profile and liver function tests), full blood count (to identify potential anaemia), exercise test and/or transthoracic echocardiography
Set up remote monitoring of implanted devices
Administration of immunizations (routine vaccines include measles–mumps–rubella, tetanus–diphtheria–pertussis, coronavirus disease 2019 (COVID-19), pneumococcal disease and influenza as well as any destination-specific vaccine that might be needed for diseases such as hepatitis A or yellow fever) or malaria chemoprophylaxis (if required)
Strategies to prevent or treat traveller’s diarrhoea (food and water precautions, oral rehydration, treatment with loperamide and bismuth subsalicylate, and antibiotic self-treatment options for severe diarrhoea)
Focused education before travel
Medical kit and documents required during travel: personal health kit (medication, device information or medical records), evacuation and health insurance
Location of medical facilities at destination
Education on heart failure medication adjustment (to avoid dehydration and volume overload), cardiac device handling, telemonitoring and factors that contribute to volume depletion (excess alcohol, coffee or salt intake; traveller’s diarrhoea)
Patients with a cardiac implanted device should avoid strong electromagnetic fields
Travel-related illnesses: altitude illness, traveller’s thrombosis, bloodborne and sexually transmitted diseases, transportation-associated illnesses, respiratory infections, rabies and other animal-associated illness, and skin conditions and wounds
Personal protection for vector-borne disease (if at risk)
Risk assessment and medication adjustment
As mentioned in the previous section, pre-travel risk assessment should consider the type and duration of travel, the travel destination, and the medical history of the patient. Typical health emergencies that patients with HF might encounter during travel are listed in Table 2 . Patients should be advised that provision of incomplete medical information during a cardiac emergency might increase the risk of death. Any accompanying travellers need to know where to find important documents (Box 4 ) in case of an emergency. Given the difficulty in obtaining prescription drugs in a different country as well as the different brands of drugs having varying strengths in different countries, extra medication should be brought on the trip. Importantly, some over-the-counter drugs might be legal in the patient’s home country but illegal elsewhere (such as certain analgesics).
Box 4 Medication and documents required during travel
Sufficient medication for the whole journey (consider bringing extra drugs in case of unforeseen delays in returning home)
Medication to be kept in carry-on luggage for flights (in case of loss of luggage or emergency)
Photocopy of last prescription
Insurance card
Patient identification card
List of diagnosed health conditions and prescribed medicines
Last discharge letter from hospital
Device interrogation print-out
List of names and phone numbers of cardiologist and other relevant clinicians
Remote device monitoring
Remote monitoring is recommended by the ESC and other professional societies for patients with cardiac implantable devices such as pacemakers, implantable cardioverter–defibrillators (ICDs) and implantable cardiac monitors 51 , 52 , 53 . Most remote monitoring systems use a transmitter (base station) placed in the vicinity of the implanted device, with information sent via an internet connection to a remote monitoring service. Alternatively, alerts can be activated after events that trigger an immediate remote transmission (for example, after ICD shock, detection of ventricular tachyarrhythmias or signs of lead failure). Given that travelling is usually associated with increased physical activity levels, daily remote monitoring might be useful for the detection of events such as arrhythmias, HF decompensation or device malfunction (Box 5 ).
Box 5 Travel-related activities and related cardiac events reported via remote monitoring
Sports (such as swimming and diving)
Arrhythmias (atrial fibrillation, ventricular tachyarrhythmia or premature ventricular contractions)
Heart failure decompensation
Damage to the implanted cardiac lead (fracture or insulation failure)
Cardiac device compression with loss of function (during diving)
Stay in high altitude
Eating out (higher intake of sodium) and alcohol consumption
Reduced adherence to medication
Arrhythmias
Travel by aircraft
Electromagnetic interference with cardiac electronic device
Travel by train or ship
Special considerations
Patients who have undergone recent surgery.
Major cardiac surgery ranges from minimally invasive approaches to complete sternotomy. The Canadian Cardiac Society guidelines on air travel recommend that patients with a haemoglobin level <9 g/dl who have undergone coronary artery bypass graft surgery should be advised against air travel 54 ; recommendations for travel in patients with HF who have undergone coronary artery bypass graft surgery should perhaps be even more conservative. These patients should be advised not to travel by air until intrathoracic gas resorption is completed given that gas expands when air pressure is reduced with increasing altitude (the Boyle law) 4 . Gas resorption usually takes 3–10 days after surgery. Any air remaining in the pericardial space or in the thoracic cavity can expand by up to 60%, which might be dangerous and painful 4 . Indeed, the Aerospace Medical Association guidelines state that pneumothorax is an absolute contraindication to air travel and advocate an interval of 2–3 weeks before flying after thoracic surgery 5 . Furthermore, patients who have had a recent operation are in a state of increased oxygen consumption owing to the trauma of surgery, possible presence of sepsis and increased adrenergic outflow. A 2017 study compared complication rates between ground and air travel 5–25 days after pulmonary resection 55 . Air travel was as safe as ground travel if the chest tubes were removed after the absence of ongoing air leak and an output <300 ml over 24 hours combined with adequate pain medication and an active ambulation schedule.
Patients with LVADs
Left ventricular assist devices (LVADs) are increasingly implanted as a bridging strategy while patients wait for heart transplantation or as a permanent therapy for end-stage HF. Patients in either category can travel by air if medically stable and rehabilitation measures have been performed 56 . Box 6 lists precautions before and during travel for patients with an LVAD.
Box 6 Considerations before and during travel for patients with an LVAD
Considerations before departure
Approval should be sought from the responsible left ventricular assist devices (LVAD) centre, including an airline information letter (templates from LVAD manufacturer)
Closest LVAD centres within the travel destination should be located as possible emergency contacts
All LVAD-related equipment needs to be stored in carry-on luggage with handling advice and emergency contact information attached and batteries should be fully charged before departure
The size and weight of the equipment should be checked to ensure that it can be carried on board the plane and the airport and airline need to be informed about the LVAD before arrival to the airport
Considerations during travel
Flight attendants and other personnel need to be informed about the LVAD and the location of the emergency information card
Patients need to maintain fluid intake to avoid low flow alarms from the LVAD pump
For flights longer than 2 hours, support stockings should be considered
Considerations while en route
Departure from home.
Patients with HF or ischaemic heart disease need to take extra caution on the way to and from the departure point, such as an airport or train station, given the multitude of stressors: commotion, a delay or any last-minute changes to the train or flight, and lifting of heavy luggage, all of which can increase physical and mental exertion and risk of myocardial ischaemia 57 , 58 . As such, travel planning should include estimation of psychological stressors and physical loads as well as a plan for any emergencies (Table 2 ). Pre-planned assistance with luggage or transport by wheelchair at the point of departure might reduce pre-travel stress and physical exhaustion.
Dehydration and fluid intake
Patients with HF are susceptible to volume depletion during travel given that fluid intake, lifestyle and diuretics are tuned precisely to maintain a state of euvolaemia 59 (Fig. 2 ). A hypovolaemic state adversely affects cardiac and renal function, aggravates HF symptoms, and might interfere with the efficacy of HF medications. Fluid loss, caused by changes in temperature, diet (higher salt intake) or as a consequence of traveller’s diarrhoea, might occur during the flight.
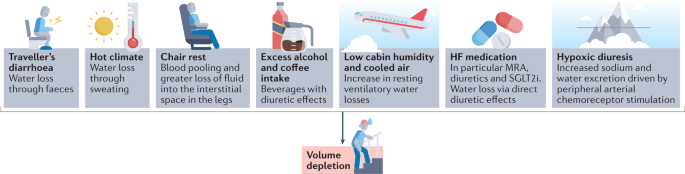
A vast array of factors contributes to volume depletion in patients with heart failure (HF) and require medication adjustment and increased fluid intake. MRA, mineralocorticoid receptor antagonists; SGLT2i, sodium–glucose cotransporter 2 inhibitor.
On board a plane, the low cabin humidity and cooled air can increase resting ventilatory water losses by approximately 200 ml per hour 60 . In addition, chair rest immobilization for 4 hours can decrease plasma volume by approximately 6% as a result of blood pooling and greater loss of fluid within the interstitial space in the legs 60 . Urinary output is often normal or only slightly reduced 61 . Sodium-free, alcoholic or caffeine-containing drinks consumed during the flight can promote diuresis and might further increase fluid loss. Furthermore, arrival to a hot and dry climate can result in loss of fluid through sweating and breathing by up to 1.2 l per day independently of physical activity 62 .
Apart from air travel and a transition in climate, acute diarrhoea is the most common illness in individuals travelling from resource-rich to resource-limited regions of the world 63 , 64 . Traveller’s diarrhoea usually occurs 4–14 days after arrival and results from bacterial (>90% of cases), viral and parasitic infections 64 . Approximately 10–40% of travellers to high-risk regions in Asia, Africa, and South and Central America experience diarrhoea during their travels 64 . Patients should be educated on food and water safety to prevent ingestion of pathogens. Cardiac dysfunction and HF management and treatment strategies, such as fluid restriction, diuretic therapy and renin–angiotensin–aldosterone system (RAAS) inhibitors, also increase the risk of diarrhoea-related complications in patients with HF during (temporal) hypovolaemia 63 , 64 .
Signs and symptoms of volume depletion and dehydration-associated electrolyte or acid–base disorders include fatigue, exercise intolerance, weight loss, increase in heart rate, muscle cramps, weakness, postural dizziness, abdominal pain, low urine volume, low blood pressure, lethargy and confusion. On the basis of invidualized risk assessment, patients should be advised to increase fluid intake by 0.5–1 l per day and to avoid alcohol or excessive coffee consumption during long-haul flights and hot weather. In case of signs and symptoms of volume depletion, therapy with diuretics, mineralocorticoid receptor antagonists and sodium–glucose cotransporter 2 inhibitors should be stopped or reduced for a day or longer until symptoms have resolved and body weight has returned to normal 65 . In case of postural or symptomatic hypotension, therapy with RAAS inhibitors and angiotensin receptor blocker–neprilysin inhibitors should be reduced or discontinued until symptoms have resolved; patients who experience postural or symptomatic hypotension require medical evaluation.
In a hot environment, patients with HF are advised to restrain from strenuous activity to avoid increased fluid loss. In case of uncomplicated traveller’s diarrhoea, patients need to increase fluid intake with oral rehydration solutions and monitor body weight and urinary output to avoid dehydration. Given that patients with HF are at an increased risk of complications, an antimotility agent (loperamide) and an antibiotic (azithromycin or rifaximin) can be prescribed for self-treatment 63 , 64 .
Venous thromboembolism
The risk of deep venous thrombosis (DVT) is greatly increased in patients with incident HF according to data from the ARIC cohort 66 and a systematic review 67 . The term ‘economy class syndrome’ has been used to describe the venous complications caused by cramped seating conditions 68 . The risk of DVT or pulmonary embolism is increased during travel that is >4 hours in duration, most probably owing to the associated immobility that is a key component of the Virchow triad of hypercoagulability, stasis and endothelial injury. Travelling in general (>4 hours in the preceding 8 weeks) is associated with a twofold increase in the risk of venous thrombosis 69 . This risk seems to be similar regardless of the mode of transportation (airplane, bus or train) 67 . The overall absolute incidence of symptomatic venous thromboembolism (VTE) in healthy individuals within the first month after a flight lasting >4 hours is approximately 1 in 4,600 flights and increases by 18% for each additional 2 hours in flight duration 2 , 70 . Importantly, the risk of VTE in individuals with pro-thrombotic risk factors, such as chronic HF, is substantially higher than in the general population. A 2021 meta-analysis found that patients with chronic HF were at an increased risk of VTE (risk ratio 1.57, 95% CI 1.34–1.84) 71 . A window seat compared with an aisle seat has been associated with a twofold greater risk of VTE or a sixfold greater risk in individuals with a BMI of >30 kg/m 2 (ref. 72 ).
Strategies to prevent VTE include appropriate loose clothing, frequent walks, calf muscle exercises, use of elastic compression stockings and adequate hydration 73 . Leg exercises have been shown to improve popliteal venous flow during prolonged immobility in seated individuals 74 . Furthermore, a systematic review of 11 randomized trials that included 2,906 individuals revealed the benefits of compression stockings (15–30 mmHg) on reducing the incidence of asymptomatic DVT and, with less evidence, of leg oedema 75 .
The evidence for thromboprophylaxis to prevent VTE during travel is very limited. The LONFLIT-3 study 76 randomly assigned 300 individuals at high risk of flight-related VTE to receive aspirin, enoxaparine (a low-molecular-weight heparin) or no prophylaxis. In total, 4.8% of patients in the control group were diagnosed with asymptomatic DVT compared with 3.6% in the aspirin group and 0% in the enoxaparine group. The authors of this small study concluded that one dose of enoxaparine might be an important option for individuals at high risk of DVT during long-haul flights 76 . Of note, specific studies of thromboprophylaxis during long-haul travel in patients with HF are lacking.
Medical emergencies during air travel
Patients with HF can travel by air if their condition is stable (Box 1 ). Commercial airplanes are required to carry basic emergency medical equipment according to regulations of the Federal Aviation Administration (FAA) in the USA and the European Aviation Safety Agency (EASA) in Europe 77 . Commercial aircrafts travelling from Europe to the USA have to meet both FAA and EASA requirements and, thus, must carry on board an external automated defibrillator, a saline infusion system and a bag-valve mask resuscitator 77 .
Data on on-board medical emergencies are sparse owing to the lack of international registries 78 . According to the available data provided by the airline Lufthansa, which contains details on approximately 20,000 on-board medical events from 2000 to 2011, cardiac emergencies accounted for 43% of on-board incidents 77 . Reported medical issues included circulatory collapse, high blood pressure, chest symptoms and dehydration 47 . On-board treatment included blood pressure management in 76% of incidents, drug administration in 54%, oxygen delivery in 48%, blood glucose measurement in 9%, monitoring of oxygen saturation in 6% and use of an automated external defibrillator in 6% 77 .
Considerations at the destination
Dietary considerations.
Dietary intake of fluids, sodium, potassium and alcohol during travel should be guided by current ESC recommendations for the management of patients with HF 3 , 79 . According to the guidelines, fluid restriction of 1.5–2.0 l per day might be considered in patients with severe HF to relieve symptoms and congestion 80 . When travelling to hot and dry destinations, an additional intake of 0.5–1.0 l per day of non-alcoholic drinks is recommended. Patients at risk of volume overload or on moderate-to-high doses of diuretics should be advised to regularly check their body weight. In case of body weight changes, patients can adjust doses of diuretics and the amount of fluid intake for a few days until body weight has normalized. Controlling sodium intake is important for patients at risk of hyponatraemia and for the management of oedema, although evidence showing the effects of sodium intake on HF outcomes is scarce 3 . During travel, increased consumption of foods high in salt can adversely affect sodium and volume balance and thereby exacerbate HF symptoms by causing fluid retention. Patients with HF and cardiorenal syndrome and/or treated with RAAS inhibitors are at increased risk of hyperkalaemia 81 . In patients with advanced chronic kidney disease (estimated glomerular filtration rate <30 ml/min/1.73 m²), a daily sodium intake of <3 g is recommended 81 . These patients should also be aware that certain foods, such as fresh fruits, juices, vegetables and milk products, contain high amounts of potassium.
Drinking habits also change during vacation. Moderate-to-heavy alcohol consumption is associated with increased risk of supraventricular arrhythmias, especially atrial fibrillation, and high blood pressure 82 , 83 . Therefore, increased intake of alcoholic beverages might aggravate HF symptoms and promote volume overload. Alcohol intake should be limited to two units per day for men with HF, one unit for women with HF, or no intake if alcohol has caused or contributed to the individual’s HF, as recommended by the ESC 3 .
Drug-induced photosensitivity
Numerous classes of drugs commonly used for the treatment of patients with HF have been associated with photo-induced, cutaneous drug eruptions, which are adverse effects that occur as a result of the exposure to a drug (and its presence in the skin) and ultraviolet or visible radiation 84 . Box 7 provides an overview of drugs that have been linked with drug-induced photosensitivity. Amiodarone can cause drug-induced photosensitivity in >50% of treated patients 84 . The typical presentation of this adverse effect is a burning and tingling sensation in sun-exposed skin, with associated erythema. Amiodarone induces a distinctive blue–grey pigmentation on sun-exposed sites in 1–2% of patients, particularly after long-term sun exposure. Another prototypical drug class associated with photosensitivity is thiazide diuretics, which includes hydrochlorothiazide 85 . Thiazide diuretics can trigger a variety of photosensitive eruptions, including an exaggerated sunburn reaction, dermatitis and a lichenoid eruption.
Various factors, such as time of day, season, geographical location, altitude and weather conditions, can affect the amount of ultraviolet radiation exposure 86 . In general, patients with HF should be advised to seek shade when outside, in particular around midday, and to keep in mind that radiation can be stronger when reflected by water, sand or snow. Patients in areas with high sun exposure should wear clothing that protects as much of the body as possible as well as sunglasses and broad-brimmed hats. Broad-spectrum sunscreens with a sun protection factor of 30 or higher are recommended 86 .
Box 7 Medications linked to drug-induced photosensitivity 80
Angiotensin-converting enzyme inhibitors
Ramipril, enalapril and quinapril
Angiotensin receptor blockers
Candesartan, irbesartan, losartan, olmesartan, telmisartan and valsartan
Anti-arrhythmic drugs
Amiodarone and dronedarone
Anti-depressant drugs
Citalopram, clomipramine, escitalopram, fluoxetine, fluvoxamine, imipramine, paroxetine, sertraline, St. John’s wort and venlafaxine
Antimicrobial drugs
Anti-fungals, anti-malarials, anti-tuberculous drugs, anti-retrovirals, β-lactams, fluoroquinolones, nalidixic acid, sulphonamides and tetracyclines
Calcium channel blockers
Amlodipine, diltiazem and nifedipine
Bumetanide, furosemide, indapamide, thiazides and triamterene
3-Hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors
Atorvastatin, pravastatin and simvastatin
Non-steroidal anti-inflammatory drugs
Ampiroxicam, celecoxib, diclofenac, ibuprofen, indomethacin, ketoprofen, meclofenamide, nabumetone, naproxen, oxaprozin, piroxicam, sulindac and tiaprofenic acid
Psychotropic drugs
Anti-psychotic drugs (aripriprazole, chlorpromazine, clozanine, flupenthixol, haloperidol, olanzapine, risperidone and thioridazine) and anxiolytics (alprazolam and chlordiazepoxide)
Considerations for drivers
Driving regulations for individuals with HF take into account the severity of HF (NYHA class plus left ventricular ejection fraction) 54 . In the European Union, individuals with NYHA class I–III HF but not those with NYHA class IV HF are permitted to drive private vehicles. Patients with HF should ensure that they are permitted to drive in their travelling destination by accessing country-specific driving regulations online.
Considerations for patients with ICDs
Electromagnetic interference.
Many patients with HF are fitted with cardiac implantable electronic devices (CIEDs; namely ICDs), cardiac resynchronization therapy devices or pacemakers. These devices might be subject to electromagnetic interference (EMI) if exposed to a strong electromagnetic field (Table 3 ). Exposure of the device to EMI can result in device failure (loss of anti-bradycardia pacing with the risk of asystole), switch to asynchronous mode (pacing at a preset rate independent of intrinsic rhythm with the risk of inducing arrhythmias, including ventricular fibrillation), inappropriate tracking (atrial oversensing leading to rapid, irregular ventricular pacing) and in the inappropriate detection of ventricular tachyarrhythmias by ICDs, potentially with inappropriate shock therapy. High-voltage lines above trains, for example, have a strong electromagnetic field but the patient is shielded when inside the train. In trams or underground trains, electric motors can be located under the seat, whereas in cars and motorbikes, the only relevant source of EMI is the ignition system. Patients with a cardiac implantable device should be careful not lean over an unshielded, running motor.
Metal detectors at airport security checkpoints do not interfere with CIEDs 87 , 88 . However, patients with ICDs should be advised to have their device card ready to show to airport personnel before walking through the security checkpoint. To minimize the risk of interference, patients should move through metal detector gates at normal walking speed and should not linger. Hand-held scanners should not affect CIED functionality 89 but patients should ask personnel to move the wand over the device quickly and only once.
Magnets are not allowed in carry-on luggage and thus cannot be used to remedy inappropriate device activity on airplanes. EMI inside airplanes is rare but has been reported, for example, in association with electronic chair handles. Finally, cosmic radiation is approximately 100-fold higher during air travel, which increases the risk of radiation-induced EMI (for example, power-on reset).
Conclusions
The list of considerations for patients with HF embarking on national or international travel is extensive. Patients should be aware of an increased risk of cardiovascular events during their travels, which can be reduced with meticulous pre-travel risk assessment, physical examination, therapy adjustment and education. Pre-travel risk assessment should involve research into the local climate, air pollution levels, the distance and time for travelling, potential jet lag and altitude. En route, patients with HF should avoid volume depletion caused by extended chair rest, low cabin humidity and cooled air, excess alcohol or coffee intake, drugs with diuretic effects, hypoxia or traveller’s diarrhoea. Upon arrival at the destination, drug-induced photosensitivity and the health effects of local foods and beverages require consideration. Special recommendations are needed for patients after implantation of cardiac rhythm devices or LVADs as well as for patients who have undergone major cardiac surgery.
Ryan, E. T. & Kain, K. C. Health advice and immunizations for travelers. N. Engl. J. Med. 342 , 1716–1725 (2000).
Article CAS PubMed Google Scholar
Freedman, D. O., Chen, L. H. & Kozarsky, P. E. Medical considerations before international travel. N. Engl. J. Med. 375 , 247–260 (2016).
Article PubMed Google Scholar
Jaarsma, T. et al. Self-care of heart failure patients: practical management recommendations from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 23 , 157–174 (2021).
Smith, D. et al. Fitness to fly for passengers with cardiovascular disease. Heart 96 (Suppl. 2), ii1–ii16 (2010).
PubMed Google Scholar
Aerospace Medical Association. Medical considerations for airline travel: surgical conditions (ASMA, 2021).
Dharmarajan, K. et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: retrospective cohort study. BMJ 350 , h411 (2015).
Article PubMed PubMed Central Google Scholar
Alba, C. et al. Complications after heart transplantation: hope for the best, but prepare for the worst. Int. J. Transpl. Res. Med. 2 , 022 (2016).
Article Google Scholar
Curriero, F. C. et al. Temperature and mortality in 11 cities of the eastern United States. Am. J. Epidemiol. 155 , 80–87 (2002).
De Blois, J. et al. The effects of climate change on cardiac health. Cardiology 131 , 209–217 (2015).
Kenny, G. P., Yardley, J., Brown, C., Sigal, R. J. & Jay, O. Heat stress in older individuals and patients with common chronic diseases. CMAJ 182 , 1053–1060 (2010).
Bouchama, A. & Knochel, J. P. Heat stroke. N. Engl. J. Med. 346 , 1978–1988 (2002).
Faunt, J. D. et al. The effete in the heat: heat-related hospital presentations during a ten day heat wave. Aust. N. Z. J. Med. 25 , 117–121 (1995).
Sommet, A., Durrieu, G., Lapeyre-Mestre, M., Montastruc, J. L. & Association of French PharmacoVigilance Centres. A comparative study of adverse drug reactions during two heat waves that occurred in France in 2003 and 2006. Pharmacoepidemiol. Drug Saf. 21 , 285–288 (2012).
McCormack, M. C. et al. Colder temperature is associated with increased COPD morbidity. Eur. Respir. J. 49 , 1601501 (2017).
AirNow. Air Quality Index (AQI) basics. AirNow https://airnow.gov/index.cfm?action=aqibasics.aqi (2019).
Miller, K. A. et al. Long-term exposure to air pollution and incidence of cardiovascular events in women. N. Engl. J. Med. 356 , 447–458 (2007).
Pope, C. A. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 287 , 1132–1141 (2002).
Article CAS PubMed PubMed Central Google Scholar
Escolar, V. et al. Impact of environmental factors on heart failure decompensations. ESC Heart Fail. 6 , 1226–1232 (2019).
Shah, A. S. et al. Global association of air pollution and heart failure: a systematic review and meta-analysis. Lancet 382 , 1039–1048 (2013).
Barregard, L. et al. Experimental exposure to wood-smoke particles in healthy humans: effects on markers of inflammation, coagulation, and lipid peroxidation. Inhal. Toxicol. 18 , 845–853 (2006).
Törnqvist, H. et al. Persistent endothelial dysfunction in humans after diesel exhaust inhalation. Am. J. Respir. Crit. Care Med. 176 , 395–400 (2007).
Wold, L. E. et al. Cardiovascular remodeling in response to long-term exposure to fine particulate matter air pollution. Circ. Heart Fail. 5 , 452–461 (2012).
Tofler, G. H. & Muller, J. E. Triggering of acute cardiovascular disease and potential preventive strategies. Circulation 114 , 1863–1872 (2006).
Higgins, J. P., Tuttle, T. & Higgins, J. A. Altitude and the heart: is going high safe for your cardiac patient? Am. Heart J. 159 , 25–32 (2010).
US Office of the Federal Register. Code of Federal Regulations: Title 14 aeronautics and space, part 25.841 (US Government Printing Office, 1986).
Seccombe, L. M. & Peters, M. J. Physiology in medicine: acute altitude exposure in patients with pulmonary and cardiovascular disease. J. Appl. Physiol. 116 , 478–485 (2014).
Imray, C., Booth, A., Wright, A. & Bradwell, A. Acute altitude illnesses. BMJ 343 , d4943 (2011).
Bärtsch, P. & Gibbs, J. S. Effect of altitude on the heart and the lungs. Circulation 116 , 2191–2202 (2007).
Jones, J. G., Bakewell, S. E., Heneghan, C. P., Jones, S. E. & Snape, S. L. Profound hypoxemia in pulmonary patients in airline-equivalent hypoxia: roles of VA/Q and shunt. Aviat. Space Env. Med. 79 , 81–86 (2008).
Sawka, M. N., Convertino, V. A., Eichner, E. R., Schnieder, S. M. & Young, A. J. Blood volume: importance and adaptations to exercise training, environmental stresses, and trauma/sickness. Med. Sci. Sports Exerc. 32 , 332–348 (2000).
Cheung, S. S. et al. Ventilatory chemosensitivity, cerebral and muscle oxygenation, and total hemoglobin mass before and after a 72-day mt. Everest expedition. High Alt. Med. Biol. 15 , 331–340 (2014).
Hughson, R. L., Yamamoto, Y., McCullough, R. E., Sutton, J. R. & Reeves, J. T. Sympathetic and parasympathetic indicators of heart rate control at altitude studied by spectral analysis. J. Appl. Physiol. 77 , 2537–2542 (1994).
Vogel, J. A. & Harris, C. W. Cardiopulmonary responses of resting man during early exposure to high altitude. J. Appl. Physiol. 22 , 1124–1128 (1967).
Heistad, D. D., Abboud, F. M. & Dickinson, W. Richards Lecture: circulatory adjustments to hypoxia. Circulation 61 , 463–470 (1980).
Agostoni, P. et al. Effects of simulated altitude-induced hypoxia on exercise capacity in patients with chronic heart failure. Am. J. Med. 109 , 450–455 (2000).
Negrao, C. E. & Middlekauff, H. R. Adaptations in autonomic function during exercise training in heart failure. Heart Fail. Rev. 13 , 51–60 (2008).
Parati, G. et al. Clinical recommendations for high altitude exposure of individuals with pre-existing cardiovascular conditions: a joint statement by the European Society of Cardiology, the Council on Hypertension of the European Society of Cardiology, the European Society of Hypertension, the International Society of Mountain Medicine, the Italian Society of Hypertension and the Italian Society of Mountain Medicine. Eur. Heart J. 39 , 1546–1554 (2018).
Pratt, M. C. et al. Effect of angiotensin converting enzyme inhibitors on erythropoietin concentrations in healthy volunteers. Br. J. Clin. Pharmacol. 34 , 363–365 (1992).
Swenson, E. R. Carbonic anhydrase inhibitors and high altitude illnesses. Subcell. Biochem. 75 , 361–386 (2014).
Stewart, S., Keates, A. K., Redfern, A. & McMurray, J. J. V. Seasonal variations in cardiovascular disease. Nat. Rev. Cardiol. 14 , 654–664 (2017).
Stewart, S., McIntyre, K., Capewell, S. & McMurray, J. J. Heart failure in a cold climate. Seasonal variation in heart failure-related morbidity and mortality. J. Am. Coll. Cardiol. 39 , 760–766 (2002).
Hayward, J. M., Holmes, W. F. & Gooden, B. A. Cardiovascular responses in man to a stream of cold air. Cardiovasc. Res. 10 , 691–696 (1976).
Westheim, A. et al. Haemodynamic and neurohumoral effects of cold pressor test in severe heart failure. Clin. Physiol. 12 , 95–106 (1992).
Barnett, A. G., de Looper, M. & Fraser, J. F. The seasonality in heart failure deaths and total cardiovascular deaths. Aust. N. Z. J. Public Health 32 , 408–413 (2008).
Moholdt, T. Excess mortality at Christmas due to cardiovascular disease in the HUNT study prospective population-based cohort in Norway. BMC Public Health 21 , 549 (2021).
Schlagenhauf, P. et al. Sex and gender differences in travel-associated disease. Clin. Infect. Dis. 50 , 826–832 (2010).
McIntosh, I. B., Power, K. G. & Reed, J. M. Prevalence, intensity, and sex differences in travel related stressors. J. Travel Med. 3 , 96–102 (1996).
Taber, J. M., Leyva, B. & Persoskie, A. Why do people avoid medical care? A qualitative study using national data. J. Gen. Intern. Med. 30 , 290–297 (2015).
Aerospace Medical Association. Medical considerations for airline travel: anemia (ASMA, 2021).
Roig, E. et al. Disabling angina pectoris with normal coronary arteries in patients undergoing long-term hemodialysis. Am. J. Med. 71 , 431–434 (1981).
Brignole, M. et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur. Heart J. 34 , 2281–2329 (2013).
Dubner, S. et al. ISHNE/EHRA expert consensus on remote monitoring of cardiovascular implantable electronic devices (CIEDs). Ann. Noninvasive Electrocardiol. 17 , 36–56 (2012).
Slotwiner, D. et al. HRS Expert Consensus Statement on remote interrogation and monitoring for cardiovascular implantable electronic devices. Heart Rhythm 12 , e69–e100 (2015).
Simpson, C. et al. Canadian cardiovascular society consensus conference. Assessment of the cardiac patient for fitness to drive and fly – executive summary. Can. J. Cardiol. 20 , 1313–1323 (2004).
Google Scholar
Cassivi, S. D. et al. Safety of air travel in the immediate postoperative period after anatomic pulmonary resection. J. Thorac. Cardiovasc. Surg. 153 , 1191–1196.e1 (2017).
MyLVAD Foundation. 10 Tips for traveling with an LVAD. MyLVAD https://www.mylvad.com/patients-caregivers/discuss-connect/forums/1048-10-tips-traveling-lvad (2011).
Kupper, N., Denollet, J., Widdershoven, J. & Kop, W. J. Cardiovascular reactivity to mental stress and mortality in patients with heart failure. JACC Heart Fail. 3 , 373–382 (2015).
Strike, P. C. & Steptoe, A. A systematic review of mental stress-induced myocardial ischaemia. Eur. Heart J. 24 , 690e703 (2003).
Mullens, W. et al. The use of diuretics in heart failure with congestion - a position statement from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 21 , 137–155 (2019).
Greenleaf, J. E., Rehrer, N. J., Mohler, S. R., Quach, D. T. & Evans, D. G. Airline chair-rest deconditioning: induction of immobilisation thromboemboli? Sports Med. 34 , 705–725 (2004).
Greenleaf, J. E., Shvartz, E., Kravik, S. & Keil, I. C. Fluid shifts and endocrine responses during chair rest and water immersion in man. J. Appl. Physiol. 48 , 79–88 (1980).
Better, O. S. Impaired fluid and electrolyte balance in hot climates. Kidney Int. Suppl. 21 , S97–S101 (1987).
CAS PubMed Google Scholar
Riddle, M. S. et al. Guidelines for the prevention and treatment of travelers’ diarrhea: a graded expert panel report. J. Travel Med. 24 (Suppl. 2), S57–S74 (2017).
Steffen, R., Hill, D. R. & DuPont, H. L. JAMA patient page. Traveler’s diarrhea. JAMA 313 , 108 (2015).
Rosenstock, J. & Ferrannini, E. Euglycemic diabetic ketoacidosis: a predictable, detectable, and preventable safety concern with SGLT2 inhibitors. Diabetes Care 38 , 1638–1642 (2015).
Fanola, C. L. et al. Incident heart failure and long-term risk for venous thromboembolism. J. Am. Coll. Cardiol. 75 , 148–158 (2020).
Trujillo-Santos, A. J., Jiménez-Puente, A. & Perea-Milla, E. Association between long travel and venous thromboembolic disease: a systematic review and meta-analysis of case-control studies. Ann. Hematol. 87 , 79–86 (2008).
Czuprynska, J. & Arya, R. Annotation: travel and thrombosis. Br. J. Haematol. 188 , 838–843 (2020).
Cannegieter, S. C., Doggen, C. J., van Houwelingen, H. C. & Rosendaal, F. R. Travel-related venous thrombosis: results from a large population-based case control study (MEGA study). PLoS Med. 3 , e307 (2006).
Kahn, S. R. et al. Prevention of VTE in nonsurgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141 (Suppl. 2), e195S–e226S (2012).
Xu, T. et al. Heart failure is associated with increased risk of long-term venous thromboembolism. Korean Circ. J. 51 , 766–780 (2021).
Schreijer, A. J., Cannegieter, S. C., Doggen, C. J. & Rosendaal, F. R. The effect of flight-related behaviour on the risk of venous thrombosis after air travel. Br. J. Haematol. 144 , 425–429 (2009).
Dusse, L. M. S., Silva, M. V. F., Freitas, L. G., Marcolino, M. S. & Carvalho, M. D. G. Economy class syndrome: what is it and who are the individuals at risk? Rev. Bras. Hematol. Hemoter. 39 , 349–353 (2017).
Hitos, K., Cannon, M., Cannon, S., Garth, S. & Fletcher, J. P. Effect of leg exercises on popliteal venous blood flow during prolonged immobility of seated subjects: implications for prevention of travel-related deep vein thrombosis. J. Thromb. Haemost. 5 , 1890–1895 (2007).
Clarke, M. J., Broderick, C., Hopewell, S., Juszczak, E. & Eisinga, A. Compression stockings for preventing deep vein thrombosis in airline passengers. Cochrane Database Syst. Rev. 9 , CD004002 (2016).
Cesarone, M. R. et al. Venous thrombosis from air travel: the LONFLIT3 study–prevention with aspirin vs low-molecular-weight heparin (LMWH) in high-risk subjects: a randomized trial. Angiology 53 , 1–6 (2002).
Graf, J., Stüben, U. & Pump, S. In-flight medical emergencies. Dtsch. Arztebl Int. 109 , 591–602 (2012).
PubMed PubMed Central Google Scholar
Goodwin, T. In-flight medical emergencies: an overview. BMJ 321 , 1338 (2000).
McDonagh, T. A. et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 42 , 3599–3726 (2021).
Seferovic, P. M. et al. Clinical practice update on heart failure 2019: pharmacotherapy, procedures, devices and patient management. An expert consensus meeting report of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 21 , 1169–1186 (2019).
Kalantar-Zadeh, K. & Fouque, D. Nutritional management of chronic kidney disease. N. Engl. J. Med. 377 , 1765–1776 (2017).
Hindricks, G. et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 42 , 373–498 (2021); erratum 42, 507 (2021); erratum 42, 546–547 (2021).
Tasnim, S., Tang, C., Musini, V. M. & Wright, J. M. Effect of alcohol on blood pressure. Cochrane Database Syst. Rev. 7 , CD012787 (2020).
Drucker, A. M. & Rosen, C. F. Drug-induced photosensitivity: culprit drugs, management and prevention. Drug Saf. 34 , 821–837 (2011).
Blakely, K. M., Drucker, A. M. & Rosen, C. F. Drug-induced photosensitivity-an update: culprit drugs, prevention and management. Drug Saf. 42 , 827–847 (2019).
US Food and Drug Administration. The Sun and your medicine (FDA, 2015).
Kolb, C. et al. Do airport metal detectors interfere with implantable pacemakers or cardioverter-defibrillators? J. Am. Coll. Cardiol. 41 , 2054–2059 (2003).
Copperman, Y., Zarfati, D. & Laniado, S. The effect of metal detector gates on implanted permanent pacemakers. Pacing Clin. Electrophysiol. 11 , 1386–1387 (1988).
Jilek, C. et al. Safety of screening procedures with hand-held metal detectors among patients with implanted cardiac rhythm devices: a cross-sectional analysis. Ann. Intern. Med. 155 , 587–592 (2011).
Download references
Acknowledgements
This Review is the result of a cooperation under the umbrella of the Study Group 10 (heart failure) of the German Cardiac Society. S.v.H. has received research funding from the German Center for Cardiovascular Research (DZHK). T.K. has received research funding from the German Heart Research Foundation and is supported by the German Research Foundation (Clinical Research Unit KFO311). R.W. has received research support from the German Center for Cardiovascular Research (DZHK).
Author information
Authors and affiliations.
Department of Cardiology and Pneumology, University of Göttingen Medical Center, Göttingen, Germany
Stephan von Haehling, Kristian Hellenkamp, Rolf Wachter & Gerd Hasenfuss
German Center for Cardiovascular Research (DZHK), Partner Site Göttingen, Göttingen, Germany
Stephan von Haehling, Rolf Wachter & Gerd Hasenfuss
Department of Internal Medicine II, University Hospital Regensburg, Regensburg, Germany
Christoph Birner
Department of Internal Medicine I, Klinikum St. Marien, Amberg, Germany
Institute of Gender in Medicine, Charité – Universitaetsmedizin Berlin, Corporate Member of Freie Universität Berlin and Berlin Institute of Health, Berlin, Germany
Elke Dworatzek
German Centre for Cardiovascular Research (DZHK), Partner Site Berlin, Berlin, Germany
Elke Dworatzek & Christoph Knosalla
Department of Internal Medicine I, University Hospital Würzburg, Würzburg, Germany
Stefan Frantz
Klinik für Innere Medizin, Kardiologie, Diabetologie and Nephrologie, Evangelisches Klinikum Bethel, Bielefeld, Germany
Carsten W. Israel
Department of Cardiology and Angiology, Hannover Medical School, Hannover, Germany
Tibor Kempf
Helios Klinikum Warburg, Idar–Oberstein, Germany
Hermann H. Klein
Department of Cardiothoracic and Vascular Surgery, German Heart Center Berlin, Berlin, Germany
Christoph Knosalla
Charité–Universitätsmedizin Berlin, corporate member of Freie Universität Berlin, Humoldt–Universität zu Berlin and Berlin Institute of Health, Berlin, Germany
Klinik und Poliklinik für Kardiologie, Universitätsklinikum Leipzig, Leipzig, Germany
Ulrich Laufs & Rolf Wachter
Department of Cardiology, Angiology and Pneumology, Heidelberg University Hospital, Heidelberg, Germany
Philip Raake
German Center for Cardiovascular Research (DZHK), Partner Site Heidelberg/Mannheim, Heidelberg, Germany
You can also search for this author in PubMed Google Scholar
Contributions
S.v.H. wrote the article. All the authors researched data for the article, contributed to discussion of content, and reviewed and edited the manuscript before submission.
Corresponding author
Correspondence to Stephan von Haehling .
Ethics declarations
Competing interests.
S.v.H. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, Boehringer Ingelheim, BRAHMS, Chugai, Grünenthal, Helsinn, Hexal, Novartis, Pharmacosmos, Respicardia, Roche, Servier, Sorin, and Vifor and has received research funding from Amgen, Boehringer Ingelheim and IMI. T.K. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Novartis, Pharmacosmos, and Vifor and has received research support from Vifor. P.R. has been a paid consultant for and/or received honoraria payments from Abbott, AstraZeneca, Bayer, BDI, Biotronik, Conventus Congressmanagement & Marketing GmbH, CTI GmbH, Daiichi-Sankyo, Deutsche Gesellschaft für Kardiologie, Diaplan, Edwards, Elisabeth-KH Essen, Heart Institute GmbH, Herzzentrum Leipzig, Kelcon, Medizinische Ausstellungs- und Werbegesellschaft Wien, Medtronic, Novartis and Vifor. R.W. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, BMS, Boehringer Ingelheim, CVRx, Daiichi, Medtronic, Novartis, Pfizer, Pharmacosmos and Servier. R.W. has received research support from Boehringer Ingelheim, Bundesministerium für Bildung und Forschung, Deutsche Forschungsgemeinschaft, European Union and Medtronic. G.H. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, Berlin Chemie, Boehringer Ingelheim, Corvia, Impulse Dynamics, Novartis, Servier, Springer and Vifor. All other authors declare no competing interests.
Additional information
Peer review information.
Nature Reviews Cardiology thanks Biykem Bozkurt, Tiny Jaarsma and Simon Stewart for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
von Haehling, S., Birner, C., Dworatzek, E. et al. Travelling with heart failure: risk assessment and practical recommendations. Nat Rev Cardiol 19 , 302–313 (2022). https://doi.org/10.1038/s41569-021-00643-z
Download citation
Accepted : 01 November 2021
Published : 06 January 2022
Issue Date : May 2022
DOI : https://doi.org/10.1038/s41569-021-00643-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Heart failure with preserved ejection fraction: diagnosis, risk assessment, and treatment.
- Stephan von Haehling
- Birgit Assmus
- Johann Bauersachs
Clinical Research in Cardiology (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Middle East latest: Worshippers in Tehran chant 'death to Israel' after strike; man 'carrying explosives' arrested at Iranian consulate in Paris
Worshippers in Tehran gather at a demonstration just hours after an apparent Israeli strike in Iran. Elsewhere, a man is arrested at the Iranian consulate in Paris after claiming to be carrying explosives.
Friday 19 April 2024 22:30, UK
- Israel-Hamas war
Please use Chrome browser for a more accessible video player
- What we know so far about Israel's apparent attack on Iran
- Iran has 'no plan for immediate retaliation'
- Blinken refuses to talk about Israel's reported attack
- Man arrested at Iranian consulate in Paris
- Worshippers in Tehran chant 'death to Israel'
- Analysis: This strike has escalation written all over it
- Analysis: Iran isn't biggest threat to the coalition right now
- Live reporting by Emily Mee
An Israeli retired major general has said he doesn't believe Israel's overnight attack on Iran is a "very significant event".
Major General Giora Eiland, the former head of the Israeli National Security Council, said the strike showed Israel can reach "even sensitive places" but it had tried to "do it way that both sides can be satisfied".
He told Sky's World with Yalda Hakim programme that he doesn't "predict real escalation after this".
Asked whether Israel's message had been received in Iran, he said countries will try to emphasise their success and minimise the success of the other side.
He added that in attacking Israel, Iran had created an international coalition against itself - "something they certainly don't want to see".
We've been hearing from our military analyst Professor Michael Clarke , who says the overnight attacks on Iran appear to be the Israelis "going after certain targets directly linked to n[Tehran's] attack last weekend".
It's not been confirmed yet, but he says Israel almost certainly used ballistic missiles - rather than the drones than Iran says were used.
"The Iranians have an interest in saying it was almost certainly a one-off attack, it was drones, it didn't matter," Professor Clarke says.
This "relieves them of the responsibility of being so outraged they have to do something even more decisive", he says.
Both sides are now "trying to save face".
Professor Clarke says Israel wanted to carry out an attack, but not one that would upset its allies too much.
Meanwhile Iran is being "careful not to overplay" Israel's attack.
We reported earlier today on a tweet from Israel's national security minister Itamar Ben Gvir, calling the attack on Iran overnight "lame".
Channel 12 is now reporting a confidant of Prime Minister Benjamin Netanyahu reached out to the far-right politician to tell him he was harming Israel's national security.
However, the network added he is unlikely to face further repercussions as Mr Netanyahu is reliant on him to remain in power.
Mr Ben Gvir is among the Israeli hardliners calling for a harsher response to Iran and more brutal measures in Gaza.
The Israeli prime minister remains in a tough spot as he is facing calls for de-escalation from Western allies, but he also needs to appease hardliners within his government to stay in power.
The Met Police has retracted its previous statement about two of its officers, who were heavily criticised for threatening to arrest a Jewish man near a pro-Palestinian march.
The officers said the antisemitism campaigner, who was wearing a kippah skull cap, was "quite openly Jewish" so they were concerned about the reaction to his presence near the march.
The Met said it had "reflected on the strength of the response to our previous statement" and wished to make a new apology.
In its earlier statement, the force had said the use of the term "openly Jewish" was a "poor choice of words and while not intended, we know it will have caused offence to many".
It continued: "In recent weeks we've seen a new trend emerge, with those opposed to the main protests appearing along the route to express their views.
"The fact that those who do this often film themselves while doing so suggests they must know that their presence is provocative, that they're inviting a response and that they're increasing the likelihood of an altercation."
But this statement was criticised by the antisemitism campaigner in the video, Gideon Falter, who accused the force of "appalling victim blaming".
"What has dented Jewish Londoners' confidence in the Met is not us making this video public, but the actions of the Met's officers telling me that I cannot be in the area whilst openly Jewish," he said.
"The assistant commissioner appears to be saying that we should have taken this on the chin and kept the video under wraps."
Here is the new statement in full:
"The use of the term 'openly Jewish' by one of our officers is hugely regrettable. We know it will have caused offence to many. We reiterate our apology.
"We have reflected on the strength of the response to our previous statement. In an effort to make a point about the policing of protest we caused further offence. This was never our intention. We have removed that statement and we apologise.
"Being Jewish is not a provocation. Jewish Londoners must be able to feel safe in this city.
"Our commitment to protecting the public extends to all communities across London. It's important that our public statements reflect that more clearly than they did today."
US officials are continuing their silence on the apparent Israeli attack on Iran overnight.
In a news conference just now, White House press secretary Karine Jean-Pierre was asked whether this is part of a strategy to de-escalate tensions in the Middle East.
She said she has "nothing to share" and was "not going to speculate on reportings".
Ms Jean-Pierre said the US does not want to see the conflict escalate and will continue to consult with partners.
Israeli fighter jets launched three missiles at an air defence radar site near the Iranian city of Isfahan in last night's overnight strike, according to a report.
ABC News, citing an unnamed US official, said the radar site was part of the protection of Iran's Natanz nuclear facility.
The official reportedly said the missiles were fired from outside Iran and the strike was "very limited".
They also said an initial assessment showed the radar site was taken out, but the assessment has not yet been completed.
Iran earlier said three drones were involved in the attack on Isfahan, and made no mention of any missiles or damage.
The US has publicly said very little about the attack, apart from confirming it was not involved.
By Alex Rossi , international correspondent on the Israel-Lebanon border
The roads through northern Israel along the border with Lebanon are empty of cars.
It is unnervingly quiet.
Since 7 October the area has been under bombardment from Hezbollah militants and tens of thousands of people have left following the government's evacuation rules.
Ariel Frish, the deputy head of security, in Kiryat Shmona, a frontline city, shows me the damage in a residential area.
A house is gutted from fire caused by the explosion from the strike.
"We got attacked by a great wave of missiles, one of the missiles hit this house," he said.
"Nobody was here because we evacuated the city one week before. And if we had not evacuated there would be no survivors.”
The Israel Defence Forces and Hezbollah have been exchanging fire on a daily basis in the north for more than six months - and it feels like a full scale war may not be far away.
Walking through the communities in the north is eerie.
You can hear the sound of birdsong and the constant noise of drones and warplanes circling overhead.
A short distance from the Lebanese border and former IDF commander, Gideon Harari, who lives in one of the communities in the line of fire, says a major confrontation is looking more likely every day.
The situation with Iran and the standoff with Hezbollah, as well as the war in Gaza, make this an incredibly dangerous time for the region.
"The shooting is daily. Rockets, drones every day," he said.
"Now is the most dangerous point in the Middle East for the last forty years. If Israel will take military measures against Iran it might drive us into a Middle East war, a big war."
The internally displaced have moved to hotels and guesthouses in safer parts of Israel.
In Tiberias the evacuees can only wonder when it will be safe to return.
"The mood of the people in Israel is very frustrated. And it is very dangerous to live here," says Daniel Boker, who left his hometown of Metula on the border, months ago.
Tensions are now the highest they've been for decades and that's reflected in the preparations Israel is making.
The national ambulance service, Magen David Adom, has been stockpiling equipment in an underground facility. Chief of staff Uri Shacham, tells me 7 October has changed everything.
"We are preparing for a long-term campaign or long-term war," he said.
"If you had talked to me in September 2023, I would have said we have a supply for one month.
"Nowadays, because of what we are expecting, [we are] preparing... many more month's [worth] of equipment."
Israel now faces crisis on multiple fronts but it is clear the current situation in the north is increasingly untenable.
It will not take much for a broader war to break out.
By Sam Doak, OSINT reporter
A video showing explosions in the sky above Isfahan provides further information on last night's attack in Iran.
Sky News determined the video was filmed next to Laleh Park in the northeast of the city by matching features including a road, park, flagpole and three cylindrical structures.
This made it possible to determine the video shows explosions in the sky to the east of the city.
While this video does not contain enough information to tell with certainty what site was targeted, explosions in this general area fit with accounts in Iranian media that a base adjoining Isfahan International Airport was attacked.
This base is located to the northeast of Isfahan. Fars News Agency, a regime-aligned Iranian outlet, has claimed that three explosions occurred near this site as a result of last night's attack. No substantial damage has been reported.
The apparent Israeli attack on Iran has prompted airlines to change flight paths, cancel flights and divert others to alternate airports over security concerns.
Iran closed its airports in Tehran, Shiraz and Isfahan in the aftermath and cleared flights from the western portion of its airspace for a few hours after the attack, according to flight tracking website FlightRadar24.
Both the airports and airspace had reopened by 4.45am UK time.
Flydubai said it had cancelled its flights to Iran and an earlier flight had turned back to Dubai.
Tracking data also showed an Iran Air flight from Rome to Tehran was diverted to Ankara, Turkey.
As we reported earlier, Germany's Lufthansa cancelled all flights to Tel Aviv and Erbil until tomorrow, and would avoid Iraqi airspace during this time period.
United Airlines said it would cancel its daily flight from Newark to Tel Aviv until 2 May, while Air Canadasaid it was pausing operations to and from Tel Aviv until the end of June.
Emirates, Flydubai, Turkish Air, Wizz Air Abu Dhabi and Belavia were among the carriers continuing to fly over the part of Iran's airspace that remained open in the initial hours after the attack early today.
Activists and aid workers are preparing another attempt to break through the Israeli blockade and deliver humanitarian aid to Gaza.
A coalition of organisations, including the IHH and the Mavi Marmara Association from Turkey, are planning to set sail soon onboard the ship Akdeniz.
The exact launch date is unclear but activists are currently sorting aid inside the cargo hold.
The same organisations were previously in charge of a flotilla that attempted to deliver aid in 2010.
Israeli commandos stormed the Mavi Marmara in international waters, leading to an altercation that left nine people dead and dozens of activists wounded.
Be the first to get Breaking News
Install the Sky News app for free


IMAGES
VIDEO
COMMENTS
Air pressure is lower at higher altitudes, which means your body takes in less oxygen. ... to keep blood flowing. ... it might be worth putting off air travel. If your eustachian tubes are clogged ...
A 2021 study states that people with high blood pressure can travel to high altitudes unless they have uncontrolled blood pressure or heart problems. In these situations, it is essential to talk ...
When planning air travel, anxiety about the prevention and treatment of a heart attack on a plane or worrying about questions such as "can flying cause heart attacks" may give you the jitters. ... Dehydration due to cabin pressure at high altitude can affect your blood pressure, causing exacerbation of heart disease. This is especially ...
Patients with unstable angina, new cardiac or pulmonary symptoms, or recent changes in medications without appropriate follow-up should not fly until stable. 11. C. Consensus/expert opinion ...
The effects of high altitude may include nausea and headaches. However, the pressurization of airplane cabins usually prevents these uncomfortable side effects. Flying with high blood pressure is possible if high blood pressure is under control. Nonetheless, anyone with high blood pressure should take the necessary precautions for air travel.
Sitting immobile on long plane flights or car, train or bus rides can slightly increase a normal person's risk of blood clots in the legs, but associated medical issues usually contribute to it. If someone has peripheral artery disease (PAD) or a history of heart failure, the clot risk increases. Recent surgery, older age and catheters in a ...
Hence, the management of hypertension is of great importance. Herein, we discuss the pathophysiological factors for elevated blood pressure during flight, and we make recommendations which should be followed by the passengers and the flight crew and the physicians for trouble-free air travel.
However, those with high blood pressure may be at a greater risk of developing hypertension which can lead to heart failure, coronary artery disease, and other health conditions. If you suffer from high blood pressure it doesn't mean you can't travel by plane, it just means you have to be cautious.
Prolonged immobilization during air travel, with pressure from the aircraft seat at the back of the legs and subsequent venous stasis, predisposes passengers to DVT and thromboembolism. 1, 2 This has long been known as a possible complication of air travel, particularly with prolonged flights, especially in those with additional risk factors ...
The effects of occasional flying on heart health are relatively unstudied. Yet, according to a recent study, even men in good health have an increased blood pressure of 6% during commercial flights. According to the CDC, about 1 in 600 flights experience a medical emergency, such as: Heart problems. Nausea or vomiting.
Quick Summary. High blood pressure or hypertension can be a concern when traveling by air due to the medical risks involved. Cabin pressurization aims to reduce the chance of symptoms; however, it is not always effective at preventing ailments like hypoxia. Certain precautions can make flying with blood pressure safer while preventing issues ...
For example, blood pressure is considered high if over 140/90mmHg, so if your blood pressure is consistently above this value then it is important to reduce it. Tips for travelling with high blood pressure: Buy travel insurance for pre-existing medical conditions to cover any high blood pressure related medical costs, should you need treatment ...
A person with pulmonary hypertension has high blood pressure in their lungs, causing their blood vessels to narrow and their heart to work harder. ... Air travel adds another hurdle. A plane at ...
Airplane Travel and Blood Oxygen Saturation. ... Typically, in-cabin air pressure is equivalent to that seen at 5000 to 8000 ft. Local hypoxia causes vasodilation (decrease in blood pressure) and ...
Relieving pain in your ears during air travel. Try taking a decongestant or a nonsteroidal anti-inflammatory medicine before you get on the airplane, particularly if you are suffering from a head cold or swollen sinuses. If you have high blood pressure or heart problems, you should not take decongestants without approval of your healthcare ...
High blood pressure, or hypertension, afflicts about 75 million people each year, according to the American Heart Association. With 195 million people flying domestically, according to Bureau of ...
People with high blood pressure and heart conditions should talk to their doctor before traveling to places at high altitude, a new scientific statement from the American Heart Association advises. ... or climbing can place too much stress on the heart and blood vessels due to lower levels of oxygen and fluctuations in air pressure, temperature ...
Blood pressure patterns; AIR TRAVEL. Incidence of in-flight medical events; Preflight assessment - Risk stratification - Contraindications to air travel - Recommendations for all travelers with cardiovascular disease - Assess the need for supplemental oxygen; Disease-specific recommendations - Acute decompensated heart failure - Stable chronic ...
For patients with chronic pulmonary disease who are planning to travel by air, ERS advises a minimum pulmonary vital capacity of 3 L, a forced expiratory volume in 1 second (FEV 1) >70% of reference, a minimum oxygen saturation of 85%, and a minimum arterial partial oxygen pressure of 70 mm Hg, as well as a stable state of vital signs ( 3, 10 ).
During air travel, cabin pressure is required to be no less than the barometric pressure at an altitude of 2,438 m ... On-board treatment included blood pressure management in 76% of incidents, ...
Your blood pressure should not be affected by air travel and therefore there is no reason why you should not fly if you are being treated for high blood pressure. However, your travel insurance may not cover the cost of any additional treatment or complications, so it is advisable to only travel once your blood pressure has been controlled and ...
Israel's national security minister writes a very short post on X after his country's strike on Iran - and a senior Iranian official says the country has no plan for immediate retaliation. In a ...