

House Calls – We Bring the Doctor’s Office to the Patient
At Mobile Physician Services, we provide comprehensive care to improve the health and quality of life of our patients – in the convenience and comfort of their own home. Our team of board-certified doctors, advance nurse practitioners, and physician assistants specialize in providing care for patients with medically complex and chronic conditions.
Our Services
We accept Medicare, many insurance plans, and self-pay.
To find out more about our services:
Call Toll-free: (855) 232-0644
E-mail us at [email protected]
Primary Care
Pain management, palliative care.
At Mobile Physician Services, our customized care teams provide patients with both comfort and familiarity as they work with a dedicated primary care provider and care coordinator to improve their health. Our physicians and staff take a proactive approach to preventive care, chronic disease management, and chronic illness support right where you live.
Each home visit includes an in-depth examination and individualized treatment plan, which is monitored and adjusted through routine follow-up visits. The primary care provider will deliver your ongoing care and will recommend to you specialty services as needed.
- Annual Wellness visits : This wellness visit allows your primary care provider to create or update your personalized prevention plan. This visit includes a review of your medical and social history related to your health and may include counseling about preventive services. This plan may help you to prevent or reduce the chances of future illness based on your current health and risk factors.
- New Illness Exams : When a new symptom or ailment arises, call us. Early indications of not feeling well could be a clue that you may be getting sick. A symptom in one part of the body may also be a sign of a problem in another part of the body. Moreover, unrelated symptoms that might seem minor on their own, could be warning signs of a more serious medical disease or condition. The new illness exam can be very brief or more detailed depending on your concerns and the provider’s findings.
- Follow-up Care: Involves a regular medical checkup, which may include a physical exam and laboratory testing. Follow-up care checks are a proactive way of assessing the potential for and preventing health problems from returning after treatment of a disease has ended or an illness has seemingly passed.
- Referral for Specialty Care : Referrals are the link between primary and specialty care. The referral coordination includes the documentation of patient care activities, the transfer of information, the inter-provider communication itself, and the integration of care services to the patient. Mobile Physician Services is a multi-specialty practice so many of these specialty referral services can be made seamlessly with little inconvenience or disruption to the patient and caregivers regular routines.
- Medication Management: Medication management is a treatment structure that ensures our patients are receiving optimal therapeutic results from their prescription medications, both in the short and long term. Our team’s goal is to mitigate medication noncompliance and monitor all prescriptions treatments so that drug interactions complement one another for the most optimal outcome for our patients.
The provider may be a physician, advanced practice nurse or a physician assistant. A dedicated care coordinator will also be assigned for each patient to help arrange comprehensive services and assist patients and their caregivers.
- Online Patient Portal: You and your designated caregiver, if you choose, will be able to connect with your provider through a convenient, safe and secure environment which allows access to your health records and a way to communicate with our staff in a timely manner.
- Telephone Assistance : On call providers are available 24/7 weekdays and weekends.

Our psychiatry team specializes in the diagnosis and management of mental, emotional and behavioral disorders. They carefully evaluate each patient to develop an individualized treatment plan to improve the patient’s overall mental and physical well-being.
- Depression : Depression is a common and often serious medical illness that negatively affects how you may feel, the way you may think, and how you may act. Depression can cause feelings of sadness, despair and hopelessness, which may lead to a loss of interest in activities you once enjoyed.
- Anxiety : Intense, excessive, and persistent worry and fear about everyday common situations. The worry or anxiety could make you feel fatigued, irritable, and interfere with your regular sleep habits.
- Dementia : An overall term that is used to describes a collection of symptoms related to an individual’s decline in memory or other thinking skills. It may be severe enough to diminish a person’s ability to perform everyday common activities. The effects of dementia can negatively influence your memory, thinking and social abilities.
- Phobias : A phobia is when you experience excessive panicking or an irrational fear reaction to a situation. If you have a phobia, you may experience a deep sense of dread or fright when you encounter the source of your fear. The fear may be a certain place, situation, object, animal or even another person.
- Behavioral disorders : Attention deficit, hyperactivity, bipolar, learning, defiant or conduct disorders are all examples of complaints that may have a detrimental impact on a person’s interpersonal relationships with family, friends, and co-workers.
Our team can provide behavioral counselling and medical therapy, when appropriate, to help a patient feel better about themselves and to assist them with better coping and managing their condition.

Our wound care specialists have been trained in the attention and treatment of all types of acute and chronic wounds. They have skill and experience in wound debridement and wound care procedures – managing chronic, non-healing wounds and infections, with a demonstrated care that fosters healing… right in the patient’s own home.
We specialize in serving homebound patients who may also be bed-bound or have difficulty in walking or moving around. As a result, immobility compression sores develop at pressure points on the body when the weight of an immobilized individual rests continuously on a firm surface, such as a mattress or wheel chair. Often these same patients are on oxygen or have high-risk medical conditions which makes it an even more challenging and stressful effort for them to travel to a doctor’s office for an appointment. Thus, the necessity for in home care and treatment.
Wounds that benefit from specialized wound care techniques include:
- Diabetic foot wounds and ulcers
- Post-surgical wounds
- Traumatic wounds caused by injury
- Arterial and vein stasis caused by lack of circulation
- Immobility pressure sores. (Bed sores from stillness)
We work closely with home health agencies to provide ongoing care and monitoring of patient’s wounds.

Our board-certified podiatrists treat foot pain, wounds, and more. Treatments may include but are not limited to treating conditions of the lower extremities which could hinder mobility.
- We will review each patients’ medical history to evaluate the condition of the feet, ankle or lower leg
- Carry out a diagnosis on the feet and lower legs through examination and medical tests
- Order physical therapy when deemed necessary
- Treat wounds of the lower extremities using various wound care modalities. This may include debridement to improve the healing potential
- Promote prevention, health & well being, the treatment and management of the foot and related problems, disability, deformity, and the pedal complications of chronic diseases for the elderly
- Prescribe and fit prosthetic appliances such as diabetic shoe inserts and evaluate for bracing if necessary
- Refer patients to other specialists for treatment, including conditions such as diabetes or arthritis
- Advise patients on ways to prevent future leg problems and increase speed of recovery
- Monitor the recovery progress of patients to determine the need for change in treatment

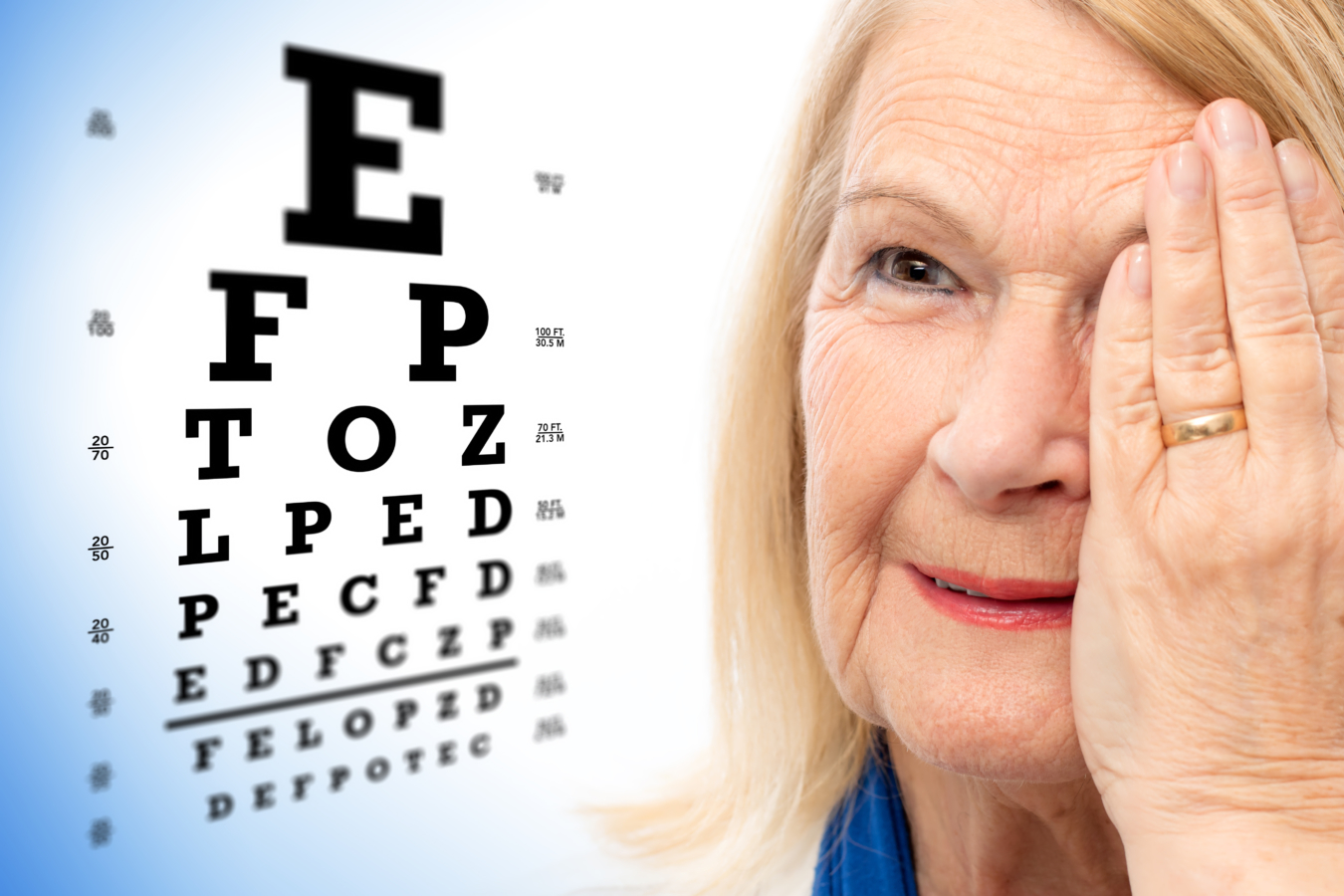
We know it’s not always easy to leave home to get the care you need for your eyes. Our optometrists bring state-of-the-art diagnostic eye equipment and technology to your home – making it much easier for you to get the vision care you need.
During a visit, your doctor will exam each eye for signs of serious issues such as glaucoma, cataracts, macular degeneration, and detached retinas, among other conditions.
Receiving regular eye exams regardless of the state of your vision can help detect serious eye problems at their earliest stages ─ when they are most treatable. During an eye exam, your doctor will observe and evaluate the health and condition of the blood vessels in your retina, which can be good indicators of the health of your blood vessels throughout the rest of your body.
- Comprehensive eye exams : This exam goes beyond a simple vision screening. A comprehensive eye exam includes a host of tests in order to do a complete evaluation of the health of your eyes and your vision.
- Annual retina exams : A retinal exam allows your doctor to evaluate the back of your eye, including the retina, the optic disk and the underlying layer of blood vessels that supply the retina.
- Eyeglass fittings : A prescription works best when your eyeglasses are properly fitted. Improper fitting may cause pinching, distorted vision, headaches, and even dizziness. Our doctors will make sure your prescription lenses and frames are working together for you.
- Diabetic eye exams : Diabetes does not have to lead to vision loss. Taking an active role in managing your diabetes can go a long way in curbing later complications. Regular eye exams, good management of your blood sugar and blood pressure, along with early intervention for vision problems can help prevent vision loss caused by diabetic retinopathy. Retinopathy is caused by damage to the blood vessels of the light-sensitive tissue at the back of your eye.
- Refractions: This test is given as part of your routine eye examination. It is often referred to as a vision test. This test assists your eye doctor in measuring you for the exact lens prescription you will need.
- Eye injuries: Eye trauma could be the result of a sudden blow to the eye. It may cause the eye to suddenly compress and retract which could cause damage to your eye and the surrounding tissue. Even if the injury may seem minor, all eye injuries should be furthered examined by a doctor for possible more serious and underlying injuries.
- Eye infections: The most common eye infection is conjunctivitis, also known as pink-eye. An eye infection can happen in almost any part of your eye, including your eye lid, cornea and optic nerve. Symptoms of eye infections may include redness, itching, swelling, discharge, pain, or problems with vision. Always consult with your doctor before treating, as recommended actions are contingent on the cause of the infection.
- Low-vision exams: A low vision exam is different from a normal eye exam. This functional-vision assessment determines how specific visual impairments affects your ability to perform everyday activities. The exam’s results assist your doctor in prescribing management tools and medications to better enhance and manage your remaining vision.
Pain management is the process of providing medical care that alleviates or reduces pain. Pain management is a subspecialty of general medicine employing an interdisciplinary approach to ease the suffering and improve the quality of life of those living with chronic pain by using a combination of pain medications, joint and muscles injections, and physical therapy techniques.
A pain management specialist is a provider with advanced training in diagnosing and treating pain. Our pain management specialists treat pain stemming from a variety of different causes, whether it’s neuropathic pain or headache, or the result of injury, a surgical procedure, cancer or another illness.

Palliative care is an approach to the holistic care of patients, including family and caregivers, to improve the quality of their lives after the diagnosis of a chronic debilitating disease or life-limiting illness that may cause a host of complaints.
Palliative care can begin at diagnosis and continue to be offered while the patient is continuing active treatment through different phases of their life limiting condition. Palliative care is for any patient with a chronic illness who is experiencing a decreased quality of life because of symptoms related to their illness or treatment, like renal dialysis, oxygen therapy or chemotherapy. The care is provided by a specially-trained team of doctors, nurse practitioners, physician assistants, and other specialists who work together to provide an extra layer of support to the patient and their caregivers.
Palliative care can help in symptom control including not only pain, but nausea, weakness, shortness of breath, fatigue and weight loss at any time during their diseases, not only at the end of life.

In Home Medical Senior Care Services | Landmark Health
- Patient or Caregiver
- Community Provider
Are you a new Landmark patient?
Burn-out is real. landmark is different..

Living with chronic health conditions? We can help.
Our providers and care teams come to you, bringing care through house call visits. This in-home medical care is designed around understanding your health needs and goals. We work with you and your regular doctors to help you stay well and stay home.
House calls and video visits in 37 states.
Landmark partners with health plans to bring medical, behavioral health, and palliative care, along with social services, to patients in communities across the U.S. Our mobile providers visit patients in their homes through in-person house calls and telemedicine visits over video and phone.
We are the future of health care.
Landmark is one of the nation’s largest healthcare companies focused on in-home care of complex, chronic patients. Our physician-led provider groups support collaborative ties between community-based organizations, primary care providers, specialists and patients and their families.
patients nationally for which Landmark bears risk
reduction in hospital admissions
reduction in mortality

Discover the benefits.
- For Patients + Caregivers
- For Community Providers
- For Partners
Health care in your home
Old-fashioned house calls by medical doctors, nurse practitioners and physician assistants bring modern medicine to you. Feel better and stay well at home.
Covered by your health plan
The Landmark program works with health plans to improve access to care for patients with multiple chronic conditions. Landmark’s team-based care is available often at no cost to you.
Keep your current doctors
Landmark coordinates its care with your primary care provider, specialists and other community resources. Landmark provides added support to those who need it most.
Available 24 / 7
Our provider-staffed call center answers any time of the day or night. We also provide urgent visits to help you avoid unnecessary trips to the emergency room.
No waiting room
With Landmark house calls, you won’t need transportation to clinics and hospitals, and you avoid waiting rooms and exposure to germs.
Reduced stress
Patients and caregivers enjoy peace of mind with Landmark support. Landmark cares for the whole patient.
Landmark house calls put patients at the center of health care.
Collaborative care for complex patients.
Landmark’s community-based mobile providers bring coordinated care to patients with multiple chronic health conditions. We augment your care in the patient’s home.
Covered by health plans
The Landmark program is included in eligible patients’ health plans to improve care coordination and healthcare access for home-limited patients.
You remain the primary care provider
Landmark care is coordinated directly with you. Our providers reinforce your care plan in the home through physician-led interdisciplinary care teams.
Access our interdisciplinary team
Landmark’s interdisciplinary care team is available to you and your patients, including behavioral health specialists, social workers, palliative care specialists, nurse care managers and pharmacists.
Reduce administrative burden
We can help your highest acuity patients by managing post-acute care, home health orders, face-to-face encounters, and more.
24 / 7 availability
You can reach us any time, including weekends and holidays. We do urgent home visits to intervene if your patient experiences a chronic disease exacerbation.
Landmark supports your patients with complex health and social needs.
Chronic care management.
We’re one of the nations’ leading risk-bearing medical groups. We focus on giving your most complex members care when they need it, right in their home.
Over 250,000 patients across the country
We bear risk for over 250,000 complex, chronic patients, spanning Medicare Advantage, Medicaid, Dual, and Commercial, populations.
Behavioral, social and palliative care
Our team of multidisciplinary clinicians may include behavioral health specialists, palliative care practitioners, social workers, nurse care managers, dietitians and pharmacists.
Urgent in-home visits
One in four of our home visits is urgent. We bring medical care to your members when they need it, to avoid unnecessary emergency room trips and hospitalizations.
Built-for-purpose infrastructure
Our technology platform is designed specifically to support the medically vulnerable, clinically complex population.
Meaningful outcomes
Landmark commonly helps health plans achieve 4- and 5-star performance on Medicare STARS clinical quality of care, while caring for the most complex patients.
Landmark provides care for complex, chronic patients to positively impact access, satisfaction, outcomes and cost.
The doctor and nurses show they care about you and your health they are really there for you when you need them I love that they come to your house we did a zoom meeting with the nurse practitioner and she gave suggestions I really appreciate them
It was a pleasure to talk and see the doctor, she was very knowledgeable of all my conditions and gave me great advice to improve my health.
Joan was very helpful. It was nice getting to know her. How Landmark can help me
Practice health care the way you always wanted — with those who need it most.
Expert insights.

Prioritizing Mental Health as a Universal Human Right
By: Neltada Charlemagne, DNP, APRN, PMHNP-BC, PHN, BHC

Outsmart Unplanned Medical Costs: 10 Steps for Managing the Unexpected
Older adults can safeguard themselves from the physical, mental and emotional toll of unexpected medical costs.

Optum Care Network – Monarch and Landmark Health bring care to you at home.
Optum Care Network – Monarch has teamed up with Landmark to deliver in-home medical care to members with multiple chronic conditions.
Have questions about Landmark? We’d love to hear from you.

Look out for your health
A UnitedHealthcare® HouseCalls visit is a no-cost, yearly health check-in that can make a big difference.
Call 1-866-799-5895 ,
TTY 711, to schedule your visit.
HouseCalls brings yearly check-in care
To you at home.
Connect for up to a full hour of 1-on-1 time with a licensed health care practitioner. Every visit includes a physical, tailored recommendations on health care screenings and plenty of time to ask questions that matter to you.
After your visit, HouseCalls connects with your primary care provider (PCP) to help keep them informed about your health. It's a great way to feel confident knowing an extra set of eyes is looking out for you between regular PCP visits.
What is a HouseCalls visit?
[Text On Screen – SAY HELLO TO HOUSE CALLS]
Say hello to HouseCalls.
[Text On Screen- PAID ACTOR PORTRAYAL.]
HouseCalls is our way of looking out for your health, so you can focus on your future. Here’s what it’s all about.
[Text On Screen – HERE’S WHAT IT’S ALL ABOUT]
Once a year, a licensed health care practitioner can come to your home to spend up to an hour with you on your health and wellness.
[Text On Screen- EASY, CONVENIENT, INFORMATIVE]
It's designed to be easy, convenient and informative.
[Text On Screen- HEAD-TO-TOE EXAM]
[Text On Screen- IMPORTANT HEALTH SCREENINGS]
[Text On Screen- HEALTH GOALS DISCUSSION]
You'll get a head-to-toe exam, important health screenings and plenty of time to talk about your health goals.
We'll also provide guidance on managing your health and if you need it, give you referrals for other health plan resources and services.
HouseCalls is a great way to stay on top of your health between regular doctor's visits.
At the end of your visit, you'll get a personalized checklist so you can feel more confident in what to discuss with your regular doctor.
[Text On Screen- COST? NO EXTRA COST TO YOU]
[Text On Screen- INCLUDED IN YOUR HEALTH PLAN]
If you're wondering how much all of this is going to cost, the best part is, there is no extra cost to you. It's included in your health plan.
[Text On Screen- HOUSECALLS VIDEO VISITS ARE NOT AVAILABLE WITH ALL PLANS.]
A HouseCalls visit takes place in the comfort of your own home or by video if you prefer.
So, say hello to HouseCalls and invite us in for a visit today.
[Text On Screen – SAY HELLO TO HOUSE CALLS TODAY]
Access one of the most popular UnitedHealthcare offerings, at no cost to you
Schedule your visit
Call 1-866-799-5895 , TTY 711
Monday–Friday, 8 a.m.–8:30 p.m. ET
Your in-home health check-in
- Up to a full hour with a licensed health care practitioner
- Ask the questions that matter to you and get valuable health tips
- No cost — it's included in your health plan
Get rewarded
Meet your friendly housecalls medical staff.

Just like the professionals you see in your regular doctor’s office, our licensed health care practitioners may be nurse practitioners, physician assistants or medical doctors. They’re state licensed and maintain national certification.
We perform background checks on these professionals to provide additional peace of mind for our members. Your loved ones, caregivers or friends are welcome to be present during the visit — it’s up to you.
Ready to open the door to better health?
Getting ready for your housecalls appointment, tips to help you prepare: .
- Wear shoes that are easily removed to have your feet checked
- Make a list of upcoming appointments with your PCP and specialists
- Make sure all of your medications, both prescription and over-the-counter vitamins and supplements, are in their original bottles for our review
- If you record blood pressure readings, please have your results available for review
- If you have diabetes, please have your blood glucose meter handy
- Make a list of questions and concerns you’d like to discuss
During your appointment
- You'll have up to a full hour of 1-on-1 time with your health care practitioner for a physical, select lab tests, health screenings and more
- A HouseCalls visit can be completed while sitting at your kitchen table or in the living room, and you can use the time to ask any health-related questions
- The visit is tailored to your individual needs, so screenings and conversation topics can vary
After your appointment
Less travel time. more face time..
Think of HouseCalls as an extra layer of care — valuable 1-on-1 time you don't always get in the doctor's office. And it's tailored to your individual needs.
Schedule today
To secure your spot, call us at 1-866-799-5895 , TTY 711
Have a question?
Find answers to frequently asked questions.
If you have a specific question about your upcoming appointment or need to reschedule, call us at 1-866-799-5895, TTY 711 , Monday–Friday, 8 a.m.–8:30 p.m. ET
We're here to help.
- 24/7 service available 847-543-0045
- see our brochures download now

Home Visiting Physicians
Be seen right at your home and start the care you need..
Your health is our priority! Your course of treatment will never be just about diagnosis, test results, and medications; it will also be about helping you reach the highest quality of life. We do this by actively listening and understanding your personal goals so we can tailor a plan-of-care that will be created with you in mind.
Where can we come?
These services can be utilized wherever the patient resides – whether that be in their home or in a facility.
Contact Us Today
What we offer
A primary care home visit by one of our board certified and caring medical providers. A visit may be for acute concerns, regular follow-up, and annual physicals.
Comprehensive medical exam in the comfort of your home; which may include orders for blood test, urine test, radiological imaging, medication prescription, and/or specialty referral.
The ability to directly reach your medical provider for any questions or concerns over the phone or email.
New prescription and renewals sent electronically to your pharmacy of choice within 24-hours
We are here to help when you need us
Free download resources.
Meridian Health Care is proud to offer the following resources for you.
- Home Health Care
- Hospice Care
- Palliative Care
- Our Mission & Vision
- Our Leadership
- Our Proud History
There was a time when doctors treated patients in their own home. This old-fashioned care matched with new medical technology is here again. At HouseCall Primary Care, we serve homebound patients wherever home may be...a patient's house, a nursing home, or assisted living. Our team of providers stay with our patients wherever they go.
HouseCall Primary Care offers these general areas of specialty. Select one of the services below to learn more.
- Find your local Age UK

- Site search Search term
- Back Information and advice
- Back Money & legal
- Back Benefits and Entitlements
- Attendance Allowance
- Benefit rates 2024-25
- Benefits Calculator – what are you entitled to?
- Bereavement Support Payment
- Carer's Allowance
- Benefits for mixed age couples
- Changes to the benefits system
- Cold Weather Payment
- Council Tax Reduction
- Disability Living Allowance
- Employment and Support Allowance
- Free bus pass and transport concessions
- Free prescriptions for over 60s
- Housing Benefit
- How to apply for a Blue Badge
- How to challenge a benefits decision through mandatory reconsideration
- How to get help with urgent or one-off expenses
- How your benefits are means tested
- Income Support
- Jobseeker's Allowance
- Pension Credit
- Personal Independence Payment
- Returning to the UK after living abroad
- Support for Mortgage Interest
- TV licence concessions
- Universal Credit
- Warm Home Discount
- Winter Fuel Payment
- More money in your pocket information guide
- Back Debt and savings
- Debt help and advice
- Energy advice for the home
- Financial jargon checker
- How to reduce your water bills
- How to trace lost money
- Using credit wisely
- Back Income and tax
- What is equity release?
- Ways to reduce Council Tax
- Inheritance tax
- How to boost your income in retirement
- Equity release information guide
- Back End of life planning
- Back Legal issues
- Finding legal advice
- How to be an executor information guide
- Making a will
- Power of attorney
- Power of attorney information guide
- Thinking about end of life information guide
- What is a living will (advance decision)?
- What to do when someone dies
- Wills and estate planning information guide
- Back Pensions advice
- Annuities explained
- Finding old pensions
- Pension calculator
- Pensions scams and fraud
- State Pension
- What are workplace pensions?
- What pension options do I have?
- Back Scams and fraud
- How to spot a catfish
- Spotting TV Licence scams
- Doorstep scams
- Postal scams
- Phone scams
- What to do if you're the victim of a scam
- Investment scams and fraud
- Avoiding scams information guide
- Help with the cost of living
- Back Consumer advice
- Changes to landline telephones
- Back Health & wellbeing
- Back Conditions and illnesses
- Bladder and bowel problems information guide
- Bowel problems
- Coronavirus
- Depression and anxiety
- Hearing loss
- High blood pressure
- Influenza (flu) prevention
- Malnutrition
- Osteoporosis
- Seasonal affective disorder (SAD)
- Urinary incontinence
- Urinary tract infections (UTIs)
- Back Health services
- Dental services for older people
9 health tests that could save your life
- Getting the most from your medicines
Getting help when feeling unwell
Nhs continuing healthcare, your hospital stay, gp services for older people.
- Leaving hospital
Complaining about NHS services and hospitals
What standards you should expect from nhs services.
- Your hospital stay information guide
- Back Being active
- Getting active when you find exercise difficult
- Getting active but not sure where to start
- Helping someone to get active
- Preventing falls
- How to look after your feet
- Walking tips
- Physical activity videos to use at home
- Staying steady information guide
- Back Mind and body
- 10 tips for ageing better
- 5 tips to boost your mood
- Getting a good night's sleep
- Your mind matters
- Mindfulness
- Staying cool in a heatwave
- Staying sharp
- Preventing and treating burns
- Back Loneliness
- A Life Less Lonely
- Caring for someone who's lonely
- Feeling lonely
- Back Keep well this winter
- Keeping warm and well in winter
- Keep your spirits up
- Look after each other
- Cold weather advice and tips
- Managing money in winter
- Winter wrapped up information guide
- Winter illnesses
- Back Relationships and family
- Financial and legal tips before remarrying
- Planning for end of life
- Protection from abuse and neglect
- Dating in later life
- Sex in later life
- How to deal with grief after a bereavement
- How to adjust to living alone
- Top tips for grandparents
- Worried about someone?
- Back Care & support
- Back Finding and arranging social care
- Care needs assessment
- Home care: how to find the care you need at home
- Back Paying for care
- Financial assessment explained
- Paying for residential care
- Paying for homecare
- How much does care cost?
- Back Help for carers looking after a loved one
- Carer's assessment
- Financial support for carers
- Balancing working and caring responsibilities
- Caring for someone with dementia
- Looking after yourself as a carer
- Respite care: having a break from caring
- What to do when your caring role changes or ends
- Carer's checklist
- Back Housing options in later life
- Assisted living and extra-care housing
- Safety in the home
- Home adaptations to simplify home tasks
- Specialist housing options
- Renting and social housing
- Homelessness
- Moving in with family
- Residential park homes
- Sheltered housing
- Back Problems with care
- How to complain about care to your local council
- Problems with homecare
- Back Work & learning
- Back Making the most of the internet
- Computer training courses
- Glossary of online terms
- Getting started on the internet
- Staying safe online
- Keeping in touch using a video call
- Making your device easier to use
- How to download apps
- Email essentials
- What's WhatsApp?
- Using social media
- Is online banking safe?
- How to transfer money and make payments
- Shopping safely online
- Online password security
- Age UK's digital instruction guides
- Back Discrimination and rights
- EU citizens and settled status after Brexit
- Help for Ukrainian nationals in the UK
- Human rights
- The Equality Act
- Windrush Scheme
- Your rights at work
- Back Education and training
- Build up your skills
- Classes and courses
- Higher education and university
- u3a – Later life learning
- Back Looking for work
- Be your own boss
- CVs and job applications
- Job interview tips
- Back Retirement
- Preparing emotionally for retirement
- Paul Lewis: Retirement planning advice
- Living abroad after retirement
- Retirement age
- Back For professionals
- Benefits hub for professionals
- Mental health hub for professionals
- Winter hub for professionals
- Information guides and factsheets
Age UK Advice Line 0800 678 1602
Free to call 8am – 7pm 365 days a year Find out more
Telephone friendship
Get a free weekly friendship call. We'll match you with one of our volunteers. Our service is flexible to suit the different needs of everyone who takes part.
- Sign up for telephone befriending
- Find services near you
- Find charity shops near you
Popular services
- Age UK Advice Line
- Befriending services
- The Silver Line Helpline
- Day Centres
- Exercise and physical activity
- Handyperson services
- IT Training
- Social activities
- Back Services
- Back Get involved
- Back Donate
- Make a donation
- Back Leave a gift in your will
- How to leave a gift in your will
- Making and amending your will to include a gift to Age UK
- Information for executors
- The difference a gift in your will could make
- Ways to write your will
- Free Wills Month 2024
- Will Aid 2024
- Back Donate to our shops
- Age UK and The Wombles join forces
- Age UK's eBay store
- Sustainability
- Back Donate in memory
- Make a donation in memory
- Fundraise for Age UK in memory of your loved one
- Make a one-off donation
- Funeral donations and collections
- Set up a Tribute Fund
- Meaningful ways to remember your loved one
- Make a major gift
- The difference your money makes
- Our professional fundraisers
- Back Fundraise
- Back The innocent Big Knit – get knitting for charity
- innocent Big Knit updates
- Back Sporting events
- Run for charity
- Skydive for charity
- Cycle for charity
- Charity walks and treks
- Charity triathlon events and obstacle courses
- Do your challenge for Age UK
- Back Fundraising ideas
- Most popular ideas
- Sporty ideas
- Fundraise at work
- Fundraise at school
- Fundraise while you celebrate
- Fundraise as a community
- Let's get fundraising
- Pay in your fundraising
- Fundraising resources
- Leeds Abbey Dash
- TCS London Marathon
- Back Stream for Ages
- Your free downloads
- Back Lottery and raffle
- Play the Age UK lottery
- Tuesday Treat Draw
- Play the Age UK raffle
- Gift the Lottery
- Player Zone
- How every entry helps
- Are you a winner?
- Lottery and Raffle rules
- Back Volunteering
- Telephone Friendship Service volunteering
- The Silver Line Helpline volunteering
- Connect and Support Service volunteering
- Age UK shops volunteering
- Local Age UK volunteering
- Support our campaigns
- Back Corporate partnerships
- Why partner with Age UK
- Back Ways we could work together
- Can your company support the Age UK Telephone Friendship Service?
- Latest jobs with Age UK
Age UK. Know what to do.
Last year, over 10 million people trusted us to help them with some of the biggest issues in their lives. Learn more about how we help.
How your support helps
Here's how, with your support, Age UK is supporting older people through the cost of living crisis.
- See the difference your donations make
Making older people's voices heard
- Age UK know what to do
- Campaigning with older people
- Discover - news, stories and features
- Media Centre
- Policy and research
- Wellbeing programmes
- Politics and government
- Back Our impact
- Back Buy products
- Back Over-50s Insurance
- Car insurance
- Home insurance
- Motor breakdown cover
- Travel insurance
- Travel insurance with medical conditions
- Back Independent living
- Bathing Solutions
- Stairlifts and Homelifts
- Personal Alarms
- Back Financial services
- Funeral Plans
- Legal services
- Back Healthcare
- Incontinence products
Health services
Although your GP doesn’t need to be your first point of contact if you're feeling unwell, everyone should be registered with a GP. If you're not, you should register with a practice as soon as possible, even if you don't currently have any health problems.
What does a GP do?
What services should i look for in a gp surgery, how do i register with a gp surgery, what if i'm too ill to visit my gp, what if i'm not registered with a gp or i'm away from home, what support can i get if i have a long-term condition.
Your General Practitioner (GP) can give you medical advice, treatment and prescribe medication.
Your GP can also refer you to other healthcare professionals to diagnose or treat specific aspects of your condition. For example, they may refer you to a chiropodist, for a hearing test, or to your local falls prevention service. These other health professionals may visit you at home or hold clinics at a local practice, health centre or hospital.
Your GP practice must allocate everyone a named, accountable GP. This GP will oversee your care and take responsibility for evaluating your current physical and psychological needs. Though this doesn’t mean the named GP is the only doctor at your practice who will or can provide care.
If you're joining a new surgery, ask about the availability of services that may be important to you, such as:
- how the appointment system works
- how far in advance you can book a non-urgent appointment
- extended opening hours
- support for carers
- availability of male and female GPs and nurses
- wheelchair access
- staff who speak languages other than English.
Some surgeries offer a 24-hour online service, which you can use to book appointments with a GP of your choice, cancel appointments, order repeat prescriptions and view your summary care record. Speak to the receptionist to find out what online services your GP surgery offers and how to register for online access.
If you have difficulty finding a practice with space for new patients, contact NHS England – it's their responsibility to find a GP practice for you.
Find out more about online services on the NHS website
You can register with a GP surgery over the phone, online or in person.
You don't need proof of ID to register with a GP, but you may find it helpful to have your passport or birth certificate handy while you're filling in your details.
Find out more about registering with a GP on the NHS website
If you can't visit your GP surgery for medical reasons, you can ask your GP to make a home visit. If possible, try to call your GP in the morning if you think you'll need a visit the same day. Your GP surgery should have accessible information explaining how to request a home visit.
If you need to see your GP but can't make it into the surgery, they must offer a home visit instead. They should factor in how urgent your condition is when arranging a home visit.
Your GP might also be able to give you advice through a telephone or video consultation as an alternative.
You should always be able to see a GP if you need urgent attention. If you become ill while you're away from home or you haven't registered with a GP, you should contact the nearest surgery and ask them to see you.
If you'll be living away from your usual address for up to 3 months, you can register as a temporary patient at a local practice. You'll still be able to remain registered as a patient with the GP where you normally live.
If you have a long-term condition, your GP should help you understand and manage your own care. This may include drawing up a care plan to help you manage your condition on a day-to-day basis and recognise symptoms that you should report to your GP.
It may also include creating an 'information prescription'. This is a collection of information that your GP thinks is helpful to you at that time and will help you understand your condition, as well as ways to prevent any further complications. This can be done with the help of the NHS website, which helps you find reliable sources of information about your condition.
Want more information?
NHS services factsheet (828 KB)
- Find out more about what you can expect from NHS services
- Visit the NHS website
- Find out how to contact NHS England
We're here to help
We offer support through our free advice line on 0800 678 1602. Lines are open 8am-7pm, 365 days a year. We also have specialist advisers at over 120 local Age UKs.
About the Age UK Advice Line Find your local Age UK
Share this page
- Share on Facebook
Last updated: Apr 08 2024
You might also be interested in...
Regardless of age, very few people feel well all the time. Here are some ways you can get help when you're ill.
Find out more about your rights and responsibilities as a patient in the NHS Constitution.
Find out more about some routine health checks that are quick to perform and can help you spot signs of illness.
Find out more about how to prepare for a hospital stay and what you can do to prepare your home for your return.
You have the right to expect good quality services from the NHS. Find out how to make a complaint about NHS services.
Find out more about NHS continuing healthcare for people who have significant ongoing healthcare needs.
Become part of our story
- Please enter a valid email address
Back to top
REcent Updates
Making sense of Medicare isn’t easy. Parts, A, B, C, D; HMOs; PFFS plans; SNPs. Navigating the system can feel like learning to code… blindfolded… with one hand tied behind your back. The point is, it can be overwhelmingly complicated. But at MD at Home one of our goals is to make quality healthcare easier to access and understand, so in this post we’re decoding the ins and outs of Medicare Advantage Plans, from A to Z.
No one wants to think about the likelihood of unfortunate events. Death, accidents, illness - we avoid these topics like the plague (both literally and figuratively). Why? Because they make us sad, because they make us uncomfortable, because sometimes superstition gets the best of us and we don’t want to tempt fate. But as difficult as they may be, these are important conversations to have with your loved ones or potential caregivers now, so that if and when the time comes, your wishes are clear. What we’re talking about is an advance healthcare directive. Here’s everything you need to know.
In 1930, house calls were standard practice for physicians, accounting for approximately 40 percent of patient visits. By 1950, this number had fallen to 10 percent, and by 1980, only about 1 percent of patient visits happened in the home. But as they say, everything old is new again, and with the coming demographic changes, it seems doctors may be making more home visits in the near future.
Diabetes and depression can each be conditions with devastation consequences on their own, let alone when a single individual suffers from both. Often times, the symptoms of one can exaggerate and accelerate the symptoms of the other, but fear not! There are a few simple steps you can follow to alleviate the symptoms and prevent the onset of both.
MD at Home provides home care, home medical doctors, and housecall physicians to patients in need with a focus on p reventing readmissions during the transition from an acute care setting to the home. For over 20 years, we’ve served as the premier healthcare resource for primary care and geriatric medicine for homebound patients in the Chicagoland area. Partnering alongside some of Chicago’s most established and respected institutions, we tailor our programs toward modern guidelines with an unwavering focus on clinical excellence, patient satisfaction, and measured clinical outcomes. Our continuum of care and individual care plans highlight the importance of readmission reduction and high level transitions from the hospital to the home setting. MD at Home is transforming healthcare through our collaborative, proactive, and preventative approach to patient health.
Our approach reduces unnecessary hospitalizations and focuses on helping patients and caregivers better manage individual health from the comfort of their home. Through our expertise in primary care and geriatric medicine, our licensed clinicians deliver a comprehensive approach in the management of chronic conditions to homebound patients, and our highly trained physicians and nurses are certified to perform most of the same services offered in a physician's office. MD at Home is transforming reactive, crisis-oriented care into proactive, preventive medicine, reducing unnecessary emergency room visits, hospitalizations, and 30-day readmissions.
Who Qualifies for a Housecall Visit?
Patients with difficulty leaving home due to a mobility limitation, patients with difficulty leaving the home due to cognitive impairment, patients who require the use of special transportation to leave the home, patients with an inability to leave the home and for whom leaving the home requires taxing effort, patients requiring the assistance of another person to leave the home, patients for whom leaving the home is medically contradictory due to the patient's medical condition, accepted insurance.
MD at Home accepts the following insurance policies:
- Medicare Part B
- Medicare Pametto GBA
- Blue Cross Blue Shield (XOF, R, XOX)
- Blue Cross Blue Shield (XOS - Must have Medicare Part B as primary insurance)
- Aetna (PPO)
- United Health Care (PPO)
- United Medical Resources (PPO)
Physician Careers
MD at Home is hiring Physicians and Nurse Practitioners. Physicians with MD at Home have a luxury many other medical doctors severely lack: time . Unlike a typical seven minute visit, our physicians spend an hour or more with each patient, gaining a holistic view of the patient's health within their native environment. This not only means more insight into the patient's daily life, but also into their care support system, including interacting with family members and caregivers. This not only leads to better care for patients , but better lives for our doctors. Our physicians only work typical workday hours, allowing them to spend more time with their families, avoiding obscure hospital rounds or late nights. Our physicians using cutting-edge EMR technology to maintain up-to-date health records for each and every patient so nothing gets lost in the shuffle.
A Letter to Physicians
More time with patients, more time with your family, move healthcare forward, schedule a home visit, fast. simple. secure..
Our HIPAA-compliant online referral system is secured with 256-bit AES encryption, the same encryption level used by most online banking systems and the same SSL technology that fuels most SecureFax systems already in use by hospitals. Prefer to schedule a visit by phone? Give us a call at (312) 243-2223. If you're a healthcare professional, please send additional medical documentation to our fax at (312) 243-8450.
HIPAA Certification Security Audit
Prefer to submit a referral by fax? Click the button below to download one of our paper referral forms and fax it to (312) 243-8450.
Area of Service
Our address.
Referral Fax: (312) 243-8450 Clinical Fax: (312) 243-2227 2003 W. Fulton Street, Suite 303 Chicago, IL 60612
Office Hours
Patient Portal Phone: (312) 243-2223 Monday – Friday 9:00AM – 5:00PM Closed Saturdays and Sundays

House Call Doctor Visits Make Life Easier for Seniors and Caregivers

Important: This is an informational article to explain how house call doctor visits can benefit seniors. DailyCaring isn’t a medical organization, we aren’t medical professionals, and we aren’t affiliated with any healthcare organizations. We aren’t qualified to respond to any medical questions.
House call doctor visits benefit older adults and caregivers
Getting your older adult to the doctor’s office for an appointment can be difficult or sometimes impossible.
Whether they’re frail, can’t walk on their own, or have Alzheimer’s or dementia , getting out of the house is hard on both of you. Going to a doctor’s office can also expose seniors to germs or harsh weather.
We explain what a house call doctor is, what type of insurance they accept, how to find one, and what to look for in terms of services.

What is a house call doctor?
Today, many doctors are bringing back the old practice of visiting patients in their homes. With house calls, older adults don’t have to go through the stress and difficulty of getting to the doctor’s office. And neither do you.
Another bonus is that these doctors usually spend more time with patients. You won’t have to fit all your questions into a 15 minute visit.
Do they accept Medicare?
Yes, many house call doctors accept Medicare , private insurance, and sometimes Medicaid . It usually costs the same as a regular office visit.
But every house call doctor is different, so make sure you understand their fees and accepted insurance plans before making an appointment.
How to find a house call doctor
Some large health care systems like Kaiser Permanente or the VA have programs that include home visits by doctors and nurses. For example, Kaiser’s home-based palliative care program includes house calls.
Even your older adult isn’t part of a large health network, it’s worthwhile to ask your older adult’s doctor if they have home doctor visit programs.
The American Academy of Home Care Medicine’s provider directory is another way to locate a house call doctor in your area.
You can also use Google to search for “house call doctor” + your city or county or “home doctor visit” + your city or county (don’t include the quotation marks).
What to look for in a house call doctor
Before booking an appointment, make sure you understand the doctor’s services, fees, and billing.
Questions to ask:
- Do you specialize in treating seniors, people with Alzheimer’s or dementia , or those with multiple chronic conditions ?
- Do you accept Medicare , Medicaid , or my older adult’s private insurance plan?
- If we want, can we also keep my older adult’s primary care doctor?
- Will you communicate with my older adult’s existing doctors and specialists so their care is coordinated?
Examples of house call doctor private practices
We want to be clear that we’re not recommending any specific home doctor services or companies and aren’t affiliated with any of these businesses. These are examples to give you an idea of what a house call doctor looks like and the type of services that are typically offered.
Examples of what a house call doctor looks like:
- Visiting Physicians Association (VPA)
- Bay Area House Call Physicians
- Kindred House Calls
Recommended for you:
- 4 Expert Tips for Managing Multiple Chronic Health Conditions in Seniors
- 7 Tips for Helping Seniors at the Doctor: Being a Health Advocate
- Should Seniors See a Geriatrician?
By DailyCaring Editorial Team Image: Now It Counts
This article wasn’t sponsored and doesn’t contain affiliate links. For more information, see How We Make Money .
- Share Article on:
Related Articles

Prevent Falls with 5 Warning Signs of Mobility Issues in Seniors

4 Great Sources of Tasty Low Sodium Recipes for Seniors

5 Questions to Ask Doctors About Tests and Treatments for Seniors

4 Common Eye Diseases That Cause Blindness in Aging Eyes
18 comments, tony carrancho.
My parent s lives in [redacted for privacy]. How do i get started locating a house call doctor. I am pretty sure there insurance covers this. Thank you. TONY
DailyCaring
We hope the tips and suggestions in the article above will help you find a house call doctor in your parents’ local area.
Susan Quercio
My 95 year old father has a deep cough and he is disoriented. Temp 99 degrees.
Please contact your father’s doctor immediately or the local hospital to find out how to safely get him examined by a doctor (to reduce risk of exposure to Covid-19).
DailyCaring isn’t a medical organization, we aren’t medical professionals, and we aren’t affiliated with any healthcare organizations.
Ruby m VanNostern
I live in [redacted for privacy] and need a doctor visit in home.
This article includes suggestions for how you can find house call doctor services in your area. At DailyCaring, we aren’t doctors and don’t provide any medical services. We hope you’re able to find a great house call doctor in your area.
Stewart Goldman
need Doctor for a home visit Andrews N.C.
Joseph Artusa
I need a doctor
Linda Williams
I was released from the hospital on Thursday after 5 days.I am not able to go to Dr office but most definitely need to be checked.Still having breaking problems and am very week.I have severe asthma and blood pressure was running very high from so much steroids.Could I possibly get help.Thanks so much.
I’m so sorry to hear that you’re not feeling well. Since you’re noticing some issues with your recovery, it’s essential to call your primary doctor immediately. Since they’re the ones who have been treating you and are familiar with your recent hospitalization, they’re the best people to advise you on what you need. If you need help getting to your doctor’s office, you may want to contact your local Area Agency on Aging or a ride sharing service. Or, use the tips in this article to search for a doctor in your area who makes house calls.
Here are some articles that may be helpful: — 8 Ridesharing Services for Seniors https://dailycaring.com/8-ridesharing-services-for-seniors/ — 6 Affordable Senior Transportation Options https://dailycaring.com/6-affordable-senior-transportation-options/ — Local Community Resources for Seniors and Caregivers: Area Agency on Aging (to connect you with local organizations that may be able to help) https://dailycaring.com/local-community-resources-for-seniors-and-caregivers-area-agency-on-aging/ — 4 Ways to Know If Seniors Need to Return to the Hospital https://dailycaring.com/4-ways-to-know-if-seniors-need-to-return-to-the-hospital/
(DailyCaring doesn’t provide any services and isn’t affiliated with any medical providers.)
What areas do you service?
This article explains that house call doctor services are available and could help senior and caregivers. We also share suggestions for finding one in your area, but we do not provide any services ourselves. I hope you’re able to find a great local house call doctor!
What areas do you service
This article includes suggestions for finding house call doctor services in your area. We at DailyCaring aren’t doctors and don’t provide any medical services. I hope you’re able to find a great house call doctor in your area.
need a home care doctor
I hope the information above helps you find a great home care doctor in your area.
Leave a Reply Click here to cancel reply.
Cancel reply.
- Research article
- Open access
- Published: 22 April 2011
Home visits - central to primary care, tradition or an obligation? A qualitative study
- Gudrun Theile 1 ,
- Carsten Kruschinski 1 ,
- Marlene Buck 1 ,
- Christiane A Müller 1 &
- Eva Hummers-Pradier 1
BMC Family Practice volume 12 , Article number: 24 ( 2011 ) Cite this article
16k Accesses
38 Citations
1 Altmetric
Metrics details
Home visits are claimed to be a central element of primary care. However, the frequency with which home visits are made is declining both internationally and in Germany despite the increase in the number of chronically ill elderly patients. Given this, the question arises as to how to ensure sufficient primary health care for this vulnerable patient group. The aim of this study was to explore German general practitioners' (GPs) attitudes with regard to the feasibility, burden and outlook of continued home visits in German primary care.
Qualitative semi-structured interviews were carried out with 24 GPs from the city of Hannover, Germany, and its rural surroundings. Data was analysed using qualitative content analysis.
The GPs indicated that they frequently conduct home visits, but not all of them were convinced of their benefit. Most were not really motivated to undertake home visits but some felt obliged to. The basic conditions covering home visits were described as unsatisfactory, in particular with respect to reimbursement and time constraints. House calls for vulnerable, elderly people remained undisputed, whereas visits of a social nature were mostly deleted. Urgent house calls were increasingly delegated to the emergency services. Visits to nursing homes were portrayed as being emotionally distressing. GPs considered good cooperation with nursing staff the key factor to ensure a successful nursing home visit. The GPs wanted to ease their work load while still ensuring quality home care but were unable to suggest how this might be achieved. Better financial compensation was proposed most often. The involvement of specially trained nurses was considered possible, but viewed with resentment.
Conclusions
Home visits are still an integral aspect of primary care in Germany and impose a considerable workload on many practices. Though the existing situation was generally perceived as unsatisfactory, German GPs could not envisage alternatives if asked to consider whether the current arrangements were sustainable in the future. To guarantee an unaltered quality of primary home care, German GPs and health care policy makers should actively initiate a debate on the need for and nature of home visits in the future.
Peer Review reports
Home visits are claimed to be a central element of general practice as this represented the primary mode of healthcare delivery by community physicians from the mid-20 th century [ 1 ]. Today in most European countries and the United States home visits are the exception and are no longer the standard method of health care delivery - although there is diversity between individual general practitioners (GPs) and different countries [ 2 ]. Self-employed GPs visit more patients at home than salaried GPs; house calls are less frequent in health care systems where GPs act as gatekeepers and patient lists are maintained [ 2 ]. Male GPs make more visits than female doctors, but the latter take more time per visit. In every system there are opponents and supporters of home visiting, e.g. in the United States special house call practices are run. There are however two facts common to all countries and doctors: the number of home visits is continuously declining while the primary target group, namely older, multimorbid people, is growing.
These contradictory findings are the results of several studies published in the last two decades, which have analysed the number of home visits from either quantitative surveys or practice data. They are also true for Germany. However, an analysis conducted at our institute has demonstrated that, despite an overall decreasing frequency of house calls, the number of house visits per home patient has been stable [ 3 ]. This finding has supported the assumption of other authors that only house calls of questionable medical importance have been eliminated [ 2 , 4 ].
Despite these considerations, the number of house calls in Germany is still comparatively high with a mean number of 34 visits per GP per week. In Austria, Benelux, and France more than 20 visits were counted on average [ 2 ]. At the same time many GPs complain of the heavy workload, the insufficient remuneration and the minimal benefits associated with home visiting. Boerma stated nearly ten years ago that patients prefer home visits much more than their doctors do. As the German primary health care system is dominated by self-employed GPs and is thereby competitive, patients' perspectives undoubtedly account for the German "traditionalism" with respect to home visits. But what are incentives for German GPs to continue or discontinue to make home visits? Who do German GPs visit at home and why? Do German GPs prefer this "delivery service" or can they suggest other models of care? Answers to such questions may be meaningful in the context of considering new potential home care models. Thus, the aim of this study was to explore the attitudes of GPs with regard to the feasibility, burden and outlook for home visits within German primary care in the future.
We chose a qualitative approach as our study focussed on subjective GPs' attitudes. As we wished to create a relaxed atmosphere that would allow the GPs to speak freely, we conducted semi-structured interviews at GPs practices or homes.
Participants
Our intention was to create a purposive sample balanced for the following characteristics: gender, years of occupation, practice location (urban/rural) and practice size (less/more than 2000 patients per quarter). GPs with an entry in the telephone book were contacted initially by telephone and subsequently, if the above mentioned characteristics were compatible, in writing. If a GP was willing to participate, a second call was organised in order to provide more detailed information about the topic and the aim of the study, and to schedule an appointment for the interview. Participants received no remuneration.
The development of the interview guideline was steered by the goal of obtaining opinions, facts and ideas related to home visiting. Potential points of interest and the wording of the questions was discussed by the two main researchers (GT, MB) and finally agreed. The following aspects were included: motivation and organisation of home visits, home visits in nursing homes, procedure and organisation, future perspectives. In addition, the interview started with a provocative warm-up question; a conclusive question at the end allowed a short résumé. (The elaborated interview guideline is depicted in Table 1 .) Two pre-tests were conducted to check comprehensibility and fluidity of the guideline. Its final version was condensed into a list of catchwords that were serving as memory hooks representing the detailed questions in order to create a natural conversation. The interviewer (MB) was trained in communication skills. In addition to voice-recordings, handwritten memos were taken in order to document specific or important aspects of each interview. After the interview, GPs filled in a short questionnaire to provide demographic data.
All interviews were digitally recorded and transcribed verbatim by the interviewer herself. Data analysis was conducted independently by two researchers (GT, MB), one of them using ATLAS.ti software, the other coding "by hand". The basis of the analysis was a predefined system of categories, which were generated by the interview guideline. This categorising system was enhanced by codes, which emerged from the text material and were agreed by both researchers after exhaustive discussion and consideration of the additional information from the handwritten notes. In situations where it was not possible to resolve a disagreement, a third researcher was involved until consensus was obtained. By using this iterative approach we refined the initial categorising system and built new codes and subcategories that accounted for themes or aspects of specific topics that had not been considered previously. Furthermore, we analysed some data from the text quantitatively, i.e. number of home visits per week, length of the visits, radius (km) around the practice for home visits as well as demographic data.
A total of 24 GPs agreed to be interviewed, 13 of them male. The median age was 54 years (interquartile range IR 38 - 57 years); the median number of years in private practice was 13 years (4 - 22 years). The GPs came from 14 practices located in Hannover City and 10 in surrounding rural areas. As GPs from group practices were much more likely to agree, single handed practices or group practices consisting of just two partners were underrepresented in the final sample (20.8%). One half of the participating GPs worked in practices with more than 2000 patients per quarter. The mean interview duration was 40 minutes.
Text Analysis
In the following we describe the theoretical framework, which evolved from the coded text material. The first sub-section is about quantitative data collected during the course of the interviews. Although these numbers cannot be representative, they give an impression of the workload and performance characteristics associated with home visits carried out by the interviewed GPs. Subsequently, different types of home visits, as described by the interviewees, are illustrated; house calls in nursing homes represent a specific category. Lastly, motivational and negative factors are discussed together with ideas for the future of house calls and home care.
Home visits in numbers
The average home visit conducted by the interviewed GPs lasted 25 min (IQR 17.5 - 30), and took place in the patient's home within a radius of 6.5 (IQR 3-10) km from the practice. The median of the number of home visits per week carried out by a single GP was 6.5 (IQR 3-17.5). For further information regarding the GPs see Table 2 . Female GPs conducted considerably fewer home visits than their male colleagues, but they invested more time per visit. The workload resulting from house calls was highest within the group of rural GPs. They required more time per house call and visited more patients per week compared to urban doctors. GPs with more than 20 years of experience conducted fewer home visits than more junior colleagues.
Types of home visits
One of the interviewees provided in his own words a very structured differentiation and definition of three types of home visits, which were relevant to most of the other interviews.
"Some of the home visits are of a supportive nature, they actually represent the need for "social interaction" and there isn't a real medical indication. Another class of home visit is to those people who really do need medical care either because they are chronically ill or find it difficult to come to the practice. And then there are those home visits, which are requested due to acute diseases which can be anything from gastrointestinal infection, influenza infection, pneumonia....."
Thus, GPs distinguish between supportive home visits, routine home visits and urgent home visits.
Supportive home visits
Home visits of a supportive nature seem to be more important to rural GPs than to those from urban areas. Provincial GPs often perceived themselves not only as medical advisors but also as real companions for their patients. Such traditional professional ethics, which sometimes cross the boundaries of self-abandonment, were rejected by most urban GPs.
"It wasn't my aim to be a minister. In my opinion it's a social problem, which has been cultivated by all of us for decades. But it's not a physician's job to solve this problem."
Business competition in districts with a high density of GPs is apparent. Home visits are reimbursed poorly in Germany and those without any medical indication are avoided.
Most urban GPs deny conducting home visits of a supportive nature, although there is a smooth transition between supportive and routine home visits.
"I have to admit that some time ago, we were more generous with home visits. If there is an old lady with a decubital ulcer or a tumour, then, of course, we still make a routine visit to her. But we don't travel to see all the elderly once a week so that all the elderly in our town get used to a doctor's visit happening every week - that we won't do."
"That is the point: what has changed in the patient? Does he somehow appear different from the last time? Does he have complaints he didn't mention on the telephone? If there's nothing, then there's some small talk, a little social support."
Routine home visits
Routine home visits for older chronically ill and increasingly immobile patients are the least challenged visits. All interviewed GPs appreciated the usefulness of routine home visits to detect changes in patients' health status, to control drugs or to achieve an overview of the adequacy of the situation at home.
"Well, you have to listen to how the patients are getting on. You've known them for some time. These are home visits you repeat again and again. You look at how they are doing. You ask after their family, their kids, what they always talk about. You have to know the social environment. You have to look not only if they are alright but also you have to look why he's not on form. Whether he's not got a place in a retirement home or such things for example. Of course you need to talk to them about such things."
Urgent home visits
These visits are characterised by an urgent, sometimes immediate need. Most practices have developed an approach to filter the objective requirements related to the patient's concern. Mostly this was done by the GP himself, but in some practices the medical assistants were trained to perform triage on the telephone.
"Yes, you'll assess what awaits you a bit on the telephone. What's good is that we know the patients. For it's either the worsening of a chronic condition, which you can quickly bring under control, or an infection with a high fever or acute diarrhoea. Some call the GP for such illnesses, others don't. In such situations it's possible to establish on the phone, can I help here?"
Only a few of the interviewed GPs left their practice during consultation hours to travel to an extreme case, occasionally after having concurrently informed the emergency services. These GPs argued that no one else knew the medical history of the affected patient as well as they did, and considered themselves the most competent first aider. Most of the other GPs, especially the urban doctors, tended to delegate the real emergency cases -those that could not be delayed- to the emergency services. These GPs rated their competency in real life-threatening situations poorly. They viewed this approach as more reasonable, both with regard to the medical care of the patient and potential economic consequences.
"Well, if I rush out, everything would become so confused - also with the scheduled appointments of other patients and so on. I can't afford that."
In case of febrile exacerbation of an infection or other acute but not life-threatening conditions, most GPs offered their visit after consultation time or during lunch break, and some asked their patients to consider a practice visit regardless of the acute symptoms. Thus, many GPs aimed to reduce the workload associated with urgent house calls.
Home visits in nursing homes
All of the interviewed GPs conducted visits to nursing homes. However, those working single-handed in a practice limited this type of house call to a very small number, just caring for a few selected patients. Whereas GPs from group practices, in particular with more than two partners, cared for a greater number of patients in nursing homes. The average GP of our interview group visited 20 nursing home patients per week within 1.7 hours. In this context, the physicians reported that they did not see every single patient but conducted mainly chart reviews.
"And I do need two and a half hours for 30 patients (....) so that's five minutes per patient. This is not much. Generally, I don't visit every single patient but only those with acute problems."
Visits in nursing homes were perceived to be quite similar to ward rounds in hospitals. They normally lacked the intimate and confidential atmosphere of a doctor's visit in his patient's home. In most cases, a nurse accompanied the doctor and sometimes family members with their own concerns were present.
Therefore cooperation with the nursing staff was an aspect broadly discussed by many of the interviewed GPs. Most of them described having "trained" the nurses of the regularly visited old people's homes with regard to appropriate telephone calls and preparation for their visits. Experienced nurses seemed to be crucial for successful cooperation, but a shortage of staff and employment of unskilled helpers were frequent problems:
"Most of the nurses are well trained and good natured. For financial reasons staffing is kept to a minimum and this is causing problems."
"There are people who know what to do, but there are also housewives and career changers, who panic and immediately call me or the emergency doctor, when someone has high blood pressure."
The everyday care and examination of a patient's health status was accomplished by the nursing staff, whereas the interviewed GPs often defined their role in nursing homes as "supervisory". Therefore, some of them applied for the right to also oversee the quality standards of the nursing homes, which included the minimum standards concerning staff training.
When reporting on nursing home visits nearly all of the interview partners used remarkably emotional language. No other aspect of the interview guide provoked so many emotive, mainly negative, statements.
"It sometimes reminds me of "One flew over the Cuckoo's Nest."
"It's always about excrement, the whole day, from morning till night."
Nursing homes were described as places of resignation, despair and sadness; they appeared to be sterile, depressing and awful. The interviewed GPs' impression was that nursing home residents were living in forced circumstances and didn't take any notice of each other. A synopsis of all the comments used to describe visits to nursing homes is provided in Table 3 . While several GPs mentioned that the nursing homes themselves, i.e. the buildings and facilities had become more pleasant during recent years, only one (female) interviewee was enthusiastic about nursing home visits: "It gives me fulfilment!" She judged these visits, in her role as a GP, as her personal contribution to society. For the other interviewees house calls in nursing homes were an obligation as a result of ethical or financial considerations. Most interview partners did not wish to find themselves in a nursing home in later years.
"I mean, if I knew my children didn't want me to live as an invalid in the area or around the corner, then of course I would have to look out a nursing home. But if I had the choice I would prefer to be run over by a bus."
Motivation for home visits
When asked about their motivation for undertaking home visits, most GPs started with quite vague and general statements, along the lines of: home visits come with the territory.
"It's true, doing home visits is simply part of the job."
"Home visits are obligatory, if you become a general practitioner you have to be prepared to do home visits."
"It's in the nature of the GP's job to be on call."
However, some of the interview partners had good reasons to conduct home visits rather than simply feeling obliged to. For example, the exploration of a patients' home setting and the experience of working in an unfamiliar environment, as opposed to the safe surroundings of their own practice were mentioned in this context.
"And you have a peek on this chaos, a mum with her two kids - there is also a dog bustling around and two cats. Then it's quite clear why these kids have asthma. Father is a smoker. These are things you don't quite realise in your practice, although you can enquire about. But by conducting a home visit you see this at a glance and that's great."
"This is a completely different situation. It's the patient's home. He is the boss and controls the situation. Here in my practice, I do things a certain way and the patient is often very meek. But in his home, he acts completely differently, more independent, and more self-sufficient."
The more positive aspects of performing home visits are summarised in Table 4 .
The aforementioned reasons promoting home visiting can not hide the fact that this mode of primary care delivery is not very popular. Just one-third of the interviewed GPs declared that they liked to conduct home visits, the remainder did not.
"It's not the right question [to ask if I like to conduct home visits]. But instead does it make sense to undertake home visits or not? I don't think anybody really likes to do house calls."
When asked for reasons as to why GPs feel reluctant to visit their patient at home pragmatic reasons were initially mentioned.
"Because it is difficult. You are out and about in terrible weather, when it rains or is windy. Most of the people have an awfully untidy apartment. Elderly people always have the windows closed. It's always extremely warm and when you come out you're always sweaty and sticky."
"Then most of the patients - some though are lying in their beds - I have to access in the corner of the living room behind the table in order to get near them. Or I have to move furniture to get to them. I have even visited people in loft beds or in cubby holes, which I have had to crawl into on all fours."
Home visits can put GPs in unpleasant or occasionally even dangerous situations. Moreover, some GPs felt exploited by their patients.
"Yes, I mean, if I'm stressed and have to drive somewhere to an urgent visit, then I sit in my car and complain to myself. My goodness, why can't that guy make a trip to my practice? Doesn't he have any relatives? They all drive to the hairdresser because it is too expensive for the hairdresser to come to them, but the GP can visit."
A couple of GPs referred to the restricted diagnostic options available in the domestic setting, others complained of the poor controllability of consultations in patients' homes. Some GPs even argued home visits promote social isolation because patients were not forced to go outside and meet people on their way to the doctor or in the waiting room. Home visits were perceived as very time consuming. Insufficient reimbursement of such visits in Germany was the most quoted reason for an unwillingness to perform them.
"Well, if I exclusively did home visits, I would go bankrupt. The more I do, the worse it is."
GPs expectations of an adequate payment for house visits were made on the basis of the fees craftsmen charged for their work. Locksmiths, electricians and television engineers were all envied for their hourly wages. Most interviewed physicians proposed a sum at least twice as high as the remuneration currently permitted.
The future of home visits
Whereas proposals for an adequate financing of home visits were made in sufficient numbers, ideas for the future of home visits rarely emerged. Although most GPs admitted that they conduct home visits reluctantly, they accepted their "duty" without looking for alternatives. Some though proposed the formation of a network of several practices to either reduce the workload of individual GPs or to permit the collective financing of a nurse practitioner who could conduct house calls. Such specially trained nurses were seen as the most favourable alternative to the current situation. In contrast, a district nurse who could also perform house calls was judged very cautiously. GPs suspected that this would introduce redundancy into the existing care arrangements.
"The idea to implement district nurses, I mean, that's fine, but to my eyes it's extremely important to ensure a very close connection to the doctor. The observation I have made is that nursing services, district nurses and all the others don't work together. That means we establish redundant structures. I believe it's very important that medical, nursing and preventive care is centralised."
In addition to concerns about interface problems, a certain fear associated with the establishment of multiple health care providers may also be relevant to statements regarding the future. There were GPs who, while they admitted that they had to get used to the idea of district nurses, nevertheless realised that the involvement of non-medical personnel was an indispensable requirement to cope with the care challenges associated with the anticipated demographic population changes.
Some GPs envisioned the involvement of public volunteers such as socially engaged neighbours to visit isolated elderly people. Few GPs anticipated the complete elimination of home visits. They predicted that in future all patients would be transported to practices somehow, or immediately to the hospital if necessary. This would be co-ordinated from a central office, which would also inform the respective GP about a particular patient's whereabouts and health status.
Home visits are still a component of normal general practice services in Germany. However, GPs are dissatisfied with the conditions associated with conducting them, especially reimbursement, and some doubt the additional value of home visits. A number of house calls are perceived as a "luxury" for demanding patients. Only house calls to vulnerable, elderly people remain undisputed. Home visits in nursing homes are often characterised as emotionally stressful. Despite these issues, the German GPs in our study lacked ideas, if asked about possible future alternatives to the current course of action, both in regard to house calls in patients' homes and to nursing home visits. The suggestions most often discussed included improved financial compensation for home visits and the involvement of nurses specifically trained to take on this duty.
The strength of our study is the good number of interview partners and the robust approach to transcript analysis. Qualitative research excels at the identification of subjective attitudes and experiences. The researcher tries to hold back his own assumptions in favour to record the knowledge of experts who are immersed in the field he wishes to learn more about. In this way, a wide range of relevant information and insights is gathered which may form the basis of further scientific research or influence policy. In this particular study we deliberatively focused on GPs' attitudes while ignoring the perspective of patients or health care policy stakeholders, because we wanted to ascertain the views of those who actually performed the home visits.
Our study also has some limitations. Single-handed practices are underrepresented in our sample, because they were less willing to participate. As the organisational and time constraints associated with home visits for those physicians is high, it can be presumed that they would have been even more critical towards this time consuming mode of primary care. Some of our interview partners from group practices admitted that, had they been in a single practice, they would not be conducting home visits. This is mainly because of the high organisational burden. If a single doctor is on a home visit, who is available to attend to unannounced patients at the practice? We assume that the reluctant willingness of single-handed practices to participate in our interview study corresponds to a reluctance to perform home visits or a desire to perform a smaller number of them. Moreover in future, most German general practices will be group practices because the number of single practices is constantly declining. Given this, the under-representation of single-handed practices in our sample not only seems to be "symptomatic" but also, at least with view to implications for policymakers, acceptable. However, we achieved saturation on all aspects of our interview guide and our findings are consistent with previous research published in this field, indicating a sufficient exploration.
Only the noticeable failure of our respondents to suggest ideas about the future of home visits could have been an indicator that our questions failed to elicit their ideas. It is possibly that focus groups could have been more fruitful with regard to this specific issue, as GPs would have had not only to consider their own experiences but to generate new solutions and to be "creative".
It should be emphasised that although many of our results are similar to those from other countries, it would be inappropriate to generalise. The aim of this study was to uncover the perceptions and issues faced by German GPs regarding home visits.
Of those GPs who participated in our survey, male GPs and those practicing in the countryside in particular routinely made a number of home visits per week. Whereas the frequency of home visits in rural areas seems to depend on the health care tradition of the respective country [ 2 ] - e. g. Aylin et al. reported a lower house call rate for the rural population in Wales [ 5 ] - the male dominance of those undertaking home visiting is a more "universal phenomenon". The same applies to the fact that female GPs visit fewer patients but spend more time with them [ 2 , 6 , 7 ]. Our sample of female doctors more frequently worked part-time. But we assume that a different, more patient-centred female working culture is also relevant to the reduced number of patient contacts associated with longer consultation times. Unlike colleagues from the United States [ 8 ], none of our interview partners referred to the risk of meeting potential aggressors during home visits. Therefore, at least in Hannover and its surroundings, the fear of attack didn't seem to be a critical issue with regard to the smaller number of home visits made by female GPs. Although most international studies reveal higher home visiting rates for experienced GPs [ 2 ] in our sample the younger doctors conducted many more house calls than their older colleagues -probably because German practice owners tend to delegate home visits to their vocational trainees. Svab et al. (2003) reported a similar trend in the Slovenian primary health care system of young residents losing their interest in home visits after completing their training [ 9 ].
There is consensus in literature that home visits should be carried out for the old and frail, and critically ill patients [ 3 , 4 , 10 – 15 ]. The respondents of our study therefore acted similarly to the majority of their colleagues in Europe, USA and Canada. Nevertheless, house calls for the elderly living at home in Germany were not always of a medical nature and this is also true in other countries [ 16 ]. This type of visit was debated by many GPs: whereas some physicians believe this form of interaction not only pleases the patient, but it additionally establishes and improves the reputation for their practice, others propose that such house calls are completely dispensable as their omission would not reduce quality of care. Although supporting data were not available, it can be assumed that a considerable proportion of home visits in Germany are of a supportive social nature. GPs in our interview group as well as in other health care settings [ 17 ] responded to this by sharpening their criteria for home visits and "educating" their patients [ 18 ], but apparently they still responded to patients' needs [ 2 , 4 ]. Boerma et al. additionally remarked in 1996, that "the strong variation between individual GPs as well as countries in the practice of home visiting suggests a lack of urgency or a need for some of the visits." This "lack of urgency", seems to be true even for genuine emergency visits (those unscheduled house calls, which are made to people with acute conditions). According to our analyses, rural GPs regarded themselves as competent first-aiders because they possessed useful information about patients` history, while urban GPs tended to delegate such emergency house calls more and more to the emergency services. This was not only due to their concerns of dealing with a life-threatening situation when there is an excellent urban emergency ambulance system, but also for economic reasons. Leaving during consultation hours is problematic and if the visit can be delayed into lunchtime or after hours, the question arises if it would not be equally justifiable for the patient to contact a hospital ambulance. Nevertheless all German doctors including specialists working in the ambulant sector are legally bound to conduct home visits. Generally GPs more or less felt obliged to adhere to these regulations. Because of the high density of alternative emergency services, urban GPs seem to be more secure with respect to the consequences of not making home visits. None of the interviewed GPs though referred explicitly to potential liabilities associated with failure to make routine or urgent home visits. GPs may however hesitate to admit that such considerations would affect their decisions.
Although home visiting in the German health care system can be troublesome and may sometimes be a low medical priority, good reasons to perform home visits do exist. Those motives are more personal, accruing from daily work and experience with patients, and are based on a micro, rather than a macro level of health care. First of all, many of our interviewed GPs, similar to other studies [ 12 ], regarded home visits as an opportunity to gain additional information about a patient's living conditions, family dynamics and lifestyle. Moreover they additionally obtained a detailed insight into the patient's abilities and their compliance, especially with regard to taking their medication and/or safety issues. Undoubtedly, the direct exploration of a patient's environment yields valuable information, which may improve the quality of care. Some of our respondents concurred with several studies that indicate the potential of home visits to reduce, or at least better inform the suitability of hospitalisation [ 19 , 20 ]. Caplan et al demonstrated that elderly patients with different acute conditions treated at home rather than in hospital were less likely to develop geriatric complications as confusion, bowel or urinary problems. While the overall number of deaths did not differ significantly between the two environments, the patients' and care givers' satisfaction was significantly higher in the "at-home-group" [ 21 ]. A recent study from Brazil has also demonstrated the cost effectiveness of home visits in the treatment of alcohol dependent patients [ 22 ]. These scientific observations would seem to suggest that home visits deliver an enhanced quality of care and can be cost effective for people suffering from chronic conditions. However, reports describing the effectiveness of home visits by family physicians for a range of conditions encountered in General Practice are still lacking.
Both in our study and in others, the interviewed GPs frequently recognised the positive marketing effect of house calls. One of our interviewees stated that home visits "make patients happy" and there is some research evidence indicating that patients are more dissatisfied with their GP if they undertake fewer home visits [ 10 ]. GPs therefore have good reasons for home visiting, even if a strong medical reason does not exist. Boerma et al. showed that in countries where GPs are mainly salaried, the estimated average number of visits per week was much lower than that in countries, such as Germany, where GPs are usually self-employed. This finding suggests that the decision to undertake a home visit can be made more critically in a non-competitive health care system, and that many self-employed GPs will tend to yield to the concrete or assumed wish of their patients - be it for marketing purposes or for liability concerns. Court et al. commented on out of hours requests for GP visits as eliciting an "inappropriate fear of complaint, which is likely to potentiate inappropriate demand for visits" [ 16 ]. He concluded that further research should explore how this defensive medical practice could be modified to benefit both patient and practitioner. Nearly 15 years later in Germany, GPs admit to feeling obliged to carry out home visits because they "sell well".
Interestingly, the reason most frequently cited against visiting patients at home is also an economic one: GPs complained about the insufficient remuneration for conducting house calls. In the current German health care system, home visits receive minimal financial compensation and their suggested economic advantages through prevention of hospital admission or psychiatric crises do not have any direct financial impact on the service provided by GPs. Therefore GPs feel that satisfactory financial recompense is one of the most important changes needed with regard to the maintenance of this special form of patient care [ 17 ].
In Germany, nursing and residential homes for the elderly do not have their own on-site doctors. Thus as a rule, the GP who has provided care to the elderly patient up to this point will continue to do so after they move into the care home. Home visits to nursing homes differ notably from the "usual" house calls in that they rather resemble ward rounds in hospitals. GPs normally talk much more to the nurses than to their patients. The GPs interviewed in this study commented on the very high emotional burden associated with this sort of home visit. A variety of reasons attracted them to make house calls in nursing homes. These ranged from the relative ease and cost-effectiveness of making visits to multiple patients in one retirement home, to it being professionally ethical to continue to provide care to a long-term patient moving to such an environment; but never has it seemed a real vocation. None of the GPs in our interview group could imagine going to a nursing home themselves in later life. GPs are not specifically trained to work in a care home environment and it is challenging both professionally and psychologically. Therefore, it is not difficult to understand Katz et al. who postulated in 2009 on the creation of a nursing home medicine speciality in the United States [ 23 ]. He quotes that the marginal involvement of physicians impedes communication and their integration in nursing home culture, which has a detrimental impact on patient outcomes. Most acute illnesses are managed by telephone, which in the light of the medical complexity of the residents, may not be in their best interests [ 24 ]. These observations from the United States are applicable to the German situation given the claims of an interview partner in our study; one GP sought to be involved in the staff management of care homes in order to enhance quality of care of the elderly patients. Consequently we feel that a discussion about specialised nursing home physicians, similar to positions already established in the Netherlands [ 25 ], should be conducted more intensely and more open-mindedly than it is currently in Germany.
However, when asked to consider the future of home visits in general, the participants of our study failed to propose any significant ideas. Very few among them had considered reorganising home visits or even home care in the German health care system. The most frequently considered alternative was for home visits to be performed by practice nurses linked to their practice. In fact, the German primary care system is currently offering courses to specially train such nurses (e.g. Versorgungsassistentin in der Hausarztpraxis (VERAH ® , or Care Assistant in Family Practice) but such supporting personnel are not widely established and reimbursement has limited attractiveness. In this regard Germany is lagging behind other countries, where nurses are medically trained and actively involved in ambulant patient care, even sometimes acting as "substitutes" for doctors. Far less conceivable for the GPs of our interview group, was the engagement of an independent nurse to conduct home visits for multiple, but not necessarily linked general practices. This is despite finding that an initial project to establish whether such an arrangement would be attractive or even essential for undersupplied rural areas in Germany had good acceptance from both patients and the participating GPs [ 26 ]. A study from the United Kingdom showed that nurse practitioners could substitute for GPs in out-of-hours-calls without any deterioration in patient satisfaction or clinical management outcomes [ 27 ]. One of our respondents could see an abolition of home visits in favour of primary care centres, which patients attend and hospital ambulances would provide transport to if necessary. This is exactly what GPs from an English investigation rated as a possible alternative to out-of-hours visits [ 17 ]. Surprisingly, our interview partners did not suggest making more use of technology (e.g. telecommunication, computer guides to diagnosis and treatment) although it is likely to both be used in future home care and change the culture of home visits [ 28 ].
The results of our study indicate that a conscious discussion is needed on the pros and cons of home visits in their current form in Germany. GPs willingness to further conduct home visits under the existing conditions is rather small. However there are suggested advantages for primary home care, as economic savings by e.g. avoiding hospital admissions or to ensure health care for housebound elderly. Such presumed advantages must be critically addressed by further health care and economic research. Moreover, patients' perspectives on home visits and those of other stakeholders from the health care system will have to be explored. Another striking point is the GPs' attitude towards nursing home visits. Further research needs to evaluate the current situation in German nursing homes by assessing the attitudes and needs of patients and nurses. Our Institute of General Practice and Family medicine will contribute to this important, under-researched field by conducting a qualitative empirical analysis of interprofessional collaboration and communication in nursing homes. The planned study is funded by the German Federal Ministry of Education and Research. It will include 120 interviews with GPs, nurses, residents and their relatives, and additional direct observations and focus groups involving another 100 individuals from the various stakeholders. In this way we hope to achieve a broad insight into medical care in nursing homes.
What ever change future will bring to the home visit system as it now stands: the quality of primary health care must be maintained while an out-dated system will have to be modernised so that it can deal with the shifting population demographics.
While home visits in Germany seem to represent a primary care tradition and are rated to have clear advantages with regard to patient care they are nevertheless perceived as an obligation by many GPs. A conscious discussion on the pros and cons of home visits in their current form in Germany seems to be indispensable. Visits to nursing homes are perceived as emotionally stressful. Further research is needed to obtain a broad insight into GPs' (negative) attitudes towards nursing homes and to develop improvement strategies concerning primary home care. If home care by GPs is politically desired or recognised by society as the best way to ensure good medical care particularly for the very old and sick, appropriate financial incentives would effectively guarantee a continuation of this "tradition". To quote Leff et al.: Sentiment alone will not be enough.
Kao H, Conant R, Soriano TMW: The past, present, and future of house calls. Clin Geriatr Med. 2009, 25: 19-34. 10.1016/j.cger.2008.10.005.
Article PubMed Google Scholar
Boerma WGW, Groenewegen PP: GP home visiting in 18 European countries. Adding the role of health system features. Eur J Gen Pract. 2001, 7: 132-7. 10.3109/13814780109094331.
Article Google Scholar
Snijder EA, Kersting M, Theile G, Kruschinski C, Koschak J, Hummers-Pradier E, Junius-Walker U: Home visits in German General Practice: findings from routinely collected computer data of 158,000 patients. Gesundheitswesen. 2007, 69: 679-85. 10.1055/s-2007-993181.
Article CAS PubMed Google Scholar
van den Berg M, Cardol M, Bongers FJM, de Bakker D: Changing patterns of home visiting in general practice: An analysis of electronical medical records. BMC Fam Pract. 2066, 7: 58-
Aylin P, Majeed A, Cook DG: Home visiting by general practitioners in England and Wales. BMJ. 1996, 313: 207-10.
Article CAS PubMed PubMed Central Google Scholar
Bass MJ, McWhinney IR, Stewart M, Grindrod A: Changing face of family practice. Trends from 1974 to 1994 in one Canadian city. Can Fam Physician. 1998, 44: 2143-9.
CAS PubMed PubMed Central Google Scholar
Bergeron R, Laberge A, Vezina L, Aubin M: Which physicians make home visits and why? A survey. CMAJ. 1999, 161 (4): 369-74.
Oldenquist GW, Scott L, Finucane TE: Home care: What a physician needs to know. Clev Clin J Med. 2001, 68 (5): 433-40. 10.3949/ccjm.68.5.433.
Article CAS Google Scholar
Svab I, Kravos A, Vidmar G: Factors influencing home visits in Slovenian general practice. Fam Pract. 2003, 20: 58-60. 10.1093/fampra/20.1.58.
De Maeseneer J, De Prins L, Heyerick JP: Home visits in Belgium: A multivariate analysis. Eur J Gen Pract. 1999, 5 (1): 11-4. 10.3109/13814789909094245.
Kersnik J: Observational study of home visits in Slovene general practice: Patient characteristics, practice characteristics and health care utilization. Fam Pract. 2000, 17 (5): 389-93. 10.1093/fampra/17.5.389.
Marcinowicz L, Chlabicz S, Gugnowski Z: Home visits by family physicians in Poland: Patients' perspective. Eur J Gen Pract. 2007, 13: 237-45. 10.1080/13814780701627362.
Meyer GS, Gibbons RV: House calls to the elderly - a vanishing practice among physicians. N Engl J Med. 1997, 337: 1815-20. 10.1056/NEJM199712183372507.
Pereles L: Home visits. An access to care for the 21st century. Can Fam Physician. 2000, 46: 2044-8.
Peppas G, Theocharis G, Karveli EA, Falagas ME: An analysis of patient house calls in the area of Attica, Greece. BMC Health Serv Res. 2006, 6: 112-10.1186/1472-6963-6-112.
Article PubMed PubMed Central Google Scholar
Court BV, Bradley CP, Cheng KK, Lancashire RJ: Responding to out of hours request for visits: A survey of general practitioner opinion. BMJ. 1996, 312: 1401-2.
Lattimer V, Smith H, Hungin P, Glasper A, George S: Future provision of out of hours primary medical care: A survey with two general practitioner research networks. BMJ. 1996, 312: 352-6.
Van Royen P, De Lepeleire J, Maes R: Home visits in general practice: An exploration by focus groups. Arch Public Health. 2002, 60: 371-84.
Google Scholar
Liang HW, Landers S: Who receives house calls?. J Am Geriatr Soc. 2008, 56: 1581-2. 10.1111/j.1532-5415.2008.01782.x.
Vinker S, Nakar S, Weingarten MA, members of the Israeli General Practice Research Network: Home visits to the housebound patient in family practice: A multicenter study. IMAJ. 2000, 2: 203-6.
CAS PubMed Google Scholar
Caplan GA, Ward JA, Brennan NJ, Coconis J, Board N, Brown A: Hospital in the home: A randomised controlled trial. Med J Australia. 1999, 170: 156-60.
Moraes E, Campos GM, Figlie NB, Laranjeira R, Ferraz MB: Cost-effectiveness of home visits in the outpatient treatment of patients with alcohol dependence. Eur Addict Res. 2010, 16: 69-77. 10.1159/000268107.
Katz PR, Karuza J, Intrator O, Mor V: Nursing home physician specialists: A response to the workforce crisis in long-term care. Ann Intern Med. 2009, 150: 411-3.
Johnson MA: Changing the culture of nursing homes. Ann Intern Med. 2010, 170 (5): 407-9. 10.1001/archinternmed.2009.550.
Koopmans RTCM, Lavrijsen JCM: Dutch elderly care physicians: A new generation of nursing home physician specialists. JAGS. 2010, 58 (9): 1807-8. 10.1111/j.1532-5415.2010.03043.x.
van den Berg N, Meinke C, Heymann R, Fiß T, Suckert E, Pöller C, Dreier A, Rogalski H, Karopka T, Opperman R, Hoffman W: AGnES: Supporting general practitioners with qualified medical practice personnel. Model project evaluation regarding quality and acceptance. Dtsch Ärztebl Int. 2009, 106 (1-2): 3-9.
PubMed PubMed Central Google Scholar
Edwards M, Bobb C, Robinson SI: Nurse practitioner management of acute in-hours home visit or assessment requests: A pilot study. Br J Gen Pract. 2009, 59: 7-11. 10.3399/bjgp09X394798.
Leff B, Burton JR: The future history of home care and physician house calls in the United States. J Gerontol. 2001, 56A (10): M603-8.
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2296/12/24/prepub
Download references
Acknowledgements
We thank all the general practitioners who participated in this study.
The study has been funded by the Institute of General Practice and Family Medicine, Hanover Medical School.
The article processing charge has been funded by a programme of the Deutsche Forschungsgemeinschaft (DFG): "Open access publication".
Author information
Authors and affiliations.
Institute of General Practice and Family Medicine, Hanover Medical School, Carl-Neuberg-Str. 1, 30625, Hannover, Germany
Gudrun Theile, Carsten Kruschinski, Marlene Buck, Christiane A Müller & Eva Hummers-Pradier
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Gudrun Theile .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
GT conceived of the study, was involved in analyzing and interpreting the data and wrote the manuscript. MB was involved in study design, conducted the interviews, and performed the analysis of the data and interpretation of the data. CK, CM and EHP contributed to the interpretation of the data, the writing, and critical revision of the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Theile, G., Kruschinski, C., Buck, M. et al. Home visits - central to primary care, tradition or an obligation? A qualitative study. BMC Fam Pract 12 , 24 (2011). https://doi.org/10.1186/1471-2296-12-24
Download citation
Received : 17 December 2010
Accepted : 22 April 2011
Published : 22 April 2011
DOI : https://doi.org/10.1186/1471-2296-12-24
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nursing Home
- Interview Partner
- German Health Care System
- Nursing Home Visit
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
- Home Visit Doctor
Home Visit Doctor General Practitioners
Committed to deliver the much-needed medical care to patients on behalf of General Practitioners, Hello Home Doctor Service has been successful in bringing smiles to millions of faces. If any of your loved ones falls ill during the after-hours, then a Home Visit Doctor sent by Hello Home Doctor Service can turn to be your ultimate source of relief. You can reach the Hello Home Doctor Service team and book Doctors for Home Visit via a call at 134-100, using the Hello Home Doctor Service mobile app or even through the online form for booking a visiting home doctor.
At Hello Home Doctor Service, we understand the significance of a helping hand when the General Practitioners aren’t available. It is through effective collaboration that we strive towards enhancing the utmost welfare of people. Our Call Centre operates from Monday to Friday (4:00 p.m. to 8:00 a.m.), 10:00 a.m. onwards on Saturday and for 24 hours on all Sundays and public holidays. The in-home doctor visits by Hello Home Doctor Service will allow you to handle any kind of medical emergency with ease.
Payment Options for Hello Home Doctor Services
Patients who’ve registered with Medicare or Veterans Affairs are being bulk billed for home visits by doctors. Here, it is vital to ensure that you have a valid Medicare or Veteran Affairs Card. If it isn’t, then a payment of $200 will apply while booking a doctor for a home visit. Since we don’t accept cheques, you’re requested to make the payment via credit card (an extra 1% surcharge would be applicable on all credit card payments). All overseas students (the ones who possess insurance via BUPA, Medibank, NIB & Allianz) who choose to avail our visiting home doctor services are bulk billed.
A closer look at our services
Hello Home Doctor Service has a panel of General Practitioners who provide a wide range of services . Every visiting home doctor is accompanied by a Chaperone who provides support to the Doctor.
Most caring home visiting doctor service
Hello Home Doctor Service is owned and operated by Ipswich doctors and provides 100% professional after-hours medical care to patients within the comfort of their homes. Our home doctor visits start from 6:00 p.m. to 8:00 a.m. the next morning during weeknights, from 12 noon on Saturdays and all day and night on Sundays and all public holidays.
Call an ambulance if patient’s condition changes
It’s absolutely essential to monitor the patient’s symptoms even after a doctor from Hello Home Doctor Service has been booked for urgent medical attention. However, under situations where the patient’s health gets worse; calling an ambulance on 000 is what we recommend. Also, you may opt for visiting your nearest local hospital.
Know the areas we service
You can use the suburb locator (available towards the top right side of the website’s home page) for confirming whether Hello Home Doctor Service serves in the entered area or not.
Booking request for home visiting doctor service is a breeze
Just reach this page https://hellohomedoctor.com.au/book-online/ and fill in the form to receive a call from our friendly call centre staff. Hello Home Doctor Service takes bookings from 4:00 p.m. during weekdays, from 10 a.m. on Saturdays and all day and night on Sundays and all public holidays.
Doctors to Home
We are a fully bulk-billed service providing after-hours doctors to home . We offer exceptional treatment for all patients who may have already visited their regular GP but are still experiencing the symptoms on a Sunday or Public Holiday. At Hello Home Doctor Service, we bulk bill the patients who have a valid Medicare or Veteran Affairs Card. For patients with no card, we charge a sum of $200 at the time of booking the Doctors to Home Ipswich .
With a high level of respect for all our patients, we operate on weeknights from 6:00 p.m. until 8:00 a.m. the following morning, 12 noon onwards on Saturdays and for 24 hours on Sundays and Public Holidays.
Can’t contact your regular GP? We’re here to help you
Choosing Hello Home Doctor Service for calling doctors at home, will entitle you to the following benefits:
- Professional and reliable medical practitioners
- Bulk billed medical treatment
- Easy transfer of your medical report (by at-home doctor ) to your regular GP
- Privacy of patients’ personal information is respected & maintained
On-road support via state-of-the-art IT systems
Doctors Who Visit Home
Weekends are always great fun for everyone. For some it is about hanging out with friends, while for others it is about spending some quality time with family members. We all look forward to weekends because they give us the opportunity to do something enjoyable after slogging it out in the office during weekdays Doctors who visit home.
What we don’t take into account though is that weekends sometimes can also bring medical emergencies at home when even our GP is not around for consultation. This is the time when Doctors who visit home can really come in handy.
At Hello Home Doctor Service, we offer you the convenience of medical care on weekends, when your GP is away on a holiday. We provide you a visiting doctor service in Ipswich, greater Springfield and Centenary suburbs on weeknights from 6.00pm till 8.00am the following morning; on weekends from 12.00pm on Saturday to 8.00am on Monday. We also offer these visiting doctor services on all public holidays including the Ipswich Show Day.
The doctors we send for home visits are completely equipped to provide treatment for acute as well as periodical conditions. They administer any medication if required to treat patient’s condition and generate a report for their record as well as for patient’s GP for updating the medical history.
For convenience of people looking for qualified doctors who visit home during weekends; our call centre begins taking bookings on weekdays from 4.00pm in the afternoon until 8.00am he next day. On Saturdays, we start taking bookings from 10.00 am, while we are operational 24 hours on Sundays and all public holidays.
Need a Doctor? Is it after hours? We are just a click away!
Call 134-100
BOOK ONLINE
FREE MOBILE APP
Check Our Postcode Coverage
Consultation hours we provide home visits to patients in their home aged care facilities and hotels.
To request after hours medical care, book online, via the APP or call 134100.
Our Call Centre is operational 24 hours a day to facilitate continuity of care.
* This search tool has been provided a guide to our Services coverage area. Please call 134100 to confirm if your address is within our coverage area. If your condition is an emergency, please call 000.
Follow us on Facebook to get all the updates.
** Please note that some postcodes may be partially covered. The Call Centre team will confirm this at the time of booking the call.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- GPs call for home...
GPs call for home visits to be removed from contract
- Related content
- Peer review
- Gareth Iacobucci
GP leaders in England have called for an end to their contractual responsibility to carry out home visits, following a tense vote at their annual conference in London.
After a passionate and polarised debate, England’s local medical committee (LMC) representatives passed a motion which said that GPs “no longer have the capacity to offer home visits” and called on the BMA’s General Practitioners Committee (GPC) for England to negotiate changes to their contract to reflect this.
The motion was voted on in three parts, all of which were carried. The first section to “remove the anachronism of home visits from core contract work” narrowly passed, with 54% voting in favour and 46% against.
Three quarters of representatives (74%) backed a separate strand urging GPC to negotiate a separate acute service for urgent visits, while 90% backed a call to demand that any such change in service is “widely advertised” to patients.
Andy Parkin of Kent LMC, who proposed the motion, insisted that the move would not disadvantage the most frail and vulnerable patients. “Moving away from routine home visits would actually improve the care of all our patients by gaining us that most precious and rare commodity—time,” he said. “No other country has on-demand home visits like the UK. This motion gives the GPC a mandate to remove the expectation that home visits are an entitlement regardless of clinical need.”
A number of doctors spoke against the motion, including Sarah Matthews from Coventry LMC, who warned that passing it would “sell the heart and soul of our profession away.” Annie Farrell, from Liverpool LMC, argued that home visits were more important than ever with more patients living longer.
Also opposed was Ian Morris from Devon LMC, who said: “We learn a lot about a patient from seeing them in their own home. We would be losing an important part of our professional identity.”
But the vote was carried after a number of GPs highlighted the need to “send a message” to the government that current demands and pressures on the profession were not sustainable.
Brian McGregor from North Yorkshire LMC said: “We are getting increasing demand, year on year. This isn’t about just home visiting, this is about workload, and about when to say ‘enough is enough’.”
Anthony O’Brien of Devon LMC also spoke in favour, arguing that GPs were currently having to contend with large volumes of unfunded work stemming from patients being discharged too early from secondary care. “We need to get this work recognised and properly funded,” he said.
Also in favour was Zishan Syed from Kent LMC, who raised the matter of safety, citing cases of GPs being physically attacked when conducting home visits. “We need a separate service where we are protected to do our work,” he said.
Greg Place from Nottinghamshire LMC spoke against the motion, warning that it would send “the wrong message” to patients and the public. “We’ve got remember we are a caring profession,” he said. “We need to rise above this.”
But Parkin said: “This motion doesn’t take away your choice to go and see patients at home who need to be seen. We do not have the capacity, the staff, or the time. Even if it can’t be negotiated, this sends a clear message to the government that we need help.”
GP mythbuster 71: Prioritising home visits
It is good practice for GP practices to have systems in place to triage and prioritise home visits.
Since the coronavirus (COVID-19) pandemic, the need for a home visit should be continue to be carefully assessed. The British Medical Association (BMA) and Royal College of General Practitioners have published COVID-19 Workload Prioritisation Unified Guidance which explains response levels. The guidance outlines types of work that should be undertaken in primary care, depending on:
- COVID-19 prevalence
- other workload
- workforce factors
The British Medical Association (BMA) has produced a COVID-19 toolkit for GPs and GP practices .
NHS England issued a patient safety alert to raise awareness of the need to have a system in place to assess:
- whether a home visit is clinically necessary , and
- the urgency of need for medical attention.
The alert states that:
"This can be undertaken, for example, by telephoning the patient or carer in advance to gather information to allow for an informed decision to be made on prioritisation according to clinical need. In some cases, the urgency of need will be so great that it will be inappropriate for the patient to wait for a GP home visit and alternative emergency care arrangements will be necessary."
"Many practices will already have systems in place to manage home visits. Where this is the case, consideration should be given to whether a review is required in light of this alert. The review should also consider whether all clinical and non-clinical staff involved in the process are aware of their responsibilities when managing requests for home visits, and if any outstanding training needs exist.”
GPs should also consider whether alternate ways of assessing the patient are appropriate. For example, video call, telephone calls or the use of virtual wards in care homes.
When delegating home visits, the provider must ensure that the Health Care Professional (HCP) has the necessary:
- competence and
- training to deliver the home visit.
The HCP should also receive appropriate supervision and support from the clinical team. Practices should ensure that the person allocated is competent to carry out home visits.
When we inspect
We will expect to see evidence of how the provider has assured themselves of the capability of non-medical HCPs, to whom they delegate home visits. This should include a process of assurance: both on initial delegation of the role and how the HCP’s capability is maintained on an ongoing basis. It should include audit of:
- their clinical decision-making
- prescribing decisions when relevant and
- a system for escalation to a senior clinician when necessary.
We use these regulations when we review if the practice is safe, effective, responsive, caring and well led. This mythbuster relates to:
- Regulation 9 (Person centred care)
- Regulation 12 (Safe care and treatment)
It is part of our key lines of enquiry (KLOEs). One of our key questions is whether services are organised so that they meet people’s needs. In particular, KLOEs:
- S2 Managing Risk
- S3 Safe care and treatment
- E3 Staff skills and knowledge
- E4 How staff, teams and services work together
- R1 Person centred care
- R3 Timely access to care and treatment
- WL8 Learning, improvement and innovation .
We may look at how the practice:
- manages and prioritises home visits
- recognises a deteriorating patient
- works with other professionals
- manages care planning, referrals and investigations.
We may also look at:
- the practice’s processes and systems to monitor patient safety through reporting patient safety incidents
- how they learn from these incidents and significant events.
This patient safety alert shows how important it is for GP practice staff to report all patient safety incidents to the National Reporting and Learning System (NRLS). Lessons can be learned across general practice.
Further information
- GP mythbuster 24: Reporting patient safety incidents to the National Reporting and Learning System (NRLS) for GP practices
- GP mythbuster 66: Advanced nurse practitioners and primary care
- GP mythbuster 100: Online and video consultations and receiving, storing and handling intimate images
- GP mythbuster 102: Pulse oximetry and monitoring vital signs outside the GP practice
- Patient Safety eForm (nrls.nhs.uk)
GP mythbusters
Snippet gp mythbusters rh.
Clearing up some common myths about our inspections of GP and out-of-hours services and sharing agreed guidance to best practice.
See all issues:
- GP mythbusters: listed by key question
- GP mythbusters: full list
- GP mythbusters: recently updated
Pay Your Bill Patient Portal
Medical Records Request
- Physician Recruiting
- Privacy Policy
- Testimonials
- Weather/Holiday Closings
Specialties
- Breast Care
- Cancer Care
- Cardiothoracic Surgery
- Colon & Rectal Care
- Endocrinology
- Gastroenterology
- General Surgery
- Maternal-Fetal Medicine
- Neurosurgery
- General Orthopedics
- Knee & Hip
- Sports Medicine
- Post-Acute Care
- Primary Care
- Pulmonary Services
- Thoracic Surgery
- Urogynecology
- Prenatal Resources
- Cancer Survivorship Program
- Clinical Pharmacy Services
Home Visits
- Nutrition Services
- Survivorship Sexual Health Program
Our Providers
- Schedule Your Mammogram
- Schedule Your Colonoscopy
Our Locations
For patients.
- COVID Information
- Colonoscopy Screening
- Flu Shot Information
- Online Appointment Scheduling
- Patient-Centered Medical Home
- Patient Education & Resources
- Patient Financial Services
- Patient Forms/Insurance
Patient Portal

Great Lakes Cardiovascular • OBGYN Associates • Great Lakes Cancer Care
We Bring the Care to You
- Ordering durable medical equipment
- Completing forms for aide service in home
- Hospital follow-ups
- Sick visits
- Established patient follow-ups
- Vatica annual well visits
Melanie Vaughn, MSN, FNP-BC
Richard Milazzo, MD
Previsit Planner & Scheduler
716.422.5677
716.314.7371
Patient Testimonial
Thank you General Physician, PC. My parents are older, with some chronic conditions and with everything going on at this time, my family felt very strongly about not sending them out to visit their doctors. It was suggested that we look into the Home Visit program. The ease of scheduling and access to a quick appointment was wonderful. The nurse practitioner immediately put both my mom and dad at ease. They were able to have vital signs sent off to a primary care and a cardiovascular doctor, bloodwork and other evaluations were done in the comfort of their own home. She was professional, courteous and most of all compassionate – we could not have asked for a better visit. Thank you General Physician, for caring and having nurses like the one who cared for my parents out in the field. What a wonderful service.
find a provider
- Pay My Bill
Find a Provider
By Location

By Specialty
Patient Information
Patient Forms
Educational Links
Pay Your Bill
Holiday Closings
Pay My Bill Patient Portal 716-852-4772

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Br J Gen Pract
- v.70(695); June 2020

GP home visits: essential patient care or disposable relic?
Introduction.
The GP home visit has long been regarded as an integral element of NHS general practice that is needed to support both proactive and reactive care to patients in the community. 1 , 2 There are increasing numbers of people living with multimorbidity and frailty, many of whom have complex healthcare needs and limited levels of social support. Now with the new challenges around providing care at home due to the COVID-19 pandemic, it could be argued that home visits or virtual consultations with patients in their homes are set to become a more essential element of general practice, including in the provision of acute care out of hours. Consulting with patients in their homes provides unique opportunities to develop insights into how illness affects their lives. However, with workloads in NHS primary care rising, and increasing pressures on the GP workforce, the place of home visits in core general practice provision is facing increasing challenge.
GPs DEBATE HOME VISITING
The requirements of the current GP General Medical Services (GMS) contract in relation to home visiting are broad. 3 The contract is not prescriptive about who should visit or where the visit should take place, and states that the decision to visit is dependent on the opinion and agreement of the GP contractor. In November 2019, the Local Medical Committee (LMC) conference debated the current contractual requirements and a motion was narrowly passed to instruct the General Practitioners Committee (GPC) (the negotiating arm of the British Medical Association) to ‘remove the anachronism of home visits from core contract work’ . 4 The majority backed a motion to negotiate a separate acute service for urgent visits.
Reporting of the LMC debate in the national press and social media highlighted how emotive the issue of home visits is, and the diversity of views among GPs that exist around their value. They were described by some as a service that is regarded by patients as an entitlement, available for purposes of convenience. 4 It is likely that GPs working in practices that are short-staffed and overwhelmed by workload pressures are more likely to view home visits as an inefficient use of their scarce resources. Others considered home visits a vital component of general practice, arguing that when patients are unwell at home it is generalist doctors who are best placed to assess them. There were concerns that removing home visits from the GP contract would compromise the values of general practice, sending a message to patients that their doctor no longer cares for those who may have pressing clinical needs but wish to be treated at home.
WHAT DO WE KNOW ABOUT GP HOME VISITING?
In a healthcare system where it is expected that contracts are informed by robust evidence-based medicine, the lack of evidence regarding GP home visits, including out of hours, is striking. There has been relatively little research to understand the circumstances in which patients request GP home visits, when and why GPs undertake home visits, and how outcomes can be optimised within a resource-constrained health service. What is known is that over the last 50 years there has been a steady decline in the extent to which GPs visit patients in their homes in the UK and internationally, 2 , 5 , 6 and that not all GPs are convinced of their benefits. 1
Some GP consultations with patients at home are reactive when there is an acute and sudden deterioration in their health, including out of hours. The visiting professional must skilfully balance the risks of continuing care at home against admission to hospital. Others are more proactive, to monitor and plan care for those with long-term health conditions that may prevent them from attending the surgery. Research suggests that GPs do not tend to dispute visit requests for vulnerable, older people. 1 For patients who are dying, there is a positive association between GP home visit rates and achieving home as the preferred place for end-of-life care. 7 GPs who gain experience of home visiting during their training are more likely to undertake home visits post-qualification. 8 GP visits to residential and nursing care homes, and the quality of care delivered, have been described as particular areas of concern. 9 Little is known about responses to other patient groups who may benefit, including: those with mental health concerns; physical disabilities; complex care needs; or those who are unwell with potentially infectious diseases, such as children who may be advised not to attend the GP surgery. Patients appreciate home visits and feel that their relationship with their GP improves as a result. 10
Although GP consultations in patients’ homes are likely to require different consultation skills from those that apply within the surgery setting, the requirements for training in the conduct of GP home visits are ill defined and are largely left for the trainee and their trainer to negotiate. For many trainees, there may be limited opportunity for their home visits to be observed, because of logistical and time constraints. 11 Formative assessment tools (Clinical Observational Tools) for home visits are lacking, and summative assessment of a simulated home visit (within the MRCGP Clinical Skills Assessment) occurs in only half of exams.
Many types of home visit have already been subsumed by other services, such as specialist community teams, early visiting services, and care home teams. Although this can be seen as relieving pressure on overstretched general practice, an unintended consequence is the fragmentation of care associated with multiple specialist teams providing care in the patient’s home. It also calls into question the role of general practice in the management of such complex patients. Obtaining timely information, communicating with each visiting specialist team, and overseeing such care risks adding to the GP workload. 12 As Abrams et al highlight in their realist review of delegated home visiting services in this issue, there is more to be done to understand how such services can be implemented effectively. 13 Research is needed to inform delegation processes, and effective system implementation is needed to support such services and to understand the impact on patient satisfaction, long-term health outcomes, and cost. 13 A pertinent issue is the need for clarity around roles and responsibilities, so that the professional status and autonomy of all involved are understood and valued. This is most likely when trusted professional relationships are developed over time and where the facility to share information effectively exists. 13
‘Good general practice will always consist of patients feeling at home with their doctor and of doctors feeling at home with their patients.’ 12 In the context of burgeoning demand and underfunding of workforce and resources, there is a need to listen to the diversity of views among GPs and primary care colleagues concerning the future of home visits. Robust research is needed to provide understanding into the value of GP consultations in patients’ homes, both through visiting and using telemedicine, and how best to optimise the delivery of primary medical care, particularly for housebound patients, 24 hours a day, 7 days a week. Increased understanding into the nuances and impact of GP home visits on patient care and the wider healthcare system would form an important evidence base to inform NHS policy and the training and development of the primary care workforce, and is necessary before changes are made to the GP core contract.
Freely submitted; externally peer reviewed.

Coding for E/M home visits changed this year. Here’s what you need to know
CPT has revised codes for at-home evaluation and management (E/M) services as of Jan. 1, 2023. Services to patients in a private residence (e.g., house or apartment) or temporary lodgings (e.g., hotel or shelter) are now combined with services in facilities where only minimal health care is provided (e.g., independent or assisted living) in these code families:
Home or residence E/M services, new patient
• 99341, straightforward medical decision making (MDM) or at least 15 minutes total time,
• 99342, low level MDM or at least 30 minutes total time,
• 99344 (code 99343 has been deleted), moderate level MDM or at least 60 minutes total time,
• 99345, high level MDM or at least 75 minutes total time.
Home or residence services, established patient
• 99347, straightforward MDM or at least 20 minutes total time,
• 99348, low level MDM or at least 30 minutes total time,
• 99349, moderate level MDM or at least 40 minutes total time,
• 99350, high level MDM or at least 60 minutes total time.
Select these codes based on either your level of medical decision making or total time on the date of the encounter , similar to selecting codes for office visits . The E/M codes specific to domiciliary, rest home (e.g., boarding home), or custodial care (99324-99238, 99334-99337, 99339, and 99340) have been deleted, and the above codes should also be used in those settings.
When total time on the date of the encounter exceeds the threshold for code 99345 or 99350 by at least 15 minutes, you can add code 99417 to report prolonged services. The exception to this is for patients with Medicare. For those patients, report prolonged home or residence services to Medicare with code G0318 in addition to 99345 (requires total time ≥140 minutes) or 99350 (requires total time ≥110 minutes). Code G0318 is not limited to time on the date of the encounter, but includes any work within three days prior to the service or within seven days after.
Services provided in facilities where significant medical or psychiatric care is available (e.g., nursing facility, intermediate care facility for persons with intellectual disabilities, or psychiatric residential treatment facility) are reported with codes 99304-99310 .
— Cindy Hughes, CPC, CFPC
Posted on Jan. 19, 2023
- Chronic care
- Medicare/Medicaid
- Physician compensation
- Practice management
- Reimbursement
- Value-based payment
Other Blogs
- Quick Tips from FPM journal
- AFP Community Blog
- Fresh Perspectives
- In the Trenches
- Leader Voices
- RSS ( About RSS )
Disclaimer: The opinions and views expressed here are those of the authors and do not necessarily represent or reflect the opinions and views of the American Academy of Family Physicians. This blog is not intended to provide medical, financial, or legal advice. Some payers may not agree with the advice given. This is not a substitute for current CPT and ICD-9 manuals and payer policies. All comments are moderated and will be removed if they violate our Terms of Use .
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

IMAGES
VIDEO
COMMENTS
Our Services. We accept Medicare, many insurance plans, and self-pay. To find out more about our services: Call Toll-free: (855) 232-0644. E-mail us at. [email protected]. Primary Care. Psychiatry. Wound Care.
Landmark partners with health plans to bring medical, behavioral health, and palliative care, along with social services, to patients in communities across the U.S. Our mobile providers visit patients in their homes through in-person house calls and telemedicine visits over video and phone. View Our Locations.
Book Your Video Visit with the Best Doctors Online. Stay safe at home while receiving top-quality medical care: online video visits and phone appointments with certified physicians. It's safe, secure, and with all the same privacy as a physical visit. We know that finding the right doctor or provider is important to your health.
Look out for your health. A UnitedHealthcare® HouseCalls visit is a no-cost, yearly health check-in that can make a big difference. Call 1-866-799-5895, TTY 711, to schedule your visit.
What we offer. A primary care home visit by one of our board certified and caring medical providers. A visit may be for acute concerns, regular follow-up, and annual physicals. Comprehensive medical exam in the comfort of your home; which may include orders for blood test, urine test, radiological imaging, medication prescription, and/or ...
To learn more about our services in the Washington, D.C., region, call us today at 202-877-0570. The MedStar Health MedStar House Call Program - MedStar Total Elder Care is nationally recognized and offers house calls by doctors, nurse practitioners and provides diagnostic tests and treatments. Learn more about our program.
The Mount Sinai Visiting Doctors Program has clinical, educational, and research missions. It is one of the largest academic home-visit programs in the nation, with its clinicians making more than 6,000 home visits annually to more than 1,000 patients. Hundreds of medical students, residents, and fellows make house calls alongside our providers ...
Caring for the seniors in our community is the mission of HouseCall Primary Care. We appreciate their special care needs, and our practice is directed toward meeting those needs wherever they are. Our care model is team-based, patient focused, and holistic, designed to deliver excellence in patient care. We strongly believe a team-based ...
The GP home visit has long been regarded as an integral element of NHS general practice that is needed to support both proactive and reactive care to patients in the community.1,2 There are increasing numbers of people living with multimorbidity and frailty, many of whom have complex healthcare needs and limited levels of social support. Now with the new challenges around providing care at ...
It seems like doctors are always needed. Everyone gets sick and everyone is going to need to get checked out at some point. But it seems like the old. GP For Home Visits. 334 likes. GP For Home Visits brings back to you that old fashioned service- Home Visits from your doctor!
We offer support through our free advice line on 0800 678 1602. Lines are open 8am-7pm, 365 days a year. We also have specialist advisers at over 120 local Age UKs. About the Age UK Advice Line Find your local Age UK. Find information about the services your GP can offer you, and what to do if you're too ill to visit your GP, and what services ...
MD at Home provides home care, home medical doctors, and housecall physicians to patients in need with a focus on preventing readmissions during the transition from an acute care setting to the home. For over 20 years, we've served as the premier healthcare resource for primary care and geriatric medicine for homebound patients in the Chicagoland area.
Yes, many house call doctors accept Medicare, private insurance, and sometimes Medicaid. It usually costs the same as a regular office visit. But every house call doctor is different, so make sure you understand their fees and accepted insurance plans beforemaking an appointment. How to find a house call doctor.
Speak with Signify Health directly. Sometimes, talking to a real person is easier. To schedule by phone, call 1-855-746-8709 (TTY: 711) Monday - Friday, 9AM to 8PM ET. If we don't hear from you, someone from the Signify Health team will reach out to help schedule your visit.
Home visits are claimed to be a central element of general practice as this represented the primary mode of healthcare delivery by community physicians from the mid-20 th century [].Today in most European countries and the United States home visits are the exception and are no longer the standard method of health care delivery - although there is diversity between individual general ...
Primary care home visits are well established in current UK practice. Home visits could help avoid unplanned hospital admission when supported with appropriate diagnostic back up. In addition when a patients' own GP is attending they may have access to patient records and history. It should enable a discussion of options and shared decision making. Primary care visits are particularly useful ...
Hello Home Doctor Service is owned and operated by Ipswich doctors and provides 100% professional after-hours medical care to patients within the comfort of their homes. Our home doctor visits start from 6:00 p.m. to 8:00 a.m. the next morning during weeknights, from 12 noon on Saturdays and all day and night on Sundays and all public holidays.
GP leaders in England have called for an end to their contractual responsibility to carry out home visits, following a tense vote at their annual conference in London. After a passionate and polarised debate, England's local medical committee (LMC) representatives passed a motion which said that GPs "no longer have the capacity to offer home visits" and called on the BMA's General ...
GP mythbuster 71: Prioritising home visits. It is good practice for GP practices to have systems in place to triage and prioritise home visits. Since the coronavirus (COVID-19) pandemic, the need for a home visit should be continue to be carefully assessed. The British Medical Association (BMA) and Royal College of General Practitioners have ...
Our Home Visit team provides Enhanced Annual Visits (EAVs) in the home for patients identified as high risk and/or homebound who have not received an EAV in 2019. In addition to the EAV, our Nurse Practitioners bring the equipment to complete an A1C, Microalbumin, Diabetic Retinal Exam and/or Bone Density screening.
At a cost of £233 for an ambulance conveyance and £132 for an ED attendance (source: NHS Reference costs), a primary care-led home visit, if appropriate, is likely to be less costly. The committee concluded that there was no clear evidence to confirm or refute the cost-effectiveness of primary care visits.
23 November 2019. Dean Mitchell/Getty Images. GPs have voted to reduce visits to patients' homes, saying they "no longer have the capacity" to offer them. Doctors supported the proposal at a ...
The GP home visit has long been regarded as an integral element of NHS general practice that is needed to support both proactive and reactive care to patients in the community. 1, 2 There are increasing numbers of people living with multimorbidity and frailty, many of whom have complex healthcare needs and limited levels of social support.
The E/M codes specific to domiciliary, rest home (e.g., boarding home), or custodial care (99324-99238, 99334-99337, 99339, and 99340) have been deleted, and the above codes should also be used in ...