

House Calls – We Bring the Doctor’s Office to the Patient
At Mobile Physician Services, we provide comprehensive care to improve the health and quality of life of our patients – in the convenience and comfort of their own home. Our team of board-certified doctors, advance nurse practitioners, and physician assistants specialize in providing care for patients with medically complex and chronic conditions.
Our Services
We accept Medicare, many insurance plans, and self-pay.
To find out more about our services:
Call Toll-free: (855) 232-0644
E-mail us at [email protected]
Primary Care
Pain management, palliative care.
At Mobile Physician Services, our customized care teams provide patients with both comfort and familiarity as they work with a dedicated primary care provider and care coordinator to improve their health. Our physicians and staff take a proactive approach to preventive care, chronic disease management, and chronic illness support right where you live.
Each home visit includes an in-depth examination and individualized treatment plan, which is monitored and adjusted through routine follow-up visits. The primary care provider will deliver your ongoing care and will recommend to you specialty services as needed.
- Annual Wellness visits : This wellness visit allows your primary care provider to create or update your personalized prevention plan. This visit includes a review of your medical and social history related to your health and may include counseling about preventive services. This plan may help you to prevent or reduce the chances of future illness based on your current health and risk factors.
- New Illness Exams : When a new symptom or ailment arises, call us. Early indications of not feeling well could be a clue that you may be getting sick. A symptom in one part of the body may also be a sign of a problem in another part of the body. Moreover, unrelated symptoms that might seem minor on their own, could be warning signs of a more serious medical disease or condition. The new illness exam can be very brief or more detailed depending on your concerns and the provider’s findings.
- Follow-up Care: Involves a regular medical checkup, which may include a physical exam and laboratory testing. Follow-up care checks are a proactive way of assessing the potential for and preventing health problems from returning after treatment of a disease has ended or an illness has seemingly passed.
- Referral for Specialty Care : Referrals are the link between primary and specialty care. The referral coordination includes the documentation of patient care activities, the transfer of information, the inter-provider communication itself, and the integration of care services to the patient. Mobile Physician Services is a multi-specialty practice so many of these specialty referral services can be made seamlessly with little inconvenience or disruption to the patient and caregivers regular routines.
- Medication Management: Medication management is a treatment structure that ensures our patients are receiving optimal therapeutic results from their prescription medications, both in the short and long term. Our team’s goal is to mitigate medication noncompliance and monitor all prescriptions treatments so that drug interactions complement one another for the most optimal outcome for our patients.
The provider may be a physician, advanced practice nurse or a physician assistant. A dedicated care coordinator will also be assigned for each patient to help arrange comprehensive services and assist patients and their caregivers.
- Online Patient Portal: You and your designated caregiver, if you choose, will be able to connect with your provider through a convenient, safe and secure environment which allows access to your health records and a way to communicate with our staff in a timely manner.
- Telephone Assistance : On call providers are available 24/7 weekdays and weekends.

Our psychiatry team specializes in the diagnosis and management of mental, emotional and behavioral disorders. They carefully evaluate each patient to develop an individualized treatment plan to improve the patient’s overall mental and physical well-being.
- Depression : Depression is a common and often serious medical illness that negatively affects how you may feel, the way you may think, and how you may act. Depression can cause feelings of sadness, despair and hopelessness, which may lead to a loss of interest in activities you once enjoyed.
- Anxiety : Intense, excessive, and persistent worry and fear about everyday common situations. The worry or anxiety could make you feel fatigued, irritable, and interfere with your regular sleep habits.
- Dementia : An overall term that is used to describes a collection of symptoms related to an individual’s decline in memory or other thinking skills. It may be severe enough to diminish a person’s ability to perform everyday common activities. The effects of dementia can negatively influence your memory, thinking and social abilities.
- Phobias : A phobia is when you experience excessive panicking or an irrational fear reaction to a situation. If you have a phobia, you may experience a deep sense of dread or fright when you encounter the source of your fear. The fear may be a certain place, situation, object, animal or even another person.
- Behavioral disorders : Attention deficit, hyperactivity, bipolar, learning, defiant or conduct disorders are all examples of complaints that may have a detrimental impact on a person’s interpersonal relationships with family, friends, and co-workers.
Our team can provide behavioral counselling and medical therapy, when appropriate, to help a patient feel better about themselves and to assist them with better coping and managing their condition.

Our wound care specialists have been trained in the attention and treatment of all types of acute and chronic wounds. They have skill and experience in wound debridement and wound care procedures – managing chronic, non-healing wounds and infections, with a demonstrated care that fosters healing… right in the patient’s own home.
We specialize in serving homebound patients who may also be bed-bound or have difficulty in walking or moving around. As a result, immobility compression sores develop at pressure points on the body when the weight of an immobilized individual rests continuously on a firm surface, such as a mattress or wheel chair. Often these same patients are on oxygen or have high-risk medical conditions which makes it an even more challenging and stressful effort for them to travel to a doctor’s office for an appointment. Thus, the necessity for in home care and treatment.
Wounds that benefit from specialized wound care techniques include:
- Diabetic foot wounds and ulcers
- Post-surgical wounds
- Traumatic wounds caused by injury
- Arterial and vein stasis caused by lack of circulation
- Immobility pressure sores. (Bed sores from stillness)
We work closely with home health agencies to provide ongoing care and monitoring of patient’s wounds.

Our board-certified podiatrists treat foot pain, wounds, and more. Treatments may include but are not limited to treating conditions of the lower extremities which could hinder mobility.
- We will review each patients’ medical history to evaluate the condition of the feet, ankle or lower leg
- Carry out a diagnosis on the feet and lower legs through examination and medical tests
- Order physical therapy when deemed necessary
- Treat wounds of the lower extremities using various wound care modalities. This may include debridement to improve the healing potential
- Promote prevention, health & well being, the treatment and management of the foot and related problems, disability, deformity, and the pedal complications of chronic diseases for the elderly
- Prescribe and fit prosthetic appliances such as diabetic shoe inserts and evaluate for bracing if necessary
- Refer patients to other specialists for treatment, including conditions such as diabetes or arthritis
- Advise patients on ways to prevent future leg problems and increase speed of recovery
- Monitor the recovery progress of patients to determine the need for change in treatment

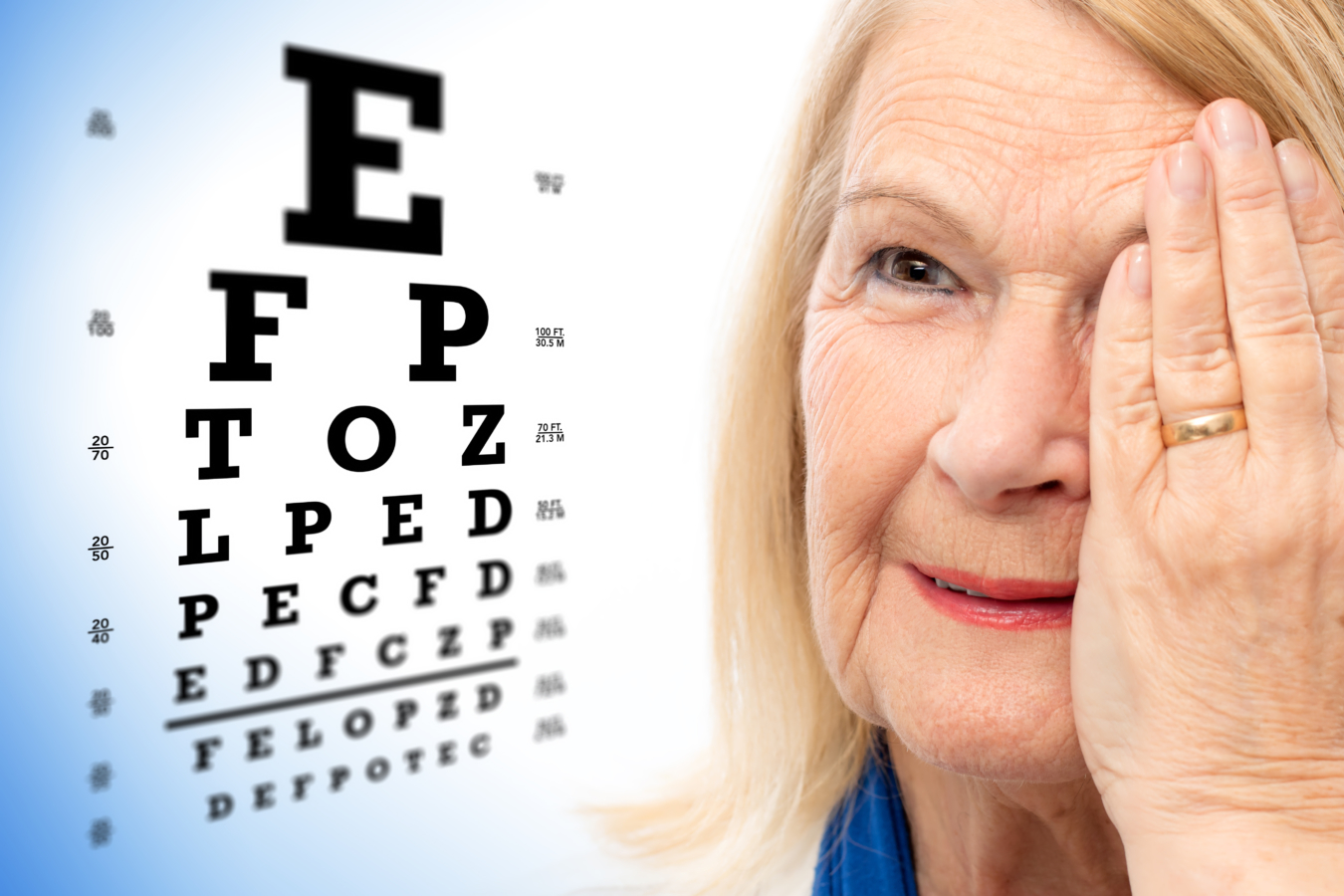
We know it’s not always easy to leave home to get the care you need for your eyes. Our optometrists bring state-of-the-art diagnostic eye equipment and technology to your home – making it much easier for you to get the vision care you need.
During a visit, your doctor will exam each eye for signs of serious issues such as glaucoma, cataracts, macular degeneration, and detached retinas, among other conditions.
Receiving regular eye exams regardless of the state of your vision can help detect serious eye problems at their earliest stages ─ when they are most treatable. During an eye exam, your doctor will observe and evaluate the health and condition of the blood vessels in your retina, which can be good indicators of the health of your blood vessels throughout the rest of your body.
- Comprehensive eye exams : This exam goes beyond a simple vision screening. A comprehensive eye exam includes a host of tests in order to do a complete evaluation of the health of your eyes and your vision.
- Annual retina exams : A retinal exam allows your doctor to evaluate the back of your eye, including the retina, the optic disk and the underlying layer of blood vessels that supply the retina.
- Eyeglass fittings : A prescription works best when your eyeglasses are properly fitted. Improper fitting may cause pinching, distorted vision, headaches, and even dizziness. Our doctors will make sure your prescription lenses and frames are working together for you.
- Diabetic eye exams : Diabetes does not have to lead to vision loss. Taking an active role in managing your diabetes can go a long way in curbing later complications. Regular eye exams, good management of your blood sugar and blood pressure, along with early intervention for vision problems can help prevent vision loss caused by diabetic retinopathy. Retinopathy is caused by damage to the blood vessels of the light-sensitive tissue at the back of your eye.
- Refractions: This test is given as part of your routine eye examination. It is often referred to as a vision test. This test assists your eye doctor in measuring you for the exact lens prescription you will need.
- Eye injuries: Eye trauma could be the result of a sudden blow to the eye. It may cause the eye to suddenly compress and retract which could cause damage to your eye and the surrounding tissue. Even if the injury may seem minor, all eye injuries should be furthered examined by a doctor for possible more serious and underlying injuries.
- Eye infections: The most common eye infection is conjunctivitis, also known as pink-eye. An eye infection can happen in almost any part of your eye, including your eye lid, cornea and optic nerve. Symptoms of eye infections may include redness, itching, swelling, discharge, pain, or problems with vision. Always consult with your doctor before treating, as recommended actions are contingent on the cause of the infection.
- Low-vision exams: A low vision exam is different from a normal eye exam. This functional-vision assessment determines how specific visual impairments affects your ability to perform everyday activities. The exam’s results assist your doctor in prescribing management tools and medications to better enhance and manage your remaining vision.
Pain management is the process of providing medical care that alleviates or reduces pain. Pain management is a subspecialty of general medicine employing an interdisciplinary approach to ease the suffering and improve the quality of life of those living with chronic pain by using a combination of pain medications, joint and muscles injections, and physical therapy techniques.
A pain management specialist is a provider with advanced training in diagnosing and treating pain. Our pain management specialists treat pain stemming from a variety of different causes, whether it’s neuropathic pain or headache, or the result of injury, a surgical procedure, cancer or another illness.

Palliative care is an approach to the holistic care of patients, including family and caregivers, to improve the quality of their lives after the diagnosis of a chronic debilitating disease or life-limiting illness that may cause a host of complaints.
Palliative care can begin at diagnosis and continue to be offered while the patient is continuing active treatment through different phases of their life limiting condition. Palliative care is for any patient with a chronic illness who is experiencing a decreased quality of life because of symptoms related to their illness or treatment, like renal dialysis, oxygen therapy or chemotherapy. The care is provided by a specially-trained team of doctors, nurse practitioners, physician assistants, and other specialists who work together to provide an extra layer of support to the patient and their caregivers.
Palliative care can help in symptom control including not only pain, but nausea, weakness, shortness of breath, fatigue and weight loss at any time during their diseases, not only at the end of life.

In Home Medical Senior Care Services | Landmark Health
- Patient or Caregiver
- Community Provider
Are you a new Landmark patient?
Burn-out is real. landmark is different..

Living with chronic health conditions? We can help.
Our providers and care teams come to you, bringing care through house call visits. This in-home medical care is designed around understanding your health needs and goals. We work with you and your regular doctors to help you stay well and stay home.
House calls and video visits in 37 states.
Landmark partners with health plans to bring medical, behavioral health, and palliative care, along with social services, to patients in communities across the U.S. Our mobile providers visit patients in their homes through in-person house calls and telemedicine visits over video and phone.
We are the future of health care.
Landmark is one of the nation’s largest healthcare companies focused on in-home care of complex, chronic patients. Our physician-led provider groups support collaborative ties between community-based organizations, primary care providers, specialists and patients and their families.
patients nationally for which Landmark bears risk
reduction in hospital admissions
reduction in mortality

Discover the benefits.
- For Patients + Caregivers
- For Community Providers
- For Partners
Health care in your home
Old-fashioned house calls by medical doctors, nurse practitioners and physician assistants bring modern medicine to you. Feel better and stay well at home.
Covered by your health plan
The Landmark program works with health plans to improve access to care for patients with multiple chronic conditions. Landmark’s team-based care is available often at no cost to you.
Keep your current doctors
Landmark coordinates its care with your primary care provider, specialists and other community resources. Landmark provides added support to those who need it most.
Available 24 / 7
Our provider-staffed call center answers any time of the day or night. We also provide urgent visits to help you avoid unnecessary trips to the emergency room.
No waiting room
With Landmark house calls, you won’t need transportation to clinics and hospitals, and you avoid waiting rooms and exposure to germs.
Reduced stress
Patients and caregivers enjoy peace of mind with Landmark support. Landmark cares for the whole patient.
Landmark house calls put patients at the center of health care.
Collaborative care for complex patients.
Landmark’s community-based mobile providers bring coordinated care to patients with multiple chronic health conditions. We augment your care in the patient’s home.
Covered by health plans
The Landmark program is included in eligible patients’ health plans to improve care coordination and healthcare access for home-limited patients.
You remain the primary care provider
Landmark care is coordinated directly with you. Our providers reinforce your care plan in the home through physician-led interdisciplinary care teams.
Access our interdisciplinary team
Landmark’s interdisciplinary care team is available to you and your patients, including behavioral health specialists, social workers, palliative care specialists, nurse care managers and pharmacists.
Reduce administrative burden
We can help your highest acuity patients by managing post-acute care, home health orders, face-to-face encounters, and more.
24 / 7 availability
You can reach us any time, including weekends and holidays. We do urgent home visits to intervene if your patient experiences a chronic disease exacerbation.
Landmark supports your patients with complex health and social needs.
Chronic care management.
We’re one of the nations’ leading risk-bearing medical groups. We focus on giving your most complex members care when they need it, right in their home.
Over 250,000 patients across the country
We bear risk for over 250,000 complex, chronic patients, spanning Medicare Advantage, Medicaid, Dual, and Commercial, populations.
Behavioral, social and palliative care
Our team of multidisciplinary clinicians may include behavioral health specialists, palliative care practitioners, social workers, nurse care managers, dietitians and pharmacists.
Urgent in-home visits
One in four of our home visits is urgent. We bring medical care to your members when they need it, to avoid unnecessary emergency room trips and hospitalizations.
Built-for-purpose infrastructure
Our technology platform is designed specifically to support the medically vulnerable, clinically complex population.
Meaningful outcomes
Landmark commonly helps health plans achieve 4- and 5-star performance on Medicare STARS clinical quality of care, while caring for the most complex patients.
Landmark provides care for complex, chronic patients to positively impact access, satisfaction, outcomes and cost.
The doctor and nurses show they care about you and your health they are really there for you when you need them I love that they come to your house we did a zoom meeting with the nurse practitioner and she gave suggestions I really appreciate them
It was a pleasure to talk and see the doctor, she was very knowledgeable of all my conditions and gave me great advice to improve my health.
Joan was very helpful. It was nice getting to know her. How Landmark can help me
Practice health care the way you always wanted — with those who need it most.
Expert insights.

Prioritizing Mental Health as a Universal Human Right
By: Neltada Charlemagne, DNP, APRN, PMHNP-BC, PHN, BHC

Outsmart Unplanned Medical Costs: 10 Steps for Managing the Unexpected
Older adults can safeguard themselves from the physical, mental and emotional toll of unexpected medical costs.

Optum Care Network – Monarch and Landmark Health bring care to you at home.
Optum Care Network – Monarch has teamed up with Landmark to deliver in-home medical care to members with multiple chronic conditions.
Have questions about Landmark? We’d love to hear from you.
- Healthcare Services
- Find a Doctor
- Patient Portal
- Research and Education

Your recent searches
- Find a Location
- Nursing Careers
- Physical Therapy Careers
- Medical Education
- Research & Innovation
- Pay My Bill
- Billing & Insurance Questions
- For Healthcare Professionals
- News & Publications
- Classes & Events
- Philanthropy
House Call Program - MedStar Total Elder Care
Browse this page
Promoting the health and dignity of frail elders
Many elders struggle with disability and severe chronic illness and have difficulty getting to the doctor’s office. As a result, their health may suffer and lead to unnecessary ER visits, hospitalization, or nursing home care. In 1999, recognizing the needs of such elders and their families, we created the MedStar House Call program - MedStar Total Elder Care to provide full medical and social services that help elders remain in their homes with dignity. These teams now serve both Washington, D.C., and Baltimore, MD.
The MedStar House Call Program - MedStar Total Elder Care is nationally recognized for the quality and outcomes of our care. We serve patients at home with a team of geriatricians, nurse practitioners (NPs), social workers, office nurses, and coordinators. We make routine and urgent house calls (in-person or via telehealth with video or audio-only phone visits). Our medical staff is also available by phone 24/7 for urgent issues. We provide access to state-of-the-art hospital and specialty care. Additionally, our physician team follows our patients if and when they are admitted to the MedStar Washington Hospital Center.
The House Call program serves our neighbors in Washington, D.C., and Baltimore.
Medstar house call program .
(operating under MedStar Total Elder Care, LLC)

Our program services
Medical house calls and primary care by doctors and nurse practitioners with expertise in the care of older adults
Counseling and caregiver support by social workers and team staff
We offer tests and treatments at-home, and at the hospital as needed
Home delivery of most medications and equipment
Coordination of specialist care at MedStar Washington or MedStar Good Samaritan
Coordination of home nursing, rehab therapy, and hospice
Coordination of support services such as home aides and legal assistance
On-call physicians: 24 hours a day, 7 days a week (by phone)
Mobile electronic health record (EHR)
D.C. Neighborhood only – Case management for Medicaid Elderly Persons with Disabilities (EPD) Waiver
Hospital care and specialists
Our team coordinates emergency, hospital, and specialty care at MedStar Washington and MedStar Good Samaritan. Patients may keep their previous specialist doctors; we work with them as needed. We refer to MedStar Good Samaritan, MedStar Washington, for home-based podiatry or other new specialist care. If House Call patients require hospitalization, and 911 is not needed, our team can arrange transportation and admission to MedStar Good Samaritan or MedStar Washington when beds are available.
Social work services
Our dedicated team of social workers provides:
Psychosocial assessment
Care Coordination
Development of an individual treatment plan
Information and referral to community resources and supports
Caregiver education, support, and counseling
Advocacy to connect with other service networks and legal counseling
Crisis intervention
Assistance with identifying alternative living arrangements, as needed
Eligibility
Enrollment and insurance.
To qualify for the MedStar House Call Program, patients must:
Be 65 years or older and have difficulty getting to the doctor’s office
Have Medicare, Medicaid, or another participating insurance plan
Stop seeing their previous primary doctor and agree to have us take on that role following the first visit
Live in a qualifying ZIP code
Our office is open 8:30 a.m. to 4:30 p.m., Monday - Friday.
When calling about new patient enrollment, please have the following information:
Patient's name, address, telephone number
Patient's date of birth and social security number
Patient's next of kin and emergency contact information
Patient's health insurance information (including type and group number)
Patient's current medical conditions and concerns
Ability to retrieve patient's recent medical records
Baltimore neighbors, print and complete our Intake Questionnaire form
As in most doctor's offices, your main health insurance (such as Medicare) covers 80 percent of House Call visit fees, and any secondary insurance covers the other 20 percent. The patients who do not have any secondary insurance are responsible for the 20 percent co-pay.
Qualifying ZIP codes
View the map below to check if you live in a qualifying ZIP code. Call our Washington, D.C., or Baltimore location to confirm MedStar House Call Program eligibility at your exact address.
Washington, D.C.,
View our brochures
Baltimore region brochure
Washington, D.C., region brochure
Washington, D.C., region team - 202-877-0570
Physicians Eric De Jonge, MD, – Section Director Guy (Binny) Chang, MD Nurse Practitioners Nancy Sassa, CRNP - Chief Alexandra (Caitlin) Geary, CRNP Michelle Sullivan, CRNP Office Nurse Kendel Ogbeab, RN Social Workers Gretchen Nordstrom, LICSW - Chief Kellie Jones, LICSW Ruth Shea, LICSW Operations Manager Isi Koroma Care Coordinators LaWanda Holeman Sandra Mills Carrie Carmon Yvette Williams
Baltimore region team – 443-444-6100
Physicians George Taler, MD Sharareh Badri, MD Nurse Practitioner Dorothy Were, CRNP Adama Panda, CRNP Nurse Nerland Dimanche, RN, MSN Social Worker Marina Nellius, LMSW Operations Director Shereen Greene, MBA Care Coordinator Taurshica Lee
Operational support
Executive Director George Hennawai, MD AVP Operations Julie Beecher, MS, MPH
Baltimore Neighborhood
To learn more about our services in the Baltimore region, call us today.at 443-444-6100.
Washington, D.C., Neighborhood
To learn more about our services in the Washington, D.C., region, call us today at 202-877-0570
Related services

Look out for your health
A UnitedHealthcare® HouseCalls visit is a no-cost, yearly health check-in that can make a big difference.
Call 1-866-799-5895 ,
TTY 711, to schedule your visit.
HouseCalls brings yearly check-in care
To you at home.
Connect for up to a full hour of 1-on-1 time with a licensed health care practitioner. Every visit includes a physical, tailored recommendations on health care screenings and plenty of time to ask questions that matter to you.
After your visit, HouseCalls connects with your primary care provider (PCP) to help keep them informed about your health. It's a great way to feel confident knowing an extra set of eyes is looking out for you between regular PCP visits.
What is a HouseCalls visit?
[Text On Screen – SAY HELLO TO HOUSE CALLS]
Say hello to HouseCalls.
[Text On Screen- PAID ACTOR PORTRAYAL.]
HouseCalls is our way of looking out for your health, so you can focus on your future. Here’s what it’s all about.
[Text On Screen – HERE’S WHAT IT’S ALL ABOUT]
Once a year, a licensed health care practitioner can come to your home to spend up to an hour with you on your health and wellness.
[Text On Screen- EASY, CONVENIENT, INFORMATIVE]
It's designed to be easy, convenient and informative.
[Text On Screen- HEAD-TO-TOE EXAM]
[Text On Screen- IMPORTANT HEALTH SCREENINGS]
[Text On Screen- HEALTH GOALS DISCUSSION]
You'll get a head-to-toe exam, important health screenings and plenty of time to talk about your health goals.
We'll also provide guidance on managing your health and if you need it, give you referrals for other health plan resources and services.
HouseCalls is a great way to stay on top of your health between regular doctor's visits.
At the end of your visit, you'll get a personalized checklist so you can feel more confident in what to discuss with your regular doctor.
[Text On Screen- COST? NO EXTRA COST TO YOU]
[Text On Screen- INCLUDED IN YOUR HEALTH PLAN]
If you're wondering how much all of this is going to cost, the best part is, there is no extra cost to you. It's included in your health plan.
[Text On Screen- HOUSECALLS VIDEO VISITS ARE NOT AVAILABLE WITH ALL PLANS.]
A HouseCalls visit takes place in the comfort of your own home or by video if you prefer.
So, say hello to HouseCalls and invite us in for a visit today.
[Text On Screen – SAY HELLO TO HOUSE CALLS TODAY]
Access one of the most popular UnitedHealthcare offerings, at no cost to you
Schedule your visit
Call 1-866-799-5895 , TTY 711
Monday–Friday, 8 a.m.–8:30 p.m. ET
Your in-home health check-in
- Up to a full hour with a licensed health care practitioner
- Ask the questions that matter to you and get valuable health tips
- No cost — it's included in your health plan
Get rewarded
Meet your friendly housecalls medical staff.

Just like the professionals you see in your regular doctor’s office, our licensed health care practitioners may be nurse practitioners, physician assistants or medical doctors. They’re state licensed and maintain national certification.
We perform background checks on these professionals to provide additional peace of mind for our members. Your loved ones, caregivers or friends are welcome to be present during the visit — it’s up to you.
Ready to open the door to better health?
Getting ready for your housecalls appointment, tips to help you prepare: .
- Wear shoes that are easily removed to have your feet checked
- Make a list of upcoming appointments with your PCP and specialists
- Make sure all of your medications, both prescription and over-the-counter vitamins and supplements, are in their original bottles for our review
- If you record blood pressure readings, please have your results available for review
- If you have diabetes, please have your blood glucose meter handy
- Make a list of questions and concerns you’d like to discuss
During your appointment
- You'll have up to a full hour of 1-on-1 time with your health care practitioner for a physical, select lab tests, health screenings and more
- A HouseCalls visit can be completed while sitting at your kitchen table or in the living room, and you can use the time to ask any health-related questions
- The visit is tailored to your individual needs, so screenings and conversation topics can vary
After your appointment
Less travel time. more face time..
Think of HouseCalls as an extra layer of care — valuable 1-on-1 time you don't always get in the doctor's office. And it's tailored to your individual needs.
Schedule today
To secure your spot, call us at 1-866-799-5895 , TTY 711
Have a question?
Find answers to frequently asked questions.
If you have a specific question about your upcoming appointment or need to reschedule, call us at 1-866-799-5895, TTY 711 , Monday–Friday, 8 a.m.–8:30 p.m. ET
We're here to help.
REcent Updates
Making sense of Medicare isn’t easy. Parts, A, B, C, D; HMOs; PFFS plans; SNPs. Navigating the system can feel like learning to code… blindfolded… with one hand tied behind your back. The point is, it can be overwhelmingly complicated. But at MD at Home one of our goals is to make quality healthcare easier to access and understand, so in this post we’re decoding the ins and outs of Medicare Advantage Plans, from A to Z.
No one wants to think about the likelihood of unfortunate events. Death, accidents, illness - we avoid these topics like the plague (both literally and figuratively). Why? Because they make us sad, because they make us uncomfortable, because sometimes superstition gets the best of us and we don’t want to tempt fate. But as difficult as they may be, these are important conversations to have with your loved ones or potential caregivers now, so that if and when the time comes, your wishes are clear. What we’re talking about is an advance healthcare directive. Here’s everything you need to know.
In 1930, house calls were standard practice for physicians, accounting for approximately 40 percent of patient visits. By 1950, this number had fallen to 10 percent, and by 1980, only about 1 percent of patient visits happened in the home. But as they say, everything old is new again, and with the coming demographic changes, it seems doctors may be making more home visits in the near future.
Diabetes and depression can each be conditions with devastation consequences on their own, let alone when a single individual suffers from both. Often times, the symptoms of one can exaggerate and accelerate the symptoms of the other, but fear not! There are a few simple steps you can follow to alleviate the symptoms and prevent the onset of both.
MD at Home provides home care, home medical doctors, and housecall physicians to patients in need with a focus on p reventing readmissions during the transition from an acute care setting to the home. For over 20 years, we’ve served as the premier healthcare resource for primary care and geriatric medicine for homebound patients in the Chicagoland area. Partnering alongside some of Chicago’s most established and respected institutions, we tailor our programs toward modern guidelines with an unwavering focus on clinical excellence, patient satisfaction, and measured clinical outcomes. Our continuum of care and individual care plans highlight the importance of readmission reduction and high level transitions from the hospital to the home setting. MD at Home is transforming healthcare through our collaborative, proactive, and preventative approach to patient health.
Our approach reduces unnecessary hospitalizations and focuses on helping patients and caregivers better manage individual health from the comfort of their home. Through our expertise in primary care and geriatric medicine, our licensed clinicians deliver a comprehensive approach in the management of chronic conditions to homebound patients, and our highly trained physicians and nurses are certified to perform most of the same services offered in a physician's office. MD at Home is transforming reactive, crisis-oriented care into proactive, preventive medicine, reducing unnecessary emergency room visits, hospitalizations, and 30-day readmissions.
Who Qualifies for a Housecall Visit?
Patients with difficulty leaving home due to a mobility limitation, patients with difficulty leaving the home due to cognitive impairment, patients who require the use of special transportation to leave the home, patients with an inability to leave the home and for whom leaving the home requires taxing effort, patients requiring the assistance of another person to leave the home, patients for whom leaving the home is medically contradictory due to the patient's medical condition, accepted insurance.
MD at Home accepts the following insurance policies:
- Medicare Part B
- Medicare Pametto GBA
- Blue Cross Blue Shield (XOF, R, XOX)
- Blue Cross Blue Shield (XOS - Must have Medicare Part B as primary insurance)
- Aetna (PPO)
- United Health Care (PPO)
- United Medical Resources (PPO)
Physician Careers
MD at Home is hiring Physicians and Nurse Practitioners. Physicians with MD at Home have a luxury many other medical doctors severely lack: time . Unlike a typical seven minute visit, our physicians spend an hour or more with each patient, gaining a holistic view of the patient's health within their native environment. This not only means more insight into the patient's daily life, but also into their care support system, including interacting with family members and caregivers. This not only leads to better care for patients , but better lives for our doctors. Our physicians only work typical workday hours, allowing them to spend more time with their families, avoiding obscure hospital rounds or late nights. Our physicians using cutting-edge EMR technology to maintain up-to-date health records for each and every patient so nothing gets lost in the shuffle.
A Letter to Physicians
More time with patients, more time with your family, move healthcare forward, schedule a home visit, fast. simple. secure..
Our HIPAA-compliant online referral system is secured with 256-bit AES encryption, the same encryption level used by most online banking systems and the same SSL technology that fuels most SecureFax systems already in use by hospitals. Prefer to schedule a visit by phone? Give us a call at (312) 243-2223. If you're a healthcare professional, please send additional medical documentation to our fax at (312) 243-8450.
HIPAA Certification Security Audit
Prefer to submit a referral by fax? Click the button below to download one of our paper referral forms and fax it to (312) 243-8450.
Area of Service
Our address.
Referral Fax: (312) 243-8450 Clinical Fax: (312) 243-2227 2003 W. Fulton Street, Suite 303 Chicago, IL 60612
Office Hours
Patient Portal Phone: (312) 243-2223 Monday – Friday 9:00AM – 5:00PM Closed Saturdays and Sundays
Ad-free. Influence-free. Powered by consumers.
The payment for your account couldn't be processed or you've canceled your account with us.
We don’t recognize that sign in. Your username maybe be your email address. Passwords are 6-20 characters with at least one number and letter.
We still don’t recognize that sign in. Retrieve your username. Reset your password.
Forgot your username or password ?
Don’t have an account?
- Account Settings
- My Benefits
- My Products
- Donate Donate
Save products you love, products you own and much more!
Other Membership Benefits:
Suggested Searches
- Become a Member
Car Ratings & Reviews
2024 Top Picks
Car Buying & Pricing
Which Car Brands Make the Best Vehicles?
Car Maintenance & Repair
Car Reliability Guide
Key Topics & News
Listen to the Talking Cars Podcast
Home & Garden
Bed & Bath
Top Picks From CR
Best Mattresses
Lawn & Garden
TOP PICKS FROM CR
Best Lawn Mowers and Tractors
Home Improvement
Home Improvement Essential
Best Wood Stains
Home Safety & Security
HOME SAFETY
Best DIY Home Security Systems
REPAIR OR REPLACE?
What to Do With a Broken Appliance
Small Appliances
Best Small Kitchen Appliances
Laundry & Cleaning
Best Washing Machines
Heating, Cooling & Air
Most Reliable Central Air-Conditioning Systems
Electronics
Home Entertainment
FIND YOUR NEW TV
Home Office
Cheapest Printers for Ink Costs
Smartphones & Wearables
BEST SMARTPHONES
Find the Right Phone for You
Digital Security & Privacy
MEMBER BENEFIT
CR Security Planner
Take Action
How to Get a House Call in the Time of COVID-19
If you’re worried about the coronavirus, you may be able to get healthcare at home, either virtually or in person

If you’re not feeling well and want to see a doctor, you may be concerned that going to a physician’s office , an urgent care facility , or a hospital could expose you to COVID-19.
“People are understandably worried that they are going to get sick if they go to the doctor,” says Ateev Mehrotra, M.D., an associate professor of healthcare policy at Harvard Medical School who conducts research on the use of telemedicine to improve healthcare. “This is a situation where going to get care can put you more at risk, and people may want to seek other options.”
In March, the World Health Organization and the Centers for Disease Control and Prevention began calling for hospital and healthcare providers to increase the use of telehealth services to ease pressure on healthcare facilities and treat people quarantined at home, as well as to reduce exposure risks for those who don’t have the virus.
And now, there are a host of options for receiving non-emergency care in your own home, from a medical doctor, physician assistant, nurse practitioner , or nurse, depending on your particular health concerns.
Possibilities range from on-demand house calls you request through an app to telemedicine services, such as virtual doctor visits via smartphone or computer. Some services will diagnose you via video consultation, then determine whether you need to see an in-person provider at home.
Telemedicine can also be as simple as emails or phone calls with your regular doctor or having a healthcare provider email you a treatment plan based on your answers to a symptom questionnaire you fill out online, Mehrotra says.
House call and telemedicine services are generally used for issues such as minor burns and cuts, conjunctivitis, back strains, rashes, flu , and urinary tract infections. House call providers can also help people manage chronic conditions like high blood pressure and provide preventive care such as vaccines.
Home healthcare is appropriate even for many people diagnosed with COVID-19, according to the CDC, because the majority are only mildly to moderately ill and can manage their symptoms at home .
And people are taking advantage of these opportunities. A representative for Kaiser Permanente, a large integrated care organization, says it is conducting approximately 8,000 televisits a day. And Nick Desai, CEO of the app-based Heal, says, “We are seeing a 340 percent increase in demand for Heal telemedicine and house call services.”
Many of the services above are covered by insurance. Of course, you may still have copays, coinsurance, or deductibles, but some fees, like copays, may be lower than those for in-person doctor’s visits. And if you don’t have insurance, you may be able to choose from a menu of services with flat fees, which run from about $50 to $200, depending on your medical needs.
5 Ways to Get Healthcare at Home
Your regular doctor. Your physician may not be able to make an old-fashioned home visit, but there’s a lot she can do by phone or by video chat via computer, tablet, or smartphone. Just under 30 percent of doctors used such telemedicine and virtual visit tools before the coronavirus pandemic, but that number is now expected to rise.
Even if your doc isn’t online yet, many will answer follow-up questions, refill prescriptions, or advise you on managing a chronic condition by phone, email, or text, or through the office’s patient portal.
Your health insurer. You may have access to at-home healthcare through your health insurance. Nearly 9 out of 10 employers with 500 or more workers that provide health insurance have a telemedicine program.
Insurers typically partner with outside vendors such as Teladoc Health, a network of primary care physicians who diagnose routine, non-emergency medical problems via the telephone or video. They can also prescribe medications, send your records to your regular doctor, and make referrals, and are available around the clock seven days a week.
Right now, Teladoc and other telehealth companies are touting themselves as a first stop for coronavirus information, and sometimes other resources as well. Amwell, another telemedicine company that often works with employers and health insurance plans, for instance, now has an infection control officer on call at all times.
For those without insurance, many of these telemedicine services charge a flat fee. Amwell, for example, charges $69 for an online urgent care visit and can provide prescriptions and recommendations for in-person follow-ups with specialists. MDLive urgent care consultations are $75 without insurance.
Local urgent care and walk-in retail clinics. An increasing number of these kinds of facilities, which may be freestanding or located in or next to chain pharmacies or big box stores, are offering video consults that allow you to get in touch with a healthcare provider quickly.
CVS, for example, which operates more than 1,000 MinuteClinics inside its stores, has video visits 24/7 for $59. These visits aren’t covered by insurance, but you can pay for them with money from a flexible spending account or health savings account, if you have one.
Through Westmed, a chain of urgent care clinics in New York and Connecticut, you can get a virtual phone or video consult between 9 a.m. and 6 p.m. Monday through Friday. Westmed takes insurance and charges $49 for those without coverage.
House calls on demand. The old-fashioned house call is making a comeback, fueled by advances like portable X-ray machines and apps that can make your cell phone function like an ultrasound machine. This option may be especially useful for people who are too ill to get to a doctor, and currently, those who are quarantined at home.
The on-demand house call company Heal promises to get a healthcare provider to your home within a few hours between 8 a.m. to 8 p.m. seven days a week. While Heal’s doctors can’t test for COVID-19, they can refer symptomatic patients to state and federal health officials. Heal, which operates in more than a dozen cities, accepts many insurance plans, but if yours isn’t covered, the cost is $159.
Remedy, another on-demand house call service, says it will send a healthcare provider to your home within 2 hours. It takes insurance, but if you don’t have coverage, it charges $199 for a house call.
High-tech healthcare hybrids. A growing number of technology companies moving into the healthcare space offer both virtual and in-person care. These hybrids are mainly in major metropolitan areas, and some are still small.
Forward, for example, which launched in 2016, is based in San Francisco and also has several locations in Southern California, New York City, and Washington, D.C. It doesn’t accept insurance, instead charging a $149-per-month fee for 24/7 remote access to its doctors, as well as unlimited in-person doctor visits.
One Medical, a network of primary clinic providers that offers virtual and in-person care, is larger, with 70 clinics in nine cities. It accepts insurance but charges a $199 fee on top of that to use its services. It also has relationships with 6,000 employers who cover the membership fee for workers. Carbon Health, which is based in California, accepts many insurance plans and also offers a virtual visit for a $49 flat fee.
Know the Limitations
Of course, getting care outside a traditional healthcare facility has its limits. “I can ask someone about their breathing, but I can’t look into their lungs,” Mehrotra says. “A telephone or video call can be a good place to start, but where you get care really depends on the condition being addressed.”
Those limitations are especially important to keep in mind right now. “The symptoms of COVID-19 are difficult to differentiate from those of the typical seasonal flu or a common cold,” says Will Kimbrough, M.D., senior medical director of clinical services at One Medical.
At all times, checking with a telehealth provider or calling your doctor can help you decide whether you need to be seen in an office setting or an emergency room, or can safely remain at home, Kimbrough says.
If you suspect an emergency in your household, call 911 right away. That includes difficulty breathing, chest pain or other severe pain (especially abdominal), broken bones, coughing up or vomiting blood, unresponsiveness, bleeding that can’t be stopped with direct pressure , and signs of a stroke , such as facial drooping, arm weakness, and speech difficulty.
Additional reporting by Jessica Branch
Donna Rosato
As a journalist on the special projects team at Consumer Reports, I investigate issues that affect consumers' health, finances, privacy, and safety. My particular focus is on helping people untangle problems with medical bills, cover steep healthcare costs, finance the skyrocketing cost of college, and manage student debt. I was previously a writer at Money magazine, wrote for The New York Times and was a business reporter at USA Today. If you have a tip, follow me on Twitter (@RosatoDonna).
Sharing is Nice
We respect your privacy . All email addresses you provide will be used just for sending this story.
Trending in Healthcare
The EpiPen Alternative That Costs Just $10
If the Doctor Asks for Your Social Security Number, Do This
How to Make an Online Will
5 Reasons to Never Pay Doctor or Hospital Bills With a Medical Credit Card or Loan

Medical House Calls

Quality Care At Your Door
Say goodbye to the hassle of sitting in a crowded waiting room or struggling to make time in your busy schedule to see your doctor.
With medical house calls, you can see a medical provider stress-free in the comfort, convenience, and privacy of your home.
- Medical Evaluation
Hassle-Free Health Care

No wait times, no crowded waiting rooms

Easy online scheduling with same-day availability

Reduced risk of exposure to germs and viruses
House calls for urgent & primary care needs, urgent care house calls.
On-demand medical attention when you need it most without leaving your home.
Receive one-on-one attention with a licensed medical provider who will diagnose, treat and prescribe medications if need be.
Urgent Care House Calls are Ideal for:
- Cold & Flu
- Sore Throat
- Bronchitis
- Sinus Infection
- Ear Infection
- Urinary Tract Infection (UTI)
- Stomach Flu
- Food Poisoning
- Muscle or Joint Pain
- Cuts, Scrapes, & Burns
- Migraines & Headaches

Primary Care House Calls
Comprehensive primary care services in the comfort of your own home.
Ideal for those with busy lifestyles and who would prefer to see a medical provider in the privacy of their residence.
Primary Care House Calls are Ideal for:
- Annual Wellness Exam
- School, Sports, & Employment Physical Exams
- Nutrition, Fitness & Exercise Consultations
- Mental Health Consultations (Anxiety & Depression)
- Pre-Op Clearance
- Anti-Aging Solutions
- Preventative Medicine
- Chronic Disease Management
- Lab Testing & Blood Work
- Prescription Refills
- Referrals to Specialists
Hear From Our Clients
Each of our reviews is a testament to the warmth, professionalism, and personalized attention we bring to every appointment. Your health journey is our passion, and these stories inspire us to continue providing exceptional care.
Ready to book?
Returning customer? Click here to login
Email address (as your login)
Remember me
Lost your password?
- First Name *
- Last Name *
- Country * United States
- Address * Street Address Address Line 2 City ZIP Code
- State * State Arizona California Georgia Hawaii Idaho Illinois Massachusetts Nevada New Jersey New York Texas Utah
- First Time Client
- Return Client
- Provider * Atlanta Austin Boise Boston Bronx & Westchester Brooklyn Central Coast Central New Jersey Chicago DEFAULT PROVIDER Hawaii - Oahu Inland Empire & Palm Springs Las Vegas Los Angeles Manhattan North New Jersey Orange County Phoenix Queens & Nassau County Sacramento San Diego St. George Suffolk County Tucson Utah
- GA Service House Call
- Date of Birth * Month Day Year
- Preferred Date of Appointment * MM slash DD slash YYYY
- Preferred Appointment Time * Select Time 8:00 AM 8:30 AM 9:00 AM 9:30 AM 10:00 AM 10:30 AM 11:00 AM 11:30 AM 12:00 PM 12:30 PM 1:00 PM 1:30 PM 2:00 PM 2:30 PM 3:00 PM 3:30 PM 4:00 PM 4:30 PM 5:00 PM 5:30 PM 6:00 PM 6:30 PM 7:00 PM 7:30 PM 8:00 PM 8:30 PM 9:00 PM 9:30 PM
- Book in Date & Time Preference * To see the booking calendar, please enter a zip code above. Please be aware, we will make every effort to accommodate your requested time. Times are subject to change based on availability. A member of our dispatch team will work to confirm your appointment as soon as we receive your booking.
- Rapid Covid Antigen Test
- Rapid Strep Test
- Rapid Flu Test
- Rapid Urinalysis Test
- Ultrasound or X-Ray
- Echocardiogram
- Anti-Inflammatory
- Pain Blocker
- Anti-Nausea
- Super Immune Boost
- Myers Cocktail
- Mental Clarity (NAD)
- Energy (B12)
- Glow (Vitamin D)
- Beauty (Biotin)
- Fat Burner (Lipostat)
- Mental Clarity (50mg)
- Mental Clarity (100mg)
- Person added
- <span class="gform-field-label gfield_label_product">Automatic Group Discount</span> <span class="screen-reader-text">Quantity</span> $0.00
- Remove Person
- What is your house call regarding? * **Please do not provide any personal health info, only general info
- Order Summary Person 1 Subtotal: $0 Service Fee: $0 Lab Fee Total: $0 Automatic Group Discount : $0 Coupon Discount: $0 Total $0.00
- I agree to the Term of Service , Privacy Policy , Consent To Treat , and Cancellation Policy
- Cancellation Terms . Bookings are subject to a $50 cancellation fee.
- Sign-up for emails to get exclusive offers & be the first to know about new services!
- Sign up for texts. By checking this box, you agree to receive recurring automated promotional and personalized marketing text messages (e.g. cart reminders) from ConciergeMD at the cell number used when signing up. Consent is not a condition of any purchase. Reply HELP for help and STOP to cancel. Msg frequency varies. Msg & data rates may apply. View Terms & Privacy .
House Call FAQs
Do you offer same-day appointments how long will it take for a provider to arrive at my location.
Yes, we understand the importance of prompt healthcare. We make every effort to offer same-day appointments whenever possible. We do our best to arrive within one to two hours of your booking.
Do we offer house calls on weekends or evenings?
Yes, we understand that your schedule may be busy during weekdays. We offer flexible scheduling, including weekends and evenings and try our very best to accommodate your preferred times. Our medical house call services are available seven days a week. We’re here to provide you with personalized healthcare when it’s most convenient for you.
Do you provide service to my place of business or hotel?
Yes, ConciergeMD is an at-your-door service. We will come to your office, home or hotel 7 days a week, 365 days a year.
What should I expect during a House Call visit?
During a house call visit, you’ll meet with the same types of professionals you see in a doctor’s office — a licensed health care practitioner. After introductions, your provider will perform a thorough history and physical examination appropriate for your specific complaints and will then recommend the appropriate treatment options. After all of your questions are answered, instructions are given, your provider will depart.
Who will come to my home for the House Call visit?
You’ll meet with a licensed health care practitioner who may be a nurse practitioner, physician assistant or medical doctor. Just like the professionals you see in your regular doctor’s office, our staff are state licensed and maintain national certification. We take the extra step of performing background checks on our clinical staff to provide additional assurance for our members.
How does a house call differ from a regular doctor office visit, Urgent Care Facility, or an Emergency Room?
We bring excellent, quality healthcare to you and on your schedule. You are seen in the comfort of your home, hotel or office and at a convenient time for you. You never have to wait again in an overcrowded waiting room. You will not be sitting next to sick patients for an extended period of time. We can treat the same illnesses that you would normally go to see in a primary care physician’s office. Our fees are affordable and often less expensive that one would pay at an Urgent Care Center or an Emergency Department.
Do you provide medications?
Our providers carry injectable medications and can prescribe medications to your local pharmacy for pick up.
What if the physician decides my illness requires additional testing and/or treatment?
We can provide all additional testing (e.g. x-rays, EKG, ultrasound, etc.) in the comfort and convenience of your home or hotel suite, and can provide referrals to any specialty if needed.
Do you draw labs?
We do offer a variety of laboratory tests and studies that can be completed in the home, hotel or workplace. Blood work can be drawn and delivered to local laboratories when necessary.
Do you offer X-ray and ultrasound services?
X-ray and ultrasound services are available to be brought to you upon request. A certified x-ray technician brings a portable x-ray machine to your home, hotel room, workplace, or wherever you are. The x-ray images are processed on site, and films are reviewed by your house call physician or a board certified radiologist. Copies of the images may be provided to the patient upon request. Various portable ultrasound studies are also available. Additional studies, including CT or MRI may be completed at a radiology center of your choice.
Will you care for the home-bound, or elderly, as a primary care doctor?
Yes, with pleasure, under most circumstances.
If I am experiencing an emergency, should I book a house call?
Concierge MD is not an Emergency Room replacement and we do not treat patients experiencing chest pain, shortness of breath, head trauma, loss of consciousness, or other life-threatening emergencies, as these conditions may require immediate hospitalization. If you are having a medical emergency, please go directly to the E.R. or dial 911 immediately.
Do you accept health insurance?
Although most insurance companies will reimburse a portion of the visit or apply the amount to your deductible if it has not been met at this time, we do not accept insurance in the traditional sense. We will provide you with the documentation that can be submitted to your health insurance company for reimbursement. You may be eligible for reimbursement through your “out-of-network” option of your PPO or HMO plan. We do not guarantee any reimbursement.
May I utilize your services while I still see my regular physician with whom I have a long term relationship?
Yes! We understand the tremendous value in long standing Doctor Patient relationships. We will confer with your physician and coordinate your care together.
What are the benefits of using Concierge MD?
- Same-day service and appointments, usually within one to two hours of your call.
- Extended and unhurried medical visits.
- Comprehensive medical care in the comfort of your own environment.
- No more waiting in waiting rooms.
- House, Office, or Hotel Visits.
- On site diagnostic testing.
- Personal relationship with your licensed clinical provider.
- Prompt follow-up on all tests and reports.
- Coordination of care with carefully selected specialists.
- Fast and Easy Prescription Renewal Anytime/Anywhere.
- Prompt telephone feedback with lab and radiology test results.
Who uses Concierge MD?
For those of you who are frustrated by excessive wait times in the ER or refuse to stay in an overcrowded urgent care clinic, Concierge MD offers a time saving, efficient alternative. With Concierge MD, you can now be taken care of in the comfort of your home, hotel or workplace, with minimal interruption to your daily life.

How much do you save with a house call?
The time and monetary savings accompanied with a house call visit are significant because of the convenience of bringing healthcare to you. House call visits offer value by providing a licensed health care practitioner on your schedule. If you are a busy individual and value the little time you have to enjoy, then ConciergeMD offers you an excellent solution when you or a loved one need medical attention. Now you can afford the luxury of not having to leave your home, office, or hotel when you are sick, deal with traffic, and spend significant time waiting for a doctor’s appointment or in the waiting room with other sick patients waiting to be seen. This can often take hours of your time.
Do I have to be a member of Concierge MD to have a provider visit me at my home, office, or hotel?
No! ConciergeMD is available to everyone. There are no membership fees or subscriptions required.
Does Concierge MD offer services for employers?
Concierge MD offers custom corporate service programs to provide medical care for your employees living in, working in, or visiting your local area. Our full line of services is available as well as custom arrangements tailored to your company’s needs. Rather than putting off a meeting or delaying a flight, we arrange medical treatment in the comfort of your employee’s office, house or hotel, and make sure that they rapidly get on the road to recovery. Make Concierge MD a valuable asset and addition to your benefits package by keeping your employees healthy and happy.
Do you offer virtual care instead? I would prefer to do this over the phone.
Yes, we do offer virtual care options for your convenience. If you prefer a remote consultation, you can learn more and schedule your virtual appointment by visiting our Virtual Consultations Page. We’re here to provide healthcare in the way that suits you best.
Experience Care with ConciergeMD
ConciergeMD offers coverage throughout the United States.

House Call Doctor Visits Make Life Easier for Seniors and Caregivers

Important: This is an informational article to explain how house call doctor visits can benefit seniors. DailyCaring isn’t a medical organization, we aren’t medical professionals, and we aren’t affiliated with any healthcare organizations. We aren’t qualified to respond to any medical questions.
House call doctor visits benefit older adults and caregivers
Getting your older adult to the doctor’s office for an appointment can be difficult or sometimes impossible.
Whether they’re frail, can’t walk on their own, or have Alzheimer’s or dementia , getting out of the house is hard on both of you. Going to a doctor’s office can also expose seniors to germs or harsh weather.
We explain what a house call doctor is, what type of insurance they accept, how to find one, and what to look for in terms of services.
What is a house call doctor?
Today, many doctors are bringing back the old practice of visiting patients in their homes. With house calls, older adults don’t have to go through the stress and difficulty of getting to the doctor’s office. And neither do you.
Another bonus is that these doctors usually spend more time with patients. You won’t have to fit all your questions into a 15 minute visit.
Do they accept Medicare?
Yes, many house call doctors accept Medicare , private insurance, and sometimes Medicaid . It usually costs the same as a regular office visit.
But every house call doctor is different, so make sure you understand their fees and accepted insurance plans before making an appointment.
How to find a house call doctor
Some large health care systems like Kaiser Permanente or the VA have programs that include home visits by doctors and nurses. For example, Kaiser’s home-based palliative care program includes house calls.
Even your older adult isn’t part of a large health network, it’s worthwhile to ask your older adult’s doctor if they have home doctor visit programs.
The American Academy of Home Care Medicine’s provider directory is another way to locate a house call doctor in your area.
You can also use Google to search for “house call doctor” + your city or county or “home doctor visit” + your city or county (don’t include the quotation marks).
What to look for in a house call doctor
Before booking an appointment, make sure you understand the doctor’s services, fees, and billing.
Questions to ask:
- Do you specialize in treating seniors, people with Alzheimer’s or dementia , or those with multiple chronic conditions ?
- Do you accept Medicare , Medicaid , or my older adult’s private insurance plan?
- If we want, can we also keep my older adult’s primary care doctor?
- Will you communicate with my older adult’s existing doctors and specialists so their care is coordinated?
Examples of house call doctor private practices
We want to be clear that we’re not recommending any specific home doctor services or companies and aren’t affiliated with any of these businesses. These are examples to give you an idea of what a house call doctor looks like and the type of services that are typically offered.
Examples of what a house call doctor looks like:
- Visiting Physicians Association (VPA)
- Bay Area House Call Physicians
- Kindred House Calls
Recommended for you:
- 4 Expert Tips for Managing Multiple Chronic Health Conditions in Seniors
- 7 Tips for Helping Seniors at the Doctor: Being a Health Advocate
- Should Seniors See a Geriatrician?
By DailyCaring Editorial Team Image: Now It Counts
This article wasn’t sponsored and doesn’t contain affiliate links. For more information, see How We Make Money .
- Share Article on:
Related Articles

Prevent Falls with 5 Warning Signs of Mobility Issues in Seniors

4 Great Sources of Tasty Low Sodium Recipes for Seniors

5 Questions to Ask Doctors About Tests and Treatments for Seniors

4 Common Eye Diseases That Cause Blindness in Aging Eyes
18 comments, tony carrancho.
My parent s lives in [redacted for privacy]. How do i get started locating a house call doctor. I am pretty sure there insurance covers this. Thank you. TONY
DailyCaring
We hope the tips and suggestions in the article above will help you find a house call doctor in your parents’ local area.
Susan Quercio
My 95 year old father has a deep cough and he is disoriented. Temp 99 degrees.
Please contact your father’s doctor immediately or the local hospital to find out how to safely get him examined by a doctor (to reduce risk of exposure to Covid-19).
DailyCaring isn’t a medical organization, we aren’t medical professionals, and we aren’t affiliated with any healthcare organizations.
Ruby m VanNostern
I live in [redacted for privacy] and need a doctor visit in home.
This article includes suggestions for how you can find house call doctor services in your area. At DailyCaring, we aren’t doctors and don’t provide any medical services. We hope you’re able to find a great house call doctor in your area.
Stewart Goldman
need Doctor for a home visit Andrews N.C.
Joseph Artusa
I need a doctor
Linda Williams
I was released from the hospital on Thursday after 5 days.I am not able to go to Dr office but most definitely need to be checked.Still having breaking problems and am very week.I have severe asthma and blood pressure was running very high from so much steroids.Could I possibly get help.Thanks so much.
I’m so sorry to hear that you’re not feeling well. Since you’re noticing some issues with your recovery, it’s essential to call your primary doctor immediately. Since they’re the ones who have been treating you and are familiar with your recent hospitalization, they’re the best people to advise you on what you need. If you need help getting to your doctor’s office, you may want to contact your local Area Agency on Aging or a ride sharing service. Or, use the tips in this article to search for a doctor in your area who makes house calls.
Here are some articles that may be helpful: — 8 Ridesharing Services for Seniors https://dailycaring.com/8-ridesharing-services-for-seniors/ — 6 Affordable Senior Transportation Options https://dailycaring.com/6-affordable-senior-transportation-options/ — Local Community Resources for Seniors and Caregivers: Area Agency on Aging (to connect you with local organizations that may be able to help) https://dailycaring.com/local-community-resources-for-seniors-and-caregivers-area-agency-on-aging/ — 4 Ways to Know If Seniors Need to Return to the Hospital https://dailycaring.com/4-ways-to-know-if-seniors-need-to-return-to-the-hospital/
(DailyCaring doesn’t provide any services and isn’t affiliated with any medical providers.)
What areas do you service?
This article explains that house call doctor services are available and could help senior and caregivers. We also share suggestions for finding one in your area, but we do not provide any services ourselves. I hope you’re able to find a great local house call doctor!
What areas do you service
This article includes suggestions for finding house call doctor services in your area. We at DailyCaring aren’t doctors and don’t provide any medical services. I hope you’re able to find a great house call doctor in your area.
need a home care doctor
I hope the information above helps you find a great home care doctor in your area.
Leave a Reply Click here to cancel reply.
Cancel reply.

House Calls
Scheduling your appointment.
Please call or email to request an appointment. Appointments are scheduled 1-2 weeks in advance according to when a doctor will be seeing patients in your area. We will call you to confirm a one to two hour appointment window for the doctor’s arrival at your home.
Your first visit

- Name and location of primary care physician
- Past medical and ocular history
- Any records from previous eye doctors, if available
- Current list of medications, or the bottles from the pharmacy. This includes all medications, over the counter supplements and vitamins– not just eye drops!
- Insurance cards
- Hospital discharge papers, if applicable
Follow up care
Your doctor will work with you to determine the frequency of future visits based on your specific ocular health needs. You can always call for a visit if you feel you need to see the doctor sooner than your next scheduled appointment!
- ALL MOSCOW TOURS
- Getting Russian Visa
- Top 10 Reasons To Go
- Things To Do In Moscow
- Sheremetyevo Airport
- Domodedovo Airport
- Vnukovo Airport
- Airports Transfer
- Layover in Moscow
- Best Moscow Hotels
- Best Moscow Hostels
- Art in Moscow
- Moscow Theatres
- Moscow Parks
- Free Attractions
- Walking Routes
- Sports in Moscow
- Shopping in Moscow
- The Moscow Metro
- Moscow Public Transport
- Taxi in Moscow
- Driving in Moscow
- Moscow Maps & Traffic
- Facts about Moscow – City Factsheet
- Expat Communities
- Groceries in Moscow
- Healthcare in Moscow
- Blogs about Moscow
- Flat Rentals
Healthcare in Moscow – Personal and Family Medicine
Emergency : 112 or 103
Obstetric & gynecologic : +7 495 620-41-70
About medical services in Moscow

Moscow polyclinic
Emergency medical care is provided free to all foreign nationals in case of life-threatening conditions that require immediate medical treatment. You will be given first aid and emergency surgery when necessary in all public health care facilities. Any further treatment will be free only to people with a Compulsory Medical Insurance, or you will need to pay for medical services. Public health care is provided in federal and local care facilities. These include 1. Urban polyclinics with specialists in different areas that offer general medical care. 2. Ambulatory and hospitals that provide a full range of services, including emergency care. 3. Emergency stations opened 24 hours a day, can be visited in a case of a non-life-threatening injury. It is often hard to find English-speaking staff in state facilities, except the largest city hospitals, so you will need a Russian-speaking interpreter to accompany your visit to a free doctor or hospital. If medical assistance is required, the insurance company should be contacted before visiting a medical facility for treatment, except emergency cases. Make sure that you have enough money to pay any necessary fees that may be charged.
Insurance in Russia

Travelers need to arrange private travel insurance before the journey. You would need the insurance when applying for the Russian visa. If you arrange the insurance outside Russia, it is important to make sure the insurer is licensed in Russia. Only licensed companies may be accepted under Russian law. Holders of a temporary residence permit or permanent residence permit (valid for three and five years respectively) should apply for «Compulsory Medical Policy». It covers state healthcare only. An employer usually deals with this. The issued health card is shown whenever medical attention is required. Compulsory Medical Policyholders can get basic health care, such as emergencies, consultations with doctors, necessary scans and tests free. For more complex healthcare every person (both Russian and foreign nationals) must pay extra, or take out additional medical insurance. Clearly, you will have to be prepared to wait in a queue to see a specialist in a public health care facility (Compulsory Medical Policyholders can set an appointment using EMIAS site or ATM). In case you are a UK citizen, free, limited medical treatment in state hospitals will be provided as a part of a reciprocal agreement between Russia and UK.
Some of the major Russian insurance companies are:
Ingosstrakh , Allianz , Reso , Sogaz , AlfaStrakhovanie . We recommend to avoid Rosgosstrakh company due to high volume of denials.
Moscow pharmacies

A.v.e pharmacy in Moscow
Pharmacies can be found in many places around the city, many of them work 24 hours a day. Pharmaceutical kiosks operate in almost every big supermarket. However, only few have English-speaking staff, so it is advised that you know the generic (chemical) name of the medicines you think you are going to need. Many medications can be purchased here over the counter that would only be available by prescription in your home country.
Dental care in Moscow

Dentamix clinic in Moscow
Dental care is usually paid separately by both Russian and expatriate patients, and fees are often quite high. Dentists are well trained and educated. In most places, dental care is available 24 hours a day.
Moscow clinics

«OAO Medicina» clinic
It is standard practice for expats to visit private clinics and hospitals for check-ups, routine health care, and dental care, and only use public services in case of an emergency. Insurance companies can usually provide details of clinics and hospitals in the area speak English (or the language required) and would be the best to use. Investigate whether there are any emergency services or numbers, or any requirements to register with them. Providing copies of medical records is also advised.
Moscow hosts some Western medical clinics that can look after all of your family’s health needs. While most Russian state hospitals are not up to Western standards, Russian doctors are very good.
Some of the main Moscow private medical clinics are:
American Medical Center, European Medical Center , Intermed Center American Clinic , Medsi , Atlas Medical Center , OAO Medicina .
Several Russian hospitals in Moscow have special arrangements with GlavUPDK (foreign diplomatic corps administration in Moscow) and accept foreigners for checkups and treatments at more moderate prices that the Western medical clinics.
Medical emergency in Moscow

Moscow ambulance vehicle
In a case of a medical emergency, dial 112 and ask for the ambulance service (skoraya pomoshch). Staff on these lines most certainly will speak English, still it is always better to ask a Russian speaker to explain the problem and the exact location.
Ambulances come with a doctor and, depending on the case, immediate first aid treatment may be provided. If necessary, the patient is taken to the nearest emergency room or hospital, or to a private hospital if the holder’s insurance policy requires it.
Our Private Tours in Moscow
Moscow metro & stalin skyscrapers private tour, moscow art & design private tour, soviet moscow historical & heritage private tour, gastronomic moscow private tour, «day two» moscow private tour, layover in moscow tailor-made private tour, whole day in moscow private tour, all-in-one moscow essential private tour, tour guide jobs →.
Every year we host more and more private tours in English, Russian and other languages for travelers from all over the world. They need best service, amazing stories and deep history knowledge. If you want to become our guide, please write us.
Contact Info
+7 495 166-72-69
119019 Moscow, Russia, Filippovskiy per. 7, 1
Mon - Sun 10.00 - 18.00
- Sign in / Join
- Contributor guidelines
- Privacy Policy
Power of AngularJS – A Comprehensive Guide to AngularJS
Comparing roofing materials – what works best for your climate, reduce packaging costs – 3 pro tips, 7 things to remember when buying a business phone system, open wellness -the rise of yoga and fitness app development, angularjs vs nodejs – a comparative comparison, predictive modeling and natural language processing, what is wireless planning and coordination (wpc), should you self-repair your phone, how much of your salary should you put into investments, 10 home-based side hustles you can start today, buster murdaugh net worth: the finances uncovered, your guide to achieving financial security, mortgage rates: what to expect in the future, the lifesaving convenience of emergency doctor home visits.
Emergencies don’t wait for appointments, and illness doesn’t adhere to schedules. In a world where time is of the essence, the concept of emergency doctor home visits is emerging as a beacon of hope. This blog delves into the lifesaving convenience of having a doctor come to your doorstep when you need it the most.
The Evolution of Medical Care
Traditional healthcare models often require patients to navigate crowded waiting rooms and adhere to strict appointment schedules. However, the landscape of medical care is changing rapidly, driven by the demand for convenience and accessibility. As a result, the concept of emergency doctor home visits is gaining traction.
What Are Emergency Doctor Home Visits?
Emergency doctor home visits, also known as house calls, entail a licensed medical professional coming to a patient’s residence to provide healthcare services. These services are not limited to minor ailments but encompass a wide range of medical needs, including urgent care, general consultations, and even specialized treatment.
The Benefits of Emergency Doctor Home Visits
- Immediate Access to Medical Care: The most significant advantage of home visits is immediate access to medical care. Patients can receive prompt attention without the need to travel or endure waiting times.
- Convenience: Home visits eliminate the stress and hassle of getting to a clinic or hospital. They are particularly beneficial for patients with mobility issues, children, or individuals with busy schedules.
- Personalized Care: Doctors can assess a patient’s home environment, which can be instrumental in diagnosing and treating certain conditions. This level of personalization is often challenging to achieve in a clinical setting.
- Reduced Risk of Infections: Home visits reduce the risk of exposure to infectious diseases that may be prevalent in clinical settings, making them an ideal choice during pandemics or flu seasons.
- Comprehensive Services: While house calls are often associated with primary care, they can encompass a wide array of medical services , from diagnostic tests to administering treatments.
When to Opt for an Emergency Doctor Home Visit
House calls are a suitable option in various situations:
- Urgent Medical Needs: When a patient requires immediate medical attention for issues like severe pain, breathing difficulties, or sudden injuries.
- chronic Conditions: Patients with chronic conditions, such as diabetes or hypertension, can benefit from routine check-ups in the comfort of their homes.
- Elderly Care: House calls are particularly valuable for the elderly, who may find it challenging to travel for medical appointments.
- Pediatric Care: Children with illnesses or injuries can be examined and treated without the stress of a clinical environment.
The Role of Technology
Advancements in telemedicine and mobile healthcare applications have significantly enhanced the feasibility and efficiency of emergency doctor home visits. Patients can request a house call through apps or websites, and doctors can access electronic health records and diagnostic tools on the go.
The Future of Healthcare
The rise of emergency doctor home visits reflects a broader shift in healthcare towards patient-centered models. It recognizes that healthcare should revolve around the patient’s needs and preferences, rather than the rigid structures of the past.
Real-Life Impact
One cannot truly grasp the value of emergency doctor home visits without considering their real-life impact. Whether it’s a senior citizen receiving timely care for a sudden ailment, a working parent addressing their child’s medical needs without disrupting their daily routine, or a patient avoiding the anxiety of crowded emergency rooms, these stories underscore the profound difference that this evolving facet of healthcare can make.
Challenges and Considerations
While the concept of emergency doctor home visits is promising, it’s not without challenges. Regulatory, logistical, and insurance-related hurdles must be navigated to ensure that this mode of healthcare becomes more widely accessible.
The concept of emergency doctor home visits offers a lifeline to individuals facing sudden health crises. However, it comes with a set of challenges and considerations. One primary challenge is response time, as navigating through traffic can delay the arrival of medical professionals. Additionally, the scope of care that can be provided at home may be limited, and some conditions may necessitate hospitalization. Ensuring that the healthcare provider is adequately equipped with necessary medical supplies is also crucial. Despite these challenges, the comfort and immediate attention offered by emergency doctor home visits remain invaluable, especially for the elderly, individuals with mobility issues, or those dealing with non-life-threatening emergencies.
In a world where time is precious and health is paramount, the convenience and immediacy of emergency doctor home visits are reshaping the way we access medical care. It’s a testament to the resilience and adaptability of the healthcare sector, continually evolving to meet the diverse needs of patients. As this model gains momentum, we can expect doctors to come to the doorstep of more patients, providing them with the comfort and expediency they need in times of necessity.
When it comes to preparing for international travel, one essential requirement that’s now a common part of the journey is a PCR test for travel . Whether you’re a seasoned traveler or embarking on your first adventure abroad, the need for a reliable PCR test is undeniable. Look no further than a qualified private doctor to ensure that your travel plans go off without a hitch.
RELATED ARTICLES
10 foods to avoid after miscarriage – what every woman should, 10 ways to reduce the appearance of wrinkles, induce labour: strategies for a smooth delivery, milialar – deciphering the mystery of tiny skin bumps, leave a reply cancel reply.
Log in to leave a comment
7 Tips to Soundproof Your Small Room
What to do when you have a flat tire, editor picks, what are the best career options for 10th-12th students: vedic astrology..., the importance of hiring a marble restoration company, personal loan vs. using your savings: which is better, popular posts, list of top android games in action genre, challenges you may face while filing tax returns, bathroom decor ideas for a heavenly spacious feel, popular category.
- Business 335
- Education 75
- Marketing 36
- Celebrity 28
- Real Estate 26
- Dmca Removal
Copyright 2023 Daily Dialers

Urgent care vs emergency room: What's the difference?

It’s Saturday, and the cold you’ve been nursing for the past few days seems to be getting worse. You’ve vomited once and have a fever. Should you head to a hospital emergency room or an urgent care clinic?
Learn more about our urgent care Learn more about our ER
If you’ve ever wondered whether to go to an ER or an urgent care clinic, you’re not alone. As physicians, we’re often asked by family, friends and patients if their symptoms warrant an ER visit, a trip to an urgent care clinic, a call to their primary care doctor or simply management at home.
If you are experiencing mild symptoms , such as mild aches and pains, a mild cough, etc., that could be caused by the flu, COVID-19, RSV or hundreds of other viruses, consider “doing what your mom used to tell you” — rest, drink plenty of fluids, take over-the-counter medications like Tylenol, if needed, and monitor your symptoms.
If your symptoms don't improve over time, or if they worsen, calling your primary care physician may be beneficial. Many primary care physicians are now offering virtual visits and can assess patients by a phone or video call fairly quickly.
However, if your symptoms are more severe and can’t wait for an appointment with your doctor, consider your other options for care.
Urgent Care
Unless a condition is life-threatening, a trip to urgent care is generally a better use of a patient’s time and resources to treat injuries, fevers, infections and other ailments.
Urgent care centers often have far shorter wait times than the ER and cost less than a traditional hospital emergency room visit. And many, like our UChicago Medicine Dearborn Station , UChicago Medicine Medical Group - Homewood and UChicago Medicine River East urgent care centers, offer convenient benefits such as walk-in appointments and on-site x-ray.
There are a variety of conditions treated at our urgent care centers , but common reasons to visit one include:
- If you are experiencing mild to moderate cold symptoms and not sure whether it is flu, COVID-19 or RSV.
- If you have a sore throat and are concerned it is viral or strep throat.
- If your virus or cold symptoms developed into infections, like ear infections or pneumonia, and may require antibiotics.
Our urgent care clinics have board-certified physicians on staff who can test for and treat these conditions and much more. We treat both adult and pediatric patients and are available 7 days a week, from 8 a.m. to 8 p.m. during weekdays and 8 a.m. to 4 p.m. on weekends and holidays.
If necessary, urgent care providers can also connect you with a higher level of care.
Emergency Room
You should call 911 or come right to the emergency room if you’re systemically sick. That’s when an illness affects your entire body, and you have severe pain or sudden onset of severe symptoms, a fever that won’t break, or “something doesn’t work,” like you’re unable to move an arm or leg or breathe normally. This includes:
- If a person has a severe injury or allergic reaction.
- If they pass out or experience any signs of a possible stroke or signs of a heart attack.
While you or the victim may have a hospital of choice, an emergency may warrant going to the nearest emergency location for immediate treatment. With their connection to hospitals for seamless admittance and advanced level of technology, ERs are the best place for actual emergencies.
Should you call 911 or go to the hospital emergency room?
The American College of Emergency Physicians (ACEP) has useful guidance on when to call 911, but common reasons include:
- The condition is life-threatening and requires attention as soon as possible.
- You are unable to move yourself or the victim without causing harm or further damage.
- You are physically or emotionally unable to drive or be transported to a hospital ER.
Urgent Aid for Lower-Level Emergencies
If you’re in the Southland, UChicago Medicine Ingalls Memorial offers an additional option to consider before heading to the ER. In our south suburban urgent aid centers , physicians provide ER-level care for lower-level emergencies — injuries, viruses and other illnesses — 24 hours a day, every day in an urgent care-like setting.
If a stable patient needs higher-level imaging such as an ultrasound or CT scan, urgent aids may be a better fit than an urgent care clinic.
The cost of an urgent aid visit is the same as the emergency department of Ingalls Memorial for the same level of care. The co-pay for emergency services will apply to your urgent aid visit, which may be higher than the co-pay for services provided by urgent care centers that are not part of a hospital’s emergency department.
Anwar Isabell, MD, is a UChicago Medicine Medical Group provider. UChicago Medicine Medical Group is comprised of UCM Care Network Medical Group, Inc. and Primary Healthcare Associates, S.C. UChicago Medicine Medical Group providers are not employees or agents of The University of Chicago Medical Center, The University of Chicago, or UChicago Medicine Ingalls Memorial.
Anwar Isabell, MD
Board-certified family medicine physician, Anwar Isabell, MD, specializes in care for the whole family.

Daniel Bickley, MD
Daniel Bickley, MD is the Interim Medical Director of the Adult Emergency Department at the University of Chicago Medicine.
Where Should I Go for Care Today?
You never know when a sudden injury or illness may happen. That's why it's so important to be prepared and know what steps you can take as soon as symptoms appear. Click below to learn more about the best times to visit primary care, urgent care or the emergency department.
When should I contact my primary care doctor?
Your regular doctor is the best person to call for minor health issues because they know your medical history.
When should I go to urgent care?
When you need care right away, but the illness or injury isn’t considered life-threatening, visit an urgent care clinic.
When should I seek emergency care?
If you have severe symptoms that could be life-threatening, call 911 or go to the emergency room right away.
Urgent and emergency care services
Services the NHS provides if you need urgent or emergency medical help.
- When to use NHS 111 online or call 111
- When to call 999
- When to go to A&E
- When to visit urgent treatment centres or other urgent care services
- Find urgent and emergency care services
- Skip to main content
- Keyboard shortcuts for audio player
Medical Treatments
Pharma reps have visited doctors for decades. what impact does it have on patients.
Sydney Lupkin
A economic research study shows that oncologists' prescribing habits change after they've been visited by pharmaceutical sales reps — and it also shows the changes do not extend patients' lives.
Copyright © 2024 NPR. All rights reserved. Visit our website terms of use and permissions pages at www.npr.org for further information.
NPR transcripts are created on a rush deadline by an NPR contractor. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of NPR’s programming is the audio record.
- Share full article
Advertisement
Supported by
Heat-Related E.R. Visits Rose in 2023, C.D.C. Study Finds

By Noah Weiland
Reporting from Washington
The rate of emergency room visits caused by heat illness increased significantly last year in large swaths of the country compared with the previous five years, according to a study published on Thursday by the Centers for Disease Control and Prevention.
The research, which analyzed visits during the warmer months of the year, offers new insight into the medical consequences of the record-breaking heat recorded across the country in 2023 as sweltering temperatures stretched late into the year.

What the Numbers Say: People in the South were especially affected by serious heat illness.
The researchers used data on emergency room visits from an electronic surveillance program used by states and the federal government to detect the spread of diseases. They compiled the number of heat-related emergency room visits in different regions of the country and compared them to data from the previous five years.
Nearly 120,000 heat-related emergency room visits were recorded in the surveillance program last year, with more than 90 percent of them occurring between May and September, the researchers found.
The highest rate of visits occurred in a region encompassing Arkansas, Louisiana, New Mexico, Oklahoma and Texas. Overall, the study also found that men and people between the ages of 18 and 64 had higher rates of visits.
How It Happens: Heat can be a silent killer, experts and health providers say.
Last year was the warmest on Earth in a century and a half, with the hottest summer on record . Climate scientists have attributed the trend in part to greenhouse gas emissions and their effects on global warming, and they have warned that the timing of a shift in tropical weather patterns last year could foreshadow an even hotter 2024.
Heat illness often occurs gradually over the course of hours, and it can cause major damage to the body’s organs . Early symptoms of heat illness can include fatigue, dehydration, nausea, headache, increased heart rate and muscle spasms.
People do not typically think of themselves as at high risk of succumbing to heat or at greater risk than they once were, causing them to underestimate how a heat wave could lead them to the emergency room, said Kristie L. Ebi, a professor at the University of Washington who is an expert on the health risks of extreme heat.
“The heat you were asked to manage 10 years ago is not the heat you’re being asked to manage today,” she said. One of the first symptoms of heat illness can be confusion, she added, making it harder for someone to respond without help from others.
What Happens Next: States and hospitals are gearing up for another summer of extreme heat.
Dr. Srikanth Paladugu, an epidemiologist at the New Mexico Department of Health, said the state had nearly 450 heat-related emergency room visits in July last year alone and over 900 between April and September, more than double the number recorded during that stretch in 2019.
In preparation for this year’s warmer months, state officials are working to coordinate cooling shelters and areas where people can be splashed by water, Dr. Paladugu said.
Dr. Aneesh Narang, an emergency medicine physician at Banner-University Medical Center in Phoenix, said he often saw roughly half a dozen heat stroke cases a day last summer, including patients with body temperatures of 106 or 107 degrees. Heat illness patients require enormous resources, he added, including ice packs, fans, misters and cooling blankets.
“There’s so much that has to happen in the first few minutes to give that patient a chance for survival,” he said.
Dr. Narang said hospital employees had already begun evaluating protocols and working to ensure that there are enough supplies to contend with the expected number of heat illness patients this year.
“Every year now we’re doing this earlier and earlier,” he said. “We know that the chances are it’s going to be the same or worse.”
Noah Weiland writes about health care for The Times. More about Noah Weiland
Explore Our Weather Coverage
Extreme Weather Maps: Track the possibility of extreme weather in the places that are important to you .
Tornado Alerts: A tornado warning demands instant action. Here’s what to do if one comes your way .
Climate Change: What’s causing global warming? How can we fix it? Our F.A.Q. tackles your climate questions big and small .
Evacuating Pets: When disaster strikes, household pets’ lives are among the most vulnerable. You can avoid the worst by planning ahead .
Why Idaho's hospitals are having pregnant patients airlifted out of state
Since January, Dr. Stacy Seyb, a maternal-fetal medicine specialist in Boise, Idaho, has had at least four of his patients wheeled onto emergency flights and airlifted out of the state while experiencing severe pregnancy complications.
One of them was a woman whose water broke around 20 weeks into her pregnancy, putting her at risk of infection. In these types of emergencies , ending the patient’s pregnancy can be part of the standard of care. But doctors at the hospital where Seyb works say they have been forced to transfer patients who have these complications out of state to comply with the state’s abortion ban.
“This has become the new normal, which is sad,” he said.
Idaho bans all abortions, with criminal penalties of up to five years in prison for anyone who performs one or assists. The law includes limited exceptions for rape, incest and to save the life of a mother, but there is no exception to protect her health.
After oral arguments Wednesday, the Supreme Court is now considering whether Idaho’s abortion ban violates a federal law that requires hospitals to offer emergency care to patients in crisis. Thus far, the justices seem split on that question, with some of the more conservative justices appearing to lean toward the state of Idaho, which has argued that federal law should not supersede its own laws on health care.
St. Luke’s Health System, which includes the hospital where Seyb works, filed an amicus brief in the case, noting that an abortion may be critical to protect a patient from nonfatal harms like loss of organs, permanent disability, severe pain or loss of fertility. It also said the ban forces patients to endure potentially risky out-of-state transfers.
Since Jan. 5, when the Supreme Court lifted an injunction that had shielded doctors providing emergency care, six pregnant patients at St. Luke’s have had to be airlifted out of Idaho, according to Dr. Jim Souza, the chief physician executive for St. Luke’s. Last year, the system saw only one such transfer, he said.
In a news conference after Wednesday's arguments, Idaho Attorney General Raúl Labrador, a Republican, questioned accounts of doctors’ transferring patients. “It’s really hard for me to conceive of a single instance where a woman has to be airlifted out of Idaho to perform an abortion,” he said.
“Our law is very clear,” he said. “It protects doctors, it protects women, it protects unborn children, and it ensures that the doctors can use a subjective standard if they believe that the life of the mother is in jeopardy.”
Out-of-state medical transfers can delay needed care and carry immense financial and emotional costs for pregnant patients, who may wind up far from home during some of the most difficult moments of their lives. The cost of the flights can exceed $10,000, and the transportation may also be considered out-of-network by insurance, increasing the share patients must shoulder themselves.

One of the most common complications is when a patient’s water breaks in the first two trimesters of pregnancy, according to Souza. Last year, the hospital system had 54 such cases, most occurring before fetal viability.
Physicians for Human Rights, an organization that has advocated for abortion rights, also filed an amicus brief in the Supreme Court case. It cites a March report for which the group interviewed several doctors who practice or practiced in Idaho, along with doctors based in neighboring states who received patients who were transferred.
Dr. Sarena Hayer, a physician in Oregon, described receiving a patient from Idaho who was gravely ill when she arrived by air. The patient was 18 weeks pregnant with twins when she suffered a severe pregnancy complication. The patient also had a history of kidney issues and had previously received a transplant.
Doctors at her Idaho hospital determined that one of her fetuses had died and her lab results were troubling. She told her doctors she “wanted them to do whatever they had to, including termination,” according to the report. But she was ultimately airlifted to Oregon. The following morning, she lost her other fetus too.
If the woman had started her care in Oregon, she would have been offered a termination almost immediately, Hayer said.
“What other medical condition can we think of that would require a patient who’s sick to get transported to another state for a legal reason?” Hayer told NBC News. “It just really feels unjust.”
“In a way, you’re torturing the women because you’re not providing the definitive care until you can say they’re at the brink of death,” Dr. Michele Heisler, the medical director for Physicians for Human Rights, said in an interview. “I think that’s the stake here.”
Doctors in Idaho also described situations in which patients with severe pregnancy complications were unable to leave the state to seek treatment.
Dr. Michael Schneider, a maternal-fetal medicine specialist in Boise, recalled a patient whose water broke around 20 weeks but declined to be airlifted out of state, in part because she could not leave her family. Expenses were another concern. The woman left the hospital, he said, then returned once she experienced contractions. She went into labor, but her fetus did not survive.
Over his decades in medicine, Schneider has learned that vulnerabilities for pregnant women are acute. On his first night of a residency at a hospital in Memphis, Tennessee, a patient with sepsis died.
“That’s what keeps me up — that somebody’s going to be placed in harm’s way, or a transport is going to go bad and there’s going to be a significant injury to the mother,” he said. “It doesn’t get any worse than losing two.”
Bracey Harris is a national reporter for NBC News, based in Jackson, Mississippi.
Differences in emergency department visits and hospitalization between German and Dutch nursing home residents: a cross-national survey
- Research Paper
- Open access
- Published: 29 April 2024
Cite this article
You have full access to this open access article

- Alexander M. Fassmer ORCID: orcid.org/0000-0001-9456-2546 1 ,
- Sytse U. Zuidema 2 ,
- Sarah I. M. Janus 2 &
- Falk Hoffmann 1
Key summary points
What is the difference in the frequency of transfers to hospital between German and Dutch nursing home residents?
In German nursing homes, residents are transported to hospital more often than in the Netherlands (e.g., at least one emergency department visit during last year: 26.5% vs. 7.9%, p < 0.0001). General practitioners in Germany are less involved in the transfer decision than elder care physicians in the Netherlands.
The differences are probably mainly due to differences in the health and care systems (e.g., very strong gatekeeper function of the general practitioner/elder care physician in the Netherlands).
Assessing and comparing German and Dutch nursing home perspectives on residents’ hospital transfers.
Cross-sectional study among German and Dutch nursing homes. Two surveys were conducted in May 2022, each among 600 randomly selected nursing homes in Germany and the Netherlands. The questionnaires were identical for both countries. The responses were compared between the German and Dutch participants.
We received 199 German (response: 33.2%) and 102 Dutch questionnaires (response: 17.0%). German nursing homes estimated the proportion of transfers to hospital during 1 year to be higher than in Dutch facilities (emergency department visits: 26.5% vs. 7.9%, p < 0.0001; hospital admissions: 29.5% vs. 10.5%, p < 0.0001). In German nursing homes, the proportion of transfers to hospital where the decision was made by the referring physician was lower than in the Dutch facilities (58.8% vs. 88.8%, p < 0.0001). More German nursing homes agreed that nursing home residents are transferred to the hospital too frequently (24.5% vs. 10.8%, p = 0.0069). German nursing homes were much more likely than Dutch facilities to believe that there was no alternative to transfer to a hospital when a nursing home resident had a fall (66.3% vs. 12.8%, p < 0.0001).
German nursing home residents are transferred to hospital more frequently than Dutch residents. This can probably be explained by differences in the care provided in the facilities. Future studies should, therefore, look more closely at these two systems and examine the extent to which more intensive outpatient care can avoid transfers to hospital.
Avoid common mistakes on your manuscript.
Introduction
In Europe, there were approximately 3.4 million long-term care beds in nursing homes in 2020 [ 1 ]. Demographic changes and the aging population will require a large increase in the number of nursing home residents in almost every country [ 2 ]. Due to increased frailty and vulnerability [ 3 , 4 ], nursing home residents have a higher need for medical care [ 5 ]. This may also be reflected in a higher risk of (acute) transfers to hospital [ 6 , 7 ]. Many of these transfers are deemed potentially avoidable [ 8 , 9 ].
Hospital transfer numbers can vary significantly between different countries [ 10 , 11 ] and major differences were found not only worldwide, but even between neighboring countries. A recent systematic review examined how hospitalizations from nursing homes differ between Germany and the Netherlands [ 12 ]. Both in the first 6 months of nursing home residency and in the last 6 months of life, the proportion of nursing home residents in Germany who were hospitalized was higher than in the Netherlands (e.g., last 30 days: Germany 48.6% to 58.0% vs. Netherlands 8.0% to 15.7%).
However, these differences need to be interpreted in the context of how healthcare and primary care are organized for residents in the two neighboring countries. In Germany, long-term care is financed by long-term social care insurance. In 2021, 793,000 residents lived in German nursing homes [ 13 , 14 ]. The residents receive medical care from general practitioners (GPs) who make home visits to the facilities. Further medical care can be provided by other specialists in private practice (e.g., ophthalmologists, urologists), but in most cases, they must be visited by the residents in their practices. Long-term care in the Netherlands is financed by a general income tax. In 2020, there were 115,000 residents living in Dutch nursing homes [ 15 ]. Medical care differs according to the type of nursing home. In “Verpleeghuizen” (type 1 nursing homes, majority of facilities), specially trained elder care physicians (ECPs) are employed directly by the providers. In the Netherlands, elder care medicine is a distinct discipline specializing in the long-term care of frail older people [ 16 ]. In “Verzorgingshuizen” (type 2 nursing homes, small-scale living facilities, many of which face closure following reform in 2015 [ 17 ]), GPs in private practice are responsible for providing medical care. In general, specialist treatment is not provided in the outpatient setting in the Netherlands [ 18 ].
These variations in the organization of care between German and Dutch nursing homes might result in differing care processes between both countries. However, the aforementioned systematic review provided only an indirect comparison between the two countries containing studies with different methods and study years [ 12 ]. Furthermore, it cannot explain the reasons for those large differences. In summary, more in-depth information around hospital transfers from nursing homes from Germany and the Netherlands is missing.
Therefore, the present cross-national study investigates the frequency of hospital transfers among German and Dutch nursing home residents, on the one hand, and compares underlying care processes, such as the involvement of GPs or ECP in transfer decisions, on the other hand.
Study design and population
This study is part of a larger public health project investigating how differences in the organization of healthcare between Germany and the Netherlands affect patient outcomes and health professionals (“Comparison of healthcare structures, processes and outcomes in the Northern German and Dutch cross-border region I (CHARE-GD I)”). The interdisciplinary project consists of four sub-projects, one of which focuses on medical care in nursing homes.
Nursing homes in Germany and the Netherlands were surveyed in a cross-sectional study. As the German source population, we identified all 11,409 nursing homes listed in the Care Navigator provided by the Federal Association of Local Health Insurance Funds ("AOK Pflege-Navigator", as of January 2022). For the Netherlands, a list of all existing 1810 nursing home locations (as of February 2022) was compiled manually. We used the Caremap of the Netherlands (“Zorgkaart Nederland”), an initiative of the Dutch patient federation (patiëntenfederatie Nederland). As Zorgkaart Nederland does not differentiate between type 1 and type 2 facilities, both types were included in the list. In both Germany and the Netherlands, a simple random sample of 600 nursing homes per country was selected and surveyed by mail in May 2022 (see Fig. 1 ). The survey was preferably addressed to the nursing staff management/head of nursing if the name was available by a manual search. If the name of the facility administration/nursing home director or the executive board was known, this was used instead. Only if no contact person could be found, the questionnaire was addressed to the current nursing staff management/head of nursing (without personal salutation). Nursing homes could participate either in paper form (with stamped envelopes) or online via a web link or QR code (SoSci Survey). Further information on the methodological procedure can be found elsewhere [ 19 ].
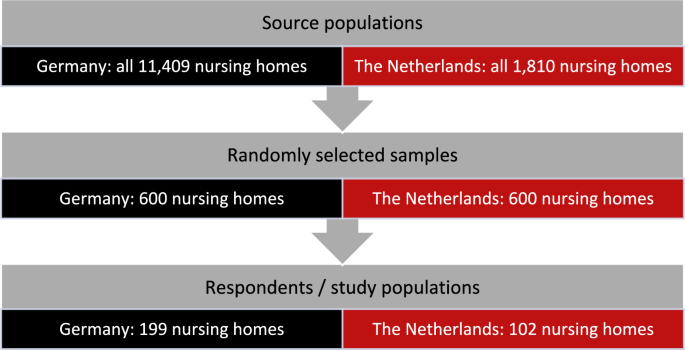
Flow chart of the study populations
Participation in this study was completely voluntary; data were collected anonymously. For both surveys, we obtained waivers from the Medical Ethics Committee of the [Carl von Ossietzky University of Oldenburg in Germany] (2022–012) and from the Medical Ethics Review Board of the [University Medical Center Groningen in the Netherlands] (2022/035).
Content of the questionnaire
The pre-tested questionnaire included questions about medical care in nursing homes, use of emergency departments and hospitalization, and end-of-life care. For this study, we first asked participants to estimate the proportion of residents from their facility who had at least one emergency department visit and hospital admission during last year, respectively. Second, the proportion of hospital transfers (emergency department visits and hospital admissions) from the facility where the decision was made by the GP/ECP was estimated. Respondents were also asked to indicate what proportion of residents who were hospitalized did the GP/ECP see within the first week of discharge (4 options: 0–25%, 26–50%, 51–75%, 76–100%). Third, we asked whether (a) nursing home residents were too frequently transferred to the hospital, (b) there was often no alternative to hospital transfer after a nursing home resident falls, and (c) telemedicine consultations could be helpful for medical care in nursing homes. The participants had to answer these questions on a 5-point Likert scale ranging from ‘0 = totally disagree’ to ‘4 = totally agree’. Fourth, the nursing homes were asked if they used (a) a fixed emergency protocol in case of an acute deterioration in a resident's condition and (b) a fixed transfer protocol to ambulance/hospital. They also had to state if they actually used telemedicine support for the care of their residents (yes or no answer category in all three cases).
Furthermore, we asked participants for the following characteristics: their age, sex, number of care places in the nursing home, location of the facility (rural ≤20,000; semi-urban between >20,000 and ≤100,000; urban >100,000 inhabitants), distance from the nearest hospital with emergency department (in kilometers [km]), and number of years working in the current position in the nursing home (nursing staff management/head of nursing, facility administration/nursing home director, executive board, other), respectively.
Statistical analyses
Analyses were performed using descriptive statistics. Continuous data are presented as means, standard deviation (SD), median and interquartile range (IQR). For categorical data, frequencies were calculated. For rating on the 5-point Likert scale, the proportions for the categories ‘totally disagree’ and ‘disagree’ as well as ‘totally agree’ and ‘agree’ are presented in summarized form. All assessed proportions were compared between German and Dutch participants by Mann–Whitney U test. Categorical variables were compared using Chi-square tests ( χ 2 -Test). Since not all participants answered every question in the questionnaire, the analyses were restricted to subjects with no missing values given in the respective questions. Statistical analysis was performed with SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Nursing home characteristics
199 German nursing homes responded to the questionnaire (response: 33.2%). The average age of the respondents was 48.1 years, and most were female (79.4%). The mean distance to the nearest hospital with an emergency department was 8.7 km.
From the Netherlands, we received 102 questionnaires (response: 17.0%). The Dutch participants were slightly younger than the German ones (mean age: 44.8 years) and the proportion of females was higher (85.9%). The nearest hospital with an emergency department was on average 10.4 km away. More information on participants from both countries is displayed in Table 1 .
Emergency department visits and hospital admissions
When there is an acute deterioration in a resident's condition, 47.5% of German nursing homes and 64.7% of Dutch nursing homes use a fixed emergency protocol ( p = 0.0052). On the other hand, almost all German nursing homes (98.5%) reported using a fixed transfer protocol to the ambulance service or hospital; in the Netherlands, this was 61.0% ( p < 0.0001). The proportion of nursing homes using telemedicine support for the care of their residents was lower in Germany than in the Netherlands (15.7% vs. 26.3%, p = 0.0287, see Table 2 ).
While the German participants estimated that on average 26.5% of residents had at least one emergency department visit in the past year, the Dutch indicated 7.9% in this respect ( p < 0.0001). A similar picture was observed for hospital admissions (Germany: 29.5% vs. Netherlands: 10.5%, p < 0.0001). In German nursing homes, the proportion of hospital transfers (emergency department visits and hospital admissions) where the decision was made by the GP/ECP was lower than in the Dutch facilities (58.8% vs. 88.8%, p < 0.0001). Similarly, in Germany, the proportion of residents discharged from the hospital who were seen by their GP within the first week was lower. In the German nursing homes, 35.2% of respondents stated that in 76–100% of hospital discharges, the GP sees the affected resident within the first week; in the Netherlands this was 70.3% ( p < 0.0001, see Table 2 ).
While 24.5% of respondents in Germany agreed that nursing home residents were transferred to the hospital too frequently, the agreement in the Netherlands was 10.8%. On the other hand, the proportion of disagreement was higher in the Netherlands (62.8% vs. 46.4%, p = 0.0069). Two thirds (66.3%) of German nursing homes saw no alternative to a hospital transfer after a resident’s fall. In the Netherlands, only 12.8% of respondents shared this opinion ( p < 0.0001). Nursing homes from both countries had similar views on the potential benefits of telemedicine for the medical care of nursing home residents, with slightly higher agreement in the Netherlands than in Germany (53.9% vs. 44.2%, p = 0.1285, see Fig. 2 ).
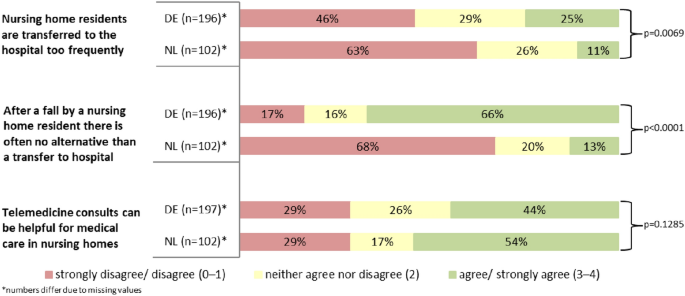
Responses to statements regarding emergency department visits and hospital admissions of nursing home residents—comparison between Germany (DE) and the Netherlands (NL)
This cross-national study showed that German nursing home residents are transferred to hospital more often than Dutch residents. Furthermore, in Germany, the transfer decisions are less often made by the physician, and more German nursing homes feel that their residents are taken to hospital too often.
The central finding of this study, that German nursing home residents are transferred to hospital more frequently, is also consistent with the results of the aforementioned systematic review [ 12 ]. Although the proportion of German nursing home residents with hospital transfers in the last 12 months is considerably higher than in the Netherlands, it is lower than in another German study in which data were collected between 2014 and 2015 [ 20 ]. Our data collection took place 2 years after the introduction of infection control measures against the COVID-19 pandemic in nursing homes [ 21 ], which may explain the lower transfer figures for Germany. The figures we found for the Netherlands are also lower than in previous Dutch studies looking at hospitalizations of nursing home residents in the last months of life, with proportions between 15.2% [ 22 ] and 27.6% [ 23 ]. However, in both studies, the proportion of type 2 nursing homes was considerably higher than it is today in the Netherlands, which may have influenced the transfer figures. In general, hospitalizations of nursing home residents are particularly common shortly after moving to the nursing home and again at the end of life. The systematic review found higher figures for Germany compared with the Netherlands for both periods, especially at the end of residents’ lives [ 12 ]. In addition to structural differences, cultural differences may also play a role in explaining these variations between the two countries. There is more discussion about quality of life versus life-sustaining treatment in the Netherlands than in Germany and refusal of potentially distressing life-sustaining treatments is more common in Dutch nursing homes [ 24 ].
However, one of the main reasons for these differences in hospital transfers is assumed to be residents’ medical care. In Dutch type 1 nursing homes (verpleeghuizen), on the one hand, there is round-the-clock care by the directly employed ECPs and, on the other hand, all types of Dutch nursing home are regularly supported by a multiprofessional team of allied health professionals (e.g., psychologists). From the same data collection on which this study is based, we know that in German nursing homes permanently employed allied health professionals are rare [ 19 ]. This outpatient multidisciplinary care delivered in Dutch nursing homes is probably more expensive than nursing home care in Germany. However, by avoiding hospital transports [ 25 ], in the Netherlands, costs could be lower overall. Besides, we know that the GP/ECP contact frequencies are comparable with Germany [ 19 ]. Therefore, we suspect that the delivery of physician care differs in the two countries. A previous study from Germany showed that GPs are often not involved in hospital transfer decisions in nursing homes, e.g., because they cannot be reached by the facilities [ 26 ]. Meanwhile, it is known that better GP accessibility can help nursing home residents receive appropriate care earlier and thus avoid hospital transfers [ 8 ]. The present study was also able to show less frequent involvement of the physician in Germany. In the Netherlands, GPs/ECPs were involved in most hospital transfer decisions. Therefore, they may have seen other alternatives to hospitalization in case of a resident’s fall, where the majority of German nursing homes would send the resident directly to hospital.
Given that the existing literature identifies a significant proportion of hospital transfers from nursing homes as potentially avoidable [ 8 , 27 ], a low number of transfers can also be seen as an indicator of good quality and well-coordinated care [ 28 ]. One indication of better coordination of care on the Dutch side could be the higher proportion of nursing homes in our study that have a fixed emergency protocol in the event of a deterioration in the condition of their residents. Although German nursing homes were more likely to have a handover protocol for the emergency services, other studies have reported that valuable information is often missing in these documents [ 29 ]. Overall, better communication, documentation, and decision support tools allow treatment without hospitalization [ 8 ]. This survey showed that Dutch nursing homes more often see a benefit in telemedical support and actually use it more often in the care of their residents. In the entire Dutch healthcare system, e-health solutions seem to play a more important role than in Germany [ 30 , 31 ]. These solutions also have the potential to avoid hospitalizations of nursing home residents and reduce care costs [ 32 ].
Limitations and strengths
Some results of this study, such as the proportions of nursing home residents with at least one hospital transfer in the past year, must be interpreted with a certain degree of caution because they are based on nursing home staff estimates. Respondents were asked to estimate data for their entire facility, but it is unclear whether participants also looked in residents’ records and how they estimated. It is possible that respondents only have current cases in mind when answering such questions, which may result in difficulties when making more general statements. Furthermore, it is possible that the nursing staff management (our preferred recipient) were not the people with the best overview in every nursing home to adequately answer our questions. However, the present study is the first to collect data on emergency department use and hospitalization of nursing home residents using the same methodology in the two neighboring countries of Germany and the Netherlands. As the primary aim of the study was to compare the frequency of hospital transfers and care processes on a nursing home level, the appropriateness of individual transfers was not assessed. Another limitation concerns the generalizability of the results. The number of cases may have been too small for some comparisons, mainly because of a lower response from the Netherlands. However, this was difficult to predict in advance. Responses from Germany and even more so from the Netherlands were not particularly high, but we previously took various measures for a higher response (including a short questionnaire, follow-up contact, among others [ 33 ]). We received responses from all German federal states as well as from all Dutch provinces. Nevertheless, a selection bias cannot be excluded in both countries. In the Netherlands, we surveyed both nursing home types (verpleeghuizen and verzorgingshuizen). While these are organized differently, we were not able to find too many differences between them in our previous article [ 19 ].
Conclusions and implications
This study was the first to compare the frequencies of emergency department visits and hospitalization between German and Dutch nursing homes using the same methodology. German nursing home residents are more likely to be hospitalized and often GPs are not involved in transfer decisions. These results are probably mainly due to the different arrangements of general and medical care in nursing homes and the immediate availability of multiprofessional teams, which simplify the direct care of residents in the Netherlands compared with Germany. Better coordination of medical care for residents is probably the best starting point for reducing unnecessary hospital transfers. Therefore, future studies should shed more light on how many hospital transfers can be avoided through this kind of outpatient care in the nursing home and whether costs can be saved overall despite comprehensive care in the facility. In order to better understand the care processes in nursing homes, the perspectives of the professionals involved (in particular nurses and GPs/ECPs) should be compared.
Availability of data and materials
The dataset generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Eurostat Statistics explained. Healthcare resource statistics—beds—Statistics Explained 2022. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Healthcare_resource_statistics_-_beds&oldid=314834#Long-term_care_beds_in_nursing_and_residential_care_facilities . Accessed 28 Apr 2023
Cushman & Wakefield France (2019) European Nursing Homes Report. Overview of the European Nursing Homes Market
Hoffmann F, Boeschen D, Dörks M, Herget-Rosenthal S, Petersen J, Schmiemann G (2016) Renal insufficiency and medication in nursing home residents—a cross-sectional study (IMREN). Dtsch Arztebl Int 113:92–98. https://doi.org/10.3238/arztebl.2016.0092
Article PubMed PubMed Central Google Scholar
Gordon AL, Franklin M, Bradshaw L, Logan P, Elliott R, Gladman JRF (2014) Health status of UK care home residents: a cohort study. Age Ageing 43:97–103. https://doi.org/10.1093/ageing/aft077
Article PubMed Google Scholar
Schröder A-K, Fassmer AM, Allers K, Hoffmann F (2020) Needs and availability of medical specialists’ and allied health professionals’ visits in German nursing homes: a cross-sectional study of nursing home staff. BMC Health Serv Res. https://doi.org/10.1186/s12913-020-05169-7
Fassmer AM, Hoffmann F (2020) Acute health care services use among nursing home residents in Germany: a comparative analysis of out-of-hours medical care, emergency department visits and acute hospital admissions. Aging Clin Exp Res 32:1359–1368. https://doi.org/10.1007/s40520-019-01306-3
Hoffmann F, Allers K (2017) Variations over time in the effects of age and sex on hospitalization rates before and after admission to a nursing home: a German cohort study. Maturitas 102:50–55. https://doi.org/10.1016/j.maturitas.2017.04.017
Lemoyne SE, Herbots HH, De Blick D, Remmen R, Monsieurs KG, Van Bogaert P (2019) Appropriateness of transferring nursing home residents to emergency departments: a systematic review. BMC Geriatr 19:17. https://doi.org/10.1186/s12877-019-1028-z
Lamb G, Tappen R, Diaz S, Herndon L, Ouslander JG (2011) Avoidability of hospital transfers of nursing home residents: perspectives of frontline staff. J Am Geriatr Soc 59:1665–1672. https://doi.org/10.1111/j.1532-5415.2011.03556.x
Brucksch A, Hoffmann F, Allers K (2018) Age and sex differences in emergency department visits of nursing home residents: a systematic review. BMC Geriatr 18:151. https://doi.org/10.1186/s12877-018-0848-6
Hoffmann F, Allers K (2016) Age and sex differences in hospitalisation of nursing home residents: a systematic review. BMJ Open 6:e011912. https://doi.org/10.1136/bmjopen-2016-011912
Fassmer AM, Allers K, Helbach J, Zuidema S, Freitag M, Zieschang T et al (2023) Hospitalization of German and Dutch nursing home residents depend on different long-term care structures: a systematic review on periods of increased vulnerability. J Am Med Dir Assoc. https://doi.org/10.1016/J.JAMDA.2023.01.030
Statistisches Bundesamt DESTATIS (Federal Statistical Office) (2022) Pflegebedürftige nach Versorgungsart, Geschlecht und Pflegegrade—Statistisches Bundesamt. https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Pflege/Tabellen/pflegebeduerftige-pflegestufe.html . Accessed 14 Dec 2023
Statistisches Bundesamt DESTATIS (Federal Statistical Office) (2022) Pflegeheime und ambulante Pflegedienste. https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Pflege/Tabellen/pflegeeinrichtungen-deutschland.html . Accessed 22 Feb 2024
Centraal Bureau voor de Statistiek (2020) 115 duizend mensen in verzorgings- of verpleeghuis. https://www.cbs.nl/nl-nl/achtergrond/2020/13/115-duizend-mensen-in-verzorgings-of-verpleeghuis . Accessed 27 Nov 2023
Koopmans RTCM, Lavrijsen JCM, Hoek JF, Went PBM, Schols JMGA (2010) Dutch elderly care physician: a new generation of nursing home physician specialists. J Am Geriatr Soc 58:1807–1809. https://doi.org/10.1111/j.1532-5415.2010.03043.x
Alders P, Schut FT (2019) The 2015 long-term care reform in the Netherlands: getting the financial incentives right? Health Policy (N Y) 123:312–6. https://doi.org/10.1016/j.healthpol.2018.10.010
Article Google Scholar
European Observatory on Health Systems and Policies, van Ginneken E, Kroneman M (2015) Long-term care reform in the Netherlands: too large to handle? Eurohealth (Lond) 21:47–50
Google Scholar
Fassmer AM, Zuidema SU, Janus SIM, Hoffmann F (2024) Comparison of medical care needs and actual care in German and Dutch nursing home residents: a cross-sectional study conducted in neighboring European countries. Arch Gerontol Geriatr 117:105178. https://doi.org/10.1016/j.archger.2023.105178
Hoffmann F, Schmiemann G (2017) Influence of age and sex on hospitalization of nursing home residents: a cross-sectional study from Germany. BMC Health Serv Res 17:55. https://doi.org/10.1186/s12913-017-2008-7
Said D, Sin MA, Zanuzdana A, Schweickert B, Eckmanns T (2023) Alten- und Pflegeheime—die COVID-19-Pandemie als Mahnung: Infektionshygienische Maßnahmen und Einflussfaktoren auf die Gesundheit der Bewohnenden. Bundesgesundheitsblatt Gesundheitsforsch Gesundheitsschutz 66:248–255. https://doi.org/10.1007/s00103-023-03657-9
Moore DC, Payne S, Keegan T, Vandenblock L, Deliens L, Gambassi G et al (2020) Length of stay in long-term care facilities: a comparison of residents in six European countries. Results of the PACE cross-sectional study. BMJ Open 10:e033881. https://doi.org/10.1136/bmjopen-2019-033881
Penders YWH, Van Den Block L, Deliens L, Donker GA, Onwuteaka-Philipsen B (2015) Comparison of end-of-life care for older people living at home and in residential homes: a mortality follow-back study among GPS in the Netherlands. Br J Gen Pract 65:e724–e730. https://doi.org/10.3399/bjgp15X687349
Hendriks SA, Smalbrugge M, Deliens L, Koopmans RTCM, Onwuteaka-Philipsen BD, Hertogh CMPM et al (2017) End-of-life treatment decisions in nursing home residents dying with dementia in the Netherlands. Int J Geriatr Psychiatry 32:e43–e49. https://doi.org/10.1002/gps.4650
Koopmans RTCM, Lavrijsen JCM, Zuidema SU (2010) The physician’s role in nursing homes: the Dutch solution. Arch Intern Med 170:1406–1407. https://doi.org/10.1001/archinternmed.2010.278
Pulst A, Fassmer AM, Schmiemann G (2020) Unplanned hospital transfers from nursing homes: who is involved in the transfer decision? Results from the HOMERN study. Aging Clin Exp Res. https://doi.org/10.1007/s40520-020-01751-5
Rolland Y, Mathieu C, Tavassoli N, Berard E, Laffon de Mazières C, Hermabessière S et al (2021) factors associated with potentially inappropriate transfer to the emergency department among nursing home residents. J Am Med Dir Assoc 22:2579-2586.e7. https://doi.org/10.1016/j.jamda.2021.04.002
Ouslander JG, Perloe M, Givens JH, Kluge L, Rutland T, Lamb G (2009) Reducing potentially avoidable hospitalizations of nursing home residents: results of a pilot quality improvement project. J Am Med Dir Assoc 10:644–652. https://doi.org/10.1016/j.jamda.2009.07.001
Pulst A, Fassmer AM, Hoffmann F, Schmiemann G (2020) Vom Pflegeheim ins Krankenhaus—Erfahrungen und potenzielle Maßnahmen zur Reduktion der Transporte aus Sicht von Rettungskräften. Notfall + Rettungsmedizin 23:575–7. https://doi.org/10.1007/s10049-020-00800-w
Leontjevas R, Knippenberg IAH, Bakker C, Koopmans RTCM, Gerritsen DL (2021) Telehealth and telecommunication in nursing homes during COVID-19 antiepidemic measures in the Netherlands. Int Psychogeriatrics 33:835–836. https://doi.org/10.1017/S1041610221000685
Feldmann KE, Müller L (2021) Niederlande: Digitalisierung im Gesundheitswesen - BMWi-Markterschließungsprogramm für KMU. Hrsg: Deutsch-Niederländische Handelskammer. https://www.gtaiexportguide.de/resource/blob/767608/6bbef8517f01c51e9349df5f330ca272/ZMA_%20Niederlande_Digitalisierung%20im%20Gesundheitswesen%20final.pdf
Valk-Draad MP, Bohnet-Joschko S (2022) Nursing home-sensitive hospitalizations and the relevance of telemedicine: a scoping review. Int J Environ Res Public Health 19:12944. https://doi.org/10.3390/IJERPH191912944
Edwards PJ, Roberts I, Clarke MJ, Diguiseppi C, Wentz R, Kwan I et al (2009) Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev 5:9. https://doi.org/10.1002/14651858.MR000008.pub4
Download references
Acknowledgements
We gratefully acknowledge the support and cooperation within the CHARE-GD study group. This study was conducted in partnership with the Cross-Border Institute of Healthcare Systems and Prevention (CBI), Groningen/Oldenburg. We thank Max Snijders for his assistance in sending the Dutch study materials.
Open Access funding enabled and organized by Projekt DEAL. The project on which this article is based was funded by the Ministry of Science and Culture of Lower Saxony (MWK) as part of the Niedersächsisches ‘Vorab’ Program (Grant Agreement No. ZN3730). The funder had no influence on the content of the study (study protocol, study design, data collection, interpretation and publication).
Author information
Authors and affiliations.
Division of Outpatient Care and Pharmacoepidemiology, Department of Health Services Research, School VI - School of Medicine and Health Sciences, Carl von Ossietzky Universität Oldenburg, Oldenburg, Lower Saxony, Germany
Alexander M. Fassmer & Falk Hoffmann
Department of Primary and Long-Term Care, University of Groningen, University Medical Center Groningen, Groningen, The Netherlands
Sytse U. Zuidema & Sarah I. M. Janus
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Alexander M. Fassmer .
Ethics declarations
Conflict of interest.
None to declare.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. The study was approved by the “Medical Ethics Committee of the Carl von Ossietzky University of Oldenburg”, Germany (No. 2022-012) and from the “Medical Ethics Review Board of the University Medical Center Groningen”, the Netherlands (2022/035). Since data in both surveys were collected anonymously both ethics committees also waived the requirement for informed consent.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Fassmer, A.M., Zuidema, S.U., Janus, S.I.M. et al. Differences in emergency department visits and hospitalization between German and Dutch nursing home residents: a cross-national survey. Eur Geriatr Med (2024). https://doi.org/10.1007/s41999-024-00975-2
Download citation
Received : 25 December 2023
Accepted : 01 April 2024
Published : 29 April 2024
DOI : https://doi.org/10.1007/s41999-024-00975-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nursing home residents
- Hospitalization
- Emergency department visits
- The Netherlands
- Find a journal
- Publish with us
- Track your research
How did Milwaukee ER doctor Amy Hummel do on 'Jeopardy!' Wednesday night?

Dr. Amy Hummel, a Milwaukee ER doctor, can now add "Jeopardy!" champion to her already-impressive title.
Hummel answered 21 total clues correctly on Wednesday night's episode and won $18,900. She'll be the returning champion for Thursday's show.
Here's a look at the many questions Hummel got right, what we learned about her, and how Final "Jeopardy!" shook out. Plus, how to tune in:
What we learned about Dr. Amy Hummel during the show
"Johnny Gilbert introduced you as hailing from Milwaukee, Wisconsin, but I understand you haven't always lived there," host Ken Jennings said to Hummel.
Hummel has lived in four states in the last 10 years, "mostly for school," she shared.
"I thought it was going to be like witness protection program or something," Jennings joked.
"Amazon gets confused 'cause I have about 20 addresses in there," she said.
Hummel attended St. Olaf College for undergrad and the University of Cincinnati College of Medicine for medical school, according to her University of Wisconsin Emergency Medicine profile .
She did her residency at the University of Wisconsin Hospitals and Clinics, and was part of the Class of 2023.
In June 2023, University of Wisconsin EM Residency tweeted that Hummel was heading to Milwaukee to work as a community emergency physician.
"Amy is excited to explore a new city and work at several different sites that each serve very distinct populations," the tweet said.
Who Dr. Amy Hummel competed against on April 24's episode of 'Jeopardy!'
Returning champion and Philadelphia professor Mark Lashley and Paul Drake, a front desk lead from Grand Blanc, Michigan.
What Dr. Amy Hummel answered correctly during the 'Jeopardy!' Round
Clue: "He called his memoir 'A Very Punchable Face,' and he's been punched in numerous sketches on 'Saturday Night Live."
Hummel: "Who is Colin Jost?"
Clue: "This Chinese exercise with flowing, rhythmic movements has forms such as parting the wild horse's mane and playing the lute."
Hummel: "What is tai chi?"
Clue: "There's a silent 'P' at the beginning of this word that comes from the Greek for 'pertaining to air' and is used of tires."
Hummel: "What is Pneumatic?"
Clue: "Finally free to tell her story. She speaks candidly about her conservatorship and Justin Timberlake in 'The Woman in Me.'"
Hummel: "Who is Britney Spears?"
Clue: "One of the final rites for pilgrims to this holy city is to throw stones at the three walls of Mina."
Hummel: "What is Mecca?"
Clue: "In Shinto households, it is common to have communion with Kami (or gods) by drinking this after a major festival."
Hummel: "What is sake?"
Clue: "In January 2024 the U.S. began striking targets of this rebel group in Yemen who were attacking Red Sea shipping."
Hummel: "Who are the Houthis?"
Clue: "The 1847 storming of Chapultepec Castle near Mexico City inspired these first five words of the Marine Corps' famous him."
Hummel: "What are From the Halls of Montezuma."
Clue: "1960s space heroes Neil Armstrong and John Glenn ('The Mig-Mad Marine') had both been combat flyers in this war."
Hummel: "What is Korea?"
Clue: "Hebrew for 'Daughter of Commandment,' this rite celebrates the transition of 12-year-old Jewish girls into adulthood."
Hummel: "What is a bat mitzvah?"
What Dr. Amy Hummel answered incorrectly during the 'Jeopardy!' Round
These were the standings at the end of the 'jeopardy' round.
- Hummel: $6,000
- Drake: $5,800
- Lashley: $4,600
What Dr. Amy Hummel answered correctly during the Double 'Jeopardy!' Round
Clue: "In 2014 this rapper released "Fancy" alongside Charli XCX and took inspiration from 'Clueless' for the song's music video."
Hummel: "Who is Iggy Azalea?"
Clue: "His satirical 1729 essay "A Modest Proposal" suggested poverty in Ireland could be lessened by killing and eating the children of the poor."
Hummel: "Who is Swift?"
Clue: "Death is stronger than I am," this British woman wrote in 'The Death of the Moth,' published the year after she took her own life."
Hummel: "Who is Virginia Woolf?"
Clue: "The city's rep as the 'Salsa Capital' has many people going (going) back (back) to Cali (Cali) in this country."
Hummel: "What is Columbia?"
Clue: "From 1612 to 1614 this cretan-born artist painted the 'Adoration of the Shepherds' for his own burial chapel."
Hummel: "Who is El Greco?"
Clue: "Uganda's Murchison Falls on the Victoria branch, the upper most part of this river is about 200 miles north of Kampala."
Hummel: "What is the Nile?"
Clue: "He went solo from his brothers for his 2014 hit 'Jealous.'"
Hummel: "Who is Nick Jonas?"
Clue: "Acre, Amazonas and Mato Grosso Do Sul are states in this nation."
Hummel: "What are Brazil?"
Clue: "In a landmark essay, Ta-Nehisi Coates argued 'the case for' these payments to descendants of slaves."
Hummel: "What are reparations?"
Clue: "Before his Rose Period, Picasso went through a period named for this color."
Hummel: "What is blue?"
What Dr. Amy Hummel answered incorrectly during the Double 'Jeopardy!' Round
When Hummel chose the category "Near the equator" for $800 during the Double "Jeopardy!" Round, she hit the "Daily Double." She wagered $4,000 of her $16,000.
The clue Jennings read: "The largest living monitor lizard shares its name with this island in the middle of the Indonesian Archipelago."
Hummel ran out of time to answer. The answer was a Komodo dragon, Jennings revealed.
Also during Double "Jeopardy!," one of the clues was: "The Mond Crucifixion by this angelic Italian Renaissance artist was painted around 1502 when he was only 19."
Hummel answered: "Who is Bocelli ... Botticelli?" That was incorrect. Drake guessed Gabriel, which was also wrong.
The correct answer was Raphael, Jennings said.
These were the standings at the end of the Double 'Jeopardy!' Round
- Hummel: $13,200
- Drake: $9,400
- Lashley: $8,600
What happened in Final 'Jeopardy!'
The Final "Jeopardy!" clue was: "Decorated with an illustration of the Montgolfiers' craft, the smoking room aboard this could be accessed only via an airlock."
All three contestants gave the correct answer of "What is the Hindenburg?" Hummel had initially started writing a different answer, but she crossed it out and wrote the right one in time.
Lashley had wagered $801, bringing his total for the day to $9,401.
Drake wagered $7,801, which took him to $17,201.
Wagering $5,700, Hummel came out on top with a total of $18,900.
How to watch Dr. Amy Hummel on 'Jeopardy!'
Hummel will be the returning champion on Thursday's episode of "Jeopardy!" The episode will air on WDJT CBS58 Milwaukee at 6 p.m. CT.
Hummel will be competing against Tyler Jarvis, a Portales, New Mexico, researcher and Ph.D. student, and Justin Brandt, a West Hills, California, attorney, according to the show's website .

IMAGES
VIDEO
COMMENTS
We accept Medicare, many insurance plans, and self-pay. To find out more about our services: Call Toll-free: (855) 232-0644. E-mail us at. [email protected]. Primary Care. Psychiatry. Wound Care. Pain Management.
We employ the same experienced professionals you would see in an urgent care, emergency room or hospital. Depending on your individual needs, your DispatchHealth team may include an emergency medicine or internal medicine physician, physician assistant, nurse practitioner, nurse, medical technician, and/or imaging technician.
House calls and video visits in 37 states. Landmark partners with health plans to bring medical, behavioral health, and palliative care, along with social services, to patients in communities across the U.S. Our mobile providers visit patients in their homes through in-person house calls and telemedicine visits over video and phone.
Las Vegas urgent medical care. DispatchHealth arrives fully equipped to test and treat everything an urgent care can, at the same cost as an urgent care visit. Proudly providing same-day medical care to adults and children throughout Las Vegas. Open 365 days a year. Only a few appointments left today!
To learn more about our services in the Washington, D.C., region, call us today at 202-877-0570. The MedStar Health MedStar House Call Program - MedStar Total Elder Care is nationally recognized and offers house calls by doctors, nurse practitioners and provides diagnostic tests and treatments. Learn more about our program.
Look out for your health. A UnitedHealthcare® HouseCalls visit is a no-cost, yearly health check-in that can make a big difference. Call 1-866-799-5895, TTY 711, to schedule your visit.
Our house call medical teams are comprised of an emergency-medicine-trained physician assistant or nurse practitioner, with in-person support from a medical technician, as well as an emergency department doctor available to provide remote support at all times. Learn more about how DispatchHealth house calls work. On-demand health care 7 days a week
Some of these patients might otherwise need to be in the hospital, emergency department, doctor's office, or a rehabilitation facility. ... Home health care for eligible patients who need support between medical visits; The Mount Sinai at Home programs exemplify Mount Sinai's commitment to cutting-edge and patient-focused medicine by ...
MD at Home is Chicago's premier leader in providing housecall doctors and housecall physicians for homebound patients. Call: (312) 243-2223 Referral Fax: (312) 243-8450 Clinical Fax: (312) 243-2227
The on-demand house call company Heal promises to get a healthcare provider to your home within a few hours between 8 a.m. to 8 p.m. seven days a week. While Heal's doctors can't test for ...
If you prefer a remote consultation, you can learn more and schedule your virtual appointment by visiting our Virtual Consultations Page. We're here to provide healthcare in the way that suits you best. Concierge MD provides on-demand house calls for primary and urgent care needs in the comfort of your home, hotel or office.
Vituity has an experienced panel of physicians that has been serving patients virtually since 2016. An On Duty® virtual visit is an easy and safe way to see a Vituity emergency room doctor to assess your potential COVID-19 symptoms or other urgent issues. Our On Duty doctors can provide confidential diagnoses, treatment plans, and ...
During the first home visit, the doctor or nurse practitioner will perform a medical exam and develop an individual care plan. Doctors and nurse practitioners provide routine and preventive care as needed. Our clinical call center nurses and on-call providers are available by phone 24/7 for emergency and urgent care needs.
House call doctor visits benefit older adults and caregivers. Getting your older adult to the doctor's office for an appointment can be difficult or sometimes impossible. Whether they're frail, can't walk on their own, or have Alzheimer'sor dementia, getting out of the house is hard on both of you.
Scheduling your appointment. Please call or email to request an appointment. Appointments are scheduled 1-2 weeks in advance according to when a doctor will be seeing patients in your area. We will call you to confirm a one to two hour appointment window for the doctor's arrival at your home.
Urgent care centers are usually cheaper. The authors of the 2021 study state that the average cost of treatment at an urgent care center is $156, while the same treatment may cost $570 or more at ...
5 min read. Hospital emergency rooms (or departments) deal with sudden illnesses and injuries. They maintain preparedness for every kind of health emergency, including vehicular accidents, heart ...
3. Emergency stations opened 24 hours a day, can be visited in a case of a non-life-threatening injury. It is often hard to find English-speaking staff in state facilities, except the largest city hospitals, so you will need a Russian-speaking interpreter to accompany your visit to a free doctor or hospital.
Emergency doctor home visits, also known as house calls, entail a licensed medical professional coming to a patient's residence to provide healthcare services. These services are not limited to minor ailments but encompass a wide range of medical needs, including urgent care, general consultations, and even specialized treatment.
The cost of an urgent aid visit is the same as the emergency department of Ingalls Memorial for the same level of care. The co-pay for emergency services will apply to your urgent aid visit, which may be higher than the co-pay for services provided by urgent care centers that are not part of a hospital's emergency department.
Services the NHS provides if you need urgent or emergency medical help. Find urgent and emergency care services When to use NHS 111 online or call 111
SberHealth | 236 followers on LinkedIn. 24/7 online consultations with over 2k doctors: therapist, pediatrician, gynecologist, dermatologist, and more. | SberHealth is an online platform that ...
Regardless of your health insurance status, you can receive initial medical care for free in emergency situations. Here are some useful numbers in case of emergency: Medical emergency number: 03; Moscow emergency medical care: 628 0003; Find a list of emergency phone numbers in Russia for all types of accidents and emergencies.
That is, doctors prescribe about 5% more oncology drugs following a visit from a pharmaceutical representative. That's according to a new study published by the National Bureau of Economic ...
Dr. Aneesh Narang, an emergency medicine physician at Banner-University Medical Center in Phoenix, said he often saw roughly half a dozen heat stroke cases a day last summer, including patients ...
Her miraculous birth brought brief hope to her surviving family. "You are my soul, my heart," Sabreen's grandmother told her, the day after she was born. "You are my beloved one."
Since Jan. 5, when the Supreme Court lifted an injunction that had shielded doctors providing emergency care, six pregnant patients at St. Luke's have had to be airlifted out of Idaho, according ...
Unless you have a medical emergency, you will usually need an appointment for treatment. If your doctor has referred you, they may make an appointment for you. Otherwise, you can make an appointment by phone or visiting the hospital. Some hospitals in Russia, especially some international medical centers, allow you to book appointments online.
Purpose Assessing and comparing German and Dutch nursing home perspectives on residents' hospital transfers. Methods Cross-sectional study among German and Dutch nursing homes. Two surveys were conducted in May 2022, each among 600 randomly selected nursing homes in Germany and the Netherlands. The questionnaires were identical for both countries. The responses were compared between the ...
Dr. Amy Hummel, a Milwaukee ER doctor, can now add "Jeopardy!" champion to her already-impressive title. Hummel answered 21 total clues correctly on Wednesday night's episode and won $18,900.