- Patient Care & Health Information
- Tests & Procedures
- Feminizing hormone therapy
Feminizing hormone therapy typically is used by transgender women and nonbinary people to produce physical changes in the body that are caused by female hormones during puberty. Those changes are called secondary sex characteristics. This hormone therapy helps better align the body with a person's gender identity. Feminizing hormone therapy also is called gender-affirming hormone therapy.
Feminizing hormone therapy involves taking medicine to block the action of the hormone testosterone. It also includes taking the hormone estrogen. Estrogen lowers the amount of testosterone the body makes. It also triggers the development of feminine secondary sex characteristics. Feminizing hormone therapy can be done alone or along with feminizing surgery.
Not everybody chooses to have feminizing hormone therapy. It can affect fertility and sexual function, and it might lead to health problems. Talk with your health care provider about the risks and benefits for you.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Feminizing hormone therapy is used to change the body's hormone levels. Those hormone changes trigger physical changes that help better align the body with a person's gender identity.
In some cases, people seeking feminizing hormone therapy experience discomfort or distress because their gender identity differs from their sex assigned at birth or from their sex-related physical characteristics. This condition is called gender dysphoria.
Feminizing hormone therapy can:
- Improve psychological and social well-being.
- Ease psychological and emotional distress related to gender.
- Improve satisfaction with sex.
- Improve quality of life.
Your health care provider might advise against feminizing hormone therapy if you:
- Have a hormone-sensitive cancer, such as prostate cancer.
- Have problems with blood clots, such as when a blood clot forms in a deep vein, a condition called deep vein thrombosis, or a there's a blockage in one of the pulmonary arteries of the lungs, called a pulmonary embolism.
- Have significant medical conditions that haven't been addressed.
- Have behavioral health conditions that haven't been addressed.
- Have a condition that limits your ability to give your informed consent.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Stay Informed with LGBTQ+ health content.
Receive trusted health information and answers to your questions about sexual orientation, gender identity, transition, self-expression, and LGBTQ+ health topics. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing to our LGBTQ+ newsletter.
You will receive the first newsletter in your inbox shortly. This will include exclusive health content about the LGBTQ+ community from Mayo Clinic.
If you don't receive our email within 5 minutes, check your SPAM folder, then contact us at [email protected] .
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Research has found that feminizing hormone therapy can be safe and effective when delivered by a health care provider with expertise in transgender care. Talk to your health care provider about questions or concerns you have regarding the changes that will happen in your body as a result of feminizing hormone therapy.
Complications can include:
- Blood clots in a deep vein or in the lungs
- Heart problems
- High levels of triglycerides, a type of fat, in the blood
- High levels of potassium in the blood
- High levels of the hormone prolactin in the blood
- Nipple discharge
- Weight gain
- Infertility
- High blood pressure
- Type 2 diabetes
Evidence suggests that people who take feminizing hormone therapy may have an increased risk of breast cancer when compared to cisgender men — men whose gender identity aligns with societal norms related to their sex assigned at birth. But the risk is not greater than that of cisgender women.
To minimize risk, the goal for people taking feminizing hormone therapy is to keep hormone levels in the range that's typical for cisgender women.
Feminizing hormone therapy might limit your fertility. If possible, it's best to make decisions about fertility before starting treatment. The risk of permanent infertility increases with long-term use of hormones. That is particularly true for those who start hormone therapy before puberty begins. Even after stopping hormone therapy, your testicles might not recover enough to ensure conception without infertility treatment.
If you want to have biological children, talk to your health care provider about freezing your sperm before you start feminizing hormone therapy. That procedure is called sperm cryopreservation.
How you prepare
Before you start feminizing hormone therapy, your health care provider assesses your health. This helps address any medical conditions that might affect your treatment. The evaluation may include:
- A review of your personal and family medical history.
- A physical exam.
- A review of your vaccinations.
- Screening tests for some conditions and diseases.
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections.
- Discussion about sperm freezing and fertility.
You also might have a behavioral health evaluation by a provider with expertise in transgender health. The evaluation may assess:
- Gender identity.
- Gender dysphoria.
- Mental health concerns.
- Sexual health concerns.
- The impact of gender identity at work, at school, at home and in social settings.
- Risky behaviors, such as substance use or use of unapproved silicone injections, hormone therapy or supplements.
- Support from family, friends and caregivers.
- Your goals and expectations of treatment.
- Care planning and follow-up care.
People younger than age 18, along with a parent or guardian, should see a medical care provider and a behavioral health provider with expertise in pediatric transgender health to discuss the risks and benefits of hormone therapy and gender transitioning in that age group.
What you can expect
You should start feminizing hormone therapy only after you've had a discussion of the risks and benefits as well as treatment alternatives with a health care provider who has expertise in transgender care. Make sure you understand what will happen and get answers to any questions you may have before you begin hormone therapy.
Feminizing hormone therapy typically begins by taking the medicine spironolactone (Aldactone). It blocks male sex hormone receptors — also called androgen receptors. This lowers the amount of testosterone the body makes.
About 4 to 8 weeks after you start taking spironolactone, you begin taking estrogen. This also lowers the amount of testosterone the body makes. And it triggers physical changes in the body that are caused by female hormones during puberty.
Estrogen can be taken several ways. They include a pill and a shot. There also are several forms of estrogen that are applied to the skin, including a cream, gel, spray and patch.
It is best not to take estrogen as a pill if you have a personal or family history of blood clots in a deep vein or in the lungs, a condition called venous thrombosis.
Another choice for feminizing hormone therapy is to take gonadotropin-releasing hormone (Gn-RH) analogs. They lower the amount of testosterone your body makes and might allow you to take lower doses of estrogen without the use of spironolactone. The disadvantage is that Gn-RH analogs usually are more expensive.
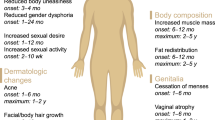
After you begin feminizing hormone therapy, you'll notice the following changes in your body over time:
- Fewer erections and a decrease in ejaculation. This will begin 1 to 3 months after treatment starts. The full effect will happen within 3 to 6 months.
- Less interest in sex. This also is called decreased libido. It will begin 1 to 3 months after you start treatment. You'll see the full effect within 1 to 2 years.
- Slower scalp hair loss. This will begin 1 to 3 months after treatment begins. The full effect will happen within 1 to 2 years.
- Breast development. This begins 3 to 6 months after treatment starts. The full effect happens within 2 to 3 years.
- Softer, less oily skin. This will begin 3 to 6 months after treatment starts. That's also when the full effect will happen.
- Smaller testicles. This also is called testicular atrophy. It begins 3 to 6 months after the start of treatment. You'll see the full effect within 2 to 3 years.
- Less muscle mass. This will begin 3 to 6 months after treatment starts. You'll see the full effect within 1 to 2 years.
- More body fat. This will begin 3 to 6 months after treatment starts. The full effect will happen within 2 to 5 years.
- Less facial and body hair growth. This will begin 6 to 12 months after treatment starts. The full effect happens within three years.
Some of the physical changes caused by feminizing hormone therapy can be reversed if you stop taking it. Others, such as breast development, cannot be reversed.
While on feminizing hormone therapy, you meet regularly with your health care provider to:
- Keep track of your physical changes.
- Monitor your hormone levels. Over time, your hormone dose may need to change to ensure you are taking the lowest dose necessary to get the physical effects that you want.
- Have blood tests to check for changes in your cholesterol, blood sugar, blood count, liver enzymes and electrolytes that could be caused by hormone therapy.
- Monitor your behavioral health.
You also need routine preventive care. Depending on your situation, this may include:
- Breast cancer screening. This should be done according to breast cancer screening recommendations for cisgender women your age.
- Prostate cancer screening. This should be done according to prostate cancer screening recommendations for cisgender men your age.
- Monitoring bone health. You should have bone density assessment according to the recommendations for cisgender women your age. You may need to take calcium and vitamin D supplements for bone health.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing hormone therapy care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/contents/search. Accessed Oct. 10, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Oct. 10, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming hormone therapy (adult). Mayo Clinic; 2022.
- Nippoldt TB (expert opinion). Mayo Clinic. Sept. 29, 2022.
- Gender dysphoria
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Gender-Affirming Hormone Therapy?
- How to Get Started
- Masculinizing Therapy
- Feminizing Therapy
- What to Expect
- Access to Treatment
Gender-affirming hormone therapy helps transgender and other gender-nonconforming people align their bodies with their gender identity . Not all transgender (trans) people are interested in hormone therapy. However, many transgender people, particularly binary transgender people, turn to hormones to affirm their gender.
Gender-affirming hormone therapy is comprised of masculizing hormone therapy used in trans men and feminizing hormone therapy used in trans women.
This article describes the goals of gender-affirming hormone therapy, how the treatment is administered, and the different types of hormones used. It also explains what to expect when undergoing gender-affirming hormone therapy and the possible risks.
Verywell / Brianna Gilmartin
Definitions
The term "gender affirmation" is preferred over "gender confirmation" because a transgender person does not need to confirm their gender to anyone. The word "confirm" suggests proof, while "affirm" means to assert strongly.
Who Is Gender-Affirming Hormone Therapy For?
Gender-affirming hormone therapy is the primary medical treatment sought by transgender people. It allows their secondary sex characteristics to be more aligned with their individual gender identity.
Gender-affirming hormone therapy comes in two types:
- Masculinizing hormone therapy used to develop typically male sex characteristics
- Feminizing hormone therapy used to develop typically female sex characteristics
Hormone therapy can be used on its own for people who have no interest in pursuing gender-affirming surgery . It can also be used in advance of surgery (usually for six months to one year) to improve the outcomes of surgery, such as breast augmentation.
According to the National Transgender Discrimination Survey, 95% of transgender people and 49% of non-binary people were interested in hormone therapy.
Hormone Therapy vs. Puberty Blockers
Puberty blockers are used to delay the onset of puberty in young, gender-diverse people prior to the start of hormone therapy. They are considered to be a distinct but complementary component of gender-affirmation therapy.
How to Get Started
Gender affirmation is a process in which hormones only play a part. It typically starts with social gender affirmation in which you alter your appearance, wardrobe, and manner of grooming while updating your name, pronouns, and legal documentation.
Medical gender affirmation is typically the next step in which you work with a healthcare provider to identify your personal goals and which type of types of treatments are needed to achieve those goals.
Hormone therapy is typically overseen by a specialist in the endocrine (hormonal) system called an endocrinologist . Other healthcare providers trained in gender-affirming medical care may be equally qualified to administer treatment.
Depending on state law and other factors, healthcare providers may be able to dispense treatment on the same day. No letter from a mental health provider may be needed. Call Planned Parenthood or your local LGBTI organization to learn about the laws in your state.
To receive authorization for insurance coverage, many insurers require a diagnosis of gender dysphoria . To do so, a therapist or mental health professional must confirm that there is a mismatch between a person's expressed or experienced gender and the gender they were assigned at birth for a period of at least six months.
How to Choose the Right Provider
Not every endocrinologist is equally well-suited to administer gender-affirming hormone therapy. Those who have undergone a comprehensive, multidisciplinary gender-affirmation training program are generally preferred.
Do not hesitate to ask about a healthcare provider's experience and qualifications in administering gender-affirming care.
Masculinizing Hormone Therapy
Masculinizing hormone therapy uses various types of testosterone to promote masculinizing changes in both binary and non-binary individuals. Testosterone is most often given as an injection, but other formations are available, including pills and creams.
There has been growing interest in the use of subcutaneous pellets for testosterone treatment, as they only need to be inserted two to four times a year. However, they are not always available or covered by insurance.
Changes that can be induced by masculinizing hormone therapy include:
- Facial and body hair growth
- Increased muscle mass
- Lowering of the pitch of the voice
- Increased sex drive
- Growth of the glans clitoris
- Interruption of menstruation
- Vaginal dryness
- Facial and body fat redistribution
- Sweat- and odor-pattern changes
- Hairline recession; possibly male pattern baldness
- Possible changes in emotions or interests
Masculinizing hormone therapy cannot reverse all of the changes associated with female puberty. If transmasculine individuals have experienced breast growth that makes them uncomfortable, they may need to address that with binding or top surgery .
Testosterone will also not significantly increase height unless it is started reasonably early. Finally, testosterone should not be considered an effective form of contraception, even if menses have stopped.
Feminizing Hormone Therapy
Feminizing hormone therapy uses a combination of estrogen and a testosterone blocker. The testosterone blocker is needed because testosterone has stronger effects on the body than estrogen.
The blocker most commonly used in the United States is spironolactone , a medication also used for heart disease. The medication used as a puberty blocker, called Supprelin LA (histerline), can also be used to block testosterone.
Various forms of estrogen can be used for feminizing hormone therapy. In general, injectable or topical forms are preferred as they tend to have fewer side effects than oral estrogens. However, some trans women prefer oral estrogens.
Changes that can be induced by feminizing hormone therapy include:
- Breast growth
- Softening of the skin
- Fat redistribution
- Reduction in face and body hair (but not elimination)
- Reduced hair loss/balding
- Muscle-mass reduction
- Decrease in erectile function
- Testicular size reduction
Estrogen cannot reverse all changes associated with having undergone testosterone-driven puberty. It cannot eliminate facial or body hair or reverse shoulder width, jaw size, vocal pitch, or facial structure. Many of these can be addressed with aesthetic or surgical treatments.
What to Expect During Treatment
Some hormones used for gender-affirming hormone therapy are self-administered or given by someone you know. Others need to be administered by a healthcare provider.
Thereafter, regular follow-ups are needed to evaluate the effects of treatment and possible side effects. Most healthcare providers recommend visiting every 3 months for the first year and every 6 to 12 months thereafter.
Effects of Therapy
It can take three to five years for your body to show the full effects of gender-affirming hormone therapy. Some changes can occur within the first six months, such as the development of larger breasts. Others, like changes in facial structure, can take years.
In addition to physical changes, hormone therapy can cause emotional changes. If you are sexually active, it may improve sexual satisfaction as well as your overall sense of well-being. Hormone therapy can also help to ease the stress associated with gender dysphoria.
If you discontinue therapy, some changes may be reversible. Others like changes in bone structure may be permanent.
Possible Risks
As beneficial as gender-affirming hormone therapy can be, it also carries certain risks depending on which hormone you are taking.
Possible risks of feminizing hormone therapy include:
- High blood pressure
- Blood clots
- Heart disease
- Type 2 diabetes
- Weight gain
- Infertility
- Breast and prostate cancer
Risks of masculinizing hormone therapy:
- Male pattern baldness
- High cholesterol
- Pelvic pain
- Sleep apnea
- Interfertility
Access to Gender-Affirming Hormone Therapy
Until relatively recently, access to gender-affirming hormone therapy was largely managed through gatekeeping models that required gender-diverse people to undergo a psychological assessment before they could access hormone treatment.
However, there has been a growing movement toward the use of an informed consent model to better reflect access to other types of medical care. This change has been reflected in the standards of care for transgender health produced by the World Professional Association of Transgender Health (WPATH).
Gender-affirming hormone therapy is considered to be a medically necessary treatment for gender dysphoria. It should be covered by most insurers in the United States after legal changes that occurred as part of the passage of the Affordable Care Act.
However, state laws vary substantially in terms of transgender protections, and some states do allow policies to exclude various aspects of transgender health care, including gender-affirming hormone therapy.
Access to hormone therapy can be prohibitively expensive for many people if they need to pay out of pocket, which may lead some people to try to get these medications from friends or other unlicensed sources.
In addition, individuals who are involved with carceral systems such as immigrant detention may be denied access to hormones. This can have significant negative physical and psychological effects.
Gender-affirming hormone therapy is the primary form of treatment for transgender people. Masculizing hormone therapy involving testosterone is used to develop secondary male sex characteristics like larger muscles. Feminizing hormone therapy involving estrogen and a testosterone blocker is used to develop secondary female sex characteristics like breasts.
Some masculinizing and feminizing effects can occur within months, while others may take years. If you stop treatment, many of the effects will reverse while some will be permanent. Regular follow-up care is needed to avoid potential side effects and long-term complications.
Gardner I, Safer JD. Progress on the road to better medical care for transgender patients . Curr Opin Endocrinol Diabetes Obesity . 2013 20(6):553-8. doi:10.1097/01.med.0000436188.95351.4d
James SE, Herman JL, Rankin S, Keisling M, Mottet M, Anafi M. The Report of the 2015 U.S. Transgender Survey . Washington, DC: National Center for Transgender Equality. 2016.
Planned Parenthood. Gender-affirming hormone therapy: what to expect on your first visit and beyond .
Boskey ER, Taghinia AH, Ganor O. Association of surgical risk with exogenous hormone use in transgender patients: A systematic review . JAMA Surg . 2019;154(2):159-169. doi:10.1001/jamasurg.2018.4598
Almazan AN, Benson TA, Boskey ER, Ganor O. Associations between transgender exclusion prohibitions and insurance coverage of gender-affirming surgery. LGBT Health . 2020;7(5). doi:10.1089/lgbt.2019.0212
White Hughto JM, Reisner SL. A systematic review of the effects of hormone therapy on psychological functioning and quality of life in transgender individuals . Transgender Health . 2016;1(1),21–31. doi:10.1089/trgh.2015.0008
Cavanaugh T, Hopwood R, Lambert C. Informed consent in the medical care of transgender and gender-nonconforming patients . AMA Journal of Ethics . 2016;18(11),1147–1155. doi:10.1001/journalofethics.2016.18.11.sect1-161
World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People (7th Version) . WPATH. 2011.
By Elizabeth Boskey, PhD Boskey has a doctorate in biophysics and master's degrees in public health and social work, with expertise in transgender and sexual health.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 07 September 2022
Gender affirming hormone therapy dosing behaviors among transgender and nonbinary adults
- Arjee Restar ORCID: orcid.org/0000-0003-2992-8198 1 , 2 , 3 ,
- E. J. Dusic 4 ,
- Henri Garrison-Desany 5 ,
- Elle Lett 3 , 6 ,
- Avery Everhart ORCID: orcid.org/0000-0001-6146-0180 3 , 7 ,
- Kellan E. Baker 5 , 8 ,
- Ayden I. Scheim 9 ,
- S. Wilson Beckham 10 ,
- Sari Reisner 11 ,
- Adam J. Rose 12 ,
- Matthew J. Mimiaga 13 , 14 ,
- Asa Radix 2 , 15 , 16 ,
- Don Operario 17 &
- Jaclyn M. W. Hughto 17 , 18
Humanities and Social Sciences Communications volume 9 , Article number: 304 ( 2022 ) Cite this article
9779 Accesses
6 Citations
11 Altmetric
Metrics details
- Health humanities
- Medical humanities
A Correction to this article was published on 21 October 2022
This article has been updated
Gender-affirming hormones have been shown to improve psychological functioning and quality of life among transgender and nonbinary (trans) people, yet, scant research exists regarding whether and why individuals take more or less hormones than prescribed. Drawing on survey data from 379 trans people who were prescribed hormones, we utilized multivariable logistic regression models to identify factors associated with hormone-dosing behaviors and content analysis to examine the reasons for dose modifications. Overall, 24% of trans individuals took more hormones than prescribed and 57% took less. Taking more hormones than prescribed was significantly associated with having the same provider for primary and gender-affirming care and gender-based discrimination. Income and insurance coverage barriers were significantly associated with taking less hormones than prescribed. Differences by gender identity were also observed. Addressing barriers to hormone access and cost could help to ensure safe hormone-dosing behaviors and the achievement trans people’s gender-affirmation goals.
Similar content being viewed by others

A systematic review of psychosocial functioning changes after gender-affirming hormone therapy among transgender people
David Matthew Doyle, Tom O. G. Lewis & Manuela Barreto
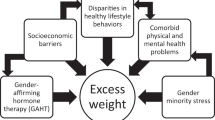
Filling a gap in care: addressing obesity in transgender and gender diverse patients
John Michael Taormina & Sean J. Iwamoto
Current use of testosterone therapy in LGBTQ populations
A. N. Tijerina, A. V. Srivastava, … E. C. Osterberg
Introduction
Access to gender-affirming hormones is crucial to many transgender and nonbinary (trans) individuals’ mental health and well-being. While not all trans individuals will seek out hormones, access to and use of hormones can be life-changing among those who do, particularly those with gender dysphoria. Individuals with gender dysphoria experience distress related to differences between their sex assigned at birth and gender identity (Ashley, 2021 ) and may experience episodes of distress, ruminative thinking, anxiety, and depression (Bouman et al., 2017 ; Chodzen et al., 2019 ; Klemmer et al., 2021 ; Silva et al., 2021 ). As gender-affirming hormones are highly effective in developing secondary sex characteristics and are less costly and more accessible than gender-affirming surgeries, hormones are most often the first or only form of gender-affirming care trans patients will seek out (Restar et al., 2019 ; White Hughto & Reisner, 2016 ). Notably, hormone use has been shown to significantly improve psychological functioning and quality of life, reduce suicidal attempts and ideations, promote body satisfaction, and decrease gender dysphoria and is therefore considered medically necessary for many trans people (Bouman et al., 2017 ; Foster Skewis et al., 2021 ; Herman et al., 2019 ; Klemmer et al., 2021 ; White Hughto & Reisner, 2016 ).
Notably, there are several major barriers to accessing hormones and other forms of gender-affirming care, including systemic issues such as lack of insurance coverage, lack of availability of competent providers who prescribe hormones, and interpersonal-level experiences of bias and discrimination (James et al., 2021 ; Lerner et al., 2021 ; Puckett et al., 2018 ; Sperber et al., 2005 ). Many studies also find that trans people experience financial barriers to accessing hormones due in part to the fact that trans people are less likely than cisgender people to have health insurance (Lerner et al., 2021 ) and many insurance plans do not cover the cost of gender-affirming medical interventions (James et al., 2021 ; Lerner et al., 2021 ), despite the fact that gender-affirming care is a cost-effective intervention (Baker, 2017 ). Discrimination and mistreatment in clinical encounters also present barriers to accessing hormones, such as providers asking invasive questions, refusing care, verbally harassing or using abusive language, and physically abusing trans patients (Hoffkling et al., 2017 ; Lerner et al., 2021 ; Redfern & Sinclair, 2014 ; Sperber et al., 2005 ). Even when providers do not explicitly discriminate or mistreat their trans patients, they often decline or refuse to provide adequate care for this population due to transphobia, lack of clinical and cultural competency, or both (Hughto et al., 2015 ; Lerner et al., 2021 ). Lack of education on how to care for and interact with trans patients creates negative interactions between patients and providers, which can lead to future avoidance of care and medical mistrust on the part of trans people (Hughto et al., 2015 ; Johnson et al., 2020 ; Lerner et al., 2021 ).
The use of gender-affirming hormones in a manner that is inconsistent with prescribed dosages can have adverse clinical and health consequences (Webb et al., 2020 ). Research on general medication adherence has shown that many factors influence an individual’s decision and ability to follow a prescribed treatment plan. Indeed, economic barriers, convenience, and poor communication with prescribing physicians have been shown to influence whether an individual will take medication as prescribed (Ratanawongsa et al., 2013 ; Sabaté & Sabaté, 2003 ; Zolnierek & DiMatteo, 2009 ). However, to our research team’s knowledge, there are currently no studies that detail why some individuals do not take hormones as prescribed. To fill this gap, the primary objective of this exploratory study is to identify the sociodemographic, healthcare indicators, and discrimination experiences associated with taking more or less hormones than prescribed, as well as trans people’s reasons for modifying their prescribed dose.
Study sample and procedures
This is a secondary cross-sectional analysis of survey data from Project VOICE (Voicing Our Individual and Community Experiences), a needs assessment led by the Fenway Institute at Fenway Health (Fenway) and the Massachusetts Transgender Political Coalition (MTPC). Between March and August 2019, trans residents of Massachusetts (MA) and Rhode Island (RI) were surveyed about their sociodemographics, healthcare experiences, and health. Respondents were purposively sampled and recruited via venues where trans people congregate, including online sites such as listservs and community-based social networking webpages, as well as in-person sites such as trans-specific community events and trans-friendly clinics. Participants were eligible for the study if they were 18 years or older, self-identified as transgender or nonbinary, resided in MA or RI, were willing to provide electronic written informed consent, and spoke either English or Spanish. Eligible respondents who completed the survey were invited to opt into a community raffle for one of 54 gift cards, with values ranging from $10 to $250. Additional details on the study procedures can be found elsewhere (Restar et al., 2020 ).
The present analysis focuses on a subsample of 379 trans respondents who indicated that they were currently taking hormones as part of their gender-affirmation care. This secondary analysis aimed to identify characteristics of trans respondents who reported taking more hormones than prescribed and respondents who reported taking less hormones than prescribed and to descriptively detail reasons for these modifying their hormone-dosing behaviors.
Sociodemographic
Respondent’s age was assessed in years and recoded as young adult (age 18–29) vs. all others (age 30+). Race/ethnicity was asked as a check-all-that-apply question and combined into White (non-Hispanic) vs. People of Color (POC, including Asian/Pacific Islander, Black, Hispanic/Latino, another race, and multiple races/ethnicities). Following the best-practice two-step method to assess gender (Reisner et al., 2016 ), we combined two items on assigned sex at birth (female, male) and current gender identity to denote respondents who are transfeminine, transmasculine, or nonbinary (e.g., genderqueer, gender non-conforming). Respondents were then asked if they were currently employed for wages or not. Lastly, low income was recoded if personal income fell below $30,000 (vs. not).
Healthcare experiences and discrimination
A series of questions about health insurance, routine care, and gender-affirming care were asked. First, health insurance coverage for hormones was recoded to “yes” if it was covered, vs. “no” if it was not covered or the patient had no insurance. Respondents were then asked if they go to the same provider for both primary and gender-affirming care, with response options as either “yes, I go to the same provider for both types of care” or “no, I see a different provider for each type of care.” Respondents were asked in years when they received routine care last, and responses were dichotomized as “yes” if care was received within the past year vs. “no.” Similarly, mental health treatment within the past year was dichotomized as yes/no.
A series of questions about past year routine care avoidance were asked. Respondents indicated “yes” if, within the past year, they have postponed or did not try to get check-ups or other preventative medical care because of (a) gender-based mistreatment, (b) not being able to afford care, or (c) a doctor or other provider refused to treat them.
To assess major gender-based discrimination experiences, respondents were asked whether, in the past year, they had experienced the following because of their gender identity: (a) discouraged by a teacher or advisor from seeking higher education, (b) denied a scholarship, (c) not hired for a job (d) not given a promotion, (e) fired, (f) prevented from renting or buying a home in the neighborhood you wanted, (g) prevented from remaining in a neighborhood because neighbors made life so uncomfortable, (h) hassled by the police, (i) denied a bank loan, (j) provided inferior service by a store/restaurant employee, plumber, mechanic, or service provider, (k) denied medical care. Responses were coded as “1” if yes or “0” if no and were summed to create a continuous score of major gender-based discrimination experiences (range: 0–11).
Hormone therapy dosing behaviors (outcome)
Hormone-dosing behaviors were assessed via two questions that asked respondents [1] how often they take more hormones than prescribed; and [2] how often they take less hormones than prescribed. The questionnaire provided the following definition: “taking what is prescribed means taking the right dose at the time as instructed by a healthcare provider.” Response options for both questions ranged from never to always and were recoded as yes (rarely, sometimes, most of the time, always) vs. no (never).
In a check-all-that-apply question design, respondents who reported taking more or less hormones than prescribed were asked to provide detailed information about why they took their hormones other than as prescribed. For those who indicated that they were taking more hormones than prescribed, potential reasons included the following: (a) I think that taking more hormones will speed up my transition/gender-affirmation process, (b) my friends suggested I should take more, (c) I don’t trust my doctor/healthcare provider’s advice, (d) I do not think my doctor/healthcare provider is giving me the right dose, (e) My hormones make me feel good, or (f) Other, please specify. Similarly, for those who indicated that they were taking less hormones than prescribed, potential reasons included the following: (a) I cannot afford it, (b) I have no health insurance, (c) I forget to take it, (d) I forget to pick up my prescription, (c) I get it through friends, online, or on the street, and it’s not always available, (d) I do not trust my doctor/healthcare provider’s advice, (e) I do not think my doctor/healthcare provider is giving me the right dose, (f) It is hard for me to get to my doctor’s appointment to get the prescription, (g) My doctor/healthcare provider said I didn’t need to take it, (f) I am afraid my hormones will not work well with the other medications I take, (g) I am worried about gaining weight, (h) My hormones make me feel sick, (i) I am not sure I want to take hormones anymore, (j) Other, please specify. Response options to these questions were based on feedback from community partners and medical providers as key informants involved in the survey design.
Data analysis
Univariate descriptive statistics [mean, standard deviation (SD), frequency, and proportions] were performed to examine the overall distribution of the final analytical sample, overall ( n = 379) and stratified by the two hormone-dosing questions. We also used bivariate analyses to examine patterns of hormone-dosing behaviors based on respondents’ sociodemographic characteristics, healthcare experiences, and discrimination.
Next, we performed a multivariable analysis using logistic regression to assess relationships between the independent variables (i.e., sociodemographic, healthcare experiences, and discrimination) and our main outcome (i.e., took more hormones than prescribed, took less hormones than prescribed. We then constructed two separate multivariable regression models, one for each outcome. Given the exploratory nature of this study, prior to building our models, we utilized a lasso procedure to select key variables to include in the model (Tibshirani, 1996 ). Given our modest sample size, we used nonparametric bootstrapping with 1000 iterations to estimate confidence intervals and reduce Type 1 error per model (Parra‐Frutos, 2014 ). The significance level was set to p < 0.05 a priori. We used Stata-MP version 17.0 to perform all statistical analyses.
Finally, we calculated the frequency of each reason for taking more or less hormones. We then utilized content analysis to examine the write-in responses under the category “other” (Kohlbacher, 2006 ). Each emergent theme was descriptively analyzed and included in the final list of reasons.
All enrolled respondents provided their electronic, written informed consent, which detailed the voluntary nature of their participation and their rights to confidentiality and privacy. All study activities were approved by the Fenway Institutional Review Board (IRB).
Sample characteristics
Sample characteristics are shown in Table 1 . About half of the respondents were young adults under the age of 30 (51%). The majority of respondents were White non-Hispanic (82%). A third of participants (33%) were transfeminine, 44% transmasculine, and 23% nonbinary. More than half of the sample was employed for wages (70%), and more than half reported having a low income (53%).
The majority of the sample reported having health insurance that covers hormones (85%), having the same provider for primary and gender-affirming care (74%), and receiving routine care in the past year (83%). A third received mental health treatment in the past year (37%). A total of 19% reported avoiding routine care in the past year due to gender-based mistreatment, and 26% avoided care due to cost. A total of 6% reported experiencing having a provider who refused them treatment in the past year. The mean number of major gender-based discrimination experiences in the past year was 1.7 out of a possible 11 (standard deviation [SD] = 1.9).
Overall, 24% of the sample reported taking more hormones than prescribed, and 57% reported taking less hormones than prescribed at some point in their lives. Less than one-fifth (19%) did not report modifying their hormone dosage. Among those who took more hormones than prescribed ( n = 90), 44.4% were transfeminine, 33.3% were transmasculine, and 22.2% were nonbinary respondents. Among those who took less hormones than prescribed ( n = 215), 27% were transfeminine, 46% were transmasculine, and 27% were nonbinary respondents.
Regression outcome: taking more hormones than prescribed
Table 2 shows the adjusted multivariable logistic regression models examining factors associated with taking more hormones than prescribed. In the final model, the odds of taking more hormones were lower among respondents who identified as transmasculine compared to transfeminine (adjusted OR [aOR]=0.45, 95% confidence interval [95% CI] = 0.23–0.88) and among low-income respondents (aOR = 0.41, 95% CI = 0.20–0.82). The odds of taking more hormones than prescribed were higher among respondents who reported having the same provider for primary and gender-affirming care (aOR = 2.14, 95% CI = 1.04–4.44) and those with an increased number of major gender-based discrimination experiences out of a possible 11 (aOR = 1.25 per experience, 95% CI = 1.08–1.44).
Regression outcome: taking less hormones than prescribed
Table 2 also shows the adjusted multivariable logistic regression models examining factors associated with taking less hormones than prescribed. In the final model, the odds of taking less hormones than prescribed were higher among nonbinary respondents compared to transfeminine respondents (aOR = 2.06, 95% CI = 1.05–4.04), those with a low income (aOR = 1.94, 95% CI = 1.13–3.32), those with no insurance coverage for hormones (aOR = 4.27, 95% CI = 1.73–10.56), and those who had received mental health treatment in the past year (aOR = 2.00, 95% CI = 1.14–3.48).
Reasons for taking more hormones
As shown in Table 3 , the most endorsed reasons for taking more hormones than prescribed were believing that it is not the right prescribed dose (37%), taking it to feel good (36%), to speed up transition or the gender-affirmation process (27%), and making up for missed doses (17%).
Emergent themes from the write-in responses included the following reasons for taking more hormones: making up for missed doses, having concerns about reproductive health, and having an imprecise practice of dose administration.
Many respondents reported making up for missed hormone doses as a reason for taking more hormones than prescribed, with some respondents indicating “doubling” or taking “a little extra” dose if missed. These respondents noted:
“ If I miss a week because my pharmacy took forever to get my T (testosterone) in, I’ll sometimes go to 0.45 on the 1 mL syringe instead of 0.4.” (transmasculine respondent, age 24)
“ Accidentally doubling my dose because I forgot that I took the first.” (transfeminine respondent, age 37)
“ I miss my shot day; I accidentally pull a little extra when getting the shot ready.” (nonbinary respondent, age 29)
Reproductive health concerns regarding menstruation also emerged as one of the reasons transmasculine people reported taking more hormones than prescribed. Specifically, many transmasculine respondents reported taking higher doses of their hormones to mitigate one’s gender dysphoria and physical discomfort related to menstruation. Participants noted:
“Experience menstrual cramping.” (transmasculine respondent, age 45)
“If I start bleeding.” (transmasculine respondent, age 29)
“Period returned making me feel dysphoric.” (transmasculine respondent, age 28).
Lastly, some respondents noted that taking more hormones than prescribed also occurred when they experienced logistical difficulty self-administering hormones via injection, as preparing the dose can sometimes lead to “imprecise” measurement. Specifically, respondents mentioned that they often increase their dose as it is “easier to go over than try to be exact” or compensate for when the medication “leaks” out of the syringe, as described below:
“I take a bit more most times because some usually leaks out.” (transmasculine respondent, age 19).
“Measurement is imprecise and I honestly don’t care about getting it perfect—easier to go over than try to be exact.” (transmasculine respondent, age 37)
Reasons for taking less hormones
As shown in Table 3 , the most commonly endorsed reasons for taking less hormones than prescribed were forgetting to take the medication (70%), forgetting to pick up the prescription (27%), cost of hormones (18%), experiencing transportation barriers when attempting to pick up their prescription (13%), having syringe concerns (e.g., phobia, pain, anxiety) (9%), health insurance issues (e.g., lack of insurance, delay in approval, changes in in-network provider) (7%), and believing that the prescribed dose was incorrect (5%).
Among those who indicated taking less hormones than prescribed, emergent themes included experiencing other physical concerns (e.g., hair loss, acne issues), pharmacy issues (e.g., delays or unavailability of refills, being stigmatized by the pharmacist), and reliance on other people to administer their hormones.
Some participants who endorsed taking less hormones than prescribed reported experiencing psychological and physical concerns about using syringes, particularly pain at the injection site, as well as anxiety and phobia related to the injection. These negative experiences and concerns with syringes could deter some participants from successfully taking their medication, as described by the following respondents:
“Intense anxiety about injecting prevents me from completing a shot.” (nonbinary age 20)
“Injection method is uncomfortable.” (transmasculine, age 26)
“Injection site pain/fatigue.” (transmasculine, age 32)
“The injections are painful, so I often procrastinate on it.” (transmasculine, age 39)
Moreover, experiencing pain from injecting could also delay the timing of hormone administration. For instance, one respondent who reported taking less hormones than prescribed elaborated on how they would adjust the frequency of taking their hormones by 5 or more days to mitigate injection pain. They noted:
“I use IM (intramuscular) injections for hormones; it is painful to use needles, so rather than every 7 days as prescribed, I do once every 12 days.” (transmasculine, age 33)
Another reason some respondents endorsed taking less hormones than prescribed is to mitigate the physical side effects of hormones. For instance, one nonbinary respondent described experiencing hair loss, and one transmasculine respondent reported experiencing acne, which would, in turn, led them to reduce their hormone dose to mitigate these side effects, as described below:
“It causes lots of hair loss so I just dab it on to feel good, but the regular application makes my hair fall out more.” (nonbinary, age 36)
“To reduce acne issues.” (transmasculine, age 29)
Additionally, one nonbinary respondent, while “liking all other effects” of testosterone, described developing distress associated with body hair grow and lowered their dose to minimize these physical changes:
“Dysphoria from body hair growth caused by T (testosterone), despite liking all the other effects.” (nonbinary, age 29)
Some respondents described prescription fill-related barriers as a reason for taking less hormones than prescribed. These barriers ranged from prescription unavailability and refill delays to forgetting to call in refills, which made some respondents ration their hormones. As the following three respondents expressed:
“Pharmacy has hard time acquiring medication.” (transmasculine, age 43)
“I’m afraid of running out/losing access to hormones and want to have a backup supply, or sometimes I forget to call in refills in time and have to stretch what I have left so I’m not off hormones cold turkey while I wait to get more.” (transfeminine, age 26)
“Very afraid of running out and not being able to get more. It’s all I have left.” (transfeminine, age 38)
Additionally, some participants reported experiencing gender-based discrimination by pharmacists when picking up their hormone prescriptions, which discouraged them from coming into the pharmacy again or caused them to delay or not obtain their hormones. This was noted by the following two respondents:
“It’s a restricted substance and the pharmacy always gives me grief trying to pick it up. It’s the only prescription I have [in which] pharmacists are weird with me about or call up my doctor for, and I’ve never had that happen even with other controlled substances.” (transmasculine, age 19)
“Discrimination faced at pharmacies filling orders.” (transmasculine, age 23)
Lastly, one respondent noted that they take less hormones than prescribed due to having to rely on others to administer their dose. This respondent noted,
I can’t administer it myself and have to rely on others. (transmasculine, age 24)
To our knowledge, this is the first study to descriptively explore and detail dosing behaviors of prescribed hormones among trans populations. Taken together, our results indicate that access barriers related to income and insurance coverage were associated with trans respondents taking less hormones than prescribed whereas taking more hormones than prescribed was associated with having one’s primary care physician also prescribe hormone treatment, as well as with experiences of gender-based discrimination. While exploratory, these findings show a critical need for examining ways to optimize adherence to gender-affirming hormones by addressing multiple levels of individual and structural barriers that can deter trans people from meeting their gender-affirmation goals.
We found that participants were more likely to take less hormones than prescribed due to a range of factors reflecting both structural barriers to access and perceived incentives to take a reduced dose. Insurance issues were a major contributor to variable dosing: specifically, a lack of insurance coverage, whether due to being uninsured or having health insurance that did not cover hormones, was highly associated with taking a reduced dose, potentially due to rationing or the inability to consistently afford the cost of their hormone prescription with no insurance coverage. A prior study found that uninsured trans people were less likely to be on any hormone treatment than insured trans people (Stroumsa et al., 2020 ). Even for people with insurance coverage, exclusions of gender-affirming care, including hormone therapy, persist among people with public insurance (particularly state Medicaid programs) and people with private insurance plans (Dowshen et al., 2019 ; Kirkland et al., 2021 ; Zaliznyak et al., 2021 ). Similarly, while the literature on distance traveled to access gender-affirming services like hormones is scant, existing research illustrates a willingness to travel further distances to access knowledgeable providers that are capable of providing gender-affirming healthcare (Cicero et al., 2019 ; Kattari et al., 2020 ). While online prescribers are growing and expanding access to more areas, state-level policies on insurance, combined with controlled substance regulations, continue to vary state-by-state; thus access to online prescribers of gender-affirming hormones may be limited for trans people in certain geographic areas (Baker, 2017 ; Beauchamp, 2013 ; Holt et al., 2019 ; Kattari et al., 2020 ). Our findings related to insurance coverage, regulations, and provider availability suggest that, while some trans people in our study are able to access hormones, they may not be able to take the prescribed dose consistently. Cost issues may be driving hormone access issues as having a low-income was associated with taking hormones at lower doses than prescribed. Even with insurance coverage, individuals who have lower incomes may still be unable to consistently afford the co-pay for their hormone prescription and so they may reduce their hormone dosage as a way to ration their medication between refill cycles. These findings are important given previous research highlighting that trans people, despite having on average higher educational attainment than cisgender people, tend to have reduced employment and reduced income compared to the general population (Adams & Vincent, 2019 ; Seelman et al., 2017 ). To improve access to hormone treatment, both the availability and quality of insurance coverage, including overall insurance and medication affordability and specific provisions for the coverage of gender-affirming hormone therapy, should be improved in states across the country.
Receiving mental health treatment was also associated with reduced hormone use, though it is not clear whether this reflects a causal relationship or merely a co-occurring phenomenon. For instance, individuals receiving mental health treatment may do so because they struggle with daily functioning, including the functioning needed to receive and take hormones consistently. The challenge of taking hormones consistently is somewhat supported by the fact that forgetting to take hormones was the most commonly reported reason for missing a hormone dose. Prior studies have shown that non-attendance and non-adherence to physical health visits and medication are associated with poor mental health (Kretchy et al., 2014 ; Marrero et al., 2020 ). Receiving hormones has been associated with better mental health outcomes among trans people, including reduced depression and anxiety and improved quality of life (Baker et al., 2021 ; White Hughto & Reisner, 2016 ). However, other barriers and burdens may be associated with more severe mental health disorders that require treatment that may impact hormone use. Regardless of potential confounding, there should also be greater provider education about the particular barriers and gender-affirmation goals of nonbinary people seeking hormones.
We also found several associations with taking more hormones than prescribed. In particular, having the same healthcare provider for primary and gender-affirming care was associated with individuals taking doses beyond what was prescribed. From the write-in responses, overdosing and underdosing were both reported among those who mistrust their provider. In previous studies of trans people’s experiences in primary healthcare, one study found that 53.6% of trans participants reported that their primary care provider did not know enough about trans people to provide adequate care (Heng et al., 2018 ). Additionally, multiple studies reported that trans patients were educating their providers and conducting their own research (Costa et al., 2018 ; Dewey, 2008 ; Roller et al., 2015 ). Therefore, respondents may perceive that a primary care physician lacks the specialization to make informed dosage decisions and take dosing into their own hands. Our findings underscore the need for better integration of gender-affirming care with primary care, and vice versa, to optimize hormone adherence. Given differences between trans-friendly and trans-specific modes of service design and provision (Everhart et al., 2022 ), perspectives from trans patients regarding the ideal integration models, such as providing gender-affirming care in primary care settings vs. having primary care services in gender-affirming specialty clinics, could be helpful in understanding which models would feel more trustworthy, affirming, and likely to improve hormone adherence.
Individuals with greater reported experiences of gender-based discrimination were more likely to increase their dose beyond what was prescribed. This mechanism may be due in part to the desire to align one’s internal perceptions of one’s gender with one’s gender-affirming hormone goals. For example, individuals who are more likely to be perceived as nonbinary may experience increased gender-related discrimination (Anderson et al., 2020 ; Anderson, 2020 ; Cruz, 2014 ; Mizock et al., 2017 ), and therefore may feel compelled to take higher doses of hormones to achieve a more binary gender presentation and avoid discrimination. Future research should examine the reasons why individuals take higher hormone doses than prescribed, including the specific roles that discrimination and gender dysphoria play in trans people’s decisions around increased hormone dosing, particularly given that some trans people may not want to conform to binary gender expectations. It is also paramount that stigma and transphobia be addressed to reduce discrimination and support trans people’s health and well-being.
There were also gender-based differences in respondents reporting of taking more or less hormones than prescribed. Indeed, transmasculine respondents had reduced odds of taking more hormones than prescribed compared to transfeminine respondents. There are several potential mechanisms that may explain these findings, including that testosterone is highly regulated as a controlled substance, adding more structural barriers for providers, pharmacists, and trans people. Additionally, this finding might also be due to the prominence of secondary sex characteristics and perceived negative side effects of taking more testosterone compared to estrogen. For transfeminine people who begin hormones post-puberty, secondary sex characteristics may be perceived as more pronounced. Therefore, there may be a greater need to take increased doses to see intended results compared to transmasculine people, who may be likely to see quicker changes in their secondary sex characteristics at the prescribed dose. Additionally, while both estrogen and testosterone may yield unwanted side effects (Getahun et al., 2018 ; T’Sjoen et al., 2019 ), testosterone may be associated with a greater likelihood of experiencing unwanted effects, such as increased acne (Motosko et al., 2019 ), concerns around mood and aggression (Kristensen et al., 2021 ), and concerns that higher levels of testosterone will convert to estrogen and not produce the desired treatment effect. Although many of these concerns have been documented among people on testosterone there is a lack of empirical evidence to support many of these claims. For example, one large study found no association between serum testosterone levels and acne prevalence among transmasculine people, though age at the start of hormones was a risk factor for acne (Thoreson et al., 2021 ). Other studies have shown mixed evidence of changes in anger following testosterone therapy, with none following up longer than the first years on treatment (Defreyne et al., 2019 ; Kristensen et al., 2021 ; Motta et al., 2018 ; Thoreson et al., 2021 ). Further, while estradiol conversion is largely understudied among transmasculine participants, one small study from Massachusetts found estradiol levels decreased with testosterone treatment, with no evidence of conversion to estrogen greater than that in cisgender men (Chan et al., 2018 ). Nonetheless, concerns around unwanted side effects persist among some trans patients on hormone therapy, likely reflecting individual clinical histories and personal and community perceptions, rather than large-scale negative side effects across the population.
We also found that identifying as nonbinary, compared to identifying as transfeminine, was associated with using a lower dose of hormones than prescribed. This gender difference may be related to the specific treatment goals of nonbinary people, which may differ from binary trans people. The lower use of hormones by nonbinary people may suggest a need for prescribers to communicate better with nonbinary patients about their gender-affirmation goals. Notably, there is a paucity of studies on nonbinary people’s health in general (Matsuno & Budge, 2017 ; Scandurra et al., 2019 ), and no studies to our knowledge have examined the specific motivations and desires of nonbinary people compared to binary trans people in their gender-affirming care. While recent articles have made a case for tailoring hormone regimens to the needs of individual nonbinary patients (D’hoore & T’Sjoen, 2022 ; T’Sjoen et al., 2019 ), providers may hesitate to tailor hormone doses due to a lack of expertize in identifying and maintaining tailored regimens. Given recent research suggesting that nonbinary people more frequently have to educate their providers about the needs of trans people than binary trans people (Reisner & Hughto, 2019 ), it is possible that nonbinary people are not being prescribed hormone doses that meet their gender-affirmation goals and therefore feel compelled to tailor their dosage themselves. Future research into intra-transgender community priorities and concerns around hormone use is important to fully understand gender differences in how trans people take their prescribed hormones. Moreover, as this study did not ascertain specific gender-affirming hormones (e.g., estrogen vs. testosterone), understanding which hormones were being prescribed and used among nonbinary people would be important to understanding and contextualizing how to best address the needs of this group.
Lastly, while our sample did not reflect concordant reporting of taking more and less hormones than prescribed, it is conceptually possible that individuals may take more and less hormones at different times—a potential point for future research investigation. The timing and circumstances of when modified dosing behaviors occur should be explored in future longitudinal, mixed-methods studies (e.g., ecological momentary assessments). Findings from such studies could be used to identify strategies to promote adherence and maintenance of hormone use among trans populations.
Limitations
This study has methodological limitations that should be considered when interpreting findings. As a cross-sectional study, causality cannot be determined. Moreover, given the use of convenience sampling and the web-based survey, it is possible that the final sample is not representative of the entire trans population, including those who do not have access to the internet. Additionally, the measures used here are based on self-report, which is subject to bias. Although the racial/ethnic composition of the sample reflected that of the Massachusetts and Rhode Island populations (U.S. Census, 2020a , 2020b ), results from this study are not generalizable to all trans people in the US, particularly communities largely comprised of racial/ethnic minority populations. Additionally, although we oversampled communities of color and recognized the heterogeneity of racial/ethnic minority communities, due to the lower percentage of participants from each racial/ethnic minority group, we had to combine all non-White participants as a single group (i.e., people of color). This analytical approach may have masked important differences in hormone usage by race/ethnicity. Ethnoracial identity in the context of healthcare provision and access is best used as a proxy for identifying individuals exposed to systemic racism (Lett et al., 2022 ). Future studies of adherence should capture a more ethnoracially diverse cohort and include direct measures of systemic racism and discrimination to understand if and how hormone regimen adherence may vary due to the noxious exposure to racism (Lett et al., 2022 ).
Conclusions
In sum, the present study found the majority of trans individuals surveyed had used hormones at a lower or higher dose than prescribed. Trans individuals who take hormones at doses different than what was prescribed may choose to modify their dose as a means of achieving their gender-affirmation goals, mitigating the adverse physical side effects of hormones, and enhancing physiological and psychological effects of hormones. Structural and interpersonal barriers to care, including cost, lack of insurance coverage, and discrimination, were also found to be key drivers of taking hormones differently than prescribed. These findings underscore the need to eliminate barriers to taking medically necessary hormones for trans populations and the importance of providers understanding the gender-affirmation goals of their trans patients so that they can prescribe appropriate hormone regimens. Future research should seek to understand how providers determine hormone dosing and communicate safety messages to ensure that trans patients are able to achieve their gender-affirmation goals safely and effectively.
Data availability
Given that this study contains data with potentially sensitive information, data from this study are available upon request. Contact the The Fenway Institutional Review Board (IRB) Committee ([email protected]) for data requests.
Change history
21 october 2022.
A Correction to this paper has been published: https://doi.org/10.1057/s41599-022-01386-z
Adams NJ, Vincent B (2019) Suicidal thoughts and behaviors among transgender adults in relation to education, ethnicity, and income: a systematic review. Transgender Health 4(1):226–246
Article PubMed PubMed Central Google Scholar
Anderson AD, Irwin JA, Brown AM, Grala CL (2020) “Your picture looks the same as my picture”: an examination of passing in transgender communities. Gender Issues 37(1):44–60
Article Google Scholar
Anderson SM (2020) Gender matters: the perceived role of gender expression in discrimination against cisgender and transgender LGBQ individuals. Psychol Women Q 44(3):323–341
Ashley F (2021) The misuse of gender dysphoria: toward greater conceptual clarity in transgender health. Perspect Psychol Sci 16(6):1159–1164
Article MathSciNet PubMed Google Scholar
Baker KE (2017) The future of transgender coverage. N Engl J Med 376(19):1801–1804
Article PubMed Google Scholar
Baker KE, Wilson LM, Sharma R, Dukhanin V, McArthur K, Robinson KA (2021) Hormone therapy, mental health, and quality of life among transgender people: a systematic review. J Endocrine Soc 5(4):bvab011
Beauchamp T (2013) The substance of borders: transgender politics, mobility, and US state regulation of testosterone. GLQ J Lesbian Gay Stud 19(1):57–78
Bouman WP, Claes L, Brewin N, Crawford JR, Millet N, Fernandez-Aranda F, Arcelus J (2017) Transgender and anxiety: a comparative study between transgender people and the general population. Int J Transgenderism 18(1):16–26
Chan KJ, Jolly D, Liang JJ, Weinand JD, Safer JD (2018) Estrogen levels do not rise with testosterone treatment for transgender men. Endocr Pract 24(4):329–333
Chodzen G, Hidalgo MA, Chen D, Garofalo R (2019) Minority stress factors associated with depression and anxiety among transgender and gender-nonconforming youth. J Adolesc Health 64(4):467–471
Cicero EC, Reisner SL, Silva SG, Merwin EI, Humphreys JC (2019) Healthcare experiences of transgender adults: an integrated mixed research literature review. Adv Nurs Sci 42(2):123
Costa AB, da Rosa Filho HT, Pase PF, Fontanari AMV, Catelan RF, Mueller A, Cardoso D, Soll B, Schwarz K, Schneider MA (2018) Healthcare needs of and access barriers for Brazilian transgender and gender diverse people. J Immigr Minor Health 20(1):115–123
Cruz TM (2014) Assessing access to care for transgender and gender nonconforming people: a consideration of diversity in combating discrimination. Social Sci Med 110:65–73
D’hoore L, T’Sjoen G (2022) Gender‐affirming hormone therapy: an updated literature review with an eye on the future. J Int Med 291(5):574–592
Defreyne J, Kreukels B, t’Sjoen G, Staphorsius A, Den Heijer M, Heylens G, Elaut E (2019) No correlation between serum testosterone levels and state-level anger intensity in transgender people: results from the European Network for the Investigation of Gender Incongruence. Hormone Behav 110:29–39
Article CAS Google Scholar
Dewey JM (2008) Knowledge legitimacy: how trans-patient behavior supports and challenges current medical knowledge. Qual Health Res 18(10):1345–1355
Article ADS PubMed Google Scholar
Dowshen NL, Christensen J, Gruschow SM (2019) Health insurance coverage of recommended gender-affirming health care services for transgender youth: shopping online for coverage information. Transgender Health 4(1):131–135
Everhart AR, Boska H, Sinai-Glazer H, Wilson-Yang JQ, Burke NB, LeBlanc G, Persad Y, Ortigoza E, Scheim AI, Marshall Z (2022) ‘I’m not interested in research; i’m interested in services’: how to better health and social services for transgender women living with and affected by HIV. Soc Sci Med 292:114610
Foster Skewis L, Bretherton I, Leemaqz SY, Zajac JD, Cheung AS (2021) Short-term effects of gender-affirming hormone therapy on dysphoria and quality of life in transgender individuals: a prospective controlled study. Front Endocrinol 12: 717766
Getahun D, Nash R, Flanders WD, Baird TC, Becerra-Culqui TA, Cromwell L, Hunkeler E, Lash TL, Millman A, Quinn VP (2018) Cross-sex hormones and acute cardiovascular events in transgender persons: a cohort study. Ann Int Med 169(4):205–213
Heng A, Heal C, Banks J, Preston R (2018) Transgender peoples’ experiences and perspectives about general healthcare: a systematic review. Int J Transgend 19(4):359–378
Herman JL, Brown TN, Haas AP (2019) Suicide thoughts and attempts among transgender adults: findings from the 2015 US Transgender Survey. UCLA School of Williams Institute
Hoffkling A, Obedin-Maliver J, Sevelius J (2017) From erasure to opportunity: a qualitative study of the experiences of transgender men around pregnancy and recommendations for providers. BMC Pregnancy Childbirth 17(2):1–14
Google Scholar
Holt NR, Hope DA, Mocarski R, Woodruff N (2019) First impressions online: The inclusion of transgender and gender nonconforming identities and services in mental healthcare providers’ online materials in the USA. Int J Transgend 20(1):49–62
Hughto JMW, Reisner SL, Pachankis JE (2015) Transgender stigma and health: a critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med 147:222–231
James S, Herman J, Rankin S, Keisling M, Mottet L, Anafi M (2021) The Report of the 2015 US Transgender Survey. Published online 2016. National Center for Transgender Equality
Johnson AH, Hill I, Beach-Ferrara J, Rogers BA, Bradford A (2020) Common barriers to healthcare for transgender people in the US Southeast. Int J Transgender Health 21(1):70–78
Kattari SK, Grange J, Seelman KL, Bakko M, Harner V (2020) Distance traveled to access knowledgeable trans-related healthcare providers. Ann LGBTQ Public Popul Health 1(2):83–95
Kirkland A, Talesh S, Perone AK (2021) Transition coverage and clarity in self-insured corporate health insurance benefit plans. Transgender Health 6(4):207–216
Klemmer CL, Arayasirikul S, Raymond HF (2021) Transphobia-based violence, depression, and anxiety in transgender women: the role of body satisfaction. J Interpers Viol 36(5-6):2633–2655
Kohlbacher F (2006) The use of qualitative content analysis in case study research. Forum Qualitative Sozialforschung/Forum, Qualitative Social Research
Kretchy IA, Owusu-Daaku FT, Danquah SA (2014) Mental health in hypertension: assessing symptoms of anxiety, depression and stress on anti-hypertensive medication adherence. Int J Mental Health Syst 8(1):1–6
Kristensen TT, Christensen LL, Frystyk J, Glintborg D, T’sjoen G, Roessler KK, Andersen MS (2021) Effects of testosterone therapy on constructs related to aggression in transgender men: a systematic review. Hormone Behav 128:104912
Lerner JE, Martin JI, Gorsky GS (2021) More than an apple a day: Factors associated with avoidance of doctor visits among transgender, gender nonconforming, and nonbinary people in the USA. Sex Res Soc Policy 18(2):409–426
Lett E, Abrams MP, Gold A, Fullerton F-A, Everhart A (2022) Ethnoracial inequities in access to gender-affirming mental health care and psychological distress among transgender adults. Soc Psychiatry Psychiatr Epidemiol 57:963–971
Lett E, Asabor E, Beltrán S, Cannon AM, Arah OA (2022) Conceptualizing, contextualizing, and operationalizing race in quantitative health sciences research. Ann Fam Med 20(2):157–163
Marrero RJ, Fumero A, de Miguel A, Peñate W (2020) Psychological factors involved in psychopharmacological medication adherence in mental health patients: a systematic review. Patient Educ Counsel 103(10):2116–2131
Matsuno E, Budge SL (2017) Non-binary/genderqueer identities: a critical review of the literature. Curr Sex Health Rep 9(3):116–120
Mizock L, Woodrum TD, Riley J, Sotilleo EA, Yuen N, Ormerod AJ (2017) Coping with transphobia in employment: strategies used by transgender and gender-diverse people in the United States. Int J Transgend 18(3):282–294
Motosko C, Zakhem G, Pomeranz M, Hazen A (2019) Acne: a side‐effect of masculinizing hormonal therapy in transgender patients. Br J Dermatol 180(1):26–30
Article CAS PubMed Google Scholar
Motta G, Crespi C, Mineccia V, Brustio PR, Manieri C, Lanfranco F (2018) Does testosterone treatment increase anger expression in a population of transgender men? J Sex Med 15(1):94–101
Parra‐Frutos I (2014) Controlling the Type I error rate by using the nonparametric bootstrap when comparing means. Br J Math Stat Psychol 67(1):117–132
Article MathSciNet PubMed MATH Google Scholar
Puckett JA, Cleary P, Rossman K, Mustanski B, Newcomb ME (2018) Barriers to gender-affirming care for transgender and gender nonconforming individuals. Sex Res Soc Policy 15(1):48–59
Ratanawongsa N, Karter AJ, Parker MM, Lyles CR, Heisler M, Moffet HH, Adler N, Warton EM, Schillinger D (2013) Communication and medication refill adherence: the Diabetes Study of Northern California. JAMA Intern Med 173(3):210–218
Redfern JS, Sinclair B (2014) Improving health care encounters and communication with transgender patients. J Commun Healthcare 7(1):25–40
Reisner SL, Deutsch MB, Bhasin S, Bockting W, Brown GR, Feldman J, Garofalo R, Kreukels B, Radix A, Safer JD (2016) Advancing methods for US transgender health research. Curr Opin Endocrinol Diab Obes 23(2):198
Reisner SL, Hughto JM (2019) Comparing the health of non-binary and binary transgender adults in a statewide non-probability sample. PLoS ONE 14(8):e0221583
Article CAS PubMed PubMed Central Google Scholar
Restar A, Jin H, Breslow A, Reisner SL, Mimiaga M, Cahill S, Hughto JM (2020) Legal gender marker and name change is associated with lower negative emotional response to gender-based mistreatment and improve mental health outcomes among trans populations. SSM Popul Health 11:100595
Restar A, Jin H, Breslow AS, Surace A, Antebi-Gruszka N, Kuhns L, Reisner SL, Garofalo R, Mimiaga MJ (2019) Developmental milestones in young transgender women in two American cities: results from a racially and ethnically diverse sample. Transgender Health 4(1):162–167
Roller CG, Sedlak C, Draucker CB (2015) Navigating the system: how transgender individuals engage in health care services. J Nurs Scholarship 47(5):417–424
Sabaté E, Sabaté E (2003) Adherence to long-term therapies: evidence for action. World Health Organization
Scandurra C, Mezza F, Maldonato NM, Bottone M, Bochicchio V, Valerio P, Vitelli R (2019) Health of non-binary and genderqueer people: a systematic review. Front Psychol 10:1453
Seelman KL, Colón-Diaz MJ, LeCroix RH, Xavier-Brier M, Kattari L (2017) Transgender noninclusive healthcare and delaying care because of fear: connections to general health and mental health among transgender adults. Transgender Health 2(1):17–28
Silva DC, Salati LR, Villas-Bôas AP, Schwarz K, Fontanari AM, Soll B, Costa AB, Hirakata V, Schneider M, Lobato MIR (2021) Factors associated with ruminative thinking in individuals with gender dysphoria. Front Psychiatry 12:799
Sperber J, Landers S, Lawrence S (2005) Access to health care for transgendered persons: Results of a needs assessment in Boston. Int J Transgenderism 8(2-3):75–91
Stroumsa D, Crissman HP, Dalton VK, Kolenic G, Richardson CR (2020) Insurance coverage and use of hormones among transgender respondents to a National Survey. Ann Fam Med 18(6):528–534
T’Sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V (2019) Endocrinology of transgender medicine. Endocr Rev 40(1):97–117
Thoreson N, Park JA, Grasso C, Potter J, King DS, Marc LG, Shen C, Peebles JK, Dommasch ED (2021) Incidence and factors associated with acne among transgender patients receiving masculinizing hormone therapy. JAMA Dermatol 157(3):290–295
Tibshirani R (1996) Regression shrinkage and selection via the lasso. J R Stat Soc Ser B 58(1):267–288
MathSciNet MATH Google Scholar
US Census (2020a) Quick facts: Massachusetts. U.S. Census Bureau. Retrieved May 26, 2020 from http://www.census.gov/quickfacts/table/PST045215/25
US Census (2020b) Quick facts: Rhode Island. U.S. Census Bureau. Retrieved May 26, 2020 from https://www.census.gov/quickfacts/fact/table/RI,US/PST045219
Webb AJ, McManus D, Rouse GE, Vonderheyde R, Topal JE (2020) Implications for medication dosing for transgender patients: a review of the literature and recommendations for pharmacists. Am J Health Syst Phar 77(6):427–433
White Hughto JM, Reisner SL (2016) A systematic review of the effects of hormone therapy on psychological functioning and quality of life in transgender individuals. Transgender Health 1(1):21–31
Zaliznyak M, Jung EE, Bresee C, Garcia MM (2021) Which US States’ medicaid programs provide coverage for gender-affirming hormone therapy and gender-affirming genital surgery for transgender patients?: a state-by-state review, and a study detailing the patient experience to confirm coverage of services. J Sex Med 18(2):410–422
Zolnierek KBH, DiMatteo MR (2009) Physician communication and patient adherence to treatment: a meta-analysis. Med Care 47(8):826
Download references
Acknowledgements
We would like to thank the participants of this study, and our research members for their assistance with this study: Jackson McMahon, Christopher Santostefano, David Pletta, and Ryan Segur. This work is supported by the Providence/Boston Center for AIDS Research (CFAR) funded by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under grant number P30AI042853. Dr. Restar is supported by the Robert Wood Johnson Foundation Health Policy Research Scholar. Drs. Restar and Radix are supported by the Yale School of Public Health’s Research Education Institute for Diverse Scholars (REIDS), funded by the National Institute of Mental Health (R25MH087217). The views and opinions expressed in this article are solely those of the authors and do not necessarily represent the official views of the sponsors.
Author information
Authors and affiliations.
Department of Epidemiology, School of Public Health, University of Washington, Seattle, WA, USA
- Arjee Restar
Department of Behavioral and Social Sciences, Yale University School of Public Health, New Haven, CT, USA
Arjee Restar & Asa Radix
Center for Applied Transgender Studies, Chicago, IL, USA
Arjee Restar, Elle Lett & Avery Everhart
Department of Biostatistics, School of Public Health, University of Washington, Seattle, WA, USA
E. J. Dusic
Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA
Henri Garrison-Desany & Kellan E. Baker
Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA
Population, Health, & Place Program, Spatial Sciences Institute, Dornsife College of Letters, Arts, & Sciences, University of Southern California, Los Angeles, CA, USA
Avery Everhart
Whitman-Walker Institute, Washington, DC, USA
Kellan E. Baker
Department of Epidemiology and Biostatistics, Dornsife School of Public Health, Drexel University, Philadelphia, PA, USA
Ayden I. Scheim
Department of Health, Behavior and Society, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA
S. Wilson Beckham
Department of Epidemiology, Harvard T.H. Chan School of Public Health, Harvard University, Boston, MA, USA
Sari Reisner
Hebrew University School of Public Health, Jerusalem, Israel
Adam J. Rose
UCLA Center for LGBTQ+ Advocacy, Research & Health, Los Angeles, CA, USA
Matthew J. Mimiaga
Department of Epidemiology, UCLA Fielding School of Public Health, Los Angeles, CA, USA
Department of Epidemiology, Columbia University, New York, NY, USA
Callen-Lorde Community Health Center, New York, NY, USA
Departments of Behavioral and Social Sciences and Epidemiology, Brown University School of Public Health, Providence, RI, USA
Don Operario & Jaclyn M. W. Hughto
Fenway Health, The Fenway Institute, Boston, MA, USA
Jaclyn M. W. Hughto
You can also search for this author in PubMed Google Scholar
Contributions
AR and JH were involved in the conceptualization of this paper. AR and JH designed the analysis for this paper. AR conducted the data analysis. AR, EJD, and HG-D wrote the paper. All authors analyzed and interpreted the data, and significantly reviewed/edited the paper.
Corresponding author
Correspondence to Arjee Restar .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (The Fenway Institutional Review Board (IRB) at Fenway Health in Boston, Massachusetts) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors. The ethics approval number for the study was: 1280264-2.
Informed consent
Electronic written informed consent was attained for all enrolled participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Restar, A., Dusic, E.J., Garrison-Desany, H. et al. Gender affirming hormone therapy dosing behaviors among transgender and nonbinary adults. Humanit Soc Sci Commun 9 , 304 (2022). https://doi.org/10.1057/s41599-022-01291-5
Download citation
Received : 17 March 2022
Accepted : 25 July 2022
Published : 07 September 2022
DOI : https://doi.org/10.1057/s41599-022-01291-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Gender-affirming hormone therapy in transgender women and risk of prostate cancer: pathophysiological mechanisms and clinical implications.
- Eugenio Bologna
- Leslie Claire Licari
- Celeste Manfredi
Prostate Cancer and Prostatic Diseases (2024)
Improving the cardiovascular health care of transgender and non-binary persons
- Carl G. Streed
Nature Reviews Cardiology (2023)
The Utility of Preclinical Models in Understanding the Bone Health of Transgender Individuals Undergoing Gender-Affirming Hormone Therapy
- Varun S. Venkatesh
- Rachel A. Davey
Current Osteoporosis Reports (2023)
Mapping Community-Engaged Implementation Strategies with Transgender Scientists, Stakeholders, and Trans-Led Community Organizations
- Brian J. Minalga
- Kristi E. Gamarel
Current HIV/AIDS Reports (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

Know Before You Go: Tips for Transgender and Nonbinary Travelers
For people whose gender identity doesn’t match the one assigned to them on their birth certificate, dealing with air travel can present a host of obstacles. here’s what u.s. travelers need to know about flying outside of the binary..
- Copy Link copied

The Transgender Pride Flag consists of five horizontal stripes: two light blue, two pink, and one white.
Illustration by Shutterstock
If you’re a transgender or nonbinary traveler, making your way through the airport can feel like a journey in itself. Different airlines and airports enforce varying policies when it comes to harassment and discrimination, but all air travel requires in some way that travelers “declare” a gender as part of their identification. For transgender people and nonbinary folk (those whose internal sense of self isn’t exclusively male or female), this means effectively outing yourself to every TSA official you encounter.
To offset the anxieties that come with navigating the airport as a transgender or nonbinary person, it can be helpful to know what to expect before traveling in order to prepare your documents and review your answers to security questions. These tips will give you the information you need to make smart decisions and figure out what works for you while preparing for air travel.
Navigating gender markers on travel documents
According to the U.S. State Department website , changing the name or gender marker on a U.S. passport requires submitting a DS-11 application form complete with a recent form of government-issued identification and a passport-appropriate photo (both of which must resemble your current appearance), proof of legal name change (for those changing their names), and a medical certification indicating that you have received—or are in the process of receiving—clinical treatment for your transition. Templates for this medical certification, which must be signed by a licensed physician, can be downloaded from the government agency’s website . It’s important to note that a description of the specific “treatment” is not required in the medical certification and need not be limited only to gender confirmation surgery—the State Department intentionally leaves it open for interpretation.
Still, some trans women have reported encountering unexpected roadblocks in getting their names and gender markers changed on their passports in the United States. In these cases, it took the intervention of a sympathetic politician to sort out a simple bureaucratic error. It’s unclear how widespread this problem is, but just in case, nonbinary and trans people hoping to use their correct names and gender identities on their travel documents should start updating their passports well in advance of their intended travel date.
Whether or not you’re able to change your name and gender marker, the main thing is that your passport photo somewhat matches your actual physical appearance. If your appearance has changed significantly since starting your transition, you may want to renew your passport with an updated photo and carry an additional piece of I.D. that matches the information on your passport. (Across the United States, rules regarding name and gender changes on drivers’ licenses vary. The National Center for Transgender Equality has a helpful search tool that spotlights policies specific to each state.)
While the United States doesn’t currently offer gender neutral passports, many other countries do provide some variation for travelers who don’t identify with the the “male” or “female” binary gender options. For instance, Australia, Denmark, Germany, Malta, New Zealand, and Pakistan also have an “X” category, while India, Ireland, and Nepal provide various third gender options. My Canadian passport has an “X” (undetermined), along with an “M” (male). Sure, it’s a bit of an unsatisfying compromise, but there’s still something reassuring about having a government document that acknowledges my nonbinary identity.
Flight tickets
Earlier this year, Airlines for America (A4A) and the International Air Transport Association (IATA) announced that starting June 1, 2019, both major trade organizations would allow airlines to offer two new gender options for travelers booking flights: “U” (undisclosed) or “X” (unspecified), in contrast to the previous binary system consisting of “M” (male) and “F” (female) titles only. Following the update, all five major airlines in the United States—United, Alaska, American, Delta, and Southwest—announced that they plan to shift toward more inclusive gender options for travelers.
This spring, United Airlines became the first U.S. airline to provide gender neutral options in its booking process. (This change came with newly implemented training sessions for United employees—offered by the Human Rights Campaign and The Trevor Project , an organization devoted to mental health advocacy for LGBTQ youth—which cover topics such as gender discrimination and use of preferred pronouns.)
Although the rest of the aforementioned airlines maintain plans to add the new gender options, most currently have no timetable for the update. All the same, the real test will be in how transgender and nonbinary people are treated in real life while traveling.
Getting through airport security
TSA pat-downs and scans
Security scans and pat-downs are infamous among transgender travelers. At U.S. airports, TSA requires passengers to go through a full-body Advanced Imaging Technology (AIT) scanner that operates on a binary gender system—it’s programmed to read certain bodies in certain ways and to see any “irregularities” as signs of danger. As you can imagine, this poses problems for some trans people, for whom a bulge in the “wrong” place is often misperceived as a security threat. (Before each passenger enters the machine, a TSA agent must press a blue “male” or pink “female” button so that the device’s Automatic Target Recognition software can detect “anomalies” not consistent with the passenger’s assigned gender.)
If an “anomaly” is detected, the AIT machine will ring an alarm, which means you’ll have to receive additional screening before passing through airport security—often in the form of a pat-down. For some people, this can be an uncomfortable experience of public humiliation. According to the TSA website , travelers can intially request a pat-down instead of an AIT scan, which avoids the potential embarrassment of the alarm (even though the end result of a pat-down is the same). You can also request an inspecting TSA agent who matches your gender identity, and you can request to have the pat-down conducted in a private area with a companion of your choosing.
Packing medications, prosthetics, and implants
Most airlines and airports will allow you to travel with medications and supplies in your carry-on, although they should be packed in a separate bag within your luggage. For transgender travelers who inject their hormones, it’s best to pack any medical syringes alongside their corresponding medications and to try to keep the pharmaceutical label intact. The TSA website also advises travelers to declare any syringes or dilators to inspectors before going through security and to travel with proof of the medical necessity of the item(s).
Transgender travelers wearing chest binders or prosthetic devices may need to undergo Explosive Trace Detection (ETD), or swabbing. (Implants should not pose any issue.) The National Center for Transgender Equality states that travelers are not required to “lift, remove, or raise an article of clothing to reveal a prosthetic item and should not be asked to remove it.” According to their website , if a TSA officer asks you to reveal a prosthetic item, you can ask to speak to a supervisor. You can also ask to be screened in a private room. Still, this whole process can be time-consuming, so make sure to arrive early to account for delays.
Transgender or nonbinary travelers with questions about medical equipment and devices can call the TSA Cares hotline in advance of their trip at 1-855-787-2227.
The most important thing to keep in mind
Airports can be unsettling spaces for everyone but especially for trans and nonbinary people—and particularly for trans people of color. Airports are not simply binary spaces; they are also under heavy security. The important thing to remember is that there’s nothing “wrong” with you or your body. There’s no reason for people to be seeing you as a threat, and you have every right to demand respectful treatment. As with any negative customer experience, if you have any issues with airline or TSA personnel, you can report it .
Remember, navigating the airport is just one part of the trip. For better or worse, your time there doesn’t have to define your travel experience. The rest of it is up to you.
>>Next: Seeing the World Through Rainbow-Colored Glasses

The Unique Anxiety of Traveling While Transgender
By Kam Burns
People tend to look at me funny when I tell them I love flying, but it’s true. I always have. I've gotten my packing process down to a science and airports give me an excuse to put my phone on airplane mode for a few hours and catch up on reading without distraction.
But as I left for a recent work trip, I was unable to ease my travel anxiety. My palms were sweaty, I felt vaguely nauseous, and the closer I got to the airport, the more my heart began to race. It was my first flight since I started my transition, so for the first time in a long time, I had no idea what to expect. Every trans person I know has an airport story, often involving an inadvertent misunderstanding with a TSA agent, others with more intentional malice and discrimination.
As it turned out, my experience ended up being pretty uneventful. When the agent scanning my boarding pass examined my passport, a flicker of recognition crossed her face before she let me go without a word. I went through the body scanner knowing I would probably be fine because I’ve had top surgery, and I was right. I’m one of the lucky ones.
Flying When You’re Trans or Gender Non-Conforming
ProPublica recently reviewed all data that’s publicly available regarding complaints against the TSA and found that five percent of civil rights complaints filed with the TSA between January of 2016 and April of 2019 were from trans and gender-nonconforming individuals, despite the fact that we make up less than one percent of the population. And that was just of the people who chose to report.
The TSA body scanners that are used in standard security protocols in airports were not designed for people with bodies that aren't gender-normative. TSA agents have just a few moments to hit a blue or pink button before a person steps into the machine. If there’s a penis or breasts where the machine thinks there should not be, an alarm goes off.
As of this year, TSA agents are now required to partake in training on how to work with transgender passengers. But resources are limited, so the training simply consists of a 30-minute online program, and the level of turnover in the TSA is high, with an approximate 17 percent attrition rate. Of the 174 people who spoke to ProPublica, one woman reported that after asking to be patted down by a woman, she was refused and instead patted down by two male agents. Others reported being forced to show their genitals to TSA agents. Some felt as though they're assigned agents based on the gender they identify as, while others felt as though how they identified was not respected.
For any trans or gender non-conforming individual , being aware of the potential for any of these possibilities can cause anxiety before one even sets foot in an airport. But there are ways to make the experience a little less stressful without foregoing air travel altogether. And if you’re an ally, there are ways to support your trans and gender non-conforming friends so they feel safer in their travels.
Things You Can Do to Prepare and Feel More At Ease
If you fly frequently, consider getting TSA PreCheck. Your line to get through security will generally be shorter, which will give you more time to deal with any issues that might come up. You’ll have an expedited screening process and the perk of not having to take your shoes off in an airport, according to the TSA website . However, it does cost $85 for a five-year membership , so if that's prohibitive for you for whatever reason, there are other things you can do to ease anxiety.
If you’re a less frequent traveler (or even if you’re not), it’s a good idea to make sure you're packing and preparing correctly for your trip. Make sure you know what you can and cannot take in your carry-on, wear comfortable shoes, and double-check any items you’re unsure of. If you have a medication that requires syringes (like testosterone), have the prescription on hand so you can show an agent if the syringes are flagged.
For those who choose to wear a packer, a binder, or any other restrictive or enhancing garment, know that there’s a chance it will set off the machine. If that happens, respond as directly as possible and in a straightforward way. For example, if you’re wearing a binder, pull the agent aside and say, “This is a chest binder I wear to make my chest appear smaller, because of my gender identity and presentation.” Having a prepared response in advance can alleviate anxiety, and if you can provide an answer with confidence, you may be able to avoid further questioning. If the TSA agent continues to make it difficult for you to move forward, providing concise yet honest answers will also likely give you more success in filing a complaint later.
How to Be Helpful If You're a Cisgender Person Traveling With a Trans Friend or Loved One
If you’re cisgender and traveling with someone who is trans, be mindful they experience things you don't have to deal with or think about. Talk to them before booking travel if you're planning the itinerary, as some airports and airlines have better reputations with trans customers than others. Ask if they would like you to intervene should a case of misgendering come up. Go through security together, if possible, and if they have asked for your help, advocate for them when and where you can. In some cases, there won’t be much you can do (as people are often pulled into separate rooms if security is an issue), but just knowing there is a friend nearby can make things a little easier.
If you or a friend ends up having a negative or unsafe experience, it’s important to know your rights. The National Center for Transgender Equality has a guide on who to talk to and how to file a report in the case of discrimination. There’s even an app called FlyRights that will let you file a report from your phone immediately.

By Aliza Kelly
By Marci Robin

The way transgender people are treated in airports is unfortunately just a symptom of a much larger problem. Unfortunately, lack of awareness around gender is a huge issue, and though it's one that extends outside of the baggage claim, TSA body scanners and airports are designed for a binary society that puts anyone outside of the norm at risk. Luckily, there are people working to make those changes on a more systemic level. But in the meantime, do what you can to take care of yourself and your friends.
Read more stories about gender identity on Allure :
- Why I Marked "F" as the Gender on My License Even Though I'm Nonbinary
- What Reading Tarot Taught Me About Gender
- What It's Like to Be Transgender and Face Dysphoria and Body Dysmorphia at the Same Time
Now, learn the story behind Allure's new clean Best of Beauty seal:
Don't forget to follow Allure on Instagram and Twitter .

Allure Daily Beauty Blast
By signing up you agree to our User Agreement (including the class action waiver and arbitration provisions ), our Privacy Policy & Cookie Statement and to receive marketing and account-related emails from Allure. You can unsubscribe at any time. This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.

By Varuna Srinivasan

By Samantha Leal

By Brenda Della Casa
You don't have to constantly take hormones to be trans, 3 people who have gone on and off hormones say
- Medical transition is often painted as a linear process for trans people.
- Three trans people who have gone on and off HRT told Insider the process was different for everyone.
- "Trans people should feel free enough to start and stop hormones," Kayden Coleman said.

Before starting hormone-replacement therapy , Simon Moore, 27, thought hard about what effects they wanted to get from testosterone.
While they had always wanted a deeper voice, they didn't want all the added muscle and hair growth that sometimes comes with a full, longer-term dose of testosterone-based HRT. Like a growing number of nonbinary people , they decided a microdose would offer a slower transition.
"There is less emotional roller coaster. The vocal cords thicken slower and more gradually," Moore said.
Moore, who is nonbinary and trans, grew up in Moscow and moved to the US with their partner in 2019. They were able to access HRT for the first time in January through Plume , an online transgender-health service, they said.
It's been seven months since Moore started testosterone (commonly referred to as "T"), and they have decided to wean off it.
"I'm not really a 'trans man.' I never really wanted to be full-on masc, like go to the gym, get ripped, and get the whole beard," Moore told Insider. "I wanted something in between. I wanted to be comfortable."
Transition is often portrayed as a linear journey that has a clear beginning and end .
But many trans people go on and off hormones for a number of reasons, such as access to care, a desire to get pregnant, medical complications, or contentment with the results of HRT they already received.
Insider spoke with three trans people who have gone on and off HRT at various points for medical or personal reasons.
You don't need surgery or hormones to be trans
A popular misconception perpetuated by TV shows, films, and general misinformation is that being trans means someone needs to " medically transition ," or get gender-affirming medical procedures , to be seen as valid.
The idea that gender-affirming care is one size fits all and people stop HRT only because they regret their decision is often used as a political argument to justify anti-trans medical bills that suppress access to medical care for trans people.
There is a small and vocal group of people who have " detransitioned " and actively say they are no longer trans. But research suggests a majority of people who stop HRT do so for other reasons . Some trans people never take hormones at all.
"Nobody needs to be on hormone therapy. Nobody needs to undergo any medical, surgical, or other procedure, or even therapy — despite what people have told us for many years — to be trans," Dr. Jerrica Kirkley, the medical director for Plume , told Insider.
Stopping treatment doesn't make a person not trans, Kirkley said.
Moore knew they wanted to be on testosterone only for a year to lower their voice
Like many young trans people who grew up with little trans visibility, Moore as a teen relied on YouTube videos on female-to-male transition to get information about gender-affirming care.
But Moore decided they wanted their care to look a little different.
On their YouTube channel, Moore blogged their personal HRT journey.
Rather than taking the standard 0.5 milligrams of testosterone every week indefinitely, Moore decided to microdose 0.3 mG of testosterone a week for just seven months.
Moore then stopped microdosing once they got a deeper voice. (Certain effects of testosterone, like facial hair and a deeper voice , are permanent, while others, like building more muscle, are not and require consistent doses of T over time.)
Related stories
Moore is happy with their results. They told Insider that while they were stopping, they were open to the idea that what their future desires could differ.
"I think a lot of people kind of want you to pick a label, stick to it, pick a journey, stick to it," Moore said. "I don't need to."
Tuck Woodstock has gone on and off testosterone 3 times in the past 1 1/2 years to relish in each stage of growth
Tuck Woodstock, a 29-year-old journalist, host of the " Gender Reveal" podcast , and cofounder of Sylveon Consulting , started testosterone in July 2020, four years after he came out as nonbinary to close friends and family.
As a gender educator, Woodstock knew testosterone was a resource for years before they made the decision to go on it.
"The reason that it took four years for me to start testosterone is because it took four years for me to want to start testosterone," Woodstock said. "It was very much, for me, an incremental journey where the way that I thought about my own gender inched very slowly away from womanhood."
Woodstock added: "Because that process was gradual, it took several years before I was interested in physical or medical transition, which I recognize is very different than most people I know who came out as trans nonbinary, trans men, and immediately started testosterone. That was not my experience at all."
In the past year and a half, Woodstock has stopped and restarted testosterone three times. This is partially because of being a podcaster and musician who relies on their voice heavily.
"When I hit a certain level of testosterone in me personally, it changes my voice so rapidly that it becomes harder to sing at all," Woodstock said.
In addition to giving their voice a break, Woodstock also wants to take time to relish the changes his body is going through while on testosterone and likes to take breaks.
"I think it's nice to take a moment and regroup because these changes often are at least semipermanent," Woodstock said. "And I like to make sure that I have a moment to spend in this version of my body before I progress on to a later version. It's not so much that I don't want them to actualize but that I want to enjoy every single moment of this journey individually."
Kayden Coleman, 35, took testosterone for 5 years before pausing, then started taking it again
Kayden Coleman , a 35-year-old trans medical advocate and educator, started taking testosterone in 2009.
While he was really excited about the changes that happened in his first year on T, he said the weekly shot became more of a hassle, especially once certain changes, like hair growth and voice deepening, plateaued.
A post shared by Kayden X Coleman (He/Him) (@kaydenxofficial)
Coleman stopped taking testosterone twice. The first time was after a surgeon told him to before he underwent top surgery in 2013, though he has since learned that may not have been medically necessary . The second time was in 2019, when he moved states, briefly lost medical coverage, and became pregnant.
"With testosterone, that first year is like, you cannot wait to take your shot because all these changes. Then, you kind of get to where you are, and you're like, 'OK, I'll take it next week,'" Coleman said. "Or like me, you'll get needle anxiety and really put it off."
When he stopped taking testosterone, he said he didn't experience many negative effects. Because Coleman already had a full beard and low voice, which are permanent effects of testosterone, he said going off it didn't change many things physically.
But he said he felt a lot more emotional going off T.
"When I'm not on testosterone, I'm like all over the place," Coleman said. "Testosterone kind of keeps me at a more level headspace."
Trans people don't have to get specific transition care to be valid
The way gender-affirming care is framed as a journey with a clear beginning and end point, Coleman said, harms trans people because it makes it seem like care needs to look the same for everyone.
"Trans people should feel free enough to start and stop hormones as a form of self-care," Coleman said.
"If I want to try for a baby, I should be able to," he added. "If I just don't feel like sticking myself in the thigh or butt cheek or arm or stomach with a needle for the next few weeks, I should just be able to not."
Watch: Medical treatments for transgender people in the US can cost over $100K, even with insurance. Here's why they're so expensive.
- Main content
Matador Original Series

#TravelingWhileTrans: How to Stay Safe While Seeing the World

As a nonbinary world traveler , each time I head through US airport security, I brace myself. How many times will I get misgendered? Will they send me back through the body scanner because they guessed my gender wrong?
These fears are mild, though, compared to what a lot of trans and gender-nonconforming people face while traveling. In fact, problems with harassment, issues with documentation, and concerns about hostile environments are often enough to keep trans and gender-nonconforming folks from hitting the road altogether.
However, don’t hang up your backpack just yet. With some extra research , preparation, and patience, traveling while trans is both possible and rewarding.
1. Know where to go.
More and more information is available on LGBTQ travel, though much of it focuses on lesbian and gay folks. Before making your travel plans, do some research. When deciding where to go, check out laws regarding gender identity and sexual orientation in the countries you’re interested in. ( Equaldex also maps LGBTQ-related laws and includes state-level data for the United States.)
In addition, review the US State Department website for travel warnings and advice. Look up the countries you’re interested in, and find information specific to LGBTQ travelers under “Special Laws and Circumstances.”
While this doesn’t have to dictate where you go, you can at least know your rights and get an idea of what things might be like on the ground.
2. Look for LGBTQ-friendly travel providers.
While there aren’t a lot of trans-specific travel companies , those that cater to the lesbian and gay community are more likely to be trans-friendly, too. For travel in Europe and the US, the International Gay and Lesbian Travel Association , Expedia , and Purple Roofs can help you find LGBTQ-friendly accommodations and resources. For travel in Asia, Utopia Asia can be a good place to look for LGBTQ-friendly tour groups, guides, and activities.
In addition, do some digging in your city or country of choice. Local LGBTQ organizations often develop travel guides that might help you figure out where to stay and what to do.
3. Update your documents.
One of the biggest hurdles for trans and gender-nonconforming travelers is documentation. Not all states and countries allow trans people to change the gender marker on their passport, and for non-binary people, very few places offer a non-binary option at all.
If it’s possible, update your passport to reflect the name you use and your gender identity. If you can’t do this, try to make sure your passport and travel visa photos reflect your current appearance to avoid extra hassles.
If you’re traveling in the US and are worried about your documents not reflecting your identity, consider using this card as a discreet way to share with the TSA agent that you’re transgender.
4. Pack wisely.
Know how to appropriately pack needles, hormones, medicines, and other items, and be sure to review such information in each country you’ll be flying into and out of as rules can differ.
Think carefully about what you wear and/or pack in your carry-on. Items like packers and other prosthetics, while typically allowed, might be cause for extra screening. In the US, if you don’t want to deal with the body scanners, you can ask for a pat down (though many trans people have given me mixed reports on this). Or if it’s in your budget, consider applying for TSA Pre-Check , which typically only requires you to go through a metal detector.
5. Make a game plan to respond to misgendering.
On the bright side, in countries where the gender binary is relatively rigid, if your gender expression fits what people expect of men or women, you might be correctly gendered more than you’d think. For example, I bind my chest, wear men’s clothes, and have short hair, and when I traveled to East Asia, a lot of people thought I was a man.
Unfortunately, though, especially for those of us who are gender-nonconforming, misgendering might happen a lot. So make a plan for how you’ll respond.
For example, when I was traveling in India, major tourist sites used gender-segregated security checks, and in Thailand, speaking the language inherently requires the use of male and female gender markers. For those that are gender-nonconforming, do some research about what to expect, and decide in advance how you’ll respond to these binary gender options.
Regardless of where you are on the trans spectrum, think through what you can do to mitigate some of these issues. In hostels, reserve a single room with a private bathroom for more privacy, or if you’re uncomfortable in a single-gender space, get a bed in a mixed dormitory. You might also consider staying at international hotels that have nondiscrimination policies that include gender identity and expression.
6. Make friends.
Trans and queer people are everywhere, whether they’re out or not. Even in countries that criminalize homosexuality, you can still find active LGBTQ (and queer-friendly) clubs, bars, bookstores, and events. See if you can catch a Pride festival while you travel, or plan your trip around a queer or trans film festival, group tour , or conference. Dig around for queer bars and clubs online or in guidebooks, find out what’s happening in the local Time Out magazine , or consider finding new friends on Meetup .
A lot of these things you’ll have to look up for each city or country, but some you might be able to find through international programs and listings (like Utopia Asia ).
7. Be prepared to be flexible — and to educate others.
Some people at home and abroad conflate gender and sexuality, and gender norms can vary greatly from country to country. Be aware that not everyone will conceptualize these ideas in the same way you do, and try to be flexible when confronted with these differences. If you’re in a social situation where it’s safe to talk about these issues, consider using it as an opportunity for cultural exchange — educating your new buddies on your own experiences while learning about their perspectives. Try to keep an open mind — but don’t put yourself in a space where you’re unsafe (mentally, emotionally, or physically).
8. Enjoy the journey.
Bring your camera, write in a journal, and enjoy taking in the world around you. Despite all the fears and the possible problems, by doing your research, being prepared, and keeping an open mind, you can plan a journey that will be fulfilling, freeing, and fun .
Additional resources
- Know Your Rights
- Lambda Legal: Know Your Rights (US)
- National Center for Transgender Equality: Know Your Rights: Airport Security (US)
- TSA Recommendations for Trans Passengers (US)
- Egale Canada Human Rights Trust: Travelling Trans (Canada and International)
Travel tips and resources
- GLAAD Transgender Resources
- Go Abroad: LGBTQ Study Abroad Guide
- A Guide to Flying While Trans
- Trans and GNC Travel Bloggers
- everywhere all the time
- Interview with Trans Travel Blogger Aaron Edwards
More like this
Trending now, part of an engine apparatus fell off during a southwest flight sunday morning, where to sit on a plane to experience the least amount of turbulence, scammers are targeting people who complain about air travel issues on x, why you should absolutely wear your seatbelt when flying, according to a pilot and flight attendant, us travelers returning from edinburgh could soon save hours by skipping customs when they land, discover matador, adventure travel, train travel, national parks, beaches and islands, ski and snow.
- International edition
- Australia edition
- Europe edition

‘They just go to Thailand’: the long and costly wait for gender-affirming surgery in Australia
Transgender Australians seeking lower body procedures can go to just a handful of local surgeons. It means long waits, huge costs and difficult decisions
- Get our morning and afternoon news emails , free app or daily news podcast
T wo years ago, Kavitha Sivasamy, an articulate, elegant Canberra lawyer, began to face her fears about undergoing gender-affirming surgery. “It’s really scary to go through something so invasive,” she says.
Gender dysphoria had been causing “a lot of distress” in Sivasamy’s day-to-day life. “It can prevent you getting out the door, having and keeping a job, sustaining healthy relationships,” the 27-year-old says. “The list goes on.”
She embarked on a course of hormone replacement therapy, and she liked the physical changes she was seeing, but this meant her “genital dysphoria became more salient”. There was a disconnect between her aspirations for her body and how it looked in the moment.

But Australia is facing a shortfall in surgeons who perform lower body gender-affirming procedures. So , in a route that experts say more Australian trans people are taking, Sivasamy will travel to Thailand for surgery under a medical tourism company’s “one-month care package”. Like some others, she will access her superannuation to pay for the $30,000 procedure.
Sivasamy made her choice after spending many months researching the experiences that others had of surgery. She decided a peritoneal pull-through, adapted from a procedure pioneered in India on cisgender women born without a vagina, was the type of vaginoplasty with the most positive benefits for her.
The standard vaginoplasty has long been a penile inversion, where penis skin is refashioned as the lining of a new vagina. The newer method, using tissue from the patient’s peritoneum membrane in the abdominal cavity, is said to offer greater vaginal depth. However, there is a lack of data on post-surgical quality of life for trans patients.
Sivasamy had been referred to Dr Kieran Hart , a Canberra-based urologist who performs this procedure, but she soon learned that she might have to wait a year and a half to have the surgery here. The idea of delay only compounded her distress.
“Having overcome family, workplace and social barriers, why put the critical years of your 20s and 30s on hold because of the wait in Australia?” she says. She will fly to Bangkok in May.
One surgeon, 120 patients waiting
Only a handful of Australian surgeons offer lower body gender-affirming surgery such as vaginoplasty for trans women, with even fewer offering phalloplasty (penis creation) for trans men. No surgical college offers formal training guidelines, forcing doctors to learn overseas.
Trans health advocates say Medicare is “woeful” and failing to offer any item numbers for medical procedures specifically for gender incongruence, causing confusion about what, if any, aspects of gender-affirming surgeries are eligible for government subsidy.
Private health insurance coverage for gender-affirming surgery is often prohibitively expensive. Even a fully insured person is left out of pocket by up to $20,000 for a vaginoplasty performed in Australia.
An evidence brief prepared in 2021 by the New South Wales community health organisation ACON found that most states and territories have elective surgery policies that “explicitly restrict access to surgical interventions for trans people through public health systems”, forcing trans people into local private care or surgery abroad.
Dr Clara Tuck Meng Soo , a GP and the president of the Australian Professional Association for Trans Health (Auspath), says a lot of her patients “now don’t even bother to go on the waitlist; they just choose to go to Thailand”.
“We have very high rates of mental health harm , and this care and affirmation and support is critical to reducing that harm,” says Soo, who is a trans woman. “But shouldn’t we also be able to access care that we feel we need as a human right?”
Hart says he has 120 trans patients booked and waiting for gender-affirming surgeries, with another 70 scheduled for consultations, and estimates “probably 10 times more” trans people are waiting for surgery across Australia.

Hart has closed his bookings and will reopen them in the second half of this year for consultations to be held in 2024 – with potential surgeries months later.
However, he says he will expedite a surgery if a psychiatrist or family is worried a patient might not survive an 18-month wait. Transgender people have vastly higher self-harm rates than the general population – a 2021 study found 43% of trans Australians surveyed had attempted suicide .
Like others performing lower body gender-affirming surgeries in Australia, Hart came by training in the area by chance: he was taught by the late Phil Thomas at London’s Charing Cross hospital. Hart had only travelled there to train in prostate and bladder cancer surgery.
Based on follow-ups of how patients fared physically and mentally after the procedures, Hart is “convinced” that surgery “must drop the suicide rate”.
Over the past year, Hart’s workload increased in part because of the waves of referrals he was getting from two surgeons winding down their vaginoplasty procedures, including Melbourne plastic surgeon Andrew Ives . Until recently Ives a high profile in the field, but, as his office confirmed in an email, he ceased performing vaginoplasty and labiaplasty procedures at the end of 2022.
In February, Melbourne’s Monash Gender Clinic told patients that it was only then booking appointments for patients referred in August 2021, and that Melbourne plastic surgeon Cheng Lo , trained in vaginoplasty and labiaplasty by Ives, has “very long wait lists”. Cheng did not respond to interview requests.
Hart says: “Andy Ives and I were looking at doing a formalised training program [for gender-affirming surgery], and as he stepped back I’ve looked at doing it myself, but it’s a daunting task. The [Royal Australasian] College of Surgeons has been a bit slow on the uptake for it, like every facet of the transgender sphere.”
In May, the college will hold a scientific congress titled Equity in Surgery in Adelaide, including for the first time talks on transgender healthcare. The college’s president, Sally Langley, admits in the program that the college’s surgeons “have not fully represented the gender … composition of our community”, but declined an interview request.
The many kinds of risk
Sivasamy acknowledges there are “risks” in having surgery in Thailand, but says the country “pioneered a lot of these procedures”.
Travelling abroad for these surgeries, even to a country that has pioneered them, comes with warnings of caution. Soo mentions reports of trans women suffering vagina narrowing or urethra complications after surgery, both in Australia and overseas. The question is: once the patient is back in Australia, who corrects the error?
Hart says surgeons are reluctant to fix another surgeon’s mistakes: “It’s impractical coming from Perth to Canberra to have it fixed up, but it’s far more practical than getting to Bangkok. As a developed nation there’s no reason people should be going overseas.”
Soo says there is also a shortfall of GPs, psychologists and other practitioners in trans health, but evidence “shows if you provide gender-affirming care, be it hormone treatment, surgery and/or social affirmation, [trans] people have very good mental health virtually indistinguishable from cisgender peers”.
Associate Prof Nicola Dean, the president of the Australian Society of Plastic Surgeons, says the federal government must create a dedicated suite of Medicare rebate item numbers for procedures for people with gender incongruence. This would encourage more surgeons into the field, Dean says, giving the surgeries a “stamp of legitimacy”.
For instance, the Medicare item number for a mastectomy was created on the assumption the procedure would be for a cisgender woman with breast cancer. “So using it for a trans man having surgery [to affirm his identity] leaves the doctor feeling vulnerable about whether they’re allowed to use those item numbers,” Dean says.
“It leaves the patient vulnerable because they’re often not sure of the financial implications.”
Associate Prof Peter Haertsch , a Sydney-based plastic surgeon, says he continues to perform about six vaginoplasty procedures a year. At his peak he was performing 30 gender-affirming procedures a year in Australia, beginning in the late 1980s after training in London.
Heartsch says some Australian surgeons have recently exited the field, but he doesn’t know why. “I have tried and am still trying to get some form of help in the way of government funding,” he says.
Another Sydney plastic surgeon, Dr David Caminer, says he performed his first vaginoplasty on a trans person in 2015, after which he toured the US and Europe to watch surgical units perform gender-affirming surgeries.
Up to the end of 2022 he had performed only a few vaginoplasties on trans patients, mainly with the penile inversion technique. But Caminer says so far in 2023 he has performed seven vaginoplasties due to the growing demand. “It was really since Andy Ives stopped doing it that I’ve been inundated with requests,” he says.
The Brisbane-based Dr Hans Goossen , who did not respond to interview requests, performs nearly all the phalloplasty procedures on trans men in Australia, according to the various trans health advocates Guardian Australia spoke to. Another surgeon, the Melbourne-based Dr Gideon Blecher , “has trained in phalloplasty and he is still trying to establish the program in Melbourne”, a spokesperson for Blecher said.
Fiona Bisshop, a Brisbane-based GP and former president of Auspath, says phalloplasty is particularly difficult for trans men to access in Australia, costing more than twice as much as a vaginoplasty. Bishop says almost all phalloplasty procedures have some complication, but three of her trans male patients who went overseas had particularly “terrible outcomes”.
“You can have some very bad experiences over in Thailand,” she says. “There are communication difficulties: the surgeons and hospital staff don’t speak very much English.”

Bisshop says many of her trans patients have “given up on gender-affirmation surgeries, because it is completely out of financial reach”, and she calls the “lack of respectability” afforded to gender-affirming surgery a “vicious circle”, because it is not offered in Australian teaching hospitals where physicians would normally train.
Gender-affirming care
Sydney-based Teddy Cook , ACON’s director of community health, says gender-affirming care means many types of “health interventions of critical need”, and such needs must be “depathologised” and trans people given autonomy.
The lack of comprehensive gender-affirming healthcare in Australia may be because this care is misunderstood as simply cosmetic or solely related to genital surgery, and because trans people are “seen through a lens of being mentally ill, as opposed to just being a natural part of human diversity”, Cook says.
Cook, who is a trans man, says not all trans people seek surgical intervention: “It’s up to the individual what sort of steps they take medically, but cruel legal gender recognition laws in NSW and other states still force surgical sterilisation to update a birth certificate.”
Cook says no reliable figures exist on how many trans people there are in Australia to better plan health services. When unveiling a 10-year national action plan for LGBTQ+ health in March, the assistant health minister, Ged Kearney, said attorney general Mark Dreyfus “might have things to say” about counting LGBTQ+ people in the census, but no announcement has been forthcoming.
As Sivasamy readies for her flight to Thailand, she knows she is one of the lucky ones, not least because she has enough money at a young age to finance the trip.
“The majority of people my age don’t have the superannuation funds to get this done,” she says.
She then opens her palms and waves her hands away, as if to banish doubts about a lack of contingency plan after the procedure. “Definitely, if there’s a readmission surgery necessary, I don’t have the money for that, you know?”
She laughs. “I have no idea what would happen. We’ll just have to cross that route if we come to it.”
- Transgender
- LGBTQ+ rights
Most viewed

Transgender
The psychological impacts of gender-affirming hormone therapy, research shows psychological benefits to gender-affirming hormone therapy..
Updated October 23, 2023 | Reviewed by Devon Frye
- Find a therapist who understands gender identity
- Gender-affirming hormone therapy is associated with reduced mental health problems in transgender people.
- It's not clear if the improvement relates to chemical changes in the brain, improved body image, or both.
- The research has limitations, but current evidence is in support of gender-affirming hormone therapy.

According to the U.S. Census Bureau, about 2.6 million Americans identify as transgender , meaning their gender identity is different from the sex assigned to them at birth.
When transgender people seek medical therapy , they most commonly receive gender-affirming hormone therapy, which involves taking hormones to develop physical characteristics that better match their gender identity . Feminizing hormone therapy can trigger the development of breasts, help redistribute body fat to the hips and thighs, and lead to thinning of facial and body hair. Masculinizing hormone therapy can lead to a deeper voice, the redistribution of body fat away from hips and thighs, increased body and facial hair, increased muscle mass, and changes to the menstrual cycle.
While hormone therapy most obviously impacts physical traits, research shows it has significant effects on psychological and social well-being.
A systematic review published this year in the journal Nature Human Behavior takes a comprehensive look at the psychosocial effects of gender-affirming hormone therapy. This is the first systematic review of its kind, and it’s especially important because data show that people who are transgender experience mental health problems – including depression , anxiety , and social isolation – at much higher rates compared to the general population.
The review – conducted by researchers at Amsterdam University Medical Centers and the University of Exeter – pulls together data from 46 journal articles. The studies were based on interviews, comparisons of people who took hormones and those who did not, and analyses of those taking hormone therapy over longer periods of time.
The report clearly demonstrates that gender-affirming hormone therapy reduces depressive symptoms and psychological distress in transgender people. The report also found that gender-affirming hormone therapy helps transgender people in key areas of psychosocial functioning, namely self-control and trust.
After reviewing the body of evidence, researchers noted that hormone therapy most often leads to reductions in distress among people who are transgender, rather than increases in positive emotional states. That is, it is more likely to alleviate feelings of depression, sadness, and isolation rather than promote positive feelings.
The research does not provide a clear picture about whether the benefits of hormone therapy result from chemical changes in the brain or from improved body image and autonomy in appearance – or both.
There is some evidence that gender-affirming hormone therapy improves quality of life, but those results are complicated by emotional changes that occur during therapy. In many studies, participants taking masculinizing hormone therapy experienced dampened emotions. At the same time, participants taking feminizing hormone therapy reported more mood swings, emotional imbalances, and increased emotional expressiveness. The research does not paint of clear picture of how existing gender stereotypes affect people taking gender-affirming hormone therapy. But researchers do know that these variables factor into participants’ reports on their overall quality of life.
While the systematic review pointed to some strong conclusions, the report also highlights many gaps in the research on gender-affirming hormone therapy: it is difficult to identify adequate control groups for randomized, controlled studies; study sizes tend to be small; and the studies involve transgender people who volunteer to participate, which could skew results.
The take-home message? Despite the gaps in the research, the evidence is clear: Gender-affirming hormone therapy reduces depressive symptoms and results in improved psychosocial functioning for transgender people.

The Bronfenbrenner Center for Translational Research at Cornell University is focused on using research findings to improve health and well-being of people at all stages of life.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
- Travel Recommendations
- Travel in the US
- The Taste of Travel
- Tips & Tricks
- Travel Experiences

Transgender travel tips: A guide to flying while trans
From choosing a destination to finally taking off on your trip, navigating air travel can be a tricky undertaking, especially if you’re transgender. What might be a minor inconvenience for many can actually lead to a distressing experience for a trans person, especially as new technology and changes in the political climate influence the way we experience air travel. Frequent misgendering and differing cultural attitudes with regards to gender norms follow me whenever I fly (and they can definitely be taxing) but they certainly won’t stop me. And they shouldn’t stop you. Here’s a helpful guide to help you prepare for flying while trans.
Planning your trip
For trans people and people in the LGBTQ+ community at large, one of the first concerns on our minds as we choose a travel destination is safety. It’s always smart to do some research on the laws of the region you’re thinking of visiting and search for any local organizations or community groups that are trans-friendly. (Here’s a cheat sheet t o g e t y o u s t a r t e d ) . Right now in the United States, for example, 23 states have policies on gender identity that negatively affect trans individuals , but that doesn’t necessarily mean you should flat-out avoid these places. Just as it’s possible for trans people to have negative experiences in places deemed trans friendly, it’s also possible to have positive experiences in places deemed unfriendly.
The best way to ensure a positive experience is to do as much research and be as prepared as you can. Be ready for all parts of your trip, from the bigger aspects like knowing the norms and expectations of the culture you’ll be visiting, to the smaller details, like looking up the locations of gender-neutral bathrooms in the airports you’ll be passing through. The TSA has also compiled a PDF listing policies that might affect trans passengers , which can be a great reference while traveling. The more you know, the smoother your experience will be.
If you’re traveling with medical supplies like syringes, medications and hormones, make sure they’re all together in the same bag, each preferably in its original packaging, with proof that they were prescribed to you. Consider checking these with your luggage unless you’ll need them in the air. If you do choose to bring them in your carry-on, remember that doing so may flag you for additional screening. Items like liquid hormones, gel-filled breast forms and other prosthetics don’t need to meet the carry-on liquid limit as they are considered medically necessary. However, if you’re concerned about flying with liquid hormones as a carry-on but need them in the air, you might want to buy a sterile vial and fill it with what you need for the duration of your flight. (This could also be a good idea if you’re concerned about losing your luggage). Ask a flight attendant to chill them if necessary, or bring a thermos. If traveling with a prosthetic, make sure it has no metal parts. If you’re selected for additional screening, you have the right to be accompanied by someone you know and to be screened in private. If you have any questions about TSA policies regarding traveling with medical equipment, call the TSA Cares hotline before your flight at 1-855-787-2227 to speak with a trained representative.
Travel documents
Flying with the proper documentation can be tricky for trans travelers. The law dictates that the gender marker and name on your boarding pass must match the one on the government-issued photo ID you show the TSA agent, and that all passengers over the age of 18 must provide proof of identity both at check-in and at security. As the National Center for Transgender Equality states , “it does not matter whether your current gender presentation matches the gender marker on your ID or your presentation in your ID photo, and TSA officers should not comment on this.” For nonbinary travelers like me, most documentation does not match our identities, but that is slowly changing in some parts of the world. Canada could be the latest country to join the other seven that offer a third gender option on identification documents such as passports.
For passengers of all stripes, going through security can be one of the more stressful aspects of air travel, so it’s good to be prepared. However, TSA screenings are particularly unpopular with the trans community. In a 2015 survey by the National Center for Transgender Equality, 43 percent of trans people who went through airport security that year experienced at least one problem related to their gender identity or expression. Screening agents use Advanced Imaging Technology (or AIT) machines that passengers must pass through for the detection of dangerous objects. Before each passenger enters the machine, a TSA employee must press a blue “male” or pink “female” button on the machine so that their Automatic Target Recognition (ATR) software can detect “anomalies” not consistent with the passenger’s assigned gender, and the TSA agent is doing this by judging your gender presentation. The TSA has taken a lot of heat for using AITs with ATR software and maintain that their employees continue to receive sensitivity training in regards to screening trans passengers. Nevertheless, issues do occur, so here’s an idea of what to expect and how to handle any situations that arise.
As of March 2017, anyone who opts out of AIT screening will be required to undergo a Universal Pat-Down (UPD), which must be performed by someone of the same gender and can be done in private or in the company of a witness of your choice with a second officer of the same gender present. TSA officers may also perform a UPD at random or if your belongings trigger an alarm. (This hold true even for TSA Pre-Check passengers.) While UPDs vary widely, they may consist of a head-to-toe search generally done with the back of the hand (though they can use the front of their hands, as they say, in “limited” cases) and can include “head coverings and sensitive areas such as breasts, groin and the buttocks,” according to the TSA website. You may be required to adjust clothing during the UPD, but Trans Equality reminds you that:
“Travelers should never be required to lift, remove, or raise an article of clothing to reveal a prosthetic item and should not be asked to remove it. This applies to binding items, breast forms and other prosthetics. If a TSA officer asks you to reveal a prosthetic item, ask to speak to a supervisor and calmly explain the situation.”
Any TSA officers performing a UPD should tell you what they will do before they do it and they’re supposed to ask you if you’d prefer to be frisked by a male or female officer. If they don’t, ask to speak to a supervisor. Another way of communicating with TSA officers discreetly is to present them with a pre-printed and filled out Notification Card , w h i c h they will immediately recognize. Additionally, before entering an AIT machine, feel free to tell the officer which button to push to avoid problems.
Reporting issues
As with any negative customer experience, if you have any issues with airline or TSA personnel, record the details of the interaction so you can report it later . And don’t forget to take care of yourself first, since the nature of flying while trans may trigger gender dysphoria for passengers. Most importantly, keep in mind that having a greater awareness of how to prepare, what to expect and what your rights are when traveling is powerful in itself. In fact, many trans passengers don’t experience any issues at all when flying, and we hope you don’t either. Following simple tips like arriving early, traveling in groups and documenting your experience can all make a world of difference in allowing yourself a smooth flight.
Interested in sharing your story, offering tips or learning more about other’s experiences? Check out the hashtag #TravelingWhileTrans on Twitter, and tweet us @Cheapflights with anything you’d like to add. For more information check out our blog about LGBTQ travel tips .
About the author
Explore more articles

- Airline fees
- Airport guides
- Low fare tips
- Terms & Conditions
California consumers have the right to opt out of the sale * of their personal information. For more information on how we securely process personal information, please see our Privacy Policy .
Do not sell my info ON
* The definition of "sale" under the California Consumer Privacy Act is applicable only to California consumers.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Long term hormonal...

Long term hormonal treatment for transgender people
- Related content
- Peer review
- Martin den Heijer , professor of endocrinology 1 2 ,
- Alex Bakker , transgender man with 20 years of experience taking hormonal treatment ,
- Louis Gooren , emeritus professor in transgender medicine 2
- 1 Department of internal medicine, VU Medical Center, Amsterdam, Netherlands
- 2 Center of expertise on gender dysphoria, VU Medical Center, Amsterdam, Netherlands
- Correspondence to M den Heijer m.denheijer{at}vumc.nl
What you need to know
Transgender people using hormone treatment need lifelong medical support and care. Hormonal treatment for gender dysphoria resembles hormone replacement therapy for people with hypogonadism.
Hormone treatment in transgender people is accepted to be safe and increases overall wellbeing in most people. The most common (though rare) side effects are venous thrombosis in trans women due to oestrogens and polycythaemia caused by androgens in trans men.
Some trans women will not have had their prostate removed and some trans men keep their ovaries. Be aware of the risk of cancer in these sites and think about the added risk of hormone supplementation.
The aim of hormone treatment in transgender people is to adjust their secondary sex characteristics to be more congruent with their experienced gender. Hormone treatment for transgender people is usually initiated by specialist gender clinics, but some people start hormone treatment of their own accord without a prescription. With growing numbers of transgender people presenting to healthcare services (estimated as 9.2 per 100 000 1 ), general practitioners, general endocrinologists, and other doctors will become increasingly involved in their long term care, the prescription of hormones, and consideration of potential side effects. Several guidelines are available on the start of hormonal treatment 2 3 4 5 6 7 ; the focus of this article is the long term hormonal care for transgender people who might no longer attend a specialist clinic. It is aimed at a more general readership of physicians occasionally seeing adult transgender people.
Transgender terminology
Language and terminology are sensitive. Some terms used in the past are no longer appropriate because they might have negative connotations.
The term gender has historically been used to refer to psychological, behavioural, and sociological characteristics, and their categorisation by society as “masculine” or “feminine.” The term sex has historically been used to refer to biological characteristics similarly categorised. Transgender people stress the importance of proper language that respects their identity. Terms like male-to-female transgender or cross-sex hormonal therapy might therefore not be appropriate because they suppose a binary view. Even the distinction between gender and sex might be perceived as an oversimplification. Be sensitive to a person’s own use of terminology and interpretation of their identity. If in doubt, ask your patient what language they prefer.
Trans woman
A woman who was assigned male at birth.
A man who was assigned female at birth.
In this article we use these terms also for people who identify as non-binary transgender and wish for partial changes. Attending physicians should be aware of possible medical problems resulting from biological aspects of the sex at birth. For example, prostate cancer in a trans woman.
Non-binary/Gender-queer
The terms “non-binary” and “gender-queer” are used by people who do not exclusively identify as man or woman, masculine or feminine, male or female.
Anti-androgens
Agents antagonising testosterone action.
Anti-gonadotropics
Agents that inhibit secretion of luteinising and follicle stimulating hormones from the pituitary.
Hormone treatment in transgender people
Many transgender people seek to adjust their physique to be more congruent with their experienced gender by using hormone treatments and/or undergoing surgical interventions. The broad aims of hormone treatment in adult transgender people are to eliminate as far as desired the earlier hormonal effects of the sex steroids of their sex at birth and to induce the desired secondary sex characteristics of the experienced gender.
Hormone preparations that are used in transgender medicine for gender dysphoria are the same that are used in gonadal endocrinology, although they are usually not licensed for treating gender dysphoria in itself. Table 1 lists these preparations.
Hormones used in transgender persons with typical doses in adults (20-50 years)
- View inline
Hormones induce more than one effect. Oestrogens, for example, influence breast growth, bone density, skin, and the clotting system. Generally, it is not possible to selectively stimulate one effect and inhibit another. The effects of gonadal hormones can differ between persons because of the individual properties of the hormone receptors. Some people show a clear change in fat distribution pattern but little breast development, while in others the opposite occurs. In general, regular hormone treatment is needed for two to three years to reach its effect. 3
Hormone treatment for trans women
The key element in treating trans women is the administration of oestrogens. Guidelines recommend using the natural form 17 β-oestradiol because ethinyloestrogen (common in oral contraceptives) has been associated with a strong increase in the risk of venous thrombosis and cardiovascular disease. 8 Progestogens cause no additional feminisation effect when prescribed alongside oestrogens.
Anti-androgen
In some people, oestrogen administration only suppresses testosterone below the upper level of cis (ie, persons for whom their gender identity matches their sex at birth). To achieve full suppression in all people, most guidelines recommend the use of oestrogen in combination with a testosterone suppressing agent. 3 7 Testosterone suppressing agents (or anti-androgens) of several pharmacological classes are available ( table 1 ). GnRH agonists are effective but more expensive (€100-150 per month). They are first line treatment in the UK. Cyproterone acetate combines anti-androgenic and anti-gonadotropic effects and is widely used in continental Europe. Spironolactone is an aldosterone antagonist with anti-androgenic properties and is used as anti-androgen primarily in the US. A recent study showed comparable effect of GnRH analogues instead of cyproterone acetate in suppressing testosterone levels. 9 If trans women have undergone orchidectomy (as part of the surgical reassignment), anti-testosterone treatment could be stopped.
Clinical effect
Important effects of combined oestrogen and anti-testosterone treatment include breast development, softer skin, loss of sexual hair growth, increase in fat mass, broader hips, a decrease of lean body mass, and a decrease or change in libido with clinically relevant mood changes. 7 Not all effects are as strong in every person. Sometimes, additional measures are needed to achieve the desired effects, such as laser and electrolysis to remove unwanted hair, or breast augmentation to achieve sufficient breast volume.
Hormone treatment for trans men
Testosterone.
In trans men, testosterone is the key hormone administered and no anti-oestrogens are needed. 6 Testosterone is converted to oestradiol (by aromatase activity in fat cells) in men and women and oestradiol plays an important role in bone physiology in cis men and trans men. 10
Important effects of testosterone are an increase in lean body mass and muscle strength, body and hair growth in a male pattern, and lowering of the voice. Testosterone supplementation given in the doses in table 1 leads to cessation of monthly periods. If uterine bleeding persists, a GnRH agonist or progestin (lynestrenol 5 mg daily or medroxyprogesterone 10 mg three times daily or another progestin) could be added to stop uterine bleeding.
Principles of dosing
Most guidelines state that dosing of hormones should be guided by blood levels of oestradiol and testosterone, based on mean levels of the desired gender. These levels are often achieved with the dosages mentioned above; however, hormone levels are not a goal in themselves. The primary goals are usually a degree of feminisation or masculinisation as specified by the patient, which are achieved with their fullest effects after two to five years, similar to the temporal pattern of hormonal puberty. After this period, the goal for hormonal treatment—especially if in the meantime the gonads have been removed—might be to avoid signs and symptoms of hypogonadism such as mood changes, fatigue, osteoporosis, and muscle weakness. While dosage advice and target levels are an aid to avoiding underdosing and overdosing, one should be aware that, due to hormone receptor properties, similar levels can have different biological effects in different individuals, and different individuals can have different ideas about the desired outcome. In other words: the clinical effects and wellbeing of the trans person are paramount, not the hormone levels themselves. This applies also to persons who do not fit in the male/female distinction (non-binary or gender queer). It is possible to achieve hormone levels that are in between male and female reference ranges for both testosterone and oestradiol, but it is important to avoid hypogonadism in patients that already have gonadectomy in order to prevent bone loss and other consequences of hypogonadism.
How well does it work and how safe is it?
It has been shown that hormone treatment in transgender people with gender dysphoria increases wellbeing in most people. 11 12 13 From a medical point of view, hormonal treatment seems to be acceptably safe. 14 15
Oestrogens increases the risk of venous thrombosis, but a study in trans women showed that long term treatment with oestrogen yields only a low thrombotic risk (one event in 1,286 person years). 16 Oral oestradiol supplementation has a more prothrombotic effect than parenteral oestradiol supplementation; therefore it might be recommended to use parenteral supplementation in people with a higher risk for venous thrombosis (ie, family history of thrombosis or age over 50). 17
Testosterone-blockers can have their own side effects, such as hyperprolactinaemia 18 and an increased risk for meningioma with cyproterone acetate (although still very rare), 19 and high potassium levels with spironolactone.
Testosterone supplementation increases the haematocrit into the male reference range and can sometimes lead to polycythaemia 20 ; therefore monitoring haematocrit is recommended every three months in the first year and them one to two times per year. 3 Liver toxicity of testosterone has been described but is rare, and no liver function tests are recommended. 3
Bone and cardiovascular disease
Bone density can be affected, but both testosterone and oestrogen in recommended dosages lead to an increase in bone density. 21 22 In general, oestradiol for trans women has a beneficial effect on cardiovascular risk factors, while testosterone for trans men has a detrimental effect. 23 But limited experience points in the opposite direction for cardiovascular disease itself: an increase in cardiovascular disease in oestrogen users (particularly ethinyl oestradiol) and decrease in testosterone users. 24 No clear explanations for this paradoxical finding are available yet.
Malignancies
Cases of cancer of the prostate and breast have been reported but recent studies showed no increased overall risk, although the estimated breast cancer risk in trans women is 33 times higher compared with cis men. 25 26 27 28
However, much of what we know about the effects of hormone treatment in transgender people is from relatively small studies ( table 2 ). Large, well designed studies, particularly in ageing subjects, are urgently needed to collect reliable estimates on effects and side effects.
Possible areas of concern in the long term follow-up of transgender persons on hormonal treatment and practical recommendations
Long term follow-up
Hormone supplementation is in principle lifelong, and people benefit from regular (yearly or two yearly) supervision by a doctor with an understanding of transgender health and hormone prescription.
Follow-up might take place in a specialist gender clinic, or with a primary care physician or other generalist with sufficient training in hormonal supplementation. Long term follow-up would include checking the hormone levels in trans men and trans women and haematocrit in trans men at every visit (yearly or two yearly). Other measurements must be guided by risk factors of the individual, such as blood lipids in case of cardiovascular risk. If there are sex specific laboratory reference values, use the reference values of the person’s new gender. 30 An exception is bone density measurement. From puberty on there are sex specific increases in bone mineral density, and reference values of the sex at birth should be used for assessment of T and Z values.
Trans women can develop prostate cancer, and breast cancer can develop in minimal residual breast cells in trans men. It would be important to consider and discuss withdrawal of hormonal treatment in these situations. We advise following the local guidelines for population screening of the cis population according to the relevant anatomy present (either prostate, cervix, or breasts).
Transgender elderly
Sex hormones rise in puberty. There is a sharp drop at menopause in women and a more gradual decrease in men. Data are lacking on whether to follow these patterns in transgender people. Many transgender people prefer to continue hormone use. The side effects of prolonged supplementation at dosages that induce young adult levels are not well studied. In our view, it seems prudent to taper the dose at increasing age, but there are no clinical data to support or dissuade from this approach. It is important, therefore, to discuss this uncertainty with the person and frame it in a general discussion about their overall health. 31
Education into practice
How confident do you feel about discussing hormone treatment with trans people in your practice?
Are you aware of any resources that might support you with their longer term care?
What might you do differently as a result of reading this article?
How patients were involved in the creation of this article
Our author group includes a trans person. The review group included a trans person. AB was asked to join us as author to enhance the patient perspective. AB is trans man with 20 years of experience taking hormonal therapy. Our first version was extensively reviewed by five reviewers (including a trans person). Their comments helped us to improve the manuscript, especially in the use of sensitive phrasing.
How this article was made
A first draft was written by MdH and LG with focus on long term hormonal treatment. We performed a search in www.pubmed.gov with search term “transgender OR transsexual” and “hormones OR oestrogen OR testosterone,” which revealed 485 papers. We largely focused on papers that were published in English in the last five years. AB was asked to join us as author to enhance the patient perspective. Our first version was extensively reviewed by five reviewers (including a trans person) and the BMJ editor. Their comments were very helpful in improving and clarifying the manuscript. They helped us to broaden the scope to practices used in other countries as well.
Case Vignettes
A 66 year old trans woman comes to her general practitioner. She started oral oestradiol (4 mg daily) 10 years ago together with an anti-androgen (cyproterone acetate 50 mg daily). She decided not to have a vaginoplasty because of the risk of complications of her obesity (she has a body mass index of 40). Two weeks ago, she was diagnosed with a deep vein thrombosis of the left leg and she commenced warfarin. She now wonders if she should stop her hormone treatment.
To consider
It is widely believed that there is a relationship between oestrogens and venous thrombosis. However, most evidence is based on cis women that use ethinyl oestradiol in combination with a prostagen. Little is known about the thrombogenicity of cyproterone acetate, although the combination of ethinyl oestradiol and cyproterone acetate in cis women is associated with increased thrombosis risk. 32 In this trans woman we would advise that she switches the cyproterone acetate for a GnRH analogue. If she wants to continue the oestrogens we would advise that she switches to a transdermal method of application.
A 36 year old trans man comes for his biannual visit to his endocrinologist. He started testosterone injections (250 mg every two weeks) eight years ago. He is feeling well, works as a bus driver, and smokes 20 cigarettes a day. His blood tests show testosterone of 15 nmol/L just before the next injections. Haematocrit is 0.55.
The definition of polycythaemia in terms of haematocrit levels differs among guidelines, but 0.55 is high. Our first advice would be to quit smoking. Furthermore, a short-acting (2-3 week) course of testosterone injections gives high peak levels and is associated with higher haematocrit levels. Therefore, we would advise he switch to either a testosterone gel or a long acting testosterone injection.
This is one of a series of occasional articles on therapeutics for common or serious conditions, covering new drugs and old drugs with important new indications or concerns. The series advisers are Robin Ferner, honorary professor of clinical pharmacology, University of Birmingham and Birmingham City Hospital, and Albert Ferro, professor of cardiovascular clinical pharmacology, King’s College London. To suggest a topic, please email us at [email protected].
We have read and understood the BMJ Group policy on declaration of interests and declare the following interests: none.
Provenance and peer review: Commissioned; externally peer reviewed.
Patient consent not applicable.
- Reisner SL ,
- Tangpricha V ,
- Coleman E ,
- Bockting W ,
- Hembree WC ,
- Cohen-Kettenis PT ,
- Deutsch MB ,
- den Heijer M
- Asscheman H ,
- T’Sjoen G ,
- Lemaire A ,
- Cerpolini S ,
- Martelli V ,
- Battista G ,
- Seracchioli R ,
- Meriggiola MC
- Gorin-Lazard A ,
- Baumstarck K ,
- Gómez-Gil E ,
- Zubiaurre-Elorza L ,
- Elamin MB ,
- Garcia MZ ,
- Wierckx K ,
- Van Caenegem E ,
- Schreiner T ,
- Weinand JD ,
- Arnold JD ,
- Sarkodie EP ,
- Coleman ME ,
- Goldstein DA
- Mohammed K ,
- Abu Dabrh AM ,
- Benkhadra K ,
- Dekker MJHJ ,
- Timoner J ,
- de Abajo FJ
- Bachman E ,
- Travison TG ,
- Basaria S ,
- Wiepjes CM ,
- Gooren LJ ,
- Prescott S ,
- Morgentaler A
- de Mutsert R ,
- Twisk JWR ,
- Roberts TK ,
- Vasilakis-Scaramozza C ,
- Things to do
Explore > Company > News > Traveling While Transgender in 2020
Traveling While Transgender in 2020
UPDATE: This article was refreshed in June, 2020 with new information on updated TSA regulations, US state-licensed, non-binary identities, and more. A new link to the Orbitz LGBTQ Welcoming Hotels hub page was also added in February, 2021.
Mark Twain once famously said, “ Travel is fatal to prejudice, bigotry, and narrow-mindedness, and many of our people need it sorely on these accounts. Broad, wholesome, charitable views of men and things cannot be acquired by vegetating in one little corner of the earth all one’s lifetime. ”
By public acclaim, the evidence for this appears to be true, or at least it is so for those who have the wealth, privilege and social position to travel.
“Travel is fatal to prejudice” – Mark Twain
But what about those who are outside of the social mainstream, especially those whose gender identity might not match their original birth certificate designation or even the physical features of their face and/or body? For them, the enlightenment and joy of travel presents a host of difficult obstacles that most gender normative people have never considered.
As an American transgender woman myself who has traveled, both before and after transitioning, I’d like to share some of the experiences we face so that you, as a potential ally to our community, may both better understand and help to make our voyages as enjoyable as yours.
Transgender traveler concerns
Public travel today is a far more complicated experience than it was in the past. The needs for heightened security on public transportation, especially in the air and at sea, has led to very strict, invasive security measures that are an unpleasant annoyance for most folks, but can be profoundly humiliating to the trans community. We face such issues as:
1. TSA Advanced Imaging Technology (AIT) body scans that reveal our bodies in which many of us have so much shame
2. Aggressive, invasive and intimate TSA pat-down searches
3. Going through TSA checks with body prosthetics
4. Traveling with prescription hormone medications (especially injection supplies)
5. Traveling before our ID has been updated for name and gender
6. Getting misgendered (sometimes intentionally) by airline and hotel staff or TSA officers
7. Being forced to sit for an extended period of time next to someone who is overtly transphobic
8. Public humiliation or overt outing by TSA officers, travel services staff or hotel front desk staff
9. International (or domestic) travel to destinations where transgender people are not socially or legally accepted in their identified gender, especially when the travel is required for work
It doesn’t begin and end at the airport, either. Even taking road trips by car can be a source of deep worry over issues such as:
1. Traveling to/through a place that is hostile to trans people (by legislation or culture, both inside the US and international)
2. Having to visit public rest stops, stores, restaurants, and gas stations in unfriendly areas on road trips
3. Facing confrontations for using the public restroom of the gender in which we identify while traveling
4. Visiting potentially unwelcoming rural areas vs. the anonymity of large urban areas
5. Going to public swimming pools, saunas or into public changing rooms
6. Being confronted with verbal abuse and, all too often, unthinkable physical violence by intolerant, local people
7. Traveling for a variety of transgender surgeries where, on the return trip, we will appear/be different than when we departed
For the trans community, all these issues and more are significant obstacles to be prepared for, dealt with, and overcome, one at a time, over and over. You simply cannot know how much mental and emotional energy it takes for trans people to get ourselves ready to leave our safe space and venture out into the unknown. It can be excruciatingly hard.
How to cope as a trans traveler
But trans people need not abandon the personally enriching experiences of travel in their lives. While the safe world is quite a bit smaller for us, there are still places we can go and things we can do to both protect ourselves and our civil rights as traveling citizens.
1. Know your rights!
Review the TSA Transgender Policies webpage and install the FlyRights app on your mobile device.
2. Consider applying for TSA PreCheck membership
The TSA PreCheck application process runs a thorough background check on all applicants. As a result, the level of trust TSA has in TSA PreCheck-identified passengers is greatly elevated, and reportedly this benefits the process of transgender passengers passing through airport security with less hassle due to lessened scrutiny at the security gate. There is a cost for this, however. For a 5-year membership, it’s $85. The Trusted Traveler program includes TSA PreCheck and other pre-screening programs that can be bundled together to help assist international travelers shorten their wait to see Customs officers.
3. Remain positive, gracious and respectful while working with TSA officers
Be so at all times in your interactions. Calmly answer all reasonable questions directly. Never shout or threaten a TSA officer. Jokes are highly discouraged as well. The goal is to get through the security screening process safely and quickly with minimal hassle, then be on your way. If necessary, calmly ask for a supervisor if the interactions with TSA officers become unreasonable.
4. Consider self-identifying to the TSA as transgender
You may consider privately self-identifying as trans to a TSA officer before going through their millimeter wave advanced imaging technology screening booth (they choose between separate, binary-gender image screening settings and “unexpected anomalies” may raise a red flag, resulting in a more thorough, body pat-down search )
5. Opt-out of body scanning
You can opt-out of the AIT body screening and ask instead for a pat-down search.
6. Carry a TSA Notification Card
Consider carrying a TSA Notification Card if you carry prescribed, injection medications or wear a prosthesis .
7. Ask for a pat-down in private
If you are selected for a pat-down search, you can ask for it to be done in a private screening area with a witness or companion of your choosing.
8. Ask for a same-gender officer as you identify for a pat-down
You can ask for a TSA officer of the same gender as your gender identity to perform the pat-down search.
9. Let TSA know if you are wearing prosthetics
You may wish to self-identify if you are wearing prosthetics prior to a screening or pat-down. If you are asked to either show a prosthetic or a body part, or lift, raise or remove any clothing, ask for a supervisor. Note that if the prosthetic alarms in the screening, the TSA requires that you conduct a self-pat-down followed by an explosives test of your hands. If those results are positive, a more thorough pat-down will be conducted, but still under the same rules as above.
10. Politely correct accidental misgenderings
Politely correct a person who initially misgendered you by mistake. If you are repeatedly misgendered or are shown disrespect, calmly ask for a supervisor.
11. Ask for a TSA Supervisor
If need be, calmly ask to speak to a TSA supervisor at any time.
12. Ask for a private luggage check screening
If your carry-on baggage is selected to be opened, you may ask for a private screening.
13. Bundle all prescription medications & supplies in one bag
If you are packing prescription medications , including hypodermic needles and hormones, inside your carry-on bag, TSA regulations require you put them all together in a separate bag, preferably in their original packaging with prescription labels.
14. Gender presentation is not relevant to your ability to travel
How you present, gender-wise, is not relevant to your ability to travel. The only thing that is relevant is matching your ID documents’ name and gender marker to your reservations. The TSA cannot reject you for your gender presentation.
15. Update your ID photo
If necessary, consider updating your government photo ID with a current photo if you haven’t had a legal name change.
16. Update your legal IDs if you have legally changed your name
If you have legally changed your name and/or gender designation, follow up by updating your driver’s license, passport, and TSA PreCheck card with new personal identity data. Note that many US states have now begun enabling their citizens to select alternative gender designations to the binary options of female and male, and more are planning to follow suit. Also, at the time of this post update, a bill has been brought before the US Congress proposing that the US State Department allow alternative gender markers on US passports.
17. Make travel reservations using your legal name
Make your flight reservations in the name based on the legal ID documents you will bring to the airport for your flight. They must match, as required per law.
18. Make travel reservations using the gender marker on the ID you’ll use
Like with your name, you’ll need to make your flight reservations using the gender marker based on the legal ID documents you will bring to the airport for your flight. They must match. Note that per the TSA, there are several forms of identification you can use. This includes your REAL ID , a secure, state-issued identification (in some cases known as an enhanced driver’s license or EDL). But as noted in an earlier question above, some US States offer alternative gender markers beyond the binary, while US passports are still (as of this post update) only offered in binary gender markers. In addition, some airlines also accept alternative gender markers. So here’s the key to making this complex system work:
- Domestic only travel. If you are flying within the US only, you can use the gender marker listed on your REAL ID to book your flight. Present your REAL ID at airport security for your ID. The new deadline date for getting a REAL ID is October 1, 2021, so if you don’t get your driver’s license upgraded to a REAL ID/EDL by that time or you don’t bring another approved form of ID with you to the airport, you will not be allowed to get through security!
- International travel. If you are going to cross any international border, even Canada or Mexico, on your trip, you will be required to use your passport instead of a REAL ID, and thus be required to book your flight using the gender marker on your passport. Even if you have a US connection in the same trip, it’s still part of the international flight trip, and the passport supersedes the REAL ID.
19. Consider carrying medical letter for HRT & gender
You may opt to carry a copy of your medical letter for prescription hormone replacement therapy (HRT) and gender designation.
20. Consider bringing a medical letter for other medical supplies
If you are bringing dilators or syringes in a carry-on, it may be helpful to bring a letter of medical necessity.
21. Consider carrying your name change court document
You may also consider carrying a copy of your name change court order document. You might also consider carrying your old ID just in case.
22. How to file a complaint for mistreatment
If need be, you can file a civil rights complaint with the TSA and/or DHS immediately after the incident or as soon as possible afterward.
23. Stay at known LGBTQIA-friendly hotels
Stay at hotels and resorts that are explicitly LGBTQ friendly. Orbitz has a huge number of them in our lodging inventory, one of the largest LGBTQ-Welcoming hotel inventories in the travel industry , and that list continues to grow weekly.
24. Travel to known safe destinations for LGBTQIA people
Consider traveling to known LGBTQIA-safe country destinations , or known LGBTQIA-safe cities in North America .
For additional details, check out Know Your Rights: Airport Security by the National Center for Transgender Equality .
Advice for service workers who interact with trans travelers
So much of the above puts the onus on trans people to be compliant with and aware of the regulatory rules and laws as well as standing up for our rights against discrimination. However, for transgender allies and just kind-hearted people who work in government jobs in TSA, Customs, and law enforcement, as well as workers in the travel and hospitality industries, there are things you can do as well to help make our travel experience be so much easier. This includes:
- Be discreet about bringing public attention to someone who may be transgender.
- Avoid using gendered salutations, such as “sir”, “ma’am”, “Mr.”, “Ms.”, “gentleman” and “lady”, in your speech, especially if there is any possibility of perceived ambiguity in the person’s gender expression.
- Discreetly ask the traveler how they want to be identified (including their personal pronouns , name, salutations, etc.).
- Never ask a transgender person deeply personal questions about surgery, genitalia, medications, their “real” name, or anything else not relevant to their travel.
- For TSA: Proactively provide options to the traveler on who can do a pat-down search if one is needed.
- Treat transgender people with the same respect and dignity as you would any other person.
Ultimately, transgender travelers are just travelers. We travel because we have to be somewhere else and have to use public transportation facilities and services to get there. Along the way, we may have to visit the bathroom. This is no different than anyone else. If you show us the same respect and dignity that you expect from us, everything will be so much easier for everyone involved.
Travel can be such a positive, even life-changing, experience. In a perfect world, transgender travelers, like everyone else, would share another one of Mark Twain’s musings resulting from the amazing experience of travel: “ There is no unhappiness like the misery of sighting land (and work) again after a cheerful, careless voyage. ”
More Articles With Company
Practical Guidelines for Transgender Hormone Treatment
Adapted from: Gardner, Ivy and Safer, Joshua D . 2013 Progress on the road to better medical care for transgender patients. Current Opinion in Endocrinology, Diabetes and Obesity 20(6): 553-558.
- In order to improve transgender individuals’ access to health care, the approach to transgender medicine needs to be generalized and accessible to physicians in multiple specialties.
- A practical target for hormone therapy for transgender men (FTM) is to increase testosterone levels to the normal male physiological range (300–1000 ng/dl) by administering testosterone.
- A practical target for hormone therapy for transgender women (MTF) is to decrease testosterone levels to the normal female range (30–100 ng/dl) without supra- physiological levels of estradiol (<200 pg/ml) by administering an antiandrogen and estrogen.
- Transgender adolescents usually have stable gender identities and can be given GnRH analogs to suppress puberty until they can proceed with hormone therapy as early as age 16.
Hormone regimes for transgender men (female to men, FTM)
1. Oral
- Testosterone undecanoate* 160–240mg/day
2. Parenterally (i.m. or subcutaneous)
- Testosterone enanthate or cypionate 50–200mg/week or 100–200mg/2 weeks
- Testosterone undecanoate 1000 mg/12 weeks
3. Transdermal
- Testosterone 1% gel 2.5 – 10 g/day
- Testosterone patch 2.5 – 7.5 mg/day
i.m., intramuscular. *Not available in the USA.
Monitoring for transgender men (FTM) on hormone therapy:
- Monitor for virilizing and adverse effects every 3 months for first year and then every 6 – 12 months.
- Monitor serum testosterone at follow-up visits with a practical target in the male range (300 – 1000 ng/dl). Peak levels for patients taking parenteral testosterone can be measured 24 – 48 h after injection. Trough levels can be measured immediately before injection.
- Monitor hematocrit and lipid profile before starting hormones and at follow-up visits.
- Bone mineral density (BMD) screening before starting hormones for patients at risk for osteo- porosis. Otherwise, screening can start at age 60 or earlier if sex hormone levels are consistently low.
- FTM patients with cervixes or breasts should be screened appropriately.
Hormone regimes for transgender women (male to women, MTF)
1. Anti-androgen
- Spironolactone 100 – 200 mg/day (up to 400 mg)
- Cyproterone acetatea 50–100mg/day
- GnRH agonists 3.75 mg subcutaneous monthly
2. Oral estrogen
- Oral conjugated estrogens 2.5–7.5mg/day
- Oral 17-beta estradiol 2–6mg/day
3. Parenteral estrogen
- Estradiol valerate 5–20mg i.m./2 weeks or cypionate 2–10mg i.m./week
4. Transdermal estrogen
- Estradiol patch 0.1–0.4mg/2X week
i.m., Intramuscular; MTF, male to female. aNot available in the USA.
Monitoring for transgender women (MTF) on hormone therapy:
- Monitor for feminizing and adverse effects every 3 months for first year and then every 6– 12 months.
- Monitor serum testosterone and estradiol at follow-up visits with a practical target in the female range (testosterone 30 – 100 ng/dl; E2 <200 pg/ml).
- Monitor prolactin and triglycerides before start- ing hormones and at follow-up visits.
- Monitor potassium levels if the patient is taking spironolactone.
- BMD screening before starting hormones for patients at risk for osteoporosis. Otherwise, start screening at age 60 or earlier if sex hormone levels are consistently low.
- MTF patients should be screened for breast and prostate cancer appropriately.
3. Leinung MC, Urizar MF, Patel N, Sood SC. Endocrine treatment of transsexual * persons: extensive personal experience. Endocr Pract 2013; 19:644 – 650.
4. Gorin-Lazard A, Baumstarck K, Boyer L, et al. Is hormonal therapy associated *with better quality of life in transsexuals? A cross-sectional study. J Sex Med 2012; 9:531–541.
5. Obedin-Maliver J, Goldsmith ES, Stewart L, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. J Am Med Assoc 2011; 306:971 – 977.
6. Safer JD, Tangpricha V. Out of the shadows: it is time to mainstream treatment for transgender patients. Endocrine Pract 2008; 14:248 – 250.
7. Reiner WG, Gearhart JP. Discordant sexual identity in some genetic males with cloacal exstrophy assigned to female sex at birth. N Engl J Med 2004; 350:333 – 341.
8. Meyer-Bahlburg HFL. Gender identity outcome in female-raised 46,XY per- sons with penile agenesis, cloacal exstrophy of the bladder, or penile ablation. Arch Sex Behav 2005; 34:423 – 438.
9. Zhou J-N, Hofman MA, Gooren LJG, Swaab DF. A sex difference in the human brain and its relation to transsexuality. Nature 1995; 378:68 – 70.
10. Kruijver FP, Zhou JN, Pool CW, et al. Male-to-female transsexuals have female neuron numbers in a limbic nucleus. J Clin Endocrinol Metab 2000; 85:2034 – 204z
11. Berglund H, Lindstro ̈ m P, Dhejne-Helmy C, Savic I. Male-to-female transsex- uals show sex-atypical hypothalamus activation when smelling odorous steroids. Cerebr Cortex 2008; 18:1900 – 1908.
12. Rametti G, Carrillo B, Go ́mez-Gil E, et al. White matter microstructure in female to male transsexuals before cross-sex hormonal treatment. A diffusion tensor imaging study. J Psychiatr Res 2011; 45:199 – 204.
13. RamettiG,CarrilloB,Go ́mez-GilE,etal.Themicrostructureofwhitematterin male to female transsexuals before cross-sex hormonal treatment. A DTI study. J Psychiatr Res 2011; 45:949–954.
14. GreenR,NewmanL,StollerR.Treatmentofboyhood‘transsexualism’.Arch Gen Psychiatry 1972; 26:213–217.
15. Liao L-M, Audi L, Magritte E, et al. Determinant factors of gender identity: a commentary. J Pediatr Urol 2012; 8:597–601.
16. World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender nonconforming people. 7th ed.; 2011. http://www.wpath.org/documents/Standards%20of%20Care% 20V7%20-%202011%20WPATH.pdf (Accessed on 24 December 2012)
17. Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA, et al. Endo- crine treatment of transsexual persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2009; 94:3132 – 3154.
18. Gooren LJ. Care of transsexual persons. N Engl J Med 2011; 364:2559– 2560.
19. BhasinS,SaferJ,TangprichaV.Thehormonefoundation’spatientguideto the endocrine treatment of transsexual persons. J Clin Endocrinol Metab 2009; 94:.
20. Bockting WO, Miner MH, Swinburne Romine RE, et al. Stigma, mental health, * and resilience in an online sample of the US transgender population. Am J Public Health 2013; 103:943 – 951.
21. Olshan JS, Spack NP, Eimicke T, et al. Evaluation of the efficacy of sub-cutaneous administration of testosterone in female to male transexuals and hypogonadal males. Endocr Rev 2013; 34:(03_MeetingAbstracts): MON- 594.
22. Nagarajan V, Chamsi-Pasha M, Tang WHW. The role of aldosterone receptor antagonists in the management of heart failure: an update. Cleve Clin J Med 2012; 79:631 – 639.
23. Asscheman H, Giltay EJ, Megens JAJ, et al. A long-term follow-up study of mortality in transsexuals receiving treatment with cross-sex hormones. Eur J Endocrinol 2011; 164:635 – 642.
24. Wierckx K, Mueller S, Weyers S, et al. Long-term evaluation of cross-sex * hormone treatment in transsexual persons. J Sex Med 2012; 9:2641–2651.
25. Wallien MSC, Cohen-Kettenis PT. Psychosexual outcome of gender-dysphoric children. J Am Acad Child Adolesc Psychiatry 2008; 47:1413 – 1423. 26. Cohen-Kettenis PT, Delemarre-van de Waal HA, Gooren LJG. The treatment of adolescent transsexuals: changing insights. J Sex Med 2008; 5:1892–1897.
27. De Vries ALC, Steensma TD, Doreleijers TAH, Cohen-Kettenis PT. Puberty suppression in adolescents with gender identity disorder: a prospective follow-up study. J Sex Med 2011; 8:2276 – 2283.
28. Safer JD, Pearce EN. A simple curriculum content change increased medical & student comfort with transgender medicine. Endocrine Pract 2013; 33:39–44.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ther Adv Endocrinol Metab
Potential immunological effects of gender-affirming hormone therapy in transgender people – an unexplored area of research
Alice a. white.
Telethon Kids Institute, University of Western Australia, Nedlands, WA, Australia
Ashleigh Lin
Xander bickendorf.
Telethon Kids Institute, University of Western Australia, WA, Australia
Gender Diversity Service, Child and Adolescent Health Service, Nedlands, WA, Australia
Blake S. Cavve
Julia k. moore.
School of Psychiatry and Clinical Neurosciences, University of Western Australia, Nedlands, WA, Australia
Aris Siafarikas
Paediatrics, Medical School, The University of Western Australia, Nedlands, WA, Australia
Deborah H. Strickland
Jonatan leffler.
Telethon Kids Institute, University of Western Australia, Perth Children’s Hospital, 15 Hospital Ave., Nedlands, WA 6009, Australia
There are well-described sex-based differences in how the immune system operates. In particular, cisgender (cis) females have a more easily activated immune system; associated with an increased prevalence of autoimmune diseases and adverse events following vaccinations. Conversely, cis males have a higher threshold for immune activation, and are more prone to certain infectious diseases, such as coronavirus disease (COVID-19). Oestrogen and testosterone have immune-modulatory properties, and it is likely that these contribute to the sexual dimorphism of the immune system. There are also important immune-related genes located on the X chromosome, such as toll-like receptor (TLR) 7/8; and the mosaic bi-allelic expression of such genes may contribute to the state of immune hyperactivation in cis females. The scientific literature strongly suggests that sex-based differences in the functioning of the immune system are related to both X-linked genes and immune modulation by sex hormones. However, it is currently not clear how this impacts transgender (trans) people receiving gender-affirming hormonal therapy. Moreover, it is estimated that in Australia, at least 2.3% of adolescents identify as trans and/or gender diverse, and referrals to specialist gender-affirming care are increasing each year. Despite the improving social awareness of trans people, they remain chronically underrepresented in the scientific literature. In addition, a small number of case studies describe new onset autoimmune disorders in adult trans females following oestrogen use. However, there is currently minimal long-term research with an immunological focus on trans people. Therefore, to ensure the positive health outcomes of trans people, it is crucial that the role of sex hormones in immune modulation is investigated further.
For the purposes of this review, ‘sex’ refers to the genetic state of being male (XY) or female (XX). ‘Gender’ refers to the way in which people may identify as men, women, non-binary or other genders regardless of their phenotypic sex identified at birth. Individuals with a biological sex that is congruent with their gender identity are referred to as cisgender (cis), denoted as cis male or cis female. Whereas, individuals with a gender identity that is incongruent with their biological sex are referred to as transgender (trans). It is indicated where reference is made to trans people using the terms trans male or trans female throughout, according to the person’s self-identified gender: for example, a person, who is genetically XX, who identifies as male, is referred to as a trans male.
Introduction
The immune system is differently regulated in cis males and cis females. In general, cis females display stronger immune responses to infections and vaccinations than cis males. 1 This corresponds to reduced mortality from infectious disease, 2 but increased risk of side effects from vaccines in cis females. 3 As a result of a more easily activated immune system, cis females also display higher rates of autoimmune disease ( Figure 1 ). 4 For example, systemic lupus erythematosus (SLE) exhibits one of the strongest sex biases and is approximately eight times more common in cis females compared with cis males. 5 Contrastingly, the cis male immune system has a higher threshold for immune activation, resulting in increased infection-induced comorbidities, 6 , 7 elevated prevalence of some cancers 8 – 10 but lower risk of autoimmune disease. 6 The difference in immune regulation between cis males and cis females is likely multifactorial, and impacted by sex hormones and chromosomal makeup. 11 , 12 Cis females are genetically XX, with two copies of the X chromosome in every nucleated cell. To prevent excessive gene expression, one X chromosome is randomly inactivated so that cis females have the same complement of these genes as XY males. 13 However, chromosome inactivation is variable in cis females, which is referred to as ‘X-inactivation silencing’ and is thought to occur in approximately 15% of X-linked genes. 13 , 14 The X chromosome contains genes, such as toll-like receptor (TLR) 7, T-cell co-activator CD40 and T-cell transcription factor FoxP3, which are important for the regulation of immune function. 11 , 14 , 15 Altered expression levels of these genes through X-inactivation silencing may contribute to differential immune regulation between the sexes, however, this relationship is complex and remains incompletely understood. 16 In addition to this, both oestrogen and testosterone have significant immune-modulatory properties, as reviewed. 17 – 19 However, it is currently unclear how interactions between X chromosomes and sex hormones may affect the functioning of the immune system. This has special relevance for trans people on gender-affirming hormonal therapy; it is currently unknown whether they have altered immune function, susceptibility to infection or adequate responses following vaccinations. These may have important health implications and necessitates further research.

An overview of the difference in disease incidence between cisgender (cis) males and cis females, and the intersection with transgender (trans) people. To date, relatively little is understood regarding the incidence of immune-mediated disease in the trans people.
Transgender people
Gender-affirming hormonal therapy for trans people is diverse. It depends on the specific goals of treatment, and may involve medications to block or reduce the effects of endogenous sex hormones, as well as oestrogen or testosterone to feminise or masculinise the trans person. Despite the increasing appreciation that sex and gender are important biological variables, a systematic review of the literature determined that more than 60% of immunology papers omitted the sex of subjects. 20 Similarly, the experiences of trans people are chronically underrepresented in the scientific literature, despite the fact that this may be pertinent to providing gender-affirming hormones to trans people. As such, the long-term health outcomes of trans people receiving gender-affirming care remain poorly researched. 21 Important epidemiological data regarding trans people, including response to infection, prevalence of non-communicable diseases and susceptibility to autoimmune diseases, are unknown.
It is also worth noting that the existing published trans health research often includes outdated terminology, pathologises trans people, and often incorrectly uses pronouns and gendered language. This is directly contradictory to the increasing social acceptance and awareness of trans people and their experiences, and indicates that there is still a lack of understanding of gender diversity within the scientific community. Historically, research has been done on and not with trans people, and therefore, there is a strong need for trans health research that is respectful, collaborative and directly benefits the lives of trans people. 22
The human immune system is sexually dimorphic
The immune system has evolved to recognise a diverse range of pathogens while maintaining tolerance against self. 23 It comprises a complex network of cell subsets, cytokine cascades and signalling pathways, which orchestrates fast and effective clearance of pathogens. 23 Immune responses involve cross-talk with regulatory processes, so that, pathogens can be neutralised while avoiding side effects to the host. 23 In addition, the interplay between the innate and adaptive immune system is crucial for adequate immune function. Both of these branches of the immune system have specialised effector functions to create sustained immunological memory and prevent against reinfections. 23
Sex hormones modulate the immune system
Sex hormones control the reproductive system, and in recent years, there is a growing number of publications reporting their regulatory effects on the immune system ( Table 1 ). 7 Cells of both the innate and adaptive arm of the immune system express receptors for sex hormones, such as oestrogen and testosterone, eliciting variable responses depending on the stimulus, target cell and hormone concentration. 1 Oestrogen and testosterone are produced in both cis males and cis females, however, at substantially different levels. The majority of hormone receptors function as hormone-activated transcription factors that bind to DNA sequences called hormone response elements, to elicit gene expression. 18
A summary of the effects of oestrogen and testosterone on immune function. The impacts of these hormones are well documented in cisgender (cis) males and cis females, however, the potential effects of sex hormones on immune function in transgender (trans) people is relatively unknown.
AIRE, autoimmune regulator gene; AR, androgen receptor; CRP, C-reactive protein; IFN, interferon; MS, multiple sclerosis; SLE, systemic lupus erythematosus; PD-1, programmed death protein-1; PD-L1, programmed death ligand-1; TLR, toll-like receptor; TNF, tumour necrosis factor.
Concentration-dependent effects of oestrogens
Oestrogens, progesterone, luteinising hormone (LH) and follicle-stimulating hormone (FSH) are the predominant sex hormones in cis females. 24 Oestrogen is routinely used as gender-affirming therapy in trans females, and there is an increasing demand for access to progesterone as a combined hormone therapy. However, since there is currently limited research on the potential immune impacts of progesterone, this review will focus on the established effects of oestrogen on immune modulation. Oestrogen receptors (ERs), including ERα and ERβ, are widely expressed in the tissues of both cis males and cis females. 25 ER subtypes are variably expressed in immune cells, and signalling via these receptors is important for development of B cells, monocytes, dendritic cells (DCs) and natural killer cells. 1
Oestrogens have immune-activating effects, including promoting Th1 cell differentiation that produces pro-inflammatory mediators, such as interferon gamma (IFN-γ), modulating B cell activation 26 , 27 and regulating type I IFN responses in DCs. 11 , 28 These effects have all been linked to disease severity in autoimmune conditions, such as SLE. 29 – 31 During pregnancy, levels of oestrogens increase, and at those concentrations, oestrogens appear to instead have immune inhibitory effects. This may be associated with involution of the thymus that occurs due to the increased levels of oestrogen. 1 , 28 , 32 The physiological importance of this association is currently unclear; however, since the maturation of T lymphocytes generally occurs in the thymus, this may be related to the maternal tolerance of a foetus. 33 , 34 Increased oestrogen concentration is also associated with promoting Th2 immunity, which may also explain why some autoimmune diseases, such as multiple sclerosis (MS), which is a Th1-mediated disease, improve during pregnancy. 33
Androgens are important immune suppressants
Androgens are a class of steroid hormones including testosterone that have ‘masculinising effects’. 35
Testosterone is synthesised in different tissues in cis males and cis females. In cis males, testosterone is converted to the more biologically active form dihydrotestosterone by 5α reductase in the testes, or to oestradiol by aromatase. 36 In cis females, the conversion of testosterone to dihydrotestosterone occurs to a lesser extent, and conversion to oestradiol is the predominant pathway. Androgen receptors (ARs) have been characterised on immune cells, including neutrophils, macrophages, as well as B and T lymphocytes. 7 , 36 In general, testosterone has immune-suppressant properties, which may contribute to the higher threshold for immune activation in cis males. 6 Decreased levels of testosterone are associated with increased levels of inflammatory markers, such as C-reactive protein and tumour necrosis factor (TNF), and increased incidence of autoimmune disease, such as rheumatoid arthritis, SLE and MS. 37 – 39 Androgens have been shown to affect the functioning of neutrophils, and have broad suppressive effects on the activation of B- and T-cells, however, the molecular mechanisms remain incompletely understood. 40
Innate immune regulation mediated by sex hormones
DCs are crucial for the activation of T-cells, and orchestrate immune responses to both self and non-self-antigens. 25 Plasmacytoid dendritic cells (pDCs) express high levels of TLR7 and 9, and are specialised in producing large amounts of type I IFN following viral detection. 41 , 42 There are also sex-based differences in pDC function; cis females have been shown to produce higher IFNα levels compared with pDCs from cis males following TLR stimulation. 11 , 43 Studies in murine models found this to be dependent on ERα signalling in the pDC. 41 The relative expression levels of ERα and ERβ may hence be important for regulating inflammatory responses. 44 This is further exemplified by ERα/ERβ knockout experiments in SLE-prone murine models, where ERα appeared to protect male mice from disease development. 4 , 45 Findings from these studies have been corroborated in humans as lower ERα expression was observed in people with SLE compared with healthy controls. 28 , 44 , 46
Recent literature also suggests that cis females are more resistant to shock, trauma and sepsis-mediated immune dysfunction, and organ injury than cis males. 47 Since the incidence of sepsis in postmenopausal cis females increases to equivalent levels to age-matched cis males, the relative concentrations of sex hormones oestrogen and testosterone are likely to contribute to this sexual dimorphism. 47 Neutrophils are important first responder cells, and play a critical role in the early innate immune response. 48 Therefore, the hormonal modulation of neutrophils may explain the difference in sepsis susceptibility. From an experimental rat model, naïve female neutrophils were more resistant to activation by burn or trauma/haemorrhagic shock compared with those derived from males. 49 However, in male rats, testosterone seemed to potentiate neutrophil activation. 49 Neutrophil development also appears dependent on functional AR-signalling, 40 whereas, oestrogen induces more pronounced type I IFN gene signatures, 50 and increase neutrophil survival in cis females compared with cis males. 47
Sex hormones modulate adaptive immune function
B cells are responsible for the antibody-mediated immune responses including autoreactive responses. 51 Sex hormones have been shown to affect B cell function in vivo . Oestrogen protects autoreactive B cell populations from negative selection and this is thought to contribute to autoimmunity. 52 Oestrogen also promotes antibody production through Th2 polarisation at high oestrogen concentrations. 44 This is supported by detection of elevated serum immunoglobulin (Ig) A and IgG coinciding with an increase in oestrogen concentration before ovulation. 44 Moreover, oestrogen between periovulatory and pregnancy levels appears stimulatory to antibody production, but inhibitory to the production of B cell precursors between the pro-B to pre-B stages. 19 , 44
In general, cis males have a lower average number of circulating T lymphocytes compared with cis females; potentially due to increased testosterone-mediated T-cell apoptosis in males. 40 , 53 This finding is supported by studies of hypogonadal cis males where testosterone supplementation decreased the number of peripheral T-cells, and the relative proportion of regulatory T-cells (Tregs) increased. 36 The effects of oestrogen on T-cell development and function is more complex, and from previous studies appear to be dose-dependent. 54 – 57 The polarisation of naïve CD4 + T-cells is essential for effective adaptive immune responses. Th1-polarised T-cells drive cell-mediated immunity towards intracellular pathogens, and Th2-polarised cells induce antibody-mediated immunity. 57 , 58 Naïve T-cells may also be polarised to suppressive Treg lineages; 15 as well as Th9 and Th17 lineages that have both been related to immune-mediated disease. 59 – 63 Cytokines produced by Th1- and Th2-polarised cells reciprocally inhibit each other and a failure to produce a sufficiently polarised T helper cell immune response can result in immune pathology, such as autoimmunity or allergy. 64 Appropriately polarised CD4 + T-cells are crucial for efficient immune responses, and dysfunction in Th1/Th2 polarisation is thought to relate to immune hyperactivation in cis females and immune deficiency in cis males. 7
Impact of the X chromosome on immune function
The X chromosome encodes important immune-associated genes, including the AR and TLR7. 56 , 65 , 66 Since cis males have only one copy of the X chromosome, they are more sensitive to mutations in X-linked genes. 67 In cis females, up to one full X chromosome undergoes transcriptional inactivation in each cell to compensate for gene dosage. 14 Expression analyses of human genes demonstrate that approximately 15% of X-linked genes consistently escape X-inactivation silencing, resulting in variable biallelic expression. 14 It has been suggested that variation in the expression levels of these X-linked genes in cis females may contribute to autoimmune conditions, such as SLE, however, research in this area is conflicting. 11 , 16
Individuals with variations in the number of X chromosomes provide insights into the contribution of X chromosomes and gene dosage on the development of autoimmune disease. Cis males with Klinefelter syndrome have the genotype XXY, and have an increased risk of SLE development compared with XY cis males. 68 There is a limited body of research that suggests that the Y chromosome exerts changes on the CD4 + T-cell transcriptome, which may translate to altered T-cell activation. 69 This may have relevance for individuals with variation in Y chromosomes, 69 however, more research is required to validate this theory.
Conversely, cis females with Turner syndrome who are genetically XO may be at an increased risk of developing autoimmune diseases. 68 , 70 This is supported by a cohort study of patients with Turner syndrome, which found that 34.4% of patients were diagnosed with one autoimmune disorder. 71 The most commonly diagnosed condition in Turner syndrome patients was general thyroid autoimmunity (29.9%), with 14.9% diagnosed with Hashimoto’s thyroiditis. 71 It is hypothesised that the haploinsufficiency of X-linked genes that affect Treg development, such as FOXP3, may prevent Tregs from being able to supress autoimmune reactions. 71 Moreover, X-linked genes may contribute to the lack of self-antigen exposure in the thymus, contributing to the pathogenesis of autoimmunity. 71 , 72
Sex-specific immune modulation likely involves the contribution of both sex hormones and X-linked genes. However, it is difficult to determine the relative effects of these biological variables in cis people. Trans people taking sex hormone treatment uncouple these biological variables, and therefore provide important insights into the effects of sex hormones and X-linked genes. A recent study collected peripheral blood mononuclear cells (PBMCs) from a small cohort of trans volunteers and young cis females with Turner syndrome. 68 From an in vitro assay, their cells were treated with a TLR7/8 agonist, and the resulting production of type I IFN was determined. The results of this experiment suggested that TLR7/8-mediated type I IFN production was dependent on the number of X chromosomes and linked to serum testosterone concentrations. 68 These are important first steps towards understanding immune regulation in trans people.
Translation of immunological impact of sex hormones
Sex hormones impact risk and pathology of autoimmune disease.
Autoimmune diseases are complex and multifactorial in origin, influenced by environmental and genetic factors, hormonal makeup and individual immune system abnormalities. 5 The increased incidence of autoimmunity in cis females is mainly observed following puberty, suggesting that female sex hormones or relative low levels of testosterone may contribute to the sex bias. 64 , 73 , 74 The ability of B and T-cells to recognise antigens is crucial for protection against pathogens, however, when these cells react to self-antigens, immune pathology can arise. 7 Both B- and T-cells express receptors for sex hormones, and the specific interaction between these cell subsets is related to the pathogenesis of autoimmune diseases. 75
Sex hormones modulate the maturation of T-cells. The thymus is the key site for the development of a diverse repertoire of T-cells and maintaining central tolerance. 18 In the thymus, expression of self-antigens is regulated by the autoimmune regulator gene (AIRE), 76 which promotes expression of self-antigens resulting in negative selection of self-reactive T-cells. 76 , 77 There is increasing evidence that AIRE expression is modulated by sex hormones; testosterone has been identified to upregulate AIRE, 18 whereas, oestrogen has been shown to decrease AIRE expression, reducing the efficiency of thymic self-tolerance; 76 , 77 this may be a central mechanism driving the increased incidence of autoimmunity in cis females. 36 , 76 , 78
Tregs are immune regulatory cells that are crucial for maintaining the balance between effective immune activation and self-tolerance. 6 Decreased numbers of functional Tregs lead to failed self-tolerance and autoimmunity. 36 The number of Tregs increases in the presence of testosterone in vitro , 39 and cis males generally have higher circulating Treg levels compared with cis females. 36 The X-linked transcription factor FoxP3 is responsible for the differentiation and regulatory programme in Tregs; FoxP3 expression can be modulated by testosterone via direct AR binding to FoxP3 gene regulatory sequences. 36 This may be related to the increased number of FoxP3 + Treg cells following testosterone treatment. 36 FoxP3 expression is also regulated by oestrogen. 1 Combined with disease-specific immune regulation, the impact of sex hormones on autoimmune disease is therefore likely significant.
Systemic lupus erythematosus
SLE carries one of the strongest sex biases of autoimmune diseases, and is between 7 and 10 times more common in cis females. 5 SLE pathogenesis is heterogeneous and patients often display anti-nuclear antibodies against double-stranded DNA and histones. 79 Anti-nuclear antibodies are considered a hallmark of SLE as they are detectable in over 97% of cases. 79 However, anti-nuclear antibodies are not specific for SLE, and are also detectable in approximately 30% of healthy individuals. 79 SLE pathogenesis has been described as a dysregulated virus response where B cells and pDC are hyper-responsive to TLR7 and/or TLR9 stimulation, resulting in aberrant type I IFN production. 16 As previously discussed, this pathway is susceptible to both sex-specific X chromosomal and hormone influence related to TLR7 gene dosing, and oestrogen-mediated regulation of type I IFN production in pDC. 64 , 80 – 82 There is also clinical evidence that oestrogen contributes to SLE severity: a meta-analysis of SLE patients found a 25% increase in SLE ‘flares’ during pregnancy. 83 Moreover, the risk of developing SLE appears to be increased in cis females taking oestrogen-containing oral contraceptives and hormone replacement therapy. 29 , 84 Conversely, studies of oestrogen deprivation found a reduction in disease severity in cis female SLE patients. 1 The incidence of SLE also decreases sharply after menopause and is uncommon before the onset of puberty. 85 There are also several case reports that document spontaneous SLE in trans females following long-term oestrogen therapy. 84 , 86 Together these findings suggest that oestrogen-based gender-affirming therapy may contribute to the development of SLE in genetically susceptible individuals. 84
Systemic sclerosis
Systemic sclerosis (SSc) is a chronic autoimmune connective tissue disorder. 87 SSc is more common in cis females compared with cis males, however, cis males experience more severe disease. 88 SSc is characterised by vasculopathy, inflammation and excessive collagen production in the skin and organs. 87 Oestrogen and androgen concentrations have been related to the clinical phenotype of SSc; however, the literature has conflicting findings, and the relationship remains incompletely understood. 88 In cis male and female SSc patients, lower concentrations of androgens have been observed compared with healthy controls. 89 A recent study described three cases of trans females developing SSc after long-term oestrogen use. 87 Together, these findings suggest that oestrogen or the reduction of androgens may increase the risk of SSc development.
Multiple sclerosis
MS is a Th1-mediated autoimmune disease that causes chronic inflammation within the central nervous system. 38 , 90 Neuroinflammation coupled with relapsing–remitting attacks of demyelination and axonal damage, results in progressive neurological deficits and disability. 90 , 91 MS is two to three times more common in cis females; however, cis males with MS tend to experience a more severe disease phenotype and generally have a worse recovery from relapses. 92 , 93 Multiple studies have reported that up to 40% of cis males with MS display abnormally low levels of testosterone, compared with controls. 38 , 94 , 95 Low testosterone has been correlated with increased disability scores, 38 , 96 and recent studies have trialled the use of testosterone as a therapeutic for MS with varied outcomes. 38 Given that testosterone can cross the blood–brain barrier and acts directly on neurons, 97 it is possible that testosterone may be neuroprotective in MS. 38 , 94 , 96 However, more research is required to validate these findings and rule out confounders, since hypogonadism can be induced by chronic disease states. 38
In contrast to other autoimmune diseases, oestrogen appears to be ameliorating in MS. 90 For pregnant people with MS, it is well established that there is a strong decline in the risk of MS relapses in the third trimester, which coincides with the highest physiological oestrogen concentrations. 98 However, after delivery when oestrogen levels decline, post-partum relapses are relatively common. 90 Therefore, the hormonal shifts associated with pregnancy may promote an increase in anti-inflammatory Th2 responses. 96 This is supported by a small clinical trial of cis females with MS, which found that supplementation of oestriol at levels consistent with pregnancy reduced the number of gadolinium-enhancing lesions. 99 However, it is important to consider that there are several important immunological adaptations that occur during pregnancy to prevent rejection of the foetus, and more research in this area is required. 100 The increased cis female incidence of MS, may also be related to the impact oestrogen has on responses to Epstein–Barr virus (EBV) as recently reviewed. 101 In patients with relapsing–remitting type MS, the clinical symptoms are often associated with a comorbid chronic or recurrent EBV infection, and the presence of EBV-infected B cells in the central nervous system. 102
A hospital-based study investigated the incidence of MS in trans males and trans females, compared with cis males and cis females. Between 1999 and 2011, this study included 1157 trans females and 2390 trans males; with 4.6 million cis males and 3.4 million cis females in the reference cohorts. 103 From their results, trans females had an increased risk of developing MS with a risk ratio of 6.63 compared with cis females (four observed MS cases and 0.6 expected MS cases). Trans males displayed a risk ratio of 1.44 compared with cis males (five observed MS cases and 3.5 expected MS cases). 103 This suggests that altered levels of both oestrogen and testosterone may contribute to development and/or disease activity in MS. 92
Trans populations may have higher rates of anti-nuclear antibodies compared with cis populations
The detection of autoimmune disease in a preclinical stage is important for preventing immune-mediated organ damage. 104 However, many autoimmune diseases have similar and overlapping symptoms, which make early and accurate diagnosis challenging. 105 Therefore, it is important to investigate potential novel diagnostic biomarkers. As previously discussed, anti-nuclear antibodies may precede development of autoimmunity; a recent study observed that 36% of trans males and 31% of trans females were positive for anti-nuclear antibodies, compared with 13% in the cis male/female population, 106 which was lower than previously reported elsewhere. 79 Since the trans male/female groups consistently reported higher positivity for anti-nuclear antibodies compared with the cis group, this indicates that both oestrogen and testosterone may modulate endogenous control mechanisms. In summary, although autoimmune diseases are rare, given the contributing effects of oestrogen to disease development, they may pose a small but significant risk in genetically susceptible trans individuals, particularly to those on oestrogen treatment.
The role of sex hormones in allergic diseases
Allergic disease is the clinical manifestation of atopic and IgE-sensitised individuals, where exposure to exogenous antigens results in acute inflammation. 107 Allergic reactions are mediated by mast cell degranulation via IgE-allergen complexes, inflammatory mediators and pro-inflammatory cytokines. 107 There is a disproportionate representation of atopy and allergic disease in cis males before puberty and cis females after puberty. 108 It is well reported that cis male children exhibit higher rates of allergic asthma compared with cis females before puberty, however, following puberty, asthma prevalence and severity increases in cis females, and conversely decreases in cis males. 109 , 110 This suggests that testosterone may be protective in allergic disease, whereas oestrogen may aggravate allergic diseases, such as asthma. 110 In non-pregnant cis females, the levels of sex hormones fluctuate significantly throughout the menstrual cycle. 24 These are associated with variability in allergic reactions, and may influence the outcome of skin prick test results. 107
Trans individuals experience significant socioeconomic disparities, which may predispose to higher rates of chronic conditions, including asthma and allergic disease, compared with cis individuals. 111 There is a case report describing one trans female with significant past medical history of allergies and asthma; 111 subsequently upon initiation of oestrogen-based gender-affirming therapy, she experienced an increase in allergic manifestations and increased asthma exacerbations. 111 It is well documented that trans people face disproportionate barriers to accessing health care compared with cis people. 112 – 114 Since it is currently not commonplace for medical practitioners to receive training on trans health, many clinicians are often uninformed of a trans person’s specific needs and unable to provide appropriate recommendations for their care. 115 As a result, trans people are more likely to delay seeking medical attention, resulting in increased morbidity from poor asthma control, for example. 111 Asthma management in trans people may also be complicated by chest binding (to minimise breast appearance) which may result in symptoms that mimic or exacerbate asthma. 111 As sex hormones have a demonstrated effect on allergic disease, 110 , 116 this is an important issue to consider, particularly for atopic individuals as they initiate gender-affirming hormone therapy. Medical treatment for atopic disease may need to be adjusted as hormone levels change, to better manage atopic exacerbations in trans individuals.
Sex hormones impact cancer development and efficiency of immunotherapy
It is well established that cis males are more susceptible to developing cancer and haematological malignancies: the lifetime risk of developing cancer is one in two for cis males, and one in three for cis females. 8 Moreover, with the average lifetime risk of dying of cancer being one in three cis males and one in six cis females, cis males also experience a disproportionately high mortality from cancer. 8 , 9 , 117 Immune surveillance is crucial in preventing the development and progression of cancer and as mentioned above, this is strongly impacted by sex hormones. 10 Moreover, in some cancers, such as breast or prostate cancer, sex hormones directly impact pathogenesis; and therefore, gonadotropin-releasing hormone (GnRH) agonist drugs are routinely used to suppress the production of sex hormones. 118 , 119 However, there are also sex differences in the incidence of other cancers at both genetic and molecular levels, and many cancers have been shown to be both positively or negatively affected by sex hormones. 117 An examination of cancer incidence across age groups found that cis male children also had an increased susceptibility to cancers, 120 suggesting that not only sex hormones contribute to the discrepancy in incidence between cis males and cis females. 121 , 122
The ability of T-cells to recognise tumour-associated antigens is an important function of immune surveillance. 123 In particular, CD8 + cytotoxic T-cells secrete cytokines, such as IFNγ and TNF to produce potent antitumour immunity. 123 CD4 + T-cells have also been shown to improve tumour clearance through recognition of tumour neo-antigens, and an ability to modulate the tumour microenvironment. 123 However, cancer cells have the ability to modify the expression of their surface molecules and key antigens, to evade the immune response and foster an environment that supports the growth of a malignancy. 123 Interestingly, some of these pathways including the function of Tregs appear to be sex-specific. 124
Immunotherapeutic agents are used to increase the activation of the immune system to fight cancer cells through cell-mediated mechanisms. 123 These have improved treatment efficacy and reduced side effects compared with traditional treatments, which are toxic and have limited specificity. 123 Sex hormones have been identified as drivers of sex-based differences in immunotherapy outcomes. 123 In particular, oestrogen appears to modulate the efficiency of immunotherapy; therefore, it is crucial to further investigate the role of sex hormones in non-reproductive cancers, to maximise the effectiveness of treatment. 123 Immune checkpoint inhibitors have had remarkable success in patients with metastatic disease; however, there are also a large number of patients that do not respond to treatment, or develop toxicities (immune-related adverse events). 125 A small number of studies suggest that cis female cancer patients experience lower rates of treatment success from checkpoint inhibitors. 125 , 126 Since immune checkpoints, including the programmed death protein/ligand (PD-1/PD-L1) pathway, are modulated upstream by oestrogen, sex hormones may influence the sex disparity in treatment success. 127 There are also important sex-based differences in terms of local tumour invasion and metastatic spread that warrants further research. 128
Melanoma was previously considered a non-hormone-related cancer, however, epidemiological data strongly suggest that cis females have a survival advantage compared with cis males. 128 Moreover, following menopause declining oestrogen levels were correlated with a reduction in survival in cis females. 128 There is also increasing evidence that the disruption of oestrogen signalling via ERα and ERβ is related to cancer initiation. 128 This is supported by findings from clinical trials using ER antagonists including tamoxifen in combination with standard chemotherapy. When bound to ERα, tamoxifen has been shown to decrease cell proliferation; this is supported by a meta-analysis investigating the use of tamoxifen in advanced melanoma. 128 From nine randomised control trials, it was found that patients treated with tamoxifen were ‘more likely to respond to chemotherapy’. 129 However, since these trials exclusively recruited patients with advanced melanoma, there were overall no differences in mortality. 129
A review, investigating primary care in trans people, suggests that cancer is the least researched aspect of the global burden of disease in trans individuals. 130 However, a recent cohort study investigated the incidence of breast cancer in cis and trans individuals in the Netherlands. 131 This study determined that although breast cancer is rare in cis males, trans females taking gender-affirming hormonal therapy were at an increased risk of invasive breast cancer. Contrastingly, trans males taking gender-affirming hormones were at a decreased risk of breast cancer compared with cis females. 131 In this cohort, most of the tumours detected were oestrogen and progesterone receptor positive; and the breast cancer found in trans females was phenotypically similar to that detected in cis females. 131 Moreover, the observed decreased risk of breast cancer in trans males may also be attributed to some participants having had a gender-affirming mastectomy (top surgery). It is important to note that the absolute risk of breast cancer in trans people is low, and from this study the incidence of breast cancer in trans males and females was lower than the incidence in cis females. 131 Moreover, gender-affirming hormonal therapy has been shown to be safe and effective. 131 However, as it is established that oestrogen and testosterone contribute to development of hormone-sensitive reproductive cancers, including breast and prostate cancer in cis people; 132 it may be beneficial for trans people taking oestrogen or testosterone to be proactively screened for breast and prostate cancer, especially for those with a family history or genetic susceptibility.
Sex hormones influence the immune response to infectious disease
Sex-based immune differences impact susceptibility to bacterial and viral pathogens. 133 , 134 Effective defence against infectious diseases requires the coordination between the innate and adaptive arm of the immune system. 24 Following the detection of an infectious agent, the innate immune response initiates a series of non-specific reactions, initiated through highly conserved pattern recognition receptors (PRRs), such as TLRs. 135 PRRs recognise molecular motifs on pathogens, such as lipopolysaccharide on gramme-negative bacteria. 136 Following the innate response, the adaptive immune system generates highly specific responses to defend the host against pathogens. The coordination between B- and T-cell subsets is vital in the production of protective immunity from infectious diseases, to produce long-lasting immunological memory. 136 , 137
In general, cis males experience a higher incidence of infectious diseases compared with cis females, which has previously been attributed to weaker innate immune responses. 138 Some of this may be due to the variability in expression of the TLRs involved in viral recognition, such as TLR7 and 8. Like TLR7, TLR8 is expressed on the X chromosome, and performs a key role in anti-viral immunity. 139 Viruses can induce inhibitory pathways mediated by interleukin 10 ( IL-10) to evade immune surveillance, and successfully infect the host. 138 Increased IL-10 production has the effect of preventing the maturation of DCs, and activating suppressive immune cells, such as Tregs. 138 From an in vitro study, following influenza infection cis male PBMCs had a four-fold higher concentration of IL-10 compared with cis females, 138 whereas, cis females instead produced elevated levels of type I IFN. 138
HIV is an infectious disease where early intervention and management is crucial for preventing long-term morbidity and mortality from AIDS progression. 140 In general, cis female patients with HIV have a better prognosis than cis males. 141 , 142 It is theorised that sex hormones impact early infection viral load, and oestrogen may modulate the production of the HIV-1 reservoir, resulting in better disease outcomes in cis females. 142 HIV-1 single stranded RNA ( ssRNA) is recognised by TLR7 on pDCs, and as previously discussed TLR7 is differentially expressed in cis males and cis females resulting in significant sexual dimorphism. 143 Experiments of HIV-1-mediated TLR7 stimulation resulted in a significantly higher number of IFNα producing pDCs in cis females compared with cis males. 144 Therefore, the anti-viral functions of IFN stimulated genes may contribute to the higher immune activation of CD4 + and CD8 + T-cells during persistent HIV-1 infection in cis females. 144 In additional studies, cis females displayed higher HIV-1 transcription suppression in response to oestradiol, and subsequently higher reactivity following oestrogen receptor 1 (ESR-1) modulation. 145 Together, these findings suggest that ESR-1 is a critical regulator of HIV-1 latency. 145
Bacterial infections appear to be more common in cis males who experience a higher incidence of gastrointestinal and respiratory bacterial diseases and sepsis compared with cis females, whereas cis females are more prone to genitourinary tract bacterial infections. 146 This discrepancy has been long established, with studies from the late 60s observing that the mortality rate following Mycobacterium tuberculosis infection was lower in gonadectomised cis males compared with cis male healthy controls. 147 Contrastingly, the tuberculosis-associated mortality was 10-fold higher in ovariectomised cis females compared with healthy controls. 147 Together, these findings indicate that sex hormones influence the outcomes of bacterial infections in cis males and cis females. These results are also supported by more recent studies observing an increase in opportunistic infections following menopause in cis females. 147 Some of these effects are mediated directly by oestradiol, but depend on the ER subtype and specific tissue compartment that is involved in the infection. 146 It is also likely that this effect stems from differential responses in macrophages in regards to TLR expression, which appears elevated in cis females compared with cis males. 146 This would allow for an increased capacity to detect and eliminate pathogens.
It is important to note that although a biological difference in immune responses is observed between cis males and cis females, different susceptibility to infections may also be a result of behavioural and environmental factors that contribute to exposure. 133 Epidemiological data found that infections with Dengue, Hantaviruses and Hepatitis B and C are more common in cis males than cis females, and this may be explained by behavioural differences that cause higher exposure rates in cis males. 133 There are also other demographic variables, such as obesity, which are associated with impaired anti-viral immunity. 133
Published literature on the susceptibility to infectious disease between the sexes consistently fails to recognise the intersection with gender. Therefore, it is unclear how to extrapolate cisgender sex-based findings in the context of infection susceptibility in trans people. Currently, there is little data regarding the broad incidence of infectious disease in trans people, however, it has been reported that trans people have a higher incidence of HIV and sexually transmitted infections (STIs), particularly in trans females compared with the cis population. 148 Trans people have often experienced discrimination, stigma and health care provider ignorance in previous attempts to access medical care, which often results in hesitancy to seek out medical attention, which delays treatment. 114 These barriers have been reported to result in less frequent HIV/STI testing. 115 In an Australian national survey of sexual health clinics, it was found that the incidence of HIV was around 3.5% in trans males and 5.7% in trans females on first visit, which is significantly higher than 1.2% in cis individuals. 140 , 148 , 149 Given the role of sex hormones and the concerning finding of increased HIV prevalence in the trans population, this is an area that requires further research.
Sex hormones impact responses to COVID-19
With the emergence of COVID-19, there has been a renewed focus on sex-specific virus-induced morbidity. As with the related severe acute respiratory syndrome (SARS) virus, 150 the SARS-CoV-2 virus also displays a disproportionally higher morbidity in cis males compared with cis females. 151 , 152 COVID-19 is a highly heterogeneous viral illness with clinical severity ranging from a mild self-limiting respiratory syndrome, to multi-organ failure and cytokine storm that is associated with a high mortality rate. 153 Case data from Europe suggest that the cis male to cis female ratio of hospitalisations is around 1.5:1, with case fatality at 1.8:1 in unvaccinated individuals. 154 There is also an exponential relationship between age and infection mortality, starting at 0.01% at age 25 and increasing to 15% at age 85. 155 SARS-CoV-2 is an ssRNA virus, therefore infection by this virus stimulates TLR7 and produces type I IFN early in the infection cascade. It is thought that severe COVID-19 disease may be related to a failure in early activation of IFN signalling in cis males. 156 This is exemplified in a case study of four severe COVID-19 cis male patients, which identified loss of function variants in TLR7 in all four patients. 156 Another study of people with severe COVID-19 identified that IFN deficiency, and the presence of anti-IFN antibodies were all related to worse clinical outcomes. 157 – 159
Although it is established that cis males are at an increased risk of severe COVID compared with cis females, there is little data on how COVID-19 morbidity/mortality affects trans individuals. As severe COVID-19 infections have been linked to early TLR failure in cis males, 160 the variable bi-allelic expression of TLRs in trans males may offer more protection compared with cis males, however, more research in this area is required. From available data, it is clear that COVID-19 has disproportionately impacted trans individuals’ access to care; with gender services being labelled as ‘non-essential’ at many facilities, trans individuals have faced new barriers to receiving their regular care. 161 , 162 Despite the recent research efforts to categorise sex-based differences in the disease progression and outcomes of COVID-19, only a minority of countries/states report on COVID infections and mortality with more than two options for gender, and trans identity is not indicated in the data. The direct impact of COVID infection on trans individuals therefore remains largely unknown.
Sex hormones impact responses to vaccines
Vaccines are an important tool in preventing infectious disease. However, historically cis males and cis male-derived cells have been predominantly used for human health research. 163 Furthermore, until the 1990s, cis females of ‘childbearing’ age were routinely excluded from drug trials, since fluctuating levels of hormones were considered an undesirable extraneous biological variable. 18 This has resulted in an underappreciation of the effect of biological sex on vaccine responses. There is an accumulating body of research that demonstrates biological sex is an important predictor of immunisation efficacy: cis females overall display higher antibody levels and T-cell activation following vaccination. 2 , 3 However, cis females also experience more frequent and severe adverse reactions. 163 , 164
The measles–mumps–rubella (MMR) vaccine consists of three strains of attenuated virus, and is routinely given to infants. 163 A cross-sectional study of children over 15 years of age found that following vaccination, the rate of seroconversion was higher in cis females compared with cis males. 165 Regression modelling indicated that time of vaccination and being female were the two most important predictors for antibody persistence following vaccination. 165 Interestingly, a study of pre-pubertal children found that cis females only had a transiently higher level of anti-rubella antibodies 2–4 weeks post-vaccination compared with cis males, and this sex difference was not apparent at a 10-week follow-up. 166 Following this, in post-pubertal adolescents (14–17 years of age follow-up), cis females consistently displayed higher anti-rubella IgG titres than cis males of the same age. 166 This observation was not only specific for rubella, but was also observed following influenza vaccination; adult cis females generated antibody titres twice as high as cis males when administered a half or full dose of an inactivated influenza vaccine. 167 Moreover, studies of the pandemic H1N1 vaccine demonstrated that cis females produced higher amounts of IL-6 and antibody responses than adult cis males. 168 Together, these findings suggest that the onset of puberty and rise in sex hormone concentration is related to the observable sexual dimorphism in vaccine-induced antibody titres.
In the age of the COVID-19 pandemic, it is also important to consider sex-based differences in responses to COVID-19 vaccinations. In Australia, over 58 million vaccine doses have been administered to date, and > 95% of people over the age of 16 are fully vaccinated. 169 There is a small amount of sex-disaggregated data on COVID-19 adverse reactions, indicating that cis females account for a higher proportion of adverse reactions (70.9–76%) when compared with cis males (22.4–28.6%). 151 This is consistent with previous findings on vaccinations. However, so far, there is little data available on rates of COVID-19 vaccination and outcomes in trans people.
Transgender young people
There is an increasing appreciation in the scientific community that sex hormones are important for immune function, as summarised in Table 1 . Despite this, there is relatively little research regarding the immune function of trans people undertaking gender-affirming hormonal therapy. Moreover, there are currently no long-term studies on the health outcomes of trans young people. From a 2012 population-based study in New Zealand, the number of trans young people was estimated by self-report to be around 1.2% of adolescents. 170 More recently, a 2019 study of high-school-aged young people in Australia indicated that 2.3% identified as trans and/or gender diverse. 171 This trend also reflects an increase of referrals for specialist gender-affirming care in recent years. 172 However, some, but not all trans young people seek gender-affirming medical treatment.
Gender-affirming medical care in trans young people depends on the age of the young person, stage of biologically determined pubertal development (described as ‘Tanner staging of puberty’), 173 , 174 the young person’s wishes, parental consent and the young person’s capacity to consent. 114 , 175 Some young transgender adolescents seek GnRH agonist treatment in the early stages of puberty to suppress further pubertal development. Following a period of puberty suppression, the trans young person as an older adolescent may wish to commence treatment with gender-affirming hormones, including oestrogen or testosterone. 154 , 172 This has the effect of inducing secondary sexual characteristics that align with their gender identity, and in Australia this treatment may commence with parental consent, over the age of 16 or when the young person is found to have mature capacity to consent to this treatment. 175 – 177 Older adolescents may present after puberty is complete, seeking oestrogen or testosterone treatment without preceding puberty suppression. For young people who have significant gender dysphoria that request gender-affirming treatment, these treatments are considered potentially lifesaving and beneficial to quality of life. This is supported by national and international guidelines, standards of care, and an increasing number of observational studies. 172 , 178 – 184
In studies of cis populations, the onset of puberty has been linked to an increase in atopic disorders and autoimmunity in cis females, 68 this suggests a mechanistic relationship between an increase in oestrogen and the development of an immune-mediated disorder in genetically predisposed individuals. The impact of gender-affirming puberty suppression, anti-androgen treatment, oestrogen and testosterone therapy on immune system function in trans adolescents is currently unknown. Therefore, it is crucial that we have a more comprehensive understanding of the potential effects of these treatments, so that trans young people can make informed decisions regarding their own health care, and health care providers can tailor care to maximise wellbeing.
There is an increasing body of research aiming to understand the mechanisms by which the immune system differs in cis males and cis females. The immunological impact of sex hormones results in different disease susceptibility between the sexes, with relevance across a range of human diseases. Given the immune-activating properties of oestrogen, 4 , 54 it seems likely that oestrogen treatment may induce a lower threshold for immune activation in trans females. Therefore, trans females with a genetic susceptibility may be at an increased risk of developing disorders of immune hyperactivation, such as autoimmunity and allergy. 84 , 87 However, they may at the same time be at reduced risk of developing cancers due to more efficient immune surveillance. 185 As cis males produce less-efficient immune responses following vaccination; 2 , 3 , 163 trans males may experience less robust antibody-mediated responses and reduced protection from previous vaccinations. This is of renewed importance in light of the COVID-19 pandemic, where successful seroconversion following vaccination is highly effective in reducing COVID-related morbidity and mortality. 151 Moreover, the generalised immune suppressive effects of androgens 6 , 186 may result in trans males being more prone to infections. Given the clear role of the sex hormones oestrogen and testosterone as immune modulators, there is a need for continued research into the immunological impact of sex hormones, and identification of associated specific health care needs, to ensure the positive long-term health outcomes of trans people.
Acknowledgments
The authors would like to acknowledge funding from the Western Australian Future Health Research and Innovation Fund and the Department of Health and Channel 7 Telethon Trust through the WA Child Research Fund 2020/21 Programme.

Contributor Information
Alice A. White, Telethon Kids Institute, University of Western Australia, Nedlands, WA, Australia.
Ashleigh Lin, Telethon Kids Institute, University of Western Australia, Nedlands, WA, Australia.
Xander Bickendorf, Telethon Kids Institute, University of Western Australia, WA, Australia. Gender Diversity Service, Child and Adolescent Health Service, Nedlands, WA, Australia.
Blake S. Cavve, Gender Diversity Service, Child and Adolescent Health Service, Nedlands, WA, Australia.
Julia K. Moore, Gender Diversity Service, Child and Adolescent Health Service, Nedlands, WA, Australia. School of Psychiatry and Clinical Neurosciences, University of Western Australia, Nedlands, WA, Australia.
Aris Siafarikas, Telethon Kids Institute, University of Western Australia, Nedlands, WA, Australia. Gender Diversity Service, Child and Adolescent Health Service, Nedlands, WA, Australia. Paediatrics, Medical School, The University of Western Australia, Nedlands, WA, Australia.
Deborah H. Strickland, Telethon Kids Institute, University of Western Australia, Nedlands, WA, Australia.
Jonatan Leffler, Telethon Kids Institute, University of Western Australia, Perth Children’s Hospital, 15 Hospital Ave., Nedlands, WA 6009, Australia.
Declarations
Ethics approval and consent to participate: Not Applicable.
Consent for publication: All authors have consented for the manuscript to be published.
Author contributions: Alice A. White: Conceptualisation; Investigation; Writing – original draft.
Xander Bickendorf: Writing – review & editing.
Blake S. Cavve: Writing – review & editing.
Julia K. Moore: Writing – review & editing.
Aris Siafarikas: Writing – review & editing.
Deborah H. Strickland: Writing – review & editing.
Jonatan Leffler: Conceptualisation; Funding acquisition; Project administration; Supervision; Writing – review & editing.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was supported by the Western Australian Future Health Research and Innovation Fund and the Department of Health and Channel 7 Telethon Trust through the WA Child Research Fund 2020/21 Programme.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and material: Not Applicable.
What the trans care recommendations from the NHS England report mean
The report calls for more research on puberty blockers and hormone therapies.
A new report commissioned by the National Health Service England advocates for further research on gender-affirming care for transgender youth and young adults.
Dr. Hillary Cass, a former president of the Royal College of Paediatrics and Child Health, was appointed by NHS England and NHS Improvement to chair the Independent Review of Gender Identity Services in 2020 amid a rise in referrals to NHS' gender services. Upon review, she advises "extreme caution" for the use of hormone therapies.
"It is absolutely right that children and young people, who may be dealing with a complex range of issues around their gender identity, get the best possible support and expertise throughout their care," Cass states in the report.
Around 2022, about 5,000 adolescents and children were referred to the NHS' gender services. The report estimated that roughly 20% of children and young people seen by the Gender Identity Development Service (GIDS) enter a hormone pathway -- roughly 1,000 people under 18 in England.
Following four years of data analysis, Cass concluded that "while a considerable amount of research has been published in this field, systematic evidence reviews demonstrated the poor quality of the published studies, meaning there is not a reliable evidence base upon which to make clinical decisions, or for children and their families to make informed choices."
Cass continued: "The strengths and weaknesses of the evidence base on the care of children and young people are often misrepresented and overstated, both in scientific publications and social debate," read the report.
Among her recommendations, she urged the NHS to increase the available workforce in this field, to work on setting up more regional outlets for care, increase investment in research on this care, and improve the quality of care to meet international guidelines.
Cass' review comes as the NHS continues to expand its children and young people's gender identity services across the country. The NHS has recently opened new children and young people's gender services based in London and the Northwest.
NHS England, the country's universal healthcare system, said the report is expected to guide and shape its use of gender affirming care in children and potentially impact youth patients in England accessing gender-affirming care.

MORE: Lawsuit filed by families against Ohio trans care ban legislation
The debate over transgender youth care.
In an interview with The Guardian , Cass stated that her findings are not intended to undermine the validity of trans identities or challenge young people's right to transition but to improve the care they are receiving.
"We've let them down because the research isn't good enough and we haven't got good data," Cass told the news outlet. "The toxicity of the debate is perpetuated by adults, and that itself is unfair to the children who are caught in the middle of it. The children are being used as a football and this is a group that we should be showing more compassion to."
In the report, Cass argued that the knowledge and expertise of "experienced clinicians who have reached different conclusions about the best approach to care" has been "dismissed and invalidated" amid arguments concerning transgender care in youth.
Cass did not immediately respond to ABC News' request for comment.
Recommendations for trans youth care
Cass is calling for more thorough research that looks at the "characteristics, interventions and outcomes" of NHS gender service patients concerning puberty blockers and hormone therapy, particularly among children and adolescents.
The report's recommendations also urge caregivers to take an approach to care that considers young patients "holistically and not solely in terms of their gender-related distress."
The report notes that identity exploration is "a completely natural process during childhood and adolescence."
Related Stories

Biden administration OKs huge oil export terminal
- Apr 11, 2:08 PM

What happens inside the brains of teenagers?
- Apr 11, 10:03 AM

State sends bill to ban 1st-cousin marriages
- Apr 11, 5:37 PM
Cass recommends that pre-pubertal children and their families have early discussions about how parents can best support their child "in a balanced and non-judgemental way," which may include "psychological and psychopharmacological treatments" to manage distress associated with gender incongruence and co-occurring conditions.
In past interviews, U.S. physicians told ABC News , that patients, their physicians and their families often engage in a lengthy process of building a customized and individualized approach to care, meaning not every patient will receive any or every type of gender-affirming medical care option.
Cass' report states that evidence particularly for puberty blockers in children and adolescents is "weak" regarding the impact on "gender dysphoria, mental or psychosocial health. The effect on cognitive and psychosexual development remains unknown."

The NHS has said it will halt routine use of puberty blockers as it prepares for a study into the practice later this year.
MORE: Amid anti-LGBTQ efforts, transgender community finds joy in 'chosen families'
According to the Endocrine Society puberty blockers, as opposed to hormone therapy, temporarily pause puberty so patients have more time to explore their gender identity.
The report also recommends "extreme caution" for transgender youth from age 16 who take more permanent hormone therapies.
"There should be a clear clinical rationale for providing hormones at this stage rather than waiting until an individual reaches 18," the report's recommendations state.
Hormone therapy, according to the Endocrine Society , triggers physical changes like hair growth, muscle development, body fat and more, that can help better align the body with a person's gender identity. It's not unusual for patients to stop hormone therapy and decide that they have transitioned as far as they wish, physicians have told ABC News.
Cass' report asserts that there are many unknowns about the use of both puberty blockers and hormones for minors, "despite their longstanding use in the adult transgender population."
"The lack of long-term follow-up data on those commencing treatment at an earlier age means we have inadequate information about the range of outcomes for this group," the report states.
Cass recommends that NHS England facilities have procedures in place to follow up with 17 to 25-year-old patients "to ensure continuity of care and support at a potentially vulnerable stage in their journey," as well as allow for further data and research on transgender minors through the years.
Several British medical organizations, including British Psychological Society and the Royal College of Paediatrics and Child Health, commended the report's recommendations to expand the workforce and invest in further research to allow young people to make better informed decisions.
“Dr Cass and her team have produced a thought-provoking, detailed and wide-ranging list of recommendations, which will have implications for all professionals working with gender-questioning children and young people," said Dr Roman Raczka, of the British Psychological Society. "It will take time to carefully review and respond to the whole report, but I am sure that psychology, as a profession, will reflect and learn lessons from the review, its findings and recommendations."
Some groups expressed fears that the report will be misused by anti-transgender groups.
"All children have the right to access specialist effective care on time and must be afforded the privacy to make decisions that are appropriate for them in consultation with a specialist," said human rights group Amnesty International. "This review is being weaponised by people who revel in spreading disinformation and myths about healthcare for trans young people."
Transgender care for people under 18 has been a source of contention in both the United States and the United Kingdom. Legislation is being pushed across the U.S. by many Republican legislators focused on banning all medical care options like puberty blockers and hormone therapies for minors. Some argue that gender-affirming care is unsafe for youth, or that they should wait until they're older.
Gender-affirming medical does come with risks, according to the Endocrine Society , including impacts to bone mineral density, cholesterol levels, and blood clot risks. However, physicians have told ABC News that all medications, surgeries or vaccines come with some kind of risk.
Major national medical associations in the U.S., including the American Academy of Pediatrics, the American Medical Association, the American Academy of Child and Adolescent Psychiatry, and more than 20 others have argued that gender-affirming care is safe, effective, beneficial, and medically necessary.
The first-of-its-kind gender care clinic at Johns Hopkins Hospital in Maryland opened in the 1960s, using similar procedures still used today.
Some studies have shown that some gender-affirming options can have positive impacts on the mental health of transgender patients, who may experience gender-related stress.
Related Topics
- United Kingdom

$780M soccer stadium next to NY Mets home approved
- Apr 11, 3:34 PM

Firefighters rescue 10-year-old stuck in chimney
- Apr 11, 12:33 PM
ABC News Live
24/7 coverage of breaking news and live events
If Kansas also bans health care for transgender kids, families will have to travel far out of state
Missouri banned gender-affirming health care for minors, and Kansas could follow suit this spring. So families are forced to move to other states or travel hundreds of miles, sometimes with the help of a growing network of groups determined to make the care available.
If Kansas bans gender-affirming care for minors, Kansas City families with transgender children will be hundreds of miles from a doctor who could help them.
Kansas lawmakers stand poised to follow a conservative playbook that 24 states, including Missouri, already have used to outlaw treatments like puberty blockers and hormone therapy.
The Kansas Legislature passed a bill last week that would ban gender care for people younger than 18 and bar transgender youth already receiving treatment from continuing it in the state. Gov. Laura Kelly is expected to veto the legislation, but an override is plausible.
Families with trans kids on both sides of the state line watch with trepidation. If care options in Kansas go away, families in Missouri will also lose their nearest outlet for care.
Parents in both states will be forced to choose between discontinuing their child’s treatment or searching for it in a city elsewhere in the country.
“We’re already seeing families from Missouri traveling all the way to Seattle,” said Katy Erker-Lynch, executive director of PROMO , a St. Louis-based LGBTQ advocacy group.

One Kansas City parent, who asked not to be identified to protect his child, said his family would look for care in Colorado or Minnesota, which would become some of the closest options if Kansas shuts down.
But traveling is only an option for families that can afford to take time off work and pay for travel and hotels.
“If you are not financially privileged, your kid will suffer,” said a Lee’s Summit woman whose 18-year-old daughter is transgender.
Networks have sprung up across the country to get women to states, like Kansas, where abortion remains available after the U.S. Supreme Court struck down Roe v. Wade. Likewise, a network is taking shape to get children and adults to states that still allow gender-affirming care.
Proponents of laws to ban gender-affirming care for minors worry the treatment will harm children and cause physical changes they might later regret.
Gender-affirming care, which the Kansas bill would make illegal in the state, is widely endorsed in the medical community. Medical professionals consider it lifesaving for some people suffering from gender dysphoria, a condition that can develop when a person’s gender identity doesn’t match their biological gender.
It includes a range of treatments, from mental health care to medical treatments, like hormone therapy and surgery. Most major health care organizations, including the American Academy of Pediatrics, agree that the care is medically necessary for most transgender people.
Care for children starts with social changes — letting a child live as the gender that matches their gender identity. That could continue.

But other types of gender-affirming care such as puberty blockers, which pause physical changes associated with puberty, and, later on, hormone therapy would be inaccessible in Kansas and Missouri. Surgery in people younger than 18 is exceedingly rare.
The Overland Park mother of a 14-year-old transgender son said the child hasn’t started taking testosterone, the male hormone, but he will when his parents and doctors believe that level of care is appropriate.
The mother, who asked not to be identified to protect her son’s privacy, doesn’t know what she will do if that care is no longer available in Kansas. But to protect her son, who was suicidal before he began living as a boy, she said she will do whatever she has to to find it.
“We’ll continue to find ways to make sure he stays safe,” she said. “Even living in a different country would not be out of the plan.”

A 2023 survey by the Trevor Project, an organization focused on the mental health of LGBTQ youth, found that half of transgender young people have seriously considered suicide in the past year and nearly one in five has attempted suicide.
When someone takes steps to transition to the gender that matches their identity, the risk of suicide goes down, health experts said. Suicide risk also drops when a person’s gender identity and pronouns are acknowledged and supported at home and school.
But the opposite is true when political rhetoric seems to constantly take aim at transgender health care, said Katie Heiden-Rootes, an associate professor at St. Louis University who works with the university’s Transgender Health Collaborative .
“It introduces seemingly culturally acceptable rhetoric about LGBTQ people,” she said, “and can really embolden discrimination and bullying in a more open way, because it seems to be OK right now to say these things and talk about trans people this way.”
The frequent attempts in state legislatures to pass laws that would remove options for transgender care are even damaging to trans people living in states where laws support them, said Roz Gould Keith, whose support group organization, Stand With Trans , is based in Michigan but offers online support groups to people throughout the country.
“The anti-trans rhetoric that is prevalent across the country affects everyone and erodes self-esteem,” she said. “People feel that in general the country wants to erase their existence.”
A survey from SLU’s Transgender Health Collaborative found that the anti-trans laws and legislation in Missouri are pushing families with trans kids out of the state. The survey found that health care providers also want to leave.
The group said 40% of survey respondents who were parents of LGBTQ youth had considered leaving Missouri, where state legislators introduced 48 bills last year affecting LGBTQ rights — and passed two that were signed into law. This year, they introduced another 34.
Parents surveyed cited increased stress, mental health, safety fears and the political climate as the top reasons for wanting to leave the state.
One in three health care providers surveyed said they had considered leaving the state because of the LGBTQ climate. Losing health care providers who are already in short supply harms everyone, said Heiden-Rootes, an author of the survey.
“We already are a state with really high amounts of medically underserved areas,” she said.
Estimates by the Williams Institute at the University of California Los Angeles School of Law suggest 1.6 million people in the United States identify as transgender. About 300,000 of those are 13 to 17 years old — including 2,100 in Kansas and 2,900 in Missouri.
The Human Rights Campaign estimated at the end of last year that three in 10 transgender youth lived in states that had banned care.
When Missouri Gov. Mike Parson signed legislation banning gender-affirming care last year, many Kansas City families found providers just across the state line in Kansas. A Kansas ban would force them to states farther away, where waiting lists can stretch beyond a year.
The Kansas bill was amended to give children until Dec. 31 to stop current treatment, including puberty blockers, testosterone, estrogen or other medications related to gender transition.
Opponents decry the effort to make patients already getting treatment to stop.
“They want to force de-transition all of these kids,” said Susan Halla, board president of TransParent , a national support and advocacy organization based in St. Louis. “They really don’t understand what de-transitioning is going to do to these kids.”
Although Missouri’s law banning minor care included a grandfather clause, which was supposed to allow children already getting care to continue it, that didn’t prevent many children in the state from losing care. In September, the Washington University Transgender Center at St. Louis Children’s Hospital said it would no longer prescribe puberty blockers or hormones to minors.
The center said the Missouri law created “unsustainable liability for health care professionals and makes it untenable for us to continue to provide comprehensive transgender care for minor patients without subjecting the university and our providers to an unacceptable level of liability.”
The University of Missouri soon followed suit, leaving patients across the eastern and central parts of Missouri with few options. Halla said many families have chosen to travel out of state rather than stop treatment.
Since 2023, the Campaign for Southern Equality in North Carolina has been working to support families in states where gender care has been outlawed. The organization’s Southern Trans Youth Emergency Project works with a network of gender clinics around the country and has helped more than 600 families find care since the program started in response to Tennessee and Mississippi passing bans.
The group has distributed $416,000 in direct emergency grants to families of trans youth or trans individuals, covering the cost of traveling to reach a doctor and other expenses associated with traveling. It also connects people to an organization that works with volunteer pilots who will fly them to appointments that are farther away.
Sometimes, the group sets up a telehealth connection, so a family only needs to cross a state line and dial into an appointment rather than having to drive farther to an in-person appointment.
“It’s certainly not just Tennessee and Mississippi, as we thought it would be at the beginning of last year,” said Carolyn Jones, who oversees the program.
And as more bills, including legislation in Kansas and Missouri, were introduced this year, the tide of people seeking transgender care in the dwindling number of states where it is still legal will likely continue to rise.
New legislation that prohibits doctors from offering care or threatens parents who help their children get gender-affirming care is regularly being introduced.
Legal challenges to the laws are ongoing across the country, including in Missouri . Some have been successful.
Last summer, a federal judge struck down an Arkansas law — the first in the country to ban transgender care. But lawmakers in that state have since passed legislation that could create a de facto ban on the care by making it more difficult for providers to get malpractice insurance.
Groups fighting the laws banning gender-affirming care hope more legal challenges will be successful.
“We’re clinging on to hope, because that’s all we have right now,” Halla said. “And that (hope) is that these will be proven illegal. … It’s an overreach of government (to say) that parents and doctors who have trained medically for this can’t provide this to children.”
There could be reason to believe the wave of anti-trans legislation could be subsiding, Erin Reed, a journalist who tracks anti-LGBTQ legislation, reported in her blog last week. Georgia, for instance, ended its legislative session without passing any of the proposed bills.
“Often when asked by other journalists about ‘where this is all going,’ I would state that, ‘We have yet to see a bottom,’” Reed wrote. “That is no longer the case — it appears that we have actually found that bottom in several states across the United States.”
But Erker-Lynch said that, at least in Missouri, restrictions could still grow.
“This is a decades-long struggle,” she said.
This story was originally published by The Beacon Kansas City , a fellow member of the KC Media Collective.

- Share full article
Advertisement
Supported by
Youth Gender Medications Limited in England, Part of Big Shift in Europe
Five European countries have recently restricted hormone treatments for adolescents with gender distress. They have not banned the care, unlike many U.S. states.

By Azeen Ghorayshi
Azeen Ghorayshi reports on transgender health and visited the world’s first youth gender clinic in Amsterdam this fall.
The National Health Service in England started restricting gender treatments for children this month, making it the fifth European country to limit the medications because of a lack of evidence of their benefits and concern about long-term harms.
England’s change resulted from a four-year review released Tuesday evening by Dr. Hilary Cass, an independent pediatrician. “For most young people, a medical pathway will not be the best way to manage their gender-related distress,” the report concluded. In a related editorial published in a medical journal, Dr. Cass said the evidence that youth gender treatments were beneficial was “built on shaky foundations.”
The N.H.S. will no longer offer drugs that block puberty , except for patients enrolled in clinical research. And the report recommended that hormones like testosterone and estrogen, which spur permanent physical changes, be prescribed to minors with “extreme caution.” (The guidelines do not apply to doctors in private practice, who serve a small fraction of the population.)
England’s move is part of a broader shift in northern Europe, where health officials have been concerned by soaring demand for adolescent gender treatments in recent years. Many patients also have mental health conditions that make it difficult to pinpoint the root cause of their distress, known as dysphoria.
In 2020, Finland’s health agency restricted the care by recommending psychotherapy as the primary treatment for adolescents with gender dysphoria. Two years later, Sweden restricted hormone treatments to “exceptional cases.”
In December, regional health authorities in Norway designated youth gender medicine as a “treatment under trial,” meaning hormones will be prescribed only to adolescents in clinical trials. And in Denmark, new guidelines being finalized this year will limit hormone treatments to transgender adolescents who have experienced dysphoria since early childhood.
Several transgender advocacy groups in Europe have condemned the changes , saying that they infringe on civil rights and exacerbate the problems of overstretched health systems. In England, around 5,800 children were on the waiting list for gender services at the end of 2023, according to the N.H.S.
“The waiting list is known to be hell,” said N., a 17-year-old transgender boy in southern England who requested to withhold his full name for privacy. He has been on the waiting list for five years, during which time he was diagnosed with autism and depression. “On top of the trans panic our own government is pushing, we feel forgotten and left behind,” he said.
In the United States, Republican politicians have cited the pullback in Europe to justify laws against youth gender medicine. But the European policies are notably different from the outright bans for adolescents passed in 22 U.S. states, some of which threaten doctors with prison time or investigate parents for child abuse. The European countries will still allow gender treatments for certain adolescents and are requiring new clinical trials to study and better understand their effects.
“We haven’t banned the treatment,” said Dr. Mette Ewers Haahr, a psychiatrist who leads Denmark’s sole youth gender clinic, in Copenhagen. Effective treatments must consider human rights and patient safety, she said. “You have to weigh both.”
In February, the European Academy of Paediatrics acknowledged the concerns about youth gender medicine. “The fundamental question of whether biomedical treatments (including hormone therapy) for gender dysphoria are effective remains contested,” the group wrote. In contrast, the American Academy of Pediatrics last summer reaffirmed its endorsement of the care, stating that hormonal treatments are essential and should be covered by health insurers, while also commissioning a systematic review of evidence.
Europeans pioneered the use of gender treatments for young people. In the 1990s, a clinic in Amsterdam began giving puberty-suppressing drugs to adolescents who had felt they were a different gender since early childhood.
The Dutch doctors reasoned that puberty blockers could give young patients with gender dysphoria time to explore their identity and decide whether to proceed with hormones to ultimately transition. For patients facing male puberty, the drugs would stave off the physical changes — such as a deeper voice and facial hair — that could make it more difficult for them to live as women in adulthood. The Dutch team’s research, which was first published in 2011 and tracked a carefully selected group of 70 adolescents, found that puberty blockers, in conjunction with therapy, improved psychological functioning.
That study was hugely influential, inspiring clinics around the world to follow the Dutch protocol. Referrals to these clinics began to surge around 2014, though the numbers remain small. At Sweden’s clinic, for example, referrals grew to 350 adolescents in 2022 from around 50 in 2014. In England, those numbers grew to 3,600 referrals in 2022 from 470 in 2014.
Clinics worldwide reported that the increase was largely driven by patients raised as girls. And unlike the participants in the original Dutch study, many of the new patients did not experience gender distress until puberty and had other mental health conditions, including depression and autism.
Given these changes, some clinicians are questioning the relevance of the original Dutch findings for today’s patients.
“The whole world is giving the treatment, to thousands, tens of thousands of young people, based on one study,” said Dr. Riittakerttu Kaltiala, a psychiatrist who has led the youth gender program in Finland since 2011 and has become a vocal critic of the care.
Dr. Kaltiala’s own research found that about 80 percent of patients at the Finnish clinic were born female and began experiencing gender distress later in adolescence. Many patients also had psychological issues and were not helped by hormonal treatments, she found. In 2020, Finland severely limited use of the drugs.
Around the same time, the Swedish government commissioned a rigorous research review that found “insufficient” evidence for hormone therapies for youth. In 2022, Sweden recommended hormones only for “exceptional cases,” citing in part the uncertainty around how many young people may choose to stop or reverse their medical transitions down the line, known as detransitioning.
Even the original Dutch clinic is facing pressure to limit patients receiving the care. In December, a public documentary series in the Netherlands questioned the basis of the treatments. And in February, months after a far-right political party swept an election in a country long known as socially liberal , the Dutch Parliament passed a resolution to conduct research comparing the current Dutch approach with that of other European countries.
“I would have liked that the Netherlands was an island,” said Dr. Annelou de Vries, a psychiatrist who led the original Dutch research and still heads the Amsterdam clinic. “But of course, we are not — we are also part of the global world. So in a way, if everybody is starting to be concerned, of course, these concerns come also to our country.”
In England, brewing concerns about the surge of new patients reached a boiling point in 2018, when 10 clinicians at the N.H.S.’s sole youth gender clinic, known as the Tavistock Gender Identity Development Service, formally complained that they felt pressure to quickly approve children, including those with serious mental health problems, for puberty blockers.
In 2021, Tavistock clinicians published a study of 44 children who took puberty blockers that showed a different result from the Dutch: The patients given the drugs, on average, saw no impact on psychological function.
Although the drugs did not lessen thoughts of self-harm or the severity of dysphoria, the adolescents were “resoundingly thrilled to be on the blocker,” Dr. Polly Carmichael, the head of the clinic, said at a 2016 conference . And 43 of the 44 study participants later chose to start testosterone or estrogen, raising questions about whether the drug was serving its intended purpose of giving adolescents time to consider whether a medical transition was right for them.
In 2020, the N.H.S. commissioned Dr. Cass to carry out an independent review of the treatments. She commissioned scientific reviews and considered international guidelines of the care. She also met with young people and their families, trans adults, people who had detransitioned, advocacy groups and clinicians.
The review concluded that the N.H.S.’s standard of care was inadequate, with long waiting lists for access to drug treatments and few routes to address the mental health concerns that may be contributing to gender distress. The N.H.S. shuttered the Tavistock center last month and opened two new youth gender clinics, which Dr. Cass said should have a “holistic” approach, with more support for those with autism, depression and eating disorders, as well as psychotherapy to help adolescents explore their identities.
“Children and young people have just been really poorly served,” Dr. Cass said in an interview with the editor of The British Medical Journal, released Tuesday. She added, “I can’t think of another area of pediatric care where we give young people potentially irreversible treatments and have no idea what happens to them in adulthood.”
The changes enacted by the N.H.S. this month are “an acknowledgment that our concerns were, in fact, valid,” said Anna Hutchinson, a clinical psychologist in London who was one of the Tavistock staff members who raised concerns in 2018. “It’s reassuring that we’re going to return to a more robust, evidence-based pathway for decisions relating to these children.”
Some critics said that Europe, like the United States, had also been influenced by a growing backlash against transgender people.
In Britain, for example, a yearslong fight over a proposed law that would have made it easier for transgender people to change the gender on their identification documents galvanized a political movement to try to exclude transgender women from women’s sports, prisons and domestic violence shelters.
“The intention with the Cass review is to be neutral, but I think that neutral has maybe moved,” said Laurence Webb, a representative from Mermaids, a trans youth advocacy organization in Britain. “Extremist views have become much more normalized.”
Other countries have seen more overt attacks on transgender rights and health care. In 2020, Hungary’s Parliament passed a law banning gender identity changes on legal documents. Last year, Russia banned legal gender changes as well as gender-related medical care, with one lawmaker describing gender surgeries as the “path to the degeneration of the nation.”
In France this year, a group of conservative legislators introduced a bill to ban doctors from prescribing puberty blockers and hormones, with punishments of two years’ imprisonment and a fine of 30,000 euros, or about $32,600. And on Monday, the Vatican condemned gender transitions as threats to human dignity.
Azeen Ghorayshi covers the intersection of sex, gender and science for The Times. More about Azeen Ghorayshi
Britain Is Leaving the U.S. Gender-Medicine Debate Behind
The Cass report challenges the scientific basis of medical transition for minors.

Listen to this article
Produced by ElevenLabs and News Over Audio (NOA) using AI narration.
In a world without partisan politics, the Cass report on youth gender medicine would prompt serious reflection from American trans-rights activists, their supporters in the media, and the doctors and institutions offering hormonal and surgical treatments to minors. At the request of the English National Health Service, the senior pediatrician Hilary Cass has completed the most thorough consideration yet of this field, and her report calmly and carefully demolishes many common activist tropes. Puberty blockers do have side effects, Cass found. The evidence base for widely used treatments is “ shaky .” Their safety and effectiveness are not settled science.
The report drew on extensive interviews with doctors, parents, and young people, as well as on a series of new, systematic literature reviews. Its publication marks a decisive turn away from the affirmative model of treatment, in line with similar moves in other European countries. What Cass’s final document finds, largely, is an absence . “The reality is that we have no good evidence on the long-term outcomes of interventions to manage gender-related distress,” Cass writes. We also don’t have strong evidence that social transitioning, such as changing names or pronouns, affects adolescents’ mental-health outcomes (either positively or negatively). We don’t have strong evidence that puberty blockers are merely a pause button, or that their benefits outweigh their downsides, or that they are lifesaving care in the sense that they prevent suicides. We don’t know why the number of children turning up at gender clinics rose so dramatically during the 2010s, or why the demographics of those children changed from a majority of biological males to a majority of biological females. Neither “born that way” nor “it’s all social contagion” captures the complexity of the picture, Cass writes.
What Cass does feel confident in saying is this: When it comes to alleviating gender-related distress, “for the majority of young people, a medical pathway may not be the best way to achieve this.” That conclusion will now inform the creation of new state-provided services in England. These will attempt to consider patients more holistically, acknowledging that their gender distress might be part of a picture that also includes anxiety, autism, obsessive-compulsive disorder, eating disorders, or past trauma.
This is a million miles away from prominent American medical groups’ recommendation to simply affirm an adolescent’s stated gender—and from common practice at American gender clinics. For example, a Reuters investigation found that, of 18 U.S. clinics surveyed, none conducted the lengthy psychological assessments used by Dutch researchers who pioneered the use of medical gender treatments in adolescents; some clinics prescribe puberty blockers or hormones during a patient’s first visit. Under pressure from its members, the American Academy of Pediatrics last year commissioned its own evidence review, which is still in progress. But at the same time, the group restated its 2018 commitment to the medical model.
The Cass report’s findings also contradict the prevailing wisdom at many media outlets, some of which have uncritically repeated advocacy groups’ talking points. In an extreme example recently noted by the writer Jesse Singal, CNN seems to have a verbal formula , repeated across multiple stories, to assure its audience that “gender-affirming care is medically necessary, evidence-based care.” On a variety of platforms, prominent liberal commentators have presented growing concerns about the use of puberty blockers as an ill-informed moral panic.
Read: The power struggle over transgender students
The truth is that, although American medical groups have indeed reached a consensus about the benefits of youth gender medicine, doctors with direct experience in the field are divided, particularly outside the United States. “Clinicians who have spent many years working in gender clinics have drawn very different conclusions from their clinical experience about the best way to support young people with gender-related distress,” Cass writes. Her report is a challenge to the latest standards of care from the U.S.-based World Professional Association for Transgender Health, which declined to institute minimum-age limits for surgery. The literature review included with her report is notably brutal about these guidelines, which are highly influential in youth gender medicine in America and around the world—but which, according to Cass, “lack developmental rigour.”
The crux of the report is that the ambitions of youth gender medicine outstripped the evidence—or, as Cass puts it, that doctors at the U.K. clinic whose practices she was examining, although well-meaning, “developed a fundamentally different philosophy and approach compared to other paediatric and mental health services.” How, she asks, did the medical pathway of puberty blockers and then cross-sex hormones—a treatment based on a single Dutch study in the 1990s—spread around the world so quickly and decisively? Why didn’t clinicians seek out more studies to confirm or disprove its safety and utility earlier? And what should child gender services look like now?
The answer to those first two questions is the same. Medicalized gender treatments for minors became wrapped up with a push for wider social acceptance for transgender people, something that was presented as the “ next frontier in civil rights,” as Time magazine once described it. Any questions about such care were therefore read as stemming from transphobic hostility, full stop. And when those questions kept coming anyway, right-wing politicians and anti-woke comedians piled on, sensing an area where left-wing intellectuals were out of touch with popular opinion. In turn, that allowed misgivings to be dismissed as “ fascism ,” even though, as the British journalist Sarah Ditum has written, “it is not damning of feminists that they are on the same page as Vladimir Putin about there being two sexes. That is just how many sexes there are.”
In Britain, multiple clinicians working at the Gender Identity and Development Service (GIDS) at the Tavistock and Portman Trust, the central provider of youth gender medicine, tried to raise their concerns, only to have their fears dismissed as hostility toward trans people. Even those who stayed within the service have spoken about pressure from charities and lobbying groups to push children toward a medical pathway. As Cass notes, “There are few other areas of healthcare where professionals are so afraid to openly discuss their views, where people are vilified on social media, and where name-calling echoes the worst bullying behaviour.”
This hostile climate has hampered attempts to collect robust data about real-world outcomes. The report’s research team at the University of York tried to follow up on 9,000 former GIDS patients but was informed by National Health Service authorities in England in January that “despite efforts to encourage the participation of the NHS gender clinics, the necessary cooperation had not been forthcoming.” Cass has since wondered aloud if this decision was “ideologically driven,” and she recommends that the clinics be “directed to comply” with her team’s request for data.
As I have written before, the intense polarization of the past few years around gender appears to be receding in Britain. Kamran Abbasi, the editor in chief of The BMJ , the country’s foremost medical journal, wrote an editorial praising the report and echoing its conclusion that many “studies in gender medicine fall woefully short in terms of methodological rigour.” The country’s left-wing Labour Party has already accepted that feminist concerns about gender self-identification are legitimate, and its health spokesperson, Wes Streeting, welcomed the Cass report as soon as it was published. (The ruling Conservatives have also enthusiastically embraced its conclusions, and the former health secretary Sajid Javid pushed through a law change that made its data collection possible.) The LGBTQ charity Stonewall responded to the report by saying that some of its recommendations could be “positive,” and urged politicians to read it. Even Mermaids, the charity most associated with pushing the affirmative model in Britain, offered only lukewarm criticism that more gatekeeping could further increase waiting times.
The Cass report is a model for the treatment of fiercely debated social issues: nuanced, empathetic, evidence-based. It has taken a political debate and returned it to the realm of provable facts. And, unlike American medical groups, its author appears to have made a real effort to listen to people with opposing views, and attempted to reconcile their very different experiences of this topic. “I have spoken to transgender adults who are leading positive and successful lives, and feeling empowered by having made the decision to transition,” she writes in the introduction. “I have spoken to people who have detransitioned, some of whom deeply regret their earlier decisions.” What a difference from America, where detransitioners are routinely dismissed as Republican pawns and where even researchers who are trans themselves get pushback for investigating transition-related regret—and where red states have passed laws restricting care even for transgender adults, or have proposed removing civil-rights protections from them.
Daniela Valdes and Kinnon McKinnon: Take detransitioners seriously
Has the Cass report gotten everything right? The methodology and conclusions of its research should be open to challenge and critique, as with any other study. But it is undoubtedly the work of serious people who have treated a delicate subject seriously. If you still think that concerns about child medical transition are nothing more than a moral panic, then I have a question: What evidence would change your mind?
As Florida restricts treatment for trans adults, one clinic presses on

ORLANDO — Any day now, Joey Knoll told himself, he’d grab the bullhorn he kept at the edge of his desk, and he’d tell everyone at Spektrum Health that their year-long nightmare was over.
All of Knoll’s patients had been on edge since the Florida legislature banned nurse practitioners like him from prescribing hormones to transgender people. Florida doesn’t have nearly enough doctors to take up the slack, and so, for many patients, the care simply disappeared when the law took effect last May. A judge had the power to change that.
Knoll booted up his computer, and he listened as Lizzo’s “2 B Loved (Am I Ready)” played in the hallways. Spektrum had always been a fun clinic. People brought their pets to work, and Knoll, a 39-year-old gay man, sports a dyed blond mohawk. But the pop song echoed down empty hallways now, and Knoll knew his inbox would once again be filled with messages from desperate patients.
Nearly 150 were out of medicine, and others were nearing the end of their supply. Even Spektrum’s chief operating officer, a trans woman, had just one refill left.
Without hormones, many had become depressed and anxious. Trans women were growing body and facial hair. Trans men said their periods had returned after a few missed doses. The state had turned on them, they said. Now, their bodies were turning on them, too.
Knoll had nowhere to send them. Every doctor he knew had a full practice, and others told him the political climate had become too dangerous to treat trans people. The legislative ban laid out all sorts of regulations not grounded in science , and if health-care providers missed one, they could spend time in prison.
Knoll hadn’t felt exactly shocked when the law passed. Over the last three years, Republican-led legislatures had introduced a record number of bills that whittled away LGBTQ rights. Politicians had targeted schools and sports teams, bathrooms and bars, and two dozen states had passed sweeping laws that prohibited adolescents from transitioning. But no state had gone as far as Florida.
Knoll glanced at the bullhorn. He’d told himself every morning since late December that today was the day he’d use it. A group of patients had argued that the law discriminates against trans people, and they’d sued the state to overturn it. The judge had said just before Christmas that he would rule soon. Months had gone by, though, and Knoll and his patients were still waiting.
Knoll loaded the court website and imagined what he’d do if the judge overturned the ban. He would rush into the clinic’s rainbow-colored hallways, and he’d use the bullhorn to tell his staff it was time. The state would appeal, so they’d have to act fast. They’d call the patients who were out of medicine, then Knoll would write as many prescriptions as he could.
Lana Dunn, Spektrum’s chief operating officer, peeked in as the court docket loaded. Knoll sighed. The last update was still a post-trial brief the state had filed in January.
“There are common and respectable reasons for regulating gender-dysphoria treatments,” lawyers for the state had written. “Believing that better medical standards should be in place for a relatively new medical condition doesn’t amount to intentional discrimination.”
Knoll didn’t understand why state officials thought nurse practitioners weren’t already surpassing medical standards. No one had ever analyzed his patient outcomes, and several researchers have found that patients fare just as well when they see a nurse practitioner.
“If it’s a no, what are we going to do?” Dunn asked.
Knoll adjusted the stethoscope he’d draped across the collar of his neon pink button-down. Some of his patients had turned to the black market. Others were despondent. He didn’t want to imagine what they’d do if the ban remained.
“I can’t tell you,” he said. “I don’t have answers for that.”
When Knoll moved to Florida in the early 2000s, he found it as welcoming as the New York neighborhood he’d left behind. He had gay friends, but he made straight ones, too, and when he began his nursing career, he didn’t look for LGBTQ-specific clinics. Knoll knew queer people suffered, but he felt others did, too, so he took jobs in hospitals and nursing homes.
That changed in 2016 when a gunman killed 49 people and wounded 53 others at Pulse nightclub, a gay bar in Orlando. The shooting was the country’s deadliest act of violence against LGBTQ people. It reshaped the way Knoll thought of himself. He no longer wanted to live or work as if being gay were just an incidental fact of his life. The next year, he took a contract job at an LGBTQ clinic treating trans patients.
The work felt so rewarding, Knoll spent much of his free time trying to become better at it. He read books about treating LGBTQ patients. He found mentors who’d offered the care for decades, and he went to conferences to learn about the risks queer people face in medicine.
Florida has more than 111,000 trans people , but appointments for hormones were still relatively hard to come by in 2017. When Knoll’s contract work ended, he opened Spektrum as a nonprofit offering primary and gender-affirming care.
Though Florida was turning increasingly Republican, the state still felt queer friendly. After the Pulse shooting, all of Orlando seemed to hoist rainbow flags, and when Ron DeSantis became governor in 2019, he visited a memorial for the shooting and said his administration would not tolerate hate against the LGBTQ community.
Trans people felt so safe coming out here, Knoll’s practice added at least 10 new patients every week. He brought on therapists and three nurse practitioners, then he opened a second location in Brevard County, one of Florida’s more conservative areas. By 2022, Spektrum had nearly 5,000 patients, a mix of adults and adolescents.
That sense of safety seemed to vanish overnight. As trans people ran for office and starred in television shows, right-wing strategists decided they could be used as a wedge issue to drive conservative voters to the polls. Groups such as the Heritage Project and Alliance Defending Freedom wrote model legislation to curb trans rights, and in 2022, states introduced a record number of anti-LGBTQ+ bills.
In Florida, DeSantis signed what critics call the “don’t say gay” bill, forbidding instruction on gender identity in the classroom. His administration targeted drag clubs and directed the state’s medical board to prohibit minors from transitioning. Then, four days before the 2023 session opened, Florida became the first in the nation to introduce health-care restrictions for transgender adults.
All of a sudden, Knoll knew he wouldn’t just need to treat patients. He’d have to fight for their rights, too.
Knoll stayed up late all spring, watching hours-long legislative hearings from his backyard after a full day of seeing patients. Republican state lawmakers had proposed 10 anti-LGBTQ+ bills , including two that banned nurse practitioners from prescribing hormones to trans patients.
Nearly two dozen states had moved to ban young people from transitioning, but no other legislature wanted to limit adults’ access to care. In Florida, Democrats pushed the Republican sponsors to explain why they hoped to be the first.
“What is the state’s compelling interest to interfere with adults’ freedom to make the sort of informed decisions for themselves?” Rep. Robin Bartleman asked Rep. Randy Fine in a March 2023 committee meeting after he introduced the House version of the ban .
“We’re not limiting their access to health care,” Fine said. “We’re making sure that they have health care in a safe fashion.”
Knoll does not consider himself an emotional person. He tends to be even-keeled and sunny, but he felt full of rage watching the hearings. Fine wasn’t just critical of protecting trans rights, he was dismissive of their very identity. Online, he referred to trans people with quotation marks. He described transgender health care as “fraud” and “evil.” And when he wrote about the bill, Fine said he planned to “relish the battle ahead.”
Fine later told The Washington Post he doesn’t think being transgender is “real,” but he dismissed the idea that his bill prevented adults from transitioning. Doctors could still prescribe hormones, he noted.
Fine represents Brevard County, the coastal community where Spektrum opened its second location. Fine has never visited Spektrum or any other gender clinic, but he said Brevard is a big county with more than 600,000 residents and plenty of doctors.
“If you can’t find a doctor here to prescribe something this serious, then maybe there’s a much larger discussion that people should be having,” Fine said.
Fine described nurse practitioners as “less educated” than doctors, but nurse practitioners can assess patients and prescribe medications, and clinics across the country use them to provide primary care. In Florida, they fill a critical gap: The state is expected to have a shortfall of 18,000 doctors by 2025.
Knoll knew many of his patients would lose access to hormones if he couldn’t prescribe them, and he worried they’d suffer. Hormones regulate a person’s mind and body, and going cold turkey could send patients into depressive spirals or worse. Patients without ovaries or testes no longer produce hormones. Without them, they’d be at an increased risk of osteoporosis and heart disease.
Knoll and his staff worked extra hours to ensure most patients would have hormones through the summer, but by the time the bill reached the governor, hundreds still hadn’t scheduled an appointment.
DeSantis signed the bill in mid-May at a private Christian school in Tampa. A local website live-streamed the event, and after Knoll saw his last patient of the day, Spektrum’s staff crowded around Knoll’s desk to watch the governor’s news conference.
“We have a very crazy age that we live in,” DeSantis told the children who’d gathered to watch him sign the legislation. “There’s a lot of nonsense that gets floated around, and what we’ve said in Florida is, we are going to remain a refuge of sanity and a citadel of normalcy.”
Seven of Knoll’s nine employees are transgender, and as DeSantis signed the legislation, Knoll fought back tears. His job had just fundamentally changed, but his employees and patients had lost something bigger. All session, Republicans lawmakers had talked about trans people as if they were dangerous. Now, the governor had taken away the medication that made them feel like themselves.
Knoll and his staff watched as the governor threw his bill-signing pens into the audience like a musician tossing guitar picks at the end of a show, then the feed went dead.
When the last employee left for the day, Knoll shut his door, sat at his desk, and cried.
That spring, Spektrum started selling “Don’t Tread on Me” T-shirts with a rattlesnake coiled against a trans flag. American Revolutionaries first used the symbol in the 1700s, and though it has been co-opted by anti-government members of the tea party, Knoll sold it as a way of reminding people that American liberties were at stake.
The law went against the training Knoll learned in eight years of nursing school programs, but nurse practitioners could go to prison for a year if they treated adults for gender dysphoria and up to five if they offered the care to minors, so he decided to comply. He tried to hire a doctor so Spektrum could continue offering hormone therapy. He placed ads and made calls, but the new law made most doctors too nervous to commit.
One demanded a $100,000 relocation fee, Knoll said, and the others told him they needed to earn at least $250,000 a year — a stretch for a nonprofit that barely breaks even. Another said he’d take the job only if he could be paid under the table.
By late summer, Knoll realized all he could do was wait for a judge to intervene.
Over the last three years, as nearly half of U.S. states have moved to restrict transgender health care, patients have turned to the court system for help. Parents with trans children filed suit in Arkansas, Indiana and Tennessee, and a group of anonymous families sued Florida over its restrictions, too. That July, one of Knoll’s adult patients joined their case.
When the trial began in December, Lucien Hamel testified that as soon as he’d learned the difference between boys and girls, he’d known he wasn’t a girl. He didn’t have a word for the feeling back then, but he felt anxious and distressed when he was grouped with girls or thought of as one.
After Hamel gave birth to his son in 2016, his depression and “feeling of incongruence” intensified. He struggled to connect with his son. He thought he had postpartum depression, so he found a therapist, but he realized in those sessions that what he actually had was gender dysphoria. (Hamel’s lawyers declined to make him available for an interview with The Post.)
A pediatric endocrinologist eventually prescribed him testosterone. The medication changed Hamel’s body and his life.
“I started to look more and more like an authentic version of myself,” he testified. “I had a much better relationship with my child after that point.”
Eventually, the pediatric endocrinologist told Hamel his practice no longer wanted him to treat adults. The doctor referred Hamel to Spektrum. There, Hamel told the judge, he received care that was “pretty much letter for letter” what he’d received at the endocrinologist’s office. If anything, Spektrum’s nurse practitioners seemed more careful. They had Hamel come in for labs every three months, rather than every six.
When DeSantis signed Senate Bill 254, Hamel said he felt “incredibly lost.” He didn’t get in for an appointment before the bill passed, and by the time his next one came up in June, he was too late. No one at Knoll’s clinic could prescribe hormones.
Hamel searched for a new provider, but most were booked through 2024. The only clinic with open appointments was three hours away in Miami, and it charged a $385 nonrefundable fee on top of all medical costs.
Hamel ran out of testosterone before he could find a doctor. Without it, he testified, he’d lost “significant muscle mass,” and his hips had “widened in a very feminine way.”
“I’m afraid people will start to see me as a woman again,” Hamel told the judge. “I’ve come so far in establishing myself as Lucien, as the man that I’ve always known myself to be, and for that to be taken away from me by a law under the guise of, you know, making sure that I receive the best care or whatever, it’s scary.”
Knoll felt optimistic. The judge, a Bill Clinton nominee named Robert L. Hinkle, legalized same-sex marriage in Florida before the Supreme Court did. In an earlier, temporary ruling against the ban on adolescents, Hinkle had called the bill “an exercise in politics, not good medicine.”
When the trial ended four days before Christmas, the judge thanked everyone for their professionalism, then said he would try to deliver an opinion “as quickly as I can.”
Winter passed without a verdict. Mid-February, Spektrum’s board of directors decided to close the organization’s location in Brevard County. That clinic’s lone nurse practitioner had quit the previous year, and Knoll had yet to find anyone willing to take her place.
In some ways, shutting down the Brevard County office hurt more than watching DeSantis sign the bill. The clinic’s rainbow flag was the only one in town, and Knoll knew it had been more than a place to get health care. In court, Hamel testified that he’d felt isolated in his community as a trans person before he visited the Brevard County clinic.
“I went to Spektrum, and there are nurses there that I saw were trans,” Hamel testified. “It was the first time really I had met, like, another trans person who lived in Florida.”
The Orlando location was quieter than it had been before the ban, but Knoll intended to keep it open for primary care. Trans people came down with colds and infections, the same as anyone else, and they wanted a provider who understood them.
His first patient on a recent morning had pinkeye, and the second was a trans woman who’d found a doctor in Georgia who was willing to prescribe estrogen as long as someone in Florida monitored her hormone levels.
Knoll bounced into the room wearing a blue button-down with a pattern as busy as a Magic Eye poster.
“Hi! How are you?” Knoll asked the woman, a 33-year-old named Key-Rei Kestrel. “Have you seen your labs? They’re perfect.”
Knoll loaded Kestrel’s records, then tilted his computer so she could see. Her liver, kidneys and electrolytes all looked good. Her testosterone levels were low, and her estrogen was well within the target range.
“I wanted to thank you,” Kestrel said. “You saved my life. But at the same time, you didn’t save my life. You gave me life.”
Kestrel pulled out her old driver’s license and handed it to Knoll. She was 100 pounds heavier in the picture and angry. Back then, she told Knoll, she didn’t have any friends.
“I don’t even know who this person is,” she said.
Kestrel told Knoll she knew she was lucky. Most of her friends couldn’t afford to travel for care, and she could. Still, it didn’t seem right. Why should she have to spend 12 hours on the road, wearing down her car, wasting her vacation days, to get health care in Georgia that Knoll was qualified to give her close to home?
That wasn’t the only thing that had changed since the law had passed. She felt a new sense of hostility that scared her. A man at her work had said he hoped DeSantis legalized “transgender murder squads,” so he could shoot her and leave her to rot in a ditch.
Knoll tried to reassure Kestrel. All his patients had a story, and he did, too.
“Do you want a hug?” Knoll asked.
“I kind of do,” Kestrel said.
After the appointment, Knoll headed to the conference room. It was Dunn’s birthday. Someone had set up a store-bought red velvet cake with candles, and as the group sang “Happy Birthday,” Knoll looked around. Every day, his employees grappled with how to care for patients the law restricted them from treating. He worried it all amounted to a front-row seat to trauma. Sometimes, he considered closing the clinic entirely.
Dunn closed her eyes, then blew out the candles. The clinic’s other nurse practitioner told Dunn she hoped all her wishes came true.
“Just the one,” Dunn said. “Come on, Judge Hinkel.”
“Oh, let me go check,” Knoll said. “Oh my God. This would be a really nice birthday gift.”
Knoll ran down the hall, suddenly sure this would be the day. He slid into his office chair, reached for the bullhorn, then hit refresh. Dunn walked in, holding a piece of uneaten cake. He knew she’d called doctors around the state, and he knew she couldn’t get an appointment anywhere.
“Nothing?” Dunn asked.
Knoll looked up, and the optimistic smile he tried to maintain faded. He was a nurse. He was supposed to help people. Dunn was his best friend, and he knew she’d be out of estrogen within a matter of weeks.
“Nothing yet,” Knoll said. “But I’m going to keep checking.”


IMAGES
VIDEO
COMMENTS
Despite the challenges, scientists say the possibilities of the new wave of research into hormone therapies is exciting, offering the chance to fundamentally change healthcare for the transgender ...
Male-to-female (MTF) hormone therapy, or estrogen hormone therapy, can cause a person to experience physical, emotional, sexual, and reproductive changes. Some changes can reach their full extent ...
Feminizing hormone therapy typically is used by transgender women and nonbinary people to produce physical changes in the body that are caused by female hormones during puberty. Those changes are called secondary sex characteristics. This hormone therapy helps better align the body with a person's gender identity.
hormone replacement treatment (HRT), specifically estrogen hormone therapy, which can produce changes in body fat distribution and skin. laser hair removal, which can slow the growth of body and ...
Here are some of the most common results of estrogen-based HRT for transfeminine people: softer skin. breast growth. decreased muscle mass/growth. redistribution of body fat. thinning or slowed ...
1. Consider the letter and spirit of non-discrimination laws at your destination: Know whether there are any travel warnings at your destination and know whether national and local laws are ...
While low-quality evidence based on 247 transgender adults from three uncontrolled prospective cohort studies suggests that hormone therapy may lead to improvements in psychological functioning ...
Gender-affirming hormone therapy is the primary medical treatment sought by transgender people. It allows their secondary sex characteristics to be more aligned with their individual gender identity. Gender-affirming hormone therapy comes in two types: Masculinizing hormone therapy used to develop typically male sex characteristics.
Plan a visit online . Contact us to learn more about our full range of gender-affirming care. Call 412-586-9700 or find an endocrinology location near you. UPMC wants to make sure you're happy and healthy when it comes to your gender. Providers offer counseling about your gender-affirming hormone therapy options.
Gender-affirming hormones have been shown to improve psychological functioning and quality of life among transgender and nonbinary (trans) people, yet, scant research exists regarding whether and ...
Abstract. Many transgender men and women seek hormone therapy as part of the transition process. Exogenous testosterone is used in transgender men to induce virilization and suppress feminizing characteristics. In transgender women, exogenous estrogen is used to help feminize patients, and anti-androgens are used as adjuncts to help suppress ...
Transgender or nonbinary travelers with questions about medical equipment and devices can call the TSA Cares hotline in advance of their trip at 1-855-787-2227. The most important thing to keep in mind. Airports can be unsettling spaces for everyone but especially for trans and nonbinary people—and particularly for trans people of color.
He writes about LGBTQ+ issues, mental health, and pop culture. Travel can be a hassle for anyone, but for transgender and gender non-conforming people, just getting through the security line can ...
You don't have to constantly take hormones to be trans, 3 people who have gone on and off hormones say. Quispe López. Nov 4, 2021, 5:00 AM PDT. Simon Moore shares their hormone-replacement ...
3. Update your documents. One of the biggest hurdles for trans and gender-nonconforming travelers is documentation. Not all states and countries allow trans people to change the gender marker on their passport, and for non-binary people, very few places offer a non-binary option at all. If it's possible, update your passport to reflect the ...
There is no evidence to support continuation or cessation of hormones for older transgender women. Since the mean age of menopause in the U.S. is 49,[41] it is reasonable in transgender women who have undergone gonadectomy to consider stopping hormone therapy around age 50. Expected effects of this may be similar to non-transgender women ...
Transgender Australians seeking lower body procedures can go to just a handful of local surgeons. ... Sivasamy will travel to Thailand for surgery under a medical tourism company's "one-month ...
Key points. Gender-affirming hormone therapy is associated with reduced mental health problems in transgender people. It's not clear if the improvement relates to chemical changes in the brain ...
If you're selected for additional screening, you have the right to be accompanied by someone you know and to be screened in private. If you have any questions about TSA policies regarding traveling with medical equipment, call the TSA Cares hotline before your flight at 1-855-787-2227 to speak with a trained representative.
Hormone treatment for transgender people is usually initiated by specialist gender clinics, but some people start hormone treatment of their own accord without a prescription. With growing numbers of transgender people presenting to healthcare services (estimated as 9.2 per 100 0001), general practitioners, general endocrinologists, and other ...
Traveling While Transgender in 2020. UPDATE: This article was refreshed in June, 2020 with new information on updated TSA regulations, US state-licensed, non-binary identities, and more. A new link to the Orbitz LGBTQ Welcoming Hotels hub page was also added in February, 2021. Mark Twain once famously said, " Travel is fatal to prejudice ...
Monitoring for transgender men (FTM) on hormone therapy: Monitor for virilizing and adverse effects every 3 months for first year and then every 6 - 12 months. Monitor serum testosterone at follow-up visits with a practical target in the male range (300 - 1000 ng/dl). Peak levels for patients taking parenteral testosterone can be measured ...
Sex hormones control the reproductive system, and in recent years, there is a growing number of publications reporting their regulatory effects on the immune system (Table 1). 7 Cells of both the innate and adaptive arm of the immune system express receptors for sex hormones, such as oestrogen and testosterone, eliciting variable responses ...
Hormone therapy, according to the Endocrine Society, triggers physical changes like hair growth, muscle development, body fat and more, that can help better align the body with a person's gender ...
The Overland Park mother of a 14-year-old transgender son said the child hasn't started taking testosterone, the male hormone, but he will when his parents and doctors believe that level of care ...
In England, around 5,800 children were on the waiting list for gender services at the end of 2023, according to the N.H.S. "The waiting list is known to be hell," said N., a 17-year-old ...
April 12, 2024, 6 AM ET. In a world without partisan politics, the Cass report on youth gender medicine would prompt serious reflection from American trans-rights activists, their supporters in ...
On April 1 doctors in England's public health system stopped prescribing puberty-blocking hormones to children and young people with gender dysphoria. The decision came after recommendations in ...
A nurse-led clinic in Florida waits for the outcome to a challenge to a state law that bans nurse practitioners from prescribing hormones to trans people. (Video: Reshma Kirpalani/The Washington ...