The importance of follow-up visits after getting discharged from the hospital

Patients often ask why it is important to see their healthcare providers after discharge from the hospital or emergency department visit. There are several reasons it’s a good idea.
First, there was a reason for the hospitalization or emergency visit. It’s important for primary care providers not only to know why this happened – perhaps a bad reaction to a new medication or a lifestyle change such as a new diet or exercise routine – but also what happened in the hospital. The goal is to keep patients healthy and out of the hospital, so we want to prevent whatever caused the event from happening again.
In addition, tests may have been performed in the hospital but the results were not in yet by the time of discharge. It is very important that all test results have been reviewed so that nothing was missed. For example, a biopsy might take a week or two to come back, or an uncommon blood test might need to go to a special lab. Although normal test results are reassuring, tests that come back abnormal are concerning. Sometimes this results in further work-up and a referral to a specialist. A follow-up appointment is a great opportunity to put everything together.
Another reason for a follow-up visit is to go over any potential medication changes. Many times, what led to a hospitalization or ED visit is a new medication, usually prescribed by a regular outpatient provider. That provider needs to know what happened, and to not restart that medication. New or added medications prescribed at discharge, such as blood thinners, sometimes need to be monitored as well. Many times, a dosing change is made on pre-hospital medications, which requires monitoring. This is also a great time to confirm medications are being taken correctly and not accidentally doubled up or underdosed. This process, called medication reconciliation, is for patient safety.
Finally, a discharge appointment may be to check on one or more vital signs or repeat blood work. It may be to check how someone is breathing and oxygenating if the reason for hospitalization was pneumonia, or to check blood pressure readings if there was a blood pressure issue. Perhaps the patient had a kidney or bleeding problem and needs a quick repeat blood test to see if the kidneys continue to recover or blood counts are stable. A very important checkup is blood sugars for newly diagnosed diabetics or diabetic patients with any medication changes.
In the end, most follow-up visits after discharge are just a check up to see how the patient is doing and ensure there aren’t any complications. It’s also a great time to talk to a primary care provider about anything else or ask questions, especially if it’s been a while since the last appointment.

Related Departments:
- Primary Care: Keeping your family healthy close to home
Thanks for visiting! GoodRx is not available outside of the United States. If you are trying to access this site from the United States and believe you have received this message in error, please reach out to [email protected] and let us know.
Medicare Interactive Medicare answers at your fingertips -->
Hospital discharge planning, inpatient hospital services.
You must be logged in to bookmark pages.
Email Address * Required
Password * Required
Lost your password?
Hospital discharge planning is a process that determines the kind of care you need after you leave the hospital. Discharge plans can help prevent future readmissions, and they should make your move from the hospital to your home or another facility as safe as possible.
Medicare requires hospitals to screen inpatients and provide discharge planning for those who need it. However, screening is only mandatory for hospital inpatients. If you are an outpatient (possibly you are on observation status ), Medicare does not require screening or discharge planning. Some states may provide outpatients with rights to discharge planning services. For more information on discharge planning in your state, please contact your State Health Insurance Assistance Program (SHIP) .
Your discharge plan should include information about where you will be discharged to, the types of care you need, and who will provide that care. It should be written in simple language and include a complete list of your medications with dosages and usage information. To help ensure that your discharge is successful, keep the following in mind:
- If you are concerned, ask your provider for a discharge planning evaluation. Some hospitals automatically evaluate the discharge needs of all patients, but others do not. You, your caregiver , and/or your provider can request screening for discharge planning.
- When developing your discharge plan, the hospital should connect with you or your representatives and, if possible, incorporate your requests. After your evaluation is completed, hospital staff should give you the opportunity to provide feedback.
- The hospital’s main goal should be for you to return to the place you left before your hospital stay. This may be your home or another facility. If this is notpossible, the hospital should recommend other, more appropriate places for you.
- Make sure hospital staff members consider your full range of needs when creating your discharge plan. If you are returning home, hospital staff must evaluate your need for home health care , meal delivery, caregivers, durable medical equipment (DME) , and changes to your home to ensure safety. If you are returning to a facility, the hospital must make sure the facility can still manage your health care needs.
- If you have another type of insurance, such as Medicaid , check which services it covers as well. The hospital should also be familiar with Medicaid’s coverage rules for certain services, such as personal care and long-term care.
- Staff should provide a clear list of instructions for your care and information on all medications you take.
- The hospital is required to provide you with a list of home health agencies or SNFs in your area that participate in Medicare.
- You or your caregiver should be told what to do if problems occur, including who to call and when to seek emergency help.
- Follow up with your primary care provider (PCP) and other providers involved in your care. Hospital staff should advise you to schedule a follow-up visit with your providers soon after your discharge. Some hospitals help you schedule these follow-up appointments. Hospital staff should send your providers information about your medical condition no later than seven days after you leave the hospital. Keep in mind that Medicare pays for your PCP to manage your care after you are discharged .
Update your browser to view this website correctly. Update my browser now
- Order this publication
- Print/download
Hospital Discharge Planning: A Guide for Families and Caregivers
By Family Caregiver Alliance and reviewed by Carol Levine.
Table of Contracts
Legal issues affecting caregivers.
- What Is Discharge Planning
Why Is Good Discharge Planning So Important?
- Caregiver’s role in the Discharge Process
Discharge to a Facility
Paying for care after discharge, what if you feel it’s too early for discharge, basic questions for caregivers to ask, this is a lot of information. any advice for people new to all of this, additional resources.
A trip to the hospital can be an intimidating event for patients and their families. As a caregiver, you are focused completely on your family member or friend’s medical care, and so is the hospital staff. You might not be giving much thought to what will happen when your friend or family member leaves the hospital.
Everything about this transition – whether the discharge is to home, a short-term rehabilitation (“rehab”) center, or a residential nursing facility – is critical to the health and well-being of the person you care for. Studies have found that improvements in hospital discharge planning can dramatically improve the outcome for patients as they move to the next level of care.
Patients, family caregivers, and health care providers all are involved in maintaining a patient’s health after discharge. Yet, while it’s a significant part of the overall care plan, there is a surprising lack of consistency in both the quality and process of discharge planning across the health care system.
This fact sheet offers information, tools, and resources to support you and the person you care for during this critical time, including:
- Keys to a successful transition from hospital to home or care center
- Suggestions for improving the process
- Checklists for caregivers to help ensure the best care
- Tips to remove barriers and encourage meaningful communication between you, the doctor, and other health care practitioners
But first, let’s cover a few legal topics that will be relevant to you as a caregiver.
HIPAA: The Health Insurance Portability and Accountability Act
You may have heard about HIPAA restrictions. HIPAA rules impact the sharing of information about patients in medical care. Although when the act was first initiated there was some confusion about how much information families and caregivers could receive about a patient’s medical situation, it is now clear that information must be shared.
- The US Department of Health and Human Services says: If the patient is present and has the capacity to make health care decisions, a health care provider may discuss the patient’s health information with a family member, friend, or other person if the patient agrees or, when given the opportunity, does not object.
- A health care provider also may share information with these persons if, using professional judgment, he or she decides that the patient does not object.
- In either case, the health care provider may share or discuss only the information that the person involved needs to know about the patient’s care or payment for care. Particularly when you are named in an Advance Directive, there should be no problem with your being able to receive information about, and speak for, your friend or family member. Check to be sure that a current copy of the Advance Directive is in the patient file. Patients can also sign an authorization form that gives health care providers permission to speak with you.
Advance Health Care Directives
These documents clarify who will speak for patients if they cannot speak for themselves.
- The documents may be referred to as living wills, health care proxies or Durable Powers of Attorney for Health Care.
- These documents can only be completed when a person is competent to do so (if someone has dementia, talk to the doctor about whether they still are competent to sign a legal document).
- They include instructions on the type of care individuals desire if they are very ill or dying.
- Many doctors’ offices and hospitals have forms available.
Caregiver Advise, Record, Enable (CARE) Act
The CARE Actis in place to ensure hospitals aren’t discharging patients without preparing family caregivers. With the CARE Act, hospitals must do three things:
- Record the name of the family caregiver on the medical record of the person being cared for.
- Inform the family caregivers when their friend or family member is to be discharged.
- Provide the family caregiver with education and instruction for the medical tasks he or she will need to perform for the patient at home.
The CARE Act has been signed into law in the majority of U.S. States as well as the District of Columbia, Puerto Rico, and the U.S. Virgin Islands. AARP (American Association of Retired Persons) championed this act and continues working toward making it a law in every state.
AARP has a helpful printable fact sheet on the CARE Act: https://www.aarp.org/content/dam/aarp/ppi/2019/03/the-care-act-implementation-progress-and-promise.pdf . You can also download your free CARE Act wallet card: https://www.aarp.org/caregiving/local/info-2017/care-act-aarp-wallet-card.html?cmp=RDRCT-4e6ca682-20200402 . Print one for you and one for the person you care for to keep in your wallets next to insurance cards, so information on the CARE Act is at your fingertips when you need it.
Language and Translation Services
You and your friend or family member have the right to have an interpreter present – it’s important that language not be a barrier to clear communication.
- If you or the person you care for prefer speaking in a language other than English, be sure to request a professional interpreter . Hospitals and clinicians are legally required to provide that service to you, so if a professional interpreter is unavailable, the health care organization should make arrangements for translation services via video or telephone.
- Written materials must be provided in your preferred language as well.
- Studies have shown that numerous, often dangerous errors can be made in home care when language is not taken into account at discharge. More than 200 different languages are spoken in the US, with approximately 25 million people speaking English at a level below “very well.” This is further complicated when the discussion includes complex medical information.
- Fortunately, based on the Civil Rights Act of 1964, patients have the right to the services of an interpreter—including sign language interpreters—in health care settings. The availability of certified interpreters able to translate medical/health care language still varies widely from state to state, and some families simply use a relative to provide translation. But when complicated medical information is delivered or treatment decisions must be made, that may not be the best choice.
Quality of Care
If you have concerns about the quality of care a hospital, rehab, or nursing facility provides, you have a right to speak up – while it’s happening as well as after being discharged.
- Your first step: Bring your complaints to the doctor and nurses, if possible. Be specific in your concerns and ask them how they will resolve the issues. Another option is requesting a conversation with a hospital social worker who has experience addressing problems and connecting patients with the right resources. Hospitals usually have a department of Patient Relations, Patient Advocates, or Customer Service; you can also make a complaint or raise your concerns with them.
- If the person you care for is covered by Medicare: You can file a complaint about their care with your State’s Quality Improvement Organization (QIO) Here’s a link to a site listing QIOs and the states they cover: https://www.ahqa.org/ahqa-member-organizations/ . QIOs act on behalf of Medicare to address care complaints from people covered by Medicare. QIOs typically take care of issues such as getting the wrong medication, having the wrong surgery, or receiving inadequate treatment. You can also find your QIO by calling 1-800-MEDICARE.
- If not covered by Medicare: Report your concerns to your state’s department overseeing health care institutions or medical licensing board. You can also make complaints to the Joint Commission , an independent nonprofit that accredits health care organizations. You can also contact your health insurance provider or state department of health insurance if you think the patient is not getting the care they need.
- At a rehabilitation or nursing home facility: Contact the ombudsperson. Go to theconsumervoice.org , and click Get Help to find the contact information for your local ombudsman program. That is the recommended first step to addressing quality of care in rehab and residence facilities .
- If you think your friend or family member is not medically ready to be discharged: There are steps you can take. We address this concern in detail a bit further into this fact sheet (see the section: What if You Feel It’s Too Early for Discharge? ).
You can find more guidance about how to complain and be heard on the website of the Agency for Healthcare Research and Quality: https://www.ahrq.gov/patients-consumers/patient-involvement/how-to-complain.html .
Now let’s get back to preparing for discharge.
What Is Discharge Planning?
According to Medicare, discharge planning is a process that determines the kind of care a patient needs after leaving the hospital. Discharge plans should ensure a patient’s transition from the hospital to another medical facility or to their home is as safe and smooth as possible.
Only a physician can authorize a patientʼs release from the hospital, but the actual process and preparation of discharge planning can be completed by a number of people. Some hospitals have a dedicated discharge planning manager on staff, but your point person could also be a social worker, nurse, or other hospital representative. Ideally, and especially for the complicated medical conditions, discharge planning is done with a team approach.
In general, the basics of a discharge plan are:
- Evaluation of the patient by qualified personnel
- Discussion with the patient and/or their representative and involving them in the planning
- Reconciling medications – a thorough review of prescriptions, plus comparing pre-hospitalization meds with post-discharge meds to be certain there are no duplications, omissions, harmful side effects, or drug interactions.
- Planning for homecoming or transfer to another care facility
- Determining the need for caregiver training or any other support
- Referrals to a home care agency and/or appropriate support organizations in the community
- Arranging for follow-up appointments or tests
- Who to contact if you need help – ensuring you have the name and email address of your go-to person for care questions, as well as a phone number where you can get help 24 hours a day, including weekends.
The planning discussion will cover everything from the types of care that will be required to equipment needs, from diet and meal planning to medication administration. Even transportation and chores should be covered.
The main reason discharge planning is such a priority – not just for hospitals and care teams, but also the U.S. Centers for Medicare and Medicaid Services – is this:
Effective discharge planning can decrease the chances the person you care for is readmitted to the hospital.
A thoughtfully developed plan aids recovery, ensures medications are prescribed, and given correctly, and adequately prepares you to take over your friend or family member’s care – all of which contribute to care that reduces the chance of readmissions.
The challenge: No single, consistent approach
Not all hospitals are successful in this. Although both the American Medical Association and the Joint Commission on the Accreditation of Health Care Organizations (JCAHO) offer recommendations for discharge planning, there is no universally utilized system in US hospitals.
What we do know is research indicates that excellent planning and good follow-up can:
- Improve patient health
- reduce readmissions
- decrease health care costs.
The Caregiver’s Role in the Discharge Process
The discharge planner will look to you, the caregiver, for history and insights about your friend or family member. As their advocate, you are likely to play a central role, managing many vital tasks:
- collect information
- speak to doctors
- transport the patient
- ensure lab tests are done
- pick up, prepare and give medications
- research treatment options and risks
- handle insurance
As discharge nears, things can feel rushed at the hospital; in that rush, it can be easy to forget what needs to be discussed. If you’re feeling hurried, it is reasonable to ask the discharge planning team to slow things down so nothing is overlooked.
You may want to print out and bring this fact sheet with you to the hospital; if for some reason the discharge planning team doesn’t cover these subjects, you should feel comfortable raising them, yourself.
Caregiver capabilities
- The discharge planners should discuss with you your willingness and ability to provide care. You may have physical, financial, or other limitations that affect your caregiving capabilities. You may have other obligations such as a job or childcare that impact the time you have available. It is extremely important to tell hospital discharge staff about those limitations.
- It is essential that you get any training you need in special care techniques. Some of the care your friend or family member needs might be quite complicated. Your discharge planning manager should ensure you know what is required with wound, feeding tube or catheter care, procedures for a ventilator, or transferring someone from bed to chair (and that you know how to get the equipment required for these tasks). Request all instructions and guidance are provided in writing. If the hospital has video resources for specific tasks (wound care, for example), ask them to include links to those in the discharge instructions.
- If the person you care for has memory problems caused by Alzheimer’s disease, stroke, or another disorder, discharge planning becomes more complicated . You may need to remind the staff about special care and communication techniques needed by your friend or family member. Even without impaired memory, older people often have hearing or vision problems or are disoriented when they are in the hospital, which means these conversations are difficult to comprehend. They will need your help and patience.
Discharge to home: Finding the help you need
Listed below are common care responsibilities you may be handling for your friend or family member after they return home:
- Personal care: bathing, eating, dressing, toileting
- Household care: cooking, cleaning, laundry, shopping
- Health care: medication management, physicianʼs appointments, physical therapy, wound treatment, injections, medical equipment and techniques
- Emotional care: companionship, meaningful activities, conversation
There is no single best path for lining up the help you will need. Patients and caregivers turn to many different sources for support.
- The community. Community organizations can help with transportation, meals, support groups, counseling, and possibly a break from your care responsibilities to allow you to rest and take care of yourself (also known as respite care). Finding those services can take some time and several phone calls. The discharge planner should be familiar with these community supports, but if not, your local senior center or a private case manager might be helpful. (See the Resources section at the end of this Fact Sheet.) Family and friends also might assist you with home care.
- Home health professional services. Hiring in-home help is an option – one that takes time to research options, check references and make decisions that often include family members. Out of necessity, hiring decisions are often made in a hurry at the time of discharge. You might be handed a list of agencies – but even with help, selecting in-home help is not something to be rushed. Start discussions around discharge plans as soon as possible after admission — that will provide you time to research your options while your friend or family member is cared for in the hospital. If medically necessary, the doctor may authorize short term Home Health services when your family member is discharged.
A few notes about in-home help and finding the right fit:
- Think about the needs of the person you are caring for as well as your needs as a caregiver – including language and cultural background.
- You have a choice between hiring an individual directly or going through a home care or home health care agency. Part of that decision may be affected by whether the help will be “medically necessary” (i.e., prescribed by the doctor), and therefore paid for by Medicare, Medicaid, or other insurance. In that case, they will most likely determine the agency you use.
- In making your decisions, consider the pros and cons of your options. Home health care agencies handle paperwork for taxes and salary, ensure substitutes will be available if the worker is sick, and may provide access to a broader range of skills. On the other hand, if you hire an individual directly, there may be a more personal relationship, and the cost is likely to be lower. In either case, try to get recommendations from nurses, social workers, friends and others familiar with your situation.
Our fact sheet on hiring in-home help includes advice and resources to get you started: https://www.caregiver.org/resource/hiring-home-help/ .
If the patient is being discharged to a rehab facility or nursing home, effective transition planning should do the following:
- ensure continuity of care
- clarify the current state of the patientʼs health and capabilities
- review medications
- help you select the facility to which the person you care for is to be released
Selecting the right facility
- Too often choosing a facility can be a source of stress for families. You may have very little time and limited information to make your decision. The list of questions included in this fact sheet (below) will give you some direction as you start your search for a facility.
- Ask for help. You can hire a private geriatric care manager (for whom you will pay an hourly fee) to help research and recommend facilities based on your friend or family member’s specific needs. A social worker can offer much needed advice and support. Consider the ratings and feedback from credible online reviews of rehab facilities and nursing homes in your area (see the Resources section of this Fact Sheet).
- Focus on quality of care. While you need to be able to easily get to the facility, you may have to sacrifice some convenience for the sake of ensuring higher quality care for your friend or family member.
Understanding and navigating payment for after-hospital care needs:
- You might not be aware that insurance, including Medicare, does not pay for all services after a patient has been discharged from the hospita l .
- Certain skilled care or equipment, however, may be covered – if it is determined by the doctor to be “medically necessary.”
- Gather your questions regarding payment and check directly with knowledgeable sources – the hospital, your insurer, or Medicare – to find out what might be covered and what you will have to pay for. Keep careful records of your conversations.
As their advocate, you have the right to appeal a decision to discharge your friend or family member from the hospital if you think it’s too early or if you think discharge to home is not safe.
- If you don’t think they are medically ready to leave the hospital, your first step is to talk with the discharge planner (often a social worker) and express your reservations. It is a good idea to put it in writing – email or text. The discharge planner will take your concerns to the doctor who makes this decision.
- While still in the hospital and if covered by Medicare or by a Medicare-managed care plan, your friend or family member can file an appeal about a discharge right on the spot. You should get a form from the hospital titled “An Important Message from Medicare,” which explains how to appeal a hospital discharge decision. Note : Appeals are free and generally resolved in 2 to 3 days. The hospital cannot discharge you until the appeal is completed.
- Formal appeals are handled through designated Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO). To get the phone number for your BFCC-QIO, visit www.Medicare.gov/contacts , or call 1-800-MEDICARE .
Questions about the illness:
- What is it and what can I expect?
- What should I watch out for?
- Will we get home care, and will a nurse or therapist come to our home to work with my friend or family member? Who pays for this service?
- How do I get advice about care, danger signs, a phone number for someone to talk to, and follow-up medical appointments?
- Have I been given information either verbally or in writing that I understand and can refer to?
- Do we need special instructions because the person I care for has Alzheimer’s or memory loss?
What kind of care is needed?
Questions when the person i care for is being discharged to the home: *.
- Is the home clean, comfortable, and safe, adequately heated/cooled, with space for any extra equipment?
- Are there stairs?
- Will we need a ramp, handrails, grab bars?
- Are hazards such as area rugs and electric cords out of the way?
- Will we need equipment such as hospital bed, shower chair, commode, oxygen tank? Where do I get this equipment?
- Who pays for these items?
- Will we need supplies such as adult diapers, disposable gloves, skin care items? Where do I get these items?
- Will insurance/Medicare/Medicaid pay for these?
- Do I need to hire additional help?
Questions about training:
- Are there special care techniques I need to learn for such things as changing dressings, helping someone swallow a pill, giving injections, using special equipment?
- Have I been trained in transfer skills and preventing falls?
- Do I know how to turn my friend or family member in bed so they don’t get bedsores?
- Who will train me?
- When will they train me?
- Can I begin the training in the hospital?
Questions when discharge is to a rehab facility or nursing home:
- How long is my friend or family member expected to remain in the facility?
- Who will select the facility?
- Have I checked online resources such as www.Medicare.gov for ratings?
- Is the facility clean, well kept, quiet, a comfortable temperature?
- Does the facility have experience working with families of my culture/language?
- Does the staff speak our language?
- Is the food culturally appropriate?
- Is the building safe (smoke detectors, sprinkler system, marked exits)?
- Is the location convenient? Do I have transportation to get there?
For longer stays:
- How many staff are on duty at any given time?
- What is the staff turnover rate?
- Is there a social worker?
- Do residents have safe access to the outdoors?
- Are there special facilities/programs for dementia patients?
- Are there means for families to interact with staff?
- Is the staff welcoming to families?
Questions about medications:
- Why is this medicine prescribed? How does it work? How long will the medicine need to be taken?
- How will we know that the medicine is effective?
- Will this medicine interact with other medications? prescription and nonprescription? or herbal preparations that the person I care for is taking now?
- Should this medicine be taken with food? Are there any foods or beverages to avoid?
- Can this medicine be chewed, crushed, dissolved, or mixed with other medicines?
- What possible problems might I experience with the medicine? At what point should I report these problems?
- Will the insurance program pay for this medicine? Is there a less expensive alternative?
- Does the pharmacy provide special services such as home delivery, online refills, or medication review and counseling?
Questions about follow-up care: *
- What health professionals will my friend or family member need to see?
- Have these appointments been made? If not, whom should I call to make these appointments?
- Where will the appointment be? In an office, at home, somewhere else?
- What transportation arrangements need to be made?
- How will our regular doctor learn what happened in the hospital or rehab facility?
- Whom can I call with treatment questions? Is someone available 24 hours a day and on weekends?
Questions about finding help in the community:
- What agencies are available to help me with transportation or meals?
- What is adult day care and how do I find out about it?
- What public benefits is the person I care for eligible for, such as In-Home Supportive Services or VA services?
- Where do I start to look for such care?
Questions about my needs as a caregiver: *
- Will someone come to my home to do an assessment to see if we need home modifications?
- What services will help me care for myself?
- Does my friend or family member require help at night and if so, how will I get enough sleep?
- Are there things that are scary or uncomfortable for me to do, e.g., changing a diaper?
- What medical conditions and limitations do I have that make providing this care difficult?
- Where can I find counseling and support groups?
- How can I get a leave from my job to provide care?
- How can I get a respite (break) from care responsibilities to take care of my own health care and other needs?
* Adapted with permission from www.nextstepincare.org , United Hospital Fund.
We know it can feel overwhelming. Here are three steps to make it a bit more manageable:
- Print this fact sheet – the whole thing – and take it with you any time you will be visiting the hospital or meeting with a clinician or other member of your friend or family member’s care team. Use it as a reminder of topics and questions you want to cover. Bring a pen, too, and you can even take notes from your conversation on the printout. You may want to use your phone to record conversations with the discharge planner or doctor to help you remember what was said.
- Check out the tools, organizations and websites we recommend under the additional resources section below.
- Talk to people – your medical care team, definitely, but other people can point you in the right direction, too. While certain aspects of your situation may be unique, hospitalization and transitions in care are experiences most people are familiar with. Friends can make recommendations and referrals while also providing much-needed support.
Family Caregiver Alliance National Center on Caregiving (415) 434-3388 | (800) 445-8106 Website: www.caregiver.org Email: [email protected] FCA CareNav: https://fca.cacrc.org/login Caregiver Services by State https://www.caregiver.org/connecting-caregivers/services-by-state/
Family Caregiver Alliance (FCA) seeks to improve the quality of life for caregivers through education, services, research, and advocacy. Through its National Center on Caregiving, FCA offers information on current social, public policy, and caregiving issues and provides assistance in the development of public and private programs for caregivers. For residents of the greater San Francisco Bay Area, FCA provides direct family support services for caregivers of those with Alzheimer’s disease, stroke, ALS, head injury, Parkinson’s, and other debilitating brain disorders that strike adults.
FCA Caregiver Resources
A listing of all caregiver resources is available online at our website ( https://www.caregiver.org/caregiver-resources/all-resources/ ).
Other Organizations and Links
Medical/Nursing Task Tutorials for Family Caregivers
Home Alone Alliance Initiative, AARP https://www.aarp.org/ppi/initiatives/home-alone-alliance/family-caregiving-videos/
Next Step in Care United Hospital Fund Comprehensive information and advice to help family caregivers and health care providers plan transitions for patients. Spanish translations available. www.nextstepincare.org
Medicare’s Nursing Home Compare www.medicare.gov/nursinghomecompare
Medicare Rights Center www.medicarerights.org
Center for Medicare Advocacy “Hospital Discharge Planning” www.medicareadvocacy.org
Aging Life Care Association www.aginglifecare.org
National Eldercare Locator https://www.eldercare.acl.gov
Caregiver Action Network https://www.caregiveraction.org/
American Association of Retired Persons (AARP) https://www.aarp.org
This information was prepared and reviewed by Family Caregiver Alliance. Sources for this information include The Official U.S. Site for Medicare ( https://www.medicare.gov ), the U.S. Department of Health and Human Services Health Information Privacy Site ( https://hhs.gov/hipaa ), the National Institutes of Health U.S. National Library of Medicine ( https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7235049/ ), the American Association of Retired Persons (AARP) ( https://www.aarp.org ), and UpToDate.com ( https://www.uptodate.com/contents/hospital-discharge-and-readmission ). Edited and updated by Trish Doherty ( http://trishdoherty.net ). Revised August 2021. © Family Caregiver Alliance. All rights reserved.
Related Resources
In depth | 17 minutes.
Caregiverʼs Guide to Medications and Aging
By Kathleen A. Cameron, R.Ph., M.P.H., and reviewed by Ron Finley, R.Ph.
Medications: A Double-Edged Sword “Any symptom in an elderly patient should be considered a drug side effect until proved otherwise.” Brown University Long-term Care Quality Letter, 1995 Modern medicines have contributed to longer life spans, improved heal
In Depth | 20 minutes
Hiring In-Home Help
By Family Caregiver Alliance
Table of Contents Do I Need Assistance? My Loved One Only Wants Me to Help How Do I Find Help? Home Care Agency Pros and Cons Private Hire What Will It Cost? How Can I afford It? How Do I Find the Right Person? Write a Job Description Interviewing Writing

An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Discharge Planning and Transitions of Care
Transitions of care refer to the movement of patients between different healthcare settings such as from an ambulance to the emergency department, an intensive care unit to a medical ward, and the hospital to home. The transition from hospital to home can be challenging as patients and families become responsible for care coordination. Hospital discharges are complicated and often lack standardization. Patients receive an onslaught of new information, medications, and follow-up tasks such as scheduling appointments with primary care providers.
Suboptimal transitions of care increase the risk of readmissions and adverse drug events after discharge. 1 The discharge process can be influenced by characteristics and activities of the health system, patient, and clinician. 2 Discharge instructions may differ between providers, or may not be tailored to a patient’s level of health literacy or current health status. 3 Prior studies have shown that an early discharge preparation process can significantly decrease hospital length of stay (LOS), readmission risk, and mortality risk. 4
As such, discharge planning should begin as soon as possible. However, studies show it is often difficult to predict the day of discharge accurately, 5 which may contribute to the practice of communicating important information on the day of discharge 6 and patients and caregivers feeling that the discharge process is rushed. Healthcare professionals may overestimate the time spent on providing discharge instructions as well as their patients’ understanding. 7 In addition, healthcare professionals and patients use different wording to describe health-related terms. 6 All of these factors can play a role in the patient’s ability to state their diagnosis, medication name, indication, or side effects. 8 Furthermore, discharge instructions oftentimes instruct patients or caregivers to schedule follow-up appointments with their primary care provider or specialty providers after discharge. However, up to half of the patients instructed to make the appointment may not understand the reasons or mechanism for doing so, and therefore do not make the appointment. 6
Identifying Risk Factors for Poor Transitions
In one seminal study, patients who understood their post-discharge plan had a lower rate of subsequent hospital utilization (ED visits or hospitalizations) than those who did not. 9 Challenges to understanding discharge instructions include patients’ lack of physical or emotional readiness to learn and the fact that family members or patient caregivers may not be consistently involved with the educational and discharge planning efforts. Discharge instructions may be unclear and may not be tailored to patient’s individual learning style, social determinants, or health literacy needs. Furthermore, education provided from different healthcare providers may include conflicting or confusing information. Discharge information should be written clearly in patient-friendly terminology and be tailored to the patient’s learning style, social determinants, and health literacy needs. 10
Assessment of patient and caregiver concerns and risk factors associated with nonadherence should be addressed throughout the hospitalization, including lack of engagement, poor continuity of care, and complex treatment regimens. 11 Oftentimes, patients may be non-adherent because of poor understanding or confusion about needed care, transportation, and how to schedule appointments. 12 Lack of follow-up appointment coordination prior to discharge results in patient and family caregivers not knowing who and when to follow up with when there are multiple providers. 3 In addition, there can be a lack of clear communication of the post-discharge care plan between the physician and the home health care team following the home health orders.
A systematic review of nine studies grouped factors for medication nonadherence into patient-related factors (i.e. disease-state knowledge, health literacy, cognitive function), drug-related factors (i.e. adverse effects, polypharmacy), patient-provider relationship, and logistical factors (i.e. transportation and medication access). 14 Proactively assessing these factors may streamline the discharge process.
Improvements in Discharge Planning and Transitions of Care
Discharge education should be provided throughout the hospitalization and then understanding confirmed on the day of discharge. There are tools available to help facilitate discharge education such as “teach-back” which assesses the key learner’s understanding of the discharge instructions. 15 Another strategy is to incorporate a discharge checklist. Some studies demonstrate the value of discharge checklists to document required components for a safe discharge. 16,17 One study found that 1 in 10 discharges include errors in discharge instructions, incorrect discharge medications, or a good catch and approximately a third of patients may need additional education prior to discharge. 18 While checklists may be helpful, they do not replace appropriate training or clinical competence. 19 Resources such as the AHRQ Re-Engineered Discharge ( RED) Toolkit can help provide evidence-based training for staff as well as outline processes to improve the discharge process and reduce readmissions. 9
Nurses play an integral role in the discharge process by coordinating care and providing timely communication with key stakeholders including families and community providers to ensure smooth transitions of care. Additionally, pharmacists can play a crucial role in medication safety during transitions of care through medication reconciliation and discharge education. 20 Pharmacists can ensure patients understand their medications and can obtain them after leaving the hospital. Furthermore, since the majority of post-discharge adverse events involve medications, pharmacists can assist with post-discharge telephone follow-up to check in with patients and proactively address any medication related issues. 21
Effective discharge planning can help reduce medical errors during transitions of care, which is known to be a time during which patients are particularly vulnerable. Planning for discharge should involve the patient and caregiver and begin as soon as possible during the hospitalization. The IDEAL discharge planning strategy is one approach emphasizing patient and family engagement in discharge planning and discharge education. 22 Additionally, AHRQ houses a library of evidence-based resources and tools to improve the discharge process and care transitions. 23
Sarah A. Bajorek, PharmD, BCACP Pharmacy Supervisor, Transitions of Care and Medication Reconciliation University of California, Davis Health [email protected]
Vanessa McElroy, RN, BSN, PHN, ACM-RN IQCI Director, Care Transition Management University of California, Davis Health [email protected]
- Agency for Healthcare Research and Quality. Readmissions and Adverse Events After Discharge. https://psnet.ahrq.gov/primer/readmissions-and-adverse-events-after-discharge
- Greenwald JL, Denham CR, Jack BW. The hospital discharge: a review of a high risk care transition with highlights of a reengineered discharge process. J Patient Saf . 2007;(3):97-106.
- HSAG Coordination Toolkit. Care Coordination Best Practices Toolkit: an overview of care coordination best practices to avert hospital readmission. Accessed April 12, 2024. [ Free full text ]
- Gabriel S, Gaddis J, Mariga NN, et al. Use of a daily discharge goals checklist for timely discharge and patient satisfaction. MedSurg Nursing . 2017;(4):236.
- Sullivan B, Ming D, Boggan JC, et al. An evaluation of physician predictions of discharge on a general medicine service. J Hosp Med . 2015;(12):808-810. [ Free full text ]
- Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center. JAMA Intern Med . 2013;(18):1715-1722. [ Free full text ]
- Calkins DR, Davis RB, Reiley P, et al. Patient-physician communication at hospital discharge and patients' understanding of the postdischarge treatment plan. Arch Intern Med . 1997;(157):1026-1030. [ Available at ]
- Mayakarus AN, Friedman EA. Patients' understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc . 2005;(8):991-994. [ Available at ]
- Agency for Healthcare Research and Quality. Re-Engineered Discharged (RED) Toolkit. https://www.ahrq.gov/patient-safety/settings/hospital/red/toolkit/index.html
- Peter D, Robinson P, Jordan M, et al. Reducing readmissions using teach-back: enhancing patient and family education. J Nurs Adm . 2015;45(1):35-42. [ Available at ]
- Naylor MD, Shaid EC, Carpenter D, et al. Components of comprehensive and effective transitional care. J Am Geriatr Soc . 2017;(65):1119-1125. [ Free full text ]
- Agency for Healthcare Research and Quality. Patient Engagement and Safety. https://psnet.ahrq.gov/primer/patient-engagement-and-safety
- Albrecht JS, Gruber-Baldini AL, Hirshon JM, et al. Hospital discharge instructions: comprehension and compliance among older adults. J Gen Intern Med . 2014;29(11):1491-1498. [ Free full text ]
- Gellad WF, Grenard JL, Marcum ZA. A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother . 2011;9(1):11-23. [ Free full text ]
- Agency for Healthcare Research and Quality. Health Literacy universal Precautions Toolkit, 3 rd edition. Use the Teach-Back Method: Tool #5. Accessed April 12, 2024. [ Free full text ]
- Soong C, Daub S, Lee J, et al. Development of a checklist of safe discharge practices for hospital patients. J Hosp Med . 2013;8(8):444-449. [ Free full text ]
- Flaster R. Four strategies cut newborn readmissions. Contemporary Pediatrics. 2017;(7):10. [ Free full text ]
- Gao MC, Martin PB, Motal J, et al. A multidisciplinary discharge timeout checklist improves patient education and captures discharge process errors. Q Manage Health Care . 2018;(27):63-68. [ Available at ]
- Agency for Healthcare Research and Quality. Checklists. https://psnet.ahrq.gov/primer/checklists
- Agency for Healthcare Research and Quality. The Pharmacist’s Role in Medication Safety. https://psnet.ahrq.gov/primer/pharmacists-role-medication-safety
- Agency for Healthcare Research and Quality. Postdischarge Follow-Up Phone Call. https://psnet.ahrq.gov/web-mm/postdischarge-follow-phone-call
- Agency for Healthcare Research and Quality. Strategy 4: Care Transitions From Hospital to Home: IDEAL Discharge Planning. https://www.ahrq.gov/professionals/systems/hospital/engagingfamilies/strategy4/index.html
- Agency for Healthcare Research and Quality. Resources and Tools to Improve Discharge and Transitions of Care and Reduce Readmissions. https://www.ahrq.gov/patient-safety/resources/improve-discharge/index.html
This project was funded under contract number 75Q80119C00004 from the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services. The authors are solely responsible for this report’s contents, findings, and conclusions, which do not necessarily represent the views of AHRQ. Readers should not interpret any statement in this report as an official position of AHRQ or of the U.S. Department of Health and Human Services. None of the authors has any affiliation or financial involvement that conflicts with the material presented in this report. View AHRQ Disclaimers
Patient Safety Primers
Inpatient Transitions of Care: Challenges and Safety Practices
Post-acute transitional services: safety in home-based care programs.
WebM&M Cases
Perspective
Perspectives on Safety
Amid lack of accountability for bias in maternity care, a California family seeks justice. August 16, 2023
Annual Perspective
Medicines-related harm in the elderly post-hospital discharge. March 27, 2019
Patient Safety Innovations
Suicide Prevention in an Emergency Department Population: ED-SAFE
Why doctors hate their computers. November 14, 2018
Overkill: An avalanche of unnecessary medical care is harming patients physically and financially. What can we do about it? May 20, 2015
The Checklist Manifesto: How to Get Things Right. January 13, 2010
Personal best. October 5, 2011
Failure and rescue. July 11, 2012
Better: A Surgeon's Notes on Performance. April 11, 2007
Complications: A Surgeon's Notes on an Imperfect Science. March 27, 2005
When doctors make mistakes. March 6, 2005
The checklist. December 12, 2007
The malpractice mess. December 7, 2005
The bell curve. March 6, 2005
Stopping deaths from incorrect drug doses. April 2, 2008
Developing a principle-based approach to safe medication practices. November 11, 2015
Hand hygiene compliance for patient safety. October 22, 2014
Nurses say stress interferes with caring for their patients. April 27, 2016
Nursing homes cited 1,000 times for medication errors. August 27, 2014
When doctors don't talk to doctors. July 1, 2015
Your new medical team: algorithms and physicians. December 16, 2015
New mother number 14. March 20, 2019
California doctors alarmed as state links their opioid prescriptions to deaths. February 6, 2019
Doctors make mistakes. A new documentary explores what happens when they do—and how to fix it. February 6, 2019
Deny, Dismiss, Dehumanise: What Happened When I Went to Hospital. May 1, 2019
Medical malpractice: the fear factor. September 29, 2010
Feud between Cedars-Sinai and surgeon puts focus on patient safety. April 21, 2010
Four patients say Cedars-Sinai did not tell them they had received a radiation overdose. October 28, 2009
The harm in pharmacy misfills. September 30, 2009
Tragic medication errors result in accidental abortions and premature birth—safety advocates say drug mistakes are still too frequent, despite advances. September 2, 2009
Program encourages reporting accidents waiting to happen: the Good Catch Awards. September 28, 2011
Using the web or an app instead of seeing a doctor? Caution is advised. July 20, 2016
Why even radiologists can miss a gorilla hiding in plain sight. February 20, 2013
The short life and lonely death of Sabrina Seelig. August 15, 2012
Massachusetts hospitals launch patient apology program. May 30, 2012
Electronic medical records may boost patient safety. July 31, 2013
Will false diagnosis cost Minnesota girl her life? January 18, 2012
Hospital mistakes kept secret. November 30, 2011
Patient safety law protects some documents in court case. September 12, 2012
The doctor doesn't listen to her. But the media is starting to. August 22, 2018
VA hospitals flooded with complaints about care. September 27, 2017
'America's other drug problem': copious prescriptions for hospitalized elderly. September 14, 2016
Anticoagulant safety practices call for pharmacist supervision. December 3, 2008
Hospital bracelets face hurdles as they fix hazard. October 8, 2008
Teams quicken response in medical emergencies. August 3, 2005
Hospital R.Ph.s weigh in on new JCAHO patient safety goals. July 27, 2005
Saving lives: hospitals have signed on to a six-part plan to avoid a multitude of unnecessary deaths. July 13, 2005
Walk inside, have surgery. But is it safe? June 29, 2005
100K Lives falling short. March 29, 2006
Reused devices, surgery's deadly suspects. January 18, 2006
High Quality Care for All: NHS Next Stage Review Final Report. July 16, 2008
The Definition of Quality and Approaches to Its Assessment. Vol 1. Explorations in Quality Assessment and Monitoring. March 27, 2005
Keeping Patients Safe: Transforming the Work Environment of Nurses. May 11, 2005
Hospital-error oversight called lax: state takes too long to investigate mistakes, patient advocates say. May 18, 2005
JCAHO to launch global patient safety center: the initial focus will be on reviewing and publicizing research findings. April 27, 2005
Safety in numbers. November 1, 2006
Long-term Care and Patient Safety
National patient safety goals.
Medication errors 2023: the year in review: January through December. March 6, 2024
Risks to Medication Delivery Using Ambulatory Infusion Pumps – Design and Usability in Inpatient Settings. February 14, 2024
Patient and Family Centered I-PASS (Family-Centered Communication Program to Reduce Medical Errors and Improve Family Experience and Communication Processes)
Medication management of COVID-19 patients during transition to virtual models of care: a qualitative study. December 6, 2023
Intervention of pharmacist included in multidisciplinary team to reduce adverse drug event: a qualitative systematic review. November 1, 2023
Reduced postdischarge incidents after implementation of a hospital-to-home transition intervention for children with medical complexity. October 4, 2023
Personal Health Literacy
Contributory factors and patient harm including deaths associated direct acting oral anticoagulants (DOACs) medication incidents: evaluation of real world data reported to the national reporting and learning system. July 12, 2023
Strategies to Improve Organizational Health Literacy.
Clinical Investigation Booking Systems Failures: Written Communications in Community Languages. May 31, 2023
Effects of a multimodal transitional care intervention in patients at high risk of readmission: the TARGET-READ randomized clinical trial. May 17, 2023
More than algorithms: an analysis of safety events involving ML-enabled medical devices reported to the FDA. May 3, 2023
Patient Safety Indicators.
What works in medication reconciliation: an on-treatment and site analysis of the MARQUIS2 study. April 12, 2023
Journal Article
Implementation of a medication reconciliation risk stratification tool integrated within an electronic health record: a case series of three academic medical centers.
AHRQ-Funded Patient Safety Project Highlights: Improving Healthcare Safety by Engaging Patients and Families. February 15, 2023
Accuracy of spinal anesthesia drug concentrations in mixtures prepared by anesthetists. January 11, 2023
Telehealth and Patient Safety.
Preventing errors when preparing and administering medications via enteral feeding tubes. December 7, 2022
Survey results from pharmacists provide support to enhance the organizational response to codes. October 26, 2022
A health system that won't learn from its mistakes. September 21, 2022
Review of medication error sources associated with inpatient subcutaneous insulin: recommendations for safe and cost-effective dispensing practices. August 24, 2022

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
Researchers in the field of Transitions of Care evaluate the effectiveness of various approaches to improve the discharge process. One classification scheme to categorize these interventions is to consider them as: pre-discharge interventions (patient education, discharge planning, medication reconciliation, scheduling a follow-up appointment); post-discharge interventions (follow-up phone call, communication with ambulatory provider, home visits); and bridging interventions (transition coaches, patient-centered discharge instructions, clinician continuity between inpatient and outpatient settings) [ 4 ].
This topic presents an overview of the discharge process, determination of the appropriate next site of care, and review of interventions to reduce the likelihood of unplanned readmissions and adverse events after discharge. Much of the discussion relates to structures of care available in the United States; there is significant variability in the availability of services and types of facilities across geographic areas.
APPROPRIATENESS FOR DISCHARGE
However, patients often appropriately remain in the hospital even when these criteria are met, due to the lack of a suitable alternative setting to provide necessary care or other social factors.
Transitional Care Management
What is medicare transitional care management (tcm).
Transitional Care Management (TCM) services address the hand-off period between the inpatient and community setting. After a hospitalization or other inpatient facility stay (e.g., in a skilled nursing facility), the patient may be dealing with a medical crisis, new diagnosis, or change in medication therapy. Family physicians often manage their patients’ transitional care.
The two CPT codes used to report TCM services are:
- CPT code 99495 – moderate medical complexity requiring a face-to-face visit within 14 days of discharge
- CPT code 99496 – high medical complexity requiring a face-to-face visit within seven days of discharge
Requirements and Components for TCM
- Contact the beneficiary or caregiver within two business days following a discharge. The contact may be via telephone, email, or a face-to-face visit. Attempts to communicate should continue after the first two attempts in the required business days until successful.
- Conduct a follow-up visit within 7 or 14 days of discharge, depending on the complexity of medical decision making involved. The face-to-face visit is part of the TCM service and should not be reported separately.
- Medicine reconciliation and management must be furnished no later than the date of the face-to-face visit.
- Obtain and review discharge information.
- Review the need for diagnostic tests/treatments and/or follow up on pending diagnostic tests/treatments.
- Educate the beneficiary, family member, caregiver, and/or guardian.
- Establish or re-establish referrals with community providers and services, if necessary.
- Assist in scheduling follow-up visits with providers and services, if necessary.
Discharge from any of the following:
- Inpatient acute care hospital
- Long-term acute care hospital
- Skilled nursing facility/nursing facility
- Inpatient rehabilitation facility
- Hospital observation status or partial hospitalization
Health Care Professionals Who May Furnish and Bill TCM Services:
- Physician (any specialty)
- Clinical nurse specialist (CNS)
- Nurse practitioner (NP)
- Physician assistant (PA)
- Certified nurse midwife
Non-physicians must legally be authorized and qualified to provide TCM services in the state in which the services are furnished.

Learn How Coordinated Care Benefits Patients, Quality Payment Program (QPP) Performance and Your Bottom Line
Transitional care management ensures patients who have a high-risk medical condition will receive the care they need immediately after discharge from a hospital or other facility. Learn more about how to get paid for this service.
Read more about transitional care management in the Making Sense of MACRA: Aligning Transitional Care Management (TCM) with the Quality Payment Program (QPP) supplement (PDF)
AAFP’s Position on TCM Services
The AAFP’s advocacy efforts have helped pave the way for Medicare payment for TCM services, giving family physicians an opportunity to be paid to coordinate care for Medicare beneficiaries as they transition between settings. We believe that family physicians should be compensated for the value they bring to their patients by delivering continuous, comprehensive, and connected health care.

What You Need to Know
As health care moves from volume to value, TCM services will be increasingly important. These services ensure patients receive the care they need immediately after a discharge from a hospital or other health care facility. Continuity of care provides a smooth transition for patients that improves care and quality of life, and helps prevent unnecessary readmission, thereby reducing costs.
Approaches to Help Your Practice Get Started
- Identify hospitals and emergency departments (EDs) responsible for most patients’ hospitalizations. With the shared goal of decreasing readmissions, develop a relationship with those hospitals to improve timeliness of notification, so the practice can reach out to patients within two business days of discharge.
- Add this service to decrease cost of care by reducing unnecessary readmissions.
- Add this service after the annual wellness visit and chronic care management (CCM) as the volume and associated revenue of this service is hard to anticipate.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Inpatient hospital care
Medicare Part A (Hospital Insurance) covers inpatient hospital care if you meet both of these conditions:
- You’re admitted to the hospital as an inpatient after an official doctor’s order, which says you need inpatient hospital care to treat your illness or injury
- The hospital accepts Medicare
Your costs in Original Medicare
You pay this in each benefit period :
- Days 1–60 : $1,632 deductible.
- Days 61–90 : $408 each day.
- Days 91 and beyond : $816 each day while using your 60 lifetime reserve days.
- Each day after you use all of your lifetime reserve days: All costs.
Frequency of services
Your doctor or other health care provider may recommend you get services more often than Medicare covers. Or, they may recommend services that Medicare doesn’t cover. If this happens, you may have to pay some or all of the costs. Ask questions so you understand why your doctor is recommending certain services and if, or how much, Medicare will pay for them.
Medicare-covered inpatient hospital services include:
- Semi-private rooms
- General nursing
- Drugs (including methadone to treat an opioid use disorder)
- Other hospital services and supplies as part of your inpatient treatment
Medicare doesn't cover:
- Private-duty nursing
- A private room (unless medically necessary)
- A television or phone in your room (if there's a separate charge for these items)
- Personal care items (like razors or slipper socks)
Things to know
Part A only pays for up to 190 days of inpatient mental health care in a freestanding psychiatric hospital during your lifetime. The 190-day limit doesn’t apply to care you get in a Medicare-certified, distinct part psychiatric unit within an acute care or critical access hospital.
Inpatient hospital care includes care you get in:
- Acute care hospitals
- Critical access hospitals
- Inpatient rehabilitation facilities
- Inpatient psychiatric facilities
- Long-term care hospitals
It also includes inpatient care you get as part of a qualifying clinical research study.
If you also have Part B, it generally covers 80% of the Medicare-approved amount for doctor’s services you get while you’re in a hospital.
Related resources
- Find hospitals
- Find long-term care hospitals
- Find inpatient rehabilitation facilities
- Steps to Choosing a Hospital Checklist
- Find out if you're an inpatient or an outpatient—it affects what you pay
- Skilled nursing facility coverage
- Long-term care hospital coverage
- Surgery (estimating costs)
- Your rights in the hospital
- Hospital Discharge Planning Checklist [PDF, 330KB]
- Medicare & You: Planning for Discharge from a Health Care Setting (video)
- See how Medicare is responding to COVID-19
Is my test, item, or service covered?
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Gen Intern Med
- v.36(8); 2021 Aug

Association of Post-discharge Service Types and Timing with 30-Day Readmissions, Length of Stay, and Costs
Hyo jung tak.
1 Department of Health Services Research and Administration, University of Nebraska Medical Center, Omaha, NE 68198 USA
Andrew M. Goldsweig
2 Division of Cardiovascular Medicine, University of Nebraska Medical Center, Omaha, NE USA
Fernando A. Wilson
3 Matheson Center for Health Care Studies, University of Utah, Salt Lake City, UT USA
Andrew W. Schram
4 Section of Hospital Medicine, University of Chicago, Chicago, IL USA
Milda R. Saunders
5 Section of General Internal Medicine, University of Chicago, Chicago, IL USA
Michael Hawking
6 Section of Hematology and Oncology, University of Chicago, Chicago, IL, USA
Tanush Gupta
7 Division of Cardiovascular Medicine, Houston Methodist Hospital, Houston, TX USA
8 Department of Radiology, University of California San Francisco, San Francisco, CA USA
9 Department of Health Sciences, University of Missouri, Columbia, MO USA
Associated Data
Although early follow-up after discharge from an index admission (IA) has been postulated to reduce 30-day readmission, some researchers have questioned its efficacy, which may depend upon the likelihood of readmission at a given time and the health conditions contributing to readmissions.
To investigate the relationship between post-discharge services utilization of different types and at different timepoints and unplanned 30-day readmission, length of stay (LOS), and inpatient costs.
Design, Setting, and Participants
The study sample included 583,199 all-cause IAs among 2014 Medicare fee-for-service beneficiaries that met IA inclusion criteria.
Main Measures
The outcomes were probability of 30-day readmission, average readmission LOS per IA discharge, and average readmission inpatient cost per IA discharge. The primary independent variables were 7 post-discharge health services (institutional outpatient, primary care physician, specialist, non-physician provider, emergency department (ED), home health care, skilled nursing facility) utilized within 7 days, 14 days, and 30 days of IA discharge. To examine the association with post-discharge services utilization, we employed multivariable logistic regressions for 30-day readmissions and two-part models for LOS and inpatient costs.
Key Results
Among all IA discharges, the probability of unplanned 30-day readmission was 0.1176, the average readmission LOS per discharge was 0.67 days, and the average inpatient cost per discharge was $5648. Institutional outpatient, home health care, and primary care physician visits at all timepoints were associated with decreased readmission and resource utilization. Conversely, 7-day and 14-day specialist visits were positively associated with all three outcomes, while 30-day visits were negatively associated. ED visits were strongly associated with increases in all three outcomes at all timepoints.
Post-discharge services of different types and at different timepoints have varying impacts on 30-day readmission, LOS, and costs. These impacts should be considered when coordinating post-discharge follow-up, and their drivers should be further explored to reduce readmission throughout the health care system.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-021-06708-6.
INTRODUCTION
Early follow-up after hospital discharge provides an opportunity to assess patient health and to provide care to reduce adverse health outcomes and 30-day readmissions. 1 – 8 Medical researchers have therefore identified barriers to early follow-up (e.g., limited resources to coordinate follow-up care, patient non-compliance) and designed interventions to promote follow-up. 1 , 7 , 9 – 15
However, some researchers have questioned the value of early follow-up because its efficacy may depend upon the likelihood of readmission at a given time after discharge 9 , 16 – 18 and upon the health conditions contributing to readmissions. 7 , 16 Among Medicare patients in the Centers for Medicare and Medicaid Services (CMS)’ initial Hospital Readmission Reduction Program (HRRP), approximately one-third of 30-day readmissions occurred within 7 days of discharge from the index admission (IA), and two-thirds occurred within 15 days, which might be earlier than scheduled follow-up care. 2 Furthermore, 30-day readmissions occur for a wide range of diagnoses different from the primary diagnosis of IA because recently discharged patients frequently experience changes in comorbidities or develop new health conditions. 2 , 19 – 24
Nonetheless, most prior studies have focused on the potential benefits of early follow-up care. Little is known about patients’ patterns of post-discharge services utilization and their outcomes, although patients utilize post-discharge services of different types and at different times to address various health care needs, and their effects on readmission and readmission resource utilization vary. Indeed, post-discharge services could improve health to reduce 30-day readmission or, alternatively, could identify post-discharge health problems that should be treated in the inpatient setting rather than office-based clinics. For example, prior research has shown that intensive primary care follow-up increased readmission among sicker patients, potentially due to physicians’ detection or patients’ complaints of medical problems unresolved during IA. 25
The present study used Medicare claims data for all-cause IA to examine how post-discharge services of 7 different types (institutional outpatient, primary care physician (PCP), specialist, non-physician provider, emergency department (ED), home health care, skilled nursing facility) and at 3 different timepoints were associated with 30-day unplanned readmission, readmission length of stay (LOS), and readmission inpatient costs.
Data Sources and Study Population
Our study used 2014 Medicare claims including data from the Master Beneficiary Summary File, Medicare Provider Analysis and Review (inpatient and skilled nursing facilities), institutional outpatient services, carrier services (ED and office-based health services across various medical provider specialties), and home health care. The initial study sample included Medicare fee-for-service (FFS) patients hospitalized for acute illness between February 1 and November 30. Health services utilization that occurred in January and December was used to account for health services 30 days prior to IA and 30 days after discharge, respectively.
We defined all-cause IA using criteria from the CMS 2014 Measure Updates and Specification Report (CMS-MUSR). 26 , 27 These criteria excluded admissions if (i) the primary diagnosis was medical treatment of cancer, rehabilitation, or psychiatric in nature; (ii) the discharge status was dead in hospital, left hospital against medical advice, or transferred to another acute care facility; and (iii) the patient unenrolled in Medicare FFS plans or died within 30 days of discharge. The unit of analysis was IA, and only admissions subsequent to IA were used to identify readmissions. When a patient was readmitted multiple times within 30 days of discharge from IA, only the first readmission was counted, and additional readmissions within this period were not counted as either new IA or readmission per CMS criterion. 2 , 26 An individual could have multiple IAs if subsequent admissions occurred more than 30 days after a prior discharge and met inclusion criteria.
We assessed readmission resource utilization per IA discharge among all IA discharges. Some researchers have measured resource utilization among readmitted patients only. However, this methodology does not assess the effect of post-discharge services utilization adequately because changes in readmission resource utilization depend upon both the probability of readmission and resources utilized by readmitted patients.
The University of Nebraska Medical Center Institutional Review Board approved this study.
Data Elements
The study had 3 co-primary outcomes: a binary outcome of unplanned 30-day readmission, average readmission LOS per IA discharge, and average readmission inpatient cost per IA discharge. Planned readmission was identified using the CMS-MUSR planned readmission algorithm, which specified diagnoses and procedures for which admissions were frequently planned. 26 Inpatient cost was measured as total charges allowed by CMS, which were the sum of CMS reimbursements and beneficiaries’ out-of-pocket payments.
Primary Independent Variables
The primary independent variables were 7 binary variables of post-discharge health services: institutional outpatient services (e.g., hospital outpatient department), office-based PCPs (general practice, family practice, internal medicine, obstetrics/gynecology, geriatrics), office-based specialists, office-based non-physician providers (e.g., nurse practitioner, physician assistant, physical therapist, rehabilitation), ED visit that did not result in readmission, home health care, and skilled nursing facility.
Utilization of each post-discharge service was measured within 7 days, 14 days, and 30 days of IA discharge to investigate the relationship between post-discharge services at different times and 30-day readmission, LOS, and costs. Given that 30-day readmission was defined as occurring anytime between 0 and 30 days of discharge, we defined 30-day post-discharge service as utilization occurring between IA discharge and unplanned 30-day readmission for patients who were readmitted or within 30 days of IA discharge for patients who were not readmitted. Services utilized on the readmission date (or 1 day prior to readmission for ED visits) were excluded. We defined 7-day and 14-day post-discharge services utilization similarly.
The outcome variable of readmission competes with the primary independent variable of health services utilization by necessity. For example, for a patient readmitted 9 days after IA discharge, 14-day post-discharge services were defined as service utilized between IA discharge and readmission at 9 days because any post-discharge services utilized after readmission could not influence this readmission despite occurring within 14 days of IA discharge. If a patient was not readmitted within 14 days of IA discharge, 14-day post-discharge services were defined as any services utilized within 14 days of discharge.
Other Explanatory Variables
Explanatory variables included pre-IA health services utilization of the 7 types listed above and characteristics of IA (weekend admission, surgical intervention, LOS during IA, discharge status). We also controlled for age categories, gender, race/ethnicity, the 20 most frequent IA discharge diagnoses by ICD-9 codes, Elixhauser comorbidity index, health insurance status (dual eligibility for Medicare and Medicaid, participation in Medicare Part D), and geographic region (Northeast, Midwest, South, West).
Statistical Analysis
To examine the association of post-discharge services utilization with unplanned 30-day readmission, we employed multivariable logistic regressions. To analyze the association of post-discharge services utilization with LOS and inpatient costs, we used multivariable two-part models 28 , 29 because the overwhelming majority of patients were not readmitted and thus had zero readmission LOS and costs. In the first part of the two-part model, logistic regression was used to estimate whether patients had no readmission versus readmission (indicated by zero versus any LOS or costs). In the second part of the model, generalized linear models with a log-link function and gamma distribution accounted for LOS and costs conditional upon any positive outcome, to control skewed nature and outliers of these variables. 30 The estimation coefficients of two-part models were converted into average marginal effects (AMEs), which represent the differences in adjusted predicted outcome between a comparison group and a reference group. AME allows us to combine the effects of post-discharge services in both parts and to interpret them in terms of the outcome value (i.e., days for LOS, dollars for cost).
For each outcome variable, we ran three estimations in which 7-day, 14-day, and 30-day post-discharge services utilizations were primary independent variables, respectively.
We performed a subsample analysis for the 6 conditions included in the HRRP (acute myocardial infarction, heart failure, pneumonia, coronary artery bypass graft surgery, chronic obstructive pulmonary disease, total hip arthroplasty and/or total knee arthroplasty). We also conducted a sensitivity analysis by constructing a categorical variable for each post-discharge service (0, 1, 2, 3–5, ≥6 visits) and comparing its effects with the estimates from the main analysis. All estimates were adjusted with a robust option and clustered by county.
The study population included 583,199 all-cause IAs. The probability of 30-day unplanned readmission was 0.1176. Among these readmissions, 33.9% and 58.8% occurred within 7 days and 14 days of discharge, respectively, similar to the trends for 3 diseases included in the CMS’ initial HRRP. 2 Among readmitted patients, the average LOS and inpatient costs were 5.67 days and $48,030, respectively. As a result, among all IA discharges, the average readmission LOS and inpatient costs per IA discharge (i.e., probability of readmission multiplied by LOS or costs conditional on readmission) were 0.67 days and $5648, respectively (Table (Table1 1 ).
Unplanned 30-Day Readmission, Hospital Length of Stay, and Inpatient Costs ( n = 583,199)
The mean age was 78.2 years, 57.8% were female, and 83.2% were non-Hispanic white. Fifty-eight percent (58.4%) of IAs was attributable to the 20 most frequent primary IA diagnoses (Table (Table2). 2 ). Utilization of each post-discharge service is detailed in Figure Figure1 1 .
Patient Sociodemographics, Health Services Utilization Prior to Index Admission (IA), Characteristics of IA, Primary Diagnoses, Elixhauser Comorbidity Index, and Geographic Regions ( n = 583,199)

Post-discharge health services utilization within 7 days, 14 days, and 30 days of discharge from index admission ( n = 583,199).
In multivariable logistic regressions (Fig. (Fig.2), 2 ), institutional outpatient visits were most substantially associated with decreased unplanned 30-day readmission, with odds ratio (OR) 0.74 (95% confidence interval (CI) 0.72 to 0.75) at 7 days post-discharge and OR 0.40 (95% CI 0.39 to 0.41) at 30 days post-discharge. Conversely, 7-day (OR 1.22; 95% CI 1.20 to 1.25) and 14-day (OR 1.06; 95% CI 1.04 to 1.08) specialist visits were associated with increased readmission, while 30-day visits (OR 0.77; 95% CI 0.75 to 0.79) were associated with decreased readmission.

Association of post-discharge health services utilization within 7 days, 14 days, and 30 days of discharge from index admission with unplanned 30-day readmission ( n = 583,199). Notes: (i) In multivariable logistic models, odds ratio (OR) and 95% confidence interval (CI) were adjusted for 7 different types of post-discharge care (institutional outpatient, primary care physician, specialist, non-physician provider, emergency department, home health care, skilled nursing facility) and all other explanatory variables listed in Table Table2. 2 . (ii) p <0.05 if 95% CI does not include one. (iii) Full estimation results are presented in Appendix Table 1 , panel A.
The multivariable two-part models for LOS (Fig. (Fig.3A) 3A ) showed that average readmission LOS per IA discharge was lower by 0.15 days (AME −0.15; 95% CI −0.17 to −0.14) among patients with institutional outpatient visits within 7 days of discharge compared to those without. The AME of 7-day institutional outpatient visits on LOS is a difference in adjusted predicted LOS with and without visits. In our analysis, adjusted predicted LOS per IA discharge was 0.56 days and 0.71 days with and without visits, yielding AME −0.15 days. The AME is statistically significant at the 0.05 level if the 95% CI does not include zero. The AME of 30-day institutional outpatient visits was strengthened to −0.46 days (95% CI −0.48 to −0.44). Specialist visits within 7 days of IA discharge increased LOS by 0.12 days (AME 0.12; 95% CI 0.10 to 0.13), but negative association was observed with visits within 30 days of IA discharge (AME −0.18; 95% CI −0.20 to −0.16).

Association of post-discharge health services utilization within 7 days, 14 days, and 30 days of discharge with 30-day readmission hospital length of stay ( a ) and readmission inpatient costs ( b ) ( n = 583,199). Notes: (i) In multivariable two-part models, average marginal effect (AME) and 95% confidence interval (CI) were adjusted for 7 different types of post-discharge care (institutional outpatient, primary care physician, specialist, non-physician provider, emergency department, home health care, skilled nursing facility) and all other explanatory variables listed in Table Table2. 2 . (ii) The AME represents the difference in adjusted predicted outcome (i.e., 30-day readmission hospital length of stay per IA discharge, and inpatient costs per IA discharge) between patients who did and did not utilize each post-discharge service. (iii) p <0.05 if 95% CI does not include zero. (iv) Full estimation results for 30-day readmission length of stay, and costs are presented in Appendix Tables 2 and 3 (panel A), respectively.
For inpatient costs (Fig. (Fig.3B), 3B ), 7-day and 30-day post-discharge institutional outpatient visits reduced average readmission inpatient costs per IA discharge by $1345 (AME −1345; 95% CI −1516 to −1173) and $3977 (AME −3977; 95% CI −4203 to −3750), respectively. On the contrary, 7-day (AME 1829; 95% CI 1648 to 2011) and 14-day (AME 1099; 95% CI 934 to 1263) post-discharge specialist visits were associated with increased costs, while 30-day visits were associated with decreased costs (AME −492; 95% CI −674 to −309).
Home health care and PCP visits exhibited pattern similar to institutional outpatient visits for 30-day unplanned readmissions, LOS, and costs. Notably, ED visits were strongly associated with increases in three outcomes at all timepoints. There were no significant trends in readmission associated with non-physician provider visits and skilled nursing facilities. Full estimation results are presented in Appendix Tables 1, 2, and 3 , panel A.
Estimates of subsample analyses showed that utilization of institutional outpatient, specialist, and skilled nursing facility care was more effective to reduce LOS and costs for the 6 conditions included in the HRRP than for all-cause IA. Full estimation results are presented in Appendix Tables 1, 2, and 3 , panel B. Sensitivity analysis estimates were similar to those from the main analyses except that increases in the number of 7-day institutional outpatient visits did not continuously reduce 30-day readmission and costs.
Using Medicare claims data for all-cause IA, we found that institutional outpatient, home health care, and PCP visits at all post-discharge timepoints were associated with reduced 30-day unplanned readmissions, LOS, and inpatient costs. For specialist visits, 7-day and 14-day post-discharge visits were associated with an increase in readmission and resource utilization while 30-day visits were associated with a decrease in outcomes. ED visits at all timepoints were associated with increases in three outcomes.
As such, this study suggests that efforts to coordinate and encourage utilization of post-discharge services may be most effective if focused on certain types of services and timepoints. This focus is particularly important given that diverse health problems such as post-discharge syndrome, varying severity of unresolved illness, and new conditions, 2 , 19 – 24 , 31 , 32 as well as poor quality care during IA, 1 , 8 , 25 , 31 , 33 – 35 contribute to readmissions. Of note, in our study, only 18.1% of readmissions occurred for the same primary diagnosis as IA. Furthermore, previous, nationally representative inpatient data suggest that the leading diagnoses contributing to 7-day and 30-day readmissions are largely the same but their ranks vary, implying that changes in severity of illness or principal diagnosis over time contribute to readmission. 2 , 17
This study makes several novel contributions to the literature. First, we accounted for all-cause IA because the Medicare Payment Advisory Commission has proposed expanding its readmission penalty program to cover all-cause IA. 36 Most readmission studies have focused on the 6 specific diagnoses covered under the HRRP and provided no data regarding the generalizability of interventions or outcomes for other health conditions. 1 , 2 , 8 , 22 , 31 , 35 , 37 Second, our study is the first to characterize 7 different types of post-discharge services and investigate their impact at 3 different timepoints. Most previous research has focused only on 7-day follow-up interventions conducted either by PCPs or any type of medical providers. 1 , 8 , 25 , 31 – 35 , 37 However, their results have been mixed, partly because a single component or the aggregate of all care did not accurately assess the role of each type of service. 1 , 35 In our analyses, utilization of 7 different types of post-discharge services was interdependent, and estimates of each service varied substantially when certain post-discharge services were excluded from multivariable regression. Third, we assessed the association of post-discharge services utilization with LOS and inpatient costs. Although a major goal of HRRP is reduction of unnecessary readmission resource utilization, most prior studies used unplanned 30-day readmission rate as a proxy due to lack of information. 1 , 6 – 8 , 10 , 13 , 16 , 31 , 35 , 37
This is an observational study, and we cannot explicitly determine why the impact of post-discharge services varies by service types and timing. However, one potential explanation is that varying health conditions and needs determine patients’ choice of service types and timepoints, which, in turn, explain their associations with readmissions and resource utilization. Intuitively, patients with specific, high-risk concerns would be more likely to seek early visits to specialists, who might identify health problems for which inpatient care is necessary. 38 Then, at timepoints further from IA discharge, patients may visit specialists due to less urgent health conditions, which would contribute to improved health status and reduced readmission. On the other hand, early PCP visits have the potential to provide holistic care to address multiple lingering health concerns and mitigate both the effects of potential relapse and post-discharge syndrome. Home health care was strongly associated with decreased readmission and resource utilization at all times, potentially because patients need these services for general health problems, not that these services were specifically effective to control particular readmission risks. Overall, the effects of post-discharges services of different types varied at early timepoints following discharge. However, their cumulative effects became similar at timepoints further from IA, contributing to reduced readmission and resource utilization regardless of the type of services.
ED visits are different than all other services as they are not scheduled, and generally, patients try to avoid them. In our study, ED visits were positively associated with all 3 outcomes at all timepoints, possibly due to high health risks and poor access to other post-discharge services.
Despite patients’ and providers’ best intentions, post-discharge follow-up can be delayed for many reasons. As a result, in 2013, the CMS adopted transitional care management services, which provide payment incentives for scheduling follow-up appointments within 14 days of discharge. 39 , 40 However, in 2015, only 7.0% of eligible discharges among Medicare FFS beneficiaries included billing for this service, 15 possibly implying limited clinical capacity for early follow-up or slow uptake of this billing code. Despite limited use of these billing codes, in our study, patients usually utilized post-discharge services, and approximately two-thirds of patients visited PCPs or specialists within 14 days of IA discharge. Of note, the rate of home health care utilization was approximately one-third of PCP visits, but both were similarly effective to reduce readmission and resource utilization. Accordingly, expansion of home health care could be an effective tool to reduce expensive post-discharge services and readmission resource utilization.
In 2011, the estimated annual Medicare cost of readmission was $26 billion, of which $17 billion was considered potentially avoidable. 41 , 42 While the rate of unplanned readmission decreased substantially in the last decade, 43 most readmissions remain unplanned 1 , 33 , 43 , 44 and impose a significant economic burden on the health care system. 15 , 31 , 34 , 35 , 37 , 45 Nonetheless, very few prior studies have investigated factors influencing LOS and costs associated with readmission, 38 , 46 , 47 and due to the lack of information, researchers have often used readmission rates as a proxy for readmission resource utilization. Our study suggests that changes in readmission rates are not proportional to readmission resource utilization and alone cannot provide adequate knowledge to design interventions to contain costs.
Our study has several important limitations. First, in an observational study, we cannot control for potential unobserved confounders that may influence post-discharge services utilization (e.g., changes in post-discharge health status) and readmissions (e.g., patient engagement and compliance with treatment plan). Second, we do not have information on patient socioeconomic status that may influence readmission patterns. 31 , 48 In this vein, we included two insurance status variables and clustered the observations by county, reasoning that the residents of each county would have similar dwelling, social, and medical infrastructure characteristics. Third, our results may not be generalizable beyond Medicare FFS beneficiaries because Medicare FFS does not require PCP referral or care within a provider network, thereby allowing flexibility in post-discharge services.
In summary, this study highlights the association of post-discharge services of different types and at different timepoints with unplanned 30-day readmission and resource utilization. These findings may inform strategies to reduce unplanned 30-day readmission and to guide medical resource utilization more effectively.
(PDF 212 kb)
Author Contribution
Dr. Tak had full access to all of the data in the study and takes the responsibility for the integrity of the data and the accuracy of the data analysis. All authors have made substantial contributions to this manuscript and attest to the validity and legitimacy of the data, as well as its interpretation.
Declarations
The authors declare that they do not have a conflict of interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
For Healthcare Questions call 1.866.KINDRED
Healthcare Headlines Blog
The importance of post-discharge follow-up in patient outcomes.
With consumers’ growing interest in their care, physicians are increasingly seeing the benefits that greater involvement can have with regard to patient satisfaction and outcomes.
For example, one research study found that inpatients who rate their care with a lower degree of satisfaction are more likely to readmit within 30 days with post-discharge complications. 1
Therefore, greater patient involvement and satisfaction are key contributors to patient outcomes.
Research shows the benefits of post-discharge follow-up
While many strategies of increasing patient-centeredness are being applied during the patient’s time in the hospital, it is important to continue this level of care after discharge. Research on the subject reveals that:
- Patients that were hospitalized with acute conditions are less likely to readmit if they are contacted as part of an early follow-up program post-discharge. 2
- 20% of readmissions are likely to be prevented in patients with three or more chronic conditions if they are contacted by a provider of care within 14 days of discharge. 3
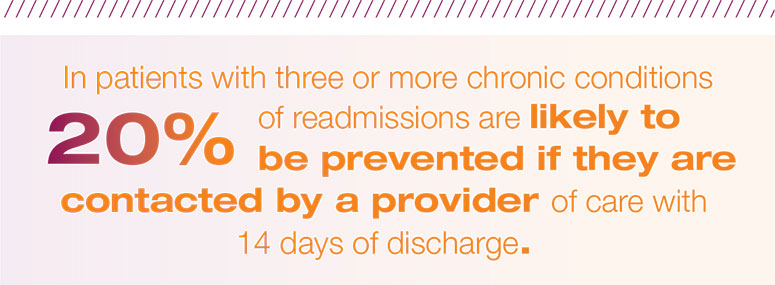
- There is no significant difference in satisfaction between nurse-led telephone follow-ups and outpatient visit follow-ups, suggesting that telephonic programs are effective patient engagement tools. 4,5
Implementing post-discharge follow-up services not only improves patient satisfaction, but can also reduce total cost of care over time as rehospitalizations or other major setbacks are prevented.
The Kindred AfterCare program is designed to help recovering patients heal and to provide the support they need once they have discharged from our hospitals. Trained staff will review patients’ charts and reach out to patients 2, 7, 14, and 31 days post-discharge. They discuss durable medical equipment, medication needs and education, primary care provider appointments, continued progress and any additional post-discharge services needed. Patients are also able to reach registered nurses 24/7 within the first 30 days after discharging from our hospital. This program improves patient outcomes and satisfaction as well as reduces the rate of readmission.
If you have a patient in need of continued acute care, call a Kindred Clinical Liaison for a patient assessment. Our experts will help you determine whether an LTACH stay is appropriate for your patient. If you are unsure of who your Kindred representative is, please feel free to contact us via recoveratkindred.com and speak with a Registered Nurse who can assist.
- https://qualitysafety.bmj.com/content/27/1/48.abstract
- https://pubmed.ncbi.nlm.nih.gov/20442387/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4369604/
- https://bmccancer.biomedcentral.com/articles/10.1186/1471-2407-10-174
- https://www.sciencedirect.com/science/article/abs/pii/S1462388910000840
Interested in learning about how Kindred Hospitals can help your medically complex patients recover?
Recent Posts
- Kindred Hospitals’ Complex Wound Care Can Reduce Readmissions and Length of Stay
- 5 Kindred Hospital Initiatives That Help Medically Complex Patients Recover
- 5 Setting Distinctions: LTACHs vs. SNFs
- Respiratory Failure: How Early Discharge to Kindred Hospitals Improves Outcomes and Reduces Readmissions
- Specialized Rehabilitation at Kindred Hospitals Can Reduce Inpatient Length of Stay
We're Social
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Hospital revisits...
Hospital revisits within 30 days after discharge for medical conditions targeted by the Hospital Readmissions Reduction Program in the United States: national retrospective analysis
- Related content
- Peer review
- Rishi K Wadhera , instructor in medicine 1 ,
- Karen E Joynt Maddox , assistant professor 2 ,
- Dhruv S Kazi , associate director 1 ,
- Changyu Shen , associate professor 1 ,
- Robert W Yeh , associate professor 1
- 1 Richard A and Susan F Smith Center for Outcomes Research in Cardiology, Division of Cardiology, Beth Israel Deaconess Medical and Harvard Medical School, 185 Pilgrim Road, Boston, MA 02215, USA
- 2 Department of Medicine, Cardiovascular Division, Washington University School of Medicine, St Louis, MO, USA
- Correspondence to: R K Wadhera rwadhera{at}bidmc.harvard.edu (or @rkwadhera on Twitter)
- Accepted 20 June 2019
Objective To determine any changes in total hospital revisits within 30 days of discharge after a hospital stay for medical conditions targeted by the Hospital Readmissions Reduction Program (HRRP).
Design Retrospective cohort study.
Setting Hospital stays among Medicare patients for heart failure, acute myocardial infarction, or pneumonia between 1 January 2012 and 1 October 2015.
Participants Medicare fee-for-service patients aged 65 or over.
Main outcomes Total hospital revisits within 30 days of discharge after hospital stays for medical conditions targeted by the HRRP, and by type of revisit: treat-and-discharge visit to an emergency department, observation stay (not leading to inpatient readmission), and inpatient readmission. Patient subgroups (age, sex, race) were also evaluated for each type of revisit.
Results Our study cohort included 3 038 740 total index hospital stays from January 2012 to September 2015: 1 357 620 for heart failure, 634 795 for acute myocardial infarction, and 1 046 325 for pneumonia. Counting all revisits after discharge, the total number of hospital revisits per 100 patient discharges for target conditions increased across the study period (monthly increase 0.023 visits per 100 patient discharges (95% confidence interval 0.010 to 0.035)). This change was due to monthly increases in treat-and-discharge visits to an emergency department (0.023 (0.015 to 0.032) and observation stays (0.022 (0.020 to 0.025)), which were only partly offset by declines in readmissions (−0.023 (−0.035 to −0.012)). Increases in observation stay use were more pronounced among non-white patients than white patients. No significant change was seen in mortality within 30 days of discharge for target conditions (−0.0034 (−0.012 to 0.0054)).
Conclusions In the United States, total hospital revisits within 30 days of discharge for conditions targeted by the HRRP increased across the study period. This increase was due to a rise in post-discharge emergency department visits and observation stays, which exceeded the decline in readmissions. Although reductions in readmissions have been attributed to improvements in discharge planning and care transitions, our findings suggest that these declines could instead be because hospitals and clinicians have intensified efforts to treat patients who return to a hospital within 30 days of discharge in emergency departments and as observation stays.
Introduction
Healthcare systems around the world are intensifying efforts to deliver higher value care. Reducing preventable hospital visits has drawn policy attention as an opportunity to improve quality of care and reduce healthcare spending in several countries, including the United States, England, Denmark, and Germany. 1 In the US, the Centers for Medicare and Medicaid Services (CMS) has implemented national initiatives that aim to push clinicians and hospitals to reduce readmissions for Medicare fee-for-service patients over the age of 65. In 2009, for example, CMS began publicly reporting 30 day readmission rates as a measure of hospital performance. One year later, the Hospital Readmissions Reduction Program (HRRP) was established, mandating that CMS impose financial penalties on acute care hospitals in the US with higher than expected 30 day readmission rates after a hospital stay for common medical conditions. Penalties under the HRRP began in 2012 and are capped at 3% of Medicare payments to hospitals; 82% of hospitals were penalized in fiscal year 2019. 2
Readmissions alone, however, do not capture the full spectrum of hospital revisits that can occur after discharge. A return visit to an emergency department, even if it does not result in an inpatient hospital stay, might also reflect inadequate care transitions or fragmented post-discharge care. In addition, observation stays, which are short hospital stays that are reimbursed differently from full inpatient hospital stays, are increasingly being used in the US as an alternative to inpatient hospital stays, and can occur in an emergency department, hospital observation unit, or a typical inpatient ward setting. 3 However, neither of these encounters (emergency department or observation stays) are included as outcomes in the 30 day readmission measure used by CMS to evaluate hospital care quality under the HRRP. 4
Understanding nationwide trends in total hospital based encounters (including treat-and-discharge visits to an emergency department, observation stays, or inpatient readmissions) within 30 days of discharge, for conditions targeted by the HRRP, is critically important from a policy perspective. A reduction in total revisits would suggest widespread improvements in discharge planning and transitions of care during hospital stays, as well as care coordination and quality in the post-discharge period, as intended by the HRRP. By contrast, if hospital revisits after discharge have not changed, or have increased, previously observed reductions in readmissions 5 might simply reflect greater management of patients in emergency departments and observation units, and the readmission measure currently used by CMS could provide an incomplete picture of hospital performance. Therefore, in this study, we aimed to answer three policy relevant questions:
Have total hospital revisits within 30 days of discharge after a hospital stay for medical conditions targeted by the HRRP changed over time?
How have rates of treat-and-discharge visits to an emergency department, observation stays (not leading to readmission), and readmissions each contributed to changes in total hospital revisits?
Do these patterns differ if all 30 day post-discharge revisits per patient are counted, to provide a more comprehensive assessment of hospital use after discharge, rather than just the first revisit as done by CMS for the readmission measure?
Study cohort
We used Medicare Provider Analysis and Review files to identify index hospital stays at acute care hospitals from 1 January 2012 to 1 October 2015 with a principal discharge diagnosis of heart failure, acute myocardial infarction, or pneumonia—medical conditions targeted by the HRRP. We defined study cohorts using ICD-9-CM (international classification of diseases, 9th revision, clinical modification) codes used in the publicly reported CMS readmission and mortality measures. We included Medicare beneficiaries aged 65 or older who were alive at discharge, and excluded patients who were discharged against medical advice, were not enrolled in Medicare fee for service for at least 30 days after discharge (absent death), or were enrolled in Medicare fee for service for less than one year before hospital admission. Transfers to other hospitals were linked to one index hospital stay. 6 Comorbidities were defined by hierarchical condition categories based on inpatient Medicare claims up to one year before hospital admission, and diagnosis codes per claim were limited to the first nine codes, 7 as has been done in previous studies. 5 6 8 9 We used outpatient claims files and previously described methods to identify observation stays 10 as well as treat-and-discharge visits to an emergency department 3 that occurred within 30 days of discharge after the index hospital stay.
Our primary outcome was the trend in total hospital revisits within 30 days of discharge after a hospital stay for medical conditions targeted by the HRRP. We also evaluated revisits by type: treat-and-discharge visits to an emergency department, observation stays (not later leading to readmission), and readmissions. For each revisit, we used two different approaches: we counted only one revisit (the first event after discharge) for each type of encounter after the index hospital stay, as CMS does for the readmission measure 4 ; and we counted all revisits within 30 days of discharge.
Statistical analysis
Logistic regression was used to fit a model for the outcome of the first post-discharge revisit among patients surviving up to discharge. We used a Poisson regression model for the outcome of all revisits. Models included reason for the index hospital stay (eg, heart failure, acute myocardial infarction, or pneumonia), demographics (age, sex, race), and clinical comorbidities as independent variables. After constructing separate models for each month (45 models for 45 months), we estimated the mean of the potential outcomes for each respective month using the demographics and clinical comorbidity profiles of patients admitted to hospital in 2014 as a reference, which was the most recent year that contained 12 calendar months of data. A smoothing spline was then fitted to the 45 data points to show temporal trends. A simple linear regression was also fitted to the 45 data points to estimate the monthly change for each type of revisit per 100 patient discharges. We then repeated this analysis to evaluate trends in revisits by patient subgroups. Additional details regarding the methodological approach and inferential strategy are provided in the supplement. Analyses were performed with SAS version 9.4 (SAS Institute). Institutional review board approval, including waiver of the requirement of participant informed consent because the data were deidentified, was provided by the Beth Israel Deaconess Medical Center.
Patient and public involvement
Patients and the public were not involved in planning, design, or interpretation of the study. The study involved examination of existing claims data and no participants were recruited for this analysis. We intend to engage patients and health policymakers by disseminating this research through press releases, blog posts, and at research meetings. This research was done without patient involvement. Patients were not invited to comment on the study design and were not consulted to develop patient relevant outcomes or interpret the results. Patients were not invited to contribute to the writing or editing of this document for readability or accuracy.
Our study cohort included 3 038 740 total index hospital stays from January 2012 to September 2015: 1 357 620 for heart failure, 634 795 for acute myocardial infarction, and 1 046 325 for pneumonia. Baseline characteristics for all index hospital stays are shown in eTable 1. Over the study period, 840 114 hospital revisits within 30 days of discharge (counting only the first revisit of any type after discharge) occurred, including 265 055 treat-and-discharge visits to an emergency department, 80 083 observation stays, and 599 664 inpatient readmissions (counting only the first revisit for each type of encounter). After counting all revisits after the index hospital stays, we found 1 064 410 total hospital revisits, of which 303 194 were treat-and-discharge visits to an emergency department, 84 169 were observation stays, and 677 047 were readmissions (eTable 2).
The number of first hospital revisits per 100 patient discharges for medical conditions targeted by the HRRP increased during the study (monthly change 0.016 revisits per 100 patient discharges (95% confidence interval 0.006 to 0.026); table 1 ). This change was driven by an increase in treat-and-discharge visits to an emergency department (0.022 (0.014 to 0.029)) and observation stays (0.022 (0.019 to 0.024)), which were only partly offset by reductions in inpatient readmissions (−0.013 (−0.023 to −0.002)).
Risk standardized monthly change in hospital revisits, treat-and-discharge visits to an emergency department, observation stays, and readmissions within 30 days of discharge for medical conditions targeted by the HRRP in the US
- View inline
These changes became more pronounced after we counted all revisits per patient within 30 days of discharge. The monthly change in total hospital revisits per 100 patient discharges increased (0.023 (95% confidence interval 0.010 to 0.035)), due to a rise in treat-and-discharge visits to an emergency department (0.023 (0.015 to 0.032)) and observation stays (0.022 (0.020 to 0.025)), while readmissions decreased (−0.023 (–0.035 to −0.012)). Figure 1 shows spline fitted trends of hospital revisits across all target conditions, and eFigures 1-2 show trends by individual target condition.

Risk standardized hospital revisits, treat-and-discharge visits to an emergency department, observation stays, and readmissions within 30 days of discharge for medical conditions targeted by the HRRP in the US. Spline fitted trends of hospital revisits are shown for all target conditions (heart failure, acute myocardial infarction, or pneumonia). Data based on Medicare fee-for-service patients aged 65 or over between 1 January 2012 and 1 October 2015. Yellow line=trends including only the first revisit for each type of encounter (eg, any hospital revisit, treat-and-discharge visit to an emergency department, observation stay, or inpatient readmission); purple line=trends including all revisits for each type of encounter
- Download figure
- Open in new tab
- Download powerpoint
Patient subgroups (age, sex, and race) were also evaluated, as shown in table 2 . Counting all revisits per patient, the monthly change in total hospital revisits per 100 patient discharges did not differ significantly among patients younger than 80 compared with patients aged 80 and over. Trends in treat-and-discharge visits to an emergency department, observation stays, and readmissions also did not differ between these age groups. In addition, we saw no significant difference in revisit trends among men compared to women. The monthly change in total hospital revisits and in treat-and-discharge visits to an emergency department were also similar among white patients compared with non-white patients. However, increases in observation stays within 30 days of discharge were more pronounced among non-white patients than white patients (monthly change 0.029 stays per 100 patient discharges (95% confidence interval 0.024 to 0.034) v 0.021 (0.018 to 0.024); P=0.006 for difference).
Risk standardized monthly change in hospital revisits, treat-and-discharge visits to an emergency department (ED), observation stays, and readmissions within 30 days of discharge for medical conditions targeted by the HRRP in the US, categorized by patient subgroups
Overall, we observed no significant changes in mortality within 30 days of discharge across the three targeted conditions (−0.0034 (95% confidence interval −0.012 to 0.0054)) from 2012 to 2015. Post-discharge mortality at 30 days did not change among patients admitted to hospital for heart failure (0.00 (−0.011 to 0.010)), acute myocardial infarction (−0.006 (−0.015 to 0.002)), or pneumonia (−0.004 (−0.013 to 0.005); fig 2 and eTable 3).

Risk standardized mortality within 30 days of discharge among Medicare patients admitted to hospital for heart failure, acute myocardial infarction, or pneumonia (medical conditions targeted by the HRRP in the US). Spline fitted trends of mortality are shown, by target condition. Data based on Medicare fee-for-service patients aged 65 or over between 1 January 2012 and 1 October 2015
In this study of Medicare beneficiaries admitted to hospital for heart failure, acute myocardial infarction, and pneumonia in the US between 2012 and 2015, we found an increase in total hospital revisits within 30 days of discharge despite a reduction in 30 day readmissions. This increase was because of a rise in treat-and-discharge visits to an emergency department and observation stays within 30 days of discharge, which on national level, exceeded the decline in readmissions. Our finding of increased healthcare use during this period was more pronounced after we included all encounters within 30 days of discharge from the index hospital stay—rather than simply including the first revisit.
In the US, nationwide reductions in readmission rates for medical conditions targeted by the HRRP have been viewed as markers of improvements in quality of care. Our findings suggest that this success could be illusory because total hospital revisits after discharge are, in fact, rising. If reductions in readmissions were being driven by widespread improvements in discharge planning, care transitions and post-discharge care after a hospital stay (as intended by the HRRP), total hospital revisits within 30 days of discharge would also be expected to decline. Instead, much of the reduction in readmissions seems to reflect intensified efforts to manage patients who return to a hospital after discharge in observation units and emergency departments, potentially because the 30 day readmission measure used to evaluate hospital performance under the HRRP does not include these types of post-discharge encounters. These observations perhaps explain why previous studies have shown that inpatient quality of care delivered to patients admitted to hospital for heart failure or acute myocardial infarction do not differ at hospitals with high versus low readmission rates. 11 12
The increase in use of observation stays and emergency department visits (compared with inpatient hospital stays) among patients who return after discharge could be a good thing if it reflects that patients are, on average, returning with lower severity illness that can be safely managed in a non-admission setting. These revisits could also be beneficial to patient care. For instance, observation stays have been associated with higher patient satisfaction than inpatient hospital stays, 13 although they can also result in higher out-of-pocket expenditures and more financial hardship for patients than inpatient hospital stays. 14 15
However, the increasing use of emergency department visits for post-discharge care could be problematic. Data have suggested that hospitals that tend to manage patients in emergency departments rather than admitting them for an inpatient stay have higher rates of early death after discharge. 16 We observed no change in post-discharge mortality at 30 days for target conditions during the HRRP (from 2012 to 2015). However, several independent analyses have found that the implementation of the HRRP was associated with an increase in post-discharge mortality at 30 days among patients admitted for heart failure and pneumonia compared with pre-HRRP trends (pre-2010), and that this increase was concentrated entirely among patients not readmitted after discharge. 6 17 18 19 Whether intensified efforts to manage returning patients in emergency departments and observation units explain increases in mortality observed in the years that preceded our study period is an important area for further research, given that this potential mechanism could explain increased mortality under the HRRP. 20 21 22 23 24
Policy implications
Our findings have important policy implications for value based programs that use the 30 day readmission measure to evaluate hospital and provider care quality. Firstly, focusing on 30 day readmissions while ignoring other types of hospital revisits overestimates the clinical and financial benefits of incentives to reduce readmissions. Secondly, use of 30 day readmissions as the sole quality metric could impede fair comparisons of hospital performance, particularly given wide variation in triage patterns in emergency departments and the availability and use of observation units. 25 Finally, given these limitations, the 30 day readmission rate seems to be an inappropriate target for financial incentives for hospitals (as used in the HRRP) or outpatient practices (as being increasingly used in pay-for-performance programs). Measuring all revisits within 30 days of discharge (that is, a “30 day return to hospital” metric) could instead provide a more comprehensive, accurate, and fair assessment of provider and hospital care quality. 26
Several countries, including England, Germany, and Denmark, have implemented national level policies that aim to reduce readmissions, and others are actively considering similar initiatives. 27 In England, incentives to reduce all cause readmissions were announced in 2010, 28 and from fiscal years 2011-12, hospitals were no longer reimbursed for readmissions within 30 days of discharge exceeding a locally set threshold. However, the extent to which reductions in readmissions in England are due to improved quality of care during the index hospital stay, or instead, are due to greater management and treatment of patients who return after discharge in emergency departments is unknown. This area is important for future study, particularly given growing concern in the US that a focus on reducing readmissions could have adversely affected patients at the margin who would have benefited from inpatient level care.
Strengths and limitations of this study
Our study had limitations. We did not examine whether the increase in total hospital revisits, and emergency department visits and observation stays in particular, was associated with changes in patient satisfaction, or changes in Medicare spending and beneficiary out-of-pocket expenditures. We were also unable to evaluate whether greater shifts in emergency department and observation use occurred in the years before our study, when the HRRP was announced in 2010, and if this affected patient experience, quality of care, and mortality. This area remains important for future research given ongoing discussions regarding the potential unintended consequences of this program. 21 22 23 26 29 30 31
Conclusions
Although readmissions for target conditions decreased from 2012 to 2015 in the US, total hospital revisits within 30 days of discharge steadily increased over that same period. This increase was due to a rise in treat-and-discharge encounters in emergency departments and observation stays, which on a national level, exceeded the decline in readmissions over the same period. Given that total hospital revisits are rising, nationwide reductions in readmissions could reflect intensified efforts to manage patients who return to a hospital after discharge to emergency departments and observation units rather than improvements in discharge planning and care transitions during index hospital stays, as intended by the HRRP. Future policy efforts in the US could benefit from measuring total hospital revisits within 30 days of discharge instead of solely focusing on readmissions, to strengthen incentives to improve quality of care and provide a more comprehensive assessment of care quality and healthcare use in the post-discharge period.
What is already known on this topic
Readmission rates at 30 days are increasingly used to measure quality of care and evaluate provider and hospital performance under value based payment programs in the United States
Readmission rates for medical conditions targeted by one such program, the Hospital Readmissions Reduction Program (heart failure, acute myocardial infarction, and pneumonia), have declined modestly on a national scale
Policymakers have attributed these reductions to improved discharge planning, care transitions, and post-discharge care after index hospital stays, but these declines could be because clinicians and hospitals have increasingly adopted strategies to manage patients who return to a hospital within 30 days of discharge in emergency departments or as observation stays—which are not included in the current readmission measure
What this study adds
Total hospital revisits within 30 days of discharge after a hospital admission for target conditions have steadily increased under the HRRP, due to a rise in treat-and-discharge visits in an emergency department and observation stays
Although reductions in readmissions have been attributed to improvements in discharge planning and transitional care, as intended by the HRRP, these declines instead appear to be due to intensified efforts to manage patients who return within 30 days of discharge in emergency departments and observation units
A metric to measure patients’ 30 day return to hospital that captures all post-discharge encounters (inpatient, emergency department, and observation stays) could provide a more comprehensive, accurate, and fair assessment of hospital quality and performance
Contributors: CS and RWY contributed equally as senior authors. All authors conceived and designed the study, analyzed and interpreted the data, and critically revised the manuscript for important intellectual content. RWY acquired the data. CS and RKW carried out the statistical analysis. RKW, KEJM, and DSK drafted the manuscript. RWY, RKW, and CS supervised the study and are the guarantors. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted
Funding: This study received no support from any organization.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organization for the submitted work; RKW receives research support from the National Heart, Lung, and Blood Institute (1K23HL148525-1), and has previously served as consultant for Regeneron, outside the submitted work; KEJM receives research support from the National Heart, Lung, and Blood Institute (R01HL143421), National Institute on Aging (R01AG060935), and Commonwealth Fund; RWY receives research support from the National Heart, Lung and Blood Institute (R01HL136708) and the Richard A and Susan F Smith Center for Outcomes Research in Cardiology and received from Abiomed, personal fees from Asahi Intecc, grants from AstraZeneca, grants and personal fees from Boston Scientific, personal fees from Medtronic, and personal fees from Teleflex outside the submitted work; DSK receives research support from the Richard A and Susan F Smith Center for Outcomes Research in Cardiology; the other authors report no conflicts; no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; and no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: This study was reviewed and granted exemption by the institutional review board at the Beth Israel Deaconess Medical Center, including waiver of the requirement of participant informed consent because the data were deidentified.
Data sharing: No additional data are available due to data use agreement with the Centers for Medicare and Medicaid Services.
The lead author affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as originally planned have been explained.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- Kristensen SR ,
- ↵ Hospital Readmissions Reduction Program (HRRP) Centers for Medicare and Medicaid Services. 2019 https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html accessed February 12 2019.
- Dharmarajan K ,
- Bierlein M ,
- ↵ 2017 Readmission Measures Updates and Specifications Report: Centers for Medicare & Medicaid Services (CMS); http://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page accessed February 2 2019.
- Zigler CM ,
- Choirat C ,
- Dominici F ,
- Wadhera RK ,
- Joynt Maddox KE ,
- Haneuse S ,
- Tsugawa Y ,
- Figueroa JF ,
- Papanicolas I ,
- Grabowski DC ,
- Ibrahim AM ,
- Dimick JB ,
- Hollingsworth JM ,
- Nuliyalu U ,
- ↵ Medicare Claims Processing ManualChapter 4 - Part B Hospital (Including Inpatient Hospital Part B and OPPS). 2019 https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c04.pdf accessed March 6 2019.
- Golwala H ,
- Kangovi S ,
- Cafardi SG ,
- Kulkarni R ,
- Sheehy AM ,
- Gangireddy S ,
- Obermeyer Z ,
- Huckfeldt P ,
- Escarce J ,
- Popescu I ,
- Wilcock A ,
- Fonarow GC ,
- Konstam MA ,
- Venkatesh AK ,
- Joynt Maddox KE
- ↵ Pricing framework for Australian public hospital services 2018-19: Independent Hospital Pricing Authority; 2017 https://www.ihpa.gov.au/sites/g/files/net4186/f/publications/pricing_framework_for_australian_public_hospital_services_2018-19.pdf accessed March 2019.
- ↵ Equity and excellence: liberating the NHS: Department of Health; 2010 https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/213823/dh_117794.pdf accessed March 2019.
- Email Us

- Channels ►
- Executive Moves
- Transaction & Valuation
- Health Equity
- Patient Experience
- Care Coordination
- Legal & Regulatory
- Compensation
- Specialties ►
- Orthopedics
- Surgery Centers
- Dental / DSO
- Becker's Healthcare Websites ►
- Dental + DSO
- Behavioral Health
- Physician Leadership
- Newsletters ►
- Sign Up For Our Free E-Newsletters
- Hospital Review
- Hospital CEO Report
- Hospital CFO Report
- Health IT & CIO Report
- Clinical Leadership
- Revenue Cycle Management
- Digital Innovation Report
- Supply Chain
- Payer Issues
- Pharmacy Report
- Women's Leadership
- Laboratory Review
- Cardiology Report
- Oncology Report
- HR + Talent Review
- Post Acute Report
- Life Sciences Report
- Behavioral Health Report
- Marketing Report
- Events ►
- Upcoming Conferences and Events
- 21st Annual Spine, Orthopedic and Pain Management-Driven ASC + The Future of Spine Conference
- Spring Future of Dentistry Roundtable
- 9th Annual Health IT + Digital Health + RCM Annual Meeting: The Future of Business and Clinical Technologies
- Becker's ASC 30th Annual Meeting: The Business and Operations of ASCs
- Fall Future of Dentistry Roundtable
- Fall Payer Issues Roundtable
- 12th Annual CEO + CFO Roundtable
- 15th Annual Meeting
- Exhibiting & Sponsoring
- Call for Speakers
- Virtual Events ►
- Upcoming Virtual Events
- Transform Hospital Operations Virtual Summit
- Infusion Center Operations Virtual Summit
- CEO + CFO Virtual Forum
- Revenue Cycle Management Virtual Event
- Oncology Virtual Forum
- AI + Digital Health Virtual Event
- Digital Innovation + Patient Experience and Marketing Virtual Event
- Dental + DSO Virtual Event
- Human Resources + Talent Virtual Event
- 9th Annual Health IT + Digital Health + RCM Virtual Event
- 12th Annual CEO + CFO Roundtable Virtual Event
- Oncology Virtual Summit
- Past Virtual Events
- Webinars ►
- Upcoming Webinars
- OnDemand Webinars
- Partner Content ►
- Current Partner Content
- Podcasts ►
- Our Podcasts
- Becker's Healthcare Podcast Episodes
- Becker’s Digital Health + Health IT Podcast
- Becker’s Payer Issues Podcast
- Podcast Summaries
- Becker's Behavioral Health Podcast
- Becker's Ambulatory Surgery Centers Podcast
- Becker's Spine and Orthopedics Podcast
- Becker's Dental + DSO Review Podcast
- Becker’s Clinical Leadership Podcast
- Becker’s Pediatric Leadership Podcast
- Becker's Cardiology + Heart Surgery Podcast
- Becker's Women's Leadership Podcast
- Lists ►
- Nominations
- Sign up for list nomination updates
- Print ►
- Current Issue
- Past Issues
- Current Issue - Becker's Clinical Leadership
- Past Issues - Becker's Clinical Leadership
- Multimedia ►
- Intuitive + Becker's Content Hub
- NRC Health Content Hub
- Now is the Time
- LeanTaaS AI Solutions
- Healthcare Upside/Down Podcast Series
- Featured Content
- Career Center
- Mass General Brigham
- AMN Healthcare
- About Us ►
- About Becker's Hospital Review
- Careers at Becker's
- Request Media Kit
- Content Specifications
- Most Read ►
- Texas hospital to close, lay off 94
The cost of unnecessary hospital days in 8 numbers
- California to redirect more than $7B in healthcare funding
- 2-midnight rule could affect 20% of Medicare Advantage patients
- Op-ed: Would leaders choose Steward hospitals for care?
- Kaiser to sell $3.5B in PE funds: WSJ
- Steward employee payment delayed over 'processing error'
- Optum forgoes physician noncompetes at Oregon medical group
- 20 things to know about site-neutral payment policies
- Kaiser posts $935M operating profit in Q1
- Top 40 Articles ►
- 100 great hospitals in America | 2019
- 29 hospitals, health systems cutting jobs
- 30 health systems with strong finances
- UPMC to lay off around 1,000 employees
- From -6.8% to 12.2%: 43 health systems ranked by operating margins
- As Steward's finances stumble, spotlight turns to CEO's yachts
- 12 hospital closures in 2024
- 418 rural hospitals at risk of closure, breakdown by state
- 15 health systems with strong finances
- Steward plans sale of all hospitals, reports $9B in debt
- Steward files for bankruptcy
- Ascension continues selling spree
- From -10.6% to 11.1%: 34 systems ranked by operating margins
- Iowa hospital blames EHR install for bankruptcy
- Rush lays off admin, leadership staff
- Walmart Health to close all 51 health clinics, virtual care
- Biden's $7.3 trillion budget: 16 healthcare takeaways
- Louisiana hospital closes after licenses revoked
- Tennessee hospital to close March 9
- Another Texas hospital files for bankruptcy
- Optum, SSM Health end partnership
- 20 hospitals, systems where charity care exceeds tax breaks
- 10 health systems with strong finances
- California hospital to lose Medicare contract
- Optum didn't build hospitals — it hired their employees
- 2 Nebraska hospitals abruptly close, 72 laid off
- 'A crisis of your creating': UnitedHealth CEO grilled by Congress on cyberattack
- A leading money loser for hospitals: Kaufman Hall
- 60 Florida system execs take buyout
- Texas hospital closes ER abruptly
- Jackson Health lays off hospital CEO, staff amid financial woes
- CHS' highest-earning executives in 2023
- New York mulls closure of SUNY Downstate
- 'Everyone is nervous': Indiana system CEO on rising hospital closures
- Closed New York hospital up for auction
- Steward looks to transfer all 9 Massachusetts hospitals amid lawmaker backlash
- Hospitals' Medicare Advantage problem hits an inflection point
- Steward to sell 'highly desired' physician group to Optum
- Nearly half of health systems are considering dropping Medicare Advantage plans
Financial Management
Hospitals across the U.S. are having capacity issues, leading to unnecessary stays and higher costs overall.
Kaufman Hall reported in a February 2024 analysis associated lower length of stay as one of with top financial performance because patients are able to move through the hospital more efficiently and incur lower unnecessary costs. In the most recent " National Hospital Flash Report " for April 2024, Kaufman Hall reported average length of stay for the month dropped 5% since 2021 but has been relatively flat year over year.
"We also have learned over the past several decades that an intense focus on improving length of stay has always been a winner," wrote Kenneth Kaufman, managing director and chair of Kaufman Hall, in a May 8 post . "Hospitals that put in place the structures, processes and technologies; hospitals that have true executive commitment to this issue–these hospitals have a significant advantage when it comes to financial performance."
Patient stays can be extended for a variety of reasons, including inefficient discharge processes, staff shortages, miscommunications and lack of post-acute beds for patients who can't be discharged home.
Here are seven points on the costs associated with unnecessarily extending length of stay.
1. The average 425-bed hospital would save more than $20 million per year in operating expenses by cutting out the costs associated with unnecessary days in the hospital, according to Mr. Kaufman's blog post.
2. Moving patients through the hospital quickly opens up additional space for other patients. For a 425-bed hospital with an average $4,500 margin per admission, dropping the length of stay by one day would add $20 million in additional margin because the hospital could accommodate more patients, according to the Kaufman Hall's report.
3. Less efficient hospitals may decide to add beds or expand capacity to accommodate patients, which has a hefty price tag. New construction typically costs around $2 million to $3 million per bed.
4. The average adjusted expenses per inpatient day at hospitals was $3,025 in 2022, according to the most recent data from Kaiser Family Foundation. At that rate, one patient staying an unnecessary day at the hospital for each of the 365 days per year totals $1.1 million in extra costs.
5. The Healthcare Association of New York State examined data from 52 hospitals and found 60,000 delay days from April to June 2022, estimating associated costs of $169 million.
6. The California Hospital Association released a report in February estimating 1 million days of unnecessary inpatient care and 7.5 million wasted emergency department hours due to discharge delays in the last year. The CHA estimated delays totaled $3.25 billion in "avoidable" healthcare costs per year at California hospitals.
7. The Minnesota Hospital Association said hospitals and health systems lost $487 million to delayed discharges in 2023. MHA also found more than 76,000 days of unnecessary hospital care in the first five months of the year; 67% of Minnesota hospitals reported operating losses for the first half of the year.
Hospitals zeroing in on lowering the length of stay are seeing financial benefits. Siri Nelson, president and CEO of Marshall Medical Center in Placerville, Calif., said reducing and managing length of stay has been a key initiative for clinical and administrative staff in the last year. In 2023, the team was able to hit their goal of an average length of stay under 4 days.
"Our success has been driven through a combination of training, education and workflow improvements to ensure timely action on care management decision-making," said Ms. Nelson. "Underpinning all of this has been a strong emphasis on the importance of team-based care."
The most consistent issue delaying discharge in the last year was difficulty obtaining durable medical equipment and skilled nursing facility placement, driven by payer delays.
Copyright © 2024 Becker's Healthcare. All Rights Reserved. Privacy Policy . Cookie Policy . Linking and Reprinting Policy .
Featured Learning Opportunities
- Whitepapers
- Finance Whitepapers
- Process Improvement Whitepapers
- Health IT Whitepapers
- Clinical Whitepapers
- Payer Whitepapers
- Other Learning Opportunities
- Finance Webinars
- Process Improvement Webinars
- Health IT Webinars
- Clinical Webinars
- Payer Webinars
- Virtual Events
- ASC/Spine Whitepapers
- Dental Whitepapers
- ASC/Spine Webinars
- Dental Webinars
- Hospital Review Virtual Events
- ASC/Spine Virtual Events
- Dental Virtual Events
Featured Whitepapers
Featured webinars.
Becker's Websites
Virtual Learning
Conferences
- 9th Annual Health IT + Digital Health + RCM Meeting: The Future of Business and Clinical Technologies
- 1.800.417.2035
- [email protected]
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Perspective
When pto stands for 'pretend time off': doctors struggle to take real breaks.
Mara Gordon

A survey shows that doctors have trouble taking full vacations from their high-stress jobs. Even when they do, they often still do work on their time off. Wolfgang Kaehler/LightRocket via Getty Images hide caption
A survey shows that doctors have trouble taking full vacations from their high-stress jobs. Even when they do, they often still do work on their time off.
A few weeks ago, I took a vacation with my family. We went hiking in the national parks of southern Utah, and I was blissfully disconnected from work.
I'm a family physician, so taking a break from my job meant not seeing patients. It also meant not responding to patients' messages or checking my work email. For a full week, I was free.
Taking a real break — with no sneaky computer time to bang out a few prescription refill requests — left me feeling reenergized and ready to take care of my patients when I returned.
But apparently, being a doctor who doesn't work on vacation puts me squarely in the minority of U.S. physicians.
Research published in JAMA Network Open this year set out to quantify exactly how doctors use their vacation time — and what the implications might be for a health care workforce plagued by burnout, dissatisfaction and doctors who are thinking about leaving medicine.
"There is a strong business case for supporting taking real vacation," says Dr. Christine Sinsky , the lead author of the paper. "Burnout is incredibly expensive for organizations."

Shots - Health News
Health workers know what good care is. pandemic burnout is getting in the way.
Researchers surveyed 3,024 doctors, part of an American Medical Association cohort designed to represent the American physician workforce. They found that 59.6% of American physicians took 15 days of vacation or less per year. That's a little more than the average American: Most workers who have been at a job for a year or more get between 10 and 14 days of paid vacation time , according to the U.S. Bureau of Labor Statistics.
However, most doctors don't take real vacation. Over 70% of doctors surveyed said they worked on a typical vacation day.
"I have heard physicians refer to PTO as 'pretend time off,'" Sinsky says, referring to the acronym for "paid time off."
Sinsky and co-authors found that physicians who took more than three weeks of vacation a year had lower rates of burnout than those who took less, since vacation time is linked to well-being and job satisfaction .
And all those doctors toiling away on vacation, sitting poolside with their laptops? Sinsky argues it has serious consequences for health care.
Physician burnout is linked to high job turnover and excess health care costs , among other problems.
Still, it can be hard to change the culture of workaholism in medicine. Even the study authors confessed that they, too, worked on vacation.
"I remember when one of our first well-being papers was published," says Dr. Colin West , a co-author of the new study and a health care workforce researcher at the Mayo Clinic. "I responded to the revisions up at the family cabin in northern Minnesota on vacation."
Sinsky agreed. "I do not take all my vacation, which I recognize as a delicious irony of the whole thing," she says.
She's the American Medical Association's vice president of professional satisfaction. If she can't take a real vacation, is there any hope for the rest of us?
I interviewed a half dozen fellow physicians and chatted off the record with many friends and colleagues to get a sense of why it feels so hard to give ourselves a break. Here, I offer a few theories about why doctors are so terrible at taking time off.
We don't want to make more work for our colleagues
The authors of the study in JAMA Network Open didn't explore exactly what type of work doctors did on vacation, but the physicians I spoke to had some ideas.
"If I am not doing anything, I will triage my email a little bit," says Jocelyn Fitzgerald , a urogynecologist at the University of Pittsburgh who was not involved in the study. "I also find that certain high-priority virtual meetings sometimes find their way into my vacations."
Even if doctors aren't scheduled to see patients, there's almost always plenty of work to be done: dealing with emergencies, medication refills, paperwork. For many of us, the electronic medical record (EMR) is an unrelenting taskmaster , delivering a near-constant flow of bureaucratic to-dos.
When I go on vacation, my fellow primary care doctors handle that work for me, and I do the same for them.
But it can sometimes feel like a lot to ask, especially when colleagues are doing that work on top of their normal workload.
"You end up putting people in kind of a sticky situation, asking for favors, and they [feel they] need to pay it back," says Jay-Sheree Allen , a family physician and fellow in preventive medicine at the Mayo Clinic.
She says her practice has a "doctor of the day" who covers all urgent calls and messages, which helps reduce some of the guilt she feels about taking time off.
Still, non-urgent tasks are left for her to complete when she gets back. She says she usually logs in to the EMR when she's on vacation so the tasks don't pile up upon her return. If she doesn't, Allen estimates there will be about eight hours of paperwork awaiting her after a week or so of vacation.
"My strategy, I absolutely do not recommend," Allen says. But "I would prefer that than coming back to the total storm."
We have too little flexibility about when we take vacation
Lawren Wooten , a resident physician in pediatrics at the University of California San Francisco, says she takes 100% of her vacation time. But there are a lot of stipulations about exactly how she uses it.
She has to take it in two-week blocks — "that's a long time at once," she says — and it's hard to change the schedule once her chief residents assign her dates.
"Sometimes I wish I had vacation in the middle of two really emotionally challenging rotations like an ICU rotation and an oncology rotation," she says, referring to the intensive care unit. "We don't really get to control our schedules at this point in our careers."
Once Wooten finishes residency and becomes an attending physician, it's likely she'll have more autonomy over her vacation time — but not necessarily all that much more.
"We generally have to know when our vacations are far in advance because patients schedule with us far in advance," says Fitzgerald, the gynecologist.
Taking vacation means giving up potential pay
Many physicians are paid based on the number of patients they see or procedures they complete. If they take time off work, they make less money.
"Vacation is money off your table," says West, the physician well-being researcher. "People have a hard time stepping off of the treadmill."
A 2022 research brief from the American Medical Association estimated that over 55% of U.S. physicians were paid at least in part based on "productivity," as opposed to earning a flat amount regardless of patient volume. That means the more patients doctors cram into their schedules, the more money they make. Going on vacation could decrease their take-home pay.
But West says it's important to weigh the financial benefits of skipping vacation against the risk of burnout from working too much.
Physician burnout is linked not only to excess health care costs but also to higher rates of medical errors. In one large survey of American surgeons , for example, surgeons experiencing burnout were more likely to report being involved in a major medical error. (It's unclear to what extent the burnout caused the errors or the errors caused the burnout, however.)
Doctors think they're the only one who can do their jobs
When I go on vacation, my colleagues see my patients for me. I work in a small office, so I know the other doctors well and I trust that my patients are in good hands when I'm away.

Doctors have their own diagnosis: 'Moral distress' from an inhumane health system
But ceding that control to colleagues might be difficult for some doctors, especially when it comes to challenging patients or big research projects.
"I think we need to learn to be better at trusting our colleagues," says Adi Shah , an infectious disease doctor at the Mayo Clinic. "You don't have to micromanage every slide on the PowerPoint — it's OK."
West, the well-being researcher, says health care is moving toward a team-based model and away from a culture where an individual doctor is responsible for everything. Still, he adds, it can be hard for some doctors to accept help.
"You can be a neurosurgeon, you're supposed to go on vacation tomorrow and you operate on a patient. And there are complications or risk of complications, and you're the one who has the relationship with that family," West says. "It is really, really hard for us to say ... 'You're in great hands with the rest of my team.'"
What doctors need, says West, is "a little bit less of the God complex."
We don't have any interests other than medicine
Shah, the infectious disease doctor, frequently posts tongue-in-cheek memes on X (formerly known as Twitter) about the culture of medicine. Unplugging during vacation is one of his favorite topics, despite his struggles to follow his own advice.
His recommendation to doctors is to get a hobby, so we can find something better to do than work all the time.
"Stop taking yourself too seriously," he says. Shah argues that medical training is so busy that many physicians neglect to develop any interests other than medicine. When fully trained doctors are finally finished with their education, he says, they're at a loss for what to do with their newfound freedom.
Since completing his training a few years ago, Shah has committed himself to new hobbies, such as salsa dancing. He has plans to go to a kite festival next year.
Shah has also prioritized making the long trip from Minnesota to see his family in India at least twice a year — a journey that requires significant time off work. He has a trip there planned this month.
"This is the first time in 11 years I'm making it to India in summer so that I can have a mango in May," the peak season for the fruit, Shah says.
Wooten, the pediatrician, agrees. She works hard to develop a full life outside her career.
"Throughout our secondary and medical education, I believe we've really been indoctrinated into putting institutions above ourselves," Wooten adds. "It takes work to overcome that."
Mara Gordon is a family physician in Camden, N.J., and a contributor to NPR. She's on X as @MaraGordonMD .
- American Medical Association

COMMENTS
The risk reduction was largest at 30 days after discharge among patients in the moderate (37 fewer readmissions per 1,000 discharges) and high (72 fewer hospital readmissions per 1,000 discharges) morbidity subgroups. The independent and joint effects by type of physician visit are also shown in Table 2. At 21 days after discharge, 80 fewer ...
A very important checkup is blood sugars for newly diagnosed diabetics or diabetic patients with any medication changes. In the end, most follow-up visits after discharge are just a check up to see how the patient is doing and ensure there aren't any complications. It's also a great time to talk to a primary care provider about anything ...
7 tips for a successful transition from hospital to home. Whether you or a loved one needs help planning a hospital discharge, here are a few helpful strategies to make going home from the hospital as easy as possible. 1. Plan ahead. Proper planning and support are essential for a smooth transition of care from hospital to home.
Hospital discharge planning is a process that determines the kind of care you need after you leave the hospital. Discharge plans can help prevent future readmissions, and they should make your move from the hospital to your home or another facility as safe as possible. Medicare requires hospitals to screen inpatients and provide discharge ...
This program, coupled with a telephone assessment performed by a case manager, has reduced 30-day hospital readmission rates from 14 percent to 6 percent. CareMore Health Plan and Medical Group in California has shifted the performance of post-hospital follow-up care from primary care physicians to its hospitalists.
The IDEAL Discharge Planning strategy highlights the key elements of engaging the patient and family in discharge planning: Include the patient and family as full partners in the discharge planning process. Discuss with the patient and family five key areas to prevent problems at home:
You should get a form from the hospital titled "An Important Message from Medicare," which explains how to appeal a hospital discharge decision. Note: Appeals are free and generally resolved in 2 to 3 days. The hospital cannot discharge you until the appeal is completed.
inpatient with a doctor's order. The day before you're discharged is your last ... and copayments, visit Medicare.gov. You can also call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048. ... • If you don't have a 3-day inpatient hospital stay and you need care after your discharge from a hospital, ask if you can get ...
Detailed hospital discharge plans help make transitions of care safer for ... studies show it is often difficult to predict the day of discharge accurately, 5 which may contribute to the practice of communicating important information ... looking beyond cost and regimen complexity. Am J Geriatr Pharmacother. 2011;9(1):11-23. [Free full text ...
In an annual basis, expenditures were $16.3 billion for hospital readmissions up to 30 days after discharge, and $97.2 billion for readmissions up to one year after discharge (findings not shown). While much of the policy focus has been on changing payment incentives in Medicare to decrease readmissions, private insurance pays for a greater ...
The cumulative incidence of post-discharge follow-up visits for HF patients generally increased (i.e., shifted upward) from 2007-2010 (Exhibit 2). For example, in 2010, 54.6% of HF patients had a follow-up visit within 10 days of discharge compared to 47.9% in 2007.
Inpatient after your admission. Your inpatient hospital stay and for most hospitals, all related outpatient services provided during the 3 days before your admission date. Your doctor services : You go to a hospital for outpatient surgery, but they keep you overnight for high blood pressure. Your doctor doesn't write an order to admit you as an ...
Primary nurse telephoned the patient 2 days after discharge, patient given an appointment to attend the primary care clinic within one week of discharge. ... Effect of discharge planning on hospital resource use and cost, Outcome 2: Primary and community care resource use and cost. ... Median time from hospital discharge to the first visit ...
INTRODUCTION. Discharging patients from the hospital is a complex process that is fraught with challenges and involves over 35 million hospital discharges annually in the United States [].The cost of unplanned readmissions is 15 to 20 billion dollars annually [].Preventing avoidable readmissions has the potential to profoundly improve both the quality of life for patients and the financial ...
Conduct a follow-up visit within 7 or 14 days of discharge, depending on the complexity of medical decision making involved. The face-to-face visit is part of the TCM service and should not be ...
In each benefit period , you pay:. A $1,632 deductible .; Days 1-60: $0 after you meet your Part A deductible.; Days 61-90: A $408 coinsurance amount each day.; After day 90: An $816 coinsurance amount each day while using your 60 lifetime reserve days.; After you use all of your lifetime reserve days, you pay all costs.
After the person pays their deductible, Medicare inpatient coverage begins. However, depending on the length of their stay, a person may need to pay coinsurance out of pocket, as follows: Days in ...
INTRODUCTION. Early follow-up after hospital discharge provides an opportunity to assess patient health and to provide care to reduce adverse health outcomes and 30-day readmissions. 1 - 8 Medical researchers have therefore identified barriers to early follow-up (e.g., limited resources to coordinate follow-up care, patient non-compliance) and designed interventions to promote follow-up. 1 ...
There is no significant difference in satisfaction between nurse-led telephone follow-ups and outpatient visit ... Trained staff will review patients' charts and reach out to patients 2, 7, 14, and 31 days post-discharge. They discuss durable medical equipment, medication needs and education, primary care provider appointments, continued ...
Objective To determine any changes in total hospital revisits within 30 days of discharge after a hospital stay for medical conditions targeted by the Hospital Readmissions Reduction Program (HRRP). Design Retrospective cohort study. Setting Hospital stays among Medicare patients for heart failure, acute myocardial infarction, or pneumonia between 1 January 2012 and 1 October 2015 ...
Information on hospital return days helps you evaluate a hospital's quality of care based on how much time patients spend back in the hospital during the first 30 days after discharge. For example, hospitals with fewer than average days are likely arranging timely follow-up, ensuring that patients have the proper medicines, and releasing ...
At that rate, one patient staying an unnecessary day at the hospital for each of the 365 days per year totals $1.1 million in extra costs. 5. The Healthcare Association of New York State examined ...
Researchers surveyed 3,024 doctors, part of an American Medical Association cohort designed to represent the American physician workforce. They found that 59.6% of American physicians took 15 days ...