
Navigating the IVF Process: Key Insights to managing the IVF Timeline and work-life balance
by Dr. John Preston Parry | Nov 9, 2023 | Doctor's Blog

Embarking on fertility treatments can be a demanding process that requires significant emotional, financial, and time commitments.
Understanding fertility treatments is the first step in what may be one of the most important journeys you’ll take as a couple. It’s about creating life and expanding your family. We’re here to guide you through the myriad of fertility treatments available today, providing you with a clear, supportive pathway to parenthood and helping you understand the potential demands and how they might intersect with your career.
How long does the IVF process take from start to finish?
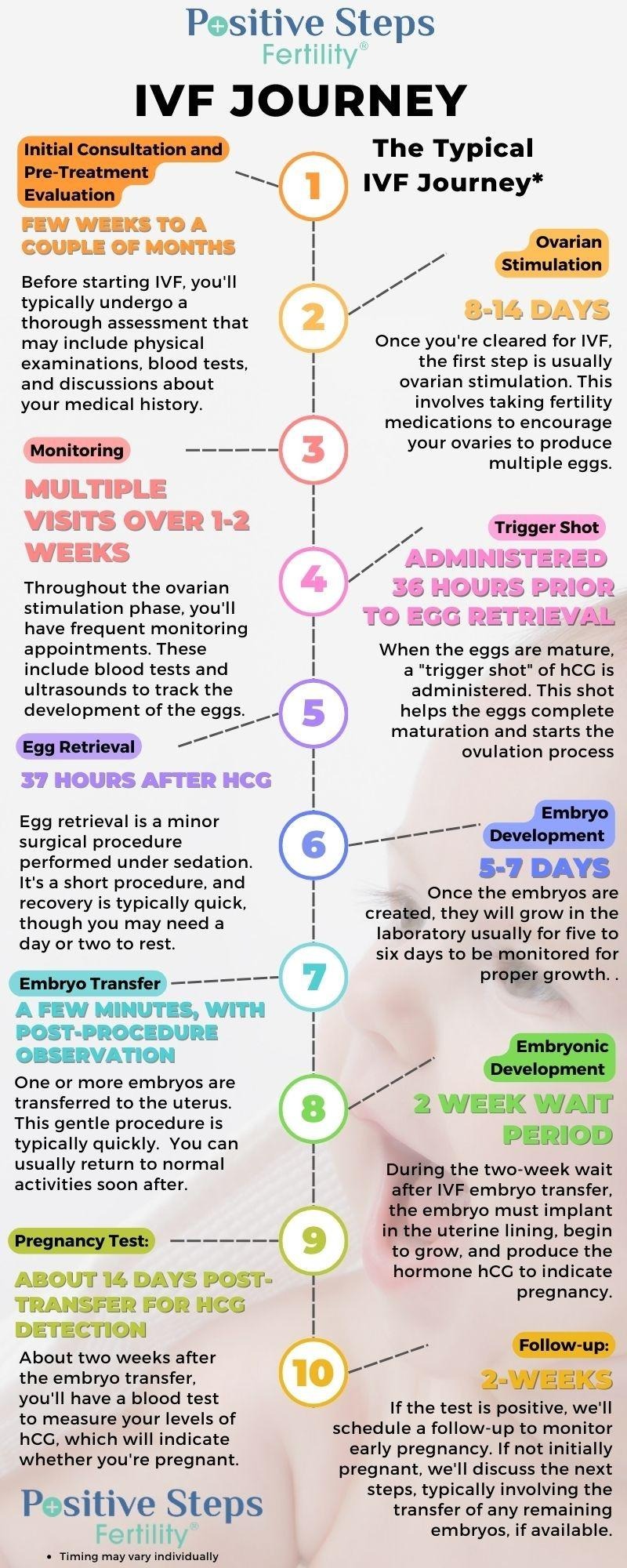
Begin by educating yourself about the IVF process. Knowing the step-by-step process, from initial consultations to procedures and follow-ups, can help you anticipate and schedule necessary time off.
The typical IVF (In Vitro Fertilization) treatment timeline is a multi-step process that usually spans several weeks. Each cycle of IVF includes multiple stages, although the exact timeline can vary based on individual circumstances and protocols of the fertility clinic.
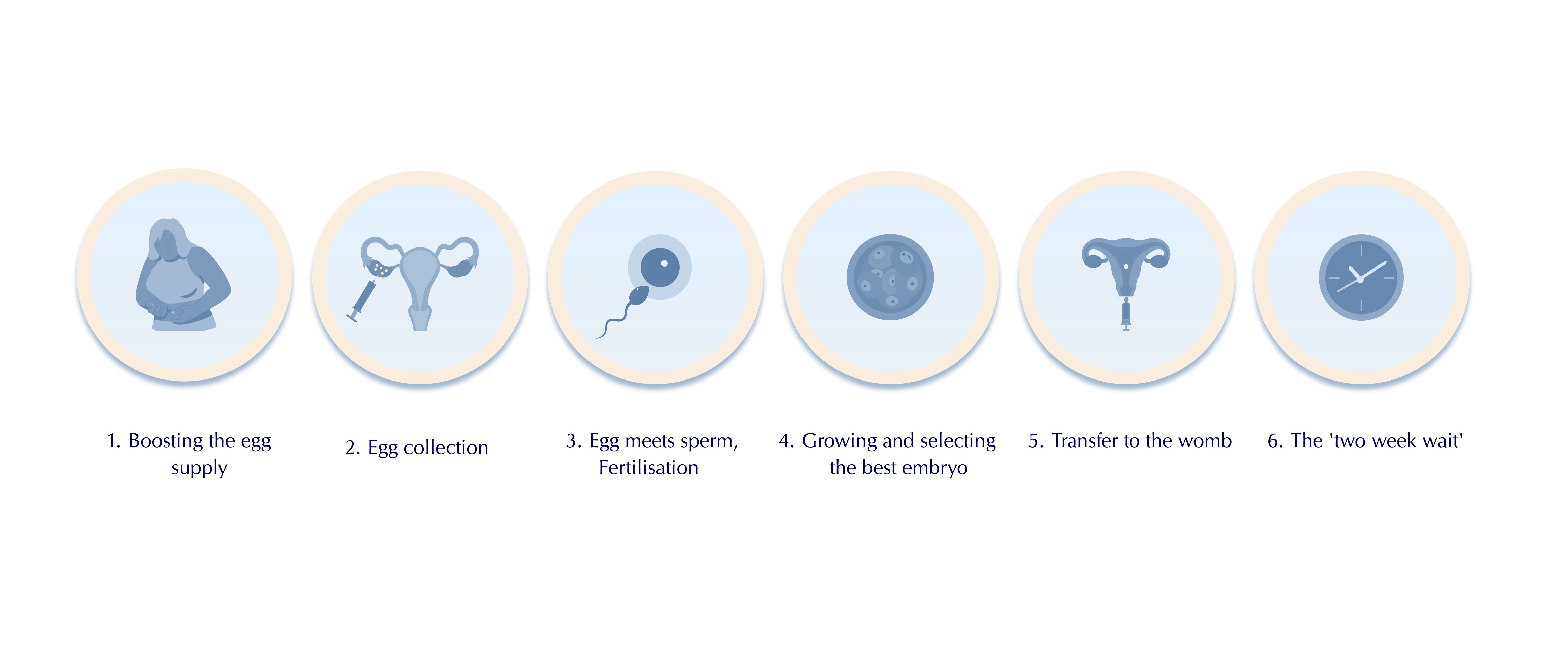
An IVF cycle typically includes the following steps or procedures:
- Medications to grow multiple eggs
- Retrieval of eggs from the ovary or ovaries
- Insemination of eggs with sperm
- Culture of any resulting fertilized eggs (embryos)
- Placement (“transfer”) of one or more embryo(s) into the uterus
- Support of the uterine lining with hormones to permit and sustain pregnancy
The IVF Process and Timeline
Embarking on the journey of in vitro fertilization (IVF) can be filled with hope and anticipation, yet it’s important to acknowledge that every couple’s path to parenthood is unique. The timeline we provide here outlines a typical IVF process, but it’s tailored with flexibility to meet your specific circumstances.
As you step forward, remember that each phase is approached with your individual needs in mind, ensuring that your journey is as smooth and successful as possible. While timelines may shift, our commitment to your family’s dream remains steadfast.
*Please note that all timelines are approximate and can vary based on individual health profiles and responses to treatment.
Navigating Work-Life Balance During Your IVF Journey
Embarking on in vitro fertilization (IVF) can feel like taking on a second full-time job. Balancing your career while undergoing IVF requires careful planning, open communication, and self-compassion. Here are some strategies to help you maintain equilibrium between your professional life and IVF treatment.
Communicate with Your Employer
If you feel comfortable, have a candid conversation with your employer or HR department about your IVF journey. Many are willing to offer flexibility once they understand the significance and requirements of the process. You’re not obligated to disclose all the details, but providing some insight can lead to accommodations like flexible hours or remote work opportunities.
Flexibility in Your Work Schedule
Look into flexible working arrangements. Flextime, compressed workweeks, or the possibility of working from home on certain days can reduce the stress of juggling work and IVF appointments. It’s crucial to arrange this in advance to minimize the impact on your professional responsibilities.
Prioritize and Delegate
Evaluate your work tasks and prioritize them. Consider what can be delegated or what projects can be put on hold. By focusing on critical tasks, you ensure your work quality remains high, which can relieve some of the pressure during your IVF treatment.
Protect Your Personal Time
Resist the urge to overcompensate at work for the time taken off for IVF procedures. Protect your personal time by setting boundaries and avoiding the pitfall of working late hours or during weekends. This time is vital for rest and recuperation.
Plan for the Unexpected
IVF can be unpredictable, with last-minute changes or unexpected outcomes. Have a contingency plan for work projects and deadlines in case you need to adjust your schedule suddenly.
Understanding Your Legal Rights in the IVF Process
Deciding to embark on an IVF journey is a monumental, intimate decision, often reached after considerable reflection and, in many cases, profound emotional challenges. While navigating the intense emotions and the deluge of medical details, you must not overlook another significant element: the complexities of the legal framework surrounding Assisted Reproductive Technology (ART) and IVF. To learn more, check out our blog on the 7 Fertility Legal Insights To Avoid Common Pitfalls .
Navigating the Emotional Landscape of IVF
The stress of fertility treatments can affect your emotional well-being and your performance at work. Tools for stress management, such as those recommended by ACOG, can be valuable resources to help you maintain your composure and focus.
According to OBGYN Nazanin E. Silver , “Before starting infertility treatment, I encourage couples to discuss what they will do if initial treatments don’t work. Would you ever consider adoption? Would your partner? You can talk through scenarios together, and it may help to consider couples therapy.”
In a recent blog , we discuss how the American College of Obstetricians and Gynecologists (ACOG) highlights that the emotional impact of infertility often mirrors that of other significant medical conditions such as cancer or heart disease. You might oscillate between feelings of denial, anger, guilt, depression, and acceptance, all of which can be overwhelming and stressful.
In a recent interview with a Positive Steps patient, the couple noted, “The most crucial advice we can offer is to remember that you are not alone. The struggle with infertility can often feel isolating, but it’s important to know that you are part of a community that understands your journey and stands with you.”
Embracing Self-Care During Your IVF Journey
Self-Care is Non-Negotiable. Amid the demands of IVF and work, self-care should be a priority. At the heart of your fertility journey is a commitment to nurturing your own well-being to enhance your fertility and increase the prospects of a successful pregnancy. Self-care in this context means taking thoughtful steps toward improving your overall health and creating the best possible environment for conception.
One of the primary self-care measures involves reviewing and potentially altering medication use, with professional guidance, to avoid substances that may hinder fertility or cause developmental issues. A healthcare provider can help determine which medications are safe to continue and which to suspend during preconception and beyond.
Maintaining a healthy body weight is also crucial, as weight can influence hormonal balance and fertility. A balanced diet and regular exercise not only support reproductive health but also improve mental well-being, a key factor in the fertility journey.
Moderation is the operative word when it comes to alcohol consumption. Reducing intake can have a positive impact on fertility, and it’s a change that partners can undertake together as part of their shared journey toward parenthood.
Furthermore, understanding the significance of timing in your sexual routine can be empowering. Aligning sexual activity with the most fertile periods can naturally increase the chances of pregnancy.
Lastly, addressing additional personal health factors, such as stress levels, sleep patterns, and other lifestyle choices, is essential. Each element of your lifestyle has the potential to affect fertility, and making positive changes can contribute to a healthier conception.
By integrating these self-care practices into your routine, you are taking control of what you can on your path to parenthood. It’s a journey that extends beyond the physical aspects of fertility to encompass the nurturing of your body, mind, and relationship.
Building a Support System: The Key to IVF Success
Navigating the complexities of fertility treatments can be emotionally taxing. During this period, a robust support system becomes invaluable. While the workplace may offer one avenue of support, expanding your search for understanding and solidarity beyond professional circles can provide comfort and connection.
At Positive Steps Fertility we are dedicated to helping individuals and couples get the support they need. These groups provide a safe space to share experiences, offer and receive advice, and foster a sense of companionship on the journey to parenthood.
It’s also important to consider the support that can come from close friends, family members, and even online forums. These personal connections can offer different perspectives and kinds of support. While friends and family provide a personal touch, online communities can offer anonymity and a broader range of experiences.
Counseling services, whether individual or as a couple, can also play a critical role in your support network. Professional therapists, particularly those specializing in fertility issues, can guide you through the emotional complexities that arise during this time, helping you to develop coping strategies and maintain mental and emotional wellness.
Remember, seeking and accepting support is not a sign of weakness; it’s a proactive step toward ensuring your emotional resilience as you navigate your fertility journey.
Preparing Financially for Your IVF Treatment
Costs associated with fertility treatments can add another layer of stress when balancing work life. At Positive Steps Fertility, our goal is to provide the highest quality fertility treatment at the most transparent and affordable cost. We understand that each fertility journey is unique, and we’re committed to getting to know you personally and designing a treatment plan that aligns with your family goals and budget. We aim to provide all the information and transparency you need to make informed decisions. So, if you have any questions, please do not hesitate to call us at 855-759-4124 or email us at [email protected] to learn more.
Embracing the IVF Journey with Confidence and Clarity
At Positive Steps Fertility, we understand that your fertility journey is just one part of your larger life tapestry, which includes your professional aspirations. As you move forward with treatments, we’re here to support you in harmonizing your career goals with the path to parenthood.
With Positive Steps Fertility, you can be assured that while you strive for success in your professional life, we are working alongside you, dedicating our expertise to help you achieve your most cherished personal goal—building a family.
Site Search

Connect with Us

Positive Steps Fertility Videos:

Recent Posts
- 5 Ways Lifestyle Factors Can Impact Your Fertility
- Battling the Shadows: The Intense War on Hormonal Imbalances and Infertility
- Your First Fertility Appointment: From Anxiety to Answers
- Fertility Under Fire: How Alabama’s Frozen Embryo Ruling Affects Hopeful Parents
- Unlocking the Science of Timed Intercourse
Our Response to the Alabama IVF Ruling
« View All Posts
How Long Does the IVF Process Take? The Timeline From Start to Finish
August 22nd, 2023 | 12 min. read
By Christina Dias, RN, BSN

Navigating the complexities of IVF isn't easy, and the abundance of information you need to absorb might leave you feeling overwhelmed. In this comprehensive guide, we will explore how long the IVF process takes and what you need to know - every step of the way.
In this article: How long does the IVF process really take? Preparing for IVF Treatment 5 Things to Do Before Starting IVF Why Preconception Health is Essential The 4 Stages of an IVF Cycle What might make my IVF cycle take longer? How long does it take an embryo to implant after transfer? How long after embryo transfer will I know if I’m pregnant?
How long does the IVF process really take?
You’ve made the decision to seek the help of a fertility specialist – which is a huge step towards achieving your family-building goals. At this point, you are likely eager to get the process started, and may be wondering: how long will IVF treatment take from start to finish?
As Illume Fertility's Director of Nursing , with many years of fertility nursing experience, I'm here to break it all down for you and - hopefully - make it a little less intimidating.
Before we dive in, let's talk about some actionable steps you can take right now to prepare for fertility treatment . As any fertility patient will tell you, this stage of the process takes time - lots of communication, consultations, phone calls, and decisions happen well before you do your first injection.
While the IVF cycle itself only takes around 4 weeks, the full process (including your preconception health regimen and fertility testing) can take up to 4 months , from your initial consultation to when you have your first beta hCG test to see if you’re pregnant.
Preparing for IVF Treatment
To give you the absolute best chance at a successful IVF cycle and healthy pregnancy, we begin by performing a variety of tests that offer a full picture of your current fertility and overall health. Fertility treatment can begin only after initial fertility testing is completed.
This will involve a medical evaluation that looks at everything from any potential genetic issues to elevated thyroid or blood sugar levels. Certain medical conditions may warrant lifestyle modifications that will make it easier for you to conceive, which can add to your timeline, but make all the difference.
Fertility testing typically includes:
- Comprehensive blood work
- Genetic carrier screening
- Transvaginal ultrasound to assess ovarian reserve
- Evaluations of the uterine cavity (SHG) and fallopian tubes (HSG)
- Semen analysis and blood work for male partner, if applicable
Did you know? Male fertility issues account for up to 40% of infertility cases! That's why evaluating the quantity and quality of sperm is essential. As sperm is produced every 64 days, focusing on preconception health is important for a male partner as well.
5 Things to Do Before Starting IVF
- Schedule your initial consultation and learn more from your doctor
- Meet with a nutritionist to give your body the very best chance at success
- Meet with a counselor who can help prepare you for the road ahead
- Connect with other fertility patients through our virtual support groups , led by Illume Fertility's Patient Advocate, Lisa Rosenthal (who also offers free, one-on-one support)
- Download our 90-Day Preconception Checklist to stay on track
Why Preconception Health is Essential
To put it simply: a healthy body has the best chance of success.
Even small changes to nutrition and lifestyle in the period leading up to IVF can increase your odds of a healthy pregnancy. For this reason, the ideal time to start focusing on your preconception wellness is around three months before the start of an IVF cycle. We have developed an easy-to-reference 90-Day Preconception Checklist for this very purpose!
During this time, you should begin your physician-approved preconception health regimen, which will likely include taking prenatal vitamins , increasing your water intake, improving your sleep hygiene, and eating a balanced and nutritious diet .
Limiting alcohol and caffeine, stopping smoking, and incorporating low-impact exercise will also prepare your body for the rigors of fertility treatment and pregnancy.
Don't forget: Now is also the perfect time to identify your emotional support network as well as inquire about your insurance benefits . Your fertility doctor will also begin testing you for various risk factors.
Trying to conceive?
Increase your chances of a healthy pregnancy by downloading our free 3-month preconception checklist and learning what steps you can take.

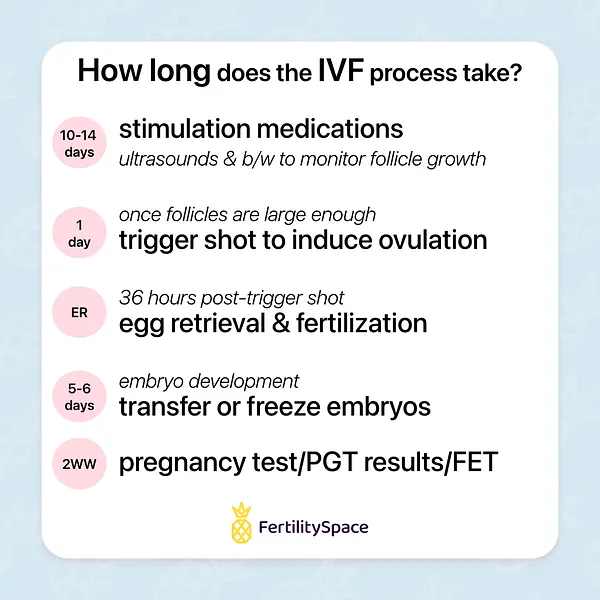
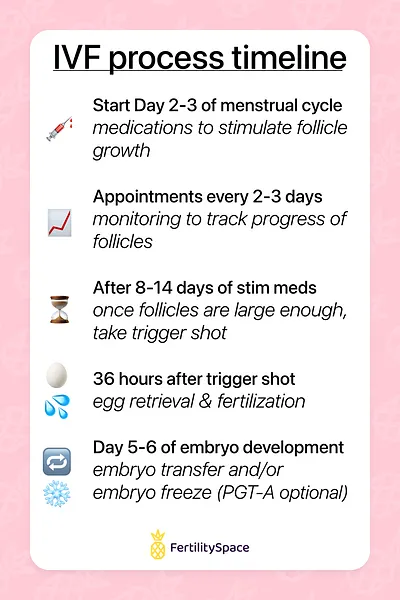
The 4 Stages of an IVF Cycle
Once diagnostic testing is complete, your IVF cycle can finally begin!
You're likely feeling a lot of conflicting emotions right now, which is completely normal. Acknowledge all the hard work you've done to get to this point, and communicate any concerns to your team as you enter your treatment cycle. Here's what to expect:
Stage 1: Oral Contraceptives
Although it may seem counterintuitive, IVF patients must take oral contraceptives (birth control) for 10-14 days prior to beginning their fertility medication protocol.
When taken before ovarian stimulation, studies have shown that oral contraceptives can increase the number of eggs available for retrieval, ensure follicles grow as a cohesive group, and support ovarian health throughout IVF.
Stage 2: Ovarian Stimulation
After completing a course of oral contraceptives, you will begin injections of fertility medication for approximately 9-11 days . These medications consist of naturally occurring hormones that help develop and mature your follicles (eggs are contained within the follicles).
The number of follicles and their size determine how many mature eggs will be available for retrieval. During this time, you should plan to be in your fertility clinic's office approximately every other day for a transvaginal ultrasound and monitoring via blood work.
Stage 3: Egg Retrieval
Egg retrieval refers to a one-day procedure where the eggs are extracted from the ovarian follicles and then handed over to the IVF lab, where they will fertilize and divide.
At Illume Fertility , we monitor the growth of your embryos in our own onsite lab. A specially-trained embryologist cares for each embryo, watching it divide and multiply for five days, at which point they transition from the "zygote" stage to the "blastocyst" stage.
Did you know? Research supports that transferring embryos into the uterus at the blastocyst stage yields better results than transferring them on Day 3 (when they're still in the less mature zygote stage).
Stage 4: Embryo Transfer
After being closely monitored in the IVF lab, an embryo will be transferred back to the uterus on Day 5. ( Egg retrieval day is considered Day 0.) This is referred to as a "fresh" transfer. If you want to wait for any reason, your embryos can be safely cryopreserved until you're ready for a "frozen" embryo transfer.
Embryo transfer is also a one-day procedure that should take approximately 20 to 30 minutes . You will be awake for this painless procedure, and will not require any anesthesia.
Following this is a waiting period to see if the embryo implants in the uterus, which typically takes 9-10 days, depending on the maturity of the embryo at the time of transfer.
What might make my IVF cycle take longer?
You've worked so hard to get to this point, and any delays in the process can feel incredibly frustrating. If your IVF cycle was delayed or cancelled (or is taking longer than expected), it's understandable to want to know why this could have happened.
Here are the three most common reasons:
#1 Poor Ovarian Response
Sometimes the body doesn’t respond as expected to IVF medications , which can delay or cancel your IVF cycle. For example, there might be a delay or cancellation if a lower number of follicles develop in the ovaries than expected, meaning fewer eggs were produced.
#2 Suboptimal Hormone Levels
Sometimes hormone levels are not ideal for continuing an IVF cycle , and delaying can actually lead to better odds of success in your next cycle.
Although this can be difficult news to receive, remember that every cycle is diagnostic, as well as therapeutic. Your fertility doctor will gain important knowledge about your body and how it responds to medication throughout each cycle, increasing your chances of success for the next one.
Remember: A poor hormonal response from this round of IVF does not mean you'll have the same fate should you decide to continue with IVF treatments . Sometimes, it just takes a little time to figure out the right protocol for your body.
Reason #3: Embryo Screening
Another reason your IVF cycle might take longer than expected is if you opt to have your embryos undergo genetic testing before transfer. This can add 4-5 weeks to the process.
Preimplantation genetic testing (PGT) can offer the highest degree of certainty for a genetically healthy child, particularly when partners are known carriers or at higher risk for passing on genetic diseases.
Whatever the reason, we understand that delays can be challenging and upsetting. Should there be a delay or cancellation, your doctor will carefully review your case and make necessary adjustments - providing support and information every step of the way.
Want our full IVF guide?
Grab our comprehensive guide to IVF to learn about how much it costs, where to find resources, and how it all works.

IVF Treatment FAQs
Have more questions about the IVF process? We've got answers!
Do I need preauthorization for IVF?
The cost of IVF is an unfortunate roadblock for the majority of people seeking treatment. The good news? An increasing number of companies offer fertility benefits, and some states even have mandated fertility coverage . (If you don't have insurance, read our guide to paying for IVF with the help of other resources, like grants, scholarships, and loans.)
Many insurance companies also provide benefits for fertility testing and procedures, though coverage varies by state and employer. Depending on the type of insurance plan you have, your policy may require that you obtain referrals or authorizations.
Beyond a simple phone call to your insurance company, we suggest requesting a written predetermination letter that outlines your fertility benefits and clarifies any specific requirements that must be met for you to be covered.
This step might be necessary for both you and your partner if you carry individual insurance. To avoid delays, seek out this information as soon as IVF becomes a consideration.
Knowing how stressful this process can be, Illume Fertility appoints you a designated Insurance & Billing Advocate to help communicate with your insurance company and understand your coverage. They will help determine your benefits, outline any out-of-pocket expenses, and review specific plan details to eliminate surprises along the way.
Why do I have to start IVF the month before my egg retrieval?
An IVF cycle corresponds with the length of a normal ovulation cycle, which is about a month long. Ovulation occurs when a mature egg is released from the ovary and "pushed" into the fallopian tube where it can be fertilized, or in the case of IVF - retrieved.
The goal of IVF is to prepare and stimulate the ovaries to produce many mature eggs for retrieval and ready your uterus for implantation. Ovarian preparation and stimulation occur at the start of and during the ovulation cycle.
How long does it take an embryo to implant after transfer?
Depending on the maturity of the embryo, it can take between 1-5 days after the transfer for the embryo to nestle into the uterine lining and successfully implant.
How long after embryo transfer will I know if I’m pregnant?
Waiting to learn if your IVF cycle was a success can be the hardest part of treatment, and it's tempting to take at-home pregnancy tests! However, it's important to know that at-home tests simply won’t be reliable if taken too early, so stay strong during that " two-week wait ."
To detect actual amounts of human chorionic gonadotropin (hCG), the hormone produced by the placenta after implantation, an in-office pregnancy blood test is performed around 9-10 days after embryo transfer .
We encourage you to practice good self care, connect with others in the same boat, and reach out for support during this often challenging waiting period!
Your IVF Experience
Remember that everyone's journey is unique.
Try not to compare your situation to anyone else's - even if they seem similar. What works for one IVF patient may not work for you. Be patient, stay connected to your team, reach out for support, and don't be afraid to ask questions. They're there to help!
We at Illume Fertility wish you all the luck on your path to parenthood, and hope this guide to the IVF process helps you feel as prepared as possible for the journey ahead.
Christina Dias, RN, BSN
Christina Dias, RN, BSN joined the team at Illume Fertility in 2004. She currently serves as our Director of Nursing, overseeing our clinical care teams. She received her Bachelor of Science in Nursing from Sacred Heart University.
No fertility coverage?
There are other ways to afford IVF treatment! Explore your options with our helpful guide.

More Fertility Resources
A twin pregnancy after years of loss & infertility | kate & mike's story.
April 26th, 2024 9 min read
Two Sets of Fraternal Twins in Three Years | Dionicio & Ruddy's Story
April 25th, 2024 8 min read
Finally Pregnant at 49: How IVF Made My Dream a Reality | Alicia's Story
April 22nd, 2024 10 min read
Trying to Conceive With a Unicornuate Uterus | Brittany's Story
April 20th, 2024 8 min read
Choosing Single Motherhood | Kaitlyn's Story
April 19th, 2024 8 min read
Our Journey to IVF Identical Twins | Christa & Aland's Story
March 27th, 2024 9 min read
23 IVF Questions to Ask a Fertility Doctor at Your First Appointment
March 20th, 2024 16 min read
Braving Recurrent Pregnancy Loss & Endometriosis | Katie's Story
March 14th, 2024 8 min read
Illume Fertility Joins the Fight to Protect IVF After Alabama Ruling
March 4th, 2024 17 min read
What Are My Chances of Success with Fertility Treatment?
February 27th, 2024 16 min read
We Don't Speak About Infertility | Shiraine's Story
February 22nd, 2024 11 min read
IVF Success After Endometriosis | Nicole's Story
February 21st, 2024 6 min read
$20,000 IVF Grants Offered to Local Families by Nest Egg Foundation
January 15th, 2024 9 min read
How Years of Infertility Led to Two Miracles | Deanna & Justin's Story
December 14th, 2023 11 min read
The Ultimate IVF Gift Guide for Fertility Warriors
December 5th, 2023 9 min read
How IVF and Genetic Testing Can Help Prevent Sickle Cell Anemia
November 29th, 2023 10 min read
From Injections to Self-Reflections: Your IVF Medication Breakdown
November 27th, 2023 13 min read
How to Pay for IVF Treatment Without Insurance
November 10th, 2023 12 min read
From Unexplained Fertility to IVF Success | Juliana & Ryan's Story
November 8th, 2023 9 min read
Becoming a Mother After Recurrent Pregnancy Loss | Alyson's IVF Story
October 25th, 2023 8 min read
Becoming a Mother After Surviving Breast Cancer | Erin's Story
October 18th, 2023 8 min read
IVF Success Stories: 44 Parents Share Their Family-Building Journeys
October 11th, 2023 14 min read
Overcoming Obstacles to Meet Our Miracle Baby | Kristen & Jeff's Story
September 15th, 2023 6 min read
In Vitro Fertilization (IVF) Step-By-Step Guide from a Fertility Nurse
August 16th, 2023 14 min read
&w=384&q=75)
0808 1961942
A typical IVF journey
&w=1920&q=75)
A typical IVF journey, whether it is for the first time or trying again, can also be called a ‘stimulated cycle’. This is because your treatment will involve taking drugs that stimulate your body so we can collect a number of eggs for fertilisation.
If you’re not sure which options are best for you, you can attend one of our FREE information events or contact your local clinic to understand your options.
1. Referrals
Your referral may come from your GP or hospital doctor, or you can self-refer. Learn more about the referrals process .
2. Pre-treatment
Preliminary fertility assessment tests and screening
To make the best decision about your treatment in the consultation, your doctor needs the results of some tests. There may be a combination of blood tests and a vaginal ultrasound scan to assess your ovaries, and a semen assessment where appropriate. Learn more about TFP fertility assessment packages .
Initial consultation
At your first consultation with a TFP fertility specialist, they will cover your medical history and explain your test results. You and your doctor will then discuss their recommended programme of treatment based on your personal results and circumstances.
3. Counselling
Counselling is available at any stage of your treatment pathway. Fertility treatment is a significant emotional journey for all patients, and counselling provides extra emotional support.
It is completely confidential. If you are going to be using donated eggs or sperm for your treatment, then you’ll be recommended to see the counsellor before starting treatment to discuss the implications for both you and any children that may be born. Learn more about fertility counselling .
4.Treatment planning appointment
At your treatment planning appointment one of our specialist fertility nurses will explain your treatment in full. You will be taken through your regime of drugs and shown how to use them.
You will have the opportunity to ask questions regarding your forthcoming treatment. It’s also the time when you officially consent to undergo fertility treatment , and we go over the legal side of things.
This is an important part of the process which ensures that your parenthood will be recognised legally after treatment. We require that everyone involved in the treatment comes to the treatment planning appointment. It generally takes 60 minutes. We use an online consent platform where you will be able to watch videos prior to electronically signing your consent. If you are funding your own treatment, you will need to pay for your treatment programme at this point. Once all the tests, consent forms and payment are completed, you are ready to start your IVF cycle. Learn more about the treatment planning appointment .
5. Starting treatment
Your treatment will start on the first day of your period. You will need to call the clinic to let us know and to receive the instruction to start the treatment plan, as explained by your fertility specialist in your consultation and nurse in your planning appointment. As you’re not undergoing ovarian stimulation, you may or may not have drugs to take in this cycle; this will be agreed upon with your doctor at your consultation. If you have a regular menstrual cycle, we will monitor you so that we can transfer the embryo(s) at the best point in your ‘natural cycle’.
6. Ovarian stimulation and monitoring
In general, treatment starts with drugs that stimulate your ovaries. This enables us to collect a number of eggs for insemination, rather than the usual single egg. The drugs are injections that can be taken at home – you’ll be shown how to do this.
Over a period of around two weeks of stimulation, you’re likely to have one to three scans and possibly blood tests, to monitor the development of the egg-producing follicles.
These are short appointments that last around 20 minutes, and the results are available later the same day. The timings are different for everyone, because treatment is tailored to suit each patient individually.
7. Trigger injection
Once your follicles are ready, the stimulation period ends with an injection that matures the eggs in the follicles to get them ready for egg collection.
8. Egg collection
The appointment to collect the eggs will take place 36-40 hours after the trigger injection. The procedure takes about half an hour, and you will be given drugs to make you sleepy during the procedure.
With the help of a scanning probe, a very fine needle is passed through the vaginal wall and into the ovary to collect the eggs. Usually, around 80% of follicles contain an egg. As you will have had sedation you cannot drive or operate machinery for 24 hours and you will need someone to stay with you.
9. Providing sperm
If your treatment uses a fresh sperm sample, it will be provided on the same day as the eggs. You provide the sample at the clinic, in one of our andrology (men’s) rooms. If you’re providing the sample via a surgical procedure, this will take place before the egg collection day, and the sample will be be frozen.
If you already have sperm in storage, or have been matched to a sperm donor, the sample will be thawed on the same day that the eggs are collected.
10. Insemination of the eggs
The sperm sample provided is prepared to ensure that the very best sperm are being used for insemination.
IVF – Prepared sperm will be added to the eggs in a culture dish.
ICSI – A single sperm will be selected and injected into each egg then put into a culture dish.
The culture dishes are placed in the incubator to allow fertilisation to take place.
11. Embryo development
The embryos are carefully monitored in the period after insemination, first to check for fertilisation, then for signs for development which indicate the embryo is growing. Time-lapse monitoring allows us to carefully monitor embryo development. Click here to learn more about time-lapse monitoring . The clinic will be able to update you on embryo development.
Shortly after egg collection, you may also start taking drugs to help prepare your uterus lining to receive an embryo (this is known as Luteal Phase Support).
If your treatment plan includes genetic testing, then this will happen during this phase.
12. Embryo transfer
The frozen embryo transfer takes place 5 days after egg collection. The embryos are monitored carefully in the Embryoscope by our Embryologists. The procedure can feel like a smear test, but it takes longer: around 15 minutes. A tiny drop of culture medium containing one or two embryos is carefully deposited in the uterus using a thin catheter.
If you decided before treatment to store any further good quality embryos for further cycles, you’ll be consulted again, and it will happen at this stage.
13. The wait
At TFP fertility clinic we appreciate how difficult this two-week wait can be. Please call us at any time if you are concerned; no worry is too small. It’s a good idea to make plans for after embryo transfer to help you feel more in control. Try to live life as normally as possible.
14. The outcome
Positive test.
If you’re pregnant, we schedule a scan in the clinic at around six to eight weeks. If everything looks good, then you’re discharged to your GP.
Negative test
If your period arrives before the test is due or if the test is negative, rest assured you are not alone.
We can meet to talk, review your treatment, and consider what the next step will be on your IVF journey. IVF conception often takes place over a number of cycles. You could be ready for a new cycle within a short time, even a couple of months if you have frozen embryos, but this is completely up to you.
Watch these 2 videos about:
What happens when a patient first starts their fertility journey with TFP?
What are the most challenging parts of the IVF journey for patients?
This service is offered in the following clinics:
&w=384&q=75)
TFP Belfast Fertility
BT3 9JQ Belfast
028 9009 7315
&w=384&q=75)
TFP 92 Harley Street
W1G 7HU London
0207 160 6379
&w=384&q=75)
TFP Boston Place Fertility
NW1 6ER London
0203 131 2152
&w=384&q=75)
TFP Wessex Fertility
SO15 5QS Southampton
0203 1318630
&w=384&q=75)
TFP Thames Valley Fertility
SL6 4BY Maidenhead
01628 702632
&w=384&q=75)
TFP Simply Fertility
CM2 8HN Chelmsford
01245 371849
&w=384&q=75)
TFP Oxford Fertility
OX4 2HW Oxford
01865 224819
&w=384&q=75)
TFP Nurture Fertility
NG10 5QG Nottingham
+44 0115 828 0246
&w=384&q=75)
TFP GCRM Fertility
G51 4FD Glasgow
0141 413 0715
&w=3840&q=75)
Ready to start your fertility journey? We're here for you
Schedule an appointment to start your fertility journey with us.

Fertility Treatments | IVF Explained
The IVF Process: Step-by-Step Fertility Treatment & Embryo Transfer Timeline
Are you curious about the IVF process timeline? In this step-by-step guide, we'll walk you through the stages of In Vitro Fertilization (IVF) – a popular assisted reproductive technology. Understanding the IVF process can be crucial for individuals or couples who are struggling with fertility challenges and seeking to conceive a child. Let's explore the IVF journey from start to finish.
Step 1: Initial Consultation and Fertility Assessment – Three to Four Weeks
The IVF process begins with an initial consultation with a fertility specialist or reproductive endocrinologist. During this consultation, you doctor will review the medical history of the individuals or couple, conduct necessary tests, and assess the potential causes of infertility. At this appointment, you and your physician will also discuss your individualized treatment plan and you should walk away with a clear understanding around your likelihood of success with IVF.
Wait times for initial consults vary from clinic to clinic, but your first appointment with your fertility specialist can be considered the first step in the IVF process. Your overall IVF timeline will be determined by either the female partner’s menstrual cycle or the clinic’s operating protocols. At Spring Fertility, we believe in mimicking a woman’s physiology as closely as possible, and so we do not believe in ‘batching’ cycles – a term that refers to clinics starting all patients’ ovarian stimulation cycles at the same time so that they can more effectively plan for scheduling egg retrieval procedures.
Step 2: Ovarian Stimulation for Egg Production – 10 – 14 Days
The next step in the IVF process is ovarian stimulation, and we generally counsel patients that the timeline for this phase of treatment is about two weeks.
The female partner will be given hormonal medications (usually injections) to stimulate the ovaries to produce multiple eggs. This is because in a natural cycle, only one egg is typically released each month, but in IVF, having multiple eggs increases the chances of successful fertilization.
Throughout the ovarian stimulation phase, the woman's response to the medications will be closely monitored through blood tests and ultrasounds. This helps the doctor determine the appropriate timing for egg retrieval.
Step 3: Egg Retrieval Procedure – 20 minutes
Once the ovarian follicles containing the eggs have matured to the appropriate size, your physician will prescribe what’s called a trigger shot to induce ovulation. 36 hours later, an egg retrieval is performed.
You’ll check in about an hour before the procedure to prep and change into a warm robe before meeting our anesthesiologist and embryologist who will be caring for you and your eggs. You’ll fall asleep under anesthesia, while our specialists aspirate your eggs using a very fine needle.
About 20 minutes later, you’ll awaken in our recovery area where our team will look after you before you are ready to go home (usually about 45 minutes). Most women take the rest of the day off and are ready to go back to work the following day.
Step 4: Sperm Collection and Fertilization – Same Day as Egg Retrieval
On the day of egg retrieval, the male partner or a sperm donor will provide a semen sample. In some cases, sperm can also be retrieved surgically if the male partner has fertility issues.
Prior to IVF or ICSI, the sperm is carefully processed in our Andrology lab by our expert embryologists. In a process that takes about 1-2 hours, the healthiest and most motile sperm are separated and washed to remove bacteria and other unwanted components. The sperm cells are activated and a particular density – or concentration – of the best sperm is achieved to optimize fertilization.
Once we have eggs and sperm, it’s time for them to meet (insemination or fertilization). This can be done in one of two ways: conventional insemination (IVF) or through ICSI. Both procedures are performed outside the body by our team of expert embryologists.
In conventional insemination, sperm are placed near the eggs and allowed to fertilize naturally, or through intracytoplasmic sperm injection (ICSI), where a single sperm is directly injected into an egg to achieve fertilization.
Step 5: Embryo Culture and Development – 5 to 6 Days
The morning after insemination, an embryologist will check to see if the eggs fertilized. Normally fertilized eggs have two “pronuclei,” DNA from the sperm and from the egg. Your fertilized egg is officially called an embryo.
Today, we increasingly care for embryos in the lab for 5–6 days until they reach the blastocyst stage. This gives us time to determine which are healthiest to be transferred back to the uterus. Patients with fewer good quality embryos may choose to transfer the embryo back into the uterus 2 or 3 days after fertilization since we are not choosing between them.
Some patients experience this step of the IVF process timeline as a relief, while others feel like it’s very challenging, because there is nothing for the patient to do but wait to hear news from the lab.
Step 6: Genetic Testing – 4 to 6 weeks
IVF patients have the opportunity to test their embryos before transferring them. While this process does add time to the overall IVF timeline, it allows us to maximize the likelihood of success by carefully sampling a few cells from each embryo and testing them to see if they are chromosomally normal (PGT-A). We can also test embryos to diagnose a disease that one or both parents are known to carry (PGT-M).
While those cells are being analyzed, your embryos are safely cryopreserved in the embryology lab. Cryopreservation of embryos has been safely performed for over 30 years, and today over 99% of embryos survive with no negative effects on IVF outcomes.
Step 7: Embryo Transfer
Once genetic testing results are received, your physician will counsel you about your options. If you have enough genetically normal (euploid) embryos to meet your family planning goals, it will be time to prepare for an embryo transfer. If not, your provider will likely talk to you about completing another ovarian stimulation cycle.
The ‘embryo transfer’ process is relatively simple. The procedure itself only takes about five minutes. An embryologist prepares your embryo by placing it in a small tube called a catheter. Your fertility specialist will then place the catheter through your cervix and into your uterus.
And that’s it!
You’ll be awake, there’s no anesthetic, and you can get up straight away and go about your day.
Step 8: Pregnancy Test & Beyond (2 weeks)
Known as “the two week wait” and often the hardest part of the entire IVF transfer process, ~11-13 days after the transfer, you’ll come back into our clinic to find out if your embryo implanted successfully. You’ll have a blood test to measure your levels of the hormone hCG (human chorionic gonadotropin). hCG in your bloodstream usually indicates a positive pregnancy test.
It's important to note that not every IVF cycle results in pregnancy, and sometimes multiple cycles may be needed to achieve a successful pregnancy. The entire IVF process can take between 6-8 weeks (without genetic testing), however it’s also important to understand that every patient’s IVF timeline will look different. After your initial consult, you’ll have a better understanding of what your individualized IVF process step by step will entail.

More like this
IVF Explained
Spring Fertility: Elevating Your Fertility Journey in the Bay Area
When it comes to embarking on the profound journey of parenthood, choosing the right fertility…
From Consultation to Conception: Navigating the IVF Experience
In vitro fertilization (IVF) has paved the way for countless families around the world to…
Egg Freezing Booklet Download
Learn more about egg freezing with our comprehensive Egg Freezing Booklet!
- First Name *
- Last Name *

- Getting Pregnant
- Fertility Challenges
IVF: What to Know About in Vitro Fertilization
These days there are so many possible paths to parenthood. If you and your fertility specialist decide that in vitro fertilization (IVF) is the right way for you to conceive, your IVF treatment plan will probably be as unique as you are. Still, it’s normal to have all the questions as you venture into this uncharted territory. Ready to explore your options? From initial steps to IVF success rate, side effects and cost factors, we’re sharing the full lowdown on what you can expect during the IVF process, straight from fertility specialists in the know.
What Is IVF?
IVF, or in vitro fertilization, is a series of procedures used to assist parents with the conception of a baby; an egg is fertilized by sperm outside the body and then transferred to a uterus for the duration of the pregnancy.
How does IVF work?
Women naturally produce one egg per cycle. But according to the Massachusetts General Hospital Fertility Center , 30 percent of human eggs aren’t usable. The IVF process, initially developed for women with tubal factor infertility, uses injectable medications to increase the number of eggs a woman’s body releases during one cycle. “With IVF, patients are using the same hormones the brain makes but at a higher concentration to bring ovaries to have multiple eggs,” says Stephanie Gustin , MD, a reproductive endocrinologist and owner of Heartland Center for Reproductive Medicine in Omaha.
Once the eggs are retrieved and then fertilized in a lab, they’re moved to a woman’s uterus. “Fourteen days later, our patients take a pregnancy test; if it’s positive, we repeat the test in two days to assess whether it’s a normal pregnancy,” says Molly Moravek , MD, an ob-gyn and associate professor at Michigan Medicine. One IVF cycle—which can be carried out with your own eggs and your partner’s sperm or donor sperm and/or donor eggs or embryos—takes anywhere from three weeks to a month or two.
IUI vs. IVF
There isn’t a one-size-fits-all approach to fertility treatments. And if your doctor has mentioned an IUI, you might be wondering how it differs from IVF, or which one is the right path to pursue first. It depends on the results of your fertility tests, but often the first step before IVF treatment will be intrauterine insemination (IUI), a procedure where sperm that have been collected and washed in a clinic are placed via catheter into your uterus around the time of ovulation.
If a couple has unexplained fertility or “mild male factor” infertility, IUI is considered favorable, says Shruthi Mahalingaiah , MD, a reproductive endocrinologist at the Massachusetts General Hospital Fertility Center. Women wanting to try a less invasive therapy are also likely to seek out IUI before attempting IVF treatment, Mahalingaiah notes, as are some prospective moms using donor sperm.
What is reciprocal IVF?
Reciprocal IVF , also known as co-maternity or co-IVF, allows same-sex female couples to both be involved physically in their pregnancy. One partner provides the eggs and the other carries the pregnancy, explains Abigail Mancuso , MD, an IVF specialist at the University of Iowa Center for Advanced Reproductive Care.
Why Is IVF Performed?
If you’re under 35 years old and you’ve been trying to get pregnant for 12 months, or if you’re older than 35 and you’ve been trying to conceive for six months, your OB may recommend that you see a fertility specialist, according to the American College of Obstetricians and Gynecologists (ACOG). They will order a fertility workup, or a series of blood tests and ultrasounds that examine your ovarian reserve, uterine shape, tubal shapes and hormone levels as well as your partner’s sperm. What happens next depends on the results of these tests and your pregnancy history, says Moravek. You’re generally considered a good candidate for IVF treatment if:
- Your fallopian tubes are blocked or damaged
- You’re over 40 years old and your fertility specialist can’t find anything obvious to fix in your screenings
- Your male partner has fertility issues, such as a low sperm count or very few normally shaped sperm
- You want to use reciprocal IVF to conceive a baby with your partner
- You’ve had IUIs, and they have not been successful
What to consider before pursuing IVF
Pursuing in vitro fertilization isn’t an easy decision. There are a number of things to talk over with your partner or family before you start the IVF process; these include cost, number of embryos to transfer and your feelings about potentially getting pregnant with more than one baby. Here are some things to consider:
- How many IVF cycles can I/we afford?
- Can we handle twins or multiple births?
- What will I/we do with extra embryos that aren’t transferred? Keep in mind that “partners have equal rights over embryos,” says Moravek. Regardless of your marriage or relationship status, your embryo is considered jointly parented, so it’s important to determine who will oversee them. What’s more, Moravek explains that, for some people, religious beliefs come into play: “Are you okay with donating embryos or discarding them?”
What’s more, there are a few important questions you’ll want to ask your doctor before you finalize your IVF plan. Here are some concerns to address in advance:
- What is the IVF success rate of patients in my age group at this fertility center/clinic?
- Does my insurance cover any part of the IVF treatment? Reach out to your carrier and ask specific questions to get a more thorough breakdown of cost and coverage.
- How many embryos should we transfer? (Most fertility specialists today recommend that, unless there’s a good chance of producing a genetically abnormal embryo, you stick with transferring one embryo at a time, says Moravek.)
A Peek into the IVF Process
Your IVF treatment plan depends on your health and pregnancy history, your finances and how many IVF cycles you want to try. Often, a typical IVF journey will start off with a few weeks on the birth control pill to make scheduling easier, according to the Massachusetts General Hospital Fertility Center. Then you’ll start fertility medications, mostly likely gonadotropins—hormone medications that stimulate your ovaries to produce eggs—that you’ll inject yourself with once or twice daily, notes Gustin. You’ll also be taking another shot to prevent yourself from prematurely ovulating. Throughout the 10 to 12 days that you’re on these IVF medications, you’ll have ultrasounds and bloodwork performed to check hormone levels, measure the thickness of your uterine lining and count the number of follicles developing inside you, says Gustin.
When your eggs are mature, you’ll use one last injection—the trigger shot, or hCG —which causes you to ovulate. Gustin says that about 34 to 36 hours later, before you ovulate, your fertility team will extract your eggs, which are then mixed with sperm in a lab before being implanted back into your uterus.
The 5 IVF steps
While every IVF treatment is slightly unique, there are five basic steps to the IVF process:
- Ovarian stimulation
- Egg retrieval
- Sperm collection
- Fertilization
- Embryo transfer
IVF Timeline: How Long Does IVF Take?
Your IVF timeline can range from weeks to years depending on how you look at it. It may include a number of different treatment options or steps, like starting with a few rounds of IUI before graduating to IVF, or using the birth control pill for a while to facilitate scheduling. A typical IVF cycle, from when you start injecting ovarian stimulation medications to when an embryo gets transferred to your uterus, takes roughly three to four weeks, says Mancuso.
What Happens During the IVF Procedure
Generally, patients are under some sort of IV anesthesia during IVF egg retrieval, says Mancuso. It’s an outpatient procedure that takes about 20 minutes. Your fertility team will use a transvaginal ultrasound with a little needle that goes into the ovary and sucks out the eggs, explains Moravek. Once the eggs have been collected and fertilized, they are biopsied and sent out for genetic testing, if that’s part of your IVF plan.
IVF embryo transfer occurs three to five days after retrieval if you’re not freezing your embryos to wait for testing or to use at a later time. “You’re awake for it,” says Moravek. “They put in a speculum like for a pap smear, clean off the cervix, insert a very small catheter into the uterus and release the embryos a centimeter or two from the uterus.” Then the waiting game begins: You’ll take your first blood pregnancy test two weeks later.
IVF Success Rates by Age
The Centers for Disease Control and Prevention (CDC) records assisted reproductive technology success rate data throughout the country. Its most recent report , which tracked 456 fertility clinics in the US, shows that 55.1 percent of procedures—the majority of which were IVF—where eggs were retrieved from and transferred to women ages 35 and under resulted in a live birth. For women ages 35 to 37, 41.9 percent of egg retrievals resulted in live births; for women ages 38 to 40, the IVF success rate was 26.6 percent and for those older than 43, 4.1 percent of egg retrievals resulted in live births.
IVF Side Effects
You can blame most IVF side effects on the medications in charge of manipulating your ovaries: Potential headaches, hot flashes, mood swings and pain at the injection site are common with the stimulation medications. You may also experience stomach issues, headaches, vaginal bleeding and redness or itching at the injection site for the drugs that limit your ovulation.
“In general, patients are going to feel something when their hormone status shifts,” says Mahalingaiah. “Although some people say they don’t feel any side effects at all.”
As your follicles get bigger and your body makes more estrogen, you might notice some breast enlargement, and as your ovaries grow you may feel bloating or intermittent pressure or cramping in your pelvis, says Gustin.
IVF treatment can also have a mental impact. “Emotions are a huge part of this,” says Mahalingaiah. “They can significantly impact the experience of going through the treatment, and the first cycle is often the hardest one to go through because it’s so new.” The stakes are high and fluctuating hormones can add fuel to the fire, so be sure to treat yourself with grace and kindness throughout the rollercoaster IVF process, and don’t be shy about reaching out for help. Mahalingaiah notes that many fertility clinics employ social workers or will refer patients to someone for additional psychological support.
How Much Does IVF Cost?
On average, one cycle of IVF treatment costs between $15,000 and $25,000, says Mancuso, although that’s akin to a base fee. “Everything else, like genetic testing or ICSI fertilization, adds on extra costs,” she says.
Is IVF covered by insurance?
If you’re wondering if IVF is covered by insurance, the answer is far from definitive. While US workplace insurance has, in recent years, offered more fertility treatment coverage, the National Conference of State Legislatures notes that only 17 states have passed laws that require insurers to either cover or offer coverage for infertility treatment—exactly how much, though, is neither universal nor clear.
Finances can definitely be a limiting factor when it comes to how your IVF journey advances. “There’s been an improvement in insurance coverage over the years, but it’s not where it needs to be yet,” says Mancuso.
Are IVF loans available?
The overwhelming expense of in vitro fertilization can be a hindrance for many hopeful parents. The slightly encouraging news is that IVF loans can sometimes help offset the initial out-of-pocket cost. Don’t know where to start? Your fertility specialist or clinic may partner with certain lenders that can potentially help you navigate financing options. (It’s best to do your due diligence and research IVF loans on your own as well.) What’s more, you might consider looking into IVF grants if you’re unable to afford the options presented.
In vitro fertilization can be a blessing for families. Still, the IVF process isn’t guaranteed, and it can be emotional, exhausting and expensive. Talk to your partner, your loved ones and your doctors to make sure you’re fully prepared, mentally and physically, before embarking on this journey.
About the experts:
Stephanie Gustin , MD, is a reproductive endocrinologist and owner of Heartland Center for Reproductive Medicine in Omaha. She received her medical degree from Georgetown University School of Medicine.
Shruthi Mahalingaiah , MD, is a reproductive endocrinologist at the Massachusetts General Hospital Fertility Center. She received her medical degree from Harvard Medical School.
Abigail Mancuso , MD, is an IVF physician at the University of Iowa Center for Advanced Reproductive Care. She received her medical degree from Creighton University, School of Medicine in Omaha, Nebraska.
Molly Moravek , MD, is an associate professor in the Department of Obstetrics and Gynecology at the University of Michigan Medical School, where she also earned her medical degree.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
5 Best Ovulation Tests to Figure Out When You’re Fertile
8 Shocking Facts About Trying to Get Pregnant
One Mom’s Story of Infertility Struggles and Survivor’s Guilt
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.
Next on Your Reading List

- For Patients
- Search Clinics
A Guide to the IVF Process & Timeline

- what day of your menstrual cycle you are on
- how you respond to fertility medications
- your personal life schedule
The IVF process can take 3-4 months from your initial consultation to the time you actually have your first beta hCG test to see if you’re pregnant.
Month 1 - Consultation and testing
- blood tests for hormones & infectious diseases
- transvaginal ultrasound to estimate your ovarian reserve
- partner's semen analysis (if you have a male partner)
Many fertility tests are time-sensitive and some can only be done on specific days of your menstrual cycle, typically Day 2 or 3 of your cycle.
- Estrogen (E2)
- Progesterone (P4)
- Luteinizing Hormone (LH)
- Follicle Stimulating Hormone (FSH)
- Anti-mullerian Hormone (AMH)
- Thyroid Hormones (TSH, T3, T4)
- Testosterone
- Infectious diseases (Hep B, Hep C, RPR, HPV, HIV, etc)
- Red blood cell count
- Other blood tests specific to your medical history
- Baseline ultrasound to count the number of follicles on each ovary
- Pelvic exam
- SIS/SHG to evaluate your uterus for any abnormalities such as fibroids, polyps, or scarring
- HSG to check if the fallopian tubes are open; it's more commonly done prior to IUI
- Hysteroscopy to evaluate the uterine cavity & remove any abnormalities that could affect embryo implantation such as polyps; less commonly ordered
- Laparoscopy which is a surgical procedure typically done for endometriosis diagnosis or treatment
- Infectious disease blood work
- Concentration
Month 2 - Start IVF cycle / finish up any testing you missed in Month 1
- get prior authorization from insurance
- get any prior authorization from insurance for medications
- have medication prescriptions sent to your pharmacy
- read our IVF insurance guide on common misconceptions when using infertility coverage
- read our guide on estimating the cost of IVF with insurance
- pay for your IVF cycle/set up payment plan
- shop around pharmacies for best medication prices
- read our tips on saving to afford IVF
- read our guide on how to deduct IVF on your taxes
IVF Cycle Timeline
Do you like your fertility clinic? 💌 🙏 Review your fertility doctor on our site! Other women need your opinion to help them choose a great fertility provider!
IVF Medications
- FSH (brand names: Gonal-F, Follistim, etc)
- FSH + LH (brand name: Menopur)
- GnRH Antagonist (brand names: Ganirelix, Cetrotide)
- hCG trigger (brand names: Pregnyl, Novarel, Ovidrel, etc) or Lupron trigger
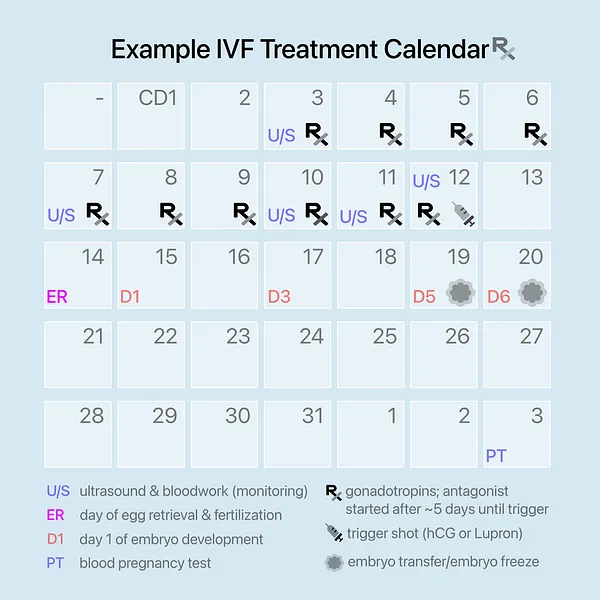
Month 3 - Frozen embryo transfer (FET) or Mock Cycle
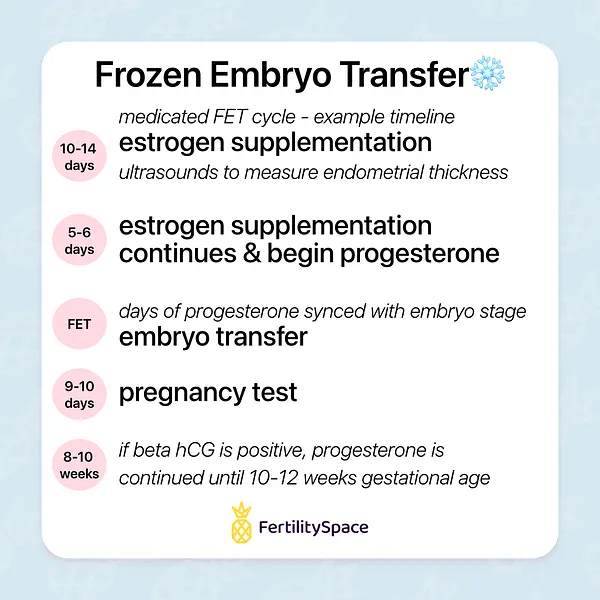
FET Cycle Timeline
Month 4 - pregnancy monitoring / fet cycle , what can cause my ivf treatment timeline to be delayed.
- needing a surgical procedure to remove polyps before your embryo transfer
- delaying your cycle due to financial stress
- delaying your cycle due to insurance authorization approval timeline
- needing to take some time off from treatment for personal reasons
IVF Success Rates
🕵️♀️ Ready to start looking for a fertility clinic? Head to our clinic search to compare options in your area & learn more about each provider & their IVF success rates.
- Search Fertility Grants
- Fertility Glossary
- 2024 FertilitySpace
- Privacy Terms
- Search all Clinics
- Review Your Doctor
- For Business
- locale-select#update" data-target='locale-select.selectInput'> English Español Chinese Arabic Hindi Deutsch Français
Are you sure?
- Fertility Knowledge
- Diagnoses & Biomarker Lexicon
- Our advisory board
- OUR FEATURES
- FERTILITY KNOWLEDGE
- DIAGNOSES & BIOMARKER LEXICON
- Test your fertility

- Book free demo
The IVF process: A step-by-step guide
Whether you’re considering starting your first IVF cycle or exploring other options to grow your family, the world of reproductive medicine might appear complex and overwhelming. In this article, we break down the stages and timeline of IVF, so you have a clear understanding of what to anticipate if you choose this treatment on your journey to parenthood.
IVF Timeline: What to expect
Consultation with a reproductive endocrinologist and infertility specialist (rei).
Before beginning IVF treatment, you’ll meet with a fertility doctor, called a reproductive endocrinologist and infertility specialist, or REI for short. REIs are obstetrician-gynecologists with specialized training in treating infertility. Average wait times to see an REI varies from clinic to clinic, but can be up to six weeks.
At the first consultation, an REI will ask you a series of questions about your medical and family history and reproductive health to start determining the underlying cause of your struggle to conceive. Next, they will order lab tests to diagnose the cause of infertility.
Your REI may also order genetic screening for you and your partner. Carrier screening is a genetic test designed to determine if you carry genes associated with specific genetic disorders. This is typically done prior to or during pregnancy which will provide insights into the likelihood of your child inheriting a genetic disorder.
If your clinic is partnered with LEVY Health, the pre-screening process happens while you’re waiting for the first consultation, cutting up to 3 months of wait time off your fertility journey so you can begin your treatment much quicker.
You’ll answer questions about your health background at home via the virtual Reproductive Health Assessment. Once that’s done (it takes about 15 minutes), you’ll receive a lab requisition form that you can take to any Labcorp or Quest site near you for testing.
With your test results explained inside our digital dashboard and educational content about fertility in LEVY Learn, you can arrive at your first appointment at the clinic empowered with the knowledge of what’s been standing in the way of pregnancy and what questions to ask your doctor. That way, you can feel confident that you’re making the right decisions about your fertility treatment.
Ovarian stimulation cycle (8-14 days)
Now that all of the pre-screening and testing are out of the way, you’re all set to begin your IVF cycle. The first step of IVF is known as hormonal stimulation and involves taking hormonal medications daily. These medications make your ovaries produce multiple follicles, each potentially containing an egg.
Your dosage may change throughout this phase based on how your follicles are reacting and growing, which will be monitored at your clinic through regular ultrasounds and blood tests. Typically, ultrasounds occur on days 1, 5, 7, and 9 (and potentially additional ultrasounds as needed).

At the end of the stimulation cycle, you’ll have what’s known as a “trigger shot”. This is an injection of hormones (human chorionic gonadotropin or hCG) that helps your ovaries mature and release eggs so that they are ready for retrieval. The trigger shot happens 36 hours before your scheduled egg retrieval.
Egg Retrieval procedure (day 0)
On the day of egg retrieval, your partner will either provide a sperm sample, or you may already have frozen partner or donor sperm stored for use. The sperm will be “washed” (a process where an embryologist separates the highest quality sperm from lower quality sperm and semen to have higher chances of success) or thawed and prepared for intracytoplasmic sperm injection (ICSI) .
To retrieve your eggs, you’ll receive anesthesia and your REI will use an ultrasound probe to guide a needle through your vagina and into one ovary at a time. The needle will then suck eggs and fluid from each follicle.
After retrieval, your eggs will go into an incubator (a device that helps maintain ideal atmospheric conditions for egg survival). An embryologist will examine each egg, remove cumulus cells (cells surrounding eggs that aid in maturation), and check its maturity
Eggs are graded in terms of maturity:
- GV = Germinal vesicle. These are the most immature eggs and will be discarded.
- MI = Metaphase I oocyte. These are immature eggs which may be kept for use during ICSI if there aren’t enough MII eggs. Some IVF labs don’t use MIs.
- MII = Metaphase II oocyte. These are mature eggs and have the highest chances for successful fertilization.
Around 4 hours following egg retrieval, an embryologist will perform ICSI. During ICSI, an embryologist selects a single sperm and injects it directly into the egg.
At this point, you’ll get an update about your IVF cycle from either your doctor, nurse, or IVF lab.
1 day after egg retrieval
The day after egg retrieval, embryologists check to see if sperm has successfully fertilized an egg. You’ll get another update on this day.
3 days after egg retrieval
It’s been 72 hours now, and an embryologist will check on how your embryos are developing and give them each a grade. Some IVF labs do it differently and won’t check the embryos on day 3 to avoid disturbing them. Now, the embryos have hopefully divided into 6, or preferably 8 cells. The more they’ve divided, the higher the chances for pregnancy.
You’ll get another update from your clinic on how things are moving along.

5 days after egg retrieval
This step of IVF is known as the blastocyst stage. It’s where a fertilized egg becomes a rapidly dividing ball of cells. The inner group of cells is the embryo and the outer group of cells nourishes and protects it.
An embryologist will evaluate and grade the embryos, likely using the most common and universally used grading system, called The Gardner Blastocyst Grading System :
- Expansion Stage: Grades 1 to 6
- 1-3 are the earliest developmental stages. An embryo must be at least a 3 to qualify for a biopsy, which is part of preimplantation genetic testing.
- 4-5 means that the blastocyst has “hatched.” This is when the blastocyst sheds its outer cellular membrane and it’s a necessary step for implantation.
- 6 is the most developed (fully hatched) stage.
- Trophectoderm (TE): Grades A to C
The trophectoderm is the collection of cells that will eventually become the placenta and pregnancy sac (fluid surrounding the embryo during the first few weeks). They are responsible for implantation of the embryo into the wall of the uterus.
- A means there are lots of cells (which is what you want).
- B means there are fewer cells.
- C is the lowest, meaning there are the least cells.
- Inner Cell Mass (ICM): Grades A to C
The inner cell mass is a mass of cells within the blastocyst which will turn into the fetus.
- A means there are many tightly packed cells (which is the best grade).
- B means that there are many loosely grouped cells.
- C means that there are very few cells.
If you’re having a fresh embryo transfer, the embryo with the best grade across all 3 categories will be transferred into your uterus on day 5. If you’re doing preimplantation genetic testing (PGT), an embryologist will take a biopsy of the additional viable embryos and then freeze them for a future frozen embryo transfer (FET).
6 days after egg retrieval
If any of your embryos haven’t reached the blastocyst stage on day 5, an embryologist will check and grade them on day 6. Like on the previous day, any embryos that will go through preimplantation genetic testing will undergo a biopsy and then get frozen. You’ll receive an update from your doctor about how your embryos are developing.
7 days after egg retrieval
Depending on your IVF lab, an embryologist may check the embryos one last time to see if any more have advanced to the blastocyst stage. Not all labs give embryos until the 7th day to develop. Like the last step, any viable embryos that advanced to day 7 will be biopsied and frozen and you’ll get an update on the progress.
Embryo transfer
Once the embryos are developed enough, they can be transferred into your uterus. Your REI will insert a catheter (a thin tube) through your vagina and cervix and into your uterus to release the embryo.
Two weeks wait
If the embryo successfully implants itself in the uterine wall, which may take around 6 to 14 days, you’ll become pregnant. You’ll need to return to your fertility clinic for a blood test to confirm the pregnancy.
IVF is an effective fertility treatment and offers hope for many aspiring parents dealing with infertility. Remember, each IVF journey is unique, and success rates can vary based on numerous factors, including age and underlying fertility issues.
While it is a complex process and can feel overwhelming at times, we hope that now that you know how IVF works you have more clarity as you embark on the next step of your fertility journey.
Don’t hesitate to reach out to your clinic for help with questions you have along the way and emotional support as you navigate the world of fertility treatment. Try not to get discouraged if the outcome isn’t one you were hoping for the first time around – it’s common for IVF to need multiple cycles to lead to a successful and healthy pregnancy.
This article has been verified by a medical professional.
In Vitro Fertilization (IVF) . Healthline. Accessed 17 January 2024.
Genetic Carrier Screening . Johns Hopkins Medicine. Accessed 17 January 2024.
ICSI Sperm Prep . Ovation Fertility. Accessed 17 January 2024.
IVF embryo quality and day 3 embryo grading after in vitro fertilization Cleavage stage embryo grading . Advanced Fertility Center of Chicago. Accessed 17 January 2024.
Blastocyst . Mayo Clinic. Accessed 17 January 2024.
Cochrane Gynaecology and Fertility Group et al.: “ Day 5 versus day 3 embryo biopsy for preimplantation genetic testing for monogenic/single gene defects. ” Cochrane Database Syst Rev. 2022;2022(11): CD013233.
Blastocyst . Cleveland Clinic. Accessed 17 January 2024.
You might also like...
Female hormones: What you need to know about reproductive hormones, the menstrual cycle, and fertility
When you’re struggling with fertility, one of the first places to look is your hormones. Certain vital reproductive hormones are in charge...
Fertility blood test: Why does it need to be cycle days 2-5?
When you test your fertility with LEVY, you will always check your basic reproductive hormone levels (including FSH, LH, TSH, Prolactin, Estradiol,...

Forms of amenorrhea and fertility
Not getting your period is a condition called amenorrhea. It’s important for fertility because not having a menstrual cycle with monthly ovulation...

6 Interesting Facts About Ovaries You Might Not Know
Women have two ovaries which are located on either side of the uterus. They’re around 3-5 cm long – about the size...

What to expect when testing your fertility with LEVY
If you’ve been trying to conceive for a while, it’s totally normal to feel frustrated. Why hasn’t it happened for you yet,...

Your Complete Guide to Birth Control Options and Fertility
If you’ve been using birth control for a while, you may be wondering how it can impact your fertility now that you...

Fertility Foods for Women to Help You Get Pregnant Faster
How you nourish your body is key not only when you have a baby in your belly, but also to help prepare...
What your AMH levels can tell you about fertility
FSH, LH, estrogen, progesterone… If you’re struggling to have a baby, you’re probably becoming an expert on all things hormones. AMH is...

Why Vitamin D matters for fertility
Vitamin D is a very important nutrient to keep our bodies healthy and working as they should. But did you know that...

- [email protected]
- 1-415-969-3373
- For Fertility Clinics

- Legal Notice
- Data Privacy
- Terms & Conditions
- Instructions for Use
Ja, ich möchte mich kostenfrei für den LEVY Fertility Code anmelden und den LEVY Newsletter abonnieren. Ich erhalte auf mich abgestimmte Informationen und weitere Details zum LEVY Fertility Code an die angegebene E-Mail-Adresse.
- Fertility Services Overview
- Conventional IVF
- Egg Donation
- Egg Freezing
- International Intended Parents
- Sperm Donation
- Gender Selection
- Ovulation Induction
- Laparoscopy
- Male Infertility Overview
- Intrauterine Insemination
- Polycystic Ovary Syndrome
- Semen Analysis
- Fertility Drugs
- Why choose PFCLA
- IVF Success rates
- Downloadable Resources
- Video Gallery
- Fertility 101
- People that inspire us
- Testimonials
- Patient Notices

In Vitro Fertilization (IVF): The Ultimate Guide
.png)
According to the National Survey of Family Growth conducted by the Centers for Disease Control and Prevention, approximately 1 in 8 couples struggle with infertility ––an estimated 49 million couples worldwide.
Building a family is a milestone for many people. Yet up until the 1960s, many individuals and couples across the world struggled to conceive and start a family.
Now, modern-day fertility treatments have made families a reality for couples struggling with infertility, with thousands of global organizations helping parents conceive. Thanks to much scientific advancement in the 21st century, we now have modern-day In Vitro Fertilization (IVF) to support individuals on their path toward parenthood.
What Is In Vitro Fertilization (IVF)?
IVF is an advanced form of Assisted Reproductive Technology (ART) that helps infertile women and couples conceive. Through IVF, eggs are manually fertilized using a sperm sample from a woman’s partner or donor.
There are many ways to tailor the In Vitro Fertilization process to intended parents, from reciprocal IVF for lesbian couples, to mini IVF treatments for people searching for a lower-impact, less expensive approach to fertility.
IVF has helped many couples with fertility issues successfully conceive, and may be right for you if you have or experience:
- Damaged, blocked, or removed fallopian tubes
- Ovulation disorders, uterine fibroids, or premature ovarian failure
- Decreased sperm count or decreased sperm motility
- Unexplained infertility
Additionally, those who are in a same-sex relationships or are intended single parents can achieve their dream of building a family through IVF.

When To Use IVF As Fertility Treatment
Since the introduction of IVF into mainstream medicine in the 1980s, nearly 5 million babies have been born through assisted reproductive technology (ART).
However, it’s also important to understand that IVF does not ensure a successful pregnancy. Some patients require multiple IVF cycles to achieve a successful pregnancy, while others unfortunately never achieve pregnancy at all.
Good candidates for IVF include:
- Women with blocked fallopian tubes
- Women with an infertility disorder ( Polycystic Ovarian Syndrome or Endometriosis)
- Women with irregular cycles of ovulation
- Male factor infertility
IVF might not be as effective for:
- Women over 37 years of age (it’s urgent you act quickly for IVF or fertility preservation)
- Women with trouble producing healthy eggs
- Women with no interest in getting an outside donor
Because IVF is unique to each patient’s situation, there is no “one-size-fits-all” approach to fertilization. However, medications, blood tests, vaginal ultrasounds, sperm and egg retrieval, fertilization and embryo transfer are all critical elements of the process.
IVF Process Calendar
The IVF treatment process can be complex and daunting as a patient. It is important that you be as informed as possible throughout the entire process.
The IVF process has many elements:
1. Consultation and Testing
When the IVF cycle begins, your clinic will order a number of pre-treatment tests. Some tests are mandated by state and federal law, while testing required by your clinician is customized to you. These tests often include a baseline ultrasound, bloodwork, and a semen analysis for the male partner to assess your fertility challenges and possibilities. However, other tests may also be required.
2. Ovarian Stimulation
Ovarian stimulation is a critical part of egg production. By using fertility medications , women can prepare for egg retrieval and increase their chances of a successful pregnancy. Oral and injectable fertility medications are often recommended in addition to hormones for optimal results. This may be conducted with a transvaginal ultrasound to determine when the eggs have matured.
3. Egg Retrieval
During the egg retrieval process , patients will receive general anesthesia to sleep during the procedure. Next, the eggs are then retrieved by placing a needle through the vaginal wall and into the ovary––and suctioned from the growing follicles and collected into test tubes. Finally, the test tubes are passed to the waiting embryologist. Here's what the egg retrieval calendar might look like:
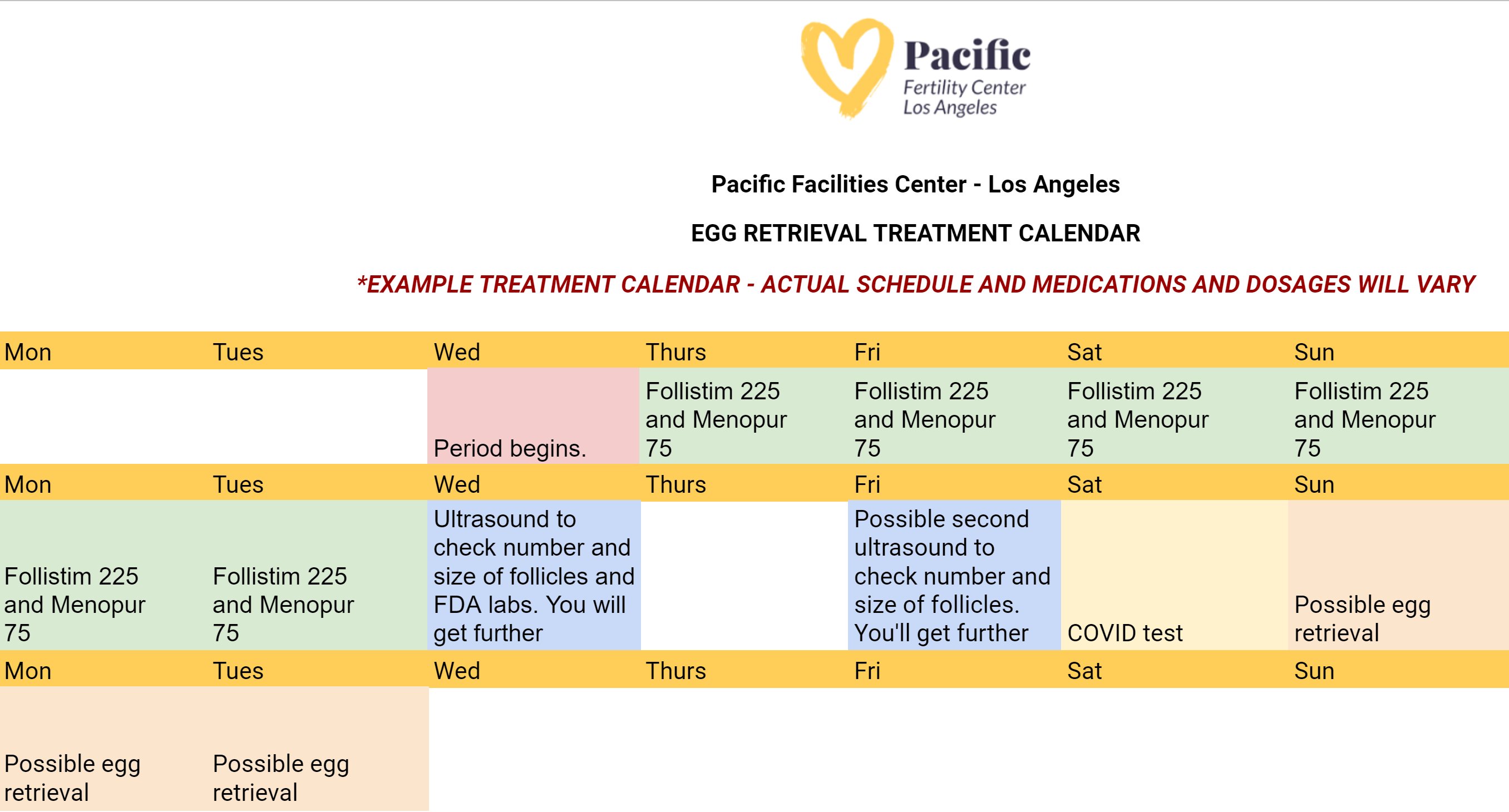
4. Fertilization
Once the eggs are in the laboratory, they will be visualized under a microscope and prepared for fertilization with either fresh or frozen sperm. A process called ICSI or Intracytoplasmic Sperm Injection is then performed to inject one healthy sperm into each of the viable eggs.
5. Embryo Freezing and Genetic Testing
The following morning, the embryologist will be able to determine how many embryos have formed. The embryos will typically spend 5-7 days in the laboratory before they are ready to be frozen, or transferred back to the uterus. Frozen embryos tend to have better success rates. Most patients will choose to test embryos for genetic or chromosome abnormalities prior to embryo transfer through preimplantation genetic screening or preimplantation genetic diagnosis.
6. Embryo Transfer
Preparing for your embryo transfer is one of the most important processes in your IVF journey. Patients at PFCLA may receive an IVF embryo transfer calendar that resembles the following:
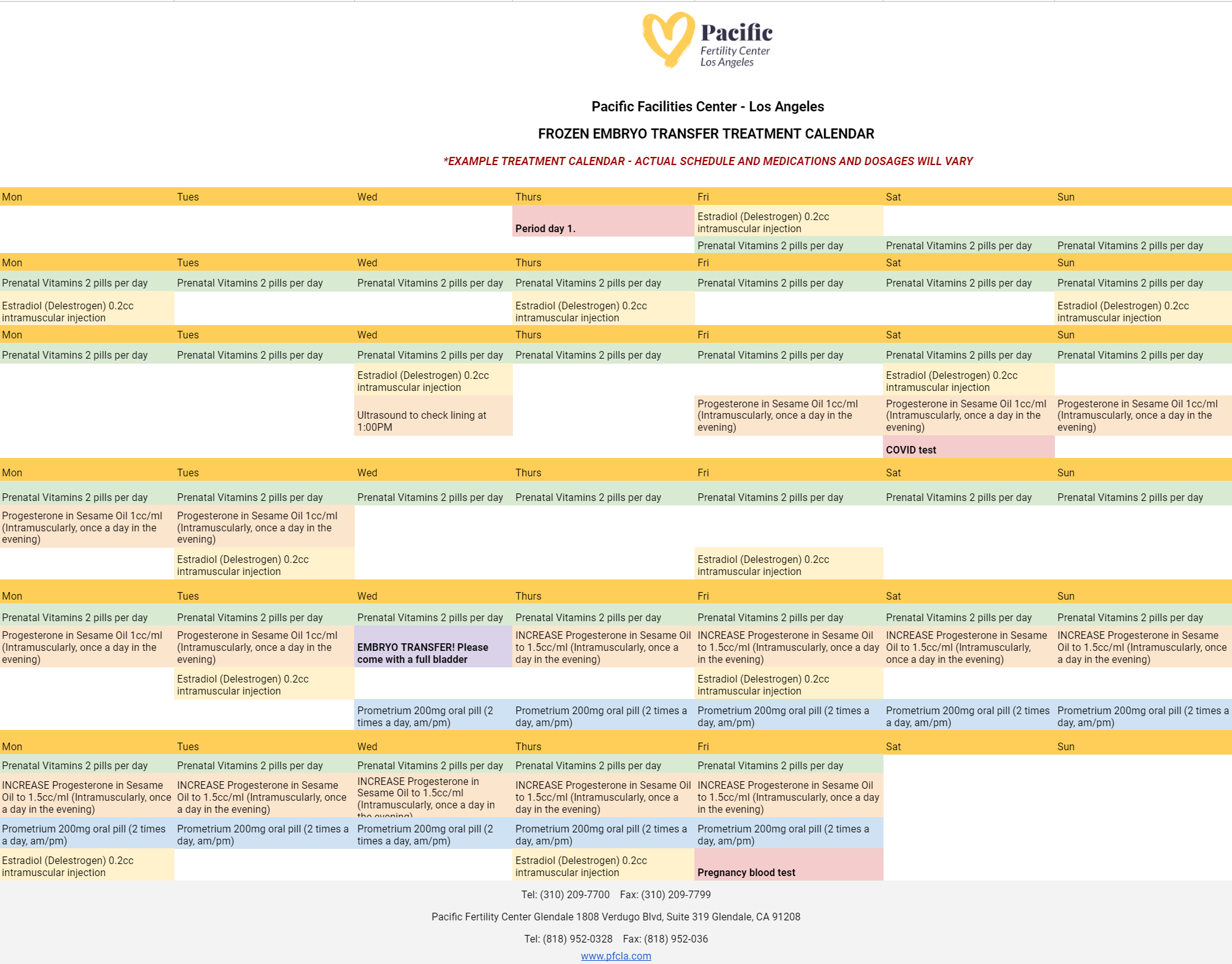
On the day of embryo transfer , the embryos will be graded based on their cell growth and development. This grading system, along with the patient’s age, will help the physician and patient to decide on the appropriate number of embryos to transfer.
An embryo transfer procedure feels similar to a pap smear and is performed while the patient is awake. To start, the cervix is visualized and cleaned. Then, a very thin catheter (tube) loaded with the embryo(s) is placed gently through the cervix and into the uterine cavity. The embryo(s) are placed near the top of the uterus using ultrasound guidance.
7. Pregnancy Test (Two Weeks After the Embryo Transfer)
Approximately ten days after the transfer, a blood pregnancy test (hCG level) is performed to determine if the patient is pregnant.
IVF vs. IUI
There are multiple available fertility treatments available today , but some are less effective than others. It’s important to talk to your doctor about what will deliver the best chances of pregnancy, so you’re not wasting precious time and money on options that may not be right for you. IUI, or intrauterine insemination, is one of these treatment options that some use because it is minimally invasive, but the success rates are usually far lower than that of IVF.
After experiencing failed IUIs , many patients turn to IVF as a more reliable fertility treatment. IVF, or in vitro fertilization, oversees most of the stages of conception to increase the chance of a successful pregnancy. Although IUI is a viable and successful fertility treatment option, it is not uncommon for a patient’s first IUI attempt to fail.
But for most who are experiencing infertility, IUI is an inferior option to IVF because IUI acts only as an assistant to natural conception. For many patients seeking fertility treatment, it can be impossible to achieve pregnancy through IUI, and your doctor may recommend starting with IVF.
How To Prepare for Your IVF Journey
To prepare for IVF, intended parents will likely need various screenings --semen analysis, uterine exams, ovarian reserve testing, and even a mock embryo transfer. This is critical to your individual IVF success, and everyone’s process will look slightly different. Preparing for IVF requires consideration of your diet, blood testing, exercise, stress, and overall health.
Before undergoing IVF, your blood work will be used to assess the level of follicle-stimulating hormone (FSH) in your system. This will give the fertility specialist an understanding of the quality and number of eggs you may have. Also, the blood work performed can help note possible incompatibilities between a mother’s blood type and father’s blood type. This blood work is also crucial in determining the presence of potential genetic disorders, viruses, and diseases that could affect the mother or baby’s health if pregnancy is achieved.
Without critical data from ultrasounds and blood work during the IVF process , the chances of a successful pregnancy are much lower, and fertility specialists can’t use the most modern techniques to truly aid patients in their journey to having a child. Additional testing may be part of the IVF process, depending on the challenges you’ve faced in getting pregnant.
After the embryo transfer, a blood test will be used to measure the pregnancy hormone levels of human chorionic gonadotropin in a woman’s system. The presence of this hormone confirms pregnancy and is typically tested for 11-12 days after an embryo transfer has been performed.
Fertility Medications and IVF
During IVF, it’s common for fertility doctors to prescribe various fertility medications to their female patients as part of the treatment process.

These fertility drugs are meant to trigger the release of various hormones and to regulate ovulation. By doing this, women are in essence made more fertile during the procedure, which improves the chances of pregnancy.
There are common fertility drugs that may be prescribed:
- Follicle-Stimulating Hormone (FSH) - Additional FSH may be used in addition to clomiphene to help stimulate the production of eggs.
- Human Menopausal Gonadotropin (hMG) - A combination of FSH and LH, and can also be used to supplement the effects of clomiphene.
- Human Chorionic Gonadotropin (hCG) - Used to trigger a woman’s ovaries to release viable eggs.
- Clomid or Serophene (Clomiphene) - A type of estrogen-blocking medication. It triggers the release of GnRH (gonadotropin-releasing hormone), FSH (follicle-stimulating hormone), and LH (luteinizing hormone), which signal your ovaries to produce eggs.
The exact medications and types of drugs required for your treatment will be determined during the consultation process. Keep in mind that some of these medications can be taken orally while others will be administered through injections.
Whatever drugs a patient requires, the effectiveness of these medications will require precise timing. Patients should take their fertility drugs as directed by their fertility specialist.
All fertility visits must also be attended on schedule to ensure optimal results. The improper dosage or administration of a fertility drug can result in a failed IVF cycle or reduced potential for a successful pregnancy.
Side Effects of the IVF Procedure
When a woman is undergoing IVF treatment, the required fertility drugs can increase specific hormone levels, such as progesterone, to prepare the body for pregnancy. Just as when progesterone levels rise naturally during pregnancy, a patient’s increased progesterone levels during IVF are likely to cause fatigue.
While changes in hormone levels are the most prominent cause of fatigue during IVF, the condition can be further exacerbated by stress or anxiety.
By the time a woman undergoes IVF treatment, she has often been dealing with infertility issues for at least a year. The worry and anticipation of repeated failed pregnancy attempts can take both a physical and mental toll, so it is understandable that many patients already feel worn down when their IVF journey begins.
Make sure to talk through all your concerns with your fertility specialist to get peace of mind during treatments and receive resources for further emotional support if needed. This will ensure you feel prepared and comfortable during your IVF treatments. Some helpful resources could be therapy for trauma-related to previous pregnancies, talking to couples who have successfully undergone IVF or joining a support group for couples going through the same process.
Because IVF requires a variety of medications throughout the treatment process, patients undergoing IVF may experience a mixture of different side effects . However, the chances of starting a family through IVF far outweigh the possible side effects.
If you do experience one of these side effects, know that they are common and can be minimized to prevent discomfort. These side effects include:
- Mild cramping and bloating
- Breast tenderness
- Constipation
- Leaking a small amount of clear or blood-tinged fluid after the procedure
- Mood swings
- Hot flashes
However, more severe risks and complications associated with IVF can include:
- Ectopic pregnancy
- Ovarian hyper-stimulation syndrome (OHSS)
- Ovarian torsion
These complications can bring side effects that should not be ignored. If you're experiencing the following, reach out to your doctor immediately:
- Pelvic pain
- Blood in urine
- Heavy vaginal bleeding
- A fever over 100.5° F
Your fertility doctor should address the side effects of IVF, as well as offer tips to deal with these symptoms. When experiencing fatigue, cramping and other side effects, it’s recommended you:
- Sleep for 8-10 hours every night
- Drink plenty of water
- Maintain a healthy, balanced diet
- Use approved over-the-counter pain relievers
- Rest warm compresses on areas of discomfort
- Meditate and use other deep breathing or relaxation techniques
Although mild cramping and pelvic discomfort are common, more severe pain should not be ignored. If your side effects are
IVF Success Rates and Outcomes

Success rates matter when it comes to the field of IVF, especially with surrogacy. Using the most experienced clinics with great success rates can provide you a better chance of having a successful pregnancy and birth, resulting in a healthy baby (or babies). You can ask any doctor or clinic for their success rates and protocols.
By having a conversation with your doctor about what you can expect, you’ll know what will and won’t be possible throughout your fertility journey. When it comes down to how many embryos will be implanted and what’s safe for you or your surrogate, trust your doctor’s counsel and let him guide you on the right path.
- Since 1985 the success rate of achieving a live birth from IVF has increased from 5% to 30% (SART).
- The Centers for Disease Control and Prevention (CDC) recorded 231,936 fertility treatment cycles in America in 2015. Of that number, 99 percent of fertility treatments involved in vitro fertilization (IVF) .
- The overall median age for women undergoing ART is 35.
- The CDC reports 186,157 ART cycles in which an embryo was transferred. Of these 186,175 procedures, 60,778 resulted in live births.
- Through ART , 72,913 infants were delivered in 2015.
- When fresh non-donor eggs or embryos were used in ART procedures, the CDC noted an 81.6 percent success rate, meaning live birth of a child or multiple children; 16.3 percent of ART procedures resulted in pregnancy loss.
Out of nearly 118,000 cycle starts from intended egg retrievals including all embryo transfers record by SART performed in the United States in 2020, under 29% (SART) resulted in live births. By contrast, PFCLA has an over 44% (SART) live birth rate from cycle start per intended egg retrieval including all embryo transfers.
Bear in mind that comparing clinics to one another is rarely an ‘apples to apples’ comparison, as different clinics and the physicians therein take different profiles of patients based on age, risk factors and services offered (whether an egg donor was used etc…). The best thing you can do to understand your personal IVF profile is consult with a physician.
Begin Your IVF Journey With Top-Rated Fertility Care
Building a family has never been more accessible and successful than ever. If you’re coping with infertility blues or looking to start your family but don’t know how, you don’t have to wait any longer to take steps toward this dream.
The fertility specialists at Pacific Fertility Center would be happy to answer any further questions you may have regarding in vitro fertilization (IVF) and your surrogacy options. Contact us to get started today.

You May Also Like
These Stories on In-Vitro Fertilization
.jpg)
Top 10 IVF Clinics in the U.S. 2024

Egg Retrieval Process Explained: What To Expect Before, During, & After

How to Prepare for a Successful IVF Cycle
Subscribe by email, no comments yet.
Let us know what you think
Westwood Location
10880 wilshire blvd ste 300 los angeles, ca 90024, call us: 310-209-7700, glendale location, 1818 verdugo blvd ste 402 glendale, ca 91208, call us: 818-952-0328.
Fertility Services
- Egg and Embryo Freezing
- Other Fertility Services
- Why Choose PFCLA
- IVF Success Rates
Subscribe to our newsletter
Note: This is not intended to be a substitute for professional medical advice, diagnosis or treatment. Information provided is for general educational purposes only and is subject to change without notice. Speak to your doctor directly with any questions you may have regarding a medical condition. Any information contained herein does not replace any care plan as determined by a physician.
¹Birth rate percentage using aggregate data from ALL age groups on the Live Births Per Intended Egg Retrieval (ALL EMBRYO TRANSFERS) of Patient's Own Eggs chart for 2020. Reference: PFCLA SART | NATIONAL SART
© 2024 PFCLA. All Rights Reserved. Privacy Policy.
- Search Please fill out this field.
- Newsletters
- Sweepstakes
- Starting a Family
- Dealing With Infertility
What the IVF Process Is Really Like
A mom who went through IVF explains what the journey was like from start to finish and offers advice to other hopeful parents.
I remember meeting with a reproductive specialist for the very first time. She explained to my husband and me the process of in vitro fertilization (IVF) using complicated charts and diagrams. It was shocking. Until that meeting, I had no idea how little I knew about what it takes to get pregnant. I'd never really had to think about it since I had previously conceived without medical treatment. Keyword: Had .
Now that we were trying to have another child "later in life," suddenly, all those aspects of human reproduction I'd never given a second thought to post-middle school sex-ed were my whole world.
I was 38 years old, and according to the Society for Assisted Reproductive Treatments (SART), I had about a 16.9% chance of having a live birth after undergoing IVF. Given everything I was about to go through, the percentage didn't seem too high. In fact, the IVF journey I was about to embark upon would push me beyond what I thought I was capable of.
How Long Does the IVF Process Take?
In the movies, an entire IVF cycle seems like no time. You inject yourself with a few hormones, and then—poof!—you're pregnant. In reality, our doctor talked us through all the steps involved, including the egg fertilization cycle and the transfer cycle.
If everything went perfectly, I would start my egg fertilization cycle that July and hope to be pregnant that October. That time frame felt especially brutal to me since we'd just suffered a pregnancy loss at almost six months along. So, it would take almost a year to return to where I was. That felt impossible.
The IVF Process Start to Finish
I showed up at my fertility clinic with $8,000 in cash. Talk about a leap of faith. That day, we fully committed to the IVF journey. It felt exciting, yes, because you hope so darn much it'll work. But more than that, I felt overwhelmed. Was I really going to go through with all of this? Just a few days later, I had my answer.
The beginning of an IVF cycle
Upon using oral meds to induce my period, which marks the beginning of a cycle, we were suddenly deep into hormones and monitoring. Something else that seemed insurmountable was all the injections I'd need to take to do this. Let's just say if you have a fear of shots, you'll need to get over it real quick to do IVF. I was in disbelief when my first shipment from the specialty pharmacy arrived at our home. The instructions were incredibly detailed, and, geez , we thought, we aren't doctors! Yet, there we were, mixing up meds and drawing up syringes each night.
Yup, the stomach is where you start with the shots. The hormones you inject at this stage are administered via fairly small needles. Nonetheless, I would grow terribly black and blue and get very bloated—a side effect of the egg stimulation hormones. There were other side effects, too, like extreme moodiness. That, coupled with the depression over our loss and my anxiety about whether all these injections would even succeed in getting me pregnant—well, it was a lot.
Another shocking aspect of this part of the IVF process is how often I needed blood work and ultrasounds. My hormone levels were being closely followed, as were the size of the follicles being stimulated by the drugs. Some weeks, I had blood drawn and a wand inserted in me just once. In other weeks, it was almost every day. Since our IVF clinic was 45 minutes from our house, this was a lot, especially with my husband's and my jobs and our kids, ages 9, 6, and 3.
I remember one time I went for morning monitoring at 5 a.m. These appointments always felt really heavy. I would look around at the others who were having their blood drawn in the cubicles around mine. They were as beat up as I was from the meds, the monitoring, and the worry. There was just this sense that every one of them had been through something—maybe a loss like me or previous failed IVF cycles. Disappointment, shame, and grief hung in the air like a fog.
To make this process seem less intense, the phlebotomists would always play music, and once, the song "Spirit in the Sky" came on. A phlebotomist practically tripped over patients in a rush to turn it off. That's how fragile some of us were. A lyric like, "Goin' up to the spirit in the sky / That's where I'm gonna go when I die," could do us in.
The egg retrieval process
After weeks of injections and monitoring, I was ready for my egg retrieval. This procedure is done under sedation, which felt like a really big deal. But the procedure was fine. It was waiting for the results that nearly gave me a panic attack.
You see, I was told the odds were that I would get one or two healthy eggs. Of those, perhaps only one would reach the embryo stage after fertilization using my husband's sperm. "If we were lucky" was a phrase I heard a lot. Luck? Yup, it seemed in addition to science, we'd need that, too.
The transfer cycle
Luck was on our side—we got several healthy embryos.
Nonetheless, I felt acutely aware of how many people weren't as "lucky" as I moved on to the next phase: the transfer cycle. Again, my doctor waited until I got my period to begin my next round of meds. These shots were no joke, with needles big enough to make me sweat. They would go in my rear end now. What a treat.
I also needed help to psych myself up each night. I held a baby hat and played Led Zeppelin while I bent over the sink, and my husband plunged a needle into my butt. Some spots hurt worse than others. I cried every time.
About four weeks later, my transfer was scheduled. Again, I felt so lucky to get here. This time, you are awake for the procedure. It's strange. The whole thing feels super clinical, even though you are about to—hopefully—get pregnant.
Several people are in the room, including a doctor, a nurse, and someone who brings your tiny embryo into the room in an incubator. The weirdest thing about it is how they verify it's your embryo via a series of numbers. I hope that's really mine , I remember thinking. But here we go!
The transfer itself is quick but painful. Your legs are spread with the speculum inserted like you're about to get a Pap smear as the doctor inserts this tube inside of you. I watched that embryo float up into my uterus on a screen. All my hopes and dreams were encapsulated in that microscopic dot. Would it become the child we'd been yearning for?
The waiting period
We'd have to wait 10 excruciating days to find out if it worked. During that time, I cried a lot, fearing the worst. Had I done all of this for nothing? It was tough not to go there. Finally, the day came when I went in for my blood test to determine if I was pregnant.
My nurse said I could take a home pregnancy test if I wanted, but I couldn't bring myself to do it. Instead, I decided to wait for that all-important phone call. When it came, I froze and didn't answer. In fact, I didn't listen to the voicemail for about an hour. When I'd built up the courage, I listened to the message.
And I was pregnant! I couldn't believe it.
After a positive pregnancy test
This was the best possible news, of course. But I was about to learn my IVF journey wasn't over.
To continue to support the pregnancy, I would inject myself with progesterone for the next eight weeks. I want to tell you these shots were easier since I was pregnant, but they weren't. At this point, I'd be getting jabbed with needles for six months. I was exhausted, and I still had an entire pregnancy to go through!
I think that's one of the hardest things about the IVF process. You have already been through so much by the time you get to the pregnancy test—it's daunting, no matter what happens next.
Case in point: Although I was blessed to give birth to my healthy son after that IVF cycle, we tried again a year and a half later, using an embryo we'd frozen. Amazingly, I got pregnant again. But at seven weeks, I miscarried. The loss killed me emotionally—I'd done all those injections and put my family through all that stress, plus I spent thousands of dollars and ended up with nothing.
It hurt. A lot. The most painful moment came when my doctor said I could just stop the injections. There was no reason to take them anymore. Suddenly, not needing those needles I so dreaded felt beyond sad. In fact, I'll confess that years later, I haven't been able to bring myself to throw them away since they are my only real connection to the baby we lost.
Finding Support for Your IVF Process
The good news is there are tons of resources for IVF patients—specifically, I was pointed to videos that walked us through every step of preparing and administering the injections. My fertility clinic also had an emergency line that we might have called a few times in a panic that we'd timed or mixed something wrong.
Luckily, I also had a great partner who huddled in the bathroom with me each night and encouraged me to take deep breaths while he plunged needle after needle into my tummy. I always felt supported and seen—although no one can truly understand what the IVF process is like unless they themselves are going through it.
Unfortunately, I didn't know anyone else who had done IVF, so I also felt incredibly isolated. I looked online for IVF support groups, but if I'm being honest, I didn't linger too long there. It's hard not to read what others are going through and apply it to your own experience, good or bad. I found it best to focus on my own journey and used yoga and meditation to find calm amid the storm of emotions and fears I was navigating.
The Bottom Line
I'd tell anyone considering IVF that firstly, you should know beyond a shadow of a doubt you want to get pregnant; secondly, it'll test you physically, emotionally, and financially.
It was almost a blessing that I didn't know what my IVF journey would entail, or else I'm not sure I could have done it. But even though it was difficult, and even though it drained my bank account and taxed my emotions and body in ways I will never fully recover from, I am so grateful IVF exists because we wouldn't have our son without it.
Related Articles

The IVF Timeline: How Long Does An IVF Cycle Take?
In this article, you will learn what an IVF timeline looks like.
From the day you have your first consultation to the day you leave with a pregnancy.
Let’s get started.
How long is the IVF process from start to finish?
Ann IVF cycle lasts approximately two weeks from the time you start your injections to when you have your eggs retrieved. A fresh embryo transfer can happen five days after the retrieval.
In contrast, a frozen embryo transfer can occur no earlier than four weeks after your retrieval.
That’s the general timeline. Now let’s break it down step-by-step.
What is the IVF process step by step? (The IVF Timeline)
An IVF treatment cycle has three distinct phases:
- Phase 1: Preparing for the IVF cycle
- Phase 2: The IVF cycle
Phase 3: The Embryo Transfer
Phase 1: ivf prep-work, step 1: initial consultation (day 1).
The first step in the fertility treatment process is the initial consultation with a reproductive endocrinologist.
During this office visit, you will discuss your medical history and have a physical exam. A transvaginal ultrasound may also be performed.
Step 2: The Fertility Work-up (Day 2-30)
Next, your doctor will order several tests to look for a possible cause of your infertility. These tests vary depending on your age, medical history, and personal preferences.
Testing includes:
- Baseline hormones and ovarian reserve (AMH)
- A uterine / cavity evaluation (hysterosalpingogram, saline infusion sonogram, or hysteroscopy)
- Other blood tests, including thyroid function and other essential health markers
All testing can take up to 30 days or more to complete.
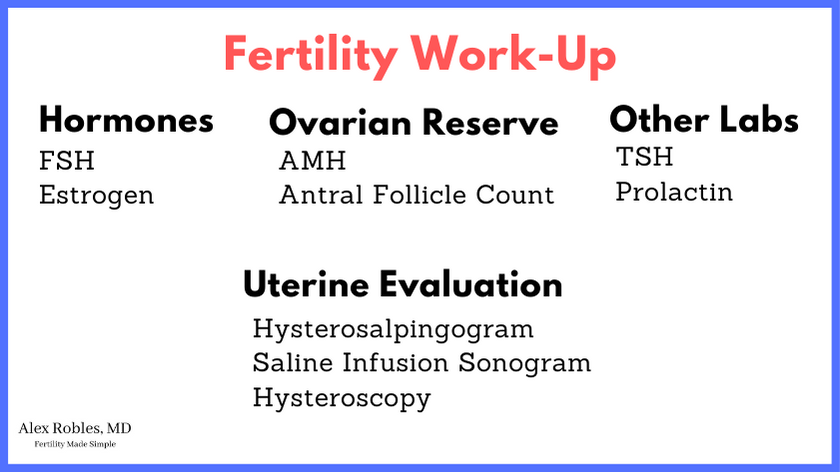
Step 3: The Follow-Up Consultation (~Day 35)
Once the testing is complete, you will return to your doctor’s office for a follow-up.
You and your doctor will review the results of your tests and discuss your treatment options.
If you both agree to IVF, you will return to the office on Day 2-3 of your next menstrual cycle to start the injections.
(*Note: Sometimes, your doctor may put you on oral contraceptives, aka birth control pills, to expedite this process).
Phase 2: The IVF Cycle
Step 4: ovarian stimulation (day 2-3).
The IVF cycle starts with you coming in on Day 2-3 of your menstrual cycle to have a baseline ultrasound and blood work done.
If all looks good with your ultrasound and hormone levels, you will begin your injections that night.
Generally, you will inject yourself once daily with two different medications.
Step 5: Monitoring Ultrasounds (Days ~5-14)
Once you begin your injections, you will have transvaginal ultrasounds every 1-3 days.
The purpose of these ultrasounds is to check on the progress of your follicles.
You will also have blood tests to check your estrogen levels, LH, and progesterone levels during this time.
On average, most cycles will require 8-12 days of injections before you take your trigger shot.
Step 6: Egg Retrieval (Day ~14-16)
The egg retrieval is then performed ~36 hours after the trigger shot. It is a simple procedure done under light anesthesia and only takes about 15 minutes to complete.
A transvaginal ultrasound is used to guide a needle into each of your ovaries. The fluid in each follicle is aspirated and collected into a tiny tube.
Your doctor may also do a mock embryo transfer at this time to assess the size and shape of your uterine cavity.
The tube is then handed to an embryologist who searches for the eggs under a microscope.
Step 7: Fertilization (Day 0-1 After Retrieval)
The embryologist will then take your preferred semen sample to fertilize your mature eggs.
There are two methods of fertilization.
- Conventional insemination (placing them on a petri dish with millions of sperm) or
- Intracytoplasmic Sperm Injection aka ICSI (injecting a single sperm into the egg)
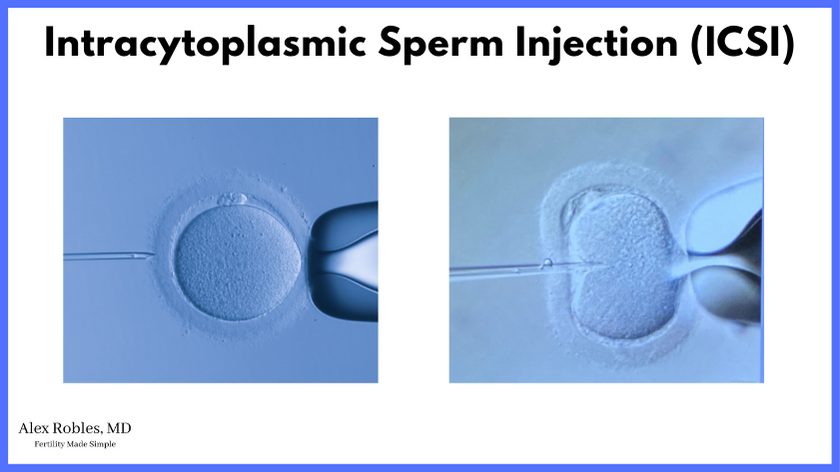
The embryologist then checks for successful fertilization the next day (~18 hours after ICSI or insemination).
Immature eggs are usually discarded as these are not viable eggs.
Step 8: Embryo Development (Days 3-7 After Retrieval)
The successfully fertilized eggs will then be left in an incubator to grow and divide.
Step 9: The Fresh Embryo Transfer (Day 3 or Day 5 After Retrieval)
If you are having a fresh Day 3 embryo transfer, it will occur three days after the egg retrieval.
If you are growing your embryos to the blastocyst stage, they are watched until Days 5, 6, or 7.
Usually, only an embryo that has made it to the blastocyst stage by Day 5 would be transferred on Day 5. If no embryos have made it blast by Day 5, then your fresh transfer will likely be canceled.
The embryo transfer procedure is pretty painless and usually straightforward.
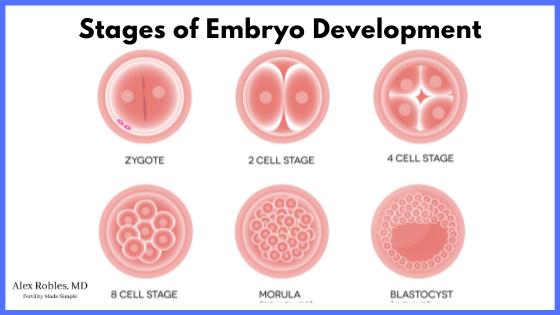
Step 10: Freezing Embryos (Days 5, 6, and 7 After Retrieval)
Any extra embryos that make it to the blast stage on Days 5, 6, or 7 will be frozen (aka vitrified).
The embryos can remain frozen indefinitely for future use.
*Of note, an embryo biopsy can also be performed before freezing to look for any chromosomal abnormalities. This is known as preimplantation genetic testing.
Step 11: The Frozen Embryo Transfer (At Any Time)
If you do not have a fresh transfer, you will do a frozen embryo transfer (FET) cycle.
Depending on your preferences, you may be able to start the cycle right away with your next period or at any time in the future.
A FET cycle also begins on Days 2 or 3 of your menstrual cycle.
Depending on the type of cycle you are doing (medicated cycle vs. natural cycle), you will have your transfer ~3 weeks later.
Step 12: The Pregnancy Test
The last step is a pregnancy blood test ~9-14 days after a blastocyst embryo transfer . If your test is positive, you will be approximately four weeks pregnant!
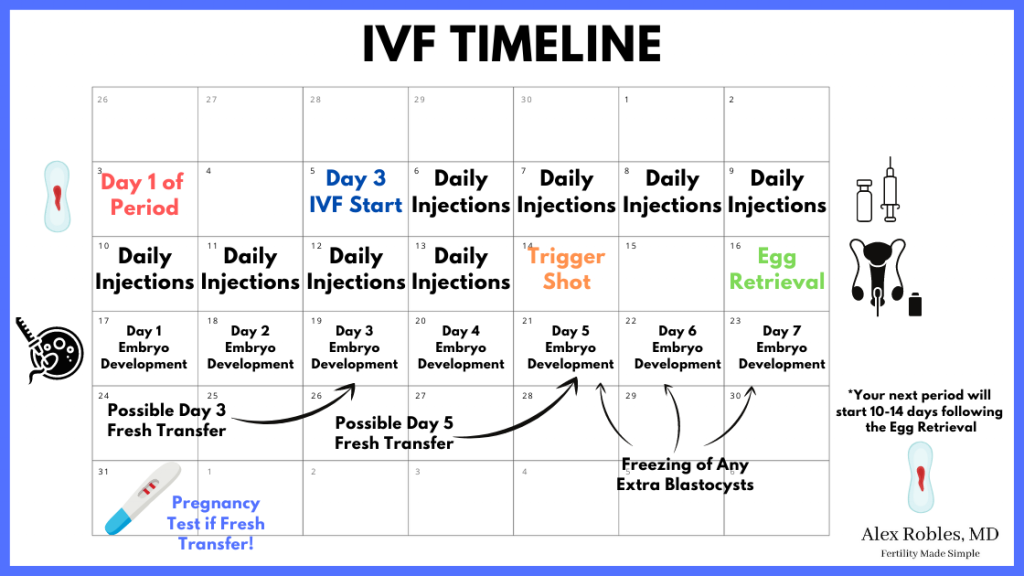
To sum it up:
So, the entire process can take as little as four weeks from the start of injections to the first pregnancy test.
If you decide on a frozen embryo transfer , you can expect an additional 4+ weeks from the start of the transfer cycle to your first pregnancy test.
Other Related Questions
How many rounds of ivf does it usually take to see success (typical ivf success rates).
Each individual IVF cycle has a success rate of about 30-50% in patients between 30-37 years of age.
In general, the more eggs collected per cycle, the higher the likelihood of success.
Success is defined as having a live birth.
As such, one to two cycles of IVF might be sufficient for patients between 30-37.
However, the success rate per cycle decreases with age, and some patients may need multiple rounds.
How many days do you take IVF injections for?
In general, most patients will need to take IVF injections for 8-12 days. The trigger shot is then administered on the last day before the egg retrieval.
What day of your cycle do you start IVF injections?
Most patients start IVF injections on Day 2 or Day 3 of the menstrual cycle.
Occasionally, some patients can have a random start (i.e., starting on any day of the cycle) if they need to do a cycle emergently.
If you start in the early follicular phase (Day 2 or 3), you will need to come in for an ultrasound and blood tests to ensure optimal timing.
What does a typical IVF injection schedule look like?
Most patients will start giving themselves daily injections from Day 2 or Day 3 of their menstrual cycle.
Usually, you will start with two injections nightly.
These usually include:
- FSH (Gonal-F or Follistim)
- and FSH and LH (Menopur)
A third injection (the antagonist) is then started around Days 5-6 of the stimulation. You will continue these three injections nightly until the trigger shot.
The trigger shot (a purified form of human chorionic gonadotropin hormone) is taken on or before Day 12 of stimulation.
Is IVF painful?
The injections themselves are not painful. There can be some discomfort and irritation at the injection site, but these symptoms are mild.
However, the egg retrieval procedure can be more uncomfortable. The amount of cramping and discomfort you feel is directly related to the number of eggs retrieved.
The good news is, most patients are back to their daily activities within 24 hours.
*Note: Ovarian hyperstimulation syndrome is a rare complication of IVF that can lead to pain, nausea, and bloating for several days following the procedure.
How long does it take for an IVF embryo to attach to the uterine lining?
An embryo transferred at the blastocyst stage will implant in the first 24-48 hours. However, it won’t begin secreting pregnancy hormone until several days later.
We often recommend that you wait at least 9-10 days before checking your first pregnancy test.
At what stage are embryos transferred in IVF?
Blastocyst stage embryos tend to have higher success rates than Day 3 embryos when it comes to
- implantation rates
- pregnancy rates
- and live birth rates
A blastocyst is more likely to be a viable embryo as it has already proven itself in the laboratory.

With that said, not every patient can make blastocysts and will elect to transfer at Day 3.
All types of fertility treatments typically follow the trend of your menstrual cycle, with the average IVF cycle lasting about two weeks.
The entire in vitro fertilization process can be as short as four weeks if you are fortunate enough to make healthy embryos right away.
However, it can take several years, depending on how many cycles it takes to achieve a healthy pregnancy.
If you ever have any questions, don’t hesitate to reach out to a fertility specialist!
Related Articles:
- Is IVF Painful? The Honest Truth
- IVF Medication Side Effects? Are They Serious?
- IVF vs IUI: When Should You Do One Over The Other?
Make An Appointment With Dr. Robles To Discuss Your Fertility Options Today!

Alex Robles, MD
Dr. Alex Robles is a Spanish-speaking Latino-American Reproductive Endocrinologist and Infertility specialist in New York City, and a board-certified OBGYN. He has a special interest in health, lifestyle, & nutrition. Make an appointment with Dr. Robles to discuss your fertility options today!
References:
- Smith ADAC, Tilling K, Nelson SM, Lawlor DA. Live-Birth Rate Associated With Repeat In Vitro Fertilization Treatment Cycles. JAMA . 2015;314(24):2654-2662. doi:10.1001/jama.2015.17296
- Kim SM, Kim JS. A Review of Mechanisms of Implantation. Dev Reprod . 2017;21(4):351-359. doi:10.12717/DR.2017.21.4.351
- Kontopoulos G, Simopoulou M, Zervomanolakis I, et al. Cleavage Stage versus Blastocyst Stage Embryo Transfer in Oocyte Donation Cycles. Medicina (Kaunas) . 2019;55(6):293. Published 2019 Jun 20. doi:10.3390/medicina55060293
Leave a Comment Cancel Reply
You must be logged in to post a comment.
- Patient Care & Health Information
- Tests & Procedures
- In vitro fertilization (IVF)
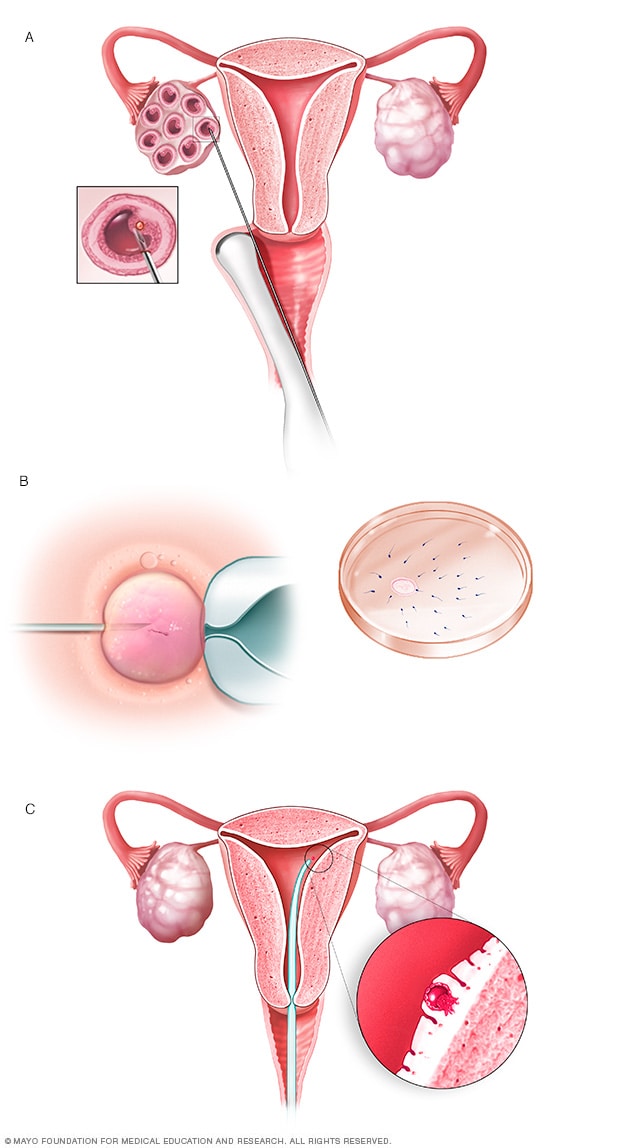
- In vitro fertilization
During in vitro fertilization, eggs are removed from sacs called follicles within an ovary (A). An egg is fertilized by injecting a single sperm into the egg or mixing the egg with sperm in a petri dish (B). The fertilized egg, called an embryo, is transferred into the uterus (C).
In vitro fertilization, also called IVF, is a complex series of procedures that can lead to a pregnancy. It's a treatment for infertility, a condition in which you can't get pregnant after at least a year of trying for most couples. IVF also can be used to prevent passing on genetic problems to a child.
During in vitro fertilization, mature eggs are collected from ovaries and fertilized by sperm in a lab. Then a procedure is done to place one or more of the fertilized eggs, called embryos, in a uterus, which is where babies develop. One full cycle of IVF takes about 2 to 3 weeks. Sometimes these steps are split into different parts and the process can take longer.
In vitro fertilization is the most effective type of fertility treatment that involves the handling of eggs or embryos and sperm. Together, this group of treatments is called assisted reproductive technology.
IVF can be done using a couple's own eggs and sperm. Or it may involve eggs, sperm or embryos from a known or unknown donor. In some cases, a gestational carrier — someone who has an embryo implanted in the uterus — might be used.
Your chances of having a healthy baby using IVF depend on many factors, such as your age and the cause of infertility. What's more, IVF involves getting procedures that can be time-consuming, expensive and invasive. If more than one embryo is placed in the uterus, it can result in a pregnancy with more than one baby. This is called a multiple pregnancy.
Your health care team can help you understand how IVF works, what the risks are and whether it's right for you.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- A Book: Mayo Clinic Guide to Fertility and Conception
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
In vitro fertilization is a treatment for infertility or genetic problems. Before you have IVF to treat infertility, you and your partner might be able to try other treatment options that involve fewer or no procedures that enter the body. For example, fertility drugs can help the ovaries make more eggs. And a procedure called intrauterine insemination places sperm directly in the uterus near the time when an ovary releases an egg, called ovulation.
Sometimes, IVF is offered as a main treatment for infertility in people over the age of 40. It also can be done if you have certain health conditions. For example, IVF may be an option if you or your partner has:
- Fallopian tube damage or blockage. Eggs move from the ovaries to the uterus through the fallopian tubes. If both tubes get damaged or blocked, that makes it hard for an egg to be fertilized or for an embryo to travel to the uterus.
- Ovulation disorders. If ovulation doesn't happen or doesn't occur often, fewer eggs are available to be fertilized by sperm.
- Endometriosis. This condition happens when tissue that's like the lining of the uterus grows outside of the uterus. Endometriosis often affects the ovaries, uterus and fallopian tubes.
- Uterine fibroids. Fibroids are tumors in the uterus. Most often, they're not cancer. They're common in people in their 30s and 40s. Fibroids can cause a fertilized egg to have trouble attaching to the lining of the uterus.
- Previous surgery to prevent pregnancy. An operation called tubal ligation involves having the fallopian tubes cut or blocked to prevent pregnancy for good. If you wish to conceive after tubal ligation, IVF may help. It might be an option if you don't want or can't get surgery to reverse tubal ligation.
- Issues with sperm. A low number of sperm or unusual changes in their movement, size or shape can make it hard for sperm to fertilize an egg. If medical tests find issues with sperm, a visit to an infertility specialist might be needed to see if there are treatable problems or other health concerns.
- Unexplained infertility. This is when tests can't find the reason for someone's infertility.
- A genetic disorder. If you or your partner is at risk of passing on a genetic disorder to your child, your health care team might recommend getting a procedure that involves IVF . It's called preimplantation genetic testing. After the eggs are harvested and fertilized, they're checked for certain genetic problems. Still, not all of these disorders can be found. Embryos that don't appear to contain a genetic problem can be placed in the uterus.
A desire to preserve fertility due to cancer or other health conditions. Cancer treatments such as radiation or chemotherapy can harm fertility. If you're about to start treatment for cancer, IVF could be a way to still have a baby in the future. Eggs can be harvested from their ovaries and frozen for later use. Or the eggs can be fertilized and frozen as embryos for future use.
People who don't have a working uterus or for whom pregnancy poses a serious health risk might choose IVF using another person to carry the pregnancy. The person is called a gestational carrier. In this case, your eggs are fertilized with sperm, but the embryos that result are placed in the gestational carrier's uterus.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
IVF raises the chances of certain health problems. From short term to longer term, these risks include:
- Stress. IVF can be draining for the body, mind and finances. Support from counselors, family and friends can help you and your partner through the ups and downs of infertility treatment.
- Complications from the procedure to retrieve eggs. After you take medicines to spur the growth of sacs in the ovaries that each contain an egg, a procedure is done to collect the eggs. This is called egg retrieval. Ultrasound images are used to guide a long, thin needle through the vagina and into the sacs, also called follicles, to harvest the eggs. The needle could cause bleeding, infection or damage to the bowel, bladder or a blood vessel. Risks are also linked with medicines that can help you sleep and prevent pain during the procedure, called anesthesia.
Ovarian hyperstimulation syndrome. This is a condition in which the ovaries become swollen and painful. It can be caused by receiving shots of fertility medicines, such as human chorionic gonadotropin (HCG), to trigger ovulation.
Symptoms often last up to a week. They include mild belly pain, bloating, upset stomach, vomiting and diarrhea. If you become pregnant, your symptoms might last a few weeks. Rarely, some people get a worse form of ovarian hyperstimulation syndrome that also can cause rapid weight gain and shortness of breath.
- Miscarriage. The rate of miscarriage for people who conceive using IVF with fresh embryos is similar to that of people who conceive naturally — about 15% for pregnant people in their 20s to over 50% for those in their 40s. The rate rises with the pregnant person's age.
- Ectopic pregnancy. This is a condition in which a fertilized egg attaches to tissue outside the uterus, often in a fallopian tube. The embryo can't survive outside the uterus, and there's no way to continue the pregnancy. A small percentage of people who use IVF will have an ectopic pregnancy.
- Multiple pregnancy. IVF raises the risk of having more than one baby. Becoming pregnant with multiple babies carries higher risks of pregnancy-related high blood pressure and diabetes, early labor and delivery, low birth weight, and birth defects than does pregnancy with a single baby.
- Birth defects. The age of the mother is the main risk factor for birth defects, no matter how the child is conceived. But assisted reproductive technologies such as IVF are linked with a slightly higher risk of a baby being born with heart issues, digestive problems or other conditions. More research is needed to find out if it's IVF that causes this raised risk or something else.
- Premature delivery and low birth weight. Research suggests that IVF slightly raises the risk that the baby will be born early or with a low birth weight.
- Cancer. Some early studies suggested that certain medicines used to stimulate egg growth might be linked with getting a specific type of ovarian tumor. But more-recent studies do not support these findings. There doesn't seem to be a significantly higher risk of breast, endometrial, cervical or ovarian cancer after IVF .
How you prepare
To get started, you'll want to find a reputable fertility clinic. If you live in the United States, the Centers for Disease Control and Prevention and the Society for Assisted Reproductive Technology provide information online about clinics' individual pregnancy and live birth rates.
A fertility clinic's success rate depends on many things. These include the ages and medical issues of people they treat, as well as the clinic's treatment approaches. When you talk with a representative at a clinic, also ask for detailed information about the costs of each step of the procedure.
Before you start a cycle of IVF using your own eggs and sperm, you and your partner will likely need various screening tests. These include:
- Ovarian reserve testing. This involves getting blood tests to find out how many eggs are available in the body. This is also called egg supply. The results of the blood tests, often used together with an ultrasound of the ovaries, can help predict how your ovaries will respond to fertility medicines.
- Semen analysis. Semen is the fluid that contains sperm. An analysis of it can check the amount of sperm, their shape and how they move. This testing may be part of an initial fertility evaluation. Or it might be done shortly before the start of an IVF treatment cycle.
- Infectious disease screening. You and your partner will both be screened for diseases such as HIV .
- Practice embryo transfer. This test doesn't place a real embryo in the uterus. It may be done to figure out the depth of your uterus. It also helps determine the technique that's most likely to work well when one or more actual embryos are inserted.
- Uterine exam. The inside lining of the uterus is checked before you start IVF . This might involve getting a test called sonohysterography. Fluid is sent through the cervix into the uterus using a thin plastic tube. The fluid helps make more-detailed ultrasound images of the uterine lining. Or the uterine exam might include a test called hysteroscopy. A thin, flexible, lighted telescope is inserted through the vagina and cervix into the uterus to see inside it.
Before you begin a cycle of IVF , think about some key questions, including:
How many embryos will be transferred? The number of embryos placed in the uterus often is based on age and the number of eggs collected. Since the rate of fertilized eggs attaching to the lining of uterus is lower for older people, usually more embryos are transferred — except for people who use donor eggs from a young person, genetically tested embryos or in certain other cases.
Most health care professionals follow specific guidelines to prevent a multiple pregnancy with triplets or more. In some countries, legislation limits the number of embryos that can be transferred. Make sure you and your care team agree on the number of embryos that will be placed in the uterus before the transfer procedure.
What will you do with any extra embryos? Extra embryos can be frozen and stored for future use for many years. Not all embryos will survive the freezing and thawing process, but most will.
Having frozen embryos can make future cycles of IVF less expensive and less invasive. Or you might be able to donate unused frozen embryos to another couple or a research facility. You also might choose to discard unused embryos. Make sure you feel comfortable making decisions about extra embryos before they are created.
- How will you handle a multiple pregnancy? If more than one embryo is placed in your uterus, IVF can cause you to have a multiple pregnancy. This poses health risks for you and your babies. In some cases, a surgery called fetal reduction can be used to help a person deliver fewer babies with lower health risks. Getting fetal reduction is a major decision with ethical, emotional and mental risks.
- Have you thought through the risks linked with using donor eggs, sperm or embryos, or a gestational carrier? A trained counselor with expertise in donor issues can help you understand the concerns, such as the legal rights of the donor. You also may need an attorney to file court papers to help you become legal parents of an embryo that's developing in the uterus.
What you can expect
After the preparations are completed, one cycle of IVF can take about 2 to 3 weeks. More than one cycle may be needed. The steps in a cycle go as follows:
Treatment to make mature eggs
The start of an IVF cycle begins by using lab-made hormones to help the ovaries to make eggs — rather than the single egg that usually develops each month. Multiple eggs are needed because some eggs won't fertilize or develop correctly after they're combined with sperm.
Certain medicines may be used to:
- Stimulate the ovaries. You might receive shots of hormones that help more than one egg develop at a time. The shot may contain a follicle-stimulating hormone (FSH), a luteinizing hormone (LH) or both.
- Help eggs mature. A hormone called human chorionic gonadotropin (HCG), or other medicines, can help the eggs ripen and get ready to be released from their sacs, called follicles, in the ovaries.
- Delay ovulation. These medicines prevent the body from releasing the developing eggs too soon.
- Prepare the lining of the uterus. You might start to take supplements of the hormone progesterone on the day of the procedure to collect your eggs. Or you might take these supplements around the time an embryo is placed in the uterus. They improve the odds that a fertilized egg attaches to the lining of your uterus.
Your doctor decides which medicines to use and when to use them.
Most often, you'll need 1 to 2 weeks of ovarian stimulation before your eggs are ready to be collected with the egg retrieval procedure. To figure out when the eggs are ready, you may need:
- Vaginal ultrasound, an imaging exam of the ovaries to track the developing follicles. Those are the fluid-filled sacs in the ovaries where eggs mature.
- Blood tests, to check on how you respond to ovarian stimulation medicines. Estrogen levels often rise as follicles develop. Progesterone levels remain low until after ovulation.
Sometimes, IVF cycles need to be canceled before the eggs are collected. Reasons for this include:
- Not enough follicles develop.
- Ovulation happens too soon.
- Too many follicles develop, raising the risk of ovarian hyperstimulation syndrome.
- Other medical issues happen.
If your cycle is canceled, your care team might recommend changing medicines or the amounts you take, called doses. This might lead to a better response during future IVF cycles. Or you may be advised that you need an egg donor.
Egg retrieval
This is the procedure to collect the eggs from one or both ovaries. It takes place in your doctor's office or a clinic. The procedure is done 34 to 36 hours after the final shot of fertility medicine and before ovulation.
- Before egg retrieval, you'll be given medicine to help you relax and keep you from feeling pain.
- An ultrasound device is placed into the vagina to find follicles. Those are the sacs in the ovaries that each contain an egg. Then a thin needle is inserted into an ultrasound guide to go through the vagina and into the follicles to collect the eggs. This process is called transvaginal ultrasound aspiration.
- If your ovaries can't be reached through the vagina this way, an ultrasound of the stomach area may be used to guide the needle through the stomach and into the ovaries.
- The eggs are removed from the follicles through a needle connected to a suction device. Multiple eggs can be removed in about 20 minutes.
- After the procedure, you may have cramping and feelings of fullness or pressure.
- Mature eggs are placed in a liquid that helps them develop. Eggs that appear healthy and mature will be mixed with sperm to attempt to create embryos. But not all eggs are able to be fertilized with success.
Sperm retrieval
If you're using your partner's sperm, a semen sample needs to be collected at your doctor's office or clinic the morning of egg retrieval. Or sperm can be collected ahead of time and frozen.
Most often, the semen sample is collected through masturbation. Other methods can be used if a person can't ejaculate or has no sperm in the semen. For example, a procedure called testicular aspiration uses a needle or surgery to collect sperm directly from the testicle. Sperm from a donor also can be used. Sperm are separated from the semen fluid in the lab.
Fertilization
Two common methods can be used to try to fertilize eggs with sperm:
- Conventional insemination. Healthy sperm and mature eggs are mixed and kept in a controlled environment called an incubator.
- Intracytoplasmic sperm injection (ICSI). A single healthy sperm is injected right into each mature egg. Often, ICSI is used when semen quality or number is an issue. Or it might be used if fertilization attempts during prior IVF cycles didn't work.
In certain situations, other procedures may be recommended before embryos are placed in the uterus. These include:
Assisted hatching. About 5 to 6 days after fertilization, an embryo "hatches" from the thin layer that surrounds it, called a membrane. This lets the embryo attach to the lining of the uterus.
If you're older and you want to get pregnant, or if you have had past IVF attempts that didn't work, a technique called assisted hatching might be recommended. With this procedure, a hole is made in the embryo's membrane just before the embryo is placed in the uterus. This helps the embryo hatch and attach to the lining of the uterus. Assisted hatching is also useful for eggs or embryos that were frozen, as that process can harden the membrane.
Preimplantation genetic testing. Embryos are allowed to develop in the incubator until they reach a stage where a small sample can be removed. The sample is tested for certain genetic diseases or the correct number of threadlike structures of DNA, called chromosomes. There are usually 46 chromosomes in each cell. Embryos that don't contain affected genes or chromosomes can be transferred to the uterus.
Preimplantation genetic testing can lower the chances that a parent will pass on a genetic problem. It can't get rid of the risk completely. Prenatal testing may still be recommended during pregnancy.
Embryo transfer
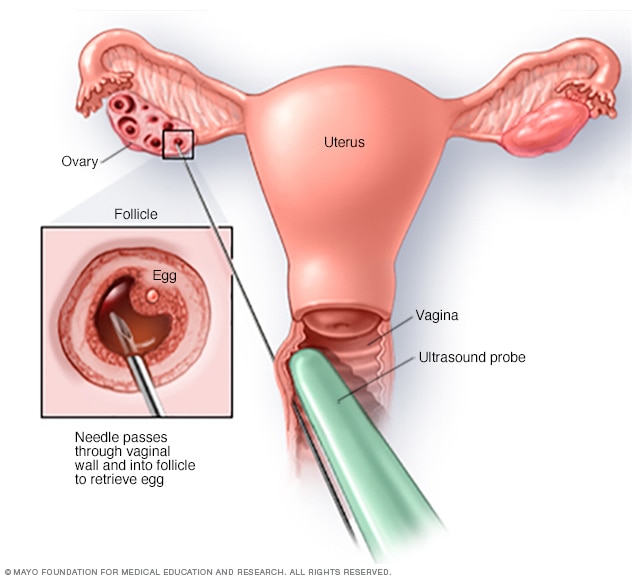
Egg-retrieval technique
Typically, transvaginal ultrasound aspiration is used to retrieve eggs. During this procedure, an ultrasound probe is inserted into the vagina to identify follicles. A needle is guided through the vagina and into the follicles. The eggs are removed from the follicles through the needle, which is connected to a suction device.
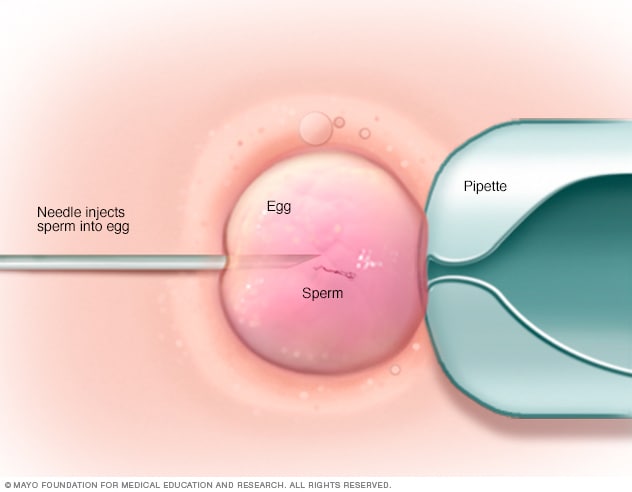
In intracytoplasmic sperm injection (ICSI), a single healthy sperm is injected directly into each mature egg. ICSI often is used when semen quality or number is a problem or if fertilization attempts during prior in vitro fertilization cycles failed.
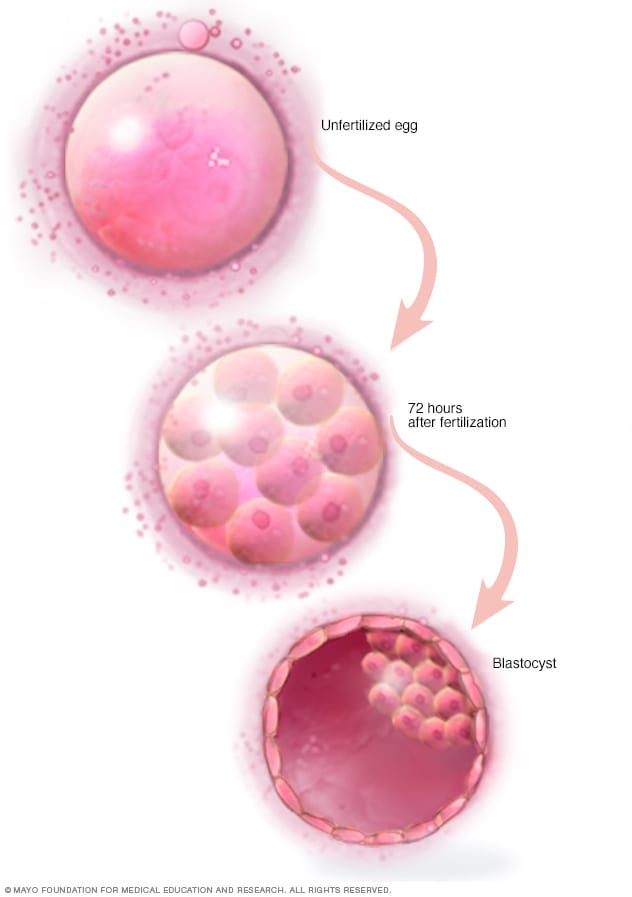
Three days after fertilization, a healthy embryo will contain about 6 to 10 cells. By the fifth or sixth day, the fertilized egg is known as a blastocyst — a rapidly dividing ball of cells. The inner group of cells will become the embryo. The outer group will become the cells that nourish and protect it.
The procedure to place one or more embryos in the uterus is done at your doctor's office or a clinic. It often takes place 2 to 6 days after eggs are collected.
- You might be given a mild sedative to help you relax. The procedure is often painless, but you might have mild cramping.
- A long, thin, flexible tube called a catheter is placed into the vagina, through the cervix and into the uterus.
- A syringe that contains one or more embryos in a small amount of fluid is attached to the end of the catheter.
- Using the syringe, the embryo or embryos are placed into the uterus.
If the procedure works, an embryo will attach to the lining of your uterus about 6 to 10 days after egg retrieval.
After the procedure
After the embryo transfer, you can get back to your usual daily routine. Your ovaries may still be enlarged, so vigorous activities or sex might cause discomfort. Ask your care team how long you should stay away from these.
Typical side effects include:
- Passing a small amount of clear or bloody fluid shortly after the procedure. This is due to the swabbing of the cervix before the embryo transfer.
- Breast tenderness due to high estrogen levels.
- Mild bloating.
- Mild cramping.
- Constipation.
Call your care team if you have moderate or severe pain, or heavy bleeding from the vagina after the embryo transfer. You'll likely to need to get checked for complications such as infection, twisting of an ovary and ovarian hyperstimulation syndrome.
At least 12 days after egg retrieval, you get a blood test to find out whether you're pregnant.
- If you're pregnant, you'll likely be referred to an obstetrician or other pregnancy specialist for prenatal care.
- If you're not pregnant, you'll stop taking progesterone and likely get your period within a week. Call your care team if you don't get your period or if you have unusual bleeding. If you'd like to try another cycle of IVF , your care team might suggest steps you can take to improve your chances of getting pregnant next time.
The chances of giving birth to a healthy baby after using IVF depend on various factors, including:
- Maternal age. The younger you are, the more likely you are to get pregnant and give birth to a healthy baby using your own eggs during IVF . Often, people 40 and older are counseled to think about using donor eggs during IVF to boost the chances of success.
- Embryo status. Transfer of embryos that are more developed is linked with higher pregnancy rates compared with less-developed embryos. But not all embryos survive the development process. Talk with your care team about your specific situation.
- Reproductive history. People who've given birth before are more likely to be able to get pregnant using IVF than are people who've never given birth. Success rates are lower for people who've already tried IVF multiple times but didn't get pregnant.
- Cause of infertility. Having an average supply of eggs raises your chances of being able to get pregnant using IVF . People who have severe endometriosis are less likely to be able to get pregnant using IVF than are those who have infertility without a clear cause.
- Lifestyle factors. Smoking can lower the chance of success with IVF . Often, people who smoke have fewer eggs retrieved during IVF and may miscarry more often. Obesity also can lower the chances of getting pregnant and having a baby. Use of alcohol, drugs, too much caffeine and certain medicines also can be harmful.
Talk with your care team about any factors that apply to you and how they may affect your chances of a successful pregnancy.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
- FAQs: Treating infertility. American College of Obstetricians and Gynecologists. http://www.acog.org/Patients/FAQs/Treating-Infertility. Accessed Feb. 23, 2023.
- In vitro fertilization. AskMayoExpert. Mayo Clinic; 2022.
- ART: Step-by-step guide. American Society for Reproductive Medicine. https://www.sart.org/patients/a-patients-guide-to-assisted-reproductive-technology/general-information/art-step-by-step-guide/. Accessed Feb. 27, 2023.
- Anchan RM, et al. Gestational carrier pregnancy. https://www.uptodate.com/contents/search. Accessed Feb. 23, 2023.
- Infertility fact sheet. Office on Women's Health. http://www.womenshealth.gov/publications/our-publications/fact-sheet/infertility.html. Accessed Feb. 23, 2023.
- Ho J. In vitro fertilization. https://www.uptodate.com/contents/search. Accessed Feb. 23, 2023.
- FAQs: IVF. Society for Assisted Reproductive Technology. https://www.sart.org/patients/frequently-asked-questions/. Accessed Feb. 23, 2023.
- FAQs: Infertility. Centers for Disease Control and Prevention. http://www.cdc.gov/reproductivehealth/Infertility/. Accessed Feb. 23, 2023.
- FAQs: Evaluating infertility. American College of Obstetricians and Gynecologists. https://www.acog.org/Patients/FAQs/Evaluating-Infertility. Accessed Feb. 23, 2023.
- Ovarian hyperstimulation. Society for Assisted Reproductive Technology. https://www.sart.org/patients/a-patients-guide-to-assisted-reproductive-technology/stimulation/ovarian-hyperstimulation-syndrome/. Accessed Feb. 23, 2023.
- Guidance on the limits to the number of embryos to transfer: A committee opinion. Practice Committee of the American Society for Reproductive Medicine and the Practice Committee for the Society for Assisted Reproductive Technologies. https://www.asrm.org/news-and-publications/practice-committee-documents/. Accessed March 1, 2023.
- In vitro fertilization (IVF): What are the risks? American Society for Reproductive Medicine. https://www.sart.org/patients/risks-of-ivf/ Accessed Feb. 2, 2024.
- Preparing for IVF: Emotional considerations. Society for Assisted Reproductive Technology. https://www.sart.org/patients/a-patients-guide-to-assisted-reproductive-technology/general-information/preparing-for-ivf-emotional-considerations/. Accessed March 1, 2023.
- Micromanipulation. Society for Assisted Reproductive Technology. https://www.sart.org/patients/a-patients-guide-to-assisted-reproductive-technology/general-information/micromanipulation/. Accessed March 1, 2023.
- Preparing for in vitro fertilization (IVF): Lifestyle factors. Society for Assisted Reproductive Technology. https://www.sart.org/patients/fyi-videos/preparing-for-in-vitro-fertilization-ivf-lifestyle-factors/. Accessed March 1, 2023.
- Ubaldi FM, et al. Advanced maternal age in IVF: Still a challenge? The present and the future of its treatment. Frontiers in Endocrinology. 2019;10:94.
- Can I freeze my eggs to use later if I'm not sick? American Society for Reproductive Medicine. https://www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/can-i-freeze-my-eggs-to-use-later-if-im-not-sick/. Accessed Feb. 24, 2023.
- Medications for inducing ovulation: A guide for patients. American Society for Reproductive Medicine. https://www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/medications-for-inducing-ovulation-booklet/. Accessed Feb. 24, 2023.
- In vitro fertilization (IVF): What are the risks? American Society for Reproductive Medicine. https://www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/in-vitro-fertilization-ivf-what-are-the-risks/. Accessed Feb. 24, 2023.
- Commonly asked questions about the US national ART surveillance system. Centers for Disease Control and Prevention. https://www.cdc.gov/art/reports/2019/commonly-asked-questions.html. Accessed Feb. 27, 2023.
- Evaluation before IVF. Society for Assisted Reproductive Technology. https://www.sart.org/patients/sart-patient-evaluation/. Accessed Feb. 27, 2023.
- Multifetal pregnancy reduction. The American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/09/multifetal-pregnancy-reduction. Accessed Feb. 27, 2023.
- Third party reproduction. Society for Assisted Reproductive Technology. https://www.sart.org/patients/third-party-reproduction/. Accessed Feb. 27, 2023.
- Ho J. In vitro fertilization: Overview of clinical issues and questions. https://www.uptodate.com/contents/search. Accessed Feb. 27, 2023.
- American Society for Reproductive Medicine. Fertility drugs and cancer: A guideline. Fertility and Sterility. 2016; doi:10.1016/j.fertnstert.2016.08.035.
- Bart CJM. Overview of ovulation induction. https://www.uptodate.com/contents/search. Accessed March 2, 2023.
- Gershenson DM, et al. In vitro fertilization. In: Comprehensive Gynecology. 8th ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed March 2, 2023.
- Barcroft JF, et al. Fertility treatment and cancers-the eternal conundrum: A systematic review and meta-analysis. Human Reproduction. 2021; doi:10.1093/humrep/deaa293.
- Hornstein MD, et al. Endometriosis: Treatment of infertility in females. https://www.uptodate.com/contents/search. Accessed March 2, 2023.
- Egg retrieval technique
- Female fertility tips
- Female infertility
- High-risk pregnancy
- Infertility
- Low sperm count
- Male infertility
- Male masturbation: Does frequency affect male fertility?
- Ovarian cysts and infertility: A connection?
News from Mayo Clinic
- Mayo Clinic in Rochester team ranked among 'America's Best Fertility Clinics' by Newsweek April 23, 2024, 05:30 p.m. CDT
- Mayo Clinic in Rochester top ranked on 'America's Best Fertility Clinics' in Newsweek rankings March 15, 2023, 01:33 p.m. CDT
- Doctors & Departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

208-342-5900

The IVF Process from Start to Finish: Creating a Reliable IVF Calendar & IVF Timeline
Planning for an infertility treatment like in vitro fertilization (IVF) is a significant step toward realizing your dream of becoming a parent—and it takes time, energy, and considerate planning. An IVF cycle calendar is one tool that can help.
Whether you’re considering IVF as an option, have just started your IVF journey, or are well into the process, creating an IVF calendar can help you know what to expect of your treatment so that you can better plan for and manage your treatment—and ultimately achieve a successful pregnancy.
How do you determine an IVF calendar?
Like many infertility treatments, IVF often involves a complex of hormone therapies, medications, and coordinating fertility treatments. With so many moving parts and diverging timelines, creating an IVF timeline calendar isn’t quite as simple as mapping out the IVF cycle itself.
The IVF process from start to finish depends on your specific goals and infertility diagnoses. Some intended parents, for example, might be using an egg donor , sperm donor, or gestational carrier to build their family with IVF. This involves coordinating with a surrogacy agency, egg donor program, or sperm bank; choosing your donor or surrogate, and legally securing the third party.
The timeline for this process varies widely, ranging anywhere from two weeks to secure a sperm donor to several months to secure a gestational carrier —depending on factors like your family’s personal third-party requirements, the availability of donors or gestational carriers, and whether you’re working with an external or in-house donor program .
Another preliminary process is pre-genetic carrier screening . Some parents choose to test their carrier status for genetic health conditions, either informing their donor selection or their selection of a healthy embryo later in the process. Depending on your IVF centre, it typically takes 1–2 weeks to receive these test results.
When it comes to the IVF cycle itself, there is still plenty of timeline variability from one family to the next—depending on personal health factors, third-party factors, and whether your treatment involves a fresh or frozen embryo transfer .
Your fertility specialist will help you create a more precise timeline, but to begin creating an IVF calendar or to get a general sense, you can work from the time ranges involved in a typical IVF cycle, which begins in coordination with your menstrual cycle.
What does a realistic IVF calendar look like?
A full round of IVF spans one menstrual cycle (1 month) for a fresh embryo transfer and at least two menstrual cycles (2 months) for a fresh cycle followed by a frozen embryo transfer cycle.
Frozen embryo transfer (FET) is the more common option for several reasons, including lower cost, reduced strain on the parent’s body, the option for preimplantation testing of embryos (PGT) , and the potential for multiple embryos which can be cryopreserved .
After retrieving and freezing embryos, intended parents can choose to wait any amount of time before beginning the FET cycle, but for the sake of presenting one continuous IVF calendar and timeline range, we’ll walk through the stages of the IVF cycle assuming no additional waiting times.
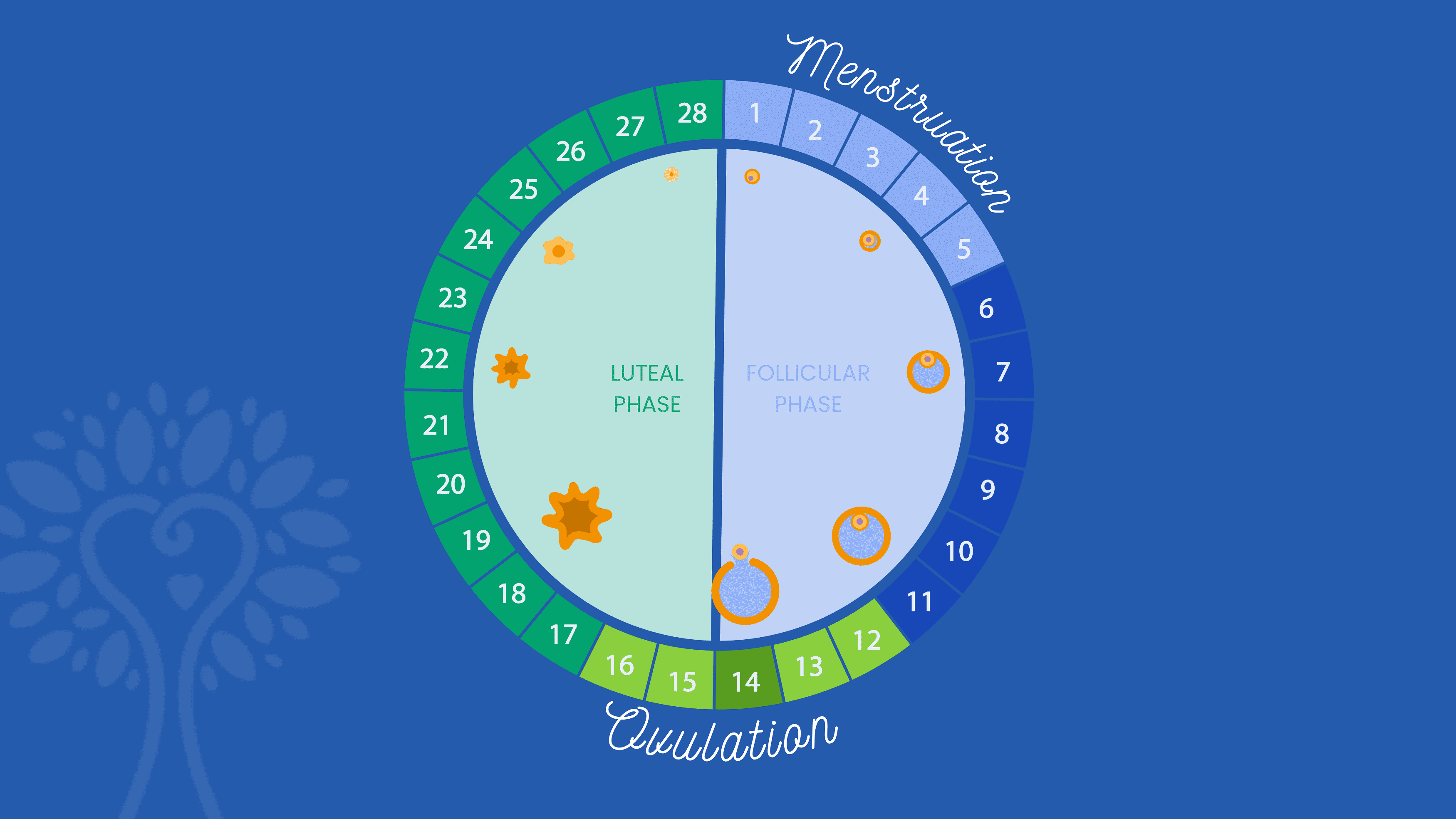
Assuming Day 1 is the first day of your menstrual cycle, here’s what a typical IVF calendar will include:
Ovarian Stimulation : The IVF cycle starts with a 9–15 day period of ovarian stimulation, using hormone injections called gonadotropins or follicle stimulating hormones, to produce multiple follicles and allow as many eggs as possible to mature for retrieval from the ovaries. Sometimes birth control pills or estrace are prescribed for you to take prior to starting the follicle stimulating hormones.
Monitoring : Throughout the ovarian stimulation phase, regular monitoring through ultrasounds and blood tests is conducted to track follicle growth and hormone levels and to inform any adjustments to medication dosages or changes in your IVF calendar.
Trigger Injection : Once a sufficient number of follicles have reached maturity, a different gonadotropin injection is administered to induce final egg maturation.
Egg Retrieval : The egg retrieval procedure is performed as an outpatient procedure under sedation or anesthesia. A needle is used to extract the mature eggs from the ovaries.
Sperm Collection and Fertilization : Sperm is either collected on the same day as the egg retrieval or cryopreserved earlier for later use. Once the eggs are retrieved and the sperm collected, both are transferred to an embryology lab where they are fertilized and closely monitored by embryologists.
Beginning of Embryo Culturing : Once fertilized, the embryos are cultured in the lab for 5–7 days, until they reach the blastocyst stage, at which point embryologists evaluate the embryos’ quality to determine which can be used. At this point, viable embryos can either be transferred back into the uterus directly or frozen for FET and/or PGT.
Day 20–27 (Optional – FET only)
Preimplantation Genetic Testing (PGT) : Often informed by a genetic risk found during the earlier carrier screening, PGT allows parents to test the carrier status and chromosomal health of each embryo . The embryos are biopsied and sent into a lab for testing, which typically takes 1–2 weeks.
Beginning of Uterine Preparation : In the case of an FET, the parent or gestational carrier undergoes 3–4 weeks of hormone treatments to enhance the uterine receptivity and support the early stages of pregnancy. This involves 2–3 weeks of estrogen treatments, followed by progesterone.
The embryo transfer is commonly done on the 6th day of progesterone. For a fresh embryo transfer, progesterone treatment is typically started within 24 hours of the egg retrieval and continues throughout the first trimester.
Embryo Transfer : On the 6th day of progesterone treatment, the fresh or thawed embryo is transferred to the uterus.
Pregnancy Test : Approximately 10–14 days after the embryo transfer, a blood test is performed to determine if pregnancy has been achieved.
How long do you have to wait after a failed round of IVF?
Experiencing a failed round of IVF—whether at the egg retrieval or embryo transfer stage—can be very discouraging and emotionally painful. Fortunately, there are often several treatment adjustments and therapeutic additions that can be made to increase odds of success in the next round. Before beginning the next IVF cycle attempt, it’s important to wait at least one menstrual cycle.
This waiting period, which typically amounts to about 4 weeks, allows the body to recover from the hormonal stimulation and any procedures associated with the previous cycle, ensuring a more stable and receptive uterine environment for the next attempt.
Like most aspects of your IVF calendar, it’s important to note that the specific waiting time may be different for each person, and your fertility specialist may recommend more based on your medical history and the reasons for the previous IVF failure.
Creating an IVF Calendar with ICRM
No matter where you find yourself on your fertility journey, the Idaho Center for Reproductive Medicine is here to provide support, guidance, and tailored treatment for your unique family.
During an IVF treatment with ICRM, our dedicated coordinators work closely with you to create and maintain an IVF calendar, schedule appointments, and navigate the intricacies of your treatment to help you achieve a successful pregnancy.
The Idaho Center for Reproductive Medicine
Quick Links
Request a Consultation
Patient Portal
Pay your Bill
Patient Resources
Refer a Patient
Freedom Injection Training
Privacy Policy
Share your Story
Patient Survey
Our Partner
1000 E. Park Blvd., Suite 110 Boise, Idaho 83712
3875 E. Overland Rd., Suite 103 Meridian, Idaho 83642
Office: 208-342-5900
Fax: 208-342-2088
Toll Free: 866-865-BABY
Email – Domestic Patients: [email protected]
Email – International Patients: [email protected]
Regular Hours of Operation: M-F 8:00am – 5:00pm. Meridian Appointment Availability: M-F 7:00am – 12:00pm

Your health in one app

Listen To Dr. Slater’s Most Recent Podcast!
In the latest episode of the SART Fertility Experts podcast, Dr. Slater and Betsy Campbell from RESOLVE discuss current barriers to reproductive medicine and how advocacy efforts are expanding access to care.

Home > Blog > The IVF journey and what to expect
The IVF journey and what to expect
IVF is often referred to as a journey. It’s not just a single procedure, but a process, involving multiple hospital visits, a variety of medication, physical and emotional challenges and a lot of waiting.
It’s therefore important to be mentally and physically prepared before you begin your IVF cycle, as feeling informed about what you can expect is a great way to start.
Is IVF the right treatment for me?
Your GP may have referred you to a fertility specialist, if you have been trying unsuccessfully to conceive or there are reasons why conceiving naturally is not an option for you.
You may have tried IUI already, without success, or you may have damaged or blocked fallopian tubes, making IVF your best option.
Your specialist will conduct a variety of tests and assessments of you (and your partner if heterosexual) which may include blood tests, an ultrasound to assess your ovaries and a semen analysis. They will also ask about your family history and any known genetic problems or fertility issues.

What can I do before I start my IVF cycle?
Counselling may be recommended before you start. You should also consider your lifestyle, as having a healthy diet and a healthy lifestyle in general, can have a positive impact on your fertility and the future health of your child. We have blog posts on our site which provide useful information about fertility diets and guidelines on what to do and what not to do for your best chance of conceiving.
You will also need to make sure that you are available to attend all appointments, often at relatively short notice. As IVF treatment depends very much on how and when your body reacts to the drugs, the timetable is individual to you and flexibility is important.
When will my treatment start?
Your IVF cycle will start on the first day of your period.
How does the IVF process start?
Usually, the process starts with fertility drugs to stimulate your ovaries to release more eggs. The medication will be administered by self-injection at home. Your fertility specialist will show you how to do the injections.
You will be asked to have scans and possibly blood tests during the stimulation stage, to observe how the follicles are responding to the medication.
When your follicles are ready, you will have an injection to mature the eggs, so they will be ready for collection.
What happens during egg collection?
Egg collection takes place 36-40 hours after the trigger injection. You will be given a light sedative to make you sleepy during the egg removal procedure, which will take around half an hour.
Eggs are collected using a fine needle, which is passed through the vaginal wall, with the help of a scanning probe.
Due to the sedation, you will need to rest after the procedure and have someone with you. Your clinic will advise you on any other possible precautions, which include not driving and not operating machinery for 24 hours.
What happens with sperm collection?
If you are using a sperm donor, the sample will have been produced much earlier and frozen, to allow time to assess for any genetic abnormalities or infections.
If you are using your partner’s sperm, a sample will need to be produced at the clinic on the same day as egg collection and a private room will be provided to do this.
After egg collection, you may be advised to take medication, to help to prepare the lining of your uterus ready for potential embryo transfer, if viable embryos are produced.
What happens in the insemination process?
The best sperm are selected and added to the eggs in a special dish. If you are having ICSI, the sperm will be injected into each egg. The dishes are then put into an incubator to enable fertilisation.
What happens next?
In the laboratory, experts will check to see if fertilisation has taken place and how any embryos are developing.
Your fertility clinic will keep you informed on the development of any embryos.
What happens during embryo transfer?
If any of the embryos are viable, five days after egg collection, you will need to go to the clinic for embryo transfer.
A catheter will be used to transfer either one or two embryos into your uterus. Only one or two embryos are transferred, to reduce the risk of multiple births. You may choose to have any other viable embryos stored to use in a later IVF cycle.
When will I know if the IVF has worked?
Your clinic will invite you in for a pregnancy test, at least 7 days after embryo transfer. It is advisable to wait for the clinic to do a test, rather than being tempted to do a test at home, as due to the medication and the timing, you may otherwise get either a false positive, or a false negative.
Pregnancy test results
The clinic will tell you whether or not the treatment has resulted in pregnancy.
If the test is positive, you will be told when to attend the clinic for a scan and given any further advice that you need for your pregnancy.
If you have a negative test, your clinic will be able to support you and talk about what your next steps may be.
Here at the IVF network, we know how challenging the IVF process can be, so we provide information and advice through our dedicated channel, blog posts and website, to help you to make informed choices throughout your fertility journey.
Thanks for visiting! GoodRx is not available outside of the United States. If you are trying to access this site from the United States and believe you have received this message in error, please reach out to [email protected] and let us know.

- Genetic Testing and Fertility
- Navigating Fertility Treatments
- Medications and Fertility
- Lifestyle and Fertility
- Hormones and Fertility
- Health Conditions and Fertility
- Fertility and Specific Populations
- Fertility and COVID19
- Beta hCG Level Calculator
- Egg Freezing Success Calculator
- IVF Due Date Calculator
- Dr. Lucky’s Comprehensive Guide to Fertility Preservation
- About Dr. Lucky
- Request an Appointment
How does IVF work? A step-by-step guide from an REI
- Posted by - Dr. Lucky Sekhon
- on - February 16, 2023
As a Reproductive Endocrinologist and Infertility Specialist (REI), I work with couples who are struggling with infertility and are looking for ways to conceive. One of the most common treatments we offer is In vitro fertilization (IVF). But, how does IVF work? IVF is a complex medical procedure that involves several steps, each of which is critical to the success of the treatment.
The first step in the typical IVF journey is an initial consultation. During this consultation, we review the couple’s medical history, perform a physical examination and assess their infertility diagnosis. We also discuss the couple’s options, and answer any questions or concerns they may have about the procedure. This consultation is a critical step to ensure that the couple is well-informed and prepared for the IVF journey.
The next step is ovarian stimulation. This involves using medications to stimulate the ovaries to produce multiple eggs. This step typically takes 8-14 days and involves daily injections of hormones that are administered by the patient or their partner. During this time, we monitor the patient’s hormone levels and follicular development to determine the optimal time for egg retrieval.
The third step in the IVF journey is egg retrieval. This is a minor surgical procedure that is performed under sedation or general anesthesia. During the procedure, a needle is guided through the vaginal wall and into the ovaries to retrieve the mature eggs. The eggs are then taken to the laboratory for fertilization.
The fourth step is fertilization. The eggs are mixed with sperm in the laboratory, and we use a technique called Intracytoplasmic Sperm Injection (ICSI) to inject a single sperm into each mature egg. The eggs are then observed in the laboratory for signs of fertilization and development.
The fifth step is embryo culture. Once the eggs have been fertilized, the resulting embryos are cultured in the laboratory for several days to allow them to grow and develop. During this time, we carefully monitor the embryos for quality and viability.
The sixth and final step is embryo transfer. This is a relatively simple procedure that involves placing the embryos into the uterus via a thin catheter. The patient does not typically require anesthesia, and the procedure is done on an outpatient basis.
Following the embryo transfer, the patient will undergo a pregnancy test to determine if the procedure was successful. If the test is positive, the patient will continue to receive medical care and monitoring throughout the pregnancy.
The IVF journey can be challenging, but it is also a rewarding experience for many couples who are looking to start a family. At our clinic, we provide compassionate care and support to our patients at every step of the way.

Dr. Lucky Sekhon
My name is Lucky Sekhon and I'm a double board-certified OBGYN, and Reproductive Endocrinologist & Infertility specialist practicing at RMA of New York . My mission is to empower women with practical and scientifically accurate information to make the right fertility decisions for themselves.
Follow me on Instagram to keep up to date with my fertility related posts and content.

IVF PROCESS TIMELINE
Here, we share a very broad overview of a typical IVF process timeline
We support thousands of people on their fertility journey each year, and we do see a common path. Here, we share a very broad overview of a typical IVF process timeline.
THE TIMELINE
One of the most common questions we are asked is – what is the IVF process timeline? Naturally, patients are keen to understand what will happen, and when, so they can prepare. Unfortunately, it’s not an easy question to answer.
Given the huge range of circumstances unique to each patient, and the corresponding range of solutions, there isn’t a ‘one-size-fits-all’ approach. That being said, we understand that going through the IVF process can be very stressful. Our team of friendly, expert patient advisors are here to support you however we can. If you’d like to chat about your IVF journey, please don’t hesitate to get in touch.
For more specific information bespoke to your fertility needs, consult with your clinic. The IVF process timeline often depends on the clinic, any waiting lists they have and what protocol they recommend for you. Use our clinic finder to see all the clinics that partner with Access Fertility in offering our programmes.
If you’re new to IVF, it can be confusing. You can use search engines to learn more, but you’ll find a minefield of misinformation and an overwhelming amount of choice.
We offer free nurse consultations to anyone who would like to explore their options. These consultations are totally free and cover all available treatment options, not just Access Fertility programmes. There is no waiting list to book our free nurse consultations – there are plenty of appointments available. You can discuss NHS treatment, private treatment or simply find out a bit more about the fertility options which exist.
Our fertility nurse, Kelly, will call you at the time you choose, for a 30 minute consultation. Come to the call with any questions or topics you’d like to cover – we’ll do our best to answer them. If you already know which treatment you need, you can skip to the next step. Please note that we can’t provide advice about any ongoing treatment. In that instance, you should speak to your doctor for information and advice.
BOOK AN APPOINTMENT
Once you have a better understanding of the options available to you, the next port of call is to find the right clinic for you. We recommend choosing a clinic that is near to where you live, as this will make the logistics of your treatment easier.
To help you find an IVF clinic near you, we have a useful map of our partner clinics, which you can look through at your leisure. All of the clinics listed here offer Access Fertility’s programmes, which are designed to lower and fix the cost of your treatment.
You will see there are contact forms on our site for you to easily get in touch with the clinic you prefer.
CLINIC FINDER
Around the same time, you can contact Access Fertility to register with us. Registration is free, and quick to complete – there are no waiting lists.
You can register over the phone, which takes around ten minutes. We don’t require you to undertake any further medical assessments to register with us. Instead, we ask for your permission to allow your clinic to share your test results with us. Once you’ve completed registration, we’ll give you access to an online portal. Here you can see all your account information whenever you need it.
Everything is done electronically or over the phone, meaning fewer physical appointments to add to your diary. You are only required to pay if you are going ahead with the programme and before you start treatment.
CONTACT US TO REGISTER
When you have found a clinic that you like, you should contact them to make an appointment. Many people assume that you will need a referral from a GP to get an appointment with a private fertility clinic. However, this isn’t actually required and you can self-refer whenever you are ready. Do note that it is standard practice for IVF clinics to register you before booking an appointment, and this can incur a small fee.
At this stage, there will be a big difference in the IVF process timeline, depending on which clinic you choose. Some clinics have a waiting list while others can see you immediately. This may be a consideration when you select the clinic that you wish to use.
Your first appointment at the IVF clinic will be an initial consultation with a fertility doctor. Some clinics offer pre-testing beforehand, others do your tests at the initial consultation itself or after.
On the one hand, if you’re sure of your preferred treatment, pre-testing can be useful, so you can discuss results straight away. On the other hand, if you’re still exploring your options it might be better to speak to the doctor first. Either way, it shouldn’t impact your IVF process timeline significantly.
At this stage, most of the tests are blood tests. Male partners will need to give a sperm sample. Some clinics may do a pelvic scan, which is done internally (transvaginally). They may also do a HyCoSy ultrasound to assess your fallopian tubes and your womb. The doctor will use a speculum to pass a dye through the cervix, which is then visible on internal (tranvaginal) ultrasound scans. If you have already had any of these tests done during NHS treatment, you may not need to do it again. Instead, the clinic will ask for your permission to access your medical notes.
Once your results are ready, the doctor will explain your options. For example, ICSI may be right for you, instead of IVF. At this time, you’ll go through the drug regime which the doctor recommends. This will allow you to more clearly see your own specific timeline for the process you’ll follow.
If you’re happy with the doctor’s recommendation, you’ll complete the clinic’s consent forms and HFEA consents to give permission for them to go ahead. This is an important step, and the clinic will explain what you’ve been asked to sign.
Before you start your treatment, the clinic fertility nurse will meet you to explain when and how to take the medication. All fertility treatment involves injecting medication, and the nurse will take you through how to do the injections. Feel free to come with any questions you have – it’s important you feel confident and comfortable.
There are two different ways you may start your treatment, and these will affect the beginning of your IVF process timeline, but not the outcome. The choice of protocol is purely based on clinic preference and your unique medical profile.
Short protocol – antagonist
Generally, most patients follow a short ‘antagonist’ drug protocol. On day one of your period, you’ll start injections of a drug that’s designed to stimulate your ovaries. You’ll follow the plan that you discussed with the clinic fertility nurse. Some people find the injections painless, while others find it very uncomfortable.
Similarly, many people manage to do their injections on their own, while others prefer to ask a partner to help. This can be a nice way to involve your partner in the process starting treatment IVF process.
The drugs you take will cause the oestrogen hormone level in your blood to rise. As a result, you may experience some breast tenderness or bloating, nausea, or increased emotions. Do talk to your fertility nurse if you have any concerns about your symptoms.
Throughout the two week period of stimulation, you’ll visit the clinic for blood tests and up to three scans. Some patients may need more than three. This is to monitor how your egg-producing follicles are developing. Your appointments will take place at times that suit you best, and take around 20 minutes.
During the short protocol treatment, your body will produce all the hormones you would normally create in a month. Part way through your treatment, you will start injecting a drug called Cetrolix, which will stop your body from ovulating prematurely. That way, the eggs can mature fully before they’re collected.
Long protocol – agonist
Conversely, a long ‘agonist’ drug protocol starts on day 21 of your period or day one. You’ll inject a drug called Buserelin for around two weeks, to suppress any ovarian activity (the down regulation). After a scan to check your ovaries are inactive and contain no cysts, you will switch to the short protocol regime, just as described above.
The long protocol is the oldest approach, and is less common. However, it is the most effective method to control the cycle and prevent premature ovulation. Doctors may prefer this option when the patient has ovarian cysts.
Side effects are more common from the Buserelin used in the long protocol. The reason for this is that the body is sent into a mini menopausal state when it suppresses all ovarian activity. As such, patients can experience hot flushes, headaches and lapses of memory. It is important to note that these effects are not permanent. Patients will usually feel fully better after treatment, when the body returns to normal.
Around 34-36 hours before you’re booked in for egg collection, you’ll do a ‘trigger injection’. You’ll do this at home, following the guidance from your fertility nurse. The trigger injection matures the eggs ready for egg collection. It contains ‘human chorionic gonadotropin’ (HcG), commonly known as the ‘pregnancy hormone’.
Once again, some patients do experience side effects from the trigger injection, while others feel none. Bloating, or stomach/pelvic pain are most common. A rarer complication is Ovarian Hyperstimulation Syndrome (OHSS), where the ovaries become swollen and filled with fluid. Your clinic will advise you on any abnormal symptoms and what to do if you have concerns.
On the day of your egg collection, you’ll visit the clinic for the procedure, which takes around half an hour. Doctors will pass a very fine needle through the vaginal wall and into the ovary to collect the eggs. You’ll be under a mild sedation to take the edge off any discomfort.
Consequently, you should plan to take the rest of the day off, and ideally the following day too, to recover from the sedation. It’s important that you have someone collect you from the clinic – you mustn’t drive because of the sedation.
If you’re planning to use a fresh sperm sample, the clinic will collect this on the same day as the eggs. The clinic will help you time this so that immediately after egg collection, they can be fertilised with sperm. Otherwise, if your treatment requires a sample taken via a surgical procedure, the sample will be taken before egg collection day and frozen. Occasionally, surgical sperm retrieval (SSR) is carried out on the day of egg collection.
Similarly, if you have sperm in storage, or are using a sperm donation, the clinic will thaw the sample on egg collection day.
Either way, on the day of egg collection, the embryologist will prepare the sperm sample so that the very best sperm are being used to fertilise the eggs.
There are two ways in which your eggs may be inseminated. artificial insemination: In Vitro Fertilisation (IVF) involves sperm being added to the eggs in a culture dish. Meanwhile, Intra-Cytoplasmic Sperm Injection (ICSI) is where the embryologist selects a single sperm and injects it into an egg, then puts the egg into a culture dish.
Either way, the culture dishes then go into an incubator for fertilisation. Your doctor will advise the right treatment for your unique circumstances.
The clinic can see within 24 hours how many eggs have been fertilised and will inform you of their progress. You’ll receive a grading of the embryos on day three that will tell you what potential they have for development.
Between day three and day five, some of those embryos will hopefully develop into blastocysts. Then, the clinic will give a blastocyst grading. This complex assessment helps the clinic to decide which are the best embryos to transfer.
Throughout this period, your clinic will keep in touch with Access Fertility to inform us of your results. That way, you can relax and focus on your treatment.
Shortly after egg collection, you’ll start taking drugs that help your body prepare to receive an embryo. This progesterone is taken as a vaginal pessary or gel all the way up until your pregnancy test (and beyond if it’s positive).
You’ll schedule embryo transfer around five days after egg collection, though this can depend on the number and quality of your embryos.
Once again, this stage of the IVF process takes place at the clinic. Some clinics do a ‘trial’ embryo transfer, so that doctors can see in advance if there will be any issues before the actual transfer. For the patient, the transfer itself will be identical. The embryo transfer procedure feels a little like a cervical smear, but lasts longer – around 20 minutes.
With the help of a speculum, a catheter carefully deposits a tiny drop containing an embryo into the uterus. Any other fertilised eggs can be frozen at this stage for future use. All our partner clinics follow HFEA guidance recommending they transfer only one embryo, to avoid the risks associated with multiple births. Immediately after embryo transfer, you can get back to normal activities, but you should avoid anything too strenuous.
It’s well-known that the two week wait after embryo transfer to find out if you are pregnant is extremely difficult. We understand how stressful it can be, and would encourage any patient to try and keep occupied during this time. It’s not necessary to have a doctor’s note for time off work – now is the time to keep your mind busy and live as normally as you can.
It is important that you wait for the full two weeks before taking a pregnancy test. Unfortunately, testing early can result in misleading results, which can cause unnecessary angst.
Some clinics ask patients to do a home pregnancy test, while others ask you to come in for a blood test. Either way, this will take place around 15 days after egg collection. pregnancy test IVF process. If you are pregnant, most clinics will offer a scan at around 6-8 weeks.
If everything looks OK, you can continue the rest of your pregnancy under the care of your GP and midwife. If your test result is negative, your clinic will be in touch to discuss your next steps. Either way, there is no need to contact Access Fertility. We will liaise directly with the clinic so you don’t have to. We understand that going through the IVF process can be very stressful.
Our team of friendly, expert patient advisors are here to support you however we can. If you’d like to chat about your IVF journey, please don’t hesitate to get in touch.
Access Fertility cover three pregnancy scans. One pregnancy ultrasound scan (6 or 7 weeks) which is conducted at your clinic. Two early dating scans between 9 and 15 weeks. The early dating scans are provided by our partner Ultrasound Direct and must take place at one of their locations. You will need to book your early dating scan via your Access Fertility patient portal .
CLINIC GUIDE
We asked 100 patients for their advice on ‘The 3 Cs of Choosing a Fertility Clinic’

IVF UNLIMITED
Our Unlimited Programme offers you as many IVF cycles as you need over two years and a 100% refund if you don’t have a baby, all for a fixed fee.

Our Access Fertility IVF Refund Programme offers you multiple IVF cycles for a fixed price, significant savings and a 100% refund if you don’t have a baby.

IVF MULTI-CYCLE
Our IVF Multi-Cycle Programme allows you to have multiple cycles of IVF for a fixed, discounted price. Giving you peace of mind that your IVF costs are managed.

IVF DONOR EGG REFUND
Our Donor Egg IVF Refund Programme offers multiple IVF cycles for a fixed price, significant savings and a 50%, 70% or 100% refund if you don’t have a baby.
GET STARTED
Call Access Fertility on 03300 10 20 40 for a free, no-obligation chat to discuss your options, or get in touch online.
If you’d like to hear more about what we offer, helpful information about fertility, and more, please submit your email address.
We promise to not get in touch too often or pass your details on to anyone else.
QUICK LINKS
- What we offer
- Refund Programme
- Privacy & cookies
- RETURNS & REFUNDS
- [email protected]
- 03300 10 20 40
LATEST BLOG

IVF Success Stories

Registered Company No. 08753396: Carlton House, High Street, Higham Ferrers, Northamptonshire, NN10 8BW
© Access Fertility 2024
UNITED KINGDOM
Understanding A Typical IVF Journey
Fertility experiences are all unique. Consequently, you can’t label any fertility treatment journey as ‘typical’. So, no matter the path your fertility specialist determines is the best for you, you can rest assured that you’ll be treated with compassion, care, and understanding throughout.
Most IVF cycles begin during a woman’s menstrual period. But, to make it easier to follow the various steps in the typical IVF cycle journey , we have grouped the steps into three Basic Principles of the process that are adjustable based on the patient’s needs.
Ovarian Stimulation & Egg Retrieval
Baseline Test: Day 1
The specialist schedules your office visit for day two or day three following the start of your menstrual flow. This visit is for a blood test and baseline ultrasound examination.
Ovarian Suppression: 2 – 4 Weeks
Before the specialist commences stimulation, they administer medication that suppresses the ovaries (like birth control pills). Ovarian suppression is typically from 1 to 4 weeks long. Your specialist then schedules another office visit at the end of this period, where they perform an ultrasound and blood test to ensure that they have achieved downregulation.
Ovarian Stimulation: 8-12 Days
The specialist uses injectable fertility medications to commence ovarian stimulation. This step happens on a day selected by the cycle coordinator. Then, you begin taking a precise dosage of fertility medications daily (preferably in the evening to accommodate any necessary dosage adjustments).
Cycle Monitoring: Starting Day 5
Regular office visits begin on day five of stimulation, then continue every one to two days until follicle aspiration. The specialist will perform an ultrasound and blood test during every visit. Additionally, you must call at the end of the day to get your blood test results and receive further instructions for continued medication.
Ovulation Induction: Between Day 8 and 12
The specialist triggers ovulation using an injection. They administer this trigger when they deem the follicles mature, typically between 8 and 12 days after you start receiving injectable fertility medications. The HCG dose timing is critical because they perform follicle aspiration 36 hours after the HCG.
Egg Retrieval: 36 Hours After HCG
The specialist will schedule your retrieval procedure. The aspiration process takes less than 30 minutes, so you can plan to have about a two-hour visit on the day of follicle aspiration.
Fertilisation & ICSI
Sperm Collection: Day of Egg Retrieval
Your fertility specialist obtains sperm from your partner (or donor, if that is the case) on the same day they perform the egg retrieval. Occasionally, they may request a final specimen the morning after egg retrieval. However, this is only necessary if there is sub-optimal fertilization and the embryologists are sure that an additional sperm sample may be useful. Note that it is best to abstain from ejaculation for two to seven days before the first sperm specimen. This approach optimizes sperm quality. In most cases, this will mean abstinence after the seventh day of fertility medications to the woman.
Fertilization: Day of Egg Retrieval
At this juncture, the specialists join the eggs and the sperm to allow fertilization. In most cases, they add a sperm solution to the eggs, at which point fertilization occurs naturally. Alternatively, they will conduct an Intra-Cytoplasmic Sperm Injection (ICSI) if indications call for it.
Assisted Hatching:
If the need arises, specialists will conduct Assisted Hatching to facilitate fertilization. This procedure is routinely performed for patients having preimplantation genetic testing done.
Preimplantation Genetic Test: 5-6 Days After Retrieval
Upon indication, specialists perform preimplantation genetic testing (testing for genetic conditions, chromosomal status, and gender determination) about 5 to 6 days after fertilization- when the embryo is at the blastocyst stage.
Embryo Transfer & Luteal Phase Support
Embryo Transfer: 3-5 Days After Egg Retrieval
Fresh embryo transfers typically occur around 3 to 5 days after egg retrieval. Frozen embryo transfers are usually scheduled during the week. This procedure is a simple one and doesn’t require anesthesia. However, the specialists occasionally give patients Valium to help with muscle relaxation. Therefore, it is essential to have someone drive you home afterward. For time scheduling purposes, please note that you must remain in bed for 30 minutes after the embryo transfer.
Excess Embryo Cryopreservation:
If there are any excess viable embryos left after the transfer back to your uterus, they may be frozen at this juncture.
Luteal Phase Support: Day of Transfer
You will get instructions outlining progesterone supplementation for your embryo transfer. But first, you must prepare to administer the progesterone via vaginal suppositories or injections. However, fertility specialists recommend using the progesterone until the end of the pregnancy’s first trimester or upon a negative second blood pregnancy test.
Pregnancy Testing: Days 12 and 14
Your physician will perform at least two pregnancy tests following the embryo transfer, after which they will contact you with the results.
The IVF journey is quite involved and often extended. However, you only need the right support system to help see you through. Moreover, remember that you can turn to your doctor for answers and reassurances to any questions and concerns you may encounter throughout the process.
Related Articles

Reports Suggest Binge Eating and Other Various Addiction Are Connected

How To Lower Fall Risks For Seniors

Premature Ejaculation (How To Last Longer In Bed)

How To Encourage A Healthy Lifestyle In Your Family
Advertisement
Uswnt legend lloyd announces pregnancy, opens up on difficult ivf journey, share this article.
U.S. women’s national team legend Carli Lloyd has announced that she and her husband Brian Hollins are expecting their first child.
Lloyd made the announcement in an Instagram post on Wednesday, saying that she is due in October.
The 41-year-old retired in 2021 after a decorated career that saw her go down as one of her sport’s all-time greats. At the time of her retirement, Lloyd said that she was hoping to start a family.
But Lloyd had a difficult journey to pregnancy, revealing in an essay for Women’s Health Magazine that it took her nearly two years and several rounds of in-vitro fertilization (IVF).
“I felt all the emotions during my career — stress, worry, fear, anxiety — but I’d never felt all the emotions that IVF brought on. I felt completely out of control. It’s an indescribable roller coaster unless you go through it,” Lloyd said.
She added: “When I look back at all the things I went through on the soccer field — whether it was a poor performance, getting benched, or missing a penalty kick in a World Cup final — there was always something I felt I could do to control the situation. I would go out and work 10 times harder. I was incredibly focused during my career. The majority of the time, the world saw me in competitor mode. A machine. I was often emotionless and numb because that’s the only way I felt I was able to survive and thrive.
“But this situation hit me so differently. I wasn’t emotionless or numb. Some nights I would lie in bed crying uncontrollably to Brian. I cried and worried a lot. I leaned on Brian more than I ever had, as well as on my family and friends. For the first time in my life, I needed their support to keep going.”
Lloyd said she wanted to fully share her story in order to let other people struggling with infertility know that they are not alone.
“I went from feeling embarrassed, ashamed, and afraid to tell people that I was going through IVF to now wanting to share my story to help others,” she said. “In times of struggle, we see what we are made of. We grow. We learn. And most important, we have more appreciation for the things we do have in life.”
View this post on Instagram A post shared by CARLI LLOYD (@carlilloyd)
USWNT to face Costa Rica in Olympic send-off match in Washington, D.C.
Uswnt 2024 schedule: results, fixtures, tv channel and streaming, carli lloyd: i was the only one brave enough to say it how it is.
Follow all of Pro Soccer Wire's USWNT coverage right here.
Most Popular
Which usmnt players could be changing clubs this summer, should de ligt's equalizer for bayern vs. real madrid have counted, pachuca vs. club america: how to watch liga mx playoffs, tv channel, live stream, uswnt striker morgan hopes to return 'very soon' from ankle injury, where to watch liga mx: tv channels, live streams, start times - thursday, may 08, la liga 2023-24 top scorers: tracking the pichichi race, stateside cup 2024: schedule, tickets, stadiums and more.
Please enter an email address.
Thanks for signing up.
Please check your email for a confirmation.
Something went wrong.
A gay couple couldn’t access IVF benefits. They’re suing New York City.
The first-of-its-kind class-action lawsuit alleges that the city’s denial of IVF benefits constitutes discrimination against gay men.

New York City is denying in vitro fertilization benefits to thousands of gay male employees of the city and their partners, a class-action lawsuit filed by a same-sex married couple alleged Thursday.
Brooklyn-based couple Nicholas Maggipinto, 38, and Corey Briskin, 35, claim the city is discriminating against male same-sex couples and violating federal, state and local laws by denying them IVF insurance benefits that other city employees are able to access.
“We were disheartened to say the least when we were told that we aren’t eligible for the IVF benefit because of the way the policy is phrased,” Briskin told The Washington Post. “We are entitled to equal treatment under the law.”
The lawsuit comes at a time when IVF has been thrust into national scrutiny after the Alabama Supreme Court ruled this year that frozen embryos are children . The lawsuit also comes at a time when LGTBQ rights are at the fore of U.S. politics, with states passing legislation to pull back gender-affirming care and to restrict the mentioning of sexual orientation in public schools.
After repeatedly asking the city to let them access IVF benefits to which more than 300,000 city employees are entitled, the couple are seeking reimbursements for all those who have been denied coverage since the benefits were made available, and they’re trying to force the city to change its policy to include gay men. The case hinges on whether the city can lawfully bar same-sex male couples from accessing IVF benefits.
A spokeswoman for City Hall, Liz Garcia, told The Post on Thursday morning that they will review the lawsuit.
The administration of New York City Mayor Eric Adams “proudly supports the rights of LGBTQ+ New Yorkers to access the health care they need,” Garcia said. “The city has been a leader in offering IVF treatments for any city employee or dependent covered by the city’s health plan who has shown proof of infertility, regardless of gender identity or sexual orientation.”
Briskin and Maggipinto had dreamed of raising children together since they began a relationship after meeting at law school in 2011. They married five years on.
“We both had a similar vision about what kind of a life we wanted,” Briskin said. “And it involved raising children together.”
They always knew that, for them, building a family would have to involve IVF and surrogacy.
For gay men and their partners, IVF is the only feasible way to conceive a child, the lawsuit says. IVF involves retrieving eggs from a patient’s ovaries, fertilizing them to create embryos and transferring embryos to the uterus.
The lawsuit alleges that the city’s policy should cover the egg retrieval and the creation of an embryo — benefits that can cost tens of thousands of dollars out of pocket that it already offers to other employees — for all couples, including gay couples. It does not allege that the city should pay for surrogacy or provide benefits for surrogates.
The city’s health-care plan has “categorically excluded gay male employees and their partners from receiving IVF benefits under the plan,” the lawsuit claims.
“It’s a real gut punch to so many of the gay men that work for the city that they are the group that needs IVF the most and they are the group that are excluded from it,” said Peter Romer-Friedman, the couple’s lawyer.
Who gets to access IVF benefits?
The couple first learned from the insurance representative for their doctor’s office that they could not receive the IVF benefits that heterosexual and same-sex female couples get because their situation did not meet the city’s definition of infertility. Then they made further inquiries on access to IVF benefits with the city’s Office of Labor Relations and a human resources employee at the district attorney’s office.
Everyone had the same answer: The couple didn’t meet the city’s definition of infertile.
According to the city’s insurance benefits policy, infertility is the inability to conceive after “12 months of unprotected intercourse” or intrauterine insemination, in which sperm is inserted directly into a uterus. The city has “interpreted it to mean intercourse between a man and a female,” the lawsuit claims.
The city’s medical definition of infertility, which Maggipinto describes as “restrictive and exclusive,” has raised questions.
“The city is discriminatory towards same-sex male couples because they cannot satisfy the definition of infertility the city is choosing to follow,” said Betsy Campbell, the chief engagement officer at Resolve: The National Infertility Association, adding that the city does not have to choose to follow New York state’s definition.
She said that the American Society for Reproductive Medicine updated its definition of infertility last year, defining it as the “need for medical intervention, including, but not limited to, the use of donor gametes or donor embryos in order to achieve a successful pregnancy either as an individual or with a partner.” ASRM said the definition is not exhaustive.
Campbell says the city may be following the definition of infertility as understood by New York state, but it is not following the spirit of the law, which seeks to be inclusive.
The law offers a provision , she said, that should have provided exceptions to Maggipinto and Briskin’s case: “Earlier evaluation and treatment may be warranted based on an individual’s medical history or physical findings.”
Moreover, then-New York Gov. Andrew M. Cuomo’s executive order in 2021 legalizing gestational surrogacy highlighted that the law should apply equally to all couples struggling to build families, Campbell said. No longer will anyone “be blocked from the joys of starting a family and raising children simply because of who they are,” Cuomo had said.
None of this has helped Maggipinto and Briskin so far.
“You still have government entities deciding who can and can’t have children,” Maggipinto said, adding that even adoption is much harder for same-sex male couples than other couples. “When you base decisions like that on nothing other than sexual orientation, then gay men are being made to look like we can’t be good parents.”
A long journey
When Briskin joined the Manhattan district attorney’s office in 2017, the couple began planning for IVF under the city’s insurance plan. He is still under that plan through COBRA, a continuation of health coverage, even though he has since left the job.
After writing to the city’s Office of Labor Relations in 2021 and learning that they are categorically barred from IVF benefits, the couple filed a complaint with the U.S. Equal Employment Opportunity Commission in 2022.
The class-action discrimination complaint against the City of New York claimed that the city’s denial of IVF benefits to the couple and other gay male employees “constitutes unlawful sex and sexual orientation discrimination.” The couple alleged that the city government violated their civil rights by refusing to pay for fertility services that were covered for women and cisgender couples.
At the time, in a statement similar to Thursday’s statement, a spokesperson for City Hall told The Post : “Our policies treat all people under the program equally, regardless of gender identity or sexual orientation.”
The statement left the couple confused, they said.
“The city has the right talking points and the intention seems to be good,” Briskin said. “But the policy that the city espouses and offers to its employees just don’t reflect that sentiment at all.”
In March — almost two years after the complaint was filed — the EEOC granted the couple the right to institute a civil action against the city because the commission had begun an investigation but had not yet reached a conclusion.
The process has taken longer than either Briskin or Maggipinto expected. They said they wanted to start a family seven years ago.
While waiting for the city to grant them access to benefits, they have paid for egg retrieval and fertilization services out of pocket, which has set them back to pay for the surrogacy part of the pregnancy.
Although the couple is hopeful that the lawsuit will take them a step closer to the outcome they have been waiting for, they said that the journey has had many disappointments.
“I made many sacrifices, including my energy and my earning potential, while serving as a prosecutor in the public sector,” Briskin said. “All that to be told that me building a family doesn’t matter to the city in the same way as other employees building a family matters to them.”


Olympia Valance shares intimate details about IVF journey
- READ MORE: Olympia Valance dishes on the Neighbours reboot
Olympia Valance has revealed intimate details about her IVF journey with husband Tom Bellchambers.
The former soap star , who memorably played Paige on Neighbours, says the lengthy process left her worn out and the 31-year-old reached a low point following a tragic miscarriage.
'My body was exhausted and my mind was spent,' she said in an interview with The Daily Telegraph on Thursday.
'I’ve always been an outgoing, happy person and found myself becoming a hermit. I needed a full reset.
'I really wanted to get out of the house and out of my comfort zone,' she continued.
Olympia jumped at the opportunity to take part in Channel Nine's real life mountaineering show The Summit, admitting it was just what she needed to recover from her IVF experience.
'When I got back, I felt great. I decided I want to live again and enjoy life,' she told the publication.
'I’m sick of being disappointed every month. I don’t want my next two to three years to revolve around IVF. So we’re going to do life and see what happens.'
In July, 2023, Valance revealed that she miscarried twin babies during the Covid pandemic and later that year revealed she had a second miscarriage at six weeks.
Olympia and football player Thomas, 34, were married in June 2022.
The half-sister of Holly Valance, Olympia will be appearing in The Summit alongside Baywatch star Simmone Jade Mackinnon and former Bardot band member Tiffani Wood.
The series, filmed in the rugged alps of New Zealand’s South Island, saw Valance thrown together with 14 strangers to climb a mountain in 15 days.
Other famous competitors on season two, which debuted last Saturday, include former NRL player Mat Rogers.
It comes after Daily Mail Australia revealed the series was on the brink of cancellation after season one failed to win high ratings.
A Nine insider told Daily Mail Australia the network previously had no plans for a season two, but decided to give it the green light.
The Jai Courtney-hosted action-adventure series, initially touted as the network's breakout series of the year, struggled to climb above around 400,000 viewers.
The source painted a picture of a series fraught with production nightmares and financial setbacks due to severe weather conditions.
Filming the action-packed 8500ft New Zealand mountain trek proved a herculean task, costing hundreds of thousands.

Service members and veterans are fighting for the right to fertility treatments
After having flown helicopters and fixed-wing aircraft in the Marines for 11 years, Jacquelyne Nichols left active-duty service and joined the reserves in part to pursue a new mission: building a family.
But Nichols and her husband — who also served in the Marines — struggled to conceive when she returned home from deployment in Qatar in 2018, launching her on a yearslong fertility journey.
“I knew that I could potentially sacrifice my life, limbs and health,” she said. “But what I didn’t know was that I could potentially lose my fertility as a result of my service.”
Nichols, 41, is undergoing in vitro fertilization treatments and qualifies for the Department of Veterans Affairs to cover the costs, but at times getting it to pay for her benefits is “a fight. It’s basically a full-time job to make sure that I’m getting what I need.”

Nichols is part of a growing push for the VA and the Defense Department to expand the availability of fertility care to veterans and service members, who may experience rates of infertility three times higher than the general population. While some progress has been made, advocates say one of the biggest remaining barriers is the requirement that veterans and service members prove that their infertility is related to their service.
The VA said in a statement to NBC News that it is “constantly working to expand access to care” and is “committed to helping as many veterans as possible raise a family.”
The Pentagon and the VA have covered fertility care for years — but the rules have limited which service members and veterans are eligible.
Last year , the National Organization for Women-New York City filed a federal lawsuit against the two agencies, alleging that they were “restricting access to fertility treatment on the basis of discriminatory and arbitrary markers” for veterans and service members struggling to build their families.
After the suit was filed, the Pentagon and the VA expanded access to IVF benefits for eligible service members and veterans who are unmarried or in same-sex couples.
But IVF is still available only for people who can prove their infertility was caused by their service, such as women who suffered injuries to their reproductive organs in combat or the partners of men who take medication for post-traumatic stress order that lowers sperm count.
Renée Mihail — an Army veteran — works with the Yale Veterans Legal Services Clinic, which is representing the plaintiffs in the suit. She applauded the agencies for ending their bans on treatment for those who are single or in same-sex couples. But, she said, the main barrier to accessing care still remains: proving that infertility is service-connected.

While it is hard to scientifically prove that infertility is linked to service, “many service members are exposed to toxic chemicals or physical or environmental hazards that impair their ability to have children,” Mihail said.
“I served with so many people who seemed to be struggling with fertility,” she said, “whether that was a result of the fact that they delayed family building in order to pursue their careers or for medical reasons that they didn’t necessarily know or understand. And it felt to me as if it was not just a coincidence.”
Infertility in the military is understudied. But in a 2018 survey , 37% of active-duty women said they struggled with infertility, a rate that is three times the national average.
Nichols said she isn’t surprised by the survey, adding that “as an aviator, a lot of it has to do with radiation exposure … flying at high altitudes. All of these things can have a negative impact on our fertility, and not just women — men, too. We don’t even know the full extent of this problem.”
Sen. Tammy Duckworth, D-Ill., an Iraq War veteran who lost her legs in combat, said it might take decades to find a direct link. But she said military infertility is much like Agent Orange — it took the VA decades to recognize that military exposure to Agent Orange, an herbicide the U.S. military dropped by the ton on jungles during the Vietnam War, is most likely linked to certain cancers.
Duckworth is pushing Congress to do something now, having introduced legislation to expand access and coverage of fertility benefits for service members and veterans, but Republicans have objected to the undefined cost of the bill.
Duckworth, who used IVF to conceive both of her children, said: “I went through almost 10 years of fertility struggle. And in that process, I learned that my infertility is likely linked to my military service. The people who defend us and protect the Constitution deserve to be able to start their families, as well, and have their American dream. And I would hate to be the one to tell a soldier, ‘Sorry, thank you for your service, but you don’t get to be a dad.’”
Meanwhile, the National Organization for Women-New York City lawsuit against the Pentagon and the VA is ongoing. Oral arguments over the government’s motion to dismiss it will be held later this month in federal court in New York.
Both departments told NBC News that they don’t comment on pending litigation.
Maite Amorebieta is a senior investigative producer with the NBC News Investigative Unit.
Chloe Atkins reports for the NBC News Investigative Unit, based in New York. She frequently covers crime and courts, as well as the intersection of reproductive health, politics and policy.
Courtney Kube is a correspondent covering national security and the military for the NBC News Investigative Unit.

IMAGES
VIDEO
COMMENTS
The typical IVF (In Vitro Fertilization) treatment timeline is a multi-step process that usually spans several weeks. Each cycle of IVF includes multiple stages, although the exact timeline can vary based on individual circumstances and protocols of the fertility clinic. ... Deciding to embark on an IVF journey is a monumental, intimate ...
An experienced fertility nurse breaks down the typical IVF timeline and answers common questions about the process. August 22nd, 2023 | 12 min. read ... Our Journey to IVF Identical Twins | Christa & Aland's Story March 27th, 2024 9 min read 23 IVF Questions to Ask a Fertility Doctor at Your First Appointment
Unite sperm and eggs. Now comes the part of IVF that everyone's the most familiar with — combining the best sperm with your best eggs. This stage is called insemination. It usually takes a few hours for a sperm to fertilize an egg. Your doctor may also inject the sperm directly into the egg instead, a process known as intracytoplasmic sperm ...
Choose lean proteins, like fish and poultry. Eat whole grains, like quinoa, farro, and whole grain pasta. Add in legumes, including beans, chickpeas, and lentils. Switch to low-fat dairy products ...
A typical IVF journey, whether it is for the first time or trying again, can also be called a 'stimulated cycle'. This is because your treatment will involve taking drugs that stimulate your body so we can collect a number of eggs for fertilisation. If you're not sure which options are best for you, you can attend one of our FREE ...
Let's explore the IVF journey from start to finish. Step 1: Initial Consultation and Fertility Assessment - Three to Four Weeks. The IVF process begins with an initial consultation with a fertility specialist or reproductive endocrinologist. During this consultation, you doctor will review the medical history of the individuals or couple ...
Often, a typical IVF journey will start off with a few weeks on the birth control pill to make scheduling easier, according to the Massachusetts General Hospital Fertility Center. Then you'll start fertility medications, mostly likely gonadotropins—hormone medications that stimulate your ovaries to produce eggs—that you'll inject ...
IVF Cycle Timeline. You'll call your clinic on Day 1 of your period. The you'll go in to the clinic on Day 2 or 3 for an ultrasound and bloodwork. At this point, your doctor will be able to clear you to begin the cycle. You'll be given a treatment calendar listing which medications to start on what days.
Remember, each IVF journey is unique, and success rates can vary based on numerous factors, including age and underlying fertility issues. While it is a complex process and can feel overwhelming at times, we hope that now that you know how IVF works you have more clarity as you embark on the next step of your fertility journey.
The Ultimate Guide to In Vitro Fertilization (IVF) Written by PFCLA. 09/28/2020. According to the National Survey of Family Growth conducted by the Centers for Disease Control and Prevention, approximately 1 in 8 couples struggle with infertility --an estimated 49 million couples worldwide. Building a family is a milestone for many people.
A mom who went through IVF explains what the journey was like from start to finish and offers advice to other hopeful parents. I remember meeting with a reproductive specialist for the very first ...
The IVF process and its timeline can be different for individuals as no two cases are similar and may require a specialized approach. Although each cycle can be a little bit different, the in vitro fertilization or IVF process usually lasts between 2 to 6 weeks. DOWNLOAD IVF TIMELINE TEMPLATE. The IVF patient uses the first 3 weeks of the cycle ...
Step 4: Ovarian Stimulation (Day 2-3) The IVF cycle starts with you coming in on Day 2-3 of your menstrual cycle to have a baseline ultrasound and blood work done. If all looks good with your ultrasound and hormone levels, you will begin your injections that night. Generally, you will inject yourself once daily with two different medications.
In vitro fertilization is the most effective type of fertility treatment that involves the handling of eggs or embryos and sperm. Together, this group of treatments is called assisted reproductive technology. IVF can be done using a couple's own eggs and sperm. Or it may involve eggs, sperm or embryos from a known or unknown donor.
journey towards maturation, about 10-20 egg follicles are typically seen within the ovary at the time of menstruation. From there, only one - the so-called dominant follicle - will mature and is released at the time of ovulation. Our goal during a typical IVF cycle is to stimulate many of these eggs to mature so that we can
Assuming Day 1 is the first day of your menstrual cycle, here's what a typical IVF calendar will include: Day 2-3. Ovarian Stimulation: The IVF cycle starts with a 9-15 day period of ovarian stimulation, using hormone injections called gonadotropins or follicle stimulating hormones, to produce multiple follicles and allow as many eggs as possible to mature for retrieval from the ovaries.
IVF is often referred to as a journey. It's not just a single procedure, but a process, involving multiple hospital visits, a variety of medication, physical and emotional challenges and a lot of waiting. It's therefore important to be mentally and physically prepared before you begin your IVF cycle, as feeling informed about what you can ...
IVF — also known as in vitro fertilization — is a widely used process that helps people get pregnant with the help of medical intervention. It involves eggs being fertilized with sperm outside of the body. Once the eggs are fertilized and turn into embryos, they are then placed inside of the uterus to grow.
The first step in the typical IVF journey is an initial consultation. During this consultation, we review the couple's medical history, perform a physical examination and assess their infertility diagnosis. We also discuss the couple's options, and answer any questions or concerns they may have about the procedure. ...
Access Fertility supports thousands of people on their fertility journey every year, here we share a typical IVF process timeline. Skip to content. CONTACT US. Call us 03300 10 20 40. Contact Us. Call us 03300 10 20 40. WHAT WE OFFER. IVF Unlimited Programme; ... If you'd like to chat about your IVF journey, please don't hesitate to get in ...
There are several steps in the average IVF journey, and egg retrieval comes about halfway through. One cycle of IVF can take three to six weeks, and the stages typically involve: ... According to one big study from Guy's and St Thomas' Foundation Trust in London, the average number of eggs collected from IVF egg retrieval is 9, with 15 eggs ...
Pre-IVF stages 1. Counselling and consent At the beginning of your IVF journey, a clinician will explain and discuss the procedure with you. At this point, you may feel overwhelmed and bewildered by the toll that IVF can take on your mental well-being. There are several aspects to consider, and important medical decisions that have to be made.
Most IVF cycles begin during a woman's menstrual period. But, to make it easier to follow the various steps in the typical IVF cycle journey, we have grouped the steps into three Basic Principles of the process that are adjustable based on the patient's needs. Ovarian Stimulation & Egg Retrieval. Baseline Test: Day 1
But Lloyd had a difficult journey to pregnancy, revealing in an essay for Women's Health Magazine that it took her nearly two years and several rounds of in-vitro fertilization (IVF). "I felt all the emotions during my career — stress, worry, fear, anxiety — but I'd never felt all the emotions that IVF brought on.
The lawsuit alleges that the city's policy should cover the egg retrieval and the creation of an embryo — benefits that can cost tens of thousands of dollars out of pocket that it already ...
Olympia Valance has revealed intimate details about her IVF journey with husband Tom Bellchambers. The former soap star, who memorably played Paige on Neighbours, says the lengthy process left her ...
Olympia Valance has told of her heartbreaking IVF journey, saying she has put her quest to become a mum on hold. Valance and her husband, former Essendon star, Thomas Bellchambers, have been open ...
Duckworth, who used IVF to conceive both of her children, said: "I went through almost 10 years of fertility struggle. And in that process, I learned that my infertility is likely linked to my ...