You are using an outdated browser. Please upgrade your browser or activate Google Chrome Frame to improve your experience.

- Pay Invoice


New Medicare Rules for Split / Shared Visits: What’s Changing and What To Do
In the 2022 Medicare Physician Fee Schedule Final Rule (Final Rule), the Centers for Medicare & Medicaid Services (CMS) announced new rules for split/shared visits in the facility setting. For 2022, such visits may be billed under the National Provider Identifier (NPI) of the physician or non-physician practitioner (NPP) who either (1) documents the support for the history, exam, or medical decision-making for the visit, or (2) provides more than 50% of the service time. For 2023, split/shared visits must be billed under the NPI of the individual who provides more than 50% of total visit time.
These new rules could significantly impact Medicare reimbursement for physician practices that use NPPs in facility settings. For evaluation and management (E/M) visits jointly furnished by a physician and NPP in the same group practice in a facility setting (e.g., place of service [POS] 21 inpatient hospital or 22 provider-based clinic), CMS has permitted the visit to be billed under the physician’s NPI. Specifically, CMS’ split/shared visit rule has required that a physician perform only some portion of the E/M visit in order to bill that service under the physician’s NPI. Thus, the practice received full payment for the visit rather than the 85% of the Physician Fee Schedule rate paid for services billed under an NPP’s NPI.
In the Final Rule, CMS clarified and made several changes to its rules for split/shared visits:
- The split/shared visit rules do not apply to office visits (place of service 11); instead, these visits may be billed ‘incident to” if the requirements are satisfied (established patient, established plan of care/condition, direct supervision). CMS has signaled that it will be reviewing the incident to rules in future rulemaking.
- CMS now will permit split/shared visits to be reported for new patients as well as established patients, for initial as well as subsequent visits, for critical care services, for prolonged E/M visits, and for skilled nursing facility/nursing facility E/M visits (other than those required to be performed in their entirety by a physician).
- CMS will require the use of a new modifier (yet to be identified) to identify all claims for split/shared visits.
- Documentation in the medical record must identify the two individuals (physician and NPP) who performed the visit.
- For 2022 only, split/shared visits may be billed under the physician’s NPI if (1) the medical record documentation indicates the physician performed one of the three key components (history, exam, or medical decision-making) in its entirety, or (2) more than half of the total time for the visit was spent by the physician. Otherwise, the visit must be billed under the NPP’s NPI. (For critical care services, only time may be used.)
- Beginning in 2023, only time will be used to determine the substantive portion of the visit.
Table 26 in the Final Rule summarizes these requirements:
Many practices now have an NPP perform initial rounds in the hospital, followed by a physician briefly seeing each patient later in the day. These practices now bill these services under the physician’s NPI and thus receive 100% of the Physician Fee Schedule rate. Going forward, however, it is unlikely the time spent by the physician will exceed the NPP’s time. Thus, these services will have to be billed under the NPP’s NPI, and the practice’s reimbursement will be reduced by 15%.
Compliance tips:
- Only apply these rules to Medicare claims reporting. Monitor other payers for their split/shared visit requirements, which are usually a part of the payer’s incident to policy.
- Review physician and NPP contracts for potential impacts to compensation as the billing for these services will likely shift to the NPP. Work relative value unit (wRVU) capture for these providers will likely be different from what was anticipated during the compensation design.
- Time-based: Select the billing provider based on the predominance (more than 50%) of time spent.
- E/M guidelines-based (2022 only): Select the physician only if history, exam, or MDM are fully documented in support of the code to be reported.
If documentation is lacking from the physician, including time or a full component, report the code under the NPP’s NPI.
- Time-based: Select the level of code based on 1995 or 1997 E/M documentation guidelines. Note that supporting this time requires documentation of counseling and/or coordination of care exceeding 50% of the physician’s unit or floor time focused on the patient. Use of total time is recommended.
- E/M guidelines-based: Use the documentation of both providers per the 1995 or 1997 E/M guidelines key components to select the level of service supported.
- Ensure Medicare enrollment for NPPs is active and accurate.
- Monitor Medicare Administrative Contractor (MAC) guidance on the application of this new policy.
- Use this PYA checklist to evaluate compliance with the new rules:
For related information, view our webinar “Timely, Tough, or Tricky – Physician Comp and FMV Topics | Group Practice Exception Changes and APPs” .
If you require assistance relating to E/M documentation and coding compliance, or with any matter involving compliance, valuation, or strategy and integration, one of our executive contacts would be happy to assist. You may email them below, or call (800) 270-9629.
Executive Contacts
Thanks for reaching out. You can contact me at 404-266-9876.
Thanks for reaching out. You can contact me at .

- Privacy Overview
- Strictly Necessary Cookies
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
Hello, please sign in
New to MGMA? Start here Access My Dashboard

2022/2023 Split/Shared Visit and Service Reference

Recent changes to the Centers for Medicare & Medicaid Services (CMS) rules for split/shared encounters involving physicians and advanced practice providers (APPs) are an important area for healthcare leaders to understand, as they are sometimes confused with teaching physician or incident-to rules. These rules, codified in CMS Regulation § 415.140, are set to be updated with implementation of a new final rule in 2023 following an initial rule update that was made effective in January 2022. This member-exclusive split/shared visit and service reference details the 2022 and 2023 substantive portion definitions, as well as place of service and modifier usage, for E/M visits in outpatient facilities (excluding office visits in non-facility settings), hospital facilities, and skilled nursing facilities.
Additional resources
- Read more about the changes planned for 2023 from Amanda Rumpke, MSN, APRN-CNP, system director of advanced practice clinicians at Pulmonary and Critical Care Consultants of Fairfield, in her recent article, “Maximizing your advanced practice workforce through implementation of CMS’ 2023 MPFS split/shared rule”
- Learn even more by registering for the June 29 member-exclusive webinar, “The 2023 Split/Shared Rule: Is your Medical Group Ready?”

Veronica Bradley , CPC, CPMA
Veronica Bradley, CPC, CPMA, has more than 20 years’ experience in medical coding and auditing in various specialties. She is also well-versed hierarchical condition category and risk adjustment coding. Other areas of expertise include E/M, procedural coding, Medicare reimbursement and other critical factors in coding and auditing. Veronica has worked in private practice, group practices, academic school of medicine and hospitals. Veronica received a bachelor’s degree in health information management and a minor in healthcare administration from Regis University in Denver.

Explore Related Content

Ask an Advisor: Medical assistants administering injections
MGMA Staff Members

Executive Session: Proactive and reactive auditing for strong compliance and maximizing revenue
Beverly Gibson

Keeping compliant can help avoid unpleasant tangles with CMS
Andy Stonehouse
2023 CPT® E/M Time-Based Coding Guide
Veronica Bradley

New CMS rule on split/shared encounters set to be delayed until 2024
Amanda Rumpke

Compliance Basics for Every Practice: Fair Market Value and Coding - on demand
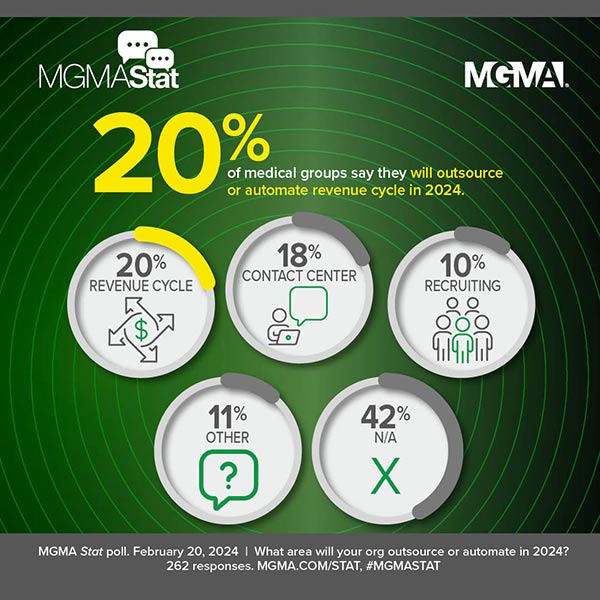
Revenue, recruiting and patients: 3 key areas of outsourcing, automation for medical groups in 2024
Chris Harrop

Strategies for accurately and compliantly coding for HCCs and E/M changes

The most-asked questions about medical coding audits following the 2021 E/M and MDM changes

Implementing the No Surprises Act
More insight articles.

HCPCS code revisions for 1st Quarter 2024

Truth in labeling: Evaluating ChatGPT’s assessment of itself for enhancing patient experience in medical practices
Jacqueline Wu
Applying people-centered leadership theories to navigate change
Steve Brewer

Beyond hierarchies: Pushing the limits of empowerment in your medical practice
Cornelia Vremes

No more flying the coop: Build a retention-driven culture in your organization
Colleen Luckett

Compensation is to recruitment as culture is to retention
Tony Stajduhar

Got reviews? Improving patient experience to enhance quality outcomes
Stacy (Yonker) Atwell

Data Mine: Defying gravity — Are medical groups entering an era of increased productivity?
David N. Gans

Key considerations for your next anesthesia arrangement
Natalie Bell

Value-based management: Taking a wellness approach for better organizational outcomes
Owen J. Dahl

4 steps for creating value in the hospital-based physician enterprise
Brian Dennen

Finding revenue despite depleted resources and payer confusion over new weight-loss medications
A roadmap to success for new medical practice leaders

Addressing productivity, burnout and access via data-driven transparency and accountability

5 key cash flow crisis management strategies for medical practices after the Change Healthcare outage
Andrew Hajde


Mirror, mirror on the wall, will the patient show at all?
Sharon V. Nir

Artificial intelligence in diagnosing medical conditions and impact on healthcare
Vikash Ayyappan

Release of information: What you don't know can cost you
Shelby A. Dodd

The lost art of customer service
Julie Ann Bouziotis

Knock, knock... Who’s there? Considerations for when private equity comes for physician acquisitions
Joe Aguilar
Explore Related Topics

- Become a Member
- Everyday Coding Q&A
- Can I get paid
- Coding Guides
- Quick Reference Sheets
- E/M Services
- How Physician Services Are Paid
- Prevention & Screening
- Care Management & Remote Monitoring
- Surgery, Modifiers & Global
- Diagnosis Coding
- New & Newsworthy
- Practice Management
- E/M Rules Archive
April 21, 2024
CMS’s 2024 Shared or Split Services Policy: Document and Report Them Correctly
In 2024, CPT expanded its definition of split/shared services, CMS updated their requirements.
- CPT expanded its definition of split/shared services in 2024, stating that the substantive portion can be determined by the practitioner who spent more than 50% of the time, or who made or approved the medical decision making.
- CMS will allow the substantive portion to be determined based on the practitioner who spent more than 50% of the time or the practitioner who performs the medical decision making (MDM). They have removed allowing documenting history or exam in its entirety, since these are not current CPT concepts.
- CMS continues to say that this is a delay until 2025 when only time can be used, but this is the third delay by my count.
- CMS says when the work is shared, “we expect that whoever performs the MDM and subsequently bills the visit would appropriately document the MDM in the medical record to support billing of the visit.”
- Services may include both face-to-face and non-face-to-face activities.
- Services billed using the physician’s NPI are paid at a higher rate than those billed by a non-physician practitioner.
- For Medicare, shared services may only be done in a facility setting; shared services may not be performed in place of service 11 for Medicare patients. CMS notes that there is an incident to benefit for the non-facility setting.
- CPT is silent about location.
- Medicare requires HCPCS modifier FS- Split (or shared) Evaluation and Management service to identify shared services.
- Terminology: CPT uses “other qualified health care professionals” and CMS uses “non-physician practitioners” to describe APRNs and PAs who have E/M in their scope of practice in the E/M section of the CPT book.
CPT Split/Shared Services Guidance 2024
All CPT quotes from p.6 CPT 2024 Professional Ed. AMA, 2024
- Download Slides
- Download this Split/Shared Services CPT CMS Comparison for quick reference
E/M services may be billed as shared or split services when they are jointly performed by a physician and another practitioner who has E/M in their scope of practice, i.e., APRNs, PAs. CPT notes that physicians and qualified health care professionals (QHPs) often act as teams in caring for patients, and may work together during a single encounter. The 2024 CPT book continues to allow practitioners to determine the substantive portion by time or MDM. If using time, he practitioner who spent greater than 50% of the time can report the service; time spent with the patient jointly by both practitioners can only be counted once.
If using MDM to determine the substantive portion. CPT says:
“… performance of a substantive part of the MDM requires that the physician(s) or other QHP(s) made or approved the management plan for the number and complexity of problems addressed at the encounter and takes responsibility for that plan with its inherent risk of complications and/or morbidity or mortality of patient management. By doing so, a physician or other QHP has performed two of the three elements used in the selection of the code level based on MDM.”
But, CPT adds a distinction between the three elements. If the number and complexity of problems and risk are used to select the level of service, the encounter can be reported by the practitioner who “takes responsibility for that plan.” If data is one of the three elements it is more complicated.
“If the amount and/or complexity of data to be reviewed and analyzed is used by the physician or other QHP to determine the reported code level, assessing an independent historian’s narrative and the ordering or review of tests or documents do not have to be personally performed by the physician or other QHP, because the relevant items would be considered in formulating the management plan. Independent interpretation of tests and discussion of management plan or test interpretation must be personally performed by the physician or other QHP if these are used to determine the reported code level by the physician or other QHP.”
That is, if data is one of the elements in selecting the level of service and there is an independent interpretation or discussion of management or test results with another health care professional that is being used to select the level of code, those activities must be done by the billing clinician (to support the substantive portion). Side note: This will be difficult to explain to practitioners and audit.
Location and wording
CPT is silent about location, not restricting the use of split/shared services to any location.
CPT is silent about who must document the visit. The wording, “… made or approved the management plan…” seems to imply that an attestation statement is sufficient.
CMS rules 2024
CMS continues to use the terms “nonfacility” and “noninstutional” to describe place of service where split/shared services are allowed. Specifically in the 2024 Final Rule, they state that in the office, incident to rules apply, not split/shared. Use CPT place of service codes to determine if the setting is a facility or non-facility. Office and other outpatient services (99202–99215) reported in place of service 11 office may not be reported as shared services. Office and other outpatient codes in place of service 19 or 22, outpatient hospital, may be reported as shared services.
This is what CMS says about documentation of split/shared services. “Although we continue to believe there can be instances where MDM is not easily attributed to a single physician or NPP when the work is shared, we expect that whoever performs the MDM and subsequently bills the visit would appropriately document the MDM in the medical record to support billing of the visit.” p. 475 of the Final Rule. Link at the end of the article.
“Appropriately document” is not defined by CMS. However, some MACs in 2023 have described what the physician needs to document to support billing the substantive portion. NGS, in their E/M Q&A section says this:
“10) Would you consider a shared/split service if the MD’s documentation was listed as an addendum on the NPP’s note? Answer: Split/shared services in the hospital setting require performance of the medically necessary elements (history, exam, MDM) or cumulative time spent by both the billing physician and NPP. The only way for a physician and NPP to describe his/her own personal contribution to the service is to document an individual note describing the portion of the service performed. Example: “I have seen and examined the pt. with the PA and agreed with A/P and physical exam findings (and then a summary of items/data already listed by the PA,” the physician is indicating his/her participation in the physical examination and review of the medical decision making; this would be adequate to support the physician’s participation. In order to bill the service as the “substantive” provider, the physician’s documentation would need to describe the physician’s work as exceeding the NPP’s work in completing the service. In either reviewing the NPP’s history and/or exam findings and in formulating a medical decision, the physician’s performance and documentation would need to exceed the NPP’s efforts and documentation of the split/shared service.”
https://www.ngsmedicare.com/ja/evaluation-and-management?lob=96664&state=97224&rgion=93623&selectedArticleId=330568
If NGS is your MAC, the physician must document their own medical decision making, if MDM is used to select the code level. Check your own MAC.
Whoever is billing for the service, CMS requires that the documentation must identify the two individuals who performed the service and the billing professional signs and dates the record.
CMS Final Rule can be found here:
https://public-inspection.federalregister.gov/2023-24184.pdf
Back to blog
Want unlimited access to CodingIntel's online library?
Including updates on CPT ® and CMS coding changes for 2024
Last revised April 1, 2024 - Betsy Nicoletti Tags: medicare incident-to and shared services
CPT®️️ is a registered trademark of the American Medical Association. Copyright American Medical Association. All rights reserved.
All content on CodingIntel is copyright protected. Any resource shared within the permissions granted here may not be altered in any way, and should retain all copyright information and logos.
- What is CodingIntel
- Terms of Use
- Privacy Policy
Our mission is to provide up-to-date, simplified, citation driven resources that empower our members to gain confidence and authority in their coding role.
In 1988, CodingIntel.com founder Betsy Nicoletti started a Medical Services Organization for a rural hospital, supporting physician practice. She has been a self-employed consultant since 1998. She estimates that in the last 20 years her audience members number over 28,400 at in person events and webinars. She has had 2,500 meetings with clinical providers and reviewed over 43,000 medical notes. She knows what questions need answers and developed this resource to answer those questions.
Copyright © 2024, CodingIntel A division of Medical Practice Consulting, LLC Privacy Policy
Soar to new heights of coding accuracy with CodingIntel's new courses
From April 15, 2024 the day I'm speaking at the AAPC meeting until April 21, 2024 my Dad's Birthday

Enroll Today at codingintel.com/courses/ Use code APRIL for savings

The Federal Register
The daily journal of the united states government, request access.
Due to aggressive automated scraping of FederalRegister.gov and eCFR.gov, programmatic access to these sites is limited to access to our extensive developer APIs.
If you are human user receiving this message, we can add your IP address to a set of IPs that can access FederalRegister.gov & eCFR.gov; complete the CAPTCHA (bot test) below and click "Request Access". This process will be necessary for each IP address you wish to access the site from, requests are valid for approximately one quarter (three months) after which the process may need to be repeated.
An official website of the United States government.
If you want to request a wider IP range, first request access for your current IP, and then use the "Site Feedback" button found in the lower left-hand side to make the request.
Split-Shared Visit Revisited Next Year
- By David M. Glaser, Esq.
- November 9, 2022

CMS will delay until next year a final decision on this contentious issue.
Every year, around this time, I feel a bit like Steve Martin in The Jerk, gleefully celebrating the arrival of the new phone books. That’s odd, sure, but excitement about the fee schedule may be even weirder.
The 2023 Medicare Physician Fee Schedule makes one important, albeit unsurprising, change to the split-shared visit policy. First, some context.
In a clinic, when a physician and a non-physician practitioner (NPP) work together to treat a patient, Medicare’s incident-to benefit allows the physician to bill for the NPP’s work. There is a regulation, 42 CFR 411.15(m), that prevents physicians from using the incident-to benefit for services in a hospital, however.
To permit physicians to bill when a physician and an NPP both see a hospital patient, Medicare created a shared-visit policy and placed it in the manuals. About a year and a half ago, the Centers for Medicare & Medicaid Services (CMS) withdrew those manuals after someone submitted a request under the “Good Guidance” regulation that allowed individuals to challenge agency policy when it was not supported by a regulation. (Unfortunately, that Good Guidance regulation has since been withdrawn, creating uncertainty about the ability to raise these issues going forward.)
Last year, in the fee schedule, CMS formally issued a regulation creating shared visits. Under the regulation, the physician must do the “substantive portion” of the visit to bill. In 2022, there were two options on how to complete the substantive portion. First, if the physician did all of any of the three key components of an evaluation and management (E&M) service (that is, all the history or the exam or the medical decision-making), the physician could bill. Alternatively, if the physician spent more than half of the time with the patient, the physician may bill. However, under the original regulation, as of Jan. 1, 2023, a physician’s option of using one of the three key components would have evaporated, and physicians would be allowed to bill only if they spent the majority of the time with the patient.
That policy drew considerable criticism.
As a result, the proposed fee schedule this year included a one-year delay in the requirement, and that proposal has now been finalized. Basically, CMS is saying that during 2023, the rule from 2022 will continue, and physicians can use either the majority of time or any one of the three key elements.
In the preamble discussion, CMS noted that many people object to the idea of using the majority of time as the mechanism to determine who can bill a shared visit. However, they didn’t totally withdraw the plan to require the use of time; they just delayed it until Jan. 1, 2024.
Fortunately, they do acknowledge that they will continue to receive comments on the topic. They also note that the American Medical Association/Current Procedural Terminology (AMA/CPT®) is evaluating how to define “the substantive portion of a visit,” and CMS is willing to consider adopting the CPT definition once it is finalized. But there is still reason to think that the very silly requirement that a physician spend the majority of the time with the patient to bill could take effect. The bottom line is that for the next year, a physician can bill for a shared visit if the physician performs all of the history, all of the exam, or all of the medical-decision making. After that, we will just have to see whether common sense prevails.
One reason I think the majority of time rule is foolish is that time is a bad measure of value. The other is summed up perfectly by the words of the late, great David Bowie, as he warned us about “changes.” “Time may change me. But you can’t trace time.” Here’s hoping that tracing time is never required for a shared visit.
Programming note: Listen to David Glaser’s live “Risky Business” report every Monday on Monitor Mondays , 10 Eastern.

- TAGS: Billing , CMS , Medicare , Physician

David M. Glaser, Esq.
Related stories.

Emerging Legal Defenses Against AI-Assisted Medicare Audits: Part I
As we know, artificial intelligence (AI) is in the spotlight these days. It is being adopted in almost every sector of the economy. It is

Remain Compliant – and Take the Money
Our first topic today is local coverage determinations (LCDs) and variation. I have written in the past about national and local coverage determinations, and I
Leave a Reply
Please log in to your account to comment on this article.
Featured Webcasts

Leveraging the CERT: A New Coding and Billing Risk Assessment Plan
Frank Cohen shows you how to leverage the Comprehensive Error Rate Testing Program (CERT) to create your own internal coding and billing risk assessment plan, including granular identification of risk areas and prioritizing audit tasks and functions resulting in decreased claim submission errors, reduced risk of audit-related damages, and a smoother, more efficient reimbursement process from Medicare.

2024 Observation Services Billing: How to Get It Right
Dr. Ronald Hirsch presents an essential “A to Z” review of Observation, including proper use for Medicare, Medicare Advantage, and commercial payers. He addresses the correct use of Observation in medical patients and surgical patients, and how to deal with the billing of unnecessary Observation services, professional fee billing, and more.

Top-10 Compliance Risk Areas for Hospitals & Physicians in 2024: Get Ahead of Federal Audit Targets
Explore the top-10 federal audit targets for 2024 in our webcast, “Top-10 Compliance Risk Areas for Hospitals & Physicians in 2024: Get Ahead of Federal Audit Targets,” featuring Certified Compliance Officer Michael G. Calahan, PA, MBA. Gain insights and best practices to proactively address risks, enhance compliance, and ensure financial well-being for your healthcare facility or practice. Join us for a comprehensive guide to successfully navigating the federal audit landscape.

Mastering Healthcare Refunds: Navigating Compliance with Confidence
Join healthcare attorney David Glaser, as he debunks refund myths, clarifies compliance essentials, and empowers healthcare professionals to safeguard facility finances. Uncover the secrets behind when to refund and why it matters. Don’t miss this crucial insight into strategic refund management.

2024 SDoH Update: Navigating Coding and Screening Assessment
Dive deep into the world of Social Determinants of Health (SDoH) coding with our comprehensive webcast. Explore the latest OPPS codes for 2024, understand SDoH assessments, and discover effective strategies for integrating coding seamlessly into healthcare practices. Gain invaluable insights and practical knowledge to navigate the complexities of SDoH coding confidently. Join us to unlock the potential of coding in promoting holistic patient care.

2024 ICD-10-CM/PCS Coding Clinic Update Webcast Series
HIM coding expert, Kay Piper, RHIA, CDIP, CCS, reviews the guidance and updates coders and CDIs on important information in each of the AHA’s 2024 ICD-10-CM/PCS Quarterly Coding Clinics in easy-to-access on-demand webcasts, available shortly after each official publication.

2024 ICD-10-CM/PCS Coding Clinic Update: Fourth Quarter
Kay Piper reviews the guidance and updates coders and CDISs on important information in the AHA’s fourth quarter 2024 ICD-10-CM/PCS Quarterly Coding Clinic in an easy to access on-demand webcast.

2024 ICD-10-CM/PCS Coding Clinic Update: Third Quarter
Kay Piper reviews the guidance and updates coders on information in the AHA’s third quarter 2024 ICD-10-CM/PCS Coding Clinic in an easy to access on-demand webcast.
Trending News

The Front Line of Climate Change: How Healthcare Coders Are Making a Difference

Feds Seeking to Save Medicare Money on High-Volume, High-Cost Procedures

Updating the Facility-Specific Coding Guidelines: Part 1

Why Even VPN Encryption Can Be Hacked – And How Huge Insurance Providers Can Still Have PHI Data Stolen
Stay connected.
Subscribe to receive free RAC news and updates.
5874 Blackshire Path, #13 Inver Grove Heights, MN 55076
Hours: 9am – 5pm CT Phone: (800) 252-1578 Email: [email protected]
Copyright © 2024 RACmonitor. Powered by MedLearn Media.
Happy National Doctor’s Day! Learn how to get a complimentary webcast on ‘Decoding Social Admissions’ as a token of our heartfelt appreciation! Click here to learn more →
Happy World Health Day! Our exclusive webcast, ‘2024 SDoH Update: Navigating Coding and Screening Assessment,’ is just $99 for a limited time! Use code WorldHealth24 at checkout.

IMAGES
VIDEO
COMMENTS
Billing Split (or Shared) Visits in 2022-2023. What didn't change for split (or shared) E/M visits is that they are still leveled using the 1995 or 1997 Documentation Guidelines for Evaluation and Management Services through the end of 2022. What did change for split (or shared) E/M visits is the selection of the billing provider.
Split (or Shared) E/M Visits. For CY 2023, we finalized a year-long delay of the split (or shared) visits policy we established in rulemaking for 2022. This policy determines which professional should bill for a shared visit by defining the "substantive portion," of the service as more than half of the total time. Therefore, for CY 2023, as ...
A: In 2023, practitioners who furnish split/shared evaluation and management services may bill based on a key component (history, physical exam, or MDM) or time.In 2024, practitioners will use total time to determine who furnished the substantive portion of the visit unless CMS changes the date or the guidance.
Application to prolonged services. Beginning January 1, 2023, the physician or practitioner who spent the substantive portion will bill for the primary E/M visit and the prolonged service code (s) when the service is furnished as a split or shared visit, if all other requirements to bill for split or shared services are met.
Beginning Jan. 1, 2023, the practitioner who spends more than half the total time will bill for the visit. Split/shared visits apply to prolonged services when determining the substantive portion of the visit based on time. (Note: Critical care services are always based on time.)
split or shared E/M visit in order to bill for the service. CMS will continue to allow physicians and qualified health care professionals to use history, physical exam, medical decision making (MDM), or more than half of the total time spent with a patient to determine the substantive portion of the split/shared visit in 2023.
For visits (other than critical care) furnished in calendar year 2022, "substantive portion" is defined as one of the three key components (history, exam, or medical decision-making), or more than half of the total time spent by the physician and nonphysician practitioner (NPP) performing the split/shared visit. For calendar year 2023 and ...
We revised our regulation at 42 CFR § 415.140 to define a split (or shared) visit as an E/M visit in a facility setting in which payment for services and supplies furnished incident to a physician or practitioner's professional services is not available under § 410.26(b)(1). Critical Care Services (CPT 99291 and 99292)
The visit requires a substantive portion to be performed by both the physician and APP. CMS is providing a 60-day public comment period on the 2023 Proposed Rule, which closes on September 6, 2022. This PYA insight will provide more clarity on how split and shared visits are addressed in the 2023 Proposed Rule. 2022 CMS Policy.
For CY 2023, we are proposing to delay the split (or shared) visits policy we finalized in CY 2022 for the definition of substantive portion, as more than half of the total time, for one year with a few exceptions. Therefore, for CY 2023, as in CY 2022, the substantive portion of a visit may be met by any of the following elements: History.
Split/Shared Visit Billing Medicare's split (or shared) billing policy will remain unchanged for 2023. To use this optional billing mechanism, a "substantive portion" of care must be performed by a physician which will continue to be defined (for non-time-based services) as one of the following: history, physical exam, or medical decision ...
For 2023, split/shared visits must be billed under the NPI of the individual who provides more than 50% of total visit time. These new rules could significantly impact Medicare reimbursement for physician practices that use NPPs in facility settings. For evaluation and management (E/M) visits jointly furnished by a physician and NPP in the same ...
For visits (other than critical care) furnished in calendar year 2022, substantive portion means one of the three key components (history, exam, or medical decision-making) or more than half of the total time spent by the physician and nonphysician practitioner (NPP) performing the split or shared visit. For calendar year 2023 and forward, the ...
When reporting a split/shared visit to CMS, modifier -FS must be appended to the appropriate code to indicate it's a split/shared visit. CPT modifier -52 describes a reduced service and should not be used to indicate a split/shared service. Documentation CMS Definition of Substantive Portion 2023 2024 Two options (select one): 1.
During the transitional period, from January 1-December 31, 2023, except for critical care visits, the substantive portion can be one of the three key E/M visit components (a medically appropriate history or exam, or medical decision-making [MDM]), or more than half of the total time spent by the physician and NPP performing the split or shared visit.
This member-exclusive split/shared visit and service reference details the 2022 and 2023 substantive portion definitions, as well as place of service and modifier usage, for E/M visits in outpatient facilities (excluding office visits in non-facility settings), hospital facilities, and skilled nursing facilities. Download the reference (PDF)
How CMS Final Rule Impacts Split/Shared Visits. In the CMS Final Rule, released in November 2021, the criteria for split/shared services changed dramatically. This caused confusion as the criteria are not completely clear and will change for 2023. Unfortunately, by the time we get the new rule down, we'll have to start over again.
In 2024, CPT expanded its definition of split/shared services, CMS updated their requirements. CPT expanded its definition of split/shared services in 2024, stating that the substantive portion can be determined by the practitioner who spent more than 50% of the time, or who made or approved the medical decision making.; CMS will allow the substantive portion to be determined based on the ...
for the Nursing Facility Visits code family to align with the Nursing Facility Visits policy published in the CY 2023 Final Rule (CMS-1770-F), titled: Revisions to Payment Policies under the Medicare Physician Fee ... changes to the current split (or shared) visit policy other than the definition of 'substantive portion'.
When CMS updated the split/shared billing rules for 2023, many practices were confused about who should report the services. Find out how to easily select the billing provider with these key tips. ... When a split/shared visit takes place, both the physician and the nonphysician provider (NPP) perform part of an E/M visit in the facility setting.
11/16/2023 view on this date view change introduced compare to most recent; 1/01/2023 ... portion means more than half of the total time spent by the physician and nonphysician practitioner performing the split (or shared) visit, or a substantive part of the medical decision making except as otherwise provided in this paragraph. For critical ...
The 2023 Medicare Physician Fee Schedule makes one important, albeit unsurprising, change to the split-shared visit policy. First, some context. In a clinic, when a physician and a non-physician practitioner (NPP) work together to treat a patient, Medicare's incident-to benefit allows the physician to bill for the NPP's work. There is a ...
In 2022, revisions were made to Chapter 12 Section 30.6.18 of the Medicare Claims Processing Manual to coding and documentation for split/shared visits. Definition of Split (or Shared) Visit - A split (or shared) visit is an evaluation and management (E/M) visit in the facility setting that is performed in part by both a physician and a ...