- Getting pregnant
- Life as a parent
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How long will it take to conceive?
- When to take a pregnancy test
- Best positions to conceive
- Top signs of pregnancy
- How to use ovulation kits
- How age affects fertility
- When can I get pregnant after c-section?
- What fertile cervical mucus looks like
- Late period but no pregnancy
- Faint line on pregnancy test
- See all in Getting Pregnant
- How big is my baby?
- Due Date Calculator
- Painful baby movements
- Symptoms you should never ignore
- Hospital bag packing checklist
- How your baby's developing
- Signs of labour
- How to tell baby position by kicks
- Baby movements: boy or girl?
- How to count pregnancy months & weeks
- Nuchal Translucency (NT) scan
- Baby Weight Chart
- See all in Pregnancy
- Baby Name Finder
- Modern Indian Baby Names
- Most Popular Names in India
- Baby Names inspired by the Quran
- Baby Names inspired by Lord Shiva
- Sanskrit Baby Names
- See all in Baby Names
- Your baby week by week
- Baby milestones by month
- Baby Rashes
- Baby skin colour
- Worms in babies and toddlers
- Sleep training methods
- Baby teething remedies
- How to do steaming for a baby
- See all in Baby
- Your toddler month by month
- How much water should toddlers drink?
- When your toddler gets frustrated
- Vegetarian meals for toddlers
- When your toddler won't eat
- Potty training
- Help your toddler sleep
- Bottle to cup
- Games & activities
- What to feed a sick toddler
- See all in Toddler
- गर्भवती होने के लिए संभोग
- प्रेगनेंसी टेस्ट में हल्की रेखा का मतलब
- गर्भावस्था के लक्षण
- गर्भावस्था में खून के धब्बे (ब्लीडिंग)
- गर्भावस्था में शिशु की हलचल
- प्रसव पीड़ा (लेबर पेन) के लक्षण
- शिशु के नक्षत्र पर आधारित नाम
- शिशु को कितनी मात्रा में फॉर्मूला दूध देना है?
- बच्चे के पेट में कीड़े: लक्षण व इलाज
- हिंदी अनुभाग देखें
- Postnatal symptoms to watch out for
- Pain and stitches after delivery
- Postnatal massage
- Postnatal diet
- Post-delivery confinement
- See all in Life as a parent
- Astrology names
- Goddess Lakshmi names
- Baby names by date of birth
- Conjunctivitis
- Combination baby names
- Goddess Durga names
- Sikh baby names
- Bengali baby names
- Eclipses and pregnancy
- Name numerology
- Lord Vishnu names
- What to feed baby with a fever
- Traditional Indian names
- Gestational age vs fetal age
- South Indian baby names
- Mythological baby names
- Pregnancy food chart
- Names that rhyme
- Goddess Saraswati names
- Are air conditioners safe for babies?
- Annaprashan rice ceremony
- Nature names
- Godh bharai: baby shower
- Sesame seeds in pregnancy

Travelling by bus when pregnant

How safe is bus travel during pregnancy?
What precautions should i take when traveling by bus, how can i make my bus journey more comfortable during pregnancy, what care should i take about my food and drink.
- You may have to spend long hours waiting for your bus to arrive at your stop. This may leave you exhausted and tired especially if the bus stop doesn't have proper seating arrangements and you have to stand while you wait .
- Most buses tend to be crowded, noisy and cramped. You may have to struggle to find a seat if you are traveling during the rush hour. Even if you have a bus pass, there's no guarantee you'll have a ready seat. This could make your commute tiresome and stressful .
- If you don't get a window seat or if your bus doesn't have air conditioning, the heat or lack of ventilation may tire you out. You may feel faint and dizzy or find your morning sickness is aggravated during the commute.
- In long journeys, you may not be able to get up and move around safely inside a bus, which could cause cramping in your legs or put you at greater risk for varicose veins .
- Lack of seat belts can put passengers at greater risk in the event of an accident.
- Never attempt to board or get off a moving bus.
- Try to find a seat in the middle of the bus. Staying in the middle may keep you safer in the unlikely event of a crash.
- It's best not to stand in a moving bus. Besides losing balance and falling down, there is the risk of being accidentally pushed by another passenger. Most buses have a separate section for women travelers. If you still can't find a seat, don't be shy to ask someone else for their seat. Or ask the bus conductor to help you out.
- Most buses don't have seat belts or air bags so, if you can, be cautious at all times. Try to stay focused to brace yourself when there is bad pot-holed road or speed breaker.
- Non air-conditioned buses can expose you to dust and fumes. In an air-conditioned bus you'll be spared from this pollution, although it may a little more expensive.
- Keep your emergency contact information on you at all times.
- Pack light, especially if you're traveling alone. You may strain your back carrying any heavy luggage.
- Carry a hand sanitiser and wet wipes to lower your chances of catching an infection .
- Some buses for long journeys may have on board toilets . Hold on to something for balance as you may find it difficult to manoeuvre in a loo while the bus is bumping down the road!
- Buses are, unfortunately, frequented by pickpockets and unruly elements. It's best to protect your belongings and stay vigilant at all times. Wear as little jewellery as possible and keep any valuable items like your wallet and mobile phone close at hand.
- For your daily commute to work , see if you can join a car pool.
- Treat yourself to cab rides or ask your husband or a relative to drive you.
- If possible, speak to your employer about changing your work timings. You could arrive a bit early and leave early so that you avoid peak hours and crowded buses. You could also apply for a transfer to a branch of the office closer to home to minimise your commute, if possible.
- Try metro or local train services , if they are available in your area. They may be crowded as well but you'll be spared from a bumpy ride!
- You may want to postpone any longer journeys, at least till you're done with the nausea and are in your second trimester . Or consider going by plane or train , if you really need to travel out of town.
- Opt for buses that do not have too many stoppages. You might also want to take another look at all the available bus routes, and then opt for the most suitable one.
- Avoid traveling in peak hours.
- Many cities have buses just for women travelers also known as "ladies specials". These tend to be less crowded and usually don't cost extra. Check your local newspaper or online for a schedule that works for you.
- Carry a small hand-fan as well. This can come handy at times when it gets really hot and humid inside the bus.
- Since seating typically is first-come, first-served, try to line up at the bus station early. That way you can get an aisle seat so you won't have to crawl over a seatmate if you need to get up.
- Buses are often too hot or too cold, so dress in layers and bring a small travel blanket just in case.
- Take advantage of scheduled pit stops to use the restrooms in bus stations or petrol pumps. If you are comfortable squatting, you may want to opt for Indian style toilets .
- If the seat next to you is empty, go ahead and stretch out a bit. Put your feet up, or even lie down and rest while you have the chance.
- Book your ticket for a non-smoking bus. Passive smoking is harmful for you and your baby.
- Try and book a sleeper coach so that you aren’t sitting all the time.
- Ask your doctor to refer you to a doctor in the place you are visiting in case of emergency.
- A toothbrush (brush and rinse with bottled water)
- toilet paper and pre-moistened paper towels or wet wipes
- a small hand towel
- bags for motion sickness
- a book light or flashlight for reading (along with a paperback book or two)
- an inflatable pillow for your neck or back
- sunglasses or eye shades for sleeping
- something to the pass the time such as a book, magazines or music player with headphones.
- any prescribed medicines you are taking
- stuffed parantha s
- sandwiches made with multigrain bread
- biscuits, namkeens and nuts are great snacks
- fresh fruits such as apples ( seb ), bananas ( kela ), oranges ( santara ), sweet limes ( musambi ).
- Is it safe to travel by a two-wheeler/scooter during the first trimester?
- What activities should I avoid during pregnancy?
- Pregnancy travel: where to go and how to decide.
Was this article helpful?
Airline rules and travel insurance in pregnancy

Pregnancy travel: where to go and how to decide

How to handle work related trips during pregnancy

How can I spot and avoid dehydration in pregnancy?

Where to go next


- Vishal's account
- Prenatal Care
Travelling By Bus During Pregnancy

Is It Safe to Travel By Bus During Pregnancy?
Risks associated with travelling by bus during pregnancy, precautions to take for bus journey during pregnancy, some tips to make your bus journey more comfortable, tips on food and drinks consumption while travelling by bus during pregnancy, some alternatives that you can consider.
Navigating travel during pregnancy requires thoughtful consideration, encompassing various factors to ensure both the mother’s and baby’s well-being. Among the multiple decisions expectant mothers face, the choice of transportation looms large, particularly when contemplating bus travel. In this article, we will tell you the pros and cons of travelling via bus during pregnancy. We will also give you some essential tips that you can follow while taking a bus journey during pregnancy so that you have a safe and comfortable road journey. By meticulously analyzing potential risks, such as the possibility of sudden movements or overcrowded conditions, this discourse endeavors to empower expectant mothers with the knowledge needed to make informed decisions regarding their mode of transportation, thereby prioritizing their health and that of their unborn child throughout the voyage.
Travelling by bus (or road travel of any kind) during pregnancy is mostly safe provided you are careful and follow certain rules. If the roads of your city are bumpy and there’s unbearable traffic, and the bus you take is usually crowded, then your bus travel can be physically taxing for you. In such cases, you should avoid travelling by bus. Furthermore, you should be extra careful in your first and third trimesters as these are the crucial months of pregnancy. In case you’re planning to travel by bus during pregnancy, you must check with your doctor first and plan accordingly (1) .
There are a few risks involved with travelling by bus during pregnancy which you should be aware of.
- Sitting for long hours in the bus can cause swelling in your feet. You may find it difficult to relax or sleep while sitting in an upright position.
- Sitting for long hours in the bus may put you at the risk of having blood clots.
- As there are no seat belts on the bus, you may experience jolts and jerks constantly, which may not be good for your baby’s health. Lack of seat belts can increase the risk of accidents too.
- Bus travels can be utterly exhausting and discomforting in pregnancy. The entire process of waiting for the bus, sitting on the bus and the long travel hours can put you at great discomfort and uneasiness.
If you have to travel on a bus in your pregnancy, then it is important that you take the following precautions:
1. Do Not Stand in a Moving Bus
It’s best that you don’t stand on a moving bus. Other than the risk of falling down and losing balance, there’s also a risk of being pushed by another passenger. If you don’t find a seat, ask someone else for their seat, but avoid standing.
2. Be Open About Your Pregnancy
The best thing you can do is inform the people around you and the bus conductor that you’re pregnant, especially in your first trimester (as your bump won’t be visible during this time). By informing the bus conductor, you will get help as and when required and even the driver will be more careful on the road.
3. Choose a Comfortable Seat
Try to find a seat in the middle (or front) of the bus while commuting to work and opt for a front seat in case of a long journey. Take the aisle seat for more leg space and for moving around easily when the bus stops.
4. Travel With a Family Member or a Friend
If it’s a long journey, it’s best that you travel with a family member or a friend. You may require assistance with different things, so it’s best that you have a person whom you can trust. In case, you’ve to travel alone, pack light and keep your emergency contact on you at all times. Also, keep your doctor’s number on speed dial.
5. Pack Your Food and Water
If it’s going to be a long journey by bus, then might we suggest that you refrain from eating outside food. Make safe choices while pregnant – carry home-cooked food and a water bottle with you. Eat healthy – avoid fried or spicy foods while travelling as it may cause nausea or heartburn .
6. Move Around Whenever Possible
If you’re going out of town by bus, there will be halts, of course. Make sure you get out of the bus at a halt and move around. Use the washroom and move around for a while to relieve any kind of muscle stiffness and to stretch your arms and legs.

Mentioned below are some useful tips that will make your bus journey comfortable during pregnancy (2) :
- No matter how important it is for you to board a bus but never ever try to board a moving bus. This can be extremely dangerous and may result in severe consequences.
- Keep yourself alert and cautious at all times because there are usually no seatbelts on buses and the bus ride can get rough on bumpy roads.
- Make sure you are seated somewhere in the middle section of the bus as this would keep you safer in case of any kind of crash.
- Travelling by a non-air-conditioned bus may expose you to dust and fumes. So if it’s feasible for you, travel in an air-conditioned bus.
- Make sure you keep all your emergency contacts on you at all times.
- Make sure you travel light in case you are travelling solo. Lifting heavy luggage can be very dangerous in pregnancy.
- Do not carry any valuable items with you and if you must then remain vigilant and take care of your belongings. Do not wear expensive jewellery that may attract any pickpockets.
- Carry wet wipes or hand sanitizers with you to lower your chances of contracting any infections.
- Sometimes longer route buses may have the facility of onboard toilets. In case you feel the urge or need to use the onboard toilet make deliberate efforts to keep up with your balance while using it.
Keep yourself well hydrated while travelling as dehydration may cause complications in pregnancy . There is a likelihood that you may not feel like eating or drinking at all while travelling, but don’t skip your meals or snacks. Avoid eating anything with more oil or fat content, and stick to light and easily digestible food items. Find out what you should eat and drink while travelling by bus.
- Carry home-cooked food and filtered drinking water with you. You can pack a vegetable sandwich, stuffed parantha, curd rice, etc. You can also pack some homemade lemonade or ginger ale.
- Pack fresh fruits such as apple , bananas and oranges with you. Fresh fruits shall provide you with energy and also offer various nutrients that are needed during pregnancy. In case you have missed packing fruits for your travel, you can buy them too but make sure you wash them thoroughly before consuming. Also, do not consume already cut fruits or vegetables.
- Carrying some roasted dry fruits is a good option to control hunger pangs. However, avoid eating them in large amounts as they may increase the body heat.
- You may also carry packed biscuits or roasted namkeen . Though you should not consume them too much as eating more of sugary and fried food items may make you feel sick or nauseous.
- If you have to buy something to eat, then it is recommended that you buy packed food items only. Packed food items are generally safer than unpacked ones and may pose less risk to you and your baby. Make sure you check for the manufacturing and expiry date on the label.
- You can have coconut water or packed fruit juices too.
- Always wash your hands or sanitize your before consuming any food items to avoid catching any infections .
- If you do not consume home-cooked food within three to four hours of its packing, then it is recommended that you do not consume it as it may no longer be fit for consumption, especially during summers.
Here are some alternative options that you may consider if you don’t want to travel by bus:
- For your daily commute to work, check if you can carpool with your friends. This option is not only viable but also very economical.
- You may ask your husband, friends or relatives to drive you to work.
- If you have a facility of metro trains in your city, then opt for them. Metro trains are not only fast but can save you from bumpy bus rides.
- You can also make use of online cab services.
- If possible postpone all your long-distance travel until you reach the second trimester of your pregnancy . If you cannot postpone your travel, consider travelling by train or by air .
1. Can travelling by bus lead to a miscarriage?
While the risk of miscarriage due to travelling in sleeper bus during pregnancy alone is low, it’s essential to consider factors like sudden movements and potential stress. Pregnant individuals should consult their healthcare provider for personalized advice and take necessary precautions, such as wearing seat belts and choosing seats with minimal jostling. Also, try to avoid bus travel during pregnancy first trimester .
2. Are there any concerns about motion sickness during pregnancy while travelling by bus?
Motion sickness can affect pregnant individuals, particularly during bus travel due to the vehicle’s movement. To mitigate this, it’s advisable to sit in the front or over the bus’s wheels, stay hydrated, and snack on light, non-greasy foods. Additionally, consulting a healthcare provider about safe anti-nausea remedies for pregnancy can be beneficial.
Travelling during the first trimester by bus should be avoided. However, if the situation demands travelling by bus while pregnant, you can follow the tips mentioned above and have a safe road journey during pregnancy!
References/Resources:
1. Pregnancy and travel; Better Health Channel (Victoria State Government); https://www.betterhealth.vic.gov.au/health/healthyliving/pregnancy-and-travel
2. Travel During Pregnancy; American Pregnancy Association; https://americanpregnancy.org/healthy-pregnancy/is-it-safe/travel-during-pregnancy/
3. Travelling in pregnancy; NHS; https://www.nhs.uk/pregnancy/keeping-well/travelling/
4. FAQs: Travel During Pregnancy; The American College of Obstetricians and Gynecologists; https://www.acog.org/womens-health/faqs/travel-during-pregnancy
5. Traveling While Pregnant or Breastfeeding; Johns Hopkins Medicine; https://www.hopkinsmedicine.org/health/conditions-and-diseases/traveling-while-pregnant-or-breastfeeding
6. Pregnant Travelers; Centers for Disease Control and Prevention; https://wwwnc.cdc.gov/travel/page/pregnant-travelers
7. What To Know About Travel During Pregnancy; Cleveland Clinic; https://health.clevelandclinic.org/traveling-while-pregnant
Also Read:
Boating while Pregnant Travelling by Car During Pregnancy Riding a Two Wheeler in Pregnancy
- RELATED ARTICLES
- MORE FROM AUTHOR

How to Effectively Take Charge of Your Pregnancy Stretch Marks
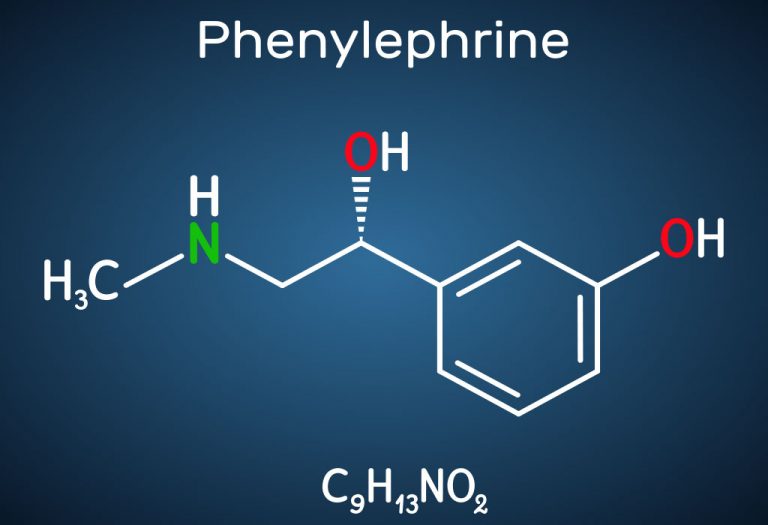
Should You Take Phenylephrine While Pregnant?

Head Lice During Pregnancy - Treatment & Preventive Measures

Kidney Infection (Pyelonephritis) in Pregnancy

Doing Sit-Ups or Abdominal Crunches during Pregnancy - Is It Safe?
Low Lymphocytes during Pregnancy
Popular on parenting.

245 Rare Boy & Girl Names with Meanings

Top 22 Short Moral Stories For Kids

170 Boy & Girl Names That Mean 'Gift from God'

800+ Unique & Cute Nicknames for Boys & Girls
Latest posts.
Cookie Monster Coloring Pages - Free Printable Pages For Kids
Robot Coloring Pages - Free Printable Pages For Kids

Cheerleading Coloring Pages - Free Printable Pages For Kids

Essay On Holi - 10 lines, Short and Long Essay for Students and Children
- How To Get Pregnant
- Infertility
- Pregnancy Week by Week
- Second Pregnancy
- Giving Birth
- Post Pregnancy
- Breastfeeding
- Development
- Browse Names
- Play & Activities
- Coloring Pages
- Food & Nutrition
- Health & Fitness
- Style & Beauty Care
- Collaborations
- New Parents
- Single Parenting
- Relationships
- Baby Eye Color Calculator
- Online Pregnancy Test
- Chinese Gender Predictor
- Implantation Calculator
- hCG Calculator
- Period Calculator
- ovulation calculator
- pregnancy due date calculator
- Child Height Predictor
- Pregnancy Weight Gain Calculator
- Breast Milk Calculator
- Child Growth Percentile Calculator
- Baby Cost Calculator
- BMI Calculator For Kids & Teens
- Contraction Calculator
- Immunization Scheduler and Chart
- C-Section Checklist
- Online Twin Pregnancy Quiz
- Numerology calculator
- Child Blood Type Calculator
- Nakshatra Calculator
- Diaper Bag Checklist
- Baby Name Combiner
Home • Pregnancy • Safety
Is It Safe To Travel By Bus During Pregnancy?
Traveling in mid-pregnancy may be safe but talk to your doctor if you have complications.
Dr Anita Gupta is currently working in University College of Medical Sciences (Medical School) & Guru Teg Bahadur Hospital, Delhi. She has been practicing as a gynecologist & obstetrician for the past 31 years and as a lactation con... more
Harshita is a graduate in commerce and holds a PG Diploma in Patent and Copyrights Law from NALSAR University. She has also pursued CA and has more than three years of internship experience in auditin... more
Rebecca is a pregnancy writer and editor with a passion for delivering research-based and engaging content in areas of fertility, pregnancy, birth, and post-pregnancy. She did her graduation in Biotec... more
Aneesha holds a Bachelor's degree in Biotechnology from USTM, Meghalaya and Master’s degree in Applied Microbiology from VIT, Vellore. With two years of experience, she has worked on different researc... more
MomJunction believes in providing reliable, research-backed information to you. As per our strong editorial policy requirements, we base our health articles on references (citations) taken from authority sites, international journals, and research studies. However, if you find any incongruencies, feel free to write to us .
Image: MomJunction Design Team
Traveling is an unavoidable aspect of our lives these days, whether for business, a doctor’s appointment, or a vacation. However, new mothers may be apprehensive about traveling long distances by public transportation. This post helps you prepare for such situations.
Read this post to learn whether it is safe to travel by bus during pregnancy, the risks associated with it, and some tips for safe bus travel during this time.
Is It Safe To Travel By Bus During Pregnancy? What Are The Risks Associated With It?
The best time to travel is mid-pregnancy (14 to 28 weeks). But travel may not be recommended for women who have pregnancy complications. If you are planning a trip, talk to your obstetrician-gynecologist (Ob-Gyn) to better understand travel restrictions if any. Get your check-up done before you leave for long-distance travel on a bus.
There are also a few risks involved with bus travel during pregnancy. Bus journeys are uncomfortable for some expectant moms.
1. If you are traveling a long distance or get stuck in a traffic jam, you cannot get up and move around often; this can put you at risk for blood clots ( 1 ) and varicose veins.
Image: Shutterstock
2. In case you are traveling on a vacation by bus, sleeping while sitting upright can be really uncomfortable. In fact, it can also lead to swelling in your legs.
3. The biggest worry in bus travel during pregnancy is the need to use the washroom, especially if you are traveling in an air conditioned bus.
4. During travel one gets thirsty more often, so you are likely to be drinking more water which can leave you wanting to run to the bathroom at the earliest.
5. Lack of a seat belt can also put you and your belly at risk of getting hurt, in case of sudden and hard braking or deep potholes on the road.
Tips For Safe Bus Travel During Pregnancy
Though traveling by bus during pregnancy has a few minor shortcomings, there are ways you can make your journey comfortable and relaxed.
1. Be Transparent: Traveling particularly during office hours can be quite a pain with buses being crowded and every one seeming to be in a hurry.
- Always inform the bus conductor or your co-passengers that you are pregnant so that you can save yourself from being pushed around.
- Also, if you are traveling a long journey out of the station, check the bus schedule in advance and plan accordingly. Informing the bus service about your pregnancy can help them facilitate a good seat with optimum air conditioning and extra support to make your journey less tiring and risky.
2. Keep ‘Em Handy: Pack your food, water, and medications in a handy manner when planning a long journey by bus. Carrying essential items handy can help ensure proper nutrition and hydration, vital for proper prenatal care ( 2 ). Avoid carrying oily items like chips that could aggravate nausea and stick to a lot of citrus fruits and drinks.
- Eat cautiously and at regular intervals as you will already feel full due to lack of activity. Also, stick to bottled water and avoid drinking water from unknown sources.
- Keep bags handy for motion sickness as buses will generally not stop at random locations. Wear supportive clothing and avoid heavy lifting while handling luggage.
3. Seating Choices: If you can request and get a comfortable seating option, it is ideal to take an aisle seat so that you can move out of your seat without crawling over with too much effort.
- Keep neck and back pillow handy particularly in case of overnight bus travels to avoid straining your body.
- Avoid front and back rows as they are riskier in case of a crash. If you get a chance and find two seats vacant do sit with your legs up to stretch your body.
4. Use The Stopovers: Every time the bus stops for breaks, take the opportunity to use the restroom facility. Also, consider walking or stretching a little to promote blood circulation and prevent the formation of blood clots ( 2 ).
- Sitting for too long can make your body stiff and stretching at breaks can help you relieve the stiffness.
- Do not go alone to restrooms or to stretch your legs. Seek the help of a fellow passenger, or go in a group.
5. Travel With A Companion: An important tip that goes without saying is to try and travel a long distance with someone and avoid traveling alone.
Image: IStock
- Keep your partner’s and doctor’s number on speed dial as emergency contacts so that you can contact them immediately in case of any emergency. Travel insurance is another important consideration while traveling during pregnancy.
- If you do decide to travel alone by bus, don’t get tense; take all necessary precautions and listen to some light soothing music to stay calm and relaxed.
Any travel plans must be undertaken with extra caution during pregnancy, especially during the first and third trimesters . During pregnancy, long-distance travel by bus can be uncomfortable and increases the risk of swelling in the legs, blood clots, and varicose veins. Since buses lack seat belts, sudden brakes can also put your bump at risk. However, if bus travel is unavoidable, opt for an aisle seat to move about more easily. Also, pick a seat in the middle rows since it may be less jerky. In addition, we recommend checking with your doctor before you travel.
Frequently Asked Questions
1. Can travel by bus lead to a miscarriage?
Pregnancy termination might depend on many factors and not just by traveling. Therefore, traveling by bus might not lead to a miscarriage. However, since there is an increased risk of miscarriages during the first trimester, your doctor might advise you to avoid traveling during that time ( 3 ).
2. Which mode of travel is safe during pregnancy?
The safety and comfort of travel during pregnancy might depend on your pregnancy and any complications. Generally, air travel is considered safe before 36 weeks of pregnancy, whereas car travel is considered safe throughout pregnancy ( 4 ). However, if you want to make travel plans, consulting with your doctor to know about the safest modes of transportation for you is advisable.
3. Is a long journey safe during pregnancy?
A long journey might not be advisable during pregnancy as it might cause exhaustion. However, consult your doctor to know the safe ways to travel if a long journey is unavoidable. Your doctor will advise you to take frequent rest stops throughout the journey and stretch your legs when you feel tired. Wearing compression stocking is a good option to improve blood circulation in the legs and reduce the risk of blood clots.
Infographic: Traveling By Bus During Pregnancy
Illustration: Momjunction Design Team
Get the high-quality PDF version of this infographic.
Key Pointers
- Inform the bus conductor and other passengers that you are pregnant to avoid being pushed.
- Bring a water bottle and snacks with you and avoid eating oily foods that can cause nausea.
- Consider bringing a friend or your partner with you for support during travel.
- Keep your doctor’s phone number handy in case of an emergency.
- When traveling overnight by bus, keep neck pillows nearby and avoid sitting in the front or back rows.
Image: Stable Diffusion/MomJunction Design Team
Embarking on a journey while expecting may seem overwhelming, but fear not! Stanford Children’s Health offers invaluable advice in this video to enhance your comfort and safety during pregnancy travels.
- Pregnancy and travel. https://www.betterhealth.vic.gov.au/health/healthyliving/pregnancy-and-travel
- Travel during pregnancy. https://americanpregnancy.org/healthy-pregnancy/is-it-safe/travel-during-pregnancy/
- Travelling in pregnancy. https://www.nhs.uk/pregnancy/keeping-well/travelling/#
- Travel during pregnancy. https://www.acog.org/womens-health/faqs/travel-during-pregnancy
- Public transport in pregnancy. https://www.tommys.org/pregnancy-information/blogs-and-stories/im-pregnant/pregnancy-news-and-blogs/public-transport-pregnancy
- Fact-checker
Dr. Anita Gupta MS
Harshita makvana b.com, pg dip, rebecca malachi bsc, aneesha amonz msc, latest articles, fungal infection in babies: risks, treatment and remedies.
Ringworm, thrush, and diaper rash are some common fungal infections in infants.
8 Home Remedies To Deal With Itchy Belly During Pregnancy
Moisturizers may relieve mild itching; severe cases may require prescription ointments.
Air Conditioner (AC) For Babies: Is It Safe, Tips And Alternatives
AC is safe for babies when used in moderation by maintaining optimal temperatures.
How To Clean Baby Toys: A Step-by-Step Guide
Say goodbye to grime and hello to playtime!
Can You Take Tramadol While Pregnant?
The drug is best avoided unless prescribed since evidence of its safety is limited.
Spider Bites In Toddlers: Facts, Symptoms & Ways To Prevent
Though these bites are painful, painkillers and antibiotics can help manage them.
Shingles In Babies: Symptoms, Causes, Diagnosis & Treatment
These itchy, pimple-like rashes make them fussy and are caused by the chickenpox virus.
15 Most Common Infant And Newborn Problems
Some common health issues they face are jaundice, cough, vomiting, and fever.
9 Months Pregnant: Symptoms, Baby Development And Diet Tips
Prepare yourself for delivery and to hold your bundle of joy soon.
What Is Viable/ Non-viable Pregnancy?
An early viability scan at around six to ten weeks helps determine the prognosis of pregnancy.
Aspirin During Pregnancy: When To Take And When Not To
Aspirin-containing OTC medications may not be safe during pregnancy, especially in the third trimester.
6 Functions Of Placenta During Pregnancy And Placental Problems
The placenta is responsible for providing the vital oxygen and nutrients the growing fetus needs.

- Pregnancy Classes

Travel During Pregnancy
As long as there are no identified complications or concerns with your pregnancy, it is generally safe to travel during your pregnancy. The ideal time to travel during pregnancy is the second trimester . In most cases, you are past the morning sickness of the first trimester and several weeks from the third stage of pregnancy when you are more easily fatigued .
Is it safe to travel during pregnancy?
Traveling by air is considered safe for women while they are pregnant; however, the following ideas might make your trip safer and more comfortable.
- Most airlines allow pregnant women to travel through their eighth month. Traveling during the ninth month is usually allowed if there is permission from your health care provider.
- Most airlines have narrow aisles and smaller bathrooms, which makes it more challenging to walk and more uncomfortable when using the restroom. Because of potential turbulence that could shake the plane, make sure you are holding on to the seatbacks while navigating the aisle.
- You may want to choose an aisle seat which will allow you to get up more easily to reach the restroom or just to stretch your legs and back.
- Travel on major airlines with pressurized cabins and avoid smaller private planes. If you must ride in smaller planes, avoid altitudes above 7,000 feet.
- Although doubtful, the risk of DVT can be further reduced by wearing compression stockings.
The Royal College of Obstetricians and Gynaecologists and the International Air Travel Association recommend that expecting mothers in an uncomplicated pregnancy avoid travel from the 37th week of pregnancy through birth. Avoiding travel from 32 weeks through birth is recommended for women who have complicated pregnancies with risk factors for premature labor, such as mothers carrying multiples.
Risk factors that warrant travel considerations include the following:
- Severe anemia
- Cardiac disease
- Respiratory disease
- Recent hemorrhage
- Current or recent bone fractures
Traveling by Sea During Pregnancy
Traveling by sea is generally safe for women while they are pregnant; the motion of the boat may accentuate any morning sickness or make you feel nauseous all over again. There are a few considerations to make your trip safer and more comfortable:
- Check with the cruise line to ensure that there is a health care provider on board in case there are any pregnancy complications .
- Review the route and port-of-calls to identify if there is access to any medical facilities if needed.
- Make sure any medications for seasickness are approved for women who are pregnant and that there is no risk to the developing baby.
- Seasickness bands use acupressure points to help prevent upset stomach and maybe a good alternative to medication.
International Travel During Pregnancy
Traveling overseas has the same considerations that local or domestic travel has, but it also has additional concerns that you need to know about before making an international trip. The information below is provided to help you assess whether an international trip is good for you at this time:
- It is important to talk with your health care provider before you take a trip internationally to discuss safety factors for you and your baby.
- Discuss immunizations with your health care provider and carry a copy of your health records with you.
- With international travel, you may be exposed to a disease that is rare here in the United States but is common in the country you visit.
- Contact the Centers for Disease Control and Prevention at (800) 311-3435 or visit their website at www.cdc.gov to receive safety information along with immunization facts related to your travels.
- Diarrhea is a common concern when traveling overseas because you may not be used to the germs and organisms found in the food and water of other countries. This can lead to a problem of dehydration .
Here are some tips to avoid diarrhea and help keep you safe:
- Drink plenty of bottled water
- Used canned juices or soft drinks as alternatives
- Make sure the milk is pasteurized
- Avoid fresh fruits and vegetables unless they have been cooked or can be peeled (such as an orange or a banana)
- Make certain that all meat and fish has been cooked completely; if you are unsure, do not eat it
Travel Tips During Pregnancy
Whether you are going by car, bus, or train, it is generally safe to travel while you are pregnant; however, there are some things to consider that could make your trip safer and more comfortable.
- It is essential to buckle-up every time you ride in a car. Make sure that you use both the lap and shoulder belts for the best protection of you and your baby.
- Keep the airbags turned on. The safety benefits of the airbag outweigh any potential risk to you and your baby.
- Buses tend to have narrow aisles and small restrooms. This mode of transportation can be more challenging. The safest thing is to remain seated while the bus is moving. If you must use the restroom, make sure to hold on to the rail or seats to keep your balance.
- Trains usually have more room to navigate and walk. The restrooms are usually small. It is essential to hold on to rails or seat backs while the train is moving.
- Try to limit the amount of time you are cooped up in the car, bus, or train. Keep travel time around five to six hours.
- Use rest stops to take short walks and to do stretches to keep the blood circulating.
- Dress comfortably in loose cotton clothing and wear comfortable shoes.
- Take your favorite pillow.
- Plan for plenty of rest stops, restroom breaks and stretches.
- Carry snack foods with you.
- If you are traveling any distance, make sure to carry a copy of your prenatal records.
- Enjoy the trip.
Want to Know More?
- How to Treat Jet Lag Naturally During Pregnancy
Compiled using information from the following sources:
1. Planning Your Pregnancy and Birth Third Ed. The American College of Obstetricians and Gynecologists, Ch. 5. William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 8.
2. Royal College of Obstetricians and Gynaecologists, Air Travel and Pregnancy (Scientific Impact Paper No. 1), https://www.rcog.org/uk, May 22, 2013.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Preconception Wellness - Prepare for the Unexpected

Leg Cramps During Pregnancy

Prenatal Vitamin Limits
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
Is traveling while pregnant safe?
When to avoid pregnancy travel, when is the best time to travel while you're pregnant , can pregnant women travel during covid, when should you stop traveling while pregnant, your pregnancy travel checklist, when to call your doctor while traveling.
Yes, it's generally safe to travel during pregnancy as long as you're not too close to your due date and you're not experiencing any serious pregnancy complications. There are special precautions to take, of course, and you may find yourself stopping to use the bathroom more than you're used to, but that babymoon can be within reach.
Before you pack your suitcase, talk with your healthcare provider to make sure it’s safe for you to travel and that your destination is a good choice. You'll want to avoid places where infectious diseases are prevalent (or there are high outbreaks of Zika or malaria, for example). The COVID-19 pandemic has made people reconsider where they feel safe traveling as well; if you're fully vaccinated, the CDC says you can travel Opens a new window , but it's always best to check with your doctor first.
And bear in mind that the activities you take part in might be different than normal – you'll want to skip the Scuba diving lessons, for example (though snorkeling is okay!).
It's safe to fly when you're pregnant as well, and most airlines will allow you to fly domestically until about 36 weeks of pregnancy. International routes may have different rules, so be sure to check with your airline before booking anything. Your doctor will tell you to avoid flying, however, if you have a health concern that might require emergency care or any other health conditions that aren’t well controlled.
It's best to avoid traveling while pregnant if you have any health conditions that can be life-threatening to both you or your baby. If you have any of the following conditions, your doctor will almost certainly advise you against travel:
- Placental abruption
- Preeclampsia
- You're in preterm or active labor
- Cervical insufficiency (incompetent cervix)
- Premature rupture of membranes (PROM)
- A suspected ectopic pregnancy
- Vaginal bleeding
You might also need to be extra-cautious or skip travel if you're experiencing intrauterine growth restriction , you have placenta previa , or you have other conditions that may place your pregnancy at a higher risk. It’s always a good idea to discuss your concerns with your healthcare provider before travel regarding any medical conditions you have, and they'll be able to advise you on what's best, depending on the trip.
The sweet spot for pregnancy travel is during your second trimester , between 14 weeks and 27 weeks. By the second trimester, any struggles you’ve had with morning sickness and fatigue during the earlier weeks of pregnancy should have hopefully subsided – and after 12 weeks, your risk of miscarriage decreases significantly as well. And you're not too far along to worry about third trimester exhaustion or going into preterm labor yet, either.
Your energy levels are likely to be good during your second trimester too (bring on the sightseeing!), and it will still be relatively easy and comfortable for you to travel and move around at this time. Keep in mind that once you hit that third trimester, pregnancy travel might be more difficult as you find it harder to move around and stay still for long periods of time.
It's complicated (and often a personal decision based on your own risk factors), but the CDC says that if you're fully vaccinated against COVID-19, you can travel. Of course, it's important you still do everything you can to keep yourself and others around you safe, including following all mask-wearing and social distancing guidelines in the destination you visit.
Women are at an increased risk for severe illness if they contract COVID-19 while pregnant , and they're more likely to experience preterm birth and other poor pregnancy outcomes. (This is why the CDC, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine all recommend that women who are pregnant, breastfeeding, or are planning on becoming pregnant get the COVID vaccine .)
If you're vaccinated and decide to travel, the CDC advises avoiding international destinations that are designated Level 4, due to high rates of local COVID-19 transmission.
Take all this information into account and talk to your doctor before you decide on where and when to travel while you're pregnant. And if you experience any symptoms of COVID-19, whether while traveling or at home, call your healthcare provider as soon as possible.
The guidelines for when to stop traveling while you're pregnant vary based on your mode of travel, but more or less, you should wrap up travel before you're 36 weeks pregnant.
Most airlines will let pregnant women fly domestically until they're 36 weeks pregnant – and many cut that off earlier for international travel. This rule is often enforced on an honor system policy, but some airlines may ask for a doctor’s note – so make sure you have that from your healthcare provider if you're traveling in the third trimester, just in case.
Most cruise ships don't allow travel after 24 weeks of pregnancy. Some cruise lines' cutoff dates vary, so verify policies before booking a cruise.
As for road trips, there's no official deadline for when you need to stop traveling, but your personal comfort level (physically and emotionally) – and your doctor's advice – might help you decide. You can drive while pregnant all the way up until your due date, but things may get considerably less comfortable on longer trips as you approach full term.
Travel of any kind requires advance preparation, but when you're pregnant and traveling, that pre-trip checklist gets a little longer. Give yourself a little more time than usual to plan for a trip – and use the tips below to stay safe and comfortable on your next adventure.
Before you travel
- Talk to your healthcare provider to determine if your trip is safe for you and if there are any medical concerns to consider. It's a good idea to discuss any activities you plan to do while you're away too. If you're planning an international trip, make sure to ask about any vaccines you may need for the areas you're visiting.
- Make sure you know your prenatal test schedule. Plan travels around any prenatal tests you need to schedule, including ultrasounds and other important screening tests.
- Book an aisle seat. You'll likely be more comfortable being able to get up to stretch or go to the bathroom on longer flights.
- Buy travel insurance. You don't need special travel insurance when you're pregnant, but it's never a bad idea to secure a policy. You may want to consider one with a “cancel for any reason” clause that reimburses you for money lost on cancelled trips for reasons (read: any reason) beyond what’s listed on the base policy. Check with your personal health insurance, too, to make sure it covers potential pregnancy complications while traveling internationally (some don’t). Consider adding evacuation insurance as part of a travel insurance plan, too.
- Gather your medical records and health information . If you’re in your second or third trimester, ask your ob-gyn or midwife for a digital copy of your prenatal chart, and have that easily accessible during your trip. Typically, this chart includes your age, your blood type, the name and contact information for your healthcare provider, the date of your last menstrual period, your due date, information about any prior pregnancies, your risk factors for disease, results of pregnancy-related lab tests (including ultrasounds or other imaging tests), your medical and surgical history, and a record of vital signs taken at each visit.
- Keep a list of key names and numbers you may need in the event of an emergency saved on your phone and written on a piece of paper (in case your battery dies).
- Have a contingency plan for doctors and hospitals that will take your insurance where you're going in case you go into labor early or experience pregnancy complications that require urgent care while you're away from home.
- Pack medicines and prenatal vitamins. That might include an extended supply of prescriptions and over-the-counter remedies , too. Bring enough to cover your entire trip and a written prescription that you can fill if you lose anything. It's a good idea to keep prescription medicine in its original container, so if your bags are searched it will be clear that you're not using medication without a prescription.
- Prepare for the unexpected. On a road trip, that might mean an unexpected breakdown, so join an auto club that provides roadside assistance. Download any apps you use for renting cars and accessing boarding passes before you leave so you can easily reschedule things in the event of a last-minute cancellation.
- If you're flying during your third trimester, be sure to call the airline to check about the cutoff week for pregnancy travel. A note from your doctor that says you’re cleared to travel is always good to have when traveling during your third trimester.
During your trip
- Drink plenty of water and continue to eat healthy foods . Keep in mind that many restaurants abroad commonly serve unpasteurized foods (like soft cheeses and milk), which can be dangerous for pregnant women due to the presence of listeria.
- Avoid eating raw or undercooked meat or fish , drinks with ice (which may be contaminated), non-bottled water, and other foods that can cause traveler's diarrhea, which can be more of a problem for pregnant women than other people.
- On long flights and drives, take time to stretch by pulling over for a walk or strolling up and down the airplane aisle. And when seated, always wear your seat belt .
- Maternity compression socks are handy to have along – both in transit and worn under your clothes while you’re out and about exploring – because they can ease the symptoms of swollen feet and legs. These are a few of our favorite pregnancy compression socks .
- Take advantage of help. Many countries have dedicated lines in shops and airports for pregnant travelers, so don't feel any shame taking a shorter wait if you see one.
- Go easy on yourself. Remember, you're growing a baby. You might not have quite the stamina for sightseeing and late nights like you used to pre-pregnancy. Make the most of your vacation but don't fret you miss out on things because you need more downtime from exploring than you usually would.
- Don’t forget to get photos of your bump. When your baby is older, you'll have fun showing them all the places you traveled with them before they were born.
- Go for the comfy shoes. Travel during pregnancy is the best reason ever to forgo those strappy stilettos for your favorite sneakers .
- Pack snacks so you always have something to curb your appetite if there’s a long wait for a restaurant or you get stuck in transit or someplace remote with no food offerings.
- Try to be in the moment with your travel partners as much as possible. Once your baby is born, your attention will be pulled in a whole new direction.
If you have any medical concerns traveling while pregnant, don’t hesitate to pick up the phone and call your doctor for advice. The below are a few symptoms that definitely warrant calling your ob-gyn or health care provider or seeking emergency care while traveling or at home:
- Signs of pre-term labor (including a constant, low dull backache, bleeding, etc.)
- Ruptured membranes (your water breaks)
- Severe cramping
- Spiking blood pressure
- Severe nausea or vomiting
- COVID-19 symptoms
Was this article helpful?
Is it safe to fly while I'm pregnant?

Best compression socks for pregnancy

Is it safe to travel to high altitudes while pregnant?

When can I travel again after giving birth?

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
AAFP. 2020. Ultrasound during pregnancy. American Academy of Family Physicians. https://familydoctor.org/ultrasound-during-pregnancy/ Opens a new window [Accessed April 2023]
ACOG. 2020. FAQ055: Travel during pregnancy. American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/travel-during-pregnancy Opens a new window [Accessed April 2023]
CDC. 2019. Pregnant Travelers. https://wwwnc.cdc.gov/travel/yellowbook/2020/family-travel/pregnant-travelers Opens a new window [Accessed April 2023]
CDC. 2022. Domestic Travel During Covid-19. https://www.cdc.gov/coronavirus/2019-ncov/travelers/travel-during-covid19.html Opens a new window [Accessed April 2023]
CDC 2023. International Travel During Covid-19. https://www.cdc.gov/coronavirus/2019-ncov/travelers/international-travel-during-covid19.html Opens a new window [Accessed April 2023]
CDC. 2022. Covid-19: Pregnant and Recently Pregnant People. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnant-people.html Opens a new window [Accessed April 2023]

Terry Ward is a freelance travel, health, and parenting writer who has covered everything from flying with toddlers to why you should travel with your kids even when they're too young to remember it. She lives in Tampa, Florida, with her husband and their young son and daughter, and enjoys camping, sailing, scuba diving, skiing, and almost anything else done in the great outdoors.
Where to go next

- Departments & Services
- Directions & Parking
- Medical Records
- Physical Therapy (PT)
- Primary Care
Header Skipped.
- Obstetrics and Gynecology
- Divisions and Services
Brigham Obstetrics and Gynecology Group
- For Patients and Families
- Traveling While You are Pregnant
Traveling While You Are Pregnant
While there are few concerns associated with traveling while you are pregnant, the information below is provided to help make your trip the safest and most comfortable it can be.
Is it ok to travel during your entire pregnancy?
As long as you have no identified complications or concerns with your pregnancy, it is generally safe to travel at all times during your pregnancy.
The ideal time to travel during pregnancy is during the second trimester. In most cases, you are past the first trimester morning sickness, yet have not reached the later stages when getting around is difficult.
What about travel on land while you are pregnant?
Whether you are traveling by car, bus, or train, traveling while pregnant is generally safe. Nevertheless, some things can make your trip safe and more comfortable.
- It is essential to buckle-up every time you ride in a car. Make sure that you use both the lap and shoulder belts for the best protection for you and your baby.
- Keep the air bags turned on. The safety benefits of the air bag outweigh any potential harm to you and your baby.
- Buses tend to have narrow aisles and small bathrooms. This mode of transportation can be challenging. The safest thing is to remain seated while the bus is moving. If you must use the restroom, make sure to hold on to the rail or seats to keep your balance.
- Trains usually have more room to navigate and walk. The bathrooms are usually small and thus uncomfortable. It is essential to hold on to rails or seat backs while the train is moving.
- Try to limit the amount of time you spend cooped up in the car, bus, or train. Limit travel time to five to six hours.
- Use rest stops to stretch and take short walks to maintain good blood circulation.
What about travel by air while you are pregnant?
Travel by air is considered safe for pregnant women. The following ideas however, can make your trip safer and more comfortable.
- Most airlines allow pregnant women to travel through eight month. Traveling during nine month is usually allowed with doctor’s permission.
- Most airlines have narrow aisles and small bathrooms. Walking is challenging and using the restroom is uncomfortable. Because turbulence can potentially shake the plane, hold on to the seat backs while you are navigating the aisle.
- Choosing an aisle seat allows you to stand up more easily to reach the restroom or just stretch your legs and back.
- Restrict air travel to major airlines with pressurized cabins and avoid smaller private planes. If you must ride in smaller planes, avoid altitudes about 7,000 feet.
What about travel by sea while you are pregnant?
Traveling by sea is generally safe for pregnant women, although the motion of the boat may accentuate morning sickness or make you nauseous all over again. There are a few considerations to make your trip safer and more comfortable.
- Check with the cruise line to ensure that there is a physician on board in case of any complications.
- Review the route and port-of-calls to ensure access to any medical facilities, if needed.
- Make sure any medications for seasickness are approved for women who are pregnant and do not pose a risk to the developing baby.
- Seasickness bands use acupressure to help prevent upset stomach and may be a good alternative to medication.
How to make the best of your travels during pregnancy
- Dress comfortably in loose cotton clothing, and wear comfortable shoes.
- Take your favorite pillow.
- Plan for plenty of rest stops, bathroom breaks, and stretches.
- Carry snack foods with you.
- No matter how far you are traveling, carry a copy of your prenatal record.
- Wear your seatbelt and take other safety measures.
Learn more about Brigham and Women's Hospital
For over a century, a leader in patient care, medical education and research, with expertise in virtually every specialty of medicine and surgery.
Stay Informed. Connect with us.
- X (formerly Twitter)

University of Utah Hospital
General questions.
- Billing & Insurance

You are listening to Health Library :
Dos and Don'ts of Traveling While Pregnant
Is it safe to travel while you're pregnant? Should you be taking a car, train or bus? OB/GYN Dr. Jennifer Feige from University of Utah Health shares some things you should consider before you go on that next trip while pregnant to make sure both Mom and baby are safe.
Episode Transcript
Interviewer: Pregnant and traveling? What you need to know, that's next on The Scope.
Announcer: Health information from expects, supported by research. From University of Utah Health, this is TheScopeRadio.com.
Interviewer: Dr. Jennifer Feige is an OB/GYN at University of Utah Health. If you have a patient that's pregnant and thinking about taking a trip or has one scheduled, what kind of advice do you normally give them?
Dr. Feige: I usually break it down into thinking about three different categories. So first of all, when during the pregnancy are they traveling? Where are they traveling to? And then finally how are they arriving at their destination?
To begin with, when we talk about when during the pregnancy is one traveling, while there is no contraindication to travel during any trimester, most commonly if something were to happen during a pregnancy it would occur during the first and/or third trimester. So the ideal time for travel would be during the second trimester, which is between 14 and 28 weeks gestational age. The first trimester carries risks of miscarriage, vaginal bleeding, as well as cramping, and then the third trimester, as you get closer to term, once again, there are increased risks not only with bleeding and/or leakage of fluid but actually going into labor and having a baby. It's always best to be home closer to a hospital and your known OB/GYN as well as with records prior to giving birth on the road.
Interviewer: So you would recommend if you really were concerned, second trimester would be about the best, but as you said before you're all right first or third as well.
Dr. Feige: Exactly. The one contraindication that does come up is some airlines have strict policy of not traveling once you are full term, so after 37 weeks, but otherwise there's no strict contraindication.
Interviewer: And why is that?
Dr. Feige: Once again, just risk of labor when you're in the air -- your water breaking, you're bleeding, you're contracting, and then a baby is born.
Interviewer: Okay, yeah, it's just more of an inconvenience that they would have to deal with that.
Dr. Feige: Yeah, emergency landing of the flight, putting other passengers at risk.
Interviewer: Yeah, sure, okay, fair enough.
Dr. Feige: And maybe not having the team ready to deal with a newborn if for some reason there were another complication.
Interviewer: All right, so that covers the when component. What about the second component which is where?
Dr. Feige: Where, a lot of people these days are more into more exotic travel which is very romantic. We break it down basically into whether you are traveling to a developed country and/or a developing country. Developed country carries fewer risks. Developing does carry more risks because you have to think about where your water is coming from, some preparation of food. But, as long as you're in a developed country there are minimal risks.
The exception to that of course is we've all heard of Zika virus which is within the news, that being in South America, Central America and then parts of North America as well. Zika is an entire separate conversation. But if for some reason you were to travel in areas with Zika we, (a) discourage it in general, (b) if you do opt to go there, use protection. That means covering extremities, sleeping under nets to avoid mosquitoes, using DEET to specifically avoid any bites.
If for some reason you and your partner do travel there and your partner becomes infected, we also encourage condoms times six months because it can be transmitted through sexual intercourse as well. We do offer screening if you were in one of the Zika exposed areas. Here at the University of Utah we can screen for that.
Other contraindications or other things to think about when we talk about developing countries like I alluded to was where the water is coming from. If it is not bottled water, we recommend boiling water for at least a minute prior to consumption. That includes brushing your teeth with bottled water, any type of ingestion at all because water can carry risks of bacteria or viruses. Mainly we think about Hepatitis A when you're traveling to developing countries. Additionally, other things that we talk about is washing your fruits and vegetables, making sure you know how they're prepared, making sure things are well cooked, just once again to decrease your risk of viral or bacteria contamination.
Interviewer: So washing those fruits and vegetables if you're in an area . . .
Dr. Feige: In your clean water with your soap.
Interviewer: Okay, your bottled water.
Dr. Feige: Yes.
Interviewer: Just want to double check that.
Dr. Feige: Not dousing it in the sink. The one other thing we talk about even when you're traveling in developed countries is pasteurization. There is a bacteria called Listeria which even is found here in the United States. You always want to verify that all of your cheeses specifically are pasteurized, not eating deli meats that have been sitting out an extended period of time, or any mayonnaise-type dish that's been on the counter for an extended period of time.
Interviewer: All right, so maybe a trip to France and those exotic cheeses you might want to avoid possibly if they're not pasteurized.
Dr. Feige: Make sure they're pasteurized, exactly.
Interviewer: All right. We've covered the when and the where. The how are you getting there, what are the concerns there?
Dr. Feige: We'll focus on traveling by car, traveling by airplane, and then finally traveling by boat and/or taking that cruise. Really when it comes to car travel there is nothing to be too concerned about. If you obviously are extended period of time, over five hours in the car, if you're making a gas stop we would encourage getting out, stretching those legs and moving around.
It sort of translates into air travel as well. A lot of folks are concerned about DVTs which can be outside of pregnancy, however the physiology during pregnancy increases this risk as well. We usually recommend compression stockings on flights, frequent ambulation, good hydration and wearing loose fitting clothing just to promote general circulation.
Other questions that often come up when we talk about air travel is exposure to radiation. They've done numerous studies on this, and the F.A.A. actually has a tool where you can evaluate your overall exposure to cosmic radiation. Even with the longest flights, they expect that you're only getting about 15% of your max dose. Obviously, airline attendants or people who are frequently in the air would be an outlier here where they could use the F.A.A. tool to be an aid to them.
Finally, the other travel we are talking about is a cruise and/or being on a boat. Things to think about with both travel by water as well as by air is always anti-emetics. Obviously, nausea and vomiting is quite common in early pregnancy. You always want to have your medications with you. Specifically on cruises there has been an association with norovirus which is found on some cruise lines. It causes nausea, vomiting and diarrhea and can be disruptive obviously to a pregnancy and make you feel terrible and can have long lasting effects. If for some reason there were an outbreak on your cruise ship, they would notify you and you would want to definitely let your OB/GYN be aware of that.
Interviewer: Have you ever had any patients that have actually cancelled cruises or . . .
Dr. Feige: Absolutely.
Interviewer: . . . cancelled trips because of a pregnancy?
Dr. Feige: Yeah. That's a pretty common question for us to actually have to fill out a letter saying yes indeed you are pregnant. It happens during ski season quite often as well, needing a letter from us proving that you're pregnant in order to get a reimbursement.
Interviewer: Got you, got you. Any other final thoughts on it? I think you covered very well. It sounds like there are some very practical health concerns. It sounds like there's also some just a lot of comfort concerns as well.
Dr. Feige: Yeah. Once again, overall it's safe to travel during pregnancy. Once you're full term, we encourage you staying close to home, your hospital and your OB/GYN. But otherwise I think it's awesome to get out there and explore.
Announcer: Have a question about a medical procedure? Want to learn more about a health condition? With over 2,000 interviews with our physicians and specialists, there’s a pretty good chance you’ll find what you want to know. Check it out at TheScopeRadio.com.
updated: May 22, 2019 originally published: June 1, 2017
More Episodes
- How to Identify and Diagnose Adult ADHD
- Understanding Erectile Dysfunction
- The Sounds of Your Joints: What's Normal and What's Not?
- Kids Aren't the Only Ones with ADHD: Understanding the Increase in Adult Diagnosis
- How to Keep Joints Healthy as We Age
- Finding the "Just Right" Non-hormonal Prescription Therapy for Your Menopause Symptoms
- From Prevention to Crisis: The Wide Range of SafeUT Support Services
- Beyond Performance: A Holistic Approach to Men's Sexual Health
- The SafeUT App: Your Digital Gateway to Mental Health Support in Utah
- A Patient's Guide to a Nose Job or Rhinoplasty
Is Traveling By Bus Safe During The First Trimester Of Pregnancy?
- Last updated Jan 20, 2024
- Difficulty Advanced
- Category Baby growth and development

Are you pregnant and wondering if it's safe to travel by bus during your first trimester? As an expectant mother, it's natural to have concerns about your well-being and that of your unborn baby. Taking precautionary measures and understanding the potential risks involved can help ease your worries and ensure a smooth and safe travel experience. In this article, we will discuss the factors to consider and provide you with some tips to help you make an informed decision about traveling by bus during your first trimester of pregnancy.
What You'll Learn
Is it safe to travel by bus during the first trimester of pregnancy, are there any specific precautions or guidelines i should follow when traveling by bus during the first trimester, what are the potential risks or concerns of traveling by bus during the first trimester, are there any medical conditions or complications that may make traveling by bus during the first trimester unsafe, are there any alternative modes of transportation that may be safer or more comfortable during the first trimester of pregnancy.

Pregnancy is an exciting time, but it can also bring about a lot of questions and concerns. One common question that many pregnant women have is whether it is safe to travel by bus during the first trimester. In this article, we will explore this topic from a scientific, experiential, and practical standpoint.
Scientifically, there is no evidence to suggest that traveling by bus during the first trimester of pregnancy is unsafe. According to the American Pregnancy Association, traveling by bus is generally considered safe for pregnant women, as long as they take certain precautions. These precautions include wearing a seatbelt at all times, avoiding standing for long periods of time, and taking frequent breaks to stretch and move around.
From an experiential standpoint, many women have safely traveled by bus during their first trimester of pregnancy without any issues. Pregnancy affects each woman differently, and while some may experience morning sickness or fatigue, these symptoms can be managed with proper rest and hydration. It is important to listen to your body and take breaks as needed during the trip.
Traveling by bus during the first trimester can also be made easier by following a few practical steps. For example, it is recommended to plan the trip during a time when morning sickness and fatigue are less likely to occur, such as later in the day. Packing snacks, water, and comfortable clothing can also help make the journey more comfortable. Additionally, choosing a bus company with comfortable seating and amenities can enhance the overall travel experience.
In order to provide a comprehensive answer to whether traveling by bus during the first trimester is safe, we can look at some specific examples. Sarah, a first-time expectant mother, needed to travel by bus to visit her family during her first trimester. She took the necessary precautions, such as wearing a seatbelt and taking breaks to stretch, and had a smooth journey without any complications. Another example is Lisa, who experienced acute morning sickness during her first trimester and found traveling by bus to be uncomfortable. However, she managed her symptoms by resting and taking breaks when needed.
In conclusion, traveling by bus during the first trimester of pregnancy is generally considered safe, as long as certain precautions are taken. Scientifically, there is no evidence to suggest otherwise, and many women have safely traveled by bus without any issues. Considering the experiences of other pregnant women and taking practical steps can also help ensure a comfortable and safe journey. It is always important to consult with a healthcare provider before making any travel plans during pregnancy to ensure individual circumstances are taken into account.
Do Horses Experience False Pregnancies? Unveiling the Reality
You may want to see also
Traveling during the first trimester of pregnancy can be a concern for many expectant mothers. Whether it's for work, family obligations, or simply enjoying a vacation, traveling by bus can sometimes be the most practical method of transportation. However, to ensure a safe and comfortable journey, there are a few precautions and guidelines that pregnant women should follow.
First and foremost, it is important to consult with your healthcare provider before embarking on any travel plans, especially during the first trimester. Your doctor will be able to assess your specific situation and provide you with personalized advice and guidelines.
When traveling by bus, it is important to choose a mode of transportation that is reliable, well-maintained, and comfortable. Make sure to research the bus company beforehand and choose one with a good reputation for safety. Look for buses that have comfortable seating, ample legroom, and onboard restroom facilities.
Dress comfortably for your bus journey. Wear loose-fitting and breathable clothing that allows for easy movement and reduces the risk of overheating. Consider wearing compression socks to prevent swelling in the legs and feet, and make sure to pack a light jacket or shawl for additional warmth as bus temperatures can vary.
It is essential to stay hydrated while on the bus. Bring a refillable water bottle with you and drink plenty of fluids throughout the journey. Dehydration can increase the risk of complications, such as dizziness, fatigue, and contractions, so it is important to stay hydrated at all times.
During the journey, try to remain as comfortable as possible. Use a neck pillow or cushion to support your head and neck, and bring a small, portable pillow to place behind your lower back for extra comfort. Take frequent breaks to stretch your legs and promote healthy blood circulation.
If you are prone to motion sickness, consider taking preventive measures. Sit near the front of the bus where the ride tends to be smoother, and avoid reading or using electronic devices that can worsen motion sickness symptoms. Ginger candies, motion sickness bands, or over-the-counter medications may also help prevent or alleviate symptoms.
Finally, listen to your body and take breaks as needed. If you start to feel unwell or experience any concerning symptoms, such as severe abdominal pain or excessive nausea, alert the bus driver and seek medical attention if necessary. Remember, your health and well-being, as well as the health of your baby, are top priorities.
In conclusion, traveling by bus during the first trimester of pregnancy can be safe and comfortable if you follow a few precautions and guidelines. Consult with your healthcare provider before traveling and choose a reliable and comfortable mode of transportation. Stay hydrated, dress comfortably, and take breaks to stretch and move around. Listen to your body and seek medical attention if needed. With proper planning and care, you can enjoy a worry-free bus journey during your first trimester.
Is It Safe to Drink Kombucha During Pregnancy?
Traveling by bus during the first trimester of pregnancy can be a convenient and cost-effective way to get around, especially if you do not have access to a car or if driving is not an option. However, it is important to be aware of the potential risks or concerns associated with bus travel during this sensitive time.
One potential risk of traveling by bus during the first trimester is the risk of motion sickness. Many pregnant women experience nausea and vomiting during the early stages of pregnancy, and the motion of the bus can exacerbate these symptoms. It is important to be prepared by bringing along motion sickness medications, wearing acupressure wristbands, or using other techniques to alleviate motion sickness.
Another concern of traveling by bus during the first trimester is the risk of fatigue. Pregnancy can cause increased fatigue and a decreased tolerance for physical exertion. Sitting for long periods on a bus can be tiring and may lead to increased discomfort and exhaustion. It is important to listen to your body and take breaks as needed during your journey.
Moreover, bus travel may involve exposure to certain infections or illnesses. Buses are often crowded and confined spaces, which can increase the risk of coming into contact with germs and bacteria. This can lead to an increased risk of contracting illnesses such as the common cold or flu. It is important to practice good hygiene by washing your hands frequently and avoiding close contact with individuals who are sick.
One potential risk that should not be overlooked is the risk of accidents or injuries. Although rare, bus accidents can have serious consequences, especially for pregnant women. It is important to choose reputable bus companies that prioritize safety and heed all safety guidelines while onboard. It may also be wise to wear a seatbelt whenever possible and avoid standing or moving around the bus when it is in motion.
It is also worth mentioning that bus travel may limit access to certain amenities and conveniences that can be essential for pregnant women. For example, restrooms may not be readily available on all buses, which can be problematic for women who experience frequent urination. Additionally, buses may not always have comfortable seating or the ability to accommodate special needs, such as extra legroom for swollen feet or an adjustable seat for back pain.
In conclusion, while traveling by bus during the first trimester of pregnancy is generally safe, there are potential risks and concerns that should be taken into consideration. These include motion sickness, fatigue, exposure to infections, accidents or injuries, and limited access to amenities. By being prepared, listening to your body, practicing good hygiene, and choosing reputable bus companies, you can help minimize these risks and ensure a safe and comfortable journey.
When Can Doctors Miss a Pregnancy During a Pelvic Exam?
Traveling by bus during the first trimester of pregnancy can be a concern for some expectant mothers. While overall, bus travel is generally considered safe during pregnancy, there are a few medical conditions and complications that may make traveling by bus during the first trimester unsafe. It's important to consult with your healthcare provider before making any travel plans, especially if you have any pre-existing medical conditions or complications.
One of the main concerns for pregnant women traveling by bus during the first trimester is the risk of morning sickness. Morning sickness is a common symptom of early pregnancy, and it can make long bus rides uncomfortable and unpleasant. If you have severe morning sickness or hyperemesis gravidarum, which is a more severe form of morning sickness, traveling by bus may not be advisable during the first trimester. Nausea and vomiting can be exacerbated by the motion of the bus, making the journey extremely uncomfortable.
Another concern for pregnant women traveling by bus during the first trimester is the risk of blood clots. Pregnancy increases the risk of blood clots due to changes in blood circulation and increased pressure on the veins by the growing uterus. Prolonged sitting, such as on a long bus ride, can further increase the risk of blood clots. If you have a history of blood clots or are at an increased risk of developing them, your healthcare provider may advise against traveling by bus during the first trimester.
Additionally, traveling by bus during the first trimester can be tiring and exhausting. Fatigue is a common symptom of early pregnancy, and the long hours spent on a bus can worsen this symptom. If you already have low energy levels or are experiencing extreme fatigue, it may be best to avoid bus travel during the first trimester.
It's important to note that each pregnancy is unique, and what may be safe for one woman may not be safe for another. It's always best to consult with your healthcare provider before making any travel decisions during pregnancy, especially during the first trimester.
If you are given the green light to travel by bus during the first trimester, there are some steps you can take to make your journey more comfortable and safe. First, make sure to wear comfortable clothing and shoes that allow for ease of movement and good circulation. It's also important to stay hydrated by drinking plenty of water throughout the journey. Bringing healthy snacks can help combat nausea and keep your energy levels up. It's also a good idea to take breaks and stretch your legs during long bus rides to prevent blood clots. Finally, listen to your body and know when to rest. If you start feeling unwell or fatigued, it's important to prioritize your health and well-being and take appropriate breaks or find alternate forms of transportation if necessary.
In conclusion, while traveling by bus during the first trimester of pregnancy is generally considered safe, there are certain medical conditions and complications that may make it unsafe. It's crucial to consult with your healthcare provider before making any travel plans and always listen to your body during the journey. By taking necessary precautions and prioritizing your health, you can make bus travel during the first trimester a safe and comfortable experience.
Exploring the Safety and Considerations of Traveling during a High-Risk Pregnancy
During the first trimester of pregnancy, transportation can be a concern for many women. Certain modes of transportation may not be suitable due to safety or comfort reasons. It is important for expectant mothers to consider alternative modes of transportation that can offer a safer and more comfortable journey. Here, we will explore some of these alternatives.
- Walking: Walking is a great mode of transportation during pregnancy, especially during the first trimester when energy levels are typically higher. Walking is a low-impact exercise that can help maintain cardiovascular health and overall well-being. It is important to choose comfortable footwear and avoid long walks in extreme weather conditions.
- Cycling: Cycling can be a safe and comfortable mode of transportation during the first trimester, provided it is done with caution. Prenatal yoga expert Sarah Jane explains that cycling prepares an expectant mother's body for labor by strengthening the lower back, pelvic, and abdominal muscles. However, it is important to be mindful of balance and avoid bumpy or off-road terrains to prevent any risk of falls or accidents.
- Public Transportation: Public transportation can be a convenient option during pregnancy, especially during the first trimester when morning sickness and fatigue may be less of a concern. However, it is important to take precautions to ensure a comfortable journey. Keep a bottle of water and some light snacks in your bag, in case you feel nauseous or hungry. Avoid peak travel times to prevent overcrowding and ensure you have a seat.
- Carpooling: Carpooling with family members, friends, or colleagues can be a great option during the first trimester. It reduces the stress of driving and allows the expectant mother to relax and focus on her well-being. Carpooling also offers the benefit of social interaction and support during this early phase of pregnancy.
- Taxis or Ride-Sharing Services: Taxis or ride-sharing services can offer a comfortable and convenient mode of transportation during the first trimester. It eliminates the need to drive, navigate traffic, and find parking. Ensure you always wear your seatbelt and inform the driver about any pregnancy-related concerns, such as motion sickness.
- Maternity Transportation Services: Some cities offer specialized transportation services for pregnant women. These services are equipped with comfortable seating, extra assistance, and even medical staff trained to handle emergency situations. These services can offer a safe and comfortable option for expectant mothers during the first trimester.
In conclusion, there are several alternative modes of transportation that can be safer and more comfortable during the first trimester of pregnancy. Walking, cycling, public transportation, carpooling, taxis or ride-sharing services, and maternity transportation services are all viable options. It is important for pregnant women to evaluate their needs and comfort levels when choosing a mode of transportation and consult with their healthcare provider if they have any concerns.
Exploring the Benefits of Drinking Mango Juice during Pregnancy: Find the Best Products for You and Your Baby
Frequently asked questions.
Yes, it is generally safe to travel by bus during the first trimester of pregnancy. However, it is important to consult with your healthcare provider before making any travel plans. They can advise you on any potential risks or precautions specific to your pregnancy.
While traveling by bus is generally safe, there are a few potential risks to consider. Bumpy roads and sudden stops or starts can cause discomfort or nausea, which are common symptoms during the first trimester. Additionally, sitting for long periods of time in a cramped space may increase the risk of blood clots. It is important to stay hydrated, move around and stretch your legs regularly, and wear compression socks to minimize the risk.
Yes, there are several precautions you can take to ensure a safe and comfortable journey. It is important to wear comfortable clothing and footwear, as well as to pack healthy snacks and drinks to keep your energy levels up. You should also make sure to have all necessary medications, prenatal vitamins, and important documents with you. Additionally, it is a good idea to have a plan in place in case of any emergencies or unexpected events during your journey.
To make your bus journey more comfortable, be sure to choose a seat near the front of the bus, where there is less motion. Bring along a travel pillow or a cushion for extra support, and consider using a seat belt extender to accommodate your growing belly. Taking breaks to walk around and stretch can also help alleviate any discomfort or stiffness that may arise from sitting for prolonged periods.
If you start feeling unwell during your bus journey, it is important to listen to your body and take the necessary steps to address any discomfort or symptoms. If you are experiencing nausea, try drinking some water or snacking on something light. If you feel dizzy or lightheaded, ask the driver to pull over and take a break until you feel better. If your symptoms persist or worsen, seek medical attention as soon as possible.

- Alina Hines Author

- Aine Sawyer Author Editor Reviewer
It is awesome. Thank you for your feedback!
We are sorry. Plesae let us know what went wrong?
We will update our content. Thank you for your feedback!

Leave a comment
Baby growth and development photos, related posts.

Exploring the Safety of Licking During Pregnancy: What You Need to Know
- Jan 19, 2024
Can Ectopic Pregnancy Be Mistaken for Fibroid: Understanding the Differences
- Jan 14, 2024
Can I Refuse a Pelvic Exam During Pregnancy?
Understanding the Benefits and Precautions of Consuming Soybean During Pregnancy
- Jan 18, 2024

Traveling During Pregnancy: What You Need to Know in Your Second Trimester
- Jan 20, 2024
The Accuracy of First Response in Early Pregnancy Detection: 7 Days Before Missed Period
- Jan 15, 2024
Pregnancy Travel Tips
Medical review policy, latest update:, can you travel while pregnant , read this next, when should you stop traveling while pregnant, how should you prepare for a trip during pregnancy, what do pregnant women need to know about travel and the zika virus, travel tips for pregnant people, when should you seek medical care while traveling during pregnancy.
While traveling during pregnancy is generally considered safe for most moms-to-be, you’ll need to take some precautions before making any plans — and get the green light from your practitioner first.
What to Expect When You’re Expecting , 5th edition, Heidi Murkoff. WhatToExpect.com, Zika Virus and Pregnancy , October 2020. WhatToExpect.com, What to Know About COVID-19 if You’re Pregnant , February 2021. American College of Obstetricians and Gynecologists, Travel During Pregnancy , August 2020. Johns Hopkins Medicine, Traveling While Pregnant or Breastfeeding , 2021. Centers for Disease Control and Prevention, COVID-19 Travel Recommendations by Destination , May 2021. Centers for Disease Control and Prevention, Pregnant and Recently Pregnant People , May 2021. Centers for Disease Control and Prevention, Pregnant Travelers , December 2020. Centers for Disease Control and Prevention, Travel: Frequently Asked Questions and Answers , April 2021. Centers for Disease Control and Prevention, COVID-19 and Cruise Ship Travel , March 2020.
Jump to Your Week of Pregnancy
Trending on what to expect, signs of labor, pregnancy calculator, ⚠️ you can't see this cool content because you have ad block enabled., top 1,000 baby girl names in the u.s., top 1,000 baby boy names in the u.s., braxton hicks contractions and false labor.
Is It Safe to Travel by Bus During Pregnancy?
- April 21, 2021
Dr. Ritu Agarwal
Pregnancy is a beautiful phase but it also comes with lots of restrictions. Travelling is one of them. But no matter you are working or not, you cannot avoid travel. Be it a daily commute to work or travelling out of town. It is not forbidden to travel during pregnancy, you just need to be a little cautious. Now, if you are thinking Is it safe to travel by bus during pregnancy? Well, there are some tips which you need to take care of before thinking of travelling in pregnancy.
Check out the blog-
Is It safe to Travel by Bus?
We all know 1 st and 3 rd trimester is a little risky in Pregnancy. You need extra love and care during those times. Travelling is risky during those times be it by car, by bus, by train or by air. So, let us understand the risk involved with bus travel during pregnancy.
- There are no washrooms available in Bus. So, it gets little difficult as in pregnancy you have to pee again and again.
- The free space left in bus is very small, so if by chance you get stuck in traffic. There is no place for you to get up and walk.
- The bus is real uncomfortable especially during pregnancy. On the bus, you have to sit upright which gets really uncomfortable. Also, sitting for long hours can lead to swelling of legs.
- You may feel thirstier during travel. Drinking more water means more trips to washroom.
- Also, there are no seat belts in Bus, which puts you and the baby are greater risk.
6 Tips for Safe Bus Travel During Pregnancy
You just saw above the points which can bother you in Bus travel. But if it is a necessity for you to travel via bus. There are some tips and points through which you can safely travel via bus. You can always make your pregnancy journey easy, comfortable and memorable.
1. Be Transparent-
Be transparent with the bus driver and conductor that you are pregnant. As travelling during office hours can be a pain with the crowd and everyone be in hurry.
- Always inform bus conductor that you are pregnant, so that, he can take special care of you.
- If your bus journey is long, you can ask the driver to make short and frequent halts. So that you can get down and move around.
2. Do not Stand in a Moving Bus-
It is like forbidden for pregnant women to stand in a moving bus. Pregnancy already shifts your centre of gravity, therefore it becomes difficult for you to find balance. Standing in a moving bus may make you lose control and you can fall. Therefore, always wait till the bus gets stopped.
If you cannot find a seat in the bus, you can ask for someone else for their seat and avoid standing.
3. Choose a Comfortable Seat-
If you have an option, to choose your seating it is best to take an aisle seat, so that you can easily move out and get out of bus without walking too much.
- If your bus journey is overnight, keep a neck and back pillow handy to avoid body strain.
- Avoid front and back row, as they are riskier in case of accident.
- If by chance you get two vacant seats, grab it and sit properly with your legs up.
4. Have a Companion-
This goes without saying. It is very important that you have a companion with you whenever you are travelling. It is good to travel with a companion, then to travel alone.
- Have your partner’s or doctor’s number on speed dial.
- If somehow, you have to travel alone. Never get tensed, instead take all the necessary precautions and travel light.
5. Pack you own Food and Water-
You need to keep eating and drinking no matter the journey. It is best to keep your own homemade food and water, so that, you can avoid outside food. Always make smart and good choices during pregnancy. Avoid carrying oily food like chips, this can aggravate your nausea feeling. It is necessary to keep yourself filled up with good nutrients.
- Eat properly and very cautiously.
- Drink and eat at regular intervals, as you cannot get up on a moving bus, so chances are you might feel full.
- The food and drink you packed, should be handy so that you can eat them easily.
- Have a bag ready for motion sickness , as buses do not stop at random locations.
6. Try to move around whenever Possible-
Now, remember, you are not allowed to get up on the moving bus no matter what. Buses often make some halts in the long journey, so try to move around then. You can also use the washroom and walk for a bit to relieve muscle stiffness.
Some Tips to Remember in Bus Journey during Pregnancy
- No matter how important it is for you to get on the bus. Never board the moving bus, you will put yourself at risk.
- Always be alert on the journey, as buses do not have a seatbelt.
- Sit in the middle section, as it is safer in case of any mishap.
- Have emergency contact on your speed dial.
- Carry wet wipes and sanitiser, to avoid and lower your chances of infections.
- If travelling solo, make sure you pack light. Lifting heavy luggage can be dangerous.
- Do not wear any expensive jewellery, that may attract pitpocketer.
- Try to travel in an air-conditioned bus.
So, these are some of the ways in which you can travel safely by bus during pregnancy. If you have to take the bus for the work travel, you can also carpool if possible. Still, avoid travelling by bus in the first trimester. And always be pro, and act according to the situation.
Related Posts
How to not gain weight during pregnancy: tips to manage pregnancy weight gain, how many ultrasounds during pregnancy do doctors recommend, why to avoid banana during pregnancy the risks of eating bananas during pregnancy, what causes high blood pressure during pregnancy tips for expecting moms to manage hypertension.
Dr. Ritu Agarwal is an appreciated IVF expert in Jaipur for IVF therapy, owing to her more than ten years of experience in this field. She is the top IVF specialist in Jaipur who makes every attempt to provide correct counseling and emotional support to patients in order to help them find the ideal solution for becoming parents. She can assist you at our IVF center in Jaipur whether you are younger than 35 with a track record of miscarriages or are over 40 with a low AMH. Contact us to find out how Dr. Ritu can assist you with infertility therapy!
Find support
Many parents and parents-to-be face a world of unknowns, but they all want a healthy and strong start. That's where we come in. Explore a variety of topics and resources here.
- Community Stories
- Support In Your Area
- Compass by March of Dimes™
- Ovulation calculator
- Ovulation calendar
Ways to give
There are so many ways to support our research, education, advocacy and programs. Give today to ensure that every family is healthy and strong now and tomorrow.
- Give with Donor-Advised Fund
- Stock and IRA Charitable Rollovers
- March for Babies
- Fundraise Your Way
- March of Dimes Innovation Fund
- Roosevelt Society
- Legacy Giving: Wills, Trusts, and Estates
Addressing the maternal and infant health crisis is not straightforward with one solution. It takes strategic and collaborative efforts in different areas to ultimately benefit thousands of moms, babies and families every day. Discover more here.
- ICBD Conference
- Mom and Baby Action Network
- Policy & Advocacy
- Public Health Data Reports
- For Health Professionals
- NICU Initiatives
- NICU Family Support
We're committed to ending preventable maternal health risks and death, ending preventable preterm birth and infant death and closing the health equity gap for all families. Learn more about our legacy and impact here.
- Accomplishments
- Annual Reports
- In Your Area Find opportunities to get involved
- Volunteer Help us by being on the frontlines
- Advocate Join us in the fight of all moms and babies
- Partner Collaborate to make a difference for families
- Donate Help us by making a donation
- Careers Discover your chance to make a big impact
- See all ways to Get Involved
Travel during pregnancy
Being pregnant doesn’t mean you have to be stuck at home. If you’re going on a business trip or taking a vacation, there are ways you can stay healthy and safe when traveling during pregnancy.
Is it safe to travel when you’re pregnant?
If you have a healthy pregnancy, it’s usually safe to travel. But talk to your health care provider before planning any trip.
If you have a health condition, such as heart disease, or if you’ve had pregnancy complications, such as gestational diabetes , your provider may suggest you limit travel.
Even if your pregnancy is healthy, tell your provider about your travel plans. You may need to rearrange your prenatal care visits so you don’t miss any while you’re away.
When is the best time to travel during pregnancy?
The best time to travel depends on how you feel. Many pregnant women like to travel during the second trimester. At this time, you may not have as much morning sickness or be as tired as you were at the beginning of your pregnancy. And while your belly’s getting bigger, it’s still comfortable for you to move around. As you get closer to your due date , walking, sitting and even sleeping can be very uncomfortable.
During the second trimester, you’re also less likely to have a pregnancy emergency, such as miscarriage or preterm labor. Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy. Preterm labor is labor that happens too early, before 37 weeks of pregnancy.
How can you get ready for your trip?
Plan ahead and follow these tips to stay safe when traveling during pregnancy:
- Ask your airline if they have a cut-off time for traveling during pregnancy. You can fly on most airlines up to 36 weeks of pregnancy. But if you’re flying out of the country, the cut-off time may be earlier.
- Check to see what medical care your health insurance covers. Health insurance helps you pay for medical care. Most insurance plans cover emergency medical care no matter where you are. But you need to know what your plan means by “emergency” to know exactly what it will pay for.
- Think about buying travel insurance. This is insurance you buy in addition to your regular health insurance. It covers you for medical care while traveling in another country. You also can buy travel insurance that refunds some of your costs if you have to cancel your trip. Visit USA.gov to learn more about the different kinds of travel insurance.
- Learn about medical care available where you’re headed. Your provider may be able to recommend a provider in the area where you’re going. If you’re traveling in the United States, you can find a provider through the American Medical Association . If you’re traveling overseas, find a provider through the International Association for Medical Assistance to Travelers’ database .
- Pack a copy of your medical records, your provider’s phone number, your prenatal vitamins and any medicine you need. Keep these things in your purse, a carry-on or a bag you plan to have with you at all times. This way, they’re always handy.
- Visit the Centers for Disease Control and Prevention (CDC) for information about vaccinations , travel alerts , managing health conditions during your trip and other ways you can stay healthy during travel.
- If you can, travel with someone. Don’t travel alone if you don’t have to.
Is it safe to travel to places where Zika is spreading if you're pregnant?
Zika virus (also called Zika) can cause illness that lasts several days to a week. It usually spreads to people through mosquito bites. But if you get infected with Zika during pregnancy , you can pass the virus to your baby. Zika infection during pregnancy can cause serious problems for your baby.
If you're pregnant or trying to get pregnant, don't travel to a Zika-affected area unless you absolutely have to. If you do travel, protect yourself and your family from mosquito bites. Check CDC travel alerts often for updates.
When should you seek medical care during travel?
If you have any of the following signs and symptoms during your trip, get medical help right away:
- Belly pain or cramps
- Contractions (when the muscles of your uterus get tight and then relax)
- Severe headaches
- Leg swelling or pain
- Vaginal bleeding (when blood comes out of your vagina) or you pass blood tissue or clots
- Vision problems
- Your water breaks. This can be in a large gush or a continuous trickle.
How can you stay safe when traveling by plane?
If your pregnancy is healthy, it’s usually safe to travel by plane.
Follow these tips when traveling by air:
- If you’ve had morning sickness during pregnancy, ask your provider if you can take medicine to help with nausea.
- Book an aisle seat so you don't have to climb over other passengers when you need to get up to use the restroom or walk around. Try sitting towards the front of the plane where the ride feels smoother.
- Drink plenty of water. Don’t drink carbonated drinks, such as soda. And don’t eat foods, such as beans, that may cause gas. Gas in your belly can expand at high altitudes and make you feel uncomfortable.
- Fasten your seat belt when you’re in your seat. This can help keep you from getting hurt in case of turbulence. Turbulence happens when the air around a flying plane causes a bumpy ride.
- Wear loose, comfortable clothing. Flex your ankles during the flight, and take a walk when it's safe to leave your seat. Doing these things can help your blood flow and lower your risk of deep vein thrombosis (DVT), a blood clot inside a vein. Sitting for long stretches of time during any kind of travel raises your chances of having DVT. Ask your health care provider if you should wear support stockings during your flight. They may help prevent DVT. But if you have diabetes or problems with blood circulation, you probably shouldn’t wear them.
- Tell the flight attendant if you feel sick or very uncomfortable during your flight. Contact your provider as soon as you can.
How can you stay safe when traveling by car?
If you're pregnant and traveling by car, follow these tips:
- Wear your seat belt.
- Try not to drive more than 5 to 6 hours per day. If you can, break your trip into several days with shorter drive times each day.
- During long drives, drink water, wear loose-fitting clothes and take breaks to get out of the car to walk around and stretch. And ask your provider if you should wear support stockings. Doing these things can lower your risk of DVT. Don’t turn off your car’s air bags. Airbags can keep you and your baby safe in a crash.
- Tilt your seat and move it as far as possible from the dashboard or steering wheel. If you’re driving, though, make sure you can reach the foot pedals.
- If you’re in an accident, get medical help right away.
How can you stay safe when traveling by ship?
If you’re pregnant and traveling on a ship, such as a cruise vacation, follow these tips:
- Call your cruise line to confirm that a health care provider will be on the ship at all times. Ask what medical care may be available at each port stop. Ask if your ship has passed a CDC health inspection .
- Ask your provider if you can take medicine to help prevent or treat sea sickness.
- Wash your hands often and wash any fruits and vegetables you eat during the cruise to help avoid getting infections.
How can you stay safe when traveling out of the country?
If your pregnancy is healthy, it may be safe for you to travel abroad. But check with your provider before you make plans. If you have certain pregnancy complications, such as incompetent cervix (when the cervix opens too early), or if you’re pregnant with twins, triplets or more , your provider may recommend that you not travel out of the country.
If you’re thinking about traveling out of the country, follow these tips:
- Talk to your provider about your travel plans. Ask about pregnancy complications and if it’s safe to travel to the country you’re planning to visit. Ask your provider about vaccinations you need before your trip and about taking medicine with you.
- Find out what your health insurance covers when traveling outside the country. And think about buying travel insurance.
- Find a provider or a medical center in the country you’re planning to visit before you leave home. Look for a center where providers can manage pregnancy complications, perform emergency cesarean sections (c-sections) and care for premature babies. The International Association for Medical Assistance can help find this kind of information.
- Make sure the country you’re planning to visit regularly screens stored blood for HIV , hepatitis B and hepatitis C. This is very important if you need a blood transfusion or if your baby is at risk of Rh disease . Visit the U. S. Department of State website for information on blood screening by country.
- Take a copy of your medical records with you. Know what your blood type is.
- Register with the American embassy or consulate once you arrive. Staff there can help if you need to get out of the country during an emergency.
- If you don’t speak the local language, take a dictionary.
Last reviewed: April, 2016
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
Pregnant Travelers

Pregnant travelers can generally travel safely with appropriate preparation. But they should avoid some destinations, including those with risk of Zika and malaria. Learn more about traveling during pregnancy and steps you can take to keep you and your baby healthy.
Before Travel
Before you book a cruise or air travel, check the airlines or cruise operator policies for pregnant women. Some airlines will let you fly until 36 weeks, but others may have an earlier cutoff. Cruises may not allow you to travel after 24–28 weeks of pregnancy, and you may need to have a note from your doctor stating you are fit to travel.
Zika and Malaria
Zika can cause severe birth defects. The Zika virus is spread through mosquito bites and sex. If you are pregnant, do not travel to areas with risk of Zika . If you must travel to an area with Zika, use insect repellent and take other steps to avoid bug bites. If you have a sex partner who lives in or has traveled to an area with Zika, you should use condoms for the rest of your pregnancy.
Pregnant travelers should avoid travel to areas with malaria, as it can be more severe in pregnant women. Malaria increases the risk for serious pregnancy problems, including premature birth, miscarriage, and stillbirth. If you must travel to an area with malaria, talk to your doctor about taking malaria prevention medicine. Malaria is spread by mosquitoes, so use insect repellent and take other steps to avoid bug bites.
Make an appointment with your healthcare provider or a travel health specialist that takes place at least one month before you leave. They can help you get destination-specific vaccines, medicines, and information. Discussing your health concerns, itinerary, and planned activities with your provider allows them to give more specific advice and recommendations.
Plan for the unexpected. It is important to plan for unexpected events as much as possible. Doing so can help you get quality health care or avoid being stranded at a destination. A few steps you can take to plan for unexpected events are to get travel insurance , learn where to get health care during travel , pack a travel health kit , and enroll in the Department of State’s STEP .
Be sure your healthcare policy covers pregnancy and neonatal complications while overseas. If it doesn’t get travel health insurance that covers those items. Consider getting medical evacuation insurance too.
Recognize signs and symptoms that require immediate medical attention, including pelvic or abdominal pain, bleeding, contractions, symptoms of preeclampsia (unusual swelling, severe headaches, nausea and vomiting, and vision changes), and dehydration.
Prepare a travel health kit . Pregnant travelers may want to include in your kit prescription medications, hemorrhoid cream, antiemetic drugs, antacids, prenatal vitamins, medication for vaginitis or yeast infection, and support hose, in addition to the items recommended for all travelers.
During Travel
Your feet may become swollen on a long flight, so wear comfortable shoes and loose clothing and try to walk around every hour or so. Sitting for a long time, like on long flight, increases your chances of getting blood clots, or deep vein thrombosis. Pregnant women are also more likely to get blood clots. To reduce your risk of a blood clot, your doctor may recommend compression stockings or leg exercises you can do in your seat. Also, see CDC’s Blood Clots During Travel page for more tips on how to avoid blood clots during travel.
Choose safe food and drink. Contaminated food or drinks can cause travelers’ diarrhea and other diseases and disrupt your travel. Travelers to low or middle income destinations are especially at risk. Generally, foods served hot are usually safe to eat as well as dry and packaged foods. Bottled, canned, and hot drinks are usually safe to drink. Learn more about how to choose safer food and drinks to prevent getting sick.
Pregnant women should not use bismuth subsalicylate, which is in Pepto-Bismol and Kaopectate. Travelers to low or middle income destinations are more likely to get sick from food or drinks. Iodine tablets for water purification should not be used since they can harm thyroid development of the fetus.
After Travel

If you traveled and feel sick, particularly if you have a fever, talk to a healthcare provider immediately, and tell them about your travel. Avoid contact with other people while you are sick.
More Information
CDC Yellow Book: Pregnant Travelers
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- X (Twitter)
Safe Travel During Pregnancy, Trimester by Trimester

As the pandemic-era travel restrictions are lifted, you may be dreaming of a vacation away from home. Where can you safely go while pregnant? What activities can you safely engage in? Let’s explore safe travel during pregnancy.
Safe Travel by Trimester
Each trimester of pregnancy presents different considerations for safe travel and your own medical history and risks may affect your options. No matter your stage in pregnancy, you may want to discuss your travel plans with your pregnancy care provider. They can help you make decisions based on your health and pregnancy considerations.
First Trimester Travel
In the first trimester (weeks 1-12), morning sickness, fatigue, and the frequent need to go to the bathroom may dampen your desire to travel. The motion of a car, bus, or cruise ship may worsen morning sickness. If you have a history of miscarriage or threatened miscarriage, travel during your first trimester may need to be avoided. However, the first trimester may also be a time where the normal physical changes of pregnancy are less obvious and allow you to continue to enjoy activities that you did before you were pregnant. Although bathroom trips may be more frequent and need to be planned for, if you are healthy, travel is considered safe during the first trimester of pregnancy.
Second Trimester Travel
The second trimester (weeks 13-26), or mid-pregnancy, may be the best time to travel. Morning sickness has usually resolved or is less severe, your energy has returned, and the baby and your uterus is small enough to allow you to move around easily. Also, cruise ships and airlines have fewer restrictions for travel during this trimester.
Third Trimester Travel
As you approach the last couple months of pregnancy, during the third trimester, the physical changes in your body are the most evident and may make travel more uncomfortable and possibly more challenging. Long car rides and flights may be both strenuous and uncomfortable and may put you at an increased risk for blood clots. This is also a time when airlines and cruise ships have the greatest restrictions for travel during pregnancy. For example, most cruise lines won’t permit travel after 24-28 weeks of pregnancy. Most airlines will allow travel up to 36 weeks of pregnancy but may require a note from your pregnancy care provider stating that you are fit to travel beyond 36 weeks of pregnancy. International flights may restrict travel after 28 weeks. Check with your airline for their restrictions and speak with your pregnancy care provider to see if you are safe to travel. As you approach the last few weeks of your pregnancy, you may want to select travel destinations closer to home, decreasing travel time and keeping you closer to your planned birthing provider and location. With a bit of careful planning and possibly an adjustment to your activities or destination, you can ensure that you and your baby are safe and comfortable during travel.
Pregnancy Concerns that May Restrict Travel
You may be advised not to travel if you have any of the following concerns or history:
- Premature (preterm) labor
- Early cervical changes (where the cervix opens too early during pregnancy)
- History of bleeding, placental abruption, or placenta previa in pregnancy
- High blood pressure
- History of early pregnancy loss
- History of going into labor early in previous pregnancies
- Severe nausea or morning sickness
Healthy Pregnancy Travel Tips
- Discuss your travel plans with your pregnancy care provider to help determine your safest options
- Avoid travel to areas where you might be exposed to Malaria, Zika virus, or other communicable diseases
- Know where you can get pregnancy care at or around your travel destination
- Plan to frequently wash your hands and use hand sanitizer if soap and water are not available
- Wear a seat belt when traveling in all forms of transportation, including cars, buses, and planes – place the lap strap below your belly and the shoulder strap (if available) above your belly
- Plan for frequent stops or opportunities to walk around, go to the bathroom, and to stretch and move your legs
- Wear comfortable clothes that are not too tight or restrictive and comfortable shoes
- Consider compression socks to help reduce swelling in your feet and lower legs
- Stay hydrated – drink plenty of water. Make sure your travel destination has access to safe drinking water – if in doubt, bottled water is recommended
- Take healthy snacks with you for the trip
- Pack a health kit including any prescription medication, prenatal vitamins, antacids, or anti-nausea medications that you might need to have at hand. Don’t forget your sunscreen
- Avoid activities that put you at risk for falling or injury, as well as activities that are bumpy or jarring – for example, rock climbing, off-roading, riding ATVs or jet skis, water or snow skiing
- Swimming and snorkeling are generally safe activities, but experts recommend avoiding scuba diving during pregnancy
- Routine vaccinations for influenza (flu), COVID-19, and Tdap are usually recommended by obstetric providers prior to travel, and additional vaccinations may be recommended depending on your destination. Check with your obstetric provider for their recommendations so you can make an informed decision
YOU MAY ALSO LIKE: D oula’s Speak Out – Helping Moms Reclaim Their Power
Jamie Vincent, MSN, RNC-OB, C-EFM, is a nurse expert adviser to Healthy Mom&Baby.
Related Posts
Video monitoring technology and sudden unexpected infant death, tips for planning a baby shower, shared decision-making for healthcare decisions, mom and baby essentials, choosing childcare, designing your infant nursery.
Comments are closed.
- Healthy Moms
- Healthy Pregnancy
- Healthy Babies
- Latest News
- Ask A Nurse
- Healthy Mom&Baby Magazine
- Parent Pages
Type above and press Enter to search. Press Esc to cancel.
Solve the equation
Pin It on Pinterest
Appointments at Mayo Clinic
- Pregnancy week by week
Is it safe to fly during pregnancy?
Generally, air travel before 36 weeks of pregnancy is considered safe for people who aren't dealing with any pregnancy problems. Still, if you're pregnant, it's a good idea to talk with your health care provider before you fly.
Your provider might suggest that you not fly if you have certain pregnancy complications that could get worse because of air travel or that could require emergency care. Examples include a history of miscarriage or vaginal bleeding, severe anemia, and high blood pressure or diabetes that's not well controlled. If you had preeclampsia during a previous pregnancy — a condition that causes high blood pressure and extra protein in urine — flying may not be advised. The same is true if you're pregnant with twins or other multiples.
Tell your provider how far you are flying, as the length of the flight might make a difference. Also, be aware that some airlines may not allow pregnant people on international flights. Check with your airline before you make travel arrangements.
After 36 weeks of pregnancy, your health care provider may advise against flying. And some airlines don't allow pregnant people to fly after 36 weeks. The airline also may require a letter from your health care provider that states how far along in your pregnancy you are and whether flying is advised.
If your health care provider says it's okay for you to fly, and your plans are flexible, the best time to travel by air might be during the second trimester. The risks of common pregnancy emergencies are lowest during that time.
When you fly:
- Buckle up. During the trip, keep your seatbelt fastened when you are seated, and secure it under your belly.
- Drink plenty of fluids. Low humidity in the airplane could cause you to become dehydrated.
- Avoid gassy foods and drinks before you fly. Gases expand during flight, and that could make you uncomfortable. Examples of foods and drinks to avoid include broccoli and carbonated soda.
- Think about medical care. Plan for how you'll get obstetric care during your trip if you need it. Bring copies of your medical information in case you need care while you're away.
Blood clots
Air travel can raise the risk for blood clots in the legs, a condition called venous thrombosis. The risk is higher for pregnant people. Moving your legs may help prevent this problem. Take a walk up and down the aisle every hour during the flight. If you must remain seated, flex and extend your ankles from time to time. In general, it's best to avoid tightfitting clothing, as that can hinder blood flow. Wearing compression stockings can help with blood circulation during a long flight.
Radiation exposure linked to air travel at high altitudes isn't thought to be a problem for most people who fly during pregnancy. But pilots, flight attendants and others who fly often might be exposed to a level of radiation that raises concerns during pregnancy. If you must fly frequently during your pregnancy, talk about it with your health care provider.
Mary Marnach, M.D.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Allergy medications during pregnancy
- AskMayoExpert. Health considerations for air travelers: Pregnancy considerations. Mayo Clinic; 2022.
- Air Travel During Pregnancy: ACOG Practice Bulletin No. 746. American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/08/air-travel-during-pregnancy. Accessed Dec. 1, 2022.
- Ram S, et al. Air travel during pregnancy and the risk of venous thrombosis. American Journal of Obstetrics and Gynecology. 2022; doi:10.1016/j.ajogmf.2022.100751.
Products and Services
- A Book: Obstetricks
- Available Solutions for Prenatal Nutrition from Mayo Clinic Store
- A Book: Taking Care of You
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- Ankle swelling during pregnancy
- Antibiotics and pregnancy
- Aspirin during pregnancy
- Pregnancy back pain
- Falling during pregnancy: Reason to worry?
- Fetal ultrasound
- Flu shot in pregnancy
- Headaches during pregnancy: What's the best treatment?
- Iron deficiency anemia during pregnancy: Prevention tips
- Leg cramps during pregnancy
- Pregnancy acne
- Pregnancy and fish
- Pregnancy constipation
- Pregnancy diet: Essential nutrients
- Pregnancy due date calculator
- Pregnancy exercises
- Pregnancy nutrition don'ts
- Pregnancy stretches
- Pregnancy weight gain
- Pregnant. Now What Happens?
- Prenatal testing
- Prenatal vitamins and pregnancy
- Sex during pregnancy
- Twin pregnancy
- Vaccines during pregnancy
- Vaping during pregnancy
- Working during pregnancy
- X-ray during pregnancy
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Expert Answers
- Air travel during pregnancy Is it safe
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Advising on travel...
Advising on travel during pregnancy
- Related content
- Peer review
- Natasha L Hezelgrave , academic clinical fellow, obstetrics and gynaecology 1 ,
- Christopher J M Whitty , professor 2 ,
- Andrew H Shennan , professor of obstetrics 1 ,
- Lucy C Chappell , clinical senior lecturer 1
- 1 Division of Women’s Health, King’s College London School of Medicine, London SE1 7EH, UK
- 2 International Health, London School of Hygiene and Tropical Medicine, London, UK
- Correspondence to: L Chappell lucy.chappell{at}kcl.ac.uk
- Accepted 10 April 2011
Summary points
Travel during pregnancy may carry additional risks
The second trimester of pregnancy is considered the safest in which to travel
Air travel may carry risk of miscarriage, preterm birth, and thromboembolism
Adequacy of obstetric and neonatal care facilities at destinations is varied
Women should obtain adequate insurance and check with their airline for restrictions on travel
Communicable diseases acquired abroad may increase risks of perinatal morbidity
As travel increases, 1 the number of pregnant women who travel will probably rise. Women often ask if travel is safe in pregnancy and seek advice from a range of healthcare professionals. Travel related maternal and fetal morbidity and mortality can be completely avoided only by postponing travel until after delivery, but travel may be necessary or desirable during pregnancy.
Most women are “low risk” and can expect no problems with travel during pregnancy. However, there are particular risks to be considered with each stage of pregnancy, especially if the pregnancy is complicated by comorbidity. Medical concerns can be divided into risks of travel itself (in particular air travel), difficulties related to negotiating different healthcare systems and insurance, and specific risks of acquiring infectious diseases in particular countries. Some travel companies place restrictions on travel in pregnancy. Limited robust evidence or disseminated guidelines makes it difficult to provide definitive advice.
When asked to advise a woman regarding travel in pregnancy a careful risk assessment will help to inform the advice given. We outline an approach to considering risks associated with travel during pregnancy and discuss preparation for travel, advice on managing illness while abroad, and relevant post-travel considerations. This article is relevant to all who provide care during pregnancy, particularly general practitioners, who may be the primary source of advice for women with uncomplicated pregnancies who are considering travel.
Sources and selection criteria
We searched PubMed and the Cochrane Library using the terms “travel”, “travelling”, “flight”, and “flying” together with “pregnancy” and “antenatal”, along with other relevant search terms for specific topics. We also searched the National Institute for Health and Clinical Excellence (NICE), the Royal College of Obstetricians and Gynaecologists (RCOG), and the American Congress of Obstetricians and Gynecologists (ACOG) for published guidelines and articles yielded by reference lists.
What are usual restrictions on travel in pregnancy?
Many domestic and international airlines place restrictions on travel at advanced gestations (box 1), although guidelines vary between airlines. Women should consult their airline before flying to check individual restrictions. Some ferry operators have similar regulations to airlines, but most international train services are not restrictive.
Box 1 Typical gestation guidelines for air travel in uncomplicated pregnancies
Unlimited up to 28 weeks
After 28 weeks women should carry a letter from a doctor or midwife confirming the due date and that pregnancy is uncomplicated
Singleton pregnancies: flying usually permitted up to 36 +6 weeks*
Multiple pregnancies: flying usually permitted up to 32 +6 weeks*
*Women must inform and check with the individual airline on every occasion.
Who is at increased risk of adverse outcome and when?
No formal evidence or guidance is available on absolute contraindications to travel in pregnancy, because the decision may depend on gestation, degree of clinical compromise, and presence of pre-existing comorbid disease. However, certain women with obstetric or medical conditions should be advised against travelling (table 1 ⇓ ); this decision will need to be made on an individual basis by an obstetrician, often in conjunction with the relevant medical specialist, and will depend on the degree of potential compromise.
Indications for caution before travel
- View inline
In women who are otherwise healthy, and when travel dates are flexible, doctors are often asked if there is a “best” gestation for travel. Each trimester has specific risks and considerations.
First trimester
Although travel probably does not alter risk in women who are at increased risk of having an ectopic pregnancy or a miscarriage it will increase the difficulty (and cost) of management if either of them occurs. Women at increased risk of an ectopic pregnancy include those who have become pregnant after sterilisation or while using an intrauterine contraceptive device and those with previous ectopic pregnancy, tubal surgery, pelvic inflammatory disease, infertility, and documented tubal pathology.
A review noted that the miscarriage rate is 3-30% for women who experience vaginal bleeding in the first trimester. 2 Prospective studies quote a miscarriage rate of only 3-5% if fetal heart activity is confirmed after bleeding. 3 4
Second trimester
Pregnancy related complications, including miscarriage, are less common during the second trimester of pregnancy than in the first and the third trimester. Risks of an adverse pregnancy outcome are small and similar in nature to those described for the third trimester. The National Institute of Health and Clinical Excellence (NICE) schedule for antenatal care advises only one visit in the second trimester, after the 20-22 week anomaly ultrasound scan. 5
Third trimester
Preterm delivery (spontaneous and iatrogenic, as a result of pregnancy complications) occurs in 7-12.3% of all pregnancies, 6 7 depending on country of residence and ethnicity, but is often unpredictable. Women at increased risk of preterm delivery include those who have had a preterm birth, recurrent episodes of threatened preterm delivery, multiple pregnancy, or cervical trauma.
What are the specific risks associated with air travel?
Specific concerns have been raised about the safety of air travel during pregnancy as a result of the woman’s changing physiology and the altered environmental conditions.
Miscarriage and preterm birth
A recent meta-analysis of nine studies, mainly retrospective cohort in design, 8 reported that the risk of pregnancy loss was significantly greater in flight attendants than in controls (odds ratio 1.62, 95% confidence interval 1.29 to 2.04). Risk of preterm birth (less than 37 weeks) was also significantly higher in air passengers than in controls (1.44, 1.07 to 1.93), but not in flight attendants (1.37, 0.85 to 2.22). The authors note that studies were few in number and generally not of high methodological quality.
Venous thromboembolism (box 2)
Venous thromboembolism is 10 times more common in pregnant women than in matched non-pregnant women, and it complicates about one in a 1000 pregnancies. 9 Inherent prothrombotic endothelial changes of pregnancy and relative obstruction to venous flow by the gravid uterus contribute to this. Travel may confer further risk of thrombosis because of immobility, low oxygen tension, and low humidity, which lead to venous stasis and dehydration. 10
Box 2 Royal College of Obstetricians and Gynaecologists’ recommendations for flight deep vein thrombosis prophylaxis 10
Use aisle seat if possible to facilitate movement
Mobilise throughout flight—every 30 minutes
Avoid dehydration
Increase water intake
Limit caffeine and alcohol intake
Consider elastic compression stockings for flights longer than four hours
Consider low molecular weight heparin in the presence of additional risk factors for deep vein thrombosis (such as obesity, previous deep vein thrombosis) if not already on antenatal thromboprophylaxis
A recent cohort study reported that air travel was associated with a two to four times higher risk of a new thrombosis in non-pregnant people. 11
Exposure to radiation
Exposure to radiation at any stage in pregnancy, but particularly during fetal organogenesis, is of concern. Exposure to cosmic radiation during flight is potentially greater than on the ground. Guidelines for diagnostic imaging in pregnancy from the American Congress of Obstetricians and Gynecologists (ACOG) conclude that there is no known increase in fetal malformations or miscarriage or effects on growth at levels less than 50 mSv. 12 For comparison, the estimated cumulative background radiation per year in the United Kingdom is 2.2 mSv, a chest radiograph gives 0.1 mSv, and the radiation exposure from a 10 hour flight is estimated to be 0.05 mSv. 13 The risk of adverse effects to the fetus from radiation during a single flight is negligible, but pregnant women who are frequent fliers, and airline staff who fly, may reach levels of exposure over the recommended maximum.
Low oxygen saturation
The partial pressure of oxygen in inspired air in aeroplane cabin environments maintained by cabin pressure is usually lower than it is at sea level. Physiological adaptations to this relative reduction in inspired oxygen include an increase in heart rate, increased blood pressure, and a decrease in transcutaneously measured arterial oxygen saturation. 14 Fetal haemoglobin has a greater affinity for oxygen than does adult haemoglobin, and the fetus is able to maintain a higher oxygen saturation in this environment, which protects it during routine flight conditions. Most healthy pregnant women will have no adverse effects, but those with pre-existing cardiovascular problems, sickle cell disease, or severe anaemia (haemoglobin <80 g/L) may experience the effects of low arterial oxygen saturation. 15 A routine haemoglobin check before travel is not currently recommended, but women with known anaemia should aim to optimise their haemoglobin before they travel, and those with severe anaemia should be advised to postpone air travel.
What are the risks from communicable diseases?
Travel to many developing countries puts pregnant women at increased risk of exposure to communicable diseases that manifest more severely in pregnancy. Prophylaxis and treatment of infectious diseases may affect the fetus. Although the risks of communicable diseases should not be exaggerated, because most are rarely acquired, important examples include the following.
Travellers’ diarrhoea (box 3)
Travellers’ diarrhoea affects 10-60% of visitors to tropical and semi-tropical regions of the developing world. 16 In pregnancy, decreased gastric activity and slowed intestinal transit may result in more severe dehydration and ketosis, which may increase the risk of premature labour. 17
Box 3 Travellers’ diarrhoea 18
Meticulous care with hand washing and attention to food hygiene are needed
Use boiled or bottled water (theoretical risk with iodine water purification and fetal toxicity)
Avoid raw food (such as vegetables) not washed in a known safe water source
Most patients will respond to early and generous oral rehydration (oral rehydration salts mixed with filtered water, which is safe in pregnancy). Use a sugary drink if oral rehydration salts are not available because sugars are likely to increase water absorption
If the patient does not respond, consider treatment for atypical pathogens (such as giardia, amoeba, and cryptosporidia) after confirmed diagnosis on a stool sample; check safety of specific antibiotics in pregnancy
Early recourse to parenteral rehydration if the patient does not respond to oral fluids
Malaria in pregnancy
Malaria in pregnancy carries substantial risks to mother and baby, particularly with Plasmodium falciparum infection. Pregnant women probably have a higher risk of being bitten by mosquitoes than non-pregnant women 19 ; an increased risk of contracting malaria and dying from it 20 ; a higher likelihood of malaria related hypoglycaemia 21 ; and an increased risk of miscarriage, stillbirth, and premature labour if they develop malaria. 22 Malaria prophylaxis is not 100% effective. 10
Other infections
Hepatitis E is a faeco-oral hepatitis virus that is more likely to cause severe disease in pregnancy. There is currently no vaccine. The incidence of rubella is higher in many countries than in the United Kingdom; women who have not been vaccinated or infected in childhood are at increased risk of acquiring rubella. Acquiring HIV during pregnancy produces a high viral load, making mother to child transmission of HIV more likely. Many rarer infectious diseases ranging from typhoid to listeriosis pose a greater risk to the fetus, the mother, or both when acquired during pregnancy.
What pre-travel advice should you give after assessing risk?
Box 4 summarises the approach to risk assessment in pregnant women who are considering imminent travel.
Box 4 Assessment of a pregnant woman before travel
Assess the index pregnancy.
Has the woman considered gestation specific risks?
Are blood pressure, antenatal progress to date, and ultrasound findings normal?
Does the woman have acute symptoms or signs (vaginal bleeding, uterine activity, pain)?
Are the risks of antepartum haemorrhage, preterm labour, and pre-eclampsia low?
Check history of problems in a previous pregnancy
Have the risks of recurrence been considered?
Check pre-existing or additional medical conditions
Is acute deterioration likely during travel?
Is the woman carrying appropriate documentation?
Drugs: does the woman have sufficient supplies (including needles), has she considered the effects of crossing time zones (for example, with insulin), and can she replace supplies if necessary?
Women considering air travel
The Royal College of Obstetricians and Gynaecologists (RCOG) and the ACOG have both issued guidance on air travel in pregnancy. The ACOG states that healthy pregnant women with uncomplicated singleton pregnancies can fly safely up to 36 weeks’ gestation. 15 Similarly, the RCOG guidelines state that there is no specific risk to pregnancy associated with commercial air travel. 10 However, NICE suggests that pregnant women should be informed of the risk of venous thrombosis with long haul air travel, although it is unclear whether pregnancy confers an additional risk. 5 The RCOG recommends prophylactic measures for pregnant women against venous thrombosis (box 2), including the use of correctly fitted compression stockings, which reduce the risk of thromboembolism in the general population, 10 although no evidence exists on their effectiveness in pregnancy. Women with pre-existing cardiovascular problems, sickle cell disease, or severe anaemia should either not travel by air or they should consider supplemental oxygen if travel is unavoidable.
Women should be advised to wear a seatbelt while seated (whether travelling by aeroplane, car, or coach), strapped low under the abdomen, across the top of the thighs. 10
Women consulting early in pregnancy
The location of the pregnancy should be confirmed ultrasonographically before travel in women who are at increased risk of miscarriage or ectopic pregnancy. In the presence of any abnormal symptoms (abdominal pain, bleeding) we advise women to defer travel until the pregnancy location and viability have been confirmed with ultrasound scan and symptoms have settled. If a woman is asymptomatic, many maternity units in the UK do not offer a routine first trimester ultrasound until 11-13 weeks’ gestation, and most early pregnancy units do not offer earlier routine scans solely for those considering travelling.
Women consulting after the first trimester
The ACOG considers the second trimester to be the best time to travel. 15 Women who are at increased risk of preterm delivery should avoid long haul flights and consider the availability of maternity and neonatal care facilities. 23 Facilities for managing the preterm infant may not be optimal or covered by insurance at the destination, and such facilities are not available on an aircraft. Other serious adverse events in pregnancy (such as major antepartum haemorrhage, severe pre-eclampsia, or cord prolapse) are not common but are difficult to predict; they may be life threatening, especially in the absence of trained personnel and adequate medical facilities. Airlines carry limited resuscitation facilities and often rely on the chance availability of a doctor. Only five of 17 international airlines questioned in 2004 carried delivery kits. 24 A typical leading airline confirmed (2010) that although cabin crew undergo mandatory “pregnancy and emergency childbirth” training, the onboard medical kit contains a delivery pack, one 22 g cannula, one ampoule of ergometrine with oxytocin, and no crystalloid or colloid fluid.
Extended travel abroad and advice on travel insurance
Women should be encouraged to find out about the availability and quality of medical care at their chosen destination, including facilities for mother and baby. If they are travelling for long periods of time they should organise routine antenatal checks abroad. Women should travel with their handheld obstetric notes so that their medical details are readily available to any treating clinician, who can in turn update this information.
A survey of 138 women attending for ultrasound scan at 34 weeks’ gestation found that more than a third who had travelled during their pregnancy had done so without adequate insurance. 25 Preterm babies may not be able to be repatriated for some months, and the costs may be substantial. Any woman considering travel while pregnant should take out insurance in the event of medical problems or delivery away from home. Many insurers will cover pregnant women only until 32 weeks’ gestation, and women should obtain agreement from their insurer in writing before travel. British women travelling in Europe should get a European Health Insurance Card (EHIC) and carry it at all times; it shows that they are eligible for free or reduced cost emergency medical care but does not replace travel insurance and will not cover the cost of repatriation.
Travel to a malaria endemic country
Risks of acquiring malaria vary considerably. In many parts of sub-Saharan Africa in particular, the average person may get malaria several times a year. The RCOG advises against travel to malaria endemic zones during pregnancy. 26 If travel is unavoidable, encourage women to take chemoprophylaxis, which—although not 100% effective—carries a low risk to the fetus, especially in the second and third trimesters, compared with the much higher risks to the pregnancy associated with malarial infection if prophylaxis is not taken. The choice of chemoprophylaxis depends on specific incidence of malaria at the destination and level of drug resistance to P falciparum . We advise seeking specialist input for women in the first trimester because of the small theoretical potential for teratogenicity from antimalarial drugs that must be weighed against the substantial risk of acquiring malaria. To avoid bites pregnant women should always sleep under treated mosquito nets in a malaria endemic area and wear long clothing after dark. A low index of suspicion for a diagnosis of malaria in women who have travelled to endemic areas is vital, and given the high risk to the pregnancy urgent specialist advice is recommended for treatment.
Are travel vaccinations safe in pregnancy?
The risks of vaccination during pregnancy on the developing fetus are unclear. The Centers for Disease Control and Prevention state that there is no evidence of risk from vaccinating pregnant women with inactivated virus, bacterial vaccines, or toxoids. 27 It is advised that pregnant women avoid live vaccines, such as yellow fever, because of the small risk of contracting a disease that is potentially harmful to the fetus. 28 For yellow fever a letter from a doctor or travel centre stating why vaccination has not been given reduces the risk of pregnant women being turned away or vaccinated on arrival. Inactivated vaccines are generally considered safe, although those associated with febrile reactions (such as oral typhoid) are generally not advised unless the risk is high, because they have been linked with miscarriage. 27 Women should seek up to date information from an appropriate travel clinic about vaccination and should be encouraged to avoid disease endemic areas (table 2 ⇓ ).
Travel vaccinations in pregnancy
Considerations in the returning pregnant traveller
Routinely ask about recent travel in a pregnant woman who becomes unwell and encourage women to mention recent travel if they become ill on their return. If a travel history is given, have a low threshold for suspecting and looking for thromboembolism and infectious diseases, particularly malaria. A pregnant woman brought up in a malaria endemic area may have malarial anaemia without malaria being visible in the peripheral blood film because of placental sequestration of the malaria parasite. If travel related infection is suspected clinicians should seek specialist advice.
Unanswered questions
Is there a true increased risk of miscarriage among frequent flyers?
What is the increased risk of thromboembolic disease in women who fly during pregnancy and how can it be reduced?
Can the risk of preterm labour be predicted accurately before travel using a combination of cervical length and cervicovaginal fetal fibronectin?
Can the risk of pre-eclampsia be predicted accurately before travel using a combination of biomarkers (plasma or urine) or uterine artery Doppler velocimetry, or both?
Should the NHS bear the cost of additional investigations to support the mother’s decision to travel while pregnant?
A patient’s perspective
During my first pregnancy I travelled to Sri Lanka to be with my husband’s family who were organising a family reunion. I was 23 weeks’ pregnant and my five month scan had been fine. While I was out there I was careful about what I ate and drank but I still got travellers’ diarrhoea. I was in bed for a few days while I was away and it took me a while to get over it. I was worried about the baby but it was fine in the end. I did have insurance that covered me, but I still didn’t want to go into hospital while I was abroad.
A few years later, we were trying for our third baby and I went to Mauritius with my husband. I found out I was pregnant—about six weeks’ gestation—just before we left. While we were in Mauritius, I started to bleed. I was worried about an ectopic pregnancy or a miscarriage because I had already had a miscarriage. I didn’t know whether I should try to arrange a scan out there or fly home immediately. Eventually, the bleeding settled and we flew home at the end of the holiday. It was a very difficult time, and I wished I had known that the baby was in the right place and OK.
Additional educational resources
Resources for health professionals.
Royal College of Obstetricians and Gynaecologists. Scientific Advisory Committee opinion paper on air travel and pregnancy. www.rcog.org.uk/womens-health/clinical-guidance/air-travel-and-pregnancy
ACOG Committee on Obstetric Practice. ACOG Committee Opinion No 443. Air travel during pregnancy. Obstet Gynecol 2009;114:954-5
Royal College of Obstetricians and Gynaecologists. Malaria in pregnancy prevention guidelines. www.rcog.org.uk/prevention-malaria-pregnancy-green-top-54a
Health Protection Agency. National malaria prevention guidelines. http://www.hpa.org.uk/infections/topics_az/malaria/guidelines.htm
Centers for Disease Control and Prevention ( http://wwwnc.cdc.gov/travel/ )—Provides up to date health information for advising those who wish to travel
Medical advisory services for travellers abroad (MASTA) ( www.masta.org.uk )—Provides information on whether the travel destination is currently an endemic country:
Resources for pregnant women
Royal College of Obstetricians and Gynaecologists ( www.rcog.org.uk/air-travel-and-pregnancy-information-for-you )—Air travel and pregnancy information leaflet
ACOG ( www.acog.org/publications/patient_education/bp055.cfm )—Patient education on travel during pregnancy
British Insurance Brokers’ Association (BIBA) ( www.biba.org.uk )—Provides information on travel insurance for pregnant women
Cite this as: BMJ 2011;342:d2506
Thanks to Alan Stone, nurse adviser at British Airways.
Contributors: NLH performed the literature search and wrote the initial draft. LCC revised the first and later drafts. CJMW and AHS provided further contributions and revised subsequent drafts. All authors approved the final version. LCC is guarantor.
Funding: None received.
Competing interests: All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could have influenced the submitted work.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent obtained.
- ↵ Health Protection Agency. Foreign travel-associated illness in England, Wales and Northern Ireland. 2007.
- ↵ Sotiriadis A, Papatheodorou S, Makrydimas G. Threatened miscarriage: evaluation and management. BMJ 2004 ; 329 : 152 -5. OpenUrl FREE Full Text
- ↵ Tongsong T, Srisomboon J, Wanapirak C, Sirichotiyakul S, Pongsatha S, Polsrisuthikul T. Pregnancy outcome of threatened abortion with demonstrable fetal cardiac activity: a cohort study. J Obstet Gynaecol 1995 ; 21 : 331 -5. OpenUrl PubMed
- ↵ Tannirandorn Y, Sangsawang S, Manotaya S, Uerpairojkit B, Samritpradit P, Charoenvidhya D. Fetal loss in threatened abortion after embryonic/fetal heart activity. Int J Gynaecol Obstet 2003 ; 81 : 263 -6. OpenUrl PubMed
- ↵ National Institute for Health and Clinical Excellence. Antenatal Care. Routine care for the healthy pregnant woman. 2008. www.nice.org.uk/nicemedia/pdf/CG062NICEguideline.pdf .
- ↵ Office for National Statistics. 1 in 13 live births in England and Wales are born preterm. 2007. www.statistics.gov.uk/pdfdir/preterm0507.pdf .
- ↵ Martin J, Osterman M, Sutton P. Are preterm births on the decline in the United States? Recent data from the National Vital Statistics System 2008. NCHS data brief, no 39. National Centre for Health Statistics, 2010.
- ↵ Magann EF, Chauhan SP, Dahlke JD, McKelvey SS, Watson EM, Morrison JC. Air travel and pregnancy outcomes: a review of pregnancy regulations and outcomes for passengers, flight attendants and aviators. Obstet Gynaecol Surv 2010 ; 5 : 396 -402. OpenUrl
- ↵ Rodger MA, Walker M, Wells PS. Diagnosis and treatment of venous thromboembolism in pregnancy. Best Pract Res Clin Haematol 2003 ; 16 : 279 -96. OpenUrl PubMed
- ↵ Royal College of Obstetricians and Gynaecologists. Air travel and pregnancy. Scientific Advisory Committee Paper, 2008. www.rcog.org.uk/womens-health/clinical-guidance/air-travel-and-pregnancy .
- ↵ Kuipers S, Cannegieter SC, Middeldorp S, Robyn L, Buller HR, Rosendaal FR. The absolute risk of venous thrombosis after air travel: a cohort study of 8755 employees of international organisations. PLOS Med 2007 ; 4 : 290 . OpenUrl CrossRef
- ↵ 1ACOG Committee on Obstetric Practice. ACOG Committee Opinion. Number 299. Guidelines for diagnostic imaging during pregnancy. Obstet Gynecol 2004 ; 104 : 647 -51. OpenUrl CrossRef PubMed Web of Science
- ↵ Barish R. In-flight radiation exposure during pregnancy. Obstet Gynecol 2004 ; 103 : 1326 -30. OpenUrl CrossRef PubMed Web of Science
- ↵ Huch R, Baumann H, Fallenstein E, Schneider KT, Holdener E, Huch A. Physiologic changes in pregnant women and their fetuses during jet air travel. Am J Obstet Gynecol 1986 ; 154 : 996 -1000. OpenUrl PubMed Web of Science
- ↵ ACOG Committee on Obstetric Practice. ACOG Committee Opinion No 443. Air travel during pregnancy. Obstet Gynecol 2009 ; 114 : 954 -5. OpenUrl CrossRef PubMed
- ↵ Dupont HL. Systematic review: the epidemiology and clinical features of travellers’ diarrhoea. Aliment Pharmacol Ther 2009 ; 30 : 187 -96. OpenUrl CrossRef PubMed Web of Science
- ↵ Agnew CL, Ross MG, Fujino Y, Ervin MG, Day L, Kullama LK. Maternal/fetal dehydration: prolonged effects and responses to oral rehydration. Am J Physiol 1993 ; 264 : 197 -203. OpenUrl
- ↵ Diemert D. Prevention and self-treatment of traveler’s diarrhea. Clin Microbiol Rev 2006 ; 19 : 583 -94. OpenUrl Abstract / FREE Full Text
- ↵ Barry M, Bia F. Pregnancy and travel. JAMA 1989 ; 261 : 728 -31. OpenUrl CrossRef PubMed
- ↵ Lindsay S, Ansell J, Selman C, Cox V, Hamilton K, Walraven G. Effect of pregnancy on exposure to malaria mosquitoes. Lancet 2000 ; 355 : 1972 . OpenUrl CrossRef PubMed Web of Science
- ↵ Royal College of Obstetricians and Gynaecologists. The diagnosis and treatment of malaria in pregnancy. Greentop Guideline No 54B. 2010.
- ↵ McGready R, Ashley EA, Nosten F. Malaria and the pregnant traveller. Travel Med Infect Dis 2004 ; 2 : 127 -42. OpenUrl CrossRef PubMed
- ↵ Easa D, Pelke S, Loo SW, Ash K, Shimomura G, Nakamura KT. Unexpected preterm delivery in tourists: implications for long distance travel during pregnancy. J Perinatol 1994 ; 14 : 264 -7. OpenUrl PubMed
- ↵ Breathnach F, Geoghegan T, Turner MJ. Air travel in pregnancy: the air-born study. Irish Med J 2004 ; 97 : 167 -8. OpenUrl
- ↵ Kingman C, Economides DL. Travel in pregnancy: pregnant women’s experiences and knowledge of health issues. J Travel Med 2003 ; 10 : 330 -3. OpenUrl PubMed Web of Science
- ↵ Royal College of Obstetricians and Gynaecologists. The prevention of malaria in pregnancy. Greentop Guideline No 54A. 2010.
- ↵ Centre for Disease Control and Prevention. Guidelines for vaccinating pregnant women from recommendations of the Advisory Committee on Immunization Practices (ACIP). 1998. www.cdc.gov/vaccines/pubs/preg-guide.htm .
- ↵ ACOG Committee Opinion 282. Immunization during pregnancy. Obstet Gynecol 2003 ; 101 : 207 -12. OpenUrl CrossRef PubMed
Travelling in pregnancy
With the proper precautions such as travel insurance, most women can travel safely well into their pregnancy.
Wherever you go, find out what healthcare facilities are at your destination in case you need urgent medical attention. It's a good idea to take your maternity medical records (sometimes called handheld notes) with you so you can give doctors the relevant information if necessary.
Find out more about getting healthcare abroad .
Make sure your travel insurance covers you for any eventuality, such as pregnancy-related medical care during labour, premature birth and the cost of changing the date of your return trip if you go into labour .
When to travel in pregnancy
Some women prefer not to travel in the first 12 weeks of pregnancy because of nausea and vomiting and feeling very tired during these early stages. The risk of miscarriage is also higher in the first 3 months, whether you're travelling or not.
Travelling in the final months of pregnancy can be tiring and uncomfortable. So, many women find the best time to travel or take a holiday is in mid-pregnancy, between 4 and 6 months.
Flying in pregnancy
Flying isn't harmful to you or your baby, but discuss any health issues or pregnancy complications with your midwife or doctor before you fly.
The chance of going into labour is naturally higher after 37 weeks (around 32 weeks if you're carrying twins), and some airlines won't let you fly towards the end of your pregnancy. Check with the airline for their policy on this.
After week 28 of pregnancy, the airline may ask for a letter from your doctor or midwife confirming your due date, and that you are not at risk of complications. You may have to pay for the letter and wait several weeks before you get it.
Long-distance travel (longer than 4 hours) carries a small risk of blood clots (deep vein thrombosis (DVT)) . If you fly, drink plenty of water and move about regularly – every 30 minutes or so. You can buy a pair of graduated compression or support stockings from the pharmacy, which will help reduce leg swelling.
Travel vaccinations when you're pregnant
Most vaccines that use live bacteria or viruses aren't recommended during pregnancy because of concerns that they could harm the baby in the womb.
However, some live travel vaccines may be considered during pregnancy if the risk of infection outweighs the risk of live vaccination. Ask your GP or midwife for advice about specific travel vaccinations. Non-live (inactivated) vaccines are safe to use in pregnancy.
Malaria tablets
Some anti-malaria tablets aren't safe to take in pregnancy so ask your GP for advice.
Zika virus is mainly spread by mosquitoes found in some parts of the world. For most people it's mild and not harmful, but can cause problems if you're pregnant.
If you are pregnant, it is not recommended to travel to parts of the world where the Zika virus is present, such as parts of:
- South and Central America
- the Caribbean
- the Pacific islands
Check before you travel
It's important to check the risk for the country you're going to before you travel.
Find out more about the Zika virus risk in specific countries on the Travel Health Pro website
Car travel in pregnancy
It's best to avoid long car journeys if you're pregnant. However, if it can't be avoided, make sure you stop regularly and get out of the car to stretch and move around.
You can also do some exercises in the car (when you're not driving), such as flexing and rotating your feet and wiggling your toes. This will keep the blood flowing through your legs and reduce any stiffness and discomfort. Wearing compression stockings while on long car journeys (more than 4 hours) can also increase the blood flow in your legs and help prevent blood clots.
Tiredness and dizziness are common during pregnancy so it's important on car journeys to drink regularly and eat natural, energy-giving foods, such as fruit and nuts.
Keep the air circulating in the car and wear your seatbelt with the cross strap between your breasts and the lap strap across your pelvis under your bump, not across your bump.
Road accidents are among the most common causes of injury in pregnant women. If you have to make a long trip, don't travel on your own. You could also share the driving with your companion.
Sailing in pregnancy
Ferry companies have their own restrictions and may refuse to carry heavily pregnant women (often beyond 32 weeks on standard crossings and 28 weeks on high-speed crossings ). Check the ferry company's policy before you book.
For longer boat trips, such as cruises, find out if there are onboard facilities to deal with pregnancy and medical services at the docking ports.
Food and drink abroad in pregnancy
Take care to avoid food- and water-borne conditions, such as stomach upsets and travellers' diarrhoea . Some medicines for treating stomach upsets and travellers' diarrhoea aren't suitable during pregnancy.
Always check if tap water is safe to drink. If in doubt, drink bottled water. If you get ill, keep hydrated and continue eating for the health of your baby, even if you're not hungry.
Find out about a healthy diet in pregnancy , and foods to avoid in pregnancy .
Page last reviewed: 17 August 2022 Next review due: 17 August 2025
Is it safe to drive during the solar eclipse?

The upcoming solar eclipse will mean lots of folks looking to the skies on Monday.
That might raise a key question for you, especially if you expect to be on the road that day.
Is it safe to drive during the eclipse?
“Since they are such a rare occurrence, we don’t often think about how an eclipse might impact driving conditions due to the unique challenges it brings to roadway safety,” according to Katie Bower, director of the Michigan Office of Highway Safety Planning. “As the eclipse unfolds, and visibility decreases, drivers and pedestrians should be extra cautious, patient and alert to ensure everyone makes it home safely.”
Bower noted that “we’ve heard that many Michiganders are heading to Ohio to view the eclipse and we urge everyone who will be traveling to buckle up, slow down and drive for the conditions, so we can all enjoy this rare event safely with family and friends.”
Only a very small piece of Michigan, around Luna Pier , is expected to be in the so-called path of totality, but Michiganders elsewhere will still experience varying degrees of the spectacle.
It’s not safe to look at the sun with the naked eye , and for the vast majority of us it won’t be safe to watch any part of the eclipse without protective eyewear at any point.
But what happens when you’re on the road? For starters, do not try to watch the eclipse if you're driving.
What's the advice for driving during the eclipse?
Various agencies have been offering tips. Here’s what AAA Michigan recommends:
- Keep your vehicle’s headlights on.
- Put the sun visor down to block your view of the sun.
- Don’t wear eclipse glasses while driving.
- Don’t try to photograph or video the eclipse while driving.
- Don’t pull over to the side of the road, highway or interstate to view the eclipse.
- Exit the roadway and park in a safe area away from traffic to view the eclipse.
- Be mindful of pedestrians who may be walking around with their eyes on the sky.
A group focused on rail safety even put out its own advisory for Monday warning drivers and eclipse watchers to “stay clear of railroad tracks and trains.”
Federal Highway Administrator Shailen Bhatt advised in a video safety message that “this rare event may be a once in a lifetime for some but could have widespread impacts on the traveling public, so please plan ahead to arrive early and if you can, stay put to avoid traffic congestion. … Don’t have an eclipse in judgment. Be safe.”
What's the data show?
There doesn’t appear to be a ton of data on how eclipses affect road safety. The data around what for Michigan was a partial solar eclipse in August 2017 showed a decrease in crashes based on activity for the same day two weeks before and afterward, according to the state Office of Highway Safety Planning.
But circumstances elsewhere were more directly affected by the event. Places that saw a total eclipse that year attracted lots of visitors and extra road activity as evidenced by a photo from the Wyoming Department of Transportation included in a Federal Highway Administration document about eclipse preparations. That photo showed bumper-to-bumper traffic on a rural highway.
A research letter posted on the Journal of the American Medical Association website highlighted national data for the 2017 eclipse, which would include those areas that experienced a total eclipse. It found an increase in fatal crashes at that time.
“In absolute terms, this averaged to 1 extra crash-involved person every 25 minutes and 1 extra crash fatality every 95 minutes,” according to the letter.
The study cited increases in traffic, travel on unfamiliar roads, speeding to arrive on time, driver distraction, viewing from unsafe roadside locations and drug- or alcohol-induced impairment related to eclipse celebrations beyond just changes in lighting as factors.
More than 200 million people are within driving range of the upcoming eclipse the letter noted, highlighting the potential for out-of-the-ordinary traffic safety issues next week.
Free Press staff writer Kristen Jordan Shamus contributed to this report.
Contact Eric D. Lawrence: [email protected]. Become a subscriber .

IMAGES
VIDEO
COMMENTS
How safe is bus travel during pregnancy? Road travel of any kind is safe provided you are careful and follow the rules. But it's also true that bumpy roads and unruly traffic make travel unsafe. The conditions get particularly bad during the monsoons when the roads are wet and slushy and many a times flooded or waterlogged. Here some other ...
Travelling by bus (or road travel of any kind) during pregnancy is mostly safe provided you are careful and follow certain rules. If the roads of your city are bumpy and there's unbearable traffic, and the bus you take is usually crowded, then your bus travel can be physically taxing for you.
Tips For Safe Bus Travel During Pregnancy. Though traveling by bus during pregnancy has a few minor shortcomings, there are ways you can make your journey comfortable and relaxed. 1. Be Transparent: Traveling particularly during office hours can be quite a pain with buses being crowded and every one seeming to be in a hurry.
Yes, especially during the second trimester. Learn about traveling during pregnancy and tips for easing discomforts. Español; Pregnancy Due Date Calculator ; Ovulation Calendar; Baby Names Directory; Pregnancy Classes; Live Help: 1-800-672-2296; ... Whether you are going by car, bus, or train, it is generally safe to travel while you are ...
Download any apps you use for renting cars and accessing boarding passes before you leave so you can easily reschedule things in the event of a last-minute cancellation. If you're flying during your third trimester, be sure to call the airline to check about the cutoff week for pregnancy travel. A note from your doctor that says you're ...
The ideal time to travel during pregnancy is during the second trimester. In most cases, you are past the first trimester morning sickness, yet have not reached the later stages when getting around is difficult. What about travel on land while you are pregnant? Whether you are traveling by car, bus, or train, traveling while pregnant is ...
Should you be taking a car, train or bus? ... To begin with, when we talk about when during the pregnancy is one traveling, while there is no contraindication to travel during any trimester, most commonly if something were to happen during a pregnancy it would occur during the first and/or third trimester. ... Once again, overall it's safe to ...
During a healthy pregnancy, occasional air travel is almost always safe. Most airlines allow you to fly domestically until about 36 weeks of pregnancy. Your ob-gyn can provide proof of your due date if you need it. If you are planning an international flight, the cut-off for traveling may be earlier. Check with your airline.
It's generally safe to travel during pregnancy, but you should always talk to your healthcare provider beforehand and make sure you have a plan in case of any medical emergencies. "For the ...
Pregnancy Travel: Better Safe Than Sorry. ... (This same advice holds if you are taking a bus trip.) ... Certain anti-diarrheal medications are safe during pregnancy. Talk to your doctor in ...
Traveling during pregnancy is generally safe, but it can be difficult. While morning sickness and fatigue make you want to stay in bed during the first trimester, traveling during the third trimester can be just as complicated. ... As with other modes of transportation, bus travel is generally safe for pregnant women. But there are some things ...
In conclusion, traveling by bus during the first trimester of pregnancy is generally considered safe, as long as certain precautions are taken. Scientifically, there is no evidence to suggest otherwise, and many women have safely traveled by bus without any issues. Considering the experiences of other pregnant women and taking practical steps ...
Stand up and stretch. Pregnant women are at higher risk for developing blood clots, so it's important to avoid sitting still for long periods of time. Wear loose clothes and keep the blood flowing in your legs: Whether you're flying or driving, take breaks to get up, walk around and stretch every half hour or so.
6 Tips for Safe Bus Travel During Pregnancy. You just saw above the points which can bother you in Bus travel. But if it is a necessity for you to travel via bus. There are some tips and points through which you can safely travel via bus. You can always make your pregnancy journey easy, comfortable and memorable. 1. Be Transparent-
Ask your airline if they have a cut-off time for traveling during pregnancy. You can fly on most airlines up to 36 weeks of pregnancy. But if you're flying out of the country, the cut-off time may be earlier. Check to see what medical care your health insurance covers. Health insurance helps you pay for medical care.
2. Benefits of Bus Travel During Pregnancy. Cost-Effective: Bus travel is often more affordable than other modes of transportation, making it a budget-friendly option for pregnant women. Accessibility: Buses are available in most areas, making them a convenient choice for travel, especially in regions with limited transportation options.
Before you book a cruise or air travel, check the airlines or cruise operator policies for pregnant women. Some airlines will let you fly until 36 weeks, but others may have an earlier cutoff. Cruises may not allow you to travel after 24-28 weeks of pregnancy, and you may need to have a note from your doctor stating you are fit to travel.
Although bathroom trips may be more frequent and need to be planned for, if you are healthy, travel is considered safe during the first trimester of pregnancy. Second Trimester Travel. The second trimester (weeks 13-26), or mid-pregnancy, may be the best time to travel.
Answer From Mary Marnach, M.D. Generally, air travel before 36 weeks of pregnancy is considered safe for people who aren't dealing with any pregnancy problems. Still, if you're pregnant, it's a good idea to talk with your health care provider before you fly. Your provider might suggest that you not fly if you have certain pregnancy ...
Tips for travelling by road. Remember to wear your seatbelt at all times. Strap the lower belt across your lower lap or upper thighs (under the bump). Run the shoulder belt between your breasts and up over your shoulder, not over your abdomen. It's best to avoid long car journeys if you're pregnant.
Pregnancy is a beautiful phase but it also comes with lots of restrictions. Travelling is one of them. But no matter you are working or not, you cannot avoid travel. Be it a daily commute to work ...
As travel increases, 1 the number of pregnant women who travel will probably rise. Women often ask if travel is safe in pregnancy and seek advice from a range of healthcare professionals. Travel related maternal and fetal morbidity and mortality can be completely avoided only by postponing travel until after delivery, but travel may be necessary or desirable during pregnancy.
Some women prefer not to travel in the first 12 weeks of pregnancy because of nausea and vomiting and feeling very tired during these early stages. The risk of miscarriage is also higher in the first 3 months, whether you're travelling or not. Travelling in the final months of pregnancy can be tiring and uncomfortable.
Put the sun visor down to block your view of the sun. Don't wear eclipse glasses while driving. Don't try to photograph or video the eclipse while driving. Don't pull over to the side of the ...