An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List


Breast cancer patient experiences through a journey map: A qualitative study
Laura ciria-suarez.
1 Clinical Psychology and Psychobiology Department, Faculty of Psychology, University of Barcelona, Barcelona, Spain
Paula Jiménez-Fonseca
2 Medical Oncology Department Hospital Universitario Central of Asturias, Oviedo, Spain
María Palacín-Lois
3 Social Psychology and Quantitative Psychology Department, Faculty of Psychology, University of Barcelona, Barcelona, Spain
Mónica Antoñanzas-Basa
4 Medical Oncology Department, Hospital Universitario Clínico San Carlos, Madrid, Spain
Ana Fernández-Montes
5 Medical Oncology Department, Complexo Hospitalario Universitario de Ourense, Ourense, Spain
Aranzazu Manzano-Fernández
Beatriz castelo.
6 Medical Oncology Department, Hospital Universitario La Paz, Madrid, Spain
Elena Asensio-Martínez
7 Medical Oncology Department, Hospital General Universitario de Elche, Elche, Spain
Susana Hernando-Polo
8 Medical Oncology Department, Hospital Universitario Fundación Alcorcón, Madrid, Spain
Caterina Calderon
Associated data.
Relevant anonymized data excerpts from the transcripts are in the main body of the manuscript. They are supported by the supplementary documentation at 10.1371/journal.pone.0244355 .
Breast cancer is one of the most prevalent diseases in women. Prevention and treatments have lowered mortality; nevertheless, the impact of the diagnosis and treatment continue to impact all aspects of patients’ lives (physical, emotional, cognitive, social, and spiritual).
This study seeks to explore the experiences of the different stages women with breast cancer go through by means of a patient journey.
This is a qualitative study in which 21 women with breast cancer or survivors were interviewed. Participants were recruited at 9 large hospitals in Spain and intentional sampling methods were applied. Data were collected using a semi-structured interview that was elaborated with the help of medical oncologists, nurses, and psycho-oncologists. Data were processed by adopting a thematic analysis approach.
The diagnosis and treatment of breast cancer entails a radical change in patients’ day-to-day that linger in the mid-term. Seven stages have been defined that correspond to the different medical processes: diagnosis/unmasking stage, surgery/cleaning out, chemotherapy/loss of identity, radiotherapy/transition to normality, follow-up care/the “new” day-to-day, relapse/starting over, and metastatic/time-limited chronic breast cancer. The most relevant aspects of each are highlighted, as are the various cross-sectional aspects that manifest throughout the entire patient journey.
Conclusions
Comprehending patients’ experiences in depth facilitates the detection of situations of risk and helps to identify key moments when more precise information should be offered. Similarly, preparing the women for the process they must confront and for the sequelae of medical treatments would contribute to decreasing their uncertainty and concern, and to improving their quality-of-life.
Introduction
Breast cancer is the most common cancer and the one that associates the highest mortality rates among Spanish women, with 32,953 new cases estimated to be diagnosed in Spain in 2020 [ 1 ]. Thanks to early diagnosis and therapeutic advances, survival has increased in recent years [ 2 ]. The 5-year survival rate is currently around 85% [ 3 , 4 ].
Though high, this survival rate is achieved at the expense of multiple treatment modalities, such as surgery, chemotherapy, radiotherapy, and hormone therapy, the side effects and sequelae of which can interfere with quality-of-life [ 5 ]. Added to this is the uncertainty surrounding prognosis; likewise, life or existential crises are not uncommon, requiring great effort to adjust and adapt [ 6 ]. This will not only affect the patient psychologically, but will also impact their ability to tolerate treatment and their socio-affective relations [ 7 ].
Several medical tests are performed (ultrasound, mammography, biopsy, CT, etc.) to determine tumor characteristics and extension, and establish prognosis [ 8 ]. Once diagnosed, numerous treatment options exist. Surgery is the treatment of choice for non-advanced breast cancer; chemotherapy, radiotherapy, and hormone therapy are adjuvant treatments with consolidated benefit in diminishing the risk of relapse and improving long-term survival [ 9 ]. Breast cancer treatments prompt changes in a person’s physical appearance, sexuality, and fertility that interfere with their identity, attractiveness, self-esteem, social relationships, and sexual functioning [ 10 ]. Patients also report more fatigue and sleep disturbances [ 11 ]. Treatment side effects, together with prognostic uncertainty cause the woman to suffer negative experiences, such as stress in significant relationships, and emotions, like anxiety, sadness, guilt, and/or fear of death with negative consequences on breast cancer patients’ quality-of-life [ 10 , 12 ]. Once treatment is completed, patients need time to recover their activity, as they report decreased bodily and mental function [ 13 ], fear of relapse [ 14 ], and changes in employment status [ 15 ]. After a time, there is a risk of recurrence influenced by prognostic factors, such as nodal involvement, size, histological grade, hormone receptor status, and treatment of the primary tumor [ 16 ]. Thirty percent (30%) of patients with early breast cancer eventually go on to develop metastases [ 17 ]. There is currently no curative treatment for patients with metastatic breast cancer; consequently, the main objectives are to prolong survival, enhance or maintain quality-of-life, and control symptoms [ 17 , 18 ]. In metastatic stages, women and their families are not only living with uncertainty about the future, the threat of death, and burden of treatment, but also dealing with the existential, social, emotional, and psychological difficulties their situation entails [ 18 , 19 ].
Supporting and accompanying breast cancer patients throughout this process requires a deep understanding of their experiences. To describe the patient’s experiences, including thoughts, emotions, feelings, worries, and concerns, the phrase “patient voice” has been used, which is becoming increasingly common in healthcare [ 20 ]. Insight into this “voice” allows us to delve deeper into the physical, emotional, cognitive, social, and spiritual effects of the patient’s life. This narrative can be portrayed as a “cancer journey", an experiential map of patients’ passage through the different stages of the disease [ 21 ] that captures the path from prevention to early diagnosis, acute care, remission, rehabilitation, possible recurrence, and terminal stages when the disease is incurable and progresses [ 22 ]. The term ‘patient journey’ has been used extensively in the literature [ 23 – 25 ] and is often synonymous with ‘patient pathway’ [ 26 ]. Richter et al. [ 26 ] state that there is no common definition, albeit in some instances the ‘patient journey’ comprises the core concept of the care pathway with greater focus on the individual and their perspective (needs and preferences) and including mechanisms of engagement and empowerment.
While the patient’s role in the course of the disease and in medical decision making is gaining interest, little research has focused on patient experiences [ 27 , 28 ]. Patient-centered care is an essential component of quality care that seeks to improve responsiveness to patients’ needs, values, and predilections and to enhance psychosocial outcomes, such as anxiety, depression, unmet support needs, and quality of life [ 29 ]. Qualitative studies are becoming more and more germane to grasp specific aspects of breast cancer, such as communication [ 27 , 30 ], body image and sexuality [ 31 , 32 ], motherhood [ 33 ], social support [ 34 ], survivors’ reintegration into daily life [ 13 , 15 ], or care for women with incurable, progressive cancer [ 17 ]. Nevertheless, few published studies address the experience of women with breast cancer from diagnosis to follow-up. These include a clinical pathway approach in the United Kingdom in the early 21st century [ 35 ], a breast cancer patient journey in Singapore [ 25 ], a netnography of breast cancer patients in a French specialized forum [ 28 ], a meta-synthesis of Australian women living with breast cancer [ 36 ], and a systematic review blending qualitative studies of the narratives of breast cancer patients from 30 countries [ 37 ]. Sanson-Fisher et al. [ 29 ] concluded that previously published studies had examined limited segments of patients’ experiences of cancer care and emphasized the importance of focusing more on their experiences across multiple components and throughout the continuum of care. Therefore, the aim of this study is to depict the experiences of Spanish breast cancer patients in their journey through all stages of the disease. To the best of our knowledge, there are no studies that examine the experience of women with breast cancer in Spain from diagnosis through treatment to follow-up of survivors and those who suffer a relapse or incurable disease presented as a journey map.
A map of the breast cancer patient’s journey will enable healthcare professionals to learn first-hand about their patients’ personal experiences and needs at each stage of the disease, improve communication and doctor-patient rapport, thereby creating a better, more person-centered environment. Importantly, understanding the transitional phases and having a holistic perspective will allow for a more holistic view of the person. Furthermore, information about the journey can aid in shifting the focus of health care toward those activities most valued by the patient [ 38 ]. This is a valuable and efficient contribution to the relationship between the system, medical team, and patients, as well as to providing resources dedicated to the patient’s needs at any given time, thus improving their quality of life and involving them in all decisions.
Study design and data collection
We conducted a qualitative study to explore the pathway of standard care for women with breast cancer and to develop a schematic map of their journey based on their experiences. A detailed description of the methodology is reported in the published protocol “Ascertaining breast cancer patient experiences through a journey map: A qualitative study protocol” [ 39 ].
An interview guide was created based on breast cancer literature and adapted with the collaboration of two medical oncologists, three nurses (an oncology nurse from the day hospital, a case manager nurse who liaises with the different services and is the ‘named’ point of contact for breast cancer patients for their journey throughout their treatment, and a nurse in charge of explaining postoperative care and treatment), and two psycho-oncologists. The interview covered four main areas. First, sociodemographic and medical information. Second, daily activities, family, and support network. Third, participants were asked about their overall perception of breast cancer and their coping mechanisms. Finally, physical, emotional, cognitive, spiritual, and medical aspects related to diagnosis, treatment, and side effects were probed. Additionally, patients were encouraged to express their thoughts should they want to expand on the subject.
The study was carried out at nine large hospitals located in six geographical areas of Spain. To evaluate the interview process, a pilot test was performed. Interviews were conducted using the interview guide by the principal investigator who had previous experience in qualitative research. Due to the Covid-19 pandemic, all interviews were completed online and video recorded with the consent of the study participants for subsequent transcription. Relevant notes were taken during the interview to document key issues and observations.
Participant selection and recruitment
Inclusion criteria were being female, over 18 years of age, having a diagnosis of histologically-confirmed adenocarcinoma of the breast, and good mental status. To ascertain the reality of women with breast cancer, most of the patients recruited (80%) had been diagnosed in the past 5 years. Patients (20%) were added who had been diagnosed more than 5 years earlier, with the aim of improving the perspective and ascertaining their experience after 5 years.
Medical oncologists and nurses working at the centers helped identify patients who met the inclusion criteria. Participants went to the sites for follow-up between December 2019 and January 2021. Eligible women were informed of the study and invited to participate during an in-person visit by these healthcare professionals. Those who showed interest gave permission to share their contact information (e-mail or telephone number) with the principal investigator, who was the person who conducted all interviews. The principal investigator contacted these women, giving them a more detailed explanation of the study and clarifying any doubts they may have. If the woman agreed to participate, an appointment was made for a videoconference.
A total of 21 women agreed to participate voluntarily in this research. With the objective of accessing several experiences and bolstering the transferability of the findings, selection was controlled with respect to subjects’ stage of cancer, guaranteeing that there would be a proportional number of women with cancer in all stages, as well as with relapses.
Data analysis
The data underwent qualitative content analysis. To assure trustworthiness, analyses were based on the system put forth by Graneheim, and Lundman [ 40 ]. Interviews were transcribed and divided into different content areas; units of meaning were obtained and introduced into each content area; meaning codes were extracted and added; codes were categorized in terms of differences and similarities, and themes were created to link underlying meanings in the categories. All members of the research team (core team, two medical oncologists, three nurses and two psycho-oncologists) reviewed the data and triangulated the outcomes between two sources of data: qualitative data from the interview and non-modifiable information, such as sociodemographic (i.e., age, marital status, having children) and clinical (i.e., cancer stage and surgery type) data. Following this process, we reached saturation of the interview data by the time we had completed 21 interviews.
Ethical considerations
This study was performed in accordance with the ethical standards of the Declaration of Helsinki, and its subsequent amendments. The study was approved by the Research Ethics Committee of University of Barcelona (Institutional Review Board: IRB00003099) and supported by the Bioethics Group of the Spanish Society of Medical Oncology (SEOM) 2018 grant. All participants received a written informed consent form that they signed prior to commencing with the interviews and after receiving information about the study.
Patient baseline characteristics
In total, 21 women with a mean age of 47 years (range, 34 to 61) were interviewed. Most of the study population was married (66.7%), had a college education (66.7%), and had 2 or more children (42.9%). All cancer stages were represented, up to 23.8% tumor recurrence, and most of the primary cancers had been resected (95.2%) (see Table 1 ).
Description of the breast cancer patient journey
The women diagnosed with breast cancer describe the journey as a process tremendously affected by the different medical stages. Each stage has its own characteristics that condition the experiences, unleashing specific physical, emotional, cognitive, and social processes. Additionally, the patients perceive this entire process as pre-established journey they must undertake to save their life, with its protocols based on the type and stage of cancer.
“ People said to me , ‘What do you think ? ’ and I answered that there was nothing for me to think about because everything is done , I have to go on the journey and follow it and wait to see how it goes” (Patient 6)
Fig 1 displays the various phases of the journey that patients with breast cancer go through; nevertheless, each woman will go through some or others, depending on their type of cancer.

Throughout the entire patient journey
Processes of loss and reinterpretation of the new circumstance . What stands out the most in the process these women go through during the diagnosis and treatment of breast cancer is loss; specifically, the loss of health and a reinterpretation of the new circumstance and the new bodily reality. In the most extreme cases, the loss of health emerges with the fear of death that many women report at the time of diagnosis or during treatment, due to the distress generated. The loss of identity seems to be related to the evolutionary (existential) moment in which the woman is; there are patients who report feelings of disability or loss of attractiveness, or fear of not being able to get pregnant in the future, especially the youngest.
I felt a terrifying fear and thought , “You have cancer you tell yourself , you’re going to die tomorrow .” (Patient 6) I feel like after the hysterectomy , as a woman , I no longer have anything , only the physical . Sure , I look great , but I tell myself that it’s just a shell , the shell I inhabit , because as a woman , I only have one breast left . (Patient 6) At that moment , I had to make the decision that I was no longer going to be a mother . (Patient 14)
Personal change . Most of the women report that with the diagnosis of breast cancer, their life stands still and from that point forward, a different journey begins. The sole focus on this journey is the disease and its implications. During all those months, the patients stop working; they focus on their medical treatments, and reflect a lot on their current situation and on life. Most of the participants state, especially those who have already been discharged, that they know themselves better now; they take better care of themselves, and they enjoy their day-to-day and the small moments more, making the most of their time, with more initiatives and fewer trivial complaints.
Clearly , you’re not the same person you were before; I don’t think she’ll ever come back; your mindset changes completely and I have sequelae from all the treatments . (Patient 1) I re-think wasting energy on lost causes; what’s more , I’ve also learnt to say no . If I’m not in the mood to go somewhere , I just say no . (Patient 7) I take much more advantage of the present now , because you realize that things can change on any given day . (Patient 3)
Trust and appreciation for their physician . Most of the interviewees stated that they fully trusted the doctors who care for them, without question or objection to the treatments proposed. They reported that, as they go forward, they discuss the tests and treatments that are going to be performed, as well as possible side effects. Several stated that they are unaware of the stage of their cancer; similarly, most also do not know the benefits expressed in X% of the treatments. A few of the participants claimed that they did talk in detail about the different types of treatments with their oncologists, that they had sought another opinion, and one of them even reported having decided to stop chemotherapy, which was very hard for her, given her physician’s insistence that she continue.
The truth is that the oncologist didn’t say much about percentages; what she told me were the steps that I had to take; I thoroughly trusted her and she gave me a lot of peace of mind . (Patient 5) I told him , “I’m going to do whatever you tell me to . ” It never occurred to me to dispute whatever the oncologist might tell me . I was willing to do whatever was needed . (Patient 8)
Most of the women, at some point during the interview, state that they are grateful for the care they received and that, within the seriousness of their situation, there is a treatment for their condition.
I am super grateful for the treatment I’ve received and with the doctors assigned to me . (Patient 2) I’m very lucky; I’m only on my second line of treatment for metastasis and I’ve got a lot more ahead of me , but I consider myself lucky and I believe things are going very well . (Patient 20)
Role of the woman . We can see that the women adopt a role of care-givers and managers of their surroundings. They worry about the disease negatively affecting the people around them, which is why they make an effort to manage the family’s activity for when they can’t do it and they try to avoid being a physical burden or cause emotional distress to the people around them.
I was very strong ; I made everything easy for people , but making it very easy , doesn’t mean that it was easy for me , but that I made it easy for everyone . (Patient 8) I didn’t want to worry anyone because that’s just the way I am , I push forward and that’s that . (Patient 5)
Support network . In all cases, the family appears to be one of the elements that is most involved in the disease process. Within the family, the partner deserves special mention. The testimonies in this regard reveal a wide spectrum of possibilities that range from the feeling of having had great support to a lack of attention and understanding that, in many situations, causes the relationship to be strained or to end. Friends tend to appear more occasionally.
I can’t complain about my husband; he was up to the challenge , very attentive toward me and he fully understood how I was feeling ; I felt very supported . (Patient 14) We’ve had a period of a lot of arguing; I’ve had to sit down with him and tell him that life had changed for me . (Patient 18) I had a partner I had lived with for five and a half years and he told me , literally , that he looked at me like a little sister , no longer as a woman , and he left me , and that hurt me tremendously . (Patient 6)
On the other hand, many patients commented on the importance of social media, where they have met people in the same situation as them. They report feeling understood and in good company; likewise, they commented on the importance of being able to share their doubts and get to know about other experiences.
It’s a situation that only someone who has gone through can understand; you can have all the good intentions in the world , but if you haven’t gone through it , you can’t even begin to understand . (Patient 8)
Use of complementary treatments . Most patients follow conventional medical treatment. However, many resort to other disciplines that help them improve their quality-of-life, like dietary changes, getting more exercise than usual, visits to a psychologist or physical therapist, or using other integrative therapies, such as acupuncture, yoga, reiki, flowers of Bach, homeopathy, cannabis, or meditation.
I started to read a whole bunch of books to see what I could do to take care of myself in terms of nutrition and exercise ; you consider everything you can do . (Patient 5)
Diagnosis/unmasking
This phase encompasses the time from when the woman detects some symptom or goes to a check-up until the medical diagnosis is made. For the woman, this is a time of a series of tests and results. We have observed that the procedures, especially the healthcare professionals that deal with the patients, and the timing vary, depending on the medical center where they are being cared for. Emotionally, this is one of the most complicated stages.
Emotional whirlwind . The wait to obtain test results has a huge emotional impact for the women, given that it is a time of great uncertainty and fear.
An entire month with all the anguish of finding out if you have something . (Patient 3) The worst part is waiting 15 days to find out the magnitude of the tragedy , if it’s throughout your entire body or only in your breast; you go through a brutal emotional whirlwind; the wait is horrible because there’s nothing else you can do , so that anguish that you carry inside is dreadful; it was hell for me . (Patient 10)
Additionally, the interviewees described many other emotions that included fear of death, fear of having no time, feeling of unreality, rage, anger, sadness, avoidance, denial…
The first thing I thought was that I was going to die and that I wouldn’t finish watching my children [grow up]; my father had died of lung cancer 25 years ago . (Patient 9) My only aim was to get back to normal , as if there were nothing wrong . (Patient 4) You have a lot of conflicting feelings; you wish this weren’t happening; you want to run away , but you say , “Where am I going to run to ? ” . (Patient 14)
Impact of medical communication . Several women comment that, when given the diagnosis, they dissociate because of the emotional impact and that they don’t listen to all the information that the medical professional is giving them.
I remember that she talked and talked , but I didn’t know what she was saying until she said , “Isabel , you’re going to be cured , okay ?”. (Patient 9)
During the diagnostic testing, the women are highly sensitive to the healthcare professionals’ words and gestures.
I looked at the face of the person who was doing the mammogram and that’s when I started to imagine the worst . (Patient 20) I say to them , “ But , is there a solution to this ? ” , and they say to me , “Don’t worry , I’m sure there is a solution . ” That “sure” is etched in my mind . (Patient 10)
Communication and managing their surroundings . After the diagnosis, the patients feel that they have to tell the people around them about their situation, especially those closest to them, the family. They all agree on how hard it is to share. Normally, the people it’s hardest to tell are their mother and their children. When they do, they try to put the most positive spin on it possible, in an attempt to keep them from worrying.
You no longer think only about yourself , you think , “Good grief , now I’ve got to tell my mother .” It’s hard . (Patient 16) I wanted to tell my kids the way I say things , always trying to look for the upside , and positive , although it was hard , but , anyway , in the end , it went well . When I finished , my husband told me , “You’ve convinced me that it’s no big deal .” (Patient 9) I told my son , “Son , don’t cry , your mom’s going to get over this , this is nothing .” (Patient 1)
During this period, the women contemplate how their situation will affect their surroundings and they try to organize it as much as possible.
I devoted myself to planning everything , to organizing what to do with my daughter , and to thinking about work , too , how I had left things at work . (Patient 4)
Surgery/cleaning out the cancer
Uncertainty and fear . The participants express that before going into surgery, they are told about the kind of procedure that will be done, but that, depending on what they find and the analysis, it may change. In light of this, they exhibit an enormous feeling of uncertainty and fear. In addition, many voice concern about how the surgery will go.
They tell you conservative surgery , but if we open up and see something we didn’t see on the tests , then everything could change . (Patient 10) Aside from the anesthesia , that I’m terrified of , you spend several hours in surgery and you don’t really know how things will go; when they clean it out , they analyze it , and you go into the operating room and you don’t know what can happen . (Patient 9)
Feeling of loss . Considering that the breast is associated with an intimate, feminine part [of their body], many women experience the operation as a loss. This loss is more acute if the operation is a mastectomy and there is no reconstruction at the same time. The loss also involves a loss of identity, compounded by the side effects of chemotherapy, such as hair loss. The interviewees who had undergone mastectomy say that following surgery, when the bandaging is removed and the scar is revealed, is one of the most critical moments, which is why they express difficulty in managing it and appreciate the caring assistance from the professionals.
It is identification with yourself , you know , it’s what you’ve seen in the mirror , what you think you’re like and , suddenly , you’re no longer like that; there’s an incredible personal crisis because you no longer recognize what you’re seeing . (Patient 11) I closed my eyes and I removed the bandaging and I didn’t dare look … with my eyes , I imagined the worst . (Patient 12)
Acceptance or demand for more aggressive intervention . The patients perceive the surgery as essential to recovering their health, which is why the process is widely accepted. Some patients who demand a more invasive intervention, normally a bilateral mastectomy, do so because that way, they feel safer with respect to a possible relapse, as well as more comfortable esthetically.
If they have to remove my breast , let them take it; what I want is to get better . (Patient 16) They say that I am in full remission , so they only removed the lump , but at first , I said that I wanted my whole [breast] removed ; then they assessed how to do it . (Patient 13) They told me that I had a genetic mutation and more possibilities of developing breast cancer and , since I felt such rejection toward my remaining breast , I decided to get rid of that one , too . (Patient 20)
Chemotherapy/loss of identity
The chemotherapy phase is one of the phases that affects the women’s lives the most, because of its physical impact and how long it lasts. No differences have been found in how they experience chemotherapy depending on whether it was neoadjuvant or adjuvant.
Negative impact of side effects . Chemotherapy is associated with many side effects that vary from one woman to another. Many indicate that they have suffered physical discomfort, such as fatigue, dysgeusia, pain, nausea and vomiting, mucositis, diarrhea, etc.
One day when I didn’t want to go to bed , I went to bed crying because I had the feeling that I wasn’t going to wake up . That day it was because I felt awful . (Patient 1)
Furthermore, all of the women suffer hair loss, which is one of the most-feared effects. Likewise, their body hair also falls out, especially on their face, and their weight fluctuates. All of these changes lead to a loss of identity that is experienced as taking away from their femininity. It must be remembered that oftentimes, chemotherapy is administered after surgery, further exacerbating this physical change. On top of all that, several women comment having to decide at the beginning of treatment whether to freeze their eggs or not; at that moment, many of them forfeit the possibility of becoming a mother or of becoming a mother again, which also adds to this loss of femininity.
Losing my hair was hard , but when it grew out again , I had an identity crisis . I didn’t recognize myself; people said I was really pretty like that , with my hair so short . I looked at myself in the mirror and I said that I’m not that woman , I can see that that woman is pretty , but it’s just that I don’t recognize myself . That’s not me or , it was like , I looked at myself and I didn’t recognize myself . That’s when I suffered a serious identity crisis , psychologically serious , but also serious because I sobbed because I looked at myself , but it wasn’t me . (Patient 6) Where’s that sexy lady , where is she ?, because you don’t feel good . I didn’t like myself at all . I was several sizes larger and I looked at myself and said , “What a monster . ” I didn’t feel good about myself . (Patient 1)
Many patients say that chemotherapy decreases their libido and dries up their mucous membranes, which is why they prefer not to have sex. For those who live as a couple, this situation can strain the relationship.
Sexually , I just didn’t feel like it , I wasn’t in the mood; not only did I not feel like it , my mucous membranes were dry and , what’s smore , I just couldn’t , I couldn’t , I felt bad for my husband , but he said , “Don’t worry .” (Patient 16)
Finally, some interviewees expressed a feeling of being poisoned by the treatment. These women tend to be highly focused on taking care of their body and have a very natural attitude toward life.
I had to really work my awareness that I was poisoning myself; at night I was at home and I thought that all that red liquid was circulating through my veins … I think I even had nightmares . (Patient 4)
Balance between caring for oneself and caring for others . The patients feel that it is time to take care of themselves, so they prioritize resting when they need it. Moreover, they worry about getting a haircut and, most of the times, they look for turbans and wigs. Some also learn how to put on make-up, which they rate as being very positive. On the other hand, those who have children or another person in their care, try to take care of them as much as they are able.
Around 11 : 00 , I no longer felt good , so I’d go to the armchair to rest and it’s like I had an angel , because I’d wake up a minute before I had to set the table and get lunch for my son who would be coming home from school . (Patient 1) While I was getting chemo , I went with the gadget and I told myself , “I’m going to teach you to apply make-up; for instance , your eyelashes are going to fall out . Make a line like this ” and at that moment when you look in the mirror , and we look like Fester in the Addams family . (Patient 13)
Vulnerability . The women experience great uncertainty and feelings of vulnerability the first times they receive chemotherapy, since they don’t know what side effects they will suffer.
With chemo , I started with a lot of fear and , later on , I became familiar with it little by little until the time comes when you go to the hospital like someone who’s going to pick up a bit of paper . (Patient 9)
In addition, those participants who join a social network or who are more closely tied to the hospital setting, know about the relapses and deaths of people around them diagnosed with breast cancer, which makes them feel highly vulnerable.
There are some people who leave the group because … it’s not like there are a lot of relapses and , geez , I think that it messes with your head . (Patient 13) We were almost always the same people at chemotherapy ; there was one guy who was really yellow who looked terrible and , there was one time when we stopped seeing him and another lady asked and the nurse said that he had died . (Patient 15)
At the same time, given the physical changes, especially those that have to do with body hair, many women feel observed when they leave home.
If I have to go out and take off my scarf because I’m hot or go straight out without any scarf on my head and whoever wants to look… let them ; I think that it’s up to us , the patients , to normalize the situation; unfortunately , there are more and more cases . (Patient 9)
Telling the kids . Since when the chemotherapy stage is going to entail many physical changes, the women look for ways to talk to their children about the treatment. Most of them comment that it is a complicated situation and all of them try to talk to their children in such a way as to protect them as much as possible.
I asked the nurse for help before I started chemotherapy to see if she had any pointers about how to talk about this with the kids and she recommended a story , but when I saw it , I didn’t like it … so , in the end , I decided to do it off the cuff . (Patient 10)
Radiotherapy/transition to normality
The “last” treatment . When the patient reaches radiotherapy, normally, they have already spent several months undergoing physically aggressive medical procedures, which is why they feel exhausted. There is a physical exhaustion resulting from the previous treatments and made worse by the radiation therapy. Furthermore, many women also report feeling emotionally drained by the entire process. However, this is generally accompanied by joy and relief because they feel that they are in the final stage of treatment.
Emotionally , it’s a marathon that has to end up at some point . (Patient 10) For me , radiotherapy was like a lull in the battle , with a winning mind-set . (Patient 4)
Comparison with chemotherapy . There is a widespread perception that radiotherapy has fewer side effects than chemotherapy, although later, when they receive it, several patients suffer discomfort, above all fatigue and dizziness. Several report that at this point, they are mentally worn out and just want to be done with the process, which is why they have less information than about chemotherapy.
I feel like radiotherapy is unknown , that you think it’s more “light ” and it turns out not to be so light . (Patient 13)
Follow-up care/the “new” day-to-day
Difficulty in getting back to normal . Once the patients are discharged, many feel that they need some time to recover, that it will be slow, in order to restore a more normalized pace of life. They are still working on their emotional and personal process.
When they tell you that you have cancer , they make it very clear : you have a goal; you have some months of chemo , some months of radio , and when you finish , you say , “And now , what do I do ?”. I say that because now I have to get back to my normal life , but I don’t feel normal . I still don’t feel cured , I’m not 100% . And you’re glad you’ve that you’ve finished it all and you’re alive , but at the same time , you say , “Gosh… this is very odd . ” It was a very strange feeling . (Patient 8)
Most patients report that their quality-of-life has diminished, due to the sequelae from the treatments. Lymphedema is one of the sequelae they name most often, although they also mention other symptoms, like digestive upset, weight issues, eye problems, scar pain, etc. The women who are on hormone therapy also suffer side effects, such as joint and muscle pain.
I have lymphedema and , although I have good mobility , I’m a little bit weak; when I go out for dinner , I generally order fish , because I can’t always cut meat well . (Patient 6)
Several interviewees also express difficulty in their affective-sexual relations. Many of them feel insecure because of all the physical changes; others have sequelae that hinder their relations, and still others are suffering symptoms of early menopause. This can cause problems in the couple and for those who don’t have a partner, suffer many complications when it comes to meeting other people.
I haven’t had sex with my husband for 2 years because , it’s also really complicated to get over; I’ve gone for pelvic physical therapy; I’ve used gels , but nothing works . (Patient 8) It’s taken me many months for me to have a relationship again; it’s been really hard because , even though everyone told me that I looked fine , I didn’t feel fine . My breast cancer had taken away all my attributes as a woman . (Patient 6)
Some women also experience difficulties when it comes to returning to work. Several state that they had been fired when they went back. They also report that when interviewing for a job, it’s complicated for them because they have to explain what happened and they mention the schedule of doctor’s visits that they have. Other women comment that they’ve been given early retirement or disability.
You go to the interview and if you tell them that you’ve had the disease , they look at you like you’re a weirdo . (Patient 13)
Breast reconstruction . How reconstruction is experienced, as well as its timing, are highly contingent upon they type of reconstruction. Each one has its pros and cons, but the opinions collected with respect to the type of reconstruction have been positive.
Although it took 18 months for the entire process to be over , I’m delighted with reconstruction with the expander . (Patient 16)
Some patients state that after the whole process, which has been long and complicated, they prefer not to undergo reconstruction immediately. In these cases, they report having felt a subtle pressure from the outside to undergo reconstruction.
Every time I went for my check-ups , they said , “You’re the only one left [who hasn’t undergone reconstruction]” and in the end , the truth is that I’m really happy because I think I look pretty . (Patient 12)
Check-ups and fear of relapse . Check-ups are one of the times that generate most worry and insecurity. The women remark that, starting a few days before and until they receive the results of the follow-up studies, they are more anxious about the possibility of relapse.
At every check-up my legs start shaking again and my stomach is in knots, although at my last one, everything turned out okay and I’m thrilled. (Patient 6) During the first stage , I did everything I had to do and I got over it , but it’s a lottery . You can do whatever you want , but it’s the luck of the draw and when you start going for check-ups , it’s like going to play Russian roulette . (Patient 8)
Maintenance hormone therapy . Hormone therapy is understood differently depending on age and on the major decision of whether or not to be a mother or to have another child. If the woman does not want to have more children, the treatment is accepted better. The patients who take it also report effects derived from menopause, for instance, joint pain or dry mucous membranes.
I did notice joint pain , but since I exercised , [I felt it] much less than my fellow women , although , for instance , when it comes to getting up from a chair , you get up like an old lady . (Patient 10)
Position of support . Several patients mention that, after discharge, they stay active on social media, they volunteer when they find out about someone or to participate in activities related to breast cancer, with the aim of being able to help other people who are in this situation.
It’s really good to meet other people who are going through the same thing , so , now that I’ve finished , I like it and I always help whenever I can , because I can share what was good for me . (Patient 13)
Relapse/starting over
Emotional impact . The diagnosis of a relapse is experienced much the same as the initial diagnosis. All of the women report fear, although they also state that they are more familiar with the processes. Other emotions emerge, such as why me, blame, disbelief, etc.
Since they had told me that it wasn’t going to happen again , I believed it , of course , I wanted to believe it and it totally surprised me; I couldn’t stop crying and crying . (Patient 17)
Telling the family again . Patients repeat that telling the family about it again, especially the children and parents, is tough and they try to minimize it in an attempt to protect them emotionally.
On the very same day that I had my mammogram , my mother says that she wants to come a see the kids . We’re in the park , when she arrives , I have to tell her that everything’s fine and when we get home , I tell her everything . My mother’s devastated again and I tell her not to worry , that everything is going to be fine . (Patient 16)
Thinking about whether something could have been done differently . Several women comment that, after their relapse, they think about whether the treatment was enough or there must have been something they could have done to avoid the relapse.
You get furious , because you say , “I wasn’t supposed to get sick , because if , 2 years ago when the first microcalcifications appeared I had had them removed , then I wouldn’t have metastasis , or maybe I would . (Patient 19)
Metastatic breast cancer/time-limited chronic
Re-interpreting the concept of metastasis . Most of the participants in this stage state that they have had to give new meaning to the word, “metastasis,” since their first perception was directly related to death. In this way, they come to understand that cancer can become chronic, although they now have to take medication and go to the hospital on a regular basis. Nevertheless, they know that their life expectancy may be a few years. The women who are involved in a group point out how hard it is to see their fellow member pass away.
What I now call my “ new normal” consists of lots of visits to the hospital and never going back to work . (Patient18)
They also state that at this stage, they do not identify with the disease generally known socially as “breast cancer”, where there is great emphasis placed on early detection and on their chances of being cured. This causes them to feel more isolated.
These pink ribbon campaigns hurt us because they tend to underscore that everything is going to turn out fine because breast cancer has a very high cure rate; there is huge lack of awareness . (Patient 20)
Physical and emotional discomfort . Most of the women in this stage report side effects from the treatments, although some comment that good quality-of-life can be preserved. On an emotional level, they say that they sometimes feel a certain agony due to not knowing how much longer the treatment will be effective. They live in a state of uncertainty that they try to cope with by focusing on their day-to-day and experience the good times deeply.
When I’m not in pain , I try not to even remember what I have and go out and have fun with my family and live . (Patient 20)
Several women who have children express with regret that they worry about their children enjoying them and remembering them when they were well. They are sad that they won’t be able to grow up in a normal family. Some also comment the impact this diagnosis is having on their partner.
What I don’t want is for them to carry this baggage of having a sick mother . (Patient 18)
A conflict with disability also appears, as many women report their desire to continue working, but feel that they can’t keep up with the pace of work. Additionally, several state that going through the medical board is a strenuous process, given that they look good physically.
It’s hard to deal with , I’m a non-practicing lawyer and I have degrees galore , but I worked the first year and I couldn’t continue . (Patient 21) Every year they call me again for the disability monitoring and they always threaten me . To be honest , the treatment doesn’t make me sick , but I don’t know how long it’s going to be like this . (Patient 19)
Social invisibility . The participants say that they do not have any physical signs of being ill, that they look fine, although they know and feel that inside, they are not well. They say that it is sometimes hard to manage socially, since on occasion, they feel misunderstood and disparaged.
I’m much sicker now , but people think or want to think that I’m fine . When I was doing chemo , it was like wearing a sign that said “cancer . ” (Patient 17)
This study describes the patient journey of women with breast cancer, specifying the different phases with the most relevant aspects of each, as well as the different cross-sectional features they report throughout the entire treatment process.
The results portray breast cancer as a process in which there is a striking feeling of loss of health and self-identity, changes in routines, personal and employment transformation, as well as emotional hardship during and after breast cancer treatment, aspects that are also reported in the literature [ 41 , 42 ]. Earlier studies state that experiencing cancer is highly stressful. It involves a major threat to life or physical integrity, in addition to mental health, interfering with the path, projects, and plans patients have for their life over the short, medium, and, on occasion, long term as well [ 6 ]. Along with reporting adverse physical and psychological impacts, patients also report positive ways in which they have grown psychologically or emotionally from the experience [ 7 , 42 ]. The diagnosis of breast cancer not only impacts the women individually, but also affects their surroundings. As reported in the literature, despite going through a very challenging time, the women struggle to put on a positive face and attempt to conserve the family’s well-being, specifically that of their children [ 7 ]. At the same time, the family is a fundamental source of support and usually provide indispensable support; however, it is not always effective, because family members do not fully understand the stresses involved in living with cancer [ 43 ]. Previous studies also reveal that for some women, their partners are one of their most significant supports; nonetheless, research also suggests that a cancer diagnosis predicts marital breakup more strongly for female survivors than males [ 44 ]. Our results reflect that the women frequently resort to other women in the same situation, possibly because they face significant unmet supportive care needs [ 30 ]. The need for social support may lead patients to seek social support groups consisting of people who are experiencing similar health crises, because such groups allow them to interact with those who best understand their suffering [ 43 ]. Another aspect that appears across the board is the relationship the participants have with the medical team. In this study, we have noted their trust in the medical team and acceptance of the treatments proposed without going into the clinical data of the disease and without needing to know the benefit provided by the treatment. Cancer patients are confronted with a potentially life-threatening [condition], feeling vulnerable, and need to rely heavily on their care providers, expecting the physician to act in their best interests [ 5 ]. Therefore, they need to have a close relationship, as well as comprehensive care [ 30 ]. Patients’ trust in a physician has been associated with a reduction of their fears and anxiety and [increased] satisfaction and adherence to treatment [ 5 , 30 ]. We believe that it would be important to provide patients with accurate information, so as to avoid misunderstandings (such as cancer being synonymous with death, regardless of stage) as several participants in this study have reported, which can lead them to believe that the risk of relapse with and without chemotherapy is much greater than the oncologists estimate [ 45 ]. We believe that in future studies that it would be worthwhile to examine the peculiarities of each kind of patient information with the aim of determining how to break it up and make it both comprehensible and tolerable to promote patients’ well-being.
A breast cancer diagnosis is generally unexpected and practically all patients suffer psychological distress, such as feelings of uncertainty, disbelief, hopelessness, vulnerability, anger, fear, anxiety, and sadness [ 46 , 47 ]. The literature has reported that many women experience peritraumatic distress or dissociation during the medical conversation in which they are given their diagnosis of cancer [ 48 ], which might account for the reactions of the respondents. Given that, when they receive their diagnosis, additional information is generally given to them, such as clinical aspects and preferred treatments. Repeating this information at subsequent appointments could contribute to improving communication with patient, since several participants stated that they found it hard to pay attention to the physician, given the emotional impact. Additionally, breast cancer patients tend to be diagnosed when they are relatively young, and often when they are in the middle furthering their career or raising children [ 12 ]. In spite of everything, the women try to put on as brave a face as they can and focus on maintaining their children’s well-being [ 7 ]. Telling children about their diagnosis is reportedly one of the biggest challenges; parents are usually unsure of how to tell them, because at the same time that they want it to be open and honest and cover their children’s developmental needs, they also want to protect them children [ 49 ].
Once diagnosed, breast cancer patients go through different treatments. The most salient experiences of these phases pertain to the impact of side effects on physical quality-of-life and psychological well-being, which is consistent with the literature [ 11 ]. Moreover, cancer therapy entails physical changes that affect their feminine identity, fertility, self-esteem, sexual functioning, and makes them more vulnerable [ 10 , 50 ]. Women described their inner self as being on an emotional rollercoaster with highs and lows throughout the various phases of treatment [ 7 ]. Given treatment side effects and sequelae, these women are more likely to experience physical symptoms and psychological disorders than patients with other kinds of tumors [ 51 ]. The side effects involve an acute sense of loss of health and quality-of-life, as well as identity and femininity. It would be interesting for future research to explore the therapies used in grief counseling with cancer patients, as understanding and exploring this perspective could comprise an additional clinical aid.
Once the women have completed their treatments, they gradually get back to normal and many contemplate returning to work. However, in line with our results, the literature reveals that even though they want to normalize their lives, female breast cancer survivors feel that they will never return to their baseline status [ 7 ]. A significant number of patients experience difficulties in physical, cognitive, and emotional functioning after their treatment, such as symptoms like lymphedema, fatigue, pain, sleep disorders, cancer-related cognitive impairment, emotional stress, symptoms of depression and anxiety, problems with relationships, reduced sexual identity, fertility problems, and fear of cancer relapse [ 13 , 14 ]. Furthermore, patients with hormone therapy suffer hot flashes, sweats, joint pain, weight gain, decreased libido, and low energy [ 52 ]. A sizeable number of these women also experience changes in employment status which can happen even 5–10 years following diagnosis [ 15 ]. Given that all these changes alter the structure of the woman’s everyday life, personalized care and treatment plans in cancer survivors are highlighted in the literature with extended specialized support being proposed that enables them to make a better psychosocially adjusted transition from treatment to follow-up [ 53 ] and advocating for the patient’s participation in all decisions that affect her during this period [ 54 ]. Further research is needed concerning how to structure the follow-up and support offered to these women during this stage so as to meet their needs and help them adjust to their new reality with the chronic sequelae caused by cancer and its treatment. On the other hand, the personal transformation of the initial stages of the journey are best seen during this phase. The literature shows that women who have had breast cancer report changes in their philosophy of life, such as embarking on a new life path, changing their priorities in life, as well as valuing life in general [ 42 ]. Most of the participants in our study place special emphasis on appreciating life, enjoying it more, and living each day to the fullest. Cancer survivors report being aware of how precarious life is, while also feeling the joy of being alive [ 55 ]. Similarly, they have been found to be more resilient and better able to repair their mood than healthy women [ 56 ].
About 5% of all patients with breast cancer are diagnosed when the disease is metastatic, whereas some 30% have suffered a relapse of an early breast cancer [ 17 ]. We saw that some women suffering a relapse after initial treatment with curative intent tend to wonder if the treatment was sufficient or if they should have done something more to prevent the relapse. Metastatic breast cancer is uncurable, which is why these women’s main psychosocial challenges are not the same as those who are diagnosed in early stages [ 18 ]. Faced with incurability, the women react with shock and fear of imminent death, but this anxiety diminishes once they begin treatment and learn that there are more treatment options [ 17 ]. During this phase, the interviewees reported impaired physical QoL and functioning, being hindered by pain, fatigue, or menopausal symptoms. Emotionally, they report suffering bouts of depression and anxiety, as well as fear because of the spread of their cancer. As for their relational QoL, their children’s welfare is their number one concern, especially for mothers of young children [ 17 , 57 ]. What’s more, these women felt isolated from society in general and, more specifically, from the non-advanced breast cancer community, inasmuch as they feel that nobody understands what they are going through [ 18 ]. A psychosocial approach is especially important in this phase to help these women to continuously adapt to the changes of their individual clinical situation and to the progression of the disease, thereby improving their coping.
Clinical implications
Having first-person information enables us to comprehend in detail the experiences of breast cancer patients, their situation, and emotional state, which favors holistic cancer care for health professionals.
Healthcare professionals should prepare women for a changed life situation, as well as to face prolonged, multimodal treatment (surgery, chemotherapy, hormone therapy, radiotherapy), and to confront physical and psychological sequelae, as well as the fear surrounding an uncertain prognosis. It is important to help them manage their expectations and fears and, to identify and address the issues and concerns that arise at different time points during treatment. The information and support offered should be adjusted to each woman’s individual needs, her life situation, her coping style, and the time and stage of their cancer. This more empathic, understanding outlook can also contribute to improving the physician-patient rapport, promoting communication, understanding, and shared decision-making.
Finally, a comprehensive understanding of the women’s psychosocial support endorses their belonging to groups of women with breast cancer, in which there is a relationship among equals. Further research is needed to specify the type needed so as to decrease both the impact of the death of women in the group, as well as the vast amount of information that they may end up obtaining, without needing it or requesting it.
Limitations
This study was performed with Spanish participants, which is why certain aspects cannot reflect the experiences of breast cancer patients from other countries, given the particularities of both the Spanish healthcare system and Spanish culture. Likewise, the data attained were specific to women with breast cancer, which can scarcely be extrapolated to individuals with other cancers. Moreover, the findings do not reflect men’s experiences with breast cancer and research with this group would enrich the field further. In addition, the age of our participants ranged from 34 to 61 years; hence the results should be interpreted for a middle-aged population and do not reflect the experiences of women diagnosed at very early or very old ages. Finally, we believe that there may be a bias regarding the women who agree to participate, as this group has probably accepted their condition more, as well as having worked on it more.
Despite these limitations, we hope that our findings can contribute to better understanding the experiences of women with breast cancer.
Acknowledgments
The authors are grateful to the investigators of the Neoetic study and the Bioetic Group of the Spanish Society of Medical Oncology (SEOM) for their contribution to this study. We would like to thank all the women who generously shared their experiences with us, the support of HealthyOnco ( www.healthyonco.com ), and Priscilla Chase Duran for editing and translating the manuscript.
Funding Statement
This work was funded by the Spanish Society of Medical Oncology (SEOM) in 2018. The sponsor of this research has not participated in the design of research, in writing the report, or in the decision to submit the article for publication.
Data Availability
Ascertaining breast cancer patient experiences through a journey map: A qualitative study protocol
Affiliations.
- 1 Clinical Psychology and Psychobiology Department, Faculty of Psychology, University of Barcelona, Barcelona, Spain.
- 2 Medical Oncology Department, Hospital Universitario Central of Asturias, Oviedo, Spain.
- 3 Social Psychology and Quantitative Psychology Department, Faculty of Psychology, University of Barcelona, Barcelona, Spain.
- 4 Medical Oncology Department, Hospital Universitario Clínico San Carlos, Madrid, Spain.
- 5 Medical Oncology Department, Complejo Hospitalario Universitario de Orense, Orense, Spain.
- 6 Medical Oncology Department, Hospital Universitario La Paz, Madrid, Spain.
- 7 Medical Oncology Department, Hospital General Universitario de Elche, Elche, Spain.
- 8 Medical Oncology Department, Hospital Universitario Fundación Alcorcón, Madrid, Spain.
- PMID: 33347475
- PMCID: PMC7751958
- DOI: 10.1371/journal.pone.0244355
Background: The current cancer care system must be improved if we are to have in-depth knowledge about breast cancer patients' experiences throughout all the stages of their disease.
Aim: This study seeks to describe breast cancer patients' experience over the course of the various stages of illness by means of a journey model.
Methods: This is a qualitative descriptive study. Individual, semi-structured interviews will be administered to women with breast cancer and breast cancer survivors. Patients will be recruited from nine large hospitals in Spain and intentional sampling will be used. Data will be collected by means of a semi-structured interview that was elaborated with the help of medical oncologists, nurses, and psycho-oncologists. Data will be processed adopting a thematic analysis approach.
Discussion: The outcomes of this study will afford new insights into breast cancer patients' experiences, providing guidance to improve the care given to these individuals. This protocol aims to describe the journey of patients with breast cancer through the healthcare system to establish baseline data that will serve as the basis for the development and implementation of a patient-centered, evidence-based clinical pathway.
Publication types
- Research Support, Non-U.S. Gov't
- Breast Neoplasms / psychology*
- Breast Neoplasms / therapy*
- Cancer Survivors / psychology*
- Patient Outcome Assessment
- Patient-Centered Care
- Qualitative Research
- Standard of Care
- Surveys and Questionnaires
Grants and funding
- About Breast Cancer
- Find Support
- Get Involved
- Free Resources
- Mammogram Pledge
- Wall of Support
- In The News
- Recursos en Espa ñ ol
- National Mammography Program
- Patient Navigator Program
- Metastatic Retreats
- Support Group
- Breast Health Education
- Breast Cancer Awareness in the Workplace
- Breast Cancer Research
Patient Navigation Program
Through our partner facilities, we provide patient navigation services to help women navigate the complex cancer care system.
Patient navigation helps guide patients through and around barriers in the complex cancer care system to help ensure timely diagnosis, treatment, and support. This is also critical to survival and early detection, and the medical community in the U.S. is seeing huge successes through patient navigation programs.
The NBCF Patient Navigator Program is a proactive approach to helping patients overcome the barriers of cost, fear, and misinformation surrounding a disease and its prevention. By helping underserved women to navigate the healthcare system, navigators provide the vision that gives women hope.

Services that navigators provide include:
- Education and outreach in the community
- Guidance through screening and diagnostic exams
- Support through treatment and survivorship
- Assistance with financial, administrative, and emotional issues
NEW! Patient Relief Fund
In collaboration with our hospital partners, NBCF has created the Patient Relief Fund to help ease the cost of breast cancer treatment, making it easier for patients to focus on survivorship.
Help support women in need
Donations are always appreciated, but there are lots of great ways to get involved.
We use cookies on our website to personalize your experience and improve our efforts. By continuing, you agree to the terms of our Privacy & Cookies Policies.

- Center on Health Equity and Access
- Health Care Cost
- Health Care Delivery
- Value-Based Care
Patient Journey Amid Breast Cancer Diagnosis
A panel of medical experts explore the impact of breast cancer diagnosis on patient quality of life and how the patient journey is navigated.

EP: 1 . Clinical Presentation of Patients Diagnosed with Early Breast Cancer
Ep: 2 . patient journey amid breast cancer diagnosis, ep: 3 . unmet needs in breast cancer treatment, ep: 4 . navigating updates in breast cancer treatment paradigms, ep: 5 . determining optimal treatment pathways for patients diagnosed with breast cancer, ep: 6 . biomarker testing in patients with hr+/her2- early breast cancer, ep: 7 . payer considerations for selecting breast cancer medications, ep: 8 . navigating adverse events and promoting treatment adherence for patients receiving treatment for breast cancer, ep: 9 . managing patients with cdk 4/6 inhibitor-resistance, ep: 10 . early breast cancer and value-based care, ep: 11 . opportunities in the early breast cancer treatment landscape.
Kirollos S. Hanna, PharmD, BCPS, BCOP, FACCC: Sarah, I’ll turn it over to you, I know in terms of quality of life you do a lot of work. How has the quality of life of a patient with breast cancer impacted diagnosis during their treatment journey? Are there things being done to help improve their quality of life? Obviously, one of the big things is that oral oncolytics have allowed us to treat cancer as a chronic disease state, but we know that it comes with a lot of burden. There is an adverse event profile these patients have to deal with and financial toxicities. What does that look like for our patients?
Sarah Sammons, MD : That’s a great question and something I feel very passionately about. Having a diagnosis of high-risk hormone receptor–positive breast cancer, which is what we’re talking about today, is life-changing. Women who are diagnosed often need to undergo chemotherapy if they are high risk from a node-positive standpoint, from a genomically high-risk standpoint. That comes with a lot of quality of life considerations. Alopecia has a dramatic impact on self-image. We have neuropathy and short-term cognitive changes that are incredibly difficult. And that’s what we manage probably every day in clinic, in our survivorship visits. We deplete their estrogen for a minimum of 5 years, and that has incredible implications on their quality of life in terms of sexual health, joint pain, and bone health. And ovarian suppression becomes a very important part of [the lives of] our young women [with high-risk disease]. We abruptly put those women into menopause. That has incredible implications on quality of life, and we can’t have enough research in that space.
Kirollos S. Hanna, PharmD, BCPS, BCOP, FACCC: Absolutely. And you brought up a great point about survivorship and what that looks like in terms of the patient’s course [of treatment]. I’ll tell you all this: My mother was diagnosed with triple-negative breast cancer probably 20 years ago, and she’s doing great, but you can see the adverse events that she has had to deal with, even post diagnosis, post mastectomy, all those kinds of things. So it’s an unfortunate complication. We see a lot of unfortunate complications from the disease, but as you mentioned, I think research in this area would play a significant role. What about in terms of the goals of therapy? Jay, you walked us through the early patient vs the metastatic patient, where we know we’re palliating that patient, not really a cure in sight. What are our goals of therapy? Obviously, from a survivorship perspective, there’s a goal there, but what about in their treatment journey? I know we said it’s a marathon that these patients are running. How does that look?
Jay Andersen, MD : Focusing on the early stage, which is the topic today, it is a journey, and I think every patient comes in frightened and overwhelmed. I think the primary goal they like to hear is that this is a curable disease. That’s the first thing we try to emphasize. Then we start unpacking what that means. For every case, it can be very different. If it’s a patient at low risk, they may have less therapy, of course. [A patient with] higher risk [may have] more complicated therapy. Every visit is a constant balance between that curative intent and managing the toxicities that were just mentioned. So it’s an ongoing, collaborative conversation. After they’re done with their acute management visits, oftentimes patients will transition to a survivorship clinic, and even then, the topics can be very engaging and complicated.
Sarah Sammons, MD : I totally agree. And a journey is one description. I’ve heard a patient describe early-stage and even advanced-stage breast cancer as more of a forced march. Not a journey that they really wanted to go through, but one they were forced to walk through. It’s constantly our job in the clinic to describe these risks and benefits. And risk and benefit ratios change for patients over time, so they continuously need to be reevaluated.
Kirollos S. Hanna, PharmD, BCPS, BCOP, FACCC: As their medical oncologists, are you finding, after you’ve achieved that goal of cure, [that you are] still seeing these patients on an annual basis? What does that look like, in terms of the longevity part of it?
Jay Andersen, MD : I tend to follow patients as long as they’re on therapy. So if they’re on hormone therapy, that’s at least for 5 years. Many of them [can be on it] up to 10 [years]. At 10 years I talk about graduation from clinic and I give patients the option. Everyone’s different. Some patients are like, “I am ready to be done with this and never come back,” and I’m OK with that at that point. Other patients feel comforted with some ongoing monitoring. I may transition them to annually, for example.
Kirollos S. Hanna, PharmD, BCPS, BCOP, FACCC: Sam or Heather, is anything different on your end from a monitoring perspective after they’ve graduated? Do they graduate from your clinics?
Heather McArthur, MD : I think it’s up to patient comfort. I adhere to the American Society of Clinical Oncology clinical follow-up guidelines. So I see patients every 3 to 6 months for the first 3 years, and then less frequently thereafter. After 5 years, I see them once a year. And then, after they’re completing their adjuvant therapy, I typically transition them. We are establishing at our site a survivorship and surveillance program that’s run by advanced practitioners, which I think will provide that comfort that a lot of our patients want, because they want to continue to be within the system and have that constant contact but don’t want to be waiting because we are running late from seeing chemotherapy patients. So we want to strike that balance of ensuring that they have an appropriate follow-up, but that the follow-up doesn’t detract from their quality of life as well.
Samyukta Mullangi, MD, MBA : On a similar note, I would also say that we always encourage our patients to plug in with their primary care physicians to really give them the holistic, comprehensive assessments that we just don’t do in a focused way in the breast cancer world. I think oftentimes folks feel such affinity toward their breast cancer oncologist that they want that person to become the guidepost for all aspects of their care, but we’re just not trained to do that.
Heather McArthur, MD : I’m Canadian and we did a study in Canada looking at follow-up, addressing that specific issue, primary care physician follow-up vs specialty follow-up, and patients did equally well if they had a primary care follow-up plan.
Kirollos S. Hanna, PharmD, BCPS, BCOP, FACCC: I think a lot of my medical oncologists practice particularly in the community setting, so they’re seeing all comers. They’ll walk in through their doors and some of my medical oncologists will joke and say, “We become a generalist as well, or a primary care physician,” because they end up caring for everything else for their patient, their blood pressure, cholesterol, and everything else that goes on that we sometimes see.
Transcript edited for clarity.

- Remember me Not recommended on shared computers
Forgot your password?
The Lancet Breast Cancer Commission (15 April 2024)
- PUBLISHED 2 hours ago
- TYPE Data, research and analysis
- CONTENT TYPE Pre-existing
- COPYRIGHT STATUS Creative Commons
- PAYWALLED No
- ORIGINAL AUTHOR Various
- ORIGINAL PUBLICATION DATE 15/04/24
- SUGGESTED AUDIENCE Everyone
- Medicine - Oncology
- Womens health
- Health inequalities
- Health Disparities
Despite tremendous advances in breast cancer research and treatment over the past three decades—leading to a reduction in breast cancer mortality of over 40% in some high-income countries—gross inequities remain, with many groups being systematically left behind, ignored, and even forgotten. The work of the Lancet Breast Cancer Commission highlights crucial groups, such as those living with metastatic breast cancer, and identifies how the hidden costs of breast cancer and associated suffering are considerable, varied, and have far-reaching effects. The Commission offers a forward-looking and optimistic road map for how the health community can course correct to address these urgent challenges in breast cancer.
Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Already have an account? Sign in here.
Related hub content
- Lancet Series: Menopause 2024 Latest comment by Patient Safety Learning
- 1,000 voices, not 1: A report highlighting differences in cancer care in the UK (9 April 2024) Latest comment by Patient Safety Learning
- Report suggests people with breast cancer are being ‘systematically left behind’ Latest comment by Patient Safety Learning
Useful external links
- Existing user? Sign In
- Communities
- Patient Safety Learning and the hub
- Become a member
- Join a private community
- Topic leaders
- How to share content
- Guide to writing a blog
- Moderation of content
- Acceptable use policy
- How the hub is being used
- Top tips for personalising your hub
- User feedback survey
- All content
- All community
- Create New...
Sponsor Content from

This content is made possible by our sponsor and is independent of The Atlantic ’s editorial staff.
Atlantic Re:think is the creative marketing studio at The Atlantic .
Advancing Treatment Options for Patients with Metastatic Breast Cancer

W hile treatments for metastatic breast cancer (MBC) have progressed significantly in recent decades, there remains an opportunity to provide patients with more flexibility and options in where and how they receive their treatments.
A recent survey 1 revealed that women with ER+, HER2- MBC sometimes encounter barriers to receiving their treatment, like time spent and transportation, that may negatively impact other areas of patients’ lives. These experiences can lead to patients feeling anxious and overwhelmed, among other emotional impacts, adding to the disruption the disease has already caused.
In conversation with Stephanie Walker, a patient with MBC, and Dr. Lillian Smyth, a medical oncologist, and oncology development leader at Lilly, we delve into the evolving landscape of MBC care, from discussing the persistent issues patients face to exploring the innovations paving the way toward additional treatment options that may benefit the lives of patients with MBC.
1 The survey was conducted online by Ipsos in partnership with LBBC and funded by Eli Lilly and Company. The survey was conducted August 23 to October 18, 2023. Read the full survey results https://www.ipsos.com/en-us/understanding-patients-metastatic-breast-cancer-preference-oral-treatments
Can you share with us what life has been like since your diagnosis?
It’s been almost nine years, and my life has changed tremendously. Metastatic breast cancer is like a thread that has been woven through every aspect of my life: from my professional life to my personal life, to my emotional and financial life.
I currently reside in a rural community, and I have to get my treatment about 100 miles away 2 . I am on what we consider my first line of treatment, and that has not been easy. It’s two painful injections every 28 days. If you can compound that over almost nine years, it’s been very impactful on my life.
2 Women with ER+, HER2- MBC spend, on average, almost two and a half hours to attend oncology appointments, including travel and wait times. Patients also reported attending appointments every six weeks, on average.
Lillian, for patients like Stephanie, the work you do has a very real impact. Tell us about your role at Lilly as it relates to metastatic breast cancer.
At Lilly, I lead the development of our breast cancer medicines and work with our discovery scientist group to identify new medicines for patients. The key piece that attracted me to this work was really the ability to make a broader impact on patient outcomes. I, like many other oncologists, just want additional treatment options for patients, and I want them urgently.
Unfortunately, metastatic breast cancer remains an incurable disease and patients need us to rapidly develop more treatment options. We continue to work very hard toward that critical goal.
How have the challenges in your journey as a patient impacted your sense of control?
I absolutely can say that I had no control of my life at one point. I was always going to the doctor’s office. I wasn’t seeing the inside of my house because of how often I was in the hospital. I was getting scanned every three months in the beginning, so I lived my life in three-month blocks. I could not plan anything outside of three months because I was too scared - I didn’t know if the treatment was going to be effective.
But that’s in the past. It is by the grace of God and all of the developments that the doctors have been able to make that I am still here.
Could you provide insight into metastatic breast cancer treatments and how they have evolved over time?
Thankfully, MBC treatment options and outcomes have improved dramatically in the last several decades. At a high level, as we’ve learned more about how cancers grow and spread, one of the ways we’ve learned how to treat them is to target (with medicines) some of those key signals/drivers of cancer growth (e.g. the estrogen- or HER2- receptors in breast cancer). This “targeted treatment” strategy has dramatically improved patient outcomes. Overall, what we’ve seen more recently is that the pace of drug development is greatly accelerating. Ultimately, that’s a good thing for patients – bringing more options to those who need them.
This recent survey highlights an important point, however, about patient experience. Specifically, that the impact of this disease and the treatment needed for it is broader than just a physical impact. It can, in fact, be quite disruptive at times 3 , emphasizing the need for effective and tolerable treatment options that are also minimally disruptive to a patient’s life.
Certainly, there have been some optimizations in how we administer treatments that can improve that patient experience. For example, some medicines or classes of medicines previously given as an infusion or an injection are now optimized to be given either as an injection or as a pill, respectively, potentially providing more convenient ways to receive treatment.
3 35% of HR+, HER2- MBC patient respondents reported having to take time off from work to accommodate their oncology appointments. 33% said they needed to find a friend or family member to accompany them to the appointment.
What do you think should be prioritized in the development of new treatments for metastatic breast cancer?
Anything that keeps us out of the doctor’s office and gives us more time at home and with our families, making memories and living a “normal” life. I hate the injections. I wish that the medication I am taking could be administered a different way. For those of us living with this disease, quality of life with minimal disruptions is an important thing 4 . For example, the development of new oral drugs that we can take at home.
4 79% of survey respondents with HR+, HER2- MBC said the freedom to take a medication in a convenient location and not having to travel to their oncologist's office for treatment are perceived benefits of an oral medication.
Looking ahead, what are some of the areas of focus for Lilly for advancing treatment options and improving outcomes for patients with metastatic breast cancer?
Fundamentally, we want to continue to build on our understanding of what those drivers of breast cancer are so that we can develop new medicines that target them effectively. Our efforts will involve optimizing and improving how we target known drivers of breast cancer, but also include us looking for new druggable targets.
Ultimately, we’re striving to create more effective and tolerable options for patients living with breast cancer and to improve the patient experience with this disease.
What were some of the most unexpected parts of your journey as a patient with metastatic breast cancer?
When I was told I couldn’t work. That statement was harder to swallow than my cancer diagnosis. In my head, I’d had the perfect job, lived the best life, and had my needs met. I never envisioned a cancer diagnosis let alone what it would take from me. Patients like me just want their life to go back to as normal as possible, including work. Hopefully, we will get closer to that with the treatments being developed.
I was also shocked to realize my lack of knowledge was a barrier [in my treatment process]. Nobody taught me [how to handle all of this] prior to when I was first diagnosed. As a nurse, I thought I was armed with all the what-ifs, but you don’t know what you don’t know.
What’s the connection between innovation and health equity * ?
Innovation can advance health equity in a variety of ways. For example, ensuring that all patient populations are represented in the development of a medicine. We know that patients can sometimes respond differently to medicines based on their age, sex, race, and ethnicity, so we need to ensure we’re evaluating our medicines across diverse populations. Unfortunately, in clinical trials of new medicines, we often see underrepresentation of diverse populations. This is something we’re working hard to remedy.
Another innovation in advancing health equity is developing treatment options that can reduce the burden of metastatic treatment, which is a hurdle for many patients. In fact, another key learning from this survey was that patients consider safety and quality of life to be the most important characteristics of metastatic breast cancer treatment. As you would expect, patients value therapies with minimal side effects that they can take conveniently with minimal disruption to their life. It’s intuitive, but it’s something that we who develop medicines need to be continually cognizant of.
At Lilly, we are committed to discovering and developing medicines with the potential to make a meaningful difference for people living with metastatic breast cancer, which includes providing more treatment options that can be taken at home. We continue to work closely with scientists, researchers, oncologists, regulators, and patient advocates on this endeavor.
* According to the World Health Organization , health equity is defined as the state in which all individuals can achieve their full potential for health and well-being.
Disclosure: Stephanie Walker was compensated by Eli Lilly and Company for her time participating in this interview.

CarePilot by Mercurial 12+
Carepilot by mercurial, mercurial ai, designed for iphone.
- 5.0 • 1 Rating
iPhone Screenshots
Description.
Empowering Breast Cancer Patients: Answer medical queries, track treatment progress, access records. Easy sign-up with Google. No fees. *App Description:* Empowering Breast Cancer Patients is a comprehensive mobile application designed to provide invaluable support and resources for individuals diagnosed with breast cancer. This user-friendly app serves as a personalized companion throughout the cancer journey, offering a range of features to enhance patient care and well-being. **Disclaimer:** Please remember to seek a doctor’s advice in addition to using this app and before making any medical decisions. *Key Features and Functionality:* 1. *Medical Query Assistance:* Users can access a wealth of medical information and research within the app, empowering them to make informed decisions about their treatment and care. 2. *Treatment Progress Tracking:* Track your treatment journey seamlessly with interactive tools to monitor how you're feeling during and after treatment sessions, ensuring you stay on top of your health. 3. *Access to Medical Records:* Easily view and manage your medical records directly from your device, providing a convenient way to stay organized and informed about your health history. 4. *Simple Sign-Up:* Sign up effortlessly using your existing Google account, streamlining the onboarding process for users. *Target Audience:* This app is tailored for adult men and women who have been diagnosed with breast cancer, offering a supportive and informative platform to aid them throughout their cancer experience. *No Fees or Paid Content:* Empowering Breast Cancer Patients is committed to providing essential resources and support free of charge, ensuring accessibility to all users without any hidden fees or paid content. *User Account Creation:* Users can easily create an account using their existing Google credentials, facilitating a smooth and hassle-free registration process. *Highlighted Features:* - *Comprehensive Home Screen:* Upon logging in, users are greeted with a guided tour to familiarize them with the app's features. The home screen provides easy navigation to various sections, including profile management, medical record uploads, treatment recommendations, and more. - *Medical Record Upload:* Seamlessly upload medical documents in PDF format, and let the app extract relevant data to enhance treatment recommendations and insights. - *Interactive Charts and Graphs:* Visualize key health metrics such as hemoglobin levels, hematocrit, and white blood cell count through intuitive graphs on the labs page. - *Personalized Medication Recommendations:* Receive personalized medication recommendations based on algorithmic analysis and consultation with in-house medical experts, ensuring tailored treatment plans. - *Treatment Diary:* Maintain a comprehensive treatment diary to record important notes, appointments, and health-related updates, providing a centralized platform for managing your cancer journey. - *News and Awareness:* Stay informed with the latest news and developments in breast cancer research and awareness through curated articles and updates on the news screen. - *Onco Chatbot:* Interact with the Onco Chatbot to seek answers to health-related queries, with a reminder to always consult with healthcare professionals for personalized medical advice. - *Symptom Tracker:* Monitor and manage symptoms effectively with insights tailored to your specific health data, aiding in proactive symptom management. - *Profile Management:* Access detailed summaries of doctor visits, provider notes, and imaging data directly within the profile section, providing users with a comprehensive overview of their health status. *Conclusion:* Empowering Breast Cancer Patients is more than just an app—it's a dedicated companion offering unwavering support and guidance throughout the breast cancer journey. With its intuitive features and user-friendly interface, it aims to empower individuals to take control of their health and well-being with confidence and clarity. Download now and embark on your journey towards empowerment and resilience.
Ratings and Reviews
App privacy.
The developer, Mercurial AI , indicated that the app’s privacy practices may include handling of data as described below. For more information, see the developer’s privacy policy .
Data Not Collected
The developer does not collect any data from this app.
Privacy practices may vary based on, for example, the features you use or your age. Learn More
Information
- Developer Website
- App Support
- Privacy Policy

You Might Also Like
THE YOGA BARN BALI
NoiseFit Assist
Barre Definition
Sameday Health
Talkspace Therapy and Support
Stress Monitor for Watch
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
Search life-sciences literature (43,920,221 articles, preprints and more)
- Free full text
- Citations & impact
- Similar Articles
Breast cancer patient experiences through a journey map: A qualitative study.
Author information, affiliations.
- Ciria-Suarez L 1
- Calderon C 1
- Jiménez-Fonseca P 2
- Palacín-Lois M 3
- Antoñanzas-Basa M 4
- Manzano-Fernández A 4
- Fernández-Montes A 5
ORCIDs linked to this article
- Ciria-Suarez L | 0000-0002-1388-6686
- Castelo B | 0000-0002-5824-9808
Plos one , 22 Sep 2021 , 16(9): e0257680 https://doi.org/10.1371/journal.pone.0257680 PMID: 34550996 PMCID: PMC8457460
Abstract
Conclusions, free full text .

Breast cancer patient experiences through a journey map: A qualitative study
Laura ciria-suarez.
1 Clinical Psychology and Psychobiology Department, Faculty of Psychology, University of Barcelona, Barcelona, Spain,
Paula Jiménez-Fonseca
2 Medical Oncology Department Hospital Universitario Central of Asturias, Oviedo, Spain,
María Palacín-Lois
3 Social Psychology and Quantitative Psychology Department, Faculty of Psychology, University of Barcelona, Barcelona, Spain,
Mónica Antoñanzas-Basa
4 Medical Oncology Department, Hospital Universitario Clínico San Carlos, Madrid, Spain,
Ana Fernández-Montes
5 Medical Oncology Department, Complexo Hospitalario Universitario de Ourense, Ourense, Spain,
Aranzazu Manzano-Fernández
Beatriz castelo.
6 Medical Oncology Department, Hospital Universitario La Paz, Madrid, Spain,
Elena Asensio-Martínez
7 Medical Oncology Department, Hospital General Universitario de Elche, Elche, Spain,
Susana Hernando-Polo
8 Medical Oncology Department, Hospital Universitario Fundación Alcorcón, Madrid, Spain,
Caterina Calderon
- Associated Data
Relevant anonymized data excerpts from the transcripts are in the main body of the manuscript. They are supported by the supplementary documentation at 10.1371/journal.pone.0244355 .
Breast cancer is one of the most prevalent diseases in women. Prevention and treatments have lowered mortality; nevertheless, the impact of the diagnosis and treatment continue to impact all aspects of patients’ lives (physical, emotional, cognitive, social, and spiritual).
This study seeks to explore the experiences of the different stages women with breast cancer go through by means of a patient journey.
This is a qualitative study in which 21 women with breast cancer or survivors were interviewed. Participants were recruited at 9 large hospitals in Spain and intentional sampling methods were applied. Data were collected using a semi-structured interview that was elaborated with the help of medical oncologists, nurses, and psycho-oncologists. Data were processed by adopting a thematic analysis approach.
The diagnosis and treatment of breast cancer entails a radical change in patients’ day-to-day that linger in the mid-term. Seven stages have been defined that correspond to the different medical processes: diagnosis/unmasking stage, surgery/cleaning out, chemotherapy/loss of identity, radiotherapy/transition to normality, follow-up care/the “new” day-to-day, relapse/starting over, and metastatic/time-limited chronic breast cancer. The most relevant aspects of each are highlighted, as are the various cross-sectional aspects that manifest throughout the entire patient journey.
Comprehending patients’ experiences in depth facilitates the detection of situations of risk and helps to identify key moments when more precise information should be offered. Similarly, preparing the women for the process they must confront and for the sequelae of medical treatments would contribute to decreasing their uncertainty and concern, and to improving their quality-of-life.
- Introduction
Breast cancer is the most common cancer and the one that associates the highest mortality rates among Spanish women, with 32,953 new cases estimated to be diagnosed in Spain in 2020 [ 1 ]. Thanks to early diagnosis and therapeutic advances, survival has increased in recent years [ 2 ]. The 5-year survival rate is currently around 85% [ 3 , 4 ].
Though high, this survival rate is achieved at the expense of multiple treatment modalities, such as surgery, chemotherapy, radiotherapy, and hormone therapy, the side effects and sequelae of which can interfere with quality-of-life [ 5 ]. Added to this is the uncertainty surrounding prognosis; likewise, life or existential crises are not uncommon, requiring great effort to adjust and adapt [ 6 ]. This will not only affect the patient psychologically, but will also impact their ability to tolerate treatment and their socio-affective relations [ 7 ].
Several medical tests are performed (ultrasound, mammography, biopsy, CT, etc.) to determine tumor characteristics and extension, and establish prognosis [ 8 ]. Once diagnosed, numerous treatment options exist. Surgery is the treatment of choice for non-advanced breast cancer; chemotherapy, radiotherapy, and hormone therapy are adjuvant treatments with consolidated benefit in diminishing the risk of relapse and improving long-term survival [ 9 ]. Breast cancer treatments prompt changes in a person’s physical appearance, sexuality, and fertility that interfere with their identity, attractiveness, self-esteem, social relationships, and sexual functioning [ 10 ]. Patients also report more fatigue and sleep disturbances [ 11 ]. Treatment side effects, together with prognostic uncertainty cause the woman to suffer negative experiences, such as stress in significant relationships, and emotions, like anxiety, sadness, guilt, and/or fear of death with negative consequences on breast cancer patients’ quality-of-life [ 10 , 12 ]. Once treatment is completed, patients need time to recover their activity, as they report decreased bodily and mental function [ 13 ], fear of relapse [ 14 ], and changes in employment status [ 15 ]. After a time, there is a risk of recurrence influenced by prognostic factors, such as nodal involvement, size, histological grade, hormone receptor status, and treatment of the primary tumor [ 16 ]. Thirty percent (30%) of patients with early breast cancer eventually go on to develop metastases [ 17 ]. There is currently no curative treatment for patients with metastatic breast cancer; consequently, the main objectives are to prolong survival, enhance or maintain quality-of-life, and control symptoms [ 17 , 18 ]. In metastatic stages, women and their families are not only living with uncertainty about the future, the threat of death, and burden of treatment, but also dealing with the existential, social, emotional, and psychological difficulties their situation entails [ 18 , 19 ].
Supporting and accompanying breast cancer patients throughout this process requires a deep understanding of their experiences. To describe the patient’s experiences, including thoughts, emotions, feelings, worries, and concerns, the phrase “patient voice” has been used, which is becoming increasingly common in healthcare [ 20 ]. Insight into this “voice” allows us to delve deeper into the physical, emotional, cognitive, social, and spiritual effects of the patient’s life. This narrative can be portrayed as a “cancer journey", an experiential map of patients’ passage through the different stages of the disease [ 21 ] that captures the path from prevention to early diagnosis, acute care, remission, rehabilitation, possible recurrence, and terminal stages when the disease is incurable and progresses [ 22 ]. The term ‘patient journey’ has been used extensively in the literature [ 23 – 25 ] and is often synonymous with ‘patient pathway’ [ 26 ]. Richter et al. [ 26 ] state that there is no common definition, albeit in some instances the ‘patient journey’ comprises the core concept of the care pathway with greater focus on the individual and their perspective (needs and preferences) and including mechanisms of engagement and empowerment.
While the patient’s role in the course of the disease and in medical decision making is gaining interest, little research has focused on patient experiences [ 27 , 28 ]. Patient-centered care is an essential component of quality care that seeks to improve responsiveness to patients’ needs, values, and predilections and to enhance psychosocial outcomes, such as anxiety, depression, unmet support needs, and quality of life [ 29 ]. Qualitative studies are becoming more and more germane to grasp specific aspects of breast cancer, such as communication [ 27 , 30 ], body image and sexuality [ 31 , 32 ], motherhood [ 33 ], social support [ 34 ], survivors’ reintegration into daily life [ 13 , 15 ], or care for women with incurable, progressive cancer [ 17 ]. Nevertheless, few published studies address the experience of women with breast cancer from diagnosis to follow-up. These include a clinical pathway approach in the United Kingdom in the early 21st century [ 35 ], a breast cancer patient journey in Singapore [ 25 ], a netnography of breast cancer patients in a French specialized forum [ 28 ], a meta-synthesis of Australian women living with breast cancer [ 36 ], and a systematic review blending qualitative studies of the narratives of breast cancer patients from 30 countries [ 37 ]. Sanson-Fisher et al. [ 29 ] concluded that previously published studies had examined limited segments of patients’ experiences of cancer care and emphasized the importance of focusing more on their experiences across multiple components and throughout the continuum of care. Therefore, the aim of this study is to depict the experiences of Spanish breast cancer patients in their journey through all stages of the disease. To the best of our knowledge, there are no studies that examine the experience of women with breast cancer in Spain from diagnosis through treatment to follow-up of survivors and those who suffer a relapse or incurable disease presented as a journey map.
A map of the breast cancer patient’s journey will enable healthcare professionals to learn first-hand about their patients’ personal experiences and needs at each stage of the disease, improve communication and doctor-patient rapport, thereby creating a better, more person-centered environment. Importantly, understanding the transitional phases and having a holistic perspective will allow for a more holistic view of the person. Furthermore, information about the journey can aid in shifting the focus of health care toward those activities most valued by the patient [ 38 ]. This is a valuable and efficient contribution to the relationship between the system, medical team, and patients, as well as to providing resources dedicated to the patient’s needs at any given time, thus improving their quality of life and involving them in all decisions.
Study design and data collection
We conducted a qualitative study to explore the pathway of standard care for women with breast cancer and to develop a schematic map of their journey based on their experiences. A detailed description of the methodology is reported in the published protocol “Ascertaining breast cancer patient experiences through a journey map: A qualitative study protocol” [ 39 ].
An interview guide was created based on breast cancer literature and adapted with the collaboration of two medical oncologists, three nurses (an oncology nurse from the day hospital, a case manager nurse who liaises with the different services and is the ‘named’ point of contact for breast cancer patients for their journey throughout their treatment, and a nurse in charge of explaining postoperative care and treatment), and two psycho-oncologists. The interview covered four main areas. First, sociodemographic and medical information. Second, daily activities, family, and support network. Third, participants were asked about their overall perception of breast cancer and their coping mechanisms. Finally, physical, emotional, cognitive, spiritual, and medical aspects related to diagnosis, treatment, and side effects were probed. Additionally, patients were encouraged to express their thoughts should they want to expand on the subject.
The study was carried out at nine large hospitals located in six geographical areas of Spain. To evaluate the interview process, a pilot test was performed. Interviews were conducted using the interview guide by the principal investigator who had previous experience in qualitative research. Due to the Covid-19 pandemic, all interviews were completed online and video recorded with the consent of the study participants for subsequent transcription. Relevant notes were taken during the interview to document key issues and observations.
Participant selection and recruitment
Inclusion criteria were being female, over 18 years of age, having a diagnosis of histologically-confirmed adenocarcinoma of the breast, and good mental status. To ascertain the reality of women with breast cancer, most of the patients recruited (80%) had been diagnosed in the past 5 years. Patients (20%) were added who had been diagnosed more than 5 years earlier, with the aim of improving the perspective and ascertaining their experience after 5 years.
Medical oncologists and nurses working at the centers helped identify patients who met the inclusion criteria. Participants went to the sites for follow-up between December 2019 and January 2021. Eligible women were informed of the study and invited to participate during an in-person visit by these healthcare professionals. Those who showed interest gave permission to share their contact information (e-mail or telephone number) with the principal investigator, who was the person who conducted all interviews. The principal investigator contacted these women, giving them a more detailed explanation of the study and clarifying any doubts they may have. If the woman agreed to participate, an appointment was made for a videoconference.
A total of 21 women agreed to participate voluntarily in this research. With the objective of accessing several experiences and bolstering the transferability of the findings, selection was controlled with respect to subjects’ stage of cancer, guaranteeing that there would be a proportional number of women with cancer in all stages, as well as with relapses.
Data analysis
The data underwent qualitative content analysis. To assure trustworthiness, analyses were based on the system put forth by Graneheim, and Lundman [ 40 ]. Interviews were transcribed and divided into different content areas; units of meaning were obtained and introduced into each content area; meaning codes were extracted and added; codes were categorized in terms of differences and similarities, and themes were created to link underlying meanings in the categories. All members of the research team (core team, two medical oncologists, three nurses and two psycho-oncologists) reviewed the data and triangulated the outcomes between two sources of data: qualitative data from the interview and non-modifiable information, such as sociodemographic (i.e., age, marital status, having children) and clinical (i.e., cancer stage and surgery type) data. Following this process, we reached saturation of the interview data by the time we had completed 21 interviews.
Ethical considerations
This study was performed in accordance with the ethical standards of the Declaration of Helsinki, and its subsequent amendments. The study was approved by the Research Ethics Committee of University of Barcelona (Institutional Review Board: IRB00003099) and supported by the Bioethics Group of the Spanish Society of Medical Oncology (SEOM) 2018 grant. All participants received a written informed consent form that they signed prior to commencing with the interviews and after receiving information about the study.
Patient baseline characteristics
In total, 21 women with a mean age of 47 years (range, 34 to 61) were interviewed. Most of the study population was married (66.7%), had a college education (66.7%), and had 2 or more children (42.9%). All cancer stages were represented, up to 23.8% tumor recurrence, and most of the primary cancers had been resected (95.2%) (see Table 1 ).
Description of the breast cancer patient journey
The women diagnosed with breast cancer describe the journey as a process tremendously affected by the different medical stages. Each stage has its own characteristics that condition the experiences, unleashing specific physical, emotional, cognitive, and social processes. Additionally, the patients perceive this entire process as pre-established journey they must undertake to save their life, with its protocols based on the type and stage of cancer.
“ People said to me , ‘What do you think ? ’ and I answered that there was nothing for me to think about because everything is done , I have to go on the journey and follow it and wait to see how it goes” (Patient 6)
Fig 1 displays the various phases of the journey that patients with breast cancer go through; nevertheless, each woman will go through some or others, depending on their type of cancer.

Throughout the entire patient journey
Processes of loss and reinterpretation of the new circumstance . What stands out the most in the process these women go through during the diagnosis and treatment of breast cancer is loss; specifically, the loss of health and a reinterpretation of the new circumstance and the new bodily reality. In the most extreme cases, the loss of health emerges with the fear of death that many women report at the time of diagnosis or during treatment, due to the distress generated. The loss of identity seems to be related to the evolutionary (existential) moment in which the woman is; there are patients who report feelings of disability or loss of attractiveness, or fear of not being able to get pregnant in the future, especially the youngest.
I felt a terrifying fear and thought , “You have cancer you tell yourself , you’re going to die tomorrow .” (Patient 6) I feel like after the hysterectomy , as a woman , I no longer have anything , only the physical . Sure , I look great , but I tell myself that it’s just a shell , the shell I inhabit , because as a woman , I only have one breast left . (Patient 6) At that moment , I had to make the decision that I was no longer going to be a mother . (Patient 14)
Personal change . Most of the women report that with the diagnosis of breast cancer, their life stands still and from that point forward, a different journey begins. The sole focus on this journey is the disease and its implications. During all those months, the patients stop working; they focus on their medical treatments, and reflect a lot on their current situation and on life. Most of the participants state, especially those who have already been discharged, that they know themselves better now; they take better care of themselves, and they enjoy their day-to-day and the small moments more, making the most of their time, with more initiatives and fewer trivial complaints.
Clearly , you’re not the same person you were before; I don’t think she’ll ever come back; your mindset changes completely and I have sequelae from all the treatments . (Patient 1) I re-think wasting energy on lost causes; what’s more , I’ve also learnt to say no . If I’m not in the mood to go somewhere , I just say no . (Patient 7) I take much more advantage of the present now , because you realize that things can change on any given day . (Patient 3)
Trust and appreciation for their physician . Most of the interviewees stated that they fully trusted the doctors who care for them, without question or objection to the treatments proposed. They reported that, as they go forward, they discuss the tests and treatments that are going to be performed, as well as possible side effects. Several stated that they are unaware of the stage of their cancer; similarly, most also do not know the benefits expressed in X% of the treatments. A few of the participants claimed that they did talk in detail about the different types of treatments with their oncologists, that they had sought another opinion, and one of them even reported having decided to stop chemotherapy, which was very hard for her, given her physician’s insistence that she continue.
The truth is that the oncologist didn’t say much about percentages; what she told me were the steps that I had to take; I thoroughly trusted her and she gave me a lot of peace of mind . (Patient 5) I told him , “I’m going to do whatever you tell me to . ” It never occurred to me to dispute whatever the oncologist might tell me . I was willing to do whatever was needed . (Patient 8)
Most of the women, at some point during the interview, state that they are grateful for the care they received and that, within the seriousness of their situation, there is a treatment for their condition.
I am super grateful for the treatment I’ve received and with the doctors assigned to me . (Patient 2) I’m very lucky; I’m only on my second line of treatment for metastasis and I’ve got a lot more ahead of me , but I consider myself lucky and I believe things are going very well . (Patient 20)
Role of the woman . We can see that the women adopt a role of care-givers and managers of their surroundings. They worry about the disease negatively affecting the people around them, which is why they make an effort to manage the family’s activity for when they can’t do it and they try to avoid being a physical burden or cause emotional distress to the people around them.
I was very strong ; I made everything easy for people , but making it very easy , doesn’t mean that it was easy for me , but that I made it easy for everyone . (Patient 8) I didn’t want to worry anyone because that’s just the way I am , I push forward and that’s that . (Patient 5)
Support network . In all cases, the family appears to be one of the elements that is most involved in the disease process. Within the family, the partner deserves special mention. The testimonies in this regard reveal a wide spectrum of possibilities that range from the feeling of having had great support to a lack of attention and understanding that, in many situations, causes the relationship to be strained or to end. Friends tend to appear more occasionally.
I can’t complain about my husband; he was up to the challenge , very attentive toward me and he fully understood how I was feeling ; I felt very supported . (Patient 14) We’ve had a period of a lot of arguing; I’ve had to sit down with him and tell him that life had changed for me . (Patient 18) I had a partner I had lived with for five and a half years and he told me , literally , that he looked at me like a little sister , no longer as a woman , and he left me , and that hurt me tremendously . (Patient 6)
On the other hand, many patients commented on the importance of social media, where they have met people in the same situation as them. They report feeling understood and in good company; likewise, they commented on the importance of being able to share their doubts and get to know about other experiences.
It’s a situation that only someone who has gone through can understand; you can have all the good intentions in the world , but if you haven’t gone through it , you can’t even begin to understand . (Patient 8)
Use of complementary treatments . Most patients follow conventional medical treatment. However, many resort to other disciplines that help them improve their quality-of-life, like dietary changes, getting more exercise than usual, visits to a psychologist or physical therapist, or using other integrative therapies, such as acupuncture, yoga, reiki, flowers of Bach, homeopathy, cannabis, or meditation.
I started to read a whole bunch of books to see what I could do to take care of myself in terms of nutrition and exercise ; you consider everything you can do . (Patient 5)
Diagnosis/unmasking
This phase encompasses the time from when the woman detects some symptom or goes to a check-up until the medical diagnosis is made. For the woman, this is a time of a series of tests and results. We have observed that the procedures, especially the healthcare professionals that deal with the patients, and the timing vary, depending on the medical center where they are being cared for. Emotionally, this is one of the most complicated stages.
Emotional whirlwind . The wait to obtain test results has a huge emotional impact for the women, given that it is a time of great uncertainty and fear.
An entire month with all the anguish of finding out if you have something . (Patient 3) The worst part is waiting 15 days to find out the magnitude of the tragedy , if it’s throughout your entire body or only in your breast; you go through a brutal emotional whirlwind; the wait is horrible because there’s nothing else you can do , so that anguish that you carry inside is dreadful; it was hell for me . (Patient 10)
Additionally, the interviewees described many other emotions that included fear of death, fear of having no time, feeling of unreality, rage, anger, sadness, avoidance, denial…
The first thing I thought was that I was going to die and that I wouldn’t finish watching my children [grow up]; my father had died of lung cancer 25 years ago . (Patient 9) My only aim was to get back to normal , as if there were nothing wrong . (Patient 4) You have a lot of conflicting feelings; you wish this weren’t happening; you want to run away , but you say , “Where am I going to run to ? ” . (Patient 14)
Impact of medical communication . Several women comment that, when given the diagnosis, they dissociate because of the emotional impact and that they don’t listen to all the information that the medical professional is giving them.
I remember that she talked and talked , but I didn’t know what she was saying until she said , “Isabel , you’re going to be cured , okay ?”. (Patient 9)
During the diagnostic testing, the women are highly sensitive to the healthcare professionals’ words and gestures.
I looked at the face of the person who was doing the mammogram and that’s when I started to imagine the worst . (Patient 20) I say to them , “ But , is there a solution to this ? ” , and they say to me , “Don’t worry , I’m sure there is a solution . ” That “sure” is etched in my mind . (Patient 10)
Communication and managing their surroundings . After the diagnosis, the patients feel that they have to tell the people around them about their situation, especially those closest to them, the family. They all agree on how hard it is to share. Normally, the people it’s hardest to tell are their mother and their children. When they do, they try to put the most positive spin on it possible, in an attempt to keep them from worrying.
You no longer think only about yourself , you think , “Good grief , now I’ve got to tell my mother .” It’s hard . (Patient 16) I wanted to tell my kids the way I say things , always trying to look for the upside , and positive , although it was hard , but , anyway , in the end , it went well . When I finished , my husband told me , “You’ve convinced me that it’s no big deal .” (Patient 9) I told my son , “Son , don’t cry , your mom’s going to get over this , this is nothing .” (Patient 1)
During this period, the women contemplate how their situation will affect their surroundings and they try to organize it as much as possible.
I devoted myself to planning everything , to organizing what to do with my daughter , and to thinking about work , too , how I had left things at work . (Patient 4)
Surgery/cleaning out the cancer
Uncertainty and fear . The participants express that before going into surgery, they are told about the kind of procedure that will be done, but that, depending on what they find and the analysis, it may change. In light of this, they exhibit an enormous feeling of uncertainty and fear. In addition, many voice concern about how the surgery will go.
They tell you conservative surgery , but if we open up and see something we didn’t see on the tests , then everything could change . (Patient 10) Aside from the anesthesia , that I’m terrified of , you spend several hours in surgery and you don’t really know how things will go; when they clean it out , they analyze it , and you go into the operating room and you don’t know what can happen . (Patient 9)
Feeling of loss . Considering that the breast is associated with an intimate, feminine part [of their body], many women experience the operation as a loss. This loss is more acute if the operation is a mastectomy and there is no reconstruction at the same time. The loss also involves a loss of identity, compounded by the side effects of chemotherapy, such as hair loss. The interviewees who had undergone mastectomy say that following surgery, when the bandaging is removed and the scar is revealed, is one of the most critical moments, which is why they express difficulty in managing it and appreciate the caring assistance from the professionals.
It is identification with yourself , you know , it’s what you’ve seen in the mirror , what you think you’re like and , suddenly , you’re no longer like that; there’s an incredible personal crisis because you no longer recognize what you’re seeing . (Patient 11) I closed my eyes and I removed the bandaging and I didn’t dare look … with my eyes , I imagined the worst . (Patient 12)
Acceptance or demand for more aggressive intervention . The patients perceive the surgery as essential to recovering their health, which is why the process is widely accepted. Some patients who demand a more invasive intervention, normally a bilateral mastectomy, do so because that way, they feel safer with respect to a possible relapse, as well as more comfortable esthetically.
If they have to remove my breast , let them take it; what I want is to get better . (Patient 16) They say that I am in full remission , so they only removed the lump , but at first , I said that I wanted my whole [breast] removed ; then they assessed how to do it . (Patient 13) They told me that I had a genetic mutation and more possibilities of developing breast cancer and , since I felt such rejection toward my remaining breast , I decided to get rid of that one , too . (Patient 20)
Chemotherapy/loss of identity
The chemotherapy phase is one of the phases that affects the women’s lives the most, because of its physical impact and how long it lasts. No differences have been found in how they experience chemotherapy depending on whether it was neoadjuvant or adjuvant.
Negative impact of side effects . Chemotherapy is associated with many side effects that vary from one woman to another. Many indicate that they have suffered physical discomfort, such as fatigue, dysgeusia, pain, nausea and vomiting, mucositis, diarrhea, etc.
One day when I didn’t want to go to bed , I went to bed crying because I had the feeling that I wasn’t going to wake up . That day it was because I felt awful . (Patient 1)
Furthermore, all of the women suffer hair loss, which is one of the most-feared effects. Likewise, their body hair also falls out, especially on their face, and their weight fluctuates. All of these changes lead to a loss of identity that is experienced as taking away from their femininity. It must be remembered that oftentimes, chemotherapy is administered after surgery, further exacerbating this physical change. On top of all that, several women comment having to decide at the beginning of treatment whether to freeze their eggs or not; at that moment, many of them forfeit the possibility of becoming a mother or of becoming a mother again, which also adds to this loss of femininity.
Losing my hair was hard , but when it grew out again , I had an identity crisis . I didn’t recognize myself; people said I was really pretty like that , with my hair so short . I looked at myself in the mirror and I said that I’m not that woman , I can see that that woman is pretty , but it’s just that I don’t recognize myself . That’s not me or , it was like , I looked at myself and I didn’t recognize myself . That’s when I suffered a serious identity crisis , psychologically serious , but also serious because I sobbed because I looked at myself , but it wasn’t me . (Patient 6) Where’s that sexy lady , where is she ?, because you don’t feel good . I didn’t like myself at all . I was several sizes larger and I looked at myself and said , “What a monster . ” I didn’t feel good about myself . (Patient 1)
Many patients say that chemotherapy decreases their libido and dries up their mucous membranes, which is why they prefer not to have sex. For those who live as a couple, this situation can strain the relationship.
Sexually , I just didn’t feel like it , I wasn’t in the mood; not only did I not feel like it , my mucous membranes were dry and , what’s smore , I just couldn’t , I couldn’t , I felt bad for my husband , but he said , “Don’t worry .” (Patient 16)
Finally, some interviewees expressed a feeling of being poisoned by the treatment. These women tend to be highly focused on taking care of their body and have a very natural attitude toward life.
I had to really work my awareness that I was poisoning myself; at night I was at home and I thought that all that red liquid was circulating through my veins … I think I even had nightmares . (Patient 4)
Balance between caring for oneself and caring for others . The patients feel that it is time to take care of themselves, so they prioritize resting when they need it. Moreover, they worry about getting a haircut and, most of the times, they look for turbans and wigs. Some also learn how to put on make-up, which they rate as being very positive. On the other hand, those who have children or another person in their care, try to take care of them as much as they are able.
Around 11 : 00 , I no longer felt good , so I’d go to the armchair to rest and it’s like I had an angel , because I’d wake up a minute before I had to set the table and get lunch for my son who would be coming home from school . (Patient 1) While I was getting chemo , I went with the gadget and I told myself , “I’m going to teach you to apply make-up; for instance , your eyelashes are going to fall out . Make a line like this ” and at that moment when you look in the mirror , and we look like Fester in the Addams family . (Patient 13)
Vulnerability . The women experience great uncertainty and feelings of vulnerability the first times they receive chemotherapy, since they don’t know what side effects they will suffer.
With chemo , I started with a lot of fear and , later on , I became familiar with it little by little until the time comes when you go to the hospital like someone who’s going to pick up a bit of paper . (Patient 9)
In addition, those participants who join a social network or who are more closely tied to the hospital setting, know about the relapses and deaths of people around them diagnosed with breast cancer, which makes them feel highly vulnerable.
There are some people who leave the group because … it’s not like there are a lot of relapses and , geez , I think that it messes with your head . (Patient 13) We were almost always the same people at chemotherapy ; there was one guy who was really yellow who looked terrible and , there was one time when we stopped seeing him and another lady asked and the nurse said that he had died . (Patient 15)
At the same time, given the physical changes, especially those that have to do with body hair, many women feel observed when they leave home.
If I have to go out and take off my scarf because I’m hot or go straight out without any scarf on my head and whoever wants to look… let them ; I think that it’s up to us , the patients , to normalize the situation; unfortunately , there are more and more cases . (Patient 9)
Telling the kids . Since when the chemotherapy stage is going to entail many physical changes, the women look for ways to talk to their children about the treatment. Most of them comment that it is a complicated situation and all of them try to talk to their children in such a way as to protect them as much as possible.
I asked the nurse for help before I started chemotherapy to see if she had any pointers about how to talk about this with the kids and she recommended a story , but when I saw it , I didn’t like it … so , in the end , I decided to do it off the cuff . (Patient 10)
Radiotherapy/transition to normality
The “last” treatment . When the patient reaches radiotherapy, normally, they have already spent several months undergoing physically aggressive medical procedures, which is why they feel exhausted. There is a physical exhaustion resulting from the previous treatments and made worse by the radiation therapy. Furthermore, many women also report feeling emotionally drained by the entire process. However, this is generally accompanied by joy and relief because they feel that they are in the final stage of treatment.
Emotionally , it’s a marathon that has to end up at some point . (Patient 10) For me , radiotherapy was like a lull in the battle , with a winning mind-set . (Patient 4)
Comparison with chemotherapy . There is a widespread perception that radiotherapy has fewer side effects than chemotherapy, although later, when they receive it, several patients suffer discomfort, above all fatigue and dizziness. Several report that at this point, they are mentally worn out and just want to be done with the process, which is why they have less information than about chemotherapy.
I feel like radiotherapy is unknown , that you think it’s more “light ” and it turns out not to be so light . (Patient 13)
Follow-up care/the “new” day-to-day
Difficulty in getting back to normal . Once the patients are discharged, many feel that they need some time to recover, that it will be slow, in order to restore a more normalized pace of life. They are still working on their emotional and personal process.
When they tell you that you have cancer , they make it very clear : you have a goal; you have some months of chemo , some months of radio , and when you finish , you say , “And now , what do I do ?”. I say that because now I have to get back to my normal life , but I don’t feel normal . I still don’t feel cured , I’m not 100% . And you’re glad you’ve that you’ve finished it all and you’re alive , but at the same time , you say , “Gosh… this is very odd . ” It was a very strange feeling . (Patient 8)
Most patients report that their quality-of-life has diminished, due to the sequelae from the treatments. Lymphedema is one of the sequelae they name most often, although they also mention other symptoms, like digestive upset, weight issues, eye problems, scar pain, etc. The women who are on hormone therapy also suffer side effects, such as joint and muscle pain.
I have lymphedema and , although I have good mobility , I’m a little bit weak; when I go out for dinner , I generally order fish , because I can’t always cut meat well . (Patient 6)
Several interviewees also express difficulty in their affective-sexual relations. Many of them feel insecure because of all the physical changes; others have sequelae that hinder their relations, and still others are suffering symptoms of early menopause. This can cause problems in the couple and for those who don’t have a partner, suffer many complications when it comes to meeting other people.
I haven’t had sex with my husband for 2 years because , it’s also really complicated to get over; I’ve gone for pelvic physical therapy; I’ve used gels , but nothing works . (Patient 8) It’s taken me many months for me to have a relationship again; it’s been really hard because , even though everyone told me that I looked fine , I didn’t feel fine . My breast cancer had taken away all my attributes as a woman . (Patient 6)
Some women also experience difficulties when it comes to returning to work. Several state that they had been fired when they went back. They also report that when interviewing for a job, it’s complicated for them because they have to explain what happened and they mention the schedule of doctor’s visits that they have. Other women comment that they’ve been given early retirement or disability.
You go to the interview and if you tell them that you’ve had the disease , they look at you like you’re a weirdo . (Patient 13)
Breast reconstruction . How reconstruction is experienced, as well as its timing, are highly contingent upon they type of reconstruction. Each one has its pros and cons, but the opinions collected with respect to the type of reconstruction have been positive.
Although it took 18 months for the entire process to be over , I’m delighted with reconstruction with the expander . (Patient 16)
Some patients state that after the whole process, which has been long and complicated, they prefer not to undergo reconstruction immediately. In these cases, they report having felt a subtle pressure from the outside to undergo reconstruction.
Every time I went for my check-ups , they said , “You’re the only one left [who hasn’t undergone reconstruction]” and in the end , the truth is that I’m really happy because I think I look pretty . (Patient 12)
Check-ups and fear of relapse . Check-ups are one of the times that generate most worry and insecurity. The women remark that, starting a few days before and until they receive the results of the follow-up studies, they are more anxious about the possibility of relapse.
At every check-up my legs start shaking again and my stomach is in knots, although at my last one, everything turned out okay and I’m thrilled. (Patient 6) During the first stage , I did everything I had to do and I got over it , but it’s a lottery . You can do whatever you want , but it’s the luck of the draw and when you start going for check-ups , it’s like going to play Russian roulette . (Patient 8)
Maintenance hormone therapy . Hormone therapy is understood differently depending on age and on the major decision of whether or not to be a mother or to have another child. If the woman does not want to have more children, the treatment is accepted better. The patients who take it also report effects derived from menopause, for instance, joint pain or dry mucous membranes.
I did notice joint pain , but since I exercised , [I felt it] much less than my fellow women , although , for instance , when it comes to getting up from a chair , you get up like an old lady . (Patient 10)
Position of support . Several patients mention that, after discharge, they stay active on social media, they volunteer when they find out about someone or to participate in activities related to breast cancer, with the aim of being able to help other people who are in this situation.
It’s really good to meet other people who are going through the same thing , so , now that I’ve finished , I like it and I always help whenever I can , because I can share what was good for me . (Patient 13)
Relapse/starting over
Emotional impact . The diagnosis of a relapse is experienced much the same as the initial diagnosis. All of the women report fear, although they also state that they are more familiar with the processes. Other emotions emerge, such as why me, blame, disbelief, etc.
Since they had told me that it wasn’t going to happen again , I believed it , of course , I wanted to believe it and it totally surprised me; I couldn’t stop crying and crying . (Patient 17)
Telling the family again . Patients repeat that telling the family about it again, especially the children and parents, is tough and they try to minimize it in an attempt to protect them emotionally.
On the very same day that I had my mammogram , my mother says that she wants to come a see the kids . We’re in the park , when she arrives , I have to tell her that everything’s fine and when we get home , I tell her everything . My mother’s devastated again and I tell her not to worry , that everything is going to be fine . (Patient 16)
Thinking about whether something could have been done differently . Several women comment that, after their relapse, they think about whether the treatment was enough or there must have been something they could have done to avoid the relapse.
You get furious , because you say , “I wasn’t supposed to get sick , because if , 2 years ago when the first microcalcifications appeared I had had them removed , then I wouldn’t have metastasis , or maybe I would . (Patient 19)
Metastatic breast cancer/time-limited chronic
Re-interpreting the concept of metastasis . Most of the participants in this stage state that they have had to give new meaning to the word, “metastasis,” since their first perception was directly related to death. In this way, they come to understand that cancer can become chronic, although they now have to take medication and go to the hospital on a regular basis. Nevertheless, they know that their life expectancy may be a few years. The women who are involved in a group point out how hard it is to see their fellow member pass away.
What I now call my “ new normal” consists of lots of visits to the hospital and never going back to work . (Patient18)
They also state that at this stage, they do not identify with the disease generally known socially as “breast cancer”, where there is great emphasis placed on early detection and on their chances of being cured. This causes them to feel more isolated.
These pink ribbon campaigns hurt us because they tend to underscore that everything is going to turn out fine because breast cancer has a very high cure rate; there is huge lack of awareness . (Patient 20)
Physical and emotional discomfort . Most of the women in this stage report side effects from the treatments, although some comment that good quality-of-life can be preserved. On an emotional level, they say that they sometimes feel a certain agony due to not knowing how much longer the treatment will be effective. They live in a state of uncertainty that they try to cope with by focusing on their day-to-day and experience the good times deeply.
When I’m not in pain , I try not to even remember what I have and go out and have fun with my family and live . (Patient 20)
Several women who have children express with regret that they worry about their children enjoying them and remembering them when they were well. They are sad that they won’t be able to grow up in a normal family. Some also comment the impact this diagnosis is having on their partner.
What I don’t want is for them to carry this baggage of having a sick mother . (Patient 18)
A conflict with disability also appears, as many women report their desire to continue working, but feel that they can’t keep up with the pace of work. Additionally, several state that going through the medical board is a strenuous process, given that they look good physically.
It’s hard to deal with , I’m a non-practicing lawyer and I have degrees galore , but I worked the first year and I couldn’t continue . (Patient 21) Every year they call me again for the disability monitoring and they always threaten me . To be honest , the treatment doesn’t make me sick , but I don’t know how long it’s going to be like this . (Patient 19)
Social invisibility . The participants say that they do not have any physical signs of being ill, that they look fine, although they know and feel that inside, they are not well. They say that it is sometimes hard to manage socially, since on occasion, they feel misunderstood and disparaged.
I’m much sicker now , but people think or want to think that I’m fine . When I was doing chemo , it was like wearing a sign that said “cancer . ” (Patient 17)
This study describes the patient journey of women with breast cancer, specifying the different phases with the most relevant aspects of each, as well as the different cross-sectional features they report throughout the entire treatment process.
The results portray breast cancer as a process in which there is a striking feeling of loss of health and self-identity, changes in routines, personal and employment transformation, as well as emotional hardship during and after breast cancer treatment, aspects that are also reported in the literature [ 41 , 42 ]. Earlier studies state that experiencing cancer is highly stressful. It involves a major threat to life or physical integrity, in addition to mental health, interfering with the path, projects, and plans patients have for their life over the short, medium, and, on occasion, long term as well [ 6 ]. Along with reporting adverse physical and psychological impacts, patients also report positive ways in which they have grown psychologically or emotionally from the experience [ 7 , 42 ]. The diagnosis of breast cancer not only impacts the women individually, but also affects their surroundings. As reported in the literature, despite going through a very challenging time, the women struggle to put on a positive face and attempt to conserve the family’s well-being, specifically that of their children [ 7 ]. At the same time, the family is a fundamental source of support and usually provide indispensable support; however, it is not always effective, because family members do not fully understand the stresses involved in living with cancer [ 43 ]. Previous studies also reveal that for some women, their partners are one of their most significant supports; nonetheless, research also suggests that a cancer diagnosis predicts marital breakup more strongly for female survivors than males [ 44 ]. Our results reflect that the women frequently resort to other women in the same situation, possibly because they face significant unmet supportive care needs [ 30 ]. The need for social support may lead patients to seek social support groups consisting of people who are experiencing similar health crises, because such groups allow them to interact with those who best understand their suffering [ 43 ]. Another aspect that appears across the board is the relationship the participants have with the medical team. In this study, we have noted their trust in the medical team and acceptance of the treatments proposed without going into the clinical data of the disease and without needing to know the benefit provided by the treatment. Cancer patients are confronted with a potentially life-threatening [condition], feeling vulnerable, and need to rely heavily on their care providers, expecting the physician to act in their best interests [ 5 ]. Therefore, they need to have a close relationship, as well as comprehensive care [ 30 ]. Patients’ trust in a physician has been associated with a reduction of their fears and anxiety and [increased] satisfaction and adherence to treatment [ 5 , 30 ]. We believe that it would be important to provide patients with accurate information, so as to avoid misunderstandings (such as cancer being synonymous with death, regardless of stage) as several participants in this study have reported, which can lead them to believe that the risk of relapse with and without chemotherapy is much greater than the oncologists estimate [ 45 ]. We believe that in future studies that it would be worthwhile to examine the peculiarities of each kind of patient information with the aim of determining how to break it up and make it both comprehensible and tolerable to promote patients’ well-being.
A breast cancer diagnosis is generally unexpected and practically all patients suffer psychological distress, such as feelings of uncertainty, disbelief, hopelessness, vulnerability, anger, fear, anxiety, and sadness [ 46 , 47 ]. The literature has reported that many women experience peritraumatic distress or dissociation during the medical conversation in which they are given their diagnosis of cancer [ 48 ], which might account for the reactions of the respondents. Given that, when they receive their diagnosis, additional information is generally given to them, such as clinical aspects and preferred treatments. Repeating this information at subsequent appointments could contribute to improving communication with patient, since several participants stated that they found it hard to pay attention to the physician, given the emotional impact. Additionally, breast cancer patients tend to be diagnosed when they are relatively young, and often when they are in the middle furthering their career or raising children [ 12 ]. In spite of everything, the women try to put on as brave a face as they can and focus on maintaining their children’s well-being [ 7 ]. Telling children about their diagnosis is reportedly one of the biggest challenges; parents are usually unsure of how to tell them, because at the same time that they want it to be open and honest and cover their children’s developmental needs, they also want to protect them children [ 49 ].
Once diagnosed, breast cancer patients go through different treatments. The most salient experiences of these phases pertain to the impact of side effects on physical quality-of-life and psychological well-being, which is consistent with the literature [ 11 ]. Moreover, cancer therapy entails physical changes that affect their feminine identity, fertility, self-esteem, sexual functioning, and makes them more vulnerable [ 10 , 50 ]. Women described their inner self as being on an emotional rollercoaster with highs and lows throughout the various phases of treatment [ 7 ]. Given treatment side effects and sequelae, these women are more likely to experience physical symptoms and psychological disorders than patients with other kinds of tumors [ 51 ]. The side effects involve an acute sense of loss of health and quality-of-life, as well as identity and femininity. It would be interesting for future research to explore the therapies used in grief counseling with cancer patients, as understanding and exploring this perspective could comprise an additional clinical aid.
Once the women have completed their treatments, they gradually get back to normal and many contemplate returning to work. However, in line with our results, the literature reveals that even though they want to normalize their lives, female breast cancer survivors feel that they will never return to their baseline status [ 7 ]. A significant number of patients experience difficulties in physical, cognitive, and emotional functioning after their treatment, such as symptoms like lymphedema, fatigue, pain, sleep disorders, cancer-related cognitive impairment, emotional stress, symptoms of depression and anxiety, problems with relationships, reduced sexual identity, fertility problems, and fear of cancer relapse [ 13 , 14 ]. Furthermore, patients with hormone therapy suffer hot flashes, sweats, joint pain, weight gain, decreased libido, and low energy [ 52 ]. A sizeable number of these women also experience changes in employment status which can happen even 5–10 years following diagnosis [ 15 ]. Given that all these changes alter the structure of the woman’s everyday life, personalized care and treatment plans in cancer survivors are highlighted in the literature with extended specialized support being proposed that enables them to make a better psychosocially adjusted transition from treatment to follow-up [ 53 ] and advocating for the patient’s participation in all decisions that affect her during this period [ 54 ]. Further research is needed concerning how to structure the follow-up and support offered to these women during this stage so as to meet their needs and help them adjust to their new reality with the chronic sequelae caused by cancer and its treatment. On the other hand, the personal transformation of the initial stages of the journey are best seen during this phase. The literature shows that women who have had breast cancer report changes in their philosophy of life, such as embarking on a new life path, changing their priorities in life, as well as valuing life in general [ 42 ]. Most of the participants in our study place special emphasis on appreciating life, enjoying it more, and living each day to the fullest. Cancer survivors report being aware of how precarious life is, while also feeling the joy of being alive [ 55 ]. Similarly, they have been found to be more resilient and better able to repair their mood than healthy women [ 56 ].
About 5% of all patients with breast cancer are diagnosed when the disease is metastatic, whereas some 30% have suffered a relapse of an early breast cancer [ 17 ]. We saw that some women suffering a relapse after initial treatment with curative intent tend to wonder if the treatment was sufficient or if they should have done something more to prevent the relapse. Metastatic breast cancer is uncurable, which is why these women’s main psychosocial challenges are not the same as those who are diagnosed in early stages [ 18 ]. Faced with incurability, the women react with shock and fear of imminent death, but this anxiety diminishes once they begin treatment and learn that there are more treatment options [ 17 ]. During this phase, the interviewees reported impaired physical QoL and functioning, being hindered by pain, fatigue, or menopausal symptoms. Emotionally, they report suffering bouts of depression and anxiety, as well as fear because of the spread of their cancer. As for their relational QoL, their children’s welfare is their number one concern, especially for mothers of young children [ 17 , 57 ]. What’s more, these women felt isolated from society in general and, more specifically, from the non-advanced breast cancer community, inasmuch as they feel that nobody understands what they are going through [ 18 ]. A psychosocial approach is especially important in this phase to help these women to continuously adapt to the changes of their individual clinical situation and to the progression of the disease, thereby improving their coping.
Clinical implications
Having first-person information enables us to comprehend in detail the experiences of breast cancer patients, their situation, and emotional state, which favors holistic cancer care for health professionals.
Healthcare professionals should prepare women for a changed life situation, as well as to face prolonged, multimodal treatment (surgery, chemotherapy, hormone therapy, radiotherapy), and to confront physical and psychological sequelae, as well as the fear surrounding an uncertain prognosis. It is important to help them manage their expectations and fears and, to identify and address the issues and concerns that arise at different time points during treatment. The information and support offered should be adjusted to each woman’s individual needs, her life situation, her coping style, and the time and stage of their cancer. This more empathic, understanding outlook can also contribute to improving the physician-patient rapport, promoting communication, understanding, and shared decision-making.
Finally, a comprehensive understanding of the women’s psychosocial support endorses their belonging to groups of women with breast cancer, in which there is a relationship among equals. Further research is needed to specify the type needed so as to decrease both the impact of the death of women in the group, as well as the vast amount of information that they may end up obtaining, without needing it or requesting it.
Limitations
This study was performed with Spanish participants, which is why certain aspects cannot reflect the experiences of breast cancer patients from other countries, given the particularities of both the Spanish healthcare system and Spanish culture. Likewise, the data attained were specific to women with breast cancer, which can scarcely be extrapolated to individuals with other cancers. Moreover, the findings do not reflect men’s experiences with breast cancer and research with this group would enrich the field further. In addition, the age of our participants ranged from 34 to 61 years; hence the results should be interpreted for a middle-aged population and do not reflect the experiences of women diagnosed at very early or very old ages. Finally, we believe that there may be a bias regarding the women who agree to participate, as this group has probably accepted their condition more, as well as having worked on it more.
Despite these limitations, we hope that our findings can contribute to better understanding the experiences of women with breast cancer.
- Acknowledgments
The authors are grateful to the investigators of the Neoetic study and the Bioetic Group of the Spanish Society of Medical Oncology (SEOM) for their contribution to this study. We would like to thank all the women who generously shared their experiences with us, the support of HealthyOnco ( www.healthyonco.com ), and Priscilla Chase Duran for editing and translating the manuscript.
- Funding Statement
This work was funded by the Spanish Society of Medical Oncology (SEOM) in 2018. The sponsor of this research has not participated in the design of research, in writing the report, or in the decision to submit the article for publication.
- Data Availability
Full text links
Read article at publisher's site: https://doi.org/10.1371/journal.pone.0257680
Citations & impact
Impact metrics, citations of article over time, alternative metrics.

Article citations
Coping with breast cancer during medical and occupational rehabilitation: a qualitative study of strategies and contextual factors..
Heidkamp P , Hiltrop K , Breidenbach C , Kowalski C , Pfaff H , Geiser F , Ernstmann N
BMC Womens Health , 24(1):183, 19 Mar 2024
Cited by: 0 articles | PMID: 38504261 | PMCID: PMC10949761
I'm still me, I'm still a person: war metaphor use and meaning making in women with metastatic breast cancer.
Hulse SB , Balogun Z , Rosenzweig MQ , Marsland AL , Palmer VM
Support Care Cancer , 32(2):108, 17 Jan 2024
Cited by: 0 articles | PMID: 38231307 | PMCID: PMC10794408
" Healthcare should be the same for everyone ": perceived inequities in therapeutic trajectories of adult patients with lung cancer in Chile, a qualitative study.
Campaña C , Cabieses B , Obach A , Vezzani F
Front Public Health , 11:1228304, 16 Aug 2023
Cited by: 0 articles | PMID: 37663832 | PMCID: PMC10468573
Digital Health Literacy and Person-Centred Care: Co-Creation of a Massive Open Online Course for Women with Breast Cancer.
Álvarez-Pérez Y , Duarte-Díaz A , Toledo-Chávarri A , Abt-Sacks A , Ramos-García V , Torres-Castaño A , Rivero-Santana A , Perestelo-Pérez L
Int J Environ Res Public Health , 20(5):3922, 22 Feb 2023
Cited by: 0 articles | PMID: 36900935 | PMCID: PMC10001393
A Digital Cancer Ecosystem to Deliver Health and Psychosocial Education as Preventive Intervention.
Ciria-Suarez L , Costas L , Flix-Valle A , Serra-Blasco M , Medina JC , Ochoa-Arnedo C
Cancers (Basel) , 14(15):3724, 30 Jul 2022
Cited by: 1 article | PMID: 35954388 | PMCID: PMC9367518
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Ascertaining breast cancer patient experiences through a journey map: A qualitative study protocol.
Ciria-Suarez L , Jiménez-Fonseca P , Palacín-Lois M , Antoñanzas-Basa M , Férnández-Montes A , Manzano-Fernández A , Castelo B , Asensio-Martínez E , Hernando-Polo S , Calderon C
PLoS One , 15(12):e0244355, 21 Dec 2020
Cited by: 6 articles | PMID: 33347475 | PMCID: PMC7751958
Palliative care experiences of adult cancer patients from ethnocultural groups: a qualitative systematic review protocol.
Busolo D , Woodgate R
JBI Database System Rev Implement Rep , 13(1):99-111, 01 Jan 2015
Cited by: 11 articles | PMID: 26447011
The decision-making journey of malaysian women with early breast cancer: a qualitative study.
Abdullah A , Abdullah KL , Yip CH , Teo SH , Taib NA , Ng CJ
Asian Pac J Cancer Prev , 14(12):7143-7147, 01 Jan 2013
Cited by: 5 articles | PMID: 24460266
Long-Term Survival of Women with Breast Cancer. Overview Supportive Care Needs Assessment Instruments.
Ktistaki P , Alevra N , Voulgari M
Adv Exp Med Biol , 989:281-284, 01 Jan 2017
Cited by: 2 articles | PMID: 28971436
Patients' experience with cancer recurrence: a meta-ethnography.
Wanat M , Boulton M , Watson E
Psychooncology , 25(3):242-252, 29 Jul 2015
Cited by: 11 articles | PMID: 26224137
Funding
Funders who supported this work.
Spanish Society of Medical Oncology (1)
Grant ID: 2018
1 publication
Europe PMC is part of the ELIXIR infrastructure
Announcements
Updates on campus events, policies, construction and more.
- Dean’s 2023 State of the School address available online
- Notice of data security incident
- COVID-19: Medical Campus updates
- Affordable mental health care for employees and their children
close
Information for Our Community
Whether you are part of our community or are interested in joining us, we welcome you to Washington University School of Medicine.
- Prospective Students
- Current Students
- Alumni & Friends
- Administrators
- Researchers
- Job Seekers
AI-assisted breast-cancer screening may reduce unnecessary testing
Using AI to help doctors read mammograms reduces follow-up testing without missing cancer cases, simulation shows
by Tamara Schneider • April 10, 2024
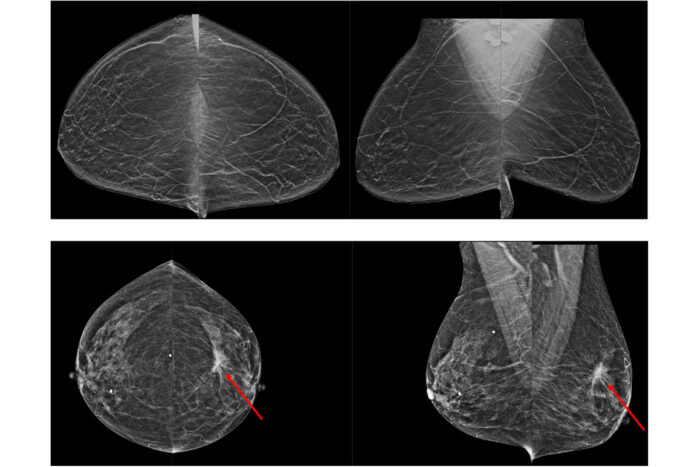
On average, radiologists find one case of cancer (bottom images) in every 200 mammograms they evaluate. The top images show no cancer. In a recent study, researchers at Washington University School of Medicine in St. Louis and Whiterabbit.ai showed that AI assistance potentially could improve breast-cancer screening by reducing the number of false positives without missing true positives.
Using artificial intelligence (AI) to supplement radiologists’ evaluations of mammograms may improve breast-cancer screening by reducing false positives without missing cases of cancer, according to a study by researchers at Washington University School of Medicine in St. Louis and Whiterabbit.ai, a Silicon Valley-based technology startup.
The researchers developed an algorithm that identified normal mammograms with very high sensitivity. They then ran a simulation on patient data to see what would have happened if all of the very low-risk mammograms had been taken off radiologists’ plates, freeing the doctors to concentrate on the more questionable scans. The simulation revealed that fewer people would have been called back for additional testing but that the same number of cancer cases would have been detected.
“False positives are when you call a patient back for additional testing, and it turns out to be benign,” explained senior author Richard L. Wahl, MD , a professor of radiology at Washington University’s Mallinckrodt Institute of Radiology (MIR) and a professor of radiation oncology. “That causes a lot of unnecessary anxiety for patients and consumes medical resources. This simulation study showed that very low-risk mammograms can be reliably identified by AI to reduce false positives and improve workflows.”
The study is published April 10 in the journal Radiology: Artificial Intelligence.
Wahl previously collaborated with Whiterabbit.ai on an algorithm to help radiologists judge breast density on mammograms to identify people who could benefit from additional or alternative screening. That algorithm received clearance from the Food and Drug Administration (FDA) in 2020 and is now marketed by Whiterabbit.ai as WRDensity.
In this study, Wahl and colleagues at Whiterabbit.ai worked together to develop a way to rule out cancer using AI to evaluate mammograms. They trained the AI model on 123,248 2D digital mammograms (containing 6,161 showing cancer) that were largely collected and read by Washington University radiologists. Then, they validated and tested the AI model on three independent sets of mammograms, two from institutions in the U.S. and one in the United Kingdom.
First, the researchers figured out what the doctors did: how many patients were called back for secondary screening and biopsies; the results of those tests; and the final determination in each case. Then, they applied AI to the datasets to see what would have been different if AI had been used to remove negative mammograms in the initial assessments and physicians had followed standard diagnostic procedures to evaluate the rest.
For example, consider the largest dataset, which contained 11,592 mammograms. When scaled to 10,000 mammograms (to make the math simpler for the purposes of the simulation), AI identified 34.9% as negative. If those 3,485 negative mammograms had been removed from the workload, radiologists would have made 897 callbacks for diagnostic exams, a reduction of 23.7% from the 1,159 they made in reality. At the next step, 190 people would have been called in a second time for biopsies, a reduction of 6.9% from the 200 in reality. At the end of the process, both the AI rule-out and real-world standard-of-care approaches identified the same 55 cancers. In other words, this study of AI suggests that out of 10,000 people who underwent initial mammograms, 262 could have avoided diagnostic exams, and 10 could have avoided biopsies, without any cancer cases being missed.
“At the end of the day, we believe in a world where the doctor is the superhero who finds cancer and helps patients navigate their journey ahead,” said co-author Jason Su, co-founder and chief technology officer at Whiterabbit.ai. “The way AI systems can help is by being in a supporting role. By accurately assessing the negatives, it can help remove the hay from the haystack so doctors can find the needle more easily. This study demonstrates that AI can potentially be highly accurate in identifying negative exams. More importantly, the results showed that automating the detection of negatives may also lead to a tremendous benefit in the reduction of false positives without changing the cancer detection rate.”
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
Editors' Picks

April 2, 2024
NIH-funded study seeks to fill gap in knowledge of exercise’s effects in people who use wheelchairs.
Medical Campus & Community, News Release

March 19, 2024
This year’s graduating class first to go completely through Gateway Curriculum.
Medical Campus & Community, Video

March 7, 2024
Ranking reflects success as thriving hub of scientific excellence, medical innovation.
Medical Campus & Community
Get the best experience and stay connected to your community with our Spectrum News app. Learn More
Continue in Browser
Get hyperlocal forecasts, radar and weather alerts.
Please enter a valid zipcode.

'My whole world came to a halt, and I was filled with fear': Breast cancer survivor shares life and hair saving treatment journey
OCOEE, Fla. — A cancer diagnoses is never an easy pill to swallow, and it’s often associated with the very difficult decision to undergo chemotherapy treatment. For Raquel Giorgio it meant exactly that, along with the daily concern of what life would look like throughout the fight she had ahead.
“My whole world came to a halt, and I was filled with fear, and I wondered if I was going to die,” Giorgio said. “I wondered if I was going to make it through chemotherapy. It was a long journey that was outlined for me, and I just wondered if I could make it through it all.”
What You Need To Know
Paxman scalp cooling is a treatment that is paired with chemotherapy treatment meant to lessen the amount of chemo that reaches the hair follicles, as a result, lessening the hair loss a patient experiences during the process officials at orlando health say the treatment is not guaranteed to work, but so far has demonstrated some success with patients raquel giorgio was diagnosed with breast cancer in 2023 and lost little to no hair during a years long journey of chemotherapy. she's crediting the paxman cooling system for helping to save her hair paxman scalp cooling treatment was not covered by insurance according to giorgio, but she says it was still worth it.
On top of those worries, Giorgio shared concerns about losing her hair, which is common for a lot of people with cancer. However, Giorgio was presented with a unique opportunity to try to save as much of her hair as possible throughout her year-long battle.
Though officials at Orlando Health said that the treatment was not guaranteed to work, Giorgio agreed to try something called the Paxman Scalp Cooling machine : a cold cap that is connected to a machine that circulates freezing cold water to the blood vessels that supply the hair follicles, lessening the amount of chemotherapy that reaches the hair follicles.

“And as a result, patients experience significantly less hair loss,” said Dr. Regan Rostorfer, an oncologist at Orlando Health .
Officials say the treatment has been successful in some cases, and the hospital has even increased the number of Paxman machines they have available. However, the journey through treatment was not an easy one, and a successful experience might not have been possible if the cancer was not caught early.
“Following the diagnosis, I called her, and I said I’m going to get a wig, and I need it to look exactly like my hair. So, we went through a series of two wigs to find the right one and colored it to look exactly like my hair and cut it to look exactly like my hair,” Giorgio said.
It wasn’t a lump in the breast or even a mammogram that helped Giorgio jump start her fight against breast cancer. Instead, it was going the extra mile and simply asking for an ultrasound.
“I didn’t feel anything,” said Giorgio. “You should get your mammogram, but when you’re at your primary care facility or at your gynecologist, you should ask for an ultrasound.”
Giorgio was diagnosed with breast cancer in 2023, but she says due to dense breast, her diagnosis might have come at a much later time.
“If we had waited for another mammogram, it would have been a year from now, and this would have been a completely different story, and I wouldn’t be as happy as I am today,” Giorgio said.
For a year, she went through chemotherapy treatment, coupled with the scalp cooling treatment. Giorgio said the process was difficult because of the intense cold on her head, but in the end, she shared it was all worth it.
“I was so scared that I’d look like a cancer patient and I would venture to say that throughout this whole time, I’ve managed to look just like myself, and that made me feel a little more normal,” she said.
“We’d wet my hair down, and it would be completely wet. We then had to put conditioner on it, and then you put this cap on that you have to get as tight as possible because if it’s not tight, it’s not going to work. And if we’re going to go through all of this, we’re going to make sure it works,” Giorgio said.
Most treatments started with an hour-and-a-half of allowing the treatment to freeze her head first before the chemo treatment would be started. After sitting through chemo for about an hour to an hour and-a-half, Giorgio said she sat another hour-and-a-half to allow the scalp cool treatment to defrost. The treatment is also not covered by insurance and ranges in pricing from $100 to $350.
Though the diagnosis and the journey to beat cancer was not something Giorgio could have ever imagined for herself, she says she was blessed to have a support system that helped to keep her optimistic, and with the scalp cooling treatment successfully helping to retain her hair, looking good helped her to feel good throughout her process.

IMAGES
VIDEO
COMMENTS
A map of the breast cancer patient's journey will enable healthcare professionals to learn first-hand about their patients' personal experiences and needs at each stage of the disease, improve communication and doctor-patient rapport, thereby creating a better, more person-centered environment. Importantly, understanding the transitional ...
Background: Breast cancer is one of the most prevalent diseases in women. Prevention and treatments have lowered mortality; nevertheless, the impact of the diagnosis and treatment continue to impact all aspects of patients' lives (physical, emotional, cognitive, social, and spiritual). Objective: This study seeks to explore the experiences of the different stages women with breast cancer go ...
Objective: This study seeks to explore the experiences of the different stages women with breast cancer go through by means of a patient journey. Methods: This is a qualitative study in which 21 women with breast cancer or survivors were interviewed. Participants were recruited at 9 large hospitals in Spain and intentional sampling methods were ...
Background: The current cancer care system must be improved if we are to have in-depth knowledge about breast cancer patients' experiences throughout all the stages of their disease. Aim: This study seeks to describe breast cancer patients' experience over the course of the various stages of illness by means of a journey model. Methods: This is a qualitative descriptive study. Individual ...
Aim: This study seeks to describe breast cancer patients' experience over the course of the various stages of illness by means of a journey model. Methods: This is a qualitative descriptive study. Individual, semi-structured interviews will be administered to women with breast cancer and breast cancer survivors.
cer go through by means of a patient journey. Methods. This is a qualitative study in which 21 women with breast cancer or survivors were inter-. viewed. Participants were recruited at 9 large ...
The journey of patients with breast cancer through the healthcare system is described to establish baseline data that will serve as the basis for the development and implementation of a patient-centered, evidence-based clinical pathway.
Breast Cancer Diagnosis Surgical Pathology Report Available Surgery Survivorship Clinic ... clinical knowledge who offers individualized assistance to patients, families, and caregivers such as: Nurse Navigator ... ˜ Psychosocial Support ˜ Community Resources ˜ Barriers to Care. Title: Breast Cancer Journey Map_FINAL Created Date: 2/7/2022 1 ...
A breast cancer patient journey map will enable health care professionals to gain first-hand. knowledge about their patients' personal experiences, enhance communication and under-
Europe PMC is an archive of life sciences journal literature.
The journey of patients with breast cancer through the healthcare system is described to establish baseline data that will serve as the basis for the development and implementation of a patient-centered, evidence-based clinical pathway. Background The current cancer care system must be improved if we are to have in-depth knowledge about breast cancer patients' experiences throughout all the ...
Patient Journey Map from the Time of Breast Cancer Diagnosis Systemic Treatment • Chemotherapy or Targeted Therapy (3-12 months) • Hormone Therapy (up to 10 years) Radiation Treatment • Palliative or Symptom (3-5 weeks) Control and Comfort • Traditional Treatment Breast Cancer Diagnosis 1 Surgical Consults (see Section C) 2 2 weeks ...
The NBCF Patient Navigator Program is a proactive approach to helping patients overcome the barriers of cost, fear, and misinformation surrounding a disease and its prevention. By helping underserved women to navigate the healthcare system, navigators provide the vision that gives women hope. Services that navigators provide include:
A map of the breast cancer patient's journey will enable healthcare professionals to learn first-hand about their patients' personal experiences and needs at each stage of the disease, improve communication and doctor-patient rapport, thereby creating a better, more person-centered environment.
This guide will help inform and empower you during your treatment for breast cancer. Download the entire PDF file, or choose the chapters that most interest you. This information isn't meant to replace the attention and advice from your medical team so be sure to bring up any questions with them. We're here to help.
Clinical Presentation of Patients Diagnosed with Early Breast Cancer. EP: 2. Patient Journey Amid Breast Cancer Diagnosis. EP: 3. Unmet Needs in Breast Cancer Treatment. EP: 4. Navigating Updates ...
Informed by actual patient quotes, the map shows common overall themes for cancer patients, concerns at key treatment points, strategies for patient engagement, and targeted behavioral goals. ... The journey of patients with breast cancer through the healthcare system is described to establish baseline data that will serve as the basis for the ...
The Journal of Oncology Navigation & Survivorship (JONS) promotes reliance on evidence-based practices in navigating patients with cancer and their caregivers through diagnosis, treatment, and survivorship.JONS also seeks to strengthen the role of nurse and patient navigators in cancer care by serving as a platform for these professionals to disseminate original research findings, exchange ...
The work of the Lancet Breast Cancer Commission highlights crucial groups, such as those living with metastatic breast cancer, and identifies how the hidden costs of breast cancer and associated suffering are considerable, varied, and have far-reaching effects. The Commission offers a forward-looking and optimistic road map for how the health ...
W hile treatments for metastatic breast cancer (MBC) have progressed significantly in recent decades, there remains an opportunity to provide patients with more flexibility and options in where ...
Our highly trained specialists are available 24/7 via phone and on weekdays can assist through video calls and online chat. We connect patients, caregivers, and family members with essential services and resources at every step of their cancer journey. Ask us how you can get involved and support the fight against cancer.
Empowering Breast Cancer Patients is a comprehensive mobile application designed to provide invaluable support and resources for individuals diagnosed with breast cancer. This user-friendly app serves as a personalized companion throughout the cancer journey, offering a range of features to enhance patient care and well-being.
Breast cancer is the most common cancer and the one that associates the highest mortality rates among Spanish women, with 32,953 new cases estimated to be diagnosed in Spain in 2020 [ 1 ]. Thanks to early diagnosis and therapeutic advances, survival has increased in recent years [ 2 ]. The 5-year survival rate is currently around 85% [ 3, 4 ].
"At the end of the day, we believe in a world where the doctor is the superhero who finds cancer and helps patients navigate their journey ahead," said co-author Jason Su, co-founder and chief technology officer at Whiterabbit.ai. "The way AI systems can help is by being in a supporting role.
The Paxman Scalp Cooling machine allows cancer patients to experience less hair loss when undergoing chemotherapy. (Spectrum News/Jaclyn Harold) "And as a result, patients experience ...