- Newsletters
- FAC Articles


Working from home?
Keep your critical coding and billing tools with you no matter where you work.
Create your Find-A-Code account today!
Find-A-Code Articles, Published 2021, September 28
When is it proper to bill nurse visits using 99211.
by Christine Woolstenhulme, QMC QCC CMCS CPC CMRS Sep 28th, 2021 - Reviewed/Updated Aug 29th
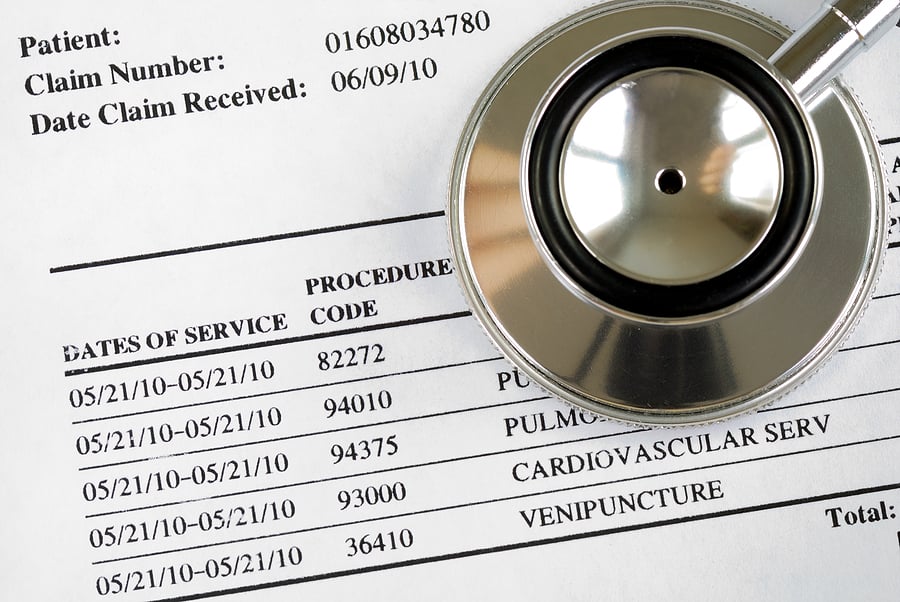
When vaccines or injections are given in the office, coding can often get confusing; for example, is it correct to report a nurse visit using 99211 and an E/M office visit reporting 99202 ‑ 99215 and include injection fees with the vaccine product? In addition, the reporting of evaluation and management (E/M) during the same visit where vaccines are administered is not always understood. The answer depends on whether the provider performs a medically necessary and significant, separately identifiable E/M visit, in addition to the immunization administration.
CMS states, when a separately identifiable E/M service (which meets a higher complexity level than CPT code 99211 ) is performed, in addition to drug administration services, you should report the appropriate E/M CPT code reported with modifier -25. Documentation should support the level of E/M service billed. For an E/M service provided on the same day, a different diagnosis is not required.
It is incorrect to bill a 99211 when the provider provides an E/M service that meets a higher complexity level than CPT code 99211 , you must bill the higher complexity, and you cannot bill for two services in one day.
Charging for Nurse Visits
There are times when it is appropriate to report for a nurse visit using CPT code 99211 . The Incident-to rule applies when reporting this code, and services provided must be documented as medically necessary services, including the clinical history, clinical exam, making a clinical decision, and physician supervision.
- NOTE: A nurse visit is not paid if billed with a drug administration service such as chemotherapy or non-chemotherapy drug infusion code, including therapeutic or diagnostic injection codes. The reasoning is because diagnostic IV infusion or injection services typically require direct physician supervision, and using 99211 is reported by qualified healthcare professionals other than physicians.
08/29/2023 NOTE: (These CPT codes,90782, 90783, 90784, or 90788 were deleted in 2006, but still showing in CMS - Claims processing manual) When reporting CPT codes 90782, 90783, 90784, or 90788 , CPT code 99211 cannot be reported. In addition, it is improper billing to report a visit solely for an injection that meets the definition of the injection codes.
When the only reason for the visit is for the patient to receive an injection, payment may be made only for the injection (if it is covered). An office visit using 99211 would not be warranted where the services rendered did not constitute a regular office visit and a part of the plan of care and not at the patient's request.
Unlike other E/M codes 99202 - 99205 , and 99212 - 99215 , time alone cannot be used when reporting 99211 when selecting the appropriate code level for E/M services. Effective January 1, 2021, time was removed as an available code-selection criterion. The typical time spent on this code is five minutes.
Other visits billed with 99211
Several other visits may be reported using 99211 , and nurses are not the only staff that can report this code; medical Assistants and technicians are also included under non-physician.
Covid-19 Testing
According to CMS ; Physician offices can use CPT code 99211 when office clinical staff furnish assessment of symptoms and specimen collection for Covid-19 incident to the billing professionals services for both new and established patients. When the specimen collection is performed as part of another service or procedure, such as a higher-level visit furnished by the billing practitioner, that higher-level visit code should be billed. The specimen collection would not be separately payable.
Examples from CMS
The following are examples of when CPT 99211 might be used:
- Office visit for an established patient for blood pressure check and medication monitoring and advice. History, blood pressure recording, medications, and advice are documented, and the record establishes the necessity for the patient's visit.
- Office visit for an established patient for return to work certificate and advice (if allowed to be by other than the physician). Exam and recommendation are noted, and the Return to Work Certificate is completed, copied, and placed in the record.
- Office visit for an established patient on regular immunotherapy who developed wheezing, rash, and swollen arm after the last injection. Possible dose adjustments are discussed with the physician, and an injection is given. History, exam, dosage, and follow-up instructions are recorded.
- Office visit for an established patient's periodic methotrexate injection. Monitoring Lab tests, query signs and symptoms, obtain vital signs, repeat testing, and injection advised. All this information is recorded and reviewed by the physician. (Note that in this circumstance, if 99211 is billed, the injection code is not separately billable). An office visit for an established patient with a new or concerning bruise is checked by the nurse (whether or not the patient is taking anticoagulants), and the patient is advised on how to care for the bruise and what to be concerned about, and, if on anticoagulants, continuing or changing current dosage is advised. History, exam, dosage, and instructions are recorded and reviewed by the physician.
- Office visit for an established patient with atrial fibrillation who is taking anticoagulants and has no complaints . The patient is queried by the nurse, vital signs are obtained, the patient is observed for bruises and other problems, the prothrombin time is obtained, the physician is advised of prothrombin time and medication dose, and medication is continued at present dose with follow up prothrombin time in one month recommended. History, vital signs, exam, prothrombin time, INR, dosage, physician's decision, and follow-up instructions are recorded.
References/Resources
About christine woolstenhulme, qmc qcc cmcs cpc cmrs.
Christine Woolstenhulme, CPC, QCC, CMCS, CMRS, is a Certified coder and Medical Biller currently employed with Find-A-Code. Bringing over 30 years of insight, business knowledge, and innovation to the healthcare industry. Establishing a successful Medical Billing Company from 1994 to 2015, during this time, Christine has had the opportunity to learn all aspects of revenue cycle management while working with independent practitioners and in clinic settings. Christine was a VAR for AltaPoint EHR software sales, along with management positions and medical practice consulting. Understanding the complete patient engagement cycle and developing efficient processes to coordinate teams ensuring best practice standards in healthcare. Working with payers on coding and interpreting ACA policies according to state benchmarks and insurance filings and implementing company procedures and policies to coordinate teams and payer benefits.
When is it Proper to Bill Nurse Visits using 99211. (2021, September 28). Find-A-Code Articles. Retrieved from https://www.findacode.com/articles/nurse-visits-and-injections-36866.html
Article Tags (click on a tag to see related articles)
Thank you for choosing Find-A-Code, please Sign In to remove ads.


7 Resources for Nurse Practitioners to Decode Primary Care Billing and Coding
Home / Nurse Practitioner Articles / 7 Resources for Nurse Practitioners to Decode Primary Care Billing and Coding
Page Sections
Coding basics, evaluation/management coding, transition of care billing and coding, medicare wellness coding and billing, pediatric coding and billing.
From insurance reimbursement and billing to coding and audits, these responsibilities can leave any healthcare provider with goosebumps – especially those who work in or own their own private practice. The most stressful part, in relation to insurance reimbursement, is that most healthcare providers like nurse practitioners are not formally trained in billing and coding and work in a clinical setting or facility with no certified billing and coding specialists. Luckily, there are a wide variety of resources available to help decode this unfamiliar territory.
Accurate coding is critical for insurance reimbursement, succinct documentation, and identifying clinical care gaps. The Healthcare Common Procedure Coding System (HCPCS) codes and International Classification of Diseases, 10th Revision (ICD-10) codes serve as the building blocks of medical coding.
- Category I: Common procedures
- Category II: Performance measurements
- Category III: Emerging technologies
- HCPCS Level II codes: These codes are used to describe products, supplies, and services provided during an encounter.
- ICD-10 codes: These codes are used to describe the reason for a patient encounter or outline a patient's characteristics, and are essential for identifying common diagnoses in a medical practice. They notify the insurance payer of the medical necessity of the visit.
Evaluation/Management (E/M) coding is the core of healthcare billing and insurance reimbursement. Understanding E/M coding can help maximize the insurance reimbursement of a practice and reduce stress levels during audits. These codes are based on several factors :
- The patient's history
- The patient's physical exam
- The provider's medical decision making
- The appointment time, specifically if the provider spent 50% of the visit coordinating care or counseling
There are different levels for the aforementioned factors, which decipher which E/M code to use.
- Problem-focused
- Expanded problem-focused
- Comprehensive
- Straightforward
- Low complexity
- Moderate complexity
- High complexity
The level of complexity related to medical decision making depends on the number of diagnoses and management options, the complexity of the patient data that was reviewed, and the risk of complications or morbidity/mortality.
Transition of care visits are an efficient way to support the continuity of care after a patient is discharged from a skilled nursing facility/nursing facility, long-term acute care hospital, rehabilitation hospital, acute care hospital, or observation stay in a hospital. A transition of care visit can only be billed one time per patient in a 30-day timeframe, and can be billed for both new and established patients at a particular clinic.
Transition of care visits can be billed using two different codes.
- 99495- This code can only be used if the patient has been contacted within two business days of their discharge, the medical decision making is of moderate complexity, and there is an in-person clinic visit within 14 days of the discharge.
- 99496- This code is used if the patient has been contacted within two business days of their discharge, the medical decision making is of high complexity, and there is an in-person clinic visit within seven days of the discharge.
Medicare wellness exams go beyond a typical annual adult wellness examination. In addition to focusing on a patient's wellness, these exams involve a thorough screening centered around disease prevention. The exam also takes a more comprehensive look at the patient's vital signs, medical/family history, and health risk assessments including their emotional and psychological well-being to develop a personalized prevention plan. Many types of healthcare providers can complete these wellness exams, including:
- Physician assistants
- Nurse practitioners
- Clinical nurse specialists
- Registered dietitians
- A team of medical professionals with an overseeing physician
RELATED: Complete Guide to the Adult-Gerontology Nurse Practitioner Specialty
Accurate coding for the pediatric population is similar to the process for the adult population with several additional considerations including behavior screenings, developmental screenings, and vaccine administration . Another complication is that not all of these screenings and vaccines are completed at every age. Each well child examination typically has different screenings and different vaccine administrations or they may not have any vaccines at all. That's why it is important to follow the recommendations of Bright Futures, which establishes guidelines that insurances follow.
RELATED: Complete Guide to the Pediatric Nurse Practitioner Specialty
Initially, the billing and coding world can be daunting and confusing. Luckily, there are a variety of resources available to help providers make sense of this information. In addition to online resources, there are several textbooks and conferences that can strengthen a provider's knowledge of accurate billing and coding. Accessing the right resources can help providers boost their understanding, which leads to more efficient documentation, increased reimbursement, and decreased stress during chart audits.
- Recent Posts
- 4 Essential Projects to Improve Primary Care Office Flow for Nurse Practitioners - October 31, 2020
- Keeping Your Sanity: How to Prevent Nurse Practitioner Burnout - October 6, 2020
- How NPs Can Tackle Difficult Conversations with Patients and Families - September 30, 2020
Related Articles
- Have You Seen “FAANP” After a Nurse Practitioner’s Credentials and Wondered What It Means?
- Is a Nurse Practitioner Residency Program for You? Weighing the Odds and the Need for Programs in Every State
- The Personality Pandemic: Managing 6 Common Character Traits During COVID-19
- Conquer Uniqueness: 5 Novel Ways to Educate Yourself and Expand Your Advanced Practice Nursing Career
- How NPs Can Tackle Difficult Conversations with Patients and Families
- Is A ‘Locum Tenens’ Job For You? The Pros and Cons for Nurse Practitioners

The Billing and Coding Course
Feel confident choosing the correct Evaluation and Management CPT® code for an outpatient, inpatient/obs, ER, nursing facility setting, so you can avoid over coding ( and under coding! ) ensuring you receive proper insurance reimbursement!
Did you learn how to properly bill and code in nurse practitioner school?
Yeah, me neither…
And yet choosing the correct Evaluation and Management code is so important in your work as a nurse practitioner.
Are you a nurse practitioner who is
- Unsure of medical coding terminology and the billing and coding process?
- Apprehensive about choosing the correct Evaluation and Management code?
- Afraid of overbilling or even underbilling?
- Not aware of additional ways to maximize RVUs (what is a RVU anyways?) and missing out on some serious $$?
The Nurse Practitioner Billing and Coding Course
Feel confident choosing the correct Evaluation and Management CPT® code for an outpatient, inpatient/obs, ER, nursing facility visit, so you can avoid over coding ( and under coding! ) ensuring you receive proper insurance reimbursement !

Hi I’m Erica D the NP
A family nurse practitioner and creator of The Burned-out Nurse Practitioner and The Nurse Practitioner Charting School.
I don’t know about you, but I had a 30 minute training on billing and coding in my nurse practitioner program.
I learned very little about choosing an evaluation and management code, let alone if I was doing it correctly.
When I first started working as a family nurse practitioner, I again did not receive adequate training to ensure I was doing it right. I had to spend the extra time and teach myself how nurse practitioners should code patient visits.
And then in 2021 and 2023, everything changed. The updates of the Evaluation and Management codes for the outpatient, inpatient/obs, ER, and nursing facility settings were much different than what I originally learned.
Again, I did not receive much training and had to learn the new guidelines myself.
If you work as an APRN and are confused as I was , you are in the right place!
I have created The Nurse Practitioner Billing and Coding Course to ease your stress and give you the confidence to practice as a nurse practitioner!
This course will help you
- Learn the basic billing and coding terminology so you can be ready to code as a nurse practitioner
- Determine how to choose the correct Evaluation and Management code in the outpatient, inpatient/obs, ER, and nursing facility setting
- Learn from real life charting examples and gain the confidence to properly code a patient encounter

Do-It-Yourself Option
Take the course independently, learn the basics of billing and coding and implement into your practice!
One time payment of $197
- STOP Charting at Home Membership
Join the all-access STOP Charting at Home Membership to get the course plus so much more!
Monthly payment of $197

What's included?
This instant access, online course offers 75 minutes of video training (broken down into easy to consume lessons) teaching you the basics of coding in the outpatient, inpatient/obs, ER, and nursing facility setting !
Coding and Billing Terminology: Discover the lingo and process of coding and billing patient encounters. (11 minutes video lesson)
Introduction to Coding: Learn the things you didn’t learn in nurse practitioner school! (14 minute video lesson)
Coding by Medical Decision Making: A complete breakdown of how to select each evaluation and management CPT® code using medical decision making. (30 minute video lesson)
Coding by Time and Prolonged Services: This lesson covers the coding by time and the 2021 and 2023 changes to the Evaluation and Management Codes. (11 minute video lesson)
Practice Coding Examples: We will discuss real world examples and learn to code using evaluation and management levels 99202-99205 and 99211-99215. (9 minute video lesson)
Plus a bonus:
6 Tips to Maximize RVUs!
Check out these 6 tips (available via PDF) to increase your Relative Value Units (RVUs) (and learn what an RVU actually is)!
Hello more $$$

Includes 1.5 continuing education hours!!
The Billing and Coding Course offers 1.5 CE hours.
This course is approved for continuing education hours through The Elite Nurse Practitioner. The Elite Nurse Practitioner is an accredited educator of nursing continuing education through the American Nurses Credentialing Center’s Commission on Accreditation.
"This course was a life saver"
Feel confident choosing the correct Evaluation and Management CPT® code for a patient visit, so you can avoid over coding ( and under coding! ) ensuring you receive proper insurance reimbursement!
Did I mention it’s risk-free?
The Nurse Practitioner Billing and Coding Course Guarantee
I offer a 100% money back guarantee. If you’re not satisfied within 7 days of purchasing the program, I will give you your money back– hassle free! I believe in the value of this program and the information is something I have used personally. I strive to help overwhelmed NPs learn how to properly code a patient visit! But I also know it may not be right for you! Be sure to reach out if you have any questions or concerns. Email [email protected] if you are not satisfied with the program and a refund will be granted!

Frequently Asked Questions
This course covers the basics of choosing an evaluation and management level as a nurse practitioner. It is perfect for nurse practitioner students, new grads, or experienced nurse practitioners who are not quite sure how to properly code.
Evaluation and Management updates for outpatient visits occurred in 2021. Evaluation and Management updates for inpatient/obs, ER, and nursing facility went into place in 2023. This course discusses all updates is and geared towards all nurse practitioners!
I realize what worked for me and other nurse practitioners I have worked with may not work for you! Please see The NP Billing and Coding Course Guarantee listed above.
Ask your employer to cover the cost! I have had many NPs ask their boss to purchase the course or had it included as their continuing education money!
The Billing and Coding Course benefits both you and your employer!
I mean, what kind of boss wouldn’t want their nurse practitioner to ensure they are properly coding the patient encounter. The knowledge gained in this course means more money for the employer and increased value for the nurse practitioner!
This course is approved for continuing education hours through The Elite Nurse Practitioner . The Elite Nurse Practitioner is an accredited educator of nursing continuing education through the American Nurses Credentialing Center’s Commission on Accreditation.
If you are ready to:
- Implement the actionable information into your current practice
- Feel confident choosing the correct Evaluation and Management code
- And increase your knowledge and overall worth as a nurse practitioner
The Nurse Practitioner Billing and Coding Course is for you!
Do-it-yourself.
Take the course independently, learn the basics of billing and coding, and implement into your practice!

- Privacy Policy
- Terms and Conditions and Legal Disclaimer
Our Courses
- 4 Charting Tips to Get Time Back (free training)
- Smart Phrases for Nurse Practitioners
- Time Management and Charting Tips Course
- Basics of Billing and Coding
- Legal Issues with Charting Course
- Save time charting with Freed AI
- The Nurse Practitioner Charting School
- @npchartingschool


Coding for E/M home visits changed this year. Here’s what you need to know
CPT has revised codes for at-home evaluation and management (E/M) services as of Jan. 1, 2023. Services to patients in a private residence (e.g., house or apartment) or temporary lodgings (e.g., hotel or shelter) are now combined with services in facilities where only minimal health care is provided (e.g., independent or assisted living) in these code families:
Home or residence E/M services, new patient
• 99341, straightforward medical decision making (MDM) or at least 15 minutes total time,
• 99342, low level MDM or at least 30 minutes total time,
• 99344 (code 99343 has been deleted), moderate level MDM or at least 60 minutes total time,
• 99345, high level MDM or at least 75 minutes total time.
Home or residence services, established patient
• 99347, straightforward MDM or at least 20 minutes total time,
• 99348, low level MDM or at least 30 minutes total time,
• 99349, moderate level MDM or at least 40 minutes total time,
• 99350, high level MDM or at least 60 minutes total time.
Select these codes based on either your level of medical decision making or total time on the date of the encounter , similar to selecting codes for office visits . The E/M codes specific to domiciliary, rest home (e.g., boarding home), or custodial care (99324-99238, 99334-99337, 99339, and 99340) have been deleted, and the above codes should also be used in those settings.
When total time on the date of the encounter exceeds the threshold for code 99345 or 99350 by at least 15 minutes, you can add code 99417 to report prolonged services. The exception to this is for patients with Medicare. For those patients, report prolonged home or residence services to Medicare with code G0318 in addition to 99345 (requires total time ≥140 minutes) or 99350 (requires total time ≥110 minutes). Code G0318 is not limited to time on the date of the encounter, but includes any work within three days prior to the service or within seven days after.
Services provided in facilities where significant medical or psychiatric care is available (e.g., nursing facility, intermediate care facility for persons with intellectual disabilities, or psychiatric residential treatment facility) are reported with codes 99304-99310 .
— Cindy Hughes, CPC, CFPC
Posted on Jan. 19, 2023
- Chronic care
- Medicare/Medicaid
- Physician compensation
- Practice management
- Reimbursement
- Value-based payment
Other Blogs
- Quick Tips from FPM journal
- AFP Community Blog
- Fresh Perspectives
- In the Trenches
- Leader Voices
- RSS ( About RSS )
Disclaimer: The opinions and views expressed here are those of the authors and do not necessarily represent or reflect the opinions and views of the American Academy of Family Physicians. This blog is not intended to provide medical, financial, or legal advice. Some payers may not agree with the advice given. This is not a substitute for current CPT and ICD-9 manuals and payer policies. All comments are moderated and will be removed if they violate our Terms of Use .
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

- Become a Member
- Everyday Coding Q&A
- Can I get paid
- Coding Guides
- Quick Reference Sheets
- E/M Services
- How Physician Services Are Paid
- Prevention & Screening
- Care Management & Remote Monitoring
- Surgery, Modifiers & Global
- Diagnosis Coding
- New & Newsworthy
- Practice Management
- E/M Rules Archive
April 25, 2024
Non-Physician Practitioners in Nursing Facilities
Find additional information about nursing facility services Everyday Coding .
Can a physician assistant see patients in a nursing facility without a physician signing each encounter? How do we bill this? Can we do wellness visits in a nursing facility?
- A physician assistant or an advanced practice registered nurse may see patients independently in a nursing facility but must bill under their own provider number. Beginning 1-1-2022, visits that are not mandated as physician services may be reported as shared services between a physician and a non-physician practitioner.
- Mandated visits: Only a physician may bill the initial nursing facility visits 99304-99306 in a skilled nursing facility or nursing facility. (There is an exception to this in a nursing facility who is not employed by the facility). Sometimes, the PA/NP sees the patient at an earlier date than the physician, who comes and does the admission. In that case, the PA/NP bills a subsequent visit, even though the initial has not been billed. This is a Medicare rule.
- I am not aware of any restrictions against billing wellness visits in the nursing facility, provided it is appropriate to do a preventive plan for the patient.
Here is a link to the MedLearn matters article . It discusses frequency of mandated physician visits.
Back to Everyday Coding Q&A
Get more tips and coding insights from coding expert Betsy Nicoletti.
Subscribe and receive our FREE monthly newsletter and Everyday Coding Q&A.
We will never share your email address. unsubscribe anytime..
CPT is a registered trademark of the American Medical Association Copyright 2019, American Medical Association All rights reserved.
Last revised April 8, 2024 - Betsy Nicoletti Tags: medicare incident-to and shared services
CPT®️️ is a registered trademark of the American Medical Association. Copyright American Medical Association. All rights reserved.
All content on CodingIntel is copyright protected. Any resource shared within the permissions granted here may not be altered in any way, and should retain all copyright information and logos.
- What is CodingIntel
- Terms of Use
- Privacy Policy
Our mission is to provide up-to-date, simplified, citation driven resources that empower our members to gain confidence and authority in their coding role.
In 1988, CodingIntel.com founder Betsy Nicoletti started a Medical Services Organization for a rural hospital, supporting physician practice. She has been a self-employed consultant since 1998. She estimates that in the last 20 years her audience members number over 28,400 at in person events and webinars. She has had 2,500 meetings with clinical providers and reviewed over 43,000 medical notes. She knows what questions need answers and developed this resource to answer those questions.
Copyright © 2024, CodingIntel A division of Medical Practice Consulting, LLC Privacy Policy

IMAGES
VIDEO
COMMENTS
Categories for Common CPT Codes. Common CPT codes will fall under the following categories (as quoted from the AMA): "Category I - These codes have descriptors that correspond to a procedure or service. Codes range from 00100-99499 and are generally ordered into sub-categories based on procedure/service type and anatomy.
CPT® code 99211 Office or other outpatient visit for the evaluation and management ... The services are rendered under the direct supervision of the physician or nonphysician practitioner (NPP) (i.e., nurse practitioner (NP), certified nurse-midwife (CNM), clinical nurse specialist (CNS), or in the case of a physician-directed clinic, the ...
Updated Guidelines for Billing and Coding for Nurse Practitioners. Watch on. Get your updated Billing and Coding Cheat Sheet here! More Resources 👇. Evaluation and Management of Services Guidelines. CPT® Evaluation and Management (E/M) Office or Other Outpatient (99202-99215) and Prolonged Services (99354, 99355, 99356, 99417) Code and ...
Whenever you report 99211, the provider should document the reason for the visit, along with any other pertinent details. Also, make sure you have the date of service, the reason for the visit, proof that the nurse performed the service per the physician's order, and the nurse's legible signature. Tip 2: Be Familiar With 99211 Components.
JAMES M. GIOVINO, MD. Fam Pract Manag. 2000;7 (7):39-42. Level-one" office visits may be the simplest of patient encounters, but when it comes to coding and documentation, they are widely ...
Using CPT code 99211 can boost your practice's revenue and improve documentation. The requirements for most evaluation and management (E/M) codes have gotten more precise over the years. However ...
How to accurately bill for new and established office visits (primary care only!) The key differences between levels 3&4 (and the most common pitfall I see!) A few patient examples to apply it to (and a walk-through of the plug-and-go cheat sheet) Download the Billing and Coding for Nurse Practitioners Cheat Sheet Below 👇
Step 1: Total time. Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if ...
The Nurse Practitioner Charting School- The one stop for all documentation resources made specifically for nurse practitioners. Offering online courses: Time Management and Charting Tips Course, Billing and Coding Course: Outpatient Visits, Legal Issues with Documentation Course, Or get all three courses together in The NP Charting Courses ...
CPT® code 99212: Established patient office or other outpatient visit, 10-19 minutes. As the authority on the CPT® code set, the AMA is providing the top-searched codes to help remove obstacles and burdens that interfere with patient care. These codes, among the rest of the CPT code set, are clinically valid and updated on a regular basis to ...
Unlike other E/M codes 99202-99205, and 99212-99215, time alone cannot be used when reporting 99211 when selecting the appropriate code level for E/M services. Effective January 1, 2021, time was removed as an available code-selection criterion. The typical time spent on this code is five minutes. Other visits billed with 99211.
Transition of Care Billing and Coding . Transition of care visits are an efficient way to support the continuity of care after a patient is discharged from a skilled nursing facility/nursing facility, long-term acute care hospital, rehabilitation hospital, acute care hospital, or observation stay in a hospital. A transition of care visit can ...
The Billing and Coding Course offers 1.5 CE hours. This course is approved for continuing education hours through The Elite Nurse Practitioner. The Elite Nurse Practitioner is an accredited educator of nursing continuing education through the American Nurses Credentialing Center's Commission on Accreditation. I'm ready to code these charts!
Billing for shared/split services allows the practice to bill under the qualified physician versus the NPP at their lower reimbursement rate. As long as the criteria are met, billing for shared/split services allows for that extra 15% reimbursement. Documentation is paramount in this type of billing. Each practitioner must thoroughly document ...
By G.J. Verhovshek, MA, CPC. A letter to the editor in the July 2012 Coding Edge, ("New vs. Established Patient Rule Applies to Physicians Only," page 10) asked how the "new vs. established patient" rule applies to visits by nurse practitioners (NP). In response, Coding Edge editors—specifically, this editor—responded that an NP ...
Insurance reimbursement coding is based on the American Medical Association CPT. 2. coding system. Under that system, the only Evaluation and Management (E/M) code that a Registered Nurse can bill to is 99211. CPT defines this code as an "office or other outpatient visit for the
Certified Nurse Assistant (CNA) Licensed Practicing Nurse (LPN) Registered Nurse (RN) Nurse Practitioner (NP) Physician Assistant (PA) Physician (MD). Prevent Denials, Prove Medical Necessity for CPT Code 99211. One of the big reasons CPT 99211 is denied is because clinicians don't meet the medical necessity requirement.
The E/M codes specific to domiciliary, rest home (e.g., boarding home), or custodial care (99324-99238, 99334-99337, 99339, and 99340) have been deleted, and the above codes should also be used in ...
A: The 99211 E/M visit is a nurse visit and should be used only by a medical assistant or a nurse when performing services such as wound checks, dressing changes or suture removal. CPT code 99211 should never be billed for physician, physician assistant or nurse practitioner services.
Coding Guidelines. Home/domiciliary services provided for the same diagnosis, same condition or same episode of care as services provided by other practitioners, regardless of the site of service, may constitute concurrent or duplicative care. When such visits are provided, the record must clearly document the medical necessity of such services.
Home and Domiciliary Visits. Home and domiciliary visits are when a physician or qualified non-physician practitioner (NPPs) oversee or directly provide progressively more sophisticated evaluation and management (E/M) visits in a beneficiary's home. This is to improve medical care in a home environment. A provider must be present and provide ...
Payable under FQHC prospective payment system (PPS). Codes G0469 and G0470 must be reported with a qualifying visit code (e.g., 90791, 90792, 90832-90839, 90845) FQHC (provider-based and free-standing) claims submitted on a 77X type of bill. Mental health visit codes G0469 and G0470 must be reported with revenue code 0900 or 0519.
Beginning 1-1-2022, visits that are not mandated as physician services may be reported as shared services between a physician and a non-physician practitioner. Mandated visits: Only a physician may bill the initial nursing facility visits 99304-99306 in a skilled nursing facility or nursing facility. (There is an exception to this in a nursing ...