
FOLASHADE S. OMOLE, MD, CHARLES M. SOW, MD, MSCR, EDITH FRESH, PhD, DOLAPO BABALOLA, MD, AND HARRY STROTHERS, III, MD, MMM
Am Fam Physician. 2011;84(7):780-784
Patient information: See related handout for family members at office visits , written by the authors of this article.
Author disclosure: No relevant financial affiliations to disclose.
The physician-patient relationship is part of the patient's larger social system and is influenced by the patient's family. A patient's family member can be a valuable source of health information and can collaborate in making an accurate diagnosis and planning a treatment strategy during the office visit. However, it is important for the physician to keep an appropriate balance when addressing concerns to maintain the alliance formed among physician, patient, and family member. The patient-centered medical home, a patient care concept that helps address this dynamic, often involves a robust partnership among the physician, the patient, and the patient's family. During the office visit, this partnership may be influenced by the ethnicity, cultural values, beliefs about illness, and religion of the patient and his or her family. Physicians should recognize abnormal family dynamics during the office visit and attempt to stay neutral by avoiding triangulation. The only time neutrality should be disrupted is if the physician suspects abuse or neglect. It is important that the patient has time to communicate privately with the physician at some point during the visit.
The physician-patient relationship is part of the patient's larger social system and is influenced by members of the patient's family. 1 There are several relationship dynamics involved in this context, such as those between the physician and the patient, the patient and his or her family, the physician and the patient's family, and the patient and society. 2 Patients often believe that the presence of a family member leads to an atmosphere of greater empathy and compassion from the professional health care team. 3 , 4 The purpose of this article is to identify and understand each person's role during an office visit when the patient is accompanied by a family member.

Definition of Family
Considering the growing cultural diversity with traditional and nontraditional families, the term “family” could be defined as any group of persons who are related biologically, emotionally, or legally. 1 , 5 Examples of nontraditional families are blended families, unmarried couples, and gay and lesbian couples or families. 1 , 6 , 7 Family members who may accompany a patient to an office visit include children, siblings, parents, spouses or significant others, hired caregivers, interpreters, neighbors, friends, and clergy or church members.
Managing the Office Visit
Family members are present about one-third of the time in the examination room, 8 and their presence usually prolongs the visit by only a few minutes. 9 Those more likely to have a family member present include patients with a low level of health literacy, patients with a chronic disease, older patients, women, gay or lesbian patients, non–English-speaking patients, and children. 6 , 7
The background of the patient's family (e.g., ethnicity, cultural values, religion, attitudes and beliefs about illness) is ever-present during the office visit, and this plays a role in the patient's decision making. 1 The patient and his or her family member mutually influence each other and the patient-physician relationship, creating a therapeutic triangle. 10
THE FAMILY MEMBER'S ROLE
There are a variety of reasons why a family member may accompany a patient to an office visit. It is common for a family member to be there to offer support during visits that may involve receiving bad news about the patient's health. Other common reasons include if the patient needs help communicating with the physician (e.g., language barrier, hearing or vision impairment) or if the patient has a physical or mental impairment or disability. For some patients, it may be a part of their family's habits or culture, or the age of the patient may be a factor, such as with older patients or children. Family members are the most central and enduring influence in the lives of children, whose health and well-being are linked to their parents' physical, emotional, and social health; social circumstances; and child-rearing practices. 11
Whatever the reasons for their presence, family members can be a valuable part of the health care team ( Table 1 12 – 14 ) . Family members help patients manage and cope with illness. 15 They also can be valuable sources of health information and can act as collaborators in making an accurate diagnosis and planning a treatment strategy. 4 , 12 , 13 , 16 , 17 However, there must be a balance in the concerns addressed during the visit to maintain the alliance formed among patient, physician, and family member. 16 , 18
THE PHYSICIAN'S ROLE
The presence of a family member during a patient encounter introduces unique considerations that require an expanded interviewing skill set from the physician 5 ( Table 2 19 , 20 ) . It is important to recognize and encourage the family member as a source of valuable information and support. 12 , 13 , 21 The degree to which the family member feels supported by the physician may influence the family member's burden, attitude, and emotional health status. 15
The office visit should involve asking the patient and his or her family member about the nature of their relationship, the family member's role in the care of the patient, and the reason for the presence of the family member. 5 , 21 It is important for physicians to maintain their relationship with the patient and be observant of the patient's role in the family member's presence. Physicians should always remember to whom they are primarily responsible. Any additional concerns of the family member should be addressed only after taking care of the patient's issues and concerns.
The Patient-Centered Medical Home . There is compelling evidence that patient-centered communication improves clinical outcomes. 17 , 22 The role of a family physician is enhanced within the concept of the patient-centered medical home, an approach to health care that recognizes the role of patients and their families in providing medical care ( Table 3 6 , 15 ) . This approach encourages collaboration among the patient, family, and health care clinicians, respecting individual and family strengths, cultures, traditions, and expertise. The patient-centered medical home performs these functions well by emphasizing the following principles: care is being provided for a person, not a condition; the patient is best understood in the context of his or her family, culture, values, and goals; and honoring that context will result in better health care, safety, and patient satisfaction. 23 Additional information and resources about the patient-centered medical home are available online from the American Academy of Family Physicians at https://www.aafp.org/online/en/home/membership/initiatives/pcmh/aafpleads/aafppcmh.html .
Although the patient-centered medical home approach recognizes the role of the family in providing medical care, the family member's presence also may add challenges to the visit.
PATIENT SAFETY
Patients may be vulnerable to abuses of power within their families. 24 Although the U.S. Preventive Services Task Force found insufficient evidence to recommend for or against routine family and intimate partner violence screening, 25 patients should be given a chance to express their concerns in private if there is any suspicion of neglect or physical, emotional, and/or financial abuse ( Table 4 26 , 27 ) . A private discussion time between the patient and physician should be set aside in most encounters, especially initially, so the physician can address concerns about whether a family member is acting in the patient's best interest and whether the patient feels safe and well cared for. The physical examination may present an opportunity to request time alone with the patient. 5 , 21 The physician can use this time to elicit fears or concerns; obtain the names of other family caregivers the patient might want the physician to contact; and determine whether the patient requires legal or social services. 15 Physicians need to be familiar with specific state reporting statutes and the implications of reporting patient neglect, abuse, or exploitation. 15
PATIENT CONFIDENTIALITY
The physician must exercise care to avoid a potential breach of the Health Insurance Portability and Accountability Act (HIPAA), which states that health professionals may share relevant health care information with the family member only if the patient agrees to, or does not object to, the disclosure. 5 , 15 A cross-sectional survey of family physician respondents found that 95 percent provided private health information to a patient's family member, but only 56 percent asked their patients for permission to share this private health information. 28 However, HIPAA should not be viewed as a barrier to communication. 15 Maintaining and respecting confidentiality is of utmost importance, and priority should always be given to the patient's right to privacy and confidentiality. 5 This is why it is imperative that the patient has time to communicate privately with the physician at some point during the visit.
FAMILY DYNAMICS AND TRIANGULATION
Physicians should recognize abnormal family dynamics during the office visit and attempt to stay neutral by avoiding triangulation (i.e., when two persons are in conflict, each will try to align with a third). 5 , 12 , 21 , 29 To achieve maximum neutrality, physicians should not take the side of the family member or the patient. The only time neutrality should be violated is if physicians suspect abuse or neglect. 29 Any other family conflict that remains unresolved may be referred to a family therapist, particularly if there is a chance that these issues might interfere with the patient's health care planning. 5
Illustrative Case
A 56-year-old man is evaluated and diagnosed with depression during an office visit that includes his wife. His physician recommends beginning treatment with an anti-depressant. The patient is undecided about taking the medication, but his wife insists that he begin treatment with the medication. She also requests refills for her own medications.
Interpretation : The presence of the patient's wife brings potential benefits, including the provision of a more complete history of diagnosis, such as duration of symptoms and impact on well-being. Although the wife's values could be imparted into the decision making, her presence also constitutes a liability. The physician can best navigate the demands of this encounter by maintaining a primary focus on the patient's needs. If the patient's wife interferes with this focus, the physician should know when to excuse her and talk to the patient in private. From a legal perspective, the physician should avoid making the wife the sole decision maker if the patient is competent. Regarding the wife's request for refills, the physician should limit curbside consultations and encourage her to make a separate appointment for herself.
Hahn SR, Feldman MD. Families. In: Feldman MD, Christensen JF, eds. Behavioral Medicine: A Guide for Clinical Practice . 3rd ed. New York, NY: Lange Medical Books/McGraw-Hill Medical Pub. Division; 2008:55–70.
Dokken D, Ahmann E. The many roles of family members in “family-centered care”—part I. Pediatr Nurs. 2006;32(6):562-565.
Axelsson ÅB, Zettergren M, Axelsson C. Good and bad experiences of family presence during acute care and resuscitation. What makes the difference?. Eur J Cardiovasc Nurs. 2005;4(2):161-169.
Labrecque MS, Blanchard CG, Ruckdeschel JC, Blanchard EB. The impact of family presence on the physician-cancer patient interaction. Soc Sci Med. 1991;33(11):1253-1261.
Lang F, Marvel K, Sanders D, et al. Interviewing when family members are present. Am Fam Physician. 2002;65(7):1351-1354.
Scholle SH. Engaging patients and families in the medical home. Rockville, Md.: Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services; 2010.
Brady DW, Schneider J, White JC. Lesbian, gay, bisexual, & transgender (LGBT) patients. In: Feldman MD, Christensen JF, eds. Behavioral Medicine: A Guide for Clinical Practice . 3rd ed. New York, NY: Lange Medical Books/McGraw-Hill Medical Pub. Division; 2008:121–129.
Medalie JH, Zyzanski SJ, Langa D, Stange KC. The family in family practice: is it a reality?. J Fam Pract. 1998;46(5):390-396.
Cole-Kelly K, Yanoshik MK, Campbell J, Flynn SP. Integrating the family into routine patient care: a qualitative study. J Fam Pract. 1998;47(6):440-445.
Doherty WJ, Baird MA, Becker L. Family medicine and the biopsychosocial model: the road toward integration. In: Doherty WJ, ed. Family Medicine: The Maturing of a Discipline . New York, NY: Haworth Press; 1987:51–70.
Schor EL. American Academy of Pediatrics Task Force on the Family. Family pediatrics: report of the Task Force on the Family. Pediatrics. 2003;111(6 pt 2):1541-1571.
Brown JB, Brett P, Stewart M, Marshall JN. Roles and influence of people who accompany patients on visits to the doctor. Can Fam Physician. 1998;44:1644-1650.
Clayman ML, Roter D, Wissow LS, Bandeen-Roche K. Autonomy-related behaviors of patient companions and their effect on decision-making activity in geriatric primary care visits. Soc Sci Med. 2005;60(7):1583-1591.
Schilling LM, Scatena L, Steiner JF, et al. The third person in the room: frequency, role, and influence of companions during primary care medical encounters. J Fam Pract. 2002;51(8):685-690.
Mitnick S, Leffler C, Hood VL American College of Physicians Ethics, Professionalism and Human Rights Committee. Family caregivers, patients and physicians: ethical guidance to optimize relationships. J Gen Intern Med. 2010;25(3):255-260.
Main DS, Holcomb S, Dickinson P, Crabtree BF. The effect of families on the process of outpatient visits in family practice. J Fam Pract. 2001;50(10):888.
Street RL, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295-301.
McBride JL. Managing family dynamics. Fam Pract Manag. 2004;11(7):70.
Campbell TL, McDaniel SH, Cole-Kelly K. Family issues in health care. In: Taylor RB, ed. Family Medicine: Principles and Practice . 6th ed. New York, NY: Springer; 2003:24–32.
World Organization of National Colleges, Academies and Academic Associations of General Practitioners/Family Physicians (WONCA). The role of the general practitioner/family physician in health care systems: a statement from WONCA, 1991. http://www.globalfamilydoctor.com/publications/Role_GP.pdf. Accessed June 8, 2011.
Greene MG, Majerovitz SD, Adelman RD, Rizzo C. The effects of the presence of a third person on the physician-older patient medical interview. J Am Geriatr Soc. 1994;42(4):413-419.
Levinson W, Lesser CS, Epstein RM. Developing physician communication skills for patient-centered care. Health Aff (Millwood). 2010;29(7):1310-1318.
O'Malley PJ, Brown K, Krug SE Committee on Pediatric Emergency Medicine. Patient- and family-centered care of children in the emergency department. Pediatrics. 2008;122(2):e511-521.
Candib LM, Gelberg L. How will family physicians care for the patient in the context of family and community?. Fam Med. 2001;33(4):298-310.
U.S. Preventive Services Task Force. Screening for family and intimate partner violence: recommendation statement. March 2004. http://www.uspreventiveservicestaskforce.org/3rduspstf/famviolence/famviolrs.htm . Accessed June 8, 2011.
Kennedy RD. Elder abuse and neglect: the experience, knowledge, and attitudes of primary care physicians. Fam Med. 2005;37(7):481-485.
Robinson L, de Benedictis T, Segal J. Helpguide.org. Elder abuse and neglect. Warning signs, risk factors, prevention, and help. http://www.helpguide.org/mental/elder_abuse_physical_emotional_sexual_neglect.htm . Accessed February 20, 2011.
Pérez-Cárceles MD, Pereñiguez JE, Osuna E, Luna A. Balancing confidentiality and the information provided to families of patients in primary care. J Med Ethics. 2005;31(9):531-535.
Gottlieb MC, Lasser J, Simpson GL. Legal and ethical issues in couple therapy. In: Gurman AS, ed. Clinical Handbook of Couple Therapy . 4th ed. New York, NY: Guilford Press; 2008:698–716.
Continue Reading
More in AFP
More in pubmed.
Copyright © 2011 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Informed Consent?
- Implied Consent
- When It Is Required
Informed consent is an important communication process that takes place between patients and their healthcare providers. It is a key part of the healthcare decision-making process.
During the informed consent process, your healthcare provider makes sure you understand your diagnosis, treatment options, and the benefits and risks of those treatment options. Depending on your treatment plan, you may be asked to sign an informed consent document that gives your healthcare provider permission to do certain tests or procedures.
This article outlines what you should know about the consent process, including the difference between informed consent and implied consent, and steps you can take to ensure you're taking an active role in your medical care.
The consent process gives patients the ability to decide what happens to their bodies and enables them to be active participants in their medical care. In short, no one should perform medical tests, procedures, or research on you without first making sure you understand the risks and benefits, and then getting your permission to proceed.
Informed consent includes:
- Information about your diagnosis
- The benefits and risks of treatments (or no treatment)
- How and by whom procedures will be carried out
For instance, if you are receiving care at a teaching hospital, you must be told if a medical trainee will be involved in your care or will be performing a specific procedure.
Your healthcare provider will let you know what they are doing and why, whether they're performing a physical exam, prescribing a medication, or developing a more complex treatment plan that requires additional tests or procedures. The other providers on your care team will do the same. If you need additional procedures or tests, you'll provide additional consent as needed.
Your healthcare provider is required to ensure you fully understand the information you've been given. They may provide information during a conversation, or use patient education materials like brochures, fact sheets, or videos. You should have the opportunity to ask questions and have them answered.
Your healthcare provider must be able to prove that you authorized tests, treatments, or interventions, so your agreement or refusal of a treatment plan will be documented in your medical record.
Elements of Informed Consent
Healthcare providers must follow four central elements of the informed consent process.
Decision-Making Ability
You must be able to make the decision. That means you can understand the options available to you and the consequences of the proposed treatments (or of not being treated). Children and patients who are unconscious lack decision-making ability and would not be able to participate in the informed consent process.
Who Can Provide Informed Consent for You?
In the United States, you must be 18 years or older to give informed consent. For minors who are 17 or younger, a parent or legal guardian makes all medical decisions.
A surrogate, or legal representative, can also give informed consent (and sign an informed consent document) if the patient is:
- Unable to understand the medical information provided
- Cannot assess the possible outcomes of treatment
- Unable to make decisions due to incapacitation or mental illness
Information Sharing
Your healthcare provider must disclose information on your diagnosis and their proposed treatments. This includes information on the effectiveness of the treatments, the benefits, and the risks. It should also include the risks and benefits of refusing treatment. Your healthcare provider must provide a full picture of what you can expect.
Understanding
One of the most important elements of informed consent is your understanding of the information. Ask questions to make sure that you fully comprehend what's being presented before you agree to treatments.
Voluntary Agreement
No one should pressure or force you to provide informed consent. Your agreement should never be given under duress.
Informed Consent vs. Consent to Treat
Most medical offices include a Consent to Treat form with its standard patient paperwork. When you sign this form, you're giving the healthcare provider permission to provide care and for the practice to bill your insurance. This form clearly states your right to discuss all procedures or treatments or to refuse them.
Implied Consent vs. Informed Consent
Implied consent takes place in situations where a more formal consent is not needed. For instance, if you make an appointment to have a blood sample drawn and roll up your sleeve, your consent is implied.
When Is Informed Consent Required?
Except under specific circumstances, informed consent—whether written or implied—is required for any treatment or medical procedure and for any research study where there is more than minimal risk to the subjects. In the majority of situations, the informed consent process happens before a test or treatment is performed.
You'll be given the opportunity to provide consent—informed (written or verbal) or implied—for everything you're asked to do. Your provider will note your consent in your record and, in some cases, document it with a signed form.
You Have the Right to Change Your Mind
You can change your mind about your treatment or other health care decisions even after you've signed an informed consent form. You always have the right to stop or switch treatments.
You won't need to provide written consent for some things, like a prescription for medication. The act of having your prescription filled implies your consent to taking the medicine.
Types of Procedures
For some procedures, you may be asked to sign an informed consent document. Written informed consent is required for medical procedures such as:
- Surgeries (both inpatient and outpatient)
- Invasive medical procedures, such as colonoscopies or biopsies
- Placement of a medical device, such as an intrauterine device (IUD)
- Chemotherapy
- Radiation therapy
Some laboratory tests, like an HIV blood test, require written consent, but not all do.
Emergency Situations
In an emergency situation, a healthcare provider may not be able to get consent from you or your representative. In these situations, treatment can be started without consent. Your healthcare provider should get official permission from you as soon as possible. Full consent must be given for any further or ongoing treatment.
Tips for Providing Informed Consent
If you are asked to sign an informed consent document, there are some steps you can take to make sure you're fully engaged in the process. Some guidelines are listed below.
Listen and Learn
Understand that signing the form tells your healthcare providers that they have permission to go forward with recommended treatments, tests, or procedures. Before you agree with this, be sure you understand:
- What your other options are: Could something else be done instead?
- What could happen during the process
- What could happen as a result of the treatment
- What could happen without the treatment
Ask For Time to Review
There's no rule that says you must sign the form as soon as it's handed to you. Sometimes, the informed consent form is mixed with other documents that must be signed before you see a healthcare provider.
Confirm with your provider's office what needs to be signed immediately and what you can take home to review before signing.
Confirm Your Understanding
When your healthcare provider describes the tests, procedures, benefits, and risks to you, take the time to repeat them back to be sure you understand them. That will give your healthcare provider a chance to clarify any information you may not fully understand.
Know the Limits
Recognize that your signature on the form provides no guarantees that the treatment will relieve your health problem or cure you. Unfortunately, medical treatment can never provide a guarantee.
However, understanding why you need the test or treatment, how it will happen, and what the risks and alternatives are, could improve the chances it will be successful.
It is also important to remember that you can, at any time, change your mind.
Informed consent is when your healthcare provider makes sure you understand your diagnosis and the risks and benefits of any tests, medical procedures, or other treatments they recommend to treat your condition. Informed consent is at the core of the shared-decision making process between a patient and their healthcare provider.
Informed consent also means that your healthcare provider will help you understand alternative treatments as well as the risks and benefits of refusing treatment. Before you provide consent, be sure all of your questions are answered and that you understand the information. Don't forget that you can change your mind about your treatment plan even after you provide informed consent.
Association of American Medical Colleges. What "informed consent" really means.
Hein IM, De Vries MC, Troost PW, Meynen G, Van Goudoever JB, Lindauer RJL. Informed consent instead of assent is appropriate in children from the age of twelve: Policy implications of new findings on children’s competence to consent to clinical research . BMC Medical Ethics . 2015;16(1):76. doi:10.1186%2Fs12910-015-0067-z
American Medical Association. Informed consent .
Agency for Healthcare Research and Quality. Health Literacy Universal Toolkit. Consent to treat form .
American Cancer Society. What is informed consent?
Kakar H, Gambhir RS, Singh S, Kaur A, Nanda T. Informed consent: Corner stone in ethical medical and dental practice. J Family Med Prim Care . 2014;3(1):68-71. doi:10.4103/2249-4863.130284
By Trisha Torrey Trisha Torrey is a patient empowerment and advocacy consultant. She has written several books about patient advocacy and how to best navigate the healthcare system.
Greater Good Science Center • Magazine • In Action • In Education
Mind & Body Articles & More
How doctors can communicate better with patients, two new books suggest that we can improve communication and care in medicine with more mindfulness and presence..
No doubt about it: Doctors are stressed out. Surveys show that physician burnout is on the rise, with the percentage of physicians in the United States reporting symptoms of burnout rising from 45 percent in 2011 to 54 percent in 2014.
If you ask doctors why they’re so stressed, many mention heavy patient loads, endless patient charts to fill out, the looming possibility of litigation, and back-and-forth communication with health insurance companies. These constant distracters can lead to the erosion of patient-clinician interactions, miscommunication, clinical errors, or worse.
Now, two new books— Attending: Medicine, Mindfulness, and Humanity , by Dr. Ronald Epstein, and What Patients Say, What Doctors Hear , by Dr. Danielle Ofri—candidly unpack the factors that contribute to physician-patient communication breakdowns and medical errors. They reveal the challenges that doctors and patients face in communicating and provide optimistic insights on how to improve health care.
Four mindfulness skills for doctors

Epstein, a professor of medicine at Rochester University and a practicing physician, is a leader of the mindfulness movement in medicine. Drawing from his own groundbreaking paper , he explains how mindful self-reflection and self-regulation are key to masterful clinical care, enabling physicians to listen attentively, make good judgments, and act compassionately.
“Medicine and meditation, etymologically, come from the same root: to consider, advise, reflect, to take appropriate measures,” he writes, suggesting that the two are closely related. This explains why doctors should consider using mindfulness in their medical practice.
Using anecdotes, Zen Buddhist stories, and thoroughly cited research, Epstein explores how the four mindfulness skills of attention, curiosity, beginner’s mind, and presence mirror those physicians need to provide quality care:
- Attention. Because of everything they have on their minds, physicians may not be fully attentive in the exam room. Doctors often rely on automatic, fast thinking when interacting with patients. But practicing mindful attention can help them slow down enough to use deliberate, more conscious thinking when patients present signs of something serious.
- Curiosity. Developing a sense of curiosity can inspire physicians to ask more questions and dig deeper with patients, as well as foster empathy and understanding for patients’ unique needs, values, and circumstances. It also helps doctors recognize when something is off with a patient so they can then “tune in.” Epstein notes that while genetics partly contributes to curiosity , supportive environments can also foster it—particularly those that allow physicians to feel comfortable freely sharing their doubts, discoveries, and mishaps.
- Beginner’s mind. Inspired by a book written by Shunryu Suzuki, Epstein advises physicians to “hold expertise lightly” and be aware that their understanding of a patient’s case, while based on expertise, may be provisional and incomplete. He warns that self-confidence can get in the way of good care , if physicians don’t recognize that there are things they may not fully know. Luckily, beginner’s mind can be taught: At least one randomized controlled study found that practicing mindfulness meditation helped people to not be “blinded by experience” from novel or obvious solutions to problems.
- Presence. Listening deeply, without judgment, interruption, or preconceptions, can be tough for physicians who have a myriad of other things to worry about. However, a physician’s presence can help a patient feel understood and acknowledged, and decrease chances of miscommunication and error. To be present, one must “quiet the mind”—a skill that can be honed through reflective, contemplative practices.
Why doctors should train in mindfulness
Epstein makes a case that almost any physician can practice mindfulness to improve patient care, and the science supports that contention.
In a study of primary care physicians, Epstein found that a year-long mindfulness practice program increased their resilience (improved mood, lower burnout), quality of care (safer and more timely, accessible, effective, and patient-centered), and patient interactions (more empathetic, compassionate, and responsive). Patients of clinicians practicing mindfulness are more likely to disclose personal (and potentially critical) information and comply better with treatments. Epstein highlights other important aspects of patient care that can benefit from mindfulness. Making good decisions involves becoming aware of one’s biases and engaging strategies to correct them, and mindfulness has been shown to support that. Also, being more mindful can help physicians be attuned to the suffering of their patients without becoming overwhelmed. While Epstein acknowledges that being with suffering can be draining, studies have found that training in compassion , self-compassion , or loving-kindness meditation can mitigate physicians’ emotional distress and increase their resilience. How can mindfulness in medicine be sustained? It starts in medical school, where compassion and listening skills could be taught and emphasized as much as anatomy or biochemistry.
Support from colleagues and medical institutions is also important, writes Epstein. Doctors are held to high standards, and they are not inclined to share their mistakes with colleagues. However, sharing stories with each other can be very therapeutic , as can being in a place that encourages doctors to admit to difficulties they are experiencing.
Epstein cites the success of a “confessions” project led by colleague Dr. Suzanne Karan, to encourage doctors to share medical errors. Intended to identify causes and prevent future errors, the program also addresses clinicians’ psychological and educational needs. Initiatives like this can help the culture of medicine become more nurturing and supportive of its healers.
How physician-patient communication breaks down
Ofri, a professor of medicine at New York University and hospital internist, shares many of Epstein’s concerns about physician-patient interactions in her book What Patients Say, What Doctors Hear . But while Epstein focuses on the benefits of mindfulness, Ofri hones in on listening and communication skills as powerful tools for exceptional patient care.
There are many barriers to effective communication between physicians and patients, according to Ofri. Doctors may be distracted by millions of other things as they try to listen to patients. Sometimes, patients don’t know their true underlying problem or what to reveal to the doctor. Meaning and intent can get lost. Although the healing professions seek to be nonjudgmental, Ofri points out that doctors’ implicit biases can prevent them from giving equal care to all patients. Studies have shown that doctors show less respect to patients with obesity, for example. African-American patients tend to get less patient-centered care, experience more verbal dominance from doctors, and receive fewer and less-aggressive treatments. (However, the flip side of implicit bias also exists; patients tend to feel more comfortable seeing doctors who are similar in race.)
The medicine of good communication
Ofri suggests that to improve communication, doctors should spend more time listening effectively during the appointment. On average, doctors interrupt patients within 12 seconds of them first speaking during primary care visits and throughout the appointment—often, before they have finished explaining an issue. One study shows that inattentive listening can distract the speaker from telling their own stories effectively, suggesting that speakers and listeners have a shared responsibility.
Doctors can help patients communicate their problems better and feel more understood by acknowledging what they’re saying and encouraging them to continue, and even removing physical barriers between the two of them (i.e., not talking from behind a computer).
Ofri also advises that doctors ask their patients, “Is there anything else?” She acknowledges that this can be daunting for doctors because it opens a Pandora’s box of dialogue that may cut into other patients’ appointment times.
However, understanding the patient as much as possible from the start can save a lot of time in subsequent visits. For example, Ofri once had a patient with a long history of trouble adhering to his numerous medication protocols (despite repeated efforts to explain them to him). It took a year of visits with her for the patient to reveal that he was illiterate and couldn’t read the bottles. She suggests that if she’d taken more care initially, she could have discovered this sooner.
Clear communication from doctors may have a healing effect. Studies on pain perception find that, similar to the placebo effect, thoughtfully walking a patient through a procedure that is being administered, or one that will occur in the future, can make them less anxious and more optimistic, leading to less pain.
Better communication can also lead to less litigation . Whereas patients may feel that doctors are indifferent toward medical errors, in reality those errors haunt doctors for years. Better understanding between parties—and a doctor’s willingness to admit to errors, show concern, and apologize —can help prevent patients from seeking retribution through lawsuits.
Amid the pressure and fast pace of medicine, doctors and other health care providers can still learn to slow down and cultivate better listening and understanding. Doing so gives patients a chance to communicate more effectively, which saves more time and more lives in the long run. Both of these books can help doctors and patients—and, really, anyone in any professional or personal partnership—to work together toward better communication and connection.
About the Author


Deborah Yip
Deborah Yip is a medical student at the University of California, San Francisco, a former GGSC research assistant, and a contributor to Greater Good .
You May Also Enjoy
This article — and everything on this site — is funded by readers like you.
Become a subscribing member today. Help us continue to bring “the science of a meaningful life” to you and to millions around the globe.
Republish This Story
Virtual or In Person: Which Kind of Doctor’s Visit Is Better, and When It Matters

When the covid-19 pandemic swept the country in early 2020 and emptied doctors’ offices nationwide, telemedicine was suddenly thrust into the spotlight. Patients and their physicians turned to virtual visits by video or phone rather than risk meeting face-to-face.
During the early months of the pandemic, telehealth visits for care exploded .
“It was a dramatic shift in one or two weeks that we would expect to happen in a decade,” said Dr. Ateev Mehrotra , a professor at Harvard Medical School whose research focuses on telemedicine and other health care delivery innovations. “It’s great that we served patients, but we did not accumulate the norms and [research] papers that we would normally accumulate so that we can know what works and what doesn’t work.”
Now, three years after the start of the pandemic, we’re still figuring that out. Although telehealth use has moderated, it has found a role in many physician practices, and it is popular with patients.
More than any other field, behavioral health has embraced telehealth. Mental health conditions accounted for just under two-thirds of telehealth claims in November 2022, according to FairHealth , a nonprofit that manages a large database of private and Medicare insurance claims.
Telehealth appeals to a variety of patients because it allows them to simply log on to their computer and avoid the time and expense of driving, parking, and arranging child care that an in-person visit often requires.
But how do you gauge when to opt for a telehealth visit versus seeing your doctor in person? There are no hard-and-fast rules, but here’s some guidance about when it may make more sense to choose one or the other.
Email Sign-Up
Subscribe to KFF Health News' free Weekly Edition.
If It’s Your First Visit
“As a patient, you’re trying to evaluate the physician, to see if you can talk to them and trust them,” said Dr. Russell Kohl , a family physician and board member of the American Academy of Family Physicians. “It’s hard to do that on a telemedicine visit.”
Maybe your insurance has changed and you need a new primary care doctor or OB-GYN. Or perhaps you have a chronic condition and your doctor has suggested adding a specialist to the team. A face-to-face visit can help you feel comfortable and confident with their participation.
Sometimes an in-person first visit can help doctors evaluate their patients in nontangible ways, too. After a cancer diagnosis, for example, an oncologist might want to examine the site of a biopsy. But just as important, he might want to assess a patient’s emotional state.
“A diagnosis of cancer is an emotional event; it’s a life-changing moment, and a doctor wants to respond to that,” said Dr. Arif Kamal , an oncologist and the chief patient officer at the American Cancer Society. “There are things you can miss unless you’re sitting a foot or two away from the person.”
Once it’s clearer how the patient is coping and responding to treatment, that’s a good time to discuss incorporating telemedicine visits.
If a Physical Exam Seems Necessary
This may seem like a no-brainer, but there are nuances. Increasingly, monitoring equipment that people can keep at home — a blood pressure cuff, a digital glucometer or stethoscope, a pulse oximeter to measure blood oxygen, or a Doppler monitor that checks a fetus’s heartbeat — may give doctors the information they need, reducing the number of in-person visits required.
Someone’s overall physical health may help tip the scales on whether an in-person exam is needed. A 25-year-old in generally good health is usually a better candidate for telehealth than a 75-year-old with multiple chronic conditions.
But some health complaints typically require an in-person examination, doctors said, such as abdominal pain, severe musculoskeletal pain, or problems related to the eyes and ears.
Abdominal pain could signal trouble with the gallbladder, liver, or appendix, among many other things.
“We wouldn’t know how to evaluate it without an exam,” said Dr. Ryan Mire , an internist who is president of the American College of Physicians.
Unless a doctor does a physical exam, too often children with ear infections receive prescriptions for antibiotics, said Mehrotra, pointing to a study he co-authored comparing prescribing differences between telemedicine visits, urgent care, and primary care visits.
In obstetrics, the pandemic accelerated a gradual shift to fewer in-person prenatal visits. Typically, pregnancy involves 14 in-person visits. Some models now recommend eight or fewer, said Dr. Nathaniel DeNicola, chair of telehealth for the American College of Obstetricians and Gynecologists. A study found no significant differences in rates of cesarean deliveries, preterm birth, birth weight, or admissions to the neonatal intensive care unit between women who received up to a dozen prenatal visits in person and those who received a mix of in-person and virtual visits.
Contraception is another area where less may be more, DeNicola said. Patients can discuss the pros and cons of different options virtually and may need to schedule a visit only if they want an IUD inserted.
If Something Is New, or Changes
When a new symptom crops up, patients should generally schedule an in-person visit. Even if the patient has a chronic condition like diabetes or heart disease that is under control and care is managed by a familiar physician, sometimes things change. That usually calls for a face-to-face meeting too.
“I tell my patients, ‘If it’s new symptoms or a worsening of existing symptoms, that probably warrants an in-person visit,’” said Dr. David Cho , a cardiologist who chairs the American College of Cardiology’s Health Care Innovation Council. Changes could include chest pain, losing consciousness, shortness of breath, or swollen legs.
When patients are sitting in front of him in the exam room, Cho can listen to their hearts and lungs and do an EKG if someone has chest pain or palpitations. He’ll check their blood pressure, examine their feet to see if they’re retaining fluid, and look at their neck veins to see if they are bulging .
But all that may not be necessary for a patient with heart failure, for example, whose condition is stable, he said. They can check their own weight and blood pressure at home, and a periodic video visit to check in may suffice.
Video check-ins are effective for many people whose chronic conditions are under control, experts said.
When someone is undergoing treatment for cancer, certain pivotal moments will require a face-to-face meeting, said Kamal, of the American Cancer Society.
“The cancer has changed or the treatment has changed,” he said. “If they’re going to stop chemotherapy, they need to be there in person.”
And one clear recommendation holds for almost all situations: Even if a physician or office scheduler suggests a virtual visit, you don’t have to agree to it.
“As a consumer, you should do what you feel comfortable doing,” said Dr. Joe Kvedar , a professor at Harvard Medical School and immediate past board chairman of the American Telemedicine Association . “And if you really want to be seen in the office, you should make that case.”
Related Topics
- Mental Health
- Telemedicine
Copy And Paste To Republish This Story
By Michelle Andrews March 6, 2023
When the covid-19 pandemic swept the country in early 2020 and emptied doctors’ offices nationwide, telemedicine was suddenly thrust into the spotlight. Patients and their physicians turned to virtual visits by video or phone rather than risk meeting face-to-face.
“It was a dramatic shift in one or two weeks that we would expect to happen in a decade,” said Dr. Ateev Mehrotra , a professor at Harvard Medical School whose research focuses on telemedicine and other health care delivery innovations. “It’s great that we served patients, but we did not accumulate the norms and [research] papers that we would normally accumulate so that we can know what works and what doesn’t work.”
Now, three years after the start of the pandemic, we’re still figuring that out. Although telehealth use has moderated, it has found a role in many physician practices, and it is popular with patients.
But how do you gauge when to opt for a telehealth visit versus seeing your doctor in person? There are no hard-and-fast rules, but here’s some guidance about when it may make more sense to choose one or the other.
If It’s Your First Visit
“As a patient, you’re trying to evaluate the physician, to see if you can talk to them and trust them,” said Dr. Russell Kohl , a family physician and board member of the American Academy of Family Physicians. “It’s hard to do that on a telemedicine visit.”
Sometimes an in-person first visit can help doctors evaluate their patients in nontangible ways, too. After a cancer diagnosis, for example, an oncologist might want to examine the site of a biopsy. But just as important, he might want to assess a patient’s emotional state.
“A diagnosis of cancer is an emotional event; it’s a life-changing moment, and a doctor wants to respond to that,” said Dr. Arif Kamal , an oncologist and the chief patient officer at the American Cancer Society. “There are things you can miss unless you’re sitting a foot or two away from the person.”
Once it’s clearer how the patient is coping and responding to treatment, that’s a good time to discuss incorporating telemedicine visits.
This may seem like a no-brainer, but there are nuances. Increasingly, monitoring equipment that people can keep at home — a blood pressure cuff, a digital glucometer or stethoscope, a pulse oximeter to measure blood oxygen, or a Doppler monitor that checks a fetus’s heartbeat — may give doctors the information they need, reducing the number of in-person visits required.
Someone’s overall physical health may help tip the scales on whether an in-person exam is needed. A 25-year-old in generally good health is usually a better candidate for telehealth than a 75-year-old with multiple chronic conditions.
“We wouldn’t know how to evaluate it without an exam,” said Dr. Ryan Mire , an internist who is president of the American College of Physicians.
“I tell my patients, ‘If it’s new symptoms or a worsening of existing symptoms, that probably warrants an in-person visit,’” said Dr. David Cho , a cardiologist who chairs the American College of Cardiology’s Health Care Innovation Council. Changes could include chest pain, losing consciousness, shortness of breath, or swollen legs.
When patients are sitting in front of him in the exam room, Cho can listen to their hearts and lungs and do an EKG if someone has chest pain or palpitations. He’ll check their blood pressure, examine their feet to see if they’re retaining fluid, and look at their neck veins to see if they are bulging .
“The cancer has changed or the treatment has changed,” he said. “If they’re going to stop chemotherapy, they need to be there in person.”
And one clear recommendation holds for almost all situations: Even if a physician or office scheduler suggests a virtual visit, you don’t have to agree to it.
“As a consumer, you should do what you feel comfortable doing,” said Dr. Joe Kvedar , a professor at Harvard Medical School and immediate past board chairman of the American Telemedicine Association . “And if you really want to be seen in the office, you should make that case.”
We encourage organizations to republish our content, free of charge. Here’s what we ask:
You must credit us as the original publisher, with a hyperlink to our kffhealthnews.org site. If possible, please include the original author(s) and KFF Health News” in the byline. Please preserve the hyperlinks in the story.
It’s important to note, not everything on kffhealthnews.org is available for republishing. If a story is labeled “All Rights Reserved,” we cannot grant permission to republish that item.
Have questions? Let us know at KHNHelp@kff.org
More From KFF Health News

Bird Flu Is Bad for Poultry and Dairy Cows. It’s Not a Dire Threat for Most of Us — Yet.

Oh, Dear! Baby Gear! Why Are the Manuals So Unclear?

California Floats Extending Health Insurance Subsidies to All Adult Immigrants

DIY Gel Manicures May Harm Your Health
Thank you for your interest in supporting Kaiser Health News (KHN), the nation’s leading nonprofit newsroom focused on health and health policy. We distribute our journalism for free and without advertising through media partners of all sizes and in communities large and small. We appreciate all forms of engagement from our readers and listeners, and welcome your support.
KHN is an editorially independent program of KFF (Kaiser Family Foundation). You can support KHN by making a contribution to KFF, a non-profit charitable organization that is not associated with Kaiser Permanente.
Click the button below to go to KFF’s donation page which will provide more information and FAQs. Thank you!

Latest Issue
Psychiatry’s new frontiers
Hope amid crisis
Recent Issues
- AI explodes Taking the pulse of artificial intelligence in medicine
- Health on a planet in crisis
- Real-world health How social factors make or break us
- Molecules of life Understanding the world within us
- The most mysterious organ Unlocking the secrets of the brain
- All Articles
- The spice sellers’ secret
- ‘And yet, you try’
- Making sense of smell
- Before I go
- My favorite molecule
- View all Editors’ Picks
- Diversity, Equity & Inclusion
- Infectious Diseases
- View All Articles
Are you listening?
Modern medicine challenges the crucial bond between doctors and patients
By Patricia Hannon
Photography by Max Aguilera-Hellweg
A conversation with her oncology team helped Kimberly Allison embrace her treatment plan after a devastating diagnosis.

Kimberly Allison, MD, was 33 when her diagnosis came. She was a couple weeks into a job directing the breast cancer pathology lab at the University of Washington Medical Center and happily settling into a new routine with her husband, a preschool daughter and an infant son.
The discovery that she had the disease she devotes her career to studying was “like Alice in Wonderland, falling down the rabbit hole.”
She couldn’t protect herself from what the scientist in her knew: Young women tend to get more deadly forms of cancer. And her cancer was ugly and big, likely having spread, undetected, during her pregnancy and breastfeeding.
Related reading
One patient who struggled with being overweight for much of her life says she finally found success because of the trusting relationship she has with her doctor.
Allison , now a professor of pathology at Stanford’s School of Medicine, recalls her deep depression after the diagnosis 10 years ago, when her mind went to the “darkest places” as she scoured the internet for answers.
“Every study I looked up had a horrible outcome. I thought this was going to be a death sentence for me,” she says. “What if you only have two years left? You go there right away.” What should she do with that time? Sadness about her children overwhelmed her. Should she quit work and spend her time with them and her husband? Should she do something soul-fulfilling like writing or painting? Or keep working in a career she loves?
She wouldn’t be able to settle those thoughts until she saw her oncology team.
At the first meeting with her surgeon and two oncologists, Allison willed emotion away. She didn’t want to “be a total mess” in front of the physicians gathered around the conference room table with her and her husband. She wanted her colleagues to see her as professional and still capable of doing her job.
They discussed the characteristics of her cancer and her treatment options in a matter-of-fact way and created a plan: six months of chemotherapy, followed by surgery, then radiation. They could start right away.
But Allison was uneasy. “OK, but I’ve seen the pathology,” she told the team. “This looks really bad to me.” That’s when her surgeon, Kristine Calhoun, MD, saw through Allison’s tough facade to the fear she was struggling to keep at bay. Calhoun told her: “I know you’ve looked up your prognosis. But there are new, targeted therapies that are changing that outcome. That data is so new it’s not in the older papers about pregnancy-associated cancers.
“This is a new ballgame,” Calhoun said. “We’re talking about seeing the grandkids.”
Allison finally had hope: “That basically reset me like, ‘OK, I’m not dying. I’m not dying right now.’”
Calhoun, who is still at the University of Washington School of Medicine, says there’s a delicate balance in giving patients hope without giving them false hope, but it was important that Allison see a positive path forward.
“People who lose hope kind of will themselves into a certain pathway,” she says. Though it was sometimes difficult to treat a friend, Calhoun says she learned a lot from how Allison handled the experience.
“It taught me to have even more empathy,” she says. “It helped me learn to not just look at patients as patients but as people, and to see that it really does change their story.”
The connection between Allison and Calhoun, which grew stronger as Allison’s treatment progressed, is what Stanford physician and author Abraham Verghese , MD, calls the “most poignant of human experiences” — one of suffering and the care of people who are suffering.
“The relationship between a care provider and a patient is vitally important in determining the health and well‑being of the patient and the outcome of treatments,” says School of Medicine Dean Lloyd Minor , MD.
He notes that, historically, the most a physician could do for suffering patients was to offer comfort by being an empathetic and understanding listener. A relatively recent explosion in biomedical knowledge and therapeutic options changed that and vastly improved care. But he says it also created a “separation between the science of medicine and the humanism and compassion of medicine” that must be addressed to nurture the ability of physicians to better understand and treat their patients.
“Each patient comes with a different history, with a different social, cultural and behavioral background,” says Minor. “Those factors are going to play heavily in determining the effectiveness of whatever scientifically based therapeutics you seek to offer.”
Listening is crucial to good health care
Clinicians across the board say the current climate of medicine cuts into the time they can spend really listening to patients, which makes it difficult to form meaningful connections, says Donna Zulman , MD, assistant professor of medicine and co-director of Stanford Presence 5 , an initiative to change clinical encounters to improve overall health care. The initiative was launched by the Stanford Presence Center — founded in 2015 by Verghese to develop methods of tearing down communication barriers created by technology.

Not listening can have negative consequences downstream, such as misdiagnosis, unnecessary or unwanted treatment, patients not following through, fragmented patient care and physician burnout, Zulman says.
She is one of many people — at Stanford and elsewhere — who are working to enhance the doctor-patient relationship by creating communication skills training for clinicians; addressing physician burnout; and developing ideas for better ways to manage care, design exam rooms and improve health record interfaces.
Zulman points to two main time-robbing culprits: reimbursement models that have resulted in appointment times across the nation being set at about 15 minutes; and electronic health records that have clinicians spending more time outside of the appointments entering, reviewing and sharing patient information.
Such demands on physicians take them far from the reasons they got into medicine.
Kelley Skeff , MD, PhD, professor of medicine, who co-directs the Stanford Faculty Development Center for Medical Teachers, says doctors came to the field “to learn and apply science for the benefit of patients.”
“But their connections to science and to the patient are commonly impeded by the requirements of the system,” he says. “And those who are the most empathetic may, in fact, burn out faster as their self-care is neglected.
“We’re asking them to do the relatively superhuman tasks of keeping humanness and empathy together for others. They’re drawn to respond to the needs of both the health care system and the patient, but their own refueling process isn’t always happening.”
“We’re asking them to do the relatively superhuman tasks of keeping humanness and empathy together for others. … but their own refueling process isn’t always happening.”
Physician burnout is at an all-time high; 54 percent of physicians across the nation reported having at least one symptom of burnout, according to national research overseen in 2014 by Tait Shanafelt , MD, the chief wellness officer and director of the Stanford Medicine WellMD Center. That was up from 46 percent in 2011. A physician wellness survey the center conducted at Stanford in 2016 showed that 34 percent of physicians surveyed that year reported having at least one burnout symptom. That was up from 25 percent in 2013.
Caring for the caregiver has been neglected for years, says Minor, but change is coming. “We have to get real about this,” he says. “I think we’re starting to recognize that our physical and mental well‑being are just as important as our knowledge base and technical skills when it comes to being effective physicians.”
One key challenge, says Minor, is to better integrate technology with medicine. For example, it’s important that electronic health records be better designed and easier to use so health care professionals and patients can access and share the information — and communicate about it — in real time.
“The care-delivery experience should not be driven and determined by the technology, it should be enabled by the technology. Listening to patients and being empathetic with patients should be the priority,” he says.
Improving how we talk to each other
Good communication, Zulman says, starts with clinicians really absorbing what patients say — about themselves, their pain, values, challenges and care goals — and being empathetic.
“Now, because of pervasive technology and other distractions in the clinical setting, we’re having to be more explicit about taking time and taking actions that will help us have meaningful interactions with patients,” she says.
Still, superb communication skills don’t come naturally to everyone, even the most experienced clinicians, says Stephanie Harman , MD, clinical associate professor of medicine. Like other aspects of medicine, being a good communicator takes practice.
“Learning how to build strong patient relationships is equally as important in medicine as learning technical or procedural skills,” says Harman, a master facilitator for Advancing Communication Excellence at Stanford , a workshop designed to help clinicians enhance communication skills that are “really at the heart of how we care for patients and their families.”
Workshop participants role-play patient interactions so patient priorities are at the center of every discussion. A total of 310 clinicians have participated in the program as of April 1 and 310 more are registered to participate between now and August. Harman says they’re encouraged to suspend the impulse to rush through patient conversations and instead listen, so that amid the “all-consuming fracas” of information and tasks they manage, clinicians can “answer the most important question in the world: What does the patient need?”
“Learning how to build strong patient relationships is equally as important in medicine as learning technical or procedural skills.”
To gain a better understanding of effective doctor-patient dynamics, Presence 5 researchers are sitting in on patient interactions with primary care providers at Stanford and in primary care clinics in the Alameda Health System, Ravenswood Family Health Center in East Palo Alto and the Veterans Affairs Palo Alto Health Care System.
If patients agree, researchers use video or audio devices to record the encounters. The data also will include survey feedback from the patients and physicians involved in the approximately 40 visits that are being observed. Researchers will eventually synthesize the information to help establish best practices for interacting with patients.
They’re watching, Zulman says, for moments when patients reveal valuable information about themselves, their symptoms or their social histories that can inform clinical decisions. “What happens in the minutes preceding that? What did the doctor do or say, how were they positioned, that helped the patient open up in that way?”
Learning what patients need most
John Kugler , MD, a clinical associate professor of medicine who launched Stanford Medicine 25 with Verghese nine years ago to promote bedside exam skills, emphasizes the importance of those personal interactions for both diagnostics and for building trust between the physician and patient.
When a trainee seeks Kugler’s advice about a patient, “My first answer is, ‘We can’t make that decision now. We need to see the patient first.’
“You learn so much stuff that’s between the lines. How much distress are they really in? Can they really not breathe? Can they talk to me in full sentences? How weak are they? I’m really trying to get a sense of the person,” he says. “That’s when the decision-making just gels a lot better. To me, so much of it is that initial laying eyes on someone.”
Verghese, the Linda R. Meier and John F. Lane Provostial Professor and a leading advocate for returning to the “timeless human-to-human ritual” of bedside exams, says he takes note of what’s in a hospital room before even approaching a patient.
“They’re totally out of their context,” he says. “So anything that they’ve brought from the outside world is enormously helpful.” One person might be in shackles, another might be reading a book or Bible. Or a hospital room might be filled with greeting cards and family photos. Such observations can reveal a lot about people, he says, including values, cultural backgrounds, cognitive abilities and support networks.
“So often we walk into a room and, because of what the chart says or what we notice, within moments we know what’s going on,” he says. “But the patient doesn’t know what we know. If you jump in and say, ‘Well, I know what’s going on,’ it just seems so rude. And they wonder, ‘What do you already know? I haven’t really finished telling you.’”
Letting them tell their stories in a way that shows respect for them as individuals also invites patients to be partners in their care.
When Allison was fighting stage-3 HER2-positive breast cancer, she wanted to keep working and keep normal routines for her kids. During the first six months, she had chemotherapy once a week. In between, she diagnosed patients and presented pathology to physician groups working on other cases. The schedule, she says, helped her “feel balanced and like I was still engaged in my life. And I found it actually quite nice to go to work and not be focusing on illness all day at home.”
But she also needed emotional support. That, she says, especially came from the wider team of oncology nurses and staff. Memories of their kindness still evoke tears of gratitude. “You’re sitting there for hours, sometimes for a whole day, and those are the people who come and sit next to you, hold your hand, bring you a warm blanket or food, and really get to know you as a person,” she says.
“The hope you gave or the care you gave where you made it personal makes a huge difference.”
Comfort also came from conversations with a hospital chaplain who visited the infusion ward. “Just having somebody to talk to who could bring up some big questions for you to ask yourself, about values and to reflect, was a growing experience without even going through cancer treatment,” Allison says. “It was like therapy.”
Now she meets with patients who want their pathology lab results explained, which is unusual for a pathologist, and speaks with patient groups, encouraging patients to do what they can, such as get a second opinion or learn more about treatments, so they trust and are comfortable with their care team and treatment plans.
She also speaks to physicians, challenging them to see patients quickly after a diagnosis — because “the worst time is that fearful time” of waiting — and to treat them as individuals.
“The hope you gave or the care you gave where you made it personal makes a huge difference,” she tells them. “I knew that I was getting the best treatments. But it was the personal interaction and support that I got as a patient that made a difference for me every day.”
Finding a model that works
Minor, who taught an undergraduate seminar this winter on literature, medicine and empathy, says the sense that the whole team is on your side is crucial for a patient’s motivation and healing and contributes greatly to the wellness of care providers. “Being a physician is a calling,” he says, “partly because of the enormous privilege of interacting with people in a way that establishes deep personal relationships that are unique to health care.”
Alan Glaseroff , MD, adjunct professor of medicine, is working with Arnold Milstein , MD, professor of medicine and director of Stanford’s Clinical Excellence Research Center, to develop new models of care that build on that kind of trust.
Glaseroff and his wife, Ann Lindsay , MD, left Humboldt County in 2011 to create the Stanford Coordinated Care program , basing it on their longtime family practice in Arcata, California, and on ideas gleaned from their more than 15 years of working with the Institute of Healthcare Improvement and other pioneers in the national movement to redesign primary care.
The coordinated care program is designed to cut costs for Stanford’s self-funded insurance plan by treating the 5 percent of employees and their dependents whose care represents 50 percent of the plan’s cost. The approach is meant to keep chronically ill patients from having repeated setbacks and hospital visits by making them partners in their own wellness. Every team member knows the patients well and focuses on goals the patients identify.
The core principle is to engage people, to just sit and talk with them, and show them respect, Glaseroff says. “And the way to engage with them is listening, and it’s focusing on what they care about, even if it seemed trivial compared with what we care about,” he says. “But I don’t think it is trivial. It turns out to be of critical importance.”
Glaseroff believes the practice can apply in all areas of medicine where there’s continuity. “It isn’t just come in, get something done and never see you again,” he says.
“What we figured out is that, if everybody was trained in this approach and we were really consistent with it, we got incredible efforts out of the patients.”
Zulman says she’s intrigued by the potential to address the challenges that get in the way of such successes by taking something that seems “vast and fairly abstract” and designing and implementing concrete interventions that make a difference for clinicians.
That could result in rituals that foster human connection during patient history-taking and exams or could lead to new care models where physicians spend less time interacting with electronic health records and have more autonomy to determine how much time they spend with individual patients.
“It’s actually a really challenging problem,” Zulman says. “If there were a simple solution, and all you have to do is make eye contact and we’re done, we would have figured that out already.”
Online extra:
Patricia Hannon
Patricia Hannon is the associate editor of Stanford Medicine magazine in the Office of Communications. Email her at [email protected] .
Email the author
customer experience
Understanding the whole patient, a model for holistic patient care.
Working in healthcare, I consistently encounter processes and care offerings that are very rigid and don’t match up with the individual needs and values that patients have. Commonly, I hear stories about patients not feeling heard or respected by clinicians because what is recommended to them doesn’t align with who they are and what they believe. A lot of these issues stem from the fact that, in medicine, people are traditionally triaged and cataloged by medical condition and/or need.
While identifying and understanding the medical needs of an individual is obviously crucial in effectively treating a collection of conditions, it is rather limiting as a means of capturing who a patient is as a person. A whole patient understanding is crucial. Quite simply, people don’t perceive themselves as a collection of conditions. Health is personal, intertwined with people’s individual perceptions and mindsets, with the environments in which they live and work and the people with whom they interact. While the notion of understanding people as people perhaps appears obvious, health systems still struggle to identify what information should be captured to understand a patient holistically, and how best to engage a patient in a conversation that uncovers this information. This gap leads to misalignment between the patient and care provider, which in turn leads to poor clinical outcomes and negative patient experiences.
With discussion in the industry about patient experience and the surrounding reimbursement challenges , it’s worth thinking about how healthcare might consider the whole person to deliver a better experience, geared toward positive outcomes.
What is a “whole person understanding” of a patient?
To succeed in providing health services centered around a patient, providers must meet patients where they are: functionally, emotionally, and socially. They must understand the values their patients hold, based on their makeup as a whole.
When we talk to people about how they perceive their health, they commonly describe it as a whole, inclusive of their mental state, family, and beliefs.
I was part of work completed at the Mayo Clinic's Center for Innovation which supports these findings that a holistic understanding of a patient is made up of many layers.

Graphic from Patient Type Research, completed by Meredith Dezutter, Mathew Jordan, and Kate Dudgeon on behalf of Mayo Clinic’s Center for Innovation.
At the core of every patient is his or her medical condition or need : heart disease, pregnancy, stage 3 breast cancer, or maybe weight loss. What’s important to note here is that if an individual has a number of health issues, he or she perceives their medical needs as a whole and interconnected. The individual is not focused on singular diseases, as perhaps a specialized clinician might be. From minor to major, the medical or health-related need is what defines the care request and clinical interaction. One of the individuals we spoke to as part of this work had suffered a debilitating fall, which left her with multiple medical and neurological issues. She felt that none of the physicians would take the time to sit down with her and come up with a holistic strategy. Her health issues were looked at “as one-offs, not as a whole person,” which led to disjointed and disconnected care.
Psychosocial:
Layered atop the medical is the psychosocial state : the mental and emotional state, social system, and functional capabilities of a patient. Does this person suffer from anxiety? Is he or she depressed? Does this person’s social support network and environment foster a positive psychosocial state?
One’s psychosocial state ties closely to what many refer to as the social determinants of one’s health . This layer is crucial to understand because it can either inhibit or enable a person’s ability to actively take part in caring for him or herself. For example, many people find themselves in a deep depression following a diagnosis, after realizing that their once-normal state is no longer. This was very true of another individual we spoke to as part of this work, who was suffering from Crohn’s disease and decided to see a psychiatrist who “helped me see and treat certain aspects of my condition that are not addressed medically.”
Attitudes and Beliefs:
Another component of a whole patient is one’s attitudes and beliefs , which break into two parts. First are the beliefs or perceptions one has formed over time regarding one’s health and care. These beliefs are often based on the individual’s own experiences or those of family and friends. People will often share about an overly positive or negative experience receiving care. For example, someone might recount waiting five hours at a certain emergency department (ED), or how his mother died after a failed regiment of a certain type of cancer treatment. Frequently, these negative experiences transform into vows to never return to a particular facility, or to never have a certain treatment, despite the fact that the facility may be widely regarded in a positive light or the treatment may be the best option for the patient.
The second part is the attitudinal category one falls into, which depends largely on how much involvement the individual has in his or her own health and care. A minimalist might be someone who denies a health condition or does the bare minimum recommended by a health care provider. A maximalist, on the other hand, might be someone who proactively seeks health information and is engaged in her own care planning. The attitudinal category one falls into is linked to an individual’s personal experiences or those of family and friends. This category will inevitably change over time, as one is exposed to new such experiences.
One proactive individual I met while conducting research for a past project had strong beliefs and perspectives against the use of blood transfusions. After giving birth to her premature baby, who was in critical condition, a number of physicians recommended a blood transfusion for her daughter. “I felt backed up against a wall,” she explained. “The doctors wouldn’t listen to me.” She eventually found a doctor that she felt would listen to her and she was able to discuss and land on a treatment option that didn’t require a transfusion. Her takeaway: “I learned that when I feel strongly about something, [doctors] have to explore it enough until you prove me otherwise. I like doctors that are willing to work with me [and] will work with me through my ignorance.”
Information and Communication Preferences:
The last component that makes up a whole patient is information and communication preferences : how someone learns, when someone is open to learning, how someone seeks out information, and how someone prefers to exchange information with a care team. For example, we have found a growing preference among people to email or message their doctor when they encounter a health question rather than initially scheduling an appointment, as it provides a quick and convenient response to their discrete need. Some will go as far as seeking out care teams that offer email or messaging services, or other communication methods that they value and use.
As these layers are added, a clearer, more complete picture of a patient’s unique values will start to emerge. The differences in the makeup of the layers highlights that—while the medical prognosis may be the same across two patients—the delivery of care, proposed care plan, and manner in which the care plan is communicated could be vastly different to best align with who those two individuals are.
One healthcare organization that has started to peel away at the layers of a patient to truly recognize and understand who they are is Iora Health, a Cambridge, Massachusetts-based primary care provider organization. Iora has built a unique care model that has recently gained traction with many other health systems. They start by working from a care team model that employs a doctor, nurse, behavioral health specialists (as needed), and a Health Coach. Health Coaches are hired both for their interpersonal skills as well as for their awareness of the communities the patients are from, helping inform the whole person understanding. As Iora's website explains, “we know people by name, but more importantly by their dreams, fears, and challenges.”
Without a whole patient understanding comes misalignment. Otherwise manageable chronic conditions will continue to spiral out of control when a patient’s denial attitude towards their health isn’t identified and supported through coaching. Otherwise straightforward heart procedures will result in continued hospital readmissions when a poor home life is not identified, or an unsupportive spouse who encourages frequent fast food meals is not educated alongside the patient, throughout the full course of a procedure. The model of healthcare will continue to be reactive, rather than proactive, if health systems aren’t set up to holistically understand and support patients.
Truly understanding patients is complex work, but focusing on them as multi-faceted individuals will enable the design and delivery of people-centered care and service offerings. Gone should be the days of patients feeling unheard or seen as a number, because it is possible to meet individual people where they are holistically: emotionally as well as medically. Models such as this one can be used as a tool to start. The process begins by recognizing the four layers to a patient and using them as a template, first to guide information-gathering from patients, and then to design the right solutions and appropriate care paths custom to the individual patient.
Related Content

Copied to clipboard
Exclusive: We have 30% off Alicia Keys' skin care line – and it's selling out fast
- TODAY Plaza
- Share this —

- Watch Full Episodes
- Read With Jenna
- Inspirational
- Relationships
- TODAY Table
- Newsletters
- Start TODAY
- Shop TODAY Awards
- Citi Concert Series
- Listen All Day
Follow today
More Brands
- On The Show
Patients now have access to doctor's visit notes: A guide to what's inside
What does your doctor really think about your condition and health concerns? For more than a year now, patients have been able to access and read the observations doctors write down about them during a visit.
The clinical notes can come with surprises. Patients may be amused to find out they’re described by their physician as “well-nourished,” “well-groomed,” “pleasant” or “normal-looking.”
“’He is not ill-appearing or toxic-appearing.’ That’s the best review I’ve ever received,” one man wrote on Twitter after reading his doctor’s notes.
But patients may also be taken aback by comments referring to them as “obese” or mentioning their marijuana use. One woman was shocked when she saw her doctor wrote down that she “seemed overly dramatic,” she complained on Reddit .
As of April 2021, healthcare providers must give patients access to all of the health information in their electronic medical records as part of the 21st Century Cures Act . That includes your doctor’s written comments about your physical condition during a visit, along with any symptoms and what the treatment should be.
The rules don’t apply to psychotherapy notes made during counseling sessions or when doctors believe a patient would harm another person or themselves after reading the information, according to OpenNotes , a non-profit organization based at Beth Israel Deaconess Medical Center in Boston that advocates for greater transparency in healthcare.
Doctors have been both supportive and cautious of the movement. In a 2020 survey of 1,628 clinicians, 74% agreed note sharing was a good idea.
“It does give the patient a lot more ownership of their medical condition because they can see what we’re thinking about, they understand our thought processes a little bit more, and they can see what the options are,” Dr. Sterling Ransone, Jr., a family physician in Deltaville, Virginia, and chair of the American Academy of Family Physicians, told TODAY.
But knowing that patients can now read his notes, Ransone finds he self-censors himself to avoid sounding critical or judgmental of a patient.
“It’s difficult because sometimes you have to leave a note to yourself what your concerns are, but they can cause anxiety with the patient,” he noted. “I can say that it really has changed the way that a lot of physicians write their notes.”
That means more accessible language, less jargon and more caution with certain terms that might offend or upset a patient.
Ransone no longer uses the abbreviation “SOB,” which stands for “short of breath” and instead writes out the full term in his notes. Same with “FU,” which stands for “follow up.”
The American Academy of Family Physicians has also urged doctors to write “patient could not recall” instead of describing them as a “poor historian;” “patient declines” instead of “patient refuses;” and “patient is not doing X” instead of describing them as “non-compliant.”
A guide to your doctor’s note:
The medical note has traditionally included four parts, Ransone said: The subjective findings, or what a patient said they were concerned about; the objective findings, or what the doctor actually observed during the visit; the physician’s assessment after evaluating the patient and the treatment plan.
Doctors are used to jotting down any observations that can offer clues to what’s going on. So writing down that a patient “seemed overly dramatic” can mean the person’s complaint wasn’t consistent with the degree of their symptoms and something else might be the reason for their visit that day, he noted.
Here are other descriptions patients may find in their doctor’s notes:
Well-groomed or pleasant: This can indicate mental status. “If someone comes in and they’re somewhat disheveled, it leads you to wonder why and what do I need to look into?” Ransone said. “Pleasant” means the patient was communicative and responded to social cues, he noted. Patients who are upset or sleepy could have a substance abuse disorder or another reason why they’re having trouble interacting.
Well-developed or well-nourished: “A lot of times when people look at open notes and they’ll say, ‘Well, of course I am. What does this mean?’” Ransone said. “It just means that we checked in our mental checklist… (that) those aren’t things that we need to worry about.” If a person isn’t well-nourished, it might mean they don’t have access to food or their teeth might be in such bad condition that they can’t chew and get nutrition.
Unremarkable: This is a good thing. “Unremarkable is exactly what you want to be when you see a physician,” Ransone said. “I joke with my patients all the time: You want to be the most boring patient that I’ve seen today, because that means we haven’t seen anything that is abnormal that we need to chase down.”
Obese : To a physician, the term means the patient is of a certain weight for their height and frame, which comes with a certain constellation of medical concerns, Ransone said. “There’s a stigma to obesity in society and a lot of patients really don’t want to have that on their charts… but it’s a very important piece of the puzzle for me as I’m trying to help a patient get healthier,” he noted.
Substance use: This isn’t necessarily bad. Doctors will note a patient has an occasional glass of wine, for example, to give them an idea of the person’s alcohol consumption habits. “The way that our society looks at, say, marijuana use has changed a lot over the years, but a lot of people don’t want that included in the medical record,” Ransone said. “I’d like to know if someone is smoking weed because it could affect the medications that I should give them for their health condition.”
Other health observations patients frequently don’t want on their chart include mental health issues such as depression, anxiety or bipolar disorder, he noted.
Some patients have called Ransone to ask that he change something in their note because they see it as a pejorative or they disagree with his assessment, but that doesn’t mean he’s wrong, the doctor noted.
One guide for physicians suggested telling the patient: “I’m sorry you disagree with my assessment. While I can’t change my medical opinion, if you’d like I can add that you disagree with it.”
Patients pointing out factual errors — such as noticing the note referenced a problem in the right knee rather than the left — is a completely different issue. If there's anything inaccurate in your chart, bring it to your doctor's attention.
In fact, patients who read their doctor’s notes may play an important role in finding errors in their records, a 2020 study published in JAMA found.
Ransone encouraged patients who are reading their doctor’s notes to keep the lines of communication with their physician open.
“Don’t necessarily assume the worst when they read things. Realize that a lot of the things that they read are open to interpretation,” he advised.
A. Pawlowski is a TODAY health reporter focusing on health news and features. Previously, she was a writer, producer and editor at CNN.

Patient and Doctor, Doctor and Patient
A look inside an important relationship..
Posted February 13, 2022 | Reviewed by Jessica Schrader
- The patient-doctor relationship is an important aspect of treatment.
- Patients and doctors are both human and their flaws play a role in their relationship.
- The relationship between patient and doctor has no room for bias, discrimination, or pre-conceived notions.
A patient’s relationship with their doctor is different than the doctor’s relationship with their patient. That there are two different relationships is often what underlies the efficacy and the success of their work together—their work being, of course, the improved health of the patient.
This shared goal of the health and quality of life for the patient is what makes this a critical and important relationship. There must be reciprocity between the two sides. It is not necessarily symmetrical but there needs to be a level of acknowledgment and certain assumptions from each party. There is no hierarchy.
There must be an acknowledgment and an assumption on the part of the doctor of the sincerity and authenticity of the suffering of the patient, and the resultant changes in their lives, including their relationships with family members, friends, and colleagues, and their ability to engage in activities and tasks as they had prior to their illness.
And there must be an acknowledgment and an assumption on the part of the patient that their doctor is human and, like all humans, has had suffering to some extent and has frailties and capacities that can change from day to day, and are very much dependent on what else may be happening in their professional or personal life.
Obviously, an important dissimilarity is that doctors have chosen to be doctors but no one chooses to be sick; this is inherent in the interaction.
Compassion and kindness toward another human being can be the spark that diffuses tension and conflict between two people, groups, or communities. We all yearn to be nurtured and cared about. Human connection is necessary for life and health and is the underpinning of the distinctive relationship between a patient and a doctor.
A doctor can sense when a patient is mistrusting and this may affect the disposition of the doctor and change the energy of the relationship. Similarly, a patient can sense when a doctor is not vested in their care or is distracted, and this too can have an impact on their bond.
The bond between a patient and a doctor can be tenuous but it can also be a source of great support. Some of my greatest experiences as a doctor are from deep connections with my patients. The art of medicine is lost today because of external controls of patient care and the ability to connect with a patient has been compromised. But it can still be obtained.
In medical school, we are trained to interview patients: Ask questions. Get answers. Fill in the algorithm and arrive at a diagnosis that will guide the treatment and discussion offered. It is recommended to not ask open-ended questions, as that may lead us off track of the purpose of the visit.
While there is certainly some truth to that and doctors need to be sure they are identifying and addressing the chief concern of the patient, this approach does not readily lead us to learn the patient’s story.
Everyone has a story that tells who they are, where they come from, how they think, and how they interpret the world around them. It is within this story that someone’s core being resides and where we can better learn what they are about. And understanding of that core can greatly help a doctor guide the conversation with a patient. Each person is something more than their symptoms and something more than their disease.
Learning the patient's story can further dispel any preconceived notions held by a doctor, as this relationship has no room for biases or discrimination .
Similarly, understanding even a piece of the doctor’s story can also improve the patient’s understanding of the doctor. But the patient rarely gets to learn the story of the doctor as a human. That is not the purpose of the visit, and it is not commonplace that a doctor’s story is told.
Both the patient and the doctor have a role to play in this relationship. The patient’s role is to explain what they are feeling and what they are experiencing in terms of physical and mental health, and certainly to advocate for themselves. The doctor’s role is to listen to the patient and work with the patient to help understand why they are feeling unwell and find therapies to help them improve their health for both the short term and the long term. This can be a journey, one that is so much more gratifying when the relationship is solid.

Real satisfaction comes from the alliance of the two toward a shared goal with a mutual understanding, dedication, and trust that both are human and both need support, albeit at varying levels.
These are excerpts from my forthcoming book.

Ilene S. Ruhoy, M.D., Ph.D. , is a board-certified neurologist, environmental toxicologist, integrative physician, and an expert in complex and chronic disease as well as health and wellness. She has a private consulting practice based in Seattle, and is the Medical Director of the ChiariEDS Center at Mount Sinai South Nassau Medical Center.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
- Programs & Events
Search form
Physician-patient relationship: case 1.
During a visit to her family physician, a 35-year-old woman discloses that she suffers from anorexia nervosa. She complains of fatigue, dizziness, depression, headaches, irregular menses, and environmental allergies. Each day, she uses 15 to 60 laxatives, exercises for several hours, and eats a salad or half a sandwich. At 5'2", she weighs 88 pounds. She demonstrates a good understanding of the diagnosis and the recommended therapy for anorexia. Despite receiving a variety of resource information, the patient refuses any medical intervention. She continues to present to the family physician, offering a variety of somatic complaints.
When a patient's preferences conflict with a physician's goal to restore health, which ethical principle should prevail, patient autonomy or physician beneficence? Does the patient's depression render her incompetent to refuse treatment for her anorexia?
Since this patient could rationally discuss her treatment options and her reasons for declining therapy, she could not be considered incompetent. Respect for autonomy is a central principle of bioethics, and it takes precedence in this case. Although the principle of beneficence could be used to argue for coercion towards treatment, compliance may be better improved by providing an ongoing partnership with the patient. Maintaining a therapeutic relationship with ongoing dialogue is more likely to provide this patient with the eventual ability to pursue therapy.

Strategic insights, perspectives and industry trends for healthcare executives. Brought to you by CareCloud .
Setting Expectations: The New Frontier For Patient Experience
By Tobi Elkin
While healthcare delivery models continue to change and evolve, attracting new patients and retaining existing ones remain key to revenue growth. Patient satisfaction will always be a critical part of growing a healthy practice. Managing expectations with respect to delays, wait times, and the components of a visit, along with communicating the costs associated with various services, can directly impact patient satisfaction and your bottom line.
“Customer experience” is a frequently used phrase that refers to the various ways in which consumers interact with a brand’s products and services. In healthcare, you only need to swap “customer” for “patient,” and “patient experience” refers to each of the touchpoints that connect patients, i.e., consumers of healthcare, to a doctor’s office.
These critical touchpoints include everything from the first call patients place to schedule an appointment (or email), to the online or on-site completion of forms, office check-in, wait-time, the taking of routine vitals, the exam itself, and checkout. Each touchpoint plays a role in a patient’s feeling properly taken care of and his or her confidence in the practice. A practice that fails in even one touchpoint in the continuum of care may see a drop in-office visits and new patients and weak ratings or reviews. And taken together, these can begin to impact revenue growth if they’re not addressed.
The patient experience is closely linked to patient satisfaction, which most practices measure on a periodic basis through surveys. “Patient satisfaction is the business we are in,” said Chrystal Schanewolf, Director, Clinic Operations for OrthoCarolina, a North Carolina–based orthopedic practice with more than 30 locations. “We review patient satisfaction on a monthly basis to identify what we can do better,” she said. A key tool for OrthoCarolina is an online patient survey, the results of which reveal areas for improvement.
One of the biggest issues that impact the patient experience is time spent sitting in the waiting room and exam rooms. “Delays in the office are operationally difficult to define and are often a point of frustration throughout healthcare. For example, some patients feel their appointment starts at their arrival [time] while others see it as their scheduled appointment time. Perspectives also change based on where someone is during the visit, such as the waiting room vs. the exam room,” Schanewolf explained. “The goal with this improvement opportunity is not to eliminate wait times but to manage expectations on the front-end and the experience during the time the patient spends in our office.”
“The goal with this improvement opportunity is not to eliminate wait times but to manage expectations on the front-end and the experience during the time the patient spends in our office.”
OrthoCarolina conducts monthly patient satisfaction surveys and tracks the percentage of patients who felt they were adequately informed of delays. It determined a need to focus on improving the patient experience around delays and wait times.
Testing Workflows To Reduce Patient Wait Time
To understand how it could reduce wait times, the practice launched a pilot program in late 2013 through its Patient Family Centered Care Committee and created a workflow that aimed to improve communications during patient visits. The group, which consisted of staff, managers, and providers, identified steps to improve all aspects of the patient’s appointment. The pilot tested workflows at two different office locations and compared the performance against the company average; it tracked patient satisfaction rates on a monthly basis and tweaked processes along the way.
Prior to the pilot, the two offices logged patient satisfaction rates of 33 percent and 42 percent. Those rates represented the percentage of patients who felt they were kept informed of any delays at the time of their visit. After the first month of data tracking, one of the two offices in the pilot saw a 54 percent satisfaction rate after the implementation of a new workflow. And while the rate dipped slightly the following month, a year and nine months into the program, satisfaction hit a high of 64 percent. The other office reached a high of 61 percent satisfaction just three months into the pilot program.
“After the first month of data tracking, one of the two offices in the pilot saw a 54 percent satisfaction rate after implementation of a new workflow.”
“Overall both offices [in the pilot] were far above the average satisfaction rate of the company. Research shows it takes a good year for a process to sustain itself, and it definitely was a lesson learned in holding accountability to communication and process implementation,” Schanewolf said. Apart from the specific question of whether patients felt properly informed of delays, OrthoCarolina’s overall patient satisfaction hovers around 80 percent annually and improves year-over-year as it targets areas of improvement such as this project.
The findings have helped inform changes. “We were able to use our patients’ feedback on how they felt delays were communicated and use this to make changes within the organization for better patient satisfaction,” Schanewolf said. OrthoCarolina, like other practices, is using technology and a patient flow system to optimize and manage its patients’ time and experience. OrthoCarolina will continue to focus on delays in the office as the demand for appointments is very high, and physicians have expressed a desire to spend more time with patients. To that end, the practice has begun rolling out a new screen-based system to track a patient’s time in various areas of the office. Digital screens are mounted outside of exam rooms to track where the patient is in the appointment process and how long they’ve been waiting in each area.
Technology Identifies Bottlenecks
Schanewolf said that by using the technology, the practices hope to identify bottlenecks in its workflow so it can see in real time when a patient is sitting stagnant in any part of their visit. The system will alert the staff when a patient is waiting too long. She said the system has been implemented in three locations and will be integrated in all-new locations.

When patients arrive, they sign in to a kiosk, which captures the exact time they came in. Then they’re moved to the next step in the visit and assigned to a different staffer who “owns” the patient for the next segment in the appointment. The tablet screen alerts the staffer after 10 minutes with a red exclamation point, which signals the patient has waited too long. The screen is visible to everyone on staff, and the patient is then updated.
The tablet screen alerts the staffer after 10 minutes with a red exclamation point, which signals the patient has waited too long. The screen is visible to everyone on staff, and the patient is then updated.
While a year’s worth of data on the new system isn’t available as of this writing, Schanewolf said OrthoCarolina has noticed that a patient’s visit is a lot longer than they expect it to be. “It’s not necessarily because they’re sitting waiting in one spot for 30 minutes, but because there are a lot of checkpoints to go through in one visit, especially in orthopedic practices.” There are electronic forms and X-rays to complete, and then a visit with the physician and more.
“We have to do a better job of setting expectations with our patients when they make appointments.” Streamlining the process is a challenge since OrthoCarolina has physicians with a lot of subspecialties, all of whom have different needs. “We need to eliminate bottlenecks, make adjustments in our physicians’ templates, spread out new patient slots, and cluster-in quicker visits and follow-ups,” she said.

By extension, the practice could also give each patient a tablet that they keep throughout the course of their visit. The tablet would be used to check in, check out, pay co-pays, and view educational videos on various topics like knee pain and shoulder issues in order to make the most of their time. OrthoCarolina is also considering offering “live” patient satisfaction surveys using the same questions as the email survey, but patients would rate their experience on the tablet, in-person.
Web App Cuts Patient Wait for Appointments with Specialists
Dr. Paula Muto, a Boston-based vascular and general surgeon, believes technology, coupled with a human touch, can help improve the patient experience. She created UberDoc in 2016, a web application designed to make it easier for patients to land appointments by offering them direct access to a specialist for an accelerated appointment date. “Going to a doctor’s office can be like going through airport security, especially if you need a referral,” Muto joked.

As a specialist based in Lawrence, Mass., and one who works with an economically disadvantaged population, she was tired of seeing patients having to go through “10 hoops” to see her due to insurance rules. “There are so many steps in the process and a wait to see a specialist in Massachusetts,” she said. Doctors who use UberDoc set aside a couple of appointment slots per week to speed patients through the process. For the first appointment, patients pay $300 via credit card or health savings account, which includes $50 to make the appointment and $250 once they’ve been seen. After the first appointment, insurance is used.
The app also enables her and the other physicians who use it to communicate with patients at any hour, on demand: “It’s like a walk-in model for specialists,” she explained.
In addition, Muto has built other efficiencies into her practice. For example, during office hours, patient calls are routed to an answering service, which makes the appointments, freeing up her staff to focus exclusively on patients who are in the office. “I want attention on my patients. I don’t like people on the phone in the office booking appointments and talking to insurance companies. I want staff to focus the time on the patient at the window,” Muto said.
Her personal touch is also part of improving the patient experience in a healthcare system dominated by online portals, EMR (electronic medical record) systems, diagnostic codes, and scuffles with insurance providers that offer conflicting answers to patients’ questions about benefits and referrals. “When it comes to a pathology report, I pick up the phone and talk to my patients; it’s low-tech and much more efficient.”
Muto would like to see UberDoc offered as a subscription model for doctors and for it to appear in the office “window” alongside of Visa, Mastercard, and American Express. “Any service where a patient can skip cumbersome administrative steps and get right to the doctor is inherently valuable and offers relief in those times of stress when a delay is no longer tolerable,” Muto said. “We need more innovative ideas that increase access and decrease cost and simplify things. We need to give patients an affordable choice and allow doctors to provide it.”
“We need more innovative ideas that increase access and decrease cost and simplify things. We need to give patients an affordable choice and allow doctors to provide it.”
“Price Estimator” Helps Set Patients’ Expectations
Elective plastic surgery procedures can feel a bit like looking at a Chinese menu—a bewildering buffet of options but without pricing. Jonathan Kaplan, a San Francisco–based board-certified plastic surgeon, does his bit to improve the patient experience by reducing sticker shock for patients and prospective patients of his practice, Pacific Heights Plastic Surgery.
“So many medically necessary services and cosmetic services are paid out of pocket now because of high-deductible health plans or because they’re not covered by insurance, so we offer a Price Estimator ,” Kaplan explained. The Price Estimator appears on Kaplan’s website and is also an app that patients who come in for a consultation can use in the waiting room. The tool offers instant gratification in terms of determining out-of-pocket costs and can be used repeatedly to calculate potential costs well before an appointment is made. When prospective patients use the Price Estimator, Kaplan’s practice obtains contact information, and the prospective patient becomes a “lead” that his practice can remain in contact with.

Consumers can scroll through different procedures using the Price Estimator and add procedures to a wishlist. After they submit the list with their contact information, they receive an email with a breakdown of pricing. “It helps them have a better idea of what they’re responsible for. The benefit is they get accurate pricing information, and we get leads,” Kaplan said.
Kaplan analyzed data that looked at 412 wish lists from 208 unique individuals over the course of a year. He found that of those 208 people, 17.8 percent came in for a consultation, and the others checked pricing information using the tool. The upshot is that he didn’t waste time on consults that went nowhere, but his practice did get contact information, and those prospects eventually came into the office. Of the 17.8 percent of the people with wish lists who came in for consultations, 62 percent of them booked a procedure. “People who knew the pricing ahead of time were 41 percent more likely to book a procedure because they were prepared. It’s a great way for patients and doctors to not waste their time, which improves the patient experience,” Kaplan added.
“People who knew the pricing ahead of time were 41 percent more likely to book a procedure because they were prepared. It’s a great way for patients and doctors to not waste their time, which improves the patient experience.”
Befitting a plastic surgeon’s spa-like facility, Kaplan offers water, tea, coffee, and healthy snacks. A bonus: Netflix is available in the CoolSculpting room.
Reducing Wait Times, Eliminating Unnecessary Steps
John Snow, Inc. (JSI), a public health research and consulting firm, offers physicians’ practices and publicly funded clinics recommendations on how to improve the patient experience. It has found that the most common complaint among patients is wait time. “There are lots of ways to approach it through staffing models, appointment scheduling adjustments, and basic clinic flow,” said Jennifer Kawatu, senior consultant at JSI, and a technical assistance provider who does patient experience work with publicly funded organizations.
“We encourage eliminating unnecessary steps to eliminate waste and improve workflow. You can put the patient in one room and have the services provided in that one room; you don’t move them around, everyone comes to them,” she said. Keys to improving the patient experience are eliminating services that aren’t of value to the patient and focusing on the specific reason for the visit.
Kawatu said that while a lot of time and energy is spent on doing quantitative surveys of practices, there is often little variation in the findings, and they can net a false sense of satisfaction. Across the board, she said, most patients in the practices she works with uncover the most useful information by asking qualitative, open-ended questions, like “What could we have done to make your visit better today?” These types of questions reveal specific complaints.
Publicly funded clinics receive subsidies to provide services and agree to accept Medicaid patients. However, they still bill for services, and it’s a way for them to see more patients. When these clinics start billing and become more sustainable practices, they might be able to attract more private-pay patients who are able to pay more. “In providing a better experience, they can attract private pay patients, those who have employer-sponsored health plans,” Kawatu said. If the family planning clinics she works with that provide same-day services can reduce wait times, they can compete with private practices.
If the family planning clinics she works with that provide same-day services can reduce wait times, they can compete with private practices.
Customized Visits, No Wait Time
Dr. Napoleon Maminta is an internist who launched his own practice, Naptown Priority Health, in 2016 after decades in corporatized healthcare settings. He grew frustrated with patient quotas and short appointment times that didn’t enable him to engage deeply with patients. In his new practice, each visit is 45 minutes long, and he sees about nine patients a day. Wait times are rarely more than five minutes.

His Noblesville, Indiana, practice is referred to as a “Direct Primary Care” model because Maminta has cut the insurance middleman out. He charges $100 a month per adult for unlimited visits and does telemedicine and home visits, which contribute to overall patient satisfaction—and his own.
Maminta offers his patients an iPad to complete a survey after their visits. While he has a waiting room stocked with a library of books, comfortable chairs, and a flat-screen TV, there’s hardly any wait time. “It’s two minutes, at most,” he said. In fact, his post-visit survey probably takes a bit longer than a patient’s wait time.
No matter how healthcare delivery and economic models evolve in the future, communicating with patients and setting expectations about their visits will always be critical to the health of your practice.
Tobi Elkin is a veteran content creator and consultant who enjoys crafting compelling narratives for diverse audiences. Based in New York City, her writing has appeared in newspapers, magazines, and on websites including Advertising Age, AOL, the Associated Press, CMO.com, Narratively, Robb Report, The Huffington Post, and many others. She has consulted on thought leadership, marketing, and content strategy for technology firms, consumer brands, and non-profit organizations.
Download the Patient Experience Playbook
Insights into every aspect of the patient journey
brought to you by

Start typing and press Enter to search
Doctors combine a pig kidney transplant and a heart device in bid to extend a woman’s life

Doctors have transplanted a pig kidney into a New Jersey woman who was near death, part of a dramatic pair of surgeries that also stabilized her failing heart.
Lisa Pisano’s combination of heart and kidney failure left her too sick to qualify for a traditional transplant, and out of options. Then doctors at NYU Langone Health devised a novel one-two punch: Implant a mechanical pump to keep her heart beating and days later transplant a kidney from a genetically modified pig.
Pisano is recovering well, the NYU team announced Wednesday. She’s only the second patient ever to receive a pig kidney — following a landmark transplant last month at Massachusetts General Hospital — and the latest in a string of attempts to make animal-to-human transplantation a reality.
This week, the 54-year-old grasped a walker and took her first few steps.
“I was at the end of my rope,” Pisano told The Associated Press. “I just took a chance. And you know, worst case scenario, if it didn’t work for me, it might have worked for someone else and it could have helped the next person.”
Dr. Robert Montgomery, director of NYU Langone Transplant Institute, recounted cheers in the operating room as the organ immediately started making urine.
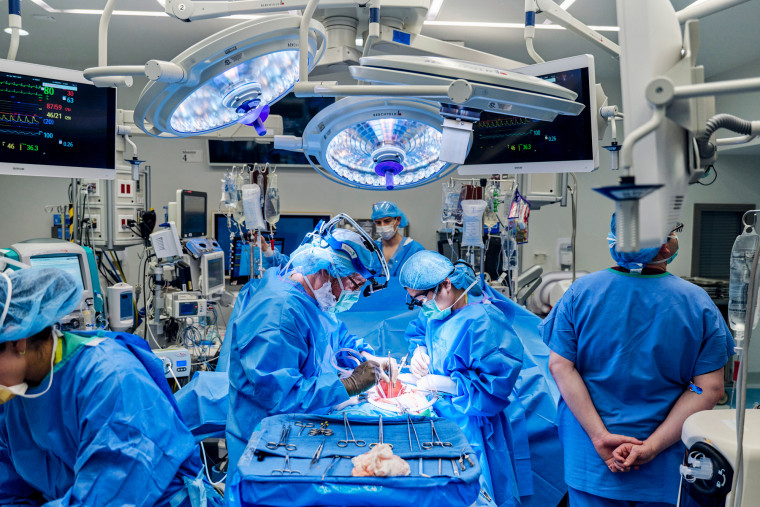
“It’s been transformative,” Montgomery said of the experiment’s early results.
But “we’re not off the hook yet,” cautioned Dr. Nader Moazami, the NYU cardiac surgeon who implanted the heart pump.
“With this surgery I get to see my wife smile again,” Pisano’s husband Todd said Wednesday.
Other transplant experts are closely watching how the patient fares.
“I have to congratulate them,” said Dr. Tatsuo Kawai of Mass General, who noted that his own pig kidney patient was healthier overall going into his operation than NYU’s patient. “When the heart function is bad, it’s really difficult to do a kidney transplant.”
The pig organ quest
More than 100,000 people are on the U.S. transplant waiting list, most who need a kidney, and thousands die waiting. In hopes of filling the shortage of donated organs, several biotech companies are genetically modifying pigs so their organs are more humanlike, less likely to be destroyed by people’s immune system.
NYU and other research teams have temporarily transplanted pig kidneys and hearts into brain-dead bodies, with promising results . Then the University of Maryland transplanted pig hearts into two men who were out of other options, and both died within months .
Mass General’s pig kidney transplant last month raised new hopes. Kawai said Richard “Rick” Slayman experienced an early rejection scare but bounced back enough to go home earlier this month and still is faring well five weeks post-transplant. A recent biopsy showed no further problems.
A complex case at NYU
Pisano is the first woman to receive a pig organ — and unlike with prior xenotransplant experiments, both her heart and kidneys had failed. She went into cardiac arrest and had to be resuscitated before the experimental surgeries. She’d gotten too weak to even play with her grandchildren. “I was miserable,” the Cookstown, New Jersey, woman said.
A failed heart made her ineligible for a traditional kidney transplant. But while on dialysis, she didn’t qualify for a heart pump, called a left ventricular assist device or LVAD, either.
“It’s like being in a maze and you can’t find a way out,” Montgomery explained — until the surgeons decided to pair a heart pump with a pig kidney.

Two surgeries in eight days
With emergency permission from the Food and Drug Administration, Montgomery chose an organ from a pig genetically engineered by United Therapeutics Corp. so its cells don’t produce a particular sugar that’s foreign to the human body and triggers immediate organ rejection.
Plus a tweak: The donor pig’s thymus gland, which trains the immune system, was attached to the donated kidney in hopes that it would help Pisano’s body tolerate the new organ.
Surgeons implanted the LVAD to power Pisano’s heart on April 4, and transplanted the pig kidney on April 12. There’s no way to predict her long-term outcome but she’s shown no sign of organ rejection so far, Montgomery said. And in adjusting the LVAD to work with her new kidney, Moazami said doctors already have learned lessons that could help future care of heart-and-kidney patients.
Special “compassionate use” experiments teach doctors a lot but it will take rigorous studies to prove if xenotransplants really work. What happens with Pisano and Mass General’s kidney recipient will undoubtedly influence FDA’s decision to allow such trials. United Therapeutics said it hopes to begin one next year.
The Associated Press

IMAGES
VIDEO
COMMENTS
Study with Quizlet and memorize flashcards containing terms like A patient visits her doctor and explains that since being hit on the cheek with a hockey puck she has been suffering from dry eyes and a dry mouth. It's apparent to the doctor that, because both lacrimal secretion and salivary secretion are affected, there may be damage to the _____ nerve., Bell palsy is a condition characterized ...
The time constraints of office visits are a concern shared by physicians and patients. Wait time and visit length can certainly affect patient satisfaction, but one study showed that what mattered ...
Patient-centered care builds on discussions and decisions that involve shared information, compassionate and empowering care provision, sensitivity to patient needs, and relationship building. 3 ...
Placing trust in a doctor helps them maintain or regain their health and well-being. This unique relationship encompasses 4 key elements: mutual knowledge, trust, loyalty, and regard. 2 Knowledge refers to the doctor's knowledge of the patient as well as the patient's knowledge of the doctor. Trust involves the patient's faith in the ...
Brown JB, Brett P, Stewart M, Marshall JN. Roles and influence of people who accompany patients on visits to the doctor. Can Fam Physician. 1998;44:1644-1650.
Patient-physician relationships: CEJA reports. Download PDFs of reports on this topic for the Council on Ethical & Judicial Affairs (CEJA) presented during the AMA Interim and Annual Meetings. The ethics of patient-physician relationships is an important topic of discussion. Learn about doctor-patient relationship ethics with the latest from ...
Summary. Informed consent is when your healthcare provider makes sure you understand your diagnosis and the risks and benefits of any tests, medical procedures, or other treatments they recommend to treat your condition. Informed consent is at the core of the shared-decision making process between a patient and their healthcare provider.
However, understanding the patient as much as possible from the start can save a lot of time in subsequent visits. For example, Ofri once had a patient with a long history of trouble adhering to his numerous medication protocols (despite repeated efforts to explain them to him). It took a year of visits with her for the patient to reveal that ...
Virtual or In Person: Which Kind of Doctor's Visit Is Better, and When It Matters. When the covid-19 pandemic swept the country in early 2020 and emptied doctors' offices nationwide, telemedicine was suddenly thrust into the spotlight. Patients and their physicians turned to virtual visits by video or phone rather than risk meeting face-to ...
Introduction. Open and clear communication between the physician and patient is paramount to the delivery of excellent health care. The empathy and quality of this communication correlates with patient satisfaction and knowledge of the diagnoses and treatment plan (1,2).Patient understanding of their medical management plan helps enhance outcomes by improving compliance with treatment plans.
Kelley Skeff, MD, PhD, professor of medicine, who co-directs the Stanford Faculty Development Center for Medical Teachers, says doctors came to the field "to learn and apply science for the benefit of patients.". "But their connections to science and to the patient are commonly impeded by the requirements of the system," he says.
Another component of a whole patient is one's attitudes and beliefs, which break into two parts. First are the beliefs or perceptions one has formed over time regarding one's health and care. These beliefs are often based on the individual's own experiences or those of family and friends. People will often share about an overly positive ...
The clinical notes can come with surprises. Patients may be amused to find out they're described by their physician as "well-nourished," "well-groomed," "pleasant" or "normal ...
Patients and doctors are both human and their flaws play a role in their relationship. The relationship between patient and doctor has no room for bias, discrimination, or pre-conceived notions. A ...
A patient visits her doctor and explains that since being hit on the cheek with a hockey puck she has been suffering from dry eyes and a dry mouth. It's apparent to the doctor that, since both lacrimal secretion and salivary secretion are affected, there may be damage to the _____ nerve. facial. A typical spinal cord in an adult is ...
THE DOCTOR-PATIENT RELATIONSHIP IN AN INTEGRATED CLINICAL METHOD. Doctor-patient relationships evolve over time and are built on regular consultations as well as other shared experiences, such as childbirth, hospitalisations or home visits.2 The goals of care at these encounters over time encompass the conventional goals of diagnosis and cure but also the broader goals of support and healing.
a patient visits her doctor and explains since being hit on the cheek with a hockey puck she has been suffering from dry eyes and a dry mouth. It's apparent to the doctor that since both lacrimal secretion and salivary secretion are affected there may be damage to the _____ nerve a. trigeminal b. hypoglossal c. glossopharyngeal d. abducens e ...
Case Number: 1. During a visit to her family physician, a 35-year-old woman discloses that she suffers from anorexia nervosa. She complains of fatigue, dizziness, depression, headaches, irregular menses, and environmental allergies. Each day, she uses 15 to 60 laxatives, exercises for several hours, and eats a salad or half a sandwich.
Managing expectations with respect to delays, wait times, and the components of a visit, along with communicating the costs associated with various services, can directly impact patient satisfaction and your bottom line. "Customer experience" is a frequently used phrase that refers to the various ways in which consumers interact with a ...
Currently, semaglutide is only approved for weight loss under the brand name Wegovy. The typical dose for weight loss is 2.4 milligrams, administered weekly as subcutaneous (under the skin) self-injections. But as interest in semaglutide for weight loss continues to grow, health care professionals are finding ways to manage the demand.
a patient visits his doctor with complaints of headaches, pounding heart, and muscle tension. with some prodding, the patient begins to talk about his extreme worry about the success of his work, the constant fear that his wife will leave him, and his apprehension about losing other important things in his life. the doctor may feel that this patient's symptoms are due to:
Doctors have transplanted a pig kidney into a New Jersey woman who was near death, part of a pair of surgeries that also stabilized her heart. Lisa Pisano, 54, is only the second patient ever to ...
Study with Quizlet and memorize flashcards containing terms like Doctors employ the Scientific Method to diagnose patients. A patient visits a doctor's office and presents the following symptoms: fever, sore throat, and headache. The doctor looks into the patient's throat and notes that the tonsils are inflamed. The doctor suspects that the patient has strep. She then swabs the throat to ...