
- For Ophthalmologists
- For Practice Management
- For Clinical Teams
- For Public & Patients
Museum of the Eye
- Managing Your Practice
- Managing Your Practice Topics
- Emergency Preparedness and Cybersecurity
- Practice Forms Library
- Practice Management News & Advice
- Lean Management
- Video Library
- My Green Doctor
- Ophthalmology Job Center
- Benchmarking & Salary Tools
- Academy Consultations
- Consultant Directory
- Coding Topics
- Ask the Coding Experts
- Cataract Surgery
- Codequest Events
- Coding for Injectable Drugs
- EM Documentation
- Ophthalmic Coding Specialist (OCS) Exam
- Savvy Coder
- Submit an Instruction Course
- Codequest Courses
- Mid-Year Forum
- Webinar Recordings
- Upcoming Webinars
- IRIS Registry
- Merit-Based Incentive Payment
- Medicare & MIPS
- Promoting Interoperability
- Improvement Activities
- Avoid a Penalty
- Medicare Participation Options
- Medicare Advantage Plans
- New Medicare Card
- Provider Enrollment, Chain and Ownership System (PECOS)
- Membership Benefits
- Renew/Pay Dues
- AAOE Membership
- AAOE Board of Directors
- Practice Views
- AAOE Content Committee
- Volunteer Opportunities
- For Practice Management /
- Ask the Coding Experts /

HCPCS Code G2211 Visit Complexity Add-on Code
Narrow your results, select code type, select topic.
- Cataract/Anterior Segment
- Coding Competency
- Coronavirus
- Oculofacial
- Pediatric/Strabismus
- Revenue Cycle Management
- Telemedicine
- Testing Services
- Trauma Coding
Select Category
About Our Coding Experts
About Our Coding Experts
Our expert staff have decades of combined experience, covering all aspects of coding and reimbursement.
John T. McAllister, MD Secretary, Federal Affairs
Michael X. Repka, MD, MBA Medical Director, Government Affairs
Joy Woodke, COE, OCS, OCSR Director, Coding and Reimbursement
Matthew Baugh, MHA, COT, OCS, OCSR Manager, Coding and Reimbursement Heather H. Dunn, COA, OCS, OCSR Manager, Coding and Reimbursement
Ask the Experts!
Email [email protected]
Note: Coding regulations and edits can change often. Academy coding advice is based on current information. Visit aao.org/coding for the most recent updates. Information provided by our coding experts is copyrighted by the American Academy of Ophthalmology and intended for individual practice use only.
- Mark Complete

All content on the Academy’s website is protected by copyright law and the Terms of Service . This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
- About the Academy
- Jobs at the Academy
- Financial Relationships with Industry
- Medical Disclaimer
- Privacy Policy
- Terms of Service
- Statement on Artificial Intelligence
- For Advertisers
FOLLOW THE ACADEMY
Medical Professionals
Public & Patients

List With CPT Codes For New Patient Office Visits | Short & Long Descriptions and Lay-Terms
4 CPT codes describe the procedures for a new patient office visit . These codes are used to record the level of complexity of the evaluation, management, and medical decision-making during the visit. You can find a complete list of office visits for both established patients and new patients here.
1. CPT Code 99202
Lay-term: CPT code 99202 is used when a healthcare provider performs an office visit for a new patient that requires a medically appropriate history and/or examination and straightforward medical decision making. The total time spent on the encounter must be 15 minutes or more.
Long description: Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and straightforward medical decision making. When using total time on the date of the encounter for code selection, 15 minutes must be met or exceeded.
Short description: New patient office visit, straightforward medical decision making, 15 minutes.
1.2. CPT Code 99203
Lay-term: CPT code 99203 is used when a healthcare provider performs an office visit for a new patient that requires a medically appropriate history and/or examination and a low level of medical decision making. The total time spent on the encounter must be 30 minutes or more.
Long description: Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using total time on the date of the encounter for code selection, 30 minutes must be met or exceeded.
Short description: New patient office visit, low level medical decision making, 30 minutes.
1.3. CPT Code 99204
Lay-term: CPT code 99204 is used when a healthcare provider performs an office visit for a new patient that requires a medically appropriate history and/or examination and a moderate level of medical decision making. The total time spent on the encounter must be 45 minutes or more.
Long description: Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and moderate level of medical decision making. When using total time on the date of the encounter for code selection, 45 minutes must be met or exceeded.
Short description: New patient office visit, moderate level medical decision making, 45 minutes.
1.4. CPT Code 99205
Lay-term: CPT code 99205 is used when a healthcare provider performs an office visit for a new patient that requires a medically appropriate history and/or examination and a high level of medical decision making. The total time spent on the encounter must be 60 minutes or more.
Long description: Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and high level of medical decision making. When using total time on the date of the encounter for code selection, 60 minutes must be met or exceeded.
Short description: New patient office visit, high level medical decision making, 60 minutes.
Similar Posts
How to use cpt code 64897.
CPT 64897 describes the use of a multiple strand nerve graft technique to repair a damaged portion of a nerve in the arm or leg. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 64897? CPT 64897 can be…
CPT Codes For End-Stage Renal Disease Services
Below is a list summarizing the CPT codes for end-stage renal disease services. CPT Code 90951 CPT 90951 describes monthly end-stage renal disease (ESRD) related services for patients younger than two years of age, including monitoring for the adequacy of nutrition, assessment of growth and development, and counseling of parents, with four or more face-to-face…
How To Use CPT Code 72132
CPT 72132 describes the diagnostic procedure of computed tomography (CT) of the lumbar spine with the use of contrast material. This article will provide an overview of CPT 72132, including its official description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information, similar codes, and examples. 1. What is CPT Code 72132? CPT…

How To Use CPT Code 11402
CPT 11402 refers to the excision of a benign lesion, excluding skin tags, on the trunk, arms, or legs with a diameter of 1.1 to 2.0 cm, including margins. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information, similar codes, and examples of CPT 11402 procedures. 1….
How To Use CPT Code 59850
CPT 59850 describes the procedure for induced abortion using intra-amniotic injections. This article will cover the description, official description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 59850? CPT 59850 can be used to describe the procedure for induced abortion using one or more…
How To Use CPT Code 64415
CPT 64415 is a code used for injections of anesthetic agents and/or steroids into the brachial plexus, including imaging guidance when performed. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information, similar codes, and examples of CPT 64415 procedures. 1. What is CPT 64415? CPT 64415 is…
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Disclaimer » Advertising
- HealthyChildren.org
- Facebook Icon
- Twitter Icon
- LinkedIn Icon
2 new codes developed for interprofessional consultation :
Current Procedural Terminology (CPT) codes 99446-99449 were created in 2014 to capture the time spent by a consultant who is not in direct contact with the patient at the time of service.
An interprofessional telephone/internet consultation (ITC) is defined as an assessment and management service in which a patient’s treating (e.g., attending or primary) physician/other qualified health care professional (QHP) requests the opinion and/or treatment advice of a consultant with specific specialty expertise to assist the treating physician/QHP in the diagnosis and/or management of the patient’s problem without the need for the patient’s face-to-face contact with the consultant.
Since the type or severity of the problem is not defined, any condition may qualify for consultative services. However, the codes typically are reported when a new problem arises or a chronic issue is not well-managed or exacerbates.
Only the consultant can report these codes. In addition, these codes require both a verbal and written follow-up report.
Some changes are in store for ITC this year. The American Medical Association Digital Medicine Payment Advisory Group developed two new ITC codes:
- Code 99451 is reported by the consultant, allowing him/her to access data/information through the electronic health record (EHR), in addition to telephone or internet.
- Code 99452 is reported by the requesting/treating physician/QHP (e.g., the primary care physician).
The table outlines distinctions between consultant codes 99446-99449 and the new consultant code 99451 as well as distinct features of code 99452.
Consultant codes99446-99449 and 99451:
- can be reported for new or established patients
- can be reported for a new or exacerbated problem
- are reported only by a consultant when requested by another physician/QHP
- cannot be reported more than once per seven days for the same patient
- are reported based on cumulative time spent, even if that time occurs on subsequent days
- are not reported if a transfer of care or request for a face-to-face consult occurs as a result of the consultation within the next 14 days
- are not reported if the patient was seen by the consultant within the past 14 days
- require that the request and the reason for the request for the consult be documented in the record
- require verbal consent for the interprofessional consultation from the patient/family documented in the patient’s medical record
Requesting/treating physician/QHP code 99452:
- is reported by the physician/QHP who is treating the patient and requesting the non-face-to-face consult for medical advice or opinion — and not for a transfer of care or a face-to-face consult
- is reported only when the patient is not on-site and with the physician/QHP at the time of the consultation
- cannot be reported more than once per 14 days per patient
- includes time preparing for the referral and/or communicating with the consultant
- requires a minimum of 16 minutes
- can be reported with prolonged services, non-direct

Q. A physician was asked to consult on a pediatric patient. The progress notes and lab studies were sent electronically for review. The patient is established to the consulting physician’s practice but is being managed primarily by her primary care physician for a condition that is not improving as expected. The consulting physician reviews the notes and documents time as follows:
- five minutes on Tuesday (chart notes and data review)
- 15 minutes on Thursday (phone consult with primary care physician) and three additional minutes writing up discussion
How is this reported?
- Report based on the total time spent. In total, the consultant spent 20 minutes, and more than 50% was spent on the consultative discussion. Because the criteria for reporting code99448 or 99451 are met, the consulting physician should report code 99448.
Q. A school counselor asked a physician in our practice to review some records and call her to discuss the patient’s behavioral issues. In total, the physician spent 15 minutes. What ITC code can we report?
A. The ITC codes are not applicable because the school counselor does not meet the criteria of a QHP.
Q. A physician (consultant) performs an ITC where she spent 15 minutes total. She drafted the written report and sent it back. Should I submit the claim right away since there is a 14-day window for a service, which will bundle the ITC codes?
A. Hold all claims until 14 days have passed. Even if the initial consult did not result in a transfer of care, the ITC codes are not separately payable if another service is performed within 14 days of the consult, including an evaluation and management (E/M) service or procedure/surgery.
Q. What written documentation and patient information are needed to file with insurers?
A. For codes 99446-99449, written documentation can include date of call; patient name, insurance information and date of birth; brief statement of the problem; pertinent physical exam findings reported by the requesting/treating physician/QHP; labs/X-ray findings; differential diagnosis (if applicable) and focused recommendations.
Documentation for codes 99451-99452 most likely will occur through each organization’s EHR. Over time, code 99452 may be used for telephone and internet consults as well. Each institution may develop a template for the requesting/treating physician/QHP and the consulting physician for documentation and billing.
Note: Billing for interprofessional services is limited to practitioners who can independently bill Medicare for E/M services. Though the descriptors for codes 99446-99449 and 99451 only include “assessment and management service provided by a consultative physician,” the text in the rule includes consultative QHPs, as long as the consulting QHP is eligible to independently bill Medicare for E/M services. CPT code 99452 applies to the treating/referring physician/QHP, and the rest of the codes apply to the consultative physician or QHP. Most importantly, the Centers for Medicare & Medicaid Services requires documentation of the patient’s/family’s verbal consent in the medical record for each interprofessional consultation service.
Dennis L. Murray, M.D., FAAP, contributed to this article.
- For more information on the interprofessional telephone/internet consultation codes, see AAP News article “New year brings new, revised CPT codes for pediatrics”
- Additional Coding Corner columns
Advertising Disclaimer »

Email alerts
1. 4 million children lose Medicaid, CHIP insurance after public health emergency protections end
2. Long hours, guilt, more compassion: Pediatrician moms share stresses, rewards
3. CDC releases 2024 immunization schedules
April issue digital edition

Subscribe to AAP News
Column collections
Topic collections
Affiliations
Advertising.
- Submit a story
- American Academy of Pediatrics
- Online ISSN 1556-3332
- Print ISSN 1073-0397
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account

CPT CODE 99391, 99395, 99396, 99397, 99394 – Preventive Exam
Sep 12, 2016 | Medical billing basics

CPT CODE AND Description
99391 – Periodic comprehensive preventive medicine reevaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, established patient; infant (age younger than 1 year) – Average fee amount $90
99392 – Periodic comprehensive preventive medicine reevaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, established patient; early childhood (age 1 through 4 years) Average fee amount $105 99393 – Periodic comprehensive preventive medicine reevaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, established patient; late childhood (age 5 through 11 years) Average fee amount $110
99394 – Periodic comprehensive preventive medicine reevaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, established patient; adolescent (age 12 through 17 years) Average fee amount $120
99395 – Periodic comprehensive preventive medicine reevaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, established patient; 18-39 years 99396 – Periodic comprehensive preventive medicine reevaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, established patient; 40-64 years 99397 – Periodic comprehensive preventive medicine reevaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, established patient; 65 years and older
Referral/notification/preauthorization requirements
There are no referral/preauthorization requirements for well baby/well child care visits when provided by a contracted FCHP primary care physician within the member’s product network.
Billing/coding guidelines
For new patients making a well baby/well child care visit:
• For infants under age 1, use CPT code 99381.
• For children ages 1 to 4 (early childhood), use CPT code 99382.
• For children ages 5 to 11 (late childhood), use CPT code 99383.
• For children ages 12 to 17 (adolescent), use CPT code 99384.
• For children age 18 (adolescent), use CPT code 99385.
For established patients making a well baby/well child care visits:
• For infants under age 1, use CPT code 99391.
• For children ages 1 to 4 (early childhood), use CPT code 99392.
• For children ages 5 to 11 (late childhood), use CPT code 99393.
• For children ages 12 to 17 (adolescent), use CPT code 99394.
• For children age 18 (adolescent), use CPT code 99395.
Preventive Medicine Visits • Not all insurers pay for preventive medicine visits. For example, these visits are not covered by Medicare.
If you suspect a patient does not have coverage, advise him or her of your billing policies.
• Insurers that do cover preventive medicine visits (eg, many HMOs) generally reimburse them at relatively high rates.
• Regardless of whether a preventive medicine visit is covered, the relevant codes can be used alone or in conjunction with a code for an E&M service (see below).

Patient and Visit Preventive Medicine Code
New patient, initial visit Age 40 through 64 years 99386 Age 65 years and older 99387 Established patient, periodic visit Age 40 through 64 years 99396 Age 65 years and older 99397
Preventive Medicine Services: Established Patients
Periodic comprehensive preventive medicine reevaluation and management of an individual includes an age- and gender-appropriate history; physical examination; counseling, anticipatory guidance, or risk factor reduction interventions; and the ordering of laboratory or diagnostic procedures. CPT Codes ICD-9-CM Codes
99391 Infant (younger than 1 year) V20.31 Health supervision for newborn under 8 days old
V20.32 Health supervision for newborns 8 to 28 days old
V20.2 Routine infant or child health check
99392 Early childhood (age 1–4 years) V20.2 Routine infant or child health check
99393 Late childhood (age 5–11 years) V20.2 Routine infant or child health check
99394 Adolescent (age 12–17 years) V20.2 Routine infant or child health check
99395 18 years or older V70.0 Routine general medical examination at a health care facility
Preventive Medicine Services [Current Procedural Terminology (CPT®) codes 99381-99387, 99391-99397, Healthcare Common Procedure Coding System (HCPCS) code G0402 are comprehensive in nature, reflect an age and gender appropriate history and examination, and include counseling, anticipatory guidance, and risk factor reduction interventions, usually separate from disease-related diagnoses. Occasionally, an abnormality is encountered or a pre existing problem is addressed during the Preventive visit, and significant elements of related Evaluation and Management (E/M) services are provided during the same visit. When this occurs, Oxford will reimburse the Preventive Medicine service plus 50% the Problem-Oriented E/M service code when that code is appended with modifier 25. If the Problem-Oriented service is minor, or if the code is not submitted with modifier 25 appended, it will not be reimbursed.existing problem is addressed during the Preventive visit, and significant elements of related Evaluation and Management (E/M) services are provided during the same visit. When this occurs, Oxford will reimburse the Preventive Medicine service plus 50% the Problem-Oriented E/M service code when that code is appended with modifier 25. If the Problem-Oriented service is minor, or if the code is not submitted with modifier 25 appended, it will not be reimbursed.
Policy Statement
Preventive medicine services are comprehensive in nature, reflect an age and gender appropriate history and examination, and include counseling, anticipatory guidance, and risk factor reduction interventions, usually separate from diseaserelated diagnoses. Occasionally, an abnormality is encountered or a pre-existing problem is addressed during the preventive visit, and significant elements of related E/M services are provided during the same visit. When this occurs, Medica will reimburse the preventive medicine E/M service at the contracted rate and the problem-oriented E/M service at 75% of the contracted rate, when appended with modifier 25.
Procedure codes used to bill preventive medicine services are:
** Current Procedural Terminology (CPT®) codes 99381-99387, 99391-99397
During a visit for a preventive medicine service, other services may be provided.
HealthWatch EPSDT codes PLUS Evaluation & Management (E&M) Codes PLUS Modifier 25*
PLUS ICD-9 Diagnosis Codes 99381–99385or 99391–99395
The components of the EPSDT visit must be provided and documented.
99203–99215 The presenting problem must be of moderate to high severity Documentation must support the use of a modifier 25
V20.2 must be the primary diagnosis code for the preventive visit Add multiple diagnosis codes for the presenting problem focused evaluation.
THE PREVENTIVE SERVICE E/M VISIT WITH A PROBLEM-ORIENTED SERVICE: AN EXAMPLE
A 52-year-old established patient presents for an annual exam. When you ask about his current complaints, he mentions that he has had mild chest pain and a productive cough over the past week and that the pain is worse on deep inspiration. You take additional history related to his symptoms, perform a detailed respiratory and CV exam, and order an electrocardiogram and chest X-ray. You make a diagnosis of acute bronchitis with chest pain and prescribe medication and bed rest along with instructions to stop smoking. You document both the problem-oriented and the preventive components of the encounter in detail. You should submit 99396, “Periodic comprehensive preventive medicine…, established patient; 40-64 years” and ICD-9 code V70.0, “Routine general medical examination at a health care facility”; and the problem-oriented code that describes the additional work associated with the evaluation of the respiratory complaints with modifier -25 attached, ICD-9 codes 466.0, “Acute bronchitis” and 786.50, “Chest pain” and the appropriate codes for the electrocardiogram and chest X-ray.
Bill Diagnosis code(s) V70.0
Routine exam Procedure code(s) 99396
Preventive service 466.0 786.50
Acute bronchitis Chest pain 99213-25*
Office outpatient E/M service for established patient 93000
Electrocardiogram 71020
Chest X-ray, PA and lateral
*The level of service represents only an example. The level reported should be determined by the documented history, exam and/or medical decision-making.
CPT Code for Initial Evaluation of New Patient (Bold)
CPT Code for Periodic Reevaluation
99381 – 99391 – Under 1 year
99382 – 99392 – 1-4
99383 – 99393 – 5-11
99384 – 99394 – 12-17
99385 – 99395 – 18-39
99386 – 99396 – 40-64
99387 – 99397 – 65 and over
Code 99420 is specific to administration and interpretation of health risk assessment instruments.
Payers may or may not allow use of this code for behavior-related questionnaires such as the Pediatric Symptom Checklist or one of the longer alcohol- or depression-related questionnaires.
Finally, the last of the preventive medicine codes is 99429, Unlisted Preventive Medicine Service. Practitioners are urged to check with the managed care plan or insurance carrier before using this code.
PREVENTIVE CODES THAT SHOULD GENERALLY BE COVERED AT NO OUT OF POCKET COST FOR BCBSIL HMO MEMBERS Preventive Medicine Services – Adult Established Patient: 99394 – adolescent (12-17) 99395 – 18-39 years 99396 – 40-64 years 99397 – 65 years and older Preventive Medicine Services – Pediatric Established patient: 99391 – age younger than 1 year 99392 – age 1-4 years 99393 – age 5-11 years
99211 99212 99213 99214 99215 Mutually Exclusive 99391 99392 99393 99394 99395 99396 99397
Therefore, 99211-99215 is submitted with 99391-99397–only 99391-99397 reimburses.
Preventive Medicine Evaluation & Management (E&M) Services
* Preventive Medicine E&M services should be reported using the age appropriate code from the Preventive Medicine Services section of the most current CPT manual.
* Services rendered should be reported using 99381-99387 for new patients or 99391-99397 for established patients. These codes include counseling/anticipatory guidance/risk factor reduction interventions which are provided at the time of the initial or periodic comprehensive preventive medicine examination.
* If an abnormality/ies is encountered, or a preexisting problem is addressed in the process of performing a preventive medicine E&M service, and if the problem/abnormality is significant enough to require additional work to perform the key components of a problem-oriented E&M service, then the appropriate office/Outpatient code 99201-99215 should also be reported.
Modifier-25 should be added to the Office/Outpatient code to indicate that a significant; separately identifiable E&M service was provided by the same physician on the same day as the preventive medicine service. Note: An insignificant or trivial problem or abnormality that is encountered in the process of performing the preventive medicine E&M service and which does not require additional work and the performance of the key components of a problem-oriented E&M service should not be reported.
Evaluation and management services including new or established patient office or other outpatient services (99201-99215), emergency department services (99281-99285), nursing facility services (99304-99318), domiciliary, rest home, or custodial care services (99324-99337), home services (99341-99350), and preventive medicine services (99381-99397) on the same date related to the admission to “observation status” should not be reported separately.” (AMA7)
“An E&M service is separately reportable on the same date of service as a procedure with a global period of 000, 010, or 090 under limited circumstances…If an E&M is performed on the same date of service as a major surgical procedure for the purpose of deciding whether to perform this surgical procedure, the E&M service is separately reportable with modifier 57. Other preoperative E&M services on the same date of service as a major surgical procedure are included in the global payment for the procedure and are not separately reportable.
REIMBURSEMENT GUIDELINES Preventive Medicine Service and Problem Oriented E/M Service
A Preventive Medicine CPT or HCPCS code and a Problem-Oriented E/M CPT code may both be submitted for the same patient by the Same Specialty Physician, Hospital, Ambulatory Surgical Center or Other Health Care Professional on the same date of service. If the E/M code represents a significant, separately identifiable service and is submitted with modifier 25 appended, Oxford will reimburse the Preventive Medicine code plus 50% of the Problem-Oriented E/M code. Oxford will not reimburse a Problem-Oriented E/M code that does not represent a significant, separately identifiable service and that is not submitted with modifier 25 appended.
Preventive Medicine Service and Other E/M Service
A Preventive Medicine CPT or HCPCS code and Other E/M CPT or HCPCS codes may both be submitted for the same patient by the Same Specialty Physician, Hospital, Ambulatory Surgical Center or Other Health Care Professional on the same date of service. However, Oxford will only reimburse the Preventive Medicine CPT or HCPCS code.
Screening Services
The comprehensive nature of a Preventive Medicine code reflects an age and gender appropriate examination. When a screening code is billed with a Preventive Medicine code on the same date of service by the Same Specialty Physician, Hospital, Ambulatory Surgical Center or Other Health Care Professional, only the Preventive Medicine code is reimbursed.
Prolonged Services
Prolonged services codes represent add-on services that are reimbursed when reported in addition to an appropriate primary service. Preventive medicine services are not designated as appropriate primary codes for the Prolonged services codes. When Prolonged service add-on codes are billed with a Preventive Medicine code on the same date of service by the Same Specialty Physician, Hospital, Ambulatory Surgical Center or Other Health Care Professional, only the Preventive Medicine code is reimbursed.
Counseling Services
Preventive Medicine Services include counseling. When counseling service codes are billed with a Preventive Medicine code on the same date of service by the Same Specialty Physician, Hospital, Ambulatory Surgical Center or Other Health Care Professional, only the Preventive Medicine code is reimbursed.
Medical Nutrition Therapy Services
According to CPT, for Medical Nutrition Therapy assessment and/or intervention performed by a physician, report Evaluation and Management or Preventive Medicine service codes. When Medical Nutrition Therapy codes are billed with a Preventive Medicine code on the same date of service by the Same Specialty Physician, Hospital, Ambulatory Surgical Center or Other Health Care Professional, only the Preventive Medicine code is reimbursed.
Visual Function and Visual Acuity Screening
The comprehensive nature of a Preventive Medicine code reflects an age and gender appropriate examination. When Visual Function Screening or Visual Acuity Screening is billed with a Preventive Medicine code on the same date of service by the Same Specialty Physician, Hospital, Ambulatory Surgical Center or Other Health Care Professional, only the Preventive Medicine code is reimbursed.
Preventive Medicine Service Provided at the Time of Covered Screening Service
A preventive medicine exam, as described by CPT-4 codes (99384 – 99397), includes a comprehensive age and gender appropriate history, examination, counseling/anticipatory guidance/risk-factor reduction interventions, and the ordering of appropriate immunization(s) and laboratory/diagnostic procedures. Sometimes these other elements are performed during the same visit as the Medicare covered services, particularly G0101 and Q0091. The following pie chart illustrates this circumstance.
The following are examples of screening services that are ineligible for separate reimbursement when reported with preventive medicine services, annual GYN examinations and/or problem oriented E/M services:
• G0101 is included in the reimbursement for:
o problem oriented E/M services (99201-99215)*
o preventive medicine services (99381-99397)
o annual GYN examinations (S0610, S0612, or S0613)
• G0102 is included in the reimbursement for:
• Q0091 is included in the reimbursement for:
o preventive medical services (99381-99397)*
o annual GYN examinations (S0610, S0612, or S0613)*
• S0610, S0612, and/or S0613 is included in the reimbursement for:
Coding for a Problem Focused Visit Within an EPSDT Visit
EPSDT codes
99381–99385 or 99391-99395 The components of the EPSDT visit must be provided and documented
PLUS Evaluation and Management (E&M)codes
99203–99215 The presenting problem must be of moderate to high severity.
PLUS Modifier 25*
Documentation must support the use of modifier 25.
PLUS ICD-9 Diagnosis codes
V20.2 or V70.0 must be the primary diagnosis diagnosis code for the visit. Add the diagnosis codes for the presenting problem focused evaluation.
Effective 4/1/2014 EPSDT/Well Child visits are all-inclusive visits. The payment for the EPSDT is intended to cover all elements outlined in the AHCCCS EPSDT Periodicity Schedule (AMPM Exhibilt 430-1). Refer to AMPM Policy 430 for exceptions to the all-inclusive visit global payment rate. Claims must be submitted on CMS 1500 form. Providers must bill for preventative EPSDT services using the preventative service, office or other outpatient services and preventative medicine CPT codes (99381 – 99385, 99391 – 99395) with an EP modifier. EPSDT visits are paid at a global rate for the services specified in AMPM Policy 430. No additional reimbursement is allowed.
Providers must use an EP modifier to designate all services related to the EPSDT well child check-up, including routine vision and hearing screenings.
Providers must be registered as Vaccines for Children (VFC) Program providers and VFC vaccines must be used. Under the federal VFC program, providers are paid a capped fee for administration of vaccines to recipients 18 years old and younger. For VFC claims incurred prior to 1/1/2013, Providers must bill the appropriate CPT code for the immunization with the “SL” (State supplied vaccine) modifier that identifies the immunization as part of the VFC program.
Providers must not use the immunization administration CPT codes 90471, 90472, 90473, and 90474 when billing under the VFC program. Because the vaccine is made available to providers free of charge, providers must not bill for the vaccine itself.
For VFC services incurred on/after 1/1/2013, Section 1202 of the Patient Protection and Affordable Care Act (ACA) requires AHCCCS to modify how providers submit claims for vaccine administration services.
EPSDT CPT codes well-child visits STAGE (Age) NEW PATIENT CPT CODE ESTABLISHED PATIENT CPT CODE
INFANCY (Prenatal – 9 months) 99381 99391 EARLY CHILDHOOD (12 months – 4 years) 99382 99392 MIDDLE CHILDHOOD (5 years – 10 years) 99383 99393 ADOLESCENCE STAGE 1 (11 years – 17 years) 99384 99394 ADOLESCENCE STAGE 2 (18 years – 21 years) 99385 99395 EPSDT CPT codes for sensory screening SERVICE CPT CODE VISION 99173 HEARING (Audio) 92551 HEARING (Pure tone-air only) 92552 Adult annual preventive care visits
New patient
CPT Code 99385: Initial Preventive Medicine New Patient age 18-39 years CPT Code 99386: Initial Preventive Medicine New Patient age 40-64 years CPT Code 99387: Initial Preventive Medicine New Patient age 65 years & older
Established patient
CPT Code 99395: Periodic Preventive Medicine Established Patient 18-39 years CPT Code 99396: Periodic Preventive Medicine Established Patient 40-64 years CPT Code 99397: Periodic Preventive Medicine Established Patient 65 years & older Adolescent annual preventive care visits
CPT Code 99382: Initial Preventive Medicine New Patient age 1-4 years CPT Code 99383: Initial Preventive Medicine New Patient age 5-11 years CPT Code 99384: Initial Preventive Medicine New Patient age 12-17 years
CPT Code 99392: Periodic Preventive Medicine Established Patient age 1-4 years CPT Code 99393: Periodic Preventive Medicine Established Patient age 5-11 years CPT Code 99394: Periodic Preventive Medicine Established Patient age 12-17 years
Preventive Visit Codes Although preventive visit codes will be accepted (99385; 99386; 99387; 99395; 99396; 99397), Medicare does not establish a rate for these codes. Sage will pay 99385 – 99387 at the rate for code 99203. Codes 99395 – 99397 will be paid at the rate for code 99213.
PARTIAL SCREENING and Modifier usage
Different providers may provide segments of the full medical screen. The purpose of this is to increase the access to care for all children and to allow providers reimbursement for those separate screens. When expanded HCY services are accessed through a partial or interperiodic screen, it is the responsibility of the provider completing the partial screening service to have a referral source to refer the child for the remaining components of a full screening service. An unclothed physical and history screen ( CPT codes 99381 52 EP-99385 52EP and 99391 52 EP -9939552EP) includes the first five sections of the age appropriate screening guide including:
• Interval history; • Unclothed physical exam; • Anticipatory guidance; • Laboratory/Immunizations; and • Age appropriate lead screening. Federal regulations require a mandatory blood lead testing by either capillary or venous method at 12 months and 24 months of age. The provider must use the HCY Lead Risk Assessment form.
PARTIAL SCREENING PROCEDURE CODES – UNCLOTHED PHYSICAL & HISTORY (Established Patient) (Provider must complete Sections 1-5 of the HCY Screening Guide)
Procedure Code (Use Age Appropriate Code) Modifier 1 Modifier 2 Fee
99391* 52 EP $20.00 99392* 52 EP $20.00 99393* 52 EP $20.00 99394* 52 EP $20.00 99395* 52 EP $20.00
*Modifier “UC” must be used if child was referred for further care as a result of the screening. DESCRIPTION OF MODIFIERS USED FOR HCY SCREENINGS
* EP – Service provided as part of MO HealthNet early periodic, screening, diagnosis, and treatment (EPSDT). * 52 – Reduced services. Modifier 52 must be used when all the components for the unclothed physical and history procedure codes (99381-99395) have not been met according to CPT. Also used with procedure code 99429 to identify that the components of a partial HCY vision screen have been met. * 59 – Distinct Service. Modifier 59 must be used to identify the components of an HCY screen when only those components related to developmental and mental health are being screened. * UC – EPSDT Referral for Follow-Up Care. The modifier UC must be used when the child is referred on for further care as a result of the screening.
All Preventive CPT CODE AND description Adult preventive care visits New patient CPT Code 99385: Initial Preventive Medicine New Patient age 18-39 years CPT Code 99386: Initial Preventive Medicine New Patient age 40-64 years CPT Code 99387: Initial Preventive Medicine New Patient age 65 years & older
Established patient CPT Code 99395: Periodic Preventive Medicine Established Patient 18-39 years CPT Code 99396: Periodic Preventive Medicine Established Patient 40-64 years CPT Code 99397: Periodic Preventive Medicine Established Patient 65 years & older
Adult annual preventive care visits New patient CPT Code 99385: Initial Preventive Medicine New Patient age 18-39 years CPT Code 99386: Initial Preventive Medicine New Patient age 40-64 years CPT Code 99387: Initial Preventive Medicine New Patient age 65 years & older
Established patient CPT Code 99395: Periodic Preventive Medicine Established Patient 18-39 years CPT Code 99396: Periodic Preventive Medicine Established Patient 40-64 years CPT Code 99397: Periodic Preventive Medicine Established Patient 65 years & older Adolescent annual preventive care visits
New patient CPT Code 99382: Initial Preventive Medicine New Patient age 1-4 years CPT Code 99383: Initial Preventive Medicine New Patient age 5-11 years CPT Code 99384: Initial Preventive Medicine New Patient age 12-17 years
DIAGNOSIS CODES FOR FULL, PARTIAL OR INTERPERIODIC SCREENS
Providers must use V20.2 as the primary diagnosis on claims for HCY screening services. There are two exceptions. CPT codes 99381EP and 99391EP must be billed with diagnosis code V20.2, V20.31 or V20.32. CPT codes 99385 and 99395 must be billed with diagnosis code V25.01-V25.9, V70.0 or V72.31.
FULL SCREENING PROCEDURE CODES (New Patient) Procedure Code (Use Age Appropriate Code)
Modifier 2 Fee 99381* EP $60.00 99382* EP $60.00 99383* EP $60.00 99384* EP $60.00 99385* EP $60.00
PARTIAL SCREENING
Different providers may provide segments of the full medical screen. The purpose of this is to increase the access to care for all children and to allow providers reimbursement for those separate screens. When expanded HCY services are accessed through a partial or interperiodic screen, it is the responsibility of the provider completing the partial screening service to have a referral source to refer the child for the remaining components of a full screening service.
An unclothed physical and history screen (CPT codes 9938152EP-9938552EP and 9939152EP-9939552EP) includes the first five sections of the age appropriate screening guide including:
• Interval history;
• Unclothed physical exam;
• Anticipatory guidance;
• Laboratory/Immunizations; and
• Age appropriate lead screening. Federal regulations require a mandatory blood lead testing by either capillary or venous method at 12 months and
Medical Billing Update
- Tips to minimize the claim denial – Dental claim
- Vision and Development screen billing overview
- patient seeing the provider on same group
- Medical billing interview question
- Healthcare clearinghouse review
Recent Posts
- Denial – Covered by capitation , Modifier inconsistent – Action
- CPT code 10040, 10060, 10061 – Incision And Drainage Of Abscess
- CPT Code 0007U, 0008U, 0009U – Drug Test(S), Presumptive
- CPT code 99499 – Billing and coding guidelines
- CPT 92521,92522,92523,92524 – Speech language pathology
- Medical billing basics
All the contents and articles are based on our search and taken from various resources and our knowledge in Medical billing. All the information are educational purpose only and we are not guarantee of accuracy of information. Before implement anything please do your own research. If you feel some of our contents are misused please mail us at medicalbilling4u at gmail dot com. We will response ASAP.
Meta releases Llama 3, claims it’s among the best open models available
Meta has released the latest entry in its Llama series of open generative AI models: Llama 3. Or, more accurately, the company has debuted two models in its new Llama 3 family, with the rest to come at an unspecified future date.
Meta describes the new models — Llama 3 8B, which contains 8 billion parameters, and Llama 3 70B, which contains 70 billion parameters — as a “major leap” compared to the previous-gen Llama models, Llama 2 8B and Llama 2 70B, performance-wise. (Parameters essentially define the skill of an AI model on a problem, like analyzing and generating text; higher-parameter-count models are, generally speaking, more capable than lower-parameter-count models.) In fact, Meta says that, for their respective parameter counts, Llama 3 8B and Llama 3 70B — trained on two custom-built 24,000 GPU clusters — are are among the best-performing generative AI models available today.
That’s quite a claim to make. So how is Meta supporting it? Well, the company points to the Llama 3 models’ scores on popular AI benchmarks like MMLU (which attempts to measure knowledge), ARC (which attempts to measure skill acquisition) and DROP (which tests a model’s reasoning over chunks of text). As we’ve written about before , the usefulness — and validity — of these benchmarks is up for debate. But for better or worse, they remain one of the few standardized ways by which AI players like Meta evaluate their models.
Llama 3 8B bests other open models such as Mistral’s Mistral 7B and Google’s Gemma 7B , both of which contain 7 billion parameters, on at least nine benchmarks: MMLU, ARC, DROP, GPQA (a set of biology-, physics- and chemistry-related questions), HumanEval (a code generation test), GSM-8K (math word problems), MATH (another mathematics benchmark), AGIEval (a problem-solving test set) and BIG-Bench Hard (a commonsense reasoning evaluation).
Now, Mistral 7B and Gemma 7B aren’t exactly on the bleeding edge (Mistral 7B was released last September), and in a few of the benchmarks Meta cites, Llama 3 8B scores only a few percentage points higher than either. But Meta also makes the claim that the larger-parameter-count Llama 3 model, Llama 3 70B, is competitive with flagship generative AI models, including Gemini 1.5 Pro, the latest in Google’s Gemini series.
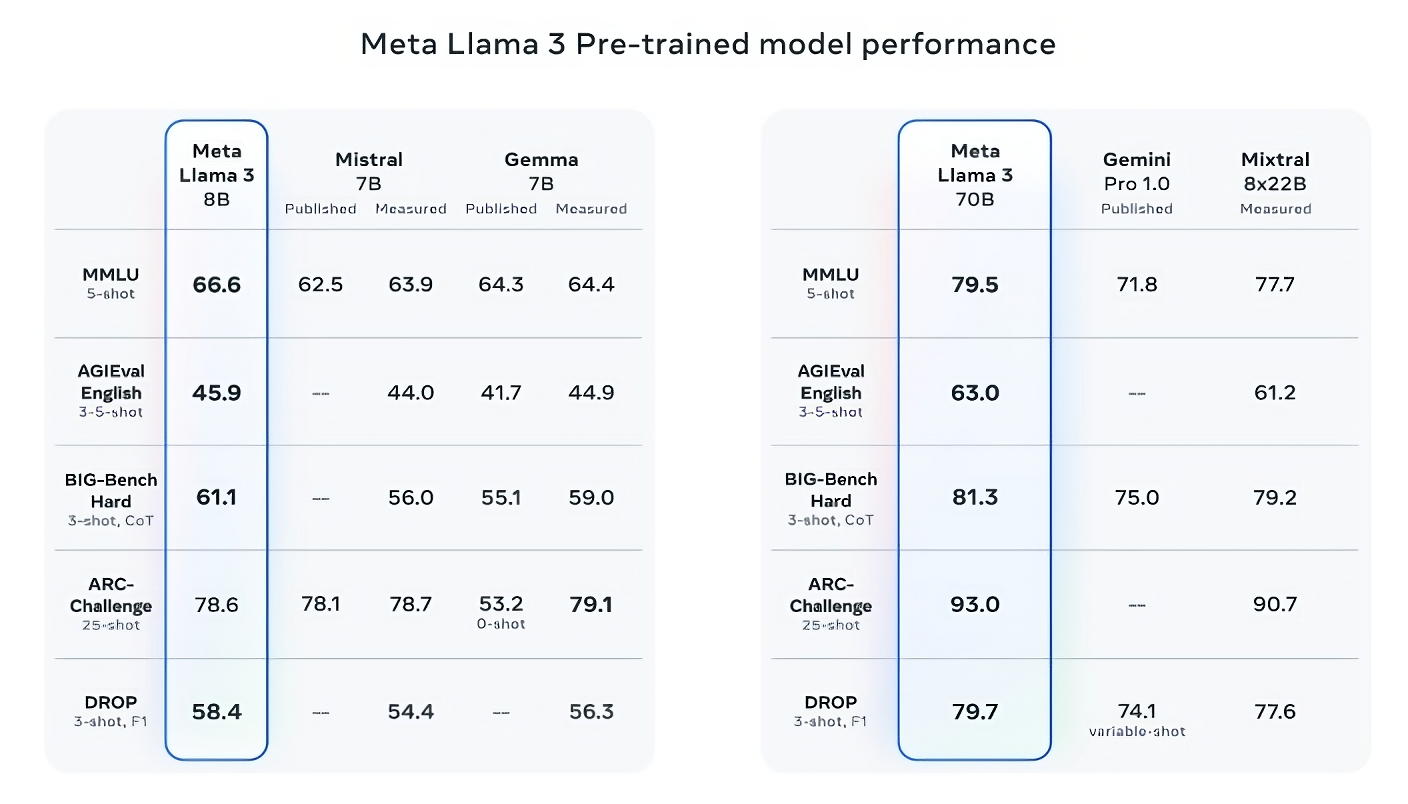
Image Credits: Meta
Llama 3 70B beats Gemini 1.5 Pro on MMLU, HumanEval and GSM-8K, and — while it doesn’t rival Anthropic’s most performant model, Claude 3 Opus — Llama 3 70B scores better than the second-weakest model in the Claude 3 series, Claude 3 Sonnet, on five benchmarks (MMLU, GPQA, HumanEval, GSM-8K and MATH).
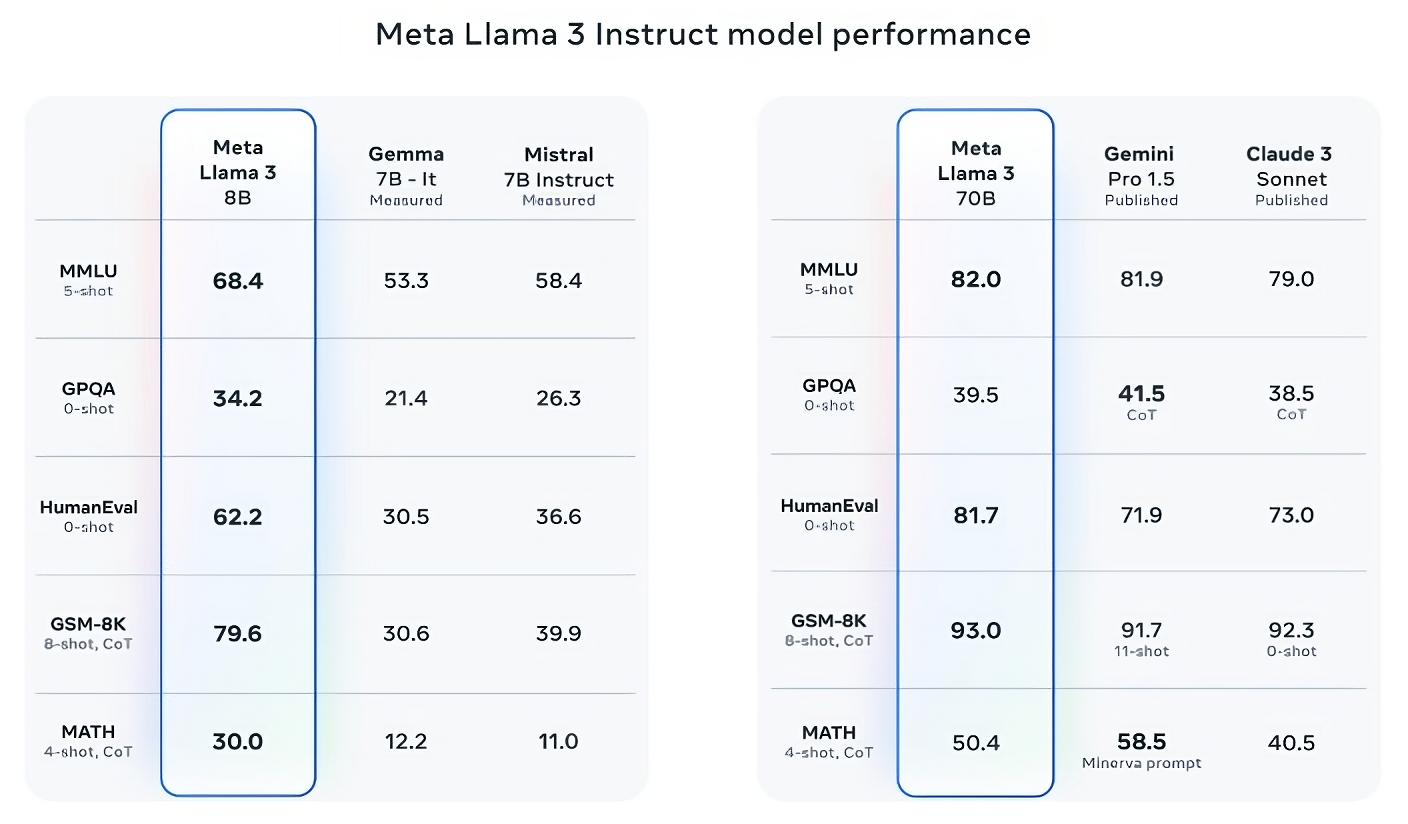
For what it’s worth, Meta also developed its own test set covering use cases ranging from coding and creative writing to reasoning to summarization, and — surprise! — Llama 3 70B came out on top against Mistral’s Mistral Medium model, OpenAI’s GPT-3.5 and Claude Sonnet. Meta says that it gated its modeling teams from accessing the set to maintain objectivity, but obviously — given that Meta itself devised the test — the results have to be taken with a grain of salt.

More qualitatively, Meta says that users of the new Llama models should expect more “steerability,” a lower likelihood to refuse to answer questions, and higher accuracy on trivia questions, questions pertaining to history and STEM fields such as engineering and science and general coding recommendations. That’s in part thanks to a much larger dataset: a collection of 15 trillion tokens, or a mind-boggling ~750,000,000,000 words — seven times the size of the Llama 2 training set. (In the AI field, “tokens” refers to subdivided bits of raw data, like the syllables “fan,” “tas” and “tic” in the word “fantastic.”)
Where did this data come from? Good question. Meta wouldn’t say, revealing only that it drew from “publicly available sources,” included four times more code than in the Llama 2 training dataset and that 5% of that set has non-English data (in ~30 languages) to improve performance on languages other than English. Meta also said it used synthetic data — i.e. AI-generated data — to create longer documents for the Llama 3 models to train on, a somewhat controversial approach due to the potential performance drawbacks.
“While the models we’re releasing today are only fine tuned for English outputs, the increased data diversity helps the models better recognize nuances and patterns, and perform strongly across a variety of tasks,” Meta writes in a blog post shared with TechCrunch.
Many generative AI vendors see training data as a competitive advantage and thus keep it and info pertaining to it close to the chest. But training data details are also a potential source of IP-related lawsuits, another disincentive to reveal much. Recent reporting revealed that Meta, in its quest to maintain pace with AI rivals, at one point used copyrighted e-books for AI training despite the company’s own lawyers’ warnings; Meta and OpenAI are the subject of an ongoing lawsuit brought by authors including comedian Sarah Silverman over the vendors’ alleged unauthorized use of copyrighted data for training.
So what about toxicity and bias, two other common problems with generative AI models ( including Llama 2 )? Does Llama 3 improve in those areas? Yes, claims Meta.
Meta says that it developed new data-filtering pipelines to boost the quality of its model training data, and that it has updated its pair of generative AI safety suites, Llama Guard and CybersecEval, to attempt to prevent the misuse of and unwanted text generations from Llama 3 models and others. The company’s also releasing a new tool, Code Shield, designed to detect code from generative AI models that might introduce security vulnerabilities.
Filtering isn’t foolproof, though — and tools like Llama Guard, CyberSecEval and Code Shield only go so far. (See: Llama 2’s tendency to make up answers to questions and leak private health and financial information .) We’ll have to wait and see how the Llama 3 models perform in the wild, inclusive of testing from academics on alternative benchmarks.
Meta says that the Llama 3 models — which are available for download now, and powering Meta’s Meta AI assistant on Facebook, Instagram, WhatsApp, Messenger and the web — will soon be hosted in managed form across a wide range of cloud platforms including AWS, Databricks, Google Cloud, Hugging Face, Kaggle, IBM’s WatsonX, Microsoft Azure, Nvidia’s NIM and Snowflake. In the future, versions of the models optimized for hardware from AMD, AWS, Dell, Intel, Nvidia and Qualcomm will also be made available.
The Llama 3 models might be widely available. But you’ll notice that we’re using “open” to describe them as opposed to “open source.” That’s because, despite Meta’s claims , its Llama family of models aren’t as no-strings-attached as it’d have people believe. Yes, they’re available for both research and commercial applications. However, Meta forbids developers from using Llama models to train other generative models, while app developers with more than 700 million monthly users must request a special license from Meta that the company will — or won’t — grant based on its discretion.
More capable Llama models are on the horizon.
Meta says that it’s currently training Llama 3 models over 400 billion parameters in size — models with the ability to “converse in multiple languages,” take more data in and understand images and other modalities as well as text, which would bring the Llama 3 series in line with open releases like Hugging Face’s Idefics2 .

“Our goal in the near future is to make Llama 3 multilingual and multimodal, have longer context and continue to improve overall performance across core [large language model] capabilities such as reasoning and coding,” Meta writes in a blog post. “There’s a lot more to come.”

It’s not hard, once you get the hang of it, but the differences from E/M coding can be confusing.
TIMOTHY OWOLABI, MD, CPC, AND ISAC SIMPSON, DO
Fam Pract Manag. 2012;19(4):12-16
Dr. Owolabi is a board-certified family physician and certified professional coder employed by Summit Physician Services, a multispecialty, hospital-owned group practice in Chambersburg, Pa. In addition to managing a busy patient panel, Dr. Owolabi independently offers coding consulting services and speaks and writes on coding topics. Dr. Simpson is a family medicine resident at Phoenix Baptist Hospital Family Medicine Residency in Phoenix, Ariz. Author disclosure: no relevant financial affiliations disclosed.
This is a corrected version of the article previously published.

In our experience, family physicians vary widely in their understanding of preventive care coding. Questions we’ve heard range from “What ICD-9 codes are appropriate with preventive care visits?” all the way down to “Preventive codes? What are preventive codes? I only use evaluation and management [E/M] codes.” No matter what your level of comfort (or discomfort) with coding preventive visits, we hope to offer information you’ll find useful. We will define the documentation components necessary to code preventive visits for patients 18 to 64 years old, review the appropriate ICD-9 and CPT codes and how to properly pair them, and discuss the proper use of modifier 25. We won’t cover the Medicare guidelines for preventive visits or how to code pediatric preventive visits. Coding resources for these visits are listed below.
Components of a preventive visit
Preventive visits, like many procedural services, are bundled services. Unlike documenting problem-oriented E/M office visits (99201–99215), which involves complicated coding guidelines, documenting preventive visits is more straightforward. The following components are needed:
A comprehensive history and physical exam findings;
A description of the status of chronic, stable problems that are not “significant enough to require additional work,” according to CPT;
Notes concerning the management of minor problems that do not require additional work;
Notes concerning age-appropriate counseling, screening labs, and tests;
Orders for vaccines appropriate for age and risk factors.
According to CPT, the comprehensive history that must be obtained as part of a preventive visit has no chief complaint or present illness as its focus. Rather, it requires a “comprehensive system review and comprehensive or interval past, family, and social history as well as a comprehensive assessment/history of pertinent risk factors.” The preventive comprehensive exam differs from a problem-oriented comprehensive exam because its components are based on age and risk factors rather than a presenting problem.
Some have attempted to use modifier 52 to denote reduced services when less than a comprehensive history and exam are performed during a preventive visit. This is inappropriate because modifier 52 applies to procedural services only. Preventive visits that do not satisfy the minimum requirements may be billed with the appropriate E/M office visit code.
When submitting a preventive visit CPT code, it is not appropriate to submit problem-oriented ICD-9 codes. Linking problem-oriented ICD-9 codes with preventive CPT codes may delay payment or result in a denied claim. See “ Acceptable codes for preventive care visits ” for the appropriate ICD-9 codes and the HCPCS and CPT codes with which to pair them.
Coverage of preventive visits varies by insurer, so it is important to be aware of the patient’s health plan. Most plans limit the frequency of the preventive visit to once a year, and not all tests are covered. Fecal occult blood tests, audiometry, Pap smear collection, and vaccines and their administration should be billed separately. Visual acuity testing is not separately reimbursed. Without a new or chronic-disease diagnosis, all labs and other tests ordered during a preventive visit are for screening purposes, and an ICD-9 code for screening should be assigned on the order form and claim.
Another service that has a preventive purpose is the preoperative clearance. Review of the details of this encounter is beyond the scope of this discussion, but it is worth mentioning that many private payers cover the preoperative clearance when billed by primary care physicians using consultation E/M codes (99241-99255).
ACCEPTABLE CODES FOR PREVENTIVE CARE VISITS
Preventive visits and the role of counseling.
Preventive visit codes 99381-99397 include “counseling/anticipatory guidance/risk factor reduction interventions,” according to CPT. However, when such counseling is provided as part of a separate problem-oriented encounter, it may be billed using preventive medicine codes 99401-99409. For example, if you provide significant counseling on smoking cessation during a visit for an ankle sprain, you could bill for the counseling in addition to submitting an E/M office visit code for the problem-oriented service. A synopsis of the counseling should be included in your documentation, and ICD-9 codes for preventive counseling should be paired with your CPT codes (see “ Acceptable codes for preventive counseling services ”). Such a visit requires the use of modifier 25.
ACCEPTABLE CODES FOR PREVENTIVE COUNSELING SERVICES
Modifier 25.
When providing a preventive visit with a problem-oriented E/M service or procedural service on the same day, including modifier 25 in your coding may enable you to be paid for both services. CPT says modifier 25 is appropriate when there is a “significant, separately identifiable evaluation and management service by the same physician on the same day.” Stated another way, if the second service requires enough additional work that it could stand on its own as an office visit, use modifier 25. Modifier 25 should usually be attached to the problem-oriented E/M code. However, if the second service is a procedure, such as removal of a skin lesion performed in conjunction with a preventive visit, the modifier should be attached to the preventive visit code because it is the E/M service.
Having a separate note for the second service can greatly decrease the likelihood of having it inappropriately bundled or denied. Note that no one item of documentation can count toward both services. A problem-oriented E/M service that requires a considerable amount of work and pertinent documentation may absorb so many of the elements that would otherwise count toward the preventive service that you don’t have a comprehensive history and exam for the preventive service. This is one reason some doctors provide two visits in these situations.
Bundling is more likely if the separate service can be considered age-appropriate, such as initiating treatment for acne. However, if a separate E/M note can be written for the problem, the CPT description of modifier 25 and the exclusions listed for the preventive visit CPT codes indicate that the separate service should not be bundled. See “ Appropriate use of modifier 25 during a preventive visit ” for examples of complaints that under some circumstances would be handled as part of a preventive visit, but under different circumstances may require additional work that should be billed separately using modifier 25.
Unfortunately, not all carriers pay for services billed with modifier 25. For example, Aetna did not reimburse at all for modifier 25 until 2006, when it changed its policy as part of a class action settlement with multiple state medical societies. The circumstances in which its use is permitted and the amount of payment for the separate service vary. The lack of consensus on the use of modifier 25 for preventive services places the onus on providers to learn the requirements of each of their payers.
APPROPRIATE USE OF MODIFIER 25 DURING A PREVENTIVE VISIT
Preventive care and productivity.
Discussing the cost-effectiveness of preventive visits for the practice is tricky because of the number of variables to consider. Time spent per preventive visit is a key confounding variable. Others include fee schedule variations between payers, payer mix, productivity variations between physicians, which preventive service is being considered (for patients in the 18–39 age group vs. those in the 40–64 age group or new vs. established), and accuracy of coding, to mention a few.
While the numerous variables make broad generalizations about the immediate cost-effectiveness of preventive visits extremely difficult, careful analysis may lead some practices to conclude that preventive care is beneficial not only for the patient but for the practice as well. As an example, we averaged payment for two visit types from nine actual payers. The visits we considered were a 40-year-old established-patient preventive visit (CPT 99396), minus immunizations and other separate charges, and a level-4, established-patient, problem-oriented visit (CPT 99214). We found the average payment for the preventive visit to be 25 percent higher than for the problem-oriented visit. That is, the preventive visit produces more revenue per unit of time unless the preventive visit takes at least 25 percent longer. Of course, if a preventive visit requires considerably more time than a comparable level-3 or level-4 E/M visit, replacing preventive visits with a larger number of problem-oriented visits could result in more reimbursement overall, at least in theory.
Role of preventive services in our health care system
Some researchers estimate that 75 percent of all health care costs are due directly to preventable chronic conditions, yet as recently as 2004, only 1 percent of money spent on health care in the United States was devoted to prevention. 1 , 2 We don’t wish to spark a debate on whether preventive services directly reduce health care costs, but we speculate that preventive care has the potential to play a more valuable role in our health care system than it does currently. The Centers for Medicare & Medicaid Services did not cover preventive care visits until the institution of the “Welcome to Medicare” visit in 2005. In contrast, many private payers have covered preventive visits for some time. Perhaps this is because they have long recognized that healthy lifestyle choices and routine health surveillance mitigate the risk of chronic disease.
PREVENTIVE VISIT ALGORITHM: PATIENTS AGES 18–64*
Regardless of insurance coverage, patients should at least be offered preventive services even if they must pay out of pocket for them. The “ Preventive visit algorithm ” illustrates how one might approach a preventive visit for a patient in the 18 to 64 age range (except for recommended pregnancy-related services). This schematic is not intended to reflect all the anticipatory guidance or all of the screening that you might recommend for a given patient, but rather includes suggestions based on the strongest evidence-based recommendations from the Centers for Disease Control and Prevention and the U.S. Preventive Services Task Force.
ADDITIONAL RESOURCES FOR CODING PREVENTIVE CARE
Coding for Pediatric Preventive Care 2012 . American Academy of Pediatrics.
What You Need to Know About the Medicare Preventive Services Expansion . FPM . Jan/Feb 2011.
Making Sense of Preventive Medicine Coding . FPM . Apr 2004.
Medicare Preventive Services: Quick Reference . Centers for Medicare & Medicaid Services.
Center for Medicare & Medicaid Services National Health Expenditures and Selected Economic Indicators, Levels and Average Annual Percent Change: Selected Calendar Years 1990–2013 Washington, DC: Center for Medicare & Medicaid Services, Office of the Actuary; 2004.
Institute of Medicine The Future of the Public’s Health in the 21st Century. Washington, DC: National Academy Press; 2002.
Continue Reading

More in FPM
Copyright © 2012 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

IMAGES
VIDEO
COMMENTS
Step 1: Total time. Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if ...
The American Medical Association (AMA) has established new coding and documentation guidelines for office visit/outpatient evaluation and management (E/M) services, effective Jan. 1, 2021. The ...
The 2021 E/M office visit coding changes allow physicians to code visits based solely on total time, which is defined as the entire time you spent caring for the patient on the date of the visit.
types of factors, the E/M visit is more complex. In this example, you may bill G2211. G2211 and Modifier 25 . G2211 may not be reported without reporting an associated O/O E/M visit. G2211 isn't payable when the associated O/O E/M visit is reported with modifier 25. You can add modifier 25 to an E/M CPT code to show the E/M service is ...
CPT ® code 99417 is parsed into 15-minute increments and may be used only when the total time on the date of the encounter exceeds the minimal time for the highest-level E/M visit by 15 minutes. For example, a provider spends a total time of 83 minutes with a new patient. The time limits for a new outpatient visit E/M visit 99205 is 60 -74 ...
Short description: 15-29 minute office visit for new patient evaluation and management. CPT Code 99203. Long description of CPT 99203: Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 30-44 minutes of total time is ...
Effective Jan. 1, 2024, the Centers for Medicare & Medicaid Services implemented a new HCPCS code G2211, an evaluation and management office visit add-on code representing complex services. Access the fact sheet for the full descriptor, code clues and an ophthalmic case study.
Download PDFs of the issue brief and other resources—the AMA's telehealth quick guide outlines policy, CPT coding and payment considerations to keep in mind during COVID-19. ... An in-person visit will not be required for a patient to be eligible for behavioral health services via telehealth through December 31, 2024.
1.4. CPT Code 99205. Lay-term: CPT code 99205 is used when a healthcare provider performs an office visit for a new patient that requires a medically appropriate history and/or examination and a high level of medical decision making. The total time spent on the encounter must be 60 minutes or more. Long description: Office or other outpatient ...
A: To bill 99441-99443 and an evaluation and management (E/M) service such as 99213, you must follow CPT® guidelines, which state, "If the telephone service ends with a decision to see the patient within 24 hours or next available urgent visit appointment, the code is not reported; rather the encounter is considered part of the preservice ...
January 4, 2019. Current Procedural Terminology (CPT) codes 99446-99449 were created in 2014 to capture the time spent by a consultant who is not in direct contact with the patient at the time of service. An interprofessional telephone/internet consultation (ITC) is defined as an assessment and management service in which a patient's treating ...
Eligible services may be found on the Medicare Telehealth Services list. Medicare allows audio-only telehealth services for office visit E/M services (CPT codes 99202-99215) for the treatment of ...
Although, "there are some notable differences in this area when it pertains to CPT® versus CMS," Jimenez forewarned. "One of the biggest changes, I think, in the 2023 changes was the elimination of observation codes," Jimenez said. Effective Jan. 1, 2023, hospital observation codes 99217-99220 and 99224-99226 are deleted.
Annual Wellness Visit (AWV) Visit to develop or update a personalized prevention plan and perform a health risk assessment. Covered once every 12 months. Patients pay nothing (if provider accepts assignment) Routine Physical Exam. Exam performed without relationship to treatment or diagnosis of a specific illness, symptom, complaint, or injury.
After the eighth visit, the patient changes insurance carriers. The eight visits prior to the insurance change are separately reportable to the initial payer. To code this scenario correctly, the physician reports 59426 (one unit). If only one to three antepartum visits were provided, report the appropriate E/M codes, according to CPT® guidelines.
Page 1 of 6. MLN901705 February 2024. We pay for specific Medicare Part B services that a physician or practitioner provides via 2-way, interactive technology (or telehealth). Telehealth substitutes for an in-person visit, and generally involves 2-way, interactive technology that permits communication between the practitioner and patient.
The E/M codes specific to domiciliary, rest home (e.g., boarding home), or custodial care (99324-99238, 99334-99337, 99339, and 99340) have been deleted, and the above codes should also be used in ...
Coding for a Problem Focused Visit Within an EPSDT Visit. EPSDT codes. 99381-99385 or 99391-99395 The components of the EPSDT visit must be provided and documented. PLUS Evaluation and Management (E&M)codes. 99203-99215 The presenting problem must be of moderate to high severity.
The preventive medicineservices codes for new patients are 99381 (under 1 year old), 99382 (1 through 4), 99383 (5 through 11), 99384 (12 through 17), and 99385 (18 through 39). The office-visit codes are 99201 through 99205. Note that the sick diagnosis code goes only on the office visit, and the well-care diagnosis code, V20.2, goes only on ...
EXAMPLES. Let's look at some examples of when it would be appropriate to bill for a problem-oriented E/M code (CPT 99202-99215) along with a preventive or wellness visit. Patient 1: A 70-year-old ...
A child has a well-child visit EPSDT (99381 - 99461), with a well child diagnosis code (Z-code) in the first position; the sick visit code (99211 - 99215) with the modifier 25 and with the illness diagnosis CPT code in the second position. To bill this way, there must be enough evidence in the medical record documentation to support a stand ...
CPT® Code: Description: 99381: Initial comprehensive preventive medicine evaluation and management, new patient; infant (age younger than 1 year): 99382 early childhood (age 1 through 4 years) 99383 late childhood (age 5 through 11 years) 99384 adolescent (age 12 through 17 years) 99385 18-39 years 99386 40-64 years 99387 65 years and older
For what it's worth, Meta also developed its own test set covering use cases ranging from coding and creative writing to reasoning to summarization, and — surprise! — Llama 3 70B came out on ...
The visits we considered were a 40-year-old established-patient preventive visit (CPT 99396), minus immunizations and other separate charges, and a level-4, established-patient, problem-oriented ...
Whenever you report 99211, the provider should document the reason for the visit, along with any other pertinent details. Also, make sure you have the date of service, the reason for the visit, proof that the nurse performed the service per the physician's order, and the nurse's legible signature. Tip 2: Be Familiar With 99211 Components.