Registered Nurse RN
Registered Nurse, Free Care Plans, Free NCLEX Review, Nurse Salary, and much more. Join the nursing revolution.

Protrusion, Retrusion, and Excursion Anatomy
In this anatomy lesson, I’m going to demonstrate protrusion, retrusion, and excursion , which are special body movement terms in anatomy that refer to forward (anterior), backward (posterior), or side to side movements.
Protrusion in Anatomy
Protrusion refers to the movement of a structure in an anterior (forward) direction. In fact, the word protrude means “projecting something forward.”
I call protrusion the kissing movement because it occurs when you pucker your lips like you’re going to give someone a kiss or stick out your tongue. Moving the mandible (lower jaw) forward is also an example of protrusion.

Retrusion in Anatomy
Retrusion is the opposite of protrusion. It refers to the movement of a structure in a posterior, or backward, direction. Putting your tongue back in your mouth, moving the lips back, or moving the mandible back are all examples of retrusion in anatomy.

Excursion in Anatomy
Finally, we have excursion , which refers to the side-to-side movement of the lower jaw (mandible). If you’ve ever heard of a character named Ernest P. Worrell, then you’ve definitely seen the excursion movement. He’s the character in those movies such as Ernest Goes to Camp, Ernest Goes to Jail, etc. When Ernest saw something nasty, he’d move his jaw back and forth and say, “Ewwww.”

Excursion can occur in either direction, and anatomists use directional terms to specify the type of excursion. When the mandible moves to either the left or right, it’s moving away from the body’s midline, so it’s called lateral excursion . When the mandible moves closer to the midline of the body, it’s called medial excursion .

Protrusion and Retrusion vs Protraction and Retraction
What about protraction and retraction ? Some anatomy textbooks will refer to the forward movement of the mandible, lips, or tongue as protraction (instead of protrusion), and the backward (posterior) movement will be called retraction (instead of retrusion). The terms are sometimes used interchangeably, so use whatever method your anatomy professor suggests (they give you the grade, not me!).
However, some anatomists today use protraction and retraction to refer almost exclusively to the scapulae, as it is a combined movement (protraction is anterolateral, and retraction is posteromedial). In contrast, protrusion and retrusion are more of an anterior/posterior movement. Then again, some anatomists prefer not to use protraction and retraction at all, even when describing shoulder blade movement.
Protrusion, Retrusion, and Excursion in Healthcare
Healthcare professionals use protrusion, retrusion, and excursion when documenting, performing assessments on patients, or treating disorders. For example, in her head-to-toe assessment , Nurse Sarah asked me to stick out my tongue (an example of protrusion), to assess cranial nerve twelve .
In addition, something called a mandibular protrusion test (MPT) is sometimes used by anesthesiologists to predict difficult airways in patients.
Free Quiz and More Anatomy Videos
Take a free protrusion vs retrusion quiz to test your knowledge, or review our protrusion vs retrusion video . In addition, you might want to watch our anatomy and physiology lectures on YouTube, or check our anatomy and physiology notes .
Please Share:
- Click to print (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to share on Pocket (Opens in new window)
- Click to share on Telegram (Opens in new window)
Disclosure and Privacy Policy
Important links, follow us on social media.
- Facebook Nursing
- Instagram Nursing
- TikTok Nurse
- Twitter Nursing
- YouTube Nursing
Copyright Notice
Analysis of sagittal condylar path inclination in consideration of Fischer's angle
Affiliation.
- 1 Department of Removable Prosthodontics, Faculty of Dental Science, Kyushu University, Fukuoka, Japan.
- PMID: 16774510
- DOI: 10.1111/j.1365-2842.2006.01590.x
This study investigated the sagittal condylar path during protrusive and lateral excursions by analysing the actually measured jaw movement data and re-evaluated the setting of the sagittal condylar path inclination in consideration of Fischer's angle. Protrusive and lateral excursions of 10 healthy subjects were measured using a three-dimensional mandibular movement analysing system. Condylar path inclinations at the hinge-axis point and the corresponding external point laterally extending from the condyle were evaluated in the sagittal plane. Fischer's angle was defined as the difference between the sagittal condylar inclinations during protrusive and lateral excursions on the non-working side, by keeping the corresponding horizontal distance from the intercuspal position (ICP) equivalent at the incisal point. Analysis was performed at three different magnitudes of excursions, where the incisal point was located at 1, 3 and 5 mm away from the ICP. There was no significant difference in the sagittal condylar path inclination or the Fischer's angle between two condylar reference points. However, they were significantly different across the three different magnitudes of excursions for both condylar reference points, i.e. sagittal condylar path inclination (P = 0.003 for protrusive excursion, and P < 0.001 for lateral excursion respectively; two-way repeated-measures anova), and Fischer's angle (P = 0.013, two-way repeated-measures anova) became smaller as the incisal point became distant from the ICP. Moreover, 3- and 5-mm eccentric positions were included in the 95% CI where Fischer's angle equals zero and were considered to be clinically acceptable to adjust the sagittal condylar inclination on the semiadjustable articulators.
Publication types
- Research Support, Non-U.S. Gov't
- Dental Articulators
- Dental Occlusion
- Imaging, Three-Dimensional / methods
- Mandibular Condyle / physiology*
- Movement / physiology
- Temporomandibular Joint / physiology*
- Email: [email protected]

- Periobasics A Textbook of Periodontics and Implantology
- Text Book of Basic Sciences for MDS Students
Occlusal adjustment / harmonization in periodontics
Introduction to occlusal trauma.
Occlusal trauma is detrimental to periodontal health. It may act as a cofactor which can increase the rate of progression of an existing periodontal disease. Thus, elimination of occlusal trauma is essential to achieve complete periodontal health. The first and foremost principle for the initial treatment of patients diagnosed with periodontitis with slow, moderate or rapid rate of disease progression in which the etiologic factors are both bacterial plaque and occlusal factors, is to eliminate and control first the plaque and then the occlusal factors, except where delay may unfavorably influence treatment of occlusal abnormalities, or cause discomfort to the patient. The end point of the occlusal therapy should be to achieve stable occlusion with the least interference to plaque control and periodontal maintenance. The following treatment modalities can be used to treat the occlusal abnormalities as a part of periodontal treatment,
- Orthodontic treatment.
- Restorative treatment.
- Occlusal adjustment.
Orthodontic treatment
It is an established fact that there is no significant relationship between malocclusion and severity of the periodontal disease. So, orthodontic treatment should not be considered as a routine treatment for preventing or treating periodontitis. However, there are specific situations where orthodontic treatment is essential to achieve optimal results of periodontal therapy. In the following situations, orthodontic treatment becomes essential to achieve periodontal health,
- Impinging overbite where trauma to gingival tissue is causing gingival recession. In extreme cases, a combination of orthodontic and surgical procedures may be required.
- Lack of lip seal and mouth breather’s gingivitis may indicate the need for orthodontic treatment.
- Up-righting of tipped teeth helps in reducing periodontal pocket depth as well as facilitate restorative treatment and plaque control.
- Presence of anterior cross-bite is an important indication for orthodontic treatment. It is accompanied by an unstable jiggling type of occlusion, which seems to aggravate periodontitis.
- Extensive open bite with contacts only on the last molars often has associated periodontal problems and orthodontic treatment may be beneficial.
- Correction of severely malpositioned teeth improves the long-term prognosis of the dentition.
- Orthodontic intrusion of anterior teeth with advanced periodontal destruction may help in improving their periodontal support.
It must be noted here that, orthodontic treatment should be done only when inflammation in periodontal tissues has subsided following scaling and root planing and the patient is maintaining good oral hygiene. Tooth movement in the presence of gingival inflammation may be detrimental.
It is a procedure by which the resistance of a tooth to the occlusal forces is increased by joining a neighboring tooth or teeth. It is a well-accepted treatment used to control irreversible tooth mobility through mechanical stabilization. It stabilizes the mobile teeth by forming a firm unit, thus minimizing tooth mobility and greatly improving the occlusal function of teeth. It not only ensures the retention of the periodontally compromised teeth, but also positively affects their longevity in the oral cavity. Splinting may be done for short term or long term. The primary objective of splinting is to ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..

Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
Buy with Instamojo
International Users:
Buy with PayPal
Restorative treatment
Restorative treatment is sometimes essential to achieve periodontal health. Food impaction, impinging overbite or various forms of unstable occlusion require restorative treatment. Permanent splints are also a component of restorative treatment. It should be noted here that permanent splinting of teeth should be considered only after other forms of occlusal therapy have been ruled out as being inadequate.
Occlusal adjustments
In order to have a healthy masticatory system, periodontal trauma because of faulty occlusion should be treated. A successful adjustment in the occlusal abnormalities results in occlusal stability. Occlusal adjustment may also eliminate food impaction and gingival impingement in some instances. It should be remembered that because occlusal adjustment involves removal of tooth structure and is an irreversible treatment, it should be carried out only after a definite diagnosis has been made regarding the presence of a traumatic lesion rather than the presence of any occlusal interferences, which may be ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Indications for occlusal adjustment
It must be remembered that occlusal adjustments result in changes in occlusal scheme. It is an irreversible treatment so should only be planned with great care. Even minor mistakes made during the occlusal adjustment may result in worsening of the situation. Following are the indications for occlusal adjustment,
- The presence of parafunctional habits in conjunction with occlusal disharmony.
- Signs of occlusal trauma, excessive occlusal attrition, and/or TMJ dysfunction.
- The presence of multiple restorations on posterior or anterior teeth, which require occlusal adjustment to achieve a harmonious occlusion.
- To eliminate occlusal interferences after the orthodontic treatment is finished.
- Some clinicians also recommend prophylactic occlusal adjustments in the absence of any periodontal or TMJ symptom to prevent future problems.
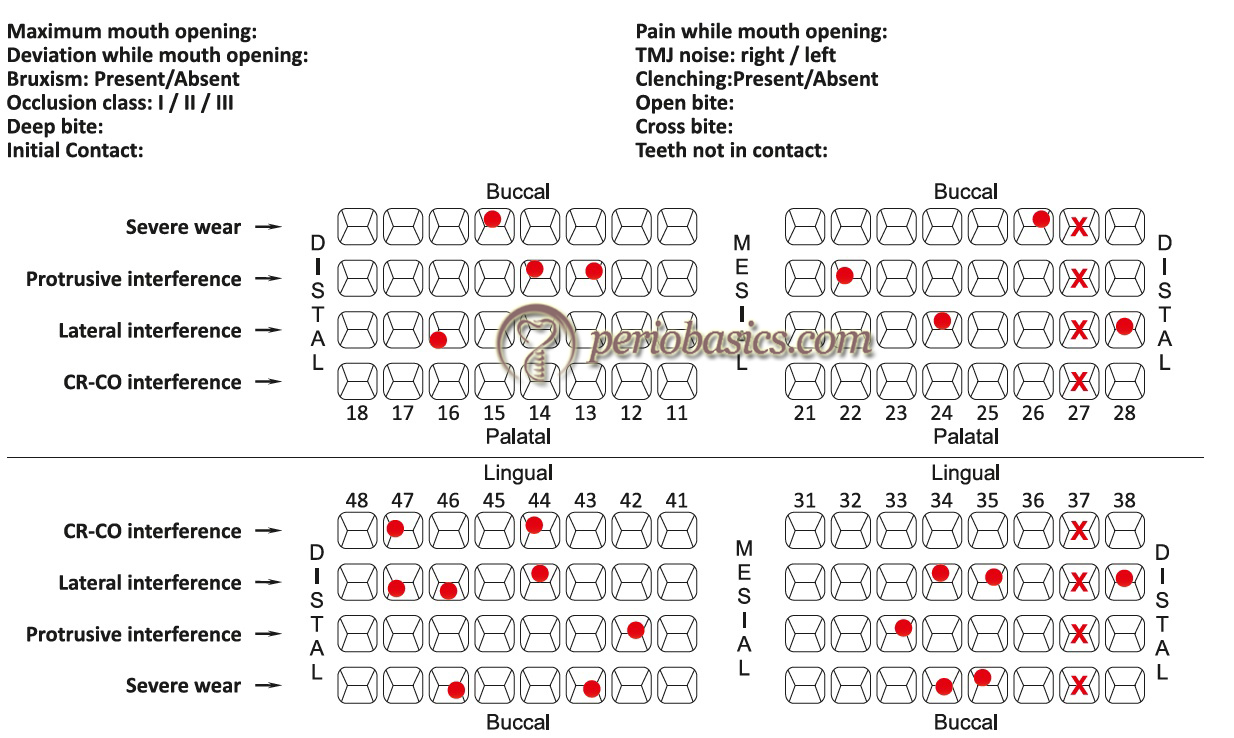
Evaluation of TMJ and occlusion
A precise occlusal history should be recorded before any occlusal examination is done. The details of the history depend on the type of occlusal symptoms and their severity. The patient’s problems and their duration should be recorded in a chronological order. The patients usually cannot relate the occlusal problems with their symptoms. So, appropriate questions should be asked to establish any relation between the patient’s symptoms and occlusal abnormalities. Para-functional habits are the most common cause of occlusal problems. So, the patient should be asked questions about the history of pain in teeth, periodontium or TMJ and associated musculature.
The patient should be asked questions like: “Do you have your teeth in tight contact when you wake up? Do you feel tiredness in the jaws on waking up?” Any positive answer indicates parafunctional habit. The patients usually do not know about night grinding. So, any other person sleeping with the patient should be asked about ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Extra-oral examination
The patient should be made to sit in a semi-recline position with head slightly tipped back. The head should be supported by the headrest. Any facial asymmetry should be noted and the cause of abnormality should be detected. The patient should be asked to open and close the mouth slowly. Any deviation during mouth opening or closing should be noted. The TMJ examination should be done by lateral palpation of the joint and auscultation of the joint should be done (For more detail, “Art of history taking in periodontics” ). The muscles of mastication should be palpated for any tenderness.
Intra-oral examination
The intra-oral examination of the patient should be done to identify any occlusal interference. It must be emphasized here that any single positive sign should not be considered as diagnostic of the occlusal problem, but should be related carefully to other findings. The following steps are followed while recording functional occlusion,
- The static relation between maxillary and mandibular teeth i.e., centric occlusion (CO) position should be determined first.
- Overjet, overbite and freeway space should be determined.
- Any occlusal variation in the occlusion plane, cross-bite, open bite, extrusion etc. should be recorded.
- Wear facets and their distribution should be recorded. It should be remembered that the presence of wear facets is related to patient’s age.
- The presence of wear facets is not always pathognomonic of traumatic occlusion. So, it must be correlated with other findings.
- Tooth/teeth with increased mobility should be identified. Along with increased tooth mobility, increased tooth sensitivity to thermal changes and to percussion should also be checked because these findings can also be due to occlusal trauma.
- Any tooth migration should be recorded. Tooth migration associated with an occlusal abnormality is usually associated with wear facet.
- Tooth migration without wear facets is usually associated with abnormal tongue habits or atypical swallowing habits.
- Radiographic examination of teeth with mobility or migration should be done. Loss of bone support or changes in periodontal ligament space are indicative of trauma from occlusion.
Diagnosis of occlusal interferences
An “occlusal interference” is any tooth contact that inhibits the remaining occluding surfaces from achieving stable and harmonious contacts 15 . Very small interferences up to 15 µm can trigger an untoward response such as tooth pain or mobility 16, 17 . Hence, these interferences must be eliminated to achieve a stable and harmonious occlusion. In a harmonious occlusion without any interference, the occlusal contact time simultaneity, by definition implies that a time of 0 seconds elapses between the first and the last occlusal contact 18 . In other words, we can say that all the occluding surfaces of the mandibular teeth come in contact with the maxillary teeth at the same instant during the mandibular closure.
There are four types of occlusal interferences:
- Non-working.
- Protrusive.
Armamentarium required for diagnosing and correcting occlusal interferences
The armamentarium used to record functional occlusion includes occlusal indicators (described below), cotton rolls, dental mirror, hand mirror, abrasive disks and wheels, cutting and abrasive burs, polishing burs and rubber polishing cones. The findings of the occlusal examination should be recorded on a chart which consists of columns for recording all the significant occlusal parameters.
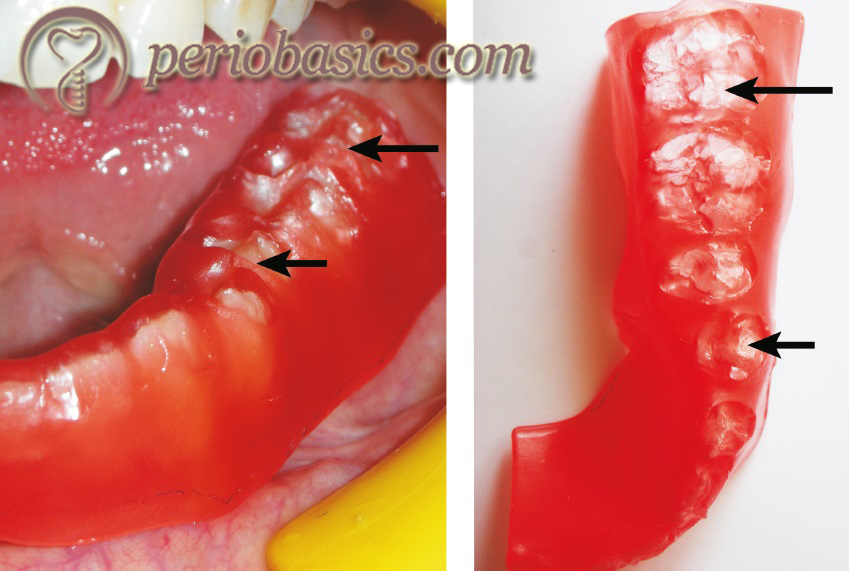
Occlusal indicators are essential components of recording functional occlusion. Occlusal indicators can be divided as qualitative and quantitative indicators. The primary difference between the qualitative and quantitative indicators is that quantitative indicators are capable of recording the tooth contact events.
Qualitative indicators:
- Articulating paper.
- Articulating silk.
- Articulating film.
- Metallic shim stock film.
- High spot indicator.
Quantitative indicators
- T-Scan occlusal analysis system.
- Virtual dental patient.
Qualitative indicators
Articulating papers:.
Articulating papers are the most commonly used occlusal indicators. These consist of a coloring agent and a bonding agent between the two layers of the film. On making tooth contact, the coloring agent is expelled from the film and the bonding agent binds it onto the tooth surface. In areas with heavy contact, the dye spreads peripheral to the actual location of the occlusal contact making a central area that is devoid of the colorant surrounded by a peripheral rim of the dye. The central area of the contact indicates interference and requires correction. Articulating papers are available with different width, thickness and ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..

Articulating silk:
A better way to avoid pseudo-markings is to use an articulating silk. It is made up of micronized color pigment, embedded in a wax-oil emulsion. However, it should be remembered that its marking capability is lost if the staining components are dried. Secondly, contamination of the field by saliva spoils the markings. Hence, it should be used in a dry field and should be stored in a cool and closed environment. It can be used on highly polished surfaces which is its important advantage over articulating papers.
Articulating films:
These are made up of emulsion ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Thin sheets of dark-colored wax are available which can be placed over the occlusal surfaces of the teeth in one arch. The opposing teeth are tapped gently into the wax until it perforates. The perforation represents interfering contacts. These are then marked with pencil and reduced. Waxes are very useful in identifying interferences on sharp line angles.
Metallic shim stock films:
These contain metallic surface on one side and coloring agent on the other side of the film. These are primarily used to accurately mark the contacts on the soft splint.
High spot indicators:
These are also used in the laboratory to check the proximal contacts of crowns, inlays, onlays, telescopic crowns and clasps. These are supplied in the form of a liquid which is applied over the proximal areas where it forms a thickness of 3 µm.
Quantitative indicators:
T-scan occlusal analysis system:.
This is a quantitative indicator which provides contact sequence in 0.01 second increments. The main advantage of this scan is that it identifies time magnitude along with the distribution of the occlusal contacts. The device consists of a piezoelectric foil sensor, a sensor handle and software and hardware to record the data. The foil sensor is placed between the maxillary and mandibular arches and an arch support is placed between the maxillary central incisors of the patient. After the recording button is pressed, the patient is asked to close his/her mouth slowly in the maximum intercuspation position without making any lateral movement.
The sequence of ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Virtual dental patient:
This is a recently introduced technology wherein patient’s dentition casts are scanned and a three-dimensional virtual occlusion is established. The functional movements on this virtual model provide us the quantitative information regarding the occlusal interferences. Similar to the T-scan, the sequence of the occlusal contacts, enables us to eliminate the initial contacts and hence the interferences.
Determination and recording of CR and CO position
The patient should be seated in a reclined and comfortable position in the dental chair with the head properly supported by the headrest. The patient should be asked to take a deep breath and relax the body as much as possible. The patient is asked to look in front and to keep the head stable during manipulation of the lower jaw.
Now, the little finger is placed slightly behind the angle of the jaw and remaining three fingers on the border of the mandible. The thumb is placed over the notch over the sym-physis. The patient is asked to open and close the mouth and the hinge movement of the mandible is felt. A firm pressure is then applied with fingers in an upward direction and with the thumb in a downward and backward direction to position the condyle of the mandible in terminal hinge position. It must be made sure that the manipulation of the mandible in the terminal hinge position should be totally free of any muscular influence. The position is then again verified by repeating the procedure. While the terminal hinge position is verified repeatedly, the patient is asked to gently close the mouth.
Sometimes, the patient complains of pain or discomfort while positioning the mandible in terminal hinge position. It indicates that the condyle meniscus assembly has not been braced against the bone. In such a situation repositioning of the mandible is done by placing cotton rolls between anterior teeth or by placing Hawley’s bite plane.
Once the CR position is well established, an articulating paper (preferably blue) is placed with the help of Miller’s forceps between the occlusal surfaces of teeth on the side making initial contacts. To avoid pseudo markings, thin articulating paper such as GHM occlusion foil (Hanel-GMH Dental GMBH, Nurtingen, Germany) which has 19 μm thickness should be used. The patient is then asked to slowly close the mouth to make contact of maxillary and mandibular teeth. The pair of teeth, making initial ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Registration of lateral and protrusive excursions
The lateral excursive movements are preferably recorded with a different color (such as red) than used for recording CR and CO. A dental tape is placed between the teeth of the patient on the right side and with the help of hand pressure mandible is moved to the right. Teeth with red marks are recorded on the occlusal chart. A similar procedure is then repeated on the left side and markings are recorded on the occlusal chart. A hand mirror can be given to the patient if he/she faces difficulty in performing lateral excursions. The protrusive excursion movements are recorded by gliding the teeth forward from the CO position without any lateral movement.
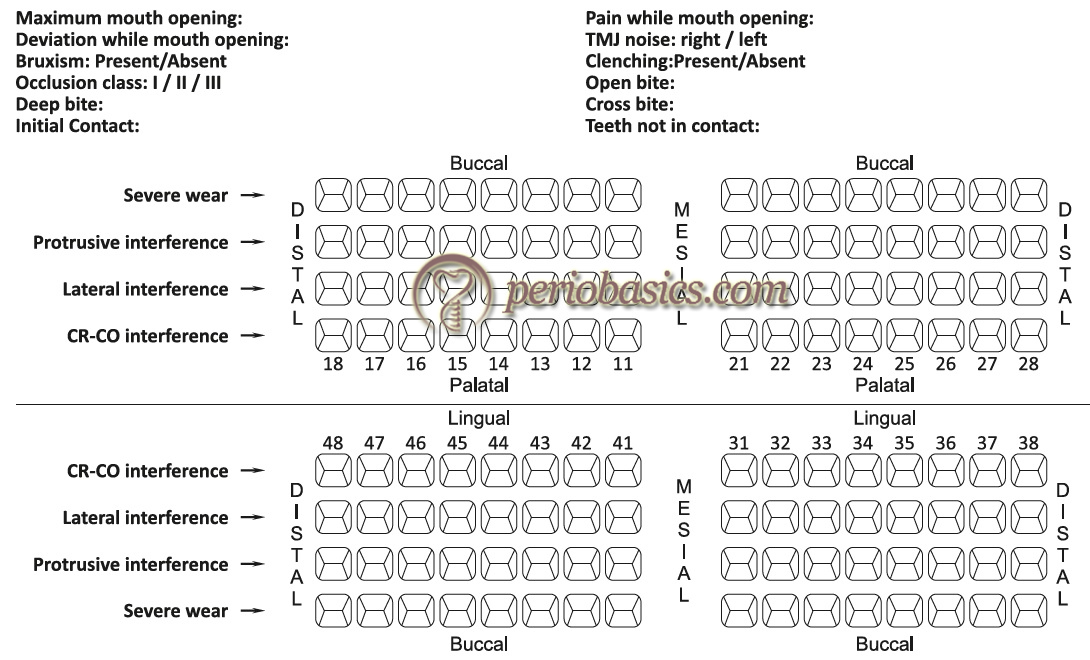
Now, the dental tape used to record CO and CR position is placed between the teeth and the patient is asked to bring teeth in CO position. The CO points of contact will superimpose on the lateral and protrusive contacts. The CO contact points (blue) can be differentiated from the lateral contacts (red) by their color difference.
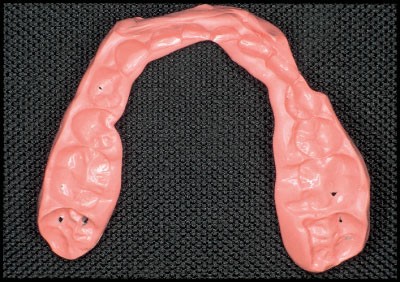
Impression making and articulator analysis
Although the information gathered from contact point markings in CR, CO, lateral and protrusive positions are sufficient to identify the occlusal interferences; but for accurate diagnosis and treatment planning, the impressions are ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Types of occlusal therapy
Occlusal therapy is any treatment that alters a patient’s occlusal condition. It can be used to improve the function of the masticatory system through the influence of occlusal contact patterns and by altering the functional jaw position. Occlusal therapy can be reversible or irreversible. Reversible therapy temporarily alters the occlusal condition, the joint position, or both. The example of this therapy is occlusal splints. The disadvantage of reversible occlusal therapy is that the original condition might return after the therapy is discontinued. On the other hand, irreversible therapy permanently alters the occlusal condition so that the original condition cannot be recovered. The examples of irreversible occlusal therapy include selective grinding, fixed prosthetic procedures, and orthodontic therapy. In the following sections, we shall discuss in detail the irreversible occlusal therapy (selective occlusal grinding).
Principles of selective grinding
The clinical procedure to eliminate occlusal interferences consists of three procedures, namely grooving, spheroiding and pointing 19. Grooving is done to re-establish the depth of developmental grooves. Spheroiding is done to restore the original tooth contour in areas with supra-contacts. Once the supra-contacts have been identified, the burs are applied with a paint brush like manner over the markings and reshaping is done up to 2-3 mm mesially and distally from the marking and 2-3 mm apical to the marking. The cusp height should be maintained during this procedure. In situations where ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Steps in the correction of occlusal interferences
Once the occlusal interferences have been identified, the clinician must determine the extent of occlusal adjustments required. As already stated, these adjustments should be first performed on the articulated casts and then should be duplicated on the patient. Another important factor to be considered while doing occlusal adjustment is the age of the patient. In younger patients, usually conservative approach is adopted because they have a developing dentition which may have many unpredictable mechanisms for occlusal harmonization. Only minor occlusal adjustment, interceptive in nature is adopted in these patients. On the other hand, in older patients extensive occlusal adjustment can be planned.
Basic principles followed to eliminate occlusal interferences
The selective occlusal grinding is done to eliminate the occlusal interferences in a stepwise manner. These are,
Step 1: Elimination of retrusive supra-contacts and deflective occlusal interferences from CR to CO. Step 2: Adjust CO to achieve stable, simultaneous, multi-pointed, widely distributed contacts. The unbalanced cuspal inclines and contacts should be eliminated to maintain or move the force vectors along the long axis of the tooth. Step 3: Test for excessive contact (fremitus) on the incisal teeth. Step 4: Remove posterior protrusive supra-contacts and establish contacts that are bilaterally distributed on the anterior teeth. Step 5: Remove all interferences to lateral excursions. Step 6: Eliminate gross occlusal disharmonies. Improve the occlusal anatomy by maintaining the cusp form, by creating correct marginal ridge relationships, cusp-fossa relationships, elimination of broad facets and narrow occlusal tables. Step 7: Re-check tooth contact relationships. Step 8: Polish all rough tooth surfaces.
Following is the detailed description of these steps,
The first step in the elimination of occlusal interferences is to remove these interferences in retrusive and CR to CO position. The primary objective here is to remove the supra-contacts and remove interferences that interfere with posterior border closure of the mandible to a stable bilateral RCP. The clinician should try to achieve following objectives by removing these interferences,
- A maximum number of centric holding contacts are achieved in CR position.
- Vertical dimension in CR should be same or a little more than in CO position.
- Removal of interferences from CR to CO position, thereby facilitating smooth gliding movement in the horizontal plane from CR to CO.
The interferences are identified by placing blue marking tape between the teeth and asking the patient to “Squeeze” once the initial contact is made. Most commonly the mesial inclines of the maxillary lingual cusps and their opposing tooth surfaces are typical sites for supra-contacts. The mesial inner incline of the lingual cusp of the maxillary first premolars is the most common initial supra-contact at the RCP.

The second step is to achieve stable centric contacts in CO position. The occlusal contacts in the CO position should be planned in such a way that maximum stability of occlusion in this position is achieved. The primary objectives of clinician during this step are,
- Achieving a cusp to fossa relationship wherever possible as compared to cusp to marginal relationship. The cusp should contact, preferably at the center of the fossae so that occlusal forces are directed along the long axis of the tooth. However, it should be remembered that in unworn teeth (young patients), the cusp tips do not reach the base of the fossa. In such situation, multiple contacts on the inclined planes are considered as stable centric holding contacts.
- There should be no cusp contacts with the inclined planes except for the lingual surfaces of the maxillary anterior teeth.
The patient is asked to tap the teeth together on both sides at the same time. This is CO position where the maxillary and mandibular teeth are in maximum contact. Now, the wax is placed ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
The third step is to remove excessive contacts from incisal surfaces. The objectives of this step are,
- Making the incisors slightly out of contact or in light contact over the maximum number of teeth.
- Eliminating supra-contact and hence trauma from occlusion on anterior teeth.
The firmness of the occlusal contact can be detected by placing a Mylar occlusal strip between the maxillary and mandibular anterior teeth held with a hemostat. The strip should just ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
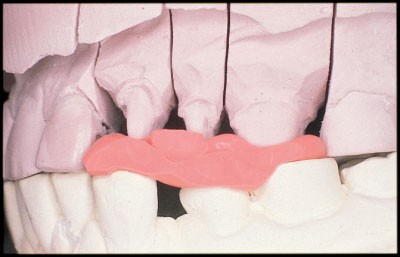
Protrusive excursion refers to the path of the mandible as it moves anteriorly between the CO and the edge to edge relationship of the anterior teeth (Figure 34.8). In this step, adjustment in protrusive excursions is done. The primary objectives of the dentist during this step are,
- Even distribution of contacts during protrusive excursions over as many teeth as possible. During the protrusive excursion, there should be no contact between the posterior teeth, except between the mesial slope of the buccal cusp of mandibular first premolar and the distal slope of maxillary cuspid.
- Reduction of the incisal edges of the extruded anterior teeth if they are interfering with the smooth protrusive excursion.
- Elimination of deep overbite by reduction of crown length of the anterior teeth. However, it must be remembered that it does not eliminate the requirement of orthodontic treatment. Only slight overbite can be eliminated by selective grinding. Moderate to severe cases require orthodontic treatment for deep bite correction.
The patient is asked to protrude the mandible slowly from CO position to edge to edge position of anterior teeth. Ideally, there should be bilateral contacts between maxillary and mandibular anterior teeth during this movement with little or no deviation of the mandible. The deviation usually is caused by a ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..

However, it should be preferred that wherever possible the adjustment is confined to the maxillary teeth to protect mandibular functional cusp height. Mandibular incisors should be ground only when the limit of grinding of the maxillary teeth has been reached because of pain, proximity to the pulp, or esthetic reasons. Following selective grinding, all the marks are removed and the patient is again asked to perform the protrusive movement. If posterior teeth are interfering with the protrusive movement, tooth structure is removed from the offending cusps until all articulating contacts between the posterior teeth have been eliminated.
This step deals with the removal or lessening of all interferences in lateral excursions. The mediotrusive interferences usually manifest as oblique facets on the first and second molar teeth on the inner inclines of the mandibular buccal cusps and the inner inclines of maxillary lingual cusps. The objectives of the dentist while eliminating lateral interferences are,
- A slight cuspid mediated disocclusion of the posterior teeth during the lateral excursion except in situations where cuspid is already worn and group function occlusion is present or cuspid is malposed and adjustment to group function of posterior teeth is necessary.
- Elimination of interferences on working side and balancing side.
- Elimination of interferences on central and lateral incisors which hinder the cuspid function during the lateral excursion except when both central and lateral incisors are in group function with cuspid and show no sign of trauma from occlusion.
While registering the lateral interferences, both habitual and passive (border) manipulation of the mandible is employed. A two-color method is used here in which the centric contact in CO are registered as blue and lateral supra-contacts are recorded in red color. For registering interferences on the working side, red ribbon is placed between the teeth in quadrant under question. Now, hold the mandible in CR position and ask the patient to close with moderate pressure. The patient is now asked to slide the mandible towards the right or left side, depending upon the side that has to be checked for working interferences. The red marks show interferences on the working side. Now, place a blue ribbon and without disturbing the red marks, establish the centric holding marks in CO position. To remove interferences, only undesirable red marks are removed. The inner inclines of maxillary buccal cusps or lingual surfaces of the upper anterior teeth are adjusted.

For registering interferences on the balancing side, a strip of adhesive occlusal registration wax is placed over the mandibular quadrant in question and another strip of folded occlusal registration wax is given to the patient that is placed on the opposite side and the patient is asked to chew this wax bolus up to five times. If there are ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
It should be remembered that while adjusting interferences on lateral excursion, reshape the inner inclines of the maxillary buccal cusps and mandibular lingual cusps. This is because grinding of the mandibular buccal cusps jeopardizes the functional cusps in CO position. Grinding should not result in the formation of flat surfaces and vertical stops should be preserved during the procedure.
This step deals with the elimination of undesirable gross occlusal features. Once all the interferences have been removed, there may be some remaining gross undesirable occlusal features which are harmful to the periodontal structures, and require modification. These include,
Extruded teeth:
These teeth are reduced to the level of the occlusal plane by grinding and reshaping within the limits permitted by proximity to the pulp.
Plunger cusps:
Plunger cusps are responsible for wedging of food in the interdental areas. Distolingual cusps of maxillary molars often are plunger cusps. These cusps should be rounded off and reshaped to eliminate food impaction.
Uneven adjacent marginal ridges:
These may also cause food impaction and should be corrected by either reducing the height of a comparatively high marginal ridge or increasing the height of a lower one with a restoration.
Rotated malposed and tilted teeth:
The most preferred treatment for rotated teeth is orthodontic de-rotation. However, minor rotations which interfere with the functional movement of the mandible or are causing food accumulation and impaction can be re-shaped by selective grinding.
The wear facets are the result of the tooth to tooth wear. These can be easily detected by drying the tooth surface and viewing under a regular dental chair lamp. These should be corrected because the periphery of these facets may produce lateral or tipping forces which are deleterious to the periodontium.
Flat occlusal wear:
Sometimes excessive wear of the occlusal surfaces of the posterior teeth results in the formation of the flat occlusal surface. Similar to facets, the margins of the occlusal wear creates force component which causes lateral and tipping forces deleterious to the periodontium. The anatomy of the occlusal surfaces should be restored by selective grinding.
All the occlusal adjustments done are re-investigated in this step. All possible movements are done to check retrusive, protrusive and lateralotrusive interferences. In cases where occlusal equilibration can be better achieved by prosthodontic, restorative or orthodontic treatment, these treatments should be considered.
All the surfaces which have been selectively reduced are then polished to achieve smooth tooth surfaces and patient is instructed regarding the maintenance of teeth.
Correction of occlusal discrepancies prior to restorative procedures
Prior to restorative treatment, the present status of patient’s functional occlusion should be carefully evaluated. The occlusal corrections, if required, should be done prior to the restorative treatment. Dentition that requires multiple occlusal restorations either immediately or in future should be corrected for occlusal abnormalities. Following types of discrepancies are commonly observed and should be corrected prior to restorative treatment,
Marginal ridge discrepancies:
Marginal ridges of the posterior teeth that do not direct the food into the fossae promote food impaction in the inter-proximal region. Before restoring these teeth, opposing marginal ridge should be ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Tooth extrusion is observed in the case where there is a massive coronal breakdown of the opposing tooth, or more frequently, if the opposite arch is edentulous. The extruded tooth should be corrected in conjunction with the restoration of the carious tooth or rehabilitation of the edentulous areas. It can be done by grinding or reshaping if the extrusion is slight or by installing a crown if the extrusion is excessive. If the extrusion is allowed to remain, it may result in functional disorders caused by occlusal interferences. Orthodontic treatment may be done to intrude the extruded tooth if extrusion is minor. However, it is difficult to intrude molars where extrusion is commonly seen. Sometimes, extrusion is so severe that intentional endodontic treatment of the extruded tooth followed by crown placement is required.
Plunger centric holding cusps commonly result because of tipping and extrusion into a grossly carious opposing occlusal surface. The correction of the plunger cusps must be done prior to the restoration of the carious tooth. Simply reducing the height of the plunging cusp would be insufficient and would result in an excessively flattened cusp. The centric holding areas should be ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Broad opposing wear facets:
Broad wear facets should be eliminated by reshaping to permit the establishment of minimal centric contact areas. However, while reshaping the surface, stable centric stops must be preserved.
Wide occlusal tables:
The wide occlusal tables are usually a symptom of excessive occlusal wear. They should be narrowed to achieve stable centric holding areas by reshaping the cusp tips.
Rotated teeth:
If possible, the rotated teeth should be treated by orthodontic treatment. Orthodontic de-rotation brings the tooth in a proper position. If orthodontic treatment is not possible, moderate reshaping of the rotated tooth may improve the occlusion.
Our primary aim of the restorative treatment is not only to restore the decayed tooth or to replace the missing tooth, but also to provide a harmonious occlusion to the patient which functions smoothly without causing any discomfort to the patient. The understanding of the basic principles of occlusion is essential to achieve this goal. It should be remembered that occlusal adjustments should be well planned because an improper treatment my worsen the existing problems of the patient.
A comprehensive TMJ and occlusal examination is an inseparable part of the complete periodontal examination. The neuromuscular harmony is the prime requirement for appropriate TMJ function and functional mandibular movements. However, it should be remembered that a thorough knowledge of occlusion is required to treat the condition otherwise the situation may worsen after the treatment. Therefore, clinical examination, which consists of the examination of the TMJ, teeth, soft tissue as well as the periodontium, should be carried out before the commencement of dental treatment. The occlusal examination and identification of the interferences should be done and in a stepwise manner, all the interferences should be eliminated.
References are available in the hard-copy of the website.
Suggested reading
- Gher ME. Changing concepts. The effects of occlusion on periodontitis. Dental Clinics of North America. 1998 Apr;42(2):285-99.
- De Boever JA, Carlsson GE, Klineberg IJ. Need for occlusal therapy and prosthodontic treatment in the management of temporomandibular disorders. Part I. Occlusal interferences and occlusal adjustment. Journal of oral rehabilitation. 2000 May;27(5):367-79.
- Rothner JT. Occlusal equilibration—A part of orthodontic treatment. American Journal of Orthodontics. 1952 Jul 1;38(7):530-7.
- McKenzie JS. Mutual problems of the periodontist and prosthodontist. Journal of Prosthetic Dentistry. 1955 Jan 1;5(1):37-42.
- Becker IM. Comprehensive occlusal concepts in clinical practice. John Wiley & Sons; 2010 Dec 20.
- Popa1a ST, Popescu2b SM, Constantinescu3c MV. OCCLUSAL EQUILIBRATION BETWEEN OPTION AND CLINICAL REALITY.
- Recent Posts
- Periodontal vaccine
- Can connective tissue attachment occurs over restorative surfaces like GIC/composite/ceramic?
- What are the oral and periodontal manifestations of Ehlers-Danlos syndrome (Type IV, VIII)?
- Periodontitis as an autoimmune disease
- Subversion of the host response in periodontitis
- Basic Periodontology
- Basic Sciences
- Clinical Periodontology
- Implantology
- Recent Research
Submit Your Query or Question. Will be Back to You Soon with an Answer
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 13 April 2002
Crowns and other extra-coronal restorations: Occlusal considerations and articulator selection
- J G Steele 1 ,
- F S A Nohl 2 &
- R W Wassell 3
British Dental Journal volume 192 , pages 377–387 ( 2002 ) Cite this article
7071 Accesses
19 Citations
Metrics details
Clarification of some of the terminology and concepts relating to occlusion as it is used in everyday practice, making clear why these concepts matter
Undertaking a simple pre-operative examination of the occlusion as a matter of routine
Helping clinicians identify cases where articulated study casts will help plan treatment and design restorations
Advice is provided about selecting an appropriate articulator and taking appropriate records at the treatment stage.
Crowns and extra-coronal restorations:
Changing patterns and the need for quality
Materials considerations
Pre-operative assessment
Endodontic considerations
Jaw registration and articulator selection
Aesthetic control
Cores for teeth with vital pulps
Preparations for full veneer crowns
Provisional restorations
Impression materials and technique
Try-in and cementation of crowns
Porcelain veneers
Resin bonded metal restorations
For many dentists, occlusion carries an air of mystique. It even seems sometimes that a perverse pleasure is derived in making the whole subject more complicated than it really is. As a clinician, you need to be able to decide what you expect from your proposed restoration, and to identify situations where you may need to alter the existing occlusal scheme. At a fundamental level, you also need to provide the laboratory with appropriate clinical records to ensure that when you fit them, adjustments to the expensively prepared restorations are minimal. This requires a sound understanding of the basics.
You have full access to this article via your institution.
Similar content being viewed by others

Occlusion: is there a third way? A discussion paper

Provisional restorations (Part 2)


Provisional restorations (Part 1)
This fifth article in the series will try to present important occlusal concepts in a way which relates directly to the provision of successful crowns. It is not a comprehensive guide to occlusion, or a manual of techniques for extensive fixed prosthodontics. There are several useful books and articles dedicated to the subject and some of these are specifically referenced (if a technique is particularly well described) or are listed in the further reading section. However, we hope that this article should allow you to avoid most of the problems associated with the provision of crowns. Occasionally some pre-operative occlusal adjustment is needed. Our experience is that this is best taught 'hands on' and we would recommend attending an appropriate course before attempting more complex adjustments.
Basic considerations – what matters?
One of the essential starting points with occlusion is to make sure that the terminology is clear. There are any number of occlusal terms, many of which overlap. There are only a few that really matter and these need to be understood if what is to follow is to make any sense.
The intercuspal position (ICP or IP)
Synonyms: centric occlusion (CO), maximum intercuspation
What is it?
Most dentate patients, when asked simply to 'bite together on your back teeth', close immediately into a comfortable, reproducible “closed” position where the maximum number of tooth contacts occur. This is the intercuspal position (ICP). Travel into this position is partly guided by the shape of teeth and partly by conditioned neuromuscular co-ordination. 1 ICP is the most 'closed' position of the jaws.
Why does this matter?
ICP is usually the position in which vertical occlusal forces are most effectively borne by the periodontium with teeth likely to be loaded axially, which helps to stabilise their position. Indeed it is the end point of the chewing cycle where maximum force is exerted. In everyday practice this is the position of the jaws in which restorations are made.
Guidance (from the teeth)
When a patient moves their mandible from side to side so that the teeth in opposing jaws slide over each other, the path taken is determined partly by the shapes of the teeth which make contact, as well as by the anatomical constraints of the temporomandibular joints (TMJs) and masticatory neuromuscular function. Each has a bearing on the other, and, for want of a better term, they should work in harmony. In these circumstances the teeth provide guidance for the movement of the mandible. The shape and form of the temporomandibular joints also guide the movement of the mandible (sometimes called posterior guidance). Guidance teeth can be any teeth, anterior or posterior.
When the patient slides the mandible out to one side, the side they move the mandible towards is called the working side (because it is usually the side on which they are about to chew). The other side, the side the mandible is moving away from, is called the non-working side. So for example, an excursion to the right (as may occur during chewing) will make the right side the working side and the left the non-working side, whilst during an excursion to the left the reverse will be true. During these excursions the upper and lower guidance teeth will be in contact and partly dictate the movement of the mandible. Canine guidance is where the upper and lower canines on the working side are the only teeth in contact during a lateral excursion, causing all of the posterior teeth to disclude ( Figs 1 and 2 ). When several pairs of teeth, usually premolars or premolars and canines (and sometimes molars) on the working side share the contacts during excursions group function is said to take place ( Fig. 3 ). Other patterns of guidance can take place, using almost any combination of teeth.

Posterior teeth are discluded but contact remains between the lateral incisors

Here the canines are the only teeth in contact

Guidance is described as being group function
Incisors and canines usually provide protrusive guidance, when the mandible slides forward, but where there is only a limited overbite the posterior teeth may be involved.
Why does it matter?
Guidance teeth are repeatedly loaded non-axially (laterally) during excursions. As a result heavily restored or crowned teeth may be at risk of fracture or decementation, particularly if these loads are heavy. Other manifestations of problems with guidance include:
Fractured teeth or restorations
Accelerated local wear
Tooth migration
Tooth mobility
TMJ dysfunction
To avoid these it is important to identify which teeth provide guidance before you start tooth preparation. If the guidance is satisfactory, and the guidance tooth or teeth are strong enough to withstand the likely loading in the long term, it is usually best to try to re-establish the same guidance pattern in the new restoration. Techniques for doing this are described later in the article. Occasionally, you may feel that a tooth that you are about to crown is insufficiently robust to carry a guidance contact and the guidance is best moved onto other teeth. A specific example of this would be where a broken down guidance canine is restored with a post retained crown. There may be a risk of root fracture of the tooth in the longer term because of the heavy lateral forces. In a case like this, by taking a little care with the shape of both preparation and crown, guidance can often be transferred from the canine to the premolars, if they are in a better position to accept the heavy loads.
Other practical reasons for identifying guidance teeth include:
The need to provide clearance from the opposing tooth during preparation, not just in ICP, but also along the guidance track. If you do not do this you can end up unwittingly transferring all the guidance forces on to your new crown.
The need to select and prescribe an appropriate material to restore the guidance surface (metal is usually best if possible).
These aspects are discussed in detail later in the series.
The message is that getting guidance right is one of the most important aspects of crown provision; problems can, and will, occur unless guidance is correctly managed on teeth to be crowned.
Interferences
What are they?
Interferences are any tooth-to-tooth contact(s), which hamper or hinder smooth guidance in excursions or closure into ICP. An interference on the side to which the mandible is moving is called a working side interference. An interference on the side from which the mandible is moving is called a non-working side interference (NWSI) or balancing side interference. There is a distinction to make between NWSIs and non-working side contacts: in the latter case, excursions are guided equally by working and non-working tooth contacts, akin to the balanced articulation often taught as an ideal complete denture occlusion. However, where there is a NWSI it acts as a cross arch pivot, disrupting the smooth movement and separating guidance teeth on the working side ( Fig. 4 ).
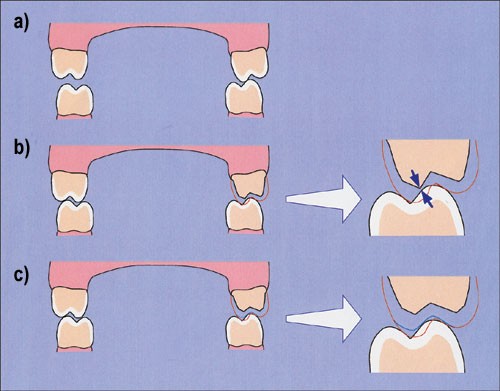
Occlusal reduction has eliminated the pivot, allowing the teeth on the working side to contact during lateral excursion. However, clearance between the preparation and opposing teeth is now inadequate which may cause problems with the provisional restoration. Worse still, the definitive restoration may require gross adjustment resulting in its perforation; c) You can avoid these problems by removing the non-working side contact prior to tooth preparation (blue line represents tooth recontoured in this way)
There has been much written about the significance or otherwise of interferences, particularly NWSIs, in relation to initiating parafunction and TMJ dysfunction. Warnings of the direst consequences to the stomatognathic system and beyond from NWSIs are frankly misleading though. Many people function perfectly happily with a mouthful of NWSIs. However, when contemplating crowns there are important implications. Most NWSIs are on molars so teeth or restorations directly involved are subject to high and often oblique occlusal forces with the consequent risk of fracture or uncementing.
As a general rule, it is best to remove interferences before tooth preparation if the interference is on a tooth which is to be prepared. This applies to all types of interference – working, non-working and protrusive. In practice it is best to do this at a separate appointment prior to tooth preparation. This will allow the patient time to adapt to a new pattern of excursive guidance, and you time to refine the guidance if necessary. The process of dealing with a non-working side interference prior to preparation is shown in Figure 4 . If you do this, it is important to identify suitable teeth on the working side to take over the guidance once the interference has been eliminated. If there are no teeth to take over the guidance, it may be impossible to eliminate the NWSI. If you are in any doubt it would be best to seek advice before cutting the tooth.
Where interferences exist on teeth that are not themselves to be prepared, the need for adjustment may be less important. Many people have asymptomatic interferences and seem to be able to lead a normal existence and we certainly would not advocate the removal of all interferences as a public health measure.
One final point is that it is disturbingly easy to introduce new interferences when you place restorations, even where there were no interferences previously. If you check your preparations for adequate clearance, not only in ICP but in lateral and protrusive excursions as well, the chances of this occurring should be minimised. Obviously, there is the opportunity to remove minor interferences on the final restoration before cementation.
Retruded Contact Position (RCP)
Synonyms: centric relation (CR), centric relation contact position (CRCP), retruded axis position (RAP), terminal hinge position.
This is the position of the mandible when the first contact between opposing teeth takes place, during closure on its hinge axis (or retruded arc of closure), that is with the condyles maximally seated in their fossae. This condylar position is one of health. Generally, as the mandible hinges closed with the condyles in this position, there is a contact between a pair of teeth somewhere around the mouth ( Fig. 5 ). The mandible will then close, from this retruded contact, down into ICP, usually sliding forward and laterally ( Fig. 6 ). If you want to try to manipulate a patient's mandible into this position it is important that they are relaxed ( Fig. 7 ), otherwise it can be very difficult and you will feel resistance to free movement of the mandible. For about 10% of people ICP will be the same as RCP 2 and in these cases if you hinge the mandible until the teeth are in contact they will go straight into ICP with no deflective contact.

Most retruded contacts cause no problems. This one resulted from over-eruption of the molar and the interference was associated with accelerated wear of the incisors
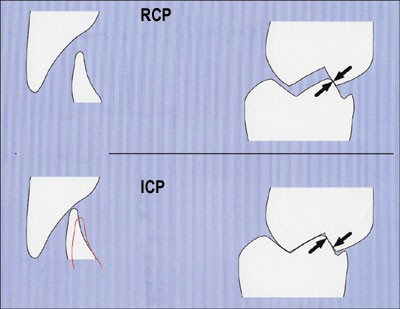
Here, in RCP the molars make first contact as shown by the arrows. The magnitude and direction of the slide can be estimated at both the molar and incisor regions

This technique is called bimanual manipulation and is designed to seat the condyles fully in their fossae with the disks interposed
There is no magic quality about RCP, but there are a number of reasons why RCP and the associated slide into ICP may be relevant when providing crowns. Box 1 contains a more detailed analysis of the situations where it may be a problem. In many, but not all cases, managing RCP is of less significance than managing guidance effectively, but there are times when adjustments need to be made and, clearly, it is always better to identify potential problems than blindly to hope for the best. To this end it is always worth examining RCP pre-operatively so that you at least know where it is. On the very few occasions where it is likely to be a major factor affecting your restorative procedure, casts mounted in RCP (or in the hinge axis just before the teeth actually contact) on a semi-adjustable articulator will facilitate occlusal examination and allow trial adjustments.
Establishing and recording RCP, and particularly re-organising the occlusion, are often difficult and we would refer you to Further Reading below if you wish to follow these subjects up in more detail.
Box 1: RCP and crowns
Most crowns and other extra-coronal restorations will be made to conform with the patient's ICP and usually a slide from RCP to ICP will be of no major relevance when providing crowns. In some circumstances additional management may be appropriate. The following are the situations where adjusting the contact in RCP is likely to be most important:
As a general rule, when RCP involves a tooth you are about to prepare it is often best to remove the deflective contact at an appointment before you start tooth preparation.
When re-organising the occlusion at a new vertical dimension you really have no option but to construct the new occlusion, if not at RCP itself , certainly around centric relation (with the condyles in the hinge axis). This represents the only reproducible starting point.
If you need space but you wish to avoid increasing the vertical dimension, there may be the scope to 'distalise' the mandible to create space lingually for anterior crowns (only possible where there is a bodily translation between RCP and ICP).
If you are about to restore anterior teeth and the RCP contact results in a strong anterior thrust against the teeth to be prepared.
Although we would usually advise removal of a deflective RCP interference before preparation if it is on a tooth you are about to prepare for a crown, many dentists do no not carry out any such adjustment and no problems result. This is probably because cutting the crown preparation effectively removes the contact. By removing it before preparation though you can ensure sufficient removal of tissue to allow space for the crown without re-introducing it in an uncontrolled way when the restoration is made. The principles involved are the same as those for removing non-working side interferences (see Fig. 4 ).
Practical aspects of occlusion: records for planning crowns
Records for planning crowns: the occlusal examination.
Before providing crowns it really is mandatory to undertake some sort of an occlusal examination. The following observations take moments to gather and are worth the effort:
Check ICP (for reproducibility and contacts on the teeth to be restored)
Check RCP (to establish whether there is any deflective contact or slide which you ought to know about). For technique see Reference 3.
Check the relationship of the teeth in lateral and protrusive excursions (to determine whether your crowns will be involved in guidance or if you need to consider removing an interference).
A more detailed and lengthy examination, where all of the contacts are marked using good quality ultra thin articulating tape ( Fig. 8 ) is sometimes indicated, particularly where there has been a history of temporomandibular dysfunction or where there is a specific occlusal problem which you need to address. The various components, which may be included in a full occlusal examination, are given in Box 2 .
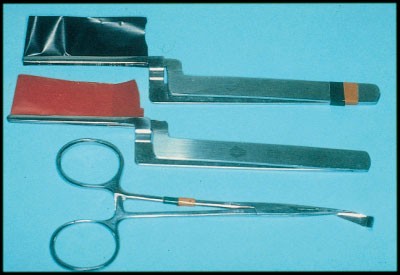
Tools for examining occlusal contacts: foil shimstock held in forceps and high quality ultra-thin articulating tapes held in Millers forceps
Box 2: Components of an occlusal examination
A full occlusal examination including all of the components below is rarely indicated, but different components may be required at different times. Visual assessments of ICP, RCP and guidance teeth are always indicated where you are planning crowns. The following may also be useful:
Examining for signs of temporomandibular dysfunction:
Palpation of muscles of mastication for tenderness.
Palpation of the temporomandibular joints and detailed assessment of any clicks or deviations in mandibular movement.
Assessment of the range of mandibular movement.
Checking for facets, fremitus, mobility and drifting (particularly where there are problems with individual teeth).
Marking up of the dry teeth in different coloured tapes ( Fig. 8 ) to show contacts in all excursions using a high quality articulating tape (where there are issues affecting the entire occlusal scheme).
Records for planning crowns: hand-held study casts
Hand-held casts can be a very useful aid to examination and treatment planning. To glean maximum information from them they need to be made from good quality impressions, which have been handled and poured correctly. We will return to this important but underrated subject later (see below: 'Opposing Casts').
Hand-held study casts enable:
A judgement to be made regarding the ease of obtaining a stable ICP. This helps to determine whether or not an interocclusal record is required for the working casts upon which the restoration(s) will be made.
An unimpeded view of ICP. It is possible to view aspects such as the lingual, which it would not be possible to see at the chairside.
Careful evaluation of clinical crown height and the availability of inter-occlusal space for restorative material. These two factors can help make the decision on how to facilitate the restoration of short teeth (see Part 3 'Pre-operative assessment' in this series).
However tempting it may be to assume otherwise, hand-held casts provide no information about excursive tooth contacts or RCP, beyond the distribution of wear facets.
Records for planning crowns: Articulated study casts
Accurate casts of the dental arches mounted in a semi adjustable articulator are the most important tools of the trade when constructing artificial crowns. The need for an articulator and the positions in which you mount the casts depend on what you need to do (see Box 3 ). Articulators are surrounded by an aura of mystery, but at the end of the day they are a tool to help give your patient a successful restoration and to help you to save time, money and hassle. The quality of the final result is much less dependent on the articulator you use than it is on the care you exercise to make and mount the casts that you put in it.
There is little merit in examining study casts for planning purposes on a simple hinge or other 'non-anatomical' articulator because the ability to replicate physiological movements will be, at best, crude, and at worst, wholly misleading. A non-anatomical articulator will allow casts to be put into a reproducible ICP, which may be helpful if there are insufficient contacts to make hand-held casts stable, but that is the limit of what a simple hinge articulator can do.
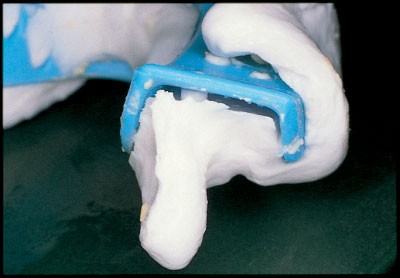
The combination of a facebow record (which locates the approximate position of the condylar hinge axis in relation to the upper arch) and a jaw relation record (which then locates the lower cast to the upper), enables movements of casts articulated on a semi-adjustable articulator to be reasonably anatomical. You can simulate the movements of the teeth in lateral and protrusive excursions, and around the hinge axis and be confident that what you see is close to what is really happening in the mouth. However, whilst the instrument is key, the quality of the casts and the care with which they are mounted are just as critical. There is no room for carelessness at this stage, wrongly articulated casts are probably worse than no casts at all as they may result in false assumptions about treatment. Similarly, inaccuracies with the original impressions can result in profound errors and the use of an accurate and stable impression material (such as addition cured silicone) may be appropriate in cases where a detailed occlusal analysis is necessary. Details of how to record a facebow record and a retruded hinge axis inter-occlusal record can be found in References 3 and 4. Some simple tips on accurate impression recording can be found in Box 4 .
This will equate to at least a 1mm occlusal error
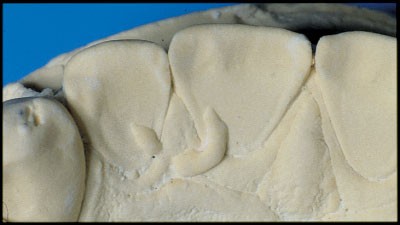
Large stone blebs on the palatal surfaces of upper anterior teeth as a result of air bubbles in the impression
Although you can see and reproduce movements with carefully articulated casts, you may often want to go on to the next stage and prepare a diagnostic wax up.
Box 3: When to use a semi-adjustable articulator during the manufacture of crowns
If you wish to ensure appropriate guidance with your new restorations, particularly where multiple crowns are involved.
If you plan to increase the vertical dimension at all.
In any case where either you are going to remove so many of the occlusal contacts that ICP will effectively be lost and/or where you plan to make a new ICP based on RCP (sometimes known as a reorganised occlusion).
Where you plan to remove occlusal interferences (the study casts can enable a trial adjustment to be carried out).
When there is a need to provide an occlusal stabilisation appliance (occlusal splint), either before treatment to stabilise jaw position or after treatment to protect restorations from the effects of bruxism.
Box 4: Taking a good opposing impression
Choose stock impression trays with adequate rigidity which, perhaps in combination with an adhesive, have sufficient retentive features to hold set alginate securely.
If the restoration is on a very posterior tooth you may need to extend the tray with a rigid material (green stick or compo but not carding wax) to ensure that the alginate is supported in important posterior areas.
Make sure adhesive has been air dried in the tray before loading alginate. Lots of wet adhesive acts as a lubricant not an adhesive, and if the alginate pulls away from the tray you are left with an enormous but not very obvious distortion in the final cast.
Dry the teeth with gauze or cotton wool to remove saliva, which aids tremendously in recording occlusal detail and producing of a smooth, hard cast surface. It can be done as the alginate is being mixed.
Smear a little alginate firmly onto the dry occlusal surfaces with your finger as the assistant finishes loading the tray.
After removal
Check to make sure the material has not pulled out of the tray ( Fig. 9 ). If it has, retake it and do not assume it will be all right or be tempted to press dislodged material back into place; you will pay in the time spent adjusting the final crown.
Cut off the heels of the impression flush with the tray if you do not need them, they are prone to distort when you lay the impression down on the bench or even when it is loaded with wet stone. This takes seconds.
If you get the chance, check the casts, if not, ask the technician to do this and to flick off any air bubbles on critical surfaces ( Fig. 10 ).
In really critical cases, consider using silicone to obtain a very accurate opposing cast especially if there is to be a delay before pouring up.
Records for planning crowns: the diagnostic wax-up
In addition to its uses in planning changes in appearance (see Aesthetic Control – the sixth article in this series), a diagnostic wax-up can be an absolutely invaluable technique where you are changing the occluding surfaces of several teeth with crowns or resin bonded restorations and allows you to plan the following:
The new static occlusal contacts (in ICP) and the shape of the guidance teeth
The impact that the modified occlusion has on appearance
The best options for creating interocclusal space for restoration(s) or optimising crown height by periodontal surgery (see Part 3: 'Pre–operative Assessment' in this series).
You can also use the completed wax-up as a template to determine the form of temporary and final restorations.
Practical aspects of occlusion: records for making crowns
When the diagnosis stage has been completed, the crowns or restorations still need to be made, and various records are essential at this stage too. This section discusses the choice of articulator and the need to obtain accurate occlusal records, including the simplest things such as opposing impressions, which are a frequent source of error. Finally, it introduces ways of controlling guidance on front teeth.
The articulator
When manufacturing the final crowns, in the interests of simplicity and cost it would seem sensible to use the simplest cast relating device that will not compromise the final restoration. 5 Small numbers of restorations, which are not involved in excursive contacts, can very reasonably be made on a non-adjustable articulator and then any adjustments made in the mouth before final cementation. However, crowns involved in excursions benefit from the use of an articulator with anatomical dimensions so that the excursive movements can be made and the shape of the crown adjusted in the lab with reasonable accuracy, saving chairside time. This becomes particularly important, and cost effective, when several restorations are being created at the same time. Highly sophisticated semi-adjustable and fully adjustable articulators are available for this purpose, but the majority of cases can be managed quite satisfactorily using a less sophisticated, fixed average value articulator in combination with a facebow.
It may not be possible to check occlusion on adhesive restorations prior to cementation, either because the act of checking may damage porcelain, which is delicate until cemented, or because they will not stay in place during excursions. In these cases, controlling the role of the restorations in guidance can be critical to their long-term survival. A semi-adjustable articulator can be invaluable in situations such as these because it allows the technician to secure restorations onto the working cast and do the critical adjustments in the lab so that all you need to do is cement them with little or no adjustment afterwards.
Opposing casts
In any discussion about articulators, it is disturbingly easy to forget the importance of an accurate cast to oppose the working cast. The opposing impression is often the last thing we do and, after a long session preparing teeth, making temporaries and taking impressions it tends to be a bit of an afterthought. However, a poor opposing impression is very easy indeed to achieve and yet can cost a great deal of precious time subsequently. A cast made with a distorted impression or a porous impression resulting in plaster blebs on occlusal surfaces will not fit comfortably into ICP. If such a cast is used in the lab it can result in a crown which looks perfectly good on the cast but which may be very high in the ICP and which can take a great deal of time to get right prior to fit. It is easy to record bad opposing impressions, but good ones are just as easy. Attention to the few steps listed in Box 4 takes, literally, no extra time but can save a lot of heartache. In an ideal world every opposing impression would be recorded in a dimensionally accurate and stable material such as an addition cured silicone, but this is probably not economically realistic. Box 4 describes the use of alginate for an opposing impression. In cases involving multiple restorations though, a very stable and accurate material may be cost effective in the long term.
Interocclusal records (IOR)
Once you have your working impression and opposing impression you then need to decide whether you need to provide additional information to the lab to allow them to mount the casts; an inter-occlusal record (IOR). There is a common perception that providing an intercuspal record (such as a wax or silicone 'bite') will improve the accuracy of mounted casts. The truth is that in many cases it does precisely the opposite. 6
For a patient with a stable intercuspal position, the loss of interocclusal contact created by preparation of a tooth for a single unit restoration, is unlikely to detract from the ease with which working and opposing casts can be located in ICP. In this circumstance, placing a layer of wax or silicone between the casts to help to locate them can often result in them failing to seat into ICP at all, and there is a very serious risk of the record introducing inaccuracies, rather than acting as the 'insurance policy' you intended. It is worth taking the opportunity of examining the ease with which any study casts can be located by hand before deciding whether an IOR is needed. Often (perhaps even usually) you are better with nothing at all.
Sometimes an IOR is required to stabilise casts, particularly where the teeth that are prepared are key support teeth in an arch. The choice of materials is generally between hard wax alone, hard wax (as a carrier) used with zinc oxide/eugenol, silicone elastomers and acrylic resins. The fundamental requirement is to obtain enough detail in a dimensionally stable recording material to enable casts to be confidently located in the laboratory whilst not recording so much detail that it stops the casts seating. Occlusal fissure patterns reproduced accurately in the IOR may well not be reproduced to the same extent in the cast, preventing full seating of the casts in the record. Furthermore, an IOR which contacts soft tissues in the mouth and causes their displacement (which is obviously not reproduced in the stone cast) will result in an IOR which will not seat accurately ( Figs 11 and 12 ). In order to meet the requirements for success, an IOR should:
Record the tips of cusps or preparations
Avoid capturing fissure patterns as much as possible
Avoid any soft tissue contact
The excessive detail may well hinder seating on a stone cast. See Fig. 12

There were sufficient tooth contacts in the intercuspal position not to need an interocclusal record for this case!
The key to a successful record is not so much the type of material used, but how it is used. The smaller the amount you use, the less it is likely to cause a problem. A small, trimmed record, restricted to the area of the preps themselves, with all interproximal tags and undercuts removed is the ideal. It is usually necessary to trim the record to achieve these requirements and silicone materials trim very easily with a scalpel ( Fig. 13 ). One final consideration is that stone casts and dies can easily be abraded by IORs especially those made of acrylic resin and special care is required in the laboratory when these materials are used in combination.
The resulting crowns needed no adjustment
Whether or not you have used an inter-occlusal record, you can easily verify the accuracy of mounted casts in the ICP using foil shimstock. When held tightly together the cast should hold the shim between the same teeth as they do in the mouth.
Copying tooth guidance
When a restoration is being provided which includes a guiding surface for mandibular excursions (lateral, protrusive or anything in between), the technician needs to know what form the contacting surface is to take. Failure to appreciate this risks introducing excursive contacts that are not in harmony with the other guidance teeth, the condylar movements and musculature. This is discussed fully earlier in the article, but common manifestations of disharmony include:
Decementing and fractured crowns
Because they are intimately involved in speech formation, getting guidance wrong on the palatal surfaces of upper anterior teeth may also come to light as phonetic problems.
The guidance of a new restoration can often be made simply to fit in with that provided by adjacent teeth (for example in group function). In this case the new functional surface is relatively straightforward to achieve on a semi-adjustable articulator or even at the chairside. However, if several teeth are to be prepared there may be no existing guiding surfaces left intact after preparation, so all clues to guidance are lost ( Fig. 14 ). Where satisfactory guidance is present before you start, there are several ways of copying it before you prepare the teeth. A commonly used technique is to use a putty matrix made on a cast of the tooth surfaces to be copied, but this technique will often not provide the tight control over tooth shape which is required. The two most effective methods to address this problem necessitate the use of a facebow and semi-adjustable articulator to allow anatomical movements in excursions. They are:
The 'crown about' method: Alternate teeth are restored, thus maintaining the shapes of functional surfaces, which continue to provide guidance for the articulated casts. This technique is well described in Reference 7.
The custom incisal guide table: This is another way of copying satisfactory anterior guidance from teeth or trial restorations that provide crucial excursive contacts. Unlike the previous method, it enables guidance to be copied for just one restoration. It involves moving study casts (on a semi-adjustable articulator) through the full range of lateral and protrusive excursions with a mound of un-set acrylic on the guide table, so that the tip of the articulator guide pin shapes the acrylic dough into (once set) a permanent record of the movements of the mandible ( Fig. 15 ). When the working casts are articulated the acrylic guide table guides the articulator through the same movements that were present in the study casts, and the palatal surfaces of the upper teeth can be shaped to conform precisely to this. This technique is described in detail, with illustrations, in Reference 4.
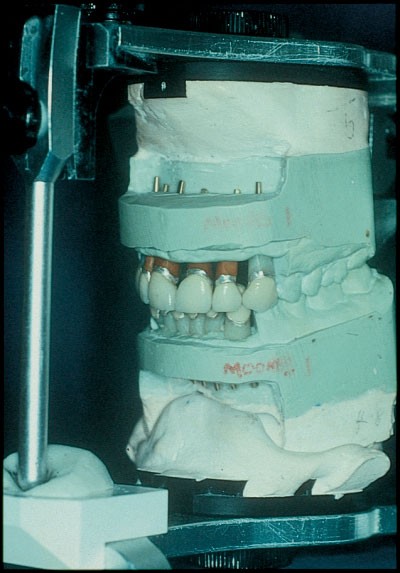
This is an excellent method of copying tooth guidance into definitive restorations

Preparation of the teeth has resulted in loss of all guiding surfaces on the anterior teeth
The extra effort involved in using these techniques is not enormous, and where several anterior teeth are to be crowned we would strongly recommend using one or other of them.
Okeson JP . Management of temporomandibular disorders and occlusion . 1998 4th Edition. St Louis: Mosby pp 47–51.
Google Scholar
Posselt U Studies in the mobility of the human mandible. Acta Odontol Scand 1952; 10 : 109.
Wise D Occlusion and restorative dentistry for the general practitioner. Part 2- Examination of the occlusion and fabrication of study casts. Br Dent J 1982; 152 : 160–165.
Article Google Scholar
Howat AP, Capp NJ, Barrett NV J A colour atlas of occlusion and malocclusion.1991 London: Wolfe Publishing pp137–139.
Loos LG Clinical criteria used to select an articulator. Compend Contin Educ Dent 1993; 14 : 80–88.
Walls AWG, Wassell RW, Steele JG A comparison of two methods for locating the intercuspal position (ICP) whilst mounting casts on an articulator. J Oral Rehabil 1991; 18 : 43–48.
Wise D Occlusion and restorative dentistry for the general practitioner. Part 9 – Restoration of anterior teeth. Br Dent J 1982; 152 : 407–413.
Wise M. Occlusion and restorative dentistry for the general practitioner. Series of ten articles published in the Br Dent J 1982; 152 : 117; 152 : 160; 152 : 197; 152 : 235; 152 : 277; 152 : 316; 152 : 347; 152 : 381; 152 : 407; 153 : 13.
Howat A P, Capp N J, Barrett N V J . A colour atlas of occlusion and malocclusion . 1991. London: Wolfe Publishing.
Shillingburg H T Jr, Hobo S, Whitset L D, Jacobi R, Brackett S E. Fundamentals of fixed prosthodontics . 3rd ed. 1997. London: Quintessence Publishing Co.
Download references
Author information
Authors and affiliations.
Senior Lecturer in Restorative Dentistry, Department of Restorative Dentistry, The Dental School, Framlington Place, NE2 4BW, Newcastle upon Tyne
Consultant in Restorative Dentistry, The Dental Hospital, Framlington Place, NE2 4AZ, Newcastle upon Tyne
Senior Lecturer in Restorative Dentistry, Department of Restorative Dentistry, The Dental School, Framlington Place, Tyne NE2 4BW, Newcastle upon
- R W Wassell
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to J G Steele .
Additional information
Refereed paper
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Steele, J., Nohl, F. & Wassell, R. Crowns and other extra-coronal restorations: Occlusal considerations and articulator selection. Br Dent J 192 , 377–387 (2002). https://doi.org/10.1038/sj.bdj.4801380
Download citation
Published : 13 April 2002
Issue Date : 13 April 2002
DOI : https://doi.org/10.1038/sj.bdj.4801380
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Over-the-counter (otc) bruxism splints available on the internet.
- R. W. Wassell
- F. Lobbezoo
British Dental Journal (2014)
Communication methods and production techniques in fixed prosthesis fabrication: a UK based survey. Part 2: Production techniques
- H. Petridis
Diagnosis and Management of Occlusal Wear: A Case Report
- V. R. Thirumurthy
- Y. A. Bindhoo
- P. Vidhiyasagar
The Journal of Indian Prosthodontic Society (2012)
Treatment of temporomandibular disorders by stabilising splints in general dental practice: results after initial treatment
British Dental Journal (2004)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Preplanned tours
- Daytrips out of Moscow
- Themed tours
- Customized tours
- St. Petersburg
Moscow Metro
The Moscow Metro Tour is included in most guided tours’ itineraries. Opened in 1935, under Stalin’s regime, the metro was not only meant to solve transport problems, but also was hailed as “a people’s palace”. Every station you will see during your Moscow metro tour looks like a palace room. There are bright paintings, mosaics, stained glass, bronze statues… Our Moscow metro tour includes the most impressive stations best architects and designers worked at - Ploshchad Revolutsii, Mayakovskaya, Komsomolskaya, Kievskaya, Novoslobodskaya and some others.
What is the kremlin in russia?
The guide will not only help you navigate the metro, but will also provide you with fascinating background tales for the images you see and a history of each station.
And there some stories to be told during the Moscow metro tour! The deepest station - Park Pobedy - is 84 metres under the ground with the world longest escalator of 140 meters. Parts of the so-called Metro-2, a secret strategic system of underground tunnels, was used for its construction.
During the Second World War the metro itself became a strategic asset: it was turned into the city's biggest bomb-shelter and one of the stations even became a library. 217 children were born here in 1941-1942! The metro is the most effective means of transport in the capital.
There are almost 200 stations 196 at the moment and trains run every 90 seconds! The guide of your Moscow metro tour can explain to you how to buy tickets and find your way if you plan to get around by yourself.
Moscow Metro Tour
- Page active

Description
Moscow metro private tours.
- 2-hour tour $87: 10 Must-See Moscow Metro stations with hotel pick-up and drop-off
- 3-hour tour $137: 20 Must-See Moscow Metro stations with Russian lunch in beautifully-decorated Metro Diner + hotel pick-up and drop off.
- Metro pass is included in the price of both tours.
Highlight of Metro Tour
- Visit 10 must-see stations of Moscow metro on 2-hr tour and 20 Metro stations on 3-hr tour, including grand Komsomolskaya station with its distinctive Baroque décor, aristocratic Mayakovskaya station with Soviet mosaics, legendary Revolution Square station with 72 bronze sculptures and more!
- Explore Museum of Moscow Metro and learn a ton of technical and historical facts;
- Listen to the secrets about the Metro-2, a secret line supposedly used by the government and KGB;
- Experience a selection of most striking features of Moscow Metro hidden from most tourists and even locals;
- Discover the underground treasure of Russian Soviet past – from mosaics to bronzes, paintings, marble arches, stained glass and even paleontological elements;
- Learn fun stories and myths about Coffee Ring, Zodiac signs of Moscow Metro and more;
- Admire Soviet-era architecture of pre- and post- World War II perious;
- Enjoy panoramic views of Sparrow Hills from Luzhniki Metro Bridge – MetroMost, the only station of Moscow Metro located over water and the highest station above ground level;
- If lucky, catch a unique «Aquarelle Train» – a wheeled picture gallery, brightly painted with images of peony, chrysanthemums, daisies, sunflowers and each car unit is unique;
- Become an expert at navigating the legendary Moscow Metro system;
- Have fun time with a very friendly local;
- + Atmospheric Metro lunch in Moscow’s the only Metro Diner (included in a 3-hr tour)
Hotel Pick-up
Metro stations:.
Komsomolskaya
Novoslobodskaya
Prospekt Mira
Belorusskaya
Mayakovskaya
Novokuznetskaya
Revolution Square
Sparrow Hills
+ for 3-hour tour
Victory Park
Slavic Boulevard
Vystavochnaya
Dostoevskaya
Elektrozavodskaya
Partizanskaya
Museum of Moscow Metro
- Drop-off at your hotel, Novodevichy Convent, Sparrow Hills or any place you wish
- + Russian lunch in Metro Diner with artistic metro-style interior for 3-hour tour
Fun facts from our Moscow Metro Tours:
From the very first days of its existence, the Moscow Metro was the object of civil defense, used as a bomb shelter, and designed as a defense for a possible attack on the Soviet Union.
At a depth of 50 to 120 meters lies the second, the coded system of Metro-2 of Moscow subway, which is equipped with everything you need, from food storage to the nuclear button.
According to some sources, the total length of Metro-2 reaches over 150 kilometers.
The Museum was opened on Sportivnaya metro station on November 6, 1967. It features the most interesting models of trains and stations.
Coffee Ring
The first scheme of Moscow Metro looked like a bunch of separate lines. Listen to a myth about Joseph Stalin and the main brown line of Moscow Metro.
Zodiac Metro
According to some astrologers, each of the 12 stops of the Moscow Ring Line corresponds to a particular sign of the zodiac and divides the city into astrological sector.
Astrologers believe that being in a particular zadiac sector of Moscow for a long time, you attract certain energy and events into your life.
Paleontological finds
Red marble walls of some of the Metro stations hide in themselves petrified inhabitants of ancient seas. Try and find some!
- Every day each car in Moscow metro passes more than 600 km, which is the distance from Moscow to St. Petersburg.
- Moscow subway system is the 5th in the intensity of use (after the subways of Beijing, Tokyo, Seoul and Shanghai).
- The interval in the movement of trains in rush hour is 90 seconds .
What you get:
- + A friend in Moscow.
- + Private & customized Moscow tour.
- + An exciting pastime, not just boring history lessons.
- + An authentic experience of local life.
- + Flexibility during the walking tour: changes can be made at any time to suit individual preferences.
- + Amazing deals for breakfast, lunch, and dinner in the very best cafes & restaurants. Discounts on weekdays (Mon-Fri).
- + A photo session amongst spectacular Moscow scenery that can be treasured for a lifetime.
- + Good value for souvenirs, taxis, and hotels.
- + Expert advice on what to do, where to go, and how to make the most of your time in Moscow.
Write your review
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Int Med Res
- v.48(10); 2020 Oct
Clinical performance of cantilevered resin-bonded fixed partial dentures for single tooth replacement in elderly patients
Hai-yan qiu.
1 Department of Geriatric Stomatology, Qingdao Stomatological Hospital, Qingdao, China
Shuang-Yan Wu
2 Department of Multidisciplinary Comprehensive Clinic, Qingdao Stomatological Hospital, Qingdao, China
To evaluate the clinical performance of cantilevered resin-bonded fixed partial dentures (CRBFPDs) in single tooth replacement in elderly patients at Qingdao Stomatological Hospital.
In total, 186 CRBFPDs in 153 patients were made from cobalt-chrome alloy. Panavia F 2.0 was used as a luting agent after air-abrasion. Restoration were evaluated at 3-month intervals with regard to function, esthetics, and possible complications.
CRBFPDs were evaluated after intervals of 12 to 40 months. The average clinical service time (i.e., length of time in situ at examination, including re-cementation after debonding) was 26.2 ± 13.6 months. Among these CRBFPDs, 87 (46.8%) were bridges in the maxilla, while 99 (53.2%) were bridges in the mandible. Most CRBFPDs (184, 98.9%) survived throughout the study period, while two (1.1%) were regarded as failed. The majority of debonded bridges had been used to replace the maxillary central incisor (60%).
Our findings confirm the successful clinical performance of CRBFPDs with tooth preparation designs involving mesial and distal vertical grooves in elderly patients.
Introduction
Resin-bonded bridges were first introduced in the 1970s, but initial implementation attempts failed. 1 Because of the continuous development of adhesives and retention designs, the clinical survival rate of resin-bonded fixed partial dentures has reached nearly 88% and continues to increase. 2 Resin-bonded fixed partial dentures have been accepted as an alternative fixed restorative treatment option for the replacement of a missing single tooth, in contrast to traditional fixed partial dentures that involve extensive preparation of abutment teeth. For cantilevered resin-bonded fixed partial dentures (CRBFPDs), the pontic generally moves with the single abutment tooth, particularly during protrusive and lateral movements under tooth contact. 3 Because of advancements concerning materials and resin cements with improved bonding capacity, CRBFPDs might constitute an alternative treatment for replacement of a missing single tooth. 4 – 7
Djemal et al. 8 reported that the risk of failure for a fixed-fixed partial denture was nearly twofold greater than the risk for a cantilevered fixed partial denture. Furthermore, with each additional abutment, the likelihood of debonding was found to increase. Botelho et al. 9 reported that two-unit CRBFPDs have significantly better success and survival than fixed-fixed three-unit resin-bonded bridges design for the replacement of a maxillary incisor. To the best of our knowledge, no study has described the clinical performance of CRBFPDs for restoration of single tooth loss in elderly patients. Therefore, the present study evaluated the clinical effectiveness of CRBFPDs in single tooth replacement in elderly patients.
Patient and abutment selection
This study included elderly individuals with single-unit edentulous spans bounded by sound teeth, all of whom were patients at Qingdao Stomatological Hospital during the period from September 2015 to January 2019. The study was conducted in accordance with the tenets of the Declaration of Helsinki; the study protocol was approved by the Ethics Committee of our hospital (No. 2020-2022). Written informed consent was obtained from each participant.
The selected abutment teeth were healthy, unrestored or minimally restored, free of caries and periodontal disease, and had adequate enamel height and width (clinical crown >4 mm). All patients underwent simple restorative clinical treatment. In addition, replacements of missing molars were limited to a premolar-sized pontic.
Clinical and laboratory procedures
Tooth preparation comprised maximization of the surface area for bonding and enhance of resistance. When possible, retention was improved by preparation of 1-mm deep mesial and distal vertical grooves. All tooth preparations were conservative at the lingual aspect with a supragingival finish line; the incisal margin of preparation was 1 mm shorter than the incisal edge in the anterior region ( Figure 1a, b ).

Clinical photographs of teeth involved in this study.
a and b: Labial and occlusal views of a cantilevered resin-bonded fixed partial denture replacing tooth 14, with tooth 15 serving as abutment. Tooth preparation comprised 1-mm-deep mesial and distal vertical grooves
c: View after laboratory procedures. The bridge framework was made with a supragingival finish line, such that the incisal margin was 1 mm shorter than the incisal edge
d and e: Occlusal and labial views after finishing. The pontic occlusion made slight contact in the centric occlusion and no contact during lateral and protrusive excursions.
After preparation, a full-arch working impression was made with polyvinylsiloxane impression material in a custom tray. The outline of the bridge framework was drawn on a working cast by a single technician. A cobalt-chrome alloy (Bondiloy, Austenal, Inc., Chicago, IL, USA) suitable for porcelain bonding was used. The minimum dimensions of the connector were 2 mm labiolingually and 4 mm cervicoincisally. The minimum thickness of the metal retainer wings was 1.0 mm. During the fitting process, pontic occlusion was adjusted to prevent occlusion contact or allow slight contact in the centric occlusion, and to provide protection from occlusion during lateral and protrusive excursions. After a satisfactory try-in, bridges were returned to the laboratory for glazing and polishing; the retainer surfaces were subjected to grit blasting with 50 μm of aluminum oxide powder at a pressure of 520 kPa. CRBFPDs were cemented with Panavia F 2.0 (Kuraray Medical, Okayama, Japan) in accordance with the manufacturer’s instructions (prepared enamel was etched with 37% phosphoric acid for 15 s prior to bonding) under rubber dam isolation ( Figure 1c–e ).
Recall and evaluation
Recalls and evaluations were conducted at 3-month intervals. Patients who did not attend clinical assessments were contacted by telephone to acquire information regarding the performance of their bridges. “Survival” of a CRBFPD was defined as any restoration that remained in situ. Complications were recorded when bridges were debonded on ≥2 occasions. To determine the degree of patient satisfaction with the bridges, the scale was subdivided into units from 0 to 100, where 0 represented “very dissatisfied” and 100 represented “very satisfied.” 10
Statistical analysis
Comparisons were performed using analysis of variance, the chi-squared test, and the t -test, as appropriate. P <0.05 was considered statistically significant.
In total, 153 patients (186 bridges) were included in the present study. Sixty-eight patients (44.4%) were men and 85 patients (55.6%) were women; their median age at the time of bridge insertion was 67.7 years. CRBFPDs were evaluated after 12 months of use. The average clinical service time (i.e., length of time in situ at examination, including re-cementation after debonding) was 26.2 ± 13.6 months ( Table 1 ). Furthermore, 87 bridges (46.8%) were in the maxilla, while 99 bridges (53.2%) were in the mandible.
Distribution of replaced teeth.
Most CRBFPDs (88%) survived throughout the study period. Most instances of debonding involved bridges that had replaced the maxillary central incisor (60%). Three CRBFPDs that replaced maxillary central incisors require re-cementation after debonding; one bridge exhibited debonding on more than one occasion (25%). However, after re-cementation, these were functioning appropriately at the end of the study census date. One prosthesis that replaced posterior teeth exhibited debonding after 25 months. Excessive occlusal contacts and pontic overload were the presumed causes of debonding of the prosthesis that replaced posterior teeth; after debonding, the patient selected a removable partial denture instead of re-cementation due to the loss of additional teeth. In total, two prostheses (1.1%) were regarded as failed. None of the abutments had a depth of ≥3 mm. The bridges that replaced mandibular teeth and maxillary premolars exhibited optimal performance without debonding. There was no statistically significant association between pontic position and debonding.
No secondary caries or obvious change in abutment mobility occurred. The degree of satisfaction with CRBFPDs was high (92.6 ± 6.1); this was not influenced by the occurrence of failure. Overall, only one score was <70; the lowest score was given for a bridge that had debonded more than twice.
In a prior in vitro study, debonding was found to result from cohesive failure within cement at the filler–resin interface. 11 Another in vitro study revealed that the use of Unifix and airborne-particle abrasion (50-µm aluminum oxide) provided the strongest physical bond. 12 In the present study, cobalt–chrome alloy was chosen as the framework material because the application of nickel–chromium alloy is decreasing in China. 13 Bond strength could be significantly improved through the airborne-particle abrasion of the alloy. Furthermore, the cement and alloy material were limited to reduce the number of clinical variables in the present study.
Locations of pontics and/or abutments
It has been suggested that a larger enamel surface area for cement is associated with greater bridge retention. 14 In our study, the bridges that replaced mandibular teeth and maxillary premolars exhibited optimal performance, without debonding. In contrast, bridge debonding occurred at sites involving maxillary incisors, maxillary canines, and maxillary molars. When compared with bridges that replaced other teeth, bridges that replaced maxillary central incisors exhibited greater likelihood of debonding. In the present study, all central incisor pontics were cantilevered from the neighboring maxillary central incisor. When a tooth with an equivalent palatal surface area is used, the bridge is cantilevered across the midline. The clinical effectiveness of this approached remains unknown and requires further investigation.
Periodontal outcomes
None of the abutments had a probing depth of ≥3 mm. The periodontal receptors of abutment teeth were presumed to prevent pontic overloading during mastication, thereby minimizing the risks of movement or tilting of the abutment tooth. Botelho 14 also warned against the use of abutment teeth with bone loss in patients with uncontrolled periodontitis because of possible drifting. It was found that there was no difference in periodontal response (e.g., swelling or pain) between CRBFPDs and a fixed-fixed resin bonded bridge. 11
Tooth preparation
Tooth preparation can increase the thickness of metal retainers and reduce the shear–peel force on the cement junction. Priest 15 recommended enhancing the resistance of abutment teeth through the use of grooves. Abuzar et al. 16 reported that the survival rates of anterior resin-bonded bridges with tooth preparation involving mesial and distal vertical grooves were 98% at 5 years, 97.2% at 10 years, and 95.1% at >12 years. The placement of supragingival retainer margins might facilitate good oral hygiene to control dental plaque and prevent gingivitis, periodontitis, and dental caries. Furthermore, this placement may simplify the impression and finishing procedures.
There were some limitations in this study. Because of the limited data, no Kaplan–Meier survival curve could be generated in this study; this analysis requires a larger sample size in a future study. Moreover, additional prospective studies are needed to observe the long-term performance of CRBFPDs in elderly patients, and to compare this performance against other bridge designs.
In this study, CRBFPDs demonstrated a high survival rate with short longevity. Thus, CRBFPDs constitute a conservative treatment suitable for both young and elderly patients.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
This study was supported by Qingdao Key Health Discipline Development Fund.
Shuang-Yan Wu https://orcid.org/0000-0001-8621-0268

IMAGES
VIDEO
COMMENTS
Protrusion, Retrusion, and Excursion in Healthcare. Healthcare professionals use protrusion, retrusion, and excursion when documenting, performing assessments on patients, or treating disorders. For example, in her head-to-toe assessment, Nurse Sarah asked me to stick out my tongue (an example of protrusion), to assess cranial nerve twelve.
Protrusion, retrusion, and excursion are terms used in anatomy to describe body movements going anteriorly (forward), posteriorly (backward), or side-to-side...
Occlusion is an integral part of dental treatment as dentists cannot repair, move or remove teeth without affecting occlusion. 1. The masticatory system comprises the teeth, the periodontal tissues and the articulatory system. The articulatory system is in itself a triumvirate comprising the temporomandibular joint (TMJ), muscles of mastication ...
From the article: Full mouth non-prep adhesive rehabilitation for erosion and attrition - The award "Excellence in Prosthodontics" 2017 winning case by Dr. I...
These tracings serve as stops in the future to record centric relations. The centric, protrusive and lateral excursion movements are recorded. Firstly, protrusive excursion movement is recorded by guiding the patient to bring the mandible into the forward position from the retruded position, approximately 6mm, anterior to the posterior position.
Occlusal contacts for both lateral and protrusive excursions of the mandible were determined by intraoral examination with the aid of shimstock to confirm the contact between the teeth, as was done in previous investigations.7,22-24 Shimstock has been shown to have greater interexaminer reliability than articulating film25 and high ...
Forward movement of the mandible so that the upper and lower central incisors were edge-to-edge was on the average 36.3% of the maximum protrusive movement. Movement of the mandible so the canines were edge-to-edge averaged 45.2% of the maximum lateral excursion on the left side, and 44.0% of the maximum right lateral excursion.
Protrusive excursions. Right lateral excursions. Left lateral excursions. The starting point of these movements as inscribed by this trace is the arrowhead ...
This study characterizes the mandibular protrusive and lateral excursions of children with primary dentition. With use of a Selspot ® system, the protrusive and lateral excursions of nine children with the primary dentition and nine adults with the permanent dentition were measured and compared. This system was able to analyse the simultaneous movements of multiple points on the mandible of a ...
summary This study investigated the sagittal condylar path during protrusive and lateral excursions by analysing the actually measured jaw movement data and re-evaluated the setting of the sagittal condylar path inclination in consideration of Fischer's angle. Protrusive and lateral excursions of 10 healthy subjects were measured using a three-dimensional mandibular movement analysing system.
Fig. Z.-Drawing indicating that the lateral and protrusive excursions are anterior to Centric position, while the occ~usal segment of the masticating cycle is distal to centric position (occlusal view). In the study of dental ])hysiology, the functional changes that take place in the dental organ as age advances are easily recognized. ...
Fischer's angle was defined as the difference between the sagittal condylar inclinations during protrusive and lateral excursions on the non-working side, by keeping the corresponding horizontal distance from the intercuspal position (ICP) equivalent at the incisal point. Analysis was performed at three different magnitudes of excursions, where ...
Protrusive excursion refers to the path of the mandible as it moves anteriorly between the CO and the edge to edge relationship of the anterior teeth (Figure 34.8). In this step, adjustment in protrusive excursions is done. The primary objectives of the dentist during this step are,
It involves moving study casts (on a semi-adjustable articulator) through the full range of lateral and protrusive excursions with a mound of un-set acrylic on the guide table, so that the tip of ...
The tradition of lateral or protrusive ` excursion' is invalid. It is emphasized that protrusive balance is frequently incompatible with natural and anterior tooth arrangements and that premature balancing contacts should be avoided at all times. INTRODUCTION THE problems associated with understanding the eccentric occlusions of the teeth arise ...
protrusive excursion: movement of the mandible to a position forward of the centric position.
The four types of occlusal interferences are (1) centric occlusal interferences, (2) working occlusal interferences, (3) nonworking occlusal interferences, and (4) protrusive occlusal interferences. The centric occlusal interference is an occlusal prematurity which causes the mandible to deflect forward and/or laterially from the optimum ...
In an evaluation of the jaw movement after treatment, a smooth and stable incisal path was demonstrated during maximal open-close movement, protrusive excursion, and lateral excursion (Figure 10A). In a chewing test using a hard gummy jelly after treatment, increases in the range of motion of both condyles and a stabilized pattern of movement ...
Moscow Metro. The Moscow Metro Tour is included in most guided tours' itineraries. Opened in 1935, under Stalin's regime, the metro was not only meant to solve transport problems, but also was hailed as "a people's palace". Every station you will see during your Moscow metro tour looks like a palace room. There are bright paintings ...
Moscow Metro private tours. 2-hour tour $87: 10 Must-See Moscow Metro stations with hotel pick-up and drop-off. 3-hour tour $137: 20 Must-See Moscow Metro stations with Russian lunch in beautifully-decorated Metro Diner + hotel pick-up and drop off. Metro pass is included in the price of both tours.
In 1938, it was granted town status. [citation needed]Administrative and municipal status. Within the framework of administrative divisions, it is incorporated as Elektrostal City Under Oblast Jurisdiction—an administrative unit with the status equal to that of the districts. As a municipal division, Elektrostal City Under Oblast Jurisdiction is incorporated as Elektrostal Urban Okrug.
The pontic occlusion made slight contact in the centric occlusion and no contact during lateral and protrusive excursions. After preparation, a full-arch working impression was made with polyvinylsiloxane impression material in a custom tray. The outline of the bridge framework was drawn on a working cast by a single technician.
Construction work will begin in the second quarter of this year. The planned completion date of the facility is the second quarter of 2022," Sergei Voskresensky noted. The construction of the wholesale distribution center will facilitate the promotion of Russian agricultural products to foreign markets. EastFruit.