

Is It Safe For Patients With Brain Tumors To Fly?
by Garni Barkhoudarian
Doctors address concerns about air travel safety for patients with brain tumors in this new study.
The global reach of medicine is becoming increasingly easier to achieve. Thanks to the ever-increasing availability of medical information available online as well as the capabilities for long distance tele-health consultations, patients have expanded options to undergo multidisciplinary treatment for their conditions with experts worldwide.
Information for International Patients
Traveling for neurosurgical care
The field of neurosurgery and brain tumor management is no exception. Patients often will seek second or third opinions at a high-volume brain tumor center of excellence and receive definitive treatment at these facilities effectively giving increased access to those living in cities without experienced teams treating such conditions. This is most relevant to patients in rural areas and those living in countries with limited resources. Hence, traveling for medical treatment (medical tourism) has demonstrated value for the patient opting to receive the best possible care for their condition, while showing financial savings when patients have fewer complications, shorter hospital stays and earlier return to work. This model has been adopted by large health systems and insurers with positive results for complex procedures like heart and transplant surgery.
Is it safe for brain tumor patients to travel by air?
A major question regarding the safety of air flight had, until recently, not been answered, despite the increasing volume of patients with large brain tumors traveling long distances for surgery. In particular, the air pressure changes that occur on high-altitude jet airplane flights (which can be equivalent to immediately ascending to an altitude of 8,000-10,000 feet) have been a concern for increasing brain swelling (edema) which could cause major symptoms during flight.

Overall, air flight was found to be safe for patients with brain tumors.
There was no correlation with brain tumor size or pre-operative symptoms. Of the 41 patients, ten (24.4%) reported new or worsened symptoms during airflight, although most of these symptoms were minor and resolved after landing. Only one patient developed a major symptom (seizure), which was also transient. If patients had no symptoms prior to their flight, none of the patients developed new symptoms during or afterwards.
Safety first
This publication is the largest study to date assessing the safety of air flight for patients with brain tumors. It is however important to note that this was a relatively small study in terms of sample size and although air flight overall was shown to be safe, one patient with a relatively large benign brain tumor did have an inflight seizure. The patient went on to have a successful surgery and is doing well now with no issues related to his seizure or surgery. This patient’s experience highlights that careful consideration by both doctor and patient are essential prior to allowing a patient to fly for their care at another center.
Specifically, for larger tumors, consideration should be given to preflight and inflight administration of steroids to reduce brain edema and anticonvulsants to reduce seizure risk. In some patients with very large brain tumors already causing cranial pressure, air flight may be considered unsafe and not recommended.
We hope that results from our study will be the impetus for larger studies to be performed to validate this data. Certainly, this study has implications for patient mobility with the goals of improving equal access to quality brain tumor treatment at established centers of excellence.
An everyday question is answered
Since its publication, the article has not only influenced the scientific community, but has also elicited a positive response from the patient community, as many have appreciated a research study that so directly impacts their lives.
Nevertheless, if patients have brain tumors and seek to travel by plane, they should have discussions with their neurosurgeon or neuro-oncologist to ensure individual safety.
Journal of Neuro-oncology, May 17, 2018. Safety of commercial airflight in patients with brain tumors: a case series. Michelle Phillips, MS, Marlon Saria, PhD, RN, Amy Eisenberg MSN, ARNP, CNRN, Daniel F. Kelly, MD & Garni Barkhoudarian, MD.
About the Author

Garni Barkhoudarian
Dr. Garni Barkhoudarian is an expert neurosurgeon and director of the Facial Pain and Adult Hydrocephalus Centers, and Co-director of the Pituitary Disorders Center at Pacific Neuroscience Institute. His philosophy for virtually all intracranial procedures is to apply the keyhole concept of minimizing disturbance to the brain and its supporting structures.
Last updated: December 13th, 2021
To give you the best possible experience, this site uses cookies and by continuing to use the site you agree that we can save them on your device.

- Brain Tumor

Is it safe to fly with a brain tumor?
my daughter has decided to go to mayo for a second opinion. I'm worried about her flying. Right now the tumor is growing very aggressively. Is it safe to fly with a tumor?
- Copy link to clipboard
- Report discussion
Interested in more discussions like this? Go to the Brain Tumor Support Group.
Good morning @Imp1 While I am not any type of medical professional, and I'd suggest your daughter run this by her physician, I can say my wife had a brain tumor and she traveled by air while she was able. We saw no ill effects from the air travel. The flights we took were of about a two hour duration.
Strength, courage, and peace!
- Report comment
@lmp1 Please let me know how things go! I will be praying for you and her
Jump to this post
@daniellemarie @IndianaScott Everything is set up for a 2nd opinion at mayo. Her appointment is Tuesday. I will update when we know something. I feel good about her going to mayo. Thank you for your support and prayers! God Bless!

Is it safe for patient with brain tumor to fly?

Hi @dimatahsin , and welcome to Connect. I did some further searching for answers and found this article from the Pacific Neuroscience Institute ( https://www.pacificneuroscienceinstitute.org/blog/brain-tumor/is-it-safe-for-patients-with-brain-tumors-to-fly/ ). In a study recently published in the Journal of Neuro-Oncology, “Safety of commercial airflight in patients with brain tumors: a case series,” (Phillips et.al. 2018), researchers reported the safety data for patients with brain tumors. Here is the full study https://link.springer.com/article/10.1007/s11060-018-2905-6
In short, the study found "Overall, airflight was found to be safe for patients with brain tumors. Nevertheless, if patients have brain tumors and seek to travel by plane, they should have discussions with their neurosurgeon or neuro-oncologist to ensure individual safety."
I'm also tagging @wkindel and @nancye3 who might appreciate this information and have some additional thoughts to add.
Dimatahsin, are you planning to fly for medical treatment? What type of brain tumor do you have? Or are you asking on behalf of a family member?
Hi collen .. thank you for your reply 🙏🏽 My father had diagnosed with brain tumor.. probably it’s a lymphoma and yes we decided to fly for medical treatment. Pray for him 😔
<p>I am in my 50's and a type 2 diabetic.For the past few years there have been autoimmune symptoms that remain undiagnosed. Then in May I began to have double vision. We finally have an appointment with Mayo Clinic next week. The diagnosis at this point is a tumor within the first of the cavernous sinus. It is causing problems with cranial nerves 5 and 6. The pain level today is pretty bad and I love in the middle of Momtana. I know that the vibration of the car will be rough but I worry about the pressure changes of flying. Any input would be appreciated.<br />Karen</p>
Hi @pejiota4jack , welcome to Connect. I glad to hear that you were able to get an appointment at Mayo Clinic. I can understand your apprehension about flying and cabin pressure if the tumor is causing problems with the cranial nerves and your pain level is high. I'm tagging fellow members, @kmart @mrector @lisakuehl @nancye3 @frit5 @ees1 @pegorr , who I believe may have traveled far for treatment and possibly flown. I hope they can share their experiences.
More specifically, I hope to hear from @jrt26 @julieannarcand and @ees1 , who have written about their experiences with cavernous sinus meningioma here: - Cavernous sinus meningioma https://connect.mayoclinic.org/discussion/cavernous-sinus-meningioma/
Jack, have you talked to your local doctor or the neurology department at Mayo to ask about travel and things they recommend to make flying comfortable?
Hi, While I didn't fly for my gamma knife and my cyberknife treatments, drove from Montana to Seattle,Washington, I have flown with head pain since. I find that if I put on my Bose noise cancelling, over the ear head phones it keeps the pressure down and the pain minimal. I hope this helps, but maybe someone else will have a better idea. Wishing you all the best. peg p.s. flying in October with 3 remaining tumors.
Thanks for the reply! My husband wants to drive so that we can take it slow.

Connect with thousands of patients and caregivers for support and answers.
- Hosted and moderated by Mayo Clinic.
- Safe and secure.
Already have an account? Sign In
Safety of commercial airflight in patients with brain tumors: a case series
Affiliations.
- 1 Pacific Neuroscience Institute, Brain Tumor Center & Pituitary Disorders Program, John Wayne Cancer Institute at Providence Saint John's Health Center, 2200 Santa Monica Blvd., Santa Monica, CA, 90404, USA.
- 2 Department of Translational Neurosciences and Neurotherapeutics, Pacific Neuroscience Institute, John Wayne Cancer Institute at Providence Saint John's Health Center, Santa Monica, CA, 90404, USA.
- 3 Pacific Neuroscience Institute, Brain Tumor Center & Pituitary Disorders Program, John Wayne Cancer Institute at Providence Saint John's Health Center, 2200 Santa Monica Blvd., Santa Monica, CA, 90404, USA. [email protected].
- PMID: 29774497
- DOI: 10.1007/s11060-018-2905-6
Introduction: Patients with intracranial masses are often advised to avoid airflight due to concerns of worsening neurological symptoms or deterioration. However, many patients often travel cross-country or internationally to tertiary care centers for definitive care. This study assesses the safety of commercial airflight for brain and skull base tumor patients without severe or progressive neurological deficits.
Methods: Patients that had traveled to our institution for surgery via commercial airflight from 2014 to 2017 were identified. An electronic survey was administered (RedCap) and flight duration, aircraft type, presenting symptoms and new or worsened peri-flight symptoms were queried. Severity was assessed using visual analogue scale (VAS). Significant change of symptoms was determined to be greater than 25%. Demographics and clinical history were obtained from electronic medical records. Providence Health System IRB: 16-168.
Results: Of 665 patients operated on for brain tumor, 63 (9.5%) traveled by airflight to our center for surgery and of these, 41 (65%) completed the study (mean age 48.5 ± 16.8 years, 63% female). Pathology included pituitary and other parasellar tumors (58%), meningiomas (22%), metastatic tumors (5%), gliomas (5%), pineal tumor (5%), cerebello-pontine tumor (5%). Average tumor volume was 11.4 cc and average maximal dimension was 2.7 cm. Ten (24.4%) patients developed worsened symptoms during airflight including: headaches 3/19 (15.8%), fatigue 3/14 (21.4%), dizziness 3/5 (60%) and ear pain 3/3 (100%), as well as one patient who had new onset seizures inflight. Seven patients (70%) sustained worsened symptoms after airflight. There were no permanent neurological deficits related to airflight. There was no correlation with tumor size, volume, location or flight duration with development of neurological symptoms. There was an inverse correlation between peri-flight corticosteroid usage and symptom exacerbation (p = 0.048). No patient with completely asymptomatic tumors developed new symptoms during flight.
Conclusions: Most patients with brain and skull base tumors can travel safely via commercial airflight with acceptable symptom exacerbation. However, consideration should be given to administering corticosteroids and possibly anticonvulsants to patients who are symptomatic and/or have relatively large tumors with mass effect and peritumoral edema.
Keywords: Air travel; Cerebral edema; Corticosteroid administration; Intracranial pressure.
Publication types
- Case Reports
- Aged, 80 and over
- Brain Neoplasms* / epidemiology
- Brain Neoplasms* / physiopathology
- Brain Neoplasms* / surgery
- Middle Aged
- Patient Safety*
- Prospective Studies
- Retrospective Studies
- Transportation of Patients
- Young Adult
Can You Fly With a Brain Tumor?

A brain tumor is an abnormal growth of cells that can occur in any part of the brain. Both malignant and benign tumors increase intracranial pressure, limit abilities and put lives at risk. These serious tumors can happen unexpectedly, causing concern when individuals live far away from treatment centers or are traveling abroad. Learn more about the risks individuals face when flying and how an air ambulance can help.
Can You Fly With a Benign Brain Tumor?
Flying is possible for those with a benign or a malignant brain tumor, but there are many risks to consider. As a plane ascends, air pressure decreases within the cabin. With less air pressure, oxygen within the cells of a body can expand, potentially causing brain tumors and cerebral fluid to also increase. Depending on the size and location of the tumor, individuals may experience seizures, increased intracranial pressure or other life-threatening effects.
It is best to get a doctor’s opinion before planning a flight. They can assess your condition, symptom severity, treatment progress and other aspects of your health to determine if it is safe for you to travel.
Air Travel Restrictions for Individuals With a Brain Tumor
If you are taking a commercial flight, you will need to check what items are allowed on the aircraft. Individuals with a brain tumor may need to inform the airline about their condition and the types of medication or equipment they need to bring on the flight. Some airliners may even require a medical certificate for certain items.
For individuals who have recently undergone surgery for their brain tumor, it is best to wait before flying. Air can become trapped in the cranial cavity during an operation, which could then expand at higher altitudes.
Best Options for Flying When You Have a Brain Tumor
Due to the possible negative effects of air pressure changes, flying alone on a commercial flight is not recommended when you have a brain tumor or are recovering from neurosurgery. These aircraft have minimal medical equipment and personnel to help in an emergency. Safer flying options include air ambulances and medical escorts.
Air Ambulance
Treatment for a brain tumor can take weeks to months, so if you discover one while traveling, you’ll need to find a safe and quick way to fly home for continued care. An air ambulance is one of your best options since it can accommodate complex traveling requirements. Air ambulances can control the cabin air pressure to ensure it remains at a steady and safe level during the flight, helping to prevent the expansion of brain tumors while traveling.
These aircraft are equipped with the latest medical equipment and staffed with medical professionals who can attend to you throughout your flight. Air ambulances also have the flexibility to tailor every part of the flight to your unique health situation. Individuals are often transported lying on a stretcher bed for greater comfort and ease .
Medical Escort
If you are recovering from neurosurgery or have received the go-ahead from your doctor to travel with your brain tumor, you might find comfort and security in flying with a medical escort. While you may be safe to travel, you can enjoy greater peace of mind knowing a medical escort is there to assist you in case of a medical emergency.
Medical escorts will accompany you throughout every step of your flight to ensure your safety. These professionals are highly trained to provide expert medical care while in the air.
What You Need to Know About Insurance, Traveling and Brain Tumors
Insurance providers have different coverage policies when it comes to medical transport. Two reasons an insurance company may cover a flight include:
- It is medically necessary: Many insurers will cover flights if they deem them medically necessary. This means an individual can only receive life-saving operations and care in their home country or a distant location, requiring a flight for speed and efficiency.
- It is medically reasonable: Some insurers may cover flight expenses for medically reasonable flights. These situations are for individuals who could receive care locally but would enjoy better health outcomes if transported to their home country.
Travel medical insurance may also help cover medical transport costs when traveling for brain tumor treatment. Thoroughly check your policy to determine what is covered.
Let REVA Transform Your Medical Transport Experience
Our mission at REVA is to enhance our clients’ lives with quality care and safe transport across the country or overseas. Your comfort, health and security are our priorities, so you can trust us to deliver the services you need to enjoy peace of mind while traveling.
We offer many benefits to our clients, including:
- Highly qualified teams: We hold our medical, ground and flight crews to the highest standards to ensure you have an enjoyable and smooth flight. Each team member undergoes thorough training so that they can provide a safe travel experience.
- 24/7 availability: REVA is always available to schedule and execute flights all around the world. Wherever you are and whenever you need us, we’ll be there to help.
- Dedicated aircraft: Our fleet of air ambulances is configured with all the critical care equipment our medical teams need to benefit our clients. In addition to our dedicated air ambulances, we have several partnerships to increase our worldwide readiness and capabilities.
- Insurance assistance: We work with multiple insurance payors to help our clients find coverage and financial assistance. Our team will manage the insurance process so that you can fly home and feel better.
- Multi-lingual communication: We prioritize communication and ensure we update our clients and their families on every aspect of the client’s health and flight. Our team speaks multiple languages to provide consistent contact for our clients.
Contact Us Today for a Quote
Our professional medical, flight and ground crews are ready to help when you need a secure, comfortable and efficient medical flight. Contact us to learn more about our capabilities, or request a quote to see how we can assist with your specific transportation needs.
Having a brain tumour diagnosis can impact a number of aspects of life, including travelling and going on holiday.
On this page you will find information about the support available to help you with travel options for day to day life and for hospital appointments, and information about travel insurance for when you go on holiday.
Travelling to appointments at the hospital

If you have had to surrender your driving licence because of your brain tumour diagnosis, this can often mean having to rely on somebody else taking you to the hospital or use public transport or taxis.
If these are not viable options, or the cost of travelling becomes unaffordable for you, there may be options available to you that can help with this.
Find out about NHS services to help with travelling to hospital
Hospital car parking charges
Hospital car parking policies can vary across the UK, so it is best to double check the policy of the hospital your will be visiting in advance.
In England , many hospitals offer free parking for people with cancer, or a discount. This isn’t always well advertised, and in some hospitals it may only be in a certain area, so try and find this information out before you travel.
In Scotland, hospital parking is free at all hospitals apart from Glasgow Royal Infirmary, the Royal Infirmary of Edinburgh and Ninewells Hospital in Dundee.
In Wales , hospital parking is free for everyone.
In Northern Ireland , hospital parking is free at all hospitals if you are having chemotherapy or radiotherapy.
Driving is a topic that is frequently spoken about among our community. When you are diagnosed with a brain tumour of any type, and you hold a valid driving licence, you must inform the DVLA of this. Once you let them know, they will then assess whether you have to surrender your driving licence. This decision is based on many different things, including the tumour type and your treatment pathway.
Our ‘Driving’ Know How goes into more detail about the process of contacting the DVLA and how long you may have to surrender your licence for.

We know that the prospect of having to surrender your driving licence is a big challenge. It can mean a loss of independence, and the uncertainty of when you may be able to resume driving can cause feelings of anxiety. Below, you will find some information on some alternative travel options while you are not able to drive.
Download ‘Driving’ Know How
Travel assistance
If you are struggling with symptoms caused by a brain tumour, you may be entitled to help with some aspects of travel and getting around. In some cases, this may help to make day-to-day living a little easier.
While a brain tumour diagnosis doesn’t give you an automatic entitlement to any of the schemes outlined here, it is always worth looking into your eligibility according to your symptom burden. Most of the items listed below require you to prove eligibility for certain disability benefits.
You can link your Disabled Person’s Railcard to your Oyster card to get a third off Oyster pay-as-you-go single fares and daily caps on National Rail, London Underground and Docklands Light Railway services. Register at any London Underground, Overground or National Rail station ticket office that issues Oyster cards.
If you live in a London borough, you can apply for a Disabled Person’s Freedom Pass to gain free travel across London and free bus journeys nationally. Some boroughs offer passes at their discretion to people who do not meet the eligibility criteria.
Contact your local county council to apply for a free bus pass.
what3words is a free app that helps you to easily and accurately identify your location to the emergency services. This could potentially be very useful if you have seizures and going out alone is a worry for you. Search ‘what3words’ in your phone’s app store.
Displaying a Blue Badge allows you to park in disabled parking bays, often meaning that you can park closer to your destination.
You may be eligible for a Blue Badge if you cannot walk or have difficulty walking, and can evidence this in your application.
Additionally, the criteria have recently been expanded so that people with ‘invisible’ disabilities are now potentially eligible for the scheme. This means that in addition to physical disabilities, non-physical disabilities, including cognitive impairment, psychological effects, such as feeling overwhelmed by busy or loud environments, and cognitive fatigue, are now taken into account.
Check your eligibility and apply here https://www.gov.uk/apply-blue-badge (England, Wales & Scotland) or here https://www.nidirect.gov.uk/information-and-services/motoring-and-transport/blue-badge-scheme (Northern Ireland).
If treatment can give you an unpredictable stomach, or if you suffer from sickness, it can make the thought of going out anywhere new really challenging. A RADAR key offers you access to the 10,000 locked disabled toilets in the UK, making going out in public far less worrying.
More information about the RADAR National Key Scheme and accessible toilets is available here: https://www.which.co.uk/later-life-care/home-care/out-and-about/radar-keys-and-locked-toilets-apsxd1p6br8k?gclid=CjwKCAiAwrf-BRA9EiwAUWwKXoro-oWYtTw0O8IDbvFYqsWt973kql_cj5v-YWXtjf7HRSAIkYPsQhoC4EEQAvD_BwE
Travel insurance
When looking for some time away, travel insurance is something that we know can be a challenge when you have a brain tumour. The brain tumour hub has a list of travel insurance companies that will provide cover for people with pre-existing medical conditions.
Find travel insurance providers
Practical travel advice
If you are travelling abroad following a brain tumour diagnosis, you may find that you have more things to think about to help you prepare for your holiday.
Find practical tips when travelling abroad
Find out more about specialist travel insurance, as well as supported holiday resorts and respite breaks on the brain tumour hub .
Did this information make you feel more resourced, more confident or more in control?
Last year your support helped:
2,339 people contacted our team of support specialists for help
825 new people accessed our support
404 people receive a Brain Box
We hosted 134 support events
110,928 people access our online information and support
3200 people in our online community to help each other to feel less alone.

- Improving access to brain tumour clinical trials in partnership with myTomorrows 3rd April 2024

- News coverage of immunotherapy treatment for glioblastoma 18th March 2024

Introduction
The Brain Tumour Data Dashboard lets you explore up -to-date, population level data about the brain tumours diagnosed in England between 2013 and 2015. Using the drop down menus on the left you can select different groups of patients to view in the charts below. In these charts the number of patients for every 100 diagnoses is displayed as images of people. Patients have been grouped by date of diagnosis, type of tumour, age, gender, and region in England.
For each group of patients you can explore the different routes to diagnosis, the proportion of those who received chemotherapy or radiotherapy, as well as the survival of the patients within each group. For more information about what these metrics mean please see the glossary.
- Select the year of diagnosis using the drop down menu.
- Tumour group
- Age at diagnosis
- Region of England
- Gender of patient
- To view a second chart to compare different groups of patients, click the ‘compare’ button.The second chart will appear below the first chart.
*Note that the tool is best used on a laptop or tablet rather than a mobile phone*
Unavailable data
Some of the data in these charts is not available.There are two main reasons for this:
- How the data has been grouped
If you cannot select a patient group from the drop down menus, the data is unavailable because of how the data has been organised.
Public Health England has grouped the data like a branching tree. The bottom of the tree contains all the patients with brain tumours, and then each branch divides the data by a certain characteristics, like age, or location of tumour. But the data is divided in an order, starting with location of the tumour (endocrine or brain), then by age, region, and gender. Age is at the start because it makes a bigger difference to survival rates and treatment rates than gender or region. Sometimes, after the data has been split by type of tumour and age, there is not enough data to be split again. This is because to protect patient confidentiality groups cannot contain less than 100 patients. Because some groups cannot be split further, you cannot create ‘totals’ for everyone by region or gender. For example, you cannot see results for all ages by region, or all brain tumours by gender. If these totals were calculated and released, it might be possible to identify patients, which is why Public Health England cannot release this data.
- Statistical reasons and data availability
If you can select a patient group from the chart menus, but the chart does not display, the data is unavailable for one of several reasons:
- Data is not yet available for the selected year from Public Health England.
- Data is not available because the data quality is too poor to release this statistic.
- Data is not available as the statistic is not appropriate for this group.
- Data is not available because the standard error of the estimate was greater than 20% and so the estimate has been supressed.
Up to date brain tumour data
Brain tumour data may influence the decisions you make about your care. data also helps you understand the bigger picture, or landscape, in which you find yourself..
Brain tumour data and statistics influence the focus, and work of organisations like brainstrust. The information helps us to understand the scale and impact of the problems we are setting out to solve.
This tool helps you understand the landscape in which you find yourself having been diagnosed with a brain tumour. This landscape can be particularly tricky to navigate as there are many different types of brain tumour, all of which have a different impact.
The information you see represents the most up-to-date, official, population level brain tumour data available for England. Over time we will be adding to the brain tumour data available and publishing reports, with recommendations, as a result of what we learn from this data.
The data behind this content has come from Public Health England’s National Cancer Registration and Analysis Service (NCRAS) and is a direct result of the ‘Get Data Out’ project.
This project provides anonymised population level brain tumour data for public use in the form of standard output tables, accessible here: http://cancerdata.nhs.uk/standardoutput
The number or rate (per head of population) of new cases of a disease diagnosed in a given population during a specified time period (usually a calendar year). The crude rate is the total number of cases divided by the mid-year population, usually expressed per 100,000 population.
Malignant tumours which grow by invasion into surrounding tissues and have the ability to metastasise to distant sites
The number or rate (per head of population) of deaths in a given population during a specified time period (usually a calendar year). The crude rate is the total number of deaths divided by the mid-year population, usually expressed per 100,000 population.
Non-malignant
Not cancerous . Non-malignant tumours may grow larger but do not spread to other parts of the body.
The length of time from the date of diagnosis for a disease, such as cancer, that patients diagnosed with the disease are still alive. In a clinical trial, measuring the survival is one way to see how well a new treatment works. Also called ‘overall survival’ or ‘OS’.
Routes to Diagnosis
Under the ‘Routes to Diagnosis’ tab in the Brain Tumour Data Dashboard, you can explore the ways patients have been diagnosed with brain tumours. There are many ways, or routes, for cancers to be diagnosed in the NHS. A ‘route to diagnosis’ is the series of events between a patient and the healthcare system that leads to a diagnosis of cancer. The routes include:
- Two Week Wait
Patients are urgently referred by their GP for suspected cancer via the Two Week Wait system and are seen by a specialist within 2 weeks where they are diagnosed.
- GP referral
Diagnosis via a GP referral includes routine and urgent referrals where the patient was not referred under the Two Week Wait system.
- Emergency Presentation
Cancers can be diagnosed via emergency situations such as via A&E, emergency GP referral, emergency transfer or emergency admission.
Outpatient cancer diagnoses include diagnoses via an elective route which started with an outpatient appointment that is either a self-referral or consultant to consultant referral. (It does not include those under the Two Week Wait referral system).
- Inpatient elective
Diagnosis via an inpatient elective route is where diagnosis occurs after the patient has been admitted into secondary care from a waiting list, or where the admission is booked or planned.
- Death Certificate Only
Diagnoses made by Death Certificate Only are made where there is no more information about the cancer diagnosis other than the cancer related death notifications. The date of diagnosis is the same as that of the date of death.
For some patients with a cancer diagnosis, there is no relevant data available to understand the route to diagnosis.
More information
If any of the statistical terms in this section of the brainstrust website are hard to understand, we recommend looking them up here:
Cancer Research UK’s Cancer Statistics Explained
http://www.cancerresearchuk.org/health-professional/cancer-statistics/cancer-stats-explained/statistics-terminology-explained#heading-Seven
If you are looking for help understanding terms relating specifically to brain tumours, and treatment, then the brainstrust glossary is available here:
https://www.brainstrust.org.uk/advice-glossary.php
Skip to Content
- Conquer Cancer
- ASCO Journals
- f Cancer.net on Facebook
- t Cancer.net on Twitter
- q Cancer.net on YouTube
- g Cancer.net on Google
- Types of Cancer
- Navigating Cancer Care
- Managing Emotions
- Physical, Emotional, and Social Effects of Cancer
- Talking With Family and Friends
- Caregiving Basics
- Tips for Being a Successful Caregiver
- Caregivers Taking Care of Themselves
- Sharing Responsibilities
- Caregiving at Home
- Caregiving at the Hospital
- Hiring Home Care Services
- Long-Distance Caregiving
- Young Adults Caring for a Parent With Cancer
- Caregiving for Adults Age 65 and Older
- Caring for a Person with a Brain Tumor or Metastatic Brain Cancer
- Finding Social Support and Information
- Cancer from the Oncologist's Perspective
- Research and Advocacy
- Survivorship
People with a tumor in their brain often have unique physical, practical, and emotional needs during and after their medical treatment. In addition to physical changes, patients can experience changes in mood, personality, and thinking. As a result, caregiving at home can be challenging. Caregiving often includes a variety of responsibilities that may feel overwhelming. Planning for your role as a caregiver will help you take good care of your loved one and support your own health and wellbeing.
What is a brain tumor? What is metastatic brain cancer?
A primary brain tumor is a tumor that starts in the brain. A secondary brain tumor is a cancerous tumor that started elsewhere in the body and then spreads to the brain. When cancer spreads to another part of the body from where it began, doctors call it metastatic cancer . An area of cancer spread is called a "metastasis."
Nearly any type of cancer can spread to the brain, but certain cancers are more likely to spread to the brain. These include breast cancer, kidney cancer, lung cancer, and melanoma.
What are the symptoms of a brain tumor or brain metastasis?
The symptoms of a tumor in the brain vary from person to person. They depend on the tumor’s size, how fast it is growing, and where in the brain the tumor forms.
Possible symptoms that may occur from a tumor in the brain are:
Physical symptoms. Physical problems from a tumor in the brain include:
Muscle weakness
Vision problems
Bowel and bladder problems
Cognitive symptoms. A tumor in the brain can change how a person's brain processes information. Cognitive problems can include:
Personality changes
Impaired judgment
Memory loss
Emotional symptoms. Brain tumors and cancer that has spread to the brain can also cause emotional changes. These include:
Other emotional changes
It is important for you to monitor these and other symptoms. The health care team will help you learn what to watch for and track these symptoms. And, be sure to talk with the team regularly about what the patient is experiencing, so they can help manage and relieve symptoms and side effects.
How can symptoms of a tumor in the brain be treated?
Relieving a person’s symptoms and treatment side effects is an important part of your loved one's medical care. This type of care is called palliative or supportive care . This type of care can continue even when active treatment to cure or slow down the cancer stops. Be sure to talk with your loved one’s health care team about new symptoms or changes to existing symptoms. There are many options to relieve different symptoms of a primary brain tumor or brain metastasis.
Medications, such as corticosteroids that lower swelling in the brain, anti-seizure drugs, and pain medicine
Assistive devices, such as wheelchairs, canes, and walkers
Emotional support, such as counseling
Rehabilitation , such as problem-solving therapy, speech and language therapy, and physical therapy
Eating nutritious food
Complementary therapies , such as breathing exercises, massage, meditation, and acupuncture
Also, many people with a brain metastasis will have radiation therapy . There are two types of radiation therapy that are used for brain metastases:
Whole brain radiation therapy (WBRT). This type of radiation therapy targets the entire brain. Common side effects include moderate to severe fatigue , an increase in short-term memory loss , and hair loss .
Stereotactic radiosurgery. This type of radiation therapy targets only the part of the brain that has the tumor. It may be completed in 1 session. Because it does not affect the whole brain, there may be fewer side effects. Common side effects include fatigue , swelling at the treatment site, and nausea and vomiting .
Learn more about the side effects of radiation therapy .
Managing caregiver responsibilities
Learn as much as you can about your loved one’s diagnosis, treatment options, and chance of recovery. It is also important to ask the health care team about the medical, financial, and coping resources available to you and your loved one. As the disease and its treatment changes, so will your role. Here are some tips that may help:
Get to know your loved one’s health care team. Request a meeting with the team. Ask for clear, accurate information about the illness and treatment. Also, learn what each provider on the team does .
Ask family and friends for help. Figure out what tasks you need to do and organize a network of people to help you. Some people create an email list, text chain, or web page. You can also use one of the many websites available to make this process easier. Learn more about sharing responsibilities .
Learn how to provide day-to-day and medical care. Ask your loved one’s health care team for details on the best ways to provide daily living care. This may include bathing, dressing, and giving meals. Also ask how to provide medical care that may be needed, such as giving injections or wound care.
Consider professional caregivers. If possible, consider medical professionals and non-medical home care aids. Medical professionals can help with medical care that you are not comfortable doing. Home care aids can help with everyday caregiving tasks, such as grooming and cooking. Your loved one’s health insurance may pay for these services. Learn more about other caregiving options and how to find this type of caregiver .
Explore community resources. Many communities have available resources for caregivers. These include case management, legal aid, financial assistance, and counseling. Ask your loved one’s health care team for local referrals.
Stay organized. Keep track of important medical information in a way that makes sense to you and is easily available when you need it. You can use the free Cancer.Net mobile app or keep a paper record of this information that you bring with you to appointments. In your notes you should:
Organize medical information
Track medical bills and health insurance claims
Track treatments
Manage medications
Monitor side effects
Plan doctor’s appointments
Learn more about how to manage common caregiving tasks and providing care at home .
Planning ahead for people with a brain tumor or brain metastases
A brain tumor or brain metastases may affect a person’s ability to communicate or make decisions. Talk with your loved one now about their treatment goals and priorities. These could range from surviving as long as possible to maintaining a specific quality of life by avoiding certain side effects. Sometimes, that means stopping treatment. This may be hard for your family to discuss. If so, ask a social worker, counselor, or another member of your loved one’s health care team to lead the conversation.
Topics to discuss include:
An advance directive. An advance directive is a legal document. It states who a person wants to speak for them if they are too sick to make decisions. It also provides information about the types of care a person does and does not want. Give a copy of the document to your loved one’s health care team. Also, keep a copy at home.
Hospice care. People expected to live less than 6 months may want to consider a type of palliative care called hospice care . Hospice care aims to provide the best possible quality of life for people who are near the end of life. Your loved one should think ahead about where they would be most comfortable if the cancer progresses. This could be at home, in a hospice center, or another health care location. Nursing care and special equipment can make staying at home an option for many families.
Caring for yourself as a caregiver
It can be hard to balance your caregiving tasks with the responsibilities of your own life. Caregivers of people with brain tumor or brain metastases are likely to have emotional challenges. For example, you may experience anxiety or depression. It is also likely for a caregiver to have physical symptoms like exhaustion.
Personality changes common to brain tumors can be distressing. You may feel sad about watching the person you love act in a different way. You may also feel guilty about experiencing anger, frustration, or other emotions. It is important to remember that there is no right way to feel as a caregiver. It is okay to take care of yourself. In fact, your mental and physical health is important to the well-being of your loved one.
Ask an oncology social worker or your loved one’s health care team about ways to connect with other caregivers, arrange respite care, join online or local support groups , counseling, and other ways to manage stress.
Caregiving during the final days
As a person nears the end of their life, it is difficult to know what to expect. Knowing how to provide care in the final days can help. When you or the patient's doctor or nurse feel that time is approaching, talk with your loved one’s health care team about how to:
Recognize the signs of approaching death
Provide comfort
Get urgent help from medical staff when needed
Handle practical matters after death
Your loved one’s health care team can also provide information on coping with grief and loss . This information can help you prepare for the loss of your loved one. It can also help you cope with changes you may experience when your caregiving journey ends .
Questions to ask the health care team
Consider asking your loved one's health care team the following questions.
Where is the tumor located in the brain? What is the stage of the disease?
What symptoms, side effects, and changes are possible due to this tumor?
Who can I talk with when side effects begin or worsen? How soon?
What can be done to manage or relieve each side effect?
Are there side effects that could require emergency medical care?
Is it time to talk with my loved one about a plan for their future care, such as creating an advanced directive? Who can help me with that discussion?
Who can I talk with if I need emotional support or practical help in my role as a caregiver? What resources are available to me?
Related Resources
ASCO Answers Fact Sheet: When Cancer Spreads to the Brain (PDF)
How I Went From Caregiver to Patient Advocate
More Information
American Brain Tumor Association
University of California, San Francisco: Orientation to Caregiving: A Handbook for Family Caregivers of Patients with Brain Tumors (PDF)
National Brain Tumor Society: Grief Support
National Brain Tumor Society: Patient & Caregiver Toolkit
Coping With Cancer
More in this section.
Timely. Trusted. Compassionate.
Comprehensive information for people with cancer, families, and caregivers, from the American Society of Clinical Oncology (ASCO), the voice of the world's oncology professionals.
Find a Cancer Doctor
Have you been diagnosed with a brain tumour? Order your free information pack.
- Log into BRIAN
- Step by Step interactive guide
- Support and Info Line
- Children and Families Service
- Young Adult Service
- Online brain tumour support groups
- Benefits and money clinic
- Counselling
- Support for professionals
- Changes in vision
- Abnormal head position
- Abnormal growth
- Reduced consciousness
- Nausea and vomiting
- Balance problems
- Behaviour changes
- Delayed puberty
- Excessive thirst
- Nausea & dizziness
- Loss of taste and smell
- Brain tumour symptoms by location
- Talking to your doctor
- Neurological examination
- Diagnostic scans
- Diagnostic scans for children
- How brain tumours are graded
- Brain tumour biology
- What to do after a brain tumour diagnosis
- Treatment for brain tumours (children)
- Brain tumour treatments for adults
- Complementary therapies
- Emerging treatments
Clinical trials
- If treatment doesn’t work
- Medulloblastoma
- Diffuse midline glioma (DIPG)
- Craniopharyngioma
- Embryonal tumours
- Brainstem glioma
- Pineoblastoma
- Choroid plexus carcinoma
- Germ cell tumour
- Glioblastoma
- Astrocytoma
- Acoustic neuroma
- Pituitary adenoma
- Oligodendroglioma
- Haemangioblastoma
- How the NHS works
- Your health team (MDT)
- Your child’s health team (MDT)
- How to get a second opinion
- Questions to ask
- Differences in care
- Step by Step: Your interactive guide to life with a brain tumour
- What to do if things go wrong
- How to choose a centre
- Rehabilitation
- Mental health
- Personality changes
- Memory difficulties
- Communication difficulties
- Fatigue or tiredness
- Cognition difficulties
- Seizures (epilepsy)
- Learning difficulties in children
- Sight problems and brain tumours
- End of Life
- Bereavement resources
- Be part of BRIAN
- Travelling by public transport
- Travel insurance
- Travelling abroad
- Employment and brain tumours
- Managing your money
- Support for couples
- Caring for somebody
- Supporting friends and family
- Supporting children
- Feeling alone
- How to Donate
- Why choose us
- Leave a gift in your Will
- Give in memory
- Donate through your salary
- Donate while you shop
- Trusts and Foundations
- Co-fund with us
- Become a Corporate Partner
- Other ways to give
- Play our Weekly Lottery
- Fundraising ideas
- Get your school involved
- Fundraise at work
- Make your money grow
- Meet your community team
- Tell us your plans
- Fundraising resources
- Our Supporter Groups
- Take part in an event
- Volunteering
- Share your story
- Campaigning for change
- Campaign with us
- Policy Library
- Future Leaders
- Quest for Cures: Collaborative Discovery Teams
- Documents for Research Funding Applications
- Assessment criteria
- Manage your grant
- Who We Fund
- Working with us
- Patient and public involvement
- Events for researchers
- Losing Myself
- Losing My Place: The Reality of Childhood with a Brain Tumour
- Finding Myself in Your Hands
- The Grey Matters
- Research Impact Report
- The Price You Pay
- Annual report and accounts
- Our accreditations
- Our Partners
- Beyond Brain Tumours
- Our progress
- How we choose what to fund
- What we’re funding
- Our partnerships
- Barriers to research
- Our history
- Senior Leadership Team
- Our Trustees
- Our Advisors
- Our high profile supporters
- Young Ambassadors
- Join the team
Going home after brain tumour surgery
Going home after neurosurgery can feel quite overwhelming and you may find you have more questions than answers. Here you’ll find some information to help you begin your recovery.

Short summary
You might be feeling a little nervous or unsure about going home after neurosurgery. We completely understand. So, we’ve put together some information that might help you with what to expect.
Here we’ll discuss the steps that come after you go home. We’ll also point out some common symptoms and some symptoms to watch out for. We’ve also added a list of frequently asked questions.
On this page:
- Next steps after brain tumour surgery
Common symptoms after neurosurgery
Symptoms to watch out for, frequently asked questions, share this with someone, get support.
If you have any questions or just need someone to talk to, please get in touch with our friendly and knowledgeable Support Team.
Get your free Information Pack
Our Brain Tumour Information Pack can help you better understand your diagnosis and feel confident talking to your medical team.
Get the BRIAN app
BRIAN is our trusted online app where you can track your experience, compare it with others who’ve been there and get the knowledge you need to make informed decisions.
We understand that this can be a difficult time and you may want to talk about how you’re feeling after surgery.
Please remember that your healthcare team are there to help and are always happy for you to contact them for advice and support. Any question is fine to ask – so don’t be afraid to voice any worries or concerns you have.
The next steps after brain tumour surgery
Holistic needs assessment (hna).
A Holistic Needs Assessment (HNA) is a chance for you and your healthcare team to look at your needs and concerns about the support you might need following surgery. Together, you’ll work out how best to meet these needs and develop a care plan.
You may have already had an assessment before your hospital stay, but you can ask for one at any time if you’re worried about how you’ll cope when you’re discharged. You should speak to your CNS (Clinical Nurse Specialist) or key worker about this.
The HNA assessment doesn’t just look at how you’re recovering physically, it takes into account your emotional, practical, financial and spiritual needs too.
After surgery, your CNS team should routinely offer appointments to update your assessment to better meet your needs. This is a good opportunity to talk about how you’re feeling and any symptoms you may be experiencing following surgery.
Post-surgery therapies
You may have seen an occupational therapist (OT), physiotherapist (physio) or speech and language therapist (SLT) during your admission to hospital. They are healthcare professionals concerned with helping you to be as independent as possible with everyday activities, such as:
- managing stairs
As well as giving you advice, the therapists may arrange for you to have equipment, such as walking aids, to assist your recovery.
If you saw a therapist during your stay, they’ll have discussed with you any ongoing referrals or recommended treatment. If you didn’t see a therapist during your inpatient stay, you can discuss any concerns with your CNS (Clinical Nurse Specialist) or GP, who’ll be able to refer you to your local area teams.
Long-term support
If you find you’re having some lasting symptoms or worries following surgery, contact your CNS team, who’ll be happy to discuss this in detail – either in clinic or over the phone.
Many patients find this consultation very useful, as it provides time for you to talk about the things that are impacting your overall recovery.
This can be a positive step forward in your recovery process and can take place at any point after your operation.
Waiting for your biopsy results
How long it takes to receive the biopsy results confirming your tumour type will vary between hospitals. Often, they won’t be available before you go home.
If you haven’t received them before you go home, the team will be in touch to arrange a time for you to go to the clinic and discuss your results. This appointment is usually arranged by your Clinical Nurse Specialist (CNS) or your consultant’s secretary.
If you’re worried about having not received your results you should speak to your healthcare team about when you’re likely to get them.
Additional treatment following surgery
In some cases following surgery, it’ll be necessary to have additional treatment. This could be radiotherapy, chemotherapy or a combination of both. Your treatment options will be discussed with you.
If such treatment is recommended, you’ll be given an appointment with an oncologist once they have all the results about the tumour you’ve been diagnosed with.
Your GP will receive a treatment summary when you’re discharged from hospital. This gives details of your surgery, progress to date and any follow-up plans.
They’ll also receive a medications summary that details any medications that have been started or changed during your hospital stay.
Clinical trials are experiments into new ways of managing a condition. This might include investigating a new treatment, a new way of giving an existing treatment, or a new approach to diagnosing illness or assessing an outcome after treatment.
If this is something you might be interested in, ask a member of your healthcare team about current research and clinical trials. You can find more information on our clinical trials page .
Please be aware that many people can’t take part in a clinical trial. This can be for various reasons, such as lack of a suitable trial in your area or for your tumour, or your not meeting the strict eligibility requirements. Also the standard treatment may be most appropriate for you.
Back to top
Helping you recover from surgery
If you would like to know more about what to expect when going home after neurosurgery, please enter your details here and we’ll email you useful information.
No two people will feel exactly the same after surgery. Some people may recover very quickly, while others may take longer – this is completely normal.
Most people will experience some of the following symptoms but they should usually settle down over time:
Tenderness and numbness around the wound area
These feelings should begin to get better each day.
A mild headache
This should be relieved effectively with simple painkillers such as paracetamol and should improve a little each day. If not, contact your healthcare team or GP.
Swelling and bruising
This may be seen around the eyes and face. This can look alarming, but isn’t a cause for concern. It will gradually fade in the days or weeks ahead.
Tiredness and fatigue
Tiredness is very common following any brain surgery and regaining good energy levels can take some time. You can find more information about managing fatigue on our coping with fatigue page .
Noises or whooshing sensations inside your head
During your recovery time, you may notice some unusual sensations in your head as things are settling down – these are often described as crackles, pops, whooshes or drips.
Additionally, if you’ve had surgery near your ear, you may experience a dull earache.
If you find that these symptoms continues in the months ahead, you should contact your Clinical Nurse Specialist (CNS) for further advice.

Join us online
Our online support communities are a safe and secure space to connect with other people affected by a brain tumour and share your experiences.
Once you’re home you should keep an eye out for signs that you may need medical attention.
If you experience any of the following symptoms listed, you should contact your healthcare team straight away.
- Nausea or vomiting.
- A severe or worsening headache.
- Limb weakness.
- New, worsening, different or more frequent seizures (epilepsy).
- Aphasia ( difficulty understanding and producing language ).
- Your wound becoming red, sore or leaking any fluid or pus.
If it’s leaking clear fluid or pus, you’ll need to ring the hospital immediately, so that your healthcare team can assess it more fully.
- A soft fluid-like swelling behind or close to the scar.
This is brain fluid collecting under the skin. It’s called a pseudomeningocele. It will usually settle on its own, but ring your healthcare team for advice.
When will the stitches (sutures) or clips be taken out?
Usually stitches or clubs will be removed seven to ten days after surgery. The ward staff will tell you the date your stitches or clips are due to be removed and who will be performing this.
Usually, this will usually be done by district nurses who visit you at your home. Or you can go to your local treatment centre, depending on the services available in your area.
If you’ve had previous surgery or radiotherapy, the stitches may be left in a little longer. This will be discussed with you before you go home.
If you have dissolvable stitches, these are usually inserted inside the scalp, so you’re unlikely to be aware of them. Occasionally they will be inserted into the scalp. They usually dissolve after 2-3 weeks. Try to avoid touching the suture line (line of stitches).
Do I need to keep taking my anti-seizure medication after my operation?
Yes – this is very important. Anti-seizure medication should only be stopped on the advice of your medical team.
Even if you haven’t had any further seizures.
Some patients need long-term, anti-seizure medication; others for just a few months following surgery.
Do I need to keep taking my steroids after I go home?
Yes. Don’t stop taking steroids suddenly.
It’s important that you keep taking your prescribed dose of steroids (usually dexamethasone) when you leave hospital, as well as continuing to take stomach-protecting tablets.
You’ll be given specific instructions to either:
- reduce the dose over a set time until you’re no longer taking any steroids, or
- reduce to a specified dose of dexamethasone tablets until your clinic appointment.
The discharge team will explain all your medications, i.e. when, how often and how long to take them for. If you have any trouble taking them or experience severe side-effects, contact your healthcare team for advice.
While in hospital my blood sugar levels were checked every day. Will this continue?
Blood sugar levels don’t necessarily have to be checked every day. But, if you’re still taking dexamethasone at home, the ward staff will arrange for your local district nurses or practice nurse to monitor your blood sugars at home
How often they’re checked will depend on what your blood sugar levels were during your hospital stay.
When can I wash my hair after surgery?
You need to wait at least 48 hours, but 72 hours is better.
If there’s been any leakage from the wound, or you’ve had previous surgery, you may be advised to wait a little longer before washing your hair.
Use a gentle shampoo, such as baby shampoo, or the hair wash provided to you before coming into hospital. And be careful not to rub around the wound area.
It’s not a problem if some water runs onto the wound – you can gently pat the area dry with a clean towel.
If you have dissolvable stitches in your scalp (rather than inside your scalp), you can wash your hair as above, but don’t put shampoo over the suture line (line of stiches).
When can I dye my hair again?
You need to wait at least 6 weeks. This is to make sure your wound is fully healed.
However, if you’re going to be starting chemotherapy or radiotherapy, you’ll need to discuss this with your oncologist.
How long before I can fly?
It is strongly advised that you seek your doctor’s advice on whether they believe that you’re fit to fly, before booking any travel arrangements. You should also speak to your airline.
There are no specific guidelines regarding the minimum time before you can fly.
However, the Civil Aviation Authority (CAA) , which is responsible for air travel safety, advise that you should avoid air travel for approximately seven to ten days following brain surgery.
The general advice from the NHS is to wait until around 6 weeks from your operation and you’ve made a full recovery from your treatment before flying.
You can find more information on our travelling abroad page.
When can I drive again?
This depends on a range of factors including:
- the type of tumour you have/had
- the type of operation you had
- the symptoms you’ve been experiencing.
This can be very difficult to adjust to, but it’s very important that you don’t drive until your healthcare team decides you are fit to drive and the DVLA return your licence.
You can find more detailed information on our driving and brain tumours page.
When will I be able to return to work?
Like most aspects of recovery, this will be different for everyone depending on their diagnosis, how their heath is following surgery and what their job is.
Most people need at least six to twelve weeks off work. However, this may be longer if you’re having further treatment or if your job involves certain risks – for example, if you drive, work at heights or use heavy machinery.
You’ll be able to discuss this with your doctors and CNS to make plans that best suit your personal circumstances.
It may be useful to discuss returning to work with your employer before your surgery. We have a range of resources available to help you have that conversation.
If you’re worried about returning to work because of financial issues it may help you to look at our financial support page .
Will I need to have further scans after my surgery?
Yes. Your healthcare team will let you know about any scans you need to have.
Initially, scans may be done more frequently, but over time the interval between scans may become longer. This will depend on the type of brain tumour you’ve been diagnosed with.
You can find more information on our diagnostic scans page .
Alternative approaches to helping recovery
People often ask about alternative treatments to help in their recovery when they go home after brain surgery.
We understand that you may want to look at these options, but it’s important to keep in mind that they’re not fully supported by medical evidence and they may interfere with your standard treatment.
You should always speak to your healthcare team before pursuing alternative treatments.
Ketogenic diet
A ketogenic diet is one that encourages eating very low amounts of carbohydrates and increased amounts of fats. Although there is currently no scientific evidence to show that a ketogenic diet is effective in treating brain tumours, it is being trialed by some specialist centres.

Cannabis oil
The use of cannabis oil is highly publicised and there is some evidence that it can help treat some side-effects caused by brain tumours – for example, pain and chemotherapy-induced nausea and vomiting,
However, there’s no supporting evidence for the treatment of the tumour itself. It’s important to remember that cannabis-based products have not been licensed for people with brain tumours.
Download our fact sheet
Going home after brain surgery – pdf.
Download our full factsheet on going home after brain surgery.
Support and Information Services
Research & clinical trials information.
You can also join our active online community .
In this section
- Neurosurgery for adults
- Inserting a shunt
- 5-ALA (The Pink Drink)
- Side effects of neurosurgery
If you need someone to talk to or advice on where to get help, our Support and Information team is available by phone, email or live-chat.
Recommended reading
- Finding myself in your hands
- What you need to know about the “Pink Drink”
- Coping with life after a brain tumour diagnosis
- How to prepare for outpatient appointments
Share your experiences and help create change
By taking part in our Improving Brain Tumour Care surveys and sharing your experiences, you can help us improve treatment and care for everyone affected by a brain tumour.
- Patient Care & Health Information
- Diseases & Conditions
- Brain metastases
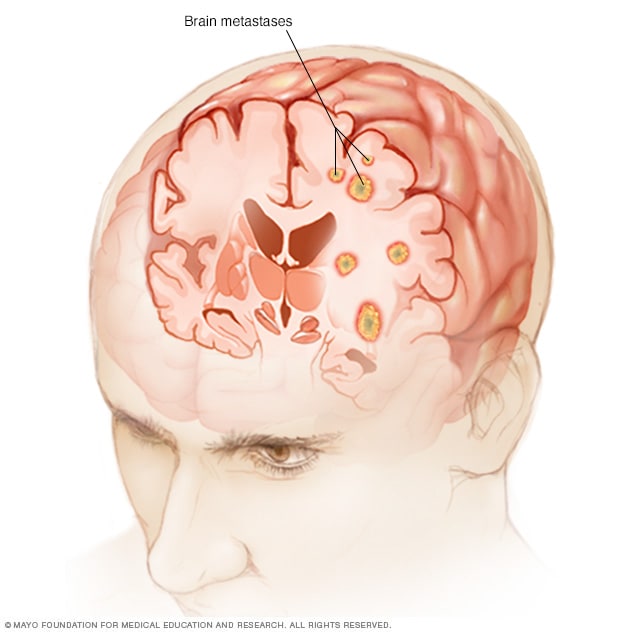
Brain metastases happen when cancer begins elsewhere in the body and spreads (metastasizes) to the brain.
Brain metastases occur when cancer cells spread from their original site to the brain. Any cancer can spread to the brain, but the types most likely to cause brain metastases are lung, breast, colon, kidney and melanoma.
Brain metastases may form one tumor or many tumors in the brain. As the metastatic brain tumors grow, they create pressure on and change the function of surrounding brain tissue. This causes signs and symptoms, such as headache, personality changes, memory loss and seizures.
Treatment for people whose cancer has spread to the brain may include surgery, radiation therapy, chemotherapy, immunotherapy or a combination of treatments. Other treatments might be recommended in certain situations. Treatment is often focused on reducing pain and symptoms resulting from the cancer.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Signs and symptoms caused by brain metastases can vary based on the location, size and rate of growth of the metastatic tumors.
Signs and symptoms of brain metastases include:
- Headache, sometimes with vomiting or nausea
- Mental changes, such as increasing memory problems
- Weakness or numbness on one side of the body
When to see a doctor
Make an appointment with your doctor if you have persistent signs and symptoms that concern you. If you've been treated for cancer in the past, tell your doctor about your medical history.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Get the latest brain tumor advice from Mayo Clinic delivered in your inbox.
Sign up for free and receive the latest on brain tumor treatment, diagnosis and surgery.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing
You will receive the first brain tumor email in your inbox shortly, which will include information on treatment, diagnosis, surgery and how brain cancer teams at Mayo Clinic approach personalized care.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Brain metastases occur when cancer cells break away from their original location. The cells may travel through the bloodstream or the lymph system and spread (metastasize) to the brain where they begin to multiply.
Metastatic cancer that spreads from its original location is known by the name of the primary cancer. For example, cancer that has spread from the breast to the brain is called metastatic breast cancer, not brain cancer.
Risk factors
Any type of cancer can spread to the brain, but some types of cancer are more likely to cause brain metastases, including:
- Lung cancer
- Breast cancer
- Colon cancer
- Kidney cancer
Brain metastases care at Mayo Clinic
- AskMayoExpert. Brain metastases (adult). Mayo Clinic; 2018.
- Niederhuber JE, et al., eds. Brain metastases and neoplastic meningitis. In: Abeloff's Clinical Oncology. 6th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Sept. 23, 2020.
- Central nervous system cancers. National Comprehensive Cancer Network. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed Sept. 23, 2020.
- Metastatic cancer. National Cancer Institute. https://www.cancer.gov/types/metastatic-cancer. Accessed Sept. 24, 2020.
- Loeffler JS. Overview of the treatment of brain metastases. https://www.uptodate.com/contents/search. Accessed Sept. 24, 2020.
- Treatments and side effects. American Brain Tumor Association. https://www.abta.org/about-brain-tumors/treatments-sideeffects. Accessed Sept. 25, 2020.
- Types of complementary therapies. Cancer.Net. https://www.cancer.net/navigating-cancer-care/how-cancer-treated/integrative-medicine/types-complementary-therapies. Accessed Sept. 25, 2020.
- Le Rhun E, et al. Leptomeningeal metastases of solid cancer. Current Opinion in Neurology. 2016; doi:10.1097/WCO.0000000000000393.
- Rades D, et al. A new scoring tool to assess overall survival in patients with intracerebral metastases from gynecological cancers. International Journal of Gynecological Cancer. 2017; doi:10.1097/IGC.0000000000000899.
- Klos KJ, et al. Brain metastases. The Neurologist. 2004; doi:10.1097/01.nrl.0000106922.83090.71.
- O'Neill BP, et al. Brain metastatic lesions. Mayo Clinic Proceedings. 1994; doi:10.1016/S0025-6196(12)61374-3.
- Heim JB, et al. Myosin-1E interacts with FAK proline-rich region 1 to induce fibronectin-type matrix. Proceedings of the National Academy of Sciences of the United States of America. 2017; doi:10.1073/pnas.1614894114.
- Brown PD, et al. Effect of radiosurgery alone vs. radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases. JAMA. 2016; doi:10.1001/jama.2016.9839.
- Brown PD, et al. NCCTG N0574 (Alliance): A phase III randomized trial of whole brain radiation therapy (WBRT) in addition to radiosurgery (SRS) in patients with 1 to 3 brain metastases. Journal of Clinical Oncology. 2015; doi:10.1200/jco.2015.33.18_suppl.lba4.
- Rades D, et al. A matched-pair study comparing whole-brain irradiation alone to radiosurgery or fractionated stereotactic radiotherapy alone in patients irradiated for up to three brain metastases. BMC Cancer. 2017; doi:10.1186/s12885-016-2989-3.
- Rades D, et al. Prognostic factors after whole-brain radiotherapy alone for brain metastases from malignant melanoma. Anticancer Research. 2016; doi:10.21873/anticanres.11271.
- Crozier JA, et al. Breast cancer brain metastases: Molecular subtype, treatment and survival. Breast Disease. 2016; doi:10.3233/BD-160237.
- Cheville AL, et al. Nested cohort study to identify characteristics that predict near-term disablement from lung cancer brain metastases. Archives of Physical Medicine and Rehabilitation. 2017; doi:10.1016/j.apmr.2016.08.473.
- Warner KJ. Allscripts EPSi. Mayo Clinic. June 30, 2020.
- Porter AB (expert opinion). Mayo Clinic. Oct. 23, 2020.
- Stereotactic radiosurgery for brain metastases
Associated Procedures
- Palliative care
- Positron emission tomography scan
News from Mayo Clinic
- Mayo Clinic Q&A podcast: Liquid biopsy can help guide cancer treatment July 19, 2022, 03:00 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Robin Roberts' nephew helps save a life as a stem cell donor
Jeremiah Craft learned in January that he was someone's match.
When Jeremiah Craft was growing up, he watched his aunt, " Good Morning America " co-anchor Robin Roberts , undergo a lifesaving bone marrow transplant .
The stem cells used in the 2012 transplant to save Roberts' life were donated by Craft's mom, Sally-Ann Roberts , who was a perfect match for her younger sister.
The journey of the Roberts sisters was a unique one, as 70% of patients in need of a bone marrow transplant do not have a fully-matched donor in their family, according to NMDP , a non-profit organization that manages a global marrow registry.
In the majority of cases, patients must rely on donations from strangers on the NMDP registry.

With those statistics in mind, Sally-Ann Roberts convinced Craft, at the time a teenager, to sign up for the NMDP registry, which involves sending in a simple swab of your inner cheek that can help match you to current or future patients.
"Basically, my mom 'voluntold' me to sign up, kind of like a mandatory suggestion," Craft, now 29, recalled to "GMA."
Several years later, to his surprise, Craft said he got a call that he was a match for a stranger.
Take the first step to sign up to become a bone marrow donor today. Visit my.nmdp.org/gma or text GMA to 61474 to request a swab kit.
At the time, Craft declined to participate in the transplant. According to NMDP, less than half of potential donors agree to donate when they are found to be a match, for a variety of reasons.
"Unfortunately, at the time, I just was thinking about me," Craft said of his decision. "It was acting selfishly, and I didn't heed the call."
Craft said he quickly regretted his decision, saying, "Up until this point, I was very, very sure that that was going to be the biggest mistake of my life."
Related Stories

Dawn Staley talks 3rd NCAA title, Caitlin Clark
- Apr 8, 8:54 AM

Shohei Ohtani's ex-interpreter Ippei Mizuhara turns self in, free on $25K bond
- Apr 12, 7:09 PM

Judge in sports betting case orders ex-interpreter for Ohtani to get gambling addiction treatment
- Apr 12, 5:16 PM
In January, Craft unexpectedly got a second chance. He received a call from NMDP notifying him that he was once again a match.
"Because I've been thinking about that person every day since then, it was just impossible for me to not say yes," Craft said of his decision to become a donor.
Added his mom, Sally-Ann Roberts, "He did not hesitate. He was ready."
MORE: 'Good Morning America' co-anchor Robin Roberts celebrates 10th anniversary of return after bone marrow transplant
Once he decided to move forward, Craft underwent five days of injections to help stimulate his blood stem cells to prepare for donation day.
Craft then traveled from New York City to Houston in March to complete his donation. As is standard protocol, Craft's travel expenses were covered by NMDP.
The organization pays travel expenses and non-medical costs for all donors, as well as any medical expenses not covered by insurance, according to its website .
Robin Roberts spoke to Craft ahead of his donation day, calling him a "superhero."

"I'm proud of you," she said to her nephew.
MORE: Reporter's notebook: ABC News reporter meets bone marrow recipient 1 year after lifesaving donation
Craft said he was "grateful to God" to have a second change at saving a life.
"I’m a regular guy trying to do the right thing for the second time," he said. "I'm just grateful to God that I can go from pretending to be a hero to growing older, learning what is important and actually saving a life."
Craft donated through peripheral blood stem cells, or PBSC, donation, a non-surgical procedure in which blood is drawn from one arm, passed through a machine that separates the blood-forming cells and then the remaining blood is returned to the other arm, according to NMDP.

For Craft, the donation took a total of five hours, but donation times can vary.
The other method for donation is bone marrow, which takes place in a hospital and is typically a one-day procedure in which needles are used to withdraw liquid marrow from the back of the pelvic bone. The donor is typically in the hospital from early morning to late afternoon and most donors feel completely recovered within weeks, according to NMDP .

Teen holding toy gun shot by Akron police
- Apr 12, 2:39 PM

Maine lawmakers approve shield law for providers of abortion and gender-affirming care
- Apr 12, 1:22 PM
ABC News Live
24/7 coverage of breaking news and live events
Watch CBS News
Did you look at the solar eclipse too long? Doctors explain signs of eye damage
By Sara Moniuszko
Edited By Allison Elyse Gualtieri
Updated on: April 8, 2024 / 3:42 PM EDT / CBS News
Did you look up at the solar eclipse without your safety glasses ? Looking at the sun — even when it's partially covered like during the eclipse on April 8 — can cause eye damage.
There is no safe dose of solar ultraviolet rays or infrared radiation, said Dr. Yehia Hashad , an ophthalmologist, retinal specialist and the chief medical officer at eye health company Bausch + Lomb.
"A very small dose could cause harm to some people," he said. "That's why we say the partial eclipse could also be damaging. And that's why we protect our eyes with the partial as well as with the full sun."
But how do you know if you've hurt your vision? We asked eye doctors what to know.
Is it a sign of eye damage if your eyes hurt after looking at the eclipse?
Your eyes likely won't hurt if you look at the eclipse without protection — but that doesn't make it any less dangerous.
In fact, the painlessness is part of why the event is so concerning to eye care professionals, said Dr. Jason P. Brinton, an ophthalmologist and medical director at Brinton Vision in St. Louis.
"Everyone knows don't look at the sun. If you go out on a bright day and try to look at the sun — it's very uncomfortable, very bright. So most people intuitively associate that with something they should not be doing," Brinton said. "But with the eclipse, so much of that is blocked and so that natural sense of discomfort and aversion to the brightness is not there."
In some cases, the sun can also damage the cornea, which can be painful, Brinton says.
"The good news is that this fully heals without lasting issues, so this is why we don't think about this aspect as much. The retinal issues, on the other hand, are painless and can have permanent, lasting effects on vision," he said.
What are other signs of eye damage from looking at a solar eclipse?
Hashad says there are a few "alarming signals" to be aware of, including:
- Blurred vision
- Scotomas, or dark spots: "You just see a black area or a black spot in the field of vision," Hashad said.
- Color changes: "You don't see the colors the same way you were seeing it before," he said.
- Distorted lines: Hashad says this is clinically known as metamorphopsia, which makes lines appear warped, distorted or bent.
"This could be happening unilateral or bilateral," he said. "So it doesn't necessarily happen in both eyes. It could be affecting one over the other or both eyes together."
Issues may not be apparent immediately, either, sometimes appearing one to a few days following the event.
And while some will regain normal visual function, sometimes the damage is permanent.
"Often there will be some recovery of the vision in the first few months after it, but sometimes there is no recovery and sometimes there's a degree to which it is permanent," Brinton said.
What should you do if you show symptoms of eye damage?
If you're experiencing any symptoms of eye damage, Hashad suggested people "immediately" seek an ophthalmologist's advice.
"Seeing an eye care professional to solidify the diagnosis and for education I think is reasonable," Brinton said.
Unfortunately, there isn't a treatment for solar retinopathy, the official name for the condition.
"Right now there is nothing that we do for this. Just wait and give it time and the body does tend to heal up a measure of it," Brinton explained.
That is why prevention is so important, and remains the "mainstay of treatment of solar retinopathy or solar damage to the retina," Hashad explained.
How long is too long to look at a solar eclipse without glasses?
Any amount of time looking at the solar eclipse without glasses is too long, experts said.
"Damage from the solar eclipse could happen to the retina in seconds," Hashad said. "That's why we don't want people to stare even for a short period of time — even if for a few seconds to the direct sun — whether eclipsed or even partially eclipsed."
Sara Moniuszko is a health and lifestyle reporter at CBSNews.com. Previously, she wrote for USA Today, where she was selected to help launch the newspaper's wellness vertical. She now covers breaking and trending news for CBS News' HealthWatch.
More from CBS News

Arizona's abortion ban likely to cause people to travel to states it's still legal
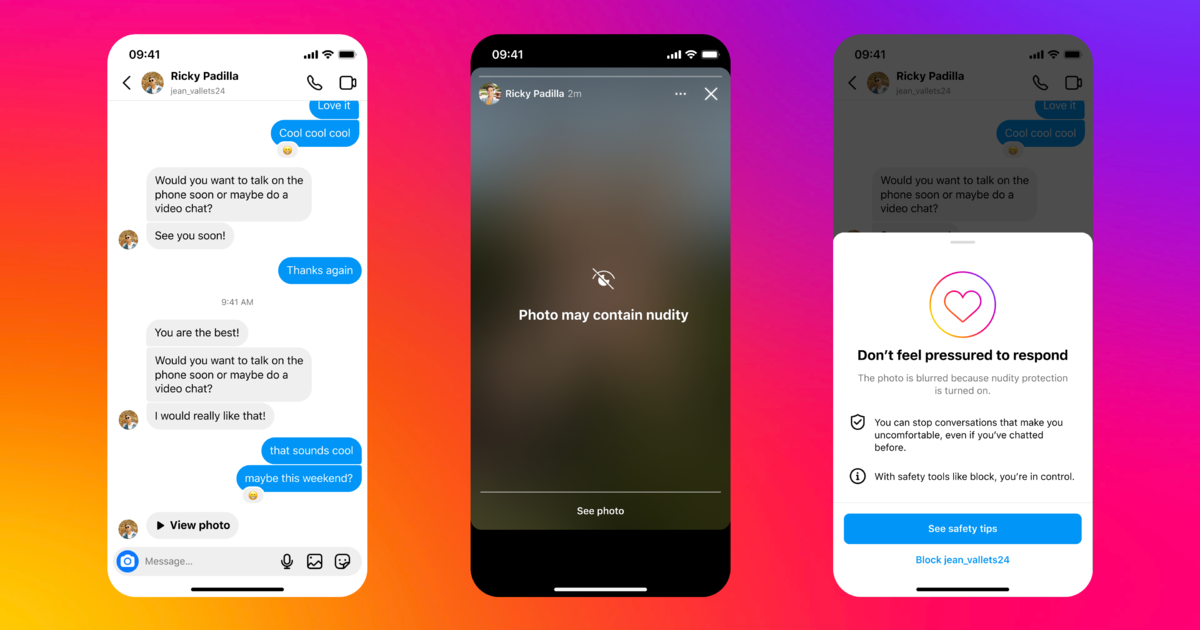
Meta tests new features on Instagram designed to fight teen sextortion

Botox shots, possibly counterfeit, linked to botulism-like illnesses

Guide dog nicknamed Dogfather retires after fathering over 300 puppies
- Skip to main content
- Keyboard shortcuts for audio player

Solar eclipse 2024: Follow the path of totality
Solar eclipse, worried about eclipse damage to your eyes don't panic.

Geoff Brumfiel

Nell Greenfieldboyce

Junior Espejo looks through eclipse glasses being handed out by NASA in Houlton, Maine. Used correctly, eclipse glasses prevent eye damage. Joe Raedle/Getty Images hide caption
Junior Espejo looks through eclipse glasses being handed out by NASA in Houlton, Maine. Used correctly, eclipse glasses prevent eye damage.
Tens of millions of Americans will have spent the day staring at a total solar eclipse, and at least a few of them may become worried that they inadvertently damaged their eyes.
But experts say there's no need to panic — the vast majority of eclipse viewers are probably fine. And even if somebody did strain their eyes, the effects could be temporary.
During the 2017 total solar eclipse it's estimated that 150 million Americans viewed the event. There were around 100 documented cases of eye damage across all of America and Canada, according to Ralph Chou, an expert on eclipse eye safety with the University of Waterloo in Canada.
Far more people turned up in emergency rooms worried that they'd damaged their eyes. Many complained of watery eyes or blurred vision, but in most cases they were fine, according to Avnish Deobhakta, an ophthalmologist at the New York Eye and Ear Infirmary of Mount Sinai, one of the largest eye hospitals in the nation.
The reason it's hard to do real damage is simple — the human eye has evolved to avoid staring directly at the sun.
"It's so bright that we're not actually capable of looking at it without either tearing or sort of not really feeling comfortable staring at this ball of light," Deobhakta says.

Shots - Health News
Here's what it looks like when you fry your eye in an eclipse.
In the rare case that someone does damage their eyes, that damage usually shows up as a blurry spot in the field of vision , hours or up to a day after watching the eclipse. In about half of cases, the problem fixes itself, but permanent damage can sometimes occur.
Anticipating the post-eclipse ocular anxiety, at least one eye clinic in Buffalo, N.Y., is offering free eye checks immediately after the eclipse on April 8.
It's always a good idea to get your eyes checked, whether or not there's an eclipse. So if you're worried at all, go ahead and use the opportunity to schedule your annual exam.
- eclipse eye damage
- 2024 eclipse
There’s a powerful story behind every headline at Ohio State Health & Discovery. As one of the largest academic health centers and health sciences campuses in the nation, we are uniquely positioned with renowned experts covering all aspects of health, wellness, science, research and education. Ohio State Health & Discovery brings this expertise together to deliver today’s most important health news and the deeper story behind the most powerful topics that affect the health of people, animals, society and the world. Like the science and discovery news you find here? You can support more innovations fueling advances across medicine, science, health and wellness by giving today.
BROUGHT TO YOU BY
- The Ohio State University
- College of Dentistry
- College of Medicine
- College of Nursing
- College of Optometry
- College of Pharmacy
- College of Public Health
- College of Veterinary Medicine
- Ohio State Wexner Medical Center
- Ohio State's Comprehensive Cancer Center – James Cancer Hospital and Solove Research Institute
Subscribe. The latest from Ohio State Health & Discovery delivered right to your inbox.
Health Talks: Bringing mobile lung cancer screenings to the underserved
On ohio state pulmonologist describes the new mobile lung cancer screening unit that travels the buckeye state to offer screenings to underserved areas..
- Share on Facebook
- Share on Linkedin
- Share via Email
- Share this page
In this video , pulmonologist Michael Wert, MD , of The Ohio State University Comprehensive Cancer Center – James Cancer Hospital and Solove Research Institute (OSUCCC – James), discusses a new mobile lung cancer screening unit that will be traveling throughout Ohio to offer important screenings to those who are most at risk of lung cancer and unlikely to have other access to screenings.
Lung cancer is the No. 1 cancer killer of men and women in the United States. Because symptoms can vary greatly and don’t always appear until the cancer has grown and spread significantly, lung cancer can be particularly difficult to treat. By screening individuals at high risk for lung cancer, detection and diagnosis can happen earlier when the cancer is most curable.
The goal of the mobile unit is to visit area businesses, local health departments, churches and other underserved locations around Ohio to provide screenings, and potentially catch lung cancer in its early stages for those at high risk.
To qualify for a screening on the mobile unit, a person must be:
- 50-80 years old
- Current smoker with a history of smoking 1 pack per day for 20 years
- Ex-smoker who has quit within the past 15 years
While screening guidelines change often, Dr. Wert says Ohio State is currently using the guidelines most insurance companies and Medicare will approve.
Watch this Health Talks video to learn more about the new mobile lung cancer screening unit and how to find out when the unit will be in your area.
At The James, there is no routine cancer
Our experts develop and deliver the most advanced targeted treatments leading to better outcomes and more hope.
- Cancer Prevention ,
- Cancer Screening ,
- Health Talks ,
- Lung Cancer ,
- Lung Cancer Screening ,
- Ohio State Wexner Medical Center ,
- OSUCCC – James
- Health Talks
Related websites
- Ohio State's Comprehensive Cancer Center – James Cancer Hospital and Solove Research Institute
Recent Videos
How to recognize signs of anal cancer, how the HPV vaccine can prevent it, and more
By Syed Husain, MBBS

How gene therapy changed everything for child born with AADC deficiency
Articles on health.
Why is my eye twitching?
By J.P. Maszczak, OD
An Ohio State optometrist explains what you can do to stop an annoying problem.

10 times you can head to a pharmacy before a doctor's office
By Rebecca Lahrman, PharmD, MS, BCACP
Though pharmacists may not be able to diagnose illnesses or prescribe medication, they can provide valuable guidance – often sooner than a doctor is available.
What to know about TIL therapy, a new treatment for skin cancer
By Richard C. Wu, MD, PhD
Which over-the-counter pain medication is best for which situation?
By Jason Holmes, PharmD
Types of headaches and migraine attacks, remedies and tips
By Kevin Weber, MD, MHA
Get articles and stories about health, wellness, medicine, science and education delivered right to your inbox from the experts at Ohio State.
Required fields
Tell us more about yourself
By clicking "Subscribe" you agree to our Terms of Use . Learn more about how we use your information by reading our Privacy Policy .
latest in US News

Body found in burning car believed to be Florida woman whose...

Former ambassador sentenced to 15 years in prison for...

World's oldest conjoined twins dead at 62

Supporter who hugged Trump at Atlanta Chick-fil-A says media...

Hunter Biden’s ‘nonsensical’ bid to dismiss federal gun...

Noisy pet rooster ruffles feathers in the Hamptons with pre-dawn...

Girlfriend of 14-year-old senselessly gunned down while...

Teen brute accused of shoving, robbing granny outside NYC church...
‘if it doesn’t fit, you must acquit’ why oj simpson’s iconic courtroom glove fitting is burned into america’s brain.
- View Author Archive
- Get author RSS feed
Thanks for contacting us. We've received your submission.
It’s a moment fit for the history books.
OJ Simpson, who died after a cancer battle this week, goes down in history not just for his achievements on the football field, but also his notorious, racially charged murder trial — with no moment more visually memorable than his courtroom glove fitting.
During the disgraced NFL great’s 1995 trial , the prosecution asked Simpson to try on bloody black gloves found at the scene of his ex-wife Nicole Brown’s murder.
Prosecutors thought the gloves were among the strongest evidence because DNA tests showed blood on them contained genetic markers for Simpson, Brown and her friend Ron Goldman, who was also stabbed to death.

But when prosecutor Christopher Darden asked Simpson to slip on the gloves in front of jurors, the defendant squirmed and struggled to fit his hands into them, making them appear far too small for him — and the case went up in flames.
Simpson made a huge show in court of struggling to slip the gloves over thinner latex gloves he had been provided, making frustrated expressions, and leading jurors to believe they might not be his.
The courtroom drama, which unfolded on June 15, 1995, became one of the most powerful images during the trial and one of its most pivotal moments, with critics later speculating that Simpson — who had appeared in the 1988 spoof movie “The Naked Gun” — channeled his acting ability to drum up doubt.

The glove incident was far from the first misstep by the prosecution in the nine-month trial, but was famously seized on by the defense team.
Stay updated with the latest coverage of OJ Simpson’s death
- Live updates: The latest on the death of NFL star, actor and murder suspect OJ Simpson
- OJ Simpson ditched his cane for final outing in Las Vegas less than 2 months before his death
- OJ Simpson assured fans he was in good health in final video before cancer death
- OJ Simpson dead from cancer at 76
- OJ Simpson dead at 76: His final photos revealed
During closing statements in the so-called “trial of the century,” Simpson’s defense attorney Johnnie Cochran proclaimed, “If it doesn’t fit, you must acquit.” Simpson was ultimately found not guilty.
Darden later insisted he didn’t regret the choice to have Simpson try on the gloves, saying the fitting wasn’t the reason Simpson was acquitted.
“I think the trial was lost way before then,” Darden said in 2016.
Share this article:

Advertisement
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
A Driver of Colorectal Cancer Growth Could Come From Your Mouth
Ivan Balvan / Getty Images
Key Takeaways
- Fusobacterium nucleatum, an oral bacterium, is linked to the development of colorectal cancer.
- The bacterium binds to cancer cells, activating growth factors that promote cancer proliferation and metastasis.
- Maintaining oral hygiene is essential to manage Fusobacterium nucleatum , reducing gum disease risk and its potential systemic health impact.
Your mouth is teeming with microbes. Most of these are harmless, and many are protective. But sometimes, certain hardy bacteria can leave the mouth and travel throughout the body. Depending on where they land, they can spur cancer and cause all sorts of other problems.
One of those microbes, Fusobacterium nucleatum , can travel down the digestive tract and latch onto cells throughout the gut. Recent research shows that the bacteria helps colorectal cancer tumors develop and metastasize.
Researchers at the Fred Hutch Cancer Center sought to understand precisely which bacteria can survive the trek through the digestive tract to promote cancer in the lower gut. In a study last month, the team examined colorectal cancer tumors from 200 patients. Half the patients had high levels of a Fusobacterium nucleatum subtype, called Fna C2, in their tumor tissue compared to healthy tissue. That bacterium was also more prevalent in the stool of people with colorectal cancer.
“Not all oral bacteria or gut bacteria can make their way into tumors, so we set out to find out what makes these tumor-homing bacteria genetically distinct or special. Our ultimate goal is to use such knowledge of tumor-homing microbes to develop new ways to screen for cancer, prevent cancer, or treat cancer,” corresponding study author Christopher Johnston, PhD , an assistant professor in the Vaccine and Infectious Disease Division at Fred Hutch Cancer Center, told Verywell in an email.
How Bacteria Can Accelerate Cancer
Fusobacteria are part of the “mobile microbiome,” said Yiping Han, PhD , professor of microbial sciences in dental medicine and microbiology and immunology at Columbia University. The bacteria can travel outside the confines of the mouth and have been detected at many sites of infection and inflammation throughout the body.
Almost all people have Fusobacterium nucleatum in their mouths, but it rarely appears in the digestive tract of healthy people. When the oral microbiome is thrown off balance, the bacteria can build up in tooth plaque and overgrow in inflamed gums, both causing and progressing gum disease.
Bacteria from the mouth may enter the bloodstream when you cut your gums or tongue, or it can flush through the gastrointestinal tract when you swallow saliva.
“There are a lot more different kinds of Fusobacteria in the saliva, but in the stomach and colon, that diversity is significantly reduced. That indicates that traveling down the GI tract is a selective process—the stomach acid probably kills a lot of them,” Han told Verywell.
Two decades ago, Han’s lab discovered how Fusobacterium nucleatum binds to cells throughout the body, including cancer cells. Under certain conditions, proteins on the outside of the bacterium fold into amyloids—the same kind of proteins that cause plaques in the brains of Alzheimer’s patients. Those sturdy exterior proteins appear to protect bacteria against the destructive properties of stomach acid.
The amyloid adhesive also helps the bacteria bind to a specific site on cancer cells, Han said. There, it activates a cancer growth factor that can cause cancerous cells to multiply and spread beyond the tumor site.
Scientists are investigating other ways that the bacteria could contribute to cancer, such as causing inflammation, which is associated with cancer in many parts of the body. There’s no evidence yet that Fusobacterium nucleatum can cause cancer to form where there are no existing precancerous cells, Han said.
Signs and Symptoms of Oral Bacteria
Gum disease is usually caused by a build-up of plaque on the teeth. That plaque is made up of lots of bacteria, including Fusobacteria , which feed on sugars in the mouth. Their waste can cause gums to become inflamed and swollen.
Gingivitis is a mild form of gum disease that causes gums to become a bit red, swollen, and prone to bleeding. With good oral hygiene, gingivitis can go away on its own. If it spreads to other parts of the periodontium, the soft tissue and bone that keep teeth anchored in the mouth, it can cause more substantial damage. In periodontitis, bacteria can lodge deeper into the gums, causing further inflammation and tooth decay. Fusobacterium nucleatum can cause periodontitis and overgrows in the mouths of people with gum disease.
Gum disease can arise from poor oral hygiene, but other risk factors play a role, too. Smoking, diabetes, and some hormonal shifts can also increase a person’s risk for gum disease.
Beyond Colorectal Cancer
Fusobacteria are implicated in many different diseases beyond colorectal cancer. The bacteria have been found in the tumors of various different gastrointestinal cancers and disorders, including inflammatory bowel disease and appendicitis.
Han said the Fusobacterium is one of the few bacteria that can cross both the blood-brain barrier and the placental barrier.
The bacteria appears to make its way into the bloodstream and contribute to pregnancy complications like stillbirth, neonatal sepsis, and preterm birth. Animal studies indicate that Fusobacteria can also contribute to Alzheimer’s Disease progression.
People with this bacteria in their tumors may have a harder time overcoming cancer and may be more likely to see a recurrence. Johnston said that people with tumors containing Fusobacteria nucleatum tend to have poorer survival and poorer prognosis than those without it.
“It’s been reported in numerous studies that not just in colorectal cancer, but also esophageal cancer, gastric cancer—the kinds that are implicated with F. nucleatum —they have a worse prognosis, shorter survival time, chemoresistance, more metastasis, things like that,” Han said.
Brush and Floss Your Teeth for Better Overall Health
Almost everyone has Fusobacteria in their mouth, but not everyone develops colorectal cancer. The bacteria doesn’t seem to be able to latch onto the lower digestive tract unless there is already an imbalance in the gut microbiome or there is already damage to, or inflammation in, the tissue there.
Scientists are still learning how frequently Fusobacterium nucleatum appears in colorectal tumors. The amount of Fusobacterium nucleatum in tissue and stool is greater in people with late-stage colorectal cancer than those in earlier stages.
There’s not yet a widely available test to identify whether you harbor harmful oral bacteria. Johnson said that pinpointing tumor-infiltrating bacteria subtypes could help scientists create screening tools to identify who is at the highest risk for colorectal cancer development.
Once scientists know what to target, they can develop vaccines or other therapies to neutralize that threat.
“Now, we keep digging into Fna C2—sorting out what makes this group special and uncovering the genetic features that are allowing it to attach to—and burrow inside of—tumors,” Johnston said. “If we figure that out, we can stop it from happening or even harness it to deliver drugs into tumors.”
In the meantime, the best way to keep Fusobacteria and other bacteria from wreaking havoc in your body is to tend to your oral health. Fusobacterium nucleatum build-up is a common cause of gum disease. Brushing and flossing your teeth consistently and visiting a dentist regularly can help keep the oral microbiome in balance and prevent harmful oral bacteria from causing issues throughout the body.
“Maintaining good oral health to prevent inflammation and keep bacteria levels low is always a good thing to do,” Han said. “Your mouth is the gateway to your overall health. You cannot separate the mouth from the rest of the body—the human body is one connected entity.”
What This Means for You
Scientists are still learning which bacteria are implicated in cancer, and there’s not yet a good way to test yourself for the cancer-causing types. Practicing good oral hygiene by brushing your teeth consistently, flossing, and visiting the dentist regularly can reduce the risk of your oral microbiome becoming imbalanced.
Zepeda-Rivera M, Minot SS, Bouzek H, et al. A distinct Fusobacterium nucleatum clade dominates the colorectal cancer niche . Nature . Published online March 20, 2024. doi:10.1038/s41586-024-07182-w
Meng Q, Gao Q, Mehrazarin S, et al. Fusobacterium nucleatum secretes amyloid-like FadA to enhance pathogenicity . EMBO Rep. 2021;22(7):e52891. doi: 10.15252/embr.202152891
Chen Y, Huang Z, Tang Z, et al. More than just a periodontal pathogen—the research progress on Fusobacterium nucleatum . Front Cell Infect Microbiol . 2022;12:815318. doi:10.3389/fcimb.2022.815318
Vander Haar EL, So J, Gyamfi-Bannerman C, et al. Fusobacterium nucleatum and adverse pregnancy outcomes: epidemiological and mechanistic evidence . Anaerobe . 2018;50:55-59. doi:10.1016/j.anaerobe.2018.01.008
Wu H, Qiu W, Zhu X, et al. The periodontal pathogen Fusobacterium nucleatum exacerbates Alzheimer’s pathogenesis via specific pathways . Front Aging Neurosci . 2022;14:912709. doi:10.3389/fnagi.2022.912709
Ou S, Wang H, Tao Y, et al. Fusobacterium nucleatum and colorectal cancer: from phenomenon to mechanism . Front Cell Infect Microbiol . 2022;12:1020583. doi:10.3389/fcimb.2022.1020583
By Claire Bugos Bugos is a senior news reporter at Verywell Health. She holds a bachelor's degree in journalism from Northwestern University.

IMAGES
VIDEO
COMMENTS
Doctors address concerns about air travel safety for patients with brain tumors in this new study. The global reach of medicine is becoming increasingly easier to achieve. Thanks to the ever-increasing availability of medical information available online as well as the capabilities for long distance tele-health consultations, patients have expanded options to undergo multidisciplinary ...
Travel is perfectly safe for cancer patients most of the time, and we want you to enjoy your life. But you never know exactly what might happen, so it's good to be prepared.". Request an appointment at MD Anderson online or by calling 1-877-632-6789. Topics. Side Effects.
Talk with a healthcare provider if you have a brain tumor or brain metastases as air travel could create brain swelling. Most people with brain tumors can travel by air safely, though symptoms may worsen. In some cases, oncologists may recommend steroids or anti-seizure drugs prior to flying.
Travelling with a brain tumour can be complicated. But, it is still possible for some people. We look at some of the questions you might have and the support that's available. Short summary. You might still want to travel after being diagnosed with a brain tumour. But, sadly, it can affect your ability to travel abroad.
Brain tumor. A brain tumor can form in the brain cells (as shown), or it can begin elsewhere and spread to the brain. As the tumor grows, it creates pressure on and changes the function of surrounding brain tissue, which causes signs and symptoms such as headaches, nausea and balance problems.
4. Travelling long distances can increase your risk of getting blood clots. People living with cancer have a greater risk for a blood clot than people without cancer. If you decide to travel and will be sitting for a long time, here are a few tips to help prevent blood clots: • Avoid alcohol. • Drink lots of water.
In short, the study found "Overall, airflight was found to be safe for patients with brain tumors. Nevertheless, if patients have brain tumors and seek to travel by plane, they should have discussions with their neurosurgeon or neuro-oncologist to ensure individual safety."
Other brain tumors can't be separated from surrounding tissue. Sometimes a brain tumor is near an important part of the brain. Surgery might be risky in this situation. ... You can go home after treatment and don't need to stay in a hospital. Side effects of radiosurgery include feeling very tired and skin changes on your scalp. The skin on ...
Traveling can seem very daunting when you have a brain tumor. Before you embark on your travel, here are a few helpful tips that might help ensure that your trip goes smoothly. • Remember to pack your medications. To help you remember to pack your medications, try setting an alarm, leave your medications out in a visible spot while you or ...
MRI Brain Cancer Picture: Cross-section (image taken from the top of the head down) of a brain tumor in a young girl. The white arrow shows the tumor. Can You Travel If You Have Brain Cancer?
Conclusions: Most patients with brain and skull base tumors can travel safely via commercial airflight with acceptable symptom exacerbation. However, consideration should be given to administering corticosteroids and possibly anticonvulsants to patients who are symptomatic and/or have relatively large tumors with mass effect and peritumoral ...
If you are recovering from neurosurgery or have received the go-ahead from your doctor to travel with your brain tumor, you might find comfort and security in flying with a medical escort. While you may be safe to travel, you can enjoy greater peace of mind knowing a medical escort is there to assist you in case of a medical emergency.
The brain tumour hub has a list of travel insurance companies that will provide cover for people with pre-existing medical conditions. Find travel insurance providers. Practical travel advice. If you are travelling abroad following a brain tumour diagnosis, you may find that you have more things to think about to help you prepare for your holiday.
Metastatic brain tumors, also called secondary brain tumors, are malignant tumors that originate as cancer elsewhere in the body and then metastasize (spread) to the brain. Metastatic brain tumors are about four times more common than primary brain tumors. They can grow rapidly, crowding or invading nearby brain tissue.
Some people might experience weakness of the face, arms or legs. If a tumor involves a sensory area, a patient may experience numbness. " The person could also have difficulty speaking, understanding or both," Weathers says. "And very rarely, if a tumor involves the back part of the brain near the brainstem, they can present with ...
Caregivers of people with brain tumor or brain metastases are likely to have emotional challenges. For example, you may experience anxiety or depression. It is also likely for a caregiver to have physical symptoms like exhaustion. Personality changes common to brain tumors can be distressing.
It can be costly to get travel insurance if you have, or had, a brain tumour. This is because travel insurers weigh up the likelihood of an individual making a claim and consider many factors. These include: the chances of you cancelling your trip due to ill health. the likelihood of you having to seek medical assistance while away.
Research & Clinical Trials Information. [email protected]. Clinical trials and research information. Get involved in research. You can also join our active online community. A guide for people who are going home after having brain tumour surgery, including the support available and symptoms to watch out for.
Brain metastases may form one tumor or many tumors in the brain. As the metastatic brain tumors grow, they create pressure on and change the function of surrounding brain tissue. This causes signs and symptoms, such as headache, personality changes, memory loss and seizures. Treatment for people whose cancer has spread to the brain may include ...
Our 24/7 cancer helpline provides information and answers for people dealing with cancer. We can connect you with trained cancer information specialists who will answer questions about a cancer diagnosis and provide guidance and a compassionate ear. ... Tumor growth in the spine or brain; Surgery, injury, or trauma to the head; Swelling in the ...
Medulloblastoma is a type of malignant tumor that accounts for about 20% of all childhood brain tumors, according to estimates published in the Journal of Clinical Neuroscience. About 300 children ...
Isabella Strahan shares good brain tumor update. Apr 10, 1:49 PM. In January, Craft unexpectedly got a second chance. ... "I'm just grateful to God that I can go from pretending to be a hero to ...
Color changes: "You don't see the colors the same way you were seeing it before," he said. Distorted lines: Hashad says this is clinically known as metamorphopsia, which makes lines appear warped ...
In the rare case that someone does damage their eyes, that damage usually shows up as a blurry spot in the field of vision, hours or up to a day after watching the eclipse.In about half of cases ...
In this video, pulmonologist Michael Wert, MD, of The Ohio State University Comprehensive Cancer Center - James Cancer Hospital and Solove Research Institute (OSUCCC - James), discusses a new mobile lung cancer screening unit that will be traveling throughout Ohio to offer important screenings to those who are most at risk of lung cancer and unlikely to have other access to screenings.
OJ Simpson, who died after a cancer battle this week, will go down in history for his notorious, racially charged murder trial — with no moment more visually memorable than his disastrous ...
Two decades ago, Han's lab discovered how Fusobacterium nucleatum binds to cells throughout the body, including cancer cells.Under certain conditions, proteins on the outside of the bacterium fold into amyloids—the same kind of proteins that cause plaques in the brains of Alzheimer's patients. Those sturdy exterior proteins appear to protect bacteria against the destructive properties of ...
Health groups want the FDA to ban a key chemical used to decaffeinate coffee due to cancer concerns. Here's what you should know about whether decaf coffee is safe.
O.J. Simpson, the former NFL star and broadcaster whose athletic achievements and fame were eclipsed by his 1995 trial in the brutal killings of his ex-wife Nicole Brown Simpson and her friend Ron ...
"The retina is an extension of the brain, so it's actually neurological tissue, and when you damage that, it doesn't always come back," Benner said. "If you damage one cell, that cell ...