- Getting pregnant
- Preschooler
- Life as a parent
- Baby essentials
- Find your birth club
- Free antenatal classes
- Meet local parents & parents-to-be
- See all in Community
- Ovulation calculator
- Am I pregnant quiz
- How to get pregnant fast
- Best sex positions
- Signs of pregnancy
- How many days after your period can you get pregnant?
- How age affects fertility
- Very early signs of pregnancy
- What fertile cervical mucus looks like
- Think you're pregnant but the test is negative?
- Faint line on pregnancy test
- See all in Getting pregnant
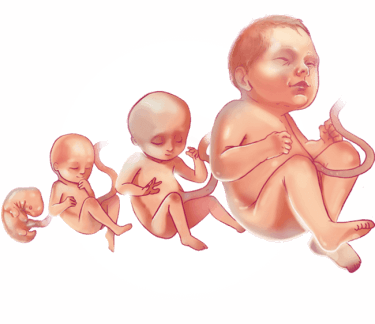
- Pregnancy week by week
- How big is my baby?
- Due date calculator
- Baby movements week by week
- Symptoms you should never ignore
- Hospital bag checklist
- Signs of labour
- Your baby's position in the womb
- Baby gender predictor
- Vaginal spotting
- Fetal development chart
- See all in Pregnancy
- Baby names finder
- Baby name inspiration
- Popular baby names 2022
- Numerology calculator
- Gender-neutral names
- Old-fashioned names
- See all in Baby names
- Your baby week by week
- Baby milestones by month
- Baby rash types
- Baby poop chart
- Ways to soothe a crying baby
- Safe co-sleeping
- Teething signs
- Growth spurts
- See all in Baby
- Your toddler month by month
- Toddler development milestones
- Dealing with tantrums
- Toddler meals
- Food & fussy eating
- When to start potty training
- Moving from a cot to a bed
- Help your child sleep through
- Games & activities
- Vomiting: what's normal?
- See all in Toddler
- Your child month by month
- Food ideas & nutrition
- How kids learn to share
- Coping with aggression
- Bedtime battles
- Anxiety in children
- Dealing with public tantrums
- Great play ideas
- Is your child ready for school?Top tips for starting school
- See all in Preschooler
- Postnatal symptoms to watch out for
- Stitches after birth
- Postpartum blood clots
- Baby showers
- Sex secrets for parents
- See all in Life as a parent
- Best baby products
- Best formula and bottles for a windy baby
- Best car seats if you need three to fit
- Best nappies
- Best Moses baskets
- Best baby registries
- Best baby sleeping bags
- Best baby humidifier
- Best baby monitors
- Best baby bath seat
- Best baby food
- See all in Baby essentials
- Back pain in pregnancy
- Pelvic girdle pain
- Perineal massage
- Signs you're having a boy
- Signs you're having a girl
- Can you take fish oil while pregnant?
- 18 weeks pregnant bump
- Can you eat salami when pregnant?
- Edwards' syndrome
- Missed miscarriage
- Should I harvest my colostrum?
- Rhesus positive vs. Rhesus negative
- What do contractions feel like?
- Hunger in early pregnancy
- First poop after birth
- When do babies sit up?
- When can babies have salt?
- MMR vaccine rash
- Vaping while breastfeeding
- How to transition from formula to milk
- When do babies start grabbing things?
- Sperm allergy: can sperm cause itching?
- How long after taking folic acid can I get pregnant?

Making the most of your midwife after birth

When will my midwife visit me after my baby's been born?
What tests and checks will my midwife carry out, what will happen at my first midwife appointment after my baby's birth, what information will my midwife give me, when will my midwife discharge me, what sort of questions can i ask my midwife, i'm struggling to cope with being a new parent. should i tell my midwife, feeding your baby, your baby’s health.
- whether your baby's umbilical cord stump has fallen off, and how the area's healing
- the number of wet and soiled nappies your baby’s having each day
- the colour of your baby’s skin, in case of jaundice
- that your baby’s eyes and mouth don't have any signs of infection
- inside your baby’s mouth for signs of tongue-tie , if they are struggling to feed
Your physical health
- signs of an infection, bleeding and vaginal discharge
- leaking wee after giving birth (stress incontinence)
- being unable to wee (urinary retention)
- constipation after birth
- sore nipples
Your mental health
- eating healthily
- staying active
- your lifestyle, including how much alcohol you drink and whether you smoke or take illegal drugs
- your contraceptive options
- resuming your sex life
- your baby’s immunisations
- I'm breastfeeding, but I want my partner to feed our baby too. Can I express ? Try to wait until your baby's about eight weeks old before offering them a bottle. Putting them to the breast is the most effective way to establish breastfeeding. There's plenty of things your partner can do in the early days, such as changing their nappy or doing skin-to-skin .
- Can I give my newborn a bath ? You can, but you don’t need to bath them every day. In the first week or so you may find it easier to wash their face, neck, hands and bottom carefully instead. This is sometimes called topping and tailing.
- My baby keeps crying. What can I do? Crying is your baby's main means of communication. As they can't talk, it's the only way they can let you know that they need something. It could be a feed, a nappy change, or just a cuddle. Watch our video for more on why your baby cries .
- How do I get my baby into a routine ? The simple answer is that you can't yet. Until your baby's about three months old, you'll probably find that no two days and nights are the same.
- My baby hasn’t had a poo today. Is there something wrong? Don’t worry, not all babies poo every day - or even every other day. It doesn’t mean there's anything wrong. Mention it to your midwife or health visitor at your next appointment.
- I have passed a blood clot. What should I do? If the blood clot is bigger than a 50p coin then call your midwife for advice. Keep your pad if you were wearing one at the time. Your midwife will ask you lots of questions and may visit if they feel it's necessary.
- I've had a c-section and I'm worried that my stitches are going to come undone. After a c-section you'll be able to see the continuous stitch that closes the skin. But underneath this, your muscle has also been stitched. So although it may feel strange, rest assured that your tummy won't suddenly open up. If you notice holes appearing along your wound, call your midwife for advice.
- What exactly is the fourth trimester?
- Life hacks for your baby's first three months
- Six ways to beat new-parent stress
- Find out How to create a safe sleep environment for your baby
Was this article helpful?
Parents’ tips: mums’ guide to the fourth trimester

Bleeding after birth (lochia)

Should I give my baby a dummy to help her sleep?

High blood pressure in pregnancy (gestational hypertension)

Francesca Whiting is digital content executive at BabyCentre. She’s responsible for making sure BabyCentre’s health content is accurate, helpful and easy to understand.
Where to go next

Ready Steady Baby
Home visits.
You should be visited several times by your midwife or family nurse at home during the first 10 days. Friends and family will want to visit to meet your baby too.
It’s OK to ask visitors to:
- call you first and to sometimes say no
- help with other things so you can have a rest or spend time with your baby
Extra support
Some new parents need more support than others. You’ll get extra support from your midwife, family nurse or other health professionals if your baby:
- was born early
- spent time in special or intensive care
- has additional needs
Tests and checks
During the first 10 days your midwife will:
- weigh your baby
- do a newborn blood spot test if you agree
You’ll also need to register your baby with a GP
More about newborn blood spot tests
Your health visitor
A health visitor’s a registered nurse or midwife who’s done further study in public health nursing.
Your health visitor will:
- take over from your midwife when your baby’s 11 days old
- get to know you and your baby
- ensure you get all the help and support you need as your baby grows
Your baby’s named person
In Scotland, the aim is that every child, young person and their parents have a `named person’ who is a clear and safe point of contact to seek support and advice about any aspect of your child’s wellbeing.
From when your child is born until they start school, your named person is your health visitor.
Your baby’s named person will:
- be a good person for you to ask for information or advice about being a parent
- talk to about any worries
- support you to look after yourself and your baby
They can also:
- put you in contact with other community professionals or services
- help you make the best choices for you and your family
The Red Book
You’ll be given a personal child health record called the Red Book. You can use it to record information about your baby’s growth, development, tests and immunisations.
Keep it safe and take it to any appointments you have with a healthcare professional.
The family nurse

Family nurses offer the Family Nurse Partnership (FNP) programme to young, first-time parents from early in their pregnancy until their child’s 2 years old. This program is available to first-time parents under the age of 20.
The programme includes home visits from a family nurse while you’re pregnant, and after your baby’s born. These visits help:
- to have a healthy pregnancy
- you and your baby grow and develop together
- you to be the best parent you can be.
Your health visitor will take over from your family nurse when your baby is two until they go to school.
The Scottish Government has more information about Family Nurse Partnership
Translations and alternative formats of this information are available from Public Health Scotland .
If you need a different language or format, please contact [email protected].
- Ready Steady Baby leaflet in Arabic, Polish, Simplified Chinese (Mandarin) and Ukrainian
- Ready Steady Baby leaflet in English (Easy Read)
Source: Public Health Scotland - Opens in new browser window
Last updated: 19 December 2023
Help us improve NHS inform
Your feedback has been received
Don’t include personal information e.g. name, location or any personal health conditions.
Also on NHS inform
Other health sites.
- Disabled Living Foundation (DLF)
- Rica: consumer research charity
- Health & Care Professions Council (HCPC)

A Vital Climate Solution

Climate change poses the greatest health challenge of our era, manifesting in increased heatwaves and natural disasters that disproportionately affect women and babies. We recognise that midwives are a vital solution in adapting health systems to climate change, and lowering carbon emissions overall. Midwives deliver safe and environmentally sustainable health services, help communities adapt to climate change and are first responders during climate disasters. For this reason, the theme for this year’s International Day of the Midwife (IDM), is Midwives: A Vital Climate Solution.
A message from ICM President, Sandra Oyarzo Torres
It’s the time of the year when we celebrate the work of midwives everywhere. IDM is a day of celebration, but also of highlighting how important the work of midwives is globally. This year, we are shining a light on the role midwives play in addressing the greatest health challenge of our time – climate change. #IDM2024 is both a celebration and a call to action for our planet and for midwifery.
As midwives, we might not always see ourselves as climate champions, but the evidence is clear. Continuity of midwife care enhances health outcomes, and contributes to environmental sustainability and adaptability by reducing the carbon footprint of health services and making them more climate resilient. As midwives, we also play a crucial role in responding to the climate crisis, providing essential care in times of climate-related disasters.
For midwives to become the workforce that our warming world needs, we need investment, resources, autonomy, recognition, and a seat at every decision-making table. It’s essential that our contributions are acknowledged, and our voices are heard in shaping policies and practices that support midwives to provide quality, accessible sexual, reproductive, maternal, newborn and infant health, that are also sustainable for our planet.
As we celebrate #IDM2024, let’s applaud midwives and advocate for the changes needed to ensure a sustainable future for midwifery and our planet. Join us to call for a future where continuity of midwife care is integral to climate-resilient health systems.
Happy IDM! Sandra Oyarzo Torres ICM President

Join us to advocate for midwives as a vital climate solution
We have prepared a set of social media messages and graphics to support our collective advocacy and celebrate the role of midwives as a vital climate solution.
Copy our messages, download our graphics, and share before, during, and after 05 May 2024. You can also download all the illustrations and social media banners in the section below. We have also prepared templates where you can enter the messages in your own language.
We encourage all midwives and partners to join us in this celebration and to advocate for action towards a healthier planet and healthier communities.
Together, we can create a more sustainable future. #IDM2024 #MidwivesAndClimate
Share our social messages and graphics
Midwives deliver environmentally sustainable health services and play a key role in making health systems more climate resilient. 🌍💪 During climate crises, midwives can adapt to ensure safe, respectful, and quality care for women and gender diverse people.️
Put simply, midwives are a vital climate solution.
Join #IDM2024 to champion investment, resources, autonomy, recognition, and representation for midwives. #MidwivesAndClimate

#IDM2024: Midwives, a vital climate solution! 🌎🌿
We deliver environmentally sustainable health services, making health systems more climate resilient.
In a warming world, we can adapt to ensure women and gender-diverse people get safe, respectful & quality care.
Midwives provide climate-friendly #SRMNAH. 🌍🌱
By providing services in communities where people live, we reduce the need for travel to health facilities. Having access to the care of a midwife ensures that the time and expertise of obstetricians is more available to women with complex care needs. This reduces the carbon footprint of health services and making them more sustainable and accessible for everyone.
#IDM2024 #MidwivesAndClimate

Midwives provide climate-friendly #SRMNAH
By working in communities, we reduce travel to health facilities.
Continuity of midwife care also ensures OB-GYNs can focus on complex health needs, reducing carbon emissions & promoting sustainable health services.
Healthcare services are responsible for 5% of greenhouse gas emissions globally. 🌍⚠️
Continuity of midwife care improves maternal health outcomes and ensures more babies are born alive, on time and healthy.
Better health outcomes mean mothers and babies are less likely to need medical care in the short- and long-term. This reduces the use of medical resources and limits medical waste.

Health services are responsible for 5% of carbon emissions. 🌍⚠️
Midwife care enhances maternal and newborn health, leading to better health outcome in the short and long term.
We use less resources and create less waste.
Midwives help mothers meet their breastfeeding goals – usually breastfeeding for longer. 🤱🏾
Breastfeeding doesn’t require packaging or shipping, it saves water and improves the health of women and babies.
Midwives supporting women to breastfeed successfully is good for babies, women and the planet!

🤱🏽 Midwives help women meet their breastfeeding goals, saving resources like packaging, shipping, and water.
This supports the health of mums, babies, and the planet! 🌍
Midwives are sexual and reproductive health champions. 💪🏽
We provide education, contraception, comprehensive abortion care and support, enabling women to manage their own reproductive health. This promotes women’s rights and economic resilience, while and reducing their vulnerability to the impacts of climate change.

Midwives are #SRH champions!
We offer education, contraception, comprehensive abortion care, & support, empowering women to manage their reproductive health. 💪🏻
This not only promotes women’s rights, economic resilience, it reduces vulnerability to climate change impacts.
Community-based midwives can more easily reach areas affected by climate disasters 🌪️, and quickly provide essential reproductive and maternal health services. We are a valuable network for evidence-based information and supply distribution, ensuring that women and babies have access to care during the worst consequences of our warming world. 🌡️
By resourcing midwifery services, funders and healthcare systems are supporting providers capable of coordinating effective crisis response plans.
#IDM2024 #MidwivesAndClimate 🌿

Community midwives can play a vital role in reaching areas hit by climate disasters, swiftly offering essential reproductive & maternal health services.
If enabled we can deliver care, information & supplies during climate emergencies. 🌡️
Download assets
Join idm events around the globe.
ICM represents over 140 midwives’ associations (MAs) across more than 120 countries. From parades to pop-up midwifery clinics, many of our associations host their own IDM celebrations and we’re excited to provide our community with a platform to promote their fantastic events and initiatives. If you’re an ICM midwives’ association, fill out this form to share your IDM event here.
Midwifing the Midwife: Key Elements to Scaling Up and Sustaining our Workforce
In celebration of International Day of the Midwife 2024, GOLD Learning is excited to welcome Midwife Ginger Breedlove as she shares her new presentation titled “Midwifing the Midwife: Key Elements to Scaling Up and Sustaining our Workforce”.
IDM: Stories of (Climate) Resilience
Learn how these resilient midwives empower their communities and inspire others to take action in addressing the climate crisis. We will also screen “Neha,” a short documentary showcasing Neha Mankani’s remarkable work taking maternal and newborn health services to communities affected by floods in Pakistan.
ABENFO Obstetric and Neonatal Nursing Training Symposium
The 1st ABENFO Symposium on Training in Obstetric and Neonatal Nursing aims to bring together coordinators, teachers and students to advance training in obstetric and neonatal nursing and strengthen the speciality.
Midwives for Women 2024
The main objective is to promote a discussion, share knowledge and investigate workable alternatives to improve the quality of healthcare services for mothers and their reproductive rights. Through keynote presentations, panel discussions and workshops.
IV Virtual Congress of Professional Midwifery of Guatemala
Every year around 5th of May, International Day of the Midwife, the Association of Professional Midwives of Guatemala – APPG holds its congress, this is an event to meet, share and continue to grow professionally with topics of national and international interest.
IDM: Midwives – the workforce we need for a warming world
This event, part of our 2024 International Day of the Midwife celebrations, will offer a unique opportunity to explore how midwives, as the frontline workforce, are not only first responders to climate catastrophes but also integral contributors to health systems striving to become more sustainable.
Midwife in the midst of war
For International Day of the Midwife 2024, the Ukrainian Midwives Union shares the incredible work midwives do every day. Therefore, they invite you, your colleagues, and anyone interested in midwifery, women’s health support, and the situation in Ukraine to attend an online meeting titled “Midwife in the Midst of War”.
Share this website to social media
Subscribe to our newsletter, what does it mean to be an icm member association.
Becoming a member association of the International Confederation of Midwives entitles you to a long list of exclusive benefits. These benefits focus on professional development, networking, leadership opportunities, association support and funding, and much more.
Find out how to take advantage of these diverse benefits to enhance the knowledge of your Association and your members, advance the midwifery profession, and champion evidence in public policy.

First Prenatal Visit: What Happens & How to Prepare
The first prenatal care visit is an exciting time but you may not know what to expect or how to prepare. Here’s an overview of what to expect.
- Written by Genevieve Howland
- Updated on May 24, 2019

From the time you pee on that pregnancy test to actually going to your first prenatal visit seems like an eternity. It. is. BRUTAL! I remember calling my midwife all giddy when I told her that I was pregnant and she said “I’ll see you in 10 weeks.” TEN WEEKS?!?! Are you crazy? What if something happens to the baby? What happens if I mess something up? What? Wha? Wha?
Then I remembered to breath… and I realized that there really isn’t anything a midwife could do to “save” my baby in these very precious early weeks. And so I surrendered. And waited. And wondered. What do I need to bring to my first prenatal visit? Can I prepare in any way? And what exactly goes on during the first prenatal visit?
Here’s what you can expect and how you can prepare.
When is my first prenatal visit?
Typically women see their healthcare provider for prenatal care between 8 and 12 weeks. If you are seeing a midwife they may suggest you wait until 10 – 12 weeks for your first appointment. This is because this is about the time when you can hear your baby’s heartbeat on a doppler. Don’t be sad or scared if they still can’t find the heartbeat, as it is really more like 12-14 weeks for a definite reading.
Many OBs and even family doctors expect you to schedule your first prenatal care appointment much earlier than this though.
An ultrasound can pick up a heartbeat as early as 6-7 weeks, and some women are led to believe that an early ultrasound is necessary for a healthy pregnancy. This analysis shows that routine ultrasound does not improve perinatal outcomes while this analysis shows no improvement in maternal outcomes.
Here’s a post dedicated to the risks vs. rewards of baby ultrasounds .
Another reason that some doctors want you to schedule an earlier appointment is for a full pelvic exam. The reasoning is that, for some women, prenatal care is their first or only chance to see a doctor and undiagnosed STDs can be dangerous for the baby.
Your provider may also take the opportunity to do a pap smear to check for cervical cancer. However, vaginal exams do carry a small risk of infection, so if you are relatively healthy and don’t have a history of ectopic pregnancy or other serious concerns, then you are probably fine to wait until around 12 weeks.
What should I expect at my first prenatal visit?
What happens during the first visit will vary from provider to provider, but for the most part you can expect to do four main things.
1. Build a relationship
One of the advantages to using midwives is that you have continuity of care, meaning that the midwife you see at each (or most) appointments will be the one who attends your birth. Even in a larger office with multiple midwives, at least each appointment was nice and long with plenty of time to talk and bond with these awesome ladies. By the end of my pregnancy, I knew I was in good hands no matter which midwife was on call and this is a very good feeling!
At the first prenatal visit you can get to know your midwife or doctor, learn about her background, and begin to build a relationship of trust. You can ask questions and get information on good books to read or specialists you may want to see during your pregnancy, such as a chiropractor or lactation consultant .
If you are using a family doctor, then you may have a similar continuity of care. With OBs in hospitals you aren’t likely to be able to choose the OB that attends your birth, so a prenatal visit won’t always focus on this kind of relationship building.
2. Assess your health
Your midwife will ask about your health history, family health history, and present health to get a baseline for what is normal for you. She will counsel you on nutrition, exercise and holistic healing and wellness. She will address common pregnancy complaints and offer holistic, natural remedies.
She will also ask if you are having unusual symptoms that may be a sign of something serious. Headaches are common in early pregnancy, but can also be a very early sign of preeclampsia. Your midwife will want to know if you are having headaches or other symptoms and will keep a record of them.
3. Routine tests
Your midwife will order a different blood tests that will tell her your blood type, red and white blood cell counts, hematocrit, hemoglobin, and platelet count. Your midwife needs to know your blood type for your safety, but the other tests should be optional.
These blood tests will also tell your midwife if you are Rh positive or negative. If you are positive (or you are negative and your partner is negative) you have nothing more to do. If you are negative and your partner is positive or you don’t know, your midwife may discuss your receiving an Rhlg shot to prevent any complications.
Your midwife will also tests for various Sexual Transmitted Diseases like syphilis, gonorrhea, chlamydia, which could harmfully affect your pregnancy if not treated. She will also take your blood pressure, pulse, weight, and check the baby’s heartbeat if you are ok using a doppler, which contains ultrasound waves. I chose to use the doppler for the first appointment so I could really believe I was pregnant and then waited till 20 weeks to use the fetoscope for the baby’s heartbeat.
She may palpate your abdomen to check the fundal height (a measure of the size of your uterus). She will rule out any medical problems that may affect your pregnancy and assess whether a homebirth or birth center birth is safe for you (it usually is).
You will also be asked to test your urine for the presence of protein (a sign of toxemia), sugar (a sign of gestational diabetes), or bacteria (a sign of Group B Strep positive). You will pee into a cup and dip a test strip in. Depending on the brand of test strips you will read it after 60 second or immediately. You will do this test at every appointment until birth.
4. Paperwork
At your first prenatal visit you will probably have some paperwork to sign and your midwife or doctor’s office will probably need a copy of your health insurance card. Many midwives will give you an estimate costs for your pregnancy and birth care, so you are both on the same page in terms of cost.
Pregnant? Get my FREE week-by-week updates! – Week by Week Promo [In-article]
Track your baby’s growth, find safe and natural remedies, and have fun along the way!
How can I prepare for my first prenatal visit?
Prepare your questions.
Your first prenatal care appointment may be the first time you meet your midwife or doctor, so it’s a good idea to have questions prepared in order to get a feel for your provider’s background and philosophy. If you are seeing a doctor, ask what her thoughts are about: labor induction , ultrasounds, the glucola drink, treating GBS+ during birth, and natural childbirth in general. You can use these questions as a guide to see if your healthcare provider is a good fit for you.
If you’ve already interviewed your practitioner, you still may have some questions about what to expect during your pregnancy, what symptoms or concerns you may have, or how many weeks pregnant you may be.
I wrote down questions beforehand so that I wouldn’t forget anything during the actual appointment (between excitement, nervousness and pregnancy brain , I had a feeling I would forget a thing or two!)
Gather health info
Ask family members about pregnancy related health concerns that may run in the family. Write down any patterns of health you notice. Also take note of your partner’s family health history, especially genetic diseases. My mom had two c-sections so I wanted to get my midwife’s thoughts on if she thought I could have a vaginal birth.
Write down any past gynecological history, like an abnormal pap smear or a previous pregnancy or miscarriage. Write down any medications you are taking.
If you don’t know your due date, use our due date calculator before your appointment. If you do know your due date and want to know when you most likely conceived, use our reverse due date calculator . And here’s an article for you if you’re unsure how many weeks pregnant you are .
Do your research for prenatal care
Do your best to pick the practitioner who is right for you. But if you go to your first visit and don’t like him or her, remember that you can change at any time! My dear friend changed her care at 34 weeks! And she was so happy that she did.
Your midwife needs to know your blood type for your safety, but the other tests should be optional. A good practitioner will let you know at each appointment what tests or procedures will be coming up at the next appointment so you can have time to research and decide what’s best for you.
A good practitioner should also be able to guide you and answer any questions you have about tests and procedures.
Best wishes for your first prenatal visit!
The first prenatal care visit is an amazing and nerve-wracking time. You may get to hear the heartbeat for the first time! That’s why I would encourage your partner to come along for that first prenatal visit. Hearing your child’s heartbeat for the first time, together as parents, is truly a special and sacred moment. Plus, you now have more “proof” that you really are pregnant.
Knowing what to expect and how to prepare should ease your mind and let you enjoy the excitement of your pregnancy!
- https://www.emedicinehealth.com/complete_blood_count_cbc/article_em.htm
- Beech, BL. Ultrasound unsound? Association for Improvements in the Maternity Services. 1996
Read This Next…
- Constipation in Pregnancy: Natural Ways to Get Things Moving
- 9 Signs You’re Having a Girl (Plus How Accurate They Really Are!)
- Cramps During Pregnancy: What’s Normal? And What’s Not?
- How Accurate Are Pregnancy Tests?
- When Will My Baby Be Born? How Accurate Is Your Due Date?
- See 4 Comments
Add Comment
About the author.
Genevieve Howland is a childbirth educator and breastfeeding advocate. She is the bestselling author of The Mama Natural Week-by-Week Guide to Pregnancy and Childbirth and creator of the Mama Natural Birth Course . A mother of three, graduate of the University of Colorado, and YouTuber with over 130,000,000 views, she helps mothers and moms-to-be lead healthier and more natural lives.
Meghan Quinn Jan 18 at 10:57 pm
Thank you for this info on what to expect! It eases my mind a bit.
Taylor Bishop Oct 26 at 11:22 am
I just wanted to thank you for going over what to expect for a prenatal visit. I didn’t know that it could be beneficial to maybe schedule this maybe 6-7 weeks in a pregnancy. My sister has been thinking of getting pregnant, so this could be good for her to know in the future.
Kendal Mar 12 at 8:52 pm
Thank you–I just had my first prenatal appointment, and this was really helpful! So glad I found your blog at the right time! I also was having trouble believing I was really pregnant, so it was relieving to see you wrote that same thought, and it helped me not feel so bad about also wanting the doppler to hear the heartbeat. Amazing!!
Sarah F. Feb 24 at 11:39 am
My first prenatal appointment led me to calling a local birth center for a meet and greet. My doctor, who I adore, suddenly became very pushy about flu shots. My (shy and quiet) husband had to argue with her about why I don’t get flu shots because after I told her I didn’t want it (they make me horribly sick, and I’d already been sick with bronchitis for 6 weeks), she ordered it anyway, until the husband put his foot down for me. I was on edge about hospital delivery before I even became pregnant, but it worries me that I couldn’t get my own doctor to listen to me over a flu shot. And there was no conceivable way for me to meet with more than 2 of the midwives and none of the OBs before I deliver in August! Hopefully everything clicks at the birth center and I can deliver there. Everyone I know who’s gone there has been thrilled with the care, and the hospitals around here seem quite notorious for C-sections. I wish my doctor had made me feel more confident, but I’m so much more comfortable with the idea that birth is normal and not a medical emergency.
Cancel Reply
Your email address will not be published. All fields are required *
Your Comment *
See What’s Up With You & Baby Right Now - Week by Week Grid
Just tap your week of pregnancy:
- 1 st trimester
- 3 weeks -->
- 4 weeks -->
- 5 weeks -->
- 6 weeks -->
- 7 weeks -->
- 8 weeks -->
- 9 weeks -->
- 10 weeks -->
- 11 weeks -->
- 12 weeks -->
- 13 weeks -->
- 2 nd trimester
- 14 weeks -->
- 15 weeks -->
- 16 weeks -->
- 17 weeks -->
- 18 weeks -->
- 19 weeks -->
- 20 weeks -->
- 21 weeks -->
- 22 weeks -->
- 23 weeks -->
- 24 weeks -->
- 25 weeks -->
- 26 weeks -->
- 27 weeks -->
- 3 rd trimester
- 28 weeks -->
- 29 weeks -->
- 30 weeks -->
- 31 weeks -->
- 32 weeks -->
- 33 weeks -->
- 34 weeks -->
- 35 weeks -->
- 36 weeks -->
- 37 weeks -->
- 38 weeks -->
- 39 weeks -->
- 40 weeks -->
- 41 weeks -->
The world’s first natural pregnancy week-by-week. #1 bestseller. Over 125,000 copies sold!
Baby name finder.
Discover thousands of unique and popular baby names with Mama Natural’s NEW Baby Name Finder.
Trending Girl Names
Trending boy names.
International Day of the Midwives
Welcome to the #idm2022 digital toolkit.
Use the below social media messages and graphics to advocate for midwives and midwifery on and beyond 5 May 2022. For additional resources to plan your #IDM2022 activities
You're invited! ICM's #IDM2022 Virtual Party ? ?
On 05 May 2022, we invite our global midwife community to tune into our #IDM2022 virtual party where will celebrate ICM’s 100th anniversary and the accomplishments of our member associations around the world.
Please note that we will hold this event twice to accommodate time zones around the world. Feel free to RSVP to and attend whichever event best fits your schedule. We can’t wait to see you there!
RSVP for ICM Member Associations ????????
Register for the event here (CEST Afternoon) Register for the event here (CEST Evening)
RSVP for all other ICM Partners and Stakeholders ????????
RSVP to ICM’s #IDM2022 Virtual Party (CEST Afternoon) RSVP to ICM’s #IDM2022 Virtual Party (CEST Evening)
Download Social Media Messages
On #IDM2022, imagine a world where we’ve achieved the investments we deserve. #ImagineIfMidwives had:
?? Equal, fair compensation ?? Fair working conditions and protections ?? Standardised regulation & education frameworks
If we can dream it, we can do it. #ICM100

? #ImagineIfMidwives were not oppressed by a hierarchical, #patriarchal health system. How much more could we accomplish with policy that promotes #genderequality? #Midwives in resourced leadership would ensure fair representation of women in health policy. #ICM100 #IDM2022.
? #ImagineIfMidwives were supported to perform their full scope of practice. Policies that allow #midwives to perform their full scope of practice strengthen primary healthcare systems and provide a pathway to ✨universal health coverage✨ #ICM100 #IDM2022 #SDGAction #UHC

? #ImagineIfMidwives were recognised as autonomous healthcare professionals, no longer conflated with nurses and obstetricians.
More women would receive high-quality #SRHR by the care provider most qualified to deliver these services: a #midwife. #ICM100 #IDM2022
? #ImagineIfMidwives were supported by a regulation framework based on @world_midwives Global Standards for Midwifery Regulation.
Women and birthing people everywhere would benefit from life-enhancing, professional #midwifery care #ICM100 #IDM2022 ⬇️
http://ow.ly/BSaE50HMPgH

? #ImagineIfMidwives had equal access to ongoing midwifery #education, as per @world_midwives standards.
ALL families would have access to culturally relevant, professional #SRHR, and maternal health outcomes would be improved all over the ?? #ICM100 #IDM2022
? #ImagineIfMidwives were recognised for what they are: a pathway to achieving the #SDGs. #SDGAction #ICM100 @UN
? SDG #3.1 is to reduce maternal mortality. Investing in #midwives would avert 2 thirds of maternal & newborn deaths by 2035. #PUSHForMidwives #IDM2022
? #ImagineIfMidwives were recognised for what they are: a pathway to achieving the #SDGs. @UN #SDGAction #ICM100 #IDM2022
SDG #3.7 is to ensure universal access to sexual and reproductive healthcare services by 2030. #Midwives = high-quality, culturally relevant, local #SRHR
? #ImagineIfMidwives were recognised for what they are: a pathway to achieving the #SDGs. @UN #SDGAction #ICM100
SDG #3.8 is to achieve #UHC by 2030. Investing in #midwives strengthens primary healthcare systems and provides a pathway to ✨universal health coverage✨ #IDM2022
In 2021, @world_midwives, @UNFPA & @WHO published #SoWMy2021, underscoring the life-saving role of midwives.
#ImagineIfMidwives were supported by governments all over the ?:
✔️ We could save 4.3 million lives per year.
#IDM2022 #ICM100 http://ow.ly/yfvF50HMVMM

#ImagineIfMidwives had already received the investment & support they need. The #COVID19 pandemic would not have had nearly the same impact on our healthcare systems as it has.
Investing in midwives strengthens primary healthcare. Midwives=sustainable healthcare #IDM2022 #ICM100
Women NEED #midwives for their health & wellbeing. But what do midwives need in order to be there for women & other birthing people?
The results of @WRAglobal & @world_midwives’s Midwives’ Voices Midwives’ Demands survey are in ⬇️ #IDM2022 #ICM100 http://ow.ly/mkoJ50I7Ujq

The results are in! Happy #IDM2022 ?
What do #midwives all over the world want in order to continue their life-enhancing work? @WRAglobal & @world_midwives conducted the “Midwives’ Voices Midwives’ Demands” survey to find out.
Results ⬇️ #ICM100
http://ow.ly/mkoJ50I7Ujq
Listen up! We asked midwives around the world to raise their voices and tell us what they want and need. Over 50,000 midwives responded across 101 countries – find out what midwives want ⬇️ #IDM2022 #ICM100
Maybe something like this that includes the # of country responses ? [GU1]

?? Equal, fair compensation ?? Fair working conditions and protections ?? Standardised regulation frameworks ?? Equal opportunities to local, standardised education
Our world would look so much different. But if we can dream it, we can do it. #IDM2022 #ICM100 #PUSHForMidwives

? #ImagineIfMidwives were not oppressed by a hierarchical, #patriarchal health system and not conflated with other professions. How much more could we accomplish with policy that promotes #genderequality?
For starters, with equal pay and policies that protect midwives against gender-based abuse and harassment, #midwives would be well supported and could save 4.3 million lives per year by 2035. #ICM100 #PUSHForMidwives #SDGAction #IDM2022 #SoWMy2021

? #ImagineIfMidwives were supported to perform their full scope of practice. What if they were recognised as autonomous practitioners and the lead healthcare professional responsible for planning, organising and delivering care to women from the initial booking of antenatal visits through to the postnatal period?
Evidence demonstrates that in order to improve maternal and neonatal health and to meet the Sustainable Development Goals, midwife-led continuity of care is crucial. Policies that support #midwives and allow them to perform their full scope of practice would strengthen primary healthcare systems all over the world ??? and foster happier, healthier families and communities. #ICM100 #PUSHForMidwives #SDGAction #UHC #IDM2022

? #ImagineIfMidwives were recognised as distinct, autonomous healthcare professionals, no longer conflated with nurses, obstetricians or other healthcare providers.
More women would receive high-quality #SRHR by the care provider most qualified to deliver these services: a #midwife. #ICM100 #IDM2022 #PUSHForMidwives

? #ImagineIfMidwives were recognised and funded for what they are: a pathway to achieving the #SDGs. @UN #SDGAction #ICM100
Sustainable Development Goal #3.1 is to reduce the global maternal mortality ratio to less than 70 per 100,000 live births by 2030. Fully investing in midwives would avert roughly two thirds of maternal, new-born deaths and stillbirths by 2035, saving 4.3 million lives per year. #PUSHForMidwives #IDM2022

? #ImagineIfMidwives were recognised for what they are: a pathway to achieving the #SDGs. @United Nations #SDGAction #ICM100
Sustainable Development Goal #3.8 is to achieve universal health coverage by 2030. A larger, fully enabled #midwifery workforce would increase women’s, children’s and adolescents’ access to health care. That is to say: investing in #midwives will strengthen the primary healthcare system and provide a pathway to ✨universal health coverage✨. #PUSHForMidwives #UHC #IDM2022
Sustainable Development Goal #3.7 is to ensure universal access to sexual and reproductive health-care services by 2030. The #midwife, by virtue of her education, sphere, scope of practice and unique relationship with women and their families is in an ideal position to provide the information, services and support which women need in planning their families, as well as to influence the type of services which are available to them. #PUSHForMidwives #SRHR #IDM2022
? #ImagineIfMidwives were supported by a regulation framework based on the @International Confederation of Midwives Global Standards for Midwifery Regulation (linked below).
The standards of #midwifery practice all over the globe ??? would be raised. Women and other birthing people everywhere would benefit from life-enhancing, professional #midwifery care #ICM100 #IDM2022 ⬇️

? #ImagineIfMidwives had equal access to ongoing midwifery #education, according to the @International Confederation of Midwives’ standards & competencies.
Not only would #midwives have greater career satisfaction and longevity, but ALL families would have access to culturally relevant, professional sexual and reproductive healthcare, and maternal health outcomes would be improved all over the world ? #ICM100 #PUSHForMidwives #IDM2022
In 2021, @world_midwives, @UNFPA and @WHO published the State of the World’s Midwifery report #SoWMy2021. The data was shocking, but also hopeful. It went like this:
#ImagineIfMidwives were supported and invested in by governments all over the world. We would see the following by 2035:
✔️ 4.3 million lives saved every year ✔️ 1.9 million stillbirths averted every year ✔️ 2 million neonatal deaths averted every year ✔️ 280K maternal deaths averted every year
The #SoWMy2021 report called on governments, policymakers, regulatory authorities, educational institutions and international and civil society organizations to turn their focus to paving the way toward universal access to sexual, reproductive, maternal, newborn and adolescent health services, addressing equity at all levels and leaving no one behind.
That way just isn’t possible without #midwives. #IDM2022 #ICM100
http://ow.ly/yfvF50HMVMM

? #ImagineIfMidwives had already received the investment and support they need when the #COVID19 pandemic hit. The virus would not have had nearly the same dire impact on our healthcare systems as it has.
A larger, fully supported #midwifery workforce would increase women’s, children’s and adolescents’ access to healthcare through #midwives, decreasing the number of patients turning to hospitals and general practitioners to provide this care. This would thus alleviate strain on hospitals by opening more hospital beds to COVID-19 patients.
Investing in midwives strengthens primary healthcare systems. It’s simple: Midwives = #sustainable healthcare. #IDM2022 #SDGAction #ICM100
@White Ribbon Alliance & @International Confederation of Midwives created the ‘Midwives’ Voices, Midwives’ Demands survey and asked over 50,000 midwives across 101 countries just that — today, we’re sharing their responses.

We asked midwives around the world to raise their voices and tell us what they want and need. Over 50,000 midwives responded across 101 countries – find out what midwives want ⬇️ #IDM2022 #ICM100
Find out what midwives want #MVMD ⬇️ #IDM2022 #ICM100

What do #midwives all over the world want in order to continue their life-enhancing work? @White Ribbon Alliance & @International Confederation of Midwives conducted the “Midwives’ Voices, Midwives’ Demands” survey to find out. See the results ⬇️ #ICM100 #MVMD
Download Social Media Graphics
Share this website to social media, subscribe to our newsletter.

Recent Blogs

Midwifery Services
If you are interested in a holistic, low-intervention and highly supportive model of care, seeing a midwife may be for you. Midwives care for women from early adolescence through menopause, including prenatal care . They provide evidence-based medicine, encourage women to make informed decisions about their healthcare, and focus on patient participation and education.
Find out more about our services:
Conditions and consultations, diagnosis and treatments, midwifery care specialists.
- Midwifery locations near you
- Midwifery specialists near you
Midwives offer consultations and personal treatment plans for a variety of everyday female needs:
- Breast lumps
- Family planning
- Pregnancy prevention
- Sexual health issues
- Vaginal issues
Back to top
Our midwives offer:
- Birth control, including oral contraceptives, intrauterine devices or contraceptive implants and injections
- Breast care
- Breastfeeding assistance
- Gynecological preventive exams
- Labor and delivery at the birthing center
- Pelvic exams
- Postpartum care
- Preconception counseling
- Prenatal care for patients who are at low risk for complications
Midwives are advanced practice providers with specialized training, education and certification in women's health. They are qualified to prescribe and administer medications as independent, licensed practitioners. Midwives work to resolve your health concerns and refer you to other specialties as needed.
Additional care may be provided by:
- Birthing Centers
- Genetic Counseling
- Mammography
- Obstetrics & Gynecology
- Prenatal Care
- Reproductive Endocrinology
Referrals to a midwife are not required. Call the appointment number of your preferred midwifery location to learn more.
What should I bring for my first appointment?
For your first appointment, bring your current prescription information and medical records from non-Mayo Clinic Health System facilities. Complete a medical records release form to authorize the transfer of health records from another healthcare facility to us. Visit our Medical Record Forms page for this form and other forms in multiple languages.
What are my payment options, and do you offer financial assistance?
Visit the billing page of your preferred location for information on insurance, billing and payments.
We care for patients in difficult financial circumstances and offer financial assistance to those who have an established need to receive medically necessary services. Learn more about financial assistance options .
Can you provide a second opinion?
Yes — call the appointment number at your preferred midwifery location . See What should I expect during my first appointment? for tips on how to prepare.
Do you have an after-hours number in case of emergency?
Always call 911 in case of emergency. For after-hours help with other issues, review our convenient care options .
Explore locations or providers near you for details on midwifery:
Locations view more.

- 651-267-5600
- 608-392-9866
Providers View More

Related Upcoming Classes & Events View More
Childbirth education, breastfeeding your baby, nursing moms network - rice lake, newborn care.
Your antenatal appointments
You'll have a number of antenatal appointments during your pregnancy, and you'll see a midwife or sometimes an obstetrician (doctor specialising in pregnancy).
They'll check the health of you and your baby, give you useful information and answer any questions.
Pregnant employees have the right to paid time off for antenatal care.
This page lists the appointments you'll be offered and when you should have them.
If you're pregnant with your first baby, you'll have more appointments than those already with children.
First contact with midwife or doctor
Contact a GP or midwife as soon as possible after you find out that you're pregnant.
They should give you information about:
- folic acid supplements
- nutrition, diet and food hygiene
- lifestyle factors – such as smoking, drinking and recreational drug use
- antenatal screening tests
You should be told about the risks, benefits and limits of these tests.
Screening for sickle cell disease and thalassaemia should be offered before 10 weeks.
This is so you can find out about all your options and make an informed decision if your baby has a chance of inheriting these conditions.
It's important to tell your midwife or doctor if:
- there were any complications or infections in a previous pregnancy or delivery, such as pre-eclampsia or premature birth
- you're being treated for a long-term condition, such as diabetes or high blood pressure
- you or anyone in your family has previously had a baby with a health condition (for example, spina bifida)
- there's a family history of an inherited condition (for example, sickle cell or cystic fibrosis)
- you know that you're a genetic carrier of an inherited condition such as sickle cell or thalassaemia – you should also tell the midwife if you know the baby's biological father is a genetic carrier of these conditions
- you have had fertility treatment and either a donor egg or donor sperm
8 to 12 weeks: booking appointment
It's best to see your midwife or doctor as early as possible to get the information you need to have a healthy pregnancy.
Some tests, such as screening for sickle cell and thalassaemia, should be done before you're 10 weeks pregnant.
Your midwife or doctor should give you information about:
- how the baby develops during pregnancy
- nutrition and diet
- exercise and pelvic floor exercises
- antenatal screening tests
- your antenatal care
- breastfeeding, including workshops
- antenatal education
- maternity benefits
- your options for where to have your baby
Your midwife or doctor should:
- give you your handheld notes and plan of care
- see if you may need additional care or support
- plan the care you'll get throughout your pregnancy
- identify any potential risks associated with any work you may do
- measure your height and weight, and calculate your body mass index (BMI)
- measure your blood pressure and test your urine for protein
- find out whether you're at increased risk of gestational diabetes or pre-eclampsia
- offer you screening tests and make sure you understand what's involved before you decide to have any of them
- offer you an ultrasound scan at 11 to 14 weeks to estimate when your baby is due
- offer you an ultrasound scan at 18 to 21 weeks to check the physical development of your baby and look for 11 rare conditions
- ask about your mood to assess your mental health
- ask about any past or present severe mental illness or psychiatric treatment
This appointment is an opportunity to tell your midwife or doctor if you're in a vulnerable situation or if you need extra support.
This could be because of domestic abuse or violence, sexual abuse or female genital mutilation (FGM) .
FGM can cause problems during labour and childbirth, which can be life threatening for you and your baby.
It's important you tell your midwife or doctor if this has happened to you.
11 to 14 weeks: dating scan
This is the ultrasound scan to estimate when your baby is due, check the physical development of your baby, and screen for possible conditions, including Down's syndrome.
16 weeks pregnant
Your midwife or doctor will give you information about the ultrasound scan you'll be offered at 18 to 21 weeks.
They'll also help with any concerns or questions you have.
Your midwife or doctor should:
- review, discuss and record the results of any screening tests
- consider an iron supplement if you're anaemic
18 to 21 weeks
You'll be offered an ultrasound scan to check the physical development of your baby. This is also known as the 20-week scan .
Screening for HIV, syphilis and hepatitis B will be offered again by a specialist midwife if you opted not to have it earlier in pregnancy.
These tests are recommended as they greatly reduce the risk of passing infection from you to your baby.
From 16 weeks, you'll be offered the whooping cough vaccine . The best time to have this vaccine is after your scan, up to 32 weeks.
But if for any reason you miss the vaccine, you can still have it up until you go into labour.
25 weeks pregnant
You'll have an appointment at 25 weeks if this is your first baby.
- use a tape measure to measure the size of your uterus
- talk about your baby’s movements. If you have any concerns or your baby is moving less than usual, you’ll be advised to contact maternity services straight away.
- use a tape measure to measure the size of your uterus
- offer more screening tests
- offer your first anti-D treatment if you're rhesus negative
- discuss how to prepare for your labour and birth
- talk to you about active labour
- discuss what happens after the birth, including how to care for your new baby and feed them
- tell you about about the vitamin K injection your baby is recommended to have
- ask about your baby's movements
You'll have an appointment at 31 weeks if this is your first baby.
- review, discuss and record the results of any screening tests from the last appointment
Your midwife or doctor should give you information about preparing for labour and birth, including how to recognise active labour, ways of coping with pain in labour, and your birth plan.
- offer your second anti-D treatment if you're rhesus negative
Your midwife or doctor should give you information about caesarean section. This discussion may take place at the 34-week appointment, or at another time during your pregnancy.
They'll discuss with you the reasons why a caesarean might be offered, what the procedure involves, the risks and benefits, and the implications for future pregnancies and births.
Your midwife or doctor should give you information about:
- breastfeeding
- caring for your newborn baby
- vitamin K and screening tests for your newborn baby
- your own health after your baby is born
- the "baby blues" and postnatal depression
Your midwife or doctor will also:
- check the position of your baby
- offer external cephalic version (ECV) if your baby is in the breech position
Your midwife or doctor will discuss the options and choices about what happens if your pregnancy lasts longer than 41 weeks.
- continue to discuss your labour and birth options with you
- ask about your baby’s movements
You'll have an appointment at 40 weeks if this is your first baby.
Your midwife or doctor should give you more information about what happens if your pregnancy lasts longer than 41 weeks.
- offer a membrane sweep
- discuss the options and choices for induction of labour
If you have not had your baby by 42 weeks and have chosen not to have an induction, you should be offered increased monitoring of the baby.

Time off for antenatal appointments
Find out more about pregnant employees' rights .
Page last reviewed: 21 April 2023 Next review due: 21 April 2026
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Eur J Midwifery

Postnatal virtual and home visits by midwives during COVID-19 pandemic
Maria gjoni.
1 Midwifery Department, University of West Attica, Athens, Greece
Efstathia M. Alevizou
Dear Editor,
During the COVID-19 pandemic postnatal midwifery-led care remains a key public health intervention for women and their families 1 , 2 . Home or virtual visits by community midwives should be provided to reduce the number of times women and newborns need to leave their home 1 . In order to comply with social distancing requirements, community midwives could deliver home or virtual visits and individualized postnatal care, according to the needs of the mother and the newborn 1 . Midwifery-led postnatal home visiting could raise consciousness in parents on establishing breastfeeding, family planning and contraception after birth, preparation of milk formula, smoke-free environments at home, home hygiene, and care of the neonatal – especially after NICU discharge 3 . Midwifery-led virtual visits via videoconferencing decrease the number of visits to health facilities and enable mothers to be consulted immediately and from their own home 4 . Virtual visits have been demonstrated to be as safe as in-person visits 5 . Therefore, as early as possible, community midwives (especially those serving rural and remote areas) should receive all the relevant technology equipment and training regarding remote consultation 5 .
The World Health Organization (WHO) recommends at least four postnatal visits for all mothers and newborns, on day 1 (first 24 hours), on day 3 (48–72 hours), between days 7–14 and six weeks after birth 6 . However, a face-to-face consultation is required for physical examination and/or screening of mother and the newborn 1 . Therefore, home visiting should be prioritized for women with psychosocial vulnerabilities, operative birth, premature or low birthweight baby and other medical or neonatal complications 1 . Awareness should be raised about exposure to COVID-19 during a home visit, where midwives should abide by strict infection control equipment and procedures when entering and leaving homes 1 .
Midwifery-led services are vital during the postpartum period for women suspected or confirmed with COVID-19. Parenting and breastfeeding support can be offered through face-to-face or virtual visits 1 . Μothers with COVID-19 should be advised to establish breastfeeding or to express breastmilk, applying appropriate infection prevention and control measures 2 , 7 . All breastfeeding women should be shown how to hand-express their breast milk and be advised on how to correctly store and freeze it. Breastfeeding counseling, neonatal care, family planning counseling, psychosocial parent support, practical feeding support and home hygiene should be provided to all mothers and their families, whether they or their children have suspected or confirmed COVID-19 7 .
Community midwives are a valuable resource either providing face-to-face visits or virtual visits 8 . They need adequate support 8 to provide quality, holistic, women-centered postnatal care to mothers and newborns 9 in these exceptionally complex circumstances in order to promote safe and respectful 10 family-centered care, during periods of crisis including the current COVID-19 pandemic.
CONFLICTS OF INTEREST
The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none was reported.
There was no source of funding for this research.
PROVENANCE AND PEER REVIEW
Not commissioned; externally peer reviewed.
Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
- Parenting, childcare and children's services
- Children's health and welfare
- Children's health
- Supporting public health: children, young people and families
- Public Health England
Care continuity between midwifery and health visiting services: principles for practice
Updated 19 May 2021
Applies to England

© Crown copyright 2021
This publication is licensed under the terms of the Open Government Licence v3.0 except where otherwise stated. To view this licence, visit nationalarchives.gov.uk/doc/open-government-licence/version/3 or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email: [email protected] .
Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned.
This publication is available at https://www.gov.uk/government/publications/commissioning-of-public-health-services-for-children/care-continuity-between-midwifery-and-health-visiting-services-principles-for-practice
Executive summary
Care continuity between midwifery and health visiting enables safe, high quality, personalised care delivered in a timely manner. This continuity is an integral part of delivering the Healthy Child Programme (2009) and reaching the ambitions set in the National Maternity Review (2016) and NHS Long Term Plan (2019).
This document is designed to act as a tool to support local practice implementation and improvements in the care continuity between midwifery and health visiting services. It was developed based on a literature search of current research, an examination of current UK guidance and policy and interviewing midwives and health visitors working in Local Maternity Systems. The document provides evidence and practice examples to consider when improving quality of care through effective transition of information and collaborative practice between midwifery and health visiting services. This document will be relevant to providers of midwifery and health visiting services (including clinical staff and managers) and service commissioners working within integrated care systems and local authorities.
Care continuity between midwifery and health visiting teams can take different forms and be via joint working, sharing information and postnatal handover. Sharing information about women and their babies care also help provide consistent information for women and their families, and is in line with the Making Every Contact Count agenda.
To implement effective care continuity between midwifery and health visiting services, midwives and health visitors need:
- contact details of local midwifery or health visiting teams
- systems (ideally digital) to share relevant information about women and their babies in a timely manner
- protocols regarding when and how to share information and with whom antenatally and postnatally
- contact between midwifery and health visiting services at all levels of service; strategic and operational
- knowledge of each professional’s role and remit and each other’s informational needs
- opportunities to meet face-to-face, to build relationships and discuss care
- access to shared or aligned records that are accessible by both midwifery and health visiting teams as well as the wider primary health team (that is, Family Nurse Partnership ( FNP ) and GPs).
- the same tools and resources to share with women to ensure consistent information is provided
Through care continuity during the antenatal and postnatal period, a seamless service can be provided to women and their families. Other benefits include:
- provision of joint care for those women who need it
- earlier identification of women requiring targeted support
- improved care and consistent information for women and their families, leading to improved outcomes for women and their babies, an improved experience and increased care satisfaction through personalised care
- increased ability of midwives and health visitors to share relevant information in a timely fashion
- improved service pathways, standard operating procedures and information sharing documents such as notification of pregnancy and discharge forms
- better aligned service commissioning and pathways
- increased importance attributed to sharing of information between midwifery and health visiting services
Figure 1 shows a summary of factors contributing to effective care continuity between midwifery and health visiting services. These include:
- effective working relationships between midwife and health visitor
- consistent health and wellbeing message from midwife and health visitor
- ensure health and wellbeing information is evidence based
- consistent information sharing and record keeping
- effective communication between professionals and women and partner
- appropriate and seamless handover tailored to expectant women and partner
- ensuring services are universal in reach and personalised in response
- primary care and intensive family support
- peer support
Taken together these factors:
- ensure that women and their partners are given the same consistent and evidence-based information throughout their maternity journey
- support women and their partner to understand when and how their health information will be shared
- enable care to be tailored to each family’s individual needs
Figure 1. Factors contributing to effective care continuity between midwifery and health visiting services
Summary of actions for main stakeholders
Midwives, health visitors and their service managers.
Recommendations for implementing effective care continuity between midwifery and health visiting services are to:
- create opportunities for midwives and health visitors to meet and discuss women’s care
- share relevant information about women and their babies throughout pregnancy and postpartum
- share lists of names and contact details of professionals in each service
- provide protected time for frontline staff to develop interprofessional communication and new systems for working
- form interprofessional health teams including health visitors, midwives, GPs and other professionals that meet regularly to discuss vulnerable families
- consider part-time secondments to develop interprofessional teams
- jointly develop templates for communication of women’s changing needs across the care pathway
- provide joint visits and appointments for women, particularly for vulnerable families, if acceptable to the individual woman
- provide joint training for midwives and health visitors on breastfeeding, safeguarding, perinatal mental health and other issues
- support collaborative working in maternity outreach hubs and community hubs
Commissioners of midwifery and health visiting services, local authorities and care commissioning groups
- support infrastructure to enable sharing of information
- develop shared electronic platforms for local care records that are accessible by all healthcare professionals involved in a woman and baby’s care
- implement service level agreements for information sharing
- provide midwifery and health visiting service in the same locations such as maternity outreach hubs or community hubs that are easy for women to access
- consider a dedicated co-ordinator or liaison roles to oversee information sharing, transfer of care, arranging visits and referrals
- engage with the local community, including Maternity Voices Partnership , to co-develop information sharing procedures taking into consideration the needs of minority and vulnerable groups
- commission interprofessional training events to develop understanding of practice areas as well as each other’s roles and responsibilities
- monitor outcomes such as breastfeeding monitor the number of antenatal contacts and new born visits within 10 to 14 days postnatal
Introduction
This document sets out the strategic context and research evidence for delivering effective care continuity by midwifery and health visiting services. Care continuity is understood in this context as planned and sustained delivery of high quality support and includes providing consistent messages, effective handover of care, joint working and good working relationships.
This document can be used as a tool to support local practice implementation and improvements in the care continuity provided by midwifery and health visiting services. It provides evidence and practice examples to consider when improving quality of care through effective transition of information and collaborative practice between midwifery and health visiting services. As such this document will be relevant to providers of midwifery and health visiting services (including clinical staff and managers) and service commissioners working within integrated care systems and local authorities.
The expected outcomes from the implementation of these practice principles are:
- more personalised, safer and effective care for women and their families
- consistent information for women and their families, leading to an improved experience and increased care satisfaction
- increased ability of midwives and health visitors to provide a seamless service
- earlier identification of and response to vulnerabilities which may impact on the health of the woman and her baby
- improved service pathways, standard operating procedures and information sharing documents such as notification of pregnancy and handover forms
- better ability of the commissioners of midwifery and health visiting services to support their workforce with care continuity during the antenatal and postnatal period
- more shared visits when clinically appropriate
- more women receiving an antenatal visit by their health visitor
How this document was developed
The development of this document was led by Justine Rooke and Monica Davison (Public Health England) and Dr Ellinor Olander and Dr Patricia Moran (Centre for Maternal and Child Health Research, City, University of London). The document was systematically developed using 3 strands of evidence; academic research, current UK guidance and policy and the experiences of those working in Local Maternity Systems.
Firstly, a literature search was conducted using Scopus and PubMed to identify UK-based empirical studies published since 2015 on care continuity as provided by midwifery and health visiting services. Relevant journals not included in these databases (such as Journal of Health Visiting) were hand searched. Search terms included midwifery, health visiting, collaboration, joint care and partnership and variations of these. Good quality evidence was ensured by only including peer-reviewed research. To be included studies had to provide information regarding care continuity or on factors influencing this. Women’s views and experiences were also included. To be included research could be randomised controlled trials, surveys, service evaluations and qualitative studies with either women or healthcare professionals. These inclusion criteria were used to ensure focus was on practical suggestions. The included research is based on qualitative evidence.
Secondly, the websites of Institute of Health Visiting, National Institute for Clinical Excellence ( NICE ), NHS England, Royal College of Midwives ( RCM ) and Public Health England ( PHE ) were searched to identify relevant and current guidelines as well as practice examples. The database OpenGrey was also used to identify practice examples. Examples were deemed appropriate if they were in line with current guidelines and provided information on positive outcomes for women. The most recent MBRRACE (Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries) reports were also checked for relevant information. Further, an email was sent out to all Local Maternity Systems to ask for practice examples. To be included, a practice example had to focus on one of the factors influencing care continuity such as information sharing, joint working and so on.
Finally, 25 interviews were conducted with staff working within the midwifery and health visiting services in England. Participants were recruited via an email to all Local Maternity Systems and the PHE network, and were interviewed between July to September 2020. Participants worked in 13 different Local Maternity Systems and included 15 participants working as midwives, 9 as health visitors and one participant was a service commissioner. Interviews were transcribed verbatim and analysed thematically. Findings confirmed previous research findings, participants viewed care continuity as important, reported different systems of sharing information and supporting families. Participants also discussed how practice had changed during coronavirus (COVID-19).
A draft of this report has been reviewed by representatives from PHE , RCM , NHS England and service managers and local Maternity System staff. Based on this feedback the document was finalised. This document benefitted from many people giving up their time to share their experiences and providing feedback, and we are very grateful for their time and input.
Main drivers, policy and strategic context
The National Maternity Review (Better Births, 2016) outlines a clear vision for maternity services across England to become safer, more personalised, kinder, professional and more family friendly. Maternity services should also enable women to make decisions about their own care and provide support centred on individual needs and circumstances. The review also recommends staff to be supported to work in high-performing teams and deliver care that is women-centred.
Implementing the vision set out in Better Births will support the Secretary of State’s ambition to halve the number of stillbirths, neonatal and maternal deaths and brain injuries by 2025.
The Maternity Transformation Programme seeks to achieve the vision set out in Better Births by bringing together a wide range of organisations to lead and deliver across 11 work streams. There are a number of initiatives implemented as part of the Maternity Transformation Programme which will aid care continuity between midwifery and health visiting services. The Better Births 4 Years On: A review of progress report (2020) presents data on how over 100 community hubs have opened nationally. Community hubs where midwifery and health visiting services are co-located will help provide care continuity for women and their families. The same document reports that over 10,000 women had been booked on a continuity of carer pathway provided by midwives by March 2019. With improved continuity from a named midwife sharing of information with health visiting services will become easier.
By 2023 to 2024, all women will be able to access their maternity notes and information through their smart phones or other devices. This will help women share their maternity notes with their health visitor.
The NHS Long Term Plan (2019) promises to implement an enhanced and targeted continuity of carer model to help improve outcomes for the most vulnerable mothers and babies. By 2024, 75% of women from ethnic minority communities and a similar percentage of women from the most deprived groups will receive continuity of carer from their midwife throughout pregnancy, labour and the postnatal period. Continuity of carer during pregnancy benefits women, and is implemented to reduce health risk and decrease health inequalities (1) . Continuity of carer has also been found to particularly benefit women with complex social factors and ethnic minority women (2 , 3) . Ethnic minority women have been found to have increased risk of maternal mortality . Compared to pregnant non-ethnic minority women, pregnant ethnic minority women were more likely to be admitted to hospital with confirmed SARS-Co-2 infection (4) .
The NHS Long Term Plan discusses increased support for mental health for women and their partners and for breastfeeding. Perinatal mental health services will be improved to enable more women access evidence-based support. All maternity services should be working towards delivering an accredited, evidence-based infant feeding programme. This provides another great opportunity for midwives and health visitors to work collaboratively to provide consistent breastfeeding messages and support to women.
Midwifery and health visiting services had to change rapidly when the COVID-19 pandemic happened in early 2020. The pandemic also impacted on care continuity and new processes had to be introduced. For example, services now had to share information on whether women or anyone in their family had suspected or confirmed COVID-19 or if they were in a shielding category. When midwives and health visitors were co-located information sharing was more readily and easily available but due to home working as a result of the pandemic, online meetings were introduced in many areas. This way of working could facilitate future collaboration between midwifery and health visiting professionals due to its ease and convenience, including cutting down on travel time.
At the start of lockdown, areas with strong established working relationships were able to work quickly to change support and care for women and their families. In practice example 1, Cambridgeshire and Peterborough Local Maternity and Neonatal System share their experiences.
Practice example 1. Changing practice during COVID-19 (Cambridgeshire and Peterborough Local Maternity and Neonatal System)
As professional relationships were already formed between midwifery and health visiting services, when the COVID-19 outbreak happened we were able to rapidly come together as senior leads to plan collaborative support and care for antenatal and postnatal women in our localities. A joint care pathway was developed and shared with all midwifery and health visiting teams across our services within the first weeks of the COVID-19 outbreak. This has been continually updated to reflect the rapid changes in service that resulted from the pandemic.
In other areas, the pandemic reinforced the need for robust information sharing between services. In practice example 2, a new communication and handover process was implemented during the pandemic.
Practice example 2. Implementing a new communication process during the COVID-19 pandemic (Humber, Coast and Vale Local Maternity System)
A midwifery handover document was created to allow midwifery discharge information and requests for future support to be shared between the midwives and the health visitors. This information sharing has ensured a better communication of needs, transparent discharge information, care continuity for the client and a platform to sense check antenatal and baby loss notification knowledge. In addition, the health visiting services set up a single point of contact by telephone facility to receive any midwifery handovers so any concerns could be easily communicated. The immediate outcome is that health visiting services receive midwifery handover information for every mother and baby which allows the health visitors to attend the new birth visit with up to date knowledge of the baby and family. This allows them to be fully informed about the families care needs and ensures that all services are fully informed about postnatal care. The handover information has also allowed us to identify families who were not known to the health visiting service in the antenatal period and to understand why this was. Through collaborative working across a geographical system we have been able to improve the care given to all parents by improving our channels of communication.
Joint home visiting and discharge or handover planning are especially important for families with complex needs so that assessment and appropriate referrals can be made to maximise support available to women (5) .
Practice example 3 provides an example of joint working between health visitor, midwife and GP that enabled appropriate care planning and support for a new mother experiencing mental health issues.
Practice example 3. Joint working to support women during the COVID-19 pandemic (Norfolk and Waveney Local Maternity System)
During the COVID-19 pandemic, a health visitor making a new birth contact via Attend Anywhere video calling with a Universal service user identified low mood in the mother directly relating to her traumatic birth experience. The mother disclosed that she had not shared her feelings with her community midwife or any other health professional. The health visitor sought her consent to speak to other health agencies – midwifery and GP services – this was given. The health visitor then liaised with the community midwifery team to ensure a referral to the debrief service was offered and that the allocated community midwife for this woman was aware. The community midwife directly contacted the health visitor and together they made a joint plan to provide support via video and midwifery home visiting contacts. Midwifery contacts were extended beyond the usual postnatal period and support was provided for the mother to access her GP. A virtual triangle meeting took place between the midwife, health visitor and GP to share information to support the care plan. Excellent communication and liaison between agencies have provided a robust care plan for this service user and ensured handover of care will be fully informed when it takes place.
Why care continuity is important
Benefits for women and their families.
Care continuity helps midwives and health visitors tailor the best care possible, which will have a positive impact on women’s and their babies care and satisfaction with services.
More and more women begin pregnancy with health risks, such as older age, a high body mass index ( BMI ) or with a long term condition. Further, more babies are born into care than ever before : approximately 1 in 200 in 2018 (6) . This is a sharp increase from 2008 when 1 in 400 babies were taken into care within one week of birth. This number is higher in deprived areas: in Blackpool 1 in 47 babies was born into care. Providing joint care is especially needed and important for these high risk women and is likely to benefit these women the most.
In line with Making Every Contact Count , midwives and health visitors can share information to promote positive changes in health behaviour. Midwives and health visitors sharing information will also ensure women receive consistent messages, which in turn can have positive effects on breastfeeding, maternal mental health and child outcomes. Women identify issues especially important to share as mental health concerns or chronic health conditions (7) . Receiving inconsistent or contradicting information on the other hand cause women unnecessary anxiety (7) . An example of early intervention and positive outcomes resulting from the timely sharing of information between midwifery and health visiting services is the smoking relapse prevention pilot carried out in Sheffield, described in practice example 4.
Midwives and health visitors sharing information will also ensure women do not have to repeat information and their experiences every time they see a new healthcare professional. Women report frustration having to repeat the same information to different healthcare professionals, leading to dissatisfaction with care and not feeling heard (7) .
Practice example 4. Smoking relapse prevention pilot in Sheffield (South Yorkshire and Bassetlaw Local Maternity System)
Sheffield implemented a pilot programme of smoking cessation support which integrated the role of health visitors to encourage post-partum follow-up and relapse prevention. Pregnant women’s smoking status was ascertained at booking with referral of all smokers to the stop smoking service. Training was provided for health visitors in using carbon monoxide monitors and identification of health visitor champions to provide ongoing support to women who quit during pregnancy. Information was shared between the midwifery service and champions on their caseload’s smoking status. This information helped health visitor champions to visit women still smoke free at 30 to 34 weeks and followed up at their birth visit offering ongoing support up to 6 to 8 weeks after birth. Health visitors also referred fathers or partners to the stop smoking service. The integration of health visitors led to 54 women (49%) accepting a referral from the midwifery service for postnatal smoking cessation relapse support with the health visitors. Among these women, 47 new birth visits were completed with 67% of women still smoke free, by 6 to 8 weeks post-partum 34 visits were completed with 25 women still smoke free.
Benefits for midwifery and health visiting services
Effective care continuity between midwifery and health visiting will improve midwifery and health visiting services and help services run more smoothly. For example, midwives sharing information about pregnant women will help health visitors deliver the mandated antenatal contact and New Birth Visit. Effective information sharing and joined-up services are also a priority in the revised Healthy Child Programme commissioning guidance (2021). Sharing of information is likely to extend the many benefits associated with continuity of carer as provided by midwives. Collaborative working will also help developing local services and effectively use resources. This includes streamlining support such as antenatal education or breastfeeding clinics and providing joint training for midwives and health visitors. For example, applying for Baby Friendly Initiative accreditation can be a good opportunity for joint training. This accreditation is based on a set of linked evidence-based standards for maternity, health visiting, neonatal and children’s centres services.
Training can also be delivered by one healthcare professional group to another to support workforce development. In practice example 5, a problem with avoidable Newborn Bloodspot testing repeats was identified within the health visiting service, and training was developed and delivered by midwifery services to help reduce these repeats.
Practice example 5. Workforce training: Newborn Bloodspot Testing ( NBS ; South East London Local Maternity System)
A problem with avoidable NBS repeats amongst health visitors was identified within the health visiting team. Avoidable repeats cause anxiety for parents and delayed identification can lead to delayed treatment of an affected baby. To reduce the number of avoidable repeats, the Lambeth Early Action Partnership Health Team (LEAP) provided a 1-hour midwifery-led NBS training session to 23 local Lambeth and Southwark health visitors and practice nurses. The team also set up a system for local health visitors to work with their local Guy’s and St Thomas’s NHS Foundation Trust and Kings College Hospital community midwifery teams to have their practical skills signed off. The training increased the attendees’ confidence and knowledge of NBS. After the training, the LEAP Health Team’s health visitor worked with the local health visiting screening lead to support ongoing internal training for health visitors. The health visitor avoidable NBS repeats went from 23.5% to 7.5% across both trusts. This suggests an improvement in health visitors’ knowledge and skill in undertaking the NBS.
Benefits for midwives and health visitors
Care continuity between midwifery and health visiting will help midwives and health visitors provide safe and tailored care for women and their families. Through collaboration and sharing information, midwives and health visitors can jointly discuss personalised care plans and support. This is more important than ever due to the pregnancy population increasing in health risk and vulnerability. Sharing of information can also lead to informal learning from other healthcare professionals, sharing of resources and job satisfaction knowing safe high quality care is provided to women and their families.
The need for these practice principles
These practice principles are needed for 3 reasons.
First, the Health visiting and midwifery partnership – pregnancy and early weeks document which promotes care continuity between midwifery and health visiting services through the perinatal pathway was published in 2015. Since then, the Maternity Transformation Programme has been implemented, the NHS Long Term Plan published, and the Healthy Child Programme is currently being revised. It is therefore time to provide recent evidence and examples on how to implement this pathway.
Second, there are inconsistences in care continuity as delivered by midwifery and health visiting services across England. Approximately 35% of health visitors report that collaboration with midwives has decreased . Some Local Maternity Systems have clear care pathways and standard operating procedures for how to deliver care continuity, other areas are still developing their procedures. In this document, we have used examples from areas who deliver care continuity between midwifery and health visiting services to share with those areas still developing their local practice.
Third, as previously mentioned, the needs and circumstances of the pregnant population are changing. For example, more and more women with long-term conditions have successful pregnancies. The proportion of deliveries complicated by diabetes mellitus has increased from 5% to 8% between 2013 to 2014 and 2018 to 2019.
Based on these health needs, the pregnant population of today and tomorrow are likely to need more care continuity throughout the perinatal period than previously. Local Maternity Systems may need to revise their current procedures to accommodate this increase in need. Care continuity may be delivered differently depending on the local context, including population and resources.
Main communication points
It’s important that care continuity between midwifery and health visiting services is provided both during and after pregnancy. There are certain important communication milestones, but this should not exclude information being shared outside of these times.
There are 4 communication points where midwifery and health visiting could share information :
Antenatally
- Booking 8 to 12 weeks
- 16 to 28 weeks
- 32 to 36 weeks
Postnatally
4. Birth visit to 10 to 14 days postnatal
Information sharing should consider women’s circumstances, for example for low risk pregnant women, the information shared could be less and at fewer timepoints compared to a woman who lives with complex needs and where ongoing collaboration may be necessary.
After birth, the health visitor will also share information with the woman’s GP ahead of her 6 to 8 week postnatal check with her GP.
Care continuity during and after pregnancy
The appropriate timing and detail of information shared during pregnancy depends on local systems and resources and women’s needs and circumstances. Information sharing and early intervention planning are vital to support women. For example, for pregnant women living with complex social factors midwives could consider a multi-agency needs assessment or refer to a multi-agency team, including health visiting services. Within the community setting, midwives and health visitors may deliver joint antenatal classes (8) , share information about and refer women to community services.
Important for all women is to receive information antenatally about the health visitor’s role. This is particularly important for first time mothers and women who have immigrated to the UK (8 , 9) to make them aware of the importance of the health visiting antenatal contact. Other important information to provide women during and after pregnancy is provided in the Health visiting and midwifery partnership – pregnancy and early weeks document as well as the High Impact Area documents breastfeeding, parental mental health, smoking, alcohol and healthy weight .
After booking, the midwifery team can notify the health visiting team of the pregnancy. They may also notify the FNP if appropriate. This notification can include assessment of social and health need, including needs of the partner or father, and referrals to other agencies such as mental health or social services (see below for examples of information that can be shared by midwifery services with the health visiting team antenatally). The health visiting team should aim to inform midwifery services of a named health visitor for every woman during this time if possible or at least contact details to the health visiting team.
As the pregnancy progresses, the midwife is to communicate any change in the pregnancy status or changes in risk to the family or child to the named health visitor or health visiting team. The midwifery team should aim to notify the health visitor in a timely manner of identifying any significant changes to maternal or child wellbeing.
Important information
The following is a list of the types of information or issues affecting a mother, parent or parents which can be shared between midwifery and health visiting services ahead of the mandated health visiting contact:
- first-time mother
- parents under 19 years
- child protection or social welfare concerns
- domestic abuse
- safeguarding referral
- drug, alcohol or substance misuse
- anxiety, depression or previous post-natal illness
- previous history of stillbirth, neonatal or cot death or baby in NICU
- smokers living in the home
- late notification of pregnancy
- single parent in need of support
- parent chronic physical or mental ill health or disability
- learning difficulties
- mother needs an interpreter (and which language)
- ambivalence regarding pregnancy, low self-esteem or relationship difficulties
- unemployment or financial difficulties
- multiple births
- housing concern
- maternal BMI , below 19 or above 35
- asylum seekers or refugees
- care leavers or history of being in care
An individualised postnatal care and support plan could be developed with the woman in the later weeks of pregnancy. The care and support plan could include:
- relevant factors from the antenatal, intrapartum and immediate postnatal period
- relevant information on family context
- details of the healthcare professionals involved in her care and that of her baby, including roles and contact details
- plans for the postnatal period including infant feeding and physical and emotional wellbeing
After the birth of the baby, the midwifery services should update the health visiting services on the health of both mother and baby. The midwife can explain the purpose of the parent-held personal child health record and how it will be used by the midwife, health visitor and GP. At discharge from community midwifery care, the midwife could complete appropriate sections of the parent-held personal child health record to facilitate transfer of care to the health visitor. A child and family needs assessment, including partner or father’s needs may also be needed.
The New Baby Review is done by the health visitor and should ideally occur within 14 days after birth. However, in some circumstances, this is not possible. Ahead of this review, health visitors should have received information from midwifery services about the woman and the baby they are visiting.
Vulnerable women
An action plan could be a particular consideration for women and partners or fathers with complex social factors . Where a woman or father or partner is identified as vulnerable (for example, maternal mental health, learning disability, obstetric issues, domestic abuse and so on) they can be asked to co-create an individualised action plan with the midwife and health visitor. It’s recommended that a joint meeting with the family is considered. A joint handover in the woman’s home could be beneficial and enable efficient information sharing and care continuity. As this is associated with additional resource, it should be planned with care and provided only when appropriate.
If women require midwifery input after day 14, the midwife and health visitor should aim to have a verbal handover in addition to a written handover. This could be via an online meeting or phone call.
Antenatal contact by health visitors
From 28 weeks of pregnancy a face-to-face contact is to be made with every pregnant woman by the health visiting service. Many women welcome the opportunity to have contact with their health visitor antenatally (9) . This is a mandated contact and often done in the woman’s home. To facilitate this contact, midwifery services need to provide information about women to the health visiting service. Many midwifery services share information after the 20-week scan when the pregnancy is seen as viable. This reduces the risk of health visitors contacting women who have suffered a miscarriage. After the contact, health visitors can share any relevant information about the woman and her pregnancy with the midwifery services.
Sharing of information with GPs
Sharing of information may also need to be done with the woman’s GP. As of 2020 to 2021, there is a new requirement for GPs to offer a 6 to 8 week postnatal check for new mothers, as an additional appointment to that for the baby. This makes communication between health visitors and GPs of greater significance than ever before. For example, for maternal mental health, a health visitor needs to refer to local service pathways or specialist services and inform the woman’s GP. It is also important to communicate with the GP if women have declined health visiting services (10) .
Using evidence to support care continuity between midwifery and health visiting services
In this section, evidence and practice examples are presented to provide suggestions of how care continuity and collaboration between midwifery and health visiting services can be provided. These consist of:
- communication and information sharing
- understanding each other’s professional roles and responsibilities
- co-location of services
Communication and information sharing
Information can be shared in a number of ways; face-to-face or online meetings, telephone or email contacts, forms and through sharing of health records. Face-to-face meetings are particularly valued by healthcare professionals when supporting families with complex needs (5) . Whatever form the communication takes, it needs to be timely and accurate to facilitate good support for women and their family. Practice example 6 shows how a midwife’s communication with a health visitor at postnatal discharge facilitated prompt action on behalf of the family.
Practice example 6: Postnatal communication (Norfolk and Waveney Local Maternity System)
A midwife discharging a postnatal woman called to inform the allocated health visitor that there was little food in the home and the access to Healthy Start support that had been in place had now ended. There were no other concerns and the family was under a universal care pathway. The health visitor was able to access a food parcel that same day and arrange delivery to the family. She then provided telephone support to the family to re-apply for Healthy Start vouchers to supplement their food budget. Although the midwife and health visitor had not needed to complete joint contacts for this family under Universal care, prompt communication of an identified need meant that health visiting services were able to respond quickly and put support in place for this family. Women report that fragmented communication between midwifery and health visiting services sometimes results in receiving inconsistent information from healthcare professionals (7) . Women also find themselves having to repeat their clinical information and needs to each healthcare professional , which can be irritating and distressing, especially for women with pregnancy- or birth-related trauma. To avoid women having to repeat themselves and to enable consistent information, a tool was developed in Sheffield to share infant feeding plans between parents, midwives and health visitors (see practice example 7).
Practice example 7: Supporting breastfeeding plans: development of a tool to communicate infant feeding plans between parents, midwives and health visitors (South Yorkshire and Bassetlaw Local Maternity System)
The infant feeding leads for both midwifery and health visiting met regularly to explore how practitioners could be supported to engage in timely and effective communication. Extensive consultation took place with main stakeholders including community and postnatal midwifery matrons, postnatal ward and health visiting team leaders, advanced neonatal nurse practitioners, midwives, nursery nurses and mothers and it was agreed that a parent-centred approach would be most appropriate in line with the current personalisation agenda. A booklet was developed where parents document feeding and expressing, read when and how the plan will be reviewed, how they will be supported back to breast feeding and access further information. It also assists health professionals to review feeding progress and to update the plan, in collaboration with the parents. In addition, a new feeding plan sticker is completed by the midwife and placed in the Child Health Record to alert the health visitor to consult the plan. This tool is part of a process to promote seamless care between the midwifery and health visiting services in Sheffield, to support mothers whose baby is on a feeding plan. Previously, communication between the midwife, health visitor and mother lacked consistency regarding ongoing support when a feeding plan was in place.
There can be inconsistencies about how much information is shared (5) . To overcome this, clear liaison forms can help information sharing. For example, Buckinghamshire, Oxfordshire and Berkshire West Local Maternity System has communication guidelines and a liaison form to help information sharing. The form outlines any additional support a woman may need at any time during her care, including physical, emotional, social or educational needs.
In some areas, information is shared via forms sent on email. In other areas, IT systems has been developed for rapid and regular information sharing. Information sharing can be challenging when different services have non-compatible or unaligned systems for women’s care records, rendering information inaccessible to other healthcare professionals. This has been identified as a communication barrier between midwifery and health visiting services, but can also include Family Nurse Partnerships and GP services as well (11) . Practice example 8 outlines the information sharing in Bedfordshire, Luton and Milton Keynes Local Maternity System between midwifery and health visiting services.
Practice example 8: Local information sharing agreement for antenatal data exchange within Bedfordshire (Bedfordshire, Luton and Milton Keynes Local Maternity System)
An information sharing agreement was designed to provide the health visiting service in Bedfordshire with the demographic details of every pregnant woman booked for delivery in the Bedfordshire hospitals. This data is used to facilitate antenatal visits by health visitors. Accurate contact and personal details, and date of expected birth are required by the health visiting service after 24 and prior to 32 weeks of pregnancy. Previously, community midwives provided information direct to health visitors, however this was patchy, often inaccurate, provided on paper and has proven difficult to achieve. As a result, a low number of antenatal women received a visit prior to the birth by health visitors.
A joint working group was identified to include commissioners, the maternity service and the health visiting service. The maternity service investigated ways in which their electronic patient records system could be interrogated to obtain the data required and used a software package that could perform this function. A process was drawn up to include the following:
- what information would be required from patient systems and an information-sharing agreement was developed by the group and approved by Caldicott guardians of all services to ensure information governance requirements were met
- women who do not consent to share their information with health visiting services are not included
- secure transfer of data from midwifery to health visiting services
- information is transferred weekly to a secure email via NHS.net and sent to the single point of access at the health visiting service.
- health visiting administrator then access the woman on SystmOne and check pregnancy is still viable and allocate the antenatal visits to the relevant case holding health visitor for contact by 34 weeks
The service is currently achieving 80% of all antenatal visits each month. Of the 20% who have not been seen the majority are booked to deliver in out of area hospitals who do not operate this system. To date, very few women have refused an antenatal contact with the health visitor. Feedback from women is regularly positive, and shows that the service is appreciated. Before the new process started, midwives were trained in the role of the health visitor, the current offer by health visitors for all pregnant women, how to gain consent from women, how to ensure the maternity system can read that consent has been given, what to do if a woman refuses to share information with the health visiting service, the importance of sharing complex information with the health visiting service and the importance of sharing late or out of area women with the health visiting team locally.
Understanding each other’s professional roles and responsibilities
Providing care continuity may be influenced by how well professionals understand each other’s commissioned service and scope of practice. If midwives and health visitors do not understand each other’s roles, it could lead to uncertainty of the tasks and timeframes the other healthcare professional is responsible for (5) . This in turn may cause women to receive conflicting advice, reduced support or incorrect advice about the support available to them from each profession. To increase uptake of the health visiting antenatal contact, Bedfordshire, Luton and Milton Keynes Local Maternity System held training for midwives regarding the health visiting role and service. This, together with an improved electronic information sharing system, increased antenatal contacts (see practice example 8).
Collaborative working and information sharing is enhanced when midwives and health visitors feel part of a team, and have mutual respect and support for each other’s roles (5) . When a midwife-health visitor team approach is adopted with women, it becomes easier for women to seek support and connect with services, and discuss their concerns. Practice example 9 provides an example of how a collaborative partnership can be developed.
Practice example 9: Developing collaborative partnerships (Cambridgeshire and Peterborough Local Maternity System)
Work undertaken by Cambridgeshire and Peterborough Healthy Child Programme (HCP) in partnership with North West Anglia Foundation Trust and The Rosie Maternity Unit at Cambridgeshire University Hospitals Foundation Trust led to the identification of the need for a clear, robust pathway for sharing information concerning antenatal booking. Initially, meetings were arranged with the midwifery leads or matrons from both acute trusts and the Clinical Lead from HCP. The purpose of these initial meetings was to review current practice and identify where improvements could be made, using a PDSA (Planning, Doing, Studying, Acting) approach. These meetings were held face-to-face. Other key individuals who could support progression of this project were identified. The digital midwives were involved very early in the discussions. Proactive commissioners have been pivotal in supporting the building of relationships and facilitating opportunities for change management. There has also been collaboration with service users.
Improved knowledge of each other’s professional roles and responsibilities can be developed through joint training. Face-to-face workshops can help build rapport and getting to know each other. This can result in an appreciation of each other’s roles, workloads and a greater willingness to work collaboratively , with the potential to improve sharing of information and providing women with consistent messages (12) .
Co-location of services
Community hubs or family hubs within settings such as children’s centres can provide one-stop shops for services in convenient locations (13) . Co-location of services can improve formal and informal communication, making it faster and more efficient to collaborate. Face to face contact can also help to build professional relationships , facilitate understanding of each other’s roles, as well as enable joint service planning and delivery (13) .
To ensure greater collaborative working within a co-located setting, clear pathways and joint policies are needed. Alongside these, facilitative organisational structures and strong managerial support needs to be provided (13) . For example, regular meetings between midwifery and health visiting managers allows for practice to be discussed and audited and any changes disseminated quickly.
A number of resources are needed to implement effective care continuity. Resources include appropriate staffing levels and workloads, adequate time, organisational and managerial support and shared IT systems (5) . For example, managerial support is needed to develop standard operating procedures. Barriers to sharing information that can facilitate care continuity includes different service commissioners and therefore funding structures, IT systems, service boundaries and places of work. For example, receiving information about women who give birth in hospitals that are outside the area of the health visiting service can be difficult due to lack of systems and pathways and different ways of working Digital maturity that’s to say how well a maternity service is currently using digital technology and how well prepared the staff, processes and technology are for adopting new digital transformation initiatives, differs across England.
An example of how enhanced resourcing through managerial support and protected staff time led to improved multi-disciplinary working and care planning can be seen in practice example 10 derived from the Lambeth Early Action Partnership ( LEAP ) Health Team.
Practice example 10: Lambeth Early Action Partnership ( LEAP ) Health Team (South East London Local Maternity System)
An interprofessional health care team was formed to examine how the primary care professionals who provide care for pregnant women and their families could work better together. The team comprised 4 front-line clinicians (a local GP, a health visitor, and 2 midwives from different local trusts), operating in a flat hierarchy. Team members were given protected time for this work, which they carried out on the basis of a one day a week secondment from their front-line work. They were given the autonomy to explore any issues that they identified, with a light-touch management steering approach, and were supported to disseminate and implement the solutions they identified. Together they developed a forensic map of what did and did not work, gathering information through shadowing, meeting stakeholders and service mapping. This led to the development of a wide-range of projects including regular interprofessional meetings to discuss vulnerable families, shared access to local care records held electronically, shared practitioner contact lists, interprofessional training, and improved resources for assessment and referral. Outcomes include improved care planning and multidisciplinary working affecting areas such as safeguarding, medical concerns and family issues.
Measures of success or outcome
High-quality data analysis tools and resources are available for all public health professionals to identify the health (and health needs) of the local population. This contributes to the decision-making process and plans to improve services and reduce inequalities. Commissioners and local services need to demonstrate the impact of their services and this can be achieved by using local measures. Below are examples of outcomes and how they can be measured.
The following indicators can be used to measure benefits for women and families:
- smoking at time of delivery (available via Maternal and child health profiles )
- maternal mental health (available via Maternal and child health profiles )
- baby’s first feed breast milk (available via maternity services dashboard )
- breastfeeding at 6 to 8 weeks (available via Maternal and child health profiles )
- infant mortality (available via Maternal and child health profiles )
- low birth weight of term babies (available via Maternal and child health profiles )
- emergency hospital admissions (available via Maternal and child health profiles )
- care satisfaction (available via Friends and family questionnaire , CQC maternity services survey , maternity voices partnership )
Benefits for services
The following indicators can be used to measure benefits for services:
- number of mothers who received a first face-to-face antenatal contact with a health visitor (available via Health visitor service delivery metrics )
- new birth visits completed within 14 days (available via Health visitor service delivery metrics )
Benefits for staff
The following indicators can be used to measure benefits for staff:
- informal learning (staff survey and appraisal)
- sharing of resources (staff survey and appraisal)
- job satisfaction (staff survey and appraisal)
A range of background factors for each local area and other indicators relating to women, children and young people can be found in the Child and maternal health section on PHE Fingertips and in the annually updated local authority child health profiles, which can be extracted in PDF format from the Fingertips platform.
Associated tools and guidance
Better Births , 2016
Better Births 4 Years On: A review of progress , 2020
Healthy Child Programme: Pregnancy and the first 5 years of life , 2009
National Maternity Transformation Programme
NHS Long-Term Plan , 2019
The Best Start for Life: A Vision for the 1,001 Critical Days , 2021
Aquino MR, Olander EK, Needle JJ, Bryar RM. ‘ Midwives’ and health visitors’ collaborative relationships: A systematic review of qualitative and quantitative studies ’, 2016, International Journal of Nursing Studies 62, 193-206
Aquino MRJV, Olander, EK, Bryar RM. ‘ A focus group study of women’s views and experiences of maternity care as delivered collaboratively by midwives and health visitors in England ’, 2018, BMC Pregnancy Childbirth 18, 505
Olander EK, Aquino MRJ, Chhoa C, Harris E, Lee S, Bryar RM. ‘ Women’s views of continuity of information provided during and after pregnancy: A qualitative interview study ’, 2019, Health and Social Care in the Community 27(5), 1214-1223
Sanders J, Channon S, Gobat N, and others. ‘ Implementation of the Family Nurse Partnership programme in England: experiences of key health professionals explored through trial parallel process evaluation ’, 2019, BMC Nursing 18, 13
Antenatal and postnatal mental health: clinical management and service guidance , NICE , 2020
Health visiting and midwifery partnership – pregnancy and early weeks , 2015
Health Visiting Programme: Pathway to support professional practice and deliver new service offer Maternal mental health pathway 3 , 2012
Making Every Contact Count
Pregnancy and complex social factors: a model for service provision for pregnant women with complex social factors , NICE , 2010
Postnatal care up to 8 weeks after birth , NICE , 2015
Examples of practice
Leap health team.
The Lambeth Early Action Partnership ( LEAP ) health team consists of 2 midwives, a health visitor, and a GP, led by a public health specialist. The team works within the South East London Local Maternity System, but was funded by the National Lottery Better Start fund. The team does not see families directly but instead works with local organisations to improve communication pathways between midwives, health visitors, GPs and other services to enhance joined-up working amongst the primary health care team surrounding pregnant women and families with children aged 0 to 3.
The team has set up inter-disciplinary training to share skills and is working with their local area on developing trauma-informed services. The team won the 2018 Royal Society of Medicine and Centre for the Advancement of Professional Education John Horder Award for a multi-disciplinary team. In 2019, they won the Maternity and Midwifery Forum Team Award.
The published case studies and local practice examples can be found in the World Health Organization Collaborating Centre library .
- Case studies
- Local practice examples
1. Sandall J and others. ‘Midwife‐led continuity models versus other models of care for childbearing women’, Cochrane Database of Systematic Reviews, 2016 (4)
2. Homer CS and others. ‘Midwifery continuity of carer in an area of high socio-economic disadvantage in London: a retrospective analysis of Albany Midwifery Practice outcomes using routine data (1997 to 2009)’, Midwifery, 2017, 48: pages 1-10
3. Edge D. ‘“It’s leaflet, leaflet, leaflet, then, see you later.” Black Caribbean women’s perceptions of perinatal mental health care’, British Journal of General Practice, 2011, 61(585): pages 256-262
4. Knight M and others. ‘Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study’, British Medical Journal, 2020, 369: page m2107
5. Aquino MRJV and others. ‘Midwives’ and health visitors’ collaborative relationships: A systematic review of qualitative and quantitative studies’, International Journal of Nursing Studies, 2016, 62: pages 193-206
6. Bilson A and PWB Bywaters. ‘Born into care: evidence of a failed state’, Children and Youth Services Review, 2020, pages 105-164
7. Olander EK, and others. ‘Women’s views of continuity of information provided during and after pregnancy: A qualitative interview study’, Health and Social Care in the Community, 2019, 27(5): pages 1,214-1,223
8. Aquino MRJV, EK Olander and RM Bryar. ‘A focus group study of women’s views and experiences of maternity care as delivered collaboratively by midwives and health visitors in England’, BMC Pregnancy and Childbirth, 2018, 18(1): page 505
9. Olander EK and others. ‘Women’s views on contact with a health visitor during pregnancy: an interview study’, Primary Health Care Research and Development, 2019, 20: page e105
10. King-Hicks K and J Jessup. ‘A 0 to 19 report on behalf of South East and North West Children, Young People and Families ADPH Networks’, 2020
11. Sanders J and others. ‘Implementation of the Family Nurse Partnership programme in England: experiences of key health professionals explored through trial parallel process evaluation’, BMC nursing, 2019, 18(1): page 13
12. Olander E and others. ‘A multi-method evaluation of interprofessional education for healthcare professionals caring for women during and after pregnancy’, Journal of Interprofessional Care, 2018, 32(4): pages 509-512
13. Olander EK, MRJ Aquino and R Bryar. ‘Three perspectives on the co-location of maternity services: qualitative interviews with mothers, midwives and health visitors’, Journal of Interprofessional Care, 2020, pages 1-9
Is this page useful?
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. We’ll send you a link to a feedback form. It will take only 2 minutes to fill in. Don’t worry we won’t send you spam or share your email address with anyone.
Iranian president vows to boost trade with Pakistan to $10 bln a year
- Medium Text

Sign up here.
Reporting by Charlotte Greenfield and Gibran Peshimam; Editing by Clarence Fernandez and Bernadette Baum
Our Standards: The Thomson Reuters Trust Principles. New Tab , opens new tab

World Chevron

Gaza aid from Cyprus resumes after pause following aid worker killings
Aid shipments to Gaza from Cyprus resumed late on Friday, a Cypriot source and a UAE official said, with a ship carrying food to the besieged Palestinian enclave after a pause following Israel's killing of seven aid workers.
The European Union criticised Russia on Saturday for putting subsidiaries of one Italian and one German company under the "temporary external management" of a Gazprom entity, saying the move underscored Moscow's disregard for international norms.

- Mobile Site
- Staff Directory
- Advertise with Ars
Filter by topic
- Biz & IT
- Gaming & Culture
Front page layout
HERE WE GO AGAIN —
Nation-state hackers exploit cisco firewall 0-days to backdoor government networks, perimeter devices ought to prevent network hacks. why are so many devices allowing attacks.
Dan Goodin - Apr 24, 2024 8:55 pm UTC

Hackers backed by a powerful nation-state have been exploiting two zero-day vulnerabilities in Cisco firewalls in a five-month-long campaign that breaks into government networks around the world, researchers reported Wednesday.
The attacks against Cisco’s Adaptive Security Appliances firewalls are the latest in a rash of network compromises that target firewalls, VPNs, and network-perimeter devices, which are designed to provide a moated gate of sorts that keeps remote hackers out. Over the past 18 months, threat actors—mainly backed by the Chinese government—have turned this security paradigm on its head in attacks that exploit previously unknown vulnerabilities in security appliances from the likes of Ivanti , Atlassian , Citrix , and Progress . These devices are ideal targets because they sit at the edge of a network, provide a direct pipeline to its most sensitive resources, and interact with virtually all incoming communications.
Cisco ASA likely one of several targets
On Wednesday, it was Cisco’s turn to warn that its ASA products have received such treatment. Since November, a previously unknown actor tracked as UAT4356 by Cisco and STORM-1849 by Microsoft has been exploiting two zero-days in attacks that go on to install two pieces of never-before-seen malware, researchers with Cisco’s Talos security team said . Notable traits in the attacks include:
- An advanced exploit chain that targeted multiple vulnerabilities, at least two of which were zero-days
- Two mature, full-feature backdoors that have never been seen before, one of which resided solely in memory to prevent detection
- Meticulous attention to hiding footprints by wiping any artifacts the backdoors may leave behind. In many cases, the wiping was customized based on characteristics of a specific target.
Those characteristics, combined with a small cast of selected targets all in government, have led Talos to assess that the attacks are the work of government-backed hackers motivated by espionage objectives.
“Our attribution assessment is based on the victimology, the significant level of tradecraft employed in terms of capability development and anti-forensic measures, and the identification and subsequent chaining together of 0-day vulnerabilities,” Talos researchers wrote. “For these reasons, we assess with high confidence that these actions were performed by a state-sponsored actor.”
The researchers also warned that the hacking campaign is likely targeting other devices besides the ASA. Notably, the researchers said they still don’t know how UAT4356 gained initial access, meaning the ASA vulnerabilities could be exploited only after one or more other currently unknown vulnerabilities—likely in network wares from Microsoft and others—were exploited.
“Regardless of your network equipment provider, now is the time to ensure that the devices are properly patched, logging to a central, secure location, and configured to have strong, multi-factor authentication (MFA),” the researchers wrote. Cisco has released security updates that patch the vulnerabilities and is urging all ASA users to install them promptly.
UAT4356 started work on the campaign no later than last July when it was developing and testing the exploits. By November, the threat group first set up the dedicated server infrastructure for the attacks, which began in earnest in January. The following image details the timeline:
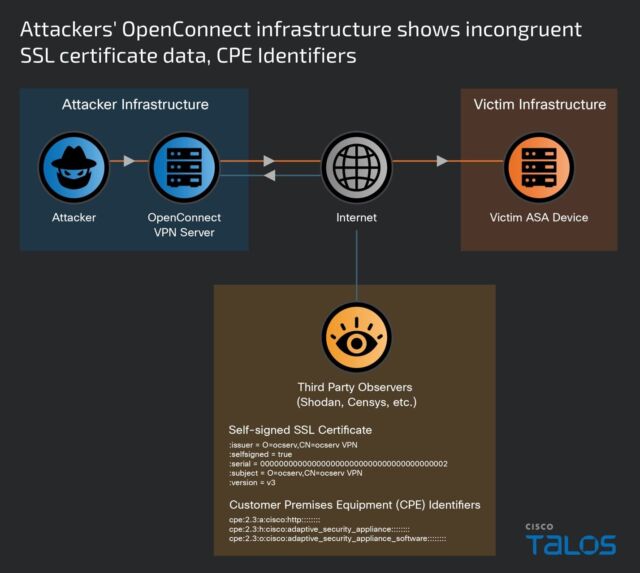
One of the vulnerabilities, tracked as CVE-2024-20359 , resides in a now-retired capability allowing for the preloading of VPN clients and plug-ins in ASA. It stems from improper validation of files when they’re read from the flash memory of a vulnerable device and allows for remote code execution with root system privileges when exploited. UAT4356 is exploiting it to backdoors Cisco tracks under the names Line Dancer and Line Runner. In at least one case, the threat actor is installing the backdoors by exploiting CVE-2024-20353 , a separate ASA vulnerability with a severity rating of 8.6 out of a possible 10.
reader comments
Channel ars technica.
- FanNation FanNation FanNation
- SI.COM SI.COM SI.COM
- SI Swimsuit SI Swimsuit SI Swimsuit
- SI Sportsbook SI Sportsbook SI Sportsbook
- SI Tickets SI Tickets SI Tickets
- SI Showcase SI Showcase SI Showcase
- SI Resorts SI Resorts SI Resorts

© Kirby Lee-USA TODAY Sports
Buffalo Bills Draft 2024: Where and when the Bills are selecting in the NFL Draft
The Buffalo Bills are scheduled to pick 10 times over the course of the three-day NFL Draft, which kicks off Thursday night in Detroit. Here's the vital info for fans who plan to watch the proceedings live.
- Author: Ralph Ventre
In this story:
It's all subject to change once general manager Brandon Beane starts working the phones, but the Buffalo Bills are scheduled to pick 10 times over the course of the three-day NFL Draft .
It all starts on Thursday, April 25 with Round 1 kicking off at 8:00 pm ET on NFL Network and ESPN. As of now, Bills' fans will be forced to wait until late into the night with 27 selections happening before Buffalo hits the clock at No. 28 overall.
"I can't really tell you whether we go up, go back or draft at 28. I have no idea how it's gonna fall," said general manager Brandon Beane in his pre-draft press conference.
The Bills currently hold only one Day 2 pick with their second-rounder slotted at No. 60 overall. Buffalo dealt its 2024 third-round selection to the Green Bay Packers in a midseason trade for starting cornerback Rasul Douglas.
Beane was anticipating receiving a Round 3 compensatory selection stemming from the loss of free agent Tremaine Edmunds, but the NFL have the Bills a fourth-rounder instead.
On Saturday, Buffalo is slated to pick twice in Round 4, thrice in Round 5, twice in Round 6 and once in Round 7. In addition to their own fifth-round selection at No. 163 overall, the Bills acquired the No. 144 pick by trading offensive lineman Ryan Bates to the Chicago Bears earlier this offseason. They also received the Packers' fifth-rounder (No. 160) as part of the Douglas deal.
Friday's television coverage (Rounds 2-3) kicks off at 7 p.m. ET. The final four rounds will unfolded on Saturday, beginning at noon ET.
2024 Bills' Draft Slots
Round 1: No. 28 overall (Thursday) Round 2: No. 60 overall (Friday) Round 4: No. 128 overall (Saturday) Round 4: No. 133 overall (Saturday) Round 5: No. 144 overall (Saturday) Round 5: No. 160 overall (Saturday) Round 5: No. 163 overall (Saturday) Round 6: No. 200 overall (Saturday) Round 6: No. 204 overall (Saturday) Round 7: No. 248 overall (Saturday)
Latest Bills News

Bills Sign Two-Time Super Bowl Champion

Bills Hosting Chargers DT for Free Agent Visit

NFL Mock Draft: Bills Land Big Ten DPOY

Giants to Meet with Free Agent CB Tre'Davious White

Bills Ex Tre'Davious White Schedules Two More Visits
- International
Day 8 of Trump New York hush money trial
By CNN's Kara Scannell, Lauren Del Valle and Jeremy Herb in the courthouse
Key takeaways from Donald Trump's hush money trial on Friday
Jurors will now have a three-day weekend to think about what they heard during the first full week of testimony in the historic Donald Trump hush money trial .
David Pecker finally stepped down from the witness stand after more than 10 hours of testimony across four days, where the former American Media Inc. chief described in detail how he helped Donald Trump suppress negative stories and pummel Trump’s rivals in the National Enquirer during the 2016 campaign.
On Friday afternoon, prosecutors called Rhona Graff, who was Trump’s assistant at the Trump Organization, where she worked for more than 30 years. She was quickly off the stand, and a banker for Cohen came next – signaling a move in the trial toward the documents at the heart of the charges against Trump.
Here are the key takeaways from Friday:
- Jury sees paper trail: The hush money case against Trump weaves a colorful narrative, but Trump is charged with 34 counts of falsifying business records — so prosecutors have warned this will in many ways be a routine, document-heavy trial . Friday afternoon prosecutors called a banker from First Republic Bank as their third witness where jurors saw the paper trail for a shell company and corresponding bank account Michael Cohen created in Delaware that was meant to be used to pay AMI for the rights to Karen McDougal’s story.
- Trump lawyer tries to puncture Pecker’s credibility: Prosecutors elicited testimony from the AMI chief about how Pecker’s 2015 deal with Trump was unique, helping him be the “eyes and ears” of the campaign. But in Pecker’s final day on the stand, Trump’s attorneys sought to undercut his testimony with a series of alleged inconsistencies, poking holes in discrepancies from prior interviews with federal and state prosecutors and disputing his testimony that AMI admitted it violated campaign finance law.
- Prosecutors try to re-establish Pecker’s credibility: Prosecutors responded during redirect to reestablish Pecker’s credibility in his answers, showing how his story was consistent and that AMI did admit to campaign finance violations. The points were small in the grand scheme of Pecker’s testimony related to the case, but the fight was really about Pecker’s credibility as a witness. That’s key to the prosecution’s case because he helps tie together the larger hush money scheme – and will be a corroborator of Cohen’s testimony.
- Trump cracks a smile for his longtime assistant: Trump’s longtime assistant Rhona Graff testified for less than an hour. Graff managed Trump’s contacts and calendar for much of her 34 years as his assistant at Trump Tower. Graff’s testimony about her former boss prompted a smile from an otherwise subdued Trump on Friday.
- Defense tries to humanize Trump: Pecker was a longtime friend of Trump dating back to the 1980s, the former AMI chief said on the stand. As his ending question, Bove asked Pecker if he believed Trump cares about his family. He replied, “Of course I do.” Graff no longer works for Trump but she spoke positively about her experience at the Trump Organization and having Trump as a boss. Other coming witnesses, like Cohen and Daniels, will have a far more hostile view of the defendant in this case.
Trump's hush money criminal trial has been on since 2 weeks. Recap what's happened so far
From CNN staff

The second week of court proceedings in Donald Trump's historic hush money criminal trial has wrapped.
To refresh your memory, here are the key moments and witnesses from the trial so far:
April 15: Trial began with jury selection
April 19: A panel of 12 jurors and six alternates was selected.
April 22: Prosecution and defense made their opening statements. Former tabloid boss David Pecker was called to testify.
April 23: Judge Juan Merchan held a Sandoval hearing for Trump's alleged gag order violations, but reserved his decision.
April 25: While Trump sat in the Manhattan courtroom, the Supreme Court heard arguments on the matter of his immunity in special counsel Jack Smith's election subversion case against him.
April 26: Pecker's direct questioning and cross-examination concluded. Trump's former longtime assistant Rhona Graff was called to testify briefly. Finally, Michael Cohen's former banker Gary Farro testified.
See courtroom sketches from Trump's trial
No cameras are allowed inside the Manhattan courtroom where Donald Trump’s hush money is underway, but sketch artists are capturing the scenes.

Trump's hush money trial has wrapped up for the week. Here's what happened on Friday
The jury in Donald Trump's hush money trial heard from two new witnesses on Friday after former National Enquirer publisher David Pecker finished his testimony.
Trump’s defense team tried to poke holes in Pecker’s story, pointing out discrepancies and trying to undermine his credibility. Pecker had testified during direct questioning from the prosecution about how he helped broker a deal with Stormy Daniels and arranged to “catch and kill” a story about an alleged affair between Trump and Karen McDougal.
Prosecutors also had the chance to revisit various lines of questions in their redirect before calling Rhona Graff , Trump’s former long-term assistant, to the stand. After that, prosecutors called finance executive Gary Farro .
Farro will continue his testimony on Tuesday. Court is not in session on Monday.
Here’s what happened in court today:
David Pecker
- Trump Tower meeting: Pecker told Trump attorney Emil Bove that the concept of “catch and kill” was not discussed at an August 2015 meeting at Trump Tower . According to Pecker’s previous testimony, that’s when he agreed to be the “eyes and ears” for the Trump campaign and flag negative stories to Michael Cohen.
- Redirect: Pecker said after the 2015 meeting, he and Cohen had an understanding that Pecker was going to use his resources at the Enquirer to flag potentially negative stories to Cohen. He testified that before the 2015 meeting, he did not previously have deals to share positive stories about candidates or agree to run stories attacking Trump’s opponents.
- Stories about Trump’s opponents: During cross-examination, Bove confirmed with Pecker that the Enquirer often recycled content from other outlets about Trump’s opponents. The outlet did that without notifying Trump, Pecker said, and confirmed the stories were based on information that was not exclusive to the Enquirer because it was not cost-efficient.
- McDougal agreement: Pecker agreed that McDougal, who said she had an affair with Trump, was not focused on the payment part of the agreement. Pecker confirmed McDougal wanted to relaunch her career and there were other provisions in the deal . He previously testified that the other elements were intended to “hide” the actual intention of the payment.
- Redirect: The prosecution revisited this point and had Pecker re-confirm that the purpose of the contract with McDougal was to suppress a potentially damaging story about Trump and influence the 2016 election.
- Legal concerns: Pecker said he told Cohen that the agreement with McDougal was legally sound . He said he reviewed the agreement with a campaign attorney and his company’s general counsel.
- Redirect: Pecker said he never spoke directly with the campaign lawyer and he did not tell the AMI general counsel about the arrangement that was struck with Trump during the August 2015 Trump Tower meeting. The prosecution is trying to infer that the lawyers who reviewed the contract did not have the full underlying context of Pecker’s agreement with Trump.
- Stormy Daniels: The former tabloid boss confirmed to the defense that he wanted nothing to do with Daniel’s story and told Cohen that his company AMI would not buy it.
- Redirect: Pecker reiterated that he called Cohen with then-editor-in-chief Dylan Howard encouraging him to buy Daniels’ story .
- FBI interview discrepancy: Pecker testified this week that Trump thanked him for handling stories about McDougal and Trump Tower doorman Dino Sajudin during a January 2017 meeting at Trump Tower. But the defense pointed out that "Trump did not express any gratitude to Pecker and AMI" during his 2018 FBI interview .
- Redirect: Steinglass read notes from an FBI meeting one week after the meeting highlighted by Bove that confirmed that Pecker told the FBI that Trump thanked him.
Rhona Graff
- Answering questions from prosecutor Susan Hoffinger, Graff said she worked for Trump for 34 years at the Trump Organization. She was largely in control of his calendar and in charge of maintaining Trump's contacts.
- She recalled seeing Daniels in the reception area at Trump Tower before Trump ran for president. She later testified to the defense that she assumed Daniels’ visits were to discuss being cast for "The Apprentice." In addition to Daniels, Graff testified she also kept contact information for McDougal .
- During cross-examination, attorney Susan Necheles asked Graff about what it was like working with Trump. She described it as a very “stimulating, exciting, fascinating place to be” and said Trump was a “respectful boss.”
- Farro was previously a senior managing director at First Republic Bank where he worked with Cohen . He said Cohen coordinated with him to set up an account for Resolutions Consultants LLC for the payment to McDougal that never happened. Jurors saw emails between Farro and Cohen.
- Farro testified that his understanding was that Cohen was opening the account for “real estate.” In the paperwork , Cohen described the entity's function to be "management consulting (including HR & marketing).”
- Farro said the Resolution Consultants LLC account was never opened because no deposit was made. Nearly two weeks later, Farro said Cohen told him he wanted to open a new account instead.
- The new account, Essential Consultants LLC , was used to pay Daniels $130,000. On the paperwork, Cohen said this account was for a real estate consulting company.
Gag order: Judge Juan Merchan said there will be a hearing on Thursday morning to discuss possible violations of the gag order against Trump.
Trump hush money criminal trial may see “quite a few somewhat dull witnesses,” expert says
From CNN’s Aditi Sangal
Donald Trump’s hush money criminal trial will see “quite a few somewhat dull witnesses,” said former federal prosecutor Ankush Khardori.
The case is less about the salacious details of Trump's alleged affair with Stormy Daniels — that he denies — and more about the allegations that he covered it up to influence the 2016 presidential election, he points.
“The crime actually has to do with all of this somewhat banal record-keeping stuff. This is a case where I think we’re going to actually see quite a few somewhat dull witnesses producing things like documents, ledgers, invoices, things that just have to come into evidence to complete this case,” he told CNN.
Meanwhile, prosecution and defense also have to be mindful of the approaching weekend.
As a prosecutor, “you like the idea of leaving [the jurors] with something solid, unchallenged, good at the end of the week,” said Trump’s former attorney Jim Trusty.
“They’re basically introducing some paperwork for the jury to look at at 4:30 before they go home, and go, oh there were checks, or there were meetings, or there were contacts.”
It’s also smart for the defense “to keep it dull, to basically not spend any time cross-examining people where you have no real reason to gain anything because they’re not establishing criminality or they’re not establishing controversial points,” he added.
Leaving court, Trump says he'll debate Biden
From CNN's Kaanita Iyer
After exiting the courtroom Friday, former President Donald Trump once again said he would debate President Joe Biden.
"I've invited Biden to debate. He can do it any time he wants, including tonight. I'm ready — here we are. ... I'm here, ready willing and able," Trump said.
Earlier Friday, Biden said in an interview with radio host Howard Stern that he'd be happy to debate Trump .
Judge Merchan says he's calling it a week
Mangold says she's at a natural stopping point and Judge Merchan says, we will "call it a week."
He is now giving the jury instructions.
Trump hit his attorney Todd Blanche on the arm and leaned over to tell him something.
Merchan reminds jurors court is dark on Monday and we are back 9:30 a.m. on Tuesday.
Merchan says, "Have a good weekend, take care."
Farro says Cohen "changed course" once before opening LLC that he used to make Stormy Daniels payment
Farro says the bank "did all of our work to establish" Cohen's original account, but it was never funded.
"A deposit was never made in the account, so the account never went live," Farro says.
Thirteen days later, on October 26, 2016, Farro received another email from his assistant to return Michael Cohen's call, according to the court exhibit.
"He stated he was changing course and no longer wanted to open Resolution Consultants, and wanted to open a new account," Farro says.
"Every time Michael Cohen spoke to me he gave a sense of urgency and this was one of those times."
The new LLC was Essential Consultants LLC, Farro says.
This is the LLC that Cohen used to pay Stormy Daniels the $130,000 payment.
On the form the bank prepared for Cohen to open the account, it stated under "business narrative" that Cohen was opening the account for a real estate consulting company to collect fees for consulting work on real estate deals.
Cohen again checked "No" on a form that asked if the entity is "associated with political fundraising/Political Action Committee (PAC)."
Cohen checked "No" on a form asking if his entity was associated with political fundraising
Cohen checked "No" on a form that asked if the entity, Resolution Consultants LLC, which was created by him as a Delaware entity, is "associated with political fundraising/Political Action Committee (PAC)."
Farro testified several times that his understanding was that Cohen was opening the account for "real estate."
Per the paperwork, Cohen described the entity's function to be "management consulting (including HR & marketing)."
Cohen was the only authorized signatory for the account.
Farro says that the bank "did all of our work to establish" Cohen's account, but it was never funded.
"A deposit was never made in the account so the account never went live," Farro says, confirming the account was not opened.
Please enable JavaScript for a better experience.

IMAGES
COMMENTS
A children's doctor (paediatrician), midwife or newborn (neonatal) nurse will check your baby is well and will offer him or her a newborn physical examination within 72 hours of birth. In the early days, the midwife will check your baby for signs of: jaundice. infection of the umbilical cord or eyes. thrush in the mouth.
The earliest your midwife will discharge you is 10 days after your baby was born. However, even though they may have discharged you, you can still contact your midwife until your baby's 28 days old. Your health visitor will visit you one to two weeks after your midwife has discharged you. If you didn't meet your health visitor when you were ...
Midwives are healthcare providers who deal with pregnancy, childbirth, newborn care and postpartum health. Some midwives provide routine reproductive care like pelvic exams, Pap tests, or counseling on birth control. Midwives tend to be more holistic and supportive of natural approaches to pregnancy and birth. People often choose a midwife when ...
Once you are at home, the midwife should visit you on the first day after you've been discharged from the hospital to check on you and your baby. There is no set number of visits you will have from your midwife after that. They will visit you for as long as they think you need their support. However, you will usually have a minimum of 3 visits ...
Some new parents need more support than others. You'll get extra support from your midwife, family nurse or other health professionals if your baby: was born early; spent time in special or intensive care; has additional needs; Tests and checks. During the first 10 days your midwife will: weigh your baby; do a newborn blood spot test if you agree
After your booking appointment at about 10 weeks, you will usually have these appointments: in your second trimester, in weeks 14-16, 25 and 28. in your third trimester in weeks 31, 34, 36, 38, 40 and 41 (if you haven't given birth before 40 weeks) If you have already had a healthy pregnancy and baby, you will have 7 appointments. As well as ...
IDM is a day of celebration, but also of highlighting how important the work of midwives is globally. This year, we are shining a light on the role midwives play in addressing the greatest health challenge of our time - climate change. #IDM2024 is both a celebration and a call to action for our planet and for midwifery.
4. Paperwork. At your first prenatal visit you will probably have some paperwork to sign and your midwife or doctor's office will probably need a copy of your health insurance card. Many midwives will give you an estimate costs for your pregnancy and birth care, so you are both on the same page in terms of cost.
200 women received 1 visit by a midwife at about 42 days postpartum. ... First visit 10‐14 days, 6 visits up to 8 weeks (weekly). 159 women completed the pre‐test (nominated by 40 health visitors). The control group received 1 health visitor visit at 10‐14 days. Health visitors provided advice and support, carried out assessments and ...
Your first midwife appointment. As soon as you find out you are pregnant, contact a GP or midwife and they will help you book your first appointment. Your first midwife appointment (also called the booking appointment) should happen before you're 10 weeks pregnant. This is because you'll be offered some tests that should be done before 10 weeks.
Sustainable Development Goal #3.8 is to achieve universal health coverage by 2030. A larger, fully enabled #midwifery workforce would increase women's, children's and adolescents' access to health care. That is to say: investing in #midwives will strengthen the primary healthcare system and provide a pathway to universal health coverage .
You'll always be given the chance to ask questions. At every appointment, your midwife will ask permission to take your blood pressure and check your urine for glucose and protein. Your midwife will feel your tummy to see how your baby is growing, and listen to your baby's heartbeat. Towards the end of your pregnancy, they'll also ask ...
Diagnosis and treatments. Our midwives offer: Birth control, including oral contraceptives, intrauterine devices or contraceptive implants and injections. Breast care. Breastfeeding assistance. Gynecological preventive exams. Labor and delivery at the birthing center. Pelvic exams. Postpartum care.
Climate change poses unprecedented challenges to health, especially for women and babies. As midwives, we play a pivotal role in reducing the effects of climate change. Our model of care is inherently sustainable, and by promoting continuity of midwife care, we can ensure healthier outcomes while using a sustainable, low-resource model of care.
1.1.4. When caring for a baby, remember that those with parental responsibility have the right be involved in the baby's care, if they choose. 1.1.5. When giving information about postnatal care, use clear language and tailor the timing, content and delivery of information to the woman's needs and preferences.
You'll have a number of antenatal appointments during your pregnancy, and you'll see a midwife or sometimes an obstetrician (doctor specialising in pregnancy). They'll check the health of you and your baby, give you useful information and answer any questions. Pregnant employees have the right to paid time off for antenatal care.
ICM - The International Confederation of Midwives supports midwives
Dear Editor, During the COVID-19 pandemic postnatal midwifery-led care remains a key public health intervention for women and their families 1,2.Home or virtual visits by community midwives should be provided to reduce the number of times women and newborns need to leave their home 1.In order to comply with social distancing requirements, community midwives could deliver home or virtual visits ...
For this reason, the theme for this year's International Day of the Midwife (IDM), is Midwives: A Vital Climate Solution. As midwives we might not immediately see ourselves in as a part of the climate solution. At the same time, it is obvious that the midwifery model of care is environmentally friendly. Evidence shows that continuity of ...
1 First health visitor visit 2 1.1.4 Consider arranging the first postnatal health visitor home visit to take 3 place between 7 and 14 days after transfer of care from midwifery care so 4 that the timing of postnatal contacts is evenly spread out. 5 1.1.5 If a woman did not receive an antenatal health visitor visit, consider
Birth visit to 10 to 14 days postnatal. ... If women require midwifery input after day 14, the midwife and health visitor should aim to have a verbal handover in addition to a written handover ...
day 3 if breastfeeding; day 5; between days 10 and 14; More frequent visits may be arranged as needed. If you require a visit or appointment before your next scheduled one you can call the Community Midwifery Enquiry Line Maternity Contacts - CHFT (cht.nhs.uk) (links to an external website)
Here are 10 players that would fit the Lions on Day 3, sorted by their projected round. Fourth Round. Note: The Lions do not currently own a fourth-round selection. In order to acquire these ...
Iran's President Ebrahim Raisi and Pakistan's Prime Minister Shehbaz Sharif vowed on Monday to boost trade between the neighbouring nations to $10 billion a year, as Raisi commenced a three-day ...
0. Hackers backed by a powerful nation-state have been exploiting two zero-day vulnerabilities in Cisco firewalls in a five-month-long campaign that breaks into government networks around the ...
With one day until the 2024 NFL Draft, here are 10 fresh mock drafts. Cooper DeJean of Iowa was a popular pick. ... Packers Will Host Ohio State Defensive Lineman on Predraft Visit.
One NFL insider thinks teams will have to get into the top-10 if they want the rights to Brock Bowers in the 2024 NFL Draft. The 2024 NFL Draft is creeping closer and closer, and now buzz is ...
The Bills are scheduled to pick 10 times over the course of the three-day NFL Draft, which kicks off Thursday night in Detroit. Here's the vital info for fans who plan to watch the proceedings live.
A model and actress who has said she had a monthslong affair with Donald Trump in 2006 and was paid $150,000 to keep quiet about it by the National Enquirer. Trump has denied the affair ...