National Geographic content straight to your inbox—sign up for our popular newsletters here

Bedbugs, ticks, and worms: A traveler’s guide to pests
Some of them are just gross; others can really harm you. Here’s how to stop creepy-crawlies from spoiling your trip.

While bedbugs have grabbed headlines lately, the tiny bloodsuckers are more icky than dangerous. In fact, “the deadliest animal in the world is the mosquito,” says Molly Keck , an entomologist who specializes in pest management at Texas A & M AgriLife . Creepy crawlies—insects, arachnids, worms, and more—are everywhere.
Bugs can carry pathogens such as bacteria, nematodes, protozoa, and viruses which transmit tricky-to-diagnose diseases to humans. Many of these illnesses (e.g., dengue fever , Lyme disease ) can start with vague symptoms like a headache, fatigue, or fever—and there’s not always a telltale bite mark.
When travelers get sick, it’s understandable to want to get home immediately to familiar medical care, says William Spangler, an emergency medicine doctor and the global medical director with insurance company AIG Travel . “It’s likely better to seek treatment locally, where practitioners know the endemic disease and how to treat it.”
( Why bedbugs are everywhere—and what you can do about them .)
Before a trip, consider visiting a travel medicine clinic , which can tailor medications and vaccinations to your destination. And read on for intel on all the bugs you really want to avoid.
The culprit: Bedbugs
Including Cimex lectularius (common bedbug) and Cimex hemipterus (tropical bedbug).
Where they are
Furniture, carpets, and suitcases around the world.
How they can hurt you and what to do
“You don’t have to travel to get bedbugs,” says Keck. “You can get them from your school, sitting in a waiting room, or from a visiting friend.”
Though bedbugs can carry viruses, they rarely transmit pathogens to humans . Their bites are painless; clusters or zigzags of itchy welts are an allergic reaction that can appear up to nine days later. “The bites can really only be treated by antihistamines and the relief will be limited,” says Spangler.
The good news? Bedbugs can’t fly. When not sucking your blood, they prefer hiding in dark places like the creases of mattresses.
“To avoid bringing bedbugs home, place your bags in the hotel tub where they cannot climb,” says Keck. “Then inspect the bed by pulling the sheets and mattress pad up, looking at the elastic areas, and checking all around the bed.” If you see the apple seed-sized reddish brown bugs, their pale yellow eggs, or blood stains, Keck says to “ask for another room not touching the one you’re in,” meaning neither next door, above, nor below it.
Bedbugs prefer cloth luggage over plastic or metal , and it’s easier to spot them on light colors if you do an inspection with your phone flashlight. Rejoice if it’s cold when you return home: storing your suitcase outside for 80 hours below 32° Fahrenheit kills the pests. Washing your clothes in hot water followed by a half-hour high-heat tumble dry helps too.
The culprit: Mosquitoes
Including Aedes mosquitoes that transmit chikungunya, dengue, yellow fever , and Zika; Culex that cause West Nile fever ; and the malaria -spreading Anopheles.
Where they are
Around the world except Iceland and Antarctica ; disease-carrying species prefer tropical, subtropical, and some temperate climates.
“Mosquito-borne diseases kill approximately one million people worldwide every year,” says Spangler. Mosquitoes cause 200 million cases of malaria annually with about 625,000 deaths , and an estimated 100 to 400 million cases of dengue with about 40,000 deaths . While 80 percent of dengue infections have no symptoms , it’s nicknamed “breakbone fever” because it can cause such intense pain.
( How travel insurance might help you if you get sick on vacation .)
People living in countries with disease-carrying mosquitoes are most affected, but travelers aren’t immune. Plus climate change is expanding mosquitoes’ territory . The U.S., for example, has suffered cases of locally acquired malaria in 2023. And the World Health Organization warns that, within this decade, dengue will become a major threat to more places in Europe and the U.S.
When planning a trip, Spangler recommends checking the Centers for Disease Control and Prevention’s (CDC) maps, which provide travel information about illnesses like dengue and malaria . Travel medicine clinics can advise if you need malaria-prevention pills and vaccinations for yellow fever. A second malaria vaccine was approved in early October . It, and a limited-use dengue vaccine , hold promise for the future.
It’s best to prevent mosquito bites in the first place. Use insect repellent with picaridin or DEET and wear long sleeves and pants, ideally treated with permethrin. Sleep with a mosquito net, but note that new research counters previously held theories that malaria mosquitoes only bite at night . A 2022 study found that 20 to 30 percent of Anopheles mosquito bites happen during the day .

The culprit: Biting midges or no-see-ums
About 4,000 species of Ceratopogonidae.
Worldwide (except Antarctica and the Arctic), especially near coasts, lakes, and rivers.
How they can hurt you and what to do
Often as tiny as a pencil point but up to an eighth of an inch long, biting midges are a type of fly. Depending on where you live, you might call them no-see-ums, midges, punkies, or, in Florida and Alabama , five-O’s—a reference to 5 p.m., when they start feasting on humans.
Biting midges are more annoying than dangerous (although they can spread rare diseases like Oropouche fever in Central and South America ). Keck says, “True no-see-ums or biting midges are actually very easy to spot because their bite is painful.” Some people get an allergic reaction that feels even worse, usually itchy red welts and swelling.
Bug spray, even with DEET, provides only limited protection . Wearing long sleeves and pants (consider tucking them into your socks), prevents bites. Hats with a fine net can protect your face.

The culprit: Ticks
Ixodidae (hard ticks) and Argasidae (soft ticks); about 60 of the 900 species can spread diseases to humans , including the “Lyme disease tick” Ixodes scapularis.
Grassy and bushy areas—even in cities—on every continent except Antarctica and in all U.S. states except Alaska .
Technically an eight-legged arachnid, ticks are bloodsuckers. They can’t fly or jump, but some ticks wait on the tips of shrubs on well-used paths and can quickly climb onto a person (or pet) that brushes by.
While they eat, ticks hold themselves in place by stabbing a barbed harpoon into your skin. This makes them difficult to remove. It can take them a day or two to finish their meal, but tick bites are usually painless, often go unnoticed, or are mistaken for mosquito bites.
“Different infectious pathogens are carried by different species of ticks,” says Lin H. Chen , director of the Mount Auburn Hospital Travel Medicine Center and a professor at Harvard Medical School. About 476,000 people in the U.S. are diagnosed with Lyme disease every year. Other U.S. tick-borne diseases include Rocky Mountain spotted fever, tularemia, and anaplasmosis. Travelers doing extensive outdoor activities in Europe and Asia are at risk of tick-borne encephalitis and might consider a vaccine .
“There are a number of readily available repellents that have some effectiveness,” says Spangler, “but in tick-prone areas, you basically want to limit your exposed skin with good footwear, long pants, and long sleeves. If you’ve been outside near tall grass or other foliage, conduct a full-body inspection to look for ticks—it’s possible to spot one on your clothes (or even your skin) before they’ve latched on.” A shower within two hours can also help wash away any ticks that haven’t yet attached themselves.

The culprit: Parasitic worms
Including blood flukes ( Schistosoma ) and hookworms ( Ancylostoma duodenale and Necator americanus ).
Tropical and subtropical countries, especially where sanitation is poor, including on beaches where dogs and cats roam freely.
While travelers rarely get infected with parasitic worms, it’s certainly something to avoid. Symptoms can be minor (stomach pain) or serious (seizures), though even the thought of a worm infection may make you nauseated. It’s possible to eat worms or their eggs, especially in undercooked meat or poorly washed vegetables. This can result in trichinosis (caused by roundworms), tapeworms, or even that headline-making worm found in an Australian woman’s brain . Kids, including in the U.S., are known for spreading pinworms , principally if they don’t wash their hands well after using the bathroom.
Travelers also need to be aware of “environmental exposures like wading in freshwater,” says Chen, which has “potential risks of schistosomiasis and leptospirosis ” and of walking barefoot through soil and sand contaminated with hookworm or Strongyloides .
About 230 million people globally have flu-like schistosomiasis (also called bilharzia) and 200,000 people die annually from it, mostly, but not exclusively, in Africa . According to the CDC, malaria is the only parasitic disease that’s more devastating than schistosomiasis . Blood flukes (schistosomes) replicate in freshwater snails found in 78 countries; they mainly spread when infected people urinate or defecate. The parasite can survive for 48 hours after leaving the snail and can enter human skin that’s in contact with contaminated water.
Poor sanitation can also lead to worm infections through the soles of your feet, especially from soil and sand where cats and dogs defecate. Keeping your shoes on is the best way to avoid larvae such as hookworms and whipworms and the lesions, diarrhea, anemia, and rectal prolapse they can cause. Prescription medications are effective for many worms, assuming you get the right diagnosis.
Feeling grossed out? That might be okay, since it can remind you to take precautions like applying bug spray and keeping your skin covered in higher-risk areas. And, as Keck says, “Remember that there are far more beneficial insects than harmful [ones]. Most are not going to sting, bite, transmit a disease, or hurt you in any way.”

Related Topics
- PUBLIC HEALTH
You May Also Like

These bug repellents actually work—if you use them correctly

New anxiety unlocked: Ticks can 'fly'
For hungry minds.

How to keep ticks out of your backyard

How to plan a food tour around northern Thailand, from Chiang Mai to Phrae

How to plan a food weekend on the UK's Suffolk coast

Salmonella can be deadly. Here’s how to protect yourself from it.

Should you still travel if you have Covid?
- Environment
History & Culture
- History & Culture
- History Magazine
- Gory Details
- Mind, Body, Wonder
- Paid Content
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved
From Contaminated Food and Water
International travelers can be at risk for a variety of infectious and non-infectious diseases. Travelers may acquire parasitic illnesses:
- through ingestion of contaminated food or water,
- by vector-borne transmission, or
- through person-to-person contact.
Contaminated food and drink are common sources for the introduction of infection into the body. The table below shows some of the more common parasitic infections that travelers can acquire from contaminated food and drink, as well as a few of the less common parasitic diseases that travelers are at risk for acquiring. The risk of acquiring these other protozoa and helminths varies greatly by region of the world and specific country. Many infectious diseases transmitted in food and water can also be acquired directly through the fecal-oral route.
From Contaminated Food and Water
more common.
- Cryptosporidiosis
- Cyclosporiasis
Less Common
- Trichinellosis (trichinosis)
- Taenia infection
- Fascioliasis
From Vector-borne Transmission
- Leishmaniasis
- Chagas disease
- Lymphatic filariasis
- African sleeping sickness
- Onchoceriasis
*This list is not comprehensive.
International travelers can take a number of simple steps before and during travel to avoid potential health problems. International travelers should
- contact their physicians, local health departments, or private or public agencies that advise international travelers at least 4 to 6 weeks before departure to schedule an appointment to receive current health information on the countries they plan to visit,
- obtain vaccinations and prophylactic medications as indicated, and
- address any special needs.
CDC’s Travelers’ Health Web site contains detailed advice for health care providers. Health departments, the travel industry, multinational corporations, missionary and volunteer organizations, and travelers can also use this information to help make international travel as healthy and safe as possible.
Related Links
- Healthy Swimming
- Healthy Water
To receive email updates about this page, enter your email address:
- Neglected Tropical Diseases
Laboratory Diagnostic Assistance (DPDx)
CDC Traveler’s Health
For Healthcare Providers, Emergency Consultations, and General Public.
Contact Us -->
Information For
- Health Professionals
- Public Health Departments
- Laboratory Science
- Parasites A-Z Index
- Parasites Glossary
- Laboratory Diagnostic Assistance [DPDx]
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
Traveler's Diarrhea
What is traveler's diarrhea, what causes traveler's diarrhea.
It’s caused by drinking water or eating food that has bacteria, viruses, or parasites. Most traveler's diarrhea is from bacteria. Diarrhea from viruses and parasites is less common. Food and water can be infected by people:
- Not washing hands after using the bathroom
- Storing food unsafely
- Handling and preparing food unsafely
- Not cleaning surfaces and utensils safely
Who is at risk for traveler's diarrhea?
You are at risk for this condition if you travel to a country that has poor public sanitation and hygiene. Poor hygiene in local restaurants is also a risk factor. Places that have the highest risk are often in developing countries in:
- Central and South America
- The Middle East
If you travel to a developing country, you are more likely to get this illness if you eat food or have drinks:
- Bought on the street, such as from a food cart
- In someone’s home
- At lodging that provides all meals (all-inclusive)
You’re also at increased risk if you:
- Take some kinds of ulcer medicine
- Have had some kinds of gastrointestinal surgery
What are the symptoms of traveler's diarrhea?
The main symptom is loose stool that occurs suddenly. The stool may be watery. Other symptoms may include:
- Belly (abdominal) pain or cramps
- Blood in the stool
- Trouble waiting to have a bowel movement (urgency)
- Feeling tired
In most cases, symptoms last less than a week.
How is traveler's diarrhea diagnosed?
How is traveler's diarrhea treated, what are possible complications of traveler's diarrhea.
The loss of body fluid from diarrhea and vomiting can lead to dehydration. This can be serious. Contact your healthcare provider if you are not urinating as much as usual.
A small number of people can develop post-infectious irritable bowel syndrome. This can cause symptoms such as:
- Long-term diarrhea
- Belly pain and cramping
What can I do to prevent traveler's diarrhea?
You can take steps to prevent traveler's diarrhea.
Only use water that has been boiled or chemically disinfected for:
- Making tea or coffee
- Brushing your teeth
- Washing your face
- Washing your hands (or use alcohol-based gel)
- Washing fruits and vegetables
- Washing food utensils, equipment, or surfaces
- Washing the surfaces of food or drink tins, cans, and bottles
Don't eat foods such as:
- Raw fruits, vegetables, or salad greens
- Unpasteurized milk, cheese, ice cream, or yogurt
- Any fish caught in tropical reefs rather than the open ocean
- Condiments that are left on the table, such as ketchup, mustard, sauces, or dips
Also make sure to:
- Not eat food from unknown sources
- Not put ice in drinks
- Only have drinks that are bottled and sealed
- Use drinking straws instead of drinking directly from glasses or cups
- Only take antibiotic or antidiarrheal medicine if advised by your health care provider (these can make symptoms worse, which can be dangerous)
When should I call my healthcare provider?
Call a healthcare provider if you:
- Have diarrhea that is severe or bloody
- Have belly pain that is getting worse or not going away
- Have a high fever
- Are not getting better within a few days
- Have signs of dehydration, such as urinating less
- Traveler's diarrhea occurs within 10 days of travel to an area with poor public hygiene. It’s the most common illness in travelers.
- It’s caused by drinking water or eating foods that have bacteria, viruses, or parasites.
- It usually goes away without treatment in a few days.
- Dehydration from diarrhea can be serious. You need to replace body fluid that has been lost.
- See a healthcare provider if your symptoms are severe or last for more than a few days.
- You can prevent it by avoiding unsafe water and not eating unsafe foods.
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Find a Doctor
Specializing In:
- Gastroenterology
- Indigestion
- Diarrheal Disease
- Clostridium Difficile
At Another Johns Hopkins Member Hospital:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Find a Treatment Center
- Gastroenterology and Hepatology
Find Additional Treatment Centers at:
Request an Appointment

Collagenous and Lymphocytic Colitis
Diarrhea in Children
Related Topics

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Traveler's guide to avoiding infectious diseases
You can stay healthy during travel by taking the right steps to protect yourself before you go. You can also do things to help prevent disease while you are traveling. Most infections you catch while traveling are minor. In rare cases, however, they can be severe, or even deadly.
Diseases vary in different places in the world. You will need to take different preventive steps, depending on where you are going. The following things should be considered:
- Insects and parasites
- Local climate
The best public sources for up-to-date travel information are the:
- Centers for Disease Control and Prevention (CDC) -- www.cdc.gov/travel
- World Health Organization (WHO) -- www.who.int/health-topics/travel-and-health#tab=tab_1
BEFORE TRAVEL
Talk to your health care provider or visit a travel clinic 4 to 6 weeks before you leave for your trip. You may need several vaccinations. Some of these need time to work.
You also may need to update your vaccinations. For example, you may need "booster" vaccines for:
- Diphtheria, tetanus, and pertussis (Tdap)
- Influenza (flu)
- Measles - mumps - rubella (MMR)
You also may need vaccines for diseases that are not commonly found in North America. Examples of recommended vaccines include:
- Hepatitis A
- Hepatitis B
- Meningococcal
Certain countries have required vaccinations. You may need proof that you have had this vaccine in order to enter the country.
- Yellow fever vaccination is required to enter certain Sub-Saharan, Central African, and South American countries.
- Meningococcal vaccination is required to enter Saudi Arabia for the Hajj pilgrimage.
- For a complete list of country requirements, check the CDC or WHO websites.
People who may have different vaccine requirements include:
- Older people
- People with weakened immune systems or HIV
- People who expect to be in contact with certain animals
- Women who are pregnant or breastfeeding
Check with your provider or local travel clinic.
PREVENTING MALARIA
Malaria is a serious disease that spreads by the bite of certain mosquitoes, typically biting between dusk and dawn. It occurs mainly in tropical and subtropical climates. Malaria can cause high fevers, shaking chills, flu-like symptoms, and anemia. There are 4 types of malaria parasites.
If you are traveling to an area where malaria is common, you may need to take medicines that prevent the disease. These medicines are taken before you leave, during your travel, and for a short period after you return. How well the medicines work varies. Some strains of malaria are resistant to some preventive medicines. You should also take steps to prevent insect bites.
Zika is a virus passed to humans by the bite of infected mosquitoes. Symptoms include fever, joint pain, rash, and red eyes (conjunctivitis). The mosquitoes that spread Zika are the same type that spread dengue fever and chikungunya virus . These mosquitoes usually feed during the day. No vaccine exists for preventing Zika.
There is believed to be a link between mothers with Zika infection and babies born with microcephaly and other birth defects. Zika can spread from a mother to her baby in the uterus (in utero) or at the time of birth. A man with Zika can spread the disease to his sex partners. There have been reports of Zika spreading through blood transfusion.
Before 2015, the virus was found mainly in Africa, Southeast Asia, and the Pacific Islands. It has now spread to many states and countries including:
- Caribbean Islands
- Central America
- North America
- South America
- Puerto Rico
The disease has been found in certain regions of the United States. For the most up-to-date information, please visit the Centers for Disease Control and Prevention's (CDC) website -- www.cdc.gov/zika .
To prevent getting the Zika virus, take steps to avoid mosquito bites. Sexual transmission of the virus can be prevented by using condoms or not having sex with a person who is possibly infected.
PREVENTING INSECT BITES
To prevent against bites from mosquitoes and other insects:
- Wear insect repellent when you are outdoors, but use it safely . Conventional repellents include DEET and picaridin. Some biopesticide repellents are oil of lemon eucalyptus (OLE), PMD, and IR3535.
- You may also need to use a bed mosquito net while you sleep.
- Wear trousers and long-sleeved shirts, particularly at dusk.
- Sleep only in screened areas.
- Do not wear perfumes.
FOOD AND WATER SAFETY
You can get some types of infections by eating or drinking contaminated food or water. There is a high risk of infection from eating undercooked or raw foods.
Stay away from the following foods:
- Cooked food that has been allowed to cool (such as from street vendors)
- Fruit that has not been washed with clean water and then peeled
- Raw vegetables
- Unpasteurized dairy foods, such as milk or cheese
Drinking untreated or contaminated water can lead to infection. Only drink the following liquids:
- Canned or unopened bottled beverages (water, juice, carbonated mineral water, soft drinks)
- Drinks made with boiled water, such as tea and coffee
Do not use ice in your drinks unless it is made from purified water. You can purify water by boiling it or by treating it with certain chemical kits or water filters.
OTHER STEPS TO PREVENT INFECTIOUS DISEASES
Clean your hands often. Use soap and water or an alcohol-based cleanser to help prevent infection.
Do not stand or swim in fresh-water rivers, streams, or lakes that have sewage or animal feces in them. This can lead to infection. Swimming in chlorinated pools is safe most of the time.
WHEN TO CONTACT A MEDICAL PROFESSIONAL
Diarrhea can sometimes be treated with rest and fluids. Your provider may give you an antibiotic to take on your trip in case you get sick with severe diarrhea while traveling.
Get medical care right away if:
- Diarrhea does not go away
- You develop a high fever or become dehydrated
Contact your provider when you return home if you were sick with a fever while traveling.
Alternative Names
Travelers' health; Infectious diseases and travelers

Beran J, Goad J. Routine travel vaccines: hepatitis A and B, typhoid. In: Keystone JS, Kozarsky PE, Connor BA, Nothdurft HD, Mendelson M, Leder, K, eds. Travel Medicine . 4th ed. Philadelphia, PA: Elsevier; 2019:chap 11.
Centers for Disease Control and Prevention website. Zika virus. For healthcare providers: clinical evaluation and disease. www.cdc.gov/zika/hc-providers/preparing-for-zika/clinicalevaluationdisease.html . Updated January 28, 2019. Accessed November 28, 2023.
Centers for Disease Control and Prevention website. Zika virus: transmission methods. www.cdc.gov/zika/prevention/transmission-methods.html . Updated July 24, 2019. Accessed November 28, 2023.
Chen LH. Approach to the patient before and after travel. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine . 27th ed. Philadelphia, PA: Elsevier; 2024:chap 265.
Christenson JC, John CC. Health advice for children travelling internationally. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics . 21st ed. Philadelphia, PA: Elsevier; 2020:chap 200.
World Health Organization website. International Travel and Health 12 May 2021 - Country List. cdn.who.int/media/docs/default-source/documents/emergencies/travel-advice/ith2021_countrylist_final_26may2021.pdf?sfvrsn=f8d06644_1&download=true . Published May 12, 2021. Accessed November 28, 2023.
Review Date 11/19/2023
Updated by: Jacob Berman, MD, MPH, Clinical Assistant Professor of Medicine, Division of General Internal Medicine, University of Washington School of Medicine, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Traveler's Health
- Patient Care & Health Information
- Diseases & Conditions
- Traveler's diarrhea
Traveler's diarrhea may get better without any treatment. But while you're waiting, it's important to try to stay hydrated with safe liquids, such as bottled water or water with electrolytes such as an oral rehydration solution (see below). If you don't seem to be improving quickly, several medicines are available to help relieve symptoms.
Anti-motility agents. These medicines — which include loperamide and drugs containing diphenoxylate — provide prompt but temporary relief by:
- Reducing muscle spasms in your gastrointestinal tract.
- Slowing the transit time through your digestive system.
- Allowing more time for absorption.
Anti-motility medicines aren't recommended for infants or people with a fever or bloody diarrhea. This is because they can delay clearance of the infectious organisms and make the illness worse.
Also, stop using anti-motility agents after 48 hours if you have stomach pain or if your symptoms worsen and your diarrhea continues. In such cases, see a doctor. You may need blood or stool tests and treatment with an antibiotic.
- Bismuth subsalicylate. This nonprescription medicine can decrease the frequency of your stools and shorten the length of your illness. However, it isn't recommended for children, pregnant women or people who are allergic to aspirin.
- Antibiotics. If you have more than four loose stools a day or severe symptoms, including a fever or blood, pus or mucus in your stools, a doctor may prescribe a course of antibiotics.
Before you leave for your trip, talk to your doctor about taking a prescription with you in case you get a serious bout of traveler's diarrhea.
Avoiding dehydration
Dehydration is the most likely complication of traveler's diarrhea, so it's important to try to stay well hydrated.
An oral rehydration salts (ORS) solution is the best way to replace lost fluids. These solutions contain water and salts in specific proportions to replenish both fluids and electrolytes. They also contain glucose to enhance absorption in the intestinal tract.
Bottled oral rehydration products are available in drugstores in developed areas, and many pharmacies carry their own brands. You can find packets of powdered oral rehydration salts, labeled World Health Organization (WHO)- ORS , at stores, pharmacies and health agencies in most countries. Reconstitute the powder in bottled or boiled water according to the directions on the package.
If these products are unavailable, you can prepare your own rehydrating solution in an emergency by mixing together:
- 3/4 teaspoon table salt.
- 2 tablespoons sugar.
- 1 quart uncontaminated bottled or boiled water.
- Sugar-free flavor powder, such as Crystal Light (optional).
You or your child can drink the solution in small amounts throughout the day as a supplement to solid foods or formula, as long as dehydration persists. Small amounts reduce the likelihood of vomiting. Breastfed infants also can drink the solution but should continue nursing on demand.
If dehydration symptoms — such as dry mouth, intense thirst, little or no urination, dizziness, or extreme weakness — don't improve, seek medical care right away. Oral rehydration solutions are intended only for urgent short-term use.
Lifestyle and home remedies
If you do get traveler's diarrhea, avoid caffeine, alcohol and dairy products, which may worsen symptoms or increase fluid loss. But keep drinking fluids.
Drink canned fruit juices, weak tea, clear soup, decaffeinated soda or sports drinks to replace lost fluids and minerals. Later, as your diarrhea improves, try a diet of easy-to-eat complex carbohydrates, such as salted crackers, bland cereals, bananas, applesauce, dry toast or bread, rice, potatoes, and plain noodles.
You may return to your normal diet as you feel you can tolerate it. Add dairy products, caffeinated beverages and high-fiber foods cautiously.
Preparing for your appointment
Call a doctor if you have diarrhea that is severe, lasts more than a few days or is bloody. If you are traveling, call an embassy or consulate for help locating a doctor. Other signs that you should seek medical attention include:
- A fever of 102 F (39 C) or higher.
- Ongoing vomiting.
- Signs of severe dehydration, including a dry mouth, muscle cramps, decreased urine output, dizziness or fatigue.
If you have diarrhea and you've just returned home from a trip abroad, share that trip information with your doctor when you call to make an appointment.
Here's some information to help you get ready, and what to expect.
Information to gather in advance
- Pre-appointment instructions. At the time you make your appointment, ask whether there are immediate self-care steps you can take to help recover more quickly.
- Symptom history. Write down any symptoms you've been experiencing and for how long.
- Medical history. Make a list of your key medical information, including other conditions for which you're being treated and any medicines, vitamins or supplements you're currently taking.
- Questions to ask your health care professional. Write down your questions in advance so that you can make the most of your time.
The list below suggests questions to ask about traveler's diarrhea.
- What's causing my symptoms?
- Are there any other possible causes for my symptoms?
- What kinds of tests do I need?
- What treatment approach do you recommend?
- Are there any possible side effects from the medicines I'll be taking?
- Will my diarrhea or its treatment affect the other health conditions I have? How can I best manage these conditions together?
- What is the safest way for me to rehydrate?
- Do I need to follow any dietary restrictions and for how long?
- How soon after I begin treatment will I start to feel better?
- How long do you expect a full recovery to take?
- Am I contagious? How can I reduce my risk of passing my illness to others?
- What can I do to reduce my risk of this condition in the future?
In addition to the questions that you've prepared, don't hesitate to ask questions as they occur to you during your appointment.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may reserve time to go over points you want to talk about in-depth. Your doctor may ask:
- What are your symptoms?
- When did you first begin experiencing symptoms?
- Have you traveled recently?
- Where did you travel?
- Have you taken any antibiotics recently?
- Have your symptoms been getting better or worse?
- Have you noticed any blood in your stools?
- Have you experienced symptoms of dehydration, such as muscle cramps or fatigue?
- What treatments have you tried so far, if any?
- Have you been able to keep down any food or liquid?
- Are you pregnant?
- Are you being treated for any other medical conditions?
- Feldman M, et al., eds. Infectious enteritis and proctocolitis. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 11th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 25, 2021.
- LaRocque R, et al. Travelers' diarrhea: Microbiology, epidemiology, and prevention. https://www.uptodate.com/contents/search. Accessed May 26, 2021.
- Ferri FF. Traveler diarrhea. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed April 28, 2023.
- Diarrhea. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/diarrhea. Accessed April 27, 2023.
- Travelers' diarrhea. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/yellowbook/2020/preparing-international-travelers/travelers-diarrhea. Accessed April 28, 2023.
- LaRocque R, et al. Travelers' diarrhea: Clinical manifestations, diagnosis, and treatment. https://www.uptodate.com/contents/search. Accessed May 26, 2021.
- Khanna S (expert opinion). Mayo Clinic. May 29, 2021.
Products & Services
- A Book: Mayo Clinic Book of Home Remedies
- A Book: Mayo Clinic on Digestive Health
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Your cart is empty
Have an account?
Log in to check out faster.
40% Off* 5-Day Frenzy | Free Shipping on Orders Over $60*

The Good Kind of Travel Bug
When planning to travel internationally, there are tonnes of exciting things to think about – where will you stay, what sights will you see, where will you go to eat?
But there is one thing to consider that isn’t so fun, and if not planned for, it could mean you have very different memories than what you were expecting - traveller’s diarrhoea (TD). Whilst this nasty travel companion is more likely to occur in particular destinations, it can happen in unexpected places too, so it is far better to be prepared than not.
Protecting the integrity of your gut can go a long way towards preventing TD. Probiotics are a simple and convenient way to do this, but it is important to choose a probiotic strain that is well researched across multiple studies to help with TD, as not every probiotic is suitable. Saccharomyces cerevisiae (boulardii), or SB for short, is a probiotic yeast that has demonstrated the benefit of decreasing the risk of TD. It also has the added benefit of decreasing the duration of diarrhoea, should an infection occur. 1
Checking the following list can minimise your chances of contracting traveller’s diarrhoea and understand how to best help yourself recover sooner should the need arise.
Before you travel 2
- Do your research - Knowing what infectious illnesses are most likely to occur in your destination is a great start. You are particularly looking out for food borne (such as salmonella) and water borne (such as E. Colli) illness.
- Pack accordingly – Hand sanitiser and antibacterial wipes need not take up too much space and could stop your holiday from becoming memorable for the wrong reasons.
- Prepare your gut – Taking 5 billion CFU of SB per day for at least 5 days before you travel helps to set you up for success. 3 Try Inner Health Travel Bug next time you’re holidaying.
Whilst travelling 4
- Practice good hand hygiene – Wash your hands with soap and water every time before eating. Carry and use hand sanitiser in destinations where water may be contaminated, or unavailable.
- Be mindful of your meals – Whilst street vendors are a great way to experience local cuisine, they may not have as stringent safety standards as an all-inclusive resort - eating steaming hot food, straight off the pan/grill will help minimise your risk of eating contaminated food.
- Support the gut - Continue to take 5 billion CFU/day of your SB probiotic to lower your TD risk 1
Should you experience diarrhoea symptoms, don’t panic! 4
- Make yourself as comfortable as possible at the place where you are staying – and stay put for a few days. Your body needs rest, plenty of fluids and a bathroom.
- Take an anti-diarrhoea medication such as a loperamide-based medicine.
- Increase your dose of SB to 20 billion CFU/day until symptoms ease, then decrease back to 5 billion CFU/day until you return home. 5
Inner Health Travel Bug contains 5 billion CFU of SB probiotics per capsule and is packaged in a convenient, shelf-stable bottle, making it travel-friendly. One bottle contains enough probiotics for 3 weeks travel, including the 5 days pre-travel dose, and is suitable for adults and children from age 3.
Safe travels!
- McFarland LV, Goh S. Travel Med Infect Di . 2019;27:11-19. doi:10.1016/j.tmaid.2018.09.007
- Infectious diseases. Australian Department of Foreign Affairs and Trade. Updated May 30, 2023. Accessed September 13, 2023. https://www.smartraveller.gov.au/before-you-go/health/diseases
- Kollaritsch HH, Wiedermann G. Prevention of Traveler’s Diarrhea: A Double-Blind Randomized Trial with Saccharomyces cerevisiae Hansen CBS 5926. In: Steffen R, Lobel H, Haworth J et al (eds) Travel Medicine . Springer. 1989. https://doi.org/10.1007/978-3-642-73772-5_69
- Food safety while travelling. Better Health Channel. Updated April 20, 2022. Accessed September 13, 2023. https://www.betterhealth.vic.gov.au/health/healthyliving/Food-safety-while-travelling
- Kollaritsch H et al. Fortschr Med . 1993;111(9):152-156.
What is a Broad Spectrum Probiotic & Do I Need ...
A broad spectrum probiotic is designed to reflect the diversity of a healthy gut. Containing multiple species and...
What is a Broad Spectrum Probiotic & Do I Need One?
What are the benefits of taking a broad spectru....
Taking a broad spectrum probiotic can provide up to 16 health benefits, including energy, digestion, immunity, skin health and...
What are the Benefits of Taking a Broad Spectrum Probiotic?
The benefits of taking probiotics daily.
For everyday gut health, immunity and general wellbeing, taking a probiotic daily can form an important part of...
Subscribe to our emails
Be the first to know about new collections and exclusive offers.
- Choosing a selection results in a full page refresh.
- Opens in a new window.
Travel warning to Brits going to Spain over virus outbreak that's fatal in one third of cases
The Foreign Office-backed Travel Health Pro website warned people thinking of going to the country to watch out for the illness which is passed on through tick bites

- 12:14, 8 May 2024
Brits travelling to Spain have been warned over a virus outbreak that is fatal in almost a third of cases.
The warning was sparked after Crimean-Congo haemorrhagic fever was discovered in Spain, a virus which is fatal in almost a third of cases. The Foreign Office-backed Travel Health Pro website warned people thinking of going to the country to watch out for the illness which is passed on through tick bites.
The Spanish Castile and León Ministry of Health said a patient is in hospital in a serious but stable condition and is in isolation in Salamanca, Bristol Live reports . The ministry said: “The patient remains admitted, stable in serious condition, at the Salamanca Hospital, where the protocolized epidemiological and care measures have been adopted.”
“The confirmed case is an elderly man who is admitted to the Salamanca Hospital with a clinical picture compatible with CCHF. He has a tick bite and remains stable, although with the clinical severity that this pathology implies, with the isolation measures and protection of health professionals provided for these situations.
The Epidemiology Section of the Territorial Health Service of the Government of Castilla y León in the province of Salamanca, in collaboration with doctors at the Hospital of Salamanca, said Crimean-Congo hemorrhagic fever is caused by a virus. It said the: “Main transmission mechanism is the bite of the tick of the genus “Hyalomma”, although it can also be transmitted from person to person through contact with blood or fluids of the patient, which can occur especially in healthcare personnel when they are not properly protected.”
The Spanish health authorities issued advice on how to take action to prevent catching CCHF. It said: “Regarding the prevention of bites by these insects, health authorities remind us of the importance of wearing appropriate clothing and footwear during outings in the countryside, as well as walking along paths and using repellents for both people and pets.
“Likewise, it must be insisted that any ticks that may have attached must be removed as soon as possible and appropriately, preferably by health professionals.”Crimean-Congo haemorrhagic fever was identified in the Crimea (as Crimean fever) in 1944 and in the Belgian Congo (now Democratic Republic of the Congo) in 1956.
In Spain, CCHF virus was first reported in ticks in 2010. The Spanish Ministry of Health reported 12 human cases and 4 deaths in Spain between 2013 and August 2022.
MORE ON Foreign Office Hospitals
Get email updates with the day's biggest stories.

More bugs are coming, spreading more disease. Are doctors ready to respond?
As the climate changes, vector-borne diseases like dengue, zika, and lyme are expanding into more areas. that challenges physicians to recognize the symptoms..

FILE - A traveler pulls his dog in a wheeled carrier at the Benito Juarez International Airport in Mexico City, Wednesday, Dec. 21, 2022. If you are bringing a dog into the U.S. — whether if you are returning from a trip overseas with Rover, visiting the U.S., or adopting a dog from abroad — you have to follow a set of new rules released by the Centers for Disease Control and Prevention on Wednesday, May 8, 2024, designed to help prevent the spread of rabies. (AP Photo/Marco Ugarte, File)
- Copy Link copied
If you are bringing a dog into the U.S. — whether if you are returning from a trip overseas with Rover, visiting the U.S., or adopting a dog from abroad — you have to follow a set of new rules designed to help prevent the spread of rabies.
The Centers for Disease Control and Prevention last updated these rules in 1956, when far fewer dogs came to the U.S. from other countries, officials say. About 1 million dogs now enter the U.S. every year.
There are additional restrictions if the dog has been in many countries where rabies is common. You can find the list of those countries on the CDC website .
The new rules go into affect Aug. 1. There’s a checklist on the CDC website .
Here’s what to know about about the rules:
— Dogs have to be healthy and at least 6 months old when they arrive in the U.S.
— The dog must have a microchip implanted under their skin, which contains identifier information.
— A CDC import form must be filled out in advance, and include a photo of the dog.
— Proof of rabies vaccination is required only if the dog was in a high-risk country in the past six months.
— For dogs vaccinated in the U.S., a certificate endorsed by the Agriculture Department is required.
— For dogs vaccinated outside the U.S., a certificate of vaccination is required along with a blood test, and the animal has to be examined at a CDC-registered facility on arrival in the U.S.
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 5 - Rubella
- Section 5 - Smallpox & Other Orthopoxvirus-Associated Infections
Rubeola / Measles
Cdc yellow book 2024.
Author(s): Paul Gastañaduy, James Goodson
Infectious Agent
Transmission, epidemiology, clinical presentation.
INFECTIOUS AGENT: Measles virus
TRAVELER CATEGORIES AT GREATEST RISK FOR EXPOSURE & INFECTION
PREVENTION METHODS
Rubeola is a vaccine-preventable disease
DIAGNOSTIC SUPPORT
Measles virus is a member of the genus Morbillivirus of the family Paramyxoviridae .
Measles is transmitted from person to person via respiratory droplets and by the airborne route as aerosolized droplet nuclei. Infected people are usually contagious from 4 days before until 4 days after rash onset. Measles is among the most contagious viral diseases known; secondary attack rates are ≥90% among susceptible household and institutional contacts. Humans are the only natural host for sustaining measles virus transmission, which makes global eradication of measles feasible.
Measles was declared eliminated (defined as the absence of endemic measles virus transmission in a defined geographic area for ≥12 months in the presence of a well-performing surveillance system) from the United States in 2000. Measles virus continues to be imported into the country from other parts of the world, however, and recent prolonged outbreaks in the United States resulting from measles virus importations highlight the challenges faced in maintaining measles elimination.
Given the large global measles burden and high communicability of the disease, travelers could be exposed to the virus in any country they visit where measles remains endemic or where large outbreaks are occurring. Most measles cases imported into the United States occur in unvaccinated US residents who become infected while traveling abroad, often to the World Health Organization (WHO)–defined Western Pacific and European regions. These travelers become symptomatic after returning to the United States and sometimes infect others in their communities, causing outbreaks.
Nearly 90% of imported measles cases are considered preventable by vaccination (i.e., the travelers lacked recommended age- and travel-appropriate vaccination). Furthermore, observational studies in travel clinics in the United States have shown that 59% of pediatric and 53% of adult travelers eligible for measles-mumps-rubella (MMR) vaccine at the time of pretravel consultation were not vaccinated at the visit, highlighting a missed opportunity to reduce the likelihood of measles introductions and subsequent spread. Encourage all eligible travelers to receive appropriate MMR vaccination. Outbreak investigations are costly and resource intensive, and infected people—in addition to productivity losses—can incur direct costs for the management of their illness, including treatment, quarantine, and caregiving.
The incubation period averages 11–12 days from exposure to onset of prodrome; rash usually appears ≈14 days after exposure. Symptoms include fever, with temperature ≤105°F (≤40.6°C); conjunctivitis; coryza (runny nose); cough; and small spots with white or bluish-white centers on an erythematous base appearing on the buccal mucosa (Koplik spots). A characteristic red, blotchy (maculopapular) rash appears 3–7 days after onset of prodromal symptoms. The rash begins on the face, becomes generalized, and lasts 4–7 days.
Common measles complications include diarrhea (8%), middle ear infection (7%–9%), and pneumonia (1%–6%). Encephalitis, which can result in permanent brain damage, occurs in ≈1 per 1,000–2,000 cases of measles. The risk for serious complications or death is highest for children aged ≤5 years, adults aged ≥20 years, and in populations with poor nutritional status or that lack access to health care.
Subacute sclerosing panencephalitis (SSPE) is a progressive neurologic disorder caused by measles virus that usually presents 5–10 years after recovery from the initial primary measles virus infection. SSPE manifests as mental and motor deterioration, which can progress to coma and death. SSPE occurs in ≈1 of every 5,000 reported measles cases; rates are higher among children <5 years of age.
Measles is a nationally notifiable disease. Laboratory criteria for diagnosis include a positive serologic test for measles-specific IgM, IgG seroconversion, or a significant rise in measles IgG level by any standard serologic assay; isolation of measles virus; or detection of measles virus RNA by reverse transcription PCR (RT-PCR) testing. The Centers for Disease Control and Prevention’s Measles Virus Laboratory is the national reference laboratory; it provides serologic and molecular testing for measles and technical assistance to state public health laboratories for the collection and shipment of clinical samples for molecular diagnostics and genetic analysis. See detailed information on diagnostic support .
A clinical case of measles illness is characterized by generalized maculopapular rash lasting ≥3 days; temperature ≥101°F (38.3°C); and cough, coryza, or conjunctivitis. A confirmed case is one with an acute febrile rash illness with laboratory confirmation or direct epidemiologic linkage to a laboratory-confirmed case. In a laboratory-confirmed or epidemiologically linked case, the patient’s temperature does not need to reach ≥101°F (38.3°C) and the rash does not need to last ≥3 days.
Treatment is supportive. The WHO recommends vitamin A for all children with acute measles, regardless of their country of residence, to reduce the risk for complications. Administer vitamin A as follows: for infants <6 months old, give 50,000 IU, once a day for 2 days; for infants 6 months old and older, but younger than 12 months, give 100,000 IU once a day for 2 days; for children ≥12 months old give 200,000 IU once a day for 2 days. For children with clinical signs and symptoms of vitamin A deficiency, administer an additional (i.e., a third) age-specific dose of vitamin A 2–4 weeks following the first round of dosing.
Measles has been preventable through vaccination since a vaccine was licensed in 1963. People who do not have evidence of measles immunity should be considered at risk for measles, particularly during international travel. Acceptable presumptive evidence of immunity to measles includes birth before 1957; laboratory confirmation of disease; laboratory evidence of immunity; or written documentation of age-appropriate vaccination with a licensed, live attenuated measles-containing vaccine 1 , namely, MMR or measles-mumps-rubella-varicella (MMRV). For infants 6 months old and older, but younger than 12 months, this includes documented administration of 1 dose of MMR; for people aged ≥12 months, documentation should include 2 doses of MMR or MMRV (the first dose administered at age ≥12 months and the second dose administered no earlier than 28 days after the first dose). Verbal or self-reported history of vaccination is not considered valid presumptive evidence of immunity.
1 From 1963–1967, a formalin-inactivated measles vaccine was available in the United States and was administered to ≈600,000–900,000 people. It was discontinued when it became apparent that the immunity it produced was short-lived. Consider people who received this vaccine unvaccinated.
Vaccination
Measles vaccine contains live, attenuated measles virus, which in the United States is available only in combination formulations (e.g., MMR and MMRV vaccines). MMRV vaccine is licensed for children aged 12 months–12 years and can be used in place of MMR vaccine if vaccination for measles, mumps, rubella, and varicella is needed.
International travelers, including people traveling to high-income countries, who do not have presumptive evidence of measles immunity and who have no contraindications to MMR or MMRV, should receive MMR or MMRV before travel per the following schedule.
Infants (6 months old and older, but younger than 12 months): 1 MMR dose. Infants vaccinated before age 12 months must be revaccinated on or after the first birthday with 2 doses of MMR or MMRV separated by ≥28 days. MMRV is not licensed for children aged <12 months.
Children (aged ≥12 months): 2 doses of MMR or MMRV separated by ≥28 days.
Adults born in or after 1957: 2 doses of MMR separated by ≥28 days.
One dose of MMR is ≈85% effective when administered at age 9 months; MMR and MMRV are 93% effective when administered at age ≥1 year. Vaccine effectiveness of 2 doses is 97%.
Adverse Reactions
In rare circumstances, MMR vaccination has been associated with anaphylaxis (≈2–14 occurrences per million doses administered); febrile seizures (≈1 occurrence per 3,000–4,000 doses administered, but overall, the rate of febrile seizures after measles-containing vaccine is much lower than the rate with measles disease); thrombocytopenia (≈1 occurrence per 40,000 doses during the 6 weeks after immunization); or joint symptoms (arthralgia develops among ≈25% of nonimmune postpubertal females from the rubella component of the MMR vaccination, and ≈10% have acute arthritis-like signs and symptoms that generally persist for 1–21 days and rarely recur; chronic joint symptoms are rare, if they occur at all). No evidence supports a causal link between MMR vaccination and autism, type 1 diabetes mellitus, or inflammatory bowel disease.
Contraindications
People who experienced a severe allergic reaction (difficulty breathing, hives, hypotension, shock, swelling of the mouth or throat) following a prior dose of MMR or MMRV vaccine, or who had an anaphylactic reaction to topically or systemically administered neomycin, should not be vaccinated or revaccinated. People who are allergic to eggs can receive MMR or MMRV vaccine without prior routine skin testing or the use of special protocols.
Immunosuppression
Enhanced replication of live vaccine viruses can occur in people who have immune deficiency disorders. Death related to vaccine-associated measles virus infection has been reported among severely immunocompromised people; thus, severely immunosuppressed people should not be vaccinated with MMR or MMRV vaccine. For a thorough discussion of recommendations for immunocompromised travelers, see Sec. 3, Ch. 1, Immunocompromised Travelers .
MMR vaccination is recommended for all people with HIV infection aged ≥12 months who do not have evidence of measles, mumps, and rubella immunity, and who do not have evidence of severe immunosuppression. The assessment of severe immunosuppression can be based on CD4 values (count or percentage); absence of severe immunosuppression is defined as CD4 ≥15% for ≥6 months for children aged ≤5 years, or CD4 ≥15% and CD4 count ≥200 cells/mL for ≥6 months for people aged >5 years.
People with leukemia in remission and off chemotherapy, who were not immune to measles when diagnosed with leukemia, may receive MMR vaccine. At least 3 months should elapse after termination of chemotherapy before administering the first dose of vaccine.
Steroids & Other Immunosuppressive Therapies
Avoid vaccinating people who have received high-dose corticosteroid therapy (in general, considered to be ≥20 mg or 2 mg/kg body weight of prednisone, or its equivalent, daily for ≥14 days) with MMR or MMRV for ≥1 month after cessation of steroid therapy. Corticosteroid therapy usually is not a contraindication when administration is short-term (<14 days) or a low to moderate dose (<20 mg of prednisone or equivalent per day).
In general, withhold MMR or MMRV vaccine for ≥3 months after cessation of other immunosuppressive therapies and remission of the underlying disease. See Sec. 3, Ch. 1, Immunocompromised Travelers , for more details.
MMR vaccines should not be administered to pregnant people or people attempting to become pregnant. Because of the theoretical risk to the fetus, people should be counseled to avoid becoming pregnant for 28 days after receiving a live-virus (e.g., MMR) vaccine.
Precautions
Personal or family history of seizures of any etiology.
Compared with administration of separate MMR and varicella vaccines at the same visit, use of MMRV vaccine is associated with a higher risk for fever and febrile seizures 5–12 days after the first dose among children aged 12–23 months. Approximately 1 additional febrile seizure occurs for every 2,300–2,600 MMRV vaccine doses administered. Use of separate MMR and varicella vaccines avoids this increased risk for fever and febrile seizures.
Thrombocytopenia
The benefits of primary immunization are usually greater than the potential risks for vaccine- associated thrombocytopenia. Avoid giving subsequent doses of MMR or MMRV vaccine, however, if an episode of thrombocytopenia occurred ≤6 weeks after a previous dose of vaccine.
Postexposure Prophylaxis
Measles-containing vaccine or immune globulin (IG) can be effective as postexposure prophylaxis. MMR or MMRV administered ≤72 hours after initial exposure to measles virus might provide some protection. If the exposure does not result in infection, the vaccine should induce protection against subsequent measles virus infection.
When administered ≤6 days of exposure, IG can be used to confer temporary immunity in a susceptible person. If the exposure does not result in modified or typical measles, vaccination with MMR or MMRV is still necessary to provide long-lasting protection. Six months after receiving intramuscularly administered IG, or 8 months after receiving intravenously administered IG, administer MMR or MMRV vaccine, provided the patient is aged ≥12 months and the vaccine is not otherwise contraindicated.
CDC website: Measles
The following authors contributed to the previous version of this chapter: Paul A. Gastañaduy, James L. Goodson
Bibliography
Centers for Disease Control and Prevention. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2013;62(RR-04):1–34.
Gastañaduy P, Redd S, Clemmons N, Lee AD, Hickman CJ, Rota PA, et al. Measles. In: Roush SW, Baldy LM, Kirkconnell Hall MA, editors. Manual for the surveillance of vaccine-preventable diseases. Atlanta: Centers for Disease Control and Prevention; 2019. Available from: www.cdc.gov/vaccines/pubs/surv-manual/chpt07-measles.html .
Hyle EP, Fields NF, Fiebelkorn AP, Taylor Walker A, Gastañaduy P, Rao SR, et al. The clinical impact and cost-effectiveness of measles-mumps-rubella vaccination to prevent measles importations among US international travelers. Clin Infect Dis. 2019;69(2):306–15.
Hyle EP, Rao SR, Bangs AC, Gastañaduy P, Parker Fiebelkorn A, Hagmann SHF, et al. Clinical practices for measles-mumps-rubella vaccination among US pediatric international travelers. JAMA Pediatr. 2020;174(2):e194515.
Hyle EP, Rao SR, Jentes ES, Parker Fiebelkorn A, Hagmann SHF, Taylor Walker A, et al. Missed opportunities for measles, mumps, rubella vaccination among departing U.S. adult travelers receiving pretravel health consultations. Ann Intern Med. 2017;167(2):77–84.
Lee AD, Clemmons NS, Patel M, Gastañaduy PA. International importations of measles virus into the United States during the post-elimination era, 2001–2016. J Infect Dis. 2019;219(10):1616–23.
National Notifiable Diseases Surveillance System. Measles (rubeola): 2013 case definition. Atlanta: CDC; 2013. Available from: https://ndc.services.cdc.gov/conditions/measles/ .
Patel MK, Goodson JL, Alexander JP Jr., Kretsinger K, Sodha SV, Steulet C, et al. Progress toward regional measles elimination—Worldwide, 2000–2019. MMWR Morb Mortal Wkly Rep. 2020;69(45):1700–5.
Pike J, Leidner AJ, Gastañaduy PA. A review of measles outbreak cost estimates from the US in the post-elimination era (2004–2017): Estimates by perspective and cost type. Clin Infect Dis. 2020;1(6):1568–76.
World Health Organization. Measles vaccines: WHO position paper—April 2017. Wkly Epidemiol Rec. 2017;92(17):205–27.
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Weird But True
- Sex & Relationships
- Viral Trends
- Human Interest
- Fashion & Beauty
- Food & Drink
- Health Care
- Men’s Health
- Women’s Health
- Mental Health
- Health & Wellness Products
- Personal Care Products
trending now in Lifestyle

Bride calls out wedding guest's 'ridiculous' RSVP: 'Nothing I can...

Billionaire's wife stinks of entitlement as messages show her...

I'm 65 and sexier than ever— people mistake me and my...

Inside Costa Rica's 'cave of death' which kills all that enters

How to find out if a woman is a psychopath — there's one...

I kicked a bridesmaid out of my wedding party for this...

These are the hilarious finalists of the Comedy Pet Photo Awards...

Dear Abby: My dad told me I'm the reason my parents are getting...
I donated my kidney to my hero of a mom — now she can travel the world.
- View Author Archive
- Follow on Twitter
- Get author RSS feed
Thanks for contacting us. We've received your submission.

A daughter who considers her mother to be her “hero” came to her mother’s rescue by giving her mother her kidney.
“I was just one month short of retirement when I got sick,” 64-year-old New Yorker Theresa Bullicer told The Post.
Bullicer, a mom of three and a grandmother of nine, worked as a nurse for 42 years before her planned retirement in November 2022. However, just weeks shy of her farewell from St. Barnabas Hospital in The Bronx, she was diagnosed with end-stage renal disease, hospitalized and placed on emergency dialysis, something she would need to have three times a week.

“I asked the doctor, ‘Do I have to be on dialysis for the rest of my life?’ He said, ‘Yes, unless you get a kidney,’” Bullicer recalled.
Matching with a kidney donor may have taken five to 10 years. Instead, her daughter donated a kidney nine months ago “without hesitation,” Bullicer said.
“Faith is very important to both of us, so I was just crying out to God, ‘How can I help my mom?’” Bullicer’s daughter Jo Marie Palazzo, a 43-year-old nurse at NewYork-Presbyterian/Columbia, told The Post. Palazzo has four children, one of whom is also a nurse.
“ I felt my husband was encouraging me and was supportive of me doing it. And so I was like, ‘Let’s go find out if I’m a match,’ because, if I can help my mom and help her … it’s like a gift of life, right?” she added.
The process
In order to give a kidney, potential donors must be tested to see if they are the right match for the recipient as well as whether they are healthy enough to give.
“Generally the main criteria is blood type matching,” Dr. Dustin Carpenter , an organ transplant surgeon at NewYork-Presbyterian/Weill Cornell who performed Bullicer’s surgery, told The Post.
He said that the hospital is sometimes able to transplant organs from a person with a different blood type but it requires a “more complicated immunosuppression regimen,” so it’s ideal if the blood type is the same. Once found to be a blood type match, donors undergo extensive health testing.
“We make sure that if they donate, it’s under the safest circumstances possible and that they have no untoward risk,” Carpenter explained.

“We make sure that their renal function is basically perfect, so that they donate safely. You know, people can live a long and healthy life with only one kidney and not even really have any changes to their lifestyle or to their length of life,” he added.
Carpenter said that the surgical procedure lasts three to four hours.
“We have to make three new connections usually,” he said of the surgery to add a kidney.
“One is to the artery, which is what brings blood to the kidney. One is to the vein, which brings blood from the kidney back to the rest of the body. And then, a final connection is between what’s called the ureter and the bladder. That’s what allows the person to urinate again and to clear the urine that gets built up from filtering the blood,” he explained.
He said that people are generally hospitalized for around four days following the transplant and that they are fully recovered after around three months.
Bullicer said after her surgery, her tests came back normal and she was already feeling much healthier.
“I walked around the first day of surgery and I was discharged after the third day … I have doctor visits, but I feel so much better,” she said.
Mom is her hero
Palazzo said that seeing her mom healed after donating her kidney to her was “one of the most rewarding experiences of my life.”
Prior to her mom getting sick, “we were already in the process of planning her retirement party because we were so happy that she worked for so hard for so long that she was finally going to be able to, you know, travel the world and enjoy her life,” Palazzo explained.
“She immigrated here from the Philippines by herself before my dad. My brother and I were left in the Philippines so she could build a life here and prepare for us to come,” Palazzo explained.

“While she was doing that, she sent all her siblings to nursing school in the Philippines so that they could have a better life in America as well,” she continued.
Her mom worked multiple jobs so that Palazzo and her two siblings could all go to private school, college and nursing school. Today, there are 15 nurses in their family.
Palazzo said it crushed her when she found out “my mom, my hero, isn’t going to be able to enjoy her retirement like she had planned.”
Traveling the world
After retiring, Bullicer planned to travel the world and go island hopping in the Philippines with her college classmates.
Her kidney disease put a damper on her plans — but luckily it was only temporary. She and her daughter already had the opportunity to explore the world together in February.
“We’ve been traveling together. We just came back from the Philippines [where we were] for a month,” Bullicer said. She plans to go back in June — and her travel plans don’t end there.
Palazzo said that when she was growing up she and her mother used to watch and listen to “The Sound of Music” together.
“So we are planning to do a ‘Sound of Music’ tour in Austria,” she said.

Live donation benefits
“We are the busiest living-donor program in New York,” Carpenter said of NewYork-Presbyterian/Weill Cornell.
A major reason he advocates for living donation, meaning the organ comes from a living family member, friend or stranger as opposed to a deceased person, is that “the average lifespan for a living donor transplant is twice that of a deceased donor.”
Another plus is “it shortens that period of time that people have to wait and oftentimes, you can get someone transplanted before they’re on dialysis,” he said.
Donating an organ to someone in need can also be a bonding experience — something Bullicer and Palazzo experienced firsthand.
“ I think this experience has definitely brought us closer … We’re just so thankful,” Palazzo said.
How to become a donor
There are over 89,000 people on the waiting list for kidney transplants and “dozens of people die every day waiting for a transplant, because there’s always a continued organ shortage.”
He said he would encourage people to be organ donors due to the shortage and because it’s a “very safe operation.”
“People can live a normal life, you know, after donating, with basically no restrictions,” Carpenter said. “We’ve had people that have run marathons within six months of donating. We’ve had people climb Mount Kilimanjaro.”
Palazzo also urged others to consider saving a life.
“If you feel that tug in your heart … go for it,” she said. “You are giving somebody a chance to live a full life again.”
Share this article:

Advertisement

Go. Explore.
(480) 435-2774
Vaccinations
We provide a full range of routine and travel vaccinations.
Schedule an Appointment
- Schedule an appointment in our travel clinic and a TravelBug Health consultant will ensure that you have the proper vaccines to protect you from travel related illnesses.
- First, we ensure your routine vaccinations (such as MMR and polio) are up-to-date. These vaccines protect you from diseases that are still common in many parts of the world.
- You may need additional travel vaccines, such as Hepatitis A and B or typhoid depending on your destination or activities.
- We are a certified Yellow Fever Vaccination provider.
- TravelBug Health is not currently administering the COVID-19 vaccine.
* indicates that a series of multiple shots may be necessary to complete immunity.

5 key benefits of taking turmeric supplements
From easing joints to supporting brain health

Turmeric contains a powerful antioxidant known as curcumin, which studies have indicated offers myriad benefits in many different areas. It’s little wonder, then, that turmeric supplements have become a daily must-have for those in the know when it comes to wellness – but not all supplements are created equal.
It’s important to look for a bioavailable (absorbable) formulation that’s backed up by scientific evidence. FutureYou Cambridge’s Turmeric+ contains the most scientifically studied curcumin on the market, with over 42 human studies, and is proven to be 30 times more absorbable than ordinary turmeric.
Considering adding turmeric supplements to your own daily regime? We’ve rounded up the research to help inform your choice.
1. Reducing chronic inflammation
One in five British people say they suffer from chronic inflammation* – this is pain and inflammation that can last for months, or even years. Studies have indicated that increasing your intake of antioxidants from food, or with the help of food supplements such as turmeric, can make a significant difference. And while chronic inflammation is often associated with age-related disorders, it can occur at any time of life, so it’s never too early to take steps to protect yourself.
2. Supporting brain health
It’s no secret that as we age, the neurons in our brains stop firing as effectively, which can lead to memory loss and changes in mood, among other symptoms. Part of this is driven by the accumulation of oxidative stress in the brain. A diet rich in antioxidant foods, such as fruits, vegetables and spices like turmeric, can help our brain cells to cope with this stress. Research published in the Frontiers journal concluded that turmeric can be a beneficial ally in delaying neurological disorders.

3. Warding off winter bugs
Researchers have discovered that turmeric may also be helpful for those who are prone to suffering from cold and flu symptoms (aka: all of us during those long winter months). And once again, it’s all thanks to the curcumin that naturally occurs in turmeric, because it has the potential to reduce inflammation linked to excessive coughing and sneezing, while also increasing antioxidant capacity to boost your immunity. To further bolster your immune system and ability to ward off sniffles, look for a turmeric supplement that includes vitamin D – like FutureYou’s Turmeric+ supplement – which is known for its flu-fighting properties. A government study found that one in six of us in the UK is lacking in vitamin D, and this deficiency has been linked to increased susceptibility to infection.
4. Aiding digestion
As we get older, our digestion may benefit from a little nudge every now and again, which is why we couldn’t not mention turmeric’s digestive-aiding properties. A 2019 study found turmeric may help with gut microbial communities because it has a prebiotic effect that helps to promote the growth of healthy bacteria in your gut (though further, larger studies are needed on the subject).
5. Boosting skin
There’s a growing body of research suggesting that turmeric can help with easing skin disorders, such as psoriasis , and even acne – though scientists are yet to fully ascertain how this works. What is clear, though, is that curcumin boosts the body’s antioxidants, and so taking a turmeric supplement can support your skin’s natural glow. To maximise this benefit even further, Turmeric+ combines turmeric with vitamin C, an ingredient loved by dermatologists for its science-backed anti-ageing properties (think: improving appearance of wrinkles and dark spots, as well as preventing sun damage).
FutureYou Cambridge is offering Good Housekeeping readers a free trial of its Turmeric+ supplement (£1.50 postage and packaging applies).
Terms and conditions apply – see futureyouhealth.com/offers/tuf348 for further details
* Survey, conducted by Atomik Research among 2,001 adults aged 18+ in the UK
@media(max-width: 64rem){.css-o9j0dn:before{margin-bottom:0.5rem;margin-right:0.625rem;color:#ffffff;width:1.25rem;bottom:-0.2rem;height:1.25rem;content:'_';display:inline-block;position:relative;line-height:1;background-repeat:no-repeat;}.loaded .css-o9j0dn:before{background-image:url(/_assets/design-tokens/goodhousekeeping/static/images/Clover.5c7a1a0.svg);}}@media(min-width: 48rem){.loaded .css-o9j0dn:before{background-image:url(/_assets/design-tokens/goodhousekeeping/static/images/Clover.5c7a1a0.svg);}} Partnerships

4 ways to achieve a luxury beach house feel

4 relaxing Warner Hotel breaks to book in 2024

Gok Wan's new series celebrates midlife

The power of a midlife career pivot

Electric cars are great for family life

5 unexpected ways to get your culture fix at sea

Join GH for an exclusive event at Heythrop Park

How this Australian collagen supplement delivers

4 ways to update your house for the future

9 coffee-based recipes to try this Christmas

5 reasons to use the Philips coffee machine
Science | Have you met Chicago’s Bug Girl? Janelle…
Share this:.
- Click to share on Facebook (Opens in new window)
- Click to share on X (Opens in new window)
- Click to print (Opens in new window)
- Click to email a link to a friend (Opens in new window)
- Restaurants, Food and Drink
- Entertainment
- Immigration
- Sports Betting
Science | Have you met Chicago’s Bug Girl? Janelle Iaccino wants to enlighten the city on the greatness of the creepy, crawly things

Iaccino is marketing director of Rose Pest Solutions, a structural pest control company that ensures nature and the environment stay outside of homes and businesses. The family owned, Northfield-based business has been in operation for hundreds of years and has 13 locations in Illinois and Indiana.
As a spokeswoman for the company in Chicago, Iaccino leads a team of women called The Bug Girls , who use their expertise and knowledge about bugs and rats to inform and educate the next generation of researchers and scientists.
“I’m usually the Bug Girl, but I also am called the Rat Lady from time to time, which is not as endearing,” said Iaccino, a 19-year employee of the company. “I’ve really made it a mission to bring people into that world.”
On a recent March afternoon, she entered the Peggy Notebaert Nature Museum carrying a bag full of Madagascar hissing cockroaches — complete with a pineapple-shaped house, like in the show “Spongebob Squarepants” — along with giant African millipedes that are like worms with shells, and a plush cicada to show how it emerges colorful after it sheds its brown shell.
She tells people about an impending bedbug infestation that is looming as more people are now traveling and about a new species of mosquito that bites in the daytime. She informs folks about what subterranean termites look like and how they should not be confused with maggots.
The native Chicagoan also wears a colorful pair of cicada earrings. Iaccino is also an artist who paints; a musician who plays multiple instruments, including jazz flute; a producer; a proprietor of her own apothecary shop; and a nature lover.
Her blog encourages folks to “embrace your weird.” As a 2023 National Pest Management Association award winner for Women in Pest Management and a 2018 Drummer Silty Clay Loam Education winner, an award given to stellar volunteers at the Peggy Notebaert Nature Museum, Iaccino does that daily.
When she’s not helping inform people about public health and pests, she’s on a mission to encourage young girls to pursue careers in science.
“I’m bopping all over Chicagoland, up to Milwaukee, down through Indianapolis and Louisville, Kentucky (with Franklin Pest Solutions),” she said. “I work a lot with the Girl Scouts. I’ve developed some STEM programs with them over the last couple of years. I was a former Girl Scout and as a kid, what opened my mind to things that I didn’t learn in school, that my parents didn’t teach me? It was Scouts. That’s how I became so interested in visual arts. We went on hikes, nature adventures all the time.”
Iaccino coordinates at least two Spark Day programs with Girl Scouts of Greater Chicago and Northwest Indiana per year, events that offer the scouts hands-on activities and exposure to industry professionals to gain skills and knowledge about career spaces they didn’t know about. The next one will be held June 8. She said female professionals will be on hand from different avenues of environmental science, such as wildlife rehabilitators, entomologists, public health experts and park rangers.

“We set up stations and the girls can be hands-on, face-to-face with these female leaders, which is so empowering for them to see,” Iaccino said. “In these industries, it’s so male dominant. That was what forced me to start reaching out to every Girl Scout troop leader I knew. It’s so rewarding when 50 girls come away from that experience, and they remember so many details. … You’re excited to see what they’ll do when they’re older.”
Iaccino’s varied interests also include taxidermy. Because she works with a team that controls the rat population, she often brings the deceased specimens to the museum to mount.
“I’ve prepared 53 specimens for the collection over the years,” Iaccino said. “The Peggy Notebaert Nature Museum is one of my personal favorites. I learned taxidermy here. It was cool to be able to do something on a different level here – not as a spectator but as an active participant in preserving natural history. It’s scientific, sure, but it’s also an art form.”
Iaccino works closely with Emily Graslie , an artist, science communicator and writer, video host, educational media producer, and creator behind the YouTube channel “ The Brain Scoop ,” which shares behind-the-scenes work of natural history museums with the world through informative videos.
“I’ve been making YouTube educational videos for 10 years,” Graslie said. “I woke up one day and was like, I want to know more about urban wildlife and what is the nastiest urban wildlife you can find? It’s rats!
“One thing that I like to try and do is help normalize things,” Graslie said. “Help other people look around at the world around us and realize that nature’s everywhere, not just in parks. Then I came to Peggy Notebaert and was like: Do you guys do anything with this? And they all said ‘Rats? You need to speak with Janelle. ‘”
When Iaccino started volunteering at the nature museum, administration told her that because they had lost a lot of their specimens to the Chicago fire, they didn’t have urban rats from Chicago. So she stepped in to help rebuild the collection . Iaccino calls it a perfect match.

“I just started collecting them and bringing them in and it wasn’t just me working on them, it was other volunteers too. And now we’ve got the collection going,” she said.
With over 600,000 subscribers, Graslie is all about education and curiosity. While she was capturing footage of Iaccino at the museum, Graslie shared stories about the extinct passenger pigeon species in Illinois, how people who study neotropical fish do biological inventories of wildlife for damming projects, and how house sparrows had adapted to less sound pollution from cars during the pandemic lockdown. All of the above was documented over the years.
“I’m just dipping my toe into the rat business in Chicago, but I wouldn’t be here without Janelle, she’s helping me spread the appreciation for these that I wouldn’t have had without knowing her,” Graslie said.
Iaccino said you’d be surprised how many “weirdos” out there now want to know about this kind of information. “I used to post something to Instagram and people would be like, ‘Why are you posting this? No one wants to see this.’ I was like, ‘Hit the unfollow button dude; this is me,’” she said. “But now everyone’s like, ‘How come you haven’t posted pics of this lately?’ There’s a lot of people who want to know now.”
She said taxidermy can get pretty gnarly. But for her, it’s all about teaching people enough that they’re not afraid. She believes education is the best defense against any kind of fear and that’s what she’s doing when she goes to schools and museums.
“I’m opening their minds because it’s a fear factor,” she said. “Everybody’s got their own threshold for what they are afraid of, and what they’ll tolerate. And being in the pest control industry, we know that better than anybody.”
Knowing that Chicago has been the rattiest city in the nation for the past nine years , she’s happy that the city’s budget for rodent abatement is robust. It’s an ongoing battle because rodents are resilient. She always tells Chicago residents to be diligent about reporting seeing rats around the city by calling 311. Iaccino says with the number of alleys in the area, there are a lot more places for them to hide and a lot more dumpsters to go through.
Iaccino’s career path started when she received a tarantula as a gift from a friend when she was in high school. Named Xanadu, after Olivia Newton-John’s 1980 film, the pet Iaccino owned for six years helped her face her fears.

“I was able to be not afraid to hold it and inch my way toward that,” she recalled. “And it’s just been a lifestyle now for many years. I’m the cool auntie who always has a trunk full of weird things.”
She landed her Rose Pest Solutions job in a similar way. What was supposed to be a part-time summer job answering phones and doing dispatch for the service team led to her wearing all the hats in the location. Six months later, she was in the field going on ride-alongs and learning every aspect of the job so that she could talk to customers better.
“That was the name of the game, listening to people’s stories. I’m curious by nature, so it helped me understand how people feel about different things. And then I could research how to comfort them and find the solution,” she said.
“Preventive tips are all we focus on because we want people to start thinking proactively. Methods that were working two or three years ago are not working anymore,” she said. “This is why we need more entomology professionals, why we need more data research people. Being in the pest control business … it’s all about balance. Humans and nature will always have to be in harmony somehow. It’s about knowing exactly that right balance so you’re not disturbing the ecosystem. … We prescribe the right treatment so that we’re not harming the earth or people, but taking care of the problem.”
More in Science

Travel | Itching to catch the next eclipse? Get your passport ready

World News | Turkey says it backs outgoing Dutch prime minister Rutte’s candidacy for NATO chief

Environment | 86% of Great Lakes litter is plastic, a 20-year study shows. And the plastic is ‘just getting smaller and smaller.’

Health | Bird flu is spreading to more farm animals. Are milk and eggs safe?
Trending nationally.
- Animation showing planned Key Bridge explosive demolition unveiled
- New COVID ‘FLiRT’ variants are spreading nationwide. Chicago health experts urge up to date vaccination.
- Stormy Daniels unfavorably compares Trump to ‘real men’ after hush-money trial testimony
- An entire California town is for sale — again. This time for $6.6M
- California adopts one of nation’s highest fixed-utility fees
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- Recalls, Market Withdrawals, & Safety Alerts
Hormel Foods Sales, LLC Recalls a Limited Number of Planters® Honey Roasted Peanuts 4 Oz. and Planters® Deluxe Lightly Salted Mixed Nuts 8.75 Oz. Because of Possible Health Risk
COMPANY ANNOUNCEMENT
When a company announces a recall, market withdrawal, or safety alert, the FDA posts the company's announcement as a public service. FDA does not endorse either the product or the company.
Company Announcement
AUSTIN, Minn. (May 3, 2024) – Hormel Foods Sales, LLC is voluntarily recalling a limited number of two PLANTERS® products that were produced at one of its facilities in April. This recall only impacts two retailers in five states. These products are being recalled because they have the potential to be contaminated with Listeria monocytogenes .
Listeria monocytogenes is an organism that can cause serious and sometimes fatal infections in young children, frail or elderly people, and others with weakened immune systems. Healthy individuals may suffer only short-term symptoms such as high fever, severe headache, stiffness, nausea, abdominal pain, and diarrhea. Listeria infection can cause miscarriages and stillbirths among pregnant women.
The products were shipped to Publix distribution warehouses in Florida, Georgia, Alabama and North Carolina and to Dollar Tree distribution warehouses in South Carolina and Georgia.
The recalled product is limited to 4 oz. packages of PLANTERS® Honey Roasted Peanuts and 8.75 oz. cans of PLANTERS® Deluxe Lightly Salted Mixed Nuts. The “Best if Used By Date” is located on the bottom of the Deluxe Lightly Salted Mixed Nuts can and the UPC code is located on the side of the can.
No other sizes, varieties, or other packaging configurations of PLANTERS® brand products are included in this recall.
There have been no reports of illness related to this recall to date, and all retailers that received the affected product have been properly notified. This recall is being initiated with the knowledge of the US Food and Drug Administration.
If a consumer has this product, they can discard the product or return it to the store where purchased for an exchange or full refund. If consumers have questions, they may contact Hormel Foods Customer Relations via email here , via chat at https://www.planters.com/ or at 1-800-523-4635, Monday-Friday, 8 a.m. – 11 a.m. and 2 p.m. – 4 p.m. Central Time, excluding holidays.
Our commitment to food safety remains our utmost priority. A full investigation is currently under way to determine the potential source of the contamination.
Company Contact Information
Product photos.
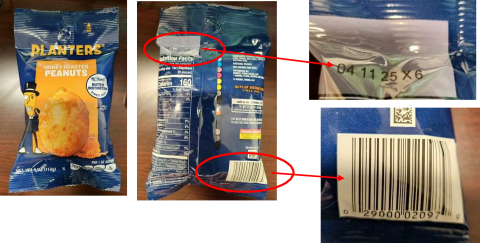
'Breaking up families': CDC announces strict rules for traveling to the US with your dog

The Centers for Disease Control and Prevention announced new restrictions Wednesday on dogs traveling to the U.S., which some say will make it harder for families returning to the country with their pets or adopting pets internationally.
The new regulation, which goes into effect August 1, bans all dogs under six months from entering the U.S. Dogs over six months must show proof they have not been in a country identified as high-risk for rabies. Without proof, the dog faces potential quarantine. Dogs must also be microchipped.
The tighter restrictions are meant "to protect the health and safety of people and animals by making sure any dog arriving in the United States is healthy and doesn’t present a risk to our communities," the CDC said in a press release Wednesday.
The U.S. eliminated rabies in 2007, and the new rules are meant to prevent the re-introduction of the viral disease, which is transmitted through biting. The agency has identified 131 countries as high risk for rabies as of Aug. 2023.
The CDC also said it has seen "recent challenges with international dog importations," such as fraudulent documents or dogs kept in unsafe conditions.
Traveling with a pet can be difficult. Download these helpful apps
However, some say the restrictions will negatively impact families and those wanting to rescue pets overseas from legitimate organizations because it can be “especially challenging” to provide proof of a dog’s whereabouts," according to the Humane Society Legislative Fund in a press release on Wednesday. “Far fewer dogs will be able to find loving homes in the U.S.," the release said.
“The CDC’s job is to maintain public health, but these new requirements may needlessly delay Americans – including government personnel and military families – from returning to the United States with their pets, creating great anguish and breaking up families in the process,” said Tracie Letterman, vice president of federal affairs at Humane Society Legislative Fund, in a statement in the release.
Airlines may also struggle to implement the new restrictions.
“Airlines will be left to their own discretion to enforce these rules, and if they err, it’s up to the airline to export the dog back to the dog’s country of origin,” the Humane Society Legislative Fund said. “To avoid confusion or difficulties, some airlines may opt out of allowing customers to travel into the U.S. with dogs.”
Kathleen Wong is a travel reporter for USA TODAY based in Hawaii. You can reach her at [email protected] .

IMAGES
VIDEO
COMMENTS
Bugs, including mosquitoes, ticks, fleas, and flies, can spread diseases such as malaria, yellow fever, Zika, dengue, chikungunya, and Lyme. While some cases are mild, these diseases can be severe and have lasting consequences. Some diseases caused by bug bites can be prevented with vaccines or medication, like yellow fever and malaria; however ...
Traveler's diarrhea is a digestive tract disorder that commonly causes loose stools and stomach cramps. It's caused by eating contaminated food or drinking contaminated water. Fortunately, traveler's diarrhea usually isn't serious in most people — it's just unpleasant. When you visit a place where the climate or sanitary practices are ...
Bugs can carry pathogens such as bacteria, nematodes, protozoa, and viruses which transmit tricky-to-diagnose diseases to humans. ... (CDC) maps, which provide travel information about illnesses ...
CDC's Travelers' Health Web site contains detailed advice for health care providers. Health departments, the travel industry, multinational corporations, missionary and volunteer organizations, and travelers can also use this information to help make international travel as healthy and safe as possible. Healthy Swimming. Healthy Water.
There are different types of travel-associated infections that cause fever, along with other symptoms to include diarrhea, vomiting, rashes, and muscle aches. The most common of these include malaria, dengue, typhoid fever, and chikungunya. Malaria. Malaria is a parasitic disease spread by mosquitoes in tropical and subtropical climates.
Travel Bug has been professional, prompt, and helpful each time I've had to internationally travel during the pandemic. ... This was my first visit to Travel Bug Health and I was very satisfied from the beginning of reception to the end of billing. They were very inviting and the wait was only 5 minutes before... Ilea S. Easy, Professional and ...
Traveler's diarrhea is the most common travel-related illness. It affects between 30% and 70% of travelers, depending on the destination and the season. It's especially common in hot and/or humid climates, where bacteria breed more easily. Most of Asia, the Middle East, Africa, Mexico and Central and South America have this type of climate ...
Your travel activities, including swimming, hiking, etc. The timeframe of your vacation. Where you stayed, such as hotels, family or friends' homes, hostels, or tents. What you ate and drank. Animals you had close contact with or touched. If you have any injuries, scratches, or bug bites. Health care or medications you received during your trip.
Find out about travel vaccinations, dealing with other travel illnesses, travel insurance, and staying safe. Before you pack your suitcase to head off on your next voyage, don't get stuck with any unwanted travel bugs. Find out about travel vaccinations, dealing with other travel illnesses, travel insurance, and staying safe. ...
Treatment. Travelers' diarrhea (TD) is the most predictable travel-related illness. Attack rates range from 30%-70% of travelers during a 2-week period, depending on the destination and season of travel. Traditionally, TD was thought to be prevented by following simple dietary recommendations (e.g., "boil it, cook it, peel it, or forget ...
Request an Appointment. 410-955-5000 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. Diarrhea is the term for bowel movements that are loose or watery. Traveler's diarrhea occurs within 10 days of travel to an area with poor public hygiene. It's the most common illness in travelers.
Clean your hands often. Use soap and water or an alcohol-based cleanser to help prevent infection. Do not stand or swim in fresh-water rivers, streams, or lakes that have sewage or animal feces in them. This can lead to infection. Swimming in chlorinated pools is safe most of the time.
Lifestyle and home remedies. If you do get traveler's diarrhea, avoid caffeine, alcohol and dairy products, which may worsen symptoms or increase fluid loss. But keep drinking fluids. Drink canned fruit juices, weak tea, clear soup, decaffeinated soda or sports drinks to replace lost fluids and minerals.
Vaccinations Required For Safe Travel To Bali. September 9, 2022. When searching for a vacation destination, many people look for warm and lush places; Bali certainly fits that criteria and more. Thanks to its stunning beaches, exquisite culture, and mouthwatering cuisine, Bali, Indonesia is consistently ranked as one of the world's choices ...
At TravelBug Health, we provide expert advice, personalized to your unique itinerary and we recommend only what you need for the best value. Whether you're going on an African safari or international business trip to India, preparation is paramount to a safe and successful trip. All travelers should be informed about the potential hazards of ...
Paris, France and the Spanish island of Tenerife ranked in 4th and 5th place with Travel Bug Index Scores of 19.4 and 19.3. Overall top European destinations for getting sick Rank
Inner Health Travel Bug contains 5 billion CFU of SB probiotics per capsule and is packaged in a convenient, shelf-stable bottle, making it travel-friendly. One bottle contains enough probiotics for 3 weeks travel, including the 5 days pre-travel dose, and is suitable for adults and children from age 3. Safe travels!
The Centers for Disease Control and Prevention has issued a travel advisory after some U.S. residents were diagnosed with suspected fungal meningitis infections following medical or surgical ...
Inner Health Travel Bug is a probiotic that reduces the risk of traveller's diarrhoea symptoms & relieves diarrhoea in adults, children & healthy infants. Inner Health Travel Bug • Reduces the risk of traveller's diarrhoea symptoms. • Relieves diarrhoea in adults & children. Made in Australia Vegetarian & Vegan Friendly Size: 20 Capsules
Brits travelling to Spain have been warned over a virus outbreak that is fatal in almost a third of cases. The warning was sparked after Crimean-Congo haemorrhagic fever was discovered in Spain, a ...
Doctors also need to ask patients about recent travel history — "I'm starting to ask that of just about every patient," she says — especially if the patient has symptoms that are not attributable to common ailments like the flu, COVID-19, or pneumonia. "Everybody needs to be more educated," about VBDs, Heaney says.
FILE - A traveler pulls his dog in a wheeled carrier at the Benito Juarez International Airport in Mexico City, Wednesday, Dec. 21, 2022. If you are bringing a dog into the U.S. — whether if you are returning from a trip overseas with Rover, visiting the U.S., or adopting a dog from abroad — you have to follow a set of new rules released by the Centers for Disease Control and Prevention on ...
A clinical case of measles illness is characterized by generalized maculopapular rash lasting ≥3 days; temperature ≥101°F (38.3°C); and cough, coryza, or conjunctivitis. A confirmed case is one with an acute febrile rash illness with laboratory confirmation or direct epidemiologic linkage to a laboratory-confirmed case.
The CDC says Lyme disease is the most prevalent disease transmitted through tick bites in the U.S. But even in high-risk regions, the chance of contracting Lyme disease from a tick bite is 1% to 3 ...
"I was just one month short of retirement when I got sick," 64-year-old New Yorker Theresa Bullicer told The Post. Bullicer, a mom of three and a grandmother of nine, worked as a nurse for 42 ...
Schedule an appointment in our travel clinic and a TravelBug Health consultant will ensure that you have the proper vaccines to protect you from travel related illnesses. First, we ensure your routine vaccinations (such as MMR and polio) are up-to-date. These vaccines protect you from diseases that are still common in many parts of the world.
3. Warding off winter bugs . Researchers have discovered that turmeric may also be helpful for those who are prone to suffering from cold and flu symptoms (aka: all of us during those long winter ...
Janelle Iaccino, aka The Bug Girl, who also does taxidermy, displays a Norway rat at the Peggy Notebaert Nature Museum on March 26, 2024. (E. Jason Wambsgans/Chicago Tribune)
Hormel Foods Sales, LLC is voluntarily recalling a limited number of two PLANTERS® products that were produced at one of its facilities in April. This recall only impacts two retailers in five ...
The U.S. eliminated rabies in 2007, and the new rules are meant to prevent the re-introduction of the viral disease, which is transmitted through biting. The agency has identified 131 countries as ...