

17.9 The Pancreas
Learning objectives.
By the end of this section, you will be able to:
Explain the role of the pancreatic endocrine cells in the regulation of blood glucose
- Describe the location and structure of the pancreas, and the morphology and function of the pancreatic islets
- Compare and contrast the function and regulation of insulin and glucagon
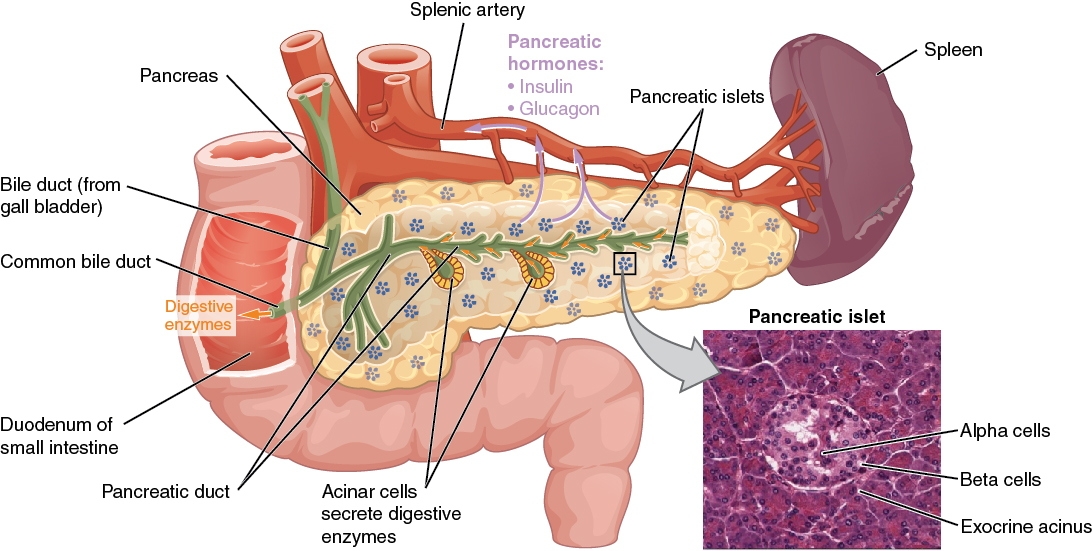
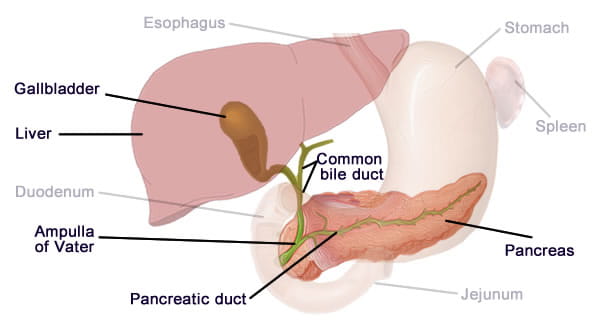
The pancreas is a long, slender organ, most of which is located posterior to the bottom half of the stomach ( Figure 17.9.1 ). Although it is primarily an exocrine gland, secreting a variety of digestive enzymes, the pancreas also has endocrine cells. Its pancreatic islets —clusters of cells formerly known as the islets of Langerhans—secrete the hormones glucagon, insulin, somatostatin, and pancreatic polypeptide (PP).
External Website

View the University of Michigan WebScope at http://141.214.65.171/Histology/Digestive%20System/Liver%20and%20Pancreas/188B_HISTO_40X.svs/view.apml to explore the tissue sample in greater detail.
Cells and Secretions of the Pancreatic Islets
The pancreatic islets each contain four varieties of cells:
- The alpha cell produces the hormone glucagon and makes up approximately 20 percent of each islet. Low blood glucose levels stimulate the release of glucagon.
- The beta cell produces the hormone insulin and makes up approximately 75 percent of each islet. Elevated blood glucose levels stimulate the release of insulin.
- The delta cell accounts for four percent of the islet cells and secretes the peptide hormone somatostatin. Recall that somatostatin is also released by the hypothalamus, stomach and intestines. An inhibiting hormone, pancreatic somatostatin inhibits the release of both glucagon and insulin.
- The pancreatic polypeptide cell (PP cell) accounts for about one percent of islet cells and secretes the pancreatic polypeptide hormone. It is thought to play a role in appetite, as well as in the regulation of pancreatic exocrine and endocrine secretions. Pancreatic polypeptide released following a meal may reduce further food consumption; however, it is also released in response to fasting.
Regulation of Blood Glucose Levels by Insulin and Glucagon
Glucose is utilized in cellular respiration as a fuel for cells of the body. The body derives glucose from the breakdown of the carbohydrate-containing foods and drinks we consume. Glucose not immediately taken up by cells for fuel can be stored by the liver and muscles as glycogen, or converted to triglycerides and stored in the adipose tissue. Hormones regulate both the storage and the utilization of glucose as required. Receptors located in the pancreas sense blood glucose levels, and subsequently the pancreatic cells secrete glucagon or insulin to maintain appropriate blood glucose.
Receptors in the pancreas can sense the decline in blood glucose levels, such as during periods of fasting or during prolonged labor or exercise ( Figure 17.9.2 ). In response, the alpha cells of the pancreas secrete the hormone glucagon , which has several effects:
- Glucagon stimulates the liver to convert its stores of glycogen back into glucose. This response is known as glycogenolysis. The glucose is then released into the circulation for use by cells throughout the body.
- Glucagon stimulates the liver to take up amino acids from the blood and convert them into glucose. This response is known as gluconeogenesis.
- Glucagon stimulates lipolysis, the breakdown of stored triglycerides into free fatty acids and glycerol. Some of the free glycerol released into the bloodstream travels to the liver, which converts the glycerol into glucose. This is also a form of gluconeogenesis.
Taken together, these actions increase blood glucose levels. The activity of glucagon is regulated through a negative feedback mechanism; rising blood glucose levels inhibit further glucagon production and secretion.
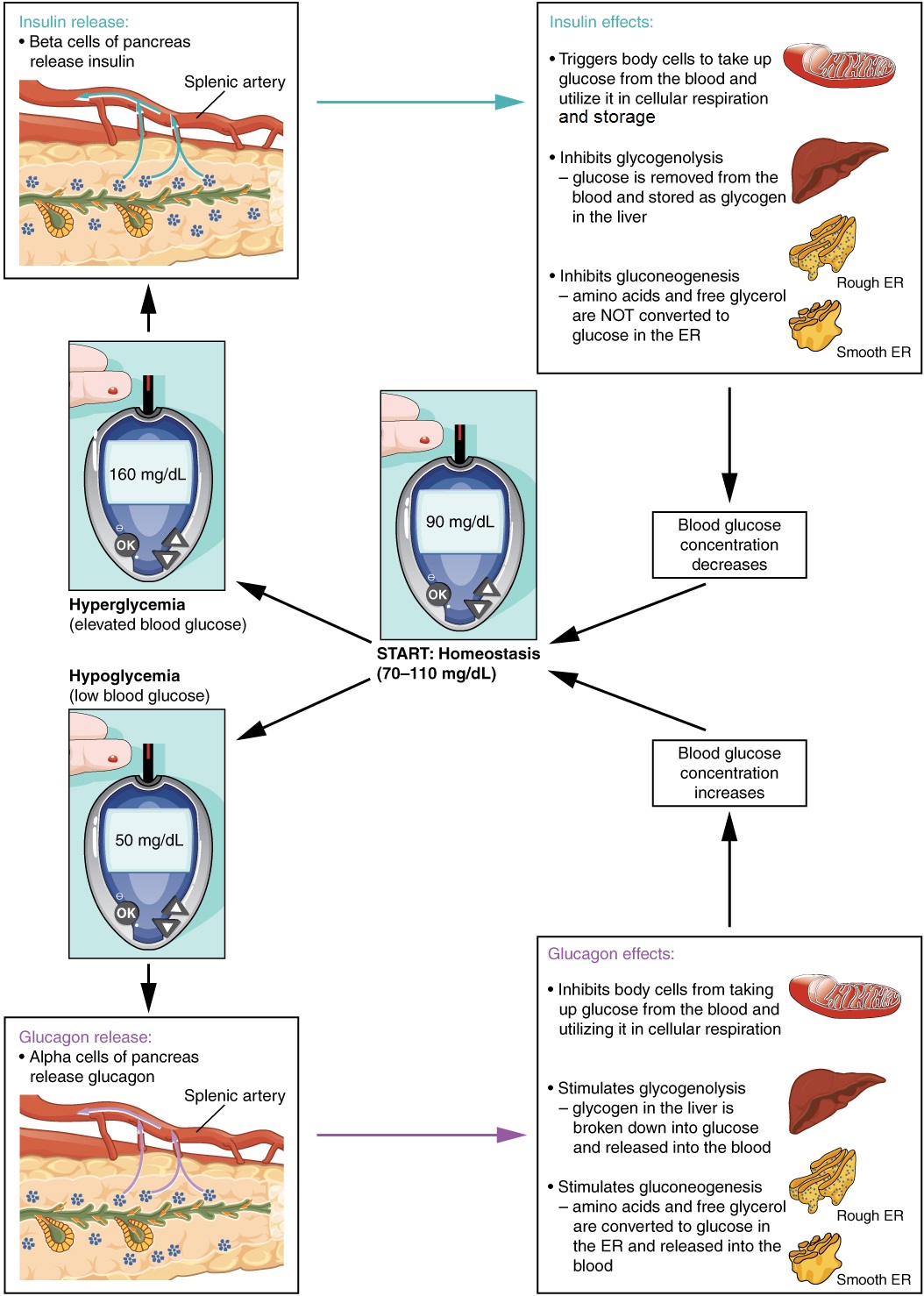
The primary function of insulin is to facilitate the uptake of glucose into body cells. Red blood cells, as well as cells of the brain, liver, kidneys, and the lining of the small intestine, do not have insulin receptors on their cell membranes and do not require insulin for glucose uptake. Although all other body cells do require insulin if they are to take glucose from the bloodstream, skeletal muscle cells and adipose cells are the primary targets of insulin.
The presence of food in the intestine triggers the release of gastrointestinal tract hormones such as glucose-dependent insulinotropic peptide (previously known as gastric inhibitory peptide). This is in turn the initial trigger for insulin production and secretion by the beta cells of the pancreas. Once nutrient absorption occurs, the resulting surge in blood glucose levels further stimulates insulin secretion.
Precisely how insulin facilitates glucose uptake is not entirely clear. However, insulin appears to activate a tyrosine kinase receptor, triggering the phosphorylation of many substrates within the cell. These multiple biochemical reactions converge to support the movement of intracellular vesicles containing facilitative glucose transporters to the cell membrane. In the absence of insulin, these transport proteins are normally recycled slowly between the cell membrane and cell interior. Insulin triggers the rapid movement of a pool of glucose transporter vesicles to the cell membrane, where they fuse and expose the glucose transporters to the extracellular fluid. The transporters then move glucose by facilitated diffusion into the cell interior.

Visit this link to view an animation describing the location and function of the pancreas. What goes wrong in the function of insulin in type 2 diabetes? Note, this animation mis-represents the glucose transport mechanism which here is simplified as a “gated” mechanism.
Insulin also reduces blood glucose levels by stimulating glycolysis, the metabolism of glucose for generation of ATP. Moreover, it stimulates the liver to convert excess glucose into glycogen for storage, and it inhibits enzymes involved in glycogenolysis and gluconeogenesis. Finally, insulin promotes triglyceride and protein synthesis. The secretion of insulin is regulated through a negative feedback mechanism. As blood glucose levels decrease, further insulin release is inhibited.
The pancreatic hormones are summarized in Table 17.7 .
Disorders of the… Endocrine System: Diabetes Mellitus
Dysfunction of insulin production and secretion, as well as the target cells’ responsiveness to insulin, can lead to a condition called diabetes mellitus . As of 2012 the American Diabetes Association reports that diabetes mellitus has been diagnosed in more than 21 million people in the United States; more than 200,000 of those are children. It is estimated that more than 8 million additional adults have the condition but have not been diagnosed. In addition, approximately 86 million people in the US are estimated to have pre-diabetes, a condition in which blood glucose levels are abnormally high, but not yet high enough to be classified as diabetes.
There are two main forms of diabetes mellitus. Type 1 diabetes is an autoimmune disease affecting the beta cells of the pancreas. Certain genes are recognized to increase susceptibility. The beta cells of people with type 1 diabetes do not produce insulin; thus, synthetic insulin must be administered by injection or infusion. This form of diabetes accounts for less than five percent of all diabetes cases.
Type 2 diabetes accounts for approximately 95 percent of all cases. Factors such as family history, ethnicity, age, and the presence of pre-diabetes greatly increase a person’s risk. Often, people with type 2 diabetes are overweight or obese, although weight is not the only risk factor. In type 2 diabetes, cells become resistant to the effects of insulin. In response, the pancreas increases its insulin secretion, but over time, the beta cells become exhausted. In many cases, type 2 diabetes can be reversed by moderate weight loss, regular physical activity, and consumption of a healthy diet; however, if blood glucose levels cannot be controlled, the type 2 diabetic may eventually require synthetic insulin injections.
Two of the early symptoms of the onset of diabetes are excessive urination and excessive thirst. These symptoms demonstrate how the out-of-control levels of glucose in the blood affect kidney function. The kidneys are responsible for filtering the blood. Excessive blood glucose draws water into the urine, and as a result the person eliminates an abnormally large quantity of urine. The use of body water to dilute the urine leaves the body dehydrated, and so the person is unusually and continually thirsty. The person may also experience persistent hunger because the body cells are unable to access the glucose in the bloodstream.
Over time, persistently high levels of glucose in the blood injure tissues throughout the body, especially those of the blood vessels and nerves. Inflammation and injury of the lining of arteries lead to atherosclerosis and an increased risk of heart attack and stroke. Damage to the microscopic blood vessels of the kidney impairs kidney function and can lead to kidney failure. Damage to blood vessels that serve the retina can lead to blindness. Blood vessel damage also reduces circulation to the limbs, whereas nerve damage leads to a loss of sensation, called neuropathy, particularly in the hands and feet. Together, these changes increase the risk of injury, infection, and tissue death (necrosis), contributing to a high rate of toe, foot, and lower leg amputations in people with diabetes. Uncontrolled diabetes can also lead to a dangerous form of metabolic acidosis called ketoacidosis. Deprived of glucose, cells increasingly rely on fat stores for fuel. However, in a glucose-deficient state, the liver is forced to use an alternative lipid metabolism pathway that results in the increased production of ketone bodies (or ketones), which are acidic. The build-up of ketones in the blood causes ketoacidosis, which—if left untreated—may lead to a life-threatening “diabetic coma.” Together, these complications make diabetes the seventh leading cause of death in the United States (2010, American Diabetes Association).
Diabetes is diagnosed when lab tests reveal that blood glucose levels are higher than normal, a condition called hyperglycemia . The treatment of diabetes depends on the type, the severity of the condition, and the ability of the patient to make lifestyle changes. As noted earlier, moderate weight loss, regular physical activity, and consumption of a healthful diet can reduce blood glucose levels in type 2 diabetics. Some patients with type 2 diabetes may be unable to control their disease with these lifestyle changes, and will require medication. Historically, the first-line treatment of type 2 diabetes was insulin. Research advances have resulted in alternative options, including medications that enhance pancreatic function.

Visit this link to view an animation describing the role of insulin and the pancreas in diabetes.
Chapter Review
The pancreas has both exocrine and endocrine functions. Alpha cells of the pancreas produce glucagon, while beta cells produce insulin. Insulin and glucagon are involved in the regulation of glucose metabolism. Insulin is produced by the beta cells in response to high blood glucose levels. It enhances glucose uptake and utilization by target cells, as well as the storage of excess glucose for later use. Dysfunction of the production of insulin or target cell resistance to the effects of insulin causes diabetes mellitus, a disorder characterized by high blood glucose levels. The hormone glucagon is produced and secreted by the alpha cells of the pancreas in response to low blood glucose levels. Glucagon stimulates mechanisms that increase blood glucose levels, such as the catabolism of glycogen into glucose.
Interactive Link Questions
Visit this link to view an animation describing the location and function of the pancreas. What goes wrong in type 2 diabetes?
Insulin receptors no longer function.
Review Questions
Critical thinking questions.
1. What is the physiological consequence of the disease that destroys the beta cells of the pancreas?
2. Why is foot care extremely important for people with diabetes mellitus?
Answers for Critical Thinking Questions
- The beta cells produce the hormone insulin, which is important in the regulation of blood glucose levels. All insulin-dependent cells of the body require insulin in order to take up glucose from the bloodstream. Destruction of the beta cells would result in an inability to produce and secrete insulin, leading to abnormally high blood glucose levels and the disease called type 1 diabetes mellitus.
- Excessive blood glucose levels damage the blood vessels and nerves of the body’s extremities, increasing the risk for injury, infection, and tissue death. Loss of sensation to the feet means that a diabetic patient will not be able to feel foot trauma, such as from ill-fitting shoes. Even minor injuries commonly lead to infection, which , can progress to tissue death without proper care, requiring amputation.
This work, Anatomy & Physiology, is adapted from Anatomy & Physiology by OpenStax , licensed under CC BY . This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images, from Anatomy & Physiology by OpenStax , are licensed under CC BY except where otherwise noted.
Access the original for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction .
Anatomy & Physiology Copyright © 2019 by Lindsay M. Biga, Staci Bronson, Sierra Dawson, Amy Harwell, Robin Hopkins, Joel Kaufmann, Mike LeMaster, Philip Matern, Katie Morrison-Graham, Kristen Oja, Devon Quick, Jon Runyeon, OSU OERU, and OpenStax is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License , except where otherwise noted.

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

9.7: Accessory Organs in Digestion- The Liver, Pancreas, and Gallbladder
- Last updated
- Save as PDF
- Page ID 34637
Learning Objectives
By the end of this section, you will be able to:
- State the main digestive roles of the liver, pancreas, and gallbladder
- Identify three main features of liver histology that are critical to its function
- Discuss the composition and function of bile
- Identify the major types of enzymes and buffers present in pancreatic juice
Chemical digestion in the small intestine relies on the activities of three accessory digestive organs: the liver, pancreas, and gallbladder. The digestive role of the liver is to produce bile and export it to the duodenum. The gallbladder primarily stores, concentrates, and releases bile. The pancreas produces pancreatic juice, which contains digestive enzymes and bicarbonate ions, and delivers it to the duodenum.

The liver is the largest gland in the body, weighing about three pounds in an adult. It is also one of the most important organs. In addition to being an accessory digestive organ, it plays a number of roles in metabolism and regulation. The liver lies inferior to the diaphragm in the right upper quadrant of the abdominal cavity and receives protection from the surrounding ribs.
The liver is divided into two primary lobes: a large right lobe and a much smaller left lobe. In the right lobe, some anatomists also identify an inferior quadrate lobe and a posterior caudate lobe, which are defined by internal features. The liver is connected to the abdominal wall and diaphragm by five peritoneal folds referred to as ligaments. These are the falciform ligament, the coronary ligament, two lateral ligaments, and the ligamentum teres hepatis. The falciform ligament and ligamentum teres hepatis are actually remnants of the umbilical vein, and separate the right and left lobes anteriorly. The lesser omentum tethers the liver to the lesser curvature of the stomach.
The porta hepatis (“gate to the liver”) is where the hepatic artery and hepatic portal vein enter the liver. These two vessels, along with the common hepatic duct, run behind the lateral border of the lesser omentum on the way to their destinations. As shown in, the hepatic artery delivers oxygenated blood from the heart to the liver. The hepatic portal vein delivers partially deoxygenated blood containing nutrients absorbed from the small intestine and actually supplies more oxygen to the liver than do the much smaller hepatic arteries. In addition to nutrients, drugs and toxins are also absorbed. After processing the bloodborne nutrients and toxins, the liver releases nutrients needed by other cells back into the blood, which drains into the central vein and then through the hepatic vein to the inferior vena cava. With this hepatic portal circulation, all blood from the alimentary canal passes through the liver. This largely explains why the liver is the most common site for the metastasis of cancers that originate in the alimentary canal.

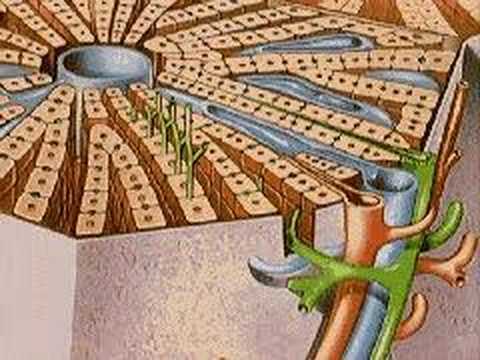
The liver has three main components: hepatocytes, bile canaliculi, and hepatic sinusoids. A hepatocyte is the liver’s main cell type, accounting for around 80 percent of the liver’s volume. These cells play a role in a wide variety of secretory, metabolic, and endocrine functions. Plates of hepatocytes called hepatic laminae radiate outward from the portal vein in each hepatic lobule .
Between adjacent hepatocytes, grooves in the cell membranes provide room for each bile canaliculus (plural = canaliculi). These small ducts accumulate the bile produced by hepatocytes. From here, bile flows first into bile ductules and then into bile ducts. The bile ducts unite to form the larger right and left hepatic ducts, which themselves merge and exit the liver as the common hepatic duct . This duct then joins with the cystic duct from the gallbladder, forming the common bile duct through which bile flows into the small intestine.
A hepatic sinusoid is an open, porous blood space formed by fenestrated capillaries from nutrient-rich hepatic portal veins and oxygen-rich hepatic arteries. Hepatocytes are tightly packed around the fenestrated endothelium of these spaces, giving them easy access to the blood. From their central position, hepatocytes process the nutrients, toxins, and waste materials carried by the blood. Materials such as bilirubin are processed and excreted into the bile canaliculi. Other materials including proteins, lipids, and carbohydrates are processed and secreted into the sinusoids or just stored in the cells until called upon. The hepatic sinusoids combine and send blood to a central vein . Blood then flows through a hepatic vein into the inferior vena cava. This means that blood and bile flow in opposite directions. The hepatic sinusoids also contain star-shaped reticuloendothelial cells (Kupffer cells), phagocytes that remove dead red and white blood cells, bacteria, and other foreign material that enter the sinusoids. The portal triad is a distinctive arrangement around the perimeter of hepatic lobules, consisting of three basic structures: a bile duct, a hepatic artery branch, and a hepatic portal vein branch.
Recall that lipids are hydrophobic, that is, they do not dissolve in water. Thus, before they can be digested in the watery environment of the small intestine, large lipid globules must be broken down into smaller lipid globules, a process called emulsification. Bile is a mixture secreted by the liver to accomplish the emulsification of lipids in the small intestine.
Hepatocytes secrete about one liter of bile each day. A yellow-brown or yellow-green alkaline solution (pH 7.6 to 8.6), bile is a mixture of water, bile salts, bile pigments, phospholipids (such as lecithin), electrolytes, cholesterol, and triglycerides. The components most critical to emulsification are bile salts and phospholipids, which have a nonpolar (hydrophobic) region as well as a polar (hydrophilic) region. The hydrophobic region interacts with the large lipid molecules, whereas the hydrophilic region interacts with the watery chyme in the intestine. This results in the large lipid globules being pulled apart into many tiny lipid fragments of about 1 µ m in diameter. This change dramatically increases the surface area available for lipid-digesting enzyme activity. This is the same way dish soap works on fats mixed with water.
Bile salts act as emulsifying agents, so they are also important for the absorption of digested lipids. While most constituents of bile are eliminated in feces, bile salts are reclaimed by the enterohepatic circulation . Once bile salts reach the ileum, they are absorbed and returned to the liver in the hepatic portal blood. The hepatocytes then excrete the bile salts into newly formed bile. Thus, this precious resource is recycled.
Bilirubin , the main bile pigment, is a waste product produced when the spleen removes old or damaged red blood cells from the circulation. These breakdown products, including proteins, iron, and toxic bilirubin, are transported to the liver via the splenic vein of the hepatic portal system. In the liver, proteins and iron are recycled, whereas bilirubin is excreted in the bile. It accounts for the green color of bile. Bilirubin is eventually transformed by intestinal bacteria into stercobilin, a brown pigment that gives your stool its characteristic color! In some disease states, bile does not enter the intestine, resulting in white (‘acholic’) stool with a high fat content, since virtually no fats are broken down or absorbed.
Hepatocytes work non-stop, but bile production increases when fatty chyme enters the duodenum and stimulates the secretion of the gut hormone secretin. Between meals, bile is produced but conserved. The valve-like hepatopancreatic ampulla closes, allowing bile to divert to the gallbladder, where it is concentrated and stored until the next meal.
Watch this video to see the structure of the liver and how this structure supports the functions of the liver, including the processing of nutrients, toxins, and wastes. At rest, about 1500 mL of blood per minute flow through the liver. What percentage of this blood flow comes from the hepatic portal system?
A YouTube element has been excluded from this version of the text. You can view it online here: pb.libretexts.org/aapii/?p=156
The Pancreas
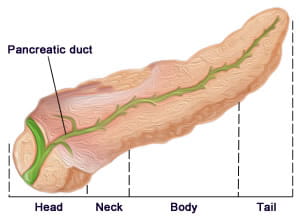
The soft, oblong, glandular pancreas lies transversely in the retroperitoneum behind the stomach. Its head is nestled into the “c-shaped” curvature of the duodenum with the body extending to the left about 15.2 cm (6 in) and ending as a tapering tail in the hilum of the spleen. It is a curious mix of exocrine (secreting digestive enzymes) and endocrine (releasing hormones into the blood) functions.

The exocrine part of the pancreas arises as little grape-like cell clusters, each called an acinus (plural = acini), located at the terminal ends of pancreatic ducts. These acinar cells secrete enzyme-rich pancreatic juice into tiny merging ducts that form two dominant ducts. The larger duct fuses with the common bile duct (carrying bile from the liver and gallbladder) just before entering the duodenum via a common opening (the hepatopancreatic ampulla). The smooth muscle sphincter of the hepatopancreatic ampulla controls the release of pancreatic juice and bile into the small intestine. The second and smaller pancreatic duct, the accessory duct (duct of Santorini), runs from the pancreas directly into the duodenum, approximately 1 inch above the hepatopancreatic ampulla. When present, it is a persistent remnant of pancreatic development.
Scattered through the sea of exocrine acini are small islands of endocrine cells, the islets of Langerhans. These vital cells produce the hormones pancreatic polypeptide, insulin, glucagon, and somatostatin.
Pancreatic Juice
The pancreas produces over a liter of pancreatic juice each day. Unlike bile, it is clear and composed mostly of water along with some salts, sodium bicarbonate, and several digestive enzymes. Sodium bicarbonate is responsible for the slight alkalinity of pancreatic juice (pH 7.1 to 8.2), which serves to buffer the acidic gastric juice in chyme, inactivate pepsin from the stomach, and create an optimal environment for the activity of pH-sensitive digestive enzymes in the small intestine. Pancreatic enzymes are active in the digestion of sugars, proteins, and fats.
The pancreas produces protein-digesting enzymes in their inactive forms. These enzymes are activated in the duodenum. If produced in an active form, they would digest the pancreas (which is exactly what occurs in the disease, pancreatitis). The intestinal brush border enzyme enteropeptidase stimulates the activation of trypsin from trypsinogen of the pancreas, which in turn changes the pancreatic enzymes procarboxypeptidase and chymotrypsinogen into their active forms, carboxypeptidase and chymotrypsin.
The enzymes that digest starch (amylase), fat (lipase), and nucleic acids (nuclease) are secreted in their active forms, since they do not attack the pancreas as do the protein-digesting enzymes.
Pancreatic Secretion
Regulation of pancreatic secretion is the job of hormones and the parasympathetic nervous system. The entry of acidic chyme into the duodenum stimulates the release of secretin, which in turn causes the duct cells to release bicarbonate-rich pancreatic juice. The presence of proteins and fats in the duodenum stimulates the secretion of CCK, which then stimulates the acini to secrete enzyme-rich pancreatic juice and enhances the activity of secretin. Parasympathetic regulation occurs mainly during the cephalic and gastric phases of gastric secretion, when vagal stimulation prompts the secretion of pancreatic juice.
Usually, the pancreas secretes just enough bicarbonate to counterbalance the amount of HCl produced in the stomach. Hydrogen ions enter the blood when bicarbonate is secreted by the pancreas. Thus, the acidic blood draining from the pancreas neutralizes the alkaline blood draining from the stomach, maintaining the pH of the venous blood that flows to the liver.
The Gallbladder
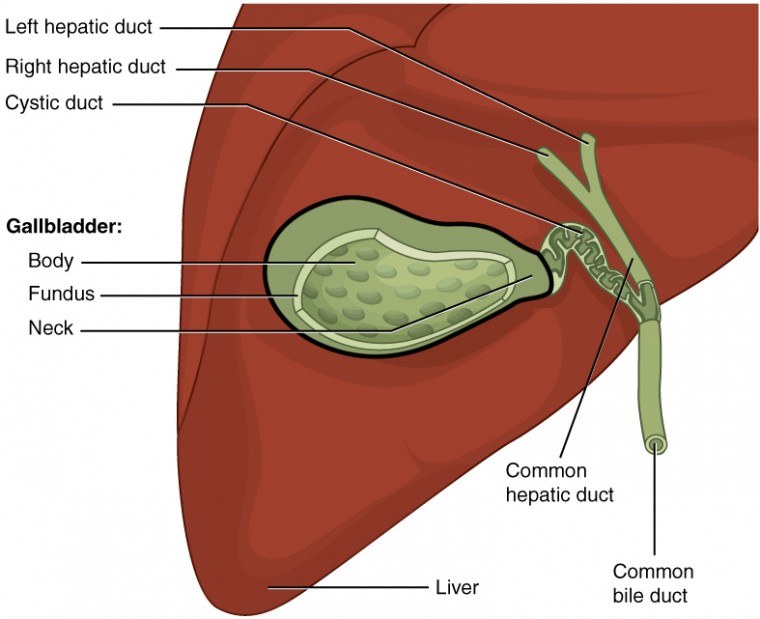
The gallbladder is 8–10 cm (~3–4 in) long and is nested in a shallow area on the posterior aspect of the right lobe of the liver. This muscular sac stores, concentrates, and, when stimulated, propels the bile into the duodenum via the common bile duct. It is divided into three regions. The fundus is the widest portion and tapers medially into the body, which in turn narrows to become the neck. The neck angles slightly superiorly as it approaches the hepatic duct. The cystic duct is 1–2 cm (less than 1 in) long and turns inferiorly as it bridges the neck and hepatic duct.
The simple columnar epithelium of the gallbladder mucosa is organized in rugae, similar to those of the stomach. There is no submucosa in the gallbladder wall. The wall’s middle, muscular coat is made of smooth muscle fibers. When these fibers contract, the gallbladder’s contents are ejected through the cystic duct and into the bile duct. Visceral peritoneum reflected from the liver capsule holds the gallbladder against the liver and forms the outer coat of the gallbladder. The gallbladder’s mucosa absorbs water and ions from bile, concentrating it by up to 10-fold.
Chapter Review
Chemical digestion in the small intestine cannot occur without the help of the liver and pancreas. The liver produces bile and delivers it to the common hepatic duct. Bile contains bile salts and phospholipids, which emulsify large lipid globules into tiny lipid droplets, a necessary step in lipid digestion and absorption. The gallbladder stores and concentrates bile, releasing it when it is needed by the small intestine.
The pancreas produces the enzyme- and bicarbonate-rich pancreatic juice and delivers it to the small intestine through ducts. Pancreatic juice buffers the acidic gastric juice in chyme, inactivates pepsin from the stomach, and enables the optimal functioning of digestive enzymes in the small intestine.
Answer the question(s) below to see how well you understand the topics covered in the previous section.
https://oea.herokuapp.com/assessments/275
Critical Thinking Questions
- Why does the pancreas secrete some enzymes in their inactive forms, and where are these enzymes activated?
- Describe the location of hepatocytes in the liver and how this arrangement enhances their function.
[reveal-answer q=”668144″]Show Answers[/reveal-answer] [hidden-answer a=”668144″]
- The pancreas secretes protein-digesting enzymes in their inactive forms. If secreted in their active forms, they would self-digest the pancreas. These enzymes are activated in the duodenum.
- The hepatocytes are the main cell type of the liver. They process, store, and release nutrients into the blood. Radiating out from the central vein, they are tightly packed around the hepatic sinusoids, allowing the hepatocytes easy access to the blood flowing through the sinusoids.
[/hidden-answer]
accessory duct: (also, duct of Santorini) duct that runs from the pancreas into the duodenum
acinus: cluster of glandular epithelial cells in the pancreas that secretes pancreatic juice in the pancreas
bile: alkaline solution produced by the liver and important for the emulsification of lipids
bile canaliculus: small duct between hepatocytes that collects bile
bilirubin: main bile pigment, which is responsible for the brown color of feces
central vein: vein that receives blood from hepatic sinusoids
common bile duct: structure formed by the union of the common hepatic duct and the gallbladder’s cystic duct
common hepatic duct: duct formed by the merger of the two hepatic ducts
cystic duct: duct through which bile drains and enters the gallbladder
enterohepatic circulation: recycling mechanism that conserves bile salts
enteropeptidase: intestinal brush-border enzyme that activates trypsinogen to trypsin
gallbladder: accessory digestive organ that stores and concentrates bile
hepatic artery: artery that supplies oxygenated blood to the liver
hepatic lobule: hexagonal-shaped structure composed of hepatocytes that radiate outward from a central vein
hepatic portal vein: vein that supplies deoxygenated nutrient-rich blood to the liver
hepatic sinusoid: blood capillaries between rows of hepatocytes that receive blood from the hepatic portal vein and the branches of the hepatic artery
hepatic vein: vein that drains into the inferior vena cava
hepatocytes: major functional cells of the liver
liver: largest gland in the body whose main digestive function is the production of bile
pancreas: accessory digestive organ that secretes pancreatic juice
pancreatic juice: secretion of the pancreas containing digestive enzymes and bicarbonate
porta hepatis: “gateway to the liver” where the hepatic artery and hepatic portal vein enter the liver
portal triad: bile duct, hepatic artery branch, and hepatic portal vein branch
reticuloendothelial cell: (also, Kupffer cell) phagocyte in hepatic sinusoids that filters out material from venous blood from the alimentary canal
Contributors and Attributions
- Anatomy & Physiology. Provided by : OpenStax CNX. Located at : http://cnx.org/contents/[email protected] . License : CC BY: Attribution . License Terms : Download for free at http://cnx.org/contents/[email protected]
- How the Body Works : The Architecture of the Liver. Located at : https://youtu.be/Gn-ibhGE7PI . License : All Rights Reserved . License Terms : StandardYouTube License
VIVO Pathophysiology
Digestive System > Pancreas
Exocrine Secretions of the Pancreas
Send comments to [email protected]
Pancreatic Juice: Characteristics, Functions and Composition
He pancreatic juice Is a clear liquid secreted by the pancreas composed mainly of water, electrolytes and enzymes.
The pancreas plays an important role in the digestion of food and it is the enzymes found in pancreatic juice that allow the body to break down carbohydrates, proteins and fats.
Pancreatic juice composition
Pancreatic juice is composed of: water, mineral salts, enzymes, amylase, lipase, inactive enzyme precursors, trypsinogen and chymotrypsinogen and procarboxypeptidase.
The alkaline nature of pancreatic juice is attributed to the presence of bicarbonate ions, which are alkaline in solution.
Pancreatic enzymes
The pancreas creates natural juices called pancreatic enzymes to break down food. These juices travel through the pancreas through ducts, and empty into the duodenum. Each day, the pancreas produces about 200 ml of digestive juice filled with enzymes. These are:
This enzyme works together with bile, which produces the liver, to break down fat. If you do not have enough lipase, your body will experience problems absorbing fat and important liposoluble vitamins (A, D, E, K). Symptoms of bad fat absorption include diarrhea And fatty bowel movements.
This enzyme breaks down the proteins we ingest. It also helps protect us from germs that can live in the intestines, such as certain bacteria and yeast. Undigested proteins can cause allergic reactions in some people.
This enzyme helps to break down starches into sugar, which the body can use for energy. An insufficiency of amylase may cause undigested carbohydrate diarrhea.
Pancreatic hormones
Many groups of Cells Produce hormones inside the pancreas. Unlike enzymes that are released into the digestive system, hormones are released into the blood and carry messages to other parts of the digestive system. Pancreatic hormones include:
This hormone is produced in the cells of the pancreas known as beta cells. Beta cells make up about 75% of pancreatic hormone cells.
Insulin is the hormone that helps the body use sugar as energy. Without enough insulin, blood sugar levels rise and diabetes develops.
Alpha cells represent about 20% of pancreatic cells that produce hormones, which produce glucagon. If the blood sugar level is too low, glucagon helps increase it by sending a message to the liver to release the stored sugar.
Gastrin and amylin
Gastrin occurs mainly in G cells in the stomach, but it also occurs in the pancreas and its function is to stimulate the stomach to produce gastric acid. Amylin is produced in beta cells and helps control the appetite and emptying of the stomach.
Functions of pancreatic juice
1- protein digestion.
The enteropeptidase converts the trypsinogen and chymotrypsinogen into the active proteolytic enzymes trypsin and chymotrypsin, which convert the polypeptides into tripeptides, dipeptides and amino acids.

Digestion of carbohydrates
Pancreatic amylase helps in the conversion of digestible polysaccharides - starch - by salivary amylase to disaccharides.
Digestion of fats
Bile salts help lipase in the conversion of fats into Acids Fatty acids and glycerol.
What is the pancreas?
The pancreas is a spongy organ, shaped like a tube, about 15 centimeters long. It is located in the back of the abdomen, behind the stomach and connected to the duodenum.
The pancreas is a vital digestive organ because it produces a variety of enzymes that break down all major food groups.
These enzymes are secreted in the duodenum along with a high concentration of bicarbonate. Bicarbonate causes pancreatic secretions to be alkaline in nature.
The pancreas produces pancreatic juices and hormones. Pancreatic juices contain enzymes that help digest food in the small intestine.
Among the hormones made by the pancreas is insulin, which controls the amount of sugar in the blood. Both enzymes and hormones are necessary for the proper functioning of the body.
This flow of alkaline fluid in the small intestine helps to neutralize the acid chyme that comes from the stomach.
Chyme is the mass of partially digested food that has just come out of the stomach. Neutralizing the acidic chyme provides a better environment for the activation of pancreatic enzymes.
Once produced, the pancreatic juices flow into the main pancreatic duct. This duct connects to the bile duct, which connects the pancreas to the liver and gallbladder.
The common bile duct, which carries bile (a fluid that helps digest fat), connects to the small intestine through an opening called a blister in the duodenum near the stomach.
Functions of the Pancreas
A healthy pancreas produces the correct chemicals in the right amounts, at the right times, to digest the food we eat.
Exocrine function
The pancreas contains Exocrine glands Which produce enzymes important for digestion. These enzymes include: trypsin and chymotrypsin to digest proteins; Amylase for the digestion of carbohydrates; And lipase to break down fats.
When food enters the stomach, these pancreatic juices are released into a duct system that culminates in the main pancreatic duct.
The pancreatic duct joins the common bile duct to form the Vater ampulla (or major duodenal papilla) found in the first portion of the small intestine called the duodenum.
The common bile duct originates in the liver and gallbladder and produces another important digestive juice called bile. The pancreatic juices and bile that are released into the duodenum, help the body digest fats, carbohydrates and proteins.
Endocrine Function
The endocrine component of the pancreas consists of islet cells (called islets of Langerhans or pancreatic islets) that create and release important hormones directly into the bloodstream.
Two of the major pancreatic hormones are insulin, which acts to lower blood sugar, and glucagon, which acts to raise blood sugar.
Maintaining adequate blood sugar levels is crucial for the functioning of key organs such as brain , Liver and kidneys.
- "The digestive process: What is the role of your pancreas in digestion?"In: Health Library Content. Columbia Doctors. New York Presbyterian. Retrieved on: May 11, 2017 from nyp.org.
- Cloe, A."What Causes the Release of Pancreatic Juice & Bile?"(April, 2011) in Livestrong. Retrieved on: May 11, 2017 from livestrong.com.
- "Pancreatic juice or pancreatic secretion"in: AC Dr. Cormillot. Retrieved on: May 11, 2017 by: drcormillot.com.
- "The Pancreas and Its Functions"at: The Pancreas Center. Columbia Doctors. Columbia University Medical Center. Retrieved on: May 11, 2017 from columbiasurgery.org.
- "The Pancreas"in: Johns Hopkins Medicine. The Sol Goldman Pancreatic Cancer Research Center. Retrieved on: May 11, 2017 from jhu.edu.
- "Pancreatic pathology"(January 2017) in Eusalud. Retrieved on: May 11, 2017 from eusalud.uninet.edu.
- "Exocrine Secretions of the Pancreas"in LIVE Pathophysiology Hypertexts for Biomedical Sciences. Retrieved on May 11, 2017 live.colostate.edu.
- "Medical Definition of Pancreatic juices"(January 2017) in Medicinenet Retrieved on May 11, 2017 from medicinenet.com.
- Beaudoin, St-Jean & Grondin"Pancreatic Juice Composition: New Views on the Cellular Mechanisms That Control the Concentration of Digestive and Nondigestive Proteins"(1989 Vol 7 No 4) Canada. Retrieved on: May 11, 2017 from karger.com.
Recent Posts
- Medical Services
- Schedule an Appointment
- Children's Health
- Hollings Cancer Center
- Education at MUSC
- Research at MUSC
- Digestive Health
- Digestive Organs
Digestive Disease Center
The pancreas and bile duct (biliary) systems together form an important part of the digestive system. The pancreas and liver produce juices (pancreatic juice and bile) which help in the process of digestion (i.e. the breakdown of foods into parts which can be absorbed easily and used by the body).
The anatomy (design) of the biliary and pancreatic ducts is not the same in every person. Variations can be important; some can cause medical problems, others may make treatment more difficult or complicated.
Papilla of Vater and Minor (Accessory) Papilla
The main papilla of Vater is a small nipple-like structure on the wall of the duodenum, in its "second part." The duodenum is the upper part of the small intestine, into which food flows from the stomach.
The papilla forms the main exit hole for the bile and pancreatic juices which flow down the bile duct and pancreatic duct. Rarely there are two separate holes close together within the same papillary nipple. The papilla remains closed at rest, because of the activity of a muscular valve (sphincter). The sphincter (of Oddi) surrounds the exit of the bile duct and pancreatic duct. It opens by reflex action when foods enter the stomach, so that juices can be released to help in their digestion.
Bile Duct System and Gallbladder
The bile duct (biliary) system provides the channels through which bile is transported from the liver to the duodenum (through the papilla of Vater).
The liver is found in the right upper corner of the abdomen, immediately below the diaphragm. In health it weighs 3-4 pounds. It is divided into right and left lobes, and each of these have several segments. The bile ducts start as tiny tubes called sinusoids which lie between rows of liver cells called hepatocytes.
These liver cells make bile, and pass it into the tiny canals (cannaliculi). The small ducts join together like branches to form the main biliary tree, with one trunk which is formed just outside the surface of the liver. This is called the common hepatic duct.
The gallbladder is a collection sac for bile, which enters and leaves through a narrow tube called the cystic duct. The gallbladder is about the size of an egg when full. The bile duct below the cystic duct is usually called the common bile duct. The common bile duct and the common hepatic duct together constitute the main bile duct. The lower end of the bile duct sweeps around behind the duodenum and through the head of the pancreas before joining the pancreatic duct at the main papilla (of Vater).
Pancreatic Duct System
There is a main pancreatic duct which collects juices from all the branches of the pancreatic stream, and exits at the main papilla of Vater. The pattern of these branches varies considerably, but this does not matter. However, there is often another important duct (named after Santorini) that connects the main pancreatic duct to another small papilla (the minor or accessory papilla) which is found about 2 cm (3/4 inch) above the main papilla of Vater in the duodenum. This (normal) arrangement comes about as a result of complex reorganization during fetal development. Early in the development of the embryo, the pancreas is in two parts (dorsal and ventral elements). These parts usually join together to form one pancreas between six and eight weeks of pregnancy. Even after joining, the santorini stays open or "patent," and drains into the minor papilla in over half of patients. Thus, the patient who develops a problem at the main papilla (like a stone or tumor) may not develop any symptoms of pancreatic obstruction if Santorini's duct and the minor papilla are open, and can take over the drainage function.
However, this fusion (joining) does not happen in about one in twelve people (at least in western populations). Then the pancreas remains divided (so called "pancreas divisum"). In patients with divisum, the largest (dorsal) part of the pancreas drains through Santorini's duct and the minor papilla, while only a small part (the ventral pancreas) drains through the usual (major) papilla. The importance of this is that the minor papilla may be too small to allow easy passage of the pancreatic juices; and some patients with pancreas divisum can develop attacks of pain and pancreatitis as a result due to this relative narrowing.
There are other rarer variations of pancreatic anatomy. Annular pancreas describes a congenital condition in which one of the branches of the pancreas swings all around the duodenum; this can narrow the duodenum sufficiently to cause obstruction and require operation. This condition usually presents in infancy (for obvious reasons), but can be discovered only later in life if the narrowing is not so tight, and sometimes when attacks of pancreatitis are associated with it. Other anomalies of pancreas development produce interesting pictures, but are not of clinical importance.
Function & Control
The tissues of the pancreas (acinar cells) produce a clear digestive fluid made up of bicarbonate, and enzymes. Bicarbonate is alkaline, and helps digestion by neutralizing the stomach acid containing the food as it passes into the duodenum. The enzymes are more important. These are designed to help breakdown (digest) complex carbohydrates (sugars), proteins, and fats in the food. The main enzymes are called amylase, proteases (trypsin, chymotrypsin), and lipase. The enzyme and bicarbonate secretions together are called the "exocrine" function of the pancreas.
The bile ducts function as a drainage system for the liver. Bile is a bitter dark fluid, composed of bile acids, bile pigments, bilirubin, cholesterol and other fats, water and electrolytes. Some of these constituents are useful for digestion, others are simply waste products (i.e. cholesterol).
The gallbladder acts to store bile, and make it more concentrated by removing water. Although thin, the gallbladder wall has muscle tissue, so that it can contract and empty when necessary.
Production of the bile and pancreas juices and their release into the duodenum through the papilla of Vater are controlled by abdominal nerves and also specific messengers (hormones) which pass to their targets through the bloodstream. These systems also control contractions of the gallbladder, and relaxation of the sphincter of Oddi (the muscular valve within the papilla of Vater). Together these insure that the juices are produced and released into the duodenum only when they are needed, that is when food arrives from the stomach ready for final digestion, and subsequent absorption.
The pancreas also has an "endocrine" function – the production of insulin and other important hormones. These are produced in separate tissues within the pancreas (islets of Langerhans), and passed directly into the blood stream (rather than into the pancreatic duct). Insulin is very important for control of sugar levels in the blood; lack of insulin results in diabetes. The pancreas produces many other enzymes (such as somatostatin, pancreatic polypeptide, glucagon, etc.), the functions of which are of less immediate importance. Glucagon helps counteract insulin and helps prevent hypoglycemia, a common problem after extensive/total pancreas surgery.
Dysfunction & Symptoms
Pancreatic juices may not reach the duodenum if the duct or papilla is blocked, or if the pancreas is so damaged by disease that it cannot produce adequate bicarbonate and enzymes. Lack of pancreatic juices results in inadequate digestion. Clinically this is noteworthy by the passage of large bowel movements, which a strong odor and are difficult to flush down the toilet because of their high content of fat. Indeed, sometimes patients with pancreatic insufficiency may note an "oil slick" on the toilet water. Excessive fat in the stools is called "steatorrhea." Because food is not absorbed properly patients usually lose weight.
These pancreatic enzymes can be replaced, at least to a certain extent, by giving them in the form of a medicine by mouth – so called pancreatic enzyme supplements. It is not usually necessary to replace the missing bicarbonate output.
Lack of bile also interferes with digestion (particularly of fats) and can also result in steatorrhea. Lack of bile in the duodenum is usually due to blockage of the main bile duct, or papilla. The liver continues to produce bile, which then spills backwards into the blood stream. Eventually this causes yellow discoloration of the body (jaundice), first noticeable in the whites of the eyes. If bile does not enter the duodenum, bowel movements lose their usual color, and look like pale putty. When the bile ducts are blocked, retention of bile salts in the blood can result also in considerable itching (pruritus). Blockage of the bile ducts or pancreatic ducts can cause pain due to overdistention.
Lack of insulin secretion by the pancreas results in diabetes. It is also possible to have too much insulin when the islets of Langerhans overact, or become tumorous. This results in the blood sugar falling below normal levels, resulting in faintness and eventually coma. Lack or excess of other pancreatic hormones (such as somatostatin, vasoinhibitory peptide, glucagon, etc.) can cause unusual symptoms very rarely.

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

18.8D: Pancreatic Juice
- Last updated
- Save as PDF
- Page ID 50443
Pancreatic fluid contains digestive enzymes that help to further break down the carbohydrates, proteins, and lipids in the chyme.
Learning Objectives
- Describe the nature and function of pancreatic juice
- Pancreatic fluid or juice contains digestive enzymes that pass to the small intestine where they help to further break down the carbohydrates, proteins, and lipids (fats) in the chyme.
- Pancreatic fluid is alkaline in nature due to its high concentration of bicarbonate ions that neutralize the gastric acid and allow effective enzymic action.
- Pancreatic juice secretion is regulated by the hormones secretin and cholecystokinin. It is produced by the walls of the duodenum upon detection of acid food, proteins, fats, and vitamins.
- pancreatic fluid : A liquid secreted by the pancreas that contains a variety of enzymes, including trypsinogen, chymotrypsinogen, elastase, carboxypeptidase, pancreatic lipase, and amylase.
The pancreas is a glandular organ in the digestive system and endocrine system of vertebrates. It is both an endocrine gland that produces several important hormones—including insulin, glucagon, somatostatin, and pancreatic polypeptide—and a digestive organ that secretes pancreatic juice that has digestive enzymes that assist the absorption of nutrients and digestion in the small intestine. These enzymes help to further break down the carbohydrates, proteins, and lipids in the chyme.
Pancreatic Juice
Pancreatic juice is a liquid secreted by the pancreas that contains a variety of enzymes, including trypsinogen, chymotrypsinogen, elastase, carboxypeptidase, pancreatic lipase, nucleases, and amylase.

Pancreatic fluid : A schematic diagram that shows pancreatic acini and the ducts where fluid is created and released.
Pancreatic juice is alkaline in nature due to its high concentration of bicarbonate ions that neutralize the gastric acid and allow effective enzymic action.
Pancreatic juice secretion is regulated by the hormones secretin and cholecystokinin. It is produced by the walls of the duodenum upon detection of acid food, proteins, fats, and vitamins. Pancreatic secretion consists of an aqueous bicarbonate component from the duct cells and an enzymatic component from the acinar cells.
Because the pancreas is a sort of storage depot for digestive enzymes, injury to the pancreas is potentially fatal. A puncture of the pancreas generally requires prompt and experienced medical intervention.
A variety of factors cause a high pressure within pancreatic ducts. Pancreatic duct rupture and pancreatic juice leakage cause pancreatic self-digestion.
LICENSES AND ATTRIBUTIONS
CC LICENSED CONTENT, SHARED PREVIOUSLY
- Curation and Revision. Authored by : Boundless.com. Provided by : Boundless.com. License : CC BY-SA: Attribution-ShareAlike
CC LICENSED CONTENT, SPECIFIC ATTRIBUTION
- Human Physiology/The gastrointestinal system.. Provided by : Wikibooks. Located at : en.wikibooks.org/wiki/Human_Physiology/The_gastrointestinal_system%23The_Digestive_System . License : CC BY-SA: Attribution-ShareAlike
- Pancreas. Provided by : Wikipedia. Located at : en.Wikipedia.org/wiki/Pancreas . License : CC BY-SA: Attribution-ShareAlike
- pancreas. Provided by : Wiktionary. Located at : en.wiktionary.org/wiki/pancreas . License : CC BY-SA: Attribution-ShareAlike
- Pancreas. Provided by : Wikimedia. Located at : upload.wikimedia.org/Wikipedia/commons/a/a3/Pancreas.jpg . License : Public Domain: No Known Copyright
- epigastrium. Provided by : Wiktionary. Located at : en.wiktionary.org/wiki/epigastrium . License : CC BY-SA: Attribution-ShareAlike
- Pancreas. Provided by : Wikimedia. Located at : upload.wikimedia.org/Wikipedia/commons/f/fe/Illu_pancreas_duodenum.jpg . License : Public Domain: No Known Copyright
- Pancreas. Provided by : Wikipedia. Located at : en.Wikipedia.org/wiki/Pancreas%23Histology . License : CC BY-SA: Attribution-ShareAlike
- acini. Provided by : Wikipedia. Located at : en.Wikipedia.org/wiki/acini . License : CC BY-SA: Attribution-ShareAlike
- islets of Langerhans. Provided by : Wiktionary. Located at : en.wiktionary.org/wiki/islets_of_Langerhans . License : CC BY-SA: Attribution-ShareAlike
- Pancreatic juice. Provided by : Wikipedia. Located at : en.Wikipedia.org/wiki/Pancreatic_juice . License : CC BY-SA: Attribution-ShareAlike
- pancreatic fluid. Provided by : Wikipedia. Located at : en.Wikipedia.org/wiki/pancreatic%20fluid . License : CC BY-SA: Attribution-ShareAlike
- Pancreatic. Provided by : Wikimedia. Located at : upload.wikimedia.org/Wikipedia/commons/8/85/Pancreas_secretions2.png . License : CC BY-SA: Attribution-ShareAlike
Optimization of Pancreatic Juice Collection: A First Step Toward Biomarker Discovery and Early Detection of Pancreatic Cancer
Affiliations.
- 1 Department of Gastroenterology & Hepatology, Erasmus MC, University Medical Center, Rotterdam, the Netherlands.
- 2 Department of Medical Oncology, Erasmus MC, University Medical Center, Rotterdam, the Netherlands.
- 3 Deceased.
- PMID: 33105193
- DOI: 10.14309/ajg.0000000000000939
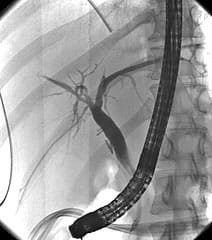
Introduction: Imaging-based surveillance programs fail to detect pancreatic ductal adenocarcinoma at a curable stage, creating an urgent need for diagnostic biomarkers.
Methods: Secretin-stimulated pancreatic juice (PJ) was collected from the duodenal lumen during endoscopic ultrasound. The yield of biomarkers and organoids was compared for 2 collection techniques (endoscope suction channel vs catheter-based) and 3 periods (0-4 vs 4-8 vs 8-15 minutes).
Results: Collection through the endoscope suction channel was superior to collection with a catheter. Collection beyond 8 minutes reduced biomarker yield. PJ-derived organoid culture was feasible.
Discussion: The optimal protocol for secretin-stimulated PJ collection is through the endoscope suction channel for 8 minutes allowing biomarker detection and organoid culture.
- Biomarkers / metabolism*
- Carcinoma, Pancreatic Ductal / diagnosis*
- Carcinoma, Pancreatic Ductal / metabolism
- Early Detection of Cancer / methods
- Endosonography
- Pancreatic Juice / metabolism*
- Pancreatic Neoplasms / diagnosis*
- Pancreatic Neoplasms / metabolism
- Prospective Studies
What Are Digestive Juices?
Numerous organs in the digestive system play a part in the production of digestive juices. These juices are released by several glands to aid with digestion. The salivary glands, stomach, liver, pancreas, and small intestine are the organs that release digestive juices. Here, let’s learn more about digestive juices.
Table of Contents
List of digestive juices, digestive juices, frequently asked questions.
The list of five main categories of digestive juices and some of the enzymes secreted by them are mentioned below:
- Gastric juices
- Gastric lipase
- Gastric amylase
- Intestinal juices
- Intestinal lipase
- Pancreatic juices
- Pancreatic amylase
- Pancreatic lipase
- Chymotrypsin
Digestive fluids aid digestion by reducing food to simple nutrients. The body uses these nutrients for a variety of purposes after that.
Enzymes found in digestive juices accelerate bodily chemical processes. The main digestive enzymes used by the body to break down food are amylase, lipase, and protease, while many other specialised enzymes are also involved. Let us have a look at the digestive juices and enzymes involved in digestion.
Gastric Juice
The primary action of gastric juice is on proteins. Pepsin and rennin are the 2 main proteolytic enzymes present in gastric juice. Other enzymes found in gastric juice include gastric amylase, gelatinase, and lipase.
- Pepsin is usually secreted as inactive pepsinogen. Hydrochloric acid converts pepsinogen into pepsin. Then, proteins are changed into proteoses, peptones, and polypeptides by pepsin. Pepsin also makes milk curdle and digest (casein).
- Gastric lipase is a lipolytic enzyme that breaks down butter fat or tributyrin into fatty acids and glycerols.
- Gelatinase breaks down collagen and type IV and type V gelatin into peptides.
- Urease reacts with urea to create ammonia.
- Gastric amylase breaks down starch, but its impact is minimal.
- Rennin is present in infants and animals only and it curdles milk.
Intestinal Juice
Intestinal juices are released by pits between intestinal villi called crypts of Lieberkuhn. The following table will provide an overview of intestinal juices and their action.
Also Check: Role of Digestive Enzymes
Pancreatic Juice
A number of digestive enzymes like amylase, trypsin and lipase are contained in the liquid released by the pancreas known as pancreatic juice. The pancreatic juice’s neutralising activity is crucial because it shields the intestine from the damaging effects of chyme’s acidic nature.
- The amylolytic enzyme found in pancreatic juice is called pancreatic amylase. The pancreatic amylase turns starch into dextrin and maltose, just like salivary amylase does.
- Trypsin and chymotrypsin are the pancreatic juice’s two main proteolytic enzymes. Nuclease, elastase, collagenase, and carboxypeptidases are further proteolytic enzymes.
- Pancreatic lipase, cholesterol ester hydrolase, phospholipase A, phospholipase B, colipase, and bile salt activated lipase are among the lipolytic enzymes found in pancreatic juice.
Bile juice is secreted by liver cells and discharged into the bile canaliculus. In order for fat to be digested, it must first be emulsified by bile. Thus it acts as a detergent and helps in the absorption of fat. Bilirubin, a byproduct created during the breakdown of red blood cells, is also excreted through bile.
Saliva is a digestive juice secreted by the salivary glands and is present in the mouth. It initiates chemical digestion while the mouth is still physically chewing the food. Saliva contains three digesting enzymes:
- Lingual lipase – It is a lipid-digesting (lipolytic) enzyme. Milk fats (pre-emulsified fats) are digested by it. Triglycerides are hydrolyzed into fatty acids and diacylglycerol by the action of lingual lipase.
- Salivary amylase – It is an enzyme that breaks down carbohydrates. It works by converting cooked or boiling starch into dextrin and maltose.
- Maltase – Maltose is transformed into glucose by the enzyme maltase, which has only trace amounts in human saliva.
Keep exploring BYJU’S Biology to learn more such exciting topics.
Recommended Video:

- Digestive Enzymes
- Digestion and Absorption
- Diagram of Digestive System
- Large Intestine (Colon) – Diagram
What is digestion?
What are the digestive juices in the small intestine, what is the function of digestive juices, what are the salivary glands in humans.
- Share Share
Register with BYJU'S & Download Free PDFs
Register with byju's & watch live videos.


COMMENTS
Pancreatic enzymes. Your pancreas creates natural juices called pancreatic enzymes to break down foods. These juices travel through your pancreas via ducts. They empty into the upper part of your small intestine called the duodenum. Each day, your pancreas makes about 8 ounces of digestive juice filled with enzymes. These are the different enzymes:
Pancreatic juice is alkaline in nature due to its high concentration of bicarbonate ions that neutralize the gastric acid and allow effective enzymic action. Pancreatic juice secretion is regulated by the hormones secretin and cholecystokinin. It is produced by the walls of the duodenum upon detection of acid food, proteins, fats, and vitamins.
Pancreatic juice. Pancreatic juice is a liquid secreted by the pancreas, [1] which contains a number of digestive enzymes, including trypsinogen, chymotrypsinogen, elastase, carboxypeptidase, pancreatic lipase, nucleases and amylase. The pancreas is located in the visceral region, and is a major part of the digestive system required for proper ...
The pancreas is a long, slender organ, most of which is located posterior to the bottom half of the stomach (Figure 17.9.1).Although it is primarily an exocrine gland, secreting a variety of digestive enzymes, the pancreas also has endocrine cells. Its pancreatic islets—clusters of cells formerly known as the islets of Langerhans—secrete the hormones glucagon, insulin, somatostatin, and ...
It delivers pancreatic juice to the duodenum through the pancreatic duct. The exocrine part of the pancreas arises as little grape-like cell clusters, each called an acinus (plural = acini), located at the terminal ends of pancreatic ducts. These acinar cells secrete enzyme-rich pancreatic juice into tiny merging ducts that form two dominant ...
Exocrine Secretions of the Pancreas. Pancreatic juice is composed of two secretory products critical to proper digestion: digestive enzymes and bicarbonate. The enzymes are synthesized and secreted from the exocrine acinar cells, whereas bicarbonate is secreted from the epithelial cells lining small pancreatic ducts.
Pancreas fluid (PF), also termed pancreatic juice, has been studied by scientists for >50 years, with the goals of better understanding pancreatic physiology and pathophysiology, and improving clinical diagnosis of pancreatic diseases. Assays of PF for pancreatic enzyme and bicarbonate concentrations became mainstays of clinical diagnosis for ...
Overview. The pancreas is a large, mixed gland composed of five parts: the head, uncinate process, neck, body and tail. The location of the pancreas is mostly retroperitoneal, except for the tail.This organ extends from the C-shaped curve of the duodenum, passes behind the stomach and finishes at the hilum of the spleen.Several pancreatic ducts extend throughout the pancreas, emptying the ...
Pancreatic juice is an alkaline fluid (pH 8) containing enzymes, pro-enzymes and electrolytes for the digestion of carbohydrates, proteins, fats and nucleic acids; 1200-1500 mL/day is secreted from the exocrine acini of epithelial cells, which comprise 98% of the pancreatic mass. The remaining 2% is comprised of the endocrine islets of ...
The sphincter of Oddi is a muscle that opens and closes to allow bile and pancreatic juice to flow into your small intestine. In sphincter of Oddi dysfunction, your sphincter muscle doesn't open when it should, which causes a backup of digestive juices and severe pain in your abdomen. Healthcare providers treat this condition with medications ...
These acinar cells secrete enzyme-rich pancreatic juice into tiny merging ducts that form two dominant ducts. The larger duct fuses with the common bile duct (carrying bile from the liver and gallbladder) just before entering the duodenum via a common opening (the hepatopancreatic ampulla). The smooth muscle sphincter of the hepatopancreatic ...
Pancreatic juice composition. Pancreatic juice is composed of: water, mineral salts, enzymes, amylase, lipase, inactive enzyme precursors, trypsinogen and chymotrypsinogen and procarboxypeptidase. The alkaline nature of pancreatic juice is attributed to the presence of bicarbonate ions, which are alkaline in solution.
The pancreas and liver produce juices (pancreatic juice and bile) which help in the process of digestion (i.e. the breakdown of foods into parts which can be absorbed easily and used by the body). The pancreas is about the same size and shape as a small banana, and lies in the upper abdomen, towards the back, near the spine. The pancreas is ...
Pancreatic juice is a liquid secreted by the pancreas that contains a variety of enzymes, including trypsinogen, chymotrypsinogen, elastase, carboxypeptidase, pancreatic lipase, nucleases, and amylase. Pancreatic fluid: A schematic diagram that shows pancreatic acini and the ducts where fluid is created and released.
For me, the journey started by becoming fascinated with the pancreas, an organ incorporating two parts, an endocrine with the islets of Langerhans and the exocrine producing a lot of juice containing enzymes for digestion. ... p53 and K-ras mutations in pancreatic juice samples from patients with chronic pancreatitis. Gastrointest Endosc, 53 (7 ...
Secretin-stimulated pancreatic juice (PJ) was collected from the duodenal lumen during endoscopic ultrasound. The yield of biomarkers and organoids was compared for 2 collection techniques (endoscope suction channel vs catheter-based) and 3 periods (0-4 vs 4-8 vs 8-15 minutes).
Introduction: Imaging-based surveillance programs fail to detect pancreatic ductal adenocarcinoma at a curable stage, creating an urgent need for diagnostic biomarkers. Methods: Secretin-stimulated pancreatic juice (PJ) was collected from the duodenal lumen during endoscopic ultrasound. The yield of biomarkers and organoids was compared for 2 collection techniques (endoscope suction channel vs ...
The pancreatic juice's neutralising activity is crucial because it shields the intestine from the damaging effects of chyme's acidic nature. The amylolytic enzyme found in pancreatic juice is called pancreatic amylase. The pancreatic amylase turns starch into dextrin and maltose, just like salivary amylase does. Trypsin and chymotrypsin are ...
Which of the following influence the release of pancreatic juice and bile: A) cholecystokinin and secretin B) secretin and gastrin C) cholecystokinin and gastrin D) ... The journey of chyme through the small intestine takes: A) 10-12 hours B) 8-10 hours C) 6-8 hours D) 2-4 hours E) 3-6 hours.
Study with Quizlet and memorize flashcards containing terms like Two hormones that promote the release of bile and pancreatic juice into the small intestine are _____. somatostatin; secretin secretin; cholecystokinin (CCK) gastric inhibitory peptide (GIP); histamine gastrin; histamine, The hormone responsible for promoting the release of pepsinogens, mucus, and hydrochloric acid in the stomach ...
Study with Quizlet and memorize flashcards containing terms like Which of the following influence the release of pancreatic juice and bile: 2) _____ A) cholecystokinin and secretin B) secretin and gastrin C) cholecystokinin and gastrin D) rennin and cholecystokinin E) gastrin and rennin, The process by which larger molecules or structures are built up from smaller ones is called: 3) _____ A ...