Section 23: The Reproductive System
Anatomy of the sperm producing and conducting organs, learning objectives.
By the end of this section, you will be able to:
- Describe the structure and function of sperm producing and conducting organs
- Describe the structure and function of the sperm cell
- Explain the events during spermatogenesis that produce haploid sperm from diploid cells
- Identify the importance of testosterone in the function of sperm producing and conducting organs
Unique for its role in human reproduction, a gamete is a specialized sex cell carrying 23 chromosomes—one half the number in body cells. Those with sperm producing and conducting (SPC) organs possess a gamete called a sperm cell (or spermatozoon), while those with egg producing and conducting (EPC) organs have a gamete known as an oocyte (or egg). At fertilization, the chromosomes in the sperm combine with the chromosomes in an oocyte. The function of SPC organs is to produce sperm and transfer them outside of the body, potentially into the egg conducting organs of another individual. The paired testes are a crucial component in this process, as they produce both sperm and androgens, the hormones that support the physiological function of SPC organs. In humans, the most important androgen for those with SPC organs is testosterone. Several accessory organs and ducts aid the process of sperm maturation and transport the sperm and other seminal components to the penis, which delivers sperm to the egg conducting organs. In this section, we examine each of these different structures, and discuss the process of sperm production and transport.

Figure 1. Click for a larger image. The sperm producing and conducting organs include the testes, the epididymides, the penis, and the ducts and glands that produce and carry semen. Sperm exit the scrotum through the ductus deferens, which is bundled in the spermatic cord. The seminal vesicles and prostate gland add fluids to the sperm to create semen.
The testes are located in a skin-covered, highly pigmented, muscular sack called the scrotum that extends from the body behind the penis. This location is important in sperm production, which occurs within the testes, and proceeds more efficiently when the testes are kept 2 to 4°C below core body temperature.
The dartos muscle makes up the subcutaneous muscle layer of the scrotum. It continues internally to make up the scrotal septum, a wall that divides the scrotum into two compartments, each housing one testis. Descending from the internal oblique muscle of the abdominal wall are the two cremaster muscles, which cover each testis like a muscular net. By contracting simultaneously, the dartos and cremaster muscles can elevate the testes in cold weather (or water), moving the testes closer to the body and decreasing the surface area of the scrotum to retain heat. Alternatively, as the environmental temperature increases, the scrotum relaxes, moving the testes farther from the body core and increasing scrotal surface area, which promotes heat loss. Externally, the scrotum has a raised medial thickening on the surface called the raphae.

Figure 2. This anterior view shows the structures of the scrotum and testes.
The testes (singular = testis) are the gonads —that is, the sperm producing organs. They produce both sperm and androgens, such as testosterone, and are active starting at puberty.

Figure 3. This sagittal view shows the seminiferous tubules, the site of sperm production. Formed sperm are transferred to the epididymis, where they mature. They leave the epididymis during an ejaculation via the ductus deferens.
Paired ovals, the testes are each approximately 4 to 5 cm in length and are housed within the scrotum. They are surrounded by two distinct layers of protective connective tissue. The outer tunica vaginalis is a serous membrane that has both a parietal and a thin visceral layer. Beneath the tunica vaginalis is the tunica albuginea, a tough, white, dense connective tissue layer covering the testis itself. Not only does the tunica albuginea cover the outside of the testis, it also invaginates to form septa that divide the testis into 300 to 400 structures called lobules. Within the lobules, sperm develop in structures called seminiferous tubules. During the seventh month of the developmental period of a fetus, each testis moves through the abdominal musculature to descend into the scrotal cavity. This is called the “descent of the testis.” Cryptorchidism is the clinical term used when one or both of the testes fail to descend into the scrotum prior to birth.
The tightly coiled seminiferous tubules form the bulk of each testis. They are composed of developing sperm cells surrounding a lumen, the hollow center of the tubule, where formed sperm are released into the duct system of the testis. Specifically, from the lumens of the seminiferous tubules, sperm move into the straight tubules (or tubuli recti), and from there into a fine meshwork of tubules called the rete testes. Sperm leave the rete testes, and the testis itself, through the 15 to 20 efferent ductules that cross the tunica albuginea.
Inside the seminiferous tubules are six different cell types. These include supporting cells called sustentacular cells, as well as five types of developing sperm cells called germ cells. Germ cell development progresses from the basement membrane—at the perimeter of the tubule—toward the lumen. Let’s look more closely at these cell types.

Sustentacular Cells
Surrounding all stages of the developing sperm cells are elongate, branching Sustentacular cells (Sertoli cells). These are a type of supporting cell that is typically found in epithelial tissue. Sustentacular cells secrete signaling molecules that promote sperm production and can control whether germ cells live or die. They extend physically around the germ cells from the peripheral basement membrane of the seminiferous tubules to the lumen. Tight junctions between these sustentacular cells create the blood–testis barrier , which keeps bloodborne substances from reaching the germ cells and, at the same time, keeps surface antigens on developing germ cells from escaping into the bloodstream and prompting an autoimmune response.
The least mature cells, the spermatogonia (singular = spermatogonium), line the basement membrane inside the tubule. Spermatogonia are the stem cells of the testis, which means that they are still able to differentiate into a variety of different cell types throughout adulthood. Spermatogonia divide to produce primary and secondary spermatocytes, then spermatids, which finally produce formed sperm. The process that begins with spermatogonia and concludes with the production of sperm is called spermatogenesis .
Spermatogenesis
As just noted, spermatogenesis occurs in the seminiferous tubules that form the bulk of each testis. The process begins at puberty, after which time sperm are produced constantly throughout a person’s life. One production cycle, from spermatogonia through formed sperm, takes approximately 64 days. A new cycle starts approximately every 16 days, although this timing is not synchronous across the seminiferous tubules. Sperm counts—the total number of sperm a man produces—slowly decline after age 35, and some studies suggest that smoking can lower sperm counts irrespective of age.
The process of spermatogenesis begins with mitosis of the diploid spermatogonia. Because these cells are diploid (2 n ), they each have a complete copy of the father’s genetic material, or 46 chromosomes. However, mature gametes are haploid (1 n ), containing 23 chromosomes—meaning that daughter cells of spermatogonia must undergo a second cellular division through the process of meiosis.

Figure 4. (a) Mitosis of a spermatogonial stem cell involves a single cell division that results in two identical, diploid daughter cells (spermatogonia to primary spermatocyte). Meiosis has two rounds of cell division: primary spermatocyte to secondary spermatocyte, and then secondary spermatocyte to spermatid. This produces four haploid daughter cells (spermatids). (b) In this electron micrograph of a cross-section of a seminiferous tubule from a rat, the lumen is the light-shaded area in the center of the image. The location of the primary spermatocytes is near the basement membrane, and the early spermatids are approaching the lumen (tissue source: rat). EM × 900. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Two identical diploid cells result from spermatogonia mitosis. One of these cells remains a spermatogonium, and the other becomes a primary spermatocyte , the next stage in the process of spermatogenesis. As in mitosis, DNA is replicated in a primary spermatocyte, and the cell undergoes cell division to produce two cells with identical chromosomes. Each of these is a secondary spermatocyte. Now a second round of cell division occurs in both of the secondary spermatocytes, separating the chromosome pairs. This second meiotic division results in a total of four cells with only half of the number of chromosomes. Each of these new cells is a spermatid . Although haploid, early spermatids look very similar to cells in the earlier stages of spermatogenesis, with a round shape, central nucleus, and large amount of cytoplasm. A process called spermiogenesis transforms these early spermatids, reducing the cytoplasm, and beginning the formation of the parts of a true sperm. The fifth stage of germ cell formation—spermatozoa, or formed sperm—is the end result of this process, which occurs in the portion of the tubule nearest the lumen. Eventually, the sperm are released into the lumen and are moved along a series of ducts in the testis toward a structure called the epididymis for the next step of sperm maturation.
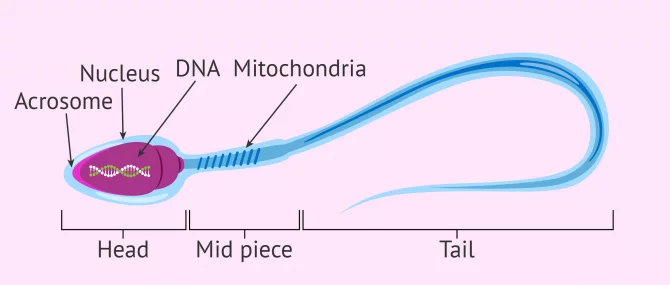
Structure of Formed Sperm
Sperm are smaller than most cells in the body; in fact, the volume of a sperm cell is 85,000 times less than that of the oocyte. Approximately 100 to 300 million sperm are produced each day, whereas typically only one oocyte is released via ovulation per month. As is true for most cells in the body, the structure of sperm cells speaks to their function. Sperm have a distinctive head, mid-piece, and tail region. The head of the sperm contains the extremely compact haploid nucleus with very little cytoplasm. These qualities contribute to the overall small size of the sperm (the head is only 5 μ m long). A structure called the acrosome covers most of the head of the sperm cell as a “cap” that is filled with lysosomal enzymes important for preparing sperm to participate in fertilization. Tightly packed mitochondria fill the mid-piece of the sperm. ATP produced by these mitochondria will power the flagellum, which extends from the neck and the mid-piece through the tail of the sperm, enabling it to move the entire sperm cell. The central strand of the flagellum, the axial filament, is formed from one centriole inside the maturing sperm cell during the final stages of spermatogenesis.

Figure 5. Sperm cells are divided into a head, containing DNA; a mid-piece, containing mitochondria; and a tail, providing motility. The acrosome is oval and somewhat flattened.
Sperm Transport
To fertilize an egg, sperm must be moved from the seminiferous tubules in the testes, through the epididymis, and—later during ejaculation—along the length of the penis and potentially out into the egg conducting organs.
Role of the Epididymis
From the lumen of the seminiferous tubules, the immotile sperm are surrounded by testicular fluid and moved to the epididymis (plural = epididymides), a coiled tube attached to the testis where newly formed sperm continue to mature. Though the epididymis does not take up much room in its tightly coiled state, it would be approximately 6 m (20 feet) long if straightened. It takes an average of 12 days for sperm to move through the coils of the epididymis, with the shortest recorded transit time in humans being one day. Sperm enter the head of the epididymis and are moved along predominantly by the contraction of smooth muscles lining the epididymal tubes. As they are moved along the length of the epididymis, the sperm further mature and acquire the ability to move under their own power. Once inside the egg conducting organs, they will use this ability to move independently toward the unfertilized egg. The more mature sperm are then stored in the tail of the epididymis (the final section) until ejaculation occurs.
Duct System
During ejaculation, sperm exit the tail of the epididymis and are pushed by smooth muscle contraction to the ductus deferens (also called the vas deferens). The ductus deferens is a thick, muscular tube that is bundled together inside the scrotum with connective tissue, blood vessels, and nerves into a structure called the spermatic cord . Because the ductus deferens is physically accessible within the scrotum, surgical sterilization to interrupt sperm delivery can be performed by cutting and sealing a small section of the ductus (vas) deferens. This procedure is called a vasectomy, and it is an effective form of birth control. Although it may be possible to reverse a vasectomy, clinicians consider the procedure permanent.
Practice Question
Watch this video to learn about a vasectomy. As described in this video, a vasectomy is a procedure in which a small section of the ductus (vas) deferens is removed from the scrotum. This interrupts the path taken by sperm through the ductus deferens. If sperm do not exit through the vas deferens, in what region of the testis do they remain?
From each epididymis, each ductus deferens extends superiorly into the abdominal cavity through the inguinal canal in the abdominal wall. From here, the ductus deferens continues posteriorly to the pelvic cavity, ending posterior to the bladder where it dilates in a region called the ampulla (meaning “flask”).
Sperm make up only 5 percent of the final volume of semen , the thick, milky fluid that the male ejaculates. The bulk of semen is produced by three critical accessory glands of the male reproductive system: the seminal vesicles, the prostate, and the bulbourethral glands.
Seminal Vesicles
As sperm pass through the ampulla of the ductus deferens at ejaculation, they mix with fluid from the associated seminal vesicle . The paired seminal vesicles are glands that contribute approximately 60 percent of the semen volume. Seminal vesicle fluid contains large amounts of fructose, which is used by the sperm mitochondria to generate ATP to allow movement through the egg conducting organs.
The fluid, now containing both sperm and seminal vesicle secretions, next moves into the associated ejaculatory duct , a short structure formed from the ampulla of the ductus deferens and the duct of the seminal vesicle. The paired ejaculatory ducts transport the seminal fluid into the next structure, the prostate gland.
Prostate Gland
As shown in Figure 1, the centrally located prostate gland sits anterior to the rectum at the base of the bladder surrounding the prostatic urethra (the portion of the urethra that runs within the prostate). About the size of a walnut, the prostate is formed of both muscular and glandular tissues. It excretes an alkaline, milky fluid to the passing seminal fluid—now called semen—that is critical to first coagulate (thicken) and then de-coagulate the semen following ejaculation. The temporary thickening of semen helps retain it within the female reproductive tract, providing time for sperm to utilize the fructose provided by seminal vesicle secretions. When the semen regains its fluid state, sperm can then pass farther into the egg conducting organs.
The prostate normally doubles in size during puberty. At approximately age 25, it gradually begins to enlarge again. This enlargement does not usually cause problems; however, abnormal growth of the prostate, or benign prostatic hyperplasia (BPH), can cause constriction of the urethra as it passes through the middle of the prostate gland, leading to a number of lower urinary tract symptoms, such as a frequent and intense urge to urinate, a weak stream, and a sensation that the bladder has not emptied completely. By age 60, approximately 40 percent of men have some degree of BPH. By age 80, the number of affected individuals has jumped to as many as 80 percent. Treatments for BPH attempt to relieve the pressure on the urethra so that urine can flow more normally. Mild to moderate symptoms are treated with medication, whereas severe enlargement of the prostate is treated by surgery in which a portion of the prostate tissue is removed.
Another common disorder involving the prostate is prostate cancer. According to the Centers for Disease Control and Prevention (CDC), prostate cancer is the second most common cancer in those with SPC organs. However, some forms of prostate cancer grow very slowly and thus may not ever require treatment. Aggressive forms of prostate cancer, in contrast, involve metastasis to vulnerable organs like the lungs and brain. There is no link between BPH and prostate cancer, but the symptoms are similar. Prostate cancer is detected by a medical history, a blood test, and a rectal exam that allows physicians to palpate the prostate and check for unusual masses. If a mass is detected, the cancer diagnosis is confirmed by biopsy of the cells.
Bulbourethral Glands
The final addition to semen is made by two bulbourethral glands (or Cowper’s glands) that release a thick, salty fluid that lubricates the end of the urethra and the vagina, and helps to clean urine residues from the penile urethra. The fluid from these accessory glands is released after becoming sexually aroused, and shortly before the release of the semen. It is therefore sometimes called pre-ejaculate. It is important to note that, in addition to the lubricating proteins, it is possible for bulbourethral fluid to pick up sperm already present in the urethra, and therefore it may be able to cause pregnancy.
Practice Question
Watch this video to explore the SPC organs and the path of sperm , which starts in the testes and ends as the sperm leave the penis through the urethra. Where are sperm deposited after they leave the ejaculatory duct?
The penis is the male organ of copulation (sexual intercourse). It is flaccid for non-sexual actions, such as urination, and turgid and rod-like with sexual arousal. When erect, the stiffness of the organ allows it to penetrate into the vagina and deposit semen.

Figure 6. Three columns of erectile tissue make up most of the volume of the penis.
The shaft of the penis surrounds the urethra. The shaft is composed of three column-like chambers of erectile tissue that span the length of the shaft. Each of the two larger lateral chambers is called a corpus cavernosum (plural = corpora cavernosa). Together, these make up the bulk of the penis. The corpus spongiosum , which can be felt as a raised ridge on the erect penis, is a smaller chamber that surrounds the spongy, or penile, urethra. The end of the penis, called the glans penis , has a high concentration of nerve endings, resulting in very sensitive skin that influences the likelihood of ejaculation. The skin from the shaft extends down over the glans and forms a collar called the prepuce (or foreskin). The foreskin also contains a dense concentration of nerve endings, and both lubricate and protect the sensitive skin of the glans penis. A surgical procedure called circumcision, often performed for religious or social reasons, removes the prepuce, typically within days of birth.
Both sexual arousal and REM sleep (during which dreaming occurs) can induce an erection. Penile erections are the result of vasocongestion, or engorgement of the tissues because of more arterial blood flowing into the penis than is leaving in the veins. During sexual arousal, nitric oxide (NO) is released from nerve endings near blood vessels within the corpora cavernosa and spongiosum. Release of NO activates a signaling pathway that results in relaxation of the smooth muscles that surround the penile arteries, causing them to dilate. This dilation increases the amount of blood that can enter the penis and induces the endothelial cells in the penile arterial walls to also secrete NO and perpetuate the vasodilation. The rapid increase in blood volume fills the erectile chambers, and the increased pressure of the filled chambers compresses the thin-walled penile venules, preventing venous drainage of the penis. The result of this increased blood flow to the penis and reduced blood return from the penis is erection. Depending on the flaccid dimensions of a penis, it can increase in size slightly or greatly during erection, with the average length of an erect penis measuring approximately 15 cm.
Disorders of SPC ORGANS: Erectile dysfunction (ED)
Erectile dysfunction (ED) is a condition in which there is difficulty either initiating or maintaining an erection. The combined prevalence of minimal, moderate, and complete ED is approximately 40 percent in people at age 40, and reaches nearly 70 percent by 70 years of age. In addition to aging, ED is associated with diabetes, vascular disease, psychiatric disorders, prostate disorders, the use of some drugs such as certain antidepressants, and problems with the testes resulting in low testosterone concentrations. These physical and emotional conditions can lead to interruptions in the vasodilation pathway and result in an inability to achieve an erection.
Recall that the release of NO induces relaxation of the smooth muscles that surround the penile arteries, leading to the vasodilation necessary to achieve an erection. To reverse the process of vasodilation, an enzyme called phosphodiesterase (PDE) degrades a key component of the NO signaling pathway called cGMP. There are several different forms of this enzyme, and PDE type 5 is the type of PDE found in the tissues of the penis. Scientists discovered that inhibiting PDE5 increases blood flow, and allows vasodilation of the penis to occur.
PDEs and the vasodilation signaling pathway are found in the vasculature in other parts of the body. In the 1990s, clinical trials of a PDE5 inhibitor called sildenafil were initiated to treat hypertension and angina pectoris (chest pain caused by poor blood flow through the heart). The trial showed that the drug was not effective at treating heart conditions, but many people experienced erection and priapism (erection lasting longer than 4 hours). Because of this, a clinical trial was started to investigate the ability of sildenafil to promote erections in those suffering from ED. In 1998, the FDA approved the drug, marketed as Viagra ® . Since approval of the drug, sildenafil and similar PDE inhibitors now generate over a billion dollars a year in sales, and are reported to be effective in treating approximately 70 to 85 percent of cases of ED. Importantly, people with health problems—especially those with cardiac disease taking nitrates—should avoid Viagra or talk to their physician to find out if they are a candidate for the use of this drug, as deaths have been reported for at-risk users.
Testosterone
Testosterone, an androgen, is a steroid hormone produced by Interstitial cells (Leydig cells). The term “interstitial” reflects their location between the seminiferous tubules in the testes. In embryos, testosterone is secreted by Interstitial cells by the seventh week of development, with peak concentrations reached in the second trimester. This early release of testosterone results in the anatomical differentiation of the SPC organs. In childhood, testosterone concentrations are low. They increase during puberty, activating characteristic physical changes and initiating spermatogenesis.
Functions of Testosterone
The continued presence of testosterone is necessary to keep the SPC organs working properly, and Interstitial cells produce approximately 6 to 7 mg of testosterone per day. Testicular steroidogenesis (the manufacture of androgens, including testosterone) results in testosterone concentrations that are 100 times higher in the testes than in the circulation. Maintaining these normal concentrations of testosterone promotes spermatogenesis, whereas low levels of testosterone can lead to infertility. In addition to intra-testicular secretion, testosterone is also released into the systemic circulation and plays an important role in muscle development, bone growth, the development of secondary sex characteristics, and maintaining libido (sex drive). In those with EPC organs, the ovaries secrete small amounts of testosterone, although most is converted to estradiol. A small amount of testosterone is also secreted by the adrenal glands in both those with EPC and SPC organs.
Aging and SPC ORGANS
Declines in Interstitial cell activity can occur beginning at 40 to 50 years of age. The resulting reduction in circulating testosterone concentrations can lead to symptoms of andropause. While the reduction in androgens such as testosterone is akin to menopause in those with EPC organs, there is no clear sign—such as a lack of a menstrual period—to denote the initiation of andropause. Instead, symptoms include reporting feelings of fatigue, reduced muscle mass, depression, anxiety, irritability, loss of libido, and insomnia. A reduction in spermatogenesis resulting in lowered fertility is also reported, and sexual dysfunction can also be associated with andropausal symptoms.
Whereas some researchers believe that certain aspects of andropause are difficult to tease apart from aging in general, testosterone replacement is sometimes prescribed to alleviate some symptoms. Recent studies have shown a benefit from androgen replacement therapy on the new onset of depression in the elderly; however, other studies caution against testosterone replacement for long-term treatment of andropause symptoms, showing that high doses can sharply increase the risk of both heart disease and prostate cancer.
Chapter Review
Gametes are the reproductive cells that combine to form offspring. Organs called gonads produce the gametes, along with the hormones that regulate human reproduction. The male gametes are called sperm. Spermatogenesis, the production of sperm, occurs within the seminiferous tubules that make up most of the testis. The scrotum is the muscular sac that holds the testes outside of the body cavity.
Spermatogenesis begins with mitotic division of spermatogonia (stem cells) to produce primary spermatocytes that undergo the two divisions of meiosis to become secondary spermatocytes, then the haploid spermatids. During spermiogenesis, spermatids are transformed into spermatozoa (formed sperm). Upon release from the seminiferous tubules, sperm are moved to the epididymis where they continue to mature. During ejaculation, sperm exit the epididymis through the ductus deferens, a duct in the spermatic cord that leaves the scrotum. The ampulla of the ductus deferens meets the seminal vesicle, a gland that contributes fructose and proteins, at the ejaculatory duct. The fluid continues through the prostatic urethra, where secretions from the prostate are added to form semen. These secretions help the sperm to travel through the urethra and into the female reproductive tract. Secretions from the bulbourethral glands protect sperm and cleanse and lubricate the penile (spongy) urethra.
The penis is the organ of copulation in those with SPC organs. Columns of erectile tissue called the corpora cavernosa and corpus spongiosum fill with blood when sexual arousal activates vasodilatation in the blood vessels of the penis. Testosterone regulates and maintains the sex organs and sex drive, and induces the physical changes of puberty. Interplay between the testes and the endocrine system precisely control the production of testosterone with a negative feedback loop.
Answer the question(s) below to see how well you understand the topics covered in the previous section.
Critical Thinking Questions
- Briefly explain why mature gametes carry only one set of chromosomes.
- What special features are evident in sperm cells but not in somatic (body) cells, and how do these specializations function?
- What do each of the three accessory glands of the SPC organs contribute to the semen?
- Describe how penile erection occurs.
- While anabolic steroids (synthetic testosterone) bulk up muscles, they can also affect testosterone production in the testis. Using what you know about negative feedback, describe what would happen to testosterone production in the testis if a someone takes large amounts of synthetic testosterone.
- Two gametes (sperm and oocyte) must combine during fertilization to produce a zygote that has a complete set of chromosomes and is the first cell of a new individual.
- Unlike somatic cells, sperm are haploid. They also have very little cytoplasm. They have a head with a compact nucleus covered by an acrosome filled with enzymes, and a mid-piece filled with mitochondria that power their movement. They are motile because of their tail, a structure containing a flagellum, which is specialized for movement.
- The three accessory glands make the following contributions to semen: the seminal vesicle contributes about 60 percent of the semen volume, with fluid that contains large amounts of fructose to power the movement of sperm; the prostate gland contributes substances critical to sperm maturation; and the bulbourethral glands contribute a thick fluid that lubricates the ends of the urethra and the vagina and helps to clean urine residues from the urethra.
- During sexual arousal, nitric oxide (NO) is released from nerve endings near blood vessels within the corpora cavernosa and corpus spongiosum. The release of NO activates a signaling pathway that results in relaxation of the smooth muscles that surround the penile arteries, causing them to dilate. This dilation increases the amount of blood that can enter the penis, and induces the endothelial cells in the penile arterial walls to secrete NO, perpetuating the vasodilation. The rapid increase in blood volume fills the erectile chambers, and the increased pressure of the filled chambers compresses the thin-walled penile venules, preventing venous drainage of the penis. An erection is the result of this increased blood flow to the penis and reduced blood return from the penis.
- Testosterone production by the body would be reduced if someone with SPC organs were taking anabolic steroids. This is because the hypothalamus responds to rising testosterone levels by reducing its secretion of GnRH, which would in turn reduce the anterior pituitary’s release of LH, finally reducing the manufacture of testosterone in the testes.
blood–testis barrier: tight junctions between Sertoli cells that prevent bloodborne pathogens from gaining access to later stages of spermatogenesis and prevent the potential for an autoimmune reaction to haploid sperm
bulbourethral glands: (also, Cowper’s glands) glands that secrete a lubricating mucus that cleans and lubricates the urethra prior to and during ejaculation
corpus cavernosum: either of two columns of erectile tissue in the penis that fill with blood during an erection
corpus spongiosum: (plural = corpora cavernosa) column of erectile tissue in the penis that fills with blood during an erection and surrounds the penile urethra on the ventral portion of the penis
ductus deferens: (also, vas deferens) duct that transports sperm from the epididymis through the spermatic cord and into the ejaculatory duct; also referred as the vas deferens
ejaculatory duct: duct that connects the ampulla of the ductus deferens with the duct of the seminal vesicle at the prostatic urethra
epididymis: (plural = epididymides) coiled tubular structure in which sperm start to mature and are stored until ejaculation
gamete: haploid reproductive cell that contributes genetic material to form an offspring
glans penis: bulbous end of the penis that contains a large number of nerve endings
gonadotropin-releasing hormone (GnRH): hormone released by the hypothalamus that regulates the production of follicle-stimulating hormone and luteinizing hormone from the pituitary gland
gonads: reproductive organs (testes in those with SPC organs, ovaries in those with EPC organs) that produce gametes and reproductive hormones
inguinal canal: opening in abdominal wall that connects the testes to the abdominal cavity
Interstitial cells: cells between the seminiferous tubules of the testes that produce testosterone
penis: organ of copulation in those with SPC organs
prepuce: (also, foreskin) flap of skin that forms a collar around, and thus protects and lubricates, the glans penis; also referred as the foreskin
prostate gland: doughnut-shaped gland at the base of the bladder surrounding the urethra and contributing fluid to semen during ejaculation
scrotum: external pouch of skin and muscle that houses the testes
semen: ejaculatory fluid composed of sperm and secretions from the seminal vesicles, prostate, and bulbourethral glands
seminal vesicle: gland that produces seminal fluid, which contributes to semen
seminiferous tubules: tube structures within the testes where spermatogenesis occurs
sperm: (also, spermatozoon) male gamete
spermatic cord: bundle of nerves and blood vessels that supplies the testes; contains ductus deferens
spermatid: immature sperm cells produced by meiosis II of secondary spermatocytes
spermatocyte: cell that results from the division of spermatogonium and undergoes meiosis I and meiosis II to form spermatids
spermatogenesis: formation of new sperm, occurs in the seminiferous tubules of the testes
spermatogonia: (singular = spermatogonium) diploid precursor cells that become sperm
spermiogenesis: transformation of spermatids to spermatozoa during spermatogenesis
Sustentacular cells: cells that support germ cells through the process of spermatogenesis
testes: (singular = testis) sperm producing organs
- Anatomy & Physiology. Provided by : OpenStax CNX. Located at : http://cnx.org/contents/[email protected] . License : CC BY: Attribution . License Terms : Download for free at http://cnx.org/contents/[email protected]
How sperm meets egg: a journey from production to fertilization
Many wonder what the sperm ´s journey is like from ejaculation to fertilization. The ultimate goal of a sperm is to fertilize the egg cell.
However, the journey of the sperm to get to the egg is not an easy one. To reach the egg cell, the sperm has to go through a long and difficult journey that can take from thirty minutes to several hours .
For this reason, fertilization needs a large number of motile spermatozoa for at least one of them to be able to overcome all barriers. Firstly for the sperm to get to the egg, and then to fertilize the egg.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1. How the sperm meets the egg
- 2. Route from the testicle to the urethra
- 2.1. Changes in the sperm
- 3. The journey through the female reproductive system
- 3.1. What barriers do spermatozoa have to cross?
- 3.2. The sperm´s arrival at the Fallopian tubes.
- 3.3. Final stage of the spermatozoon: acrosome reaction
- 4. FAQs from users
- 4.1. How long does it take from sperm production to ejaculation?
- 4.2. How can ovulation be calculated so that the sperm and egg meet?
- 4.3. How long can a sperm live in the female reproductive tract?
- 4.4. How many sperm make it to the egg?
- 4.5. How long does it take sperm to reach the egg?
- 4.6. After sperm meets egg, how long until implantation?
- 4.7. Where do the sperm cells pass through on their way to the egg?
- 4.8. Where does the sperm need to get to, to be able to fertilize the egg?
- 5. Recommended reading
- 6. References
- 7. Authors and contributors
How the sperm meets the egg
Colloquially,the path to fertilization we understand as a race in which only the best sperm will be able to reach the finish line and win the prize. Effectively, it is something like this: many spermatozoa start the race, but only one will fertilize the egg.
The route of the sperm to the egg can be divided into two major stages:
- Male reproductive system: the journey of sperm in the male body is from the testicles to the outside world.
- Female reproductive system: from the vagina, where semen is deposited, to the Fallopian tubes, where the egg is found.
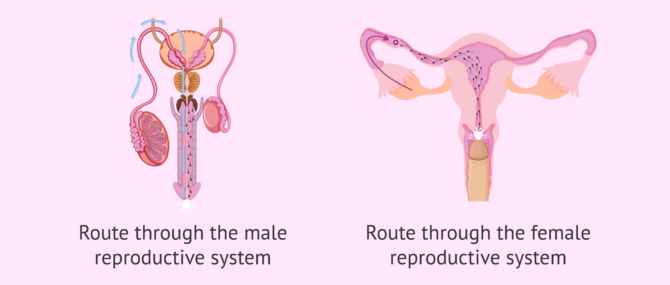
It should not be forgotten that during these two phases of the journey the sperm meet certain obstacles. To follow, we discuss what they are.
Route from the testicle to the urethra
It takes about 90 days for spermatozoa to develop and acquire the necessary maturation before they can be expelled in an ejaculation.The birth of spermatozoa takes place in the seminiferous tubules of the testes. They subsequently pass to the epididymis.
The seminiferous tubules are the internal structures of the testicle where sperm are made. The epididymis is a long structure that connects the testicle and the vas deferens.
At the moment of intercourse, a large quantity of sperm (about 250 million) leave the epididymis and pass through the vas deferens and the urethra. Along the way, the sperm are bathed in fluids released from the seminal vesicles and the prostate. In this way, the semen, the mix of sperm and fluids, is formed.
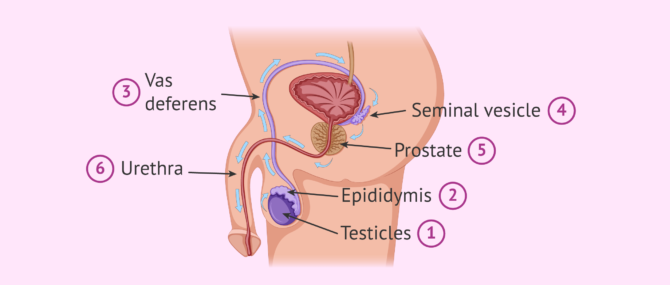
The main function of these seminal fluids is to make is possible for the sperm to enter into the vagina. Sperm will shoot out of the urethra through the penis until they enter the female reproductive tract , specifically the vagina.
Changes in the sperm
During this journey from the testicle to the outside, the sperm acquire the correct shape and structure to allow fertilization of the egg. The changes that occur at this final stage of sperm maturation are:
- DNA compaction to allow the head (where the DNA is stored) to be as small as possible and therefore move better. This also helps it to pass through the zona pellucida (egg shell).
- The tail acquires the perfect design so the sperm have great speed and resistance.
- The middle piece has a large number of mitochondria for high energy production. This gives the spermatozoon great efficiency in energy usage.
If you wish to continue reading information about what the spermatozoon cell is like, we suggest you visit this article: How are spermatazoa formed
The journey through the female reproductive system
In the process of ejaculation, sperm cells leave the man and enter the vagina. This is where the sperm cells begin the second part of their journey to fertilization.
During this second part of the journey the sperm again encounter an large number of obstacles. These obstacles and barriers can hinder the sperms arrival at the Fallopian tubes, where the egg is waiting.
There is a distance of between 15 and 18 cm and time is of the essence. Sperm cannot afford to delay, since the egg, once it has left the ovary (i.e., after ovulation ), has a half-life of about 24 hours. The survival time of the egg is short compared to that of the sperm. Sperm can live between 2 and 5 days in the female reproductive tract.

After ejaculation, the race of the sperm cells begins. It is a race not only of speed but also of endurance . Defective sperm and/or those with poor motility will fall by the wayside.

What barriers do spermatozoa have to cross?
Some obstacles, or barriers, encountered by sperm are as follows:
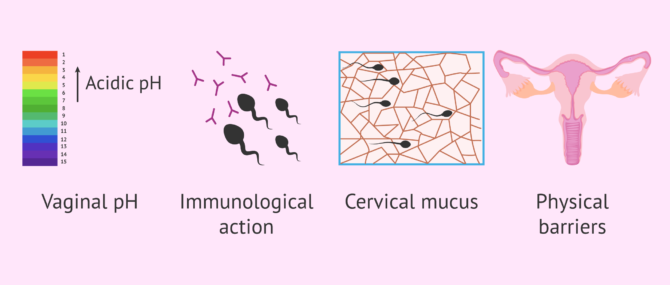
However, it is not all difficulties in the journey of the sperm. The egg tries to pave the way for the sperm by releasing molecules and sending signals. The fallopian tubes and uterus exert a suction force through rhythmic contractions and the cervical mucus becomes less dense allowing the sperm to swim better.
For its part, the seminal fluid that accompanies the sperm neutralizes the pH and provides sugars to the sperm. This fluid also serves as a protective shield against the woman´s white blood cells.
The sperm´s arrival at the Fallopian tubes.
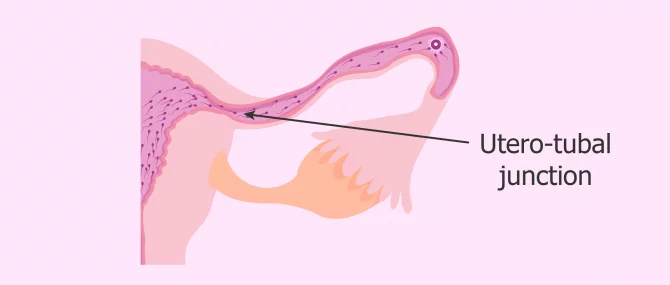
Once the vaginal, cervical and uterine barriers have been overcome, we encounter the narrowest part of the course: the uterotubal junction . Only a few thousand of the average 250 million spermatozoa in freshly ejaculated semen reach this point.
Along the way, the strongest spermatozoa, i.e. those that have been able to overcome the female obstacles, acquire an extraordinary ability: the ability to fertilize . This is known as sperm hyperactivation . From this moment on, its tail moves with much more force and energy, allowing a vigorous movement that helps it arrive at the egg.
Once they reach the fallopian tubes, many sperm remain attached to the tube walls, exhausted and unable to continue their journey.
At this point, few sperm are left in the race, as the vast majority have been lost along the way. Of the few dozen sperm that remain before the egg's watchful eye, only one will make it through the thick doorway to the egg: the zona pellucida.
The chosen sperm, the strongest and most capable one, upon contact with the zona pellucida, initiates the so-called acrosome reaction .
Final stage of the spermatozoon: acrosome reaction
As mentioned above, when the most able sperm has reached the egg, the acrosome reaction takes place. This is the release of the contents of the acrosome, which is composed of a series of enzymes. The purpose of this enzymatic release is to weaken the zona pellucida of the ovum and facilitate penetration.
The acrosome is a structure located in the head of the sperm. It serves as a reservoir for enzymes and other substances that the sperm needs to pass through the zona pellucida.
This reaction "wakes up" the egg, which releases cortical granules , organelles that prevent any other sperm from penetrating. It is as if the ovum plants a flag indicating to the rest of the spermatozoa around it that it has already been conquered by the winning spermatozoa and, therefore, that the doors of its kingdom are closed.
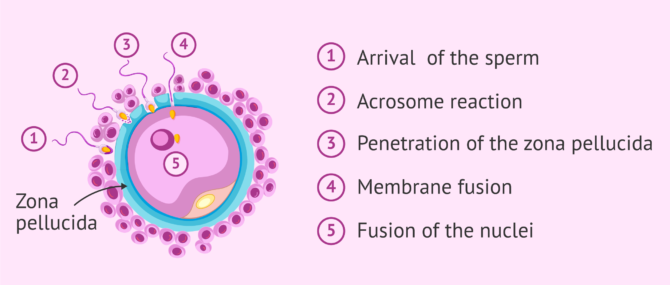
Once the sperm penetrates the oocyte, their two nuclei fuse. This is what we know as fertilization . If you want to know the details about how the sperm enters the egg and how the new being is formed, you can read this article: The steps of fertilization in humans.
We're already 773!
Join our inviTRA community
FAQs from users
How long does it take from sperm production to ejaculation.
Spermatogenesis is the process whereby male reproductive cells are formed, from the immature ones, spermatogonia, until the mature ones, spermatozoa. This complicated process occurs within the seminiferous tubule in the testis and takes about 64-72 days.
Once spermatozoa (sperm cells) have been produced, they leave the testis and travel to the epididymis, where they will acquire the necessary motility in a process that lasts 10 days approximately. Spermatozoa will be stored in the epididymis until they are expelled with ejaculation. When ejaculation starts, sperm travel through the vas deferends and mixes with the seminal fluid that originates in the secretory glands, creating what we all know as semen . Finally, it is expelled through the urethra.
How can ovulation be calculated so that the sperm and egg meet?
It can be calculated by measuring the daily basal temperature and by performing a urine LH test.
How long can a sperm live in the female reproductive tract?
Once ejaculation occurs and the sperm are released into the vagina, they have a half-life of 2 to 5 days. The stronger ones will survive longer. The weaker ones will die on the way. After fertilization, the dead spermatozoa and the live ones that have remained unable to fertilize the egg will be eliminated by phagocytosis (the body's own system of neutralization and elimination of substances).
How many sperm make it to the egg?
To answer this question, we will split the answer into various figures, each one corresponding to a stage in the journey:
- There are approximately 200-250 million sperm in each ejaculation, but only about 2 million make it to the cervix.
- Once there, out of the 2 million sperm entering the cervix, only about 1 million are able to make it to the uterus.
- Out of the 1 million that enter the uterus, only 10,000 are able to travel to the top of this organ.
- Out of the 10,000 that survive at this point, only half of them travel in the right direction, that is, toward the egg cell.
- Out of the approximately 5,000 sperm that enter the utero-tubal junction, about 1,000 get inside the Fallopian tube.
- Finally, out of the 1,000 that enter the tube, it is estimated that only 200 make it to the egg.
However, in the end, only 1 sperm out of the 200 that reach the egg is able to penetrate and fertilize it.
How long does it take sperm to reach the egg?
There is no set time, since the spermatozoa with the best quality, that is, with great ability to overcome obstacles and great strength of movement, will be able to reach the egg in just half an hour. However, there will be others that will need about two days to cross the entire female reproductive tract.
After sperm meets egg, how long until implantation?
Implantation occurs approximately within 3-7 days after fertilization, as the fertilized egg cell has to travel from the point where it was fertilized to the point where it implants. It depends on how high the point where they meet in the Fallopian tube is. For instance, if they meet high in the tube, it will take about 7 days.
Related stories: What Are the First Signs & Symptoms of Embryo Implantation?
Where do the sperm cells pass through on their way to the egg?
As mentioned above, they must first pass through the male reproductive tract and then, after ejaculation, through the female reproductive tract. In the first part of the journey, they leave the testicle and pass through the epididymis, the vas deferens and the urethra. During this part, they are impregnated with secretions from the prostate and seminal vesicle.
In the second part of the course, the spermatozoa pass from the vagina, where they are deposited, to the cervix. Subsequently, they pass through the uterus and reach the fallopian tubes, where the egg is found or where they wait for it to arrive, in case ovulation has not yet occurred.
Where does the sperm need to get to, to be able to fertilize the egg?
The sperm has to reach the fallopian tubes, where the egg is waiting. Once there, it will be able to fuse with it and give rise to the embryo. Subsequently, the embryo will leave the fallopian tubes, reach the uterus and implant in the endometrium of the uterine cavity. This is the beginning of pregnancy.
Recommended reading
The final goal of this whole journey of the sperm is to meet the egg, fuse with it and allow the birth of a new cell. This cell, after about nine months of successive divisions and processes of differentiation and specialization, will give rise to the future baby.
If you want to know more information about what happens after fertilization, we recommend reading this article: Pregnancy stages month by month
If you are interested in knowing more about the hormones responsible for sperm formation, you can visit this link: Male hormone check .
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
Austin CR. Observations on the penetration of the sperm in the mammalian egg. Aust J Sci Res B. 1951;4(4):581–596.
Bennett M. Shapiro. The existential decision of a sperm, Cell 49, no. 3 (May 1987): 293-94, esp. 293.
Chang MC. Fertilizing capacity of spermatozoa deposited into the fallopian tubes. Nature. 1951;168(4277):697–698 ( View )
Choza J. (1991): Antropología de la Sexualidad. Ed. Rialp. Madrid, 1.ª Edición ( View )
J Clin Invest. (2010). Fertilization: a sperm’s journey to and interaction with the oocyte. Research Institute for Microbial Diseases, Osaka University, Osaka, Japan. School of Biological and Biomedical Sciences, Durham University, United Kingdom. 120(4) 984–994 ( View )
Lennart Nilsson, A portrait of the sperm. In: The functional anatomy of the spermatozoan, ed. Bjorn A. Afzelius (New York: Pergamon, 1975), 79-82.
Martin E. The egg and the sperm: how science has constructed a romance-based on stereotypical male-female roles. “Signs”. Vol. 16. No. 3 (Spring, 1991), pp. 485-501. Published by: The University of Chicago Press ( View )
Stein KK, Primakoff P, Myles D. Sperm-egg fusion: events at the plasma membrane. J Cell Sci. 2004; 117(Pt 26):6269–6274 ( View )
Paul M. Wassarman, The biology and chemistry of fertilization, Science 235, No. 4788 (January 30, 1987): 553-60, esp. 554 ( View )
Paul M. Wassarman, Fertilization in mammals, Scientific American 259, no. 6 (December 1988): 78-84, esp. 78, 84
FAQs from users: 'How long does it take from sperm production to ejaculation?' , 'How can ovulation be calculated so that the sperm and egg meet?' , 'How long can a sperm live in the female reproductive tract?' , 'How many sperm make it to the egg?' , 'How long does it take sperm to reach the egg?' , 'After sperm meets egg, how long until implantation?' , 'How does it feel when sperm meets the egg?' , 'How long after IUI does sperm meet egg?' , 'Can sperm meet egg before ovulation?' , 'Where do the sperm cells pass through on their way to the egg?' , 'Where does the sperm go when you have a vasectomy?' , 'Where does the sperm need to get to, to be able to fertilize the egg?' , 'When pregnant, where does sperm go?' , 'When does sperm die outside the body?' , 'When does sperm leave the female body?' and 'How many sperm fertilize an egg for identical twins?' .
Authors and contributors

Find the latest news on assisted reproduction in our channels.
And when do men expel the so-called pre-ejaculatory fluid? I want to know it because then my boyfriend and I will be able to use the pull-out method more accurately. Thnxs!
Hello Katie1,
Firstly, the pull-out method, coitus interruptus , or withdrawal method is not a safe birth control method because it does not prevent you from the transmission of STDs (sexually transmitted diseases) and HIV infection (AIDs). Besides, it is actually an extremely unreliable method.
Apart from that, there are several theories about why pre-ejaculatory fluid exists, none of them proved. While some say the only function of this fluid is providing some lubrication for intercourse, others believe they protect the sperm by acting as a sort of pre-clearing of the urethra, making the environment more conductive for sperm to survive the journey and lowering the acidity. On the other hand, the function of sperm is reproduction.
I hope I have clarified your concerns,
My husband has had a vasectomy and we want to try for a baby. Is there any way we can do this without surgery?
It is possible for a man to become a father after again after a vasectomy. However, this is not possible without some kind of surgical treatment. There are different options available and you can find lots more information in our article: Pregnancy after vasectomy
I hope this helps and good luck.
Interesting article, thanks. It is very interesting that so many sperm are needed to fertilize just one egg and reading this makes me realize why!
Leave a Reply
Privacy Overview
Wellcome uses cookies.
The great sperm race., about this work, description.
What makes one sperm succeed in reaching and fertilising an egg rather than another? This documentary re-enacts the journey of a sperm using human volunteers. Using computer animated graphics the process of male ejaculation and fertilisation is illustrated. The human volunteers attempt to overcome the obstacles faced by a sperm on its way to an egg.
Publication/Creation
Physical description, contributors.
- Pacey, Allan.
- Ellington, Joanna.
- Miller, Geoffrey, 1965-
- de Jonghe, Chris.
- Travis, Alex.
Copyright note
Creator/production credits, type/technique.
- Spermatozoa
- Infertility, Male
Where to find it
Permanent link.
All about sperm
The Great Sperm Race Documentary: A Fascinating Insight into Fertilization

Short answer: The Great Sperm Race is a British documentary that explores the scientific process of fertilization. Released in 2009, it uses computer graphics to create a simulated race between sperm to reach the egg. The film includes interviews with fertility experts and couples struggling to conceive, and has been praised for its informative and accessible approach to a complex topic.
Uncovering the Secrets of Fertilization: An Overview of The Great Sperm Race Documentary
How the great sperm race documentary sheds light on the miracle of conception, a step-by-step guide to the journey of sperm: an in-depth look at the great sperm race, frequently asked questions about the great sperm race documentary – answered, up close and personal with fertility: an in-depth analysis of the great sperm race, the impact of the great sperm race documentary on fertility research and awareness.
Table of Contents
Fertilization is a complicated biological process that most people are familiar with, but few really understand. However, the Great Sperm Race documentary aims to change all of that by offering viewers an in-depth look at this fascinating process. The film, produced by the BBC, provides audiences with an insightful and entertaining overview of everything from egg production to sperm delivery.
One of the primary strengths of the Great Sperm Race documentary is its accessibility. Even if you’ve never taken a biology class or read a science book, you’ll be able to follow along with the explanations provided throughout the film. From cartoonish animations to real-life footage, there are plenty of visual aids to help explain complex concepts and provide context for what’s going on.
The documentary introduces us to key players in fertilization: the sperm and the egg. We learn how eggs develop into fully matured ova, which then travel through various stages before being released from their follicles when ovulation occurs. On the other hand, we also get an insight into how millions of sperm are produced daily in men’s bodies.
Viewers will also gain insights into sexual biology such as sex determination – masculine vs feminine traits – , what role hormones play in fertility (both male and female), conception odds (less common than most would think) etc.
What makes this documentary so engaging though is not only its informative aspects but also its comedic relief moments; many puns about swimmers caught me off my guard! Plus there’s always something inherently interesting when nature meets comedy whether it involves gags or punchlines about giant sperm wearing tiny capes en route to fertilization stardom(!).
Another important aspect covered within this documentary is eugenics relating particularly to natural selection where top-performing sperm cells are chosen naturally during reproductive processes as opposed having been selected beforehand by techniques such as artificial insemination or IVF treatment.
Overall, Uncovering the Secrets of Fertilization: An Overview of the Great Sperm Race Documentary is a fascinating, witty, and clever daw-dropping documentary that offers a closer look at one of nature’s most intriguing processes. Whether you have an interest in biology or simply enjoy well-crafted documentaries, this film has something to offer everyone. So if you want to learn more about fertilization without getting bogged down in technical terms or endless textbook readings, definitely give this film a watch – it’s well worth your time!
The miracle of conception has been a subject of fascination for centuries, but it wasn’t until the 21st century that we were able to witness its intricate details through documentary film. “The Great Sperm Race” is one such documentary that sheds light on this biological phenomenon like never before.
The premise of the documentary is simple – follow the millions of sperm as they race their way towards fertilizing an egg in a woman’s body. It sounds like something out of science fiction, but this is actually what happens every time a man and a woman come together to create life.
Not only does “The Great Sperm Race” provide us with stunning visuals of how sperm navigate through the female reproductive system, but it also gives us insight into the incredible odds that must be overcome for fertilization to occur. Out of millions of sperm, only one can successfully reach and penetrate an egg. This means that only one winner emerges from each race, making conception an incredibly rare and miraculous event.
One fascinating aspect uncovered by the documentary is how sex selection plays a role in determining whether a male or female embryo develops. Although there is no surefire way to control which gender will result from intercourse, scientists have discovered that male sperm tend to be faster swimmers than female sperm, yet die off quicker. On the other hand, female sperm might not swim quite as fast but stand up better against harsh conditions within the vagina. These subtle differences between male and female sperm make all the difference when competing for fertilization.
In addition to scientific details about conception itself, “The Great Sperm Race” also explores societal and cultural aspects surrounding pregnancy and birth around the world – including traditions around childbirths as well as ethical problems associated with embryonic research conducted during In Vitro Fertilisation (IVF) treatments.
Overall, “The Great Sperm Race” offers much more than just stunning visuals – it’s an enlightening look into one of the most incredible biological phenomena on the planet. By watching millions of sperm in action and learning about the odds involved with fertilization, viewers truly appreciate just how special each new life is.
Are you curious about the journey of sperm? If so, then welcome to our in-depth look at The Great Sperm Race. In this article, we’ll guide you through each and every step of this fascinating process that takes place inside the male body.
First off, let’s start with some basic anatomy. The male reproductive system is made up of a number of different parts including the testes, prostate gland, seminal vesicles, epididymis and vas deferens. It’s within these organs where the magic happens.
When a man becomes sexually aroused, his brain sends a signal to the tissues in his penis causing it to become erect. This prepares for ejaculation – which is when millions upon millions of sperm cells are sent on their way into the world.
So, let’s follow those little swimmers as they make their way towards their intended destination: an egg cell waiting in one of the female’s two fallopian tubes.
Step One: Let’s Get Ready to Rumble! As soon as ejaculation occurs, the race begins! Alongside millions more ‘competitors,’ sperm cells begin swimming forward rapidly – propelled by tiny tails called flagella that wiggle back and forth.
Step Two: The Holding Place Just behind your balls lies one single long tube called epididymis where billions of new sperms are produced each day. Once matured- after around 70 days or so – they’re able to leave here via a lengthy coiled series of tubes (vas deferentia)
Step Three: Meet Mr Seminal Vesicle Once sperm cells join up with fluids from several other glands along its path (including seminal vesicles), this new liquid mixture helps protect them until they reach their final destination; otherwise known as semen.
Step Four: A Sticky Situation Semen provides a transport medium designed specifically for allowing sperm to travel comfortably and avoid desiccation outside deep within female reproductive tract. The mucus-like mixture helps the sperm stick to the cervix of a female’s uterus.
Step Five: A Race Against Time In less than 30 minutes after ejaculation, sperms start to get tired and some will die, with others getting lost along their journey. However, a small minority of these tiny competitors are able to outrun the rest and move ever closer to squaring off against their final opponent: an egg.
Step Six: Mission Accomplished Once that one lucky sperm makes contact with an egg and successfully penetrates its outer layer – fertilization has officially occurred! After several days of cell division and meandering down into fallopian tubes, your baby-to-be eventually implants itself inside the walls of the mother’s womb where it starts growing into a wonderfully magical human.
And there you have it – our step-by-step guide to The Great Sperm Race! This incredible process is just one of many complex biological wonders that occurs naturally within our bodies. So next time you sit down for sex-ed class discussion about
The Great Sperm Race is a fascinating and award-winning documentary that delves into the mysterious world of human reproduction. From the moment of fertilization to the birth of a child, this documentary provides a captivating insight into every aspect of conception.
Since its release, The Great Sperm Race has generated lots of buzz and attention with many people having several questions. Here are some frequently asked questions about The Great Sperm Race Documentary – answered!
What Is The Great Sperm Race About?
As mentioned earlier, The Great Sperm Race is a documentary that explores human reproduction and focuses on the journey sperm must undertake to fertilize an egg successfully. It follows 250 million competitors as they race to be the lucky one to fertilize an egg and create new life.
Is This A Scientifically Accurate Film?
Yes! There’s no doubt about it. Everything you witness in this documentary is scientifically accurate, so viewers can expect to learn a lot about how human conception works in reality. However, because some parts have been dramatized for effect quite unlike what happens in real life or within specific species (such as animals), it’s clear where creative license was taken.
Is It Suitable For Children To Watch The Great Sperm Race Documentary?
Although there’s nothing inappropriate visually or language-wise in terms of age rating on the film itself or otherwise; whether it’s suitable for your child will depend entirely on your parental discretion.
The subject matter might seem somewhat graphic for kids under eight years old. Still safe-to-watch-impressionable young ones — depending on their maturity levels — could learn scientific lessons from watching this informative experiment unfold online or via streaming services available by subscription like Netflix etc,.
Where Can I Watch “The Great Sperm Race” Documentary?
Fortunately, if you missed watching “The great sperm race” when it was first aired over ten years ago now either due to scheduling conflicts then lost out recording it onto PVR you still stand a chance to catch up via streaming services like Netflix.
Netflix is one of the best platforms to watch this exciting documentary that provides invaluable insight into human reproduction. But, you could also look for various other options on Amazon Prime and YouTube.
Is There A Sequel For This Documentary In The Works?
Sadly, no. As far as we are aware, there’s no sequel or new series in the works yet. Regrettably, this means fans of “The Great Sperm Race” will have to keep waiting patiently for any updates from the creators if the post-production phase sees successful outcomes having gathered valuable resources and funding.
However, there are lots of other similar documentaries out there that explore human biology from different angles that interested parties could seek out instead!
Should You Watch “The Great Sperm Race” Documentary?
If you’re somebody who enjoys learning about human anatomy and wants an in-depth study regarding the path sperm take struggle across distance amidst competition — then yes! “The Great Sperm Race” is thoroughly recommended watching.
Apart from being informative and educational about human science, it
Fertility is one of the most fascinating and important topics when it comes to human biology. The ability to conceive a child is not only a biological function but also an emotional and psychological one. And while there are many different factors that can affect fertility, one of the key players is undoubtedly sperm.
With this in mind, we turn our attention to a BBC documentary series called The Great Sperm Race. This groundbreaking series took us on an incredible journey through the male reproductive system as millions of sperm raced to fertilize an egg.
So, what makes this series so special? Well, for one thing, it offers an up-close-and-personal look at what happens inside the male body during intercourse – something that has never been seen before on film! But beyond its novelty factor, The Great Sperm Race provides viewers with a comprehensive understanding of how sperm works and how it plays a critical role in fertility.
The show begins by taking us on a journey through the development process of sperm cells, from their creation in the testicles all the way to their release into semen. We learn about how semen itself is made up of several different substances that help keep the sperm alive and mobile as they move towards the ultimate goal: fertilization of an egg.
But perhaps what’s most fascinating about this series is its exploration of just how difficult it is for sperm to reach their destination. From navigating impenetrable barriers within female reproductive tracts to facing off against other competing sperm cells along the way, nearly 90% of all sperm will never make it to the egg.
Yet somehow amidst all these obstacles, one lucky little swimmer ultimately emerges victorious by successfully penetrating and fertilizing an egg – paving the way for new life to begin.
Ultimately, The Great Sperm Race serves as both an educational tool and source of entertainment. It gives us a deep dive into how our bodies work while also showcasing some truly remarkable special effects (like the stunning 3D animation of millions of sperm cells in motion). But more than anything, the series encourages us to appreciate just how complex and remarkable our bodies are – particularly when it comes to bringing new life into the world.
The Great Sperm Race is a captivating and informative documentary that explores the complex biological processes behind conception. It chronicles the journey of millions of sperm cells as they fight their way to the egg, and ultimately, the miracle of fertilization. The documentary has had a significant impact on fertility research and awareness, shedding light on some important issues related to fertility.
Firstly, The Great Sperm Race has brought attention to male infertility in a way that was not previously possible. Historically, discussions around infertility centered around female reproductive health. However, thanks to this documentary, we now understand how important it is to consider male infertility as a significant factor in fertility problems.
Secondly, The Great Sperm Race has highlighted the importance of timing when it comes to conception. Couples who are trying for a baby need to know when ovulation is occurring so that they can increase their chances of successful fertilization. This understanding can be hugely beneficial for couples who have been struggling with infertility for an extended period.
Furthermore, The Great Sperm Race has made people more aware of lifestyle factors that can affect fertility. For example, smoking and excessive alcohol consumption can damage sperm quality and decrease chances of conception significantly.
The insights gained from this fantastic documentary have contributed immensely towards advancing our understanding about reproduction and fertility mechanisms further. Both researchers and families who want children now have access to invaluable information about what it takes to become pregnant successfully.
In this regard, we can positively deduce that watching documentaries such as “The Great Sperm Race” educates us thoroughly on various aspects concerning our lives’ development stage if taken seriously; one may start implementing healthy changes towards increasing their chances of becoming pregnant successfully within reach but also helps us create awareness among society too regarding how lifestyle choices impact reproductive health.
Overall! We must commend “The great sperm race” for giving researchers groundbreaking insights into human reproduction while also serving as an excellent resource for anyone interested in understanding all aspects of fertility and reproductive health. It positively impacted the way people view conception and infertility, empowering them with knowledge to make informed decisions on their lifestyle choices that impact reproduction while debunking myths surrounding conception dynamics.

- International
- Schools directory
- Resources Jobs Schools directory News Search
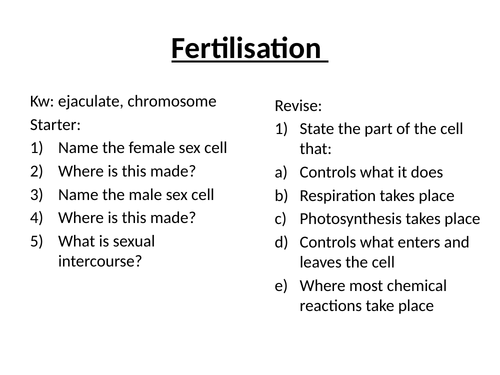
Fertilisation DIFFERENTIATED with answers KS3 Journey of Sperm writing task and chromosomes.
Subject: Biology
Age range: 11-14
Resource type: Lesson (complete)
Last updated
3 January 2020
- Share through email
- Share through twitter
- Share through linkedin
- Share through facebook
- Share through pinterest
Starter activity with answers Storytime activity Journey of a sperm writing task Story board for low ability Exam questions
Tes paid licence How can I reuse this?
Your rating is required to reflect your happiness.
It's good to leave some feedback.
Something went wrong, please try again later.
This resource hasn't been reviewed yet
To ensure quality for our reviews, only customers who have purchased this resource can review it
Report this resource to let us know if it violates our terms and conditions. Our customer service team will review your report and will be in touch.
Not quite what you were looking for? Search by keyword to find the right resource:

IMAGES
COMMENTS
Find out more with BBC Bitesize. For students between the ages of 11 and 14. ... Fertilisation occurs when a sperm and egg join to form an embryo. ... Describe the journey of a sperm from testis ...
Learn how the male and female reproductive systems work with BBC Bitesize Third Level Science. ... The sperm pass through the sperm ducts, and mix with fluids produced by the glands. The fluids ...
During sexual intercourse sperm are transferred from the penis of the male into the vagina of the female. They then swim through the uterus to the oviduct and can fertilise an egg cell if one is ...
Parthenogenesis is a type of reproduction in which the egg can develop into an embryo without the help of sperm. This phenomenon can be seen in several organisms, including bees, turkeys, and sharks. ... Let's take a brief look at the zygote's journey. Cleavage and implantation. The image below summarizes the events that occur between ...
This 3D animation shows the magic that happens when a sperm meets an egg and the sparks fly. Fertilization happens when a sperm cell successfully meets an eg...
This takes about 3 days, during which time the zygote will divide several times to form a ball of cells known as an embryo. In the uterus, the embryo embeds itself in the thick lining ( implantation) and continues to grow and develop. The gestation period for humans is 9 months. Major development of organs takes place within the first 12 weeks ...
The sperm producing and conducting organs include the testes, the epididymides, the penis, and the ducts and glands that produce and carry semen. Sperm exit the scrotum through the ductus deferens, which is bundled in the spermatic cord. The seminal vesicles and prostate gland add fluids to the sperm to create semen.
Out of the approximately 5,000 sperm that enter the utero-tubal junction, about 1,000 get inside the Fallopian tube. Finally, out of the 1,000 that enter the tube, it is estimated that only 200 make it to the egg. However, in the end, only 1 sperm out of the 200 that reach the egg is able to penetrate and fertilize it.
Fertility is the ability to produce offspring. Fertility is continuous in males and cyclical in females. Infertility can have a number of causes and there are a range of infertility treatments that work in different ways.
Let' uncover the fascinating science behind male reproduction, exploring the basics of anatomy of the male reproductive system, puberty, the ejaculation mech...
Lesson 3: The Journey of a Sperm. Grade 5. DOWNLOAD THE .PDF FILE . SEXUAL HEALTH EDUCATION. Teacher Webinars and Workshops; Understanding Your Role; Information by Topic; Responding to Student Questions; Student FAQs; Submit a Student Question; Managing Sensitive Issues; LESSONS PLANS & RESOURCES. Lesson Plan & Resource Finder; Differing ...
What makes one sperm succeed in reaching and fertilising an egg rather than another? This documentary re-enacts the journey of a sperm using human volunteers. Using computer animated graphics the process of male ejaculation and fertilisation is illustrated. The human volunteers attempt to overcome the obstacles faced by a sperm on its way to an egg.</p>
Journey of a Sperm Cell. Subject: Biology. Age range: 11-14. Resource type: Worksheet/Activity. File previews. docx, 67.8 KB. docx, 67.9 KB. KS3 Biology journey of a sperm cell literacy task with 10 multiple choice questions. Created for higher ability pupils.
When the sperm leave the penis, it is called ejaculation. On the day in question, it just so happened that the sperm got to be released from the body. First, the. (4.______________) became larger, longer and firmer until it stuck out from the body. (When the penis gets this way it is called an (5.
The journey of sperm begins inside the testicles. Males begin to produce sperm at the start of puberty at around 12 or 13 years old. It is a process that requires a slightly cooler temperature, which is why testicles hang outside men's bodies. Nor is it a quick process: the production of sperm takes about 70 days.
The film, produced by the BBC, provides audiences with an insightful and entertaining overview of everything from egg production to sperm delivery. ... The Great Sperm Race is a documentary that explores human reproduction and focuses on the journey sperm must undertake to fertilize an egg successfully. It follows 250 million competitors as ...
Starter activity with answers Storytime activity Journey of a sperm writing task Story board for low ability Exam questions
Play Bitesize Primary games. game Play Bitesize Primary games. Fun and educational primary games in science, maths, English, history, geography, art and design, computing and modern languages.