
Set My Location
Providing your location allows us to show you nearby providers and locations.

The Ultimate Pregnancy Appointment Guide: What to Expect Week by Week at Your Prenatal Visits
Central to ensuring the health and well-being of you and your growing baby is seeing your care team regularly for touchpoints and milestones that are part of your pregnancy appointment schedule. Diana Kaufman, MD , UnityPoint Health, shares the recommended timeline for prenatal visits, and the importance of each test and discussion that’ll prepare you for a safe pregnancy and delivery.
Confirming Your Pregnancy
Every woman’s body is unique, but it’s a good idea to visit a doctor to confirm a pregnancy when you’re experiencing early symptoms, such as a missed period or you’ve received a positive home pregnancy test. Typically, this visit happens at 6-8 weeks of pregnancy.
Your doctor may confirm your pregnancy through urine tests, blood tests or ultrasounds.
Initial Prenatal Appointment: 5-12 Weeks
Your first prenatal visit consists of important screenings and discussions, so your healthcare team can create a care plan that ensures you and baby stay healthy throughout your pregnancy. Prepare a few things for this visit, including:
- Complete medical history: It’s important for your doctor to know your past and present health conditions or concerns, medications and any history of disease, substance abuse or known genetic conditions in your family.
- Insurance information: This includes consents for care, your insurance carrier and other paperwork
Here’s what to expect at your first pregnancy appointment
- A physical, which will likely include a breast and pelvic exam.
- A urine sample is collected to check for certain infections and conditions that can occur during pregnancy. Urine tests may be taken at your following prenatal visits as well. Urine drug screening tests are also recommended for women, or their partners, with a history of substance use — including smoking.
- Routine testing that includes blood draws to check your blood type and complete blood count (CBC) and look for specific diseases including hepatitis, HIV, syphilis and checking for immunity against rubella. Other testing that may occur includes genetic screening and testing for diabetes.
Your care team will review prenatal educational materials with you and remedies for any unpleasant pregnancy symptoms, such as nausea or vomiting . Your team also will provide an estimated due date for baby.
It’s also important to take good care of your teeth and gums during pregnancy. Changing hormone levels make your gums more sensitive to disease, which increases your risk for a low-birth weight or premature baby. Consider making an appointment to see your dentist during your first trimester.
Prenatal Appointment: Second Trimester (13 – 26 Weeks)
During weeks 13-26, you’ll see your doctor every four weeks. It’s a good idea to write down questions or concerns before your appointments to ensure they’re addressed.
At each appointment throughout the rest of your pregnancy, your care team will check the following:
- Blood pressure
- Position of baby
- Baby’s heartbeat
Here are some additional things to expect.
- Prenatal genetic testing: There are many different options for prenatal genetic testing. Your care team will review these with you.
- Pregnancy blood tests: These are tailored to your specific needs. Most patients are tested for anemia and diabetes of pregnancy between weeks 24-28. Other recommended tests will be reviewed with you.
- Ultrasound: It’s common to have an ultrasound in the first trimester to confirm the estimated due date. Ultrasound is also common at 20 weeks to check on baby's growth and development. Further ultrasounds could be needed if changes in your pregnancy make it necessary, such as concerns about baby’s growth or to see if baby is head down.
- Discuss preterm labor signs: Preterm labor refers to labor that begins before the 37th week of pregnancy and requires medical attention. Knowing what to look for — such as contractions, changes in vaginal discharge — is important for preventing potential complications.
- Childbirth classes: It’s a good idea to register for a class to help you prepare for baby’s arrival.
When to Call Your Doctor
Pregnancy creates new and unfamiliar symptoms in many women. However, some symptoms need attention. Here’s when to call your doctor in the second trimester:
- Vaginal bleeding, even a small amount
- Leg pain with numbness or leg weakness
- Pain or tenderness in one of both calves that doesn’t go away
- Thoughts of hurting yourself or others
- Severe headaches that don’t go away with Tylenol
- Persistent changes in vision such as blurriness or floaters
- More than five contractions in an hour
Now, your visits to your care team become more frequent — happening every two weeks until you’re 36 weeks pregnant. Your care team continues to monitor you and baby. Here’s what else to expect:
Prenatal Appointments: Third Trimester (27 Weeks – Baby’s Arrival)
- Check fetal movement: It’s important to be aware of your baby's movements. If you notice a sudden change or absence of fetal movement, let you care team know.
- Rhogam injections: If an Rh-negative blood type was found during your initial prenatal visit, you’ll receive an injection to prevent immune system complications for future pregnancies. This usually happens at 28 weeks.
- Additional prenatal testing: Around 35-37 weeks, you’re checked to see if you carry group B streptococcus bacteria . This is one of many bacteria that can live on our skin and typically does not cause problems. However, it can infect a newborn when you deliver. Antibiotics are given during delivery to prevent infection in a newborn if you test positive.
Prenatal Appointments: 36 Weeks – End of Pregnancy
Once you’ve reached 36 weeks, you’ll see your doctor every week until you deliver. These visits are essential for ensuring the well-being of both you and your little one, as well as preparing for a safe and smooth delivery. In addition to routine physical examinations and checking baby’s heartbeat and movement, here’s what else you can expect:
- Cervical exams: If you’re having frequent contractions or preparing to be induced, your doctor will likely need to perform this exam.
- Discuss labor signs: You’ll likely discuss signs of labor with your doctor and when to go to the hospital.
- Discuss birth preferences: It’s not necessary to have a birth plan. Your care team has that covered. Our goal is to keep you and your baby healthy throughout the entire pregnancy and delivery process. However, if you have strong desires or needs for delivery, please discuss those during a prenatal appointment. It’s also helpful to write these things down and bring them to the hospital, since you may not be able to fully express your wishes during labor.
Postpartum Visits
After delivering baby, but before you leave the hospital, call your doctor to make your postpartum appointment, if it hasn’t been scheduled yet. This visit typically occurs around 6 weeks after you deliver. Other visits are scheduled based on your individual needs.
These visits are a time for your doctor to check on your healing , discuss normal or abnormal postpartum bleeding, talk about your well-being and any signs of postpartum depression or anxiety , discuss when it’s safe to start exercising again and address other questions or concerns you may have .
Our UnityPoint Health care team is here to care for you and baby throughout the entirety of your pregnancy and beyond. Call us to schedule your first appointment or if you have questions about any future appointments.
More Maternity Content
Group B Strep in Pregnancy: Understanding Risks, Testing and Treatment
Second Time Mom Gets Wish of Vaginal Birth After C-Section
An OBGYN Answers 17 Questions to Help You Prepare for Postpartum
- Trying to Conceive
- Signs & Symptoms
- Pregnancy Tests
- Fertility Testing
- Fertility Treatment
- Weeks & Trimesters
- Staying Healthy
- Preparing for Baby
- Complications & Concerns
- Pregnancy Loss
- Breastfeeding
- School-Aged Kids
- Raising Kids
- Personal Stories
- Everyday Wellness
- Safety & First Aid
- Immunizations
- Food & Nutrition
- Active Play
- Pregnancy Products
- Nursery & Sleep Products
- Nursing & Feeding Products
- Clothing & Accessories
- Toys & Gifts
- Ovulation Calculator
- Pregnancy Due Date Calculator
- How to Talk About Postpartum Depression
- Editorial Process
- Meet Our Review Board
Week 40 of Your Pregnancy
Verywell / Bailey Mariner
- Baby Development
Your Newborn at Birth
Self-care tips, advice for partners.
- Doctor Visits
Special Considerations
At 40 weeks pregnant, you've reached the milestone everyone's been counting down to from the beginning. Hopefully, you’ll be welcoming your brand-new baby this week. Whether that happens or you find yourself overdue , the road ahead is a short one. Though those at this stage of pregnancy are often ready for their pregnancy to end, the feelings that come with the reality of "the big day" can take many by surprise.
40 Weeks Pregnant Is How Many Months? 10 months
Which Trimester? Third trimester
How Many Weeks to Go? 0 weeks
Your Baby's Development at 40 Weeks
At 40 weeks, a baby is about 14 1/4 inches (36.3 centimeters) from the top of their head to the bottom of their buttocks (known as the crown-rump length ), and baby's height may stretch over 20 inches (51.7 centimeters) from the top of their head to their heel (crown-heel length). This week, baby might weigh close to 8 pounds (3617 grams).
Birth Weight and Length
Your newborn may measure in close to the averages above. However, its normal for a healthy newborn to be smaller or larger than those numbers. A healthy full-term baby can have a measure between 17 3/4 inches (45 centimeters) to nearly 22 inches (55 centimeters) long. It is also normal for a healthy newborn to weigh anywhere between 5 1/2 pounds (2,500 grams) to 10 pounds (4,500 grams).
This week, your baby is right on target at 40 weeks, which is considered " full term ." Babies born at full term encounter fewer risks and generally have better health outcomes.
Explore a few of your baby's week 40 milestones in this interactive experience.
After months of nothing more than occasional peeks at your little one via ultrasound, it's time to get ready to meet your baby face-to-face.
Your newborn might not look how you expect . Those perfect, plump babies in magazines are usually a few weeks old. Right after birth, newborns are wet and often show the signs of the birth they just experienced.
- Baby’s skull will be soft and pliable, which allows for a smoother transition through the birth canal, but it can also leave them with a temporarily cone-shaped head if you deliver vaginally.
- Your new baby may sport some lingering vernix (the waxy, white substance that covers their skin in utero) and lanugo (the thin, soft hair that covers their skin in utero).
- Baby's eyes may be quite swollen.
- Their hands and feet may be tinged blue.
- There may be white dots, acne, or a red rash on baby's face or skin.
- Baby's breasts and genitals may be swollen.
While the look of your baby may be a little strange at first, these variations in appearance are normal expectations in healthy newborns. As the hours and days go on, your baby will look more and more ready for their magazine cover shoot.
Baby's Post-Birth Tests and Procedures
After baby is born, there are a few procedures and tests that will take place right away, and a few more that will take place during the first few days:
- Skin-to-skin : Right after delivery, your healthcare provider may suction mucus and amniotic fluid out of your baby’s mouth and nose, dry the baby, and place them on your stomach or chest for skin-to-skin contact—and your first hug. If you don't get to hold your baby right away, it is likely because they are showing signs of distress or you had a C-section, in which case they may need to be evaluated by a pediatrician first.
- Umbilical cord : Your partner or your healthcare provider will cut the umbilical cord officially separating baby from the placenta that's nourished them throughout pregnancy.
- Weight and length : These initial measurements may be taken almost immediately after birth, or they may be delayed to facilitate skin-to-skin time for baby. These measurements will be repeated at every pediatrician visit going forward.
- APGAR score : Hospital or birth center staff will assess baby’s skin color, heart rate, respiratory effort, muscle tone, and reflexes; these assessments make up baby's APGAR score. The APGAR score is measured at one to five minutes after your baby is born and can usually be done while baby is on your chest.
- Eye drops or ointment : Unless you decline, healthcare providers will apply erythromycin antibiotic eye drops or ointment to baby's eyes to help prevent infection.
- Vitamin K injection : Usually given within six hours of birth, a vitamin K injection is important to ensure proper blood clotting, which reduces baby’s risk of brain and other bleeding.
- Hepatitis B vaccine : The American Academy of Pediatrics (AAP) recommends that all newborn babies receive the first dose of the hep B vaccine within 24 hours of birth. You will be asked to sign a parental consent form for this routine procedure.
- Hearing test : To test their hearing, baby’s ears are exposed to sounds through headphones while nodes placed on their head determine how well the tones are heard.
- PKU test : This is also called the newborn screening test and it’s most likely performed when your baby is between 24 to 48 hours old. For these tests, your healthcare provider pricks baby’s heel to collect several drops of blood to test for up to roughly 50 different illnesses, including phenylketonuria (PKU), galactosemia, and congenital hypothyroidism. (What exactly is tested for varies by state .)
- Circumcision : If you decide to circumcise your child, the procedure will be offered in hospital within a day or two after birth. Is it possible, however, to delay or decline the procedure entirely. For example, many Jewish families delay circumcision until eight days after birth in a religious ceremony known as a bris milah . Many other families chose not to circumcise at all.
Stay Calm Mom: Episode 10
Watch all episodes of our Stay Calm Mom video series and follow along as our host Tiffany Small talks to a diverse group of women and top doctors to get real answers to the biggest pregnancy questions.
How to Deal With Unwanted Pregnancy Advice
Your common symptoms this week.
At 40 weeks pregnant, you are full term, but if you do not have your baby this week, you aren't alone.
What Experts Say
"Only 19% of women actually go into labor during week 40, with 14% going into labor at 41 weeks or more.”
—Allison Hill, MD, OB/GYN
With babies coming on their own schedule more often than not, you might still find yourself still waiting on your little one's arrival this week. Patience is definitely key.
When you do go into labor, you can expect to experience several stages :
- The first stage includes early labor, active labor, and transition.
- The second stage is pushing and birth.
- The third stage is after baby's birth with the delivery of the placenta.
Here's a look at the parts of labor.
Early Labor
With early labor, you’ll experience telltale uterine contractions .
“The early (latent) phase of labor can consist of irregular, not-very-painful contractions that last 30 to 45 seconds. But it can also consist of painful contractions from the get-go.”
With each contraction, your cervix continues to open (dilate) and thin (efface) . Unlike Braxton Hicks, labor contractions don’t stop when you shift positions. They start in the back and move to the front of your abdomen, and they feel stronger than the "practice contractions" you've experienced until now. This early stage of labor can last a day or two , so call your doctor or clinic to let them know and get instructions.
Active Labor
Active labor can start when the cervix is dilated anywhere from 3 to 6 centimeters. Once you enter the active stage of early labor, your cervix may dilate roughly 1 centimeter an hour.
During active labor:
- Contractions become more regular and occur closer together.
- Contractions are stronger, longer, and more painful.
- The baby is moving down toward the birth canal.
You’ll want to make your way to the hospital or birthing center at some point during this stage of labor. Dr. Hill recommends going when contractions are strong and have consistently been three to five minutes apart for at least a few hours:
- You can ask your partner to help you keep track of your contractions . You can do this with a notepad and timer or you may consider using a mobile app designed to make this task easier.
- Keep in contact with your healthcare provider to determine the best time for you to head to your chosen birth location.
- Keep anticipated travel time in mind when determining departure time, as traffic at certain times of day may make your trip a bit slower than you’d like.
Transition is the last part of the first stage of labor. It is commonly considered the hardest part, but its also often the shortest. During transition, contractions are long and intense. The time between contractions is short, so it's difficult to rest or relax. This is a time when the cervix is opening to its widest point. During transition you may start uncomfortable shivering or develop nausea and start to vomit. Although unpleasant, this is usually entirely normal.
Full Dilation
When you reach full dilation or 10 centimeters, you enter the second stage of labor . The second stage can last anywhere from 20 minutes to a few hours.
You'll feel the pressure of your baby’s head between your legs along with a strong urge to push. If you have an epidural , however, the sensation may be dampened.
Pushing and Delivery
When it's time to push, it may feel like you have to move your bowels. Your provider will help you know when it's time to push. Each push helps to move the baby down the birth canal.
During the pushing stage, your baby’s head will begin to emerge from your vagina with each contraction. When the baby’s head remains visible without slipping back inside, baby is crowning . Once your baby's head is visible, you will continue to push as you or your provider helps guide your baby into the world.
The second stage of labor ends with the birth of your baby. The second stage can take a little longer with an epidural than without one. However, it shouldn't greatly impact your ability to push when it’s time .
Delivering the Placenta
After your baby is born, you’ll enter the final stage of labor: delivering the afterbirth or placenta. During this stage, you begin to have contractions again and you may have to push again. The placenta is usually delivered within 30 minutes, and your labor is over once it is out of your body.
It’s important to remember that no two birthing experiences are the same. While your curiosity may be satisfied by hearing others’ stories, your experience (how you deliver, how long it takes, and more) will be your own.
Self-care becomes even more important—and yes, often more complicated—as you prepare for labor and the birth of your baby as well as the transition from pregnancy to postpartum.
If You're Still Waiting
If you've reached 40 weeks and you're still waiting to meet your baby, the best advice is just to do your best to be patient. It may not be what you want to hear, but it's important to remember that babies come when they're ready. In the meantime, you can continue to try to encourage your baby to get into position and help get labor on its way by:
- Going for walks
- Stimulating your nipples
- Having intercourse
"One of the most common reasons that your baby has not come out yet is that they may not be in the proper position . Encourage your baby to drop into the pelvis by staying active, going on walks, and gently stretching your hips and groin.”
Once Your Baby Arrives
Once your baby is here, it can become very easy to neglect your own needs. But remember, whether you had a Cesarean or vaginal birth, you’ll be recovering from one of the most physically and mentally demanding experiences a person can have. It will be important to honor that and ensure that you and your loved ones do what you can to support the recovery process .
Supporting Your Physical Health
To ease vaginal and perineum pain:
- Use an anesthetic spray to numb the area.
- Soak your bottom in a warm sitz bath to soothe soreness.
- Wear frozen maxi pads. (Soak a pad with witch hazel and squirt aloe vera gel down the center; fold and place in a zipped bag inside the freezer.) Use as needed for 10 to 20 minutes at a time.
- Sit on a doughnut cushion to take pressure off your sensitive perineum area.
- Ask your provider about taking ibuprofen to ease pain, cramping, and post-birth bleeding.
To make using the bathroom easier:
- Use a peri bottle to indirectly squirt lukewarm water on your vulva and perineum as you pee to cool the sting; you can use this in lieu of toilet paper after urinating.
- Ask your healthcare provider about taking a gentle stool softener as constipation after giving birth is common.
- Drink plenty of fluid and eat high-fiber foods to prevent or ease constipation as well.
To soothe sore breasts:
- Consider wearing nursing pads between feedings to shield sore nipples from rubbing against clothing.
- To reduce painful engorgement swelling , apply cold compresses on your breasts.
- Wear a comfortable, supportive bra.
- Talk to your doctor about using a safe pain medication, if needed.
In addition, if you experience any worrisome physical symptoms , such as fever, excessive bleeding, an inflamed C-section scar, pain, chills, or difficulty breathing, do not wait until your postpartum checkup to seek care and guidance from your physician or midwife.
Supporting Your Mental Health
Many new parents do not feel prepared for the postpartum period . Dealing with the physical recovery of childbirth and the change in healthcare support during this period can be overwhelming and can impact your mental health.
Despite what you might see in commercials, you’d be hard-pressed to find a new parent who doesn’t experience bouts of crying following the birth of their baby. Postpartum blues (also known as the "baby blues") are common in the first two weeks after delivery. However, symptoms that continue beyond those initial weeks or become more severe may be a sign of postpartum depression .
“It's not what you’re feeling, exactly. It's how often you feel it, how long you’ve been feeling that way, and how much it interferes with your everyday functioning.”
—Shara Marrero Brofman, PsyD
While temporarily feeling blue postpartum is to be expected, experiencing postpartum depression or anxiety requires special attention .
Postpartum depression affects as many as 1 in 5 parents following birth. If you are experiencing one or more of the following symptoms, seek the help of your healthcare provider as soon as possible:
- Feeling weepy and overwhelmed for longer than three weeks
- Continuously crying
- Feeling unable to enjoy your baby; not wanting to spend time with baby
- Experiencing intense rage
- Experiencing anxious thoughts about your baby being hurt
- Being unable to sleep when exhausted; wanting to sleep all the time; or sleeping more than usual
- Pondering harming yourself, your baby, or others
- Experiencing a dramatic shift in appetite
- Assuming your family would be better off without you
Your Week 40 Checklist
- Continue taking prenatal vitamins —even after birth, especially if you are breastfeeding.
- Continue drinking about eight to 12 glasses of water a day.
- Continue doing your Kegel exercises daily (they're helpful for birth and your recovery).
- Continue doing your daily perineal massages (unless you've already delivered).
- Review how to time contractions .
- Get ready for the big day and for those first weeks postpartum .
Even though your pregnant partner is doing the heavy lifting of labor and delivery, you’re still a key part of the whole process, especially when it comes to offering encouragement and support; timing contractions; and helping to gauge when it’s time to go to the hospital or birthing center.
Timing Contractions
Remember to time contractions by the second, using the stopwatch feature on your phone or an app. You’ll time each of your partner’s contractions from start to finish to figure out how long the contractions are.
Next, you’ll time the distance between the start of one contraction and the start of the next. This is how far apart your partner’s contractions are. Record all of this information and repeat the process a few times to check for regularity.
Do yourself and your pregnant partner a favor and refrain from timing every contraction. Only do it when there appears to have been a change (and/or once every hour).
Heading to the Hospital
You or partner should speak to the healthcare provider once you believe labor has started. Your doctor or midwife will give you instructions on when to head to the hospital. Don't hesitate to go straight to the hospital if:
- Your partner's water has broken but they're not experiencing any contractions.
- Your partner is experiencing vaginal bleeding.
- Your partner is in a lot of pain.
- The baby isn't moving as much as before.
If you are unsure of what to do, go to the hospital or birthing center. The staff can evaluate the situation and decide if it's time to be admitted or if you should go home and wait a little longer .
At the Hospital
Take direction from the hospital or birthing center staff, as well as your partner, when they're in labor—and know that just being there and holding their hand (if that brings them comfort) may be the best thing you can do in that moment. If you prefer not to see the actual birth, voice that to staff so you can be positioned at the head of the bed (or elsewhere).
Returning Home
Once your partner and baby are discharged from the hospital and you head home for the first time as a new family, you may feel uncertain of the best ways to help, especially if your partner is breastfeeding—a unique responsibility, should they choose to.
Do what you can to help your partner focus on their own recovery, as well as the care of your newborn. Bring them water when they're nursing. Change baby’s diaper . Learn how to burp baby after a feeding and how to swaddle them for soothing and sleep. Ask what supplies you can pick up at the store.
Most of all, remember that in the days, weeks, and months ahead, you both will be working to learn the ins and outs of your newborn, parenthood, and perhaps even life as a family of four , five, or more, if baby has siblings. Try to be patient with and understanding of each other—and yourself.
At Your Doctor’s Office
If you find yourself still pregnant and at your physician or midwife’s office this week, hang in there. Know that you are not officially considered "post-term" until you are 42 weeks pregnant.
Stripping the Membranes
Due dates are not an exact science ; things like irregular periods and an inaccurate menstrual history can throw off delivery-day calculations. Regardless, your healthcare provider may offer to strip your membranes in an effort to kickstart labor at your visit this week.
Upcoming Doctor’s Visits
If you don’t go into labor within a week, you’ll likely have a non-stress test and/or a biophysical profile (BPP) to check on baby’s heart rate, movement, and overall well-being. Your healthcare provider will review the results to determine if an induction is advised.
Postpartum Care
The American College of Obstetricians and Gynecologists (ACOG) positions postpartum care as an ongoing process. After your care at birth, you should be in contact with your doctor within 3 weeks and you should see your doctor for a thorough postpartum exam no later than 12 weeks after the birth of your baby.
Care should be individualized based on need and those with a high risk of postpartum depression or other health concerns should be in contact with their doctor and see their doctor sooner.
During your comprehensive postpartum appointment, you can expect a:
- Pelvic exam to make sure that your uterus, ovaries, and cervix have returned to their pre-pregnancy state
- Pap test to check for abnormal cervical cells
- Perineum exam to review swelling and/or episiotomy or tear recovery
- Breast exam to look for abnormal growths and blocked milk ducts
- Cesarean scar exam (if applicable)
- Postpartum depression screening
Your provider will also answer your questions about sex and birth control. Yes, it is physically possible to get pregnant very soon after birth .
Take this opportunity to also talk about your labor and delivery and clear up any questions you may have. Share how you are feeling both physically and emotionally as a new parent.
Don’t hesitate to review any lingering pregnancy-related health issues such as hemorrhoids , varicose veins, and skin changes . And bring up any issues that may have recently cropped up, like urinary or anal stress incontinence.
Chances are good that you just might meet your baby this week, but how you give birth will ultimately depend on a multitude of factors. Even if you plan to give birth vaginally, it can be helpful to be familiar with the alternative in case you're faced with a change in plans.
Chances of Childbirth This Week
Research suggests that you have a good chance of having your baby this week. In a large U.S. study of over 34 million births, 54% to 60% of those expecting had their baby between 39 and 40 weeks.
Cesarean Section
A cesarean section is a surgery to deliver a baby. With this surgical procedure, instead of going through the birth canal, the baby is born through an incision in the abdomen and uterus.
About 32% of babies born in the United States arrive via Cesarean section (C-section) . For some, the procedure is planned due to circumstances such as:
- Prior C-section with no intention of attempting a VBAC (vaginal birth after Cesarean)
- Carrying multiples (twin pregnancy or more)
- Breech presentation
- Placenta previa
- Certain parental conditions or prior uterine surgery for which labor is not advised
- Personal preference
But for most people, a C-section is an unplanned change in plans due to unforeseen complications such as labor not moving along as it should or concerns for parent or baby's health during the labor process.
If you have a Cesarean birth, you can expect the following:
- An anesthesiologist will give you an epidural or spinal , if you haven’t already had one. Beware that this anesthesia may affect your ability to sense your muscles moving, leaving you with a sensation that you are not able to take deep breaths. Try not to panic: You are breathing just fine and you're being closely monitored.
- Your abdomen will be scrubbed with an antibiotic cleanser.
- Drapes and curtains will be placed over and around you to stave off infection and shield you from witnessing the surgery if that’s your preference. (Some birthing facilities offer clear drapes if you desire them.)
- Your arms may be loosely strapped to armrests placed away from your body. (This is simply to remind you not to touch any part of your belly that has been sterilized.)
- Once you’re numb, your healthcare provider will make an incision in your abdomen through your skin, muscle, fat, peritoneum (lining of the abdominal cavity), uterus, and finally the amniotic sac.
- When it’s time to deliver the baby, you will feel pushing, pulling, pressure , and possible nausea, but no pain.
- Once your baby is delivered, they will be evaluated by a pediatrician. Most providers will bring the baby to you so you can see them first.
- Your healthcare provider will then deliver your placenta; inspect and clean your uterus; and close your incision, which is the longest part of the entire procedure.
- Once your incision is closed, you will spend roughly one hour in the recovery room before being sent to your postpartum room. Unless your baby is being monitored or treated, or your hospital or birthing center has another policy, your baby will join you bedside in recovery.
- Most likely, you will stay in the hospital for about four days.
- Your stitches or staples will likely be removed about 8 to 10 days after the surgery.
A Word From Verywell
As you near the end of your pregnancy journey, it can be tempting for all the focus to be on getting to the finish line, but if you can, take some time to reflect. Whether you basked in your pregnancy glow or struggled through challenges, try to appreciate these final moments with your baby before they are born. Most importantly, be sure to give yourself the credit you deserve for all the hard work your body has done growing and nourishing your baby-to-be, and embrace that strength as you transition to new parenthood.
Oyer CE, Sung CJ, Friedman R, et al. Reference values for valve circumferences and ventricular wall thicknesses of fetal and neonatal hearts . Pediatr Dev Pathol . 2004;7(5):499-505. doi:10.1007/s10024-004-1117-6
Kiserud T, Piaggio G, Carroli G, et al. The World Health Organization Fetal Growth Charts: A multinational longitudinal study of ultrasound biometric measurements and estimated fetal weight . PLoS Med . 2017;14(3):e1002284. doi:10.1371/journal.pmed.1002220
Centers for Disease Control and Prevention, National Center for Health Statistics. Clinical Growth Charts .
University of Michigan Medicine. Physical Growth in Newborns .
Definition of term pregnancy. Committee Opinion No. 579 . Obstet Gynecol . 2013;122:1139-40. doi:10.1097/01.aog.0000437385.88715.4a
University of Rochester Medical Center. Newborn appearance .
Kilpatrick SJ, Papile LA, Macones GA. Guidelines for perinatal care 8th Edition . American Academy of Pediatrics and American College of Gynecologists and Obstetricians. 2017.
Rota A, Antolini L, Colciago E, Nespoli A, Borrelli SE, Fumagalli S. Timing of hospital admission in labour: latent versus active phase, mode of birth and intrapartum interventions. A correlational study . Women Birth . 2018;31(4):313-318. doi:10.1016/j.wombi.2017.10.001
Zhang J, Landy HJ, Branch DW, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes . Obstet Gynecol . 2010;116(6):1281-7. doi:10.1097/AOG.0b013e3181fdef6e
Eunice Kennedy Shriver National Institute of Child Health and Human Development. What are the stages of labor? .
U.S. Department of Health and Human Services, Office on Women's Health. Labor and birth .
Anim-Somuah M, Smyth RM, Cyna AM, Cuthbert A. Epidural versus non-epidural or no analgesia for pain management in labour . Cochrane Database Syst Rev . 2018;5(5):CD000331. doi:10.1002/14651858.CD000331.pub4
Health Essentials. Truth or tale? 8 ways to (maybe) move labor along naturally . Cleveland Clinic.
Mohamed HA, El-Nagger NS. Effect of self perineal care instructions on episiotomy pain and wound healing of postpartum women . J Am Sci . 2012;8(6):640-50.
Postpartum pain management. ACOG Committee Opinion No. 742 . Obstet Gynecol . 2018;132. doi:10.1097/AOG.0000000000002683
Turawa EB, Musekiwa A, Rohwer AC. Interventions for treating postpartum constipation . Cochrane Database of Systematic Reviews . 2014(9). doi:10.1002/14651858.CD010273.pub2
Berens P, Brodribb W. ABM Clinical Protocol #20: Engorgement, revised 2016 . Breastfeeding Med . 2016;11(4):159-63. doi:10.1089/bfm.2016.29008.pjb
March of Dimes. Warning signs of health problems after birth .
Martin A, Horowitz C, Balbierz A, Howell EA. Views of women and clinicians on postpartum preparation and recovery . Matern Child Health J . 2014;18(3):707-13. doi:10.1007/s10995-013-1297-7
Committee opinion no. 666: Optimizing postpartum care . Obstet Gynecol. 2016;127(6):e187-92. doi:10.1097/AOG.0000000000001487
Centers for Disease Control and Prevention. Depression Among Women .
March of Dimes. Contractions and signs of labor .
American College of Obstetricians and Gynecologist. How to tell when labor begins .
American College of Obstetricians and Gynecologists. Labor induction .
American College of Obstetricians and Gynecologists. When pregnancy goes past your due date .
Optimizing postpartum care. ACOG Committee Opinion No. 736 . Obstet Gynecol. 2018;131:e140–50(5):e140-50. doi:10.1097/aog.0000000000002633
Ananth CV, Goldenberg RL, Friedman AM, Vintzileos AM. Association of temporal changes in gestational age with perinatal nortality in the United States, 2007-2015 . JAMA Pediatr. 2018;172(7):627-634. doi:10.1001/jamapediatrics.2018.0249
American College of Obstetricians and Gynecologist. Cesarean birth .
National Center for Health Statistics. Births - method of delivery .
Safe prevention of the primary cesarean delivery. Obstetric Care Consensus No. 1 . Obstet Gynecol . 2014;123:693-711. doi:10.1016/j.ajog.2014.01.026
Rollins M, Lucero J. Overview of anesthetic considerations for Cesarean delivery . British Medical Bulletin. 2012;101(1). doi:10.1093/bmb/ldr050
Vejnović TR, Costa SD, Ignatov A. New technique for Caesarean section . Geburtshilfe Frauenheilkd . 2012;72(9):840–845. doi:10.1055/s-0032-1315347
Pearlstein T, Howard M, Salisbury A, Zlotnick C. Postpartum depression . Am J Obstet Gynecol . 2009;200(4):357-364. doi:10.1016/j.ajog.2008.11.033
By Holly Pevzner Holly Pevzner is an award-winning writer who specializes in health, nutrition, parenting, and family travel.
25% OFF Suncare Collection* w/ code SUN25 | Free Shipping on all orders $50+

- > Prenatal Visit Schedule: What To Expect During Each Appointment
Prenatal Visit Schedule: What To Expect During Each Appointment
Prenatal care is an important part of a healthy pregnancy and allows your doctor to regularly monitor you and your baby . But what should you expect when it comes to your prenatal visit schedule?
Basically, you’ll visit your doctor once a month at the beginning of your pregnancy and then once a week at the end of your pregnancy. That said, it’s important to schedule your first prenatal visit as soon as you see a positive pregnancy test!
In this article, the experts at Mustela discuss how your prenatal visit schedule will most likely look and what to expect during each appointment.
Prenatal Visit Schedule: First Trimester

This is such an exciting time in your life! When you saw the positive pregnancy test , you were probably four to six weeks pregnant, so go ahead and call your doctor to schedule your first appointment.
During the first trimester , you will have your initial prenatal visit, and then your doctor will schedule your visits every four weeks or once a month.
Check with the doctor or staff for a printout of your prenatal visit schedule.
What To Expect At Your First Appointment
Your first prenatal visit will be around six to nine weeks and will most likely be the lengthiest of all your appointments, so block out a good bit of time on your calendar.
Your doctor will ask a good bit of detailed questions and perform a pretty thorough check. Let’s take a look at what they’ll do during this appointment.
Medical History
Your doctor will ask questions about your:
- Last menstrual cycle so they can give you a due date
- Gynecological history
- Obstetrical history (any past pregnancies)
- Personal and family medical history
- Supplements or medicines you’re taking (if any)
- Lifestyle (use of tobacco products, alcohol, and caffeine; eating and exercising habits)
- Recent travel adventures
- Feelings of depression or anxiety (if any)
Your doctor will order various lab work to check your blood for:
- Blood type and Rh status
- Hemoglobin levels
- Infections such as hepatitis B, syphilis, gonorrhea, chlamydia, and HIV
- Thyroid levels
- Any other important screenings
Physical Exam
To give you and your baby the best care, your doctor will need to do a thorough physical exam, which most likely will also include a Pap smear to detect any abnormal cervical cells.
Your doctor’s observation also includes:
- Checking your blood pressure
- Measuring your height and weight to determine your recommended weight gain for a healthy pregnancy
- A breast exam
- A pelvic exam
- Screening your heart, lungs, and thyroid
Discuss any pregnancy discomforts , such as nausea and fatigue, with your doctor. Be honest with your doctor so they can take care of you and your baby to the best of their knowledge.

Some doctors also do an ultrasound during the first trimester to confirm or date your pregnancy. (Your first prenatal visit will vary based on the specific policies of your doctor’s office.)
What To Expect At Your 12-Week Appointment
You're nearing the end of your first trimester! During this appointment, you can expect your doctor to check the following:
- Weight and blood pressure
- Urine for sugar and protein levels
- Your baby’s heartbeat (This will be the first time you’ll hear it!)
- Size of your uterus
- Hands and feet for any swelling
Prenatal Visit Schedule: Second Trimester

Assuming you have a healthy pregnancy and no further examinations are necessary, this is what your prenatal visit schedule will look like during your second trimester :
- Four-month appointment (around 16 weeks)
- Five-month appointment (around 20 weeks)
- Six-month appointment (around 24 weeks)
What To Expect During Routine Appointments
Many of your appointments from here on out will look similar regarding what your doctor will check for. During these visits, you can expect your doctor to look at:
- Your baby’s heartbeat
- Your fundal height (The size of your uterus is used to assess fetal growth and development. Your doctor will get this measurement by measuring the length from the top of your uterus to the top of your pubic bone. This measurement should match how many weeks you are. Example: If you’re 20 weeks pregnant, your fundal height should equal 20 centimeters.)
- Hands and feet for swelling
- Any symptoms you’ve been experiencing
At this point in your pregnancy, you may notice your skin becoming dry and starting to stretch a bit. Don’t worry; it’s completely normal!
To tackle dry skin, try Mustela’s Stretch Marks Cream . This velvety, hard-working cream delivers immediate moisture and comfort to your skin!
And our Stretch Marks Oil treats recently formed stretch marks. It’s a fast-absorbing oil that hydrates your skin throughout your pregnancy!
What To Expect During Your 20-Week Sonogram:
Sometime around your 20-week appointment, your doctor will schedule an ultrasound to determine the gender of your baby! During this sonogram, your sonographer will take a look at:
- Baby’s size and all their major organs
- Amniotic fluid
- Location of placenta
Your sonographer passes this information to your doctor to give them a clear picture (literally!) of the overall health of your baby and your pregnancy.
Prenatal Visit Schedule: Third Trimester

During your third trimester , your prenatal visits will be every two weeks until the last month of your pregnancy, when you’ll have them every week. So that means your prenatal visit schedule will look like this:
What To Expect At Your Seventh- and Eighth-Month Visits
During your seventh and eighth months of pregnancy, expect your doctor to check the following:
- Urine for sugar and protein
- Your fundal height (top of your uterus)
- Size and position of your baby
- Feet and hands for swelling
- Varicose veins in your legs
- Glucose screen test (read below for more information)
- Group B strep test (read below for more information)
- Blood test for anemia
- Any symptoms you’ve been having

Glucose Screen Test
This test is used to determine if you have gestational diabetes. Once you arrive at your doctor’s office, be prepared to have your blood drawn first.
Next, you’ll drink a very sugary drink that tastes like flat orange soda. Some women enjoy the taste, while others feel a little queasy afterward!
After you consume the entire drink, you’ll wait one hour before having your blood drawn again. If your blood work comes back with elevated numbers, your doctor will order the next level of tests, which is used to officially diagnose gestational diabetes.
Should you need to take the second test (no studying required!), you’ll have to fast before the appointment. Just like with the initial round of tests, your doctor will draw your blood first and then have you consume the drink.
The only difference is this time, your blood will be drawn every hour for three hours. Be prepared to stay in your doctor’s office for three to four hours.
If the results from this test also come back elevated, your doctor will discuss management techniques for gestational diabetes.
But don’t let this information worry you. Most women who monitor their blood sugar levels and work closely with their doctor have perfectly normal pregnancies and healthy babies!

Group B Strep Test
Group B Strep (GBS) is bacteria that can be found in the vaginas of healthy women. (It’s not related to strep, the throat infection.)
If you are a carrier of GBS, your baby can catch the infection during delivery when they pass through the birth canal. While this bacteria isn’t harmful to you, it can be dangerous for your baby.
To check for GBS, your doctor will perform a test just like they would a Pap smear. If the test shows that you’re a carrier, you’ll receive antibiotics through an IV once you’re in labor. This way, you won’t pass the infection to your baby!
You’re routinely tested for GBS around the seventh or eighth month of pregnancy so your doctors can be prepared to give you the antibiotics at the onset of labor.
What To Expect During Your Ninth Month
Similar to months seven and eight, your doctor will closely monitor you and your baby during this time. Since you’re getting closer to your due date, expect a few additional observations from your doctor.
During your last month of pregnancy, they will take a look at:
- Your cervix by an internal examination to check for effacement (thinning) and dilation (opening)
- Baby’s heartbeat
- Baby’s size (At this point in your pregnancy, your doctor may give you an estimation of your baby’s weight. They can tell your baby’s presentation: head or bottom first, and their position: front- or rear-facing.)
- Any questions or concerns you may have about delivery
A Beautiful Pregnancy And Beautiful Skin

Throughout these nine months , your prenatal visits are special moments of checking on your sweet little baby. It’s exciting to see your belly grow with each visit! But that also means possible stretch marks.
The good news is that Mustela offers a line of prenatal products, including our Stretch Marks Cream and Bust Firming Serum , to soothe and hydrate your skin while you manage the busyness of your prenatal visit schedule.
Let Mustela help you start your beautiful pregnancy with beautiful skin!

Suggested Articles

6 Tips For Finding The Best Maternity Clothes

7 Breastfeeding Myths & Realities

The Best Postpartum Care Plan For New Mothers
Get tips, news and exclusive offers
- Choosing a selection results in a full page refresh.
- Press the space key then arrow keys to make a selection.
Appointments at Mayo Clinic
- Pregnancy week by week
Prenatal care: 1st trimester visits
Pregnancy and prenatal care go hand in hand. During the first trimester, prenatal care includes blood tests, a physical exam, conversations about lifestyle and more.
Prenatal care is an important part of a healthy pregnancy. Whether you choose a family physician, obstetrician, midwife or group prenatal care, here's what to expect during the first few prenatal appointments.
The 1st visit
When you find out you're pregnant, make your first prenatal appointment. Set aside time for the first visit to go over your medical history and talk about any risk factors for pregnancy problems that you may have.
Medical history
Your health care provider might ask about:
- Your menstrual cycle, gynecological history and any past pregnancies
- Your personal and family medical history
- Exposure to anything that could be toxic
- Medications you take, including prescription and over-the-counter medications, vitamins or supplements
- Your lifestyle, including your use of tobacco, alcohol, caffeine and recreational drugs
- Travel to areas where malaria, tuberculosis, Zika virus, mpox — also called monkeypox — or other infectious diseases are common
Share information about sensitive issues, such as domestic abuse or past drug use, too. This will help your health care provider take the best care of you — and your baby.
Your due date is not a prediction of when you will have your baby. It's simply the date that you will be 40 weeks pregnant. Few people give birth on their due dates. Still, establishing your due date — or estimated date of delivery — is important. It allows your health care provider to monitor your baby's growth and the progress of your pregnancy. Your due date also helps with scheduling tests and procedures, so they are done at the right time.
To estimate your due date, your health care provider will use the date your last period started, add seven days and count back three months. The due date will be about 40 weeks from the first day of your last period. Your health care provider can use a fetal ultrasound to help confirm the date. Typically, if the due date calculated with your last period and the due date calculated with an early ultrasound differ by more than seven days, the ultrasound is used to set the due date.
Physical exam
To find out how much weight you need to gain for a healthy pregnancy, your health care provider will measure your weight and height and calculate your body mass index.
Your health care provider might do a physical exam, including a breast exam and a pelvic exam. You might need a Pap test, depending on how long it's been since your last Pap test. Depending on your situation, you may need exams of your heart, lungs and thyroid.
At your first prenatal visit, blood tests might be done to:
- Check your blood type. This includes your Rh status. Rh factor is an inherited trait that refers to a protein found on the surface of red blood cells. Your pregnancy might need special care if you're Rh negative and your baby's father is Rh positive.
- Measure your hemoglobin. Hemoglobin is an iron-rich protein found in red blood cells that allows the cells to carry oxygen from your lungs to other parts of your body. Hemoglobin also carries carbon dioxide from other parts of your body to your lungs so that it can be exhaled. Low hemoglobin or a low level of red blood cells is a sign of anemia. Anemia can make you feel very tired, and it may affect your pregnancy.
- Check immunity to certain infections. This typically includes rubella and chickenpox (varicella) — unless proof of vaccination or natural immunity is documented in your medical history.
- Detect exposure to other infections. Your health care provider will suggest blood tests to detect infections such as hepatitis B, syphilis, gonorrhea, chlamydia and HIV , the virus that causes AIDS . A urine sample might also be tested for signs of a bladder or urinary tract infection.
Tests for fetal concerns
Prenatal tests can provide valuable information about your baby's health. Your health care provider will typically offer a variety of prenatal genetic screening tests. They may include ultrasound or blood tests to check for certain fetal genetic problems, such as Down syndrome.
Lifestyle issues
Your health care provider might discuss the importance of nutrition and prenatal vitamins. Ask about exercise, sex, dental care, vaccinations and travel during pregnancy, as well as other lifestyle issues. You might also talk about your work environment and the use of medications during pregnancy. If you smoke, ask your health care provider for suggestions to help you quit.
Discomforts of pregnancy
You might notice changes in your body early in your pregnancy. Your breasts might be tender and swollen. Nausea with or without vomiting (morning sickness) is also common. Talk to your health care provider if your morning sickness is severe.
Other 1st trimester visits
Your next prenatal visits — often scheduled about every four weeks during the first trimester — might be shorter than the first. Near the end of the first trimester — by about 12 to 14 weeks of pregnancy — you might be able to hear your baby's heartbeat with a small device, called a Doppler, that bounces sound waves off your baby's heart. Your health care provider may offer a first trimester ultrasound, too.
Your prenatal appointments are an ideal time to discuss questions you have. During your first visit, find out how to reach your health care team between appointments in case concerns come up. Knowing help is available can offer peace of mind.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Lockwood CJ, et al. Prenatal care: Initial assessment. https://www.uptodate.com/contents/search. Accessed July 9, 2018.
- Prenatal care and tests. Office on Women's Health. https://www.womenshealth.gov/pregnancy/youre-pregnant-now-what/prenatal-care-and-tests. Accessed July 9, 2018.
- Cunningham FG, et al., eds. Prenatal care. In: Williams Obstetrics. 25th ed. New York, N.Y.: McGraw-Hill Education; 2018. https://www.accessmedicine.mhmedical.com. Accessed July 9, 2018.
- Lockwood CJ, et al. Prenatal care: Second and third trimesters. https://www.uptodate.com/contents/search. Accessed July 9, 2018.
- WHO recommendations on antenatal care for a positive pregnancy experience. World Health Organization. http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/anc-positive-pregnancy-experience/en/. Accessed July 9, 2018.
- Bastian LA, et al. Clinical manifestations and early diagnosis of pregnancy. https://www.uptodate.com/contents/search. Accessed July 9, 2018.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 1st trimester pregnancy
- Can birth control pills cause birth defects?
- Fetal development: The 1st trimester
- Implantation bleeding
- Nausea during pregnancy
- Pregnancy due date calculator
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Prenatal care 1st trimester visits
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
- Search Please fill out this field.
- Newsletters
- Sweepstakes
- Labor & Delivery

What to Do When You're 40 Weeks Pregnant With No Sign of Labor
Being 40 weeks pregnant with no signs of labor can be stressful—but try not to worry. We turned to experts to learn more about how to cope.
- What to Know About Due Dates
Risks of Going Past Your Due Date
- What Happens When You're Overdue
- Will I Need to Be Induced?
- Will I Need a C-Section?
- Things to Do While Waiting
GETTY IMAGES
When you're pregnant and waiting for your baby to join the world, those last few weeks can feel like they drag on forever. And if you're 40 or more weeks pregnant , the waiting game can feel exponentially challenging. But what should you do when you're overdue, contractions have yet to start, and there's no sign of labor ?
We turned to experts to learn more about due dates, things you can do to coax labor along, and when you should consider calling a health care provider for help.
Remember That Due Dates Are Just an Estimate
Bear in mind that it's impossible to predict the exact day a baby will be born, just as it's hard to pinpoint the exact age of a fetus. Due dates ultimately are just an estimate.
"No one should feel nervous or anxious if they're still pregnant past their due date," says Alex C. Vidaeff, MD, MPH , an OB-GYN and maternal-fetal medicine researcher and practitioner at Texas Children's Hospital in Houston.
Doctors and midwives use several methods to calculate their best estimate of a due date, including:
- Menstruation : The most common method of estimation is based on the first day of your last menstrual period (LMP).
- Conception : This estimation is based on the time your baby was likely conceived. You might also the embryo transfer date if doing IVF .
- Fundal height : A clinical examination of the uterus can help estimate the age of the fetus.
- Ultrasound : During early pregnancy, your doctor can estimate fetal age based on an ultrasound . This method is not as effective in later trimesters.
Even so, the reality is that 80% of babies arrive between 38 and 42 weeks of pregnancy, so your due date window is much bigger than you might think. "You might really be 39 weeks when you think you're at 40," says Dr. Vidaeff, adding that pregnancy length is, in many cases, genetically determined.
You can also use our due date calculator to determine when your baby might arrive.
Fewer than one in 10 babies are officially overdue, which means that the baby is born after 42 weeks of pregnancy . However, delivery after 40 weeks may come with certain risks, and it's important to be mindful of them.
OB-GYNs and health care providers are aware of these potential outcomes, and they can advise you accordingly if your due date has come and gone. "We now change our clinical practices at 40 weeks to prevent potential complications," explains Carri R. Warshak, MD , an OB-GYN and professor in the department of maternal-fetal medicine at the University of Cincinnati.
While they're rare, complications associated with being overdue include:
- Reduced placenta function : The placenta's ability to provide the baby with adequate oxygen and nutrients may be compromised.
- Decreased amniotic fluid levels : The volume of essential amniotic fluid may decline as the baby grows, which increases the possibility of a pinched umbilical cord.
- Fetal distress : The risk of fetal distress increases.
- Fetal macrosomia : The baby could grow too large to pass safely through the birth canal.
I'm 40 Weeks Pregnant and Overdue—What Happens Next?
At the 40-week mark, a health care provider will become more vigilant about monitoring the overdue baby. "Expect twice-a-week visits if you go past 40 weeks," says Sheryl A. Ross, MD , an OB-GYN in private practice in Santa Monica, California. Methods that a prenatal health care provider can use to monitor your post-term baby's condition include the following:
A "kick count" is a record you keep of how often your baby moves. A health care provider will tell you to contact them immediately should you notice your baby suddenly decreases their movements. This could be a sign of fetal distress, requiring immediate testing to determine your baby's condition and assess whether delivery should be initiated quickly.
Nonstress test
Nonstress tests, a type of electronic fetal monitoring, use a special instrument to measure how your baby's heart reacts when its body moves. With the results, your health care provider can determine if your baby is in distress.
Contraction stress test
When your uterus contracts, this test (which is another form of electronic fetal monitoring) measures your baby's heart rate with a special instrument. It helps determine your baby's condition during labor and allows your doctor to see if there's any fetal distress.
A physician can determine your baby's size , position, respiratory rate, heartbeat, and body movements with an ultrasound. Ultrasound can also gauge how much amniotic fluid surrounds your baby. Insufficient amniotic fluid for prolonged periods can cause labor complications.
In addition, a health care provider can assess the size and position of the placenta using ultrasound. This information is important because the placenta provides your baby with life-sustaining oxygen. Plus, "if the fetus weighs more than 8 pounds, 13 ounces, you may have difficulty pushing during labor , and using a forceps or vacuum may be necessary for delivery," says Dr. Warshak.
If I'm 40 Weeks Pregnant With No Signs of Labor. Will I Need to Be Induced?
After 39 or 40 weeks, it's sometimes best to deliver sooner rather than later. Studies have shown that newborn admissions to the neonatal intensive care unit (NICU) increase slightly when a baby is overdue. And stillbirth, though rare, becomes slightly more common as the pregnancy progresses past the due date.
If labor hasn't started spontaneously, you'll probably be induced between 41 to 42 weeks. "If your cervix has started to dilate , odds are in your favor for a successful induction," says Dr. Warshak.
Whether or not you'll be induced depends on your own health, the status of your cervix, and the baby's well-being as determined by a non-invasive procedure called fetal non-stress testing.
The conditions inside your uterus past the due date may also stress the baby during labor and vaginal delivery. As a result, says Dr. Warshak, "Even if your cervix is at 8 centimeters and labor is progressing, we'll do a C-section if the overdue baby is not tolerating labor well."
If I'm 40 Weeks Pregnant With No Signs of Labor, Will I Need a C-Section?
An ongoing concern has been whether induction, as opposed to what's known as expectant management (waiting for labor to start spontaneously while monitoring the parent and baby's well-being), might lead to a higher risk for emergency C-section , and research has been conflicting.
However, a comprehensive study funded by the National Institutes of Health found that inducing labor at week 39 is not connected with higher C-section rates, compared with waiting for labor to begin spontaneously. In fact, researchers found that the rate of surgical intervention was lower in the group that was induced by a rate of 18.6%, compared with 22.2% for the expectant management group.
Things To Do While Waiting for an Overdue Baby
At 40 weeks pregnant with no sign of labor, you're likely tired of the aches and pains of pregnancy, and you're eager to hold your baby in your arms. Here are some things to do while you wait.
Get a massage
Some Eastern healers believe that certain pressure points on the hands and feet may stimulate the body's natural labor process, although Dr. Ross says this hasn't been proven. Even if you can't get your tired body to a prenatal massage therapist, asking your partner to give you a rubdown might help your aching back, not to mention your mood.
Eat spicy food
Sadly, there's no magic meal that's guaranteed to bring on labor. Still, Dr. Ross has had several clients report that things, ahem, got moving after they indulged in a spicy meal.
Spicy foods fall into that "can't hurt, might help" category, and we say that once you're more than 40 weeks pregnant with no signs of labor, go ahead and eat your baby's weight in your favorite spicy food.
Have an orgasm (or two!)
The hormone oxytocin surges when you have an orgasm, which can trigger labor in at-term individuals. So, the more orgasms, the better!
Keep moving
We're not saying that exercising is easy when you're 40 weeks pregnant with a baby overdue, but try to stay active. Although stretching, doing prenatal yoga , or going for a short walk isn't likely to bring on labor, they're all good for you and your baby. (But don't overdo it: If you do go into labor, you don't want to be tuckered out from the get-go!)
Make good use of your time
If your baby is overdue, take advantage of the time to rest, finish the nursery, and stock your freezer with ready-made meals. Also, consider addressing birth announcements and thank-you notes.
Key Takeaway
It can be frustrating or disappointing when your due date comes and goes, and you're still pregnant. But don't worry, you'll be in labor—and your little one will be in your arms—before you know it. In the meantime, enjoy your last days of pregnancy (as best you can) and consult your doctor and/or midwife about any concerning symptoms or questions you have.
Methods for Estimating the Due Date . American College of Obstetricians and Gynecologists . 2017.
Constructing the uncertainty of due dates . Health Communication . 2014.
Pregnancy and Birth: When Your Baby’s Due Date Has Passed . Institute for Quality and Efficiency in Health Care (IQWiG); 2018.
When Pregnancy Goes Past Your Due Date . American College of Obstetricians and Gynecologists . Updated 2021.
Sonography Evaluation of Amniotic Fluid . StatPearls [Internet]. Updated 2023.
Stanford Medicine Children's Health. The Neonatal Intensive Care Unit (NICU).
Risk of stillbirth and infant death stratified by gestational age . Obstet Gynecol . 2012.
Labor induction doesn’t always reduce caesarean birth risk or improve outcomes for term pregnancies. University of Michigan Medicine . 2023.
Labor Induction versus Expectant Management in Low-Risk Nulliparous Women . N Engl J Med . 2018.
Related Articles

- Pregnancy Classes

Your First Prenatal Visit
If you did not meet with your health care provider before you were pregnant, your first prenatal visit will generally be around 8 weeks after your LMP (last menstrual period ). If this applies to you, you should schedule a prenatal visit as soon as you know you are pregnant!
Even if you are not a first-time mother, prenatal visits are still important since every pregnancy is different. This initial visit will probably be one of the longest. It will be helpful if you arrive prepared with vital dates and information. This is also a good opportunity to bring a list of questions that you and your partner have about your pregnancy, prenatal care, and birth options.
What to Expect at Your First Pregnancy Appointment
Your doctor will ask for your medical history, including:.
- Medical and/or psychosocial problems
- Blood pressure, height, and weight
- Breast and cervical exam
- Date of your last menstrual period (an accurate LMP is helpful when determining gestational age and due date)
- Birth control methods
- History of abortions and/or miscarriages
- Hospitalizations
- Medications you are taking
- Medication allergies
- Your family’s medical history
Your healthcare provider will also perform a physical exam which will include a pap smear , cervical cultures, and possibly an ultrasound if there is a question about how far along you are or if you are experiencing any bleeding or cramping .
Blood will be drawn and several laboratory tests will also be done, including:
- Hemoglobin/ hematocrit
- Rh Factor and blood type (if Rh negative, rescreen at 26-28 weeks)
- Rubella screen
- Varicella or history of chickenpox, rubella, and hepatitis vaccine
- Cystic Fibrosis screen
- Hepatitis B surface antigen
- Tay Sach’s screen
- Sickle Cell prep screen
- Hemoglobin levels
- Hematocrit levels
- Specific tests depending on the patient, such as testing for tuberculosis and Hepatitis C
Your healthcare provider will probably want to discuss:
- Recommendations concerning dental care , cats, raw meat, fish, and gardening
- Fevers and medications
- Environmental hazards
- Travel limitations
- Miscarriage precautions
- Prenatal vitamins , supplements, herbs
- Diet , exercise , nutrition , weight gain
- Physician/ midwife rotation in the office
Possible questions to ask your provider during your prenatal appointment:
- Is there a nurse line that I can call if I have questions?
- If I experience bleeding or cramping, do I call you or your nurse?
- What do you consider an emergency?
- Will I need to change my habits regarding sex, exercise, nutrition?
- When will my next prenatal visit be scheduled?
- What type of testing do you recommend and when are they to be done? (In case you want to do research the tests to decide if you want them or not.)
If you have not yet discussed labor and delivery issues with your doctor, this is a good time. This helps reduce the chance of surprises when labor arrives. Some questions to ask include:
- What are your thoughts about natural childbirth ?
- What situations would warrant a Cesarean ?
- What situations would warrant an episiotomy ?
- How long past my expected due date will I be allowed to go before intervening?
- What is your policy on labor induction?
Want to Learn More?
- Sign up for our weekly email newsletter
- Bonding With Your Baby: Making the Most of the First Six Weeks
- 7 Common Discomforts of Pregnancy
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Leg Cramps During Pregnancy

Prenatal Vitamin Limits

Skin Changes During Pregnancy
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
- Pregnancy Symptoms Week 40
- Pregnancy Checklist
Highlights this week
You made it.
Congratulations – you made it to your due date! Your pregnancy is full term and your baby is fully developed and ready to meet you.
How to get labor going
Natural ways to induce labor aren't proven to work – and some can be dangerous. But there are two methods that are worth a try: walking and having sex (if sex is still safe and comfortable for you). There's no solid proof that these will start your labor, but they could help, and you may enjoy them!
Staying positive
If you're anxious about going through labor or having a C-section , or frustrated with being hugely pregnant, practice a few helpful pregnancy affirmations . "I trust my body to know what to do" and "I am capable of amazing things" are good ones to start with.
Baby development at 40 weeks
How big will your baby be.
It's hard to say for sure, but the average baby weight for newborns in the United States is between 7 and 8 pounds. The average length is about 20 inches.
Your baby's skin color
Babies of all ethnicities are born with reddish-purple skin that changes to pinkish-red in a day or so. The pink tint comes from the red blood vessels that are visible through your baby's skin . Because your baby's blood circulation is still maturing, their hands and feet may be bluish for a few days. Babies of darker-skinned parents typically have lighter skin that gains pigment over time. Around 6 months old, your baby's skin will reach its permanent color.
Your baby's skull isn't one large bone, like an adult's. It starts out as separate bones joined by flexible tissue. After your baby is born, you'll be able to feel the soft spots between the bones, called fontanels, on the top and back of your newborn's head.

Your baby is about the size of a small pumpkin
Pregnancy symptoms during week 40.
Ripening cervix
Your healthcare provider may check your cervix to see if it's "ripening." Its condition – how soft, thinned out, and dilated (open) it is – can be a sign that labor's near . Still, it's not a sure-fire predictor of labor, so don't get too disappointed if you don't have the progress you're hoping for. On the other hand, labor can still be many days away even if you've begun to dilate and efface.
Water breaking
In the movies, labor usually starts with a big, dramatic gush of water hitting the floor. But the truth is, you don't have to worry about your water breaking in a sudden and cinematic fashion. Less than 15 percent of women have their water break before other symptoms of labor start. For the vast majority, their water breaks once contractions are already in progress. In short, don't stress about your water bursting while you're wrapping things up at work or making one last dash to the grocery store.
If you're in the minority and your water does break before labor, this is known as premature rupture of membranes, or PROM . Usually, labor will begin within 24 hours of your water breaking. If it doesn't happen naturally, your provider may induce labor.
Your water breaking isn't always obvious – in fact, you could have a slow leak of amniotic fluid. It may even be hard to tell whether what you're seeing is amniotic fluid, discharge, or pee. This is where your senses can come in handy: pee is typically yellow-hued, while vaginal discharge is often creamy or white. Amniotic fluid should be clear and have a slightly sweet smell.
If you've gotten close and personal and still aren't sure whether your water broke, put on a pad and wait half an hour. If the pad is wet after that time, it's likely the liquid is amniotic fluid.
If your water breaks, or even if you think it might have, call your doctor or midwife.
Now that you're full-term, your baby likely weighs 7 to 8 pounds and is the size of a small pumpkin. That weight, plus the additional pounds from your placenta, fluid, and breasts will continue to put more and more strain on your back. It's no wonder that more than 60 percent of pregnant women experience back pain .
Find relief any way you can. Swimming or floating; getting a massage; and doing some easy, gentle stretching and walking can ease your discomfort.
If you experience any sudden changes to your back pain (for example, it gets much worse, or starts up for the first time), this may be a sign that labor has started. Intense back pain during labor (called back labor ) usually means that your baby's head is pressing against your lower back, though one theory suggests that the pain may be "referred" from your uterus to your lower back.
Contractions
At 40 weeks, you're probably very familiar with Braxton Hicks contractions. But how can you tell so-called "false labor" from the real thing?
There are some easy ways to tell the difference between Braxton Hicks and real labor contractions. For starters, Braxton Hicks are usually not painful, and they don't get closer together. If you drink water and rest, they'll probably stop, at least for now. You'll feel Braxton Hicks on the front of your belly most often, whereas real contractions often start in the back and radiate around to the front.
Unlike Braxton Hicks, real contractions are painful. They'll arrive at regular intervals, getting closer together and more intense over time. And real contractions will persist, even if you lie down, take a bath, or find another way to relax.
Once you've started having real contractions, follow your provider's advice about when to go to the hospital for labor . Usually, it's time to go when you've had contractions at regular intervals (such as every four or five minutes) that last about a minute each, for an hour or more.
Having trouble sleeping? Insomnia is incredibly common now – it affects about two-thirds of women by late pregnancy.
Coping with insomnia can be hard, especially when you know that you'll have more sleepless nights once your baby is here. Having a consistent bedtime routine may help. Using tons of pillows to get in a comfortable sleep position, snoozing in a lounge chair, and taking naps during the day are all perfectly acceptable if they help you get enough sleep.
Pelvic pain and pressure
As your baby continues to drop lower in preparation for their grand entrance, you're likely noticing more pelvic pain and pressure . This can feel like tightness or pain in your hips, groin, and pelvic floor.
Resting, icing, and sitting in more comfortable positions (if you can find them) might help. If the pain is severe, talk to your provider about other options for pain relief.
By now, your baby has probably dropped. That means their head is engaged in your pelvis. This is known as " lightening ," since some women feel lighter once their baby has descended. Others, however, experience even more pelvic pain once their baby has dropped.
Thanks to lightening, you may find yourself waddling even more than before. And you'll probably take more frequent trips to the bathroom to go pee. The silver lining? Since your lungs have more room to expand, you can take a nice, deep breath.
Don't see your symptom?
Wondering about a symptom you have? Find it on our pregnancy symptoms page .

Pregnancy checklist at 40 weeks
Do some exercises to prepare for labor.
There's nothing you can do to make labor go faster, but simple exercises might help your body get ready for the effort ahead. Doing these exercises to help with labor may help you feel better now and once you're ready to deliver your baby.
Finalize your baby names list
Waiting until you meet your baby to make a final decision on names? That's fine! But make sure you have some good baby name options ready to go.
Learn what will happen after birth
Take time to learn about what happens to your baby after delivery , and what to expect at the hospital or birth center. While you're at it, review your birth plan – you'll be needing it very soon.
Kick back and relax
Watch your favorite shows, read a novel, call an old friend, sleep in, or take naps when you can. It won't be long until your baby is here.
40 weeks pregnant bellies
After months of anticipation, your due date rolls around, and ... you're still pregnant. It's a frustrating but common situation. You may not be as late as you think, especially if you're relying solely on a due date calculated from the day of your last period. (That's because sometimes women ovulate later than expected.) But even with reliable calculations, some women go past their due date . It's especially likely if you're a first-time mom.
If you don't go into labor soon, your provider may order tests to check on your baby or induce labor . Some providers will recommend induction once you reach 41 weeks. Though the risk of some complications increases with overdue pregnancies, most "late" babies and their moms do just fine.

This week's video
BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
ACOG. 2021. How your fetus grows during pregnancy. American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/how-your-fetus-grows-during-pregnancy Opens a new window [Accessed January 2023]
ACOG. 2022. Induction of Labor at 39 Weeks. American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/induction-of-labor-at-39-weeks Opens a new window [Accessed January 2023]
ACOG. 2021. When Pregnancy Goes Past Your Due Date. American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/when-pregnancy-goes-past-your-due-date Opens a new window [Accessed January 2023]
Cleveland Clinic. 2020. Fetal Development: Stages of Growth. https://my.clevelandclinic.org/health/articles/7247-fetal-development-stages-of-growth Opens a new window [Accessed January 2023]
Hadlock FP et al. 1991. In utero analysis of fetal growth: A sonographic weight standard. Radiology 181 (1). https://pubs.rsna.org/doi/10.1148/radiology.181.1.1887021 Opens a new window [Accessed January 2023]
Hadlock FP et al. 1992. Fetal cross-rump length: Reevaluation of relation to menstrual age (5-18 weeks) with high-resolution real-time US. Radiology 182: 5-1-505. https://pubmed.ncbi.nlm.nih.gov/1732970/ Opens a new window [Accessed January 2023]
Hadlock FP. 1984. Estimating fetal age: Computer-assisted analysis of multiple fetal growth parameters. Radiology 152: 497-501. https://pubmed.ncbi.nlm.nih.gov/6739822/ Opens a new window [Accessed January 2023]
Kerbsbach, Lacy. 2017. How to know if your water breaks. Sanford Health . https://news.sanfordhealth.org/womens/did-my-water-break/ Opens a new window [Accessed January 2023]
Mayo Clinic. 2021. Fetal development: The 3rd trimester. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/fetal-development/art-20045997 Opens a new window [Accessed January 2023]
MedlinePlus (ADAM). 2019. Fetal development. https://medlineplus.gov/ency/article/002398.htm Opens a new window [Accessed January 2023]
MedlinePlus (ADAM). 2022. Premature rupture of membranes. https://medlineplus.gov/ency/patientinstructions/000512.htm Opens a new window [Accessed January 2023]
Vintzileos AM et al. 1984. The ultrasound femur length as a predictor of fetal length. Obstetrics & Gynecology 64(6): 779-82. https://pubmed.ncbi.nlm.nih.gov/6390277/ Opens a new window [Accessed January 2023]

Kelly Burch is a freelance journalist covering health, entrepreneurship, family, and more. She's passionate about bringing complex topics to life through stories that are easy to read and informative. Burch lives in New Hampshire with her husband and two young daughters. When she's not at her desk, you'll find her kayaking or hiking in the wilderness around her home. Burch is currently writing a book about traveling around the United States in an RV with her family for seven months.
Relaxation tips to ease labor pain

Social Security numbers and why your baby needs one

The baby blues

How to swaddle a baby

Where to go next

Your First Prenatal Appointment
Medical review policy, latest update:.
Medically reviewed for accuracy.
When should I schedule my first prenatal visit?
When will my first prenatal visit take place, read this next, how should i prepare for my first pregnancy appointment, what will happen at my first prenatal visit, will i see my baby on an ultrasound at my first prenatal visit, updates history, jump to your week of pregnancy, trending on what to expect, signs of labor, pregnancy calculator, ⚠️ you can't see this cool content because you have ad block enabled., top 1,000 baby girl names in the u.s., top 1,000 baby boy names in the u.s., braxton hicks contractions and false labor.
Amid syphilis surge, doctors call for more testing during pregnancy

The nation’s largest coalition of obstetricians issued an urgent warning Thursday calling on doctors to expand testing for syphilis during pregnancy amid a surge of cases in recent years.
The American College of Obstetricians and Gynecologists updated its recommendations, advising a routine blood screening at the first prenatal visit and screenings in the third trimester of pregnancy and at birth. This contrasts with previous recommendations, which called for testing in the third trimester exclusively for individuals living in communities with high syphilis rates and for those at risk of syphilis exposure during pregnancy.
“We’re always trying to create healthier families, and some of the diseases that we can easily diagnose and treat are things that we should prioritize, especially when they can be devastating to a baby,” said Laura E. Riley, chair of the obstetrician coalition’s immunization work group. Riley helped write the guidance.
“Sometimes, it’s difficult to know that you’ve been exposed to syphilis, and it’s not like you can raise your hand and say, ‘I have this, please give me treatment,’ because you may not even know you have it,” said Riley, chair of obstetrics and gynecology at Weill Cornell Medicine in New York.
Rates of syphilis have been skyrocketing, with cases hitting their highest level since the 1950s. Reported syphilis cases increased 80 percent from 2018 to 2022 in the United States, soaring from about 115,000 cases to more than 207,000, according to the Centers for Disease Control and Prevention .
In 2022, more than 3,700 babies were born with syphilis, with 231 stillbirths and 51 infant deaths attributed to transmission of syphilis from pregnant people to their babies.
Experts say these rising numbers reflect decreased condom use and an uptick in substance use, The Washington Post reported.
Syphilis is a sexually transmitted infection caused by the bacterium Treponema pallidum. When a pregnant person is infected with syphilis, the infection can pose severe consequences for the pregnant individual and the unborn baby. Left untreated, syphilis can progress to advanced stages and damage organs and nerves.
It can also be transmitted to the fetus during pregnancy or at childbirth, resulting in congenital syphilis, which can lead to severe health problems for the baby, including premature birth, low birth weight, stillbirth, developmental delays and other complications.
Nicole Smith, medical director of maternal-fetal medicine at Brigham and Women’s Hospital in Boston, said that by calling for routine syphilis testing, the guidelines should prove to be a useful tool for physicians, especially when stigma surrounding sexually transmitted infections persists.
“Some populations are less likely to be either screened or treated … due to the locations where they’re receiving care or because there’s a concern among that population that they’re being stigmatized because they’re being tested,” Smith said.
“So if we say, ‘No, this is nothing about you in particular, this is something that we’re doing for every single pregnant person in this country … we’re treating everyone the same way,’ and therefore some of the barriers to appropriate treatment should be diminished or ideally removed,” she said.
A single injection of a long-acting dose of penicillin can cure early-stage syphilis.
If a person has late-latent syphilis or does not know how long they had the infection, the CDC suggests three doses of long-acting benzathine penicillin G, given weekly. While the treatment can eliminate the infection and stop more harm, it can’t undo damage that has already occurred.
Hurdles exist for syphilis patients, including getting access to testing and medication. Drug shortages — a long-standing issue for many medications — have contributed to rising syphilis cases, experts say.
In April 2023, the Food and Drug Administration announced a shortage of penicillin in the United States attributed to increased demand.
To combat the ongoing shortages, the FDA granted temporary approval for a French drug, Extencilline, which is used for syphilis treatment but is not FDA-approved. While the Food, Drug, and Cosmetic Act prohibits importing unapproved drugs into the United States, the secretary of Health and Human Services can authorize temporary importation and distribution of such drugs to address shortages until domestic production returns to normal levels.
Riley said the updated guidance from the obstetricians group is essential because it makes physicians aware of the alternative treatment for syphilis amid the shortage.
In June 2023, the maker of penicillin, Pfizer, said it would prioritize making the drug available, with the shortage expected to be relieved within the next few months of this year.


Video released of Israeli American hostage captured by Hamas

At least 34 arrested at UT Austin pro-Palestinian demonstration

Pro-Palestinian protest moves off campus as LAPD moves in

LAPD begins arresting protesters on USC campus

LAPD marches towards USC protesters
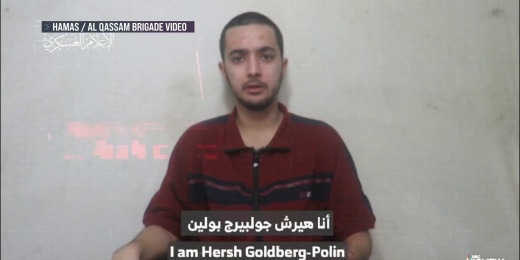
Hamas releases video of hostage Hersh Goldberg-Polin

New pro-Palestinian protests on campuses across the country

Johnson calls for Columbia University president to ‘bring order to this chaos’

What ‘telltale signs’ will indicate Israel’s military operation in Rafah?

‘It has to be stopped’: Netanyahu condemns U.S. college protests

Hersh Goldberg-Polin’s parents react to new Hamas hostage video

Brown University students join pro-Palestinian protests
Biden: Foreign aid package will 'make the world safer'

Columbia students representing Jewish and pro-Palestinian sides speak about protests

Pro-Palestinian protest grows at UC Berkeley campus

Senate passes $95 billion foreign aid package for Ukraine, Israel and Taiwan

Jewish student protesters say antisemitism is being weaponized against them

Pro-Palestinian encampments grow on college campuses in the U.S.

Heartbreak and hope as Gaza baby is delivered

Campus protests spread around the country
Watch: doctors save the baby of pregnant woman killed in an airstrike on rafah.
Doctors at Rafah's Kuwaiti Hospital performed an emergency cesarean section on a woman who was 30 weeks pregnant and had died in an Israeli airstrike. The newborn was later transferred to the city's Emirati Hospital for specialist care, where NBC News captured medical professionals tending to her. April 22, 2024
Best of NBC News
NBC News NOW
Kagan asks trump lawyer if a president calling for a coup is an official act.

NBC News Channel
One student killed, one in custody after texas school shooting.

Curtain Call: ‘El Niño’ makes its Metropolitan Opera debut with a retelling of the Nativity

Protesters demonstrate outside Supreme Court ahead of Trump immunity case

NFL Draft 2024: Here are the expected top picks

Venice launches 5-euro tourist entry fee to curb overcrowding

IMAGES
VIDEO
COMMENTS
Typical prenatal appointment schedule. The number of visits you'll have in a typical pregnancy usually total about 10 to 15, depending on when you find out you're expecting and the timing of your first checkup. In most complication-free pregnancies, you can expect to have a prenatal appointment with the following frequency: Weeks 4 to 28 ...
Visits #8-10: 38-40 weeks. By week 38, the big day will be close enough that your care team will start keeping closer track of your progress. Again, each pregnancy is different, but from this point on, you may have a prenatal appointment every week until you deliver. These visits will feel similar to the routine prenatal appointments you're ...
Weeks 4 to 28 — One prenatal visit every four weeks. Weeks 28 to 36 — One prenatal visit every two weeks. Weeks 36 to 40 — One prenatal visit every week. Each scheduled visit on the timeline ...
Here's what to expect at your first pregnancy appointment. A physical, which will likely include a breast and pelvic exam. A urine sample is collected to check for certain infections and conditions that can occur during pregnancy. Urine tests may be taken at your following prenatal visits as well. Urine drug screening tests are also ...
Check your weight, blood pressure, and urine. Check for swelling. Measure your abdomen. Check the position of your baby. Listen to your baby's heartbeat. Perform other exams and order tests, as appropriate. Give you the appropriate vaccinations. Closely monitor any complications you have or that you develop, and intervene if necessary.
For a healthy pregnancy, your doctor will probably want to see you on the following recommended schedule of prenatal visits: Weeks 4 to 28: 1 prenatal visit a month. Weeks 28 to 36: 1 prenatal ...
Overdue Pregnancy Visits . At 40 or 41 weeks of pregnancy, you may begin to see your midwife or doctor every few days. Here is what these visits may look like: Check your blood pressure; Listen for baby's heartbeat; Measure your fundal height to check baby's growth; Palpate to check baby's position (vertex, breech, posterior, etc.)
During your first trimester, your provider will check your blood to determine your blood type and look for signs of: Blood issues, such as anemia (low iron). Immunity to rubella (German measles ...
22 to 26 Weeks Prenatal Care Appointments. Dr. Chisholm explains that between 24 and 28 weeks of pregnancy, you can expect a glucose challenge screening test, which screens for gestational diabetes. You will be asked to drink a sweet liquid (glucose), wait one hour, and then have your blood drawn. The blood test examines how well your body ...
At 40 weeks pregnant, your baby may measure 14 1/4 inches (CRL), 20 1/4 inches in height, and weigh almost 8 pounds. Learn more about your symptoms and how your baby is growing this week. ... Doctor Visits. Special Considerations. At 40 weeks pregnant, you've reached the milestone everyone's been counting down to from the beginning. Hopefully ...
As with other visits, your doctor will: Check your weight and blood pressure. Measure the height of your uterus to gauge your baby's growth. Check your baby's heart rate. Ask if your baby's ...
Your first appointment will be the longest of your first trimester visits. At this initial visit, your healthcare provider will confirm your pregnancy and perform a full physical and pelvic exam. He or she will also do a Pap test to check for cervical cancer and vaginal infections. The staff will check your weight and blood pressure.
So that means your prenatal visit schedule will look like this: 28 weeks 30 weeks 32 weeks 34 weeks 36 weeks 37 weeks 38 weeks 39 weeks 40 weeks What To Expect At Your Seventh- and Eighth-Month Visits During your seventh and eighth months of pregnancy, expect your doctor to check the following: Weight and blood pressure Urine for sugar and ...
During the third trimester, prenatal care might include vaginal exams to check the baby's position. By Mayo Clinic Staff. Prenatal care is an important part of a healthy pregnancy, especially as your due date approaches. Your health care provider might ask you to schedule prenatal care appointments during your third trimester about every 2 or 4 ...
Currently, the Institute of Medicine recommends the following for moms of multiples based on BMI: A BMI between 18.5 and 24.9: 37 to 54 pounds. A BMI between 26 and 30: 31 to 50 pounds. A BMI greater than 30: gain 25 to 42 pounds. That said, everyone's pregnancy will look different and that includes pregnancy weight gain.
Prenatal care: 1st trimester visits. Pregnancy and prenatal care go hand in hand. During the first trimester, prenatal care includes blood tests, a physical exam, conversations about lifestyle and more. By Mayo Clinic Staff. Prenatal care is an important part of a healthy pregnancy. Whether you choose a family physician, obstetrician, midwife ...
Keep moving. We're not saying that exercising is easy when you're 40 weeks pregnant with a baby overdue, but try to stay active. Although stretching, doing prenatal yoga, or going for a short walk ...
Your First Prenatal Doctor's Visit. Medically Reviewed by Traci C. Johnson, MD on March 22, 2023. ... The first visit is designed to confirm your pregnancy and to determine your general health. In ...
If you did not meet with your health care provider before you were pregnant, your first prenatal visit will generally be around 8 weeks after your LMP (last menstrual period ). If this applies to you, you should schedule a prenatal visit as soon as you know you are pregnant! Even if you are not a first-time mother, prenatal visits are still ...
If you have any questions about labor or induction, you don't need to wait until your next appointment. However, at 40 weeks pregnant, you should contact your doctor immediately if you experience: Severe cramping. Vaginal bleeding. Unusual changes in vaginal discharge. Fever.
Pregnancy symptoms during week 40. Ripening cervix. Your healthcare provider may check your cervix to see if it's "ripening." Its condition - how soft, thinned out, and dilated (open) it is - can be a sign that labor's near.Still, it's not a sure-fire predictor of labor, so don't get too disappointed if you don't have the progress you're hoping for.
The most common tests at your first prenatal visit will likely include: [3] Urine test. Your urine may be checked for protein, glucose (sugar), white blood cells, blood and bacteria. Bloodwork. A sample of your blood will be used to determine blood type and Rh status and check for anemia. Trusted Source Mayo Clinic Rh factor blood test See All ...
The nation's largest coalition of obstetricians issued an urgent warning Thursday calling on doctors to expand testing for syphilis during pregnancy amid a surge of cases in recent years.
Doctors at Rafah's Kuwaiti Hospital performed an emergency cesarean section on a woman who was 30 weeks pregnant and had died in an Israeli airstrike. The newborn was later transferred to the city ...