

Star Excursion Balance Test
The Star Excursion Balance Test (SEBT) is a simple, but time intensive, test used to measure dynamic balance/dynamic postural control.
By Owen Walker Last updated: February 29th, 2024 8 min read
Contents of Article
What is the Star Excursion Balance Test?
Why is balance important in sports, how do you conduct the star excursion balance test, what is the star excursion balance test scoring system, is the star excursion balance test valid and reliable, further reading.
- About the Author
The Star Excursion Balance Test was developed to be a reliable measure of dynamic stability. Since then, it has proven to be a sensitive indicator of lower limb injury risk in a variety of populations. To add to this, the Star Excursion Balance Test has been shown to have high levels of intra-rater test-retest reliability , though no validity coefficients have been studied.
The Star Excursion Balance Test (SEBT) is a relatively simple, but somewhat time-intensive, test used to measure dynamic balance, otherwise known as dynamic postural control (1). It measures dynamic balance by challenging athletes to balance on one leg and reach as far as possible in eight different directions (2). Though the SEBT is very similar to the Y Balance Test TM , it is important to understand that these are in fact different, with the Y Balance Test TM being a newer and condensed version of the SEBT.
Performance on the SEBT has been shown to differentiate between individuals with lower limb conditions such as chronic ankle instability (3-10), patellofemoral pain (11), and anterior cruciate ligament reconstruction (12). To add to this, the SEBT is even capable of assessing improvements in dynamic balance following training interventions (13, 14).
Perhaps the SEBT’s greatest talent is its ability to identify athletes with a higher risk of lower limb injury. For example, an anterior reach asymmetry of greater than 4cm during the SEBT has been suggested to predict which individuals are at higher risk of lower limb injury (15). However, other researchers have found that only female athletes with a composite score of less than 94 % of limb length were at greater risk of injury (15). More recent research in collegiate American football players has shown that athletes with a composite score of less than 90 % are 3.5 times more likely to sustain an injury (16).
All of this information suggests that each sport and population (e.g. gender) appear to have their own injury risk cut-off point (15, 16).
Balance, otherwise known as ‘postural control’, can be defined statically as the ability to maintain a base of support with minimal movement, and dynamically as the ability to perform a task while maintaining a stable position (17, 18). In a chaotic sporting environment, the ability to maintain a stable position is vital not only for successful application of the skill but to also reduce the likelihood of injury (15, 16, 19).
As dynamic balance is an integral part of performance, and poor balance is related to a higher risk of injury (20, 21, 15), then it may be of great interest to test and monitor an athlete’s dynamic stability.
It is important to understand that whenever fitness testing is performed, it must be done so in a consistent environment (e.g. facility) so it is protected from varying weather types, and with a dependable surface that is not affected by wet or slippery conditions. If the environment is not consistent, the reliability of repeated tests at later dates can be substantially hindered and result in worthless data.
Required Equipment Before the start of the test, it is important to ensure you have the following items:
- Reliable and consistent testing facility (minimum 2×2 metres (m)).
- Test administrator(s)
- Sticky tape (minimum 8m)
- Measuring tape
- Performance recording sheet
Test Configuration Video 1 displays the test configuration for the SEBT. This setup must be adhered to if accurate and reliable data is desired. The test administrator should stick four 120 cm lengths of sticky tape onto the floor, intersecting in the middle, and with the lines placed at 45° angles (2).
Participants should thoroughly warm up prior to the commencement of the test. Warm-ups should correspond to the biomechanical and physiological nature of the test. In addition, sufficient recovery (e.g. 3-5 minutes) should be administered following the warm-up and prior to the commencement of the test.
Conducting the test
- The athlete should be wearing lightweight clothing and remove their footwear. After doing so, they are then required to stand in the centre of the star and await further instruction.
- When using the right foot as the reaching foot, and the left leg to balance, the athlete should complete the circuit in a clockwise fashion. When balancing on the right leg, the athlete should perform the circuit in an anti-clockwise fashion.
- With their hands firmly placed on their hips, the athlete should then be instructed to reach with one foot as far as possible and lightly touch the line before returning back to the starting upright position.
- With a pencil, the test administrator should mark the spot at which the athlete touched the line with their toe. This can then be measured from the centre spot after the test to calculate the reach distance of each reach direction. Reach distances should be recorded to the nearest 0.5cm (22).
- They should then repeat this with the same foot for all reach directions before changing foot.
- After they have completed a full circuit (every reach direction) with each foot, they should then repeat this process for a total of three times per leg. For example, they should have three anterior reach performances for both their right and left leg.
- Once the athlete has performed three successful reaches with each foot in all directions, they are then permitted to step away from the testing area.
- The test administrator should have recorded the reach distance of each successful attempt, with a pencil, in order to calculate the athlete’s SEBT score after the test.
NOTE: Failed attempts include the following:
- The athlete cannot touch their foot down on the floor before returning back to the starting position. Any loss of balance will result in a failed attempt.
- The athlete cannot hold onto any implement to aid their balance.
- The athlete must keep their hands on their hips at all times throughout the test.
- The athlete must lightly touch their toe on the reach line whilst staying in full control of their body. Any loss of balance resulting in a heavy toe/foot contact with the floor should be regarded as a failed attempt.
With the test complete and all performances measured and recorded, the test administrator can then calculate the athlete’s SEBT performance scores using the following simple equations (17):
- Average distance in each direction (cm) = Reach 1 + Reach 2 + Reach 3 / 3
- Relative (normalised) distance in each direction (%) = Average distance in each direction / leg length * 100
These calculations should be performed for both the right and left leg in each direction, providing you with a total of 16 scores per athlete.
Though no validity coefficients are available for the SEBT, authors (23) have provided evidence that the SEBT is sensitive for screening various musculoskeletal injuries (17). Furthermore, high intratester reliability has been found for the SEBT (intraclass correlation coefficients = 0.78 – 0.96) (24).
We suggest you now check out this article on The Landing Error Scoring System (LESS).
All information provided in this article is for informational and educational purposes only. We do not accept any responsibility for the administration or provision of any testing conducted, whether that results in any positive or negative consequences. As an example, we do not take any responsibility for any injury or illness caused during any test administration. All information is provided on an as-is basis.
- Nelson, Brian D., “Using the Star Excursion Balance test as a predictor of lower extremity injury among high school basketball athletes” (2012).Theses and Dissertations. Paper 389. [Link]
- Gribble PA, Kelly SE, Refshauge KM, Hiller CE. Interrater Reliability of the Star Excursion Balance Test. Journal of Athletic Training 2013;48(5):621–626. [PubMed]
- Akbari M, Karimi H, Farahini H, Faghihzadeh S. Balance problems after unilateral lateral ankle sprains. J Rehabil Res Dev. 2006;43(7): 819–824. [PubMed]
- Gribble PA, Hertel J, Denegar CR. Chronic ankle instability and fatigue create proximal joint alterations during performance of the Star Excursion Balance Test. Int J Sports Med. 2007;28(3):236–242. [PubMed]
- Gribble PA, Hertel J, Denegar CR, Buckley WE. The effects of fatigue and chronic ankle instability on dynamic postural control. J Athl Train. 2004;39(4):321–329. [PubMed]
- Hale SA, Hertel J, Olmsted-Kramer LC. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J Orthop Sport Phys Ther. 2007;37(6):303–311. [PubMed]
- Hertel J, Braham RA, Hale SA, Olmsted-Kramer LC. Simplifying the Star Excursion Balance Test: analyses of subjects with and without chronic ankle instability. J Orthop Sport Phys Ther. 2006;36(3):131– 137. [PubMed]
- Martinez-Ramirez A, Lecumberri P, Gomez M, Izquierdo M. Wavelet analysis based on time-frequency information discriminate chronic ankle instability. Clin Biomech (Bristol, Avon). 2010;25(3): 256–264. [PubMed]
- Nakagawa L, Hoffman M. Performance in static, dynamic, and clinical tests of postural control in individuals with recurrent ankle sprains. J Sport Rehabil. 2004;13(3):255–268. [Link]
- Olmsted LC, Carcia CR, Hertel J, Shultz SJ. Efficacy of the Star Excursion Balance Tests in detecting reach deficits in subjects with chronic ankle instability. J Athl Train. 2002;37(4):501–506. [PubMed]
- Aminaka N, Gribble PA. Patellar taping, patellofemoral pain syndrome, lower extremity kinematics, and dynamic postural control. J Athl Train. 2008;43(1):21–28. [PubMed]
- Herrington L, Hatcher J, Hatcher A, McNicholas M. A comparison of Star Excursion Balance Test reach distances between ACL deficient patients and asymptomatic controls. Knee. 2009;16(2):149–152. [PubMed]
- McKeon PO, Ingersoll CD, Kerrigan DC, Saliba E, Bennett BC, Hertel J. Balance training improves function and postural control in those with chronic ankle instability. Med Sci Sports Exerc. 2008; 40(10):1810–1819. [PubMed]
- McLeod TC, Armstrong T, Miller M, Sauers JL. Balance improvements in female high school basketball players after a 6- week neuromuscular-training program. J Sport Rehabil. 2009;18(4): 465–481. [PubMed]
- Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36(12):911–919. [PubMed]
- Butler RJ, Lehr ME, Fink ML, Kiesel KB, Plisky PJ. Dynamic balance performance and noncontact lower extremity injury in college football players: an initial study. Sports Health. 2013;5(5): 417–422. [PubMed]
- Bressel E, Yonker JC, Kras J, Heath EM. Comparison of Static and Dynamic Balance in Female Collegiate Soccer, Basketball, and Gymnastics Athletes. Journal of Athletic Training 2007;42(1):42–46. [PubMed]
- Winter DA, Patla AE, Frank JS. Assessment of balance control in humans. Med Prog Technol. 1990;16:31–51. [PubMed]
- Zazulak B, Cholewicki J, and Reeves NP. Neuromuscular control of trunk stability: Clinical implications for sports injury prevention. J Am Acad Orthop Surg 16: 497–505, 2008. [PubMed]
- de Noronha M, Franca LC, Haupenthal A, Nunes GS. Intrinsic predictive factors for ankle sprain in active university students: a prospective study [published online January 20, 2012]. Scan J Med Sci Sports. doi:10.1111/j.1600-0838.2011.01434. [PubMed]
- McGuine T. Sports injuries in high school athletes: a review of injury-risk and injury-prevention research. Clin J Sports Med. 2006;16:488-499. [PubMed]
- Shaffer SW, Teyhen DS, Lorenson CL, Warren RL, Koreerat CM, Straseske CA, Childs JD. Y-Balance Test: a reliability study involving multiple raters. Mil Med. 2013;178(11):1264-70. [PubMed]
- Olmstead L, Carcia C, Hertel J, Shultz S. Efficacy of star excursion balance test in detecting reach deficits in subjects with chronic ankle instability. Journal of Athletic Training. 2002;37(4):501-507. [PubMed]
- Hertel J, Miller S, Denegar C. Intratester and intertester reliability during the star excursion balance test. Journal of Sport Rehabilitation. 2000;9(1):104-116. [Link]

Access our course on Agility for FREE!
Learn how to improve your athletes' agility. This free course also includes a practical coaching guide to help you design and deliver your own fun and engaging agility sessions.
Owen Walker
Owen is the Founder of Science for Sport and has a Master’s degree in Strength & Conditioning and a Bachelor’s degree in Sports Conditioning & Rehabilitation from Cardiff Metropolitan University. Before founding Science for Sport, he was the Head of Academy Sports Science at Cardiff City Football Club, and an interim Sports Scientist for the Welsh Football Association.
He’s published research on the ‘Practical Applications of Water Immersion Recovery Modalities for Team Sports’ in the Strength & Conditioning Journal by the NSCA (National Strength & Conditioning Association). He has also been featured in the Sports Business Journal and The Roar, Australia’s leading sports opinion website.
Learn from a world-class coach how you can improve your athletes' agility. This course also includes a practical coaching guide to help you to design and deliver your own fun and engaging agility sessions.

Why we exist
Our mission is to improve the performance of athletes and teams around the world by simplifying sports science and making it practical.
Try out our Academy and access our growing library of sports science courses.
Pricing FAQs Reviews Free trial
Blog Courses Newsletter Community Podcast Tools
About us Contact us Join our team Privacy policy Terms of use Terms and conditions Disclaimer
© 2024 Science for Sport | Catapult Sports
- MMT Online Seminar
- MMT Insiders

- Online Mentoring
- Top Products
Star Excursion Balance Test & Dynamic Postural Control
- Anterior (ANT), posteromedial (PM) and posterolateral (PL) lines.
- Stand on the central point.
- Hands on hips.
- Reach as far as you can along the line and gently tap the line.
- Do not come to rest on the line.
- Do not transfer your body weight onto the reaching leg.
FACTORS AFFECTING PERFORMANCE
- Vastus medialis is most active in anterior reach.
- Vastus lateralis is least active in lateral reach.
- Medial hamstring is most active during anterolateral reach.
- Bicep femoris was most active during posterior and posterolateral reach.
WHAT DOES THE SEBT TELL US?
Chronic ankle instability (cai):.
- In CAI, all three directions have the ability to identify reach deficits in participants compared to healthy controls, however, the PM is the most representative of the overall performance (Hertel, Braham, Hale & Olmsted-Kramer., 2006).
- Anterior reach is more impacted by dorsiflexion ROM and plantar cutaneous sensation, meaning that mechanical restrictions and sensory deficits impact this movement.
- DF ROM is best evaluated with the knee to wall weight bearing lunge test compared to non weight bearing AROM (Dill et al., 2014).
- Posteromedial and posterolateral reach is more impacted by eversion strength and balance control.
- De la Motte, Arnold & Ross (2015) studied the movement pattern differences in trunk rotation and found that patients with CAI are more likely to use increased trunk flexion during anterior reach which suggests a compensation strategy for reduced ankle control is to manipulate the pelvis and trunk.
ANTERIOR CRUCIATE LIGAMENT RECONSTRUCTION (ACLR):
- The same authors (De la Motte, Arnold & Ross., 2015, p.358) also studied trunk movements in ACL patients and found that following an ACLR, when reaching forward, patients are more likely to rotate their trunk away (backwards) from the reach leg and externally rotate the pelvis on the stance leg.
- In a different study following ACLR, researchers found that when looking above the ankle and at the knee, patients with reduced quadricep strength have reduced reach capacity in the anterior directions (Clagg, Daterno, Hewett & Schmitt., 2015).
- These same authors also found that hip abductions strength impacts all 3 directions, telling us that dynamic balance has contributions from the foot, ankle, knee, hip and trunk and our assessment of movement patterns should try consider all these areas too.
PATELLOFEMORAL PAIN SYNDROME (PFPS):
IMPLEMENTATION INTO REHAB

REFERENCES:

Erson Religioso III, DPT, FAAOMPT
Post a comment, become a tmj/headache speciliast.

Eval, Reset, and Stabilize System

Get Certified in BFR Online!
Search for jobs.

IASTM Technique 2.0

EDGE Restriction System BFR Cuffs

Knee Rehab Done Right
Google workspace for emr.

Modern Manual Therapy Insiders
Featured Post
How to explain sij pain without using sij, rotation, or innominate.
One of the most frequently asked questions I get at Modern Manual Therapy courses is, "How do you explain SIJ dysfunction without us...
Total Pageviews
Blog archive.
- Dr. E's Private Network
- Dr. E's Shop
- Modern Manual Therapy
- EDGE Rehab and Sport Science
- Online Seminars
Unlimited CEUs

CashPT Blueprint

Copyright © 2023
Copyright 2015 Modern Manual Therapy Blog - Manual Therapy, Videos, Neurodynamics, Podcasts, Research Reviews | Designed by Veethemes.com
Star Excursion Balance Test
The Star Excursion Balance Test (SEBT) is a dynamic test that requires strength, flexibility, and proprioception. It is a measure of dynamic balance that provides a significant challenge to athletes and physically active individuals.
The test can be used to assess physical performance, but can also be used to screen deficits in dynamic postural control due to musculoskeletal injuries (e.g. chronic ankle instability), to identify athletes at greater risk for lower extremity injury, as well as during the rehabilitation of orthopedic injuries in healthy active adults (1)
Research has suggested to use this test as a screening tool for sport participation as well as a post-rehabilitation test to ensure dynamic functional symmetry.
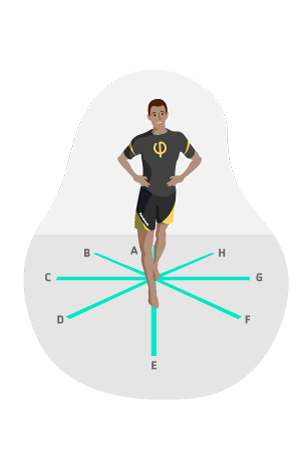
Figure (physiopedia)
How to perform The SEBT:
Conducting the Test (science for sport)
- The athlete should be wearing lightweight clothing and remove their footwear. After doing so, they are the required to stand in the centre of the star, and await further instruction.
- When using the right foot as the reaching foot, and the left leg to balance, the athlete should complete the circuit in a clockwise fashion. When balancing on the right leg, the athlete should perform the circuit in an anti-clockwise fashion.
- With their hands firmly placed on their hips, the athlete should then be instructed to reach with one foot as far as possible and lightly touch the line before returning back to the starting upright position.
- With a pencil, the test administrator should mark the spot at which the athlete touched the line with their toe. This can then be measured from the centre spot after the test to calculate the reach distance of each reach direction. Reach distances should be recorded to the nearest 0.5cm (22).
- They should then repeat this with the same foot for all reach directions before changing foot.
- After they have completed a full circuit (every reach direction) with each foot, they should then repeat this process for a total of three times per leg. For example, they should have three anterior reach performances for both their right and left leg.
- Once the athlete has performed 3 successful reaches with each foot in all directions, they are then permitted to step away from the testing area.
- The test administrator should have recorded the reach distance of each successful attempt, with a pencil, in order to calculate the athlete’s SEBT score after the test.
Scoring System
With the test complete and all performances measured and recorded, the test administrator can then calculate the athlete’s SEBT performance scores using the following simple equations:
- Average distance in each direction (cm) = Reach 1 + Reach 2 + Reach 3 / 3
- Relative (normalised) distance in each direction (%) = Average distance in each direction / leg length * 100
These calculations should be performed for both the right and left leg in each direction, providing you with a total of 16 scores per athlete.
Normative data
Figure ( Miller, T., 2012).
- According to Hertel, Miller, and Deneger (2000), the reliability of the SEBT ranges between r = 0.85-0.96
- According to Plisky et al (2006), the reliability of this test ranges between 0.82-0.87 and scores 0.99 for the measurement of limb length
- Chaiwanichsiri et al (2005) concluded that the Star Excursion Balance training was more effective than a conventional therapy program in improving functional stability of a sprained ankle
- Plisky et al (2009) concluded that the intra-rater reliability of the SEBT as being moderate to good (ICC 0.67- 0.97) and inter-rater reliability as being poor to good (0.35-0.93) [2]

Supporting Articles/text
Advanced fitness assessment and exercise prescription. Heyward V. Human kinetics, 6th edition: 303 (5)
Miller, T. (2012). National Strength and Conditioning Association. Test and Assessment. Human Kinetics. Champagne, IL.
Bressel E, Yonker JC, Kras J, Heath EM. Comparison of Static and Dynamic Balance in Female Collegiate Soccer, Basketball, and Gymnastics Athletes. Journal of Athletic Training 2007;42(1):42–46.
Chaiwanichsiri D., Lorprayoon E., Noomanoch L. (2005). Star Excursion Balance Training : Effects on Ankle Functional Stability after Ankle Sprain. Journal of Medical Association Thailand 88(4): 90-94 (1B)
Plisky P., Rauh M., Kaminski T., Underwood F (2006) Star Excursion Balance Test as a Predictor of Lower Extremity Injury in High School Basketball Players. Journal of Orthopaedic and Sports Physical Therapy. 36 (12) (1B)
Plisky P et al. (2009). The Reliability of an Instrumented Device for Measuring Components of the Star Excursion Balance Test. American Journal of Sports Physical Therapy. 4(2): 92–99. (2B)

Sports Videos

Description of the Star Excursion Balance Test (SEBT)
March 22nd, 2018 · no comments · balance.
The Star Excursion Balance Test (SEBT) is a test of dynamic balance, which requires subjects to balance on one leg and reach as far as possible in eight different directions. This test has been used as an indicator of lower limb injury risk. Read about the Star Excursion Balance Test , and the similar Y-Balance Test which was derived from this test.
Tags: balance
Search This Site
- Bench Press
- Vertical Leap
- Olympic Games
- Adventure Racing
- Football (Gridiron)
- Football (Soccer)
- Rugby League
- Rugby Union
- Table Tennis
- Tenpin Bowling
- Disc Sports
- Toe Wrestling
- Weight Lifting
- Figure Skating
- Ski Jumping
- Skiing-Alpine
- Skiing-Cross-Country
- Skiing-Freestyle
- Snowboarding
- Speed Skating
- Shuttle Runs
- Anthropometry
- Flexibility
- Vertical Jump
- Reaction Time
- Grip Strength
home search sitemap store
SOCIAL MEDIA
newsletter facebook twitter
privacy disclaimer copyright
contact author info advertising

Star excursion balance test (SEBT)
The Star Excursion Balance Test (SEBT) is a widely used test to assess and/or detect deficiencies in dynamic postural control due to asymmetries, decompensations or musculoskeletal injuries, such as instability of the ankle, knee, hip or lack of strength in the core. This test allows to detect individuals at risk of suffering a lower limb injury thanks to its requirements in terms of strength, flexibility and proprioception.
- Required Material : A flat, non-slip surface, a tape measure and 4 strips of adhesive tape of approximately 1.8 and 2.5 metres long. An “8-pointed star” will be drawn on the floor, with lines separated 45° from each other (see illustration).
- Procedure : The subject stands barefoot in the middle of the “8-pointed star”, as shown in the illustration, keeping balance on one leg. With his/her other leg, the subject will try to reach as far as possible with the tip of his/her toes on each of the 8 branches of the star. Then the distances reached will be measured. The anterior, posteromedial and posterolateral directions will be the most important in detecting instability and will indicate an increased risk of injury. The test should be performed on both legs and the results will be analysed.
- Assessment : It is measured in centimetres (cm) and a single result will be registered although it is always advisable to take several measurements to obtain a more reliable value. When the subject shows a large difference between one leg and the other, there is a decompensation.
- Remarks : The SEBT is a widely used test for injury risk prevention. This test has been proposed as a way of analysing muscle symmetry/asymmetry in athletes of different disciplines. Test results have been shown to improve after the prescription of appropriate training.There is a very similar variant of this test, called the Y Balance Test (YBT), also available from Fisicalcoach, which simplifies the work as it has been shown that the posteromedial direction is the most indicative of injury risk.
View other balance tests | View all tests
Take this test and 139 more in our App
134k seguidores
13k seguidores
288k seguidores
812k seguidores
Star Excursion Balance Test | Controle postural | Retorno ao jogo

- E-Book de avaliação
- Comentários
O Star Excursion Balance Test, abreviado como SEBT, consiste em uma série de tarefas de alcance com a extremidade inferior em oito direções. De acordo com um estudo realizado por Gribble et al. (2013) , o SEBT tem excelente confiabilidade entre avaliadores, entre 0,86 e 0,92, e demonstrou ser capaz de diferenciar indivíduos com problemas nos membros inferiores, como instabilidade crônica do tornozelo, dor patelo-femoral e reconstruções do LCA. Por esse motivo, consideramos o SEBT como um teste com alto valor clínico na prática.
Para realizar o teste, primeiro, coloque 6 tiras de fita no chão em um ângulo de 45°. Antes de iniciar o teste real, são necessárias de 4 a 6 tentativas de prática em cada direção, após as quais o paciente pode descansar por 5 minutos.
Para o teste real, o paciente tem 3 momentos de teste medidos oficialmente. Para começar, peça ao paciente para ficar descalço em um membro com as mãos nos quadris e peça-lhe para tentar alcançar o máximo possível com cada fita. A fita métrica deve ser tocada levemente com a porção mais distal do pé de alcance, sem deslocar o peso para o pé do membro de alcance ou repousar sobre ele, e o examinador marca o ponto de contato mais distal na fita métrica.
Uma tentativa não é considerada completa se o participante tocar pesadamente, parar no touchdown, tiver que fazer contato com o solo com o pé de alcance para manter o equilíbrio, ou levantar ou deslocar qualquer parte do pé do membro de apoio durante a tentativa.
Após cada tentativa em uma direção, o paciente retorna o membro que está alcançando para a posição inicial no ápice da grade, retomando a postura bilateral novamente. Em seguida, repita o mesmo procedimento com o mesmo membro em outra direção. Um circuito completo é feito para um membro se todas as direções tiverem sido cobertas. Em seguida, troque de perna e complete outro circuito completo. Ao final do Star Excursion Balance Test, o paciente deve ter completado três circuitos completos com as duas pernas e a distância de cada tentativa deve ser medida.
Pontuação: Para pontuar o SEBT, primeiro calcule a distância média de alcance em cada direção, em centímetros, dividindo a soma de todas as 3 tentativas por perna por 3. Portanto, você deve ter 16 valores. Em seguida, calcule a distância relativa (ou normalizada) em cada direção como uma porcentagem, tomando a distância média em cada direção, dividida pelo comprimento da perna do paciente e multiplicada por 100. Se agora você comparar as pernas entre si, poderá identificar os atletas com maior risco de lesão. Por exemplo, Plisky et al. (2006) descobriram que uma assimetria de alcance anterior maior que 4 cm durante o SEBT previa indivíduos com maior risco de lesões nos membros inferiores em jogadores de basquete.
Pollock et al. (2010) descobriram que jogadores de futebol americano universitário com uma pontuação composta inferior a 90% têm 3,5 vezes mais chances de sofrer uma lesão.
Obviamente, essas são apenas amostras de dois grupos específicos de esportes, razão pela qual é importante mencionar que a aplicação e a generalização do SEBT devem ser cuidadosamente consideradas para cada esporte e sexo, pois há uma enorme variação no desempenho do SEBT e no risco de lesões entre esportes e sexos!
APRENDA A OTIMIZAR A REABILITAÇÃO E A TOMADA DE DECISÕES DE RTS APÓS A RECONSTRUÇÃO DO ACL

Outros testes de desempenho úteis que podem ser de seu interesse são:
- Teste de equilíbrio Y
- Teste de salto com queda
- Cluster de teste de lúpulo
Referências
Butler RJ, Lehr ME, Fink ML, Kiesel KB, Plisky PJ. Desempenho de equilíbrio dinâmico e lesão de extremidade inferior sem contato em jogadores de futebol universitário: um estudo inicial. Saúde esportiva. 2013 Sep;5(5):417-22.
Bressel E, Yonker JC, Kras J, Heath EM. Comparação do equilíbrio estático e dinâmico em atletas universitárias de futebol, basquete e ginástica. Journal of athletic training. 2007 Jan;42(1):42.
Gribble PA, Kelly SE, Refshauge KM, Hiller CE. Confiabilidade entre avaliadores do teste de equilíbrio de excursão em estrela. Journal of athletic training. 2013;48(5):621-6.
Hubbard TJ, Kramer LC, Denegar CR, Hertel J. Fatores que contribuem para a instabilidade crônica do tornozelo. Foot & ankle international. 2007 Mar;28(3):343-54.
Plisky PJ, Gorman PP, Butler RJ, Kiesel KB, Underwood FB, Elkins B. A confiabilidade de um dispositivo instrumentado para medir componentes do star excursion balance test. North American journal of sports physical therapy (Jornal norte-americano de fisioterapia esportiva): NAJSPT. 2009 May;4(2):92.
Robinson RH, Gribble PA. Suporte para uma redução no número de tentativas necessárias para o teste de equilíbrio de excursão em estrela. Archives of physical medicine and rehabilitation (Arquivos de medicina física e reabilitação). 1 de fevereiro de 2008;89(2):364-70.
Seguir um curso
- Aprenda em qualquer lugar, a qualquer hora e em seu próprio ritmo
- Cursos on-line interativos de uma equipe premiada
- Credenciamento CEU/CPD na Holanda, Bélgica, EUA e Reino Unido
Torne-se um especialista em reabilitação de LCA neste curso on-line de primeira classe e acerte em cheio o retorno de seus pacientes ao esporte!

O que os clientes têm a dizer sobre este curso on-line

Crie sua conta gratuita para ter acesso a esse conteúdo exclusivo e muito mais!
Baixe nosso aplicativo gratuito de fisioterapia com todo o conhecimento de que você precisa.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Sports (Basel)
- PMC10383250
Star Excursion Balance Test as a Predictor of Musculoskeletal Injury and Lower Back Pain in Non-Professional Soccer Players
Iva sklempe kokic.
1 Faculty of Kinesiology, Josip Juraj Strossmayer University of Osijek, 31000 Osijek, Croatia; [email protected] (I.S.K.); rh.sofik@anukd (D.K.)
Katarina Petric
2 Faculty of Health Studies, University of Rijeka, 51000 Rijeka, Croatia; [email protected]
Danijela Kuna
Stjepan jelica.
3 Department of Health Studies, College of Applied Sciences, “Lavoslav Ruzicka” in Vukovar, 32000 Vukovar, Croatia; rh.uvev@acilejs
Tomislav Kokic
4 Faculty of Medicine, Josip Juraj Strossmayer University of Osijek, 31000 Osijek, Croatia
5 Department of Orthopaedics and Traumatology, County General Hospital Vinkovci, 32100 Vinkovci, Croatia
Associated Data
The data presented in this study are available on request from the corresponding author.
Soccer is a sport with worldwide popularity but has a substantial risk of injury. Clinical screening tools are an important factor in strategies of injury prevention. The purpose of the study was to examine the relationship between the Star Excursion Balance Test (SEBT) and injury and lower back pain (LBP) in amateur soccer players. The research was performed as a longitudinal cohort study on 42 amateur male soccer players with 15.8 ± 6.6 years of soccer playing (age: 25.5 ± 6 years). Participants were surveyed with regard to their soccer playing, injuries, and LBP, and the SEBT was performed. They were followed for 3.5 months. At the follow-up, an additional set of data regarding injuries and LBP was gathered. Significant differences were found in all directions and in the composite score of the SEBT between uninjured and injured players. Shorter distance in all directions and a lower composite score were associated with injury in general. Shorter distances in all but the anterior direction and a lower composite score were associated with lower extremity injury, and shorter anterior distance was associated with LBP. Amateur soccer players with lower SEBT scores are more prone to injuries in general, as well as injuries of the lower extremities. SEBT presents as a useful clinical screening tool in identifying amateur soccer players at risk of injury.
1. Introduction
Soccer is a sport with worldwide popularity; however, the risk of injuries during practice and the game is high. The incidence of injuries in amateur soccer players ranges from 2.7 to 4.5 per 1000 h of practice and from 12.3 to 24.7 per 1000 h of game time [ 1 , 2 , 3 ]. The majority of soccer related injuries (68–88%) occur in the lower extremities [ 4 , 5 ]. Lower back pain (LBP) is another very common musculoskeletal disorder in soccer players with a yearly prevalence of 64% [ 6 ]. Participation in soccer can also have a significant role in the development of strength asymmetries leading to injury occurrence [ 7 ].
Prevention of injuries has an important role in reducing the injury burden in non-professional soccer players [ 8 , 9 ]. The use of clinical screening tools became an important component in the prevention of sports injuries. Previous studies have suggested that the use of an injury-screening tool related to dynamic balance may be beneficial in the identification of the risk of injury [ 10 , 11 , 12 , 13 ]. Dynamic balance can be defined as an individual’s ability to maintain total body stability of their center of mass during movement and is an integral part of neuromuscular control [ 14 ]. Deficits in lower extremity dynamic neuromuscular control, including impaired dynamic balance, is a known risk factor for injury [ 13 , 15 , 16 ]. Furthermore, dynamic balance is also impaired in individuals with LBP [ 17 , 18 ]. Dynamic neuromuscular control is a frequently utilized component of injury prevention programs as well as an outcome measure for return to sport criterion [ 10 ].
There is the need to further establish the relationship between dynamic balance and the risk of musculoskeletal injury and LBP in the amateur athlete population and to assess whether a clinical screening test for dynamic balance can be useful in the prediction of injuries and LBP. A valid and reliable screening tool for dynamic balance could be used in identifying those at risk and in the planning of preventive strategies. One of the very common screening tools for dynamic balance is the Star Excursion Balance Test (SEBT) [ 13 , 19 ]. The SEBT evaluates dynamic postural stability [ 20 ]. It is an inexpensive, simple, and quick method of measuring dynamic balance with good reliability reported [ 19 , 21 ]. In addition to dynamic balance, SEBT also requires other characteristics of neuromuscular control, such as coordination, flexibility, and strength, and each reach direction activates muscles in a different pattern [ 13 , 22 ].
Previous studies reported that reach asymmetries in anterior, posteromedial, and posterolateral direction of ≥4 cm, a normalized composite score <89.6%, and shorter individual reach distances during the SEBT and modified SEBT were associated with future injury risk [ 10 , 16 ]. However, the majority of the studies were not performed on non-professional athletes. Current information regarding the predictive value of SEBT for musculoskeletal injury and LBP in amateur athletes is still limited.
Therefore, the purpose of this study was to examine the relationship between SEBT reach distances and musculoskeletal injury and LBP among non-professional soccer players. We hypothesized that the SEBT can be used in the prediction of musculoskeletal injury and LBP in this population, and that there will be significant associations between shorter reach distances and injuries and LBP.
2. Materials and Methods
2.1. study design and participants.
The study was performed as a longitudinal cohort study on 42 amateur male soccer players from three amateur soccer clubs in Eastern Croatia. All three soccer clubs are part of the regional league, and they compete at the regional level. Ethical approval for the study was obtained from the Ethics Committee for Biomedical Research, Faculty of Health Studies, University of Rijeka, Croatia (21 February 2019). The study was carried out in accordance with the Declaration of Helsinki and participants gave their written consent. The inclusion criteria for participants were as follows: amateur soccer player, regular practice and games in the soccer club for at least six months before the beginning of the study, and an active soccer player for at least 5 years. Exclusion criteria were injuries or painful symptoms in the period of performing the screening tests and any other serious medical conditions, including surgery or concussion, six months before the testing.
2.2. Procedures
Participants completed the questionnaire with the baseline information, which included demographic data, body height and body mass, health-related history, duration of soccer practice, training loads in the past six months, existence of injuries and lower back pain in the past six months, as well as leg dominance. Leg length was measured on each lower limb 3 times, from the greater trochanter to the lateral malleolus. Body mass index was obtained using the standard equation. After the initial interview, participants performed the SEBT after 10 min of warm up. Participants were followed up 3.5 months after the initial interview with another questionnaire, which included information on training loads, injuries, and lower back pain in the period after the initial interview. An injury was defined as any injury sustained during training or competition resulting in restricted performance or time lost from play [ 23 ]. Lower back pain (LBP) was defined as pain and discomfort localized below the costal margin and above the inferior gluteal folds, with or without leg pain [ 24 ].
2.3. Star Excursion Balance Test
The Star Excursion Balance Test comprises a single-leg balance with an oppositional reaching movement measuring the anterior, posterolateral, and posteromedial reach of both legs [ 13 ]. The test was explained and demonstrated to the participants. Before the formal testing, they practiced six trials in each direction. Participants were positioned with their foot in the center of the testing grid, which was created by aligning a series of three tape measures secured on the floor. Athletes were instructed to keep their hands on their hips, head facing forward, and to keep their stance foot flat on the floor. In that position they were instructed to reach as far as possible in the three directions with the toe of the other foot and make a single, light toe touch on the tape measure.
Reach distance was marked by the tape with the pen and then measured using a tape measure. The maximum value of three trials was used for analysis. The trial was repeated if the athlete failed to maintain a unilateral stance, lifted or moved the stance foot from the center of the grid, touched down with the reach foot, or failed to return the reach foot to the starting position. The distance reached was normalized to leg length by dividing excursion distance by leg length and they multiplying it by 100. The sum of the three reach directions divided by three times the leg length and then multiplied by 100 was used to calculate the composite scores.
2.4. Statistical Analysis
Statistical analysis was performed using SPSS 25.0 (IBM, Armonk, NY, USA). The normality of the data was checked using Shapiro–Wilk test. Descriptive statistics included the mean and standard deviation for numeric variables or frequency and percentages for categorical variables.
The Welch test was used for comparison of the SEBT scores between the group of participants without injury and the group of participants with injury in general or specific injuries and LBP. Differences in the injury rate before and after the testing were calculated using McNemar’s test.
Binary logistic regression was initially performed to examine whether normalized SEBT scores for anterior, posteromedial, and posterolateral directions of both legs; composite scores and asymmetries ≥4 cm could identify those at risk of injury in general, lower extremity injury, contact lower leg injury, non-contact lower leg injury, and lower back pain. Odds ratio (OR) and 95% confidence intervals (CI) were calculated.
Hierarchical multiple linear regression analyses were conducted to determine the impact of SEBT variables on injuries. Variables with a p value of <0.20 on the Wald test [ 25 ] in the univariate models were entered into multiple regression analyses. In these models age, previous injury, BMI, total training load, and number of training sessions per week were entered in Step 1, and SEBT variables were entered in Step 2. Tolerance and variance inflation factor (VIF) were used to check for multicollinearity. Results were considered significant at p < 0.05.
Sixty amateur soccer players were invited to participate in the study. Forty-two players accepted the invitation and fulfilled the inclusion criteria. Table 1 shows the participant’s general characteristics. Regarding their tactical position in soccer, the majority of participants (N = 19; 45.2%) had the position of midfielder. Furthermore, there were 10 (23.8%) strikers, 7 (16.7%) defenders, and 6 (14.3%) goalkeepers. Their injuries and LBP before and after the testing are presented in Table 2 . There were no significant differences in the injury and LBP rate between the period 6 months before the testing and at the end of the period 3.5 months after the testing.
General characteristics of the participants (N = 42).
N—sample; SD—standard deviation; BMI—body mass index.
Characteristics of the injuries and lower back pain among the participants (N = 42).
N—sample; LE—lower extremity; LBP—lower back pain.
The SEBT results for the total sample and according to injury status and LBP are presented in Table 3 . Significant differences were found in all directions as well as in the composite score in the SEBT results between uninjured and injured players with any injury and lower extremity injury. In addition, significant differences were found in the anterior direction of both the dominant and non-dominant leg between those with and without LBP. None of the participants had anterior asymmetry ≥4 cm; however, 5 (11.9%) participants had posteromedial asymmetry ≥4 cm. Four (9.5%) participants had posterolateral asymmetry ≥4 cm. All but one participant had their SEBT score <89.6%.
SEBT results for the total sample and according to injury status and LBP.
N—sample; SD—standard deviation; LE—lower extremity; LBP—low back pain; ANT—anterior; PMED—posteromedial; PLAT—posterolateral; LL—normalized score; * statistically significant.
Table 4 shows the SEBT results according to lower extremity injury mechanism. There were no significant differences between those with and without a contact and non-contact mechanism of injury.
SEBT results according to LE injury mechanism.
N—sample; SD—standard deviation; LE—lower extremity; ANT—anterior; PMED—posteromedial; PLAT—posterolateral; LL—normalized score.
Table 5 presents results of univariate logistic regression analysis for injuries and LBP as well as ORs with their 95% CI. Shorter distance in all directions of SEBT as well as a lower composite score for both the dominant and non-dominant lower extremities were associated with any injury. Shorter distance in all but the anterior direction of the dominant leg as well as lower composite scores were associated with lower extremity injury. Only the anterior reach of the non-dominant leg was associated with LBP.
Univariate logistic regression analysis for injuries and LBP.
LE—lower extremity; LBP—low back pain; ANT—anterior; PMED—posteromedial; PLAT—posterolateral; LL—normalized score; * statistically significant.
The results of the univariate logistic regression analysis for contact and non-contact lower extremity injuries are shown in Table 6 . No directions of the SEBT nor the composite score could correctly identify those at risk of contact or non-contact lower extremity injury. Posteromedial and posterolateral asymmetries ≥4 cm could not identify those at risk of injury or LPB.
Univariate logistic regression analysis for contact and non-contact LE injuries.
LE—lower extremity; ANT—anterior; PMED—posteromedial; PLAT—posterolateral; LL—normalized score.
Multiple regression analysis revealed that age, previous injury, BMI, total training load, and number of training sessions per week explained 28% of the injury variance, while the composite score for the non-dominant leg added an extra 13% ( Table 7 ). There was a positive association between BMI and injury, and negative associations between training load, SEBT composite score of the non-dominant leg, and injury in general. Age, previous, injury, BMI, total training load, and number of training sessions per week explained 47% of the lower extremity injury variance. The composite score for the non-dominant leg added an extra of 11%. There were negative associations between training load and the SEBT composite score of the non-dominant leg and lower extremity injury. Other SEBT variables did not contribute to neither model.
Multiple regression analysis examining the contribution of age, previous injury, BMI, training load, and selected SEBT variables to injury and LE injury.
* p < 0.05, ** p < 0.01; SE—standard error; b—unstandardized coefficient; β—standardized coefficient.
4. Discussion
This study aimed to examine if there is a relationship between SEBT reach distances and musculoskeletal injury and LBP among non-professional soccer players. Furthermore, it aimed to determine whether the SEBT scores can be used in the prediction of injuries and LBP. The results partially confirmed our hypothesis. Shorter reach distances in all directions and lower composite score were associated with musculoskeletal injury in general. Likewise, shorter reach distances in all but the anterior direction of the dominant leg and a lower composite score were associated with lower extremity injury. LBP was associated with a shorter reach distance in the anterior direction of the non-dominant leg. However, SEBT results could not identify those at risk of specific lower extremity injuries. Asymmetries in posterolateral and posteromedial directions ≥4 cm could not identify those at risk of injury or LBP. To the best of our knowledge, only one previous study investigated predictive value of the SEBT in non-professional soccer players. This adds some new aspects regarding the association between the SEBT and musculoskeletal injury and LBP in very specific population, amateur soccer players, with the possibility to lower the risk of injuries and LBP by using screening and implementing prevention strategies according to the results of the screening. We specifically selected this population because there were not enough previous studies which included amateur athletes and data in the literature for professional athletes cannot be generalized to amateur athletes.
A previous similar study performed by Gonell et al. [ 26 ], which examined the relationship between modified SEBT scores and soft tissue injury incidence in a soccer team, included a total of 74 soccer players. Forty of these participants were amateur athletes. All reach directions, including the composite score, exceeded values of the results in our sample; however, the results were similar to ours, showing an increased risk of injury with decreased reach directions of the SEBT. A significant relationship was found between below the average normalized anterior reach distance and contact injuries, as well as below the average normalized posteromedial reach distance and non-contact injuries. Below the average values of the normalized posterolateral reach distance and normalized composite reach distance were related to an increased risk of total and non-contact injuries. Participants with a composite reach distance below the average of the sample were approximately two times more likely to sustain an injury.
Another previous study examining the predictive value of SEBT scores on lower extremity injuries was performed by Plisky et al. [ 13 ]. They investigated whether SEBT reach distance was associated with the risk of lower extremity injury among high school basketball players, which makes their sample quite different than ours. However, their results were similar. They reported that an anterior right/left reach distance difference ≥4 cm, decreased the normalized right anterior reach distance and decreased the normalized posteromedial, posterolateral, and composite reach distances bilaterally were significantly associated with lower extremity injury.
O’Connor et al. [ 27 ] examined whether modified SEBT results can identify those at risk of contact or non-contact lower extremity injury in a population of adolescent and collegiate footballers and hurlers. Poor scores were unable to ascertain those at risk of contact or non-contact lower extremity combined and ankle injuries with sufficient sensitivity. Contrary to that, a study performed by Ko et al. [ 28 ] established that the posteromedial and posterolateral reach of the SEBT can identify adolescent athletes who will incur a subsequent lateral ankle sprain. Indeed, the literature reported that asymmetry in the anterior direction is more common among those with a history of lateral ankle sprain in comparison to those without [ 29 ]. In our study, we did not find asymmetries related to future injuries; however, ankle sprain was not specifically taken into account.
Research by Ganesh et al. [ 18 ] reported on significant reductions in excursion distances for all directions of the SEBT in group of subjects with lower back pain. Contrary to that, another study investigating SEBT results in young athletes with back pain did not find significant differences between the reach distances in all three directions of those with and without back pain [ 30 ]. In our study, we find only differences in the anterior reach for both the dominant and non-dominant leg between those with and without LBP. In addition, a shorter distance of the anterior reach of the non-dominant leg was associated with the occurrence of LBP.
Indeed, impaired balance is established as a risk factor for lower limb injury [ 31 ]. Neuromuscular risk factors for lower extremity injury in male soccer players include m. quadriceps dominance, leg dominance (asymmetry), knee valgus, trunk dominance, and reduced dynamic stability [ 32 ]. Furthermore, previous research reported impaired postural control in LBP and proposed that balance impairment in LBP patients correlates with deficits in the musculoskeletal and neural systems [ 33 , 34 ]. Controlling balance requires the interaction of the neurological, musculoskeletal, proprioceptive, vestibular, and visual systems [ 18 ]. Therefore, it is very important to develop and validate appropriate screening methods for assessments of neuromuscular control, including balance, with the goal of identifying those which may be at a greater risk of injury or LBP.
We have demonstrated that the SEBT can be a useful and simple method of clinical screening in amateur soccer players. The test could be incorporated into the pre-participation screening of athletes to help identify those at risk of injury or LBP. These deficits could be improved through a neuromuscular training program prior to the competitive season. There is the need to establish cut-off points, which will be population- and sport-specific, in order to more accurately determine the future injury risk. Cut-off points and previous research on professional soccer players are not generalizable to the amateur athlete population due to different training loads and the frequency of training sessions and competitions.
Our study’s prospective design allowed us to minimize recall bias regarding the injuries. However, our study had some limitations. First, our sample was small and consisted of only male amateur soccer players from three soccer clubs. This makes difficult to generalize our results to other populations of athletes. Furthermore, the follow-up period was relatively short. Future studies should consider a larger sample consisting of both genders from different sports, and a longer period of follow up. It is also important to note that we examined only the results of the SEBT in terms of injury prediction, and we did not take into account many of the other variables that could influence the risk of injury and LBP. Strong points of the study include the use of a valid and reliable test, a homogenous population, and the prospective design.
5. Conclusions
In conclusion, our data suggests the predictive value of the SEBT for injuries in general, lower extremity injuries, and LBP occurrence. It seems that amateur soccer players with lower SEBT scores are more prone to injuries in general, as well as injuries of the lower extremities. Amateur soccer players have different training loads and lifestyle in comparison to professional athletes, and there is also lack of financial resources for the amateur soccer clubs. However, use of simple screening procedures could have a positive impact on injuries and LBP. Further studies are needed to confirm these findings and to establish specific cut-off points, which would allow more precise predictions.
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization, I.S.K., K.P. and T.K.; methodology, I.S.K. and D.K.; software, K.P.; validation, I.S.K. and S.J.; formal analysis, I.S.K., S.J. and D.K.; investigation, K.P. and S.J.; data curation, I.S.K.; writing—original draft preparation, K.P., S.J. and T.K.; writing—review and editing, I.S.K. and D.K.; supervision, I.S.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and was approved by the Ethics Committee for Biomedical Research, Faculty of Health Studies, University of Rijeka, Croatia (21 February 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.

IMAGES
VIDEO
COMMENTS
The star excursion balance test can be used to test lower extremity balance. Improving balance may prevent injury and enhance sports performance. This eviden...
The Star Excursion Balance Test (SEBT) is a reliable, responsive, and clinically relevant functional assessment of lower limbs' dynamic postural control. However, great disparity exists regarding its methodology and the reported outcomes. Large and specific databases from various population (sport, age, and gender) are needed to help clinicians when interpreting SEBT performances in daily ...
The Star Excursion Balance Test was developed to be a reliable measure of dynamic stability. Since then, it has proven to be a sensitive indicator of lower limb injury risk in a variety of populations. To add to this, the Star Excursion Balance Test has been shown to have high levels of intra-rater test-retest reliability, though no validity ...
The star excursion balance test is a test to measure an individual's postural control, range of motion, strength, and proprioceptive abilities.ENROLL IN OUR ...
The Star Excursion Balance Test (SEBT) is one of my favourite dynamic balance assessment tools and this blog covers the construct and current literature existing around it's use. The SEBT is not an injury-specific test and has been the subject of research for almost 20 years, and was first described in 1998 (Gribble, Hertel & Plisky., 2012).
The Star Excursion Balance Test (SEBT) is a dynamic test that requires strength, flexibility, and proprioception. It is a measure of dynamic balance that provides a significant challenge to athletes and physically active individuals. The test can be used to assess physical performance, but can also be used to screen deficits in dynamic postural ...
The Star Excursion Balance Test (SEBT) is a test of dynamic balance, using in a single-leg stance that requires strength, flexibility, core control and proprioception. The test requires participants to balance on one leg and reach as far as possible in eight different directions. The similar Y-Balance Test was derived from this test.
mented clinical tests to iden-tify at-risk individuals and target them for prevention programs is therefore neces-sary.2 The Star Excursion Balance Test (SEBT), ini-tially described by Gray,3 is a functional test originated from rehabilitation exercises of the lower limb. Since its inception,theSEBThasbeen frequently described in the
balance and proprioception May 22, 2023. 1:12. The Star Excursion Balance Test (SEBT) is one of our favourite tests and one of the major reasons we developed the MAT to rid the world of ugly pieces of sports tape stuck to the floor of clinics and gyms everywhere. This assessment has been well researched to demonstrate high inter and intra ...
N The Star Excursion Balance Test should be considered a highly representative noninstrumented dynamic balance test for physically active people. N The Star Excursion Balance Test is a reliable measure and a valid dynamic test to predict risk of lower extremity injury, to identify dynamic balance deficits in patients with lower extremity ...
The Star Excursion Balance Test (SEBT) is a test of dynamic balance, which requires subjects to balance on one leg and reach as far as possible in eight different directions. This test has been used as an indicator of lower limb injury risk. Read about the Star Excursion Balance Test, and the similar Y-Balance Test which was derived from this test.
The Star Excursion Balance Test is a versatile test, and its benefits are 3-fold:1) It can be used as a rehab exercise 2) It can be used to guide return to s...
The Star Excursion Balance Test (SEBT) is a reliable, responsive, and clinically relevant functional assessment of lower limbs' dynamic postural control. However, great disparity exists regarding ...
It is a simple yet challenging test to perform, and it can be time-consuming. The commonly used Y Balance Test (YBT) was derived from the SEBT to improve test procedure standardization. 28,29 Although the mSEBT and YBT tests are similar, the score of a particular reaching direction should not be used interchangeably between these 2 tests. 12,29,30
The Star Excursion Balance Test (SEBT) is a common assessment used across clinical and research settings to test dynamic standing balance. The primary measure of this test is maximal reaching distance performed by the non-stance limb. Response time (RT) is a critical cognitive component of dynamic balance control and the faster the RT, the ...
The Star Excursion Balance Test (SEBT) is a widely used test to assess and/or detect deficiencies in dynamic postural control due to asymmetries, decompensations or musculoskeletal injuries, such as instability of the ankle, knee, hip or lack of strength in the core. This test allows to detect individuals at risk of suffering a lower limb ...
An updated review of the design, implementation, and interpretation of the SEBT is provided and guidelines to standardize SEBT procedures are proposed for better comparisons across studies are proposed. The Star Excursion Balance Test (SEBT) is a reliable, responsive, and clinically relevant functional assessment of lower limbs' dynamic postural control. However, great disparity exists ...
Você sabe aplicar, na prática, de forma correta, o Star Excursion Balance Test modificado? Se sabe, reveja. Se não, assista ao meu novo vídeo do canal. Aprov...
O Star Excursion Balance Test, abreviado como SEBT, consiste em uma série de tarefas de alcance com a extremidade inferior em oito direções. De acordo com um estudo realizado por Gribble et al. (2013), o SEBT tem excelente confiabilidade entre avaliadores, entre 0,86 e 0,92, e demonstrou ser capaz de diferenciar indivíduos com problemas nos ...
The Star Excursion Balance Test (SEBT) and lower quarter Y-Balance Test (YBT) are two of the most prominent tools in the literature to measure dynamic balance of the lower extremity. 10 The SEBT began as a star comprised of four lines, all crossing at the same center point. 11 To complete the test, an individual stands at the center of the star ...
O controle postural dinâmico envolve algum nível de movimento esperado em torno de uma base de apoio. Isso pode incluir tarefas, como pular ou pular para um ...
2.3. Star Excursion Balance Test. The Star Excursion Balance Test comprises a single-leg balance with an oppositional reaching movement measuring the anterior, posterolateral, and posteromedial reach of both legs . The test was explained and demonstrated to the participants. Before the formal testing, they practiced six trials in each direction.