Thanks for visiting! GoodRx is not available outside of the United States. If you are trying to access this site from the United States and believe you have received this message in error, please reach out to [email protected] and let us know.
- Open access
- Published: 19 April 2023

“But at home, with the midwife, you are a person”: experiences and impact of a new early postpartum home-based midwifery care model in the view of women in vulnerable family situations
- Bettina Schwind 1 , 2 ,
- Elisabeth Zemp 1 , 2 ,
- Kristen Jafflin 1 , 2 ,
- Anna Späth 1 , 2 ,
- Monika Barth 3 ,
- Karen Maigetter 1 , 2 ,
- Sonja Merten 1 , 2 &
- Elisabeth Kurth 1 , 2 , 3
BMC Health Services Research volume 23 , Article number: 375 ( 2023 ) Cite this article
1949 Accesses
Metrics details
Postpartum home-based midwifery care is covered by basic health insurance in Switzerland for all families with newborns but must be self-organized. To ensure access for all, Familystart, a network of self-employed midwives, launched a new care model in 2012 by ensuring the transition from hospital to home through cooperation with maternity hospitals in the Basel area. It has particularly improved the access to follow-up care for families in vulnerable situations needing support beyond basic services. In 2018, the SORGSAM (Support at the Start of Life) project was initiated by Familystart to enhance parental resources for better postpartum health outcomes for mothers and children through offering improved assistance to psychosocially and economically disadvantaged families. First, midwives have access to first-line telephone support to discuss challenging situations and required actions. Second, the SORGSAM hardship fund provides financial compensation to midwives for services not covered by basic health insurance. Third, women receive financial emergency support from the hardship fund.
The aim was to explore how women living in vulnerable family situations experienced the new early postpartum home-based midwifery care model provided in the context of the SORGSAM project, and how they experienced its impact.
Findings are reported from the qualitative part of the mixed-methods evaluation of the SORGSAM project. They are based on the results of seven semi-structured interviews with women who, due to a vulnerable family postpartum situation at home, received the SORGSAM support. Data were analyzed following thematic analysis.
Interviewed women experienced the early postpartum care at home, as “relieving and strengthening” in that midwives coordinated patient care that opened up access to appropriate community-based support services. The mothers expressed that they felt a reduction in stress, an increase in resilience, enhanced mothering skills, and greater parental resources. These were attributed to familiar and trusting relationships with their midwives where participants acknowledged deep gratitude.
The findings show the high acceptance of the new early postpartum midwifery care model. These indicate how such a care model can improve the well-being of women in vulnerable family situations and may prevent early chronic stress in children.
Peer Review reports
Based on evidence that lifelong health and human development are strongly influenced by experiences during the first years of life, early childhood interventions are increasingly the focus of research and policies [ 1 , 2 , 3 , 4 , 5 ]. Interventions during this period are found to be more effective and less costly than later efforts [ 3 ], and especially children in vulnerable family situations seem to profit from early interventions. Studies show in particular, that early chronic stress and its long-term consequences can be mitigated [ 6 ]. Evidence suggests that parents, caregivers, and families need support for providing responsive, nurturing care and protection for young children so that they may achieve their developmental potential [ 3 , 7 ]. Programs designed to meet the needs of families in difficult circumstances lead to enhanced parental resources and thereby better outcomes for children [ 8 , 9 , 10 , 11 , 12 , 13 ].
Positive effects on developmental outcomes have been documented for three types of family support and strengthening: quality services, support, and skills building [ 3 ]. However, studies [ 14 , 15 , 16 , 17 , 18 , 19 , 20 ] have shown that especially psychosocially and economically disadvantaged families have limited access to postpartum care at home and use the available services less frequently. Midwives, due to their immediate access to vulnerable families, may therefore be key actors for early prevention, i.e. the early assessment and support of families with, or expecting an infant whose living situations are overstraining their capacities to cope [ 19 , 21 ].
Only a few, mostly Scandinavian, studies have addressed the perspective of parents receiving postpartum home-based care by midwives, and research on the impact of such care on infants and their families is still scarce. A Swedish study on first-time parents’ experiences of home-based postpartum care after early hospital discharge showed that midwives took a supporting role and strengthened parents’ self-confidence [ 21 ]. In a Norwegian study on women’s experiences of home visits by midwives in the early postpartum period, three central themes, relational continuity, postpartum talk, and vulnerability emerged [ 22 ]. Specifically, relational continuity with a midwife appeared as a crucial part of care, as expressed by a cited quote “postpartum care provided by a named midwife”. The importance of relational continuity in care was supported by a study from the UK that linked care across pregnancy, birth, and new motherhood with improved health outcomes for women and babies in socially disadvantaged and diverse communities [ 23 ]. An Australian home visit program for vulnerable families in disadvantaged areas also improved clients’ parenting skills and well-being, increased participation in community networks, and access to support services [ 24 ]. In Sweden, parents in vulnerable situations who received extended home visits reported improved parenting skills and confidence in discussing problems with professionals [ 25 ], especially fathers with migration histories who benefited equally through home visiting programs [ 26 ]. Furthermore, a German study applying a longitudinal mixed-method design investigated the effects of family midwives in 734 vulnerable families in Sachsen-Anhalt [ 27 ]. Results showed an increase in mothers’ skills in three areas: childcare, self-help/organization of family life, and searching for and accepting external help.
Because the literature so far has largely focused on the context of extended home visiting programs and outcomes for families in vulnerable situations [ 25 , 26 ] and was less concerned with experiences of families in vulnerable situations with very early home-based midwifery care and its impact, these issues were addressed in a Swiss study.
In Switzerland, early home-based postpartum care is mainly provided by independent midwives and family nurses [ 18 ]. Organizing postpartum care at home before birth is usually the responsibility of the pregnant woman and/or her relatives. Basic insurance covers 10–16 regular home visits by an independent midwife over 56 days. Little is known about the practices that go beyond standard care. Several local midwifery networks guarantee a seamless transition for all mothers and newborns from the hospital to the home setting [ 28 , 29 ]. These networks coordinate a postpartum care pathway in collaboration with maternity hospitals, independent midwives, and other maternal and child health care providers [ 30 , 31 , 32 ]. They assure that all women who give birth in the collaborating hospitals receive standardized care in that a midwife comes to their homes after hospital discharge and ensures further care. A first evaluation study in Switzerland suggested a great value of organized, guaranteed postpartum outpatient care by a midwifery network, especially for socially disadvantaged families [ 16 ]. It appeared that the accessibility and reliability of the midwives were crucial to women. The midwife network not only eased the burden on families and reduced stress, and for many women, the midwife evolved into an important reference person and was recognized as a cultural mediator by women with migration history.
In the Basel area, a Familystart network model has been running since 2012. Due to the guaranteed access to postpartum home care, midwives regularly visit disadvantaged families who may have fewer resources to organize postpartum care themselves, yet need support beyond services covered through basic health insurance. Set up in late 2018, the project “SORGSAM – Support at the start of life” aimed to offer vulnerable families improved assistance in dealing with complex postpartum situations [ 33 ]. The SORGSAM project supports independent midwife care activities for families in situations of stress and risk in three ways: first, midwives have access to first-line telephone support (7 days a week) to discuss challenging situations and required actions with a midwife specialized in psychosocial care [ 33 ]; second, the SORGSAM hardship fund provides financial compensation to midwives for services not covered by basic health insurance, e.g. for their time and costs in emergencies or for coordinating inter-professional services; and third, women may receive financial emergency support from a hardship fund.
We specifically aimed to investigate how women in vulnerable family situations experienced early postpartum home-based care by independent midwives provided in the context of the SORGSAM project, and how they viewed the impact of obtained care.
The study and this report were conducted following the Consolidated Criteria for Reporting Qualitative Research (COREQ) [ 34 ]. The research team of the SORGSAM evaluation consisted of an interdisciplinary team dealing with society and health care in Switzerland anchored at the Swiss Tropical and Public Health Institute, University of Basel [ 35 ]. Ethical approval by the Northwest Switzerland Ethics Committee was obtained before the start of the study (BASEC 2019–02030), and in an amendment during the COVID pandemic concerning the conduction of zoom interviews and directly contacting the families through the caring midwife.
Research design
This article reports findings from the qualitative part of the mixed-methods evaluation of the SORGSAM project in the area of Basel, Switzerland [ 35 ]. It is based on the results of semi-structured interviews with women in a vulnerable family situation in the postpartum period who experienced home based support from a Familystart midwife. The midwife made use of the SORGSAM support, including coaching/counseling by a specialized midwife and financial support from the SORGSAM hardship fund.
Open-ended, narrative-generating interview questions were developed in consultation with the research team and included three thematic blocks: (1) perception of the postpartum situation, (2) perception of the midwife’s care, and (3) perception of the current situation. Towards the end of the interview, participants could talk freely about topics that were not previously addressed but were important to them. An additional document shows the interview guide in detail (additional file 1). For the purpose of publication the guide was translated from (Swiss) German into English.
Sampling and recruitment
Criterion-based maximum variety sampling was used to select participants based on two available SORGSAM routine documentations, namely: (1) reports of the SORGSAM reimbursement from the hardship fund and, (2) reports of provision of first-line telephone support provided by a specialized midwife for colleagues encountering complex family situations. The criteria consisted of poverty, migrant history, single parent, health, and/or psychosocial stressors to maximize the diversity of complex family situations. Women were eligible to participate if they received care from a Familystart midwife who requested SORGSAM support in 2019. Individuals with severe mental illness, and/or receiving support from a midwife who were not Familystart members, and/or having language barriers were excluded. The selection based on the sampling criteria was documented, discussed, and validated by the team.
Eligible participants were approached by their midwives and informed about the study. When they were interested, the informed consent packages were sent via mail. They had sufficient time to read through the documents, clarify questions and consider whether they wanted to participate in the study. Written informed consent was obtained from all participants before the interview.
Among 55 eligible participants, nine agreed on a contact date for an interview, whereas 32 refused to participate or did not react; four persons showed insufficient language skills for interviewing, and 10 could not be reached. Two participants did not attend the agreed appointment due to the illness of a family member. As they were no longer reachable afterwards, this was considered as a withdrawal from participation. Once seven interviews were completed, recruitment had to be suspended due to the financial constraints of the project.
Data collection
Between February and July 2020, a senior researcher with a background in health and social sciences conducted seven interviews in the area of Basel in the German language. Each participant was free to choose the place of the interview. The first interview was conducted in February 2020, face-to-face in a café. Due to the increasingly tense pandemic situation, all subsequent interviews were conducted virtually via Zoom. The virtual approach appeared to be convenient for participants, as they did not have to find childcare for their children. All interviews were audio-recorded and lasted approximately one hour. The semi-structured interview method with open-ended questions allowed delving into participants’ perspectives so that women could talk freely about their experiences. Observations on the research process including the pandemic situation were noted in a reflexive diary by the interviewer.
Data analysis
After transcription of the interviews data were analyzed following Braun and Clarke’s thematic analysis [ 36 , 37 ], a method designed for researching the views and experiences of research participants. The qualitative data analysis software package MAXQDA 2018 was used to support the analysis steps for coding following thematic analysis [ 36 , 37 ]. These included familiarization with the data (step 1), assignment of preliminary codes (step 2), search for preliminary themes (step 3), review and definition of themes (steps 4 and 5) and provide a written record (step 6). At a stakeholder workshop, consisting of 12 participants, the themes identified through the analysis were presented, revisited, discussed, and validated. No themes were corrected or determined to be missing. Based on the results of the analysis, a thematic model was jointly developed by the research team that formed the basis of the results section.
Participants
Of the seven participating women, five had a migration history (see Table 1 ). One participant was of Swiss nationality, and one woman was a cross-border commuter living in Germany. Their ages ranged from 23 to 44 years. Four women had a tertiary education and three had attended primary school. At the time of the interviews, only one woman was employed (100%), whereas two reported unemployment status and four reported not working and currently not seeking paid work. Four women were married; three were single or living alone. The partners of the four married women worked full-time.
Research findings
Three themes emerged from the analysis of the interviews, each containing several sub-themes and respective codes:
complex postpartum situation,
comprehensive postpartum care, and
psychosocial relief and empowerment.
The themes were grouped into a thematic model as shown in Fig. 1 , displaying midwife care and its perceived effects on women. They emerged from the accounts of the women, who found themselves in “complex postpartum situations” at home. Women described the “comprehensive postpartum care” by explaining “what it comprised” and “what it meant” to them. They indicated that the care received resulted in their “psychosocial relief and empowerment”. In the following, the three emergent themes are consecutively described:
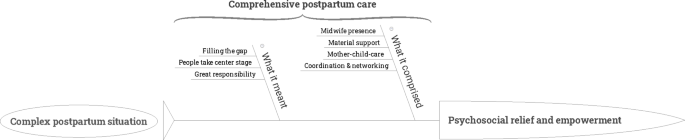
Thematic model
Theme 1: complex postpartum situation
Women described challenging situations at home. Four sub-themes became apparent, including the aspects: “health situation”, “social situation”, “psychosocial situation” and “financial and material situations” (see Fig. 2 ).

Theme “Complex postpartum situation”
Specific to the present study, however, was that the postpartum situations were considered complex, due to the intersection of health challenges of mother and/or newborn, but also the precarious social and financial situation, partly with experience and/or fear of violence as the following example shows:
“At the beginning, it wasn’t easy,…after the birth I had problems with my leg, I could not walk properly…and I am overweight…and I am here alone, without family. I had problems with my boyfriend at that time and with my boyfriend’s father, yes, and I have another child…and she was kidnapped when she was one year old, and the problems plus my fear that my new child would also be kidnapped, that made my life quite difficult.“ (Interview 3).
Theme 2: “comprehensive postpartum care”
Women reported how they experienced the care provided by midwives as shown in Fig. 3 . Therewith, the sub-themes “what it comprised” and “what it meant” emerged from the data, each including different thematic aspects that added up to what was understood as “comprehensive postpartum care”.

Theme “Comprehensive postpartum care”
Sub-theme “what it comprised”
The sub-theme “what it comprised” is composed of the thematic aspects of “mother-child-care”, “midwife presence”, “coordination and networking”, and “material support”. “Mother-child-care” included ordinary aspects of midwifery care in the postpartum situation, such as bathing the newborn, checking wound sutures, breastfeeding support, assuring weight gain of the newborn, and checking for emotional distress and/or anxiety/depression. To focus on the three further thematic aspects that go beyond ordinary midwifery care, mother-child care was not elaborated on in more detail.
“Midwife presence” emerged as a very central element in the women’s narratives. Women described the feeling that midwives were always there for them and their families, and even in case of emergencies:
“She was always there when we needed her, always…” (Interview 1) . “When I need help, when I write, she always calls.“ (Interview 4) . “She really helped me and never minded, even if it was raining.“ (Interview 6) .
Thus, the reachability and availability of midwives appeared as a crucial aspect to ensure emotional, parental and material support to promote feelings of security - especially in case of uncertainties at home. This was the case for example, when women were worrying about how to deal with the newborn, how to feed the baby, or if there were no nappies due to financial constraints, but also if they were fearing violence. This kind of accessibility and reliability to medical, social, and emotional support appeared especially important for women who felt challenged having to navigate through the health system and therefore they were able to receive the help at the time they needed it:
“[Doctors] were often not available,…nobody came by…and I was…also not so well organized, but there was…a big gap…I somehow think that the midwifery care was a very personal, individual care.” (Interview 6) .
The low threshold of accessibility and reliability, e.g. to text midwives and receive an answer via SMS, appeared as a supportive cornerstone. However, it was not only the perceived reachability and availability of the midwife that was important for the women, but also that the midwife’s presence at home was felt to be without any apparent time pressure:
“I think it was important for us that she was simply there, that she always took her time, sometimes she was even there for two hours and didn’t look at the clock, … that she wasn’t in a hurry, but that she took her time and asked three more times, with, um, is it everything now, is there anything else?… Yes. That was good.“ (Interview 7) .
The quotes suggest that the women perceived an unconditionality in the midwifery care received, presumably creating feelings of trust and being taken seriously. The women also reported that the midwife was not only there as a contact and care person for them and the newborn, but also for the whole family, as evidenced in the next quote of a woman who experienced stillbirth:
“Yes, and I liked the fact that she looked after us as a family and not just after me as a woman, because there wasn’t much to control in terms of the baby…that the family was looked after, that the brother was looked after, asked how he was dealing with it, right? Things like that.“ (Interview 7) .
Furthermore, one woman described a situation of domestic violence, in which her midwife provided her with emergency help:
“Because once I was in a situation there, I couldn’t call the police or get help somehow, then I wrote to her and she got the police for me, you know?…I didn’t know what to do, I didn’t have a car, my baby was sick…so, or violence,…something happened to him,…I couldn’t go to the hospital right away, then she helped me, even though it wasn’t working time, or, so she came with her car, she helped me go to the hospital”. (Interview 6).
Overall, the thematic aspect of “midwife presence” indicates that the interviewed women appreciated the midwife’s accessibility, availability, and continuity of care without time pressure. They described midwives as “carers” for their families and as trusted confidants - especially for themselves, and who were called in during emergencies such as in cases of domestic violence.
Women interviewed reported on the different forms of “coordination and networking” functions of midwives. They described midwives’ work as mediating, organizing, and coordinating services and institutions to improve complex domestic situations. Midwives were reported to have organized parent-child counseling, breastfeeding counseling, social services, and home care services for domestic help (e.g. the Red Cross). Women also indicated that midwives contacted various doctors, police, and cantonal offices. The women interviewed described this central interface function:
“And, she gave me a lot of contacts…la Leche ligue, and now I’m a member and other mothers…that was very good.“ (Interview 1) . “So yes, so I was sad, so not good, since the birth and yes, the midwife, has found such a person…a therapist, and I had gone there with (child).“ (Interview 2) .
The range of this interface network function went from quick fixes to complex coordination activities as illustrated in the following example:
“At the beginning, she just put away the toys…and then afterward she…asked at Spitex [home care service for domestic help], can someone cook there? And, do a bit of housework and a bit of cleaning. And they said, no, they just do the flat a bit. And then she …first asked in Canton X because the children were born there and then,…but I live in Canton Y…then she had asked if she could organize someone from the Red Cross if they would take over something. Then they said, no, have to ask Canton Y. She called Canton Y, and then they understood my situation, then Canton Y just took over and also organized it further.“ (Interview 4) .
The midwifes’ networking activities included professional groups or organizations or institutions, and networking among mothers. Women with a migratory background who felt or were alone mentioned this positively and emphasized the important role of their home-country language in feeling understood:
“Because the [other mothers] speak Spanish and it was…my midwife was the midwife of this mother and my midwife, and [she said] I know other Spanish mothers - do you want their phone number? And she asked for the other mother too, and we made contact and we are friends.“ (Interview 1) .
Beyond midwife’s care and coordination support, women also described to have received material support, ranging from getting diapers to breast pumps to children’s clothes:
“If I need some clothes or something bed and things like that…if I need that…all the organizing…for cot or something, you know…I didn’t buy much and she also tried to get [this] organized. That was also…great, how do you say, yeah because everybody thinks only about one health side, the other side…she helped on both sides, yeah.“ (Interview 4) .
Women also received information and knowledge about where to obtain assistance in case of financial bottlenecks, e.g. where to get second-hand clothing and toys free.
Sub-theme “what it meant”
The sub-theme “what it meant” is composed of the thematic aspects of “filling the gap”, “people take center stage”, and “great responsibility”. The interviewed women described the overall postpartum care received not only as extensive, but also contrasted it with the care provided by medical doctors where they described midwives as “filling a gap” in the care system:
“With the doctors a bit like that…so, ‘I do that, that’s my problem…They don’t see a collective problem…and he just looks at the child. I find the medicine a bit separate…The midwife! it’s in the middle…she’s worked with both of us so far, so that’s so her job, she’s doing great.“ (Interview 2).
Women also described as being seen and treated by the midwife as a person, which also included much of their emotional situation.
“Because in hospital you are a patient with blood pressure, this and that and the values, but at home, with the midwife, you are a person with feelings and yes…that was a completely different approach. (Interview 7).
“I mean, it isn’t just the baby what the midwife works on…she helped me in other ways too.” (Interview 6).
Women also emphasized the great responsibility that this entails for the midwife:
“I felt that the midwife took more responsibility than she…had to.” (Interview 2) .
The quotes highlighted that women understood the care they received as comprehensive postpartum care that occurred at the interface between somatic and psychosocial care, and as interconnecting between professions and institutions. This meant for women that a gap in postpartum care was being filled, which they described as a great responsibility for midwives.
Theme 3: Psychosocial and emotional impact
The theme “psychosocial and emotional impact” developed from the data, covering the sub-themes “psychosocial relief”, “empowerment”, and “feeling grateful”, see Fig. 4 .

Theme “Psychosocial relief and empowerment”
Sub-theme “psychosocial relief”
What appeared as important for the interviewed women was that the received care was experienced as personal and emotional, and was labeled “human”. This aspect was particularly memorable for the interviewed women as they described the midwife’s care as supporting “physical, emotional recovery and relaxation” which helped them to relax:
“Helped me to relax a bit, because I was always very stressed and so (groans), and I…was breastfeeding (child),…so and she helped me to relax a little bit like that, and to breathe…and to get a little bit, yeah, calm, so that was…that was good”. (Interview 2).
“It all sounds like a commercial now…she couldn’t have done it better. She was also great interpersonally…That really supported me insanely.“ (Interview 4) .
The quotes indicated how women no longer felt alone due to the midwife’s presence and the interpersonal relationship, which supported women in dealing better with the new postpartum situation. They also stated how important it was for them to be able to “build and experience trust” with the midwife:
“I could trust her…that was important for me, that I could trust her, I could also talk so openly with her.” (Interview 6).
“She was actually my contact person number one and I think that was actually almost the most important thing.” (Interview 5).
The quotes underlined the importance of interpersonal closeness and trust so that women could open up and thereby feel relief and relaxation at the same time. They experienced a reduction of concerns and stress.
Sub-theme “empowerment”
From the different interview texts, it became manifest that the women not only felt relieved by the comprehensive midwifery care but that they also felt strengthened to survive the difficult life situations. The following quotes expressed how women felt to “become stronger and courageous”, also through “competence and knowledge enhancement” on where and how they could obtain help:
“That made me a bit strong,…um, I don’t know, is there this expression in Switzerland or German, that you can stand on your feet? [Yes. That was like that for me. So I know where, where I can go for help if anything happens…yeah…And that made it a bit easier, the situation made that, became a bit easier. It’s not easy, but it has become easier.“ (Interview 3).
“During the birth or after the birth a little bit so, just, like nice, so, just, so, just, um, agreeing with the situation or so a little bit braver, we can help, we can organize something, not worrying or so a little bit, yeah, so just with the others, just helping would be nice (laughs)” (Interview 4).
The midwifes’ presence provided security and confidence to better deal with and accept the current situation so that women described, “feeling good and safe”:
“So yeah, now it’s, um, now it’s really like, I hope, I don’t know, but like…right now I’m somewhere good with my baby” (Interview 6).”
Through these different forms of emotional and social self-empowerment, they described feeling “good and safe” again.
Sub-theme “feeling grateful”
Starting from the question about changes compared to the current situation, women made statements that indicated, in retrospect, a positive assessment and gratitude for the care and support they had received that still lasted at the time of the interview. This was exemplified in interview 6:
“She just…helped a lot, a lot, and I’m very grateful that she kind of saved my life, twice.“ (Interview 5) .
This gratitude was rooted in the comprehensive support, which was described as “coming from the heart”, as it was formulated in interview 5:
“She helped me in many ways, you know…in clothes, in healthy, in emotional, she was … a person…she did so many things with me, helped…she did it from the heart.“ (Interview 5) .
“She has been like a god when she asked like that and organized the help like that, that’s, yeah, that’s a big help, you know? I won’t forget that.“ (Interview 3) .
The quotes illustrated both the gratitude towards the midwife as well as her central role, possibly because the interviewed women have had little support in their vulnerable family situations.
Our study showed that women living in vulnerable family situations and who were cared for in the context of the SORGSAM project, evaluated the early postpartum home-based midwifery care as a relieving and strengthening experience. Midwives not only ensured the mother and child’s postpartum health but also coordinated further care and opened up access to appropriate community-based support services. Mothers described the received care as comprehensive, personal, and reliable, allowing them to better deal with complex family situations. They reported that it eased the burden of social isolation, made it easier to talk about challenges such as fears and violence, and led to de-escalation in situations of tension. They expressed how receiving care resulted in stress reduction, increased resilience, and empowerment and that it enhanced their mothering skills and parental resources.
Our study highlights that the benefits of early home-based midwifery care for women in precarious family situations are rooted in the close and trusting relationship with their midwife, resulting in deep gratitude for this experience. Participating women described their complex life situations and commented in detail on the supportive, comprehensive midwifery care they experienced. They reported that they felt strengthened by the continuous and easily accessible midwifery care during the uncertain phase of the early home transition, in terms of health, as well as social and emotional aspects.
”Midwife presence”, provided them with emotional and material equipment support, and supported them in accessing different community networks. This kind of supporting role by the midwife was described before, as in the study of Johansson in healthy families after early hospital discharge in Sweden [ 21 ], or in a recent Swedish study in families with low socioeconomic status, where the support of midwives was considered reassuring [ 25 ]. In our study, this aspect appeared to be very pronounced. Women expressed the impact of receiving midwifery care by memorable wordings such as “saved my life twice, somehow”, or “otherwise I would be dead”. Women included in the study used metaphors such as “angel” or even “God” to describe the midwives. Similar expressions by postpartum women have also been documented in a recent study in Zurich involving socially disadvantaged women [ 16 ]. These expressions may reflect, on the one hand, the hardships experienced in vulnerable situations and, on the other hand highlighted that support in such situations was perceived as particularly helpful. According to the Swiss study by Grylka-Baeschlin et al., midwives who provided postpartum care evolved into important support persons, and, among women with migration history, in that the midwives became cultural mediators [ 16 ]. Relational continuity has also been described as a crucial part of midwifery care in the review of Dahlberg [ 22 ], and it was linked to improved outcomes [ 23 ]. The high accessibility and reliability of the midwife appeared very central also in the other recent Swiss study [ 16 , 38 ]. The building of trust probably occurred fully only if midwives could be immediately present in the homes of new mothers, recognize situations of psychosocial and emotional emergency, and act as first professional responders. As the mothers in our study reported, bridging to further help systems was a further, crucial part of care, and networking helped prevent social isolation. These findings are in line with those of a Swedish and an Australian study, that reported an increased knowledge of societal and local resources for families [ 26 ], increased access to support services, and improved participation in community networks [ 24 ].
Our findings exemplify that stress in the very first phase of life can be mitigated by early midwifery home care even in very difficult social situations. Mothers described impacts on themselves in terms of calming down, de-escalation of situations, strain relief, and stress reduction. Grylka-Baeschlin et al. found that home-based postpartum care eased the burden on families and reduced stress [ 16 ]. This should, in turn, positively impact mothering skills, the mother-infant relationships, and the further development of the children, as it has been shown, that a high level of parenting stress is associated with a poor dyadic co-regulation between mother and child [ 39 ]. “Midwife presence” seems to be helpful for what is called a “co-regulation in therapeutic processes” resulting in mitigating high-stress levels in the mother [ 40 ], which can be seen as a key factor for preventing/decreasing early chronic stress in the child.
A key finding of our study relates as to how early midwifery home care strengthened self-confidence and resilience, including knowledge and assurance on access to further support services. Women described that they felt to be seen and treated as “a person”, how they became ‘stronger and more courageous’. They furthermore reported increased competencies and knowledge of where to get help, and impressively described increased resilience. These findings postpartum are in line with several studies reporting that home-based early midwifery care had positive effects on parenting and self-confidence [ 21 , 24 , 25 , 26 , 38 ]. The mothers in our study also reported to have more confidence in that they now knew where and how to get the help they needed. It may thus be understood as a prerequisite for the promotion and prevention of mother and child health, including mental health aspects.
Limitations and strengths
The positive picture given by postpartum women may be too optimistic due to a participation bias. Indeed, enormous efforts were needed for the recruitment of participants, and among the 55 eligible families, around half did not react to the study invitation or refused to participate. Ten women had no valid address, and four women had difficulty mastering the German language and this appeared to be too limited to participate in an interview. In particular, no woman could be recruited who was involved in a child welfare issue. Among the participants, six women had a migrant history, thus, migrant women were well represented.
Saturation is usually accepted as the criterion for the number of interviews conducted. Saturation is described to be reached - depending on the research questions and study population - at approximately 12 to 20 interviews, but the basic elements for a thematic ordination are reported to be already identified at six interviews [ 41 ]. Even though the sample was small by using a maximum variety sampling, we have succeeded in mapping the diversity and complexity of care for vulnerable postpartum family situations. The data collection was also quickly adapted to the pandemic measures and was carried out digitally. This actually was a simplified access for women in vulnerable family situations, as they were not burdened by the additionally needed childcare.
Furthermore, the information provided by the interviewed women was very congruent with the information in the midwives’ case documentation [ 35 ]. In these files, psychosocial problems were recorded in approximately 60% of cases, and midwives noted that they could contribute to a more stable situation, by lowering tension, exhaustion, and stress, and they notably documented a positive course in most of the cases. The thematic mapping was conducted by the research team and validated at the stakeholder workshop. Although there was no systematic assessment of the impact on children in our study, the findings suggested that SORGSAM care might influence favorably on children’s well-being as several of the interviewed mothers explicitly reported improved breastfeeding, and two out of the seven interviewed mothers mentioned a decrease in the crying of their children.
In conclusion, our findings are supportive of a potential beneficial effect of postpartum midwifery care for the improvement of resilience and well-being of women in vulnerable family situations. Midwives appear to be important players in early childhood interventions with a comprehensive biopsychosocial approach breaching the interface of medical and psychosocial care. To allow midwives to make full use of their potential, it is necessary to install programs such as SORGSAM, which reimburse midwives for their coordinative services and give them access to a hardship fund enabling them to provide short-term financial support to families in acute need. Investing in midwifery services may be understood as a direct investment in earliest childhood interventions as described by Magistretti Meier [ 42 ] to prevent early chronic stress at early onset. The findings are suggesting that midwifery home care was a “door opener” for interprofessional coordinated early childhood support, strengthened parenting skills and self-confidence, and might alleviate early adverse childhood experiences, potentially reducing health care disparities and improving health equity. However, more studies are needed to quantitatively assess associations of midwifery home care with positive outcomes in mothers, and in particular, to assess and quantify its longer-term effects on the well-being of families, women, and particularly the development of children.
Data Availability
The datasets produced and analyzed in this study are not publicly available due to the confidentiality of the information, especially in a small region like Basel, Switzerland, as this is the only way to ensure the non-identifiability of individuals. Upon reasonable request, the anonymized data are available from the authors.
Shonkoff JP, Garner AS. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):232–46.
Article Google Scholar
Aboud FE, Yousafzai AK. Global health and development in early childhood. Annu Rev Psychol. 2015;66:433–57.
Article PubMed Google Scholar
Britto PR, Lye SJ, Proulx K, Yousafzai AK, Matthews SG, Vaivada T, et al. Nurturing care: promoting early childhood development. The Lancet. 2017;389(10064):91–102.
Richter L, Black M, Britto P, Daelmans B, Desmond C, Devercelli A, et al. Early childhood development: an imperative for action and measurement at scale. BMJ Glob Health. 2019;4(Suppl 4):e001302.
Article PubMed PubMed Central Google Scholar
World Health Organization. Nurturing care for early childhood development: a framework for helping children survive and thrive to transform health and human potential. Geneva: World Health Organization; 2018.
Google Scholar
Thompson RA, Haskins R. Early stress gets under the skin: promising initiatives to help children facing chronic ddversity. The Future of Children. Prinction Brookings; 2014.
Richter LM, Cappa C, Issa G, Lu C, Petrowski N, Naicker SN. Data for action on early childhood development. The Lancet. 2020;396(10265):1784–6.
Walker AM, Johnson R, Banner C, Delaney J, Farley R, Ford M, et al. Targeted home visiting intervention: the impact on mother-infant relationships. Community Pract. 2008;81(3):31–4.
PubMed Google Scholar
Knerr W, Gardner F, Cluver L. Improving positive parenting skills and reducing harsh and abusive parenting in low- and middle-income countries: a systematic review. Prev Sci. 2013;14(4):352–63.
Gertler P, Heckman J, Pinto R, Zanolini A, Vermeersch C, Walker S, et al. Labor market returns to an early childhood stimulation intervention in Jamaica. Science. 2014;344(6187):998–1001.
Article CAS PubMed PubMed Central Google Scholar
Gardini ES, Schaub S, Neuhauser A, Ramseier E, Villiger A, Ehlert U et al. Methylation of the glucocorticoid receptor promoter in children: Links with parents as teachers, early life stress, and behavior problems.Development and Psychopathology. 2020:1–13.
Morrison J, Pikhart H, Ruiz M, Goldblatt P. Systematic review of parenting interventions in european countries aiming to reduce social inequalities in children’s health and development. BMC Public Health. 2014;14:1040.
Renner I, Scharmanski S, Paul M. Frühe Hilfen – Wirkungsforschung und weiterer Bedarf. Hebamme. 2018;31(02):119–27.
DiBari JN, Yu SM, Chao SM, Lu MC. Use of postpartum care: predictors and barriers. J Pregnancy. 2014;2014:530769.
Wilcox A, Levi EE, Garrett JM. Predictors of non-attendance to the postpartum follow-up visit. Matern Child Health J. 2016;20(Suppl 1):22–7.
Grylka-Baeschlin S, Iglesias C, Erdin R, Pehlke-Milde J. Evaluation of a midwifery network to guarantee outpatient postpartum care: a mixed methods study. BMC Health Serv Res. 2020;20(1):565.
Ruderman RS, Dahl EC, Williams BR, Davis K, Feinglass JM, Grobman WA, et al. Provider perspectives on barriers and facilitators to postpartum care for low-income individuals. Womens Health Rep. 2021;2(1):254–62.
Erdin Springer R, Iljuschin I, Pehlke-Milde J. Postpartum midwifery care and familial psychosocial risk factors in Switzerland: a secondary data analysis.International Journal of Health Professions. 2017;4(1).
Sann A. Familienhebammen in den Frühen Hilfen: Formierung eines “hybriden” Tätigkeitsfeldes zwischen Gesundheitsförderung und Familienhilfe. Diskurs Kindheits- und Jugendforschung. 2014;9(2):227–32.
Meier Magistretti C, Walter-Laager C, Schraner M, Schwarz J. Angebote der Frühen Förderung in Schweizer Städten (AFFiS). Kohortenstudie zur Nutzung und zum Nutzen von Angeboten aus Elternsicht. Luzern, Graz: Hochschule Luzern – Soziale Arbeit, Karl-Franzens Universität Graz; 2019.
Johansson K, Aarts C, Darj E. First-time parents’ experiences of home-based postnatal care in Sweden. Ups J Med Sci. 2010;115(2):131–7.
Dahlberg U, Haugan G, Aune I. Women’s experiences of home visits by midwives in the early postnatal period. Midwifery. 2016;39:57–62.
Homer CS, Leap N, Edwards N, Sandall J. Midwifery continuity of carer in an area of high socio-economic disadvantage in London: a retrospective analysis of Albany Midwifery practice outcomes using routine data (1997–2009). Midwifery. 2017;48:1–10.
Stubbs JM, Achat HM. Sustained health home visiting can improve families’ social support and community connectedness. Contemp Nurse. 2016;52(2–3):286–99.
Bäckström C, Thorstensson S, Pihlblad J, Forsman AC, Larsson M. Parents’ experiences of receiving professional support through extended home visits during pregnancy and early childhood - a phenomenographic study. Front Public Health. 2021;9:578917.
Tiitinen Mekhail K, Lindberg L, Burström B, Marttila A. Strengthening resilience through an extended postnatal home visiting program in a multicultural suburb in Sweden: fathers striving for stability. BMC Public Health. 2019;19(1):102.
Ayerle GM, Frühstart. Familienhebammen im Netzwerk Frühe Hilfen. Bundesministerium für Familie S, Frauen und Jugend, editor. Köln:Nationales Zentrum Frühe Hilfen; 2012.
Familystart. Support before and after birth - Near basel 2022 [Available from: https://familystart.ch/en .
Familystart Zürich [Website], Zurich. Familystart Zurich; 2020 [Available from: https://www.familystart-zh.ch .
Kurth E. FamilyStart beider Basel – ein koordinierter Betreuungsservice für Familien nach der Geburt. Hebammech. 2013;7/8:35–7.
Frey P, Reber SM, Krähenbühl K, Putscher-Ulrich C, Iglesias C, Portmann U, et al. editors. Bedarfsanalyse zur postpartalen Betreuung zeigt Lücken auf - FamilyStart Zürich bietet Lösung 2015.
Zemp E, Signorell A, Kurth E, Reich O. Does coordinated postpartum care influence costs? Int J Integr care. 2017;17(1):7.
Kurth E, Barth M, Loosli B, Ruffieux A, Lüscher U, Späth A, et al. Das Pilotprojekt «Sorgsam – Support am Lebensstart» unterstützt Hebammenarbeit im Frühbereich. Obstetrica. 2019;6:47–8.
Booth A, Hannes K, Harden A, Noyes J, Harris J, Tong A. COREQ (Consolidated criteria for reporting qualitative studies) In: Moher D, Altman D, Schulz K, Simera I, Wager E, editors. Guidelines for reporting health research: a user’s manual Wiley; 2014. p. 214 – 26.
Zemp E, Schwind B, Jafflin K. Evaluationsprojekt SORGSAM 2019/2020, Schlussbericht. 2020.
Braun V, Clarke V. What can “thematic analysis” offer health and wellbeing researchers? Int J Qualitative Stud Health Well-being. 2014;9(1):26152.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77–101.
Ayerle GM, Makowsky K, Schucking BA. Key role in the prevention of child neglect and abuse in Germany: continuous care by qualified family midwives. Midwifery. 2012;28(4):E469–77.
Azhari A, Leck WQ, Gabrieli G, Bizzego A, Rigo P, Setoh P, et al. Parenting stress undermines mother-child brain-to-brain synchrony: a hyperscanning study. Sci Rep. 2019;9(1):11407.
Sossin MK, Charone-Sossin J. Embedding: co-regulation within therapeutic process: lessons from development: response to “co-regulated interactions: implications for psychotherapy … paper by Stanley Greenspan. J Infant Child Adolesc Psychother. 2007;6(3):259–79.
Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82.
Meier Magistretti C, Villiger S, Luyben A, Varga I. Qualität und Lücken der nachgeburtlichen Betreuung. Lucerne: Lucerne University of Applied Sciences; 2014.
Download references
Acknowledgements
A thanks goes to Alessia Kiener for her valuable support in the realization of the evaluation. We would also like to thank the participants, especially for their trust despite their emotionally challenging and stressful family situations.
Open access funding provided by University of Basel.
Author information
Authors and affiliations.
Swiss Tropical and Public Health Institute, Basel, Switzerland
Bettina Schwind, Elisabeth Zemp, Kristen Jafflin, Anna Späth, Karen Maigetter, Sonja Merten & Elisabeth Kurth
University of Basel, Basel, Switzerland
Midwifery Network, Familystart beider Basel, Basel, Switzerland
Monika Barth & Elisabeth Kurth
You can also search for this author in PubMed Google Scholar
Contributions
Study conception and design were done by EZ, EK, and BS. MB recruited the participants. BS conducted the qualitative part of the mixed-methods-based SORGSAM evaluation. The results of the thematic analysis were jointly discussed and finalized by BS and EZ through the development of the thematic map. BS and EZ contributed to the subsequent draft. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Bettina Schwind .
Ethics declarations
Competing interests.
EK has a part-time position as the managing director and MB is a part-time co-worker of the Midwifery Association “Familystart” located in Basel. The authors BS, EZ, KJ, AS, KM, and SM declare that they have no competing interests. The Swiss Tropical and Public Health Institute was commissioned to evaluate the SORGSAM project.
Ethics approval and consent to participate
Ethical approval, including an amendment due to the COVID pandemic, was obtained by the Northwest Switzerland Ethics Committee (BASEC 2019–02030). All methods were carried out in accordance with relevant guidelines and regulations. Written informed consent was obtained from all participants of the study.
Consent for publication
Not applicable.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Evaluation SORGSAM
: Interview guide with women experiencing vulnerable family situation postpartum at home
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Schwind, B., Zemp, E., Jafflin, K. et al. “But at home, with the midwife, you are a person”: experiences and impact of a new early postpartum home-based midwifery care model in the view of women in vulnerable family situations. BMC Health Serv Res 23 , 375 (2023). https://doi.org/10.1186/s12913-023-09352-4
Download citation
Received : 28 December 2022
Accepted : 30 March 2023
Published : 19 April 2023
DOI : https://doi.org/10.1186/s12913-023-09352-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Early postpartum care
- Home visits
- Women’s experiences
- Vulnerable family situations
- Empowerment
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Women's experiences of home visits by midwives in the early postnatal period
Affiliations.
- 1 St. Olavs University Hospital, Department of Women's Health, Olav Kyrres gt. 17, 7006 Trondheim, Norway. Electronic address: [email protected].
- 2 Department of Nursing Science and Center for Health Promotion Research, Norwegian University of Science and Technology, Trondheim, Norway.
- 3 Department of Nursing Science, Midwifery Education, Faculty of Health and Social Science, Norwegian University of Science and Technology, Trondheim, Norway.
- PMID: 27321721
- DOI: 10.1016/j.midw.2016.05.003
Objective: The aim of the present study is to gain a deeper understanding of women's experiences of midwifery care in connection with home visits during the early postnatal period.
Research design/setting: A qualitative approach was chosen for data collection, and the data presented are based on six focus group interviews (n: 24). The women were both primiparous and multiparous, aged 22-37, and lived with their partners. All participants had given birth at a maternity unit responsible for about 4000 births a year. The transcribed interviews were analysed through systematic text condensation.
Findings: The findings are reflected in three main themes: 'The importance of relational continuity', 'The importance of a postpartum talk' and 'Vulnerability in the early postnatal period'. When the woman had a personal relationship with the midwife responsible for the home visit she experienced predictability, availability and confidence. The women wanted recognition and time to talk about their birth experience. They also felt vulnerable in their maternal role in the early postnatal period and the start of the breast-feeding process.
Conclusions: It is important to promote relational continuity models of midwifery care to address the emotional aspects of the postnatal period. Women generally wish to discuss their birth experience, preferably with the midwife who was present during the birth. Due to the short duration of postnatal care in hospitals, the visit from the midwife a few days after childbirth becomes all the more important.
Keywords: Continuity of care; Home visit; Postnatal care; Postpartum talk.
Copyright © 2016 Elsevier Ltd. All rights reserved.
- Focus Groups
- House Calls*
- Midwifery / standards*
- Mothers / psychology*
- Patient Satisfaction*
- Postnatal Care / standards*
- Qualitative Research
Birth how you want to
You want to dance? Sleep? Shower? Eat? Your choice.
Birth in the water? On your bed? In the hallway? Your choice.
Birth with whom you want to
Partner. Doula. Sister. Mother. Children.
Whomever you want by your side, it's your home, it's your choice.
Birth where you want to
A house in the suburbs? An apartment? A farmhouse? A motorhome?
Have your baby in the comfort of whatever you call home.
About Homebirth

Planned homebirth with skilled midwives is safe for low-risk pregnancies.
- High rate of completed home birth (89.1%)
- High rate of vaginal birth (93.6%)
- High rate of completed vaginal birth after cesarean (VBAC; 87.0%)
- Cesarean section rate of 5.2%
MANA stats

Women have the right to choose their maternity care provider and the location of their birth. They have the right to informed consent - full knowledge of risks and benefits before making decisions.
Certified Professional Midwives may legally practice in South Carolina so long as they hold a current state license.

Women and babies experience a natural, mutually regulating, hormonally driven process of birth - from the onset of labor through birth of the baby and placenta, as well as the establishment of breastfeeding and the development of mother-baby attachment - with appropriate support and protection from external interference.
Milbank Report
Meet the Midwife - Angela Springer, LM, CPM
I have given birth three times and though each birth experience was vastly different, they have something in common - I will never forget them. I would love for every woman to have a special and meaningful childbirth experience. My experiences many years ago first led me to lactation peer counseling and postpartum support. My passion to serve and empower women led me to become a birth doula and eventually a midwife. I am certified as a Certified Professional Midwife through the North American Registry of Midwives and hold a Midwifery Bridge Certificate. I am a Licensed Midwife in the state of South Carolina. I am certified in Basic Life Support for healthcare workers (CPR for adults and children) and the Neonatal Resuscitation Program (CPR for newborns). I serve as Vice President of the Palmetto Association of Licensed Midwives.
Meet the Midwife - Chloe Clauser, LM, CPM
I have always been passionate about nurturing and caring for women during their journey to motherhood. Being a mother of four myself, I have learned firsthand just how sacred the journey is each and every time. It is a life-changing event that has the ability to leave you feeling empowered and confident as you start your new journey with your baby. As I follow my calling in midwifery, I find my passion to serve women only growing. I am certified as a Certified Professional Midwife through the North American Registry of Midwives . I am a Licensed Midwife in the state of South Carolina. I am certified in Basic Life Support for healthcare workers (CPR for adults and children) and the Neonatal Resuscitation Program (CPR for newborns).
The Midwifery Model of Care
- Relationship - develop a trusting relationship with your midwife at every appointment
- Informed consent - make informed decisions for you and your baby
- Woman-centered - caring for your physical, emotional, and social well-being
- Family-friendly - include your spouse, significant other, children, or other support people
- Evidence-based - receive the latest, proven, unbiased information and maternity care
- Natural birth - experience an unmedicated, low-intervention, normal physiological birth
- Trauma-informed - expect safety, sensitivity, and support
Homebirth is an answer to the current “perinatal paradox” of doing more and accomplishing less.
Conventional maternity care in the United States spends far more per capita for maternity care than any other nation, and yet has higher rates of perinatal, neonatal, and maternal mortality. Disproved practices are in wide use, while proven beneficial practices are underused. Although most childbearing women and newborns in the United States are healthy and at low risk for complications, essentially all women who give birth in hospitals experience high rates of interventions with risks of adverse effects. Cesarean section is the most common operating room procedure in the country, accounting for 32% of all pregnancies even though the WHO is trying to reduce this rate since there is no evidence that the mortality rate improves when C-section rates rise above 10% .
Let’s do less and accomplish more!
Before Birth
- Holistic prenatal care
- Nutritional counseling
- Pregnancy, childbirth, and breastfeeding education
- Midwife visits in the office
- Routine laboratory tests
- Two physician consult visits
- Anatomy scan ultrasound
- Homevisit at 36 weeks
During Birth
- Labor support in your home
- Eat and drink as you desire
- Water birth option
- Intermittent heart tone monitoring
- Trained to handle emergencies
- Birth in the position and location of your choice
- Natural delayed cord clamping
After Birth
- Newborn exam
- Three postpartum home visits
- Newborn metabolic screening
- Newborn heart defect screening
- Newborn hearing screening
- Mother and baby care for 6 weeks
- Lactation support
- Birth certificate and SSN filing
- 6-week postpartum office visit
Empowering Women Through Education
For a current class schedule, please message us or follow us on social media.
Birth Story Circle
A community gathering where everyone can share, learn, grow, and heal. This is a safe space to share your birth experience, hear from others, ask questions, and form friendships.
This gathering is free.
Pregnancy 101
This class covers everything you need to know about pregnancy including nutrition, body mechanics, tests and procedures offered in pregnancy, and how to deal with common complaints in pregnancy.
This 2.5 hour class is $60.
An interactive and informative childbirth class covering the anatomy and physiology of labor, stages of labor, comfort measures, birth options, and immediate postpartum care of mother and baby.
This 3 hour class is $80.
Breastfeeding
A warm approach to education on the anatomy and physiology of breastfeeding, proper positioning and latch, supply and demand, feeding on demand, early feeding cues, pumping, and common problems.
This 2.5 hour class is $60.
Birth is about making mothers... strong, competent, capable mothers who trust themselves and know their inner strength.
Barbara Katz Rothman
Frequently Asked Questions
The midwifery package includes all prenatal visits, labor & delivery in your home, postpartum and newborn care in your home (3 home visits in the first week), and a six-week postpartum visit in the office for $5000. All education classes are free for clients. Labs and ultrasounds are not included and can be billed directly to your insurance.
We are considered out of network with most insurance companies. You will pay the full fee upfront and have the option to work with a biller to get a reimbursement.
We also accept some Medicaid plans, though not all homebirth expenses are covered by Medicaid.
Angela and Chloe take turns doing office visits and attending births. Having two midwives allows each of us to have family time and a healthy work-life balance. A partnership means there's always a well-rested midwife available for your birth. In the rare event that two women are in labor at the same time, each will have a midwife she already knows and trusts rather than a backup midwife.
We’d like to see you around 10 weeks for your initial visit. Then every 4 weeks until 30 weeks, every 2 weeks until 36 weeks, and then every week until you deliver. One visit, around 36 weeks, will be in your home. All other appointments will be at the office.
Appointments generally last one hour. This time is not spent in a waiting room or sitting alone in an empty exam room waiting for a doctor. We will spend the hour together chatting, getting to know one another, discussing any complaints or questions you may have, reviewing pregnancy and birth education, nutritional counseling, and assessing the health of you and your growing baby.
We will provide all of your prenatal care. SC regulations require that you see a physician for two visits during your pregnancy. There are several providers that we can coordinate these visits with and we will find the best fit for you based on location, insurance, and personal preference. An anatomy scan ultrasound will be performed at one of these visits. You do not need to see a doctor before starting care with us.
Midwives in South Carolina are legally licensed to carry equipment and medications to safely manage normal deliveries at home. This includes: Monitoring equipment for you and your baby; Instruments to clamp and cut the cord; Supplies for the newborn exam and any newborn procedures that you choose; Antihemorrhagic drugs to stop excessive postpartum bleeding; Resuscitation equipment for baby and mother, including oxygen.
Midwives are trained to handle complications and know when hospital transport may be necessary. I have had specific training in emergency skills and hold a NARM Midwifery Bridge Certificate . Through training and equipment, most complications can be handled safely at home. The most common reason for transporting a pregnant woman to the hospital is during a very long labor; either labor is stalled, the mother nears clinical exhaustion, or has decided she desires pain relief medications. In this case, the hospital can provide IV fluids, an epidural, and/or pitocin augmentation, which are tools we do not have in a home setting.
We will help you minimize any mess with instructions on how to set up for your birth. After the birth, we will clean up including washing the laundry and taking out the trash. Your home should feel back to normal with the exception of a new baby.
We have been manipulated to believe that the medical model is the safer option. And then when you start to look at the statistics you can see so clearly that it is not safer.
Dr. Stu and Midwife Blyss of Birthing Instincts #326
Testimonials
Angela, Chloe, and Amanda were amazing from the first phone call to our last office visit. They went above and beyond to care for me while pregnant, and then my daughter and me after delivery. The BEST part was having home visits after delivery.
We absolutely loved our experience having a home birth — and it was because of Angela and Chloe! We always looked forward to the appointments leading up to the birth and left feeling so excited and informed. The birth itself was the most amazing experience! We felt so prepared and safe. Even after we had our baby, whenever we had a question or concern we would text/call her and she always answered no matter the time! We cannot recommend her enough!!
Angela, Chloe, and Amanda provided excellent prenatal, birth, and postnatal care for me and my baby. I am so thankful for the powerful birthing experience they helped me have. I highly recommend them a million times over!!
I had Angela for my second child, first home birth, and it was an amazing experience! Especially after being at an OBGYN that made me feel so alone. Angela is very personable and is truthful and will answer any and all questions. I wouldn’t change anything about my birth experience!
Angela helped us with our second pregnancy and choosing her as our medical care this time around was the best decision hands down. She helped us get through a tough time in our pregnancy that could have landed us in preterm labor at MUSC. With her knowledge of homeopathic remedies we were able to get back to a healthy pregnancy and birth our son at home at 40 weeks and 4 days. Recovery has been amazing and after having our first in the hospital with an epidural and our second at home all natural I can tell you a natural birth at home is the way to go!
My at home water birth experience was amazing thanks to my amazing midwife Angela Springer. Best experience ever, you get to be in control and the atmosphere is so free spirited. For those who are thinking about at home water births please go for it.
I always knew I wanted a home birth, but I am a plus size woman, and was led to believe it wouldn’t be in the cards for me. I sought after it anyways and chose Angela as my provider. The care I received from her and her team was/is night and day to any care I have ever previously received. They carried me through my entire pregnancy, the home birth of my DREAMS and even postpartum continue to be here for me any time of any day. There is nothing like midwifery care, if you’re even considering going this route I highly suggest reaching out and meeting Angela, she is full of knowledge surrounding pregnancy, birth and babies and is eager and passionate about sharing it. We love her!
Angela was absolutely amazing in every aspect when providing care for me during my pregnancy and delivery, which was a totally different experience than I had received at my OBGYN office in which I experienced feeling rushed and not heard or understood, pushed to the side, and the use of scare tactics. Angela was very personal, understanding, and provided me with informed consent on any choices I made during my pregnancy and regarding the birth of my baby. I love building a relationship and even a friendship with the person I knew would be helping me bring my sweet babe earth side. She will always come highly recommended by me. We managed to deliver a 10lb 14oz healthy baby at home in a birth pool safely!!
Angela is amazing. I’m so happy I had her as my midwife! And I’m eternally grateful I was able to give birth at home. She provides excellent personal and professional care, resources, a water tub, an excellent team, education, and a great attitude. She obviously loves her work and takes great pride in serving her local community with her midwifery practice. She helped me deliver a super healthy boy last week, for my first time giving birth, and I felt extremely safe and secure in her care. Even with some minor complications, we were able to avoid a hospital birth, and she handled everything like a pro! We need more midwives, period, and more like her. I can’t recommend Angela enough!
Licensed Midwives providing prenatal, home birth and postpartum care.
Serving Horry, Georgetown, Williamsburg, Florence, Marion, Dillon, Marlboro, and Darlington counties of South Carolina.
Send Message
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Natural Birth at Home
Located in downtown Conway, SC
By appointment only
Copyright © 2022-2024 Natural Birth at Home, LLC - All Rights Reserved.
Photos courtesy of Triple M Photography by Savannah Messer.
Powered by GoDaddy
This website uses cookies.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.
- Research article
- Open access
- Published: 29 August 2018
Early postnatal home visits: a qualitative study of barriers and facilitators to achieving high coverage
- Yared Amare 1 ,
- Pauline Scheelbeek 2 ,
- Joanna Schellenberg 2 ,
- Della Berhanu 2 &
- Zelee Hill 3
BMC Public Health volume 18 , Article number: 1074 ( 2018 ) Cite this article
4817 Accesses
12 Citations
1 Altmetric
Metrics details
Timely interventions in the postnatal period are important for reducing newborn mortality, and early home visits to provide postnatal care are recommended. There has been limited success in achieving timely visits, and a better understanding of the realities of programmes is needed if improvements are to be made.
We explored barriers and facilitators to timely postnatal visits through 20 qualitative interviews and 16 focus group discussions with families and Health Extension Workers in four Ethiopian sites.
All sites reported some inaccessible areas that did not receive visits, but, Health Extension Workers in the sites with more difficult terrain were reported to make more visits that those in the more accessible areas. This suggests that information and work issues can be more important than moderate physical issues. The sites where visits were common had functioning mechanisms for alerting workers to a birth; these were not related to postnatal visits but to families informing Health Extension Workers of labour so they could call an ambulance. In the other sites, families did not know they should alert workers about a delivery, and other alert mechanisms were not functioning well. Competing activities reducing Health Extension Worker availability for visits, but in some areas workers were more organized in their division of their work and this facilitated visits. The main difference between the areas where visits were reported as common or uncommon was the general activity level of the Health Extension Worker. In the sites where workers were active and connected to the community visits occurred more often.
Conclusions
If timely postnatal home visits are to occur, CHWs need realistic catchment areas that reflect their workload. Inaccessible areas may need their own CHW. Good notification systems are essential, families will notify CHWs if they have a clear reasons to do so, and more work is needed on how to ensure notification systems function. Work ethic was a clear influencer on whether home visits occur, studies to date have focused on understanding the motivation of CHWs as a group, more studies on understanding motivation at an individual level are needed.
Peer Review reports
Approximately 2.9 million neonates die every year, which accounts for 44% of deaths among children under five years of age. 73% of these deaths are in the first week of life, and 36% on the first day [ 1 , 2 ]. This highlights the importance of timely intervention in this vulnerable period [ 2 ]. Several life saving newborn behaviours can be promoted, and interventions delivered, through early postnatal care (PNC). These include an assessment of the baby and treatment or referral, and counselling on breastfeeding, thermal care, hygiene, cord care and on danger signs [ 3 , 4 ].
Evidence shows that home visits by community health workers (CHWs) can be an effective means of delivering postnatal care in high mortality settings, and can reduce mortality [ 5 , 6 ], and this strategy has been adopted by 59 of the 75 countries in the Countdown to 2015 report [ 7 ]. Observational data suggest that these visits need to occur within 2 days of delivery to be effective [ 8 ]. The World Health Organization recommends that those who deliver at home should receive a home visit within 24 h of delivery, and those who deliver in a facility should receive PNC in the facility for the first 24 h and home visits from day three [ 3 ].
There have been mixed results in achieving timely visits. Data from sub-Saharan Africa show modest coverage of postnatal care home visits by CHWs, even in study and pilot program settings. In Malawi only 11% of women received a PNC visit within 3 days of delivery, in Tanzania only 15% within 2 days, in Uganda 26% received a visit on day 1, and in Ghana 38% received a visit on day 1 or 2 (figures calculated from authors data) [ 6 , 9 , 10 , 11 , 12 ]. Data from government programmes show even lower coverage levels [ 7 ]. Given the timing of newborn deaths and the importance of early visits, the need for research in this area has been acknowledged [ 13 ]. We identified only three quantitative studies exploring factors affecting the coverage of postnatal care home visits. A meta-analysis of quantitative data from Bangladesh, Malawi and Nepal found that early visits were more likely if a mother had been visited in pregnancy, if they had notified the CHW about the birth, and if the birth had been at home. In Ethiopia attending ANC, having more than two family meetings in pregnancy with a CHW, delivering with a CHW or skilled attendant, and having the CHW’s phone number were associated with receiving early home visits [ 14 ]. No association with maternal socio-demographic characteristics were found in any of the studies [ 10 , 11 , 14 ]. A program review that conducted qualitative interviews with government policy makers and technical specialists identified the need for a functioning primary health care system, a feasible PNC visit schedule, community demand, a functioning system to notify CHWs of a birth, and a cadre of CHWs who are qualified, motivated, have adequate time, access and transport [ 7 ]. We identified no qualitative studies at community level. Such research could provide evidence on why visits may, or may not, occur based on the experiences of the providers and beneficiaries. This paper reports the findings of a study, conducted in Ethiopia, on factors affecting early postnatal home visits by CHWs - Health Extension Workers. This is particularly timely as a Community Based Newborn Care program is currently being rolled out across the country, which includes early postnatal contacts to identify and manage neonatal sepsis at community level, and to provide counselling to families on newborn care [ 15 ].
Program description
The Health Extension Program was introduced in 2003, and has provided one year of training to over 30,000 female Health Extension Workers (HEW). Two salaried workers, educated to at least grade 10, are selected by local councils to serve an area of around 5000 people. They are stationed in health posts and are supported by a network of community volunteers, called the Health Development Army (HDA). HEWs provide health promotion, and disease prevention and treatment, both in the community and at the Health Post [ 16 , 17 , 18 ]. In 2009 a program to equip HEWs with the skills to provide essential newborn care was introduced, which included early post natal visits [ 19 ], and Community Based Newborn Care (CBNC) was added in 2014 including the identification and treatment of sepsis at community level.
Study setting selection and characteristics
The study was conducted in the Amhara and Southern Nations, Nationalities and Peoples (SNNP) regions of Ethiopia. The study was conducted in areas where the Health Extension Program, including CBNC activities, are supported by The Last Ten Kilometers programme (L10 K), a project implemented by JSI Research & Training Institute, Inc. In addition to routine HEW activities, L10 K has implemented a Community Based Data for Decision Making platform that includes tracking pregnant women, recording their service needs and linking them with the health system, and Family Conversations to promote key maternal and newborn health messages [ 20 , 21 , 22 , 23 ].
We were interested in understanding barriers and facilitators to early postnatal care within a reasonably functioning system, and L10 K provided us with a list of woreda (districts) and kebeles (lowest administrative units) that they considered had a functioning HEW and HDA system. From this list we selected two typical woreda in each region, and one kebele in each woreda that was reasonably accessible to the data collection team. We refer to the selected kebele s as kebele “A-D” to maintain anonymity. Table 1 shows the characteristics of the selected kebeles , all of which had a predominantly subsistence farming based economy. There were no reports of the use of the private sector by any study participants and we did not identify any private providers of PNC in the study areas.

Data collection
Data were collected from end of March, 2015 to May, 2015. Ethical approval was gained from the research ethics committees of the London School of Hygiene and Tropical Medicine, and from the Ministry of Science and Technology in Ethiopia. Written informed consent was obtained from all respondents. Data were collected using pre-tested semi structured guides developed by the authors. Data were collected as part of a wider study on the mechanisms of behaviour change related to key maternal and newborn care practices.
Data were collected from recent mothers, grandmothers, fathers, HEWs and HDA members using narrative and in-depth interviews, friendship pair interviews and focus group discussions. Collecting data from several respondent groups, and using a range of methods, ensured we captured a range of views and allowed for data triangulation. Sample sizes, respondent groups, the rationale for using each method, and the content related to early PNC visits are shown in Table 2 . Sample sizes were based on prior experience of when saturation was likely to be reached. The possibility of conducting additional interviews and FGDs was built into the data collection plan in case saturation was not reached as anticipated.
The recent mothers and grandmothers were identified with the assistance of HEWs and HDAs and through snowball sampling. They were eligible for inclusion if they, or their daughter/daughter in law, received at least one home visit by an HEW or HDA in the ante or postnatal period. Recent mothers were purposively selected to ensure a range of ages, educational levels, parities, sex of newborn and socio-economic status that reflected the variation within the study site. For example, less than 14% of women in the study regions had secondary school education [ 24 ], and our purposive sampling focused on women with no or primary education. Place of delivery was also set as a selection criteria but it proved difficult to get many respondents who delivered at home. Fathers were recruited through the local authorities or through the HEWs and HDAs. All HDAs in a kebele were invited for the HDA FGDs. As there were only 2 HEWs per kebele , HEWs from neighbouring health posts were invited to the HEW FGDs. Selected respondents were approached in their home or place of work by the interviewers who explained the study, answered questions and took consent. Three participants refused: one wanted to attend a funeral, and the other two were too busy with their household chores to be able to participate.
Data were collected by four trained interviewers in the local language, with translators used in SNNPR. Interviews lasted from 1 to 2 h and took place in respondents’ houses. FGDs consisted of 3–7 participants and lasted from 1.5 to 2.5 h. They were conducted in neutral locations such as community centres. Interviews and FGDs were audio-recorded and fully transcribed in English within a week of data collection. During data collection, interviewers received regular feedback from senior researchers on their transcripts, interview techniques and to discuss emerging themes. The research team met twice during data collection to ‘pre-analyse’ the data in-order to document emerging themes and identify areas that needed to be explored in subsequent interviews and focus groups and to determine if saturation had been reached.
Data analysis
We conducted a thematic analysis, this consisted of multiple readings of the postnatal care sections of the transcripts to ensure familiarity with the data, to get an understanding of the data as a whole, to begin to identify recurring ideas, and core, a-typical or notable ideas, − these were captured in reflective notes. General themes were derived deductively from the research aims, these were: Timing and content of PNC visits, reactions to PNC visits, and factors influencing the occurrence of visits. Analysis for the timing of, content and reaction to PNC was semantic/descriptive, while coding for factors influencing the occurrence of visits included examining the data for latent constructs. Interviews and focus groups were coded within the broad themes using NVIVO. Coding consisted of reading each transcript and identifying the underlying meaning of each segment of text. For each segment we considered what the segment was about, what message it was giving, what stuck out, and how it was different or similar to others segments, each segment was then given one or more code related to its underlying meaning. Codes that contained similar concepts were sorted and placed into themes. Themes and codes were refined and adjusted by looking for patterns, links and contradictions within themes. Data credibility was checked by triangulating data between respondent groups and between data collection methods. Data analysis was done by two of the senior researchers who discussed their coding regularly to enhance conceptual thinking and increased coding rigor.
There was considerable variability in the reported occurrence and timing of post-natal care (PNC) visits by HEW among the four study kebele . Respondents from all respondent groups consistently reported that HEWs in kebele A and B in Amhara visit most mothers within 3 days of giving birth. But the replacement of two longstanding HEWs by temporary workers in kebele B was reported to have led to a recent decline in visits. Visits were reported as occurring late or not at all in kebele C in SNNPR, and were said to be largely non-existent in kebele D in SNNPR. Reflecting their reportedly frequent occurrence, PNC visits in the Amhara kebeles were described as ‘ordinary’, while in kebele D respondents had ‘never heard’ of this type of visit.
Through our inductive coding three main interlinked themes related to why early PNC visit may or may not occur emerged. These were physical issues related to accessibility and transport issues; information issues related to whether the HEW knew about the delivery; and work issues related to HEW availability, HEW performance and organization. We found no pattern in relation to PNC visits and maternal education level, with nearly all of the mothers interviewed having no or primary education levels.
Physical issues
The main physical barriers to early PNC visits were related to accessibility (distance, spread of villages and topography) and to transport. In all study areas, there were households that were classed as inaccessible by all participants due to time or terrain issues. For example, in kebele A, there were some areas that were accessible only by ladders or only in the dry season, and these were difficult for the HEWs to visit:
‘Some of the places are quite mountainous, and other places can only be accessed using a ladder to descend a ravine….There are places that we can’t access in the wet season…. Those that are nearer are not problematic. We get them within 24 hours’ [ kebele A, Amhara, HEW – FGD].
Generally a flat topography and clustered settlements were seen to facilitate visits and a hilly terrain and scattered settlements were seen as a barrier. A flat terrain meant that households were generally accessible by transportation, which was facilitated by the few HEWs that had bicycles: ‘The topography of this kebele is flat like …. no ups and downs It is accessible for cars and walking’ [ kebele D, SNNPR, Fathers – FGD].
Although extreme distances and terrains were limiting factors for PNC visits, moderate difficulties were not a limiting factor. Kebele A and B had the most difficult terrain overall, but these kebele are where community members reported that early PNC visits were most common. In contrast kebele D was generally flat and accessible but PNC visits were reported by community members as not occurring at all suggesting that information and work issues can be more important barriers than moderate physical difficulties.
Information issues
Whether the HEWs’ knew a birth had occurred was a key theme in whether early PNC visits occurred. The main sub-themes were whether there was a functioning alert mechanism; and minor sub themes were place of delivery, migration in pregnancy and whether the pregnancy carried any stigma.
In the Amhara kebeles (A and B), where visits were reported as being common, mothers reported that HEWs knew they had delivered because they were involved in the delivery or in calling the ambulance. Women in these kebeles reported that they were told to inform the HEW when they went into labor, and few women had the ambulance number themselves: ‘ I directly went to their office [health post] when I felt labor pain, and it is the HEWs who called for Ambulance services’ [ kebele A, Amhara, mother-narrative]. In the difficult to access areas of these kebeles , HEWs reported that they relied on the HDAs informing them of the delivery, which was hampered by accessibility issues as HDAs went in person or sent a messenger to inform an HEW of a delivery:
‘The problem is that we do not get the feedback through the HDAs on time. They have to go a lot of distance and they sometimes send the feedback through students…….because of that we visit them after 7 days. So that is our major problem’ [ kebele A Amhara, HEW-FGD].
In the SNNP kebeles (C and D), where PNC visits were reported as occurring late or not at all, women were given the ambulance number directly, often by the HDA. The HEWs thus relied on the HDA leaders informing them that a woman had given birth, and this did not always occur. In particular, HDAs in kebele D (where PNC visits were rare) reported that they did not always tell the HEWs about a delivery ‘The problem may be with us [HDA].….for example there was a mother that had delivered; I did go and visit her but I have not come and tell the HEW about it’ [ kebele D, SNNPR, HDA – FGD]. This lack of provision of information was not linked to a lack of HDA activity, which was high in these kebele . Instead, there were some reports that the HDAs were tasked by the HEWs to conduct their visits and did not see any benefit of informing them of a delivery.
Other means of identifying delivered women were using the expected date of delivery, word of mouth and being informed by the family. Using the expected date of delivery was reported as problematic as the date were not accurate, and word of mouth was only useful where HEWs were very active in the community and made regular visits. In kebele A, in Amhara, and kebele C, in SNNPR, HEWs reported that the women themselves were meant to inform the HEW of the delivery, but mothers did not know that they should inform the HEW, and this mechanism was not functioning.
At the time of the study, few women in the study Kebles reported delivering at home, with major efforts from HEWs and HDAs to ensure all women delivered in a facility. Delivering at home was reported as shameful, with threats of sanctions and a fear that the HEW and HDA would be angry. Respondents from the mother, father and HEW/HDA FGDs all reported that HEWs would not know about women who delivered at home ‘If a woman gives birth at home, the HEWs won’t hear about it. Nobody tells them that she has given birth’ [ kebele A, Amhara, Mother – FGD]. In the few cases we found where the HEWs knew about a home delivery, the women felt that they were denied PNC visits as a sanction for not delivering at a facility or not attending ANC, and this was reiterated in a mothers in the FGDs: ‘ If she [mother] refused and decided to stay at home, they [HEW] will never visit her and she just sit at her house alone….they won’t be at her side [kebele A, Amhara, Mother- FGD]. In general attending ANC was a proactive decision by the family, while the families’ roles in receiving PNC visits was passive, with no active care seeking decisions in relation to the home visits. We found no pattern or link between attending ANC and receiving a PNC visit.
Other minor themes related to HEWs being unaware of deliveries, that were reported in the HEW/HDA FGDs, were that some first time mothers travel to their own mother in another kebele to deliver, and that unmarried ‘teenagers’ keep their pregnancies and deliveries secret due to the stigma attached to them.
Work issues
Two main sub themes related to work issues that affected whether timely PNC visits were made were: HEW availability and HEW work ethic and organization. Mothers, HEWs and HDAs reported workload and HEW availability as barriers to making timely PNC visits. Issues included being unavailable for visits as they were escorting women for delivery, multiple women delivering in different locations at the same time, staff absences, and participation in training workshops, meetings and health campaigns: ‘There are only two HEWs. They have lots of activities, which they are expected to perform. Therefore, they cannot cover all mothers in the three days after delivery’ [ kebele C, SNNPR, Mother – FGD]. Some HEWs were more organized in terms of dividing up the community and having a clear plan for visiting communities, and these plans facilitated early visits.
Differences in HEW work ethic was also identified as a reason for no or late PNC visits, and the main differences between the kebele with reported high and low levels of early PNC visits was the general level of activity of the HEWs. In kebeles with low PNC visits HEWs were reported as only coming to the community for vaccinations, being rarely at the health post, or rarely leaving the health post: ‘They [HEWs] spend the whole day here [at health post] but no one come to here…..they didn’t go inside the village’ [ kebele D, SNNPR, Father - FGD]. Temporary HEWs were reported as having particular issues with poor links with the community and with the HDA. This translated into few PNC visits being made: ‘Such staff [temporary] have a feeling that they will not be there in the kebele for long and show some sort of reluctance. They will not take their job … they believe that another person will take over from them very soon’ [ kebele A, Amhara, HEW – FGD]. In kebeles with low PNC coverage the HEWs sometimes relied on strong HDA teams to conduct activities, or were reported as only being interested in ensuring facility deliveries occurred.
In contrast, in those kebeles with reported high PNC coverage, community members described a general high level of HEW activity and a sense of connectedness between the community and the HEW:
‘ They themselves live with us. They are with us when the baby is delivered. They visit us every day. They do not do only visiting within three days. They call for Ambulance; they escort us to the health facility and assist us in delivery’ [ kebele B, Amhara, Mother - FGD].
Home visits by community health workers to provide postnatal care have the potential to reduce newborn mortality [ 5 , 6 ], but observational data suggest that these need to occur within 24 h to be effective [ 8 ]. Despite the importance of PNC visits, achieving early visits in sub Saharan African settings has proved difficult [ 6 , 9 , 10 , 11 , 25 ], and there has been little research on why early visits are not achieved. We found that visits were affected by three inter-linked issues: physical issues (accessibility and transport), information issues (whether the HEW knows about the delivery), and work issues (HEW availability and performance).
Accessibility as a barrier to CHW performance has been found in several settings [ 26 ], and there were areas in all the study sites that were inaccessible due to topography or distance constraints. We found that moderate accessibility issues were not barriers to early visits if HEWs were active, organized and well connected to the community. Care should be taken when demarcating work areas to exclude areas that are unreachable; such areas may require their own CHW for timely visits to occur. The demarcation of small and realistic catchment areas was hypothesized as a reason why Village Health Workers (VHW) in a study in Bangladesh achieved a coverage of early home visits of 87% [ 13 ].
Knowing that a delivery has occurred was essential for HEWs making a timely PNC visit, and no or late notification of a delivery has been identified as a barrier to early home visits in other settings [ 8 , 10 , 13 ]. In the study areas formal notification strategies existed through HDAs informing HEWs of a delivery, although this did not always occur despite the existence of enhanced tracking of pregnant women through L10Ks’ Community Based Data for Decision Making platform. Timely notification by HDAs was hindered by distance, and HDAs did not report using mobile phones for notification. Providing mobile phones or air time could improve notification rates, with an association between having the HEWs phone number and receiving an early PNC visit found in a previous Ethiopian study [ 14 ]. Evidence suggests that using mobile phones to increase communication is highly valued by CHWs because it reduces travel time and enhances efficiency [ 27 ], however, this may be difficult where mobile phone coverage levels are low.
In two of the study kebeles families notified the HEWs directly when they went into labour, and HEWs played an active role in calling an ambulance or assisting with the delivery. This demonstrates that when families are aware of the need to notify a HEW, and have a reason to do so, then they are able and willing to do this. Our study suggests that family led notification, especially if done in labor, may result in earlier PNC visits than HDA led notification. Family led notification is likely to be enhanced by HEWs making pregnancy visits, especially if family members are included [ 10 , 14 ], as this may improve links between the HEW and the family, and helps ensure that families know their role in notification. Facilities did not play a role in the notification process in the study kebeles . As rates of facility delivery increase facilities could play an important role in notification, particularly for newborns identified as high risk who may benefit most from early visits. The passive role that families currently play in PNC home visits may explain why we saw no pattern in visits by education levels, mirroring the lack of association between socio demographic characteristics and PNC visits found in other studies [ 10 , 11 , 14 ].
Issues with HEW availability were also reported as affecting PNC coverage, with competing tasks meaning that HEWs were not always available for timely visits. Such factors are largely out of control of the HEWs, and care needs to be taken to ensure that CHW tasks are feasible and take into account travel time. There was some evidence that HEWs and HDAs were focusing on facility deliveries to the detriment of their other activities.
The greatest difference between kebeles with high and low PNC coverage was the general activity level of the HEW. This affected notification issues and was more important than moderate physical barriers. In some kebeles , HEWs were reported as rarely coming to the community or relying on active HDAs to perform tasks, whilst in others they were reported as making frequent visits and were clearly well connected to the community. There was a particular problem with temporary workers. The role of motivation in performance is well recognized and numerous studies have reported on general motivators of CHWs. Few studies have explored variability in motivation across areas, nor the role of contextual issues, although these appear to be important [ 26 ]. We identified only one study that aims to rigorously evaluate methods of improving CHW motivation: the results of this study are yet to be reported and more research is needed [ 28 ].
We found little evidence of socio-cultural barriers from the community side for early visits, except that home delivery may be a barrier for notifying HEWs for fear for sanctions, and that some first time mothers travel to their home community for delivery. The use of sanctions for those who deliver at home may lead to vulnerable families not receiving vital services. There is much attention now being paid to the disrespect and abuse of women in facilities [ 29 , 30 ]: there is also the potential for this to occur during home visits.
During this study we took several steps to maximize data quality and data transferability such as the use of multiple study sites, methods and respondent groups; the use of methods that aimed to overcome social desirability bias; purposive sampling to saturation; regular meetings and feedback during data collection to enhance reflective thinking; triangulation of data and team analysis. Despite this there is the potential for reporting and recall bias. Data were collected from small geographic areas that were accessible to the study teams and had reasonably functioning HEW systems, the findings may not apply to other areas with significantly different contextual issues, however the study findings suggest several issues that could be explored and considered when exploring issues related to PNC coverage in other settings. Studies in other settings in Ethiopia would further enhance transferability.
If timely postnatal home visits are to occur, programs need to ensure that CHWs have realistic catchment areas that reflect their workload. Inaccessible areas may need their own CHW. Good notification systems are essential, families will notify CHWs if they have a clear reasons to do so, and more work is needed on how to ensure other potential notification systems function. Work ethic was a clear influencer on whether home visits occur, studies to date have tended to explore the motivation of CHWs as a group rather than exploring differences between CHWs, more studies on understanding motivation at an individual level are needed.
Darmstadt GL, Kinney MV, Chopra M, Cousens S, Kak L, Paul VK, et al. Who has been caring for the baby? Lancet. 2014;384(9938):174–88.
Article PubMed Google Scholar
Lawn JE, Blencowe H, Oza S, You D, Lee AC, Waiswa P, et al. Every newborn: progress, priorities, and potential beyond survival. Lancet. 2014;384(9938):189–205.
World Health Organization. WHO recommendations on postnatal care of the mother and newborn. Geneva: World Health Organization; 2013. Report No.: 978 92 4 150664 9
Google Scholar
World Health Organization and UNICEF. Home visits for the newborn child: a strategy to improve survival. Geneva: World Health Organization and UNICEF; 2009.
Gogia S, Sachdev HS. Home visits by community health workers to prevent neonatal deaths in developing countries: a systematic review. Bull World Health Organ. 2010;88(9):658–666B.
Article PubMed PubMed Central Google Scholar
Kirkwood BR, Manu A, ten Asbroek AH, Soremekun S, Weobong B, Gyan T, et al. Effect of the Newhints home-visits intervention on neonatal mortality rate and care practices in Ghana: a cluster randomised controlled trial. Lancet. 2013;381(9884):2184–92.
McPherson R, Hodgins S. Postnatal home visitation: lessons from country programs operating at scale. J Glob Health. 2018;8(1):010422.
Baqui AH, Ahmed S, El Arifeen S, Darmstadt GL, Rosecrans AM, Mannan I, et al. Effect of timing of first postnatal care home visit on neonatal mortality in Bangladesh: a observational cohort study. BMJ. 2009;339:b2826.
Waiswa P, Pariyo G, Kallander K, Akuze J, Namazzi G, Ekirapa-Kiracho E, et al. Effect of the Uganda newborn study on care-seeking and care practices: a cluster-randomised controlled trial. Glob Health Action. 2015;8:24584.
Sitrin D, Guenther T, Murray J, Pilgrim N, Rubayet S, Ligowe R, et al. Reaching mothers and babies with early postnatal home visits: the implementation realities of achieving high coverage in large-scale programs. PLoS One. 2013;8(7):e68930.
Article PubMed PubMed Central CAS Google Scholar
Callaghan-Koru JA, Nonyane BA, Guenther T, Sitrin D, Ligowe R, Chimbalanga E, et al. Contribution of community-based newborn health promotion to reducing inequities in healthy newborn care practices and knowledge: evidence of improvement from a three-district pilot program in Malawi. BMC Public Health. 2013;13:1052.
Hanson C, Manzi F, Mkumbo E, Shirima K, Penfold S, Hill Z, et al. Effectiveness of a home-based counselling strategy on neonatal care and survival: a cluster-randomised trial in six districts of rural southern Tanzania. PLoS Med. 2015;12(9):e1001881.
Shah R, Munos MK, Winch PJ, Mullany LC, Mannan I, Rahman SM, et al. Community-based health workers achieve high coverage in neonatal intervention trials: a case study from Sylhet. Bangladesh J Health Popul Nutr. 2010;28(6):610–8.
PubMed Google Scholar
Tesfaye S, Barry D, Gobezayehu AG, Frew AH, Stover KE, Tessema H, et al. Improving coverage of postnatal care in rural Ethiopia using a community-based, collaborative quality improvement approach. J Midwifery Womens Health. 2014;59(Suppl 1):S55–64.
The Last Ten Kilometers. Community based newborn care. In: Kilometers TLT, editor. News from the last ten kilometers. Addis Ababa: The Last Ten Kilometers; 2014.
Banteyerga H. Ethiopia's health extension program: improving health through community involvement. MEDICC Rev. 2011;13(3):46–9.
Koblinsky M, Tain F, Gaym A, Karim A, Carnell M, Tesfaye S. Responding to the maternal health care challenge: The Ethiopian Health Extension Program. Ethiop J Health Dev. 2010;24(Special Issue 1):105–9.
Legesse H, Degefie T, Hiluf M, Sime K, Tesfaye C, Abebe H, et al. National scale-up of integrated community case management in rural Ethiopia: implementation and early lessons learned. Ethiop Med J. 2014;52(Suppl 3):15–26.
Karim AM, Admassu K, Schellenberg J, Alemu H, Getachew N, Ameha A, et al. Effect of ethiopia’s health extension program on maternal and newborn health care practices in 101 rural districts: a dose-response study. PLoS One. 2013;8(6):e65160.
The Last Ten Kilometers. Improving maternal and newborn health care practices. The role of community based data for decision making in: kilometers TLT, editor. News from the last ten kilometers. The Last Ten Kilometers: Addis Ababa; 2013.
Betemariam B, Karim A, Getachew N. Evidence based scaling-up an innovative community-based maternal and newborn health strategy in Ethiopia. In: 141st American Public Health Assocition annual meeting. Boston, USA; 2013.
Darmstadt GL, Marchant T, Claeson M, Brown W, Morris S, Donnay F, et al. A strategy for reducing maternal and newborn deaths by 2015 and beyond. BMC Pregnancy Childbirth. 2013;13:216.
Karim A. Effectiveness evaluation of a large-scale community-based program: Lessons from Ethiopia. Annals of Global Health. 2015;81(1):192.
Article Google Scholar
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland: CSA and ICF. p. 2016.
Penfold S, Manzi F, Mkumbo E, Temu S, Jaribu J, Shamba DD, et al. Effect of home-based counselling on newborn care practices in southern Tanzania one year after implementation: a cluster-randomised controlled trial. BMC Pediatr. 2014;14:187.
Kok MC, Kane SS, Tulloch O, Ormel H, Theobald S, Dieleman M, et al. How does context influence performance of community health workers in low- and middle-income countries? Evidence from the Literature Health Res Policy Syst. 2015;13:13.
Thondoo M, Strachan DL, Nakirunda M, Ndima S, Muiambo A, Kallander K, et al. Potential roles of Mhealth for community health workers: formative research with end users in Uganda and Mozambique. JMIR Mhealth Uhealth. 2015;3(3):e76.
Kallander K, Strachan D, Soremekun S, Hill Z, Lingam R, Tibenderana J, et al. Evaluating the effect of innovative motivation and supervision approaches on community health worker performance and retention in Uganda and Mozambique: study protocol for a randomised controlled trial. Trials. 2015;16:157.
Bohren MA, Vogel JP, Hunter EC, Lutsiv O, Makh SK, Souza JP, et al. The Mistreatment of Women during Childbirth in Health Facilities Globally: A Mixed-Methods Systematic Review. PLoS Med 2015;12(6):e1001847; discussion e1001847.
Freedman LP, Kruk ME. Disrespect and abuse of women in childbirth: challenging the global quality and accountability agendas. Lancet. 2014;384(9948):e42–4.
Download references
The study was funded by the Bill and Melinda Gates foundation as part of the IDEAS study.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available due to issues of confidentiality and privacy. Although respondents’ names are not included in transcripts they do include place names and any names mentioned by respondents, for example, names of Health Extension Workers.
Author information
Authors and affiliations.
Consultancy for Social Development, PO Box 70196, Addis Ababa, Ethiopia
Yared Amare
London School of Hygiene and Tropical Medicine, Keppel Street, London, WC1E 7HT, UK
Pauline Scheelbeek, Joanna Schellenberg & Della Berhanu
University College London, 30 Guilford Street, London, WC1N 1EH, UK
You can also search for this author in PubMed Google Scholar
Contributions
ZH and JS conceived the study; ZH, YA and PA designed the study and the data collection tools. YA, PA and DB were responsible for the acquisition of data. ZH, PS and YA were responsible for analysing and interpreting the data. ZH and YA prepared the first draft of the paper and all authors commented on the paper and approved the final version.
Corresponding author
Correspondence to Zelee Hill .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was obtained from the Institutional Review Boards of the London School of Hygiene and Tropical Medicine and the Ministry of Science and Technology in Ethiopia. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Amare, Y., Scheelbeek, P., Schellenberg, J. et al. Early postnatal home visits: a qualitative study of barriers and facilitators to achieving high coverage. BMC Public Health 18 , 1074 (2018). https://doi.org/10.1186/s12889-018-5922-7
Download citation
Received : 29 August 2017
Accepted : 01 August 2018
Published : 29 August 2018
DOI : https://doi.org/10.1186/s12889-018-5922-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Community health worker
- Qualitative
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Your baby after the birth
Having skin-to-skin contact with your baby straight after the birth can help keep her or him warm and can help with getting breastfeeding started.
First feed, weight gain and nappies
Some babies feed immediately after birth and others take a little longer.
The midwives will help you whether you choose to:
- feed with formula
- combine breast and bottle feeds
It's normal for babies to lose some weight in the first few days after birth. Putting on weight steadily after this is a sign your baby is healthy and feeding well.
Read more about your baby's weight , and your baby's nappies, including healthy poo .
Tests and checks for your baby
A children's doctor (paediatrician), midwife or newborn (neonatal) nurse will check your baby is well and will offer him or her a newborn physical examination within 72 hours of birth.
In the early days, the midwife will check your baby for signs of:
- infection of the umbilical cord or eyes
- thrush in the mouth
On day 5 to 8 after the birth, you'll be offered the blood spot (heel prick) test for your baby.
Before you baby is 5 weeks old you should be offered a newborn hearing screening test .
If your baby is in special care , these tests may be done there. If your baby is at home, the tests may be done at your home by the community midwife team.
Learn how to tell when a baby is seriously ill .
Safe sleeping for your baby
Make sure you know how to put your baby to sleep safely to reduce the risk of sudden infant death syndrome (SIDS) .
2 weeks and beyond
You don't need to bathe your baby every day. You may prefer to wash their face, neck, hands and bottom carefully instead.
Most babies will regain their birthweight in the first 2 weeks. Around this time their care will move from a midwife to a health visitor.
The health visitor will check your baby's growth and development at regular appointments and record this in your baby's personal child health record (PCHR) , also known as their "red book".
You after the birth
The maternity staff caring for you will check you're recovering well after the birth.
They will take your temperature, pulse and blood pressure.
They'll also feel your tummy (abdomen) to make sure your womb is shrinking back to its normal size.
Some women feel tummy pain when their womb shrinks, especially when they're breastfeeding. This is normal.
Seeing a midwife or health visitor
Midwives will agree a plan with you for visits at home or at a children's centre until your baby is around 10 days old. This is to check that you and your baby are well and support you in these first few days.
Bleeding after the birth (postnatal bleeding)
You'll have bleeding (lochia) from your vagina for a few weeks after you give birth.
The bleeding usually stops by the time your baby is 12 weeks old.
Non-urgent advice: Speak to your GP, midwife or health visitor if you've got postnatal bleeding and any of these:
- a high temperature over 38C
- the bleeding smells unusual for you
- tummy pain that gets worse
- the bleeding gets heavier or doesn't get any less
- lumps (clots) in the blood
- pain between the vagina and anus (perineum) that gets worse
It could be a sign of infection.
Make sure you know the signs of a serious heavy bleed after giving birth (postpartum haemorrhage, or PPH). This is rare and needs emergency care.
Immediate action required: Call 999 if you've got postnatal bleeding and:
- the bleeding suddenly gets heavier
- you feel faint, dizzy or have a pounding heart
This could mean you're having a very heavy bleed (postpartum haemorrhage) and need emergency treatment.
Read more about your body after the birth , including when you might need urgent medical attention.
Feeding your baby
When you're breastfeeding in the early days , breastfeed your baby as often as they want. This may be every 2 hours.
Let your baby decide when they've had enough (this is called baby-led feeding).
You can express your breast milk if you're having problems with breastfeeding . Problems can include breast engorgement or mastitis .
Get breastfeeding and bottle feeding advice .
Your baby's crying
Crying is your baby's way of telling you they need comfort and care. It can be hard to know what they need, especially in the early days.
There are ways you can soothe your crying baby .
How you feel
Find out how to cope if you feel stressed after having a baby . There are support services for new parents that may help.
You may feel a bit down, tearful or anxious in the first week after giving birth. This is normal.
If these feelings start later or last for more than 2 weeks after giving birth, it could be a sign of postnatal depression .
Postnatal depression and anxiety are common, and there is treatment. Speak to your midwife, GP or health visitor as soon as possible if you think you might be depressed or anxious.
Sex and contraception
You can have sex as soon as you feel ready after having a baby.
There are no rules about when to have sex after giving birth. Every woman's physical and emotional changes are different.
You can get pregnant from 3 weeks (21 days) after giving birth. This can happen before you have a period, even if you're breastfeeding.
You need to start using contraception from 21 days after the birth every time you have sex if you don't want to get pregnant again.
Talk to your doctor, midwife or contraception (family planning) nurse about contraception after having a baby . They can arrange contraception before you have sex for the first time.
Being active may feel like a challenge when you're tired, but gentle exercise after childbirth can help your body recover and may help you feel more energetic.
You should also do pelvic floor exercises to strengthen the muscles around your bladder, vagina and anus.
Page last reviewed: 8 July 2022 Next review due: 8 July 2025
Ready Steady Baby
Home visits.
You should be visited several times by your midwife or family nurse at home during the first 10 days. Friends and family will want to visit to meet your baby too.
It’s OK to ask visitors to:
- call you first and to sometimes say no
- help with other things so you can have a rest or spend time with your baby
Extra support
Some new parents need more support than others. You’ll get extra support from your midwife, family nurse or other health professionals if your baby:
- was born early
- spent time in special or intensive care
- has additional needs
Tests and checks
During the first 10 days your midwife will:
- weigh your baby
- do a newborn blood spot test if you agree
You’ll also need to register your baby with a GP
More about newborn blood spot tests
Your health visitor
A health visitor’s a registered nurse or midwife who’s done further study in public health nursing.
Your health visitor will:
- take over from your midwife when your baby’s 11 days old
- get to know you and your baby
- ensure you get all the help and support you need as your baby grows
Your baby’s named person
In Scotland, the aim is that every child, young person and their parents have a `named person’ who is a clear and safe point of contact to seek support and advice about any aspect of your child’s wellbeing.
From when your child is born until they start school, your named person is your health visitor.
Your baby’s named person will:
- be a good person for you to ask for information or advice about being a parent
- talk to about any worries
- support you to look after yourself and your baby
They can also:
- put you in contact with other community professionals or services
- help you make the best choices for you and your family
The Red Book
You’ll be given a personal child health record called the Red Book. You can use it to record information about your baby’s growth, development, tests and immunisations.
Keep it safe and take it to any appointments you have with a healthcare professional.
The family nurse

Family nurses offer the Family Nurse Partnership (FNP) programme to young, first-time parents from early in their pregnancy until their child’s 2 years old. This program is available to first-time parents under the age of 20.
The programme includes home visits from a family nurse while you’re pregnant, and after your baby’s born. These visits help:
- to have a healthy pregnancy
- you and your baby grow and develop together
- you to be the best parent you can be.
Your health visitor will take over from your family nurse when your baby is two until they go to school.
The Scottish Government has more information about Family Nurse Partnership
Translations and alternative formats of this information are available from Public Health Scotland .
If you need a different language or format, please contact [email protected].
- Ready Steady Baby leaflet in Arabic, Polish, Simplified Chinese (Mandarin) and Ukrainian
- Ready Steady Baby leaflet in English (Easy Read)
Source: Public Health Scotland - Opens in new browser window
Last updated: 19 December 2023
Help us improve NHS inform
Your feedback has been received
Don’t include personal information e.g. name, location or any personal health conditions.
Also on NHS inform
Other health sites.
- Disabled Living Foundation (DLF)
- Rica: consumer research charity
- Health & Care Professions Council (HCPC)


Prattville Home Midwifery, LLC

Midwifery Care
A midwife is a trained professional who specializes in caring for women in any stage of life, especially before, during, and after childbirth. The m idwifery philosophy of care focuses on the whole-person, rather than medical intervention. We strive to provide holistic care that encompasses the physical, psychological, social, and spiritual aspects of the healthcare experience. We are passionate about educating and empowering our clients to make informed decisions about their health and actively work to ensure that our services are accessible and inclusive to all. We believe that everyone should have access to quality care and strive to provide it.
At Prattville Home Midwifery, LLC we specialize in providing evidenc e-based gynecological care, family planning, prenatal care, and home-birth services for low-risk pregnancies. Kim Taylor, CNM is an experienced midwife who is dedicated to providing inclusive and personalized care with sensitivity and compassion.

Annual Wellness Visits
A Happy, Healthy You. We offer pap smears, breast/chest exams, mammogram referrals, yearly lab monitoring, and STI screenings.

Pregnancy and Birth
Offering prenatal, birth, and postpartum care to low-risk birthing people in the location of their choice.

Contraception Management
Whether you simply need a refill of your birth control or a consult to decide the best method for you. We offer IUDs and Implants, too!

Routine STI screening
Screening for all sexually transmitted infections by collecting urine, swabs, and blood draws.

"Problem" Gynecology Visits
Common issues include UTI symptoms, irregular or painful periods, vaginal infections, pain with intercourse, or hormonal imbalances like PCOS.

Hormone Support
Offering both integrative medicine and basic hormone therapy options to support menopause, fertility, and trans-individuals (coming soon).

Clinic Hours
7:30 am to 1:00 pm
Prattville Home Midwifery (and midwife Kim) believes that your care provider should offer evidence-based, compassionate, trauma-informed care that is also anti-racist, weight inclusive, and identity-affirming. We believe in providing you access to truly informed consent (and declination), with respect to your right to autonomy over your body.
210 Medical Center Dr.
Prattville, AL 36066
334-895-3705
Fax: 334-568-6755
- Tech & Science
5 reasons to visit Moscow
Currently hosting the Confederations Cup, and home to some of the most beautiful medieval churches, Moscow is a city one never forgets when visiting. From skyscrapers, art galleries, to the hustle and bustle of the Russian capital, Moscow is a city one should visit in their life.
Advertisement
From ballet, to Russian architect, to galleries and vodka. Russia is a diverse city. The Russian capital is deemed to be one of the most beautiful in the world. Naturally being the capital of the largest country in the world, Moscow is sure to impress. Here are five reasons why Moscow should be your next destination.
1. Moscow’s Architect and Art
Leave your hotel or Airbnb and not too far, you’ll feel as if you time travelled back into Russian history as one feels it when walking through the streets of Moscow. Take a trip to the Kremlin and Red Square where one is sure to have their breath taken away with these magnificent views. Keeping up the with the Russian style, it is home to Saint Basil’s Cathedral, one of Moscow’s most iconic landmarks, as well as the Kremlin Palace, the official residence of the Russian president.
One can also take in views of the Moskva River. Tverskaya Street can give a Soviet Empire taste to tourists and can also be found in Moscow Central avenues. Now, when it comes to art in Moscow, look no further for a museum that will give a sense of the Russian culture. From the Moscow Museum of Modern Art to the State Tretyakov Gallery, all are bound to give you a unique experience with their collections and exhibitions as well.
2. City Parks
We know we know, we constantly brag about each cities parks, but each one has a unique vibrancy to them, and Moscow exceeds the expectations when it comes to parks. Becoming the “pride” of Moscow, and more “green” the parks of Moscow give peace and tranquillity. Never short of something to do one can ride a bike, play sports, go to a cafe or concert, or simply just take in the incredible views and just relax and walk. Fili Park, and Sokolniki Park are just of the many parks that are deemed to be an experience.
3. Nightlife
Like most cities, Russia has an amazing nightlife culture. Home to one of the most common alcoholic beverages, vodka, one can be sure to have a surreal experience when it comes to the nightlife in this vibrant capital. Diverse more than ever before, Moscow offers not only spectacular nightclubs and bars, but also distinctive ones. From amazing cocktails, to trendy bars, to intellectual bars where the hip hang out, Moscow gives away to some of the most fun nightlife cultures around.
4. Theater Traditions
If nightlife isn’t really your thing, and you’d much rather settle for a night out to the theatre then Moscow might as well become your second home. Theatres thrive in Moscow as plays and ballets are guaranteed to give a spectacular evening and experience. The Bolshoi Theater is among one of the most famous not just in Moscow or Russia, but the world. The theatre offers world famous opera and ballet performances guaranteed to have you on your feet at the end. Not in the mood for the old, then go for the new! New theatres such as the Praktika Theatre give contemporary performances with a modern vibe.
5. The Metro
You’re probably not going to see another metro or subway classier and pretty as this one. It’s no dirty and confusing New York City subway, nor is it as modern as the Tokyo metro but it is one of the most beautiful and largest in the world, not to mention convenient when getting around the city. With its dramatic sculptures, beautiful architecture, and detailed mosaics, it is sure to leave you with a lasting impression. Not only are they transportation systems but they’ve become tourist attractions with their unique stations.

Stephanie Valenzuela
Address Beach Resort: The world's highest infinity pool has opened in Dubai
New zealand volcano: five dead after white island eruption, hurricane michael may have forever changed unspoiled part of florida pan, hurricane florence brings devastating flooding, damaging winds and storm surge t, nepal says will measure mount everest next year to see if lost height, thousands evacuated as volcano rumbles on indonesian holiday spot bali, twitter has suspended one million accounts for promoting terrorism, review - kingsman: the secret service, how to obtain healthy teeth using qi-gong, an ancient practice, ethan coen's film career, depression can be set off by poor family relations, foo fighters crack down on ticket touts in london, a new experience for learner drivers, ny red bulls' fall to sporting kc, how to interpret a reading for your class, sophia loren's illustrious career, instagram may switch to a four-across photo grid system, canelo vs ggg fight ends in draw and controversy, how can you use social media to find a date this weekend, hurricane maria officially makes landfall in puerto rico, future prison sentence for the man who broke a baby's ribs and legs, review: 'archer' post dreamland, jeremy iron's film career, lions trash giants, cormier reinstated; ufc 214 result overturned strips jon jones of championship, energy - where does the gas come from to fuel the uk economy, a year of new apple, the hurricane name game, james marsden's film and entertainment career, poor lifestyle is more damaging to your health than low dose radiation, foods to keep you well this autumn, tom hardy's film career, potus & flotus test positive for covid-19, trump's health risks, economic impact.
With US President Donald Trump and First Lady Melania Trump announcing early Friday that they had tested positive for the coronavirus — after playing down the pandemic for months — reactions ...
Dr. Dre hospitalized after reportedly suffering brain aneurysm
Elon musk is now the richest person in the world, passing jeff bezos.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Prev Med
- v.5(1); 2014 Jan
Comparison of Effects of Home Visits and Routine Postpartum Care on the Healthy Behaviors of Iranian Low-Risk Mothers
Seyedeh t. mirmolaei.
Department of Midwifery, Faculty of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran
Mehrnoosh A. Valizadeh
Mahmood mahmoodi.
1 Department of Biostatistics, Faculty of Health, Tehran University of Medical Sciences, Tehran, Iran
Zeinab Tavakol
Background:.
Postpartum care at home is a post delivery care method that can be provided by public health nurses, trained health workers, or midwifery nurses. A study conducted to compare effect of two midwife visits at home to usual postpartum care on the healthy behaviors of low-risk Iranian mothers.
A randomized controlled trial conducted on 200 mothers at a reference center for screening for infant hypothyroidism in Tehran. Mothers were randomized to either home-based ( n = 100) or routine-based postpartum care ( n = 100). Each mother and her neonate received two cares. Home-based cares were provided by a midwife in the intervention group. Postpartum cares in the control group were provided by care providers of primary health care system. Healthy behavior was measured using a validated and reliable researcher made instrument. The data were analyzed using independent sample t -tests, paired t -test, and χ 2 -test.
The data showed that a significant number of subjects in the control group did not receive their postpartum care ( P < 0.001). The mean score of maternal healthy behaviors in the intervention group increased from 120.5 (SE = 0.76) to 148.9 (SE = 1.02) ( P < 0.001) and in the control group from 119.9 (SE = 1.06) to 140.9 (SE = 1.08) ( P < 0.001). The mean score of maternal healthy behaviors in the intervention group had significant differences with that in the control group at the end of study ( P < 0.001).
Conclusion:
Early postpartum care at home by trained midwives can be positively effective for improving maternal healthy behaviors in less developed countries.
INTRODUCTION
Postpartum time is a critical physiological adaptation phase and therefore has a meaningful impact on the future maternal and neonatal health.[ 1 , 2 ] Its importance is also due to the risk level of mortality and morbidity in this period. In recent years, about 40% of the under 5 year deaths have occurred in the neonatal period in the world.[ 2 ] Estimates show that over four million neonatal deaths occur annually within the first 4 weeks after birth in the world and about 3 million cases in the early neonatal period.[ 2 ] On the other hand, approximately 50 million women are annually affected by postpartum maternal morbidity in the world.[ 3 ] In this period, the mother is faced with many physical and emotional challenges.[ 4 , 5 ] She also should learn about the infant-care behaviors in addition to her health problems. Hence, the mother needs more social, educational, and medical support.[ 6 ]
Studies have shown that a considerable rate of maternal morbidity and mortality is inevitable by standard postpartum care.[ 7 ] Although some efficient postpartum care packages have been identified and confirmed to reduce neonatal mortality and morbidity,[ 8 , 9 , 10 , 11 , 12 , 13 ] postpartum health care is a neglected issue.[ 14 ] This inadequacy occurs during the routine postpartum care where the mother's demands do not meet the provided care[ 14 ] and leads to chronic and long-term health problems.[ 15 , 16 ]
From the past, providing appropriate care based on sociocultural beliefs and economic status of the mother is considered a goal for standard care.[ 17 ] It is due to deep influence of many factors including the performance of service providers, enjoying social support, and the rate of adaption to the mother conditions on the effectiveness of this care.[ 18 , 19 , 20 , 21 , 22 ]
Postpartum care at home is a post delivery care method that can be provided by public health nurses, trained health workers, or midwifery nurses.[ 20 , 23 ] This type of maternal and neonatal care includes mother and neonate health problems assessment and training for self and child care and also, under particular conditions, refers them to specialized maternal and neonatal service centers.[ 24 , 25 ]
Although the general efficacy of home visits as a type of postpartum care has been approved in various studies,[ 8 , 9 , 10 , 11 , 12 , 13 , 26 , 27 ] its effects are influenced by socioeconomic and cultural conditions of the mother and her family.[ 19 ] Therefore, assessing its effects in different settings would be reasonable.
Bashour et al .[ 3 ] from Syria have shown that postpartum home care improved the exclusive breastfeeding but has not any other positive effects on maternal or neonatal health status. Against their results, Quinlivan and his colleagues concluded that postpartum home visiting do not have any improving effect on breastfeeding but positively affect the contraception usage and adverse neonatal events.[ 9 ]
Although postpartum care at home is universal in many western countries, but in less developed countries such as Iran, it is not known as a widespread and routine program.[ 26 ] In Iran, although postpartum care is usually provided in governmental and nongovernmental facilities, all these types of care are provided outside of the home. The high costs[ 26 ] or lack of controlled trial studies that provide some positive evidence on efficacy of this method in Iranian cultural and the socioeconomic conditions are two main obstructing factors for providing this type of care as a routine care. Therefore, as a part of evidence providing on postpartum home visiting in Iran, effects of postpartum care provided at home were compared with outside home routine cares on the low-risk Iranian mothers during 2010.
This study was a randomized controlled trial of 200 mothers who had recently given birth during September–December 2010. The Ethics Committee of Tehran University of Medical Sciences approved the study protocol. The sampling was conducted at a reference center for screening infant hypothyroidism in Tehran. The convenient sampling method was used in this study. On the basis of a pilot study and considering the assumptions of 90% of the statistical power, a two-sided a error of 0.05% and 20% drop-out rate, the original sample size was estimated 100 persons in each group.
The inclusion criteria were limited to a woman who had a healthy and term newborn in her recent low-risk pregnancy, recourse to the sampling environment between 3 and 5 days after delivery, received the first postpartum care in health service centers by a general physician and a dentist, ability to discuss and understand the Persian language, and being a resident of any of 10, 11, or 17 zones of Tehran metropolitan and the first or second birth order for her infant. The exclusion criteria were consisting of known physical or mental disorder in each mother or neonate, divorce, and also mother or infant hospitalization for more than 72 h.
After initial sampling, study information and participation guidelines were explained to the mother and she was asked to complete and sign the informed consent form. Then using a table of random numbers, subjects were manually assigned to intervention and control groups. Baseline data were collected prior to random allocation.
Following the random allocation, each mother and her neonate were assigned four cares: Two for the mother and two for the newborn. The first maternal (second based on the national guideline) was within 10-15 days and the second (third based on the national guideline) within 42-60 days after delivery. Neonatal cares provided simultaneously with maternal care.
Postpartum care package was the same to both groups, according to the Iranian National Guideline of Maternal and Neonatal Postpartum Cares designed by Ministry of Health (revised Spring 2008) but for the intervention group, care was assigned at home whereas routine postpartum care for the control group was provided at health service centers. On the basis of our national guideline, postpartum care includes three cares at 3-5, 10-15, and 42-60 days after delivery. In this study, mothers and their neonates received the first postpartum care at health service centers in both groups. Second and third cares were provided by health care providers (who are mostly midwives) at a referral health service center for the control group and by a trained midwife for the intervention group.
Postpartum home visiting includes greeting and establishing an intimate relationship with the mother, identifying mother's socioeconomic status (SES) and lifestyle, assessing vital signs, consciousness, alcoholism, convulsion, breathing problems, abdominal or flank pain, any bleeding, suture complications, defection problems, vertigo, inflammation of the gums, shock, symptoms of psychological disorders, comorbidities and medical history, consultations on family planning (FP), breastfeeding and medicinal supplements, examination of extremities, breasts, eyes, abdomen and urinary and reproductive organs, identifying wife and any social abuse and as a main component providing health education based on her SES and health status.
The data collection instrument was consisted of two structured semi-self-reported questionnaires. First of them was designed for assessment of background and demographic data and second for evaluation of maternal healthy behaviors. Questionnaires were reviewed and approved by a team of 10 members of the midwifery department in Tehran University of Medical Sciences for face and content validity. The reliability of the maternal healthy behavior questionnaire was assessed by estimating the correlation coefficient of test–retest with 15 days interval and also Cronbach's α. The correlation coefficient of the first and second responses and overall α were estimated to be 75% and 72%. This instrument was included 64 questions and 9 categories.
The outcome was assessed at 2 months after the start of the study. Our desired outcome was maternal healthy behaviors. Healthy behaviors included maternal behaviors in relation to nutrition, physical activity, cigarette smoking and alcohol consumption, breastfeeding, FP, personal and mental health, and ability to taking care of the newborn. An outcome measure was constructed by awarding one point to each true answer and then summing up the participant points.
The data were analyzed using univariate statistical tests such as independent sample t -tests, paired t -tests, and χ 2 tests (SPSS version 11.5).
Although 200 mothers were enrolled and randomized, at the time of analysis 88 of them remained in the intervention group and 86 in the control group (The study profile is presented in Figure 1 ). In the control group, two participants were excluded because their newborns were hospitalized for over 72 h, five people had to be referred to other health centers outside the study coverage, three patients refused to continue the study, and four cases for other reasons. In the intervention group, four people were excluded because of hospitalization of their newborn for over 72 h, one due to emigration and seven others for refusal.

Full trial profile
The mean age and the standard error, respectively, were 27.18 and 0.47 in the intervention group and 3.28 and 0.51 in the control group. Comparison of the means of maternal age showed no significant statistical difference in the two groups ( P = 0.104).
Table 1 shows the data of the background and demographic characteristics of mothers between each study groups. The last right-hand column presents the P values for the corresponding variables.
Background and demographic characteristics of participants of the three study groups

Results showed the mean score of maternal healthy behaviors in the intervention group increased from 120.5 (SE = 0.76) to 148.9 (SE = 1.02) and in the control group from 119.9 (SE = 1.06) to 140.9 (SE = 1.08). The findings of the independent two-sample t -tests showed significant differences between the intervention and control groups before and after the study. Also for both groups, comparison of the mean scores of the healthy behavior before and after the intervention indicates significant differences between the two times. Table 2 shows the mean score of maternal healthy behaviors in each subcategory as well as the status of each group related to care provision.
Mean score of maternal healthy behaviors in each subcategory and status of each group related to care receiving

This study showed that postpartum home-visiting by trained midwives can improve maternal healthy behaviors. Yet, the study results suggest that healthy behaviors in both groups compared with their previous differences were statistically significant. This finding is in accordance with our earlier sentence which effectiveness of home-visits after delivery was approved by many studies.[ 12 , 28 ] However, one study ruled out improving the effectiveness of this type of care in low-risk mothers.[ 26 ] Two probable reasons to justifying this disagreement are the effects of home visiting postpartum care could be dependent on the local, cultural, and the socioeconomic conditions and also differences between hospital-based postpartum care (the control group in the study of Escobar et al .) and health service center care provided for the control group in our study. Further, several studies showed that the effect of home visits depended on several factors and believed that some of the subgroups of new mothers needed special postpartum care.[ 3 , 9 , 19 ]
Statistical comparisons of baseline characteristics showed that the groups were comparable at the baseline with the exception of the first neonatal care, which had no significant differences. This strength can improve the internal validity of the study.
Significant differences of healthy behaviors between intervention and control groups can be interpreted as a kind of difference in receiving care, because a considerable proportion of the control group do not receive at least one of the two planned care periods. The results of the study along with a lack of care by a large number of participants in the control group can provide reasons on the superiority of active postpartum care. Gogia et al .[ 23 ] conducted a systematic review and concluded that the active care provided at home by community health workers would be useful in the developing countries. Therefore, our finding can be due to postpartum home-visit is a type of active care.
Although, based on our findings, home-visits are better than routine care to improve healthy behaviors, active efforts to provide routine care may have adequate benefits. Sword et al .[ 20 ] emphasized that home-visits are more effective care than telephone follow-up care. On the other hand, studies which show that apart from the effects of care on some of the outcome, satisfaction of care was better in home-visiting[ 3 , 26 ] which clarifies that precise studies of this issue are necessary to identify cost-effective methods for postpartum care. Recommendation of routine home-visits after delivery is doubtful in developing countries because of the costs,[ 26 ] dependency of its effectiveness on various factors, and lack of evidence.
In this study, maternal care was provided twice at home and on the other hand, the outcome measurement was conducted almost immediately after the second care. Considering this and the significant results in both groups after the study follow-up, we can conclude that even one timely postpartum care at home or outside can improve the mother's ability to deal with the maternal and neonatal challenges. Bashour et al .[ 3 ] and Baqui et al .[ 21 ] also addressed this issue in separate studies. They recommended immediate and timely care after delivery. It is may be because of effects of timely providing mother's demands with lowest time from delivery. Further works can be recommended to assessing effects of various numbers of postpartum cares and also those distances from delivery.
The findings of this study indicate that home care compared with routine care had no significant effects on healthy behaviors associated with nutritional behaviors, sunbathing, and somewhat physical activity. Considering the need of long education to affect nutritional and physical behaviors of mothers against cultural and local costumes we could justify this finding. However, more research is needed to be done in this area, especially in Iran.
The results of this study confirm those of other studies[ 9 , 11 ] in relation to the significant improvements in FP behaviors by postpartum home-visits. During the postpartum period, the mother strongly feel for need of FP because of her recent hardships of pregnancy and delivery, so she looking for family planning. During home-visits, knowledge on mother's SES helps care providers to recommend best FP methods. These points may be probable justifications for significant effect of home-based FP educations.
In this study, short-term maternal mental health was influenced positively by home care more than by routine care, while it seems to have no statistically significant difference from other types of postpartum care.[ 11 ]
Like some other studies[ 3 , 26 ] and unlike evidence,[ 9 ] this study confirms a positive effect of home care on short-term breastfeeding. First time and some other mothers know less on the correct method of breastfeeding, thus they need to learn about it but during postpartum care at health service centers although care providers explain the correct breastfeeding position for them there is a public setting and mothers cannot learn and practice for breastfeeding. Against that, during home visits breastfeeding training and breastfeeding education were provided at most private setting for mothers. Considering cultural and religious barriers of public setting to teaching and also learning of female issues may help us to interpret the positive effect of home visit postpartum cares on the breastfeeding.
In this study, due to the limitations on the sample size a multivariate analysis was impossible to conduct considering potential confounders. The effects of the intervention on other subgroups of mothers were not possible to estimate because of the restriction of sampling for low-risk mothers. Nobody was blind in the study. In this study, no effort was made to control the completeness of routine care in the nonintervention group and so a remarkable proportion of this group did not receive all of three postpartum cares. The last limitation could interpret as low complete postpartum care delivery in Iran and need of active postpartum cares.
CONCLUSIONS
Early postpartum care at home by trained midwives is effective in improving maternal healthy behaviors such as breastfeeding and family planning. Due to the higher costs of home-visits and realistic assumption of the low rates of receiving routine care in developing countries such as Iran, the cost effectiveness assessments of other methods for postpartum care can enable health policymakers.
Source of Support: Master of Science thesis in midwifery funded by Tehran University of Medical Sciences
Conflict of Interest: None declared.

IMAGES
COMMENTS
Dear Editor, During the COVID-19 pandemic postnatal midwifery-led care remains a key public health intervention for women and their families 1,2.Home or virtual visits by community midwives should be provided to reduce the number of times women and newborns need to leave their home 1.In order to comply with social distancing requirements, community midwives could deliver home or virtual visits ...
This price doesn't include prenatal and postnatal visits. Midwife flat rates can range from $3,000 to $9,000 for prenatal, birth, postpartum, and newborn care services. Those fees usually don't include lab tests and birthing supplies. Flat rates or all-inclusive packages may require private pay outside of insurance.
Basic insurance covers 10-16 regular home visits by an independent midwife over 56 days. Little is known about the practices that go beyond standard care. Several local midwifery networks guarantee a seamless transition for all mothers and newborns from the hospital to the home setting [28, 29].
completion of a postpartum visit with a healthcare provider within 8 weeks of giving birth (Fitzgerald Lewis et al., 2018). The American College of Obstetricians and Gynecologists (ACOG) describes the postpartum visit as follows (ACOG, 2018, Comprehensive postpartum visit and transition to well-woman care section, para. 2):
Aksu 2011 examined the effect of one postnatal visit by a trained supporter versus no postnatal visits; Bashour 2008a; Bashour 2008b compared four or one postnatal home visits from midwives versus no home visits following hospital discharge. Ransjo‐Arvidson 1998 compared four midwife home visits versus one midwife home visit. In these three ...
Midwives are healthcare providers who deal with pregnancy, childbirth, newborn care and postpartum health. Some midwives provide routine reproductive care like pelvic exams, Pap tests, or counseling on birth control. Midwives tend to be more holistic and supportive of natural approaches to pregnancy and birth. People often choose a midwife when ...
Objective: The aim of the present study is to gain a deeper understanding of women's experiences of midwifery care in connection with home visits during the early postnatal period. Research design/setting: A qualitative approach was chosen for data collection, and the data presented are based on six focus group interviews (n: 24). The women were both primiparous and multiparous, aged 22-37 ...
The services in the postnatal period have until recently consisted of a home visit from a public health nurse 7-14 days after birth. The care provided to the woman during pregnancy, birth and the postnatal period has been widely debated in Norway. The maternity care is fragmented and the women interact with several different midwives and other ...
The midwifery package includes all prenatal visits, labor & delivery in your home, postpartum and newborn care in your home (3 home visits in the first week), and a six-week postpartum visit in the office for $5000. All education classes are free for clients. Labs and ultrasounds are not included and can be billed directly to your insurance.
Timely interventions in the postnatal period are important for reducing newborn mortality, and early home visits to provide postnatal care are recommended. There has been limited success in achieving timely visits, and a better understanding of the realities of programmes is needed if improvements are to be made. We explored barriers and facilitators to timely postnatal visits through 20 ...
On the morning of your visit, your midwife will phone or text you a message with the time they expect to arrive at your home. They will try to arrive on time, but traffic and other visits can make this difficult. Please make sure that your phone is charged and nearby so you can answer their calls. Your midwife will check:
The midwives will help you whether you choose to: breastfeed; feed with formula; ... If your baby is at home, the tests may be done at your home by the community midwife team. ... Midwives will agree a plan with you for visits at home or at a children's centre until your baby is around 10 days old. This is to check that you and your baby are ...
Aksu 2010 examined the effect of one postnatal visit by a trained supporter versus no postnatal visits; Bashour 2008a; Bashour 2008b compared four or one postnatal home visits from midwives versus no home visits following hospital discharge. Ransjo‐Arvidson 1998 compared four versus one midwife home visits. In these three studies, carried out ...
In the current study, midwives described an abrupt stop in postpartum home visits during the first wave of the COVID‐19 pandemic; however, the midwives quickly found alternative solutions. The midwives were left to make important decisions, and while fearful of causing infection, they also felt the experience was an opportunity to re ...
When you interview a home birth midwife, once the interview is complete, and you return home, allow yourself quiet, down time to reflect on the experience. Allow yourself to process how the meeting went. ... How many postpartum visits are offered under your care and on what days do these visits occur? Question #36.
The programme includes home visits from a family nurse while you're pregnant, and after your baby's born. These visits help: to have a healthy pregnancy. you and your baby grow and develop together. you to be the best parent you can be. Your health visitor will take over from your family nurse when your baby is two until they go to school.
7 First midwife visit after transfer of care from the place of birth or after a 8 home birth 9 1.1.3 Arrange the first postnatal visit by a midwife to take place between 12 and 10 36 hours after transfer of care from the place of birth or after a home birth. 11 The visit should usually be at the woman's home, depending on her
Friday. 7:30 am to 1:00 pm. Prattville Home Midwifery (and midwife Kim) believes that your care provider should offer evidence-based, compassionate, trauma-informed care that is also anti-racist, weight inclusive, and identity-affirming. We believe in providing you access to truly informed consent (and declination), with respect to your right ...
Currently hosting the Confederations Cup, and home to some of the most beautiful medieval churches, Moscow is a city one. ... Moscow is a city one should visit in their life. From ballet, to Russian architect, to galleries and vodka. Russia is a diverse city. The Russian capital is deemed to be one of the most beautiful in the world. Naturally ...
Price per person. 641,69. View details. About the tour Reviews 10. 8 days / 7 nights. St. Petersburg Moscow. We offer you a unique opportunity to visit Russia's two largest cities, Moscow and St. Petersburg. This fascinating, week-long tour will take you to the historic Russian capitals that have always played the most important part in the ...
During this visit, your Midwife will talk to you about your overall health and ask questions about your current and past pregnancies. Please bring any recent pathology or ultrasound reports with you. Your Midwife will start your "hand-held" pregnancy record, go over routine antenatal tests and screenings, and discuss any potential risk factors.
Postpartum care at home is a post delivery care method that can be provided by public health nurses, trained health workers, or midwifery nurses. A study conducted to compare effect of two midwife visits at home to usual postpartum care on the healthy behaviors of low-risk Iranian mothers.
The White House responded with a statement saying "President Trump looks forward to having President Putin to Washington after the first of the year, and he is open to visiting Moscow upon ...