How sperm meets egg: a journey from production to fertilization
Many wonder what the sperm ´s journey is like from ejaculation to fertilization. The ultimate goal of a sperm is to fertilize the egg cell.
However, the journey of the sperm to get to the egg is not an easy one. To reach the egg cell, the sperm has to go through a long and difficult journey that can take from thirty minutes to several hours .
For this reason, fertilization needs a large number of motile spermatozoa for at least one of them to be able to overcome all barriers. Firstly for the sperm to get to the egg, and then to fertilize the egg.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1. How the sperm meets the egg
- 2. Route from the testicle to the urethra
- 2.1. Changes in the sperm
- 3. The journey through the female reproductive system
- 3.1. What barriers do spermatozoa have to cross?
- 3.2. The sperm´s arrival at the Fallopian tubes.
- 3.3. Final stage of the spermatozoon: acrosome reaction
- 4. FAQs from users
- 4.1. How long does it take from sperm production to ejaculation?
- 4.2. How can ovulation be calculated so that the sperm and egg meet?
- 4.3. How long can a sperm live in the female reproductive tract?
- 4.4. How many sperm make it to the egg?
- 4.5. How long does it take sperm to reach the egg?
- 4.6. After sperm meets egg, how long until implantation?
- 4.7. Where do the sperm cells pass through on their way to the egg?
- 4.8. Where does the sperm need to get to, to be able to fertilize the egg?
- 5. Recommended reading
- 6. References
- 7. Authors and contributors

How the sperm meets the egg
Colloquially,the path to fertilization we understand as a race in which only the best sperm will be able to reach the finish line and win the prize. Effectively, it is something like this: many spermatozoa start the race, but only one will fertilize the egg.
The route of the sperm to the egg can be divided into two major stages:
- Male reproductive system: the journey of sperm in the male body is from the testicles to the outside world.
- Female reproductive system: from the vagina, where semen is deposited, to the Fallopian tubes, where the egg is found.
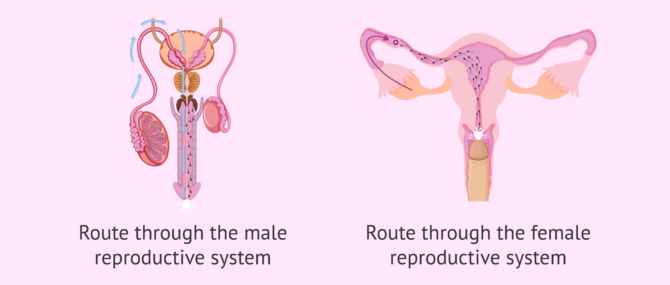
It should not be forgotten that during these two phases of the journey the sperm meet certain obstacles. To follow, we discuss what they are.
Route from the testicle to the urethra
It takes about 90 days for spermatozoa to develop and acquire the necessary maturation before they can be expelled in an ejaculation.The birth of spermatozoa takes place in the seminiferous tubules of the testes. They subsequently pass to the epididymis.
The seminiferous tubules are the internal structures of the testicle where sperm are made. The epididymis is a long structure that connects the testicle and the vas deferens.
At the moment of intercourse, a large quantity of sperm (about 250 million) leave the epididymis and pass through the vas deferens and the urethra. Along the way, the sperm are bathed in fluids released from the seminal vesicles and the prostate. In this way, the semen, the mix of sperm and fluids, is formed.
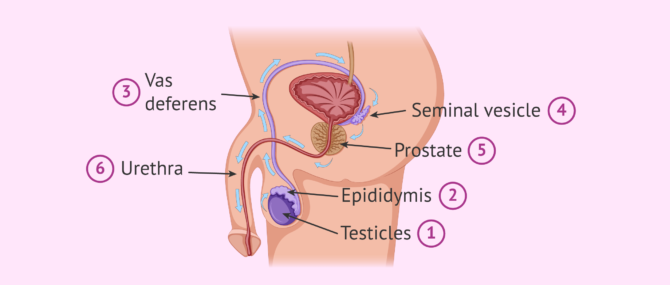
The main function of these seminal fluids is to make is possible for the sperm to enter into the vagina. Sperm will shoot out of the urethra through the penis until they enter the female reproductive tract , specifically the vagina.
Changes in the sperm
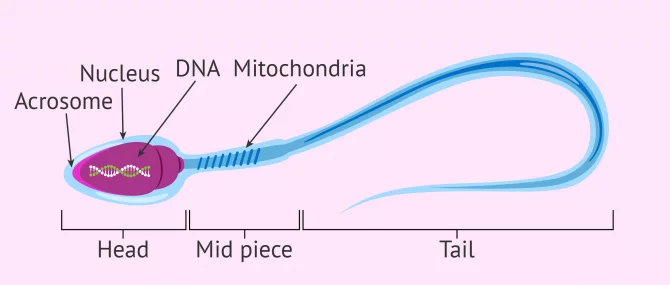
During this journey from the testicle to the outside, the sperm acquire the correct shape and structure to allow fertilization of the egg. The changes that occur at this final stage of sperm maturation are:
- DNA compaction to allow the head (where the DNA is stored) to be as small as possible and therefore move better. This also helps it to pass through the zona pellucida (egg shell).
- The tail acquires the perfect design so the sperm have great speed and resistance.
- The middle piece has a large number of mitochondria for high energy production. This gives the spermatozoon great efficiency in energy usage.
If you wish to continue reading information about what the spermatozoon cell is like, we suggest you visit this article: How are spermatazoa formed
The journey through the female reproductive system
In the process of ejaculation, sperm cells leave the man and enter the vagina. This is where the sperm cells begin the second part of their journey to fertilization.
During this second part of the journey the sperm again encounter an large number of obstacles. These obstacles and barriers can hinder the sperms arrival at the Fallopian tubes, where the egg is waiting.
There is a distance of between 15 and 18 cm and time is of the essence. Sperm cannot afford to delay, since the egg, once it has left the ovary (i.e., after ovulation ), has a half-life of about 24 hours. The survival time of the egg is short compared to that of the sperm. Sperm can live between 2 and 5 days in the female reproductive tract.

After ejaculation, the race of the sperm cells begins. It is a race not only of speed but also of endurance . Defective sperm and/or those with poor motility will fall by the wayside.
What barriers do spermatozoa have to cross?
Some obstacles, or barriers, encountered by sperm are as follows:
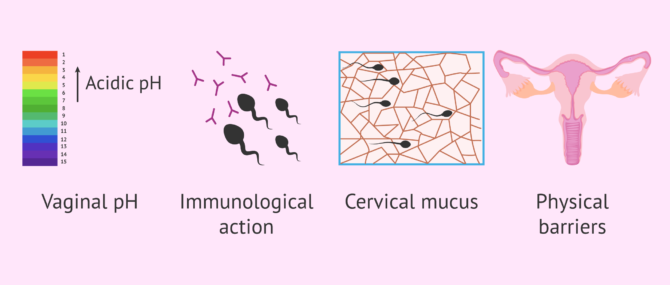
However, it is not all difficulties in the journey of the sperm. The egg tries to pave the way for the sperm by releasing molecules and sending signals. The fallopian tubes and uterus exert a suction force through rhythmic contractions and the cervical mucus becomes less dense allowing the sperm to swim better.
For its part, the seminal fluid that accompanies the sperm neutralizes the pH and provides sugars to the sperm. This fluid also serves as a protective shield against the woman´s white blood cells.
The sperm´s arrival at the Fallopian tubes.
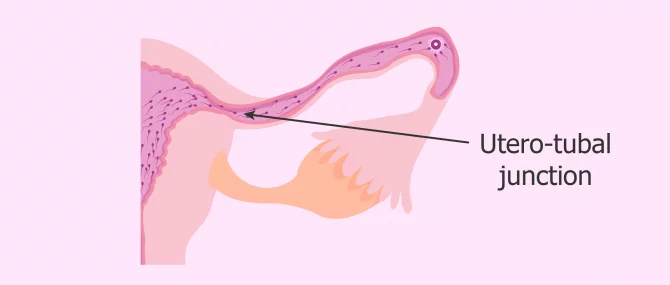
Once the vaginal, cervical and uterine barriers have been overcome, we encounter the narrowest part of the course: the uterotubal junction . Only a few thousand of the average 250 million spermatozoa in freshly ejaculated semen reach this point.
Along the way, the strongest spermatozoa, i.e. those that have been able to overcome the female obstacles, acquire an extraordinary ability: the ability to fertilize . This is known as sperm hyperactivation . From this moment on, its tail moves with much more force and energy, allowing a vigorous movement that helps it arrive at the egg.
Once they reach the fallopian tubes, many sperm remain attached to the tube walls, exhausted and unable to continue their journey.
At this point, few sperm are left in the race, as the vast majority have been lost along the way. Of the few dozen sperm that remain before the egg's watchful eye, only one will make it through the thick doorway to the egg: the zona pellucida.
The chosen sperm, the strongest and most capable one, upon contact with the zona pellucida, initiates the so-called acrosome reaction .
Final stage of the spermatozoon: acrosome reaction
As mentioned above, when the most able sperm has reached the egg, the acrosome reaction takes place. This is the release of the contents of the acrosome, which is composed of a series of enzymes. The purpose of this enzymatic release is to weaken the zona pellucida of the ovum and facilitate penetration.
The acrosome is a structure located in the head of the sperm. It serves as a reservoir for enzymes and other substances that the sperm needs to pass through the zona pellucida.
This reaction "wakes up" the egg, which releases cortical granules , organelles that prevent any other sperm from penetrating. It is as if the ovum plants a flag indicating to the rest of the spermatozoa around it that it has already been conquered by the winning spermatozoa and, therefore, that the doors of its kingdom are closed.
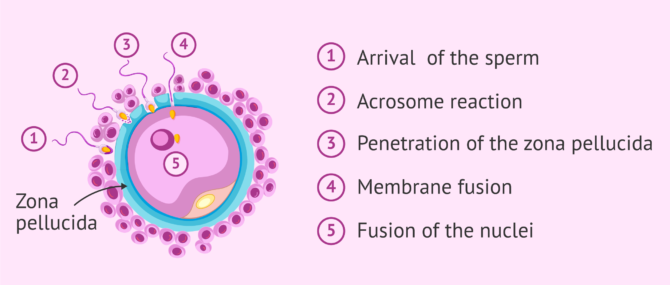
Once the sperm penetrates the oocyte, their two nuclei fuse. This is what we know as fertilization . If you want to know the details about how the sperm enters the egg and how the new being is formed, you can read this article: The steps of fertilization in humans.
We're already 773!
Join our inviTRA community
FAQs from users
How long does it take from sperm production to ejaculation.
Spermatogenesis is the process whereby male reproductive cells are formed, from the immature ones, spermatogonia, until the mature ones, spermatozoa. This complicated process occurs within the seminiferous tubule in the testis and takes about 64-72 days.
Once spermatozoa (sperm cells) have been produced, they leave the testis and travel to the epididymis, where they will acquire the necessary motility in a process that lasts 10 days approximately. Spermatozoa will be stored in the epididymis until they are expelled with ejaculation. When ejaculation starts, sperm travel through the vas deferends and mixes with the seminal fluid that originates in the secretory glands, creating what we all know as semen . Finally, it is expelled through the urethra.
How can ovulation be calculated so that the sperm and egg meet?
It can be calculated by measuring the daily basal temperature and by performing a urine LH test.
How long can a sperm live in the female reproductive tract?
Once ejaculation occurs and the sperm are released into the vagina, they have a half-life of 2 to 5 days. The stronger ones will survive longer. The weaker ones will die on the way. After fertilization, the dead spermatozoa and the live ones that have remained unable to fertilize the egg will be eliminated by phagocytosis (the body's own system of neutralization and elimination of substances).
How many sperm make it to the egg?
To answer this question, we will split the answer into various figures, each one corresponding to a stage in the journey:
- There are approximately 200-250 million sperm in each ejaculation, but only about 2 million make it to the cervix.
- Once there, out of the 2 million sperm entering the cervix, only about 1 million are able to make it to the uterus.
- Out of the 1 million that enter the uterus, only 10,000 are able to travel to the top of this organ.
- Out of the 10,000 that survive at this point, only half of them travel in the right direction, that is, toward the egg cell.
- Out of the approximately 5,000 sperm that enter the utero-tubal junction, about 1,000 get inside the Fallopian tube.
- Finally, out of the 1,000 that enter the tube, it is estimated that only 200 make it to the egg.
However, in the end, only 1 sperm out of the 200 that reach the egg is able to penetrate and fertilize it.
How long does it take sperm to reach the egg?
There is no set time, since the spermatozoa with the best quality, that is, with great ability to overcome obstacles and great strength of movement, will be able to reach the egg in just half an hour. However, there will be others that will need about two days to cross the entire female reproductive tract.
After sperm meets egg, how long until implantation?
Implantation occurs approximately within 3-7 days after fertilization, as the fertilized egg cell has to travel from the point where it was fertilized to the point where it implants. It depends on how high the point where they meet in the Fallopian tube is. For instance, if they meet high in the tube, it will take about 7 days.
Related stories: What Are the First Signs & Symptoms of Embryo Implantation?
Where do the sperm cells pass through on their way to the egg?
As mentioned above, they must first pass through the male reproductive tract and then, after ejaculation, through the female reproductive tract. In the first part of the journey, they leave the testicle and pass through the epididymis, the vas deferens and the urethra. During this part, they are impregnated with secretions from the prostate and seminal vesicle.
In the second part of the course, the spermatozoa pass from the vagina, where they are deposited, to the cervix. Subsequently, they pass through the uterus and reach the fallopian tubes, where the egg is found or where they wait for it to arrive, in case ovulation has not yet occurred.
Where does the sperm need to get to, to be able to fertilize the egg?
The sperm has to reach the fallopian tubes, where the egg is waiting. Once there, it will be able to fuse with it and give rise to the embryo. Subsequently, the embryo will leave the fallopian tubes, reach the uterus and implant in the endometrium of the uterine cavity. This is the beginning of pregnancy.
Recommended reading
The final goal of this whole journey of the sperm is to meet the egg, fuse with it and allow the birth of a new cell. This cell, after about nine months of successive divisions and processes of differentiation and specialization, will give rise to the future baby.
If you want to know more information about what happens after fertilization, we recommend reading this article: Pregnancy stages month by month
If you are interested in knowing more about the hormones responsible for sperm formation, you can visit this link: Male hormone check .
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
Austin CR. Observations on the penetration of the sperm in the mammalian egg. Aust J Sci Res B. 1951;4(4):581–596.
Bennett M. Shapiro. The existential decision of a sperm, Cell 49, no. 3 (May 1987): 293-94, esp. 293.
Chang MC. Fertilizing capacity of spermatozoa deposited into the fallopian tubes. Nature. 1951;168(4277):697–698 ( View )
Choza J. (1991): Antropología de la Sexualidad. Ed. Rialp. Madrid, 1.ª Edición ( View )
J Clin Invest. (2010). Fertilization: a sperm’s journey to and interaction with the oocyte. Research Institute for Microbial Diseases, Osaka University, Osaka, Japan. School of Biological and Biomedical Sciences, Durham University, United Kingdom. 120(4) 984–994 ( View )
Lennart Nilsson, A portrait of the sperm. In: The functional anatomy of the spermatozoan, ed. Bjorn A. Afzelius (New York: Pergamon, 1975), 79-82.
Martin E. The egg and the sperm: how science has constructed a romance-based on stereotypical male-female roles. “Signs”. Vol. 16. No. 3 (Spring, 1991), pp. 485-501. Published by: The University of Chicago Press ( View )
Stein KK, Primakoff P, Myles D. Sperm-egg fusion: events at the plasma membrane. J Cell Sci. 2004; 117(Pt 26):6269–6274 ( View )
Paul M. Wassarman, The biology and chemistry of fertilization, Science 235, No. 4788 (January 30, 1987): 553-60, esp. 554 ( View )
Paul M. Wassarman, Fertilization in mammals, Scientific American 259, no. 6 (December 1988): 78-84, esp. 78, 84
FAQs from users: 'How long does it take from sperm production to ejaculation?' , 'How can ovulation be calculated so that the sperm and egg meet?' , 'How long can a sperm live in the female reproductive tract?' , 'How many sperm make it to the egg?' , 'How long does it take sperm to reach the egg?' , 'After sperm meets egg, how long until implantation?' , 'How does it feel when sperm meets the egg?' , 'How long after IUI does sperm meet egg?' , 'Can sperm meet egg before ovulation?' , 'Where do the sperm cells pass through on their way to the egg?' , 'Where does the sperm go when you have a vasectomy?' , 'Where does the sperm need to get to, to be able to fertilize the egg?' , 'When pregnant, where does sperm go?' , 'When does sperm die outside the body?' , 'When does sperm leave the female body?' and 'How many sperm fertilize an egg for identical twins?' .
Authors and contributors

Find the latest news on assisted reproduction in our channels.
And when do men expel the so-called pre-ejaculatory fluid? I want to know it because then my boyfriend and I will be able to use the pull-out method more accurately. Thnxs!
Hello Katie1,
Firstly, the pull-out method, coitus interruptus , or withdrawal method is not a safe birth control method because it does not prevent you from the transmission of STDs (sexually transmitted diseases) and HIV infection (AIDs). Besides, it is actually an extremely unreliable method.
Apart from that, there are several theories about why pre-ejaculatory fluid exists, none of them proved. While some say the only function of this fluid is providing some lubrication for intercourse, others believe they protect the sperm by acting as a sort of pre-clearing of the urethra, making the environment more conductive for sperm to survive the journey and lowering the acidity. On the other hand, the function of sperm is reproduction.
I hope I have clarified your concerns,
My husband has had a vasectomy and we want to try for a baby. Is there any way we can do this without surgery?
It is possible for a man to become a father after again after a vasectomy. However, this is not possible without some kind of surgical treatment. There are different options available and you can find lots more information in our article: Pregnancy after vasectomy
I hope this helps and good luck.
Interesting article, thanks. It is very interesting that so many sperm are needed to fertilize just one egg and reading this makes me realize why!
Leave a Reply
Privacy Overview
Appointments at Mayo Clinic
- Getting pregnant
How long do sperm live after ejaculation?
The life span of sperm after ejaculation depends on the circumstances.
Ejaculated sperm remain viable for several days within the female reproductive tract. Fertilization is possible as long as the sperm remain alive — up to five days.
Sperm can also be preserved for decades when semen is frozen.
Patricio C. Gargollo, M.D.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Secondary infertility
- Frequently asked questions: Contraception FAQ024: Fertility awareness-based methods of family planning. American College of Obstetricians and Gynecologists. https://www.acog.org/Patients/FAQs/Fertility-Awareness-Based-Methods-of-Family-Planning. Accessed Jan. 24, 2020.
- Hatcher RA, et al., eds. Fertility awareness-based methods. In: Contraceptive Technology. 21st ed. Ayer Company Publishers; 2018.
- Rozati H, et al. Process and pitfalls of sperm cryopreservation. Journal of Clinical Medicine. 2017; doi:10.3390/jcm6090089.
Products and Services
- A Book: Obstetricks
- Birth control pill FAQ
- Elective abortion and subsequent pregnancies
- Female fertility tips
- Fertility preservation
- Healthy sperm: Improving your fertility
- How to get pregnant
- Is a home sperm test useful?
- Ovulation signs
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Expert Answers
- Sperm - How long do they live after ejaculation
Make twice the impact
Your gift can go twice as far to advance cancer research and care!

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Sperm release pathway
Sperm are produced and released by the male reproductive organs.
The testes are where sperm are produced. The testes are linked to the rest of the male reproductive organs by the vas deferens, which extends over the base of the pelvic bone or ilium, and wraps around to the ampulla, seminal vesicle, and prostate. The urethra then runs from the bladder through the penis.
Sperm production in the testes takes place in coiled structures called seminiferous tubules.
Along the top of each testicle is the epididymis. This is a cordlike structure where the sperm mature and are stored.
The release process starts when the penis fills with blood and becomes erect. Continuing to stimulate the penis will cause an ejaculation.
Mature sperm begin their journey by travelling from the epididymis to the vas deferens, which propels sperm forward with smooth muscle contractions.
The sperm arrive first at the ampulla just above the prostate gland. Here, secretions from the seminal vesicle located next to the ampulla are added.
Next, the seminal fluid is propelled forward through the ejaculatory ducts toward the urethra. As it passes the prostate gland, a milky fluid is added to make semen.
Finally, the semen is ejaculated from the penis through the urethra.
Review Date 10/15/2023
Updated by: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Male Infertility
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 14 December 2020
Sperm biology and male reproductive health
- Ricardo P. Bertolla ORCID: orcid.org/0000-0001-6892-9244 1
Scientific Reports volume 10 , Article number: 21879 ( 2020 ) Cite this article
11k Accesses
7 Citations
4 Altmetric
Metrics details
- Cell biology
Sperm are unique cells, produced through the complex and precisely orchestrated process of spermatogenesis, in which there are a number of checkpoints in place to guarantee delivery of a high-quality and high-fidelity DNA product. On the other hand, reproductive pressure in males means that to produce more is, in very general terms, to perform better. Balancing quantity and quality in sperm production is thus a delicate process, subject to specific cellular and molecular control mechanisms, and sensitive to environmental conditions, that can impact fertility and offspring health. This Collection is focused on these aspects of sperm biology, as well as their impact on reproductive performance and male infertility.
Anisogamy, defined as gamete size dimorphism alongside binary fusion, is the most observed gametic system in multicellular organisms 1 . Early mathematical anisogamy models demonstrated that the most efficient rate of gamete fusion would be achieved if small and large gametes were produced, due to increased collision events (reviewed by Lehtonen and Parker 2 ). Under this understanding, males may be generically defined as those counterparts that produce smaller gametes (i.e., sperm), while females conversely produce the larger ones (ova) 3 . Both gametes, thus, have accumulated very specialized traits in terms of cellular morphological specialization (and polarity, in sperm), molecular machinery, and responsiveness to external stimuli.
Sperm are unique in that they carry out their functions outside their organism of origin. In humans, for example, fertilization occurs within the uterine tubes, in the female reproductive tract 4 . In some species of fish, fertilization occurs under different osmotic pressures 5 . During their development, sperm therefore need to be prepared, as best as possible, for all the possible hindrances and events that will occur between the moment they are released and the moment they effectively penetrate the oocyte. One could putatively divide the life of each sperm into four general moments: (i) spermatogenesis—the process by which diploid spermatogonia undergo meiosis and morphological alterations to produce sperm; (ii) post testicular maturation and storage—the moment after spermatogenesis but before ejaculation, in which sperm interact with extracellular proteins, lipids and microRNAs, among other molecules; (iii) capacitation—the moment after ejaculation in which sperm effectively acquire the capacity to fertilize and oocyte; and (iv) fertilization—the process by which the spermatozoon penetrates the oocyte’s outer protective layers and transfers its genomic material to the oolemma, the initial step in the formation of a zygote (fully reviewed in 6 ).
Spermatogenesis is directly connected to testicular physiology. This is initially determined by testis formation during fetal development. In humans, use of endocrine disruptors by pregnant women, for example, has been shown to be associated with future infertility in their male offspring 7 . Holland et al. demonstrated that there is no effect of a maternal androgenic environment (due to polycystic ovarian syndrome) on the male reproductive axis 8 , while Lessard et al. demonstrated that prenatal exposure to persistent organic pollutants reduced semen quality in male offspring 9 . After the onset of puberty, with the development of secondary sexual traits, spermatogenesis initiates, during which there are a number of conditions that may affect the quality of ejaculates—varicocele, for example, is detected in up to 80% of men with secondary infertility 10 , while testicular heat stress, in bovines, is a cause for lower fertility rates in sires 11 .
In a recent analysis of a large retrospective cohort, Siqueira et al. observed that, over the previous 23 years, semen quality has been steadily decreasing in men attending a reference infertility center in Brazil 12 . This fairly large cohort (a little over 9000 men) agrees, as the authors discussed, with other studies that have observed a downward trend in semen quality over the past decades. There is still much debate as to the reasons for this trend, ranging from artifactual alteration due to subjectivity in some of the analyses, to increased awareness leading to more men with potential fertility problems seeking evaluation, to a true decrease in male reproductive health. Whichever the case, the authors demonstrated that the decrease in semen quality is observed even when only an objective measure, such as total motile sperm count, is utilized.
This has led to the obvious association between environmental conditions and testicular alterations. Greeson et al. examined environmental exposure to PBB153, a polybrominated biphenyl compound used as a flame retardant that accidentally entered the food chain in 1973, and led to alterations in liver and thyroid functions, as well as to increased odds of lymphomas and cancers of the digestive tract. The authors demonstrated that higher serum PBB153 levels were associated with decreased methylation of imprint control regions, which in turn demonstrated that this contaminant determines alterations to the germ line which are then potentially transferred to the offspring of these men 13 . Other environmental effects, such as diets, are more difficult to measure. While some studies have observed effects of obesity on male fertility, others have not. Gómez-Elías et al. studied the effect of high fat diets in mice on high reproductive performance and did not observe a detrimental effect 14 . Elenkov et al., on the other hand, did observe that men who were treated by ICSI had a higher risk for being under treatment for hypertension or metabolic syndrome 15 . Interestingly, a mechanistic cause for hypertension, as it leads to testicular alteration, was later demonstrated by Colli et al. 16 .
The next point of interest, after understanding how the environment affects the testes, would be to understand how sperm interact with their environment. Epididymal proteins and RNAs actively interact with sperm via extracellular vesicles in order to modulate sperm activity 17 . Increased epididymal expression of interleukin 6, for example, has been shown to lead to male infertility in a mouse model 18 . Extracellular vesicle communication remains important after ejaculation. Studies have shown that, in humans, prostatic fluid releases prostasomes that modulate acrosome reaction 17 . Murdica et al. demonstrated that endometrial cells also produce extracellular vesicles that are uptaken by sperm 19 . This is an important demonstration that sperm remain responsive to environmental conditions well after ejaculation, and that this is likely a means by which they acquire the capacity to adapt to the female reproductive tract. If this also holds true for species that present external fertilization remains to be demonstrated.
While this Collection is dedicated to observing this and many other questions, I believe the articles generally fall within the four putative steps presented at the initial portion of this text, with the caveat that biotechnologies may affect one or more of these steps at any given time. Given the broad spectrum that sperm biology covers, both in terms of species and in terms of the many events that are associated, this Collection has sought to bring together as much as possible, while stringing these together under three general areas of research: (i) testis, sperm, and their environment; (ii) biotechnologies and assisted reproduction; and (iii) clinical, experimental, and epidemiologic studies on male infertility.
In sexual reproduction, life begins with the fusion of two gametes. This is the best answer one can produce to the age-old question of where we come from. To understand the life and times of sperm is to understand the foundations of our biological origins, and is a gateway towards understanding early development.
Lessells, C. M., Snook, R. R. & Hosken, D. J. 2—the evolutionary origin and maintenance of sperm: selection for a small, motile gamete mating type. In Sperm Biology (eds Birkhead, T. R. et al. ) 43–67 (Academic Press, Cambridge, 2009).
Chapter Google Scholar
Lehtonen, J. & Parker, G. A. Gamete competition, gamete limitation, and the evolution of the two sexes. Mol. Hum. Reprod. 20 , 1161–1168 (2014).
Article Google Scholar
Togashi, T. & Cox, P. A. The Evolution of Anisogamy: A Fundamental Phenomenon Underlying Sexual Selection (Cambridge University Press, Cambridge, 2011).
Book Google Scholar
Ikawa, M., Inoue, N., Benham, A. M. & Okabe, M. Fertilization: a sperm’s journey to and interaction with the oocyte. J. Clin. Investig. 120 , 984–994 (2010).
Article CAS Google Scholar
Dzyuba, V. & Cosson, J. Motility of fish spermatozoa: from external signaling to flagella response. Reprod. Biol. 14 , 165–175 (2014).
Toshimori, K. & Eddy, E. M. Chapter 3—the Spermatozoon. In Knobil and Neill’s Physiology of Reproduction 4th edn (eds Plant, T. M. & Zeleznik, A. J.) 99–148 (Academic Press, Cambridge, 2015).
Sharma, A. et al. Endocrine-disrupting chemicals and male reproductive health. Reprod. Med. Biol. 19 , 243–253 (2020).
Holland, S., Prescott, M., Pankhurst, M. & Campbell, R. E. The influence of maternal androgen excess on the male reproductive axis. Sci. Rep. 9 , 18908 (2019).
Article ADS CAS Google Scholar
Lessard, M. et al. Prenatal exposure to environmentally-relevant contaminants perturbs male reproductive parameters across multiple generations that are partially protected by folic acid supplementation. Sci. Rep. 9 , 13829 (2019).
Article ADS Google Scholar
Gorelick, J. I. & Goldstein, M. Loss of fertility in men with varicocele. Fertil. Steril. 59 , 613–616 (1993).
Morrell, J. M. Heat stress and bull fertility. Theriogenology 153 , 62–67 (2020).
Siqueira, S. et al. Changes in seminal parameters among Brazilian men between 1995 and 2018. Sci. Rep. 10 , 6430 (2020).
Greeson, K. W. et al. Detrimental effects of flame retardant, PBB153, exposure on sperm and future generations. Sci. Rep. 10 , 8567 (2020).
Gómez-Elías, M. D. et al. Association between high-fat diet feeding and male fertility in high reproductive performance mice. Sci. Rep. 9 , 18546 (2019).
Elenkov, A., Al-Jebari, Y. & Giwercman, A. More prevalent prescription of medicine for hypertension and metabolic syndrome in males from couples undergoing intracytoplasmic sperm injection. Sci. Rep. 8 , 14521 (2018).
Colli, L. G. et al. Systemic arterial hypertension leads to decreased semen quality and alterations in the testicular microcirculation in rats. Sci. Rep. 9 , 11047 (2019).
Simon, C. et al. Extracellular vesicles in human reproduction in health and disease. Endocr. Rev. 39 , 292–332 (2018).
Gao, S., Zhang, Y., Yang, C., Perez, G. I. & Xiao, H. NCOA5 haplo-insufficiency results in male mouse infertility through increased IL-6 expression in the epididymis. Sci. Rep. 9 , 15525 (2019).
Murdica, V. et al. In vitro cultured human endometrial cells release extracellular vesicles that can be uptaken by spermatozoa. Sci. Rep. 10 , 8856 (2020).
Download references
Author information
Authors and affiliations.
Division of Urology, Department of Surgery, Universidade Federal de São Paulo, Rua Napoleão de Barros, 715, 2º andar, São Paulo, SP, 04024-002, Brazil
Ricardo P. Bertolla
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ricardo P. Bertolla .
Ethics declarations
Competing interests.
The author declares no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Bertolla, R.P. Sperm biology and male reproductive health. Sci Rep 10 , 21879 (2020). https://doi.org/10.1038/s41598-020-78861-7
Download citation
Published : 14 December 2020
DOI : https://doi.org/10.1038/s41598-020-78861-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Microfluidics as an emerging paradigm for assisted reproductive technology: a sperm separation perspective.
- Mohammadjavad Bouloorchi Tabalvandani
- Zahra Saeidpour
- Majid Badieirostami
Biomedical Microdevices (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

28.1 Fertilization
Learning objectives.
By the end of this section, you will be able to:
- Describe the obstacles that sperm must overcome to reach an oocyte
- Explain capacitation and its importance in fertilization
- Summarize the events that occur as a sperm fertilizes an oocyte
Fertilization occurs when a sperm and an oocyte (egg) combine and their nuclei fuse. Because each of these reproductive cells is a haploid cell containing half of the genetic material needed to form a human being, their combination forms a diploid cell. This new single cell, called a zygote , contains all of the genetic material needed to form a human—half from the mother and half from the father.
Transit of Sperm
Fertilization is a numbers game. During ejaculation, hundreds of millions of sperm (spermatozoa) are released into the vagina. Almost immediately, millions of these sperm are overcome by the acidity of the vagina (approximately pH 3.8), and millions more may be blocked from entering the uterus by thick cervical mucus. Of those that do enter, thousands are destroyed by phagocytic uterine leukocytes. Thus, the race into the uterine tubes, which is the most typical site for sperm to encounter the oocyte, is reduced to a few thousand contenders. Their journey—thought to be facilitated by uterine contractions—usually takes from 30 minutes to 2 hours. If the sperm do not encounter an oocyte immediately, they can survive in the uterine tubes for another 3–5 days. Thus, fertilization can still occur if intercourse takes place a few days before ovulation. In comparison, an oocyte can survive independently for only approximately 24 hours following ovulation. Intercourse more than a day after ovulation will therefore usually not result in fertilization.
During the journey, fluids in the female reproductive tract prepare the sperm for fertilization through a process called capacitation , or priming. The fluids improve the motility of the spermatozoa. They also deplete cholesterol molecules embedded in the membrane of the head of the sperm, thinning the membrane in such a way that will help facilitate the release of the lysosomal (digestive) enzymes needed for the sperm to penetrate the oocyte’s exterior once contact is made. Sperm must undergo the process of capacitation in order to have the “capacity” to fertilize an oocyte. If they reach the oocyte before capacitation is complete, they will be unable to penetrate the oocyte’s thick outer layer of cells.
Contact Between Sperm and Oocyte
Upon ovulation, the oocyte released by the ovary is swept into—and along—the uterine tube. Fertilization must occur in the distal uterine tube because an unfertilized oocyte cannot survive the 72-hour journey to the uterus. As you will recall from your study of the oogenesis, this oocyte (specifically a secondary oocyte) is surrounded by two protective layers. The corona radiata is an outer layer of follicular (granulosa) cells that form around a developing oocyte in the ovary and remain with it upon ovulation. The underlying zona pellucida (pellucid = “transparent”) is a transparent, but thick, glycoprotein membrane that surrounds the cell’s plasma membrane.
As it is swept along the distal uterine tube, the oocyte encounters the surviving capacitated sperm, which stream toward it in response to chemical attractants released by the cells of the corona radiata. To reach the oocyte itself, the sperm must penetrate the two protective layers. The sperm first burrow through the cells of the corona radiata. Then, upon contact with the zona pellucida, the sperm bind to receptors in the zona pellucida. This initiates a process called the acrosomal reaction in which the enzyme-filled “cap” of the sperm, called the acrosome , releases its stored digestive enzymes. These enzymes clear a path through the zona pellucida that allows sperm to reach the oocyte. Finally, a single sperm makes contact with sperm-binding receptors on the oocyte’s plasma membrane ( Figure 28.1.1 ). The plasma membrane of that sperm then fuses with the oocyte’s plasma membrane, and the head and mid-piece of the “winning” sperm enter the oocyte interior.
How do sperm penetrate the corona radiata? Some sperm undergo a spontaneous acrosomal reaction, which is an acrosomal reaction not triggered by contact with the zona pellucida. The digestive enzymes released by this reaction digest the extracellular matrix of the corona radiata. As you can see, the first sperm to reach the oocyte is never the one to fertilize it. Rather, hundreds of sperm cells must undergo the acrosomal reaction, each helping to degrade the corona radiata and zona pellucida until a path is created to allow one sperm to contact and fuse with the plasma membrane of the oocyte. If you consider the loss of millions of sperm between entry into the vagina and degradation of the zona pellucida, you can understand why a low sperm count can cause male infertility.
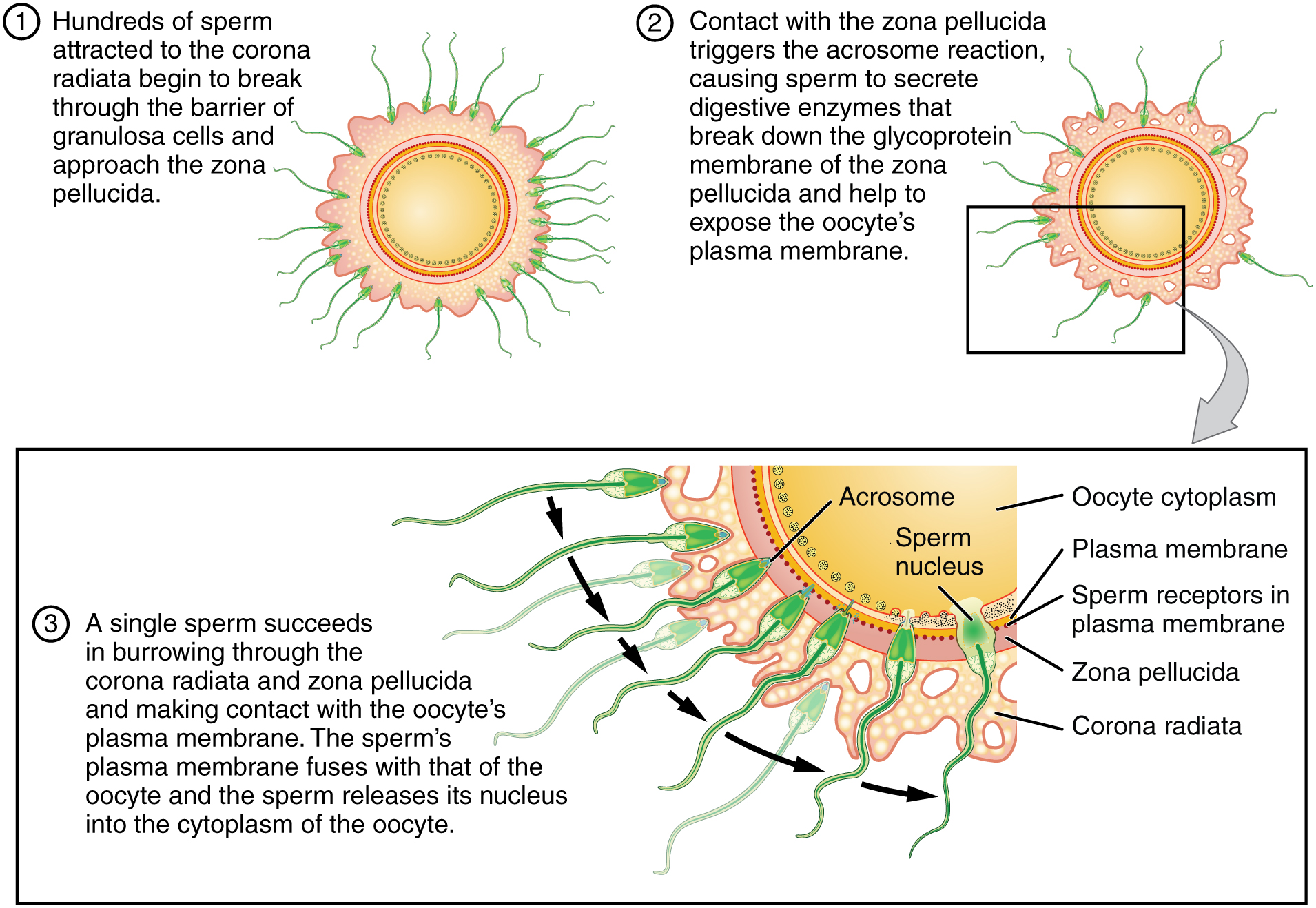
When the first sperm fuses with the oocyte, the oocyte deploys two mechanisms to prevent polyspermy , which is penetration by more than one sperm. This is critical because if more than one sperm were to fertilize the oocyte, the resulting zygote would be a triploid organism with three sets of chromosomes. This is incompatible with life.
The first mechanism is the fast block, which involves a near instantaneous change in sodium ion permeability upon binding of the first sperm, depolarizing the oocyte plasma membrane and preventing the fusion of additional sperm cells. The fast block sets in almost immediately and lasts for about a minute, during which time an influx of calcium ions following sperm penetration triggers the second mechanism, the slow block. In this process, referred to as the cortical reaction , cortical granules sitting immediately below the oocyte plasma membrane fuse with the membrane and release zonal inhibiting proteins and mucopolysaccharides into the space between the plasma membrane and the zona pellucida. Zonal inhibiting proteins cause the release of any other attached sperm and destroy the oocyte’s sperm receptors, thus preventing any more sperm from binding. The mucopolysaccharides then coat the nascent zygote in an impenetrable barrier that, together with hardened zona pellucida, is called a fertilization membrane .
Recall that at the point of fertilization, the oocyte has not yet completed meiosis; all secondary oocytes remain arrested in metaphase of meiosis II until fertilization. Only upon fertilization does the oocyte complete meiosis. The unneeded complement of genetic material that results is stored in a second polar body that is eventually ejected. At this moment, the oocyte has become an ovum, the female haploid gamete. The two haploid nuclei derived from the sperm and oocyte and contained within the egg are referred to as pronuclei. They decondense, expand, and replicate their DNA in preparation for mitosis. The pronuclei then migrate toward each other, their nuclear envelopes disintegrate, and the male- and female-derived genetic material intermingles. This step completes the process of fertilization and results in a single-celled diploid zygote with all the genetic instructions it needs to develop into a human.
Most of the time, a woman releases a single egg during an ovulation cycle. However, in approximately 1 percent of ovulation cycles, two eggs are released and both are fertilized. Two zygotes form, implant, and develop, resulting in the birth of dizygotic (or fraternal) twins. Because dizygotic twins develop from two eggs fertilized by two sperm, they are no more identical than siblings born at different times.
Much less commonly, a zygote can divide into two separate offspring during early development. This results in the birth of monozygotic (or identical) twins. Although the zygote can split as early as the two-cell stage, splitting occurs most commonly during the early blastocyst stage, with roughly 70–100 cells present. These two scenarios are distinct from each other, in that the twin embryos that separated at the two-cell stage will have individual placentas, whereas twin embryos that form from separation at the blastocyst stage will share a placenta and a chorionic cavity.
Everyday Connections
In Vitro Fertilization IVF, which stands for in vitro fertilization, is an assisted reproductive technology. In vitro, which in Latin translates to “in glass,” refers to a procedure that takes place outside of the body. There are many different indications for IVF. For example, a woman may produce normal eggs, but the eggs cannot reach the uterus because the uterine tubes are blocked or otherwise compromised. A man may have a low sperm count, low sperm motility, sperm with an unusually high percentage of morphological abnormalities, or sperm that are incapable of penetrating the zona pellucida of an egg.
A typical IVF procedure begins with egg collection. A normal ovulation cycle produces only one oocyte, but the number can be boosted significantly (to 10–20 oocytes) by administering a short course of gonadotropins. The course begins with follicle-stimulating hormone (FSH) analogs, which support the development of multiple follicles, and ends with a luteinizing hormone (LH) analog that triggers ovulation. Right before the ova would be released from the ovary, they are harvested using ultrasound-guided oocyte retrieval. In this procedure, ultrasound allows a physician to visualize mature follicles. The ova are aspirated (sucked out) using a syringe.
In parallel, sperm are obtained from the male partner or from a sperm bank. The sperm are prepared by washing to remove seminal fluid because seminal fluid contains a peptide, FPP (or, fertilization promoting peptide), that—in high concentrations—prevents capacitation of the sperm. The sperm sample is also concentrated, to increase the sperm count per milliliter.
Next, the eggs and sperm are mixed in a petri dish. The ideal ratio is 75,000 sperm to one egg. If there are severe problems with the sperm—for example, the count is exceedingly low, or the sperm are completely nonmotile, or incapable of binding to or penetrating the zona pellucida—a sperm can be injected into an egg. This is called intracytoplasmic sperm injection (ICSI).
The embryos are then incubated until they either reach the eight-cell stage or the blastocyst stage. In the United States, fertilized eggs are typically cultured to the blastocyst stage because this results in a higher pregnancy rate. Finally, the embryos are transferred to a woman’s uterus using a plastic catheter (tube). Figure 28.1.2 illustrates the steps involved in IVF.
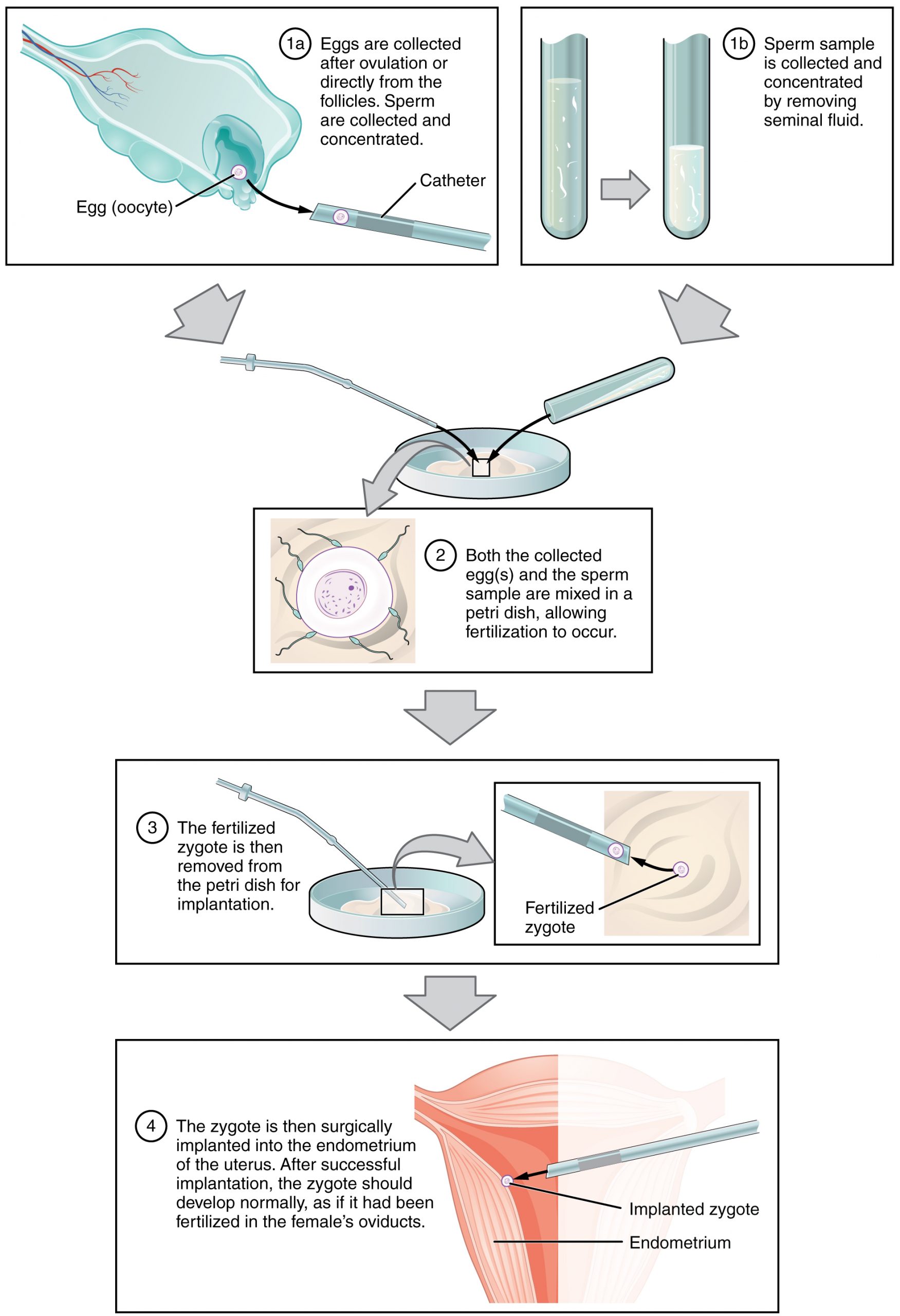
IVF is a relatively new and still evolving technology, and until recently it was necessary to transfer multiple embryos to achieve a good chance of a pregnancy. Today, however, transferred embryos are much more likely to implant successfully, so countries that regulate the IVF industry cap the number of embryos that can be transferred per cycle at two. This reduces the risk of multiple-birth pregnancies.
The rate of success for IVF is correlated with a woman’s age. More than 40 percent of women under 35 succeed in giving birth following IVF, but the rate drops to a little over 10 percent in women over 40.
External Website

Go to this site to view resources covering various aspects of fertilization, including movies and animations showing sperm structure and motility, ovulation, and fertilization.
Chapter Review
Hundreds of millions of sperm deposited in the vagina travel toward the oocyte, but only a few hundred actually reach it. The number of sperm that reach the oocyte is greatly reduced because of conditions within the female reproductive tract. Many sperm are overcome by the acidity of the vagina, others are blocked by mucus in the cervix, whereas others are attacked by phagocytic leukocytes in the uterus. Those sperm that do survive undergo a change in response to those conditions. They go through the process of capacitation, which improves their motility and alters the membrane surrounding the acrosome, the cap-like structure in the head of a sperm that contains the digestive enzymes needed for it to attach to and penetrate the oocyte.
The oocyte that is released by ovulation is protected by a thick outer layer of granulosa cells known as the corona radiata and by the zona pellucida, a thick glycoprotein membrane that lies just outside the oocyte’s plasma membrane. When capacitated sperm make contact with the oocyte, they release the digestive enzymes in the acrosome (the acrosomal reaction) and are thus able to attach to the oocyte and burrow through to the oocyte’s zona pellucida. One of the sperm will then break through to the oocyte’s plasma membrane and release its haploid nucleus into the oocyte. The oocyte’s membrane structure changes in response (cortical reaction), preventing any further penetration by another sperm and forming a fertilization membrane. Fertilization is complete upon unification of the haploid nuclei of the two gametes, producing a diploid zygote.
Review Questions
Critical thinking questions.
1. Darcy and Raul are having difficulty conceiving a child. Darcy ovulates every 28 days, and Raul’s sperm count is normal. If we could observe Raul’s sperm about an hour after ejaculation, however, we’d see that they appear to be moving only sluggishly. When Raul’s sperm eventually encounter Darcy’s oocyte, they appear to be incapable of generating an adequate acrosomal reaction. Which process has probably gone wrong?
2. Sherrise is a sexually active college student. On Saturday night, she has unprotected sex with her boyfriend. On Tuesday morning, she experiences the twinge of mid-cycle pain that she typically feels when she is ovulating. This makes Sherrise extremely anxious that she might soon learn she is pregnant. Is Sherrise’s concern valid? Why or why not?
Answers for Critical Thinking Questions
- The process of capacitation appears to be incomplete. Capacitation increases sperm motility and makes the sperm membrane more fragile. This enables it to release its digestive enzymes during the acrosomal reaction. When capacitation is inadequate, sperm cannot reach the oocyte membrane.
- Sherrise’s concern is valid. Sperm may be viable for up to 4 days; therefore, it is entirely possible that capacitated sperm are still residing in her uterine tubes and could fertilize the oocyte she has just ovulated.
This work, Anatomy & Physiology, is adapted from Anatomy & Physiology by OpenStax , licensed under CC BY . This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images, from Anatomy & Physiology by OpenStax , are licensed under CC BY except where otherwise noted.
Access the original for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction .
Anatomy & Physiology Copyright © 2019 by Lindsay M. Biga, Staci Bronson, Sierra Dawson, Amy Harwell, Robin Hopkins, Joel Kaufmann, Mike LeMaster, Philip Matern, Katie Morrison-Graham, Kristen Oja, Devon Quick, Jon Runyeon, OSU OERU, and OpenStax is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License , except where otherwise noted.
All about sperm
Sperm Travel Path: Understanding the Route to Fertilization
Short answer sperm travel path: Sperm travel from the testes through the epididymis, vas deferens, and ejaculatory duct before being released through the urethra during ejaculation. The journey takes approximately 64-72 days to complete.
Exploring the Fascinating Journey: Sperm Travel Path
Understanding how sperm travel path affects conception: step by step guide, all you need to know about sperm travel path: frequently asked questions, the intriguing process of fertilization: an in-depth look at sperm travel path, breaking down the miracle of life: inside the male reproductive tract and its role in sperm travel path, discovering the unseen world of conception: the hidden secrets of sperm travel path.
Table of Contents
When it comes to the miracle of human life, there are plenty of fascinating facts and intricate details that often go unnoticed. One aspect of this journey that is particularly intriguing is the path that sperm travel during fertilization. Despite their tiny size, these cells embark on a complex and challenging journey in order to reach the egg.
To begin with, it’s important to understand the basic anatomy of sperm. Each one features a head, midpiece, and tail. The head contains genetic material (DNA) while the midpiece holds mitochondria needed for energy production. Finally, the tail – which resembles a whip-like structure – propels sperm towards its ultimate destination.
The first step in this journey begins when sperm cells are released from the testes. They enter into a part of the male reproductive system known as the epididymis where they mature over several weeks before being released during ejaculation. From here, they must travel through various ducts, including the vas deferens and urethra before exiting through the penis.
Once outside of the male body, sperm face further challenges as they navigate through cervix into uterine cavity via vaginal canal during intercourse or other artificial methods like IVF. Here, they must contend with acidic pH levels in female reproductive tract as well as immune cells that may see them as foreign invaders attempting to harm host (woman carrying embryo).
As if all this wasn’t difficult enough, sperm still have a long way yet to travel! They must then make their way through fallopian tube where fertilization occurs based on their fortunate meeting with an egg cell.
Sperm can remain viable for up to five days within female reproductive tract which provides extra opportunities for fertilization attempting at ovulation time – roughly midpoint menstrual cycle when ovary releases an egg cell into its respective Fallopian tube readying itself for fertilization.
Overall, exploring the fascinating journey undertaken by sperm cells provides us with insight into the incredible complexity involved in human reproduction. From their early maturation in the epididymis to their ultimate goal of reaching and fertilizing an egg, these tiny cells face a veritable obstacle course and yet still manage to achieve what amounts to nothing short of a miracle – when successful fertilization occurs! So let us honor this journey that we often overlooks as we get caught up with complexities of our lives!
When it comes to conception, understanding the process of sperm travel is essential. After all, it takes a single sperm to fertilize an egg and result in pregnancy. So, how does this little swimmer make its way up towards the egg? In this step-by-step guide, we’ll explore the complex journey that sperm must undertake in order to reach their ultimate destination.
The first step in understanding how sperm travel path affects conception is knowing where they come from. Sperm are produced in the testes of males and mature over approximately 72 days. Whenever a man ejaculates, he releases millions of these little swimmers which then navigate through several obstacles before they can reach their final goal.
The next critical step is for them to make their way into the cervix – the opening that separates a woman’s uterus from her vagina. This passage can prove challenging for many sperm as its narrow opening and acidic environment can be quite hostile. Only a relatively small proportion of these hardy cells will remain viable enough to make it through this initial challenge.
Once through the cervix, those swimmer’s that do survive are launched into even rougher waters, weaving their way upstream through thick mucus membranes located inside the female reproductive tract; One by one-many falling by wayside losing momentum along with movement- until only very few finally come close enough to take on and fertilize the coveted ovum or egg.
Fertilization happens when one lucky little guy makes it past all these hurdles and meets a waiting egg emerging around day 14 after ovulation within your fallopian tubes-enabling mothers await with pregnancy tests eagerly due for conception notice.
Overall factors such as age, lifestyle choices such as diet or smoking habits can play vital roles in altering what size or quality of sperms actually end up reaching these prized eggs much later on hence affecting fertility rates drastically causing recurring patterns of infertility rejections for some couples trying to conceive.
In conclusion, the journey of sperm travel is a complex, multi-step process that’s far from easy. However, understanding how it all works can help you boost your chances of conception. With proper planning regarding sexual timing and fertility wellness strategies like stress management or nutritional interventions advised by professionals, it is possible for many couples to overcome these hurdles and bring their family dream into fruition despite any challenges in the path~!
When it comes to reproduction, people often focus on the act of sex itself without giving much thought to what happens after ejaculation. However, understanding the journey that sperm cells take from release into the vagina to reaching their destination can be essential in ensuring successful conception. In this article, we’ll address some frequently asked questions about sperm travel path and give you all you need to know about reproductive biology.
Q: What is sperm? A: Sperm are tiny male reproductive cells that are produced by the testes and contain genetic material needed for fertilization. During sex, they swim through seminiferous tubules and gather in the epididymis before they’re ready for ejaculation.
Q: How does ejaculation work? A: When a man is sexually aroused, his parasympathetic nervous system takes over and signals his body to prepare for ejaculation. Once he reaches orgasm, the muscles surrounding his urethra contract and push semen out of his penis. The average man releases around 2-5 milliliters of semen per ejaculate, containing millions of sperm cells.
Q: Where do sperm go after ejaculation? A: After being released during ejaculation, sperm enter the vagina through semen. While their journey towards their final destination may seem short, it’s actually very intricate due to several variables including acidity levels in cervical mucus as well as vaginal fluctuation in pH.
Q: How long does it take for sperm to reach an egg? A: On average, it takes up anywhere between 30 minutes to three days for a single sperm cell to travel from the cervix up into one of a woman’s fallopian tubes where fertilization can occur with an available egg cell – but depending on conditions like distance between partners’ bodies or time since ovulation conception might never happen at all!
Q: What requirements do sperms have to meet so that they can successfully fertilize an egg? A: Before fertilizing an egg, sperm have to go through a series of tests such as the cervical mucus test and the penetration test. From there, if sperm find their way into the fallopian tubes where an egg is present then they can potentially meet up with waiting eggs for fertilization.
Q: What are some factors that could decrease sperm count or make them less mobile? A: There are several lifestyle habits that could worsen sperm health like smoking or excessive drinking, sedentary behavior and stress which reduces levels of testosterone in males. Poor nutrition, chronic illness, sexually transmitted infections (STIs), genetics, medications you take regularly for other conditions – such as antidepressants- poor sleep hygiene also negatively impacts reproductive function in both men and women.
In conclusion, there’s more to reproductive biology than just intercourse. Understanding the journey that sperms travel from ejaculation to fertilization is essential in ensuring successful conception. While various variables can come into play at times making it challenging for some couples to conceive according to expectations; taking care of yourself and reducing harmful lifestyle choices
Fertilization is a miraculous process that has fascinated researchers since the beginning of time. The combination of genetic material from two different organisms results in the creation of a totally unique being—a blend of traits and characteristics that make each individual distinct and special.
For conception to occur, a male’s sperm must travel through a complex maze before it meets with the female’s egg. This journey starts from the moment an ejaculation occurs and ends when fertilization takes place.
The path sperm take is nothing short of remarkable. It can take anywhere from five minutes to several days for them to reach their destination—a feat, given that sperm cells are minuscule compared to human beings and have to overcome several obstacles along the way.
Once released into the vagina during intercourse, sperm begin their arduous journey upwards into the fallopian tubes, where the female’s egg awaits fertilization. Sperm swim against gravity through multiple barriers such as cervical mucus, which can be difficult to penetrate even for healthy sperm cells.
Sperm’s motility, or ability to move quickly towards their destination, is also crucial in fertilization. They move like tiny propellers driven by a whip-like tail called flagellum, which helps them traverse through different kinds of fluids present throughout their journey.
As they progress further towards fallopian tubes, they encounter various natural filters such as immunity system cells protecting against foreign invaders trying to access eggs leading up to white blood cell towers defending these pathways along their long course “mountains”.
When finally reaching mature ovum awaiting them in its zone at the end of this journey in ampulla regions or points (depending on woman cycle), millions come close but only one makes it inside and fertilize egg marking beginning stages an embryo genesis phase; all others either die or get lost along this path filled with numerous biochemical obstacles preventing successful fertilization at every step (Incredible!).
The process of fertilization carried out by sperm is truly intriguing; it’s a testament to the amazing power and resilience of these tiny, yet mighty cells. It’s a fascinating journey that spans several days and involves crossing numerous barriers and obstacles.
It’s no wonder that researchers and scientists continue to study this complex process, hoping to unravel its mysteries further. Just imagine what other secrets could yet be hidden within the intricate processes of human pregnancy – who knows what new discoveries await us as we delve deeper into the world of reproductive biology!
The miracle of life is a fascinating phenomenon that never ceases to amaze us. We all know that the human reproductive system plays a vital role in bringing new life into this world, but have you ever wondered about the intricacies of the male reproductive tract and its role in sperm travel path? Let’s dive deeper and explore this miraculous journey.
The Male Reproductive Tract
The male reproductive system mainly comprises two organs, the testes and the penis. The testes are responsible for producing sperm cells, which are then transported out of the body by way of the penis. However, it is not as simple as it sounds; several structures and mechanisms ensure that sperm travel along their designated path.
Sperm Production
Sperm production takes place inside a network of tiny tubes called seminiferous tubules located within each testicle. Within these tubes, cells undergo meiosis – a special cell division mechanism – to produce mature, functional sperm cells with half the genetic material required for reproduction.
Transportation
Once produced, mature sperm cells move from seminiferous tubules toward epididymis (a duct situated above each testis). During that journey, they acquire motility from surrounding fluids secreted by accessory glands like prostate gland and seminal vesicle. The fluid also provides nutrients to sustain their energy needs while they swim to reach their ultimate destination — an egg inside female reproductive tract.
Ejaculation
When sexual stimulation or arousal occurs, muscles surrounding the epididymis contract, forcing sperm into vas deferens – muscular ducts that carry them upwards towards prostate gland. Here they mix with seminal fluid when ejaculation occurs—from here; millions of swimming soldiers commence their incredible race to find familiar eggs.
Travel Path
When semen shoots out through penis during ejaculation inevitably makes some contact with outsides surfaces before it enters female genitalia. Inclined vaginal walls help channel movement up toward cervix opening leading deeper into reproductive tract. There are more hurdles to overcome inside a female’s body than one would expect as the path is full of obstacles. This includes acidic environments in the vagina, and barriers produced by mucus on the cervix.
Final Thoughts
The male reproductive tract and its role in sperm travel can be viewed as a remarkable example of evolution at work. The closely coordinated response between organs & proteins secretion, advanced muscular contractions, transportation throughout several ducts – all these mechanisms adapted to enhance chance of fertilization success showcases nature’s brilliance. As humans, we must appreciate how our bodies have evolved over millennia to bring new life into this world. And now that you know just how incredible and fascinating the male reproductive system is let us take a moment to marvel at it.
Conception is one of nature’s most fascinating and intricate processes. It represents the merging of two cells, the sperm and the egg, which leads to a new life. This process has fascinated scientists for years, leading to numerous studies and research in an attempt to uncover all its mysteries. One particular area of discovery that continues to intrigue researchers is the path travelled by sperm during conception.
Sperm travel through a series of complex environments within the female reproductive system on their journey to fertilize an egg. To understand this journey, it’s essential first to know what happens when a male ejaculates.
When males ejaculate, semen – a mixture made up of sperm, enzymes, proteins and other substances – is released from the penis into the female reproductive system via intercourse or direct injection techniques such as artificial insemination. After entering into this environment created by a woman’s body temperature and hormones, some sperm die instantly due to unfriendly conditions like acidity.
The surviving sperms start their journey through different parts of the female reproductive system such as cervix-uterus-fallopian tubes over several hours or days depending on individuals’ anatomy and physiology before finding themselves in contact with an egg cell. This trip requires them first navigating against gravity’s pull entirely; once they reach the uterus at about 45mins/1hour after ejaculation, contractions of cervical mucus carry them further up into fallopian tubes where most successful healthy fertilisations take place under ideal ovulation timing.
While this process seems straightforward enough in theory: get from point A (ejaculation) to point B (an egg cell), there are no guarantees that any given sperm will reach its destination successfully fertilizing an egg cell ultimately. In fact, only about 300 million out of billions released sperm amount actually get close enough for chance encounter with unprotected eggs for natural conceptions: The vast majority wastes existing energy resources lingering around due unfavourable conditions and possible sperm anomalous health issues.
Overall, for conception to occur, the intricate symphony of events leading up to fertilization must work seamlessly together. Even slight disruptions in any of the stages could result in infertility or no viable pregnancies.
Discovering the secrets of sperm travel path is only part of our knowledge pool about reproductive health sciences- as there are still many things we do not know yet; however, it’s an exciting area of study that has vast potential implications for infertility treatments and fertility preservation efforts. It’s an undiscovered universe that presents much promise for improving human reproduction management in spite of its challenging terrain- uncovering more about this unseen world wouldn’t hurt!


How Long Does Sperm Live After Ejaculation?
- Fact checked
- Male Fertility
Last updated on Jan 25th, 2023
Table of contents
- How Long Does Sperm Live in the Female Reproductive Tract?
- How about Skin and Dry Surfaces?
- Ejaculating in Water?
- What is the Lifespan of Frozen Sperm?
Start Your Fertility Journey
Knowing how long sperm can live after ejaculation is important for those trying to conceive. This also applies to those trying to avoid pregnancy while using birth control and/or having unprotected sex. The lifetime of sperm outside the body depends on several physical and environmental factors (cervical mucus, humidity, body temperature etc). Today we’ll discuss how long sperm lives after ejaculation in water, the female reproductive tract, on the skin, and more.

After intercourse sperm can live in the female body up to 5 days depending on its environment.
Men may ejaculate over 40 million sperm cells at once during intercourse. These sperm swim upwards towards the fallopian tubes , looking for a mature egg to fertilize. Fast swimming sperm can reach a mature egg as quickly as 30 minutes.
The lifespan of sperm is under debate once it enters a woman’s body. The lifespan of sperm and sperm motility(swimming) is heavily influenced by cervical mucus. Because mucus provides sperm with the nutrients and the environment needed to live longer.
This is amazing considering that sperm can have a brief lifespan. When there is no cervical mucus present, sperm dries out within a few hours. Tracking cervical mucus is essential to understanding your fertility because of this.
When your cervical mucus is rich in nutrients, the lifespan of sperm inside the vagina is prolonged. This gives the sperm extra time to reach and fertilize the egg. Sperm may also simply remain idle until the egg is released and ready to be fertilized.
Research shows that the chances of conceiving are more likely when intercourse is a few days before ovulation. Partly due to cervical mucus becoming more fertile approaching ovulation.
Learning to read the changes in mucus takes time. Also, mucus can be affected by :
- Other health related variables
However, the Mira fertility tracker measures your actual fertility hormone concentrations and shows your unique hormone curve. Thus, helping you accurately track your ovulation cycle even if you have variable cycles.
In conclusion, the lifespan of sperm inside a vagina strongly correlates to the conditions of the cervical mucus. Your cervical mucus changes as your menstrual cycle progress, gradually becoming more sticky and egg-white when closer to ovulation. However, accurately tracking the fertile window of your reproductive system using cervical mucus is chancy .
Sperm left out on a dry surface(skin) becomes non-fertile within a few hours and can not get you pregnant. After previously dried sperm becomes rehydrated, it will still be non-fertile ( more on what to do and not do after sex here ).
When using the withdrawal method of sex, depending on the conditions, ejaculation usually occurs further away from the vulva. Although, sperm on the vulva or on the upper thighs can possibly find their way into the vagina, resulting in pregnancy .
The condition of the pH and temperature that a sperm cell resides in is important in determining how long it survives. A sperm’s lifespan is practically nonexistent in chlorinated pools, hot tubs, and jacuzzis. Yet, it is possible for sperm to survive for a couple of minutes with plain water in a warm bath . However, a pregnancy occurring from warm bath water with sperm in it is not likely, assuming no prior intercourse has taken place.
When sperm is properly stored in a frozen container, it continues to be fertile for an indefinite time period. There have been reported pregnancies for cases where sperm was stored for 21 years , before being thawed then inseminated .
Sperm is usually frozen at -70˚C when it is stored. Roughly 50% of sperm cells end up fertile after being frozen and then thawed out. Fortunately, the sperm cells are still capable of fertilization after this process.
Mira’s Editorial Process
All content produced by Mira meets stringent editorial standards, ensuring excellence and accuracy in language and medical precision. Every piece undergoes thorough fact-checking and review by qualified professionals. Check out our full editorial process to learn more.
Related articles

11 minutes read
Prolactin and Fertility: Everything You Need to Know

10 Ways to Improve Male Fertility and Increase Sperm Count

6 minutes read
What are the effects of smoking cannabis on fertility – a detailed research
Science helps you get pregnant faster.
Get the real-time accuracy Mira has to offer and reach your fertility goals.

Please wait while you are redirected to the right page...
Please share your location to continue.
Check our help guide for more info.

Sperm Biology from Production to Ejaculation
- First Online: 01 January 2015
Cite this chapter

- Damayanthi Durairajanayagam 4 ,
- Anil K. Rengan BA 4 , 5 ,
- Rakesh K. Sharma 4 &
- Ashok Agarwal 4
2105 Accesses
3 Citations
21 Altmetric
Spermatogenesis is a sequence of highly intricate stages by which an undifferentiated diploid spermatogonium matures into a specialized, genetically unique haploid spermatozoon. Within the Sertoli cells, both mitosis and meiosis are responsible for transforming the diploid spermatogonial cells into unique haploid spermatids. This process requires the assistance of hormones regulated via the hypothalamus–pituitary–gonadal axis—namely, gonadotropin-releasing hormone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH). However, not all spermatogonia are destined to mature. In fact, most undergo apoptosis and are phagocytosed. Through spermiogenesis, spermatids elongate to form spermatozoa, which then leave the Sertoli cells and enter the epididymis for final maturation. Here, they acquire motility and acrosomal function, which are necessary for successful fertilization. This entire process from production to ejaculation of mature spermatozoa takes, on average, 64 days to complete. Essentially, spermatogenesis and spermiogenesis create fully functional spermatozoa that can travel efficiently through the female reproductive tract to the ovum and allows for the contribution of exclusive male genes to the offspring genome. This chapter serves as a comprehensive overview of sperm biology from production to ejaculation.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Agger P. Scrotal and testicular temperature: its relation to sperm count before and after operation for varicocele. Fertil Steril. 1971;22(5):286–97.
CAS PubMed Google Scholar
Candas V, Becmeur F, Bothorel B, Hoeft A. Qualitative assessment of thermal and evaporative adjustments of human scrotal skin in response to heat stress. Int J Androl. 1993;16(2):137–42.
Article CAS PubMed Google Scholar
Middendorff R, Muller D, Mewe M, Mukhopadhyay AK, Holstein AF, Davidoff MS. The tunica albuginea of the human testis is characterized by complex contraction and relaxation activities regulated by cyclic GMP. J Clin Endocrinol Metab. 2002;87(7):3486–99.
Roosen-Runge EC, Holstein AF. The human rete testis. Cell Tissue Res. 1978;189(3):409–33.
Holstein AF, Schafer E. A further type of transient cytoplasmic organelle in human spermatids. Cell Tissue Res. 1978;192(2):359–61.
Davidoff MS, Breucker H, Holstein AF, Seidl K. Cellular architecture of the lamina propria of human seminiferous tubules. Cell Tissue Res. 1990;262(2):253–61.
Holstein AF, Maekawa M, Nagano T, Davidoff MS. Myofibroblasts in the lamina propria of human semi-niferous tubules are dynamic structures of heterogeneous phenotype. Arch Histol Cytol. 1996;59(2):109–25.
Holstein AF, Schulze W, Davidoff M. Understanding spermatogenesis is a prerequisite for treatment. Reprod Biol Endocrinol. 2003;1:107.
Article PubMed Central PubMed Google Scholar
Wang H, Xiong W, Chen Y, Ma Q, Ma J, Ge Y, et al. Evaluation on the phagocytosis of apoptotic spermatogenic cells by Sertoli cells in vitro through detecting lipid droplet formation by Oil Red O staining. Reproduction. 2006;132(3):485–92.
Holstein AF. Spermatogenese beim Menschen: Grundlagenforschung und Klinik. Ann Anat. 1999;181:427–36.
Cheng CY, Mruk DD. A local autocrine axis in the testes that regulates spermatogenesis. Nat Rev Endocrinol. 2010;6(7):380–95.
Article CAS PubMed Central PubMed Google Scholar
DeKretser DM, Kerr JB. The cytology of the testis. In: Knobill E, Neil JD, Editors. The physiology of reproduction. New York: Raven; 1994. p. 1177–290.
Google Scholar
Sharpe RM. Regulation of spermatogenesis. In: Knobill E, Neil JD, Editors. The physiology of reproduction. New York: Raven; 1994. p. 1363–434.
Jegou B. The Sertoli cell. Baillieres Clin Endocrinol Metab. 1992;6(2):273–311.
Clermont Y. Kinetics of spermatogenesis in mammals: seminiferous epithelium cycle and spermatogonial renewal. Physiol Rev. 1972;52(1):198–236.
Missell LM, Holochwost D, Boban D, Santi N, Shefi S, Hellerstein MK, Turek PJ. A stable isotop-mass spectrometric method for measuring human spermatogenesis kinetics in vivo. J Urol. 2006;175:242–6.
Culty M. Gonocytes, the forgotten cells of the germ cell lineage. Birth Defects Res C Embryo Today. 2009;87(1):1–26
Dym M, Fawcett DW. Further observations on the numbers of spermatogonia, spermatocytes, and spermatids connected by intercellular bridges in the mammalian testis. Biol Reprod. 1971;4(2):195–215.
Holstein AF, Roosen-Runge EC, Schirren C. Illustrated pathology of human spermatogenesis. Berlin: Grosse; 1988.
Izaurralde E, Kas E, Laemmli UK. Highly preferential nucleation of histone H1 assembly on scaffold-associated regions. J Mol Biol. 1989;210(3):573–85.
Adachi Y, Kas E, Laemmli UK. Preferential, cooperative binding of DNA topoisomerase II to scaffold-associated regions. EMBO J. 1989;8(13):3997–4006.
CAS PubMed Central PubMed Google Scholar
Giroux CN. Meiosis: components and process in nuclear differentiation. Dev Genet. 1992;13(6):387–91.
Auger J, Schoevaert D, Negulesco I, Dadoune JP. The nuclear status of human sperm cells by TEM image cytometry: nuclear shape and chromatin texture in semen samples from fertile and infertile men. J Androl. 1993;14(6):456–63.
Miller D, Brinkworth M, Iles D. Paternal DNA packaging in spermatozoa: more than the sum of its parts? DNA, histones, protamines and epigenetics. Reproduction. 2010;139(2):287–301.
Braun RE. Packaging paternal chromosomes with protamine. Nat Genet. 2001;28(1):10–2.
Balhorn R. The protamine family of sperm nuclear proteins. Genome Biol. 2007;8(9):227.
Bedford JM, Calvin H, Cooper GW. The maturation of spermatozoa in the human epididymis. J Reprod Fertil Suppl. 1973;18:199–213.
Russell LD, Griswold MD. The Sertoli cells. Clearwater: Cache Press; 1993.
Breucker H, Schafer E, Holstein AF. Morphogenesis and fate of the residual body in human spermiogenesis. Cell Tissue Res. 1985;240(2):303–9.
Sharma R, Agarwal A. Spermatogenesis: An Overview. In: Zini A, Agarwal A, Editors. Sperm chromatin: biological and clinical applications in male. New York: Springer; 2011. p. 19–44.
Chapter Google Scholar
WHO. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 5. ed. Cambridge: Cambridge University Press; 2010.
Katz DF, Overstreet JW, Samuels SJ, Niswander PW, Bloom TD, Lewis EL. Morphometric analysis of spermatozoa in the assessment of human male fertility. J Androl. 1986;7(4):203–10.
WHO. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 4. ed. Cambridge: Cambridge University Press; 1999.
Hafez ES. The human semen and fertility regulation in the male. International Conference in Andrology. J Reprod Med. 1976;16(2):91–6.
Menkveld R, Stander FS, Kotze TJ, Kruger TF, van Zyl JA. The evaluation of morphological characteristics of human spermatozoa according to stricter criteria. Hum Reprod. 1990;5(5):586–92.
Kruger TF, Menkveld R, Stander FS, Lombard CJ, Van der Merwe JP, van Zyl JA, et al. Sperm morphologic features as a prognostic factor in in vitro fertilization. Fertil Steril. 1986;46(6):1118–23.
Langlais J, Roberts KD. A molecular membrane model of sperm capacitation and the acrosome reaction of mammalian spermatozoa. Gamete Res. 1985;12(2):183–224.
Article CAS Google Scholar
Osheroff JE, Visconti PE, Valenzuela JP, Travis AJ, Alvarez J, Kopf GS. Regulation of human sperm capacitation by a cholesterol efflux-stimulated signal transduction pathway leading to protein kinase A-mediated up-regulation of protein tyrosine phosphorylation. Mol Hum Reprod. 1999;5(11):1017–26.
Song X, Li F, Cao G, Zhang J, Han Y. Distribution of alpha-D-mannose residues on zona pellucida and their role(s) in fertilization in pigs. Sci China C Life Sci. 2007;50(2):170–7.
Benoff S, Hurley I, Cooper GW, Mandel FS, Hershlag A, Scholl GM, et al. Fertilization potential in vitro is correlated with head-specific mannose-ligand receptor expression, acrosome status and membrane cholesterol content. Hum Reprod. 1993;8(12):2155–66.
Heller CH, Clermont Y. Kinetics of the germinal epithelium in man. Recent Prog Horm Res. 1964;20:545–75.
Schulze W, Rehder U. Organization and morphogenesis of the human seminiferous epithelium. Cell Tissue Res. 1984;237(3):395–407.
Filippini A, Riccioli A, Padula F, Lauretti P, D’Alessio A, De Cesaris P, et al. Control and impairment of immune privilege in the testis and in semen. Hum Reprod Update. 2001;7(5):444–9.
Mahi-Brown CA, Yule TD, Tung KS. Evidence for active immunological regulation in prevention of testicular autoimmune disease independent of the blood-testis barrier. Am J Reprod Immunol Microbiol. 1988;16(4):165–70.
Sharpe RM. Environmental/lifestyle effects on spermatogenesis. Philos Trans R Soc Lond B Biol Sci. 2010;365(1546):1697–712.
Magelssen H, Brydoy M, Fossa SD. The effects of cancer and cancer treatments on male reproductive function. Nat Clin Pract Urol. 2006;3(6):312–22.
Yeung BH, Wan HT, Law AY, Wong CK. Endocrine disrupting chemicals: multiple effects on testicular signaling and spermatogenesis. Spermatogenesis. 2011;1(3):231–9.
Mathur PP, D’Cruz SC. The effect of environmental contaminants on testicular function. Asian J Androl. 2011;13(4):585–91.
Esteves SC, Zini A, Aziz N, Alvarez JG, Sabanegh ES, Jr., Agarwal A. Critical appraisal of World Health Organization’s new reference values for human semen characteristics and effect on diagnosis and treatment of subfertile men. Urology. 2012;79(1):16–22.
Article PubMed Google Scholar
Download references
Author information
Authors and affiliations.
Center for Reproductive Medicine, Cleveland Clinic, Cleveland, OH, USA
Damayanthi Durairajanayagam, Anil K. Rengan BA, Rakesh K. Sharma & Ashok Agarwal
7 Setter Place, 08824, Kendall Park, NJ, USA
Anil K. Rengan BA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Anil K. Rengan BA .
Editor information
Editors and affiliations.
Ronald O. Perelman and Claudia Cohen Center for Reproductive Medicine, Weill Cornell Medical College, New York, New York, USA
Glenn L. Schattman
Andrology and Human Reproduction Clinic Referral Center for Male Reproduction, ANDROFERT, Campinas, São Paulo, Brazil
Sandro C. Esteves
Andrology Center & Center for Reproductive Medicine, Lerner College of Medicine Case Western Reserve University, Cleveland, Ohio, USA
Ashok Agarwal
Rights and permissions
Reprints and permissions
Copyright information
© 2015 Springer Science+Business Media, LLC
About this chapter
Durairajanayagam, D., Rengan, A., Sharma, R., Agarwal, A. (2015). Sperm Biology from Production to Ejaculation. In: Schattman, G., Esteves, S., Agarwal, A. (eds) Unexplained Infertility. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-2140-9_5
Download citation
DOI : https://doi.org/10.1007/978-1-4939-2140-9_5
Published : 13 May 2015
Publisher Name : Springer, New York, NY
Print ISBN : 978-1-4939-2139-3
Online ISBN : 978-1-4939-2140-9
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Search Please fill out this field.
- Newsletters
- Sweepstakes
- Starting a Family
Do You Need To Take Steps To Prevent Sperm Leakage After Sex?
And can you still get pregnant if sperm leaks after penis-in-vagina sex? We spoke with an expert to learn more.
- Why It's OK If Some Semen Leaks Out
The Journey Sperm Take After Sex
- You Don't Need To Take Steps To Prevent Sperm Leakage
When To See a Health Care Provider
If you're trying to get pregnant, you might start viewing penis-in-vagina sex a little differently. For instance, you might begin to time sex to increase your chances of conceiving and trying positions that are prime for baby-making —and keeping semen inside the vagina.
You might also notice how sperm sometimes comes out of the vagina hours after sex. This might lead you to look for steps to prevent sperm leakage.
When trying to conceive (TTC), it's normal to be worried if you notice that a small amount of semen (and, by extension, sperm) leaks out of your vagina after your partner ejaculates. This leakage is nothing to worry about but can be discouraging when the goal is conception. You're left to wonder: "How is sperm supposed to fertilize my eggs if it's not making it there?"
In actuality, though, it's entirely normal for some sperm to leak out of the vagina after sex that ends in your partner ejaculating into your vagina, says Michele Hakakha, MD, FACOG, an OB-GYN in Beverly Hills and author of Expecting 411 . Good news: Some semen coming out of the vagina after baby-making sex is expected and doesn't affect your chances of getting pregnant.
Read on to learn why you can still get pregnant even if sperm comes out after sex.
Why It's OK If Some Semen Leaks Out
To understand why it's OK if some semen comes out of the vagina after baby-making sex, it helps to get a basic run-down of how conception works. "Semen (the stuff that comes out of the penis with ejaculation) is made up of a lot of different things," explains Dr. Hakakha. "One of its components is sperm ."
Healthy ejaculate contains anywhere from 20 to 150 million sperm per milliliter, and 60% of those have normal shape and motility (forward movement). And just one sperm is needed to fertilize your egg for conception to occur.
So, in reality, while you may notice what appears to be quite a lot of semen leaking out of the vagina after penis-in-vagina sex, sperm is just one component of that fluid—and there's likely still plenty of it to reach an egg if that is your goal.
Michele Hakakha, MD, FACOG
You don't need to lie in bed with your legs up after intercourse to get pregnant. The fact that semen is leaking out afterward doesn't decrease your chances of conceiving.
Ejaculate often leaks out of the vagina after baby-making sex, and while there are not many steps you can take to prevent sperm leakage, that's OK. In fact, some amount of leakage could be a good sign since it could indicate a healthy amount of semen.
Adene Sanchez/E+/Getty Images
If you're still uneasy about the amount of semen you find leaking out after sex, it can be helpful to think about the journey sperm takes after ejaculation. How can you confirm how many sperm went inside? Well, it may help to know that few sperm actually ends up where it needs to go to conceive successfully ( assuming the timing is right , of course).
Here are some places sperm may end up after entering the vagina:
- Some semen will inevitably leak out of the vagina upon standing or changing positions.
- Foundational research has shown that some of the sperm will remain in the back of the vagina (the posterior fornix).
- An even smaller amount will make its way through the cervix, into the uterus, and down the fallopian tubes.
Sperm travels quickly, so it begins trekking to the fallopian tubes within minutes. "It's here, in the fallopian tubes, that the sperm and egg meet," says Dr. Hakakha.
You Don't Need To Take Steps To Prevent Sperm Leakage
The bottom line is that it's perfectly normal if some amount of semen (and sperm) leaks from the vagina after baby-making sex. And you don't need to worry about trying to prevent sperm leakage to keep it inside, either.
"You don't need to lie in bed with your legs up after intercourse to get pregnant," says Dr. Hakakha. "The fact that semen is leaking out afterward doesn't decrease your chances of conceiving."
A pregnancy can still result if the right circumstances are in place. For instance, timing sex with ovulation makes it more likely that an egg will be ready to be fertilized.
But keep in mind that conception often takes time . Research shows the average time to conception is about four months. That same research found that those with average cycle lengths tend to conceive faster than those with shorter or longer cycles.
According to the American College of Obstetricians and Gynecologists (ACOG), if you're under 35 and you've been trying to conceive for one year with no results, you may want to consider a fertility evaluation. If you're over 35 years old, the time frame decreases to six months, and those over 40 should get one right away.
The first step is to talk to an OB-GYN who may refer you to a reproductive endocrinologist (an obstetrician-gynecologist specializing in infertility issues). There are many potential factors involved in infertility; talking to a specialist can help you and your partner chart a path toward a treatment plan that may help you successfully conceive.
Key Takeaways
There is no cause for alarm if semen leaks out of the vagina after ejaculation during sex—and there is no need to take steps to prevent sperm leakage if you want to conceive. Thankfully, this is a normal and common part of baby-making sex, and you can still conceive even if it happens. Talk to a health care provider if you have questions about increasing your chances of getting pregnant .
Timed Intercourse for Couples Trying To Conceive . Cochrane Library . 2023.
Semen Analysis . MedlinePlus National Library of Medicine . 2022.
Detection of Spermatozoa Following Consensual Sexual Intercourse . Forensic Science International . 2012.
Why So Many Sperm Cells? . Communicative and Integrative Biology . 2015.
Time to conception and the menstrual cycle: an observational study of fertility app users who conceived . Hum Fertil (Camb) . 2021.
Evaluating Infertility . American College of Obstetricians and Gynecologists . 2022.
Related Articles
- Search the site GO Please fill out this field.
- Newsletters
- Sexual Health
What Happens When You Don't Ejaculate (Release Sperm) for a Long Time?
Wendy Wisner is freelance journalist and international board certified lactation consultant (IBCLC). She has written about all things pregnancy, maternal/child health, parenting, and general health and wellness.
:max_bytes(150000):strip_icc():format(webp)/WendyWisner2022-d8111a5bfee84913ac464f394bc98516.jpeg)
- Side Effects
Benefits of Not Ejaculating
Benefits of ejaculating.
- Side Effects of Frequent Ejaculation
When To See a Healthcare Provider
FatCamera / Getty Images
Ejaculation refers to semen being released from the penis during orgasm. There are many reasons why someone may not ejaculate for a long time. Some people do it intentionally for personal or religious reasons. Some people abstain to increase their sperm count for fertility purposes. Other people may have a health condition that makes ejaculation difficult or impossible.
The effects of not ejaculating haven’t been studied extensively, but there is no evidence that doing so—even for extensive periods—is harmful. There are no known negative side effects of not ejaculating. That said, if you are unable to ejaculate, or are having trouble ejaculating, it’s important to see a healthcare provider to find out if you have an underlying health condition that may be causing this.
Reasons You're Not Ejaculating
There are several reasons why someone may not be ejaculating. Sometimes the reasons are intentional, and sometimes they are not.
Intentionally Abstaining
Whether or not to engage in sexual activity or masturbation is a personal choice. Some people make mindful choices not to ejaculate for specific periods or extended periods. For example:
- Many religions advise abstention from masturbation or sexual activity.
- Someone may also choose not to ejaculate for personal reasons or as a part of a spiritual journey.
- Healthcare providers might recommend abstaining from ejaculating for several days while trying to conceive or before fertility treatments .
Delayed Ejaculation
A sexual disorder called delayed ejaculation can be the cause of not ejaculating. Delayed ejaculation is defined as either a delay in the ability to ejaculate or a complete inability to ejaculate.
Delayed ejaculation is not common and experts aren’t sure what causes it. It used to be believed that relationship issues or psychological issues cause delayed ejaculation. It might be caused by endocrine, genetic, or neurobiological conditions, or it might be a medication side effect. Endocrine conditions are hormone-related, such as low testosterone.
Retrograde Ejaculation
Retrograde ejaculation is when semen is not expelled through the penis during orgasm, but enters the bladder instead. This is often referred to as a “dry orgasm” because you experience an orgasm, but you see a very low volume of semen or no semen at all.
Conditions like diabetes, previous pelvic surgeries, neurological conditions, and bladder malformations can cause retrograde ejaculation. It may also be a side effect of certain medications.
Anejaculation
Anejaculation is when you don’t ejaculate at all during sexual activity. A person with anejaculation experiences erections without ejaculation. However, they may ejaculate during nocturnal emissions (wet dreams) or while masturbating.
There are various potential causes of anejaculation, including health conditions like spinal cord injuries, diabetes, and multiple sclerosis. Potential psychological causes include a lack of body awareness, guilt or shame about sex, and performance anxiety .
People with male reproductive organs can ejaculate and produce sperm for their entire lives—there isn’t a particular age where this ability goes away. However, similarly to people with female reproductive organs, reproductive capacity decreases as they age. As such, it can be more difficult to experience erections and orgasms/ejaculations as they get older.
Side Effects of Not Ejaculating for a Long Time
There is nothing inherently harmful about not ejaculating for a long time. There are no known dangerous physical or psychological side effects. However, some general side effects are possible for certain individuals.
Physical Effects
Testes constantly produce sperm. If you don’t ejaculate it, the sperm becomes reabsorbed into the body. Some people are concerned that you will get “blue balls” if you don’t ejaculate, or pain due to sexual arousal that doesn’t end in orgasm. However, there are no known medical problems associated with this phenomenon, and any discomfort resolves without intervention.
Psychological Effects
The mental health effects of not ejaculating or abstaining from ejaculating aren’t well-researched at this time. However, many people report different emotions when they haven’t ejaculated for a long period of time. Some people might experience clarity or peace of mind , while others may report feeling more irritated or distressed.
People who experience ejaculated-related health problems, such as delayed ejaculation or anejaculation, may experience relationship stress, or anxiety surrounding sexual contact and sexual desire.
There are no reported benefits of not ejaculating, and the benefits of this practice have not been studied. Nevertheless, people who intentionally refrain may report benefits, such as mental and emotional balance, decreased fixation on sex, increased energy, and stress relief.
While many people abstain from ejaculating for several days while trying to conceive, or going through fertility treatments, the effectiveness of this practice is not clear. Research has found that abstaining from ejaculating for several days increases sperm count and semen volume. It’s less clear if this practice is helpful for other sperm aspects, such as motility (movement speed), vitality, and morphology (sperm shape).
Again, the mental health benefits of ejaculating or not ejaculating are not well studied. Still, there are some immediate benefits to experiencing orgasm, including reduced stress, improved mood, and even pain relief.
There is some evidence that ejaculation frequency might be protective against developing prostate cancer . For example, one 2016 study found that participants who reported higher rates of ejaculation were less likely to be diagnosed with prostate cancer.
Side Effects of Ejaculating Too Frequently
It’s normal to ejaculate frequently, and ejaculating daily or even several times a day has no known negative side effects. Ejaculating frequently may cause certain side effects, such as chafing of the skin (usually from masturbation specifically) or fatigue .
Some people may be concerned that frequent ejaculation may cause sex addiction or other sexual disorders. While the exact causes of sex addiction haven’t been identified yet, it is not thought to be caused by excessive masturbation or sexual activity. On the other hand, excessive masturbation or sexual activity may be a symptom of a sex addiction.
Masturbating frequently might affect sexual function, leading to issues like sexual desensitization, where you become less sensitive to sexual stimulation. Some people who masturbate frequently experience trouble getting erections or reaching orgasm through other forms of sexual activity.
It’s normal for some people to not ejaculate for a long time. In most cases, it will not cause physical or psychological harm.
See a healthcare provider if you have any concerns about your ejaculation patterns. If you are intentionally not masturbating because of guilt or shame about sex or masturbation, you may want to speak to a therapist about your feelings and concerns.
Conditions like diabetes, multiple sclerosis, and sexual disorders can result in an inability to ejaculate. Endocrine disorders, neurological disorders, and medication side effects may also cause these symptoms. A healthcare provider can evaluate you for any underlying medical conditions and discuss treatment plans.
A Quick Review
Not ejaculating for several days, weeks, or even longer, is not damaging to your health. Some people abstain from ejaculating for religious reasons, personal reasons, or to increase sperm count while trying to conceive .
If you are unable to ejaculate, you may have an underlying medical condition causing these symptoms. It's important to visit your healthcare provider for an evaluation.
Albobali Y, Madi MY. Masturbatory guilt leading to severe depression . Cureus . 2021;13(3):e13626. doi:10.7759/cureus.13626
Hanson BM, Aston KI, Jenkins TG, et al. The impact of ejaculatory abstinence on semen analysis parameters: A systematic review . J Assist Reprod Genet . 2018;35(2):213-220. doi:10.1007/s10815-017-1086-0
Gopalakrishnan R, Thangadurai P, Kuruvilla A, et al. Situational psychogenic anejaculation: A case study . Indian J Psychol Med . 2014;36(3):329-331. doi:10.4103/0253-7176.135393
Abdel-Hamid IA, Ali OI. Delayed ejaculation: Pathophysiology, diagnosis, and treatment . World J Mens Health . 2018;36(1):22-40. doi:10.5534/wjmh.17051
Society for Male Reproduction and Urology. Treatment options for patients with ejaculatory dysfunction .
Gunes S, Hekim GN, Arslan MA, et al. Effects of aging on the male reproductive system . J Assist Reprod Genet . 2016;33(4):441-454. doi:10.1007/s10815-016-0663-y
MedlinePlus. Sperm release pathway .
Levang S, Henkelman M, Neish R, et al. “Blue balls” and sexual coercion: A survey study of genitopelvic pain after sexual arousal without orgasm and its implications for sexual advances . Sex Med . 2023;11(2):qfad016. doi:10.1093/sexmed/qfad016
Mascherek A, Reidick MC, Gallinat J, et al. Is ejaculation frequency in men related to general and mental health? Looking back and looking forward . Front Psychol . 2021;12:693121. doi:10.3389/fpsyg.2021.693121
MedlinePlus. Delayed ejaculation .
Gianotten WL. The Health Benefits of Sexual Expression . In: Geuens S, Polona Mivšek A, Gianotten W. (eds). Midwifery and Sexuality . doi:10.1007/978-3-031-18432-1_4
Rider JR, Wilson KM, Sinnott JA, et al. Ejaculation frequency and risk of prostate cancer: Updated results with an additional decade of follow-up . Eur Urol . 2016;70(6):974-982. doi:10.1016/j.eururo.2016.03.027
Fong TW. Understanding and managing compulsive sexual behaviors . Psychiatry (Edgmont) . 2006;3(11):51-58.
Huang S, Niu C, Santtila P. Masturbation frequency and sexual function in individuals with and without sexual partners . Sexes . 2022; 3(2):229-243. doi:10.3390/sexes3020018
Related Articles
Does ejaculating often reduce your risk of prostate cancer?
Senior Lecturer in Biochemistry, Sheffield Hallam University
Disclosure statement
Daniel Kelly does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
Sheffield Hallam University provides funding as a member of The Conversation UK.
View all partners
In terms of men’s health issues, prostate cancer features high on the agenda. It’s the second most diagnosed cancer in men globally – closely followed by lung cancer. And it’s the most common cancer in men in the UK.
As the prostate is a reproductive organ with its main job being to help make semen – the fluid that carries sperm in ejaculate – researchers have long questioned the effect of sexual factors on a man’s prostate cancer risk. Specifically, does ejaculation protect against prostate cancer risk?
Interestingly, there is some evidence that supports this idea. A recent review looking at all the relevant medical investigations taking place over the last 33 years showed that seven out of the 11 studies reported some beneficial effect of ejaculation frequency on prostate cancer risk.
Although the mechanisms are not completely understood, these studies fit with the idea that ejaculation can reduce prostate cancer by decreasing the concentration of toxins and crystal-like structures that can accumulate in the prostate and potentially cause tumours.
Similarly, ejaculation may alter the immune response within the prostate reducing inflammation – a known risk factor for cancer development – or by increasing immune defence against tumour cells.
Alternatively, by reducing psychological tension ejaculation may lower the activity of the nervous system which then prevents certain prostate cells from dividing too rapidly and increasing the chance of them becoming cancerous.
Despite these suggested mechanisms, in the research implying ejaculation is protective, it appears that specifics are important.
Age plays its part. Sometimes frequency of ejaculation was only protective at ages 20-29 , or 30-39 , and sometimes only in later life (50s and older) and actually increased the risk in younger life (20s).
Other times, ejaculation in adolescence (when the prostate is still developing and maturing) had the greatest impact on the risk of prostate cancer decades later.
But how frequent is frequent? Well, very frequent in some cases.
A study from Harvard University found that men who ejaculated 21 or more times a month enjoyed a 31% lower risk of prostate cancer compared with men who reported four to seven ejaculations per month across their lifetimes.
Similar findings have come from Australia where prostate cancer is 36% less likely to be diagnosed before the age of 70 in men who averaged about five to seven ejaculations a week compared with men who ejaculated less than two to three times a week.
Other research has a much more modest view with greater than four per month being the ejaculation frequency to give protective effects in some age groups and patients.
No firm conclusion
Drawing overall conclusions from this research is difficult, especially when the studies differ so much in the way they were conducted.
Factors like the varied populations of men investigated, the numbers of men included in the analyses, and differences in the way ejaculation frequency is measured (whether this includes intercourse, masturbation and unprompted release usually at night) can all cloud the picture.
In fact, measurement of ejaculation frequency relies on self-reporting and often from many years and decades ago. So this is an estimate at best and can be biased by attitudes, both personal and societal, towards sexual activity and masturbation potentially leading to both over- and under-reporting.
There may also be a bias in the detection of prostate tumours with highly sexually active men delaying or not going to the hospital for the fear that cancer treatment may stop their sexual activity. These men with high ejaculation frequency may therefore actually have prostate cancer that goes unreported in these studies.
It is also possible that ejaculation may not guard against prostate cancer and the links may be due to other factors. For example, men who ejaculate more often might have healthier lifestyles that lower their chances of being diagnosed with cancer.
Reduced ejaculation frequency is related to increased body mass index (BMI), reduced physical activity and divorce – all factors related to poorer general health that in turn may contribute to cancer development.

Testosterone may be important
Testosterone, the main male sex hormone, is also a crucial part of the picture.
It is well known to increase sex drive, so a man with low levels of testosterone may not have the same desire for sexual activity leading to ejaculation as a man with higher levels.
Contrary to early opinions that high testosterone levels in men raise prostate cancer risk, the current view suggests that not only does it not elevate this risk, it is actually low testosterone concentrations that increase risk . This is particularly true for men with existing prostate cancer who have a worse disease outcome when their testosterone is low.
So it may be testosterone reducing a man’s risk of prostate cancer and additionally driving their motivation for sexual activity.
Despite this, most studies do not measure testosterone levels and, at best, only recognise it as a possible influencing factor. One study that did measure the male sex hormone found that men who ejaculated frequently had higher testosterone levels. And it was these men who also had a reduced risk of prostate cancer.
There are benefits of sexual activity and ejaculation beyond the prostate including positive effects on the heart, brain, immune system, sleep and mood. So while the link between ejaculation frequency and prostate cancer is not fully understood and there is a real need for more research, frequent ejaculation (within reason) will certainly do no harm, probably does good and should therefore form part of a man’s healthy lifestyle.
- Prostate cancer
- Male health
- ejaculation

Assistant Editor - 1 year cadetship

Program Development Officer - Business Processes

Executive Dean, Faculty of Health

Lecturer/Senior Lecturer, Earth System Science (School of Science)

Sydney Horizon Educators (Identified)

IMAGES
VIDEO
COMMENTS
Usually, the sperm reaches the egg within 15 to 45 minutes of ejaculation. However, the process could be much longer than that if you haven't ovulated yet by the time you have sex, because sperm can live inside a reproductive tract and wait for an egg for up to five days. While the journey to the egg is certainly long and arduous for the tiny ...
The journey through the female reproductive system. In the process of ejaculation, sperm cells leave the man and enter the vagina. This is where the sperm cells begin the second part of their journey to fertilization. During this second part of the journey the sperm again encounter an large number of obstacles.
Capacitation takes place after ejaculation, in the female reproductive tract, and is required only by mammalian sperm. ... To accomplish the journey to the egg, sperm are equipped to overcome various obstacles that lie ahead, such as navigating the uterotubal junction (UTJ) and penetrating the egg extracellular matrices.
During ovulation, this barrier becomes thinner and changes its acidity creating a friendlier environment for the sperm. The cervical mucus acts as a reservoir for extended sperm survival. Once the sperm have entered the uterus, contractions propel the sperm upward into the fallopian tubes. The first sperm enter the tubes minutes after ejaculation.
The pathway of sperm is the journey that sperm cells take from the testes to the female reproductive tract during fertilization. The journey involves a series of steps, including production, maturation, and transport. Sperm cells are produced in the testes through a process called spermatogenesis that begins at puberty and continues throughout ...
Transport of sperm via erection and ejaculation. This video explores the journey of sperm from the male reproductive system to the female reproductive system. It details the two-step process of erection and ejaculation, explaining the role of the brain and blood vessels in achieving an erection. The video also delves into the anatomy of the ...
Step 1: Production. Sperm production starts at the testicles, where millions of them are produced every day. It takes about 74 days for the male body to produce fully mature and functional sperm. Step 2: Maturation. After being produced in the testicles, immature sperm travel through a tube called the epididymis.
On average, with each ejaculation, nearly 200 to 300 million sperm are released. To meet the egg, semen must travel from the vagina to the fallopian tubes, a tough journey that few sperm survive.
Answer From Patricio C. Gargollo, M.D. The life span of sperm after ejaculation depends on the circumstances. Ejaculated sperm remain viable for several days within the female reproductive tract. Fertilization is possible as long as the sperm remain alive — up to five days. Sperm can also be preserved for decades when semen is frozen.
This is a cordlike structure where the sperm mature and are stored. The release process starts when the penis fills with blood and becomes erect. Continuing to stimulate the penis will cause an ejaculation. Mature sperm begin their journey by travelling from the epididymis to the vas deferens, which propels sperm forward with smooth muscle ...
Extracellular vesicle communication remains important after ejaculation. ... Benham, A. M. & Okabe, M. Fertilization: a sperm's journey to and interaction with the oocyte. J. Clin. Investig. 120 ...
During ejaculation, hundreds of millions of sperm (spermatozoa) are released into the vagina. Almost immediately, millions of these sperm are overcome by the acidity of the vagina (approximately pH 3.8), and millions more may be blocked from entering the uterus by thick cervical mucus. ... Their journey—thought to be facilitated by uterine ...
Author spermblog Reading 15 min Views 260 Published by 18.06.2023. Short answer sperm travel path: Sperm travel from the testes through the epididymis, vas deferens, and ejaculatory duct before being released through the urethra during ejaculation. The journey takes approximately 64-72 days to complete. Contents.
Let' uncover the fascinating science behind male reproduction, exploring the basics of anatomy of the male reproductive system, puberty, the ejaculation mech...
The journey of sperm begins inside the testicles. Males begin to produce sperm at the start of puberty at around 12 or 13 years old. It is a process that requires a slightly cooler temperature, which is why testicles hang outside men's bodies. Nor is it a quick process: the production of sperm takes about 70 days.
The remarkable journey that successful sperm take to reach the oocyte is long and tortuous, filled with viscous fluid, dead ends, and potentially hostile immune cells. ... Spermadhesins represent 90% of the total boar seminal plasma protein and they become peripherally associated with the sperm plasma membrane after ejaculation (Sanz et al., 1993).
After intercourse sperm can live in the female body up to 5 days depending on its environment. Men may ejaculate over 40 million sperm cells at once during intercourse. These sperm swim upwards towards the fallopian tubes, looking for a mature egg to fertilize. Fast swimming sperm can reach a mature egg as quickly as 30 minutes.
The ejaculate, or semen, is freshly produced at the time of ejaculation. Ejaculation normally occurs in a definite sequence. First, a small amount of Cowper's gland fluid is extruded followed by prostatic fluid and the sperm-rich fraction from the ampulla, and finally secretions from the seminal vesicle (Table 5.3 ).
The Journey Sperm Take After Sex . ... There is no cause for alarm if semen leaks out of the vagina after ejaculation during sex—and there is no need to take steps to prevent sperm leakage if ...
People with male reproductive organs can ejaculate and produce sperm for their entire lives—there isn't a particular age where this ability goes away. However, similarly to people with female ...
Prior literature has shown that opacity and sperm concentration of the semen will progressively decrease if the ejaculation occurs shortly after a prior ejaculation and every additional recent ejaculation before that . It should also be noted that colorless mucus-like ejaculate is likely to be pre-ejaculatory fluid from the bulbourethral glands.
As the prostate is a reproductive organ with its main job being to help make semen - the fluid that carries sperm in ejaculate - researchers have long questioned the effect of sexual factors ...