

House Calls – We Bring the Doctor’s Office to the Patient
At Mobile Physician Services, we provide comprehensive care to improve the health and quality of life of our patients – in the convenience and comfort of their own home. Our team of board-certified doctors, advance nurse practitioners, and physician assistants specialize in providing care for patients with medically complex and chronic conditions.
Our Services
We accept Medicare, many insurance plans, and self-pay.
To find out more about our services:
Call Toll-free: (855) 232-0644
E-mail us at [email protected]
Primary Care
Pain management, palliative care.
At Mobile Physician Services, our customized care teams provide patients with both comfort and familiarity as they work with a dedicated primary care provider and care coordinator to improve their health. Our physicians and staff take a proactive approach to preventive care, chronic disease management, and chronic illness support right where you live.
Each home visit includes an in-depth examination and individualized treatment plan, which is monitored and adjusted through routine follow-up visits. The primary care provider will deliver your ongoing care and will recommend to you specialty services as needed.
- Annual Wellness visits : This wellness visit allows your primary care provider to create or update your personalized prevention plan. This visit includes a review of your medical and social history related to your health and may include counseling about preventive services. This plan may help you to prevent or reduce the chances of future illness based on your current health and risk factors.
- New Illness Exams : When a new symptom or ailment arises, call us. Early indications of not feeling well could be a clue that you may be getting sick. A symptom in one part of the body may also be a sign of a problem in another part of the body. Moreover, unrelated symptoms that might seem minor on their own, could be warning signs of a more serious medical disease or condition. The new illness exam can be very brief or more detailed depending on your concerns and the provider’s findings.
- Follow-up Care: Involves a regular medical checkup, which may include a physical exam and laboratory testing. Follow-up care checks are a proactive way of assessing the potential for and preventing health problems from returning after treatment of a disease has ended or an illness has seemingly passed.
- Referral for Specialty Care : Referrals are the link between primary and specialty care. The referral coordination includes the documentation of patient care activities, the transfer of information, the inter-provider communication itself, and the integration of care services to the patient. Mobile Physician Services is a multi-specialty practice so many of these specialty referral services can be made seamlessly with little inconvenience or disruption to the patient and caregivers regular routines.
- Medication Management: Medication management is a treatment structure that ensures our patients are receiving optimal therapeutic results from their prescription medications, both in the short and long term. Our team’s goal is to mitigate medication noncompliance and monitor all prescriptions treatments so that drug interactions complement one another for the most optimal outcome for our patients.
The provider may be a physician, advanced practice nurse or a physician assistant. A dedicated care coordinator will also be assigned for each patient to help arrange comprehensive services and assist patients and their caregivers.
- Online Patient Portal: You and your designated caregiver, if you choose, will be able to connect with your provider through a convenient, safe and secure environment which allows access to your health records and a way to communicate with our staff in a timely manner.
- Telephone Assistance : On call providers are available 24/7 weekdays and weekends.

Our psychiatry team specializes in the diagnosis and management of mental, emotional and behavioral disorders. They carefully evaluate each patient to develop an individualized treatment plan to improve the patient’s overall mental and physical well-being.
- Depression : Depression is a common and often serious medical illness that negatively affects how you may feel, the way you may think, and how you may act. Depression can cause feelings of sadness, despair and hopelessness, which may lead to a loss of interest in activities you once enjoyed.
- Anxiety : Intense, excessive, and persistent worry and fear about everyday common situations. The worry or anxiety could make you feel fatigued, irritable, and interfere with your regular sleep habits.
- Dementia : An overall term that is used to describes a collection of symptoms related to an individual’s decline in memory or other thinking skills. It may be severe enough to diminish a person’s ability to perform everyday common activities. The effects of dementia can negatively influence your memory, thinking and social abilities.
- Phobias : A phobia is when you experience excessive panicking or an irrational fear reaction to a situation. If you have a phobia, you may experience a deep sense of dread or fright when you encounter the source of your fear. The fear may be a certain place, situation, object, animal or even another person.
- Behavioral disorders : Attention deficit, hyperactivity, bipolar, learning, defiant or conduct disorders are all examples of complaints that may have a detrimental impact on a person’s interpersonal relationships with family, friends, and co-workers.
Our team can provide behavioral counselling and medical therapy, when appropriate, to help a patient feel better about themselves and to assist them with better coping and managing their condition.

Our wound care specialists have been trained in the attention and treatment of all types of acute and chronic wounds. They have skill and experience in wound debridement and wound care procedures – managing chronic, non-healing wounds and infections, with a demonstrated care that fosters healing… right in the patient’s own home.
We specialize in serving homebound patients who may also be bed-bound or have difficulty in walking or moving around. As a result, immobility compression sores develop at pressure points on the body when the weight of an immobilized individual rests continuously on a firm surface, such as a mattress or wheel chair. Often these same patients are on oxygen or have high-risk medical conditions which makes it an even more challenging and stressful effort for them to travel to a doctor’s office for an appointment. Thus, the necessity for in home care and treatment.
Wounds that benefit from specialized wound care techniques include:
- Diabetic foot wounds and ulcers
- Post-surgical wounds
- Traumatic wounds caused by injury
- Arterial and vein stasis caused by lack of circulation
- Immobility pressure sores. (Bed sores from stillness)
We work closely with home health agencies to provide ongoing care and monitoring of patient’s wounds.

Our board-certified podiatrists treat foot pain, wounds, and more. Treatments may include but are not limited to treating conditions of the lower extremities which could hinder mobility.
- We will review each patients’ medical history to evaluate the condition of the feet, ankle or lower leg
- Carry out a diagnosis on the feet and lower legs through examination and medical tests
- Order physical therapy when deemed necessary
- Treat wounds of the lower extremities using various wound care modalities. This may include debridement to improve the healing potential
- Promote prevention, health & well being, the treatment and management of the foot and related problems, disability, deformity, and the pedal complications of chronic diseases for the elderly
- Prescribe and fit prosthetic appliances such as diabetic shoe inserts and evaluate for bracing if necessary
- Refer patients to other specialists for treatment, including conditions such as diabetes or arthritis
- Advise patients on ways to prevent future leg problems and increase speed of recovery
- Monitor the recovery progress of patients to determine the need for change in treatment

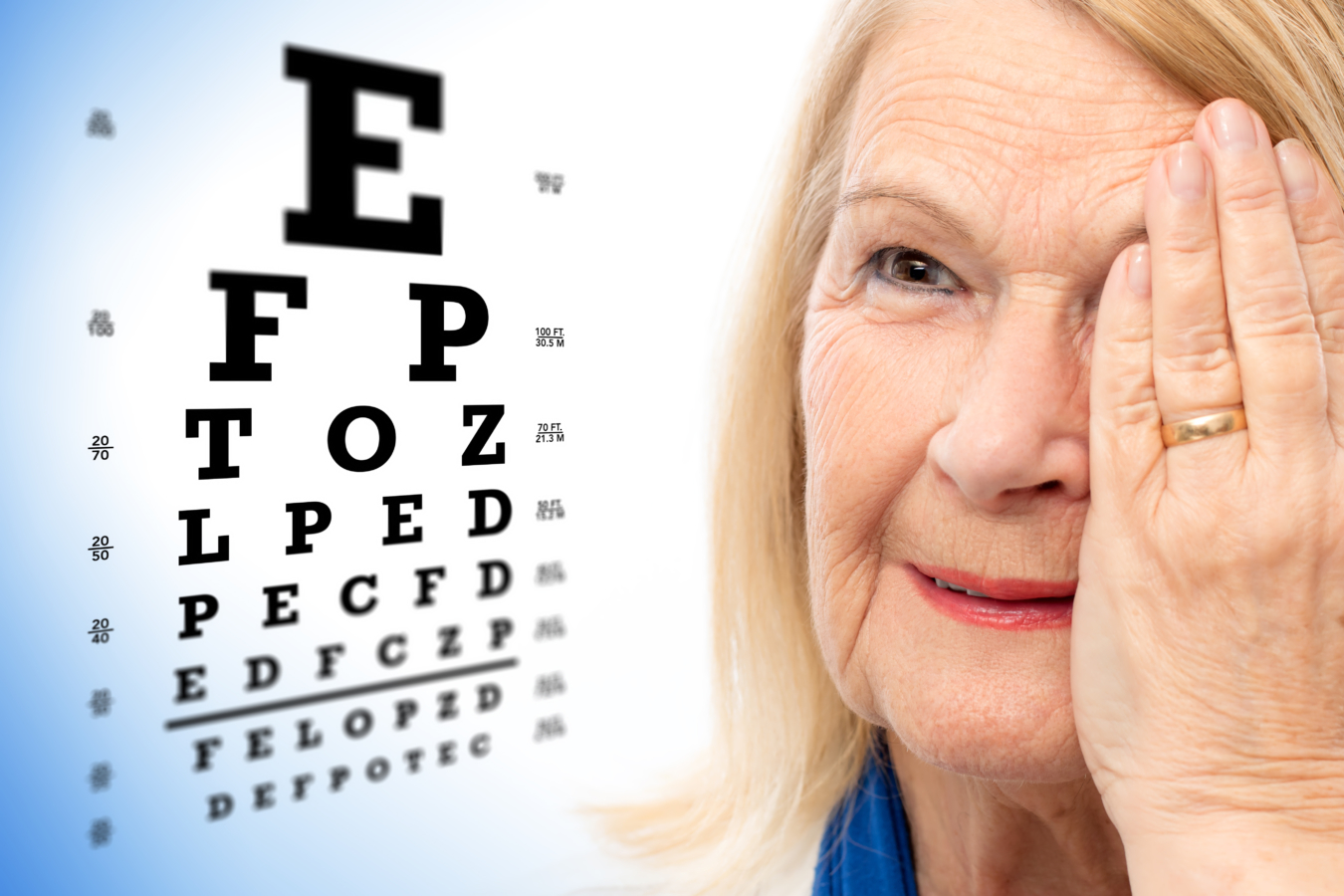
We know it’s not always easy to leave home to get the care you need for your eyes. Our optometrists bring state-of-the-art diagnostic eye equipment and technology to your home – making it much easier for you to get the vision care you need.
During a visit, your doctor will exam each eye for signs of serious issues such as glaucoma, cataracts, macular degeneration, and detached retinas, among other conditions.
Receiving regular eye exams regardless of the state of your vision can help detect serious eye problems at their earliest stages ─ when they are most treatable. During an eye exam, your doctor will observe and evaluate the health and condition of the blood vessels in your retina, which can be good indicators of the health of your blood vessels throughout the rest of your body.
- Comprehensive eye exams : This exam goes beyond a simple vision screening. A comprehensive eye exam includes a host of tests in order to do a complete evaluation of the health of your eyes and your vision.
- Annual retina exams : A retinal exam allows your doctor to evaluate the back of your eye, including the retina, the optic disk and the underlying layer of blood vessels that supply the retina.
- Eyeglass fittings : A prescription works best when your eyeglasses are properly fitted. Improper fitting may cause pinching, distorted vision, headaches, and even dizziness. Our doctors will make sure your prescription lenses and frames are working together for you.
- Diabetic eye exams : Diabetes does not have to lead to vision loss. Taking an active role in managing your diabetes can go a long way in curbing later complications. Regular eye exams, good management of your blood sugar and blood pressure, along with early intervention for vision problems can help prevent vision loss caused by diabetic retinopathy. Retinopathy is caused by damage to the blood vessels of the light-sensitive tissue at the back of your eye.
- Refractions: This test is given as part of your routine eye examination. It is often referred to as a vision test. This test assists your eye doctor in measuring you for the exact lens prescription you will need.
- Eye injuries: Eye trauma could be the result of a sudden blow to the eye. It may cause the eye to suddenly compress and retract which could cause damage to your eye and the surrounding tissue. Even if the injury may seem minor, all eye injuries should be furthered examined by a doctor for possible more serious and underlying injuries.
- Eye infections: The most common eye infection is conjunctivitis, also known as pink-eye. An eye infection can happen in almost any part of your eye, including your eye lid, cornea and optic nerve. Symptoms of eye infections may include redness, itching, swelling, discharge, pain, or problems with vision. Always consult with your doctor before treating, as recommended actions are contingent on the cause of the infection.
- Low-vision exams: A low vision exam is different from a normal eye exam. This functional-vision assessment determines how specific visual impairments affects your ability to perform everyday activities. The exam’s results assist your doctor in prescribing management tools and medications to better enhance and manage your remaining vision.
Pain management is the process of providing medical care that alleviates or reduces pain. Pain management is a subspecialty of general medicine employing an interdisciplinary approach to ease the suffering and improve the quality of life of those living with chronic pain by using a combination of pain medications, joint and muscles injections, and physical therapy techniques.
A pain management specialist is a provider with advanced training in diagnosing and treating pain. Our pain management specialists treat pain stemming from a variety of different causes, whether it’s neuropathic pain or headache, or the result of injury, a surgical procedure, cancer or another illness.

Palliative care is an approach to the holistic care of patients, including family and caregivers, to improve the quality of their lives after the diagnosis of a chronic debilitating disease or life-limiting illness that may cause a host of complaints.
Palliative care can begin at diagnosis and continue to be offered while the patient is continuing active treatment through different phases of their life limiting condition. Palliative care is for any patient with a chronic illness who is experiencing a decreased quality of life because of symptoms related to their illness or treatment, like renal dialysis, oxygen therapy or chemotherapy. The care is provided by a specially-trained team of doctors, nurse practitioners, physician assistants, and other specialists who work together to provide an extra layer of support to the patient and their caregivers.
Palliative care can help in symptom control including not only pain, but nausea, weakness, shortness of breath, fatigue and weight loss at any time during their diseases, not only at the end of life.

Mobile Physician Services, Inc. Corporate Headquarters 6804 Cecelia Drive New Port Richey, FL 34653
- Assisted Living Facilities
- FAQs | Medical housecall practice questions
- Health Plans
- Mobile Physician Services News Blog
- Patients and MPS
- Privacy Policy & Notices
Latest Blog
- Insomnia – Signs, Symptoms, and Complications February 15, 2023 - 06:58
- How do you know blood donations are safe? January 3, 2023 - 11:54
- Be Prepared to Stay Safe and Healthy in Winter December 13, 2022 - 12:51
- High Blood Pressure – Signs, Symptoms, and Complications November 17, 2022 - 08:38
In Home Medical Senior Care Services | Landmark Health
- Patient or Caregiver
- Community Provider
Are you a new Landmark patient?
Burn-out is real. landmark is different..

Living with chronic health conditions? We can help.
Our providers and care teams come to you, bringing care through house call visits. This in-home medical care is designed around understanding your health needs and goals. We work with you and your regular doctors to help you stay well and stay home.
House calls and video visits in 37 states.
Landmark partners with health plans to bring medical, behavioral health, and palliative care, along with social services, to patients in communities across the U.S. Our mobile providers visit patients in their homes through in-person house calls and telemedicine visits over video and phone.
We are the future of health care.
Landmark is one of the nation’s largest healthcare companies focused on in-home care of complex, chronic patients. Our physician-led provider groups support collaborative ties between community-based organizations, primary care providers, specialists and patients and their families.
patients nationally for which Landmark bears risk
reduction in hospital admissions
reduction in mortality

Discover the benefits.
- For Patients + Caregivers
- For Community Providers
- For Partners
Health care in your home
Old-fashioned house calls by medical doctors, nurse practitioners and physician assistants bring modern medicine to you. Feel better and stay well at home.
Covered by your health plan
The Landmark program works with health plans to improve access to care for patients with multiple chronic conditions. Landmark’s team-based care is available often at no cost to you.
Keep your current doctors
Landmark coordinates its care with your primary care provider, specialists and other community resources. Landmark provides added support to those who need it most.
Available 24 / 7
Our provider-staffed call center answers any time of the day or night. We also provide urgent visits to help you avoid unnecessary trips to the emergency room.
No waiting room
With Landmark house calls, you won’t need transportation to clinics and hospitals, and you avoid waiting rooms and exposure to germs.
Reduced stress
Patients and caregivers enjoy peace of mind with Landmark support. Landmark cares for the whole patient.
Landmark house calls put patients at the center of health care.
Collaborative care for complex patients.
Landmark’s community-based mobile providers bring coordinated care to patients with multiple chronic health conditions. We augment your care in the patient’s home.
Covered by health plans
The Landmark program is included in eligible patients’ health plans to improve care coordination and healthcare access for home-limited patients.
You remain the primary care provider
Landmark care is coordinated directly with you. Our providers reinforce your care plan in the home through physician-led interdisciplinary care teams.
Access our interdisciplinary team
Landmark’s interdisciplinary care team is available to you and your patients, including behavioral health specialists, social workers, palliative care specialists, nurse care managers and pharmacists.
Reduce administrative burden
We can help your highest acuity patients by managing post-acute care, home health orders, face-to-face encounters, and more.
24 / 7 availability
You can reach us any time, including weekends and holidays. We do urgent home visits to intervene if your patient experiences a chronic disease exacerbation.
Landmark supports your patients with complex health and social needs.
Chronic care management.
We’re one of the nations’ leading risk-bearing medical groups. We focus on giving your most complex members care when they need it, right in their home.
Over 250,000 patients across the country
We bear risk for over 250,000 complex, chronic patients, spanning Medicare Advantage, Medicaid, Dual, and Commercial, populations.
Behavioral, social and palliative care
Our team of multidisciplinary clinicians may include behavioral health specialists, palliative care practitioners, social workers, nurse care managers, dietitians and pharmacists.
Urgent in-home visits
One in four of our home visits is urgent. We bring medical care to your members when they need it, to avoid unnecessary emergency room trips and hospitalizations.
Built-for-purpose infrastructure
Our technology platform is designed specifically to support the medically vulnerable, clinically complex population.
Meaningful outcomes
Landmark commonly helps health plans achieve 4- and 5-star performance on Medicare STARS clinical quality of care, while caring for the most complex patients.
Landmark provides care for complex, chronic patients to positively impact access, satisfaction, outcomes and cost.
Joan was very helpful. It was nice getting to know her. How Landmark can help me
They came same day and were excellent!
Very much appreciated for the attention of my account
Practice health care the way you always wanted — with those who need it most.
Expert insights.

Prioritizing Mental Health as a Universal Human Right
By: Neltada Charlemagne, DNP, APRN, PMHNP-BC, PHN, BHC

Outsmart Unplanned Medical Costs: 10 Steps for Managing the Unexpected
Older adults can safeguard themselves from the physical, mental and emotional toll of unexpected medical costs.

Optum Care Network – Monarch and Landmark Health bring care to you at home.
Optum Care Network – Monarch has teamed up with Landmark to deliver in-home medical care to members with multiple chronic conditions.
Have questions about Landmark? We’d love to hear from you.
- Healthcare Services
- Find a Doctor
- Patient Portal
- Research and Education

Your recent searches
- Find a Location
- Nursing Careers
- Physical Therapy Careers
- Medical Education
- Research & Innovation
- Pay My Bill
- Billing & Insurance Questions
- For Healthcare Professionals
- News & Publications
- Classes & Events
- Philanthropy
House Call Program - MedStar Total Elder Care
Browse this page
Promoting the health and dignity of frail elders
Many elders struggle with disability and severe chronic illness and have difficulty getting to the doctor’s office. As a result, their health may suffer and lead to unnecessary ER visits, hospitalization, or nursing home care. In 1999, recognizing the needs of such elders and their families, we created the MedStar House Call program - MedStar Total Elder Care to provide full medical and social services that help elders remain in their homes with dignity. These teams now serve both Washington, D.C., and Baltimore, MD.
The MedStar House Call Program - MedStar Total Elder Care is nationally recognized for the quality and outcomes of our care. We serve patients at home with a team of geriatricians, nurse practitioners (NPs), social workers, office nurses, and coordinators. We make routine and urgent house calls (in-person or via telehealth with video or audio-only phone visits). Our medical staff is also available by phone 24/7 for urgent issues. We provide access to state-of-the-art hospital and specialty care. Additionally, our physician team follows our patients if and when they are admitted to the MedStar Washington Hospital Center.
The House Call program serves our neighbors in Washington, D.C., and Baltimore.
Medstar house call program .
(operating under MedStar Total Elder Care, LLC)

Our program services
Medical house calls and primary care by doctors and nurse practitioners with expertise in the care of older adults
Counseling and caregiver support by social workers and team staff
We offer tests and treatments at-home, and at the hospital as needed
Home delivery of most medications and equipment
Coordination of specialist care at MedStar Washington or MedStar Good Samaritan
Coordination of home nursing, rehab therapy, and hospice
Coordination of support services such as home aides and legal assistance
On-call physicians: 24 hours a day, 7 days a week (by phone)
Mobile electronic health record (EHR)
D.C. Neighborhood only – Case management for Medicaid Elderly Persons with Disabilities (EPD) Waiver
Hospital care and specialists
Our team coordinates emergency, hospital, and specialty care at MedStar Washington and MedStar Good Samaritan. Patients may keep their previous specialist doctors; we work with them as needed. We refer to MedStar Good Samaritan, MedStar Washington, for home-based podiatry or other new specialist care. If House Call patients require hospitalization, and 911 is not needed, our team can arrange transportation and admission to MedStar Good Samaritan or MedStar Washington when beds are available.
Social work services
Our dedicated team of social workers provides:
Psychosocial assessment
Care Coordination
Development of an individual treatment plan
Information and referral to community resources and supports
Caregiver education, support, and counseling
Advocacy to connect with other service networks and legal counseling
Crisis intervention
Assistance with identifying alternative living arrangements, as needed
Eligibility
Enrollment and insurance.
To qualify for the MedStar House Call Program, patients must:
Be 65 years or older and have difficulty getting to the doctor’s office
Have Medicare, Medicaid, or another participating insurance plan
Stop seeing their previous primary doctor and agree to have us take on that role following the first visit
Live in a qualifying ZIP code
Our office is open 8:30 a.m. to 4:30 p.m., Monday - Friday.
When calling about new patient enrollment, please have the following information:
Patient's name, address, telephone number
Patient's date of birth and social security number
Patient's next of kin and emergency contact information
Patient's health insurance information (including type and group number)
Patient's current medical conditions and concerns
Ability to retrieve patient's recent medical records
Baltimore neighbors, print and complete our Intake Questionnaire form
As in most doctor's offices, your main health insurance (such as Medicare) covers 80 percent of House Call visit fees, and any secondary insurance covers the other 20 percent. The patients who do not have any secondary insurance are responsible for the 20 percent co-pay.
Qualifying ZIP codes
View the map below to check if you live in a qualifying ZIP code. Call our Washington, D.C., or Baltimore location to confirm MedStar House Call Program eligibility at your exact address.
Washington, D.C.,
View our brochures
Baltimore region brochure
Washington, D.C., region brochure
Washington, D.C., region team - 202-877-0570
Physicians Eric De Jonge, MD, – Section Director Guy (Binny) Chang, MD Nurse Practitioners Nancy Sassa, CRNP - Chief Alexandra (Caitlin) Geary, CRNP Michelle Sullivan, CRNP Office Nurse Kendel Ogbeab, RN Social Workers Gretchen Nordstrom, LICSW - Chief Kellie Jones, LICSW Ruth Shea, LICSW Operations Manager Isi Koroma Care Coordinators LaWanda Holeman Sandra Mills Carrie Carmon Yvette Williams
Baltimore region team – 443-444-6100
Physicians George Taler, MD Sharareh Badri, MD Nurse Practitioner Dorothy Were, CRNP Adama Panda, CRNP Nurse Nerland Dimanche, RN, MSN Social Worker Marina Nellius, LMSW Operations Director Shereen Greene, MBA Care Coordinator Taurshica Lee
Operational support
Executive Director George Hennawai, MD AVP Operations Julie Beecher, MS, MPH
Baltimore Neighborhood
To learn more about our services in the Baltimore region, call us today.at 443-444-6100.
Washington, D.C., Neighborhood
To learn more about our services in the Washington, D.C., region, call us today at 202-877-0570
Related services

Look out for your health
A UnitedHealthcare® HouseCalls visit is a no-cost, yearly health check-in that can make a big difference.
Call 1-866-799-5895 ,
TTY 711, to schedule your visit.
HouseCalls brings yearly check-in care
To you at home.
Connect for up to a full hour of 1-on-1 time with a licensed health care practitioner. Every visit includes a physical, tailored recommendations on health care screenings and plenty of time to ask questions that matter to you.
After your visit, HouseCalls connects with your primary care provider (PCP) to help keep them informed about your health. It's a great way to feel confident knowing an extra set of eyes is looking out for you between regular PCP visits.
What is a HouseCalls visit?
[Text On Screen – SAY HELLO TO HOUSE CALLS]
Say hello to HouseCalls.
[Text On Screen- PAID ACTOR PORTRAYAL.]
HouseCalls is our way of looking out for your health, so you can focus on your future. Here’s what it’s all about.
[Text On Screen – HERE’S WHAT IT’S ALL ABOUT]
Once a year, a licensed health care practitioner can come to your home to spend up to an hour with you on your health and wellness.
[Text On Screen- EASY, CONVENIENT, INFORMATIVE]
It's designed to be easy, convenient and informative.
[Text On Screen- HEAD-TO-TOE EXAM]
[Text On Screen- IMPORTANT HEALTH SCREENINGS]
[Text On Screen- HEALTH GOALS DISCUSSION]
You'll get a head-to-toe exam, important health screenings and plenty of time to talk about your health goals.
We'll also provide guidance on managing your health and if you need it, give you referrals for other health plan resources and services.
HouseCalls is a great way to stay on top of your health between regular doctor's visits.
At the end of your visit, you'll get a personalized checklist so you can feel more confident in what to discuss with your regular doctor.
[Text On Screen- COST? NO EXTRA COST TO YOU]
[Text On Screen- INCLUDED IN YOUR HEALTH PLAN]
If you're wondering how much all of this is going to cost, the best part is, there is no extra cost to you. It's included in your health plan.
[Text On Screen- HOUSECALLS VIDEO VISITS ARE NOT AVAILABLE WITH ALL PLANS.]
A HouseCalls visit takes place in the comfort of your own home or by video if you prefer.
So, say hello to HouseCalls and invite us in for a visit today.
[Text On Screen – SAY HELLO TO HOUSE CALLS TODAY]
Access one of the most popular UnitedHealthcare offerings, at no cost to you
Schedule your visit
Call 1-866-799-5895 , TTY 711
Monday–Friday, 8 a.m.–8:30 p.m. ET
Your in-home health check-in
- Up to a full hour with a licensed health care practitioner
- Ask the questions that matter to you and get valuable health tips
- No cost — it's included in your health plan
Get rewarded
Meet your friendly housecalls medical staff.

Just like the professionals you see in your regular doctor’s office, our licensed health care practitioners may be nurse practitioners, physician assistants or medical doctors. They’re state licensed and maintain national certification.
We perform background checks on these professionals to provide additional peace of mind for our members. Your loved ones, caregivers or friends are welcome to be present during the visit — it’s up to you.
Ready to open the door to better health?
Getting ready for your housecalls appointment, tips to help you prepare: .
- Wear shoes that are easily removed to have your feet checked
- Make a list of upcoming appointments with your PCP and specialists
- Make sure all of your medications, both prescription and over-the-counter vitamins and supplements, are in their original bottles for our review
- If you record blood pressure readings, please have your results available for review
- If you have diabetes, please have your blood glucose meter handy
- Make a list of questions and concerns you’d like to discuss
During your appointment
- You'll have up to a full hour of 1-on-1 time with your health care practitioner for a physical, select lab tests, health screenings and more
- A HouseCalls visit can be completed while sitting at your kitchen table or in the living room, and you can use the time to ask any health-related questions
- The visit is tailored to your individual needs, so screenings and conversation topics can vary
After your appointment
Less travel time. more face time..
Think of HouseCalls as an extra layer of care — valuable 1-on-1 time you don't always get in the doctor's office. And it's tailored to your individual needs.
Schedule today
To secure your spot, call us at 1-866-799-5895 , TTY 711
Have a question?
Find answers to frequently asked questions.
View FAQ's >
If you have a specific question about your upcoming appointment or need to reschedule, call us at 1-866-799-5895, TTY 711 , Monday–Friday, 8 a.m.–8:30 p.m. ET
We're here to help.

House Call Doctor Visits Make Life Easier for Seniors and Caregivers

Important: This is an informational article to explain how house call doctor visits can benefit seniors. DailyCaring isn’t a medical organization, we aren’t medical professionals, and we aren’t affiliated with any healthcare organizations. We aren’t qualified to respond to any medical questions.
House call doctor visits benefit older adults and caregivers
Getting your older adult to the doctor’s office for an appointment can be difficult or sometimes impossible.
Whether they’re frail, can’t walk on their own, or have Alzheimer’s or dementia , getting out of the house is hard on both of you. Going to a doctor’s office can also expose seniors to germs or harsh weather.
We explain what a house call doctor is, what type of insurance they accept, how to find one, and what to look for in terms of services.
What is a house call doctor?
Today, many doctors are bringing back the old practice of visiting patients in their homes. With house calls, older adults don’t have to go through the stress and difficulty of getting to the doctor’s office. And neither do you.
Another bonus is that these doctors usually spend more time with patients. You won’t have to fit all your questions into a 15 minute visit.
Do they accept Medicare?
Yes, many house call doctors accept Medicare , private insurance, and sometimes Medicaid . It usually costs the same as a regular office visit.
But every house call doctor is different, so make sure you understand their fees and accepted insurance plans before making an appointment.
How to find a house call doctor
Some large health care systems like Kaiser Permanente or the VA have programs that include home visits by doctors and nurses. For example, Kaiser’s home-based palliative care program includes house calls.
Even your older adult isn’t part of a large health network, it’s worthwhile to ask your older adult’s doctor if they have home doctor visit programs.
The American Academy of Home Care Medicine’s provider directory is another way to locate a house call doctor in your area.
You can also use Google to search for “house call doctor” + your city or county or “home doctor visit” + your city or county (don’t include the quotation marks).
What to look for in a house call doctor
Before booking an appointment, make sure you understand the doctor’s services, fees, and billing.
Questions to ask:
- Do you specialize in treating seniors, people with Alzheimer’s or dementia , or those with multiple chronic conditions ?
- Do you accept Medicare , Medicaid , or my older adult’s private insurance plan?
- If we want, can we also keep my older adult’s primary care doctor?
- Will you communicate with my older adult’s existing doctors and specialists so their care is coordinated?
Examples of house call doctor private practices
We want to be clear that we’re not recommending any specific home doctor services or companies and aren’t affiliated with any of these businesses. These are examples to give you an idea of what a house call doctor looks like and the type of services that are typically offered.
Examples of what a house call doctor looks like:
- Visiting Physicians Association (VPA)
- Bay Area House Call Physicians
- Kindred House Calls
Recommended for you:
- 4 Expert Tips for Managing Multiple Chronic Health Conditions in Seniors
7 Tips for Helping Seniors at the Doctor: Being a Health Advocate
- Should Seniors See a Geriatrician?
By DailyCaring Editorial Team Image: Now It Counts
This article wasn’t sponsored and doesn’t contain affiliate links. For more information, see How We Make Money .
- Share Article on:
Related Articles

4 Common Eye Diseases That Cause Blindness in Aging Eyes

Improve Seniors’ Doctor Visits with 3 Communication Tips

Why Seniors Need a Health Advocate: 7 Health Benefits
18 comments, tony carrancho.
My parent s lives in [redacted for privacy]. How do i get started locating a house call doctor. I am pretty sure there insurance covers this. Thank you. TONY
DailyCaring
We hope the tips and suggestions in the article above will help you find a house call doctor in your parents’ local area.
Susan Quercio
My 95 year old father has a deep cough and he is disoriented. Temp 99 degrees.
Please contact your father’s doctor immediately or the local hospital to find out how to safely get him examined by a doctor (to reduce risk of exposure to Covid-19).
DailyCaring isn’t a medical organization, we aren’t medical professionals, and we aren’t affiliated with any healthcare organizations.
Ruby m VanNostern
I live in [redacted for privacy] and need a doctor visit in home.
This article includes suggestions for how you can find house call doctor services in your area. At DailyCaring, we aren’t doctors and don’t provide any medical services. We hope you’re able to find a great house call doctor in your area.
Stewart Goldman
need Doctor for a home visit Andrews N.C.
Joseph Artusa
I need a doctor
Linda Williams
I was released from the hospital on Thursday after 5 days.I am not able to go to Dr office but most definitely need to be checked.Still having breaking problems and am very week.I have severe asthma and blood pressure was running very high from so much steroids.Could I possibly get help.Thanks so much.
I’m so sorry to hear that you’re not feeling well. Since you’re noticing some issues with your recovery, it’s essential to call your primary doctor immediately. Since they’re the ones who have been treating you and are familiar with your recent hospitalization, they’re the best people to advise you on what you need. If you need help getting to your doctor’s office, you may want to contact your local Area Agency on Aging or a ride sharing service. Or, use the tips in this article to search for a doctor in your area who makes house calls.
Here are some articles that may be helpful: — 8 Ridesharing Services for Seniors https://dailycaring.com/8-ridesharing-services-for-seniors/ — 6 Affordable Senior Transportation Options https://dailycaring.com/6-affordable-senior-transportation-options/ — Local Community Resources for Seniors and Caregivers: Area Agency on Aging (to connect you with local organizations that may be able to help) https://dailycaring.com/local-community-resources-for-seniors-and-caregivers-area-agency-on-aging/ — 4 Ways to Know If Seniors Need to Return to the Hospital https://dailycaring.com/4-ways-to-know-if-seniors-need-to-return-to-the-hospital/
(DailyCaring doesn’t provide any services and isn’t affiliated with any medical providers.)
What areas do you service?
This article explains that house call doctor services are available and could help senior and caregivers. We also share suggestions for finding one in your area, but we do not provide any services ourselves. I hope you’re able to find a great local house call doctor!
What areas do you service
This article includes suggestions for finding house call doctor services in your area. We at DailyCaring aren’t doctors and don’t provide any medical services. I hope you’re able to find a great house call doctor in your area.
need a home care doctor
I hope the information above helps you find a great home care doctor in your area.
Leave a Reply Click here to cancel reply.
Cancel reply.

Interest in home-based primary care is growing as payments increase, technology improves, and the population ages.
THOMAS CORNWELL, MD, FAAFP, AND BRIANNA PLENCNER, CPC, CPMA
Fam Pract Manag. 2021;28(3):22A-22G
Author disclosures: no relevant financial affiliations disclosed.

The United States is experiencing a resurgence of home-based primary care (HBPC) after a rapid decline during the last century. Steady growth in physician house calls started with the doubling of house call payment rates in 1998 and a doubling and tripling of domiciliary payment rates in 2006. Other factors include the aging of our society; increased technology that allows X-rays, ultrasounds, electrocardiograms, and lab tests to be done in the home; and new CPT payments that target complex patients such as those who need chronic care management, remote patient monitoring, and advance care planning.
HBPC's value has been demonstrated through improved outcomes and reduced costs for complex patients. Medicare's Independence at Home house call program improved outcomes and decreased costs by $2,000 per patient per year, and the U.S. Department of Veterans Affairs' HBPC program reduced hospital days by 60%, readmissions by 21%, and nursing home use by an astounding 89%. 1 The data generated support for HBPC on Capitol Hill, at the Centers for Medicare & Medicaid Services (CMS), from Medicare Advantage plans, and from investors.
More recently, the COVID-19 public health emergency (PHE) brought virtual care into patients' homes in a remarkable way. But telehealth is beyond the scope of this article. Currently, Congressional action is needed to enable telehealth to continue in the home after the PHE.
Still, family physicians can take advantage of the growing support for HBPC. This article outlines steps for adding house calls to an office-based practice. Reasons to do so include the following:
Continuity of care for patients who have difficulty getting to the office, ensuring they are not lost in the system.
Better quality of care, increased time with patients, and improved doctor-patient-caregiver relationships, resulting in increased patient satisfaction scores, increased referrals from family members, increased physician satisfaction, and decreased burnout.
Improved end-of-life care, fulfilling the wishes of the majority of patients who desire to be at home surrounded by loved ones at the time of death.
Improved value-based care performance from superior risk capture, reducing gaps in care, improving quality, and lowering the total cost of care.
Increased reimbursement for complex patient care.
Increased payment, improved technology, and the aging of the population have all contributed to steady growth in physician house calls.
House calls have been shown to improve patient outcomes and decrease costs by $2,000 per patient per year.
When adding house calls to an office-based practice, three ingredients necessary to success are patients, processes, and payments.
THREE INGREDIENTS FOR SUCCESS
A successful house call program requires three ingredients: patients, processes, and payments.
Patients . There is some flexibility in choosing which patients should receive home visits. Medicare has never required house call patients to meet the homebound definition that it requires for receiving skilled nursing and therapy services in the home. But until January 2019, Medicare required additional documentation of medical necessity for every home visit, describing why a house call was needed in “lieu of an office visit.” The 2019 Medicare Physician Fee Schedule Final Rule removed this requirement as of Jan. 1, 2019.
Still, most house call programs focus on complex patients who have difficulty getting to the office. Some practices use data analytics to identify and target high-risk patients. Common candidates for HBPC include the following:
Frail older adults with multiple (often five or more) chronic conditions and deficiencies in activities of daily living (ADL).
Younger homebound patients, usually with one principal neuromuscular condition such as multiple sclerosis, amyotrophic lateral sclerosis, or cervical spine injuries (some on ventilators).
Patients with high-risk diagnoses like congestive heart failure and chronic obstructive pulmonary disease.
Patients with high hospital and emergency department (ED) utilization in the past six to 12 months.
Patients with hierarchical condition category (HCC) scores greater than 2.0.
Another group well-suited for HBPC is post-acute, transitional care management (TCM) patients. During the high-risk transition period, these patients benefit from a short course of HBPC that reduces complications and readmissions. Payments for TCM (CPT codes 99495 and 99496) have increased more than 20% over the past two years. CMS has also unbundled virtually all care management services that previously were not billable within the 30-day TCM period. These include chronic care management, care plan oversight for home health and hospice services, face-to-face and non-face-to-face prolonged services, and more when reasonable and necessary. Numerous hospitals are partnering with HBPC programs to reduce their readmission rates.
Logistical considerations for choosing house call patients include the following:
Geography: A geographic radius should be determined for home visits based on driving time (e.g., no more than 20 minutes from the physician's office or home). Telehealth, at least while it is allowed under the PHE, is an excellent way to provide care for more distant patients.
Established vs. new house call patients: Some practices may decide to limit house calls to established patients. But if you desire to grow a house call practice, the largest referral source tends to be home health agencies, followed by hospital and rehabilitation discharge planners, social services, and word of mouth.
Place of service: Practices may offer house calls to patients at home or in domiciliary settings (e.g., assisted living facilities or group homes). There are economies of scale in domiciliary care because you can see multiple patients in the same location on the same day, and the payments are roughly the same as home visits.
Capacity: A good way to start is with a half day or one full day of house calls per week, and then increase that time as volume demands.
Operational processes . Practices will need to address operational issues such as scheduling, visit preparation, staffing, supply management, and safety.
Efficient scheduling is critical to reduce travel time, and can be achieved through the following steps:
Schedule patients in close proximity. This is facilitated by assigning days to specific geographic areas and using mapping/routing software.
Map and route patients one to two days before the visit, notify patients or caregivers of the approximate visit time (usually providing a two- to four-hour window or simply indicating morning or afternoon), and verify the address (sometimes the address on file is for mailing the bill and is not the patient's physical location).
Use electronic health record flags/alerts for travel notes, communication preferences, and patient preferences. Special visit instructions should be noted on the schedule (e.g., “call daughter ahead,” “go in back door,” or “dogs need to be secured”).
Call when en route to the visit so the patient is ready and has medication out.
Give patients follow-up timeframes (e.g., four to six weeks or two to three months) instead of exact dates to allow the schedule to be fluid, to facilitate scheduling patients within the same geographic area, and to enable last-minute schedule changes based on patient acuity.
Make sure that clerical tasks are done before the visit, including obtaining signed forms and medical records (e.g., HIPAA forms, consent for treatment, or medical history forms) when possible.
Staffing considerations include the following:
Medical assistant (MA) support: Many physicians choose to do house calls solo, mainly because of the cost of including an MA. But having an MA route and drive saves the physician significant time and allows charting and phone calls while in transit. During the house call, the MA can check vitals, do immunizations, draw blood, assist with medication reconciliation and refills, get forms signed, review gaps in care, do assessments (such as PHQ-2/9, Mini-Cog, nutritional, and safety surveys), assist with wound care, help with orders (e.g., durable medical equipment, home health, and hospice), and increase safety. Making one extra house call a day covers the MA's cost, and the time savings more than allow for that one extra call.
Advanced practice provider visits: Nurse practitioner and physician assistant house calls have dramatically increased over the past decade; they are now the largest provider group making house calls. This is a cost-effective model with good outcomes, when provided with physician support.
Supply management involves keeping track of what supplies are used and restocking at the end of the day. Unlike in the office, you cannot walk down the hall to a storage closet if you run out of something during a home visit. Ensure equipment is sanitized and charged. Have a container in the car for standard supplies that are not damaged by temperature extremes (e.g., wound care items). Review schedules in advance to identify any special supply needs (e.g., a cooler for storing and transporting drawn labs).
Safety concerns include higher crime areas and homes with potentially dangerous patients, caregivers, or pets. Safety and emergency plans should include the following:
Handling car accidents and other incidents such as falls with injuries, needle-sticks, etc.
Handling pets in the home. Some HBPC programs require pets be caged during visits. Others leave it to the discretion of the pet owner and the physician.
Sitting on a hard surface chair to avoid unseen soiling, bedbugs, etc.
Washing or sanitizing hands before, during, and after the visit.
Noting safety issues on the schedule, including a history of multi-resistant organisms, bed bugs, or firearms (which should always be locked). During the PHE, conduct COVID-19 screening questions when notifying the patient of the appointment time and again when en route to the patient's home.
Seeing patients in higher crime areas during daylight hours. There is debate among HBPC clinicians about wearing clothing that identifies them as health care workers, such as a lab jacket. Some think it's better to avoid drawing attention to themselves. Others believe it is good for people to know they are there to provide care. Determine which is more comfortable for you.
Turning on smartphone location service apps, which enable the office to know the physician's location and allow the physician to quickly call in an emergency through a simple touch or verbal command.
Planning for inclement weather or natural disasters. Patients may need to be rescheduled.
Exiting the premises if the physician feels unsafe. Consider having a code word to alert staff if you need assistance.
Clinical processes . The Institute for Healthcare Improvement's Age-Friendly Health Systems' "4Ms" framework is an excellent approach to complex house call patients. The 4Ms are what matters , medication , mentation , and mobility. What matters is determined through conversations with patients about their goals of care, leading to advance directives. The home is an ideal setting to have these conversations. It is also the best place to reconcile and optimize medications , which often includes deprescribing in frail older adults. Mentation refers to diagnosing and managing dementia, depression, and delirium. Mobility focuses on ADLs, maintaining function, gait, safety, and independence. (See “ Common assessments in HBPC .”)
A house call's main clinical difference is that the exam room is in the patient's home. This requires bringing the office to the patient. The table below shows the modern-day “black bag.” The supply list will vary somewhat depending on what the physician is comfortable doing in the home. The home also provides tremendous information about the patient, including diet, safety (are there grab bars, fall hazards, etc.), social determinants of health, and what matters to the patient (pictures, religious objects, etc.). It is important to be culturally sensitive in patients' homes, which is best accomplished by asking about patient and caregiver preferences.
It is wise to review charts the day before the home visit to see if fasting blood work or any unique supplies are needed, such as injections, immunizations, or gastrostomy tubes. It also helps to review charts for complex, new, and TCM patients ahead of the visit and start pre-charting. Extensive prep time (more than 30 minutes) can be billed using CPT codes for prolonged evaluation and management (E/M) services. (See “ Commonly used CPT codes in home-based primary care .”)
House call practices commonly have 20% to 25% mortality rates, so it is critical to discuss goals of care such as the patient's desired medical decision-maker if needed, level of hospital care, cardiopulmonary resuscitation (CPR), and end-of-life wishes (e.g., desired place of death, hospice services, and funeral arrangements). These advance care planning (ACP) discussions can be billed with CPT code 99497 if a minimum of 16 minutes is spent and the patient consents to the conversation voluntarily (be sure to note this in your documentation). These discussions often take place over several visits, and there is no limit on how often ACP can be billed. Copays are waived for ACP done during annual wellness visits, but co-pays will apply if performed with another service.
House call patients are best served by an interdisciplinary team providing a range of services, often virtually, including the following:
Ancillary service providers (mobile X-ray, ultrasound, and phlebotomy).
Home health and hospice (Medicare pays physicians for the certification and recertification of home health and care plan oversight if they spend 30 minutes in a calendar month overseeing home health or hospice).
Care coordination departments (such as ED or hospital discharge planning).
Durable medical equipment companies.
Community organizations (Area Agencies on Aging can assist with Meals on Wheels, utilities, home maintenance, etc.; other community organizations may provide behavioral health, private duty, or respite care; and websites such as findhelp.org by Aunt Bertha list resources by ZIP code).
Other professionals making house calls (audiologists, dentists, optometrists, podiatrists, etc.).
PAYMENT FOR HOUSE CALLS
Medicare fee-for-service (FFS) payments fund most house call programs. The 2021 changes in office outpatient E/M documentation requirements do not apply to home or domiciliary visit codes, so you are still required to use the 1995 or 1997 E/M documentation guidelines for these visits. Billing by time still requires that more than 50% of the visit be spent in counseling and/or coordination of care. (See “ Home and domiciliary E/M codes and payment rates .”) Other commonly used CPT codes in HBPC and their payment rates are listed in the table above. Most of these CPT codes are new in the past decade.
Value-based care (VBC) payments are fueling the growth of house calls. Payments can vary, from shared savings with only upside potential and no downside risk, to global capitation with full risk for all patient care. Three things are essential for success: 1) capturing risk scores for accurate payment, 2) improving quality and the patient experience and closing gaps in care, and 3) lowering costs principally by reducing acute care utilization. House calls do all three exceedingly well and lower acute-care usage more than any other intervention. For family practices involved in Accountable Care Organizations or other forms of VBC, house calls can significantly contribute to the bottom line.
American Academy of Family Physicians Home-based Primary Care Member Interest Group (AAFP members only)
Rerucha CM, Salinas R, Shook J, Duane M. House calls . Am Fam Physician . 2020;102(4):211–220.
Home Centered Care Institute
HCCIntelligence™ Resource Center
American Academy of Home Care Medicine
Cornwell T. House calls are reaching the tipping point — now we need the workforce. J Patient Cent Res Rev . 2019;6(3):188-191.
Continue Reading

More in FPM
More in pubmed.
Copyright © 2021 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

4 Benefits of House Calls for Primary Care Visits

When you're feeling unwell, the last thing you want to do is travel to the hospital or doctor's office. Usually, preparing for a doctor's appointment entails a lot, from scheduling time off work to waiting far too long in the waiting room for the doctor to see you.
House calls are a more convenient version of urgent care or a walk-in medical clinic appointment. You can avoid long lines and the possibility of being infected or infecting others, save time traveling, and avoid the discomfort of visiting the clinic when you are sick. For some patients, the house is a secure haven that might help with a more thorough examination.
In this article, we are going to go over 4 benefits of house calls for primary care visits. Read on to find out more.
1. They reduce waiting times
How many times have you arrived at a doctor's office on time just to be forced to wait? Imagine being able to see your doctor from the comfort of your own home, rather than having to wait in a packed waiting room. Waiting a long time to see a doctor might even aggravate or increase stress levels, making it difficult to accurately assess some tests, such as the correct blood pressure or heartbeat. Scheduling your appointment at home removes the need for this wait time and ensures better service. In addition, you are more likely to feel comfortable and can accurately describe your symptoms, which allows for a thorough diagnosis.
Young folks and parents with young children recognize that one significant advantage of house calls is convenience. House calls can eliminate the need to make an appointment later in the week or drive to an office and spend time in the waiting room waiting to be seen. The truth is very few of us enjoy going to the doctor's office, and there are now more reasons than ever to avoid it. With the outbreak of the COVID-19 pandemic, most of us are understandably anxious about being in close quarters with someone who may have contracted the virus or other illnesses such as the flu.
2. They ensure patient safety
Americans are becoming older, and by 2030, 70 million of them will be above the age of 65. A large proportion of this population is also housebound. Over a third of individuals aged 75 to 85 have difficulties walking a block. The health of the elderly and those who are critically ill can deteriorate at any time. They may require immediate medical treatment and care since failure to do so can result in life-threatening problems and diseases. That is where a house call doctor comes in.
House calls can be an incredibly convenient and safe option for the elderly because they are unable to walk to the clinic, especially when there is no transportation available. House calls also allow doctors to check in on patients who have limited mobility to see if they are taking their medications on a regular basis, eating well, and staying safe from accidents or falls.
3. They reduce expensive hospitalizations
Health-care spending in the United States is widely believed to be on course to exceed 20 percent of GDP — and the 5% of patients who are the most expensive to treat account for 50% of total healthcare expenditure. These individuals are often frail and elderly, suffering from a variety of chronic illnesses; many of them also have unmet behavioral and mental health needs.
One study discovered that a physician assistant home care program that included house calls lowered the 30-day readmission rate by 25%. Medication adjustment was the most common house call intervention. Primary care that is easily accessible and consistent may help prevent ED visits. House call visits can also provide follow-up until you are better, something that medical clinics and hospitals don't do.
4. They ensure more personalized care is provided
According to research conducted by the American Academy of Family Physicians , physicians might gain vital information about their patients during house calls. For example, doctors can check to make sure patients take their medications correctly, eat nutritiously, and aren't at an increased risk of accidents or falls by watching them do ordinary everyday tasks in their most familiar surroundings.
In-home care is more tailored than the majority of patients in a doctor's office or hospital and significantly reduces hospitalizations and emergency room visits. Numerous physicians see as many as twenty people per day, with each visit lasting barely a few minutes. Delivering care to the patient in their own home becomes substantially more personalized, where treatment is tailored to the medical demands of each patient. House calls can provide patients and their families peace of mind.
There is no doubt that a house call can have various benefits for patients. A house call can help reduce waiting times, reduce expensive hospitalizations, ensure patient safety, and offer a more personalized type of care. Aside from the advantages mentioned above, numerous on-demand medical house call services today use modern medical technology to deliver more comprehensive and convenient medical treatment and medical support.
Community Healthcare Partners is committed to providing the highest quality health care to our patients in Lincoln, Omaha, Fremont, and surrounding areas. Our nurse practitioners and physician assistants provide comprehensive care in the comfort of the patient's home. Our professionals assist patients in navigating the health care system, including referrals to specialists, coordination of hospital care, and follow-up treatment. As a result, patients and caregivers benefit from the peace of mind knowing that quality healthcare is only a phone call away. Care encompasses everything from mild ailments to significant, chronic conditions.
Read about our services to find out more, or get in touch today to arrange an appointment with one of our compassionate doctors.
22 Mar 2022
We earn a commission for products purchased through some links in this article.
Home visits and out-of-hours care
Many patients believe there is an automatic right to a home visit from a GP between 8am and 6.30pm, but this is not the case

Home visits
Many patients believe there is an automatic right to a home visit from a GP between 8am and 6.30pm, but this is not the case.
Doctors will always encourage people to come into the surgery because this is where the best care can be provided. Specialist equipment is there, tests can be carried out more easily and drugs issued if necessary.
GPs tend to visit a patient at home when:
- the patient is confined due to illness or disability
- urgent treatment can be given more quickly by visiting.
The one thing guaranteed to damage a doctor-patient relationship is to ask for a home visit when it's not medically necessary and then be out when the doctor arrives at your home.
In the time it takes to see one person at home, your GP can see between two and four patients at the surgery.
For this reason, if you request a home visit, your GP may call you back to find out more about your problem before deciding to come out.
Out-of-hours care
All doctors have an emergency service outside of normal surgery hours.
Most surgeries have an answering machine message that refers you to out-of-hours telephone numbers or the NHS Direct helpline.
The out-of-hours service is only for urgent medical problems that cannot wait until the next day to be treated.
It's usually based at a local medical centre or attached to a local hospital and is a co-operative manned by local GPs.
When you phone the out-of-hours service, a nurse or GP will take your details and ask you about your symptoms. You'll then be dealt with in one of three ways.
- You'll be given telephone advice.
- You'll be asked to come into the medical centre to see a doctor.
- A home visit will be arranged if you are too ill to leave your house.
If you're seen out of hours, your doctor will be informed of any consultation you've had with another doctor.
A&E (accident and emergency)
Sometimes called casualty departments, around 13 million people visit A&E every year.
A&E is designed to assess and treat people with serious injuries and those in need of emergency treatment. They are open 24 hours a day, 365 days of the year.
Typical reasons for going to A&E include:
- severe breathing problems
- chest pain and heart attacks
- severe bleeding
- major trauma
- head injuries
- lack of consciousness
- severe burns or scalds
- broken bones
- severe abdominal pain
- drug overdose.
Normal cuts, bruises and sprains aren't usually considered to be emergencies since these can usually be treated at home or by your GP.
If you're not sure if your problem is an emergency, call NHS Direct (details below) for advice on what to do.
A&E shouldn't be used as an alternative to your GP.
Walk-in centres
These deal with minor illnesses and injuries such as infections, cuts and fractures, emergency contraception, stomach upsets and burns.
Predominantly nurse led, most centres are open 365 days a year and are available to everyone.
You don't need to register or make an appointment, but some don't treat children so it's best to check this before you go.
Viewed as a complementary service to GP and A&E services, they're not designed for treating long-term conditions or immediately life-threatening problems.
The contact number of your nearest walk-in centre should be in your local phone book or via NHS 111.
NHS 111 is a service that you can call if you urgently need medical help or advice but it's not a life-threatening situation. Available 24 hours a day, 365 days a year, calls are free from landlines and mobile phones.
You can call for advice if you are feeling ill and you're not sure what to do. The NHS 111 service is staffed by a team of fully trained advisers, supported by experienced nurses and paramedics. They will ask you questions to assess your symptoms, then give you the healthcare advice you need or direct you straightaway to the local service that can help you best.
That could be A&E, an out-of-hours doctor, an urgent care centre or a walk-in centre, a community nurse, an emergency dentist or a late-opening chemist.
Where possible, the NHS 111 team will book you an appointment or transfer you directly to the people you need to speak to.
NHS 111 can also tell you where to find your nearest doctor, pharmacist or dentist.
Other people also read:
A to Z of professionals : there are lots of different people who work in NHS hospitals.
A to Z of hospital departments : there are many hospital departments.
NHS hospitals : choosing a hospital.
How to choose a GP : how do I find a surgery?
Getting the most out of a GP appointment : be prepared.
Last updated 01 .03.2016

Medical House Calls

Quality Care At Your Door
Say goodbye to the hassle of sitting in a crowded waiting room or struggling to make time in your busy schedule to see your doctor.
With medical house calls, you can see a medical provider stress-free in the comfort, convenience, and privacy of your home.
- Medical Evaluation
Hassle-Free Health Care

No wait times, no crowded waiting rooms

Easy online scheduling with same-day availability

Reduced risk of exposure to germs and viruses
House calls for urgent & primary care needs, urgent care house calls.
On-demand medical attention when you need it most without leaving your home.
Receive one-on-one attention with a licensed medical provider who will diagnose, treat and prescribe medications if need be.
Urgent Care House Calls are Ideal for:
- Cold & Flu
- Sore Throat
- Bronchitis
- Sinus Infection
- Ear Infection
- Urinary Tract Infection (UTI)
- Stomach Flu
- Food Poisoning
- Muscle or Joint Pain
- Cuts, Scrapes, & Burns
- Migraines & Headaches

Primary Care House Calls
Comprehensive primary care services in the comfort of your own home.
Ideal for those with busy lifestyles and who would prefer to see a medical provider in the privacy of their residence.
Primary Care House Calls are Ideal for:
- Annual Wellness Exam
- School, Sports, & Employment Physical Exams
- Nutrition, Fitness & Exercise Consultations
- Mental Health Consultations (Anxiety & Depression)
- Pre-Op Clearance
- Anti-Aging Solutions
- Preventative Medicine
- Chronic Disease Management
- Lab Testing & Blood Work
- Prescription Refills
- Referrals to Specialists
Hear From Our Clients
Each of our reviews is a testament to the warmth, professionalism, and personalized attention we bring to every appointment. Your health journey is our passion, and these stories inspire us to continue providing exceptional care.
Ready to book?
Returning customer? Click here to login
Email address (as your login)
Remember me
Lost your password?
- First Name *
- Last Name *
- Country * United States
- Address * Street Address Address Line 2 City ZIP Code
- State * State Arizona California Georgia Hawaii Idaho Illinois Massachusetts Michigan Minnesota Nevada New Jersey New York Texas Utah Wisconsin
- First Time Client
- Return Client
- Provider * Atlanta Austin Boise Boston Bronx & Westchester Brooklyn Central Coast Central New Jersey Chicago DEFAULT PROVIDER Detroit Hawaii - Oahu Inland Empire & Palm Springs Las Vegas Los Angeles Madison Manhattan Milwaukee Minneapolis North New Jersey Orange County Phoenix Queens & Nassau County Rockford Sacramento San Diego St. George Suffolk County Tucson Utah
- GA Service House Call
- Date of Birth * Month Day Year
- Preferred Date of Appointment * MM slash DD slash YYYY
- Preferred Appointment Time * Select Time 8:00 AM 8:30 AM 9:00 AM 9:30 AM 10:00 AM 10:30 AM 11:00 AM 11:30 AM 12:00 PM 12:30 PM 1:00 PM 1:30 PM 2:00 PM 2:30 PM 3:00 PM 3:30 PM 4:00 PM 4:30 PM 5:00 PM 5:30 PM 6:00 PM 6:30 PM 7:00 PM 7:30 PM 8:00 PM 8:30 PM 9:00 PM 9:30 PM
- Book in Date & Time Preference * To see the booking calendar, please enter a zip code above. Please be aware, we will make every effort to accommodate your requested time. Times are subject to change based on availability. A member of our dispatch team will work to confirm your appointment as soon as we receive your booking.
- Rapid Covid Antigen Test
- Rapid Strep Test
- Rapid Flu Test
- Rapid Urinalysis Test
- Ultrasound or X-Ray
- Echocardiogram
- Anti-Inflammatory
- Pain Blocker
- Anti-Nausea
- Super Immune Boost
- Myers Cocktail
- Mental Clarity (NAD)
- Energy (B12)
- Glow (Vitamin D)
- Beauty (Biotin)
- Fat Burner (Lipostat)
- Mental Clarity (50mg)
- Mental Clarity (100mg)
- Person added
- <span class="gform-field-label gfield_label_product">Automatic Group Discount</span> <span class="screen-reader-text">Quantity</span> $0.00
- Remove Person
- What is your house call regarding? * **Please do not provide any personal health info, only general info
- Order Summary Person 1 Subtotal: $0 Service Fee: $0 Lab Fee Total: $0 Automatic Group Discount : $0 Coupon Discount: $0 Total $0.00
- I agree to the Term of Service , Privacy Policy , Consent To Treat , and Cancellation Policy
- Cancellation Terms . Bookings are subject to a $50 cancellation fee.
- Sign-up for emails to get exclusive offers & be the first to know about new services!
- Sign up for texts. By checking this box, you agree to receive recurring automated promotional and personalized marketing text messages (e.g. cart reminders) from ConciergeMD at the cell number used when signing up. Consent is not a condition of any purchase. Reply HELP for help and STOP to cancel. Msg frequency varies. Msg & data rates may apply. View Terms & Privacy .
House Call FAQs
Do you offer same-day appointments how long will it take for a provider to arrive at my location.
Yes, we understand the importance of prompt healthcare. We make every effort to offer same-day appointments whenever possible. We do our best to arrive within one to two hours of your booking.
Do we offer house calls on weekends or evenings?
Yes, we understand that your schedule may be busy during weekdays. We offer flexible scheduling, including weekends and evenings and try our very best to accommodate your preferred times. Our medical house call services are available seven days a week. We’re here to provide you with personalized healthcare when it’s most convenient for you.
Do you provide service to my place of business or hotel?
Yes, ConciergeMD is an at-your-door service. We will come to your office, home or hotel 7 days a week, 365 days a year.
What should I expect during a House Call visit?
During a house call visit, you’ll meet with the same types of professionals you see in a doctor’s office — a licensed health care practitioner. After introductions, your provider will perform a thorough history and physical examination appropriate for your specific complaints and will then recommend the appropriate treatment options. After all of your questions are answered, instructions are given, your provider will depart.
Who will come to my home for the House Call visit?
You’ll meet with a licensed health care practitioner who may be a nurse practitioner, physician assistant or medical doctor. Just like the professionals you see in your regular doctor’s office, our staff are state licensed and maintain national certification. We take the extra step of performing background checks on our clinical staff to provide additional assurance for our members.
How does a house call differ from a regular doctor office visit, Urgent Care Facility, or an Emergency Room?
We bring excellent, quality healthcare to you and on your schedule. You are seen in the comfort of your home, hotel or office and at a convenient time for you. You never have to wait again in an overcrowded waiting room. You will not be sitting next to sick patients for an extended period of time. We can treat the same illnesses that you would normally go to see in a primary care physician’s office. Our fees are affordable and often less expensive that one would pay at an Urgent Care Center or an Emergency Department.
Do you provide medications?
Our providers carry injectable medications and can prescribe medications to your local pharmacy for pick up.
What if the physician decides my illness requires additional testing and/or treatment?
We can provide all additional testing (e.g. x-rays, EKG, ultrasound, etc.) in the comfort and convenience of your home or hotel suite, and can provide referrals to any specialty if needed.
Do you draw labs?
We do offer a variety of laboratory tests and studies that can be completed in the home, hotel or workplace. Blood work can be drawn and delivered to local laboratories when necessary.
Do you offer X-ray and ultrasound services?
X-ray and ultrasound services are available to be brought to you upon request. A certified x-ray technician brings a portable x-ray machine to your home, hotel room, workplace, or wherever you are. The x-ray images are processed on site, and films are reviewed by your house call physician or a board certified radiologist. Copies of the images may be provided to the patient upon request. Various portable ultrasound studies are also available. Additional studies, including CT or MRI may be completed at a radiology center of your choice.
Will you care for the home-bound, or elderly, as a primary care doctor?
Yes, with pleasure, under most circumstances.
If I am experiencing an emergency, should I book a house call?
Concierge MD is not an Emergency Room replacement and we do not treat patients experiencing chest pain, shortness of breath, head trauma, loss of consciousness, or other life-threatening emergencies, as these conditions may require immediate hospitalization. If you are having a medical emergency, please go directly to the E.R. or dial 911 immediately.
Do you accept health insurance?
Although most insurance companies will reimburse a portion of the visit or apply the amount to your deductible if it has not been met at this time, we do not accept insurance in the traditional sense. We will provide you with the documentation that can be submitted to your health insurance company for reimbursement. You may be eligible for reimbursement through your “out-of-network” option of your PPO or HMO plan. We do not guarantee any reimbursement.
May I utilize your services while I still see my regular physician with whom I have a long term relationship?
Yes! We understand the tremendous value in long standing Doctor Patient relationships. We will confer with your physician and coordinate your care together.
What are the benefits of using Concierge MD?
- Same-day service and appointments, usually within one to two hours of your call.
- Extended and unhurried medical visits.
- Comprehensive medical care in the comfort of your own environment.
- No more waiting in waiting rooms.
- House, Office, or Hotel Visits.
- On site diagnostic testing.
- Personal relationship with your licensed clinical provider.
- Prompt follow-up on all tests and reports.
- Coordination of care with carefully selected specialists.
- Fast and Easy Prescription Renewal Anytime/Anywhere.
- Prompt telephone feedback with lab and radiology test results.
Who uses Concierge MD?
For those of you who are frustrated by excessive wait times in the ER or refuse to stay in an overcrowded urgent care clinic, Concierge MD offers a time saving, efficient alternative. With Concierge MD, you can now be taken care of in the comfort of your home, hotel or workplace, with minimal interruption to your daily life.
How much do you save with a house call?
The time and monetary savings accompanied with a house call visit are significant because of the convenience of bringing healthcare to you. House call visits offer value by providing a licensed health care practitioner on your schedule. If you are a busy individual and value the little time you have to enjoy, then ConciergeMD offers you an excellent solution when you or a loved one need medical attention. Now you can afford the luxury of not having to leave your home, office, or hotel when you are sick, deal with traffic, and spend significant time waiting for a doctor’s appointment or in the waiting room with other sick patients waiting to be seen. This can often take hours of your time.
Do I have to be a member of Concierge MD to have a provider visit me at my home, office, or hotel?
No! ConciergeMD is available to everyone. There are no membership fees or subscriptions required.
Does Concierge MD offer services for employers?
Concierge MD offers custom corporate service programs to provide medical care for your employees living in, working in, or visiting your local area. Our full line of services is available as well as custom arrangements tailored to your company’s needs. Rather than putting off a meeting or delaying a flight, we arrange medical treatment in the comfort of your employee’s office, house or hotel, and make sure that they rapidly get on the road to recovery. Make Concierge MD a valuable asset and addition to your benefits package by keeping your employees healthy and happy.
Do you offer virtual care instead? I would prefer to do this over the phone.
Yes, we do offer virtual care options for your convenience. If you prefer a remote consultation, you can learn more and schedule your virtual appointment by visiting our Virtual Consultations Page. We’re here to provide healthcare in the way that suits you best.
Experience Care with ConciergeMD
ConciergeMD offers coverage throughout the United States.
GP mythbuster 71: Prioritising home visits
It is good practice for GP practices to have systems in place to triage and prioritise home visits.
Since the coronavirus (COVID-19) pandemic, the need for a home visit should be continue to be carefully assessed. The British Medical Association (BMA) and Royal College of General Practitioners have published COVID-19 Workload Prioritisation Unified Guidance which explains response levels. The guidance outlines types of work that should be undertaken in primary care, depending on:
- COVID-19 prevalence
- other workload
- workforce factors
The British Medical Association (BMA) has produced a COVID-19 toolkit for GPs and GP practices .
NHS England issued a patient safety alert to raise awareness of the need to have a system in place to assess:
- whether a home visit is clinically necessary , and
- the urgency of need for medical attention.
The alert states that:
"This can be undertaken, for example, by telephoning the patient or carer in advance to gather information to allow for an informed decision to be made on prioritisation according to clinical need. In some cases, the urgency of need will be so great that it will be inappropriate for the patient to wait for a GP home visit and alternative emergency care arrangements will be necessary."
"Many practices will already have systems in place to manage home visits. Where this is the case, consideration should be given to whether a review is required in light of this alert. The review should also consider whether all clinical and non-clinical staff involved in the process are aware of their responsibilities when managing requests for home visits, and if any outstanding training needs exist.”
GPs should also consider whether alternate ways of assessing the patient are appropriate. For example, video call, telephone calls or the use of virtual wards in care homes.
When delegating home visits, the provider must ensure that the Health Care Professional (HCP) has the necessary:
- competence and
- training to deliver the home visit.
The HCP should also receive appropriate supervision and support from the clinical team. Practices should ensure that the person allocated is competent to carry out home visits.
When we inspect
We will expect to see evidence of how the provider has assured themselves of the capability of non-medical HCPs, to whom they delegate home visits. This should include a process of assurance: both on initial delegation of the role and how the HCP’s capability is maintained on an ongoing basis. It should include audit of:
- their clinical decision-making
- prescribing decisions when relevant and
- a system for escalation to a senior clinician when necessary.
We use these regulations when we review if the practice is safe, effective, responsive, caring and well led. This mythbuster relates to:
- Regulation 9 (Person centred care)
- Regulation 12 (Safe care and treatment)
It is part of our key lines of enquiry (KLOEs). One of our key questions is whether services are organised so that they meet people’s needs. In particular, KLOEs:
- S2 Managing Risk
- S3 Safe care and treatment
- E3 Staff skills and knowledge
- E4 How staff, teams and services work together
- R1 Person centred care
- R3 Timely access to care and treatment
- WL8 Learning, improvement and innovation .
We may look at how the practice:
- manages and prioritises home visits
- recognises a deteriorating patient
- works with other professionals
- manages care planning, referrals and investigations.
We may also look at:
- the practice’s processes and systems to monitor patient safety through reporting patient safety incidents
- how they learn from these incidents and significant events.
This patient safety alert shows how important it is for GP practice staff to report all patient safety incidents to the National Reporting and Learning System (NRLS). Lessons can be learned across general practice.
Further information
- GP mythbuster 24: Reporting patient safety incidents to the National Reporting and Learning System (NRLS) for GP practices
- GP mythbuster 66: Advanced nurse practitioners and primary care
- GP mythbuster 100: Online and video consultations and receiving, storing and handling intimate images
- GP mythbuster 102: Pulse oximetry and monitoring vital signs outside the GP practice
- Patient Safety eForm (nrls.nhs.uk)
GP mythbusters
Snippet gp mythbusters rh.
Clearing up some common myths about our inspections of GP and out-of-hours services and sharing agreed guidance to best practice.
See all issues:
- GP mythbusters: listed by key question
- GP mythbusters: full list
- GP mythbusters: recently updated
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Guideline Centre (UK). Emergency and acute medical care in over 16s: service delivery and organisation. London: National Institute for Health and Care Excellence (NICE); 2018 Mar. (NICE Guideline, No. 94.)
Emergency and acute medical care in over 16s: service delivery and organisation.
Chapter 6 gp-led home visits, 6. gp led home visits, 6.1. introduction.
Primary care home visits are well established in current UK practice. Home visits could help avoid unplanned hospital admission when supported with appropriate diagnostic back up. In addition when a patients’ own GP is attending they may have access to patient records and history. It should enable a discussion of options and shared decision making. Primary care visits are particularly useful with people who have complex care needs.
This review question examined whether primary care led home visits reduced unplanned hospital admission for adults and young people with a suspected or confirmed AME or at risk of an AME.
6.2. Review question: Do primary care led home visits reduce unplanned hospital admissions?
For full details see review protocol in Appendix A .
PICO characteristics of review question.
6.3. Clinical evidence
No relevant clinical studies were identified.
6.4. Economic evidence
Published literature.
No relevant economic evaluations were identified.
The economic article selection protocol and flow chart for the whole guideline can found in the guideline’s Appendix 41A and Appendix 41B .
In the absence of health economic evidence, unit costs were presented to the guideline committee – see Chapter 41 Appendix I .
6.5. Evidence statements
6.6. recommendations and link to evidence.
View in own window
Appendix A. Review protocol
Table 2 review protocol: do primary care led home visits reduce unplanned hospital admissions, appendix b. clinical article selection.
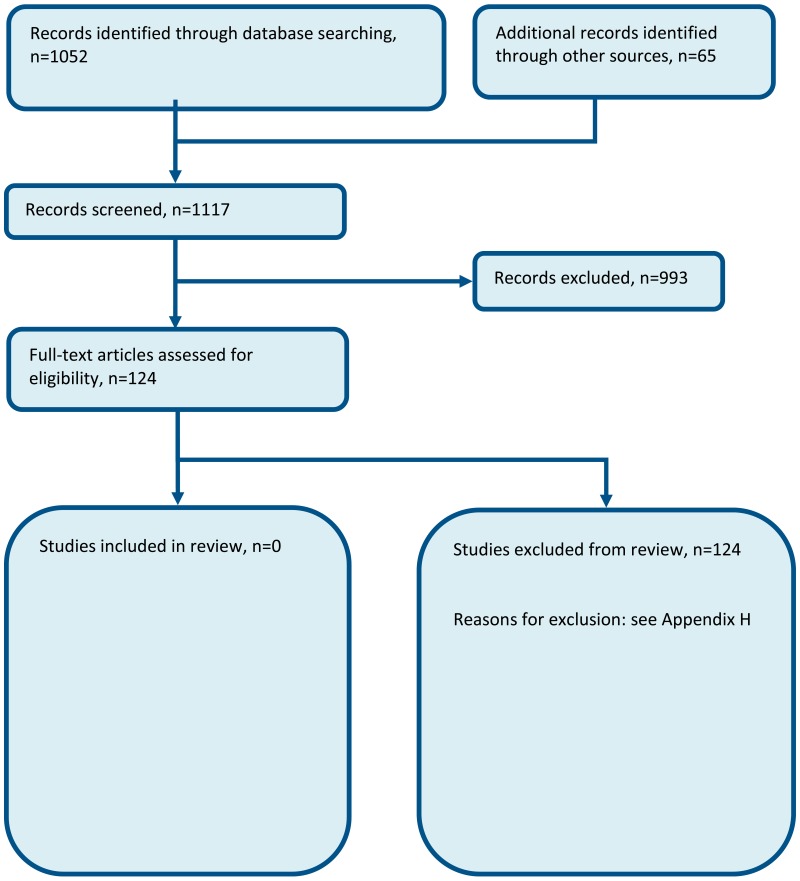
Figure 1 Flow chart of clinical article selection for the review of GP home visits
Appendix c. forest plots, appendix d. clinical evidence tables, appendix e. economic evidence tables.
No studies were included.
Appendix F. GRADE tables
Appendix g. excluded clinical studies, table 3 studies excluded from the clinical review, appendix h. excluded economic studies.
No studies were excluded.
- Cite this Page National Guideline Centre (UK). Emergency and acute medical care in over 16s: service delivery and organisation. London: National Institute for Health and Care Excellence (NICE); 2018 Mar. (NICE Guideline, No. 94.) Chapter 6, GP-led home visits.
- PDF version of this page (888K)
In this Page
- GP led home visits
Other titles in this collection
- National Institute for Health and Care Excellence: Guidelines
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- GP-led home visits - Emergency and acute medical care in over 16s: service deliv... GP-led home visits - Emergency and acute medical care in over 16s: service delivery and organisation
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- International edition
- Australia edition
- Europe edition

The paramedic will see you now: home visits by ambulance staff lighten GPs’ load
Patients – many of them housebound – have responded positively to an initiative that relieves pressure on family doctors
Ambulance services are helping to relieve GPs’ huge workloads by using some of their paramedics to carry out home visits to sick patients, a service traditionally undertaken by family doctors.
Paramedics are swapping answering 999 calls for tending people who have asked for a GP to see them at home because they are too ill or frail to come into the surgery.
NHS bosses say paramedics taking on this role is fast emerging as a way of helping GPs , stopping patients ending up in hospital unnecessarily and tackling chronic understaffing.
The North East ambulance service (NEAS) is one of several services that is seconding paramedics to work with GPs because they believe that home visits help the NHS overall, including reducing pressure on A&E, which is experiencing record demand for care.
“It helps GPs , patients like it and paramedics enjoy working like this,” said Paul Younger, who has been with the NEAS since 2002 and is one of its six paramedics who work in primary care.
“It takes about 45 minutes for a GP to go and see a patient for a home visit. But they can see four to five patients in their surgery in that time if a paramedic does the home visit instead.
“Plus, we paramedics can get there quicker, sometimes in as little as 15 minutes, whereas if a GP was going to visit someone at home who’d rung the surgery that morning, they’d have to wait until they’d seen all their patients that morning and then go, so not until lunchtime.”
Three NEAS paramedics work like this every weekday around Berwick, and another three in North Tyneside, including Whitley Bay, North Seaton and Wallsend. They drive unmarked cars rather than NHS ambulances.
“Initially, some local GPs were a bit dubious. GPs have been doing primary care for decades so, with the change, some thought: do the paramedics know what they’re doing? Are patients safe? But over time they’ve learned that they can play an important part of looking after patients in primary care,” added Younger.
Almost all the patients he and his colleagues visit are housebound. Most referrals have come from a GP but sometimes a district nurse, care home or domiciliary care worker makes the request. The NEAS paramedics also cover care homes – they comprise one in seven of their visits.

“The range of clinical cases paramedics deal with is vast,” said Paul Aitken-Fell, NEAS’s lead consultant paramedic, who set up the service in 2019. The most common problem they encounter is trouble breathing, for example because of chronic obstructive pulmonary disease. But they deal with a wide range of conditions including joint pain, skin problems, infections and heart attacks.
“If you are having a heart attack you’d be better off with a paramedic turning up at your house than a GP because, being specialists in urgent and emergency care, we see them more than GPs,” added Younger. Only one in 10 patients ends up going to hospital because paramedics’ experience means they can treat most of them on the spot and draw up a care plan, sometimes with input from a GP.
NEAS is in talks with GPs elsewhere on its patch to start providing the service, including Hartlepool and Easington, said Aitken-Fell. NEAS’s ability to deal with 999 calls is not undermined by the scheme because the six are dedicated home-visit paramedics, and deploying them like this should ultimately cut the number of people needing a blue light ambulance, he added.
“This is a great example of different parts of the NHS coming together and working in new ways to deliver better care for patients,” says Saffron Cordery, deputy chief executive of NHS Providers, which represents England’s NHS trusts, including the 10 specialist ambulance trusts. “It’s a win-win-win: for the organisations involved, for staff and above all for patients, who feel listened to, safe and confident in the care provided.”
NHS Providers has highlighted NEAS’s work with GPs in a report to be published this week on the creative solutions that trusts are adopting, given the health service in England is short of almost 100,000 staff.
Several other ambulance services offer GP-style home visits. London ambulance service paramedics have undertaken home visits and worked in GP surgeries in the boroughs of Redbridge and Merton since last year.
LAS is expanding its efforts to help hard-pressed GP surgeries. Thirty of its paramedics are currently on a training course, in conjunction with Health Education England, to enable them to work in GP surgeries alongside family doctors, practice nurses and their colleagues.
“Arrangements like this are proving to be a virtuous circle where everybody benefits. We must expand these schemes to help keep primary care sustainable,” said one NHS boss.
- The Observer
Most viewed

After-hours GP home visits strain the budget (and don’t help emergency departments)
Postdoctoral Research Fellow, Health Economics, University of Tasmania
Head, Discipline of General Practice, University of Tasmania
Disclosure statement
Barbara de Graaff receives funding from Primary Health Tasmania to evaluate primary health care in the after-hours..
Mark Nelson does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
University of Tasmania provides funding as a member of The Conversation AU.
View all partners
After-hours home medical services are a burden on our health budget and don’t ease the strain on emergency departments after all, new research shows.
The roll out of after-hours GP-type home visits is linked with as much as a ten-fold increase in Medicare claims in one jurisdiction. And rather than reducing the need to visit the emergency department, their rise in popularity has been accompanied by a slight increase in visits.
Our findings, published today in the Australian Family Physician journal, question whether these convenient house calls are really the best use of taxpayers’ money.
What are after-hours home medical services?
The way people access GP-type services after their regular doctor’s surgery has closed for the day, or at weekends, has changed considerably in recent years.
In the past, if you called your GP after hours, you might hear a recorded message with the phone number of an after-hours medical service to attend. Alternatively, the message would recommend you go to the local emergency department.
But over the past five years, there has been a proliferation of after-hours medical services that come to you. These services advertise 100% bulk-billed consultations by GPs and other doctors in the home.

A blow-out in Medicare claims
Doctors can claim one of several Medicare items to reimburse them for providing care after hours . The precise item number depends on whether the service they provide is urgent, where they provide that service and the length of the consultation.
There’s been a rapid growth in claims reported for all after-hours Medicare items. And since 2014, claims for these items increased five times faster than the rate of standard GP consultations.
Attention has focused on Medicare item 597 , the key item number for such, “urgent” after-hours consultations.
We reviewed the Medicare statistics website from 2010/11, when these after-hours services started to be launched. In the period since then until 2015/16 the number of claims for item 597 increased by 170%.
This growth has naturally affected Medicare expenditure. In the five years before 2010/11, annual expenditure on item 597 increased from A$55 million to A$72 million, a 29% increase. But in the next five years, expenditure increased to A$197 million, a 136% increase.
What’s driving this increase?
So what’s driving this increase, not only in the number of Medicare claims, but how much they cost the taxpayer?
We examined whether there was any truth in media reports suggesting the emergence of after-hours home medical services was largely responsible.
We identified key dates when the services were set up or expanded in Western Australia (WA), Tasmania, Australian Capital Territory (ACT) and Northern Territory (NT). Then we tracked changes in quarterly Medicare rebates against item 597 in each jurisdiction.
All jurisdictions had rapid and substantial increases in claims for item 597 after services in their area were set up or expanded.
To illustrate this, we charted the growth in claims from the quarter before the services were established up to the second quarter of 2016.
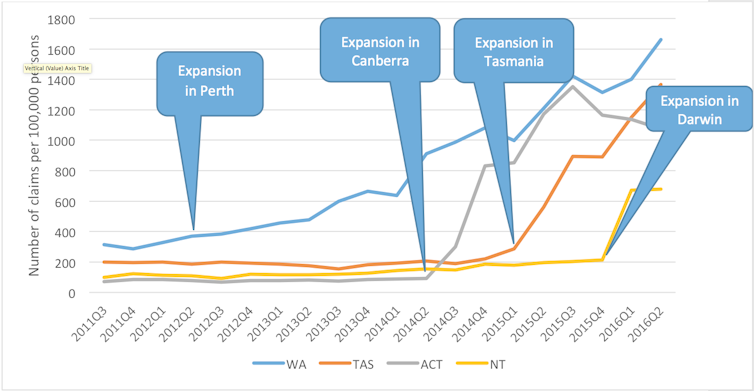
In the ACT, there was a 1,057% increase in claims since the second quarter of 2014; Tasmania saw a 521% increase since the fourth quarter of 2014; in WA there was a 348% increase since the second quarter of 2012; and for the NT, a 219% increase since the first quarter of 2015 was reported.
Impact on emergency department visits
Supporters of after-hours home medical services say the growth in Medicare claims associated with these services reduces government expenditure. This is because fewer people use emergency departments.
A recent report by Deloitte Access Economics, commissioned by the National After-Hours Medical Deputising Service, estimated A$724 million in savings over four-years due to reduced emergency department presentations. This estimate was based on the assumption that 25% of “avoidable GP-type” emergency department presentations would receive care through after-hours home visiting medical services instead. However, there is no evidence to support this assumption.
According to the latest report from the Australian Institute of Health and Welfare, emergency department presentations in all states increased between 2011/12 and 2015/16 by 2.7%.
Indeed, both emergency presentations and, as we have shown, Medicare claims for item 597 are increasing.
Recently released Senate Estimates documents provide interesting reading. An estimated 180,000 people received three or more “urgent” consultations from an after-hours home visiting medical service between 2014 and 2016. Of these, more than 10,000 had no contact with a regular GP.
If these services are truly meeting previously unmet demand for urgent medical care, then we should see a decrease in emergency department presentations. However, this is not occurring.
What’s behind these figures?
What we are likely observing is clever marketing, using multiple channels – like web-based advertising, YouTube videos, flyers in pharmacies – to fuel demand for these new services.
Another potential reason for the increased claims for item 597 relates to reimbursement. As the rate for urgent after-hours consultations is higher than non-urgent consultations, some doctors or businesses may be tempted to claim an urgent consultation.
What needs to happen next?
There is no definition of “urgent” in the Medicare Benefits Schedule as doctors are well-placed to decide what’s urgent. However, greater scrutiny of claims against item numbers for urgent consultations, such as regular audits, may be warranted.
As part of wider Medicare reforms, the federal health department and Royal Australian College of General Practitioners are aiming to set up a new after-hours rebate structure and will also review after-hours billing practices.
The Medicare Benefits Schedule review is also expected to publish its recommendations about after-hours medical care soon.
- Health economics
- Emergency departments
- Health funding
- after hours GP
- Emergency services

Project Officer, Student Volunteer Program

Audience Development Coordinator (fixed-term maternity cover)

Lecturer (Hindi-Urdu)

Director, Defence and Security

Opportunities with the new CIEHF
Advertisement
A Palestinian American doctor walked out of the White House. He explains why
Copy the code below to embed the wbur audio player on your site.
<iframe width="100%" height="124" scrolling="no" frameborder="no" src="https://player.wbur.org/hereandnow/2024/04/04/palestinian-doctor-white-house"></iframe>
Palestinian American Dr. Thaer Ahmad is an emergency room physician in Chicago. He was at the White House this week in a meeting with President Biden, Vice President Kamala Harris and Muslim-American community leaders. He says he spoke briefly, urging Biden to take action to prevent an Israeli incursion into Rafah, before walking out of the meeting.
Here & Now 's Deepa Fernandes talks with Ahmad about his reasons for doing that.
This segment aired on April 4, 2024.
More from Here & Now
- Skip to main content
- Keyboard shortcuts for audio player

Solar eclipse 2024: Follow the path of totality
Solar eclipse, worried about eclipse damage to your eyes don't panic.

Geoff Brumfiel

Nell Greenfieldboyce

Junior Espejo looks through eclipse glasses being handed out by NASA in Houlton, Maine. Used correctly, eclipse glasses prevent eye damage. Joe Raedle/Getty Images hide caption
Junior Espejo looks through eclipse glasses being handed out by NASA in Houlton, Maine. Used correctly, eclipse glasses prevent eye damage.
Tens of millions of Americans will have spent the day staring at a total solar eclipse, and at least a few of them may become worried that they inadvertently damaged their eyes.
But experts say there's no need to panic — the vast majority of eclipse viewers are probably fine. And even if somebody did strain their eyes, the effects could be temporary.
During the 2017 total solar eclipse it's estimated that 150 million Americans viewed the event. There were around 100 documented cases of eye damage across all of America and Canada, according to Ralph Chou, an expert on eclipse eye safety with the University of Waterloo in Canada.
Far more people turned up in emergency rooms worried that they'd damaged their eyes. Many complained of watery eyes or blurred vision, but in most cases they were fine, according to Avnish Deobhakta, an ophthalmologist at the New York Eye and Ear Infirmary of Mount Sinai, one of the largest eye hospitals in the nation.
The reason it's hard to do real damage is simple — the human eye has evolved to avoid staring directly at the sun.
"It's so bright that we're not actually capable of looking at it without either tearing or sort of not really feeling comfortable staring at this ball of light," Deobhakta says.

Shots - Health News
Here's what it looks like when you fry your eye in an eclipse.
In the rare case that someone does damage their eyes, that damage usually shows up as a blurry spot in the field of vision , hours or up to a day after watching the eclipse. In about half of cases, the problem fixes itself, but permanent damage can sometimes occur.
Anticipating the post-eclipse ocular anxiety, at least one eye clinic in Buffalo, N.Y., is offering free eye checks immediately after the eclipse on April 8.
It's always a good idea to get your eyes checked, whether or not there's an eclipse. So if you're worried at all, go ahead and use the opportunity to schedule your annual exam.
- eclipse eye damage
- 2024 eclipse
The Doctor Will Ask About Your Gun Now
More physicians are making gun safety part of routine visits. But should they be?
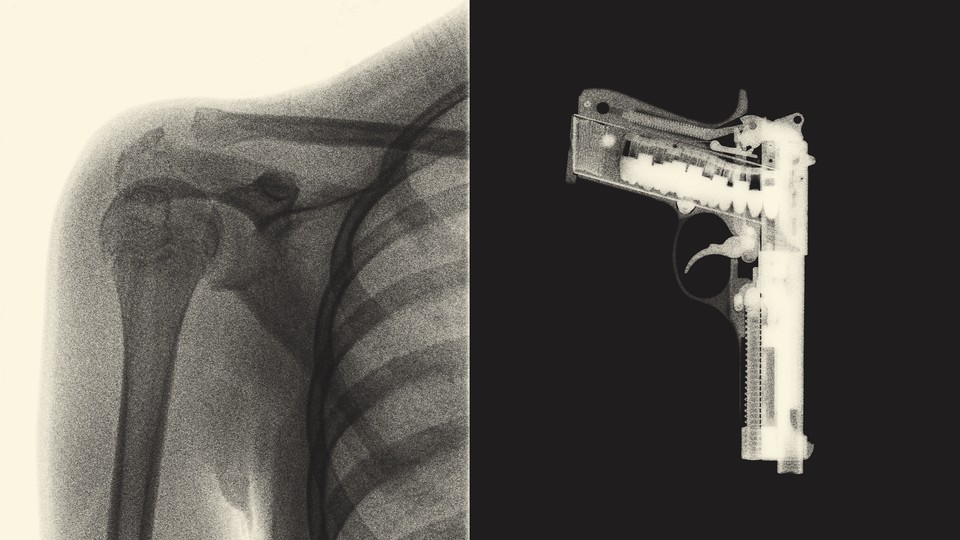
Updated at 3:23 p.m. ET on April 3, 2024
A man comes to Northwell Health’s hospital on Staten Island with a sprained ankle. Any allergies? the doctor asks. How many alcoholic drinks do you have each week? Do you have access to firearms inside or outside the home? When the patient answers yes to that last question, someone from his care team explains that locking up the firearm can make his home safer. She offers him a gun lock and a pamphlet with information on secure storage and firearm-safety classes. And all of this happens during the visit about his ankle.
Northwell Health is part of a growing movement of health-care providers that want to talk with patients about guns like they would diet, exercise, or sex—treating firearm injury as a public-health issue. In the past few years, the White House has declared firearm injury an epidemic, and the CDC and National Institutes of Health have begun offering grants for prevention research. Meanwhile, dozens of medical societies agree that gun injury is a public-health crisis and that health-care providers have to help stop it.
Asking patients about access to firearms and counseling them toward responsible storage could be one part of that. “It’s the same way that we encourage people to wear seat belts and not drive while intoxicated, to exercise,” Emmy Betz, an emergency-medicine physician and the director of the University of Colorado’s Firearm Injury Prevention Initiative, told me. An unsecured gun could be accessible to a child, someone with dementia, or a person with violent intent—and may increase the chance of suicide or accidental injury in the home. Securely storing a gun is fundamental to the National Rifle Association’s safety rules , but as of 2016 , only about half of firearm owners reported doing so for all of their guns.
Some evidence shows that when health-care workers counsel patients and give them a locking device, it leads to safer storage habits. Doctors are now trying to figure out the best way to broach the conversation. Physicians talk about sex, drugs, and even (if your earbuds are too loud) rock and roll. But to many firearm owners, guns are different.
Not so long ago, powerful physicians argued that if guns were causing so much harm, people should just quit them. In the 1990s, the director of the CDC’s injury center said that a public-health approach to firearm injury would mean rebranding guns as a dangerous vice, like cigarettes. “It used to be that smoking was a glamor symbol—cool, sexy, macho,” he told The New York Times in 1994. “Now it is dirty, deadly—and banned.” In the 2010s, the American Academy of Pediatrics’ advice was to “NEVER” have a gun in the home, because the presence of one increased a child’s risk of suicide or injury so greatly. (“Do not purchase a gun,” the group warned bluntly.) And when asked in 2016 whom they would go to for safe-storage advice, firearm owners ranked physicians second to last, above only celebrities.
In the past couple of decades, some states have toyed with laws that curtail doctors’ ability to talk with patients about firearms and the information they can collect, to assuage gun owners’ privacy concerns. Only in Florida did the most restrictive version—what physicians call a “gag law”—pass, in 2011; six years later, a federal court struck it down. But “I think the gag orders, even though they’re not in effect now, really scared people,” Amy Barnhorst, an emergency psychiatrist and firearm-injury-prevention researcher at UC Davis, told me. A smattering of studies have found that doctors—particularly pediatricians —generally think talking with their patients about firearm safety is important, but most of the time, they’re not doing it. As of 2019, only 8 percent of firearm owners said their doctor had ever brought it up.
That year, in California, Barnhorst launched the state-funded BulletPoints Project, a free curriculum that teaches health-care workers how and when to talk about firearms with their patients. The program instructs them to keep politics and personal opinions out of the conversation, and to ask only those patients who have particular reasons for extra caution—including people with children, those experiencing domestic violence, or those living with someone with a cognitive impairment. It also suggests more realistic advice than “Do not purchase a gun.” Maybe a patient has a firearm for self-defense (the most common reason to have one), so they’d balk at the idea of storing a gun unloaded and locked, with the ammunition separate. A health-care worker might recommend a quick-access lockbox instead.
Researchers are now testing whether these firearm conversations have the best outcome if doctors broach them only when there’s a clear reason or if they do it with every patient. Johns Hopkins is trialing a targeted approach, talking about firearms and offering gun locks in cases where pediatric patients have traumatic injuries. Meanwhile, Northwell Health, which is New York State’s largest health system, asks everyone who comes into select ERs about gun access and offers locks to those who might need them. Both of these efforts are federally funded studies testing whether doctors feel confident enough to actually talk with patients about this, and whether those conversations lead people to store their firearms more securely.
For doctors, universal screening means “there’s no decision point of who you’re going to ask or when you’re going to ask,” Sandeep Kapoor, an assistant professor of emergency medicine who is helping implement the program at Northwell Health, told me. So far, Northwell’s trial has screened about 45,000 patients, which signals that the approach can be scaled up. Kapoor told me that with this strategy, gun-safety conversations could eventually become as routine for patients as having their blood pressure taken. When she was in primary pediatrics, Katherine Hoops, a core faculty member at Johns Hopkins’s Center for Gun Violence Solutions, worked firearm safety into every checkup, as she would bike helmets and seat belts. (The American Academy of Pediatrics still maintains that the safest home for a child is one without a gun, but the organization now recommends that pediatricians talk about secure storage with every family, and offers a curriculum on how to have this conversation.) Universal screening can also find people whom a targeted approach might miss: The team at Northwell recently learned through screening questions that a 13-year-old who came in with appendicitis had been threatened with guns by bullies, and brought in his parents, a team of social workers, and the school to help.
But a patient in the ER for a sprained ankle may understandably wonder why a doctor is asking about firearms. “There’s no context,” says Chris Barsotti, an emergency-medicine physician and a co-founder of AFFIRM at the Aspen Institute, which aims to reduce firearm injuries through health-focused interventions. The firearm community, he said, remembers when “the CDC wanted to stigmatize gun ownership,” so any movement for health care workers to raise these questions needs nuance. To his mind, these should be tailored conversations. Betz, of the University of Colorado, raises the question only when a patient is at risk, and believes that firearm safety can otherwise be in the background of a practice—for example, in a waiting room where secure-storage brochures are displayed alongside pamphlets on safe sex and posters on diabetes prevention.
About half of firearm-owning patients agree that it’s sometimes appropriate for a doctor to talk with them about firearms, according to a 2016 study by Betz and her colleagues. They’re even more okay with it if they have a child at home. The physicians I asked said that the majority of the time, these conversations go smoothly. But Betz’s study also found that 45 percent of firearm-owning patients thought doctors should never bring up guns. Paul Hsieh, a radiologist and a co-founder of the group Freedom and Individual Rights in Medicine, wrote in an email that gun owners he’s spoken with “find the question about firearms ownership intrusive in a different way than questions about substance use or sexual partners.”
Chethan Sathya, a pediatric trauma surgeon and the director of Northwell Health’s Center for Gun Violence Prevention, pointed out that those topics used to be contentious for physicians to talk about. To treat guns as a public-health issue, “we can’t be uncomfortable having conversations,” he told me. But doctors have more power in this situation than they do in others. They might tell someone with diabetes to stop having soda three times a day, but they can’t literally take soda away from a patient. With guns, they might be able to. In states with extreme-risk laws, if a health-care provider believes that their patient poses an immediate threat to themselves or others, they can work with law enforcement to petition the court to temporarily remove someone’s firearms; a handful of states allow medical professionals to file these petitions directly. There are many people “across America right now who own guns and won’t come to counseling, because they don’t want their rights taken away for real or imagined reasons,” Jake Wiskerchen, a mental-health counselor in Nevada who advocates for such patients, told me. They worry that if their doctor includes gun-ownership status in their medical record, they could be added to a hypothetical national registry of firearm owners. And if questions about guns were to become truly routine in a doctor’s office—such as on an intake form—he said owners might just lie or decide they “don’t want to go to the doctor anymore.”
Physicians accordingly choose their words carefully. They talk about preventing firearm injury instead of gun violence —both because the majority of gun deaths are suicides, not homicides, and because it’s a less loaded term. Telling a diabetic patient to cut back on soda might work, but people “are not just going to throw their guns in the trash,” Barnhorst, of UC Davis, told me. “There’s a lot more psychological meaning behind firearms for people than there is for sodas.”
Barsotti says a public-health approach to firearm safety requires more engagement with the upwards of 30 percent of American adults who own a firearm. Owners of shooting ranges and gun shops are already “practicing public health without the benefit of medical or public-health expertise,” he told me. They’re running their own storage programs for community members who don’t want their guns around for whatever reason; they’re bringing their friends for mental-health treatment when they might be at risk. Betz’s team collaborated with gun shops, shooting ranges, and law-enforcement agencies in Colorado to create a firearms-storage map of sites willing to hold guns temporarily, and she counsels gun clubs on suicide prevention, as a co-founder of the Colorado Firearm Safety Coalition . Exam-room conversations can be lifesaving, but in curbing gun injury, Betz told me, health-care workers “have one role to play. We’re not the solution.”

1-208-882-4534
Our Facility
Why Choose Us
Privacy Policy
- Pre-Arrangements
- Pre-Arrangements Form
- The Talk of a Lifetime
- Veterans Overview
- Veterans Headstones
- Veterans Burial Flags
- Making Arrangements
- Grief Support
- When Death Occurs
- Funeral Etiquette
- Social Security Benefits
- Frequent Questions
- Links of Interest
The caring and experienced professionals at Short's Funeral Chapel are here to support you through this difficult time. We offer a range of personalized services to suit your family’s wishes and requirements. You can count on us to help you plan a personal, lasting tribute to your loved one. And we’ll carefully guide you through the many decisions that must be made during this challenging time.
You are welcome to call us at any time of the day, any day of the week, for immediate assistance. Or, visit our funeral home in person at your convenience. We also provide a wealth of information here on our web site so you can learn more from the privacy of your own home.
In this section
A year of daily grief support.
Our support in your time of need does not end after the funeral services. Enter your email below to receive a grief support message from us each day for a year. You can unsubscribe at any time.

IMAGES
VIDEO
COMMENTS
Our Services. We accept Medicare, many insurance plans, and self-pay. To find out more about our services: Call Toll-free: (855) 232-0644. E-mail us at. [email protected]. Primary Care. Psychiatry. Wound Care.
House calls and video visits in 37 states. Landmark partners with health plans to bring medical, behavioral health, and palliative care, along with social services, to patients in communities across the U.S. Our mobile providers visit patients in their homes through in-person house calls and telemedicine visits over video and phone.
To learn more about our services in the Washington, D.C., region, call us today at 202-877-0570. The MedStar Health MedStar House Call Program - MedStar Total Elder Care is nationally recognized and offers house calls by doctors, nurse practitioners and provides diagnostic tests and treatments. Learn more about our program.
If you don't have insurance, or we don't work with your insurance provider, you can still receive care from DispatchHealth at a flat rate of $375 per visit. This cost covers everything we do, including administering medication, procedures, and on-site lab tests. You can pay your bill by credit, debit, health savings account (HSA), health ...
Our house call medical teams are comprised of an emergency-medicine-trained physician assistant or nurse practitioner, with in-person support from a medical technician, as well as an emergency department doctor available to provide remote support at all times. Learn more about how DispatchHealth house calls work. On-demand health care 7 days a week
Look out for your health. A UnitedHealthcare® HouseCalls visit is a no-cost, yearly health check-in that can make a big difference. Call 1-866-799-5895, TTY 711, to schedule your visit.
Yes, many house call doctors accept Medicare, private insurance, and sometimes Medicaid. It usually costs the same as a regular office visit. But every house call doctor is different, so make sure you understand their fees and accepted insurance plans beforemaking an appointment. How to find a house call doctor.
Visit with an online doctor from the comfort of your home and get expert advice, a treatment plan and a prescription if needed. If you are visually impaired you will need to call us at 1-888-548-3432.
The Mount Sinai Visiting Doctors Program has clinical, educational, and research missions. It is one of the largest academic home-visit programs in the nation, with its clinicians making more than 6,000 home visits annually to more than 1,000 patients. Hundreds of medical students, residents, and fellows make house calls alongside our providers ...
Transitional care management visit within 14 calendar days of discharge, moderate MDM: 99496: $281.59: 3.79: Transitional care management visit within 7 calendar days of discharge, high MDM: 99483 ...
In-home care is more tailored than the majority of patients in a doctor's office or hospital and significantly reduces hospitalizations and emergency room visits. Numerous physicians see as many as twenty people per day, with each visit lasting barely a few minutes.
For this reason, if you request a home visit, your GP may call you back to find out more about your problem before deciding to come out. Out-of-hours care All doctors have an emergency service ...
During a house call visit, you'll meet with the same types of professionals you see in a doctor's office — a licensed health care practitioner. After introductions, your provider will perform a thorough history and physical examination appropriate for your specific complaints and will then recommend the appropriate treatment options.
Call Us 843-501-2031. HouseCalls-MD provides prompt on-site physician service! A physician comes to your residence, be it your house, assisted living facility or place of business, equipped with almost everything you can find in the doctor's office. X-rays and lab work samples collection is provided on the spot, when needed.
5 min read. Hospital emergency rooms (or departments) deal with sudden illnesses and injuries. They maintain preparedness for every kind of health emergency, including vehicular accidents, heart ...
The British Medical Association (BMA) has produced a COVID-19 toolkit for GPs and GP practices. NHS England issued a patient safety alert to raise awareness of the need to have a system in place to assess: whether a home visit is clinically necessary, and. the urgency of need for medical attention. The alert states that:
Primary care home visits are well established in current UK practice. Home visits could help avoid unplanned hospital admission when supported with appropriate diagnostic back up. In addition when a patients' own GP is attending they may have access to patient records and history. It should enable a discussion of options and shared decision making. Primary care visits are particularly useful ...
"It takes about 45 minutes for a GP to go and see a patient for a home visit. But they can see four to five patients in their surgery in that time if a paramedic does the home visit instead.
Dr. Kurt Martyn, MD is an emergency medicine specialist in Moscow, ID and has over 50 years of experience in the medical field. He graduated from Medical College of Wisconsin in 1973. He specializes in Emergency Medicine and Emergency Medical Technology (EMT).
Published: May 31, 2017 4:18pm EDT. After-hours home medical services are a burden on our health budget and don't ease the strain on emergency departments after all, new research shows. The roll ...
Highly qualified specialists provide consultations on emergency hospitalization and treatment. Make an appointment online or call +7 (499) 999-31-31. All the pros of ... Call a doctor at home. RU en. K+31 on Lobachevskogo. st. Lobachevskogo, 42/4 +7 499 999-31-31. K+31 Petrovskie Vorota. 1st Kolobovsky lane, 4. 74999993131. K+31 West ...
April 04, 2024. Palestinian American Dr. Thaer Ahmad is an emergency room physician in Chicago. He was at the White House this week in a meeting with President Biden, Vice President Kamala Harris ...
What to do if you're worried the eclipse damaged your eyes : Solar eclipse 2024: Follow the path of totality Eye damage is rare and sometimes temporary, but it never hurts to get it checked.
Doctors are now trying to figure out the best way to broach the conversation. Physicians talk about sex, drugs, and even (if your earbuds are too loud) rock and roll. But to many firearm owners ...
Nursing Home Information. 101 residents. 112 certified beds. Participates in Medicare and Medicaid. Continuing Care Retirement Community - Continuing Care Retirement Communities offer multiple housing options and levels of care.Residents may move from one level to another based on needs while still remaining in the community.
1225 East 6th Street. | Moscow, ID 83843. | Tel: 1-208-882-4534. |. About Us - Short's Funeral Chapel offers a variety of funeral services, from traditional funerals to competitively priced cremations, serving Moscow, ID and the surrounding communities. We also offer funeral pre-planning and carry a wide selection of caskets, vaults, urns and ...