
Mistakes in medical billing codes can lead to claim denials and forfeiting of reimbursements. CPT codes, including code 99284, play a crucial role in the clean claims process. This code describes an emergency department visit for the evaluation and management of a patient. It requires a detailed history, examination, and moderate complexity medical decision making. Providers need to optimize their coding and claims process to increase clean claims and improve hospital reimbursement. Utilizing electronic mental health billing software can greatly improve coding accuracy and streamline the billing process.

Key Takeaways:
- Understanding CPT codes is essential for accurate medical billing and coding.
- CPT code 99284 represents an emergency department visit with a detailed history, examination, and moderate complexity medical decision making.
- Clean claims are crucial for timely reimbursement and effective revenue cycle management.
- Utilizing electronic billing software can streamline the coding and claims process and improve accuracy.
- Outsourcing billing services to managed billing providers like Medical Bill Gurus can optimize coding and increase clean claims.
Understanding CPT Codes in Medical Billing
When it comes to medical billing, CPT codes are crucial for accurately describing and billing for services rendered in the healthcare field. CPT, or Current Procedural Terminology, codes cover a wide range of services, including diagnostic testing, procedures, evaluations, and ancillary services. These codes play a vital role in healthcare coding and ensure that healthcare providers receive appropriate reimbursement for the services they provide.
The complexity of a CPT code is determined by the level of detail in the history, examination, and medical decision making. This level of detail reflects the intensity and complexity of the service provided. For emergency department visits, the evaluation and management of patients is captured using CPT codes 99281-99285.
Let’s take a closer look at CPT codes and their significance in medical billing:
- Accurate Description: CPT codes provide a standardized way to describe various medical services, ensuring clarity and consistency in medical billing.
- Billing for Services Rendered: CPT codes enable healthcare providers to bill for the specific services they have provided to their patients, allowing for proper reimbursement.
- Outpatient Services: CPT codes cover a wide range of outpatient services, including office visits, procedures, laboratory tests, radiology services, and more.
Understanding and correctly applying the appropriate CPT code is essential for healthcare providers to ensure accurate billing and maximize reimbursement for the services they provide.
Take a look at the table below for an overview of the CPT codes commonly used for emergency department visits:
Understanding the appropriate CPT code, such as code 99284, is vital for accurately billing emergency department visits and ensuring proper reimbursement. By utilizing the right codes and documenting services accurately, healthcare providers can navigate the complexities of medical billing and maximize their revenue.
The Importance of Clean Claims for Reimbursement
Clean claims are an essential aspect of the healthcare billing process, ensuring timely reimbursement and effective revenue cycle management. They refer to claims that are approved after the first submission, without any errors or discrepancies that may lead to claim denials.
Insurance companies are rigorous in their assessment of claims, scrutinizing them for inaccuracies, missing information, or incorrect coding. Even a minor mistake can result in claim denials and delayed reimbursement, negatively impacting a provider’s cash flow and overall revenue. Therefore, perfecting the claims process is crucial to minimize denials and optimize reimbursement.
Accurate coding plays a vital role in generating clean claims. Properly assigning CPT codes, such as CPT code 99284 for emergency department visits, is imperative to ensure the claim reflects the services provided accurately. Using the correct CPT code increases the chances of claim approval and appropriate reimbursement.
Insurance billing for healthcare services involves navigating complex rules, regulations, and policies set by payers. It requires extensive knowledge of coding guidelines and comprehensive documentation of services provided. Therefore, providers must stay updated with the latest coding requirements and guidelines to maximize the chances of clean claims and avoid claim denials.
To illustrate the importance of clean claims, consider the following data:
These statistics highlight the significant impact that clean claims have on a provider’s financial stability. By avoiding claim denials and submitting clean claims, providers can shorten reimbursement cycles and maintain a steady cash flow for their practice.
Understanding CPT Code 99284
CPT code 99284 specifically represents an emergency department visit for the evaluation and management of a patient. It requires a detailed history, a detailed examination, and moderate complexity medical decision making. This code is typically used when the presenting problem is of high severity but does not pose an immediate significant threat to life or physiological function. Providers must accurately document and code the elements required for CPT code 99284 to ensure proper billing and reimbursement.
Elements of CPT Code 99284
- Detailed History: Providers must gather relevant information about the patient’s condition, including their symptoms, medical history, and any potential risk factors. This detailed history helps determine the severity of the presenting problem.
- Detailed Examination: A thorough physical examination is performed to assess the patient’s condition. This includes evaluating vital signs, performing diagnostic tests, and conducting a comprehensive assessment of the patient’s overall health.
- Moderate Complexity Medical Decision Making: Providers must analyze and evaluate the patient’s information, including their history, examination findings, and any diagnostic results. Based on this assessment, they make a medical decision regarding the appropriate course of action, which may include further testing, treatment, or referrals.
Accurate and comprehensive documentation is essential for successful billing and reimbursement using CPT code 99284. Providers need to ensure they include relevant details, such as the patient’s chief complaint, history of present illness, review of systems, physical examination findings, and medical decision-making process. Properly coding CPT code 99284 reflects the complexity and severity of the visit, enabling providers to receive appropriate reimbursement for their services.
Other Codes Related to CPT Code 99284
CPT code 99284 is part of a set of codes that describe different levels of evaluation and management for emergency department visits. These codes include:
These codes encompass a range of problem severities and complexity levels, allowing healthcare providers to accurately document and bill for emergency department visits. It is essential to choose the appropriate code based on the level of evaluation and management required for each patient encounter.
Improving Coding and Claims Process for CPT Code 99284
At our practice, we understand the importance of efficient coding and a streamlined claims process. To enhance our use of CPT code 99284 and ensure clean claims, we have implemented state-of-the-art electronic billing software. This software has revolutionized our billing procedures, resulting in improved coding accuracy and increased successful claim submissions.
Our electronic billing software offers a range of features that have significantly benefited the coding and claims process:
- Electronic billing for primary and secondary insurances: We can conveniently submit claims electronically, eliminating the need for paper claims and reducing the chances of errors during manual submission.
- Claim status checks: With just a few clicks, we can easily track the status of submitted claims. This allows us to promptly address any issues or follow up on pending payments.
- Payment and authorization tracking: Our software provides a centralized platform to monitor payments and authorizations, ensuring we stay on top of our revenue cycle management.
Implementing electronic billing software has relieved the coding pressure on our team, allowing us to redirect our focus towards delivering exceptional patient care. Our staff can confidently code for CPT code 99284, knowing that our software streamlines the process and increases the chances of clean claims and optimized reimbursement.
Managed Billing Services for Mental Health Providers
In addition to electronic billing software, mental health providers have the option to outsource their billing needs to managed billing services. These services, offered by companies like Medical Bill Gurus, provide specialized expertise in medical coding, billing, and claims management. By partnering with a reliable billing company, mental health providers can ensure accurate coding for CPT code 99284 and other related codes, increasing the chances of clean claims and optimized reimbursement.
Benefits of Managed Billing Services
Outsourcing billing needs to a managed billing service can offer numerous benefits for mental health providers:
- Expertise: Managed billing services have extensive experience in medical coding and billing, ensuring accurate and compliant coding for CPT code 99284 and other relevant codes.
- Efficiency: Dedicated billing professionals streamline the billing process, allowing providers to focus on patient care rather than administrative tasks.
- Claims Management: Managed billing services handle the entire claims process, from submission to follow-up, reducing the burden on mental health providers.
- Optimized Reimbursement: By ensuring accurate coding and clean claims, managed billing services maximize reimbursement for mental health services, improving financial outcomes.
By utilizing managed billing services, mental health providers can navigate the complexities of medical coding and billing, ultimately enhancing their revenue cycle management and practice efficiency.

Table: Comparison of Managed Billing Services
Table Note: Comparison of the benefits offered by different managed billing services for mental health providers.
Challenges and Consequences of Incorrect Coding
Incorrect coding can have serious repercussions, leading to claim denials, penalties, and alterations in reimbursement rates. Insurance companies and payers are vigilant in detecting potential fraudulent claims and are quick to deny those that are not accurately coded. The consequences of incorrect coding can range from delays in payment to audit requests and financial complications for healthcare providers.
When claims are inaccurately coded, they are more likely to be denied by insurance companies, resulting in a loss of revenue for the provider. Denied claims can lead to delays in reimbursement, affecting the cash flow of the practice and hindering its financial stability. Additionally, repeated claim denials can harm the provider’s reputation and credibility.
Insurance companies may also impose penalties on providers who consistently submit claims with coding errors. These penalties can further impact the provider’s bottom line and their ability to provide quality care to patients. Moreover, inaccurate coding can result in alterations to reimbursement rates, ultimately affecting the financial viability of the practice.
Another consequence of incorrect coding is the increased likelihood of an audit. Insurance companies and government agencies, such as Medicare, regularly conduct audits to ensure the accuracy and integrity of claims submitted. An audit can be a time-consuming and stressful process for providers, requiring them to provide extensive documentation and evidence to justify their coding decisions.
To mitigate the challenges and consequences of incorrect coding, providers must prioritize coding accuracy and take necessary measures to ensure compliance with coding guidelines. This includes staying updated on coding changes and seeking continuous education and training to enhance coding proficiency. Investing in reliable coding resources and leveraging technology, such as electronic billing software, can also improve accuracy and streamline the coding process.
Compliance with Insurance Company Rules and Guidelines
When it comes to proper billing and coding, insurance companies like Blue Cross and Blue Shield have strict rules and guidelines in place. As healthcare providers, we must ensure compliance with these requirements to avoid claim denials and potential liability. One important aspect of compliance involves understanding the restrictions on using CPT codes for specific places of service.
For instance, CPT codes 99281-99285 are designated for emergency department visits and should not be used for other places of service. It’s crucial to accurately select the appropriate CPT code based on the location where the patient is treated. Failure to follow these guidelines can result in claim denials, delayed reimbursement, and potential financial consequences.
Understanding insurance company rules and billing requirements is essential for healthcare providers to navigate the complex landscape of medical coding and billing. By staying compliant, we can ensure that our claims are processed smoothly and that we receive timely reimbursement for the services we provide.
CPT Code Restrictions and Emergency Place of Service
One key aspect of compliance with insurance company rules is adhering to CPT code restrictions based on the place of service. As mentioned earlier, CPT codes 99281-99285 are specifically meant for emergency department visits. These codes capture the level of evaluation and management provided during these critical situations.
It’s important to note that using these codes for other places of service, such as outpatient clinics or non-emergency settings, can lead to claim denials and potential audit scrutiny. Insurance payers require accurate coding that reflects the actual services rendered in each specific location.
Here is a table illustrating the CPT code restrictions based on the place of service:
By understanding and adhering to these CPT code restrictions, healthcare providers can maintain compliant billing practices, reduce the risk of claim denials, and ensure accurate reimbursement for the services they provide.
Image: An illustration depicting the importance of adhering to CPT code restrictions based on the place of service.
Best Practices for Mental Health Coding and Billing
Mental health providers often have minimal training in medical coding and billing practices. This can lead to inaccuracies in coding and billing, resulting in claim denials and financial complications. To ensure accurate coding and streamlined billing practices, mental health providers should consider implementing the following best practices:
1. Medical Coding Training
Investing in medical coding training for staff members can greatly enhance coding accuracy and understanding. By equipping the team with comprehensive knowledge of mental health coding practices, providers can ensure accurate code selection, proper documentation, and improved compliance with billing requirements. This training may cover topics such as CPT codes related to mental health services, evaluation and management coding, and the use of modifiers specific to mental health.
2. Outsourcing to a Third-Party Billing Agency
Outsourcing coding and billing to a third-party agency specialized in mental health services can be a viable solution for providers facing administrative burdens and seeking expert assistance. A reliable third-party billing agency, such as ABC Billing Services, provides access to experienced professionals who possess in-depth knowledge of mental health coding and billing practices. By leveraging the expertise of these professionals, providers can optimize clean claims, increase reimbursement rates, and reduce claim denials.
In addition to these best practices, mental health providers should prioritize ongoing professional development and stay updated with the latest coding changes and industry guidelines. Collaboration with a reputable medical billing company, like ABC Billing Services, can provide continuous support and ensure compliance with regulatory requirements in mental health coding and billing practices.
Coding Documentation Requirements for CPT Code 99284
Accurate coding is essential for proper reimbursement when using CPT code 99284. To ensure accurate coding, detailed documentation of the patient’s history, examination, and medical decision making is required. Each of these components must be thoroughly documented to support the level of complexity required for this code.
When documenting the patient’s history, include a detailed account of the patient’s current condition, including the onset, duration, and any relevant factors. Document any past medical history, including previous treatments, surgeries, or chronic conditions that may impact the current visit.
The examination documentation should include a comprehensive assessment of the patient’s vital signs, physical appearance, and any relevant findings from the examination. Any tests, procedures, or diagnostic results should also be documented.
Medical decision making is a critical aspect of coding documentation for CPT code 99284. Document the thought process behind the diagnosis and treatment plan, including the assessment of risks and benefits. Include any consultations or referrals made and document any medications prescribed or administered.
Accurate coding documentation is crucial for generating clean claims and optimizing reimbursement. Providers must ensure that the documentation aligns with the requirements of CPT code 99284 to avoid claim denials and revenue loss.
Benefits of Using Medical Bill Gurus for Billing Services
When it comes to navigating the complexities of healthcare coding and insurance billing, medical providers need a reliable partner to ensure accurate coding and optimized reimbursement. That’s where Medical Bill Gurus come in. We offer comprehensive billing services for healthcare providers, including mental health professionals, with expertise in medical coding, insurance billing, and claims management.
With our in-depth knowledge of the industry, we understand the intricacies of billing for CPT code 99284 and other related codes. Our team works with all insurance payers, including Medicare, to ensure that your coding is accurate and compliant. We know the specific requirements and guidelines of each payer, allowing us to maximize your reimbursement rates.
By choosing Medical Bill Gurus as your billing services partner, you can benefit from our streamlined billing process. Our advanced technology and automated systems enable us to efficiently handle your billing needs, saving you time and ensuring accuracy. By outsourcing your billing to us, you can focus on what matters most – delivering quality care to your patients.
Why Choose Medical Bill Gurus for Your Billing Services?
- Expertise in medical coding: Our team of experienced coders ensures that your claims are accurately coded, minimizing the risk of claim denials and optimizing your revenue.
- Insurance payer knowledge: We have extensive knowledge of insurance payer guidelines and requirements, allowing us to navigate the complexities of insurance billing with ease.
- Comprehensive claims management: Our end-to-end claims management process ensures that your claims are submitted accurately and timely, maximizing your chances of clean claims approval.
- Automated systems: Our advanced technology automates mundane tasks, freeing up your staff’s time and improving coding accuracy.
- Focus on compliance: We stay up-to-date with the latest industry regulations and coding updates, ensuring compliance and minimizing the risk of penalties or audit requests.
Partnering with Medical Bill Gurus allows you to optimize your revenue cycle and improve your bottom line. With our expertise in healthcare coding and billing, you can trust us to handle your billing needs efficiently and effectively.
With Medical Bill Gurus as your billing services partner, you can ensure accurate coding, minimize claim denials, and maximize reimbursement rates. Let us handle your billing needs so that you can focus on providing exceptional care to your patients.
Accurate coding and clean claims are essential for mental health providers to optimize reimbursement in the healthcare industry. Understanding the requirements and documentation for CPT code 99284 is crucial when billing for emergency department visits. Providers can greatly improve coding accuracy and streamline the billing process by utilizing electronic billing software or outsourcing their billing services.
By partnering with a reliable billing company like Medical Bill Gurus, mental health providers can focus on delivering quality care to their patients while ensuring accurate coding and maximizing their revenue cycle. Medical Bill Gurus offers comprehensive billing services, including expertise in medical coding, insurance billing, and claims management. Their streamlined billing process and experience with all insurance payers, including Medicare, ensures accurate coding and optimized reimbursement for mental health providers.
Optimizing the coding and claims process for CPT code 99284 through accurate documentation, electronic billing software, or outsourcing billing services can lead to increased clean claims and improved hospital reimbursement. Providers should prioritize clean claims and accurate coding to minimize claim denials, penalties, and financial complications. By following best practices and partnering with trusted billing services, mental health providers can navigate the complexities of medical billing and focus on their core mission of delivering excellent patient care.
What is CPT code 99284?
CPT code 99284 represents an emergency department visit for the evaluation and management of a patient. It requires a detailed history, examination, and moderate complexity medical decision making.
What are CPT codes used for in medical billing?
CPT codes are used to accurately describe and bill for services provided in the healthcare field, including diagnostic testing, procedures, evaluations, and ancillary services.
Why are clean claims important for reimbursement?
Clean claims, which are approved after the first submission, are crucial for timely reimbursement and effective revenue cycle management.
What are the other codes related to CPT code 99284?
Other codes related to CPT code 99284 include CPT code 99281, 99282, 99283, and 99285, which capture different levels of evaluation and management for emergency department visits.
How can providers improve their coding and claims process for CPT code 99284?
Providers can improve their coding and claims process by utilizing electronic billing software, which can streamline the billing process and increase coding accuracy.
Are there managed billing services available for mental health providers?
Yes, managed billing services like Medical Bill Gurus offer specialized expertise in medical coding, billing, and claims management for mental health providers.
What are the consequences of incorrect coding?
Incorrect coding can lead to claim denials, penalties, alterations in reimbursement rates, and other financial complications for providers.
What rules and guidelines should providers comply with when billing CPT code 99284?
Providers should comply with insurance company rules, including restrictions on the use of CPT codes for specific places of service such as the emergency department.
What are the best practices for mental health coding and billing?
Mental health providers can consider investing in medical coding training for their staff or outsourcing their coding and billing needs to a third-party agency to ensure accuracy and efficiency.
What documentation is required for accurate coding of CPT code 99284?
Providers must ensure proper documentation of the patient’s history, examination, and medical decision making to support the level of complexity required for CPT code 99284.
How can Medical Bill Gurus benefit healthcare providers?
Medical Bill Gurus offers comprehensive billing services, including expertise in medical coding, insurance billing, and claims management, to maximize reimbursement for healthcare providers.
Why is accurate coding and clean claims important in medical billing?
Accurate coding and clean claims are essential for optimal reimbursement and revenue cycle management in the healthcare industry.
Leave a Comment Cancel Reply
Your email address will not be published. Required fields are marked *

AVAILABLE MON-FRI
From 8 am to 8 pm mst, houston office:.
525 N Sam Houston Pkwy E, Suite #246 Houston, Texas, 77060
Denver Office:
3000 Lawrence Street Suite #15 Denver, CO 80205
Tampa Office:
260 1st Ave S, #34 St Petersburg, Florida 33701
Phoenix Office:
7042 E Indian School Rd #100 Scottsdale, AZ 85251
Copyright © 2024 | All Rights Reserved | Medical Billing Company | XML Sitemap | Privacy Policy | Cookie Policy | HIPPA Compliance Policy
Digital Marketing by Denver Digital Marketing Agency

What Is CPT Code 99284 & How To Know When To Use It

Errors in medical billing codes tend to be one of the most common reasons that a claim is denied or rejected by mental and behavioral health payers. Not only can this lead to massive delays and inconsistencies in your practice’s revenue stream, but it can cause other long-term complications.
A solo practitioner or a small practice that has frequent medical coding errors can sometimes draw a red flag from a private insurance company, public health institution, or another type of payer organization. These red flags can sometimes lead to audits that waste your practice’s valuable time. In some cases, it can even draw penalties or alterations in your practice’s reimbursement rate from that payer institution.
Of course, the overall memorization requirements and correct application of CPT codes can be immense. Especially for providers who don’t have an in-house administrative staff or a third-party medical billing agency to handle their coding needs. This is part of what makes insurance billing so complicated for solo practitioners and small practices.
Being able to use every CPT code in the correct context will factor into a provider’s ability to produce clean claims. This in turn leads to a more consistent revenue cycle. Yet with so many different CPT codes, it can be difficult to know exactly when to apply each one for each instance and case.
Consequences Of Coding & Medical Billing Errors
There are a lot of potential consequences that come with incorrect coding that goes beyond simply forfeiting reimbursements. It’s a well-known fact that insurance companies and public health institutions are always on the lookout for potential fraud. Over the years it has made them prone to seeking out any opportunity to deny a provider’s claim for reimbursement.
The term “Clean Claim” is for medical billing claims that are approved with the first submission. Clean claims are the ideal scenario for any provider or small practice working with insurance. It essentially means they will be reimbursed in a timely manner thanks to their diligent insurance billing practices.
Of course, the foundation of a truly clean claim is the CPT codes used to generate their claim. Accuracy in this area is a major factor in getting the claim paid promptly, avoiding costly audits, as well as maximizing your potential for negotiating higher reimbursement rates from a payer institution in the future.
Current Procedural Terminology (CPT) is used to reflect a wide range of factors. This includes:
- Diagnostic Testing
- Evaluations
- Ancillary Services Provided
CPT codes are used for a wide range of patients in many disciplines. This included medical, surgical, general healthcare, imaging diagnostics, mental healthcare, and a wide range of behavioral health fields.
Fortunately, there are several different ways that solo practitioners, small practices, and specialist providers can refine their coding and claims process to optimize their clean claims. Especially for mental health providers who frequently need to use CPT code 99284. Knowing precisely when and how to use it, as well as what tools you can use it for, will go a long way toward increasing the number of clean claims your practice has approved.
What Is CPT Code 99284 & How To Use It?
CPT code 99284 is just one part of a set of codes that are often used to describe emergency department visits. This includes the evaluation and management of a specific patient.
CPT code 99284 is defined in the official CPT code book manual as being for “Emergency department visit for the evaluation and management of a patient, which requires these 3 key components.”
- Component 1: Must include a detailed history
- Component 2: Requires a detailed examination
- Component 3: Clearly delineated medical decision-making of a moderate complexity
A lot of times counseling and coordination of care with other physicians, qualified health care professionals, diagnosticians, specialist providers, or agencies happen with consistency. Most of the time, the presenting problem is of high severity, which then requires urgent evaluation by the physician or some other type of qualified health care professional. Even if it doesn’t pose an immediate or significant threat to life or the individual’s physiologic function.
Many critical details need to be included any time you use CPT Code 99284. This includes the history collected, the detail in the examination, and the level or the complexity of the decision-making process.
Common Codes Used in Conjunction with CPT Code 99284
Of course, CPT code 99284 is rarely standalone in most emergency situations. It often occurs with other codes, and the details linking these codes with the prevailing condition also need to be accurate to generate a truly clean claim that will get approved with the first submission.
CPT Code 99281
CPT Code 99281 is one of the more common codes used in conjunction with Code 99284. It can be used to denote several things such as:
- Problem Focused History
- Problem Focused Examination
- Straightforward Medical Decision Making
- Presenting Problem Is Usually Minor
CPT Code 99282
CPT Code 99282 is another common code used with clean claims involving Code 99284. It must include:
- Expanded Problem-Focused History
- Expanded Problem-Focused Examination
- Medical Decision-Making of Low Complexity
- Problem is Usually Low Severity
CPT Code 99283
With CPT Code 99283, the severity of the problem is typically higher. This code includes:
- Medical Decision Making of Moderate Complexity
- Problem is Usually Moderate Severity
CPT Code 99285
CPT Code 99285 is also used for emergency department visits for the evaluation and management of a patient. It also requires 3 key components to generate a clean claim. Though there are specific constraints imposed by the urgency of the patient’s clinical condition or their current mental status. It requires the provider to include:
- A Comprehensive History
- A Comprehensive Examination
- The Medical Decision Making of High Complexity
The Problem Also Needs To Be Usually of High Severity/Poses an Immediate/Significant Threat to Life or Physiologic Function
Ways to Improve Mental Health Coding & Billing Practices
A lot of mental health care providers and ABA specialists only receive a minimal level of training in medical coding and billing practices. This only makes sense as their focus rightly should be on treating their patients. Fortunately, there are a few things you can do to ensure that you are using CPT Code 99284 and other important medical billing codes correctly.
This includes things like using up-to-date medical coding & billing software. Hiring an in-house administrative staff to specialize in medical coding, billing, and claims management.
Though a lot of small practices and solo practitioners find that outsourcing their medical coding and billing practices to a third-party agency like Operant Billing Solutions is the ideal way to ensure that all CPT codes are correctly entered when submitting a clean claim.
You can trust our experts to turn a keen eye toward making sure all aspects of your claim are coded and submitted correctly. This frees you and any in-house staff you have to focus on providing the highest level of care to your patients, as well as giving you more time to explore ways to expand your practice in the long term.

Related Posts

Optimizing ABA Practice Management: Using Analytics for Data-Driven Decisions

Using QuickBooks for ABA Therapy Billing: Benefits and Limitations

Improving Authorization Management in ABA Therapy: A Path to Financial Health and Client Success

Navigating Anti-Kickback Laws: Compliance For Your Practice

Scaling Beyond the 3-5 Million Revenue Mark: A Blueprint for ABA Therapy Companies
- Testimonials
Our Services
- Enrollment Services / Credentialing
- Claims Management Services
- Revenue Cycle Management Services
- Eligibility and Benefits Verification
- CentralReach Outsourced Billing Solutions
- Enterprise Billing Management Solutions
Practitioners We Help
- (BCBA) Board Certified Behavior Analysts
- Counselors (LPC/LMHC/NCC)
- Marriage and Family Therapist
- Occupational Therapists
- Psychologist / Mental Health
- Physical Therapist
- Social Worker
- (SLP) Speech-Language Pathologists
Operant Billing Solutions
We make getting paid simple, schedule a free consultation, 20+ years of billing expertise.
2023 Documentation Guideline Changes for ED E/M Codes 99281-99285

On July 1, 2022, the American Medical Association (AMA) released a preview of the 2023 CPT Documentation Guidelines for Evaluation and Management (E/M) services. These changes reflect a once-in-a-generation restructuring of the guidelines for choosing a level of emergency department (ED) E/M visit impacting roughly 85 percent of the relative value units (RVUs) for typical members. Since 1992, a visit level was based on a combination of history, physical exam, and medical decision-making elements. Beginning in 2023, the emergency department E/M services will be based only on medical decision making.
You Might Also Like
- Documentation Pearls for Navigating Abscess Incision/Drainage Codes
- ICD-10 Diagnosis Codes to Use for Zika Virus Documentation
- Avoid Patient History Documentation Errors in Medical Coding
Explore This Issue
The American College of Emergency Physicians (ACEP) represents the specialty in the AMA current procedural technology (CPT) and AMA/Specialty Society RVS Update Committee (RUC) processes. In fact, they are your only voice in those arenas. The AMA convened a joint CPT/RUC work group to refine the guidelines based on accepted guiding principles. Although the full CPT code set for 2023 has not yet been released, the AMA recognized that specialties needed to have access to the documentation guidelines changes early to educate both their physicians on what to document and their coders on how to extract the elements needed to determine the appropriate level of care based on chart documentation. Additionally, any electronic medical record or documentation template changes will need to be in place prior to January 1, 2023, to maintain efficient cash flows and ensure appropriate code assignment.
ACEP was able to convince the Joint CPT/RUC Workgroup that time should not be a descriptive element for choosing ED levels of service because emergency department services are typically provided on a variable intensity basis, often involving multiple encounters with several patients over an extended period of time. It would be nearly impossible to track accurate times spent on every patient under concurrent active management.
The prior requirements to document a complete history and physical examination will no longer be deciding factors in code selection in 2023, but instead the 2023 Guidelines simply require a medically appropriate history and physical exam. That leaves medical decision making as the sole factor for code selection going forward. These changes are illustrated by the 2023 ED E/M code descriptors, which will appear as follows:
The 2023 E/M definitions have been updated to reflect simply Medical Decision Making determining the level.
- 99281: ED visit for the evaluation and management of a patient that may not require the presence of a physician or other qualified health care professional.
- 99282: ED visit for the evaluation and management of a patient, which requires a medically appropriate history and/or examination and straightforward medical decision making.
- 99283: ED visit for the evaluation and management of a patient, which requires a medically appropriate history and/or examination and low medical decision making.
- 99284: ED visit for the evaluation and management of a patient which requires a medically appropriate history and/or examination and moderate medical decision making.
- 99285: ED visit for the evaluation and management of a patient, which requires a medically appropriate history and/or examination and high medical decision making.
Pages: 1 2 3 | Single Page
Topics: 2023 guidelines Coding CPT guidelines Practice Management Reimbursement & Coding

Uncovering Hidden ACEP Member Resource Gems

Medicare’s Reimbursement Updates for 2024

Workplace Violence and Mental Health in Emergency Medicine
Current issue.
ACEP Now: Vol 43 – No 05 – May 2024
Download PDF
No Responses to “2023 Documentation Guideline Changes for ED E/M Codes 99281-99285”
Leave a Reply Cancel Reply
Your email address will not be published. Required fields are marked *

- Find a Doctor
Coding and Billing Guidelines for Emergency Department
- Provider Service: 800-368-2312
- For Medicaid Expansion: 833-777-5779
- Caring Foundation
- Privacy & Legal
- Our Partners in Health:
Fargo (Headquarters) 4510 13th Ave. S. Fargo, N.D., 58121
Blue Cross Blue Shield of North Dakota is an independent licensee of the Blue Cross Blue Shield Association, serving residents and businesses in North Dakota. All rights reserved.
© 2024 Blue Cross Blue Shield of North Dakota
- Non-Discrimination Notice
- العَرَبِيَّة
- Diné Bizaad
Processing...
Please wait while your form is being submitted

(2022) CPT Code 99284 | Description, Guidelines & Clinical Examples
This article will define CPT Code 99284, explain the medical necessity to report CPT 99284, and the guidelines and clinical examples of CPT 99284. This article is about the 2022 version of this code. Be aware that this code was revised in 2023.
CPT Code 99284 Description
CPT Code 99284 is defined by the CPT manual as follows (the text in Italic is the official definition of CPT 99284):
“ Emergency department visit for the evaluation and management of a patient, which requires these 3 key components:
Component 1: A detailed history
Component 2: A detailed examination
Component 3: Medical decision making of moderate complexity
Counselling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs.
Usually, the presenting problem(s) are of high severity, and require urgent evaluation by the physician, or other qualified health care professionals but do not pose an immediate significant threat to life or physiologic function. “
No contract is made between new and established Emergency Department (ED) patients. Evaluation and management (E / M) services in the ER category can be noted for any new or established patient presenting for treatment in the ER. Time is also not a detailed component for E / M service levels in the ED because emergency room services are generally provided at varying intensity, often including several encounters with various patients over a long period.
It is often over-ambitious for doctors to estimate the time they spend face-to-face with each patient correctly.
CPT 99284 BCBS Guidelines
Documentation of the patient’s medical history for emergency room (ED) diagnosis and treatment must include current symptoms, diagnoses, and treatment plans.
It must also include a written order from the physician, which must be documented in their medical history.
Medical history and itemized bills may be requested from the provider to assist in the level of care provided.
Medical history and records are used to define the scope of the medical history, the scope of the examination performed, the complexity of medical decision-making (number of diagnoses or treatment options, quantity and/or complexity of the data to be reviewed, and risk of complications), and/or morbidity or mortality) and services provided.
This information about the level of care billed is verified, and its suitability is evaluated.
Below are four billing examples of CPT code 99284.
Emergency department visit for a 4-year-old who fell off a bike sustaining a head injury with brief loss of consciousness.
Emergency department visit for an elderly female who has fallen and is now complaining of pain in her right hip and cannot walk.
Emergency department visit for a patient with flank pain and hematuria.
Emergency department visit for a female presenting with lower abdominal pain and a vaginal discharge.
Similar Posts
Cpt codes for incision procedures on the spine and spinal cord.
Below is a list summarizing the CPT codes for incision procedures on the spine and spinal cord. CPT Code 63170 CPT 63170 describes a laminectomy with myelotomy (e.g., Bischof or DREZ type) of the cervical, thoracic, or thoracolumbar region. CPT Code 63172 CPT 63172 describes laminectomy with an intramedullary cyst/syrinx drainage to the subarachnoid space….
How To Use CPT Code 73503
CPT 73503 describes the radiologic examination of the hip, specifically the unilateral hip, with the inclusion of the pelvis if performed. This article will provide an overview of the code, including its official description, the procedure involved, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information, similar codes, and examples of when CPT 73503…
How To Use CPT Code 27680
CPT 27680 describes the procedure for tenolysis of a single flexor or extensor tendon in the leg and/or ankle. This article will cover the description, official description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 27680? CPT 27680 can be used to describe the…

Change In Inpatient Psychiatric Facility Prospective Payment System
Prior to rate year (RY) 2012, the Inpatient Psychiatric Facility Prospective Payment System (IPF PPS) was on a July 1st – June 30 th annual update cycle. The first update to the IPF PPS occurred on July 1, 2006, and every July 1 thereafter. Effective with RY 2012, the IPF PPS payment rate update period…
How To Use CPT Code 33852
CPT 33852 describes the repair of a hypoplastic or interrupted aortic arch using autogenous or prosthetic material without cardiopulmonary bypass. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 33852? CPT 33852 can be used to describe the repair…
How To Use CPT Code 34530
CPT 34530 describes a procedure known as saphenopopliteal vein anastomosis. This article will cover the official description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 34530? CPT 34530 is a code used to describe the surgical procedure of saphenopopliteal vein anastomosis. This procedure involves…
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

An official website of the United States government
The .gov means it’s official. A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Telehealth for emergency departments
Billing for telehealth in emergency departments.
During the COVID-19 public health emergency, additional emergency care services are covered by Medicare as telehealth. Other related services, such as remote patient monitoring and e-consults, are not considered telehealth for billing purposes, but are reimbursable.
On this page:
Medicare billing guidance, private insurance, have a question.
Below are common codes used to bill for these services. Note: some of these services are temporarily covered during the COVID-19 public health emergency.
Tip: Services provided virtually while the provider and patient are in the same location — for instance, over a tablet from different rooms within a hospital — are not billed as telehealth.
For more details about billing and reimbursement:
- See the complete list of telehealth services covered by Medicare during the public health emergency from the Centers for Medicare & Medicaid Services
While each state is different, most have expanded coverage for telehealth due to COVID-19. Many are now matching Medicare’s telehealth coverage. Check your state’s current laws and reimbursement policies to see what is covered. For updates on COVID-19 reimbursement and related Medicaid codes and procedures for your state, see:
- COVID-19 Related State Actions — from the National Policy Center - Center for Connected Health Policy
- Coverage and Payment of Interprofessional Consultation (PDF) — Centers for Medicare and Medicaid Services
Many code changes for COVID-19 care cover telehealth and include specific information for visits that are video- or audio-only. It is important to note that most states distinguish between reimbursement standards for permanent telehealth policies and temporary COVID-19 reimbursement policies. For tips on coding private insurance claims, see:
- Current State Laws & Reimbursement Policies (Private Payer Laws) — from the National Policy Center - Center for Connected Health Policy
- Coding Scenarios during COVID-19 — from the American Academy of Family Physicians
Contact the staff at the regional telehealth resource center that’s closest to you for help with your telehealth program.
- Billing for telehealth during COVID-19 →

Emergency CPT – 99283, 99284, 99285, 99281, 99282
by Medical Billing | Jan 9, 2013 | CPT modifiers | 1 comment
99283 (CPT G0382) Emergency department visit for the evaluation and management of a patient, which requires these 3 key components: An expanded problem focused history; An expanded problem focused examination; and Medical decision making of moderate complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the presenting problem(s) are of moderate severity.
99284 (CPT G0383) Emergency department visit for the evaluation and management of a patient, which requires these 3 key components: A detailed history; A detailed examination; and Medical decision making of moderate complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the presenting problem(s) are of high severity, and require urgent evaluation by the physician but do not pose an immediate significant threat to life or physiologic function. average fee payment – $110 – $120 Moderate-High Complexity (99284/G0383): The presented problem(s) are of high severity, and require urgent evaluation by the physician but do not pose an immediate significant threat to life or physiologic function. Head injury instructions, crutch training, bending, lifting, weight-bearing limitations, prescription medication with review of side effects and potential adverse reactions; patient may have questions, but otherwise demonstrates adequate understanding of instructions either verbally or by demonstration.
99285 (G0384) Emergency department visit for the evaluation and management of a patient, which requires these 3 key components within the constraints imposed by the urgency of the patient’s clinical condition and/or mental status: A comprehensive history; A comprehensive examination; and Medical decision making of high complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the presenting problem(s) are of high severity and pose an immediate significant threat to life or physiologic function. average fee amount – $170 – $180
99288 Physician direction of emergency medical systems (EMS) emergency care, advanced life support Billing and Coding Guidelines. Medicare requires that modifier –25 always be appended to the emergency department (ED)E/M code (99281-99285) when provided on the same date as a diagnostic medical/surgical and/or therapeutic medical/surgical procedure(s). Example #1: A patient is seen in the ED with complaint of a rapid heartbeat. A 12-lead ECG is performed. In this case, the appropriate code(s) from the following code ranges can be reported: 99281-99285 (Emergency Department Services) with a modifier –25 93005 (Twelve lead ECG) Example #2: A patient is seen in the ED after a fall. Lacerations sustained from the fall are repaired and radiological x-rays are performed. In this case, the appropriate code(s) from the following code ranges can be reported: 99281-99285 (Emergency Department Services) with a modifier –25 12001-13160 (Repair/Closure of the Laceration) 70010-79900 (Radiological X-ray) Example #3: A patient is seen in the ED after a fall, complaining of shoulder pain. Radiological x-rays are performed. In this case, the appropriate code(s) from the following code ranges can be reported: 99281-99285 (Emergency Department Services) with a modifier –25 70010-79900 (Radiological X-ray) NOTE: Using example #3 above, if a subsequent ED visit is made on the same date, but no further procedures are performed, appending modifier –25 to that subsequent ED E/M code is NOT appropriate. However, in this instance, since there are two ED E/M visits to the same revenue center (45X), condition code G0 (zero) must be reported in form locator 24 or the corresponding electronic version of the UB92. Per CPT definition, the codes 99281-99285 are for reporting evaluation and management services in the emergency department. An emergency department is defined as an organized hospital-based facility for the provision of unscheduled episodic services to patients who present for immediate medical attention. The facility must be available 24 hours a day. Based on this definition, codes 99281-99285 will be denied provider liable as incompatible if submitted with any place of service (POS) other than 23.
If my patient is registered in the emergency department and I am asked to see him/her, may I submit the emergency service? Answer: Yes. Any physician seeing a patient registered in the emergency department (ED) may use ED visit codes for services matching the code description. It is not required that the physician be assigned to the ED. If the patient is admitted by this provider, the initial hospital service (CPT codes 99221-99223) with the AI HCPCS modifier would be submitted instead of the ED visit codes. Please keep in mind the service must be medically necessary and the documentation must meet the level of complexity of the service rendered. The following guidelines apply to the ED CPT codes 99281 through 99285 billing: ED service is provided to the patient by both the patient’s personal physician and ED physician. If the ED physician, based on the advice of the patient’s personal physician who came to the ED to see the patient, sends the patient home, then the ED physician should bill the appropriate level of ED service. The patient’s personal physician should also bill the level of ED code that describes the service he or she provided in the ED. If the patient’s personal physician does not come to the hospital to see the patient, but only advises the ED physician by telephone, then the patient’s personal physician may not bill. If the ED physician requests that another physician evaluate a given patient, the other physician should bill an ED visit code. If the patient is admitted to the hospital by the second physician performing the evaluation, he/she should bill an initial hospital care code and not an ED visit code. Overuse and Misuse of CPT Code 99285 The Arizona Healthcare Cost Containment System’s (AHCCCS) Claims Medical Review Unit has noted an increased use of CPT code 99285 on claims for billed emergency room visits. When submitting a claim using CPT code 99285, please document the following: • Comprehensive history • Comprehensive examination • Medical decision for services involving high complexity conditions. Usually the presenting problem(s) are of high severity, are a potential life threatening problem and require the immediate attention of the physician. Services for constipation, earaches and colds, for example, should not be billed using CPT code 99285. AHCCCS will refer any improper billing trends to the Office of the Inspector General.
CPT Code 99285 Emergency Department Visit: Emergency department visit for the evaluation and management of a patient, which requires these 3 key components within the constraints imposed by the urgency of the patient’s clinical condition and/or mental status: • Comprehensive history • Comprehensive examination • Medical decision making of HIGH complexity Comprehensive History: • Reason for admission • Problem pertinent review of systems • Extended history of present illness (HPI) – Includes 4 or more elements of the HPI or the status of at least three chronic or inactive conditions • Review of systems directly related to the problem(s) identified in the HPI • Medically necessary review of ALL body systems’ history • Medically necessary complete past, family, and social history HPI – History of Present Illness: A chronological description of the development of the patient’s present illness from the first sign and/or symptom or from the previous encounter to the present. Descriptions of present illness may include: • Location • Quality • Severity • Timing • Context • Modifying factors • Associated signs/symptoms significantly related to the presenting problem(s) Chief Complaint: The Chief Complaint is a concise statement from the patient describing: • The symptom • Problem • Condition • Diagnosis • Physician recommended return, or other factor that is the reason for the encounter Review of Systems: An inventory of body systems obtained through a series if questions seeking to identify signs and/or symptoms which the patient may be experiencing or has experienced. For purpose of Review of Systems the following systems are recognized: • Constitutional (i.e., fever, weight loss) • Eyes • Ears, Nose, Mouth Throat • Cardiovascular • Respiratory • Gastrointestinal • Genitourinary • Musculoskeletal • Integumentary (skin and/or breast) • Neurologic • Psychiatric • Endocrine • Hematologic/Lymphatic • Allergic/Immunologic Past, Family, and/or Social History (PFSH): Consists of a review of the following: • Past history (patient’s past experiences with illnesses, operations, injuries, and treatments • Family History (a review of medical events in the patient’s family, including diseases which may be hereditary or place the patient at risk) • Social History (an age appropriate review of past and current activities Additional Information: • Medicare Providers are responsible for assuring that visits are coded accurately; the unique provider number used when a service is billed ensures that the provider has reviewed and authenticated the accuracy of everything on the submitted claim. • Clearly document your clinical perception of the patient’s condition to assure claims are submitted with the correct level of service. • Comorbidities and other underlying diseases in and of themselves are not considered when selecting the E/M codes UNLESS their presence significantly increases the complexity of the medical decision making. • Practitioner’s choosing to use time as the determining factor: – MUST document time in the patient’s medical record – Documentation MUST support in sufficient detail the nature of the counseling – Code selection based on total time of the face-to-face encounter (floor time), the medical record MUST be documented in sufficient detail to justify the code selection Coding Guidelines Evaluation and management services including new or established patient office or other outpatient services (99201-99215), emergency department services (99281-99285), nursing facility services (99304-99318), domiciliary, rest home, or custodial care services (99324-99337), home services (99341-99350), and preventive medicine services (99381-99397) on the same date related to the admission to “observation status” should not be reported separately.” Exceptions to Modifier 59 Override: The Health Plan has determined that there are certain circumstances which are exempt from modifier 59 overriding an unbundling edit, or that there are circumstances in which appending modifier 59 to a code is inappropriate. The following is a list of some, but not all of the circumstances, in which appending modifier 59 to a CPT/HCPCS code will not cause the override of the applicable edit, and will not allow for separate reimbursement (See also our Screening Services with Evaluation & Management Services and our Bundled Services and Supplies reimbursement policies.): • Duplicate coding • Services and supplies specified in the Bundled Services and Supplies Policy • E/M or DME item codes • National Correct Coding Initiative (NCCI) edit code pairs with a ‘superscript’ of zero, or a modifier allowance indicator of zero. • In addition, modifier 59 will not override an edit, and will not allow for separate reimbursement for the first code(s) listed in the following code to code relationship examples: 700XX-788XX, G01XX-G03XX, S8035-S8092, and S9024 (These code ranges include all applicable radiology interpretation codes, as well as radiology codes with modifier 26) reported with 99221-99233 and 99281-99285* 93010, 93018, 93042, 93303, 93307-93308, 93312-93318, 93320-93321, 93325, 93350-93352, and 0180T reported with 99281-99285 Modifier 25 Guidelines 1. Should a separately identifiable E/M service be provided on the same date that a diagnostic and/or therapeutic procedure(s) is performed, information substantiating the E/M service must be clearly documented in the patient’s medical record, to justify use of the modifier –25. 2. Modifier –25 may be appended only to E/M service codes and then only for those within the range of 99201-99499. For outpatient services paid under OPPS, the relevant code ranges are: 99201-99215 (Office or Outpatient Services) 99281-99285 (Emergency Department Services) 99291 (Critical Care Services) 99241-99245 (Office or Other Outpatient Consultations) NOTE: For the reporting of services provided by hospital outpatient departments, off-site provider departments, and provider-based entities, all references in the code descriptors to “physician” are to be disregarded. Example: A patient reports for pulmonary function testing in the morning and then attends the hypertension clinic in the afternoon. The pulmonary function tests are reported without an E/M service code. However, an E/M service code with the modifier –25 appended should be reported to indicate that the afternoon hypertension clinic visit was not related to the pulmonary function testing. 3. Medicare requires that modifier –25 always be appended to the emergency department (ED)E/M code (99281-99285) when provided on the same date as a diagnostic medical/surgical and/or therapeutic medical/surgical procedure(s). Example #1: A patient is seen in the ED with complaint of a rapid heartbeat. A 12-lead ECG is performed. In this case, the appropriate code(s) from the following code ranges can be reported: 99281-99285 (Emergency Department Services) with a modifier –25 93005 (Twelve lead ECG) 045X 99281-99285, 99291 Emergency visit hospital billing UB 04 *Revenue codes have not been identified for these procedures, as they can be performedin a number of revenue centers within a hospital, such as emergency room (0450), operating room (0360), or clinic (0510). Hospitals are to report these HCPCS codes under the revenue center where they were performed. EXAMPLE 1 If a patient receives a laboratory service on May 1st and has an emergency room (ER) visit on the same day, two separate bills may be submitted since the laboratory service is paid under the clinical diagnostic laboratory fee schedule and not subject to OPPS. In this situation, the laboratory service was not related to the ER visit or done in conjunction with the ER visit. EXAMPLE 2 If a patient was seen in the emergency room (ER) and the same patient received nonpartial hospitalization psychological services on the same day as well as several other days in the month, the provider should report the ER visit on the monthly repetitive claim along with the psychological services, since both services are paid under OPPS. Days after the date covered services ended, such as noncovered level of care, or emergency services after the emergency has ended in nonparticipating institutions; • Days for which no Part A payment can be made because the patient was on a leave of absence and was not in the hospital. • Days for which no Part A payment can be made because a hospital whose provider agreement has terminated, expired, or been cancelled may be paid only for covered inpatient services during the limited period following such termination, expiration, or cancellation. All days after the expiration of the period are noncovered. See Chapter 3 for determining the effective date of the limited period and for billing for Part B services; and • Days after the time limit when utilization is not chargeable because the beneficiary is at fault. FL 19 – Type of Admission/Visit Required on inpatient bills only. This is the code indicating priority of this admission. Code Structure: 1 Emergency – The patient required immediate medical intervention as a result of severe, life threatening or potentially disabling conditions. Generally, the patient was admitted through the emergency room. 2 Urgent- The patient required immediate attention for the care and treatment of a physical or mental disorder. Generally, the patient was admitted to the first available, suitable accommodation. 3 Elective – The patient’s condition permitted adequate time to schedule the availability of a suitable accommodation. FL 20 – Source of Admission Required For Inpatient Hospital. The provider enters the code indicating the source of this admission or outpatient registration. Code Structure (For Emergency, Elective, or Other Type of Admission): 1 Physician Referral Inpatient: The patient was admitted to this facility upon the recommendation of their personal physician. Outpatient: The patient was referred to this facility for outpatient or referenced diagnostic services by their personal physician or the patient independently requested outpatient services (self-referral). 2 Clinic Referral Inpatient: The patient was admitted to this facility upon the recommendation of this facility’s clinic physician. Outpatient: The patient was referred to this facility for outpatient or referenced diagnostic services by this facility’s clinic or other outpatient department physician. 3 HMO Referral Inpatient: The patient was admitted to this facility upon the recommendation of a HMO physician. Outpatient: The patient was referred to this facility for outpatient or referenced diagnostic services by a HMO physician. 4 Transfer from a Hospital Inpatient: The patient was admitted to this facility as a transfer from an acute care facility where they were an inpatient Outpatient: The patient was referred to this facility for outpatient or referenced diagnostic services by a physician of another acute care facility. 5 Transfer from a SNF Inpatient: The patient was admitted to this facility as a transfer from a SNF where they were an inpatient. Outpatient: The patient was referred to this facility for outpatient or referenced diagnostic services by a physician of the SNF where they are an inpatient. 6 Transfer from Another Health Care Facility Inpatient: The patient was admitted to this facility from a health care facility other than an acute care facility or SNF. This includes transfers from nursing homes, long term care facilities and SNF patients that are at a nonskilled level of care. Outpatient: The patient was referred to this facility for outpatient or referenced diagnostic services by a physician of another health care facility where they are an inpatient. 7 Emergency Room Inpatient: The patient was admitted to this facility upon the recommendation of this facility’s emergency room physician. Outpatient: The patient received services in this facility’s emergency department. 8 Court/Law Enforcement Inpatient: The patient was admitted to this facility upon the direction of a court of law, or upon the request of a law enforcement agency representative. Outpatient: The patient was referred to this facility upon the direction of a court of law, or upon the request of a law enforcement agency representative for outpatient or referenced diagnostic services. 9 Information Not Available Inpatient: The means by which the patient was admitted to this facility is not known. Outpatient: For Medicare outpatient bills, this is not a valid code. A Transfer from a Critical Access Hospital (CAH) Inpatient: The patient was admitted to this facility as a transfer from a CAH where they were an inpatient. Outpatient: The patient was referred to this facility for outpatient or referenced diagnostic services by (a physician of) the CAH were the patient is an inpatient. Code Title Definition 44 Inpatient Admission Changed to Outpatient For use on outpatient claims only, when the physician ordered inpatient services, but upon internal utilization review performed before the claim was originally submitted, the hospital determined that the services did not meet its inpatient criteria. Effective April 1, 2004 45 Reserved for national assignment 46 Non-Availability Statement on File A nonavailability statement must be issued for each TRICARE claim for nonemergency inpatient care when the TRICARE beneficiary resides within the catchment area (usually a 40-mile radius) of a Uniformed Services Hospital. 47 Reserved for TRICARE Code Title Definition 59 Non-primary ESRD Facility Code indicates that ESRD beneficiary received non-scheduled or emergency dialysis services at a facility other than his/her primary ESRD dialysis facility. 60 Operating Cost Day Outlier Day Outlier obsolete after FY 1997. (Not reported by providers, not used for a capital day outlier.) PRICER indicates this bill is a length-of-stay outlier. The FI indicates the cost outlier portion paid value code 17. AM Non-emergency Medically Necessary Stretcher Transport Required For ambulance claims. Non-emergency medically necessary stretcher transport required. Effective 10/16/03 AN Preadmission Screening Not Required Person meets the criteria for an exemption from preadmission screening. Effective 1/1/04 G0 Distinct Medical Visit Report this code when multiple medical visits occurred on the same day in the same revenue center. The visits were distinct and constituted independent visits. An example of such a situation would be a beneficiary going to the emergency room twice on the same day, in the morning for a broken arm and later for chest pain. Proper reporting of Condition Code G0 allows for payment under OPPS in this situation. The OCE contains an edit that will reject multiple medical visits on the same day with the same revenue code without the presence of Condition Code G0. Code Title Definition A4 Covered Self-Administrable Drugs – Emergency The amount included in covered charges for self-administrable drugs administered to the patient in an emergency situation. (The only covered Medicare charges for an ordinarily noncovered, selfadministered drug are for insulin administered to a patient in a diabetic coma. 045X Emergency Room Charges for emergency treatment to those ill and injured persons who require immediate unscheduled medical or surgical care. Rationale: Permits identification of particular items for payers. Under the provisions of the Emergency Medical Treatment and Active Labor Act (EMTALA), a hospital with an emergency department must provide, upon request and within the capabilities of the hospital, an appropriate medical screening examination and stabilizing treatment to any individual with an emergency medical condition and to any woman in active labor, regardless of the individual’s eligibility for Medicare (Consolidated Omnibus Budget Reconciliation Act (COBRA) of 1985). Subcategory Standard Abbreviations 0 – General Classification EMERG ROOM 1 – EMTALA Emergency Medical screening services ER/EMTALA 2 – ER Beyond EMTALA Screening ER/BEYOND EMTALA 6 – Urgent Care URGENT CARE 9 – Other Emergency Room OTHER EMER ROOM 051X Clinic Clinic (nonemergency/scheduled outpatient visit) charges for providing diagnostic, preventive, curative, rehabilitative, and education services to ambulatory patients.Rationale: Provides a breakdown of some clinics that hospitals or third party payers may require. Subcategory Standard Abbreviations 0 – General Classification CLINIC 1 – Chronic Pain Center CHRONIC PAIN CL 2 – Dental Clinic DENTAL CLINIC 3 – Psychiatric Clinic PSYCH CLINIC Usage Notes: 1. To be used by trauma center/hospitals as licensed or designated by the state or local government authority authorized to do so, or as verified by the American College of Surgeons and involving a trauma activation. 2. Revenue Category 068X is used for patients for whom a trauma activation occurred. A trauma team activation/response is a “Notification of key hospital personnel in response to triage information from pre-hospital caregivers in advance of the patient’s arrival.” 3. Revenue Category 068X is for reporting trauma activation costs only. It is an activation fee and not a replacement or a substitute for the emergency room visit fee; if trauma activation occurs, there will normally be both a 045X and 068X revenue code reported. 4. Revenue Category 068X is not limited to admitted patients. 5. Revenue Category 068X must be used in conjunction with FL 19 Type of Admission/Visit code 05 (“Trauma Center”), however FL 19 Code 05 can be used alone. 098X Professional Fees – Extension of 096X & 097X Subcategory Standard Abbreviations 1 – Emergency Room PRO FEE/ER 2 – Outpatient Services PRO FEE/OUTPT 3 – Clinic PRO FEE/CLINIC 4 – Medical Social Services PRO FEE/SOC SVC 5 – EKG PRO FEE/EKG 6 – EEG PRO FEE/EEG 7 – Hospital Visit PRO FEE/HOS VIS 8 – Consultation PRO FEE/CONSULT 9 – Private Duty Nurse FEE/PVT NURSE • Accommodations – 0100s – 0150s, 0200s, 0210s (days) • Blood pints – 0380s (pints) • DME – 0290s (rental months) • Emergency room – 0450, 0452, and 0459 (HCPCS code definition for visit or procedure) • Clinic – 0510s and 0520s (HCPCS code definition for visit or procedure) • Dialysis treatments – 0800s (sessions or days) • Orthotic/prosthetic devices – 0274 (items) • Outpatient therapy visits – 0410, 0420, 0430, 0440, 0480, 0900, and 0943 (Units are equal to the number of times the procedure/service being reported was performed.) • Outpatient clinical diagnostic laboratory tests – 030X-031X (tests) • Radiology – 032x, 034x, 035x, 040x, 061x, and 0333 (HCPCS code definition of tests or services) • Oxygen – 0600s (rental months, feet, or pounds) • Drugs and Biologicals- 0636 (including hemophilia clotting factors) If the patient is self-referred (e.g., emergency room or clinic visit), the provider enters SLF000 in the first six positions, and does not enter a name FL19 – Type of Admission a. One numeric position. b. Required only if the type of bill is 11X or 41X. c. Valid codes are: 1 Emergency 2 Urgent 3 Elective 9 Information unavailable c. Valid codes are: 1. Physician referral 2. Clinic referral 3. HMO referral 4. Transfer from a hospital 5. Transfer from a SNF 6. Transfer from another health care facility 7. Emergency room 8. Court/Law enforcement 9. Information not available A. Inpatient – Patient admitted to this facility as an inpatient transfer from a CAH. Outpatient – Patient referred to this facility for outpatient or referenced diagnostic services by (a physician of) the CAH where the patient is an inpatient. B. Patient admitted to this HHA as a transfer from another HHA. C. Patient readmitted to this HHA within the same home health episode period.
Reimbursement for emergency inpatient hospital services is permitted only for those periods during which the patient’s state of injury or disease is such that a health or life-endangering emergency existed and continued to exist, requiring immediate care that could be provided only in a hospital. The allegation that an emergency existed must be substantiated by sufficient medical information from the physician or hospital. If the physician’s statement does not provide it, or is not supplemented by adequate clinical corroboration of this allegation, it does not constitute sufficient evidence. Death of the patient does not necessarily establish the existence of a medical emergency, since in some chronic, terminal illnesses, time is available to plan admission to a participating hospital. The lack of adequate care at home or lack of transportation to a participating hospital does not constitute a reason for emergency hospital admission, without an immediate threat to the life and health of the patient. Since the existence of medical necessity for emergency services is based upon the physician’s assessment of the patient prior to admission, serious medical conditions developing after a non-emergency admission are not “emergencies” under the emergency services provisions of the Act. The emergency ceases when it becomes safe, from a medical standpoint, to move the individual to a participating hospital, another institution, or to discharge the individual. Emergency Medical Condition Federal Medicaid regulations define an emergency medical condition (including emergency labor and delivery) as a sudden onset of a physical or mental condition which causes acute symptoms, including severe pain, where the absence of immediate medical attention could reasonably be expected to: ** Place the person’s health in serious jeopardy; or ** Cause serious impairment to bodily functions; or ** Cause serious dysfunction of any bodily organ or part.
B. Criteria Since the decision that a medical emergency existed can be a matter of subjective medical judgment involving the entire gamut of disease and accident situations, it is impossible to provide arbitrary guidelines. 1. Diagnosis is Considered “Usually an Emergency” An emergency condition is an unanticipated deterioration of a beneficiary’s health which requires the immediate provision of inpatient hospital services because the patient’s chances of survival, or regaining prior health status, depends upon the speed with which medical or surgical procedures are, or can be, applied. While many diagnoses (e.g., myocardial infarction, acute appendicitis) are normally considered emergencies, the hospital must check medical documentation for internal consistencies (e.g., signs and symptoms upon admission, notations concerning changes in a preexisting condition, results of diagnostic tests). EXAMPLE: If the diagnosis is given as “coronary,” the physician’s statement is “coronary,” without further explanatory remarks, and the statement of services rendered gives no indication that an electrocardiogram was taken, or that the patient required intensive care, etc., further information is required. On the other hand, if the diagnosis is one that ordinarily indicates a medical and/or surgical emergency, and the treatment, diagnostic procedures, and period of hospitalization are consistent with the diagnosis, further documentation may be unnecessary. An example is: admitting diagnosis – appendicitis; discharge diagnosis – appendicitis; surgical procedures – appendectomy; period of inpatient stay – 7 days. 2. Patient Dies During Hospitalization If an emergency existed at the time of admission and the patient subsequently expires, the claim is allowed for emergency services if the period of coverage is reasonable. However, death of the patient is not prima facie evidence that an emergency existed; e.g., death can occur as a result of elective surgery or in the case of a chronically ill patient who has a long terminal hospitalization. Such claims are denied. 3. Patient’s Physician Does Not Have Staff Privileges at a Participating Hospital The fact that the beneficiary’s attending physician does not have staff privileges at a participating hospital has no bearing on the emergency services determination. If the lack of staff privileges in an accessible participating hospital is the governing factor in the decision to admit the beneficiary to an “emergency hospital,” the claim is denied irrespective of the seriousness of the medical situation. 4. Beneficiary Chooses to be Admitted to a Nonparticipating Hospital The claim is denied if the beneficiary chooses to be admitted to a non-participating hospital as a personal preference (e.g., participating hospital is on the other side of town) when a bed for the required service is available in an accessible, participating hospital. 5. Beneficiary Cannot be Cared for Adequately at Home The patient who cannot be cared for adequately at home does not necessarily require emergency services. The claim is denied in the absence of an injury, the appearance of a disease or disorder, or an acute change in a pre-existing disease state which poses an immediate threat to the life or health of the individual and which necessitates the use of the most accessible hospital equipped to furnish emergency services. 6. Lack of Suitable Transportation to a Participating Hospital Lack of transportation to a participating hospital does not, in and of itself, constitute a reason for emergency services. The availability of suitable transportation can be considered only when the beneficiary’s medical condition contraindicates taking the time to arrange transportation to a participating hospital. The claim is denied if there is no immediate threat to the life or health of the individual, and time could have been taken to arrange transportation to a participating hospital. 7. “Emergency Condition” Develops Subsequent to a Non-emergency Admission to a Nonparticipating Hospital Program payment cannot be made for emergency services furnished by a nonparticipating hospital when the emergency condition arises after a non-emergency admission. An example: treatment of postoperative complications following an elective surgical procedure or treatment of a myocardial infarction that occurred during a hospitalization for an elective surgical procedure. The existence of medical necessity for emergency services is based upon the physician’s initial assessment of the apparent condition of the patient at the time of the patient’s arrival at the hospital, i.e., prior to admission. 8. Additional “Emergency Condition” Develops Subsequent to an Emergency Admission to a Nonparticipating Hospital If the patient enters a nonparticipating hospital under an emergency situation and subsequently has other injuries, diseases or disorders, or acute changes in preexisting disease conditions, related or unrelated to the condition for which the patient entered, which pose an immediate threat to life or health, emergency services coverage continues. Emergency services coverage ends when it becomes safe from a medical standpoint to move the patient to an available bed in a participating institution or to discharge the patient, whichever occurs first. Emergency Medical Condition An illness, injury, symptom (including severe pain), or condition severe enough to risk serious danger to your health if you didn’t get medical attention right away. If you didn’t get immediate medical attention you could reasonably expect one of the following: 1) Your health would be put in serious danger; or 2) You would have serious problems with your bodily functions; or 3) You would have serious damage to any part or organ of your body. Emergency Medical Transportation Ambulance services for an emergency medical condition. Types of emergency medical transportation may include transportation by air, land, or sea. Your plan may not cover all types of emergency medical transportation, or may pay less for certain types. Emergency Room Care / Emergency Services Services to check for an emergency medical condition and treat you to keep an emergency medical condition from getting worse. These services may be provided in a licensed hospital’s emergency room or other place that provides care for emergency medical conditions. Urgent Care Care for an illness, injury, or condition serious enough that a reasonable person would seek care right away, but not so severe as to require emergency room care. MISUTILIZATION OF EMERGENCY DEPARTMENT SERVICES Criteria include, but are not limited to, the following: ** More than three emergency department visits in one quarter. ** Repeated emergency department visits with no follow-up with a primary care provider (PCP) or specialist when appropriate. ** More than one outpatient hospital emergency department facility in one quarter. ** Repeated emergency department visits for non-emergent conditions. Emergency Department Visits (Codes 99281 – 99288) A.Use of Emergency Department Codes by Physicians Not Assigned to Emergency Department Any physician seeing a patient registered in the emergency department may use emergency department visit codes (for services matching the code description). It is not required that the physician be assigned to the emergency department. B.Use of Emergency Department Codes In Office Emergency department coding is not appropriate if the site of service is an office or outpatient setting or any sight of service other than an emergency department. The emergency department codes should only be used if the patient is seen in the emergency department and the services described by the HCPCS code definition are provided. The emergency department is defined as an organized hospital-based facility for the provision of unscheduled or episodic services to patients who present for immediate medical attention. C.Use of Emergency Department Codes to Bill Nonemergency Services Services in the emergency department may not be emergencies. However the codes (99281 – 99288) are payable if the described services are provided. However, if the physician asks the patient to meet him or her in the emergency department as an alternative to the physician’s office and the patient is not registered as a patient in the emergency department, the physician should bill the appropriate office/outpatient visit codes. Normally a lower level emergency department code would be reported for a nonemergency condition. D.Emergency Department or Office/Outpatient Visits on Same Day As Nursing Facility Admission Emergency department visit provided on the same day as a comprehensive nursing facility assessment are not paid. Payment for evaluation and management services on the same date provided in sites other than the nursing facility are included in the payment for initial nursing facility care when performed on the same date as the nursing facility admission. E.Physician Billing for Emergency Department Services Provided to Patient by Both Patient’s Personal Physician and Emergency Department Physician If a physician advises his/her own patient to go to an emergency department (ED) of a hospital for care and the physician subsequently is asked by the ED physician to come to the hospital to evaluate the patient and to advise the ED physician as to whether the patient should be admitted to the hospital or be sent home, the physicians should bill as follows: *If the patient is admitted to the hospital by the patient’s personal physician, then the patient’s regular physician should bill only the appropriate level of the initial hospital care (codes 99221 – 99223) because all evaluation and management services provided by that physician in conjunction with that admission are considered part of the initial hospital care when performed on the same date as the admission. The ED physician who saw the patient in the emergency department should bill the appropriate level of the ED codes. *If the ED physician, based on the advice of the patient’s personal physician who came to the emergency department to see the patient, sends the patient home, then the ED physician should bill the appropriate level of emergency department service. The patient’s personal physician should also bill the level of emergency department code that describes the service he or she provided in the emergency department. If the patient’s personal physician does not come to the hospital to see the patient, but only advises the emergency department physician by telephone, then the patient’s personal physician may not bill. F.Emergency Department Physician Requests Another Physician to See the Patient in Emergency Department or Office/Outpatient Setting If the emergency department physician requests that another physician evaluate a given patient, the other physician should bill an emergency department visit code. If the patient is admitted to the hospital by the second physician performing the evaluation, he or she should bill an initial hospital care code and not an emergency department visit code.
Reimbursement Information:BCBS guidelines
The patient’s medical record documentation for diagnosis and treatment in the Emergency Department (ED) must indicate the presenting symptoms, diagnoses and treatment plan and a written order by the physician should be clearly documented in the medical record. Medical records and itemized bills may be requested from the provider to support the level of care that is rendered. Medical records will be used to determine the extent of history, extent of examination performed, complexity of medical decision making (number of diagnoses or management options, amount and/or complexity of data to be reviewed and risk of complications and/or morbidity or mortality) and services rendered. This information will be reviewed in conjunction with the level of care billed and evaluated for appropriateness.
Applicable service codes: Revenue code 450 and/or one of the following procedure codes 99281, 99282, 99283, 99284, 99285, 99288, 99291, 99292, G0380, G0381, G0382, G0383, and G0384.
If observation services are billed with any of the ER associated Evaluation and Management codes, MCG Criteria will be used to evaluate the medical necessity of these observation hours.
Coverage is subject to the terms, conditions, and limitations of an individual member’s programs or products and the Clinical Payment and Coding Policy criteria listed below. The ED provides services to patients who are there for immediate medical attention. The physician or other qualified healthcare professional level of service is determined by the following:
1. Straight Forward Complexity (99281/G0380):
The presented problem(s) are self-limited or minor conditions with no medications or home treatment required.
Emergency department visit for the evaluation and management of a patient, which requires these
3 key components:
1) A problem focused history; 2) A problem focused examination; and 3) Straightforward medical decision making.
Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the presenting problem(s) are self-limited or minor.
2. Low Complexity (99282/G0381):
The presented problem(s) are of low to moderate severity. Over the counter (OTC) medications or treatment, simple dressing changes; patient demonstrates understanding quickly and easily. Emergency department visit for the evaluation and management of a patient, which requires these
1) An expanded problem focused history; 2) An expanded problem focused examination; and 3) Medical decision making of low complexity.
Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the presenting problem(s) are of low to moderate severity.
3. Moderate Complexity (99283/G0382):
The presented problem(s) are of moderate severity. Emergency department visit for the evaluation and management of a patient, which requires these 3 key components:
1) An expanded problem focused history; 2) An expanded problem focused examination; and 3) Medical decision making of moderate complexity.
Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the presenting problem(s) are of moderate severity.
4. Moderate-High Complexity (99284/G0383): Usually, the presented problem(s) are of high severity, and require urgent evaluation by the physician but do not pose an immediate significant threat to life or physiologic function. Emergency department visit for the evaluation and management of a patient, which requires these 3 key components:
1) A detailed history; 2) A detailed examination; and 3) Medical decision making of moderate complexity.
Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs.
5. High Complexity (99285/G0384):
The presented problem(s) are of high severity and pose an immediate significant threat to life or physiologic function. Emergency department visit for the evaluation and management of a patient, which requires these 3 key components within the constraints imposed by the urgency of the patient’s clinical condition and/or mental status:
1) A comprehensive history; 2) A comprehensive examination; and 3) Medical decision making of high complexity.
Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the presenting problem(s) are of high severity and pose an immediate significant threat to life or physiologic function.
6. Physician direction of Emergency Medical Systems (EMS) emergency care, advanced life support. (99288)
7. Critical Care (99291) & 99292
The assignment of the Critical Care code 99291 likewise follows the same instructions applicable to the six E&M codes listed above. There is a 30 minute time requirement for facility billing of critical care. The first 30-74 minutes equal code 99291. Any additional 30 minute increments beyond the first 74 minutes is coded 99292.
IV CPT 99284
Type A: APC 615 Type B: APC 629 HCPCS: G0383
Could include interventions from previous levels, plus any of: Preparation for 2 diagnostic tests: (Labs, EKG, X-ray) Prep for plain X-ray (multiple body areas):
C-spine & foot, shoulder & pelvis Prep for special imaging study (CT, MRI, Ultrasound,VQ scans) Cardiac Monitoring (2) Nebulizer treatments
Port-a-cath venous access
Administration and Monitoring of infusions or parenteral medications (IV, IM, IO, SC) NG/PEG Tube Placement/Replacement Multiple reassessments Prep or assist w/procedures such as: eye irrigation with Morgan lens, bladder irrigation with 3-way foley, pelvic exam, etc.
Sexual Assault Exam w/ out specimen collection Psychotic patient; not suicidal
Discussion of Discharge Instructions (Complex) Blunt/ penetrating trauma- with limited diagnostic testing Headache with nausea/
vomiting Dehydration requiring treatment
Vomiting requiring treatment
Dyspnea requiring oxygen Respiratory illness relieved with (2) nebulizer treatments
Chest Pain–with limited diagnostic testing Abdominal Pain – with limited diagnostic testing
Non-menstrual vaginal bleeding Neurologic symptoms – with limited diagnostic testing V
Type A: APC 616 Could include interventions from previous levels, plus any of:
Requires frequent monitoring of multiple vital signs (i.e. 02 sat, BP, cardiac rhythm, respiratory rate) Preparation for = 3 diagnostic tests: (Labs, EKG, X-ray) Prep for special imaging study (CT, MRI, Ultrasound, VQ Blunt/ penetrating trauma requiring multiple diagnostic tests Systemic multi-system medical emergency requiring multiple Medicare payment guidelines
All of the following requirements must be met in order for a hospital to receive an APC payment for the extended assessment and management composite APCs:
1. Observation Time
a. Observation time must be documented in the medical record.
b. A beneficiary’s time in observation (and hospital billing) begins with the beneficiary’s admission to an observation bed.
c. A beneficiary’s time in observation (and hospital billing) ends when all clinical or medical interventions have been completed, including follow-up care furnished by hospital staff and physicians that may take place after a physician has ordered the patient be released or admitted as an inpatient.
d. The number of units reported with HCPCS code G0378 must equal or exceed 8 hours.
2. Additional Hospital Services
a. The claim for observation services must include one of the following services in addition to the reported observation services. The additional services listed below must have a line item date of service on the same day or the day before the date reported for observation:
• An emergency department visit (CPT code 99284 or 99285) or
• A clinic visit (CPT code 99205 or 99215); or
• Critical care (CPT code 99291); or
• Direct admission to observation reported with HCPCS code G0379, must be reported on the same date of service as the date reported for observation services.
b. No procedure with a “T” status indicator can be reported on the same day or day before observation care is provided.
3. Physician Evaluation
a. The beneficiary must be in the care of a physician during the period of observation, as documented in the medical record by admission, discharge, and other appropriate progress notes that are timed, written, and signed by the physician. b. The medical record must include documentation that the physician explicitly assessed patient risk to determine that the beneficiary would benefit from observation care.
4. Payment for Direct Admission to Observation
For CY 2008, direct admission to observation care continues to be reported using HCPCS code G0379 (Direct admission of patient for hospital observation care). Hospitals should report G0379 when observation services are the result of a direct admission to observation care without an associated emergency room visit, hospital outpatient clinic visit, critical care service, or surgical procedure (T status procedure) on the day of initiation of observation services. Hospitals should only report HCPCS code G0379 when a patient is admitted directly to observation care after being seen by a physician in the community.
Payment for direct admission to observation will be made either separately as a low level hospital clinic visit under APC 604, packaged into payment for composite APC 8002 (Level I Prolonged Assessment and Management Composite), or packaged into payment for other separately payable services provided in the same encounter.
The criteria for payment of HCPCS code G0379 under either APC 8002 or APC 0604 include:
1. Both HCPCS codes G0378 (Hospital observation services, per hr) and G0379 (Direct admission of patient for hospital observation care) are reported with the same date of service.
2. No service with a status indicator of T or V or Critical Care (APC 0617) is provided on the same date of service as HCPCS code G0379.
If either of the above criteria is not met, HCPCS code G0379 will be assigned status indicator N and will be packaged into payment for other separately payable services provided in the same encounter.
Composite APCs and Criteria for Composite Payment Composite APC
Composite APC Title Criteria for Composite Payment 8000 Cardiac Electrophysiologic
Evaluation and Ablation Composite
At least one unit of CPT code 93619 or 93620 and at least one unit of CPT code 93650, 93651 or 93652 on the same date of service 8001 Low Dose Rate Prostate
Brachytherapy Composite One or more units of CPT codes 55875 and 77778 on the same date of service 8002 Level I Extended Assessment and Management Composite
1) 8 or more units of HCPCS code G0378 are billed–
* On the same day as HCPCS code G0379; or
* On the same day or the day after CPT codes 99205 or 99215 and
2) There is no service with SI=T on the claim on the same date of service or 1 day earlier than G0378
8003 Level II Extended Assessment and Management Composite
1) 8 or more units of HCPCS code G0378 are billed on the same date of service or the date of service after 99284, 99285 or 99291 and
2) There is no service with SI=T on the claim Composite APC Composite APC Title Criteria for Composite Payment on the same date of service or 1 day earlier than G0378.
0034 Mental Health Services Composite
A great ageing U . s . population and also modifications in order to Medicare insurance rules inside the first nineties get made the flourishing medical charging sector. Healthcare methods merely can't cope underneath the strain regarding escalating report do the job and also consumer inquiries. When you want a talented work at home career while using prospective in order to pay the bills plus much more, the actual Insurance Agents charging sector is good for anyone.

Medical Billing Modifier Guide
Recent posts.
- Mammogram ICD code and guildelines
- HOW TO Work on Duplicate claim denial – CO 18
- CPT 10009, 10010, 10021 -Fine Needle Aspiration Biopsy –
- CPT Code 0010U ,0011M, 0011U – Infectious Disease (Bacterial)
- CPT code 78451 and 78451 – SPECT guidelines
CPT modifiers update
Recent comments.
- Anonymous on CPT code 99211 – Billing Guide, office visit documentation
- Unknown on Medicare CPT code G0444, 99420 – covered ICD and frequency
- Unknown on CPT 97140, 97530, 97112, 97760, 97750 – Therapeutic procedure
- Anonymous on CPT 95921 , 95922- 95943 – Autonomic function tes
- Saqib_aleeeee on CPT code – 97802, 97803, 97804, G0270, G0271, G0108, dx code

Evaluation and Management Services
Emergency department services, new or established patient emergency department services, emergency department visit for the evaluation and management of a patient, which requires a medically appropriate history, cpt ® 99284 in section: emergency department visit for the evaluation and management of....
CPT ® Code Set
99284 - CPT® Code in category: Emergency department visit for the evaluation and management of a pati... CPT Code information is available to subscribers and includes the CPT code number, short description, long description, guidelines and more. CPT code information is copyright by the AMA. Access to this feature is available in the following products: Find-A-Code Essentials Find-A-Code Professional Find-A-Code Premium Find-A-Code Elite Find-A-Code Facility Base Find-A-Code Facility Plus Find-A-Code Facility Complete CPT Code information is available to subscribers and includes the CPT code number, short description, long description, guidelines and more. CPT code information is copyright by the AMA. sign IN sign UP

- Find-A-Code Professional
- Find-A-Code Premium
- Find-A-Code Elite
- Find-A-Code Facility Base
- Find-A-Code Facility Plus
- Find-A-Code Facility Complete
- HCC Standard
Save time with a Professional or Facility subscription! You will be able to see the most common modifiers billed to Medicare along with this code.
* Note: Medicare may or may NOT reimburse you for this code. The fees provided below are based on values established by CMS/Medicare. Please check with your local Medicare contact on whether this code is eligible for reimbursement.
Medicare vs. My Fee Evaluation
Medicare participating - assignment accepted (mandatory), medicare non-participating - assignment accepted (check to doctor), medicare non-participating - assignment not accepted (check to patient).
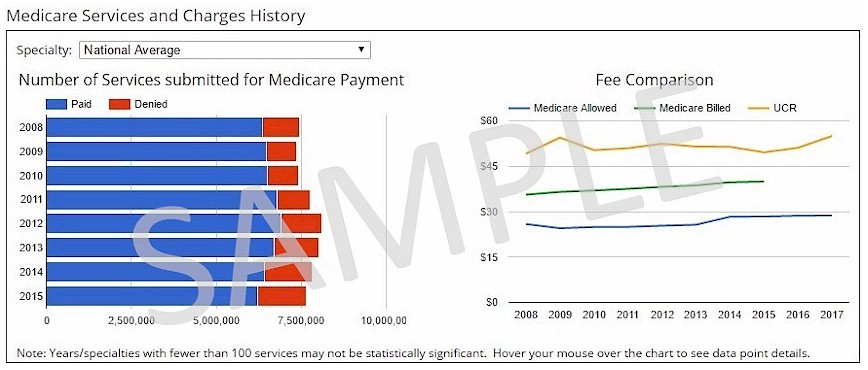
Thank you for choosing Find-A-Code, please Sign In to remove ads.

Sign up for our free newsletters!
- Consumer updates newsletter
- Industry insider newsletter

ClearHealthCosts
Bringing transparency to the health care marketplace.
99284 Emergency Care - Level 4
50 price reports
Check out our prices, then share what you paid . How did we do this?
Refine results
Price reports for 99284 emergency care - level 4.
Price charged
Insurance paid
Results are limited to 50 items. Please narrow your search to get more accurate results.
Read more here. "> What Medicare pays here?
Related procedures.

- Search forums
- If this is your first visit, be sure to check out the FAQ & read the forum rules . To view all forums, post or create a new thread, you must be an AAPC Member . If you are a member and have already registered for member area and forum access , you can log in by clicking here . If you've forgotten your username or password use our password reminder tool . To start viewing messages, select the forum that you want to visit from the selection below..
- Medical Coding
- Emergency Department
Wiki 2 E.D. visits same day 99283/99284
- Thread starter mmunoz21
- Start date Feb 11, 2010
- Feb 11, 2010
Is the E.R. doctor allowed to bill 2 E&M on the same day? patient came in the morning, dx:colitis, came back in the evening same day with vomitting/nausea...
- Feb 12, 2010
Hi, Yes you can bill two visits.
only in certain circumstances... Hi there, My experience is actually quite different - I believe that there are few circumstances that allow you to bill 2 visits by the same specialty on the same DOS. i.e. I would not bill a 99283 and a 99284 on the same DOS for the same PT. My belief is that one E/M will be denied outside of certain situations. We get denials from visits where the PT has been seen in another ED on the same DOS, and I do not believe that the denials are dx related. An E/M and then Critical Care services on the same DOS are billable, in which case one would add a -25 modifier to the initial service. If a patient has 2 visits on the same DOS in our ED, we accumulate the time and effort from both visits and bill one E/M. In the event that someone has identifiable visits with different carries (i.e. bronchitis at 8am, and then back pain from an MVA at 10am - and therefore health and then MVA insurance), we bill those separately. With procedures, a -76 or a -77 modifier may apply, but those are worth exploring on a case-by-case basis. In my experience, even if we had a patient come in once with sinusitis and then later with a broken wrist from a fall at home, we would not bill two separate E/Ms. From the CMS website (and I think it can be applied for ED as well - I could not unfortunately find explicit language about "2 visits in the ED on the same DOS", though that is the same as "two visits in the same specialty" so...): "The Medicare Claims Processing Manual (Chapter 12, Section 30.6.7), Paragraph B, clarifies “physician in a group practice” for office/outpatient E/M visits provided on the same day of unrelated problems, are as follows: • As for all other E/M services except where specifically noted, carriers may not pay two E/M office visits billed by a physician (or physician of the same specialty from the same group practice) for the same beneficiary on the same day unless the physician documents that the visits were for unrelated problems in the office or outpatient setting which could not be provided during the same encounter (e.g., office visit for blood pressure medication evaluation, followed five hours later by a visit for evaluation of leg pain following an accident)." [from] http://www.cms.hhs.gov/mlnmattersarticles/downloads/MM4032.pdf Also, the discussion in the forum about critical care services and other E/M services on the same DOS may be helpful. I hope this helps...sorry if a bit long-winded. It would be great to see a reference either way (that it's explicitly ok in the ED, or not) - anyone have one? would love to know. good luck!
Thank you very much for all your info. it was great...
I am going to ask my supervisor how this process works for us because I have noticed that we have many return visits in the same day by the same PT. We do not use a modifier on the E/M though I will not be able to ask until Monday now. This is something I have wondered about myself when I see a return visit. One day recently I noticed the Dr had written on the record that this was the second visit this day so I checked the system for another visit and discovered this patient had been there 57 times in a two month period (psych case). To say the least this got me wondering how they were all paid. When I recieve an answer I will post it, if I get an answer.
- Feb 15, 2010
Here is the way we proces a return visit within same date for the same DX. First the Dr needs to document the return visit or we would not recognize it as so, we do not check the system for each visit each pt. If it is for a commercial ins we code as usual and apply a modifier 25 ; for Medicare we void/no charge the entire visit. And thank you mmunoz21 for posting this question.
Contributor
- Feb 27, 2010
on the facility side we afix a modifier 27 on the second visit:
Davieda Skobel
- Mar 3, 2010
2 er visits same day We also combine the 2 visits. The CMS rule regarding paying 2 visits/ same specialty/same day does usually hold true unless the visits are totally unrelated. We look at both visit notes and combine the time and documentation and choose our level of E/M by that. ER physicians are usually in the same group so all the money goes to the same place anyway. Use both DX codes and if you have to appeal it, send both notes.
- Oct 20, 2014
Can anyone help? How to code, if two ER visits are billed for same patient by same physician for same diagnosis on same DOS in different invoices? Thanks, imai
- Oct 21, 2014
For same reason Many ED coding entities will combine the two visits based on total documentation and bill only once. The reason is usually that if a patient returns for the same reason or symptoms were not resolved, the hopsital will not want to penalize the patient for what may have been an oversite by ED providers, also I believe many payors will not pay in the scenario you described based on medical necessity. If the pateint came in for an ankle sprain and returned for chest pain, that is a strong argument for billing twice. But in your scenario, better to combine. If you do bill twice use 25 modifier for physician and 27 for facility. Jim S.
vicentevelasco2000
- Jun 18, 2016
Vicente Velasco, CPC-P As a payer here in Abu Dhabi, UAE we do collect deductible for all types of Consultation whether it is emergency or not. My question is, if the provider billed two Emergency E&M wherein from the first E&M we already collected the deductible and since there is no follow up for emergency, is it right to collect another deductible for the second emergency visit? Please note that the patient is complaining for the same problem, visited on the same day with four hours gap. Does it matter if the patient was seen by a different emergency doctor? Thank you very much!
- Jun 19, 2016
That would depend on the patients medical plan benefits.
- Jul 18, 2016
E/M Question.. Can anyone explain correct answer The patient is a 35-year-old male who presents to the emergency department (ED) after several hours of low back pain, nausea, and chills. The ED physician takes a detailed history and performs a comprehensive examination. A urinalysis lab and CT of the abdomen is ordered. The results of the CT show two small kidney stones. The ED physician discusses the results with the patient and tells him the stones are small and will pass on their own. Medical decision making (MDM) of moderate complexity is made with the patient being discharged, with a prescription of pain medication, and with a diagnosis of kidney stones. Select the E/M code and diagnosis code(s). 1) 99283, N20.0 2) 99284, N20.0 Can anyone help me to get correct answer for this question with explanation?
- Jul 19, 2016
We combine visits also unless the patient presents with a different problem. Then we bill both visits.
[email protected]
- Jul 25, 2016
different e/m's I believe as long as its two diff dx, the modifier 24 can be used,,,, depending if unrelated procedures were done you may have to use mod 79,,,,, if it comes down to the same physician, same dos, same dx, with procedures, use mod 78, without procedures, modifier 25 is the one that fits best,,, hope this helps
[email protected] said: I believe as long as its two diff dx, the modifier 24 can be used,,,, depending if unrelated procedures were done you may have to use mod 79,,,,, if it comes down to the same physician, same dos, same dx, with procedures, use mod 78, without procedures, modifier 25 is the one that fits best,,, hope this helps Click to expand...
- Sep 27, 2019
Hello, 2 Visits on same day for the same problem in ED dept. I am confused when pt. is staying overnight and then is coming back for same problem. Example: PT. came in on 9/26 at 10:00pm for low back pain. and was discharged on 9/27 at 3:00am. then is coming back on 9/27 at 9:00am for low back pain again and nausea and then is discharged on 9/27 at 1:00pm. I am assigning 2 facility levels with -27 on second level and I am assigning only 1 profee level on the second visit. I am discussing this issue with my co-workers and we have a different view on this subject. I would like to know other coders opinion. What should be taken under consideration admission date or discharge date when coding for 2 visits on same day on same problem? Thank you so much for any help, Niki
[email protected]
- Oct 16, 2019
Can ED Codes 99281 -99285 be used by other physicians who are not employed by the hospital? Are these codes reserved for ED staff only? All work is done in the ED. Example: A patient comes into the ER with bladder pain. The ED Physician orders a CT and finds a bladder stone. The ED Doc calls a Urologist in to consult the issue. The Urologist consults the patient and performs a Cysto to remove the stone. Can the Urologist bill a 99283 and 52310? Or should he/she bill 99203 and 52310? The Urologists is rounding at the hospital that day. Thanks for all input Andia
- Oct 30, 2019
Good morning, I have a peds patient that was seen in the ED at 5am for severe ear pain, the pt was treated and released. The patient has a a separate scheduled appt regarding behavior on the same day at 4pm. The hospital and peds office have the same tax id. Will the office be reimbursable since the child was seen in the ED on the same day of the scheduled unrelated appt?

IMAGES
VIDEO
COMMENTS
Navigate the complexities of billing a level 4 ER visit with our guide on cpt code 99284, ensuring accurate hospital reimbursement. ... Properly assigning CPT codes, such as CPT code 99284 for emergency department visits, is imperative to ensure the claim reflects the services provided accurately. Using the correct CPT code increases the ...
In November 2019, CMS adopted the AMA's revisions to the Evaluation and Management (E/M) office visit CPT codes (99201-99215), code descriptors, and documentation standards. ... 99284 - Emergency department visit for the evaluation and ... an illness or injury that warrants a visit to the emergency room seems to exceed what would be ...
HPI flushes out the chief complaint in grea t er d e t a il. There are two types of HPI identified for the purpose of coding. A brief HPI consists of 1-3 elements (99281-99283) An extended HPI consists of at least 4 elements (99284-99285) 27. Brief- 32 year old male with left shoulder. injury, occurred 4 hours ago.
CPT code 99284 is defined in the official CPT code book manual as being for "Emergency department visit for the evaluation and management of a patient, which requires these 3 key components.". Component 1: Must include a detailed history. Component 2: Requires a detailed examination.
These changes are illustrated by the 2023 ED E/M code descriptors, which will appear as follows: The 2023 E/M definitions have been updated to reflect simply Medical Decision Making determining the level. 99281: ED visit for the evaluation and management of a patient that may not require the presence of a physician or other qualified health ...
Coding & Billing Guidelines. Emergency Department (ED) Evaluation and Management (E/M) codes are typically reported per day and do not differentiate between new or established patients. There are 5 levels of emergency department services represented by CPT codes 99281 - 99285. The ED codes require the level of Medical Decision Making (MDM) to ...
visits. To that end, CMS coding principles applicable to emergency department services provide that facility coding guidelines should: follow the intent of the CPT code descriptor in that the guidelines should be designed to reasonably ... (E/M) codes Level 4 (99284/G0383) and Level 5 (99285/G0384) for services rendered in an emergency department.
The Current Procedural Terminology (CPT ®) code 99284 as maintained by American Medical Association, is a medical procedural code under the range - New or Established Patient. Subscribe to Codify by AAPC and get the code details in a flash.
CPT Code 99284 Description. CPT Code 99284 is defined by the CPT manual as follows (the text in Italic is the official definition of CPT 99284): " Emergency department visit for the evaluation and management of a patient, which requires these 3 key components: Component 1: A detailed history. Component 2: A detailed examination.
Coding Thought Process • NOPP provides Clear Differentiation between ED Levels • In Choosing a 99282 to 99284 NOPP Terms are more clearly Defined Than • History which is the same for 99282 and 99283 (Expanded Problem Focused) • And MDM which is the Same for 99283 and 99284 (Moderate Complexity)
What should I know before my telehealth visit? ... 99283, 99284, 99285. Critical care. First hour: 99291. Additional 30 min: 99292. Observation services. Discharge: 99217. Initial: 99218, 99219, 99220. Subsequent: 99224, 99225, 99226 ... Many code changes for COVID-19 care cover telehealth and include specific information for visits that are ...
CPT®Code 99284 Details. Upcoming and Historical Information Change Type Change Date Previous Descriptor Code Changed 01-01-2023 Emergency department visit for the evaluation and management of a patient, which requires these 3 key components: • A detailed history; • A detailed examination; and • Medical decision making of moderate complexity.
• An emergency department visit (CPT code 99284 or 99285) or • A clinic visit (CPT code 99205 or 99215); or • Critical care (CPT code 99291); or • Direct admission to observation reported with HCPCS code G0379, must be reported on the same date of service as the date reported for observation services. b.
The prior requirements to document a complete history and physical examination will no longer be deciding factors in code selection in 2023, but instead the 2023 Guidelines simply require a medically appropriate history and physical exam. ... 99284 Emergency department visit for the evaluation and management of a patient which requires a ...
visit code (9922x-Ai). if the patient is admitted for observation, codes 99218-99220 are reported. For patients receiving hospital ... 99284 3.36 99244 5.20 99223 5.30 99285 4.93 99245 6.36 tABL 4.e 2013 totAL iNitiAL HosPitAL, iNPAtieNt AND outPAtieNt CoNsuLtAtioN
99284 - CPT® Code in category: Emergency department visit for the evaluation and management of a pati... CPT Code information is available to subscribers and includes the CPT code number, short description, long description, guidelines and more.
An emergency department is defined as an organized hospital-based facility for the provision of unscheduled episodic services to patients who present for immediate medical attention. The facility must be available 24 hours a day. Based on this definition, codes 99281-99285 will be denied provider liable as incompatible if submitted with any ...
• An emergency department visit (CPT code 99284 or 99285) or • A clinic visit (CPT code 99205 or 99215); or • Critical care (CPT code 99291); or • Direct admission to observation reported with HCPCS code G0379, must be reported on the same date of service as the date reported for observation services. b.
Emergency room cpt codes 30.6.11 - Emergency Department Visits (Codes 99281 - 99288) (Rev. 1875, Issued: 12-14-09, Effective: 01-01-10, Implementation: 01-04-10) A. Use of Emergency Department Codes by Physicians Not Assigned...
In my case, went to ER for kidney stone, first time experiencing ER visit and what a sticker shock. 1 bill from the hospital, 1 bill for the attending doctor, 1 bill from radiology department. This bill from Fairfax Hospital, INVOA healthcare system. Service code 99284 Emergency Eval & MGT $1068.00.
Mar 3, 2010. #8. 2 er visits same day. We also combine the 2 visits. The CMS rule regarding paying 2 visits/ same specialty/same day does usually hold true unless the visits are totally unrelated. We look at both visit notes and combine the time and documentation and choose our level of E/M by that.