- Search Menu
- Advance Articles
- Editor's Choice
- Supplements
- Patient Perspectives
- Methods Corner
- ESC Content Collections
- Author Guidelines
- Instructions for reviewers
- Submission Site
- Why publish with EJCN?
- Open Access Options
- Self-Archiving Policy
- Read & Publish
- About European Journal of Cardiovascular Nursing
- About ACNAP
- About European Society of Cardiology
- ESC Publications
- Editorial Board
- Advertising & Corporate Services
- War in Ukraine
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, why patient journey mapping, how is patient journey mapping conducted, use of technology in patient journey mapping, future implications for patient journey mapping, conclusions, patient journey mapping: emerging methods for understanding and improving patient experiences of health systems and services.
Lemma N Bulto and Ellen Davies Shared first authorship.
Conflict of interest: none declared.
- Article contents
- Figures & tables
- Supplementary Data
Lemma N Bulto, Ellen Davies, Janet Kelly, Jeroen M Hendriks, Patient journey mapping: emerging methods for understanding and improving patient experiences of health systems and services, European Journal of Cardiovascular Nursing , 2024;, zvae012, https://doi.org/10.1093/eurjcn/zvae012
- Permissions Icon Permissions
Patient journey mapping is an emerging field of research that uses various methods to map and report evidence relating to patient experiences and interactions with healthcare providers, services, and systems. This research often involves the development of visual, narrative, and descriptive maps or tables, which describe patient journeys and transitions into, through, and out of health services. This methods corner paper presents an overview of how patient journey mapping has been conducted within the health sector, providing cardiovascular examples. It introduces six key steps for conducting patient journey mapping and describes the opportunities and benefits of using patient journey mapping and future implications of using this approach.
Acquire an understanding of patient journey mapping and the methods and steps employed.
Examine practical and clinical examples in which patient journey mapping has been adopted in cardiac care to explore the perspectives and experiences of patients, family members, and healthcare professionals.
Quality and safety guidelines in healthcare services are increasingly encouraging and mandating engagement of patients, clients, and consumers in partnerships. 1 The aim of many of these partnerships is to consider how health services can be improved, in relation to accessibility, service delivery, discharge, and referral. 2 , 3 Patient journey mapping is a research approach increasingly being adopted to explore these experiences in healthcare. 3
a patient-oriented project that has been undertaken to better understand barriers, facilitators, experiences, interactions with services and/or outcomes for individuals and/or their carers, and family members as they enter, navigate, experience and exit one or more services in a health system by documenting elements of the journey to produce a visual or descriptive map. 3
It is an emerging field with a clear patient-centred focus, as opposed to studies that track patient flow, demand, and movement. As a general principle, patient journey mapping projects will provide evidence of patient perspectives and highlight experiences through the patient and consumer lens.
Patient journey mapping can provide significant insights that enable responsive and context-specific strategies for improving patient healthcare experiences and outcomes to be designed and implemented. 3–6 These improvements can occur at the individual patient, model of care, and/or health system level. As with other emerging methodologies, questions have been raised regarding exactly how patient journey mapping projects can best be designed, conducted, and reported. 3
In this methods paper, we provide an overview of patient journey mapping as an emergent field of research, including reasons that mapping patient journeys might be considered, methods that can be adopted, the principles that can guide patient journey mapping data collection and analysis, and considerations for reporting findings and recognizing the implications of findings. We summarize and draw on five cardiovascular patient journey mapping projects, as examples.
One of the most appealing elements of the patient journey mapping field of research is its focus on illuminating the lived experiences of patients and/or their family members, and the health professionals caring for them, methodically and purposefully. Patient journey mapping has an ability to provide detailed information about patient experiences, gaps in health services, and barriers and facilitators for access to health services. This information can be used independently, or alongside information from larger data sets, to adapt and improve models of care relevant to the population that is being investigated. 3
To date, the most frequent reason for adopting this approach is to inform health service redesign and improvement. 3 , 7 , 8 Other reasons have included: (i) to develop a deeper understanding of a person’s entire journey through health systems; 3 (ii) to identify delays in diagnosis or treatment (often described as bottlenecks); 9 (iii) to identify gaps in care and unmet needs; (iv) to evaluate continuity of care across health services and regions; 10 (v) to understand and evaluate the comprehensiveness of care; 11 (vi) to understand how people are navigating health systems and services; and (vii) to compare patient experiences with practice guidelines and standards of care.
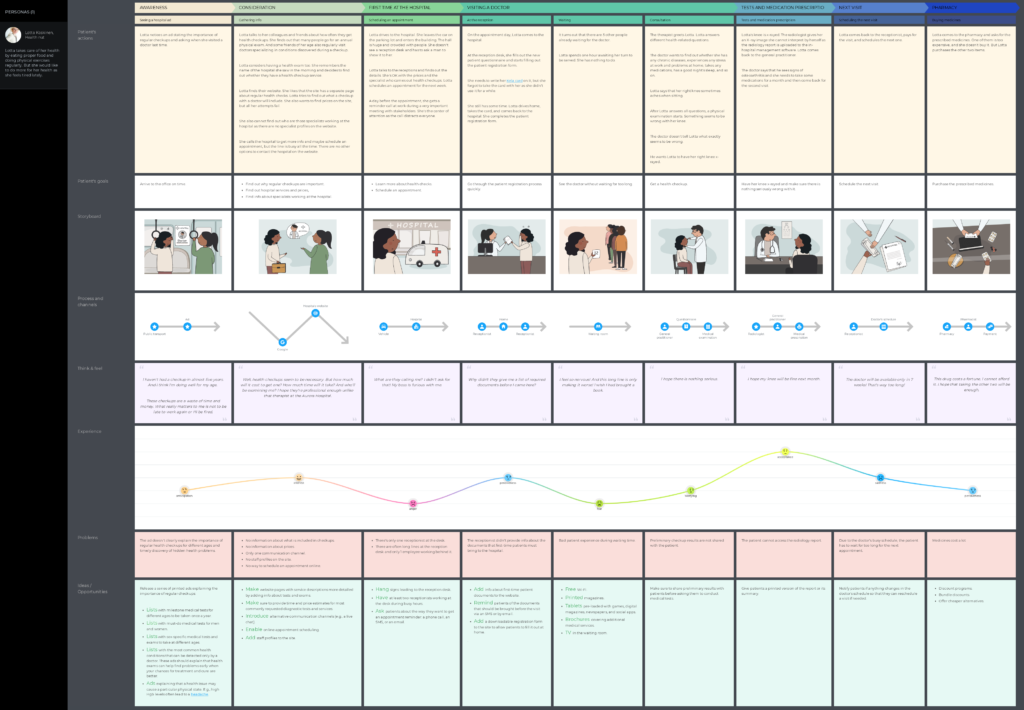
Patient journey mapping approaches frequently use six broad steps that help facilitate the preparation and execution of research projects. These are outlined in the Central illustration . We acknowledge that not all patient journey mapping approaches will follow the order outlined in the Central illustration , but all steps need to be considered at some point throughout each project to ensure that research is undertaken rigorously, appropriately, and in alignment with best practice research principles.
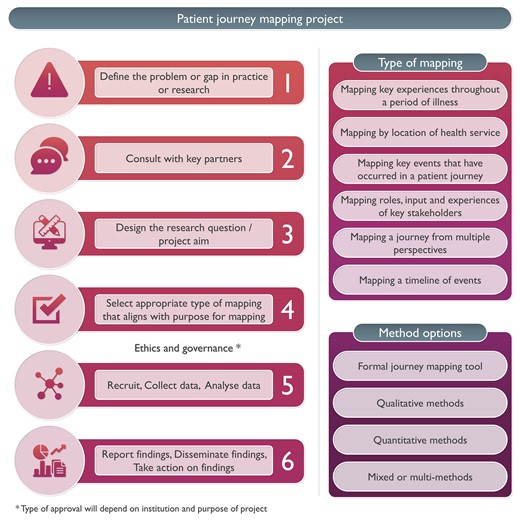
Steps for conducing patient journey mapping.
Five cardiovascular patient journey mapping research examples have been included in Figure 1 , 12–16 to provide specific context and illustrate these six steps. For each of these examples, the problem or gap in practice or research, consultation processes, research question or aim, type of mapping, methods, and reporting of findings have been extracted. Each of these steps is then discussed, using these cardiovascular examples.
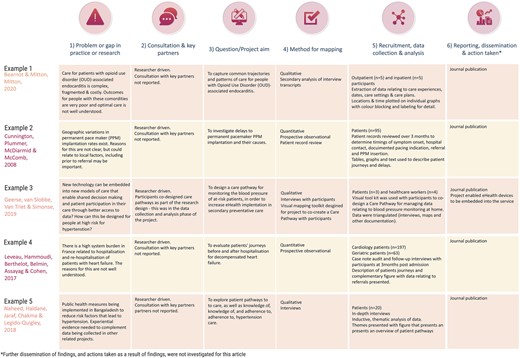
Examples of patient journey mapping projects.
Define the problem or gap in practice or research
Developing an understanding of a problem or gap in practice is essential for facilitating the design and development of quality research projects. In the examples outlined in Figure 1 , it is evident that clinical variation or system gaps have been explored using patient journey mapping. In the first two examples, populations known to have health vulnerabilities were explored—in Example 1, this related to comorbid substance use and physical illness, 13 and in Example 2, this related to geographical location. 13 Broader systems and societal gaps were explored in Examples 4 and 5, respectively, 15 , 16 and in Example 3, a new technologically driven solution for an existing model of care was tested for its ability to improve patient outcomes relating to hypertension. 14
Consultation, engagement, and partnership
Ideally, consultation with heathcare providers and/or patients would occur when the problem or gap in practice or research is being defined. This is a key principle of co-designed research. 17 Numerous existing frameworks for supporting patient involvement in research have been designed and were recently documented and explored in a systematic review by Greenhalgh et al . 18 While none of the five example studies included this step in the initial phase of the project, it is increasingly being undertaken in patient partnership projects internationally (e.g. in renal care). 17 If not in the project conceptualization phase, consultation may occur during the data collection or analysis phase, as demonstrated in Example 3, where a care pathway was co-created with participants. 14 We refer readers to Greenhalgh’s systematic review as a starting point for considering suitable frameworks for engaging participants in consultation, partnership, and co-design of patient journey mapping projects. 18
Design the research question/project aim
Conducting patient journey mapping research requires a thoughtful and systematic approach to adequately capture the complexity of the healthcare experience. First, the research objectives and questions should be clearly defined. Aspects of the patient journey that will be explored need to be identified. Then, a robust approach must be developed, taking into account whether qualitative, quantitative, or mixed methods are more appropriate for the objectives of the study.
For example, in the cardiac examples in Figure 1 , the broad aims included mapping existing pathways through health services where there were known problems 12 , 13 , 15 , 16 and documenting the co-creation of a new care pathway using quantitative, qualitative, or mixed methods. 14
In traditional studies, questions that might be addressed in the area of patient movement in health systems include data collected through the health systems databases, such as ‘What is the length of stay for x population’, or ‘What is the door to balloon time in this hospital?’ In contrast, patient mapping journey studies will approach asking questions about experiences that require data from patients and their family members, e.g. ‘What is the impact on you of your length of stay?’, ‘What was your experience in being assessed and undergoing treatment for your chest pain?’, ‘What was your experience supporting this patient during their cardiac admission and discharge?’
Select appropriate type of mapping
The methods chosen for mapping need to align with the identified purpose for mapping and the aim or question that was designed in Step 3. A range of research methods have been used in patient journey mapping projects involving various qualitative, quantitative, and mixed methods techniques and tools. 4 Some approaches use traditional forms of data collection, such as short-form and long-form patient interviews, focus groups, and direct patient observations. 18 , 19 Other approaches use patient journey mapping tools, designed and used with specific cultural groups, such as First Nations peoples using artwork, paintings, sand trays, and photovoice. 17 , 20 In the cardiovascular examples presented in Figure 1 , both qualitative and quantitative methods have been used, with interviews, patient record reviews, and observational techniques adopted to map patient journeys.
In a recent scoping review investigating patient journey mapping across all health care settings and specialities, six types of patient journey mapping were identified. 3 These included (i) mapping key experiences throughout a period of illness; (ii) mapping by location of health service; (iii) mapping by events that occurred throughout a period of illness; (iv) mapping roles, input, and experiences of key stakeholders throughout patient journeys; (v) mapping a journey from multiple perspectives; and (vi) mapping a timeline of events. 3 Combinations or variations of these may be used in cardiovascular settings in the future, depending on the research question, and the reasons mapping is being undertaken.
Recruit, collect data, and analyse data
The majority of health-focused patient journey mapping projects published to date have recruited <50 participants. 3 Projects with fewer participants tend to be qualitative in nature. In the cardiovascular examples provided in Figure 1 , participant numbers range from 7 14 to 260. 15 The 3 studies with <20 participants were qualitative, 12 , 14 , 16 and the 2 with 95 and 260 participants, respectively, were quantitative. 13 , 15 As seen in these and wider patient journey mapping examples, 3 participants may include patients, relatives, carers, healthcare professionals, or other stakeholders, as required, to meet the study objectives. These different participant perspectives may be analysed within each participant group and/or across the wider cohort to provide insights into experiences, and the contextual factors that shape these experiences.
The approach chosen for data collection and analysis will vary and depends on the research question. What differentiates data analysis in patient journey mapping studies from other qualitative or quantitative studies is the focus on describing, defining, or exploring the journey from a patient’s, rather than a health service, perspective. Dimensions that may, therefore, be highlighted in the analysis include timing of service access, duration of delays to service access, physical location of services relative to a patient’s home, comparison of care received vs. benchmarked care, placing focus on the patient perspective.
The mapping of individual patient journeys may take place during data collection with the use of mapping templates (tables, diagrams, and figures) and/or later in the analysis phase with the use of inductive or deductive analysis, mapping tables, or frameworks. These have been characterized and visually represented in a recent scoping review. 3 Representations of patient journeys can also be constructed through a secondary analysis of previously collected data. In these instances, qualitative data (i.e. interviews and focus group transcripts) have been re-analysed to understand whether a patient journey narrative can be extracted and reported. Undertaking these projects triggers a new research cycle involving the six steps outlined in the Central illustration . The difference in these instances is that the data are already collected for Step 5.
Report findings, disseminate findings, and take action on findings
A standardized, formal reporting guideline for patient journey mapping research does not currently exist. As argued in Davies et al ., 3 a dedicated reporting guide for patient journey mapping would be ill-advised, given the diversity of approaches and methods that have been adopted in this field. Our recommendation is for projects to be reported in accordance with formal guidelines that best align with the research methods that have been adopted. For example, COREQ may be used for patient journey mapping where qualitative methods have been used. 20 STROBE may be used for patient journey mapping where quantitative methods have been used. 21 Whichever methods have been adopted, reporting of projects should be transparent, rigorous, and contain enough detail to the extent that the principles of transparency, trustworthiness, and reproducibility are upheld. 3
Dissemination of research findings needs to include the research, healthcare, and broader communities. Dissemination methods may include academic publications, conference presentations, and communication with relevant stakeholders including healthcare professionals, policymakers, and patient advocacy groups. Based on the findings and identified insights, stakeholders can collaboratively design and implement interventions, programmes, or improvements in healthcare delivery that overcome the identified challenges directly and address and improve the overall patient experience. This cyclical process can hopefully produce research that not only informs but also leads to tangible improvements in healthcare practice and policy.
Patient journey mapping is typically a hands-on process, relying on surveys, interviews, and observational research. The technology that supports this research has, to date, included word processing software, and data analysis packages, such as NVivo, SPSS, and Stata. With the advent of more sophisticated technological tools, such as electronic health records, data analytics programmes, and patient tracking systems, healthcare providers and researchers can potentially use this technology to complement and enhance patient journey mapping research. 19 , 20 , 22 There are existing examples where technology has been harnessed in patient journey. Lee et al . used patient journey mapping to verify disease treatment data from the perspective of the patient, and then the authors developed a mobile prototype that organizes and visualizes personal health information according to the patient-centred journey map. They used a visualization approach for analysing medical information in personal health management and examined the medical information representation of seven mobile health apps that were used by patients and individuals. The apps provide easy access to patient health information; they primarily import data from the hospital database, without the need for patients to create their own medical records and information. 23
In another example, Wauben et al. 19 used radio frequency identification technology (a wireless system that is able to track a patient journey), as a component of their patient journey mapping project, to track surgical day care patients to increase patient flow, reduce wait times, and improve patient and staff satisfaction.
Patient journey mapping has emerged as a valuable research methodology in healthcare, providing a comprehensive and patient-centric approach to understanding the entire spectrum of a patient’s experience within the healthcare system. Future implications of this methodology are promising, particularly for transforming and redesigning healthcare delivery and improving patient outcomes. The impact may be most profound in the following key areas:
Personalized, patient-centred care : The methodology allows healthcare providers to gain deep insights into individual patient experiences. This information can be leveraged to deliver personalized, patient-centric care, based on the needs, values, and preferences of each patient, and aligned with guideline recommendations, healthcare professionals can tailor interventions and treatment plans to optimize patient and clinical outcomes.
Enhanced communication, collaboration, and co-design : Mapping patient interactions with health professionals and journeys within and across health services enables specific gaps in communication and collaboration to be highlighted and potentially informs responsive strategies for improvement. Ideally, these strategies would be co-designed with patients and health professionals, leading to improved care co-ordination and healthcare experience and outcomes.
Patient engagement and empowerment : When patients are invited to share their health journey experiences, and see visual or written representations of their journeys, they may come to understand their own health situation more deeply. Potentially, this may lead to increased health literacy, renewed adherence to treatment plans, and/or self-management of chronic conditions such as cardiovascular disease. Given these benefits, we recommend that patients be provided with the findings of research and quality improvement projects with which they are involved, to close the loop, and to ensure that the findings are appropriately disseminated.
Patient journey mapping is an emerging field of research. Methods used in patient journey mapping projects have varied quite significantly; however, there are common research processes that can be followed to produce high-quality, insightful, and valuable research outputs. Insights gained from patient journey mapping can facilitate the identification of areas for enhancement within healthcare systems and inform the design of patient-centric solutions that prioritize the quality of care and patient outcomes, and patient satisfaction. Using patient journey mapping research can enable healthcare providers to forge stronger patient–provider relationships and co-design improved health service quality, patient experiences, and outcomes.
None declared.
Farmer J , Bigby C , Davis H , Carlisle K , Kenny A , Huysmans R , et al. The state of health services partnering with consumers: evidence from an online survey of Australian health services . BMC Health Serv Res 2018 ; 18 : 628 .
Google Scholar
Kelly J , Dwyer J , Mackean T , O’Donnell K , Willis E . Coproducing Aboriginal patient journey mapping tools for improved quality and coordination of care . Aust J Prim Health 2017 ; 23 : 536 – 542 .
Davies EL , Bulto LN , Walsh A , Pollock D , Langton VM , Laing RE , et al. Reporting and conducting patient journey mapping research in healthcare: a scoping review . J Adv Nurs 2023 ; 79 : 83 – 100 .
Ly S , Runacres F , Poon P . Journey mapping as a novel approach to healthcare: a qualitative mixed methods study in palliative care . BMC Health Serv Res 2021 ; 21 : 915 .
Arias M , Rojas E , Aguirre S , Cornejo F , Munoz-Gama J , Sepúlveda M , et al. Mapping the patient’s journey in healthcare through process mining . Int J Environ Res Public Health 2020 ; 17 : 6586 .
Natale V , Pruette C , Gerohristodoulos K , Scheimann A , Allen L , Kim JM , et al. Journey mapping to improve patient-family experience and teamwork: applying a systems thinking tool to a pediatric ambulatory clinic . Qual Manag Health Care 2023 ; 32 : 61 – 64 .
Cherif E , Martin-Verdier E , Rochette C . Investigating the healthcare pathway through patients’ experience and profiles: implications for breast cancer healthcare providers . BMC Health Serv Res 2020 ; 20 : 735 .
Gilburt H , Drummond C , Sinclair J . Navigating the alcohol treatment pathway: a qualitative study from the service users’ perspective . Alcohol Alcohol 2015 ; 50 : 444 – 450 .
Gichuhi S , Kabiru J , M’Bongo Zindamoyen A , Rono H , Ollando E , Wachira J , et al. Delay along the care-seeking journey of patients with ocular surface squamous neoplasia in Kenya . BMC Health Serv Res 2017 ; 17 : 485 .
Borycki EM , Kushniruk AW , Wagner E , Kletke R . Patient journey mapping: integrating digital technologies into the journey . Knowl Manag E-Learn 2020 ; 12 : 521 – 535 .
Barton E , Freeman T , Baum F , Javanparast S , Lawless A . The feasibility and potential use of case-tracked client journeys in primary healthcare: a pilot study . BMJ Open 2019 ; 9 : e024419 .
Bearnot B , Mitton JA . “You’re always jumping through hoops”: journey mapping the care experiences of individuals with opioid use disorder-associated endocarditis . J Addict Med 2020 ; 14 : 494 – 501 .
Cunnington MS , Plummer CJ , McDiarmid AK , McComb JM . The patient journey from symptom onset to pacemaker implantation . QJM 2008 ; 101 : 955 – 960 .
Geerse C , van Slobbe C , van Triet E , Simonse L . Design of a care pathway for preventive blood pressure monitoring: qualitative study . JMIR Cardio 2019 ; 3 : e13048 .
Laveau F , Hammoudi N , Berthelot E , Belmin J , Assayag P , Cohen A , et al. Patient journey in decompensated heart failure: an analysis in departments of cardiology and geriatrics in the Greater Paris University Hospitals . Arch Cardiovasc Dis 2017 ; 110 : 42 – 50 .
Naheed A , Haldane V , Jafar TH , Chakma N , Legido-Quigley H . Patient pathways and perceptions of treatment, management, and control Bangladesh: a qualitative study . Patient Prefer Adherence 2018 ; 12 : 1437 – 1449 .
Bateman S , Arnold-Chamney M , Jesudason S , Lester R , McDonald S , O’Donnell K , et al. Real ways of working together: co-creating meaningful Aboriginal community consultations to advance kidney care . Aust N Z J Public Health 2022 ; 46 : 614 – 621 .
Greenhalgh T , Hinton L , Finlay T , Macfarlane A , Fahy N , Clyde B , et al. Frameworks for supporting patient and public involvement in research: systematic review and co-design pilot . Health Expect 2019 ; 22 : 785 – 801 .
Wauben LSGL , Guédon ACP , de Korne DF , van den Dobbelsteen JJ . Tracking surgical day care patients using RFID technology . BMJ Innov 2015 ; 1 : 59 – 66 .
Tong A , Sainsbury P , Craig J . Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups . Int J Qual Health Care 2007 ; 19 : 349 – 357 .
von Elm E , Altman DG , Egger M , Pocock SJ , Gøtzsche PC , Vandenbroucke JP , et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies . Lancet 2007 ; 370 (9596): 1453 – 1457 .
Wilson A , Mackean T , Withall L , Willis EM , Pearson O , Hayes C , et al. Protocols for an Aboriginal-led, multi-methods study of the role of Aboriginal and Torres Strait Islander health workers, practitioners and Liaison officers in quality acute health care . J Aust Indigenous HealthInfoNet 2022 ; 3 : 1 – 15 .
Lee B , Lee J , Cho Y , Shin Y , Oh C , Park H , et al. Visualisation of information using patient journey maps for a mobile health application . Appl Sci 2023 ; 13 : 6067 .
Author notes
Email alerts, citing articles via.
- Recommend to Your Librarian
- Advertising and Corporate Services
- Journals Career Network
Affiliations
- Online ISSN 1873-1953
- Print ISSN 1474-5151
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Case studies
- Expert advice
Patient journey mapping: what it is, its benefits, and how to do it
We've all been patients at some point, but our journeys were not the same. Patient journey mapping holds the key to unraveling this mystery, providing a strategic lens into the diverse pathways individuals tread throughout their healthcare experiences.
In this article, we'll explore the pivotal role of patient journey mapping in the healthcare industry, uncovering its profound benefits for both providers and patients. From amplifying patient satisfaction to streamlining operational processes, the impact is transformative.
But how does one embark on this journey of understanding and improvement? We'll guide you through the essential steps and considerations, offering insights into the art of crafting a meaningful healthcare patient journey map.
Join us as we peel back the layers of patient experience journey mapping. This powerful tool not only illuminates the complexities of healthcare but also empowers providers to reshape and enhance the patient experience.
- 1.1 Difference from other customer journeys
- 2 Patient journey mapping benefits
- 3 Patient journey stages
- 4.1 Clinical journey maps
- 4.2 Service delivery maps
- 4.3 Digital journey maps
- 4.4 Chronic disease management maps
- 4.5 Emergency care journey maps
- 4.6 Pediatric patient journey maps
- 4.7 Palliative care maps
- 5 How to do patient journey mapping?
- 6.1 Patient-centered care
- 6.2 Streamlined access to care
- 6.3 Effective communication
- 6.4 Education and empowerment
- 6.5 Care coordination
- 6.6 Technology integration
- 6.7 Feedback and continuous improvement
- 6.8 Cultural competency
- 6.9 Emotional support
- 6.10 Efficient billing and financial assistance
- 7 Templates
- 8 Wrapping up
What is a patient journey?

A patient journey is the entire process a person goes through when seeking and receiving a healthcare service. It covers everything from first noticing symptoms or realizing the need for care and medical attention to finally resolving the health issue. The journey involves patient interactions with healthcare professionals, diagnostic procedures, treatment activities, and follow-up care.
Mapping and understanding the patient journey can help boost the quality of hospital care and improve patient satisfaction. By pinpointing challenges, patient communication gaps, and areas for enhancement, care providers can refine their services to better cater to patients' needs. It also contributes to promoting patient-centered care, shifting the focus beyond just treating diseases to considering the overall well-being and experience of the patient.
Difference from other customer journeys
While the concept of patient journey mapping is similar to customer journey mapping , there are unique aspects specific to the healthcare domain. This is how a patient journey differs from any other customer journey:
- Emotional intensity. Health-related experiences often involve heightened emotions, including fear, anxiety, uncertainty, a sense of losing control, and a dependence on others. The emotional aspect is more pronounced in patient journeys compared to customer journeys in most industries.
- Complexity and uncertainty. Healthcare journeys often involve multiple stakeholders, various diagnostic and treatment options, and inherent uncertainties. Navigating these complexities requires a different approach compared to more straightforward consumer experiences. Comparing buying eyeglasses online and visiting a doctor — both are experiences, but how different they are!
- Regulatory and ethical considerations. Healthcare is heavily regulated, and ethical considerations play a significant role there. Patient journeys must align with regulatory standards and ethical principles that other industries don’t have.

- Clinical decision points. Patient journeys involve critical clinical decision points, such as diagnosis and treatment choices. These decisions not only impact the patient's health but also influence the overall trajectory of the journey.
- Care continuum. Patient journeys often extend beyond a single episode of care. They may involve long-term management, follow-up appointments, and ongoing support, creating a continuous care continuum.
- Interdisciplinary collaboration. Healthcare is often delivered by a team of professionals from different disciplines. The patient journey may involve collaboration among physicians, nurses, specialists, and other healthcare providers.
Patient journey mapping benefits

Mapping a patient journey offers a range of benefits that contribute to improving the overall quality of healthcare delivery. Here are some key advantages:
- Visualization of the entire patient journey helps healthcare providers identify critical patient journey touchpoints that impact patient satisfaction and experience and require immediate attention. By paying more attention to these touchpoints, you ensure a more positive overall journey.
- Gaps in care and challenges are highlighted among healthcare professionals. Addressing these issues ensures a more seamless and collaborative approach to patient care.
- Pain points and barriers become evident, enabling healthcare providers to proactively address issues that may hinder effective care delivery.
- Understanding individual patient journeys allows for more personalized ongoing care plans. Tailoring interventions to specific needs and preferences improves patient engagement and outcomes.
- By mapping a patient journey, you can identify resource-intensive stages and areas where efficiency can be improved, enabling a healthcare organization to allocate resources more effectively.
- It's a great way to identify opportunities for smoother transitions between different stages of care, ensuring continuity and preventing gaps in treatment.
- It becomes clear where patient involvement in the decision-making process can contribute to their healthcare journey.
Example: Tom, recovering from surgery, feels more empowered as his healthcare team provides clear post-operative care instructions, making him an active participant in his recovery.
In summary, patient journey mapping provides a comprehensive framework for healthcare improvement, addressing specific challenges at each stage and leading to tangible enhancements in patient experience, communication, and overall care delivery.
Patient journey stages
Patient journeys can differ, and if we take a broad perspective, some key stages would include:
Awareness
This stage involves the patient recognizing symptoms and becoming aware of a potential health issue.
- Key considerations: Pay attention to how patients identify and interpret their symptoms, as well as the information sources they consult.
Example: John notices persistent joint pain and, through online research, suspects it might be arthritis. His journey begins with a heightened awareness of his symptoms.
Seeking information
Patients actively look for information to understand their symptoms, potential causes, and the importance of consulting a healthcare professional.
- Key considerations: Review the information sources patients use and how well they understand the need for professional medical advice.
- Example: Emily researches her persistent cough online, learning about various respiratory conditions and recognizing the importance of seeing a doctor for an accurate diagnosis.
First contact
This marks the initial interaction with the healthcare system, typically through scheduling an appointment with a primary care physician.
- Key considerations: Assess the ease of access to healthcare services and the patient's initial experience with medical professionals.
- Example: Alex schedules an appointment with his family doctor to discuss recent changes in his vision, initiating his journey within the healthcare system.
Diagnostic process
Patients undergo diagnostic tests to identify the root cause of their symptoms.
- Key considerations: Examine the efficiency of the diagnostic process and the clarity of communication about the tests.
- Example: Maria undergoes blood tests and imaging to determine the cause of her abdominal pain, marking the diagnostic phase of her journey.
Treatment planning
Patients receive a diagnosis, and healthcare providers collaborate on creating a personalized treatment plan.
- Key considerations: Evaluate how well the diagnosis is communicated and involve patients in treatment decisions.
- Example: Emily receives a diagnosis of rheumatoid arthritis. Her healthcare team takes the time to explain the condition, discusses various treatment options, and actively involves her in deciding on a comprehensive plan that combines medication, physical therapy, and lifestyle adjustments.
Treatment and clinical care service
Patients initiate the recommended treatment plan, experiencing the day-to-day challenges and improvements associated with their patient journey in a hospital.
- Key considerations: Monitor treatment adherence, side effects, and the patient's overall experience during this active phase.
- Example: Sarah starts chemotherapy for her cancer, navigating the treatment process with the support of her healthcare team.
Psychological support
Patients deal with the emotional toll of managing a health condition, including anxiety, frustration, or isolation.
- Key considerations: Acknowledge and address the emotional aspects of the journey, providing resources for mental health support.
- Example: James copes with the emotional challenges of managing chronic pain, seeking counseling to navigate the psychological impact.
Regular checkups
Patients undergo routine checkups to monitor their health status and adjust treatment plans as needed.
- Key considerations: Ensure consistent communication and scheduling of regular checkups to track progress and address any emerging issues.
- Example: Sarah, diagnosed with hypertension, attends regular checkups where the healthcare team monitors blood pressure, discusses lifestyle adjustments, and ensures medication efficacy. The routine checkups create a proactive approach to managing her condition.
Patients provide feedback on their experiences, allowing healthcare providers to refine and tailor their care.
- Key considerations: Establish mechanisms for patients to share feedback easily and transparently, encouraging an open dialogue.
- Example: John shares his experiences with a new treatment plan, providing feedback on its effectiveness, side effects, and overall impact on his daily life. This feedback loop allows the healthcare team to make timely adjustments and improve the patient's journey.
The stages may vary based on diverse scenarios and individual health circumstances. For instance, when a patient undergoes surgery or faces an acute medical event, the trajectory of their journey can diverge significantly from a more routine healthcare experience.
Factors such as the need for emergency care, hospitalization, and specialized interventions can introduce unique stages and considerations. Additionally, variations may arise due to the specific nature of medical conditions, treatments, and the individual preferences and needs of patients.
Recognizing this variability is crucial for comprehensive journey mapping, allowing for a more nuanced understanding of the patient experience across different healthcare contexts.
Types of healthcare journey maps

Healthcare journey maps can take various forms depending on their focus, purpose, and the specific aspects of the patient experience they aim to understand.
Here are a few types of healthcare journey maps:
Clinical journey maps
Focus: Emphasize the clinical aspects of a patient's experience, including diagnosis, treatment, and recovery.
Purpose: Help healthcare providers understand the medical processes and interventions involved in the patient's journey.
Example: A clinical journey map for a cancer patient would detail the steps from initial symptoms to diagnosis, treatment modalities, and post-treatment care.
Service delivery maps
Focus: Highlight the various touchpoints and services a patient encounters throughout their healthcare journey. Then, detail the back and front processes your team does or has to do during each stage.
Purpose: Enable healthcare organizations to assess the efficiency and effectiveness of service delivery.
Example: Mapping the service delivery for a patient undergoing surgery, including preoperative consultations, surgical procedures, and post-operative care.
Digital journey maps
Focus: Examine the patient's interaction with digital tools and technologies, such as online portals, mobile apps, and telehealth platforms.
Purpose: Help improve the digital aspects of patient engagement and communication.
Example: Mapping the patient's journey when using a telehealth platform for virtual consultations, prescription refills, and accessing medical records.

Chronic disease management maps
Focus: Explore the long-term journey of patients managing chronic conditions.
Purpose: Aid in understanding the challenges and opportunities for supporting patients in their ongoing self-management.
Example: A journey map for a diabetes patient would encompass regular monitoring, medication management, lifestyle adjustments, and periodic checkups.
Emergency care journey maps
Focus: Examine the patient’s experience during emergencies, from the onset of symptoms to emergency room admission and follow-up care.
Purpose: Help optimize response times, communication, and the overall emergency care process.
Example: Mapping the journey of a patient experiencing chest pain, from the initial call to emergency services to the triage process and subsequent cardiac care.
Pediatric patient journey maps
Focus: Tailored specifically for the unique needs and considerations of pediatric patients and their families.
Purpose: Address the emotional and practical aspects of pediatric healthcare experiences.
Example: Such a map is good for a child undergoing surgery to consider the role of parents, age-appropriate communication, and post-operative care.
Palliative care maps
Focus: Center on the patient's journey when facing serious illness, with a focus on providing comfort and support.
Purpose: Enhance the quality of life for patients and their families during end-of-life care.
Example: This kind of journey map suits a patient receiving palliative care when considering symptom management, emotional support, and coordination of services.
The mentioned types of maps cover different patient scenarios and clinical cases. There can also be "AS-IS" and "TO-BE" maps, reflecting the current state of the journey and the desired one, respectively.
All these types of healthcare journey maps offer a nuanced understanding of the diverse aspects of patient experiences, allowing healthcare providers and organizations to tailor their services to meet the unique needs of different patient populations.
How to do patient journey mapping?

Mapping a patient's journey is a thorough process that needs careful planning, teamwork, and analysis. Here's a guide on how to do it:
- Define the objectives
Clearly articulate the goals of the patient journey mapping exercise. Determine what aspects of the patient experience you want to understand and improve. All involved parties should be aware of these goals and agree with them.
- Assemble a cross-functional team
Form a team that includes representatives from various departments, including healthcare providers, administrative staff, patient advocates, and anyone involved in the patient experience.
- Do research
Conduct thorough research to gather quantitative and qualitative data related to the patient experience. This may involve analyzing patient records, studying existing feedback, diving into analytics and market research, and reviewing relevant literature on best practices in healthcare.
- Select a patient segment
Identify a specific patient segment or persona to focus on. This could be based on demographics, health conditions, or specific healthcare services.
Tip: You can leverage your segments or patient personas to craft an empathy map , which is particularly valuable in healthcare.
- Conduct stakeholder interviews
Interview stakeholders, including healthcare professionals and administrative staff. Gather insights into their perspectives on the patient journey, pain points, and opportunities for improvement.
- Define the stages
Outline the patient journey by mapping out each stage and interaction with the healthcare system. This can include pre-visit, during a visit, and post-visit experiences.
Tip: To speed up the process, run a journey mapping workshop with your team. It will help with the next step, too.
- Create the patient journey map
Develop a visual representation of the patient journey. This can be a timeline or infographic that illustrates each stage, touchpoint, and the emotional experience of the patient.
- Identify pain points and opportunities
Analyze the collected data to pinpoint pain points, areas of friction, and opportunities for improvement. Consider emotional, logistical, and clinical aspects of the patient experience.

- Review and validate
Consider collaborative journey mapping . Share the draft patient journey map with stakeholders, including frontline staff and patients, to validate its accuracy. Incorporate feedback to ensure a comprehensive and realistic representation.
- Develop actionable plans
Generate specific, actionable plans based on the identified pain points and opportunities. Each initiative should be feasible, considering resources and organizational constraints.
- Prioritize and implement changes
Prioritize the recommendations based on impact and feasibility. Begin implementing changes that address the identified issues, whether they involve process improvements, staff training, or technology enhancements.
- Monitor and iterate
Continuously monitor the impact of implemented changes. Gather feedback from both staff and patients to understand the effectiveness of the improvements. Iterate on the patient journey map and make recommendations as needed.
- Measure your success
You can also establish KPIs to measure the success of any improvements made based on the patient journey mapping insights. These could include patient satisfaction scores, reduced wait times, or improved communication metrics.
- Document insights (optional)
And keep a record of the lessons learned during the patient journey mapping process. This documentation can inform future initiatives and contribute to ongoing efforts to enhance the patient experience.
- Promote a culture of continuous improvement
Foster a culture within the organization that values continuous improvement in patient care. Encourage ongoing feedback and regularly revisit your journey map to ensure its relevance over time.
By following these steps, healthcare organizations can gain valuable insights into the patient experience, leading to targeted improvements that enhance healthcare quality and patient satisfaction.
How to improve the patient journey?

Striving for a seamless patient journey involves enhancing the overall experience that individuals have when seeking and receiving healthcare services. Here are some strategies to consider:
Patient-centered care
- Prioritize patient needs and preferences.
- Emphasize education and empower patients to actively participate in their healthcare journey.
- Foster open communication and active listening.
Streamlined access to care
- Reduce wait times for appointments and procedures.
- Implement online scheduling and appointment reminders.
- Provide options for virtual consultations when appropriate.
Effective communication
- Ensure clear and understandable communication with patients.
- Provide information about treatment plans, medications, and follow-up care.
- Confirm that patients are well-informed about the potential risks and benefits of treatment options.
Education and empowerment
- Offer educational resources to help patients understand their conditions and treatment options.
- Encourage patients to actively participate in their health management.
- Provide tools for self-monitoring and self-management when possible.
Care coordination
- Improve collaboration and communication among healthcare providers to strengthen care coordination, ensuring a more cohesive and seamless experience for patients throughout their healthcare journey.
- Define and implement standardized protocols for communication and handovers between care teams, reducing the risk of errors and ensuring continuity of care.
- Implement remote monitoring technologies to track patients' health remotely, enabling timely interventions and reducing the need for frequent in-person visits.
Technology integration
- Adopt electronic health records (EHRs) for efficient information sharing.
- Use telemedicine to enhance accessibility and convenience.
- Implement mobile health apps for appointment reminders, medication management, and health tracking.
Feedback and continuous improvement
- Conduct regular surveys to gather specific insights into patient satisfaction, allowing for a more nuanced understanding of their experiences.
- Establish easily accessible channels for patients to provide real-time feedback, ensuring that their voices are heard promptly.
- Respond promptly to patient feedback, address concerns, and communicate any changes or resolutions, fostering a sense of responsiveness and accountability.
Cultural competency
- Train healthcare staff to be culturally competent and sensitive to diverse patient needs.
- Promote diversity in healthcare staff to reflect the communities served, fostering a more inclusive and culturally sensitive environment.
- Recognize and celebrate cultural awareness events within the healthcare setting, fostering an inclusive atmosphere that appreciates the richness of diverse traditions.
Emotional support
- Address the emotional and psychological aspects of healthcare.
- Provide resources for mental health and emotional well-being.
- Consider support groups or counseling services.
Efficient billing and financial assistance
- Simplify billing processes and provide clear information about costs.
- Offer financial assistance programs for patients in need.
- Communicate transparently about insurance coverage and out-of-pocket expenses.
Staff training:
- Train healthcare staff in patient-centered communication and empathy.
- Ensure staff is knowledgeable about the resources available to patients.
- Foster a culture of empathy and compassion in the healthcare environment.
By focusing on these aspects, healthcare providers can contribute to a more positive and effective patient journey. Regularly reassessing and adapting strategies based on feedback and evolving healthcare trends is crucial for ongoing improvement.
UXPressia already has some healthcare journey map examples:
- Surgical patient journey
This map focuses on the healthcare journey of a patient persona, Robin, from the moment when the patient understands that something is wrong to the recovery period. This journey is long and very detailed.
- Non-surgical patient journey
This map visualizes the journey of a patient, Lotta, who decides to undergo a checkup at a hospital. She schedules a visit, gets a consultation, takes some tests, and starts taking some medicine prescribed by her doctor.
More healthcare and well-being templates are available in our library.
Wrapping up
In wrapping up, think of patient journey mapping as a powerful tool reshaping the healthcare landscape, with the patient's experience taking center stage. It's like creating a roadmap that intricately traces every step of a patient's interaction within the healthcare system.
This deliberate mapping isn't just a plan; it's a compass guiding healthcare organizations toward key points where they can enhance patient satisfaction, simplify access to care, and cultivate a more compassionate and patient-focused healthcare environment. Investing in patient journey mapping is more than a strategy—it's a dedication to raising the bar in care quality, amplifying the patient's voice, and ensuring that every leg of the healthcare journey is characterized by empathy, understanding, and an unwavering pursuit of excellence in patient experience.
Related posts
Rate this post

- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Process mapping the...
Process mapping the patient journey: an introduction
- Related content
- Peer review
- Timothy M Trebble , consultant gastroenterologist 1 ,
- Navjyot Hansi , CMT 2 1 ,
- Theresa Hydes , CMT 1 1 ,
- Melissa A Smith , specialist registrar 2 ,
- Marc Baker , senior faculty member 3
- 1 Department of Gastroenterology, Portsmouth Hospitals Trust, Portsmouth PO6 3LY
- 2 Department of Gastroenterology, Guy’s and St Thomas’ NHS Foundation Trust, London
- 3 Lean Enterprise Academy, Ross-on-Wye, Hertfordshire
- Correspondence to: T M Trebble tim.trebble{at}porthosp.nhs.uk
- Accepted 15 July 2010
Process mapping enables the reconfiguring of the patient journey from the patient’s perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital.
Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the patient’s perspective to identify problems and suggest improvements. 1 2 We outline the steps involved in mapping the patient’s journey, as we believe that a basic understanding of this versatile and simple technique, and when and how to use it, is valuable to clinicians who are developing clinical services.
What information does process mapping provide and what is it used for?
Process mapping allows us to “see” and understand the patient’s experience 3 by separating the management of a specific condition or treatment into a series of consecutive events or steps (activities, interventions, or staff interactions, for example). The sequence of these steps between two points (from admission to the accident and emergency department to discharge from the ward) can be viewed as a patient pathway or process of care. 4
Improving the patient pathway involves the coordination of multidisciplinary practice, aiming to maximise clinical efficacy and efficiency by eliminating ineffective and unnecessary care. 5 The data provided by process mapping can be used to redesign the patient pathway 4 6 to improve the quality or efficiency of clinical management and to alter the focus of care towards activities most valued by the patient.
Process mapping has shown clinical benefit across a variety of specialties, multidisciplinary teams, and healthcare systems. 7 8 9 The NHS Institute for Innovation and Improvement proposes a range of practical benefits using this approach (box 1). 6
Box 1 Benefits of process mapping 6
A starting point for an improvement project specific for your own place of work
Creating a culture of ownership, responsibility and accountability for your team
Illustrates a patient pathway or process, understanding it from a patient’s perspective
An aid to plan changes more effectively
Collecting ideas, often from staff who understand the system but who rarely contribute to change
An interactive event that engages staff
An end product (a process map) that is easy to understand and highly visual
Several management systems are available to support process mapping and pathway redesign. 10 11 A common technique, derived originally from the Japanese car maker Toyota, is known as lean thinking transformation. 3 12 This considers each step in a patient pathway in terms of the relative contribution towards the patient’s outcome, taken from the patient’s perspective: it improves the patient’s health, wellbeing, and experience (value adding) or it does not (non-value or “waste”) (box 2). 14 15 16
Box 2 The eight types of waste in health care 13
Defects —Drug prescription errors; incomplete surgical equipment
Overproduction —Inappropriate scheduling
Transportation —Distance between related departments
Waiting —By patients or staff
Inventory —Excess stores, that expire
Motion —Poor ergonomics
Overprocessing —A sledgehammer to crack a nut
Human potential —Not making the most of staff skills
Process mapping can be used to identify and characterise value and non-value steps in the patient pathway (also known as value stream mapping). Using lean thinking transformation to redesign the pathway aims to enhance the contribution of value steps and remove non-value steps. 17 In most processes, non-value steps account for nine times more effort than steps that add value. 18
Reviewing the patient journey is always beneficial, and therefore a process mapping exercise can be undertaken at any time. However, common indications include a need to improve patients’ satisfaction or quality or financial aspects of a particular clinical service.
How to organise a process mapping exercise
Process mapping requires a planned approach, as even apparently straightforward patient journeys can be complex, with many interdependent steps. 4 A process mapping exercise should be an enjoyable and creative experience for staff. In common with other audit techniques, it must avoid being confrontational or judgmental or used to “name, shame, and blame.” 8 19
Preparation and planning
A good first step is to form a team of four or five key staff, ideally including a member with previous experience of lean thinking transformation. The group should decide on a plan for the project and its scope; this can be visualised by using a flow diagram (fig 1 ⇓ ). Producing a rough initial draft of the patient journey can be useful for providing an overview of the exercise.
Fig 1 Steps involved in a process mapping exercise
- Download figure
- Open in new tab
- Download powerpoint
The medical literature or questionnaire studies of patients’ expectations and outcomes should be reviewed to identify value adding steps involved in the management of the clinical condition or intervention from the patient’s perspective. 1 3
Data collection
Data collection should include information on each step under routine clinical circumstances in the usual clinical environment. Information is needed on waiting episodes and bottlenecks (any step within the patient pathway that slows the overall rate of a patient’s progress, normally through reduced capacity or availability 20 ). Using estimates of minimum and maximum time for each step reduces the influence of day to day variations that may skew the data. Limiting the number of steps (to below 60) aids subsequent analysis.
The techniques used for data collection (table 1 ⇓ ) each have advantages and disadvantages; a combination of approaches can be applied, contributing different qualitative or quantitative information. The commonly used technique of walking the patient journey includes interviews with patients and staff and direct observation of the patient journey and clinical environment. It allows the investigator to “see” the patient journey at first hand. Involving junior (or student) doctors or nurses as interviewers may increase the openness of opinions from staff, and time needed for data collection can be reduced by allotting members of the team to investigate different stages in the patient’s journey.
Data collection in process mapping
- View inline
Mapping the information
The process map should comprehensively represent the patient journey. It is common practice to draw the map by hand onto paper (often several metres long), either directly or on repositionable notes (fig 2 ⇓ ).
Fig 2 Section of a current state map of the endoscopy patient journey
Information relating to the steps or representing movement of information (request forms, results, etc) can be added. It is useful to obtain any missing information at this stage, either from staff within the meeting or by revisiting the clinical environment.
Analysing the data and problem solving
The map can be analysed by using a series of simple questions (box 3). The additional information can be added to the process map for visual representation. This can be helped by producing a workflow diagram—a map of the clinical environment, including information on patient, staff, and information movement (fig 3 ⇓ ). 18
Box 3 How to analyse a process map 6
How many steps are involved?
How many staff-staff interactions (handoffs)?
What is the time for each step and between each step?
What is the total time between start and finish (lead time)?
When does a patient join a queue, and is it a regular occurrence?
How many non-value steps are there?
What do patients complain about?
What are the problems for staff?
Fig 3 Workflow diagram of current state endoscopy pathway
Redesigning the patient journey
Lean thinking transformation involves redesigning the patient journey. 21 22 This will eliminate, combine and simplify non-value steps, 23 limit the impact of rate limiting steps (such as bottlenecks), and emphasise the value adding steps, making the process more patient-centred. 6 It is often useful to trial the new pathway and review its effect on patient management and satisfaction before attempting more sustained implementation.
Worked example: How to undertake a process mapping exercise
South Coast NHS Trust, a large district general hospital, plans to improve patient access to local services by offering unsedated endoscopy in two peripheral units. A consultant gastroenterologist has been asked to lead a process mapping exercise of the current patient journey to develop a fast track, high quality patient pathway.
In the absence of local data, he reviews the published literature and identifies key factors to the patient experience that include levels of discomfort during the procedure, time to discuss the findings with the endoscopist, and time spent waiting. 24 25 26 27 He recruits a team: an experienced performance manager, a sister from the endoscopy department, and two junior doctors.
The team drafts a map of the current endoscopy journey, using repositionable notes on the wall. This allows team members to identify the start (admission to the unit) and completion (discharge) points and the locations thought to be involved in the patient journey.
They decide to use a “walk the journey” format, interviewing staff in their clinical environments and allowing direct observation of the patient’s management.
The junior doctors visit the endoscopy unit over two days, building up rapport with the staff to ensure that they feel comfortable with being observed and interviewed (on a semistructured but informal basis). On each day they start at the point of admission at the reception office and follow the patient journey to completion.
They observe the process from staff and patient’s perspectives, sitting in on the booking process and the endoscopy procedure. They identify the sequence of steps and assess each for its duration (minimum and maximum times) and the factors that influence this. For some of the steps, they use a digital watch and notepad to check and record times. They also note staff-patient and staff-staff interactions and their function, and the recording and movement of relevant information.
Details for each step are entered into a simple table (table 2 ⇓ ), with relevant notes and symbols for bottlenecks and patients’ waits.
Patient journey for non-sedated upper gastrointestinal endoscopy
When data collection is complete, the doctor organises a meeting with the team. The individual steps of the patient journey are mapped on a single long section of paper with coloured temporary markers (fig 2 ⇑ ); additional information is added in different colours. A workflow diagram is drawn to show the physical route of the patient journey (fig 3 ⇑ ).
The performance manager calculates that the total patient journey takes a minimum of 50 minutes to a maximum of 345 minutes. This variation mainly reflects waiting times before a number of bottleneck steps.
Only five steps (14 to 17 and 22, table 2 ⇑ ) are considered both to add value and needed on the day of the procedure (providing patient information and consent can be obtained before the patient attends the department). These represent from 13 to 47 minutes. At its least efficient, therefore, only 4% of the patient journey (13 of 345 minutes) is spent in activities that contribute directly towards the patient’s outcome.
The team redesigns the patient journey (fig 4 ⇓ ) to increase time spent on value adding aspects but reduce waiting times, bottlenecks, and travelling distances. For example, time for discussing the results of the procedure is increased but the location is moved from the end of the journey (a bottleneck) to shortly after the procedure in the anteroom, reducing the patient’s waiting time and staff’s travelling distances.
Fig 4 Workflow diagram of future state endoscopy pathway
Implementing changes and sustaining improvements
The endoscopy staff are consulted on the new patient pathway, which is then piloted. After successful review two months later, including a patient satisfaction questionnaire, the new patient pathway is formally adopted in the peripheral units.
Further reading
Practical applications.
NHS Institute for Innovation and Improvement ( https://www.institute.nhs.uk )—comprehensive online resource providing practical guidance on process mapping and service improvement
Lean Enterprise Academy ( http://www.leanuk.org )—independent body dedicated to lean thinking in industry and healthcare, through training and academic discussion; its publication, Making Hospitals Work 23 is a practical guide to lean transformation in the hospital environment
Manufacturing Institute ( http://www.manufacturinginstitute.co.uk )—undertakes courses on process mapping and lean thinking transformation within health care and industrial practice
Theoretical basis
Bircheno J. The new lean toolbox . 4th ed. Buckingham: PICSIE Books, 2008
Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 [online publication 29 April]
Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998; 7 (suppl):S30-6
Graban M. Lean hospitals, improving quality, patient safety and employee satisfaction . New York: Taylor & Francis, 2009
Womack JP, Jones DT. Lean thinking . 2nd ed. London: Simon & Schuster, 2003
Cite this as: BMJ 2010;341:c4078
Contributors: TMT designed the protocol and drafted the manuscript; TMT, MB, JH, and TH collected and analysed the data; all authors critically reviewed and contributed towards revision and production of the manuscript. TMT is guarantor.
Competing interests: MB is a senior faculty member carrying out research for the Lean Enterprise Academy and undertakes paid consultancies both individually and from Lean Enterprise Academy, and training fees for providing lean thinking in healthcare.
Provenance and peer review: Not commissioned; externally peer reviewed.
- ↵ Kollberg B, Dahlgaard JJ, Brehmer P. Measuring lean initiatives in health care services: issues and findings. Int J Productivity Perform Manage 2007 ; 56 : 7 -24. OpenUrl CrossRef
- ↵ Bevan H, Lendon R. Improving performance by improving processes and systems. In: Walburg J, Bevan H, Wilderspin J, Lemmens K, eds. Performance management in health care. Abingdon: Routeledge, 2006:75-85.
- ↵ Kim CS, Spahlinger DA, Kin JM, Billi JE. Lean health care: what can hospitals learn from a world-class automaker? J Hosp Med 2006 ; 1 : 191 -9. OpenUrl CrossRef PubMed
- ↵ Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998 ; 7 (suppl): S30 -6. OpenUrl
- ↵ Peterson KM, Kane DP. Beyond disease management: population-based health management. Disease management. Chicago: American Hospital Publishing, 1996.
- ↵ NHS Modernisation Agency. Process mapping, analysis and redesign. London: Department of Health, 2005;1-40.
- ↵ Taylor AJ, Randall C. Process mapping: enhancing the implementation of the Liverpool care pathway. Int J Palliat Nurs 2007 ; 13 : 163 -7. OpenUrl PubMed
- ↵ Ben-Tovim DI, Dougherty ML, O’Connell TJ, McGrath KM. Patient journeys: the process of clinical redesign. Med J Aust 2008 ; 188 (suppl 6): S14 -7. OpenUrl PubMed Web of Science
- ↵ King DL, Ben-Tovim DI, Bassham J. Redesigning emergency department patient flows: application of lean thinking to health care. Emerg Med Australas 2006 ; 18 : 391 -7. OpenUrl CrossRef PubMed
- ↵ Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 ; published online 29 April.
- ↵ Rath F. Tools for developing a quality management program: proactive tools (process mapping, value stream mapping, fault tree analysis, and failure mode and effects analysis). Int J Radiat Oncol Biol Phys 2008 ; 71 (suppl): S187 -90. OpenUrl PubMed Web of Science
- ↵ Womack JP, Jones DT. Lean thinking. 2nd ed. London: Simon & Schuster, 2003.
- ↵ Graban M. Value and waste. In: Lean hospitals. New York: Taylor & Francis, 2009;35-56.
- ↵ Westwood N, James-Moore M, Cooke M. Going lean in the NHS. London: NHS Institute for Innovation and Improvement, 2007.
- ↵ Liker JK. The heart of the Toyota production system: eliminating waste. The Toyota way. New York: McGraw-Hill, 2004;27-34.
- ↵ Womack JP, Jones DT. Introduction: Lean thinking versus Muda. In: Lean thinking. 2nd ed. London: Simon & Schuster, 2003:15-28.
- ↵ George ML, Rowlands D, Price M, Maxey J. Value stream mapping and process flow tools. Lean six sigma pocket toolbook. New York: McGraw Hill, 2005:33-54.
- ↵ Fillingham D. Can lean save lives. Leadership Health Serv 2007 ; 20 : 231 -41. OpenUrl CrossRef
- ↵ Benjamin A. Audit: how to do it in practice. BMJ 2008 ; 336 : 1241 -5. OpenUrl FREE Full Text
- ↵ Vissers J. Unit Logistics. In: Vissers J, Beech R, eds. Health operations management patient flow logistics in health care. Oxford: Routledge, 2005:51-69.
- ↵ Graban M. Overview of lean for hospital. Lean hospitals. New York: Taylor & Francis, 2009;19-33.
- ↵ Eaton M. The key lean concepts. Lean for practitioners. Penryn, Cornwall: Academy Press, 2008:13-28.
- ↵ Baker M, Taylor I, Mitchell A. Analysing the situation: learning to think differently. In: Making hospitals work. Ross-on-Wye: Lean Enterprise Academy, 2009:51-70.
- ↵ Ko HH, Zhang H, Telford JJ, Enns R. Factors influencing patient satisfaction when undergoing endoscopic procedures. Gastrointest Endosc 2009 ; 69 : 883 -91. OpenUrl CrossRef PubMed Web of Science
- ↵ Del Rio AS, Baudet JS, Fernandez OA, Morales I, Socas MR. Evaluation of patient satisfaction in gastrointestinal endoscopy. Eur J Gastroenterol Hepatol 2007 ; 19 : 896 -900. OpenUrl CrossRef PubMed Web of Science
- ↵ Seip B, Huppertz-Hauss G, Sauar J, Bretthauer M, Hoff G. Patients’ satisfaction: an important factor in quality control of gastroscopies. Scand J Gastroenterol 2008 ; 43 : 1004 -11. OpenUrl CrossRef PubMed Web of Science
- ↵ Yanai H, Schushan-Eisen I, Neuman S, Novis B. Patient satisfaction with endoscopy measurement and assessment. Dig Dis 2008 ; 26 : 75 -9. OpenUrl CrossRef PubMed Web of Science
Root out friction in every digital experience, super-charge conversion rates, and optimize digital self-service
Uncover insights from any interaction, deliver AI-powered agent coaching, and reduce cost to serve
Increase revenue and loyalty with real-time insights and recommendations delivered to teams on the ground
Know how your people feel and empower managers to improve employee engagement, productivity, and retention
Take action in the moments that matter most along the employee journey and drive bottom line growth
Whatever they’re are saying, wherever they’re saying it, know exactly what’s going on with your people
Get faster, richer insights with qual and quant tools that make powerful market research available to everyone
Run concept tests, pricing studies, prototyping + more with fast, powerful studies designed by UX research experts
Track your brand performance 24/7 and act quickly to respond to opportunities and challenges in your market
Explore the platform powering Experience Management
- Free Account
- For Digital
- For Customer Care
- For Human Resources
- For Researchers
- Financial Services
- All Industries
Popular Use Cases
- Customer Experience
- Employee Experience
- Employee Exit Interviews
- Net Promoter Score
- Voice of Customer
- Customer Success Hub
- Product Documentation
- Training & Certification
- XM Institute
- Popular Resources
- Customer Stories
- Market Research
- Artificial Intelligence
- Partnerships
- Marketplace
The annual gathering of the experience leaders at the world’s iconic brands building breakthrough business results, live in Salt Lake City.
- English/AU & NZ
- Español/Europa
- Español/América Latina
- Português Brasileiro
- REQUEST DEMO
- Experience Management
- Sector Specific
- Patient Experience
- Patient Journey
Try Qualtrics for free
The patient journey: what it is and how it’s vital for success.
10 min read In the digital age, the patient experience has become more complex but also more critical as it relates to patient retention, reimbursement, and patient satisfaction. In order to thrive in today’s healthcare landscape, it’s important to look at the patient journey when aiming to improve the patient experience.
Does your healthcare organization ask patients for feedback following clinical encounters? This is a common approach used to improve the patient experience . You may gather key insights about a specific encounter, but you’ll miss out on an untapped system of important patient interactions throughout the care journey .
Stay up-to-date on patient experience management trends with our guide
Improving patient experiences requires looking at the entire healthcare ecosystem. Patients communicate with their healthcare providers through a variety of channels, while interacting with a wide range of departments and individuals along the way.
To stand out in the market and provide an optimal experience for your patients , hospitals and health systems should look beyond clinical service delivery and begin patient journey mapping.
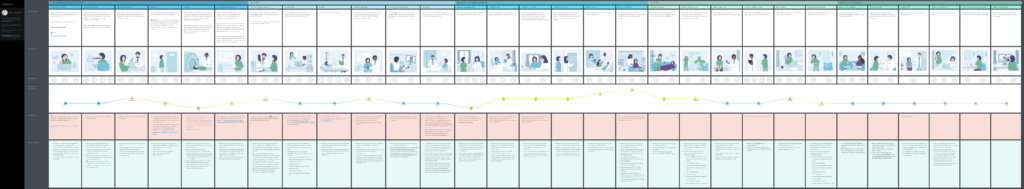
The patient journey is the entire sequence of events that begins when the patient first develops a need for clinical care and engages with your organization. It follows the patient’s steps as they navigate your healthcare system, from initial scheduling to treatment to continuous care.
The patient journey vs. the patient experience
Why is the patient journey important? Each touchpoint of the patient engagement journey, from a simple visit to your website to checking in for an appointment, has downstream effects that can help or hinder meeting patient needs.
As the patient experience evolves , it’s important to expand how you are listening to your patients in order to close gaps and make continuous improvements.
In recent years, emphasis on the patient experience has become the focus of regulatory programs and payment incentives. Many quality measures today center around collecting patient feedback on the healthcare experience.
To satisfy these measures and drive quality improvement efforts, many organizations turn to post-transactional patient satisfaction surveys . The feedback from these surveys often measures only a limited set of touchpoints while overlooking other critical data from the full patient journey.
A holistic view
Patient experience programs often hone in on clinical service delivery, and many regulatory programs focus solely on numerical scores to measure improvement. These approaches may fail to identify pain points occurring in dozens of patient interactions within a healthcare system.
A holistic view of the patient journey is the key to modernizing and strengthening your efforts to meet your patients’ needs . By breaking down silos into separate patient events, you can begin to identify blind spots where hidden challenges exist in your patient experiences.
By the time your patients engage with their care providers, they’ve likely interacted with your organization a number of times. These interactions can occur digitally, over the phone, or in person. Navigating your website, verifying insurance coverage, and scheduling an appointment are all examples of pain points that may be creating barriers to care.
It’s easy to assume any given touchpoint is more or less important than another. The fact is that each one provides unique value to the patient’s experience. Each of them plays a role in helping the patient achieve their goals.
Patient engagement with your organization doesn’t begin when the patient is examined by the healthcare provider, or even when they enter your medical facility. From initial awareness to ongoing care, the patient journey encompasses every separate interaction throughout the process of seeking, receiving, and continuing care within a health system.
There are several stages of the patient journey you should consider.
What triggers the patient’s need for care, and how does the patient learn about your organization?
- Quality ratings and online reputation
- Campaign management
- Community involvement
Consideration
What drives a patient to choose your organization over another?
- Coverage and benefits
- Healthcare provider search
What impacts your patient’s ability to receive care or support from your organization?
- Patient portal
- Call center
- Price transparency
Service delivery
What is your patient’s experience with their clinical care?
- Interaction with healthcare professionals
- Check-in and check-out
- Discharge process
Ongoing care
What type of patient engagement occurs after a visit?
- Wellness and care management
- Social determinants of health
- Population health
All of these examples influence the way in which your patients make decisions. It’s essential to understand which touchpoints along the patient’s journey are the most impactful or leave the largest gaps in care. There are patient expectations surrounding each type of interaction.
Patient journey mapping
How do you move beyond patient feedback on service delivery and focus instead on the end-to-end patient journey? Patient journey mapping can provide context around what your patients experience as they move through the various channels of your organization.
A patient journey map is a visual representation of the steps the patient takes as they engage with your organization in order to receive care. Patient journey maps should capture pre-visit and post-visit touchpoints in addition to those that occur when the patient is onsite at your medical facility.
Your patient journey may be broad and applicable to your entire patient base, or it may be specific to certain specialties, patient personas , demographics , or health events.
Start with an inventory of all the touchpoints for which you currently collect patient feedback. Next, determine what’s missing. Envision moving through your organization from your patient’s point of view. Your patient journey map should include Interactions that take place pre-visit and post-visit, which are not always captured by traditional or regulatory surveys.
Benefits of patient journey mapping
There are many benefits to capturing key moments along the whole patient journey.
- A patient journey map allows you to walk in your patient’s shoes and think the way they think as they engage with your organization. Patient journey mapping looks at patient experiences from the outside in.
- Mapping your patient journeys helps you to hone in on the areas where you may not be listening to your patients, but should be.
- You can uncover inconsistencies, gaps in care, and common pain points with patient journey mapping. These are difficult to identify when you collect feedback only on service delivery. Collecting data around these areas can aid in process optimization and improve patient satisfaction.
- A patient journey map can give you a cross-functional view of your patient experience so you can engage all teams and stakeholders in gathering and understanding patient insights .
- Patient journey mapping provides context around behavior and attitudes as patients move throughout the channels of your organization. Are patients having to repeat paperwork? Do patients understand their follow-up care instructions? Are your patients able to easily navigate your patient portal? Patient journey mapping can help to answer these types of questions.
- Mapping the patient journey can transform your patient care approach from a reactive one to a proactive one.
Using patient journey data
Once you can visualize the end-to-end patient journey within your organization, it’s time to listen to your patients and start gathering data.
Gather the right data
Collect data on all the touchpoints of the patient journey. Understand how your patients are interacting with every aspect of your organization, including non-clinical interactions such as your website, scheduling, and billing. Involve multiple stakeholders during this process, including managers, doctors, nurses, other healthcare professionals, and administrative staff.
It’s important to capture all steps involved in each of these stages. For example, when looking for potential pain points surrounding the patient portal, consider how the patient sets up an account, logs in, navigates the interface, gets technical assistance, and so forth.
Also, consider patient expectations and usage–what are they using the portal to accomplish? Look for potential gaps in these experiences , such as paying a bill, contacting the provider with a question, reviewing test results, or scheduling an appointment.
Understanding the patient’s goals and actions along all the different paths of your patient journeys is essential to gathering the data you need to take action.
Understand the data
Gain insights using analytics , benchmarking, and visualizations to identify gaps and discover opportunities at each step of the patient’s journey. Trends along the various touchpoints can help you to discover pain points and identify opportunities.
It’s also important to engage all the right stakeholders when reviewing the data you collect. Involving the right teams and people is essential to understanding gaps and improving experiences.
Take action
Use the insights from all touchpoints along your patient journey to develop solutions to improve your patient experience.
A closed-loop system is ideal for taking action to close gaps along the patient journey. For example, if a patient gives a low score on a survey for your online scheduling tool, you could follow up with the patient to ensure they were able to schedule an appointment.
Using the data you collect to drive specific actions and feed into processes is vital to creating a seamless patient journey.
Why Qualtrics?
At Qualtrics, we want to enable you to listen to and understand your patients across all aspects of their journey, all within a single platform. Omnichannel distribution lets you gather feedback from patients from where they are at during each touchpoint, with powerful built-in analytics for uncovering meaningful insights.
The Qualtrics XM Platform™ provides a single source for all of your patient journey data. Real-time feedback displayed in role- and location-based dashboards helps deliver pertinent information to the right people, allowing you to take prompt action where needed.
Ready to collect data and drive action along your patient journey?
Related resources
Patient experience 12 min read, symptoms survey 10 min read, nurse satisfaction survey 11 min read, cahps surveys 6 min read, patient journey mapping 15 min read, patient feedback 15 min read, healthcare branding 13 min read, request demo.
Ready to learn more about Qualtrics?
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Exploring the hospital patient journey: What does the patient experience?
Raffaella gualandi.
1 Department of Nursing, Università Campus Bio-Medico di Roma, Rome, Italy
Cristina Masella
2 Department of Management Economics and Industrial Engineering, Politecnico di Milano, Milan, Italy
Daniela Viglione
Daniela tartaglini, associated data.
All relevant data are within the paper and its Supporting Information files.
To understand how different methodologies of qualitative research are able to capture patient experience of the hospital journey.
A qualitative study of orthopaedic patients admitted for hip and knee replacement surgery in a 250-bed university hospital was performed. Eight patients were shadowed from the time they entered the hospital to the time of transfer to rehabilitation. Four patients and sixteen professionals, including orthopaedists, head nurses, nurses and administrative staff, were interviewed.
Through analysis of the data collected four main themes emerged: the information gap; the covering patient-professionals relationship; the effectiveness of family closeness; and the micro-integration of hospital services. The three different standpoints (patient shadowing, health professionals’ interviews and patients’ interviews) allowed different issues to be captured in the various phases of the journey.
Conclusions
Hospitals can significantly improve the quality of the service provided by exploring and understanding the individual patient journey. When dealing with a key cross-functional business process, the time-space dynamics of the activities performed have to be considered. Further research in the academic field can explore practical, methodological and ethical challenges more deeply in capturing the whole patient journey experience by using multiple methods and integrated tools.
Introduction
In the healthcare knowledge-based system, literature has given increasing attention over time to improving clinical knowledge, including by making use of the patient's insider perspective [ 1 – 3 ]. In particular, patient experience of healthcare and the delivery of care is emerging as an important area of knowledge, but one that is sometimes overlooked [ 4 , 5 ].
The Beryl Institute defines patient experience as “the sum of all interactions, shaped by an organization’s culture, that influence patient perceptions, across the continuum of care”[ 6 ]. Wolf et al. specify that interactions are “The orchestrated touchpoints of people, processes, policies, communications, actions, and environment” and patient perceptions are “what is recognized, understood and remembered by patients and support people”[ 7 ].
In the last few years, emphasis on the emotional drivers of engagements has led many authors to enhance the customer experience starting from an analysis of the customer journey [ 8 ]. In the hospital context, the patient journey is a key cross-functional business process where patient and providers share action and information flows between people and systems across various touchpoints. Providers aim to manage hospital patient flow in order to provide safe and efficient patient care while ensuring the best use of hospital resources (i.e.: beds, operating theatres, clinics and specialized staff). Poor patient flow may result in decreasing levels of productivity, increasing risk of harming patients and decreasing levels of quality perceived by patients [ 9 – 11 ]. Patients aim to receive the best care together with a high quality of service. As a matter of fact, the patient is the only actor who experiences the whole path by connecting each step of the journey. Therefore, hospitals can significantly improve the quality of the service provided by exploring and understanding the individual patient journey [ 12 – 14 ].
Many tools may be used to measure and understand patient experience [ 15 , 16 ]. Surveys are the methods mainly used to capture the patient experience and to evaluate the quality and safety of various clinical processes [ 17 , 18 ]. However, questionnaires or traditional static observation may not be well-suited to reveal all the aspects of patient experience [ 19 ]. In the complex hospital environment, multiple factors can affect the patient experience, including the time-space dynamics of the activities performed and the patients’ perceptions and emotions lived at the time of the experience [ 20 ]. Moreover, some authors emphasize that what the patient remembers is different from what he/she experiences in real-time, depending on the length of the recall period [ 21 , 22 ]. Therefore, as what the patient remembers may change over time, gathering accurate and immediate data on the experience lived also depends on the time of the interview.
A recent study reports how the use of unstructured diaries completed in a patient’s own words can capture the hospital-stay experience from the patient’s own perspective. However, it is not clear how real-time experiences are reported in relation to high-emotional situations or clinical activities that can interfere with the patient’s ability and willingness to write (i.e. during the transfer to the operating theatre or in the post-operative period, immediately after surgery). Furthermore, the authors show how study participants with a tertiary education wrote more in their diaries than those without [ 23 ]. This could potentially eliminate important aspects of the experience lived by vulnerable people.
Some authors have emphasized the value of shadowing for phenomenological research, by giving a more complete picture of the phenomenon in the real-time context of an organization [ 24 , 25 ]. Patient shadowing may have an especially valuable role in gaining insights into complex cross-hospital processes, in particular when dealing with vulnerable people who could be excluded from interview studies [ 26 , 27 ]. Furthermore, some studies have reported how, through shadowing methodology, it is possible to assess the lived experience of patients in a patient-centred perspective [ 28 , 29 ]. However, methodological and ethical issues of shadowing still need to be explored in greater depth [ 25 , 30 ].
While on the one hand patient experience is increasingly considered as a driver for health services improvement, on the other it is still not clear how to capture the whole patient experience in traversing hospital services [ 31 – 33 ]. Therefore, this study seeks to explore which aspects of the hospital patient journey experience may be captured by the three different standpoints: patient shadowing, health professionals’ interviews and patients interviews. Accordingly, it aims to answer the following questions: what does the patient experience through the hospital journey? How can it be captured?
Materials and methods
Study design.
This study was a qualitative study with a phenomenological‐hermeneutic approach using participant interviews and patient shadowing [ 34 , 35 ]. The Consolidated Criteria for Reporting Qualitative Research—COREQ checklist was used as a guideline to report the study data [ 36 ]. The study was undertaken in a 250-bed Italian academic teaching hospital. Orthopaedic patients undergoing total hip (THA) or knee arthroplasty (TKA) were selected in order to analyse a standard clinical path ( Fig 1 ). Urgently admitted patients were excluded due to the different clinical path they have to follow. The unit of analysis was the hospital patient’s journey starting from the first outpatient visit and concluding with the first follow-up visit. The study was approved by the Hospital Ethics Committee.

Data collection
Between August 2016 and April 2017, a total of twelve patients and sixteen key professionals were invited to participate and all agreed. There were no prior relationships between researchers and patients; two researchers knew some healthcare professionals because they worked in the same hospital, though in different units and without patient care roles. The possibility of coercion was minimized by guaranteeing data anonymity, by requesting voluntary participation in the study and by dealing with issues on which the researchers had no power to influence anything or anyone at hospital managerial level.
A convenience sample of patients was selected based on whether their inpatient admission and follow-up visit fell within the observation period. Inclusion criteria were: patients scheduled to undergo surgery for THA or TKA, for the shadowing phase; patients who had had a THA or TKA ad were in follow-up, for the interviews. Exclusion criteria were: <18 years, inability to understand, not wanting to participate, inability to read/speak Italian. Patients were asked to participate in the study at the time they arrived in the hospital. The first author invited patients to participate in the study when they met at the hospital for preoperative tests or on the day of admission. Patients accepting the invitation were provided with further information about the project by the first author, and were asked to sign their consent to participate in the study and to the anonymous use of their data.
Eight patients admitted between August and September 2016 were selected for the shadowing phase. A shadowing methodology was used in order to provide an embodied understanding of patients’ experiences in context [ 26 ]. Two female students from the nursing and industrial engineering degree courses, with no roles in the delivery of patient care, were trained for data collection by the first author. In this way, the risk of not reporting negative feedback during the study by the participants, and subjective interpretations by the authors in capturing data, was minimized. Patients were shadowed from the time of hospital admission to the time of discharge, with the shadower observing the patient during daytime hours and completing a data collection form prepared by the research group. This involved recording every step of the hospital journey process, by analysing each touchpoint and including time, patient, caregiver, activity, shadower’s observations, and impressions. In particular, touchpoint observations indicated where patients and families go (setting), with whom they come into contact, how long the experience at each touchpoint takes (time), what patients and caregivers do, and a description of any comments of the patient and family, including any observable emotional state of the patient. By considering patients’ emotion as consistent responses to internal or external events, the Plutchik’s model was used as framework to understand its intensity in a positive or negative characterization [ 37 ]. In particular, Plutchik suggests emotions are low, medium or high-intensity, and if left unchecked, they can intensify. Accordingly, the patient's emotional journey was also assessed in reference to external events that altered the patient's emotional level.
Patient care procedures were not noted because they were not relevant for the current research objectives. The shadower observed the patients during all hospital transfers and entered the patients’ rooms only to verify their general state and to gather any statements about their experience. The shadower was mainly passive during the observation, but was active in informal conversations. This level of proximity made it possible for the patients not to perceive shadowers as intrusive or disrespectful of their privacy.
Between September 2016 and April 2017, four patients and sixteen healthcare professionals participated in face-to-face open interviews lasting 30–45 minutes and performed by the first and the third author. A few main open questions were identified by the research group in order to analyse the main steps of the patients’ journeys, the patients’ experiences, and their reported emotions. Patients were interviewed at the first outpatient follow-up visit ( Fig 1 ), scheduled one month after discharge from the ward, in order to include their perceptions of discharge.
In order to capture viewpoints representing various different roles, a collaborative purposive sampling technique was used among professionals with different level of professional experience who take care of orthopaedic patients. In particular, according to Benner’s stages of clinical competence [ 38 ], two nurses with experience of at least five years, identified as expert nurses by their managers, and three nurses with experience of up to four years, identified as competent nurses, were selected. In addition, two orthopaedic surgeons and one medical doctor under training were involved. Finally, three members of the administrative staff, the director responsible for the quality of care processes, and the head nurses of the units involved in the patient journeys (i.e.: two Ward Units, one Surgery Room, one Rehabilitation Unit), were interviewed.
All interviews were audio-recorded and transcribed verbatim with participant permission. Data from the field notes and the interviews were transferred to an Excel spreadsheet database to systematize them and for the subsequent analysis.
Data analysis
Data analysis was performed on three levels as suggested by Ricoeur [ 30 ]: a naïve reading, a structural analysis and a critical analysis and discussion. The first author performed a thematic analysis of the text material. In the structural analysis, the units of meaning (what was said) were reflected in units of significance (what the texts were talking about) from which the key themes emerged ( Table 1 ). Patients’ emotions, reported or observed, were classified according to Plutchik’s Wheel of Emotions [ 37 ]. After that, a critical analysis was carried out by the researchers in order to analyse the coding process, the categories and the meanings that emerged.
The main characteristics of the participants involved in the study are reported in Table 2 . Patients involved ranged in age from 56–78 years with an average age of 67.3 years, and they were hospitalized on average 4.4 days. All had a regular clinical trajectory with no noteworthy complications. Healthcare professionals ranged in age from 29–61 years with an average age of 38.8 years and a work experience average of 10.6 years.
* TKA = total knee arthroplasty; THA = total hip arthroplasty
**LOS = Length of Stay
The hospital patient journey
In the patient hospital journeys studied, seven main phases and forty-four consequent steps were traced by shadowing patients and interviewing the main actors. Table 3 shows which steps were identified from the interviews and which from the shadowing. In particular, the patient shadowing enabled more accurate reconstruction of all the steps, compared to what patients narrated after a period of time. This information can be obtained from the health professionals' interviews only by summarizing their different points of view. Furthermore, through shadowing it was possible to detect that within the hospital the patient went through eighteen different places and was in contact with more than fifty different health professionals. The patients’ emotions as reported by the health professionals corresponded to what was observed by shadowing, but they did not match the general state of serenity reported by patients when interviewed.
The three different standpoints, (i.e.: patient shadowing, healthcare professional interviews and patient interviews) allowed different issues to be captured at the various phases of the journey. In particular, the shadowing was able to capture the 'connections' between one stage and another of the journey, such as movement from admissions to the ward and transport from the ward to the operating theatre, while the journey narrated by each professional and patient allowed the most significant touchpoints to be identified ( Table 3 ).
When interviewed about a month after discharge, patients remembered a generally positive experience, linked specifically to the success of surgery and to a good relationship with the professionals. They showed appreciation and satisfaction and they declared that there were no major problems to deal with. One patient reported "I was fine , look , I have to say the night of the surgery I was fine , the next day they also made me get up . They made me sit in the chair , my head was spinning a little , so it's not that ehm … then nothing else , everything else went well” (Patient 1); Another reported “What can I say ? Better than that I don't think it is; that… we may be worse , but I have not found that I was worse , and I have only good things to say about the professor and all his assistants” (Patient 3).
However, when shadowed, some discrepancies emerged. When going independently to the ward patients experienced confusion and anxiety, due to not having clearly understood indications, and to the waiting times before entering the assigned ward (Patient 5, 6, 7, 8, 9,12). Another critical step was the transfer and waiting in the operating theatre. They felt 'lost' when they were transferred and emotions of fear and anxiety emerged (Patient 10; 11). These experiences also emerged from the interviews with professionals (Healthcare professional 4, 6, 8, 12, 14 16).
Some other interesting points, detected by the shadowing, reveal how the hospital environment and management of patient flow can affect the patient experience, in particular on the day of admission. After the administrative acceptance, one patient took the wrong elevator and did not immediately reach the indicated ward. When arriving at the entrance of the ward, he found it difficult to use the intercom. When entering the ward, he was dissatisfied with the lack of staff to welcome him. When waiting in the room for surgery he showed apprehension and he reported a desire to have more information and to have a family member nearby (Patient 9). Another patient reported having received incorrect information to reach the ward and that the hospital directional signs were too small and difficult to read (Patient 1).
During the journey it is possible to identify some key steps, though with different levels of importance from patients’ and professionals’ perspectives. From the patient perspective and by shadowing the journey, the day of hospitalization was the most critical, and they experienced mainly negative emotions (Patient 5, 6, 7, 8, 9,12). From the interviews with the professionals it emerges that when returning to the ward after surgery patients were calm (Healthcare professional 7, 8, 16) but in the following days, they began to experience a lack of autonomy and this could make them nervous (Healthcare professional 13). Professionals involved in the pre-hospitalization phase report that waiting in the days before hospital admission can negatively affect patient experience. Patients can feel abandoned, if no one gives them information on the outcome of the outpatient clinic examination, or if all the procedures related to hospitalization are not properly programmed (Healthcare professional 1, 9).
Through analysis of the data collected four main themes emerged underlying both the shadowing and the interviews: the information gap; the covering patient-professionals relationship; the effectiveness of family closeness; and the micro-integration of hospital services.
The most significant issues are reported below.
The information gap
When interviewed, patients did not mention any problems with the information received in the course of their hospital journey. However, when patients were shadowed on arrival at the hospital, they did not seem to be aware of any information regarding their hospitalization (e.g. visiting hours for family members, the hospital route to the ward), but asked the first professionals they met. The patients seemed lost, especially after going through the admission process and on looking for their assigned wards. Moreover, when they arrived in the ward they needed information about their hospitalization, but healthcare professionals did not immediately assist them (Patient 5, 6, 9). This seemed to contribute to their state of anxiety about the surgery. This issue is confirmed by what the professionals reported. When they arrive at the hospital, patients put the same questions to any professional they come into contact with (Healthcare professional 4, 6). A nurse reports how each patient has "so many anxieties , fears , uncertainties , questions , as soon as he steps into the ward and I follow him , until he leaves the ward" (Healthcare professional 1). A head nurse reports "Family members also ask many questions . Many times it seems that what was already explained by the doctor , actually , has not sunk in ( … ) And so here they repeat the same questions many times , in different ways . What worries them a lot ( … ) is what will happen after discharge , when ‘I find him at home or in a rehabilitation clinic’” (Healthcare professional 13). Apprehension before surgery was observed in one patient, even though the patient claimed to have received very good information on how the surgery would be performed (Patient 2).
The time of waiting while the patient is in the operating theatre seems endless for family members, and waiting without information is a cause of anxiety (Healthcare professional 6). Professionals recognize the importance of informing the patient and family members about procedures, clinical pathways and pain management, before surgery (Healthcare professional 1, 2, 4, 7).
The covering patient-professionals relationship
The relationship between patient and professionals is a key issue for the quality of the service perceived by the patient, even when the health care provider fails to respond immediately to the patient's needs. Indeed, as many as 35 touchpoints occur throughout the patient journey ( Table 3 ). What the patient thinks and feels on this topic, emerges especially from the interviews, while the shadowing is not able to immediately capture thoughts or observations re-elaborated by the patient. In particular, when interviewed the patients remember, even after some time, some aspects of the relationship with professionals that are not directly related to clinical care, but which are perceived as being of value for the patients, since in these they receive attention as an individual. Even after some time, a patient remembered: “Early in the morning the nurse came to say goodbye before she went off duty , because I was being discharged later that day , so she wouldn't see me again . Really good . ” (Patient 3). A patient also remembered a rough response to a request for help to get dressed after the X-ray during outpatient clinic examination (Patient 2). Moreover, a patient pointed out how reassuring the relationship with the surgeon could be just before the surgery (Patient 3). One of the key moments appears to be the contact with the anaesthesiologist and the surgeon while the patient is waiting in the operating theatre: “Then the anaesthesiologist told me ‘Don’t worry , my dear , we do the epidural , we will sedate you’” (Patient 1). From the professionals’ perspective, the relationship with the patient is a key point to "buffer" a series of disruptions in the hospital journey and to reassure the patient: “ Patients always thank us because even if there is a gap in the organization and the patient has to wait a little , we apologize in the best way , with a smile" (Healthcare professional 3). As the nurse is the first person patients encounter when entering the ward, she knows she has the important role of reassuring patients by explaining to them how to orientate themselves in the ward and which procedures will be carried out, even if patients should already have been informed about all these things (Healthcare professional 4). Professionals recognize the importance of calming patients through interaction with the surgeon especially when they are waiting just before surgery (Healthcare professional 3, 13). An orthopaedist reports, “When you check or welcome the patient in the operating surgery where the surgeon and the anaesthesiologist are , the patient sees them and this helps him or her a lot , and so one thing that I think is in our favour ( … ) is communication , the possibility of having a point of reference” (Healthcare professional 3).
The effectiveness of family closeness
Family closeness is felt to be important for both patients and professionals, if programmed at the right times of the clinical journey. From the patient interviews and from shadowing it emerges that patients like family members to stay with them when waiting for surgery (Patient 4, 9). Once the surgery has been performed, when fears are diminished and pain is controlled, patients do not consider the presence of family members necessary, in particular immediately after returning to the ward from the operating theatre (Patient 1, 4). From the shadowing it emerges that after the first few days, when patients have recovered from the post-operative stage and close assistance has diminished, they then like to be with their family without interruptions for clinical-assistance reasons (Patient 10).
For professionals, family presence is important especially shortly before and after surgery, to reassure family members that the patient is doing well (Healthcare professional 5, 7, 13). When possible, professionals try to facilitate this, even outside regular visiting hours (Healthcare professional 13). In the days after surgery, “It is mainly relatives who come from outside the city who logically stay here , maybe in a hotel or some bed & breakfast , and would like to stay in the room all day; because they say–quite rightly , as I realize– : ‘But I have nothing else to do; my husband , my wife , my son is there . I'm with him’” (Healthcare professional 12). At this stage of the clinical journey, professionals do not see the closeness of family members as a need of the patient. Immediately after surgery, patients prefer to rest rather than having many people in their room. Conversely, the presence and closeness of family can greatly affect the patient experience in the rehabilitation period, especially when it comes to discharging elderly patients (Healthcare professional 15).
The micro-integration of hospital services
Even for a relatively simple routine surgical pathway, patients go through multiple stages. The behind-the-scenes coordination remains invisible to them and they are able to capture only some of the effects related to it. By contrast, professionals emphasize many critical issues in the management of the patient journey that affect the patient's experience.
When interviewed, patients reported the difficulty of having to move from one clinic to another during the outpatient clinic examination (Patient 1). Before hospital admission, an admissions office administrator shows how necessary it is to “decrease calls to the patient ( …), also depending on their age which is on average quite advanced …. cut out some calls that often from their point of view are unconnected . For instance , on one day I call you for admission , then the doctor calls you for blood tests , then another doctor calls you to arrange the meeting ( …), then if you take cardioaspirin the doctor calls you to give you information on cardioaspirin … All these calls could be grouped into maybe one by the doctor and one by the administrative staff” (Healthcare professional 10). At the time of hospital admission some critical points are revealed by the shadowing. After arriving at the hospital, patients waited an average of 21 minutes before being taken in charge by the Administrative Office to carry out admission procedures. At the end of the administrative registration procedures, patients made their own way to the ward, taking an average of 11 minutes. In this time, patients could get lost; they experienced anxiety about not getting to the right place, and waited outside the closed door of the ward without knowing what to do (Patient 5, 6, 7, 9). During their hospitalization, patients reported a lack of communication: a drug intolerance reported in their previous admissions had not been recorded in the notes. Orthopaedists reported critical issues concerning the management of operating theatres, such as delays in transporting patients from the ward to the operating theatre or delays in preparing the operating theatre for the next operation (Healthcare professional 2, 3). The accumulation of such delays could lead to the cancellation of the last scheduled patient, with a negative impact on the patient who had been waiting in a state of anxiety for many hours (Healthcare professional 2). A head nurse reported that waiting for transport to and from the radiology department for the post-operative radiography could slow down all the care processes, make the patient wait unnecessarily, and increase the pain, due to the temporary suspension of the continuous-infusion pain-killer (Healthcare professional 12). Finally, a patient reported that she was offered no choice when she was transferred to the rehabilitation unit recommended by the doctors, and she expressed the desire for a follow-up visit by the same doctor who had operated on her (Patient 1).
Exploring the individual patient journey can lead healthcare organizations to improve patient experience by focusing on the patient perspective, rather than the provider perspective [ 39 ]. Understanding what organizations can do to improve patient experience is critical [ 40 ]. However, the literature is still exploring the best methods to capture the patient's experience [ 17 , 23 , 30 ]. This study deals with the lived experience of orthopaedic patients by capturing the different points of view of patients and professionals on individual hospital patient journeys. Patients’ reported experience is analysed by shadowing them during hospitalization and by interviewing them at the end of the whole journey.
Historically, researchers and health care managers have focused on the study of how to achieve effective care through the definition of clinical pathways and by increasing patient adherence to treatment. However, reducing the patient's path to the clinical perspective may fail to reveal aspects that are relevant to patients, that influence their experience and their perception of quality of service [ 42 , 42 ]. In this study on patients’ hospital journeys, some important issues emerged through the shadowing of the hospital journey of the patients, and interviews with the key players. With the integrated use of these methods it was possible to identify which touchpoints are most critical for the patient, when family closeness is most effective, and how professionals can provide for the needs shown by patients over the entire journey. If on one hand the study of clinical pathways is now heading towards the active involvement of patients in decisions related to their own health issues [ 43 ], on the other hand the analysis of the hospital journey from a patient perspective can lead organizations to improve cross-hospital processes by creating procedures and focusing healthcare professionals on overall patient experience.
In line with Liberati's analysis [ 30 ], the shadowing method can contribute to patient-centredness by considering all the aspects of service delivery, not just the clinical one. In this study, both interviews and shadowing are able to “see the world from someone else’s point of view” [ 24 ]. However, the patient’s observations, focused on the whole service experienced, can reveal areas of potential improvement of the patient experience not otherwise identifiable. Shadowing highlights what the patient experiences in the different contexts and when going through one service and on to another, which professionals do not see since this falls outside the scope of their direct responsibility. Moreover, unlike using diaries completed by patients [ 23 ], this methodology allows the patient to be observed in the moment and in the spaces in which the relationship with the professionals takes place. However, this necessarily determines a subjective interpretation of what the researcher observes with respect to what the patient affirms.
Unlike what was pointed out by Gill [ 44 ], when dealing with the patient journey perspective, shadowing has an important potential for revealing invisible steps and spaces of the journey, more than intimate spaces and micro-processes of the decision. It is true that even now, in the healthcare sector, the provider establishes the patient path, while the patient is 'carried forward' through processes designed and managed by others.
In this study, when interviewed after time, patients focused on the overall clinical experience, forgetting other issues related to their hospitalization. For example, when interviewed, patients reported that they had had all the information they needed, while when shadowed shortly before the surgery the same patients appeared lost and asked for information from all the professionals they met. These data are also confirmed by interviews with professionals, who reported how highly emotional touchpoints, such as telling the patient they needed an operation, or the time immediately before transfer to the operating theatre, may affect patients’ perceptions and the effectiveness of the information [ 41 , 45 ]. As suggested by Ziebland, there is a difference between what patients said they experienced and what they actually experienced in real-life settings [ 20 ]. In this sense, the use of shadowing helps to understand the experience in a real time context. Moreover, it is always useful to evaluate whether the tools and information methods used for giving information to patients are effective, and which is the best moment for each patient to receive all the information they need, by considering their ability to absorb the information in a stressful situation [ 46 – 48 ].
In this study, both patients and professionals recognized the value of a personalized relationship in improving patient experience. Moreover, professionals report how a good relationship with the patient can compensate for the organization's inefficiencies. Interaction with the patient is especially important in the perceived patient-critical touchpoints. However, relevant steps of the journey are different from patients’ and from professionals’ points of view. From the patient’s point of view, the most critical steps occur when entering the hospital and just before surgery, where their emotional involvement is greater. On the other hand, from the professionals’ point of view, planning hospitalization and preparing patients for surgery is one of the most critical steps that affect patient experience. Indeed, patients, when interviewed, seem not to perceive critical issues in what happens ‘behind the scenes’, while professionals are able to identify issues related to the organization that can positively or negatively affect patients’ experience. These results highlight how frontline professionals are the key players in transforming organizational procedures into personalized care pathways, but the misalignment of views should be considered when improving the hospital journey by including the patients’ perspective.
The study has important limitations with respect to the sample and the setting considered and therefore its potential for generalization may be limited. The issues that emerged would need to be studied in depth in different care settings and with other types of patients to allow comparison of data and methodologies.
Patients’ experiences have become increasingly central to assess the performance of healthcare organizations and to redesign the services around the real needs of patients [ 20 , 41 , 42 , 45 , 49 ]. In this study, the analysis of the hospital journey from the patient perspective and the integration of three different standpoints, patient shadowing, healthcare professional interviews and patient interviews, highlights important areas of improvement otherwise hidden by the analysis of the clinical pathway only.
The nature of the study and its originality by subject matter and methods adopted can stimulate both academics and healthcare managers to explore important new fields. On the one hand, it is important to further investigate methodologies for capturing the patient experience and use it deeply and effectively at various organizational levels. In this way, shadowing seems to give a more patient-centric perspective, but it raises questions about its effectiveness as a single methodology for gathering the whole patient experience within a complex hospital process. On the other hand, the results of this study are a starting-point for healthcare managers who want to improve a key cross-functional hospital process in which the patient is the main actor. By considering the overall patient experience, as well as services performance and clinical pathways, they will able to create a distinctive value both for the patient and for the organization.
Acknowledgments
We are grateful to Eugenia Di Sabatino and Michela Ceri for their contribution to data collection.
Funding Statement
The author(s) received no specific funding for this work.
Data Availability
- PLoS One. 2019; 14(12): e0224899.
Decision Letter 0
30 Aug 2019
PONE-D-19-19443
Exploring the hospital patient journey: how can we capture the patient’s experience?
Dear Dr. Gualandi ,
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
==============================
Please address reviewer comments as well as the following:
Literature review - further detail on the theoretical basis of shadowing and rationale for it's use.
Data collection - was there any prior relationship between the researcher and potential participants? How were issues of possible coercion dealt with?
Please provide further information on shadowing and how the field notes were dealt with
Much greater detail is required in reference to Plutchik's Wheel of Emotions and the rationale for its use as a framework in this study.
Line 146 include "with participant permission"
Please include some minimal demographic characteristics of participants.
Please provide a better link between the text and Table 2
The data presented seems to come from the interviews - where is the data from the shadowing included?
We would appreciate receiving your revised manuscript by 30 September 2019. When you are ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter.
To enhance the reproducibility of your results, we recommend that if applicable you deposit your laboratory protocols in protocols.io, where a protocol can be assigned its own identifier (DOI) such that it can be cited independently in the future. For instructions see: http://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols
Please include the following items when submitting your revised manuscript:
- A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). This letter should be uploaded as separate file and labeled 'Response to Reviewers'.
- A marked-up copy of your manuscript that highlights changes made to the original version. This file should be uploaded as separate file and labeled 'Revised Manuscript with Track Changes'.
- An unmarked version of your revised paper without tracked changes. This file should be uploaded as separate file and labeled 'Manuscript'.
Please note while forming your response, if your article is accepted, you may have the opportunity to make the peer review history publicly available. The record will include editor decision letters (with reviews) and your responses to reviewer comments. If eligible, we will contact you to opt in or out.
We look forward to receiving your revised manuscript.
Kind regards,
Rosemary Frey
Academic Editor
Journal Requirements:
1. When submitting your revision, we need you to address these additional requirements.
Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
http://www.journals.plos.org/plosone/s/file?id=wjVg/PLOSOne_formatting_sample_main_body.pdf and http://www.journals.plos.org/plosone/s/file?id=ba62/PLOSOne_formatting_sample_title_authors_affiliations.pdf
2. Please include captions for your Supporting Information files at the end of your manuscript, and update any in-text citations to match accordingly. Please see our Supporting Information guidelines for more information: http://journals.plos.org/plosone/s/supporting-information .
3. Please consider including more information on the number of interviewers, their training and characteristics.
4. Thank you for stating the following financial disclosure:
NO - The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript
a) Please provide an amended Funding Statement that declares *all* the funding or sources of support received during this specific study (whether external or internal to your organization) as detailed online in our guide for authors at http://journals.plos.org/plosone/s/submit-now .
b) Please state what role the funders took in the study. If any authors received a salary from any of your funders, please state which authors and which funder. If the funders had no role, please state: "The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript."
Please include your amended statements within your cover letter; we will change the online submission form on your behalf.
[Note: HTML markup is below. Please do not edit.]
Reviewers' comments:
Reviewer's Responses to Questions
Comments to the Author
1. Is the manuscript technically sound, and do the data support the conclusions?
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Reviewer #1: Partly
Reviewer #2: Yes
2. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #1: N/A
3. Have the authors made all data underlying the findings in their manuscript fully available?
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
Reviewer #1: Yes
Reviewer #2: No
4. Is the manuscript presented in an intelligible fashion and written in standard English?
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
Reviewer #1: No
5. Review Comments to the Author
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #1: Title: Exploring the hospital patient journal: how can we capture the patient’s experience?
Manuscript number: PONE D 19 19443
General comments
Your title is Exploring the patient journey: how can we capture the patient experience?
And the research questions are Which aspects of hospital patient journey experience may be captured by 3 different standpoints – shadowing, professional and patient interviews. What does the patient experience through the hospital journey and how can it be captured?
The complexity and number of steps in the patient journey decoded by your research is very interesting as were other findings of patient journey. I commend you for using an ethnographic approach to try to capture the lived experiences of the patients your followed.
These tools captured patient journey, the physical aspects of movement through a hospital experience; however, I am interested to know other aspects of patient experience. For example, did the hospital context/system facilitate patient understanding of their own condition and care (health literacy)? Could that be a lens you view the data gleaned from shadowing?
Shadowing as a research methodology also requires more analysis in the paper. I don’t get a sense of the ‘rich’ description that the ethnographic shadowing approach should generate. It would be good to see what else that data revealed beside the annotation of components of the hospital journey, given you were trying to capture the broader experience of patients – viz Line 328 - patient mainly feels and remembers, while shadowing highlights what the patient experiences in the different contexts and going through one service and on to another, which professionals do not see since this falls outside the scope of their direct responsibility.
See also Gill, R. (2011). The shadow in organizational ethnography: moving beyond shadowing to spect -acting. Qualitative Research in Organizations and Management: An International Journal, 6(2), 115-133
Line 15 – delete “the’ – definite article.
Line 26 – “professionals” – a possessive?
Line 32 – comma after process
Line 43 – vague reference to “some others”
Line 87 – reference for phenomenological-hermeneutic approach
Line 90 – unless that is the name of the hospital, only ‘Italian’ should have capitalisation; however, your use of the indefinite article makes me think it is not a proper noun.
Use of appendix – perhaps not needed – the table could be condensed and summarised inside a table in the text or using words.
Lines 119-122 This is unclear - we need some researcher reflexivity here – what were the researchers’ roles in the delivery of patient care?
Line 136 – patient’s journey/experience or patients’ journeys/experiences?
Line 140 – can you explain more about sampling decisions for professional staff, esp the nurses
Line 157 – Plutchik’s Wheels of Emotion needs some backgrounding – why is that appropriate and how did it fit with your phenomenological-hermeneutic approach and your research question? Table 2 reveals that patient emotions were captured, but was there any particular part of the 3 different standpoints which captured emotion?
Line 180 – rules of long quotes – over 40 words – indented? Italics?
Line 195 - “they began to experience a lack of autonomy and this could make them nervous (N2)” – Could you clarify what the coding stands for in your results? E.g. N or P or H? Also does one reference (N2) here mean only one person had this experience?
Line 210 – verb aspect – going/gone – delete ‘having’
Lines 233 on – was this data gained from the interviews or shadowing?
? hegemonic/power relationships in that context? Any critical analysis?
Line 227 – The relationship between Table 2 and patient-professional relationships could be clarified further.
Line 373/4 – where was the review of the shadowing methodology challenges?
Reviewer #2: Overall this is an interesting, well written study. The topic of the patient experience is important and new ways of capturing it, and using this information to improve patient care, are central to modern healthcare. Specific points follow.
Page 2, line 15: “hospital patient journey experience” is an ugly noun cluster, please unpack – “the experience of the hospital patient journey”?
Page 4, line 64 and in discussion: you talk a lot about different data collection methods and perspectives on the patient experience and mention a number of them – three complementary forms of which your study covers. However, one rather obvious method and perspective that you fail to mention is a hospital-stay diary completed by the patient themselves. This should at least be mentioned in discussion as another such method. A recent good example of this method is: Webster CS, Jowsey T, Lu LM, et al. Capturing the experience of the hospital-stay journey from admission to discharge using diaries completed by patients in their own words: a qualitative study. BMJ Open 2019;9:e027258. doi:10.1136/bmjopen-2018-027258
Page 4, line 70: “what he/she experiences IN real-time…”
Page 4, line 72: “accurate and real data on the experience” – what does “real data” mean in this context? Who’s definition of real are you using? Better to use a different word here I think.
Page 5, line 92: Line starting “Scheduled surgical patients were…” – this sentence doesn’t make much sense to me.
Page 6, line 108: Sentence starting “Inclusion criteria were scheduled…” – this sentence doesn’t make much sense either. I am unsure how inclusion criteria get scheduled or performed? Do you mean the inclusion criteria were that patients must be scheduled for their procedure for the shadowing phase and must have had the procedure performed for the interviews?
Page 6, line 113: “consent to participation in the study” – should be consent to participate…
Page 7, line 137: “Professionals ranged…” Please make it clear that you are talking about healthcare professionals throughout – there are other kinds of professionals.
Page 8, line 154: In my understanding content analysis and thematic analysis are not the same things – yet here you appear to suggest that they are? It looks more to me that you did a thematic analysis.
Page 8, line 160 (table 1): I am unconvinced that the unit of meaning is a good one to support the significance of the text, or the theme. “I didn’t understand anything”, to me does not demonstrate calming of the patient, or covering professional relationships – I am sure the patient would be much calmer if they did understand what was going on, and this is the anaesthetist’s professional obligation.
Page 9, line 173: “each actor allowed…” who is the actor here? The patients, clinician or researcher?
Page 9, line 186 and elsewhere: I can guess that P1 means patient one (but please define), but what does PJ1, H1 etc mean? Please define on first use of each numbering scheme.
Page 10, line 219: If patients ask the same questions over and over why does the hospital not supply them with a simple written information pack with frequently asked questions (FAQs)?
Page 12, table 2: What is the significance of the filled dots vs the unfilled dots? Please explain or make consistent.
Page 13, 241: we see the same quote as from Table 1 in the text here, why? Why not use another? Also it also seems odd to me that the anaesthetist would not address the patient by her name, rather than calling her “lady”, which actually seems rather rude.
Page 15, line 277: “simple ordinary surgical pathway…” Ordinary in this context sounds strange, do you mean routine?
Page 15, line 296: “had not been passed on.” – or recorded in the notes?
Page 17, line 324: “…perceptions and effectiveness of the information” – surely it is more about the patient’s ability to absorb the information in a stressful situation rather than the effectiveness of the information itself?
Page 18, line 359: “does not allow any generalization of results” – I would say that generalisation maybe limited rather than entirely ruled out. For example, your findings are substantially similar to those in the BMJ Open paper I mentioned previously using the patient diary method.
6. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
If you choose “no”, your identity will remain anonymous but your review may still be made public.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy .
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files to be viewed.]
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email us at gro.solp@serugif . Please note that Supporting Information files do not need this step.
Author response to Decision Letter 0
AUTHORS’ RESPONSES TO REFEREES’ AND EDITOR’S COMMENTS
• Literature review - further detail on the theoretical basis of shadowing and rationale for it's use.
We have included more details in the introduction to explain the theoretical basis of shadowing and the rational for its use.
• Methods
Data collection - was there any prior relationship between the researcher and potential participants? How were issues of possible coercion dealt with?
We have added this information in the first paragraph: “There were no prior relationships between researchers and patients; while two researchers knew some healthcare professionals because they worked in the same hospital, though in different units and without patient care roles. The possibility of coercion was minimized by guaranteeing data anonymity, by requesting voluntary participation in the study and by dealing with issues on which the researchers had no power to influence anything or anyone at hospital managerial level.”
Please provide further information on shadowing and how the field notes were dealt with.
We have provided further information on shadowing by explaining in more detail how we collected data.
We have added more details on Plutchik's Model and to its use in our study, in the ‘Data Collection’ section.
• Results
We have included the main demographic characteristics by summarizing them in a paragraph at the beginning of the ‘Results’ section and we have transferred the table from the Appendix to the main manuscript, naming it Table 2.
We have renamed Table 2 as Table 3 and we have added some data in the 'The hospital patient journey' Section to better link the text to the results shown in the table. In this way, data deriving from shadowing are better represented.
The manuscript has been significantly revised in light of your suggestions in order to make its validity clearer.
In accordance with the qualitative nature of the study, all data are now included as part of the main manuscript.
We have had external proof reading of the manuscript carried out by a native English translator.
• Your title is Exploring the patient journey: how can we capture the patient experience?
We have rewritten the title so that it is more consistent with the research questions. The new title is “Exploring the hospital patient journey: what does the patient experience ?”
• The complexity and number of steps in the patient journey decoded by your research is very interesting as were other findings of patient journey. I commend you for using an ethnographic approach to try to capture the lived experiences of the patients your followed. These tools captured patient journey, the physical aspects of movement through a hospital experience; however, I am interested to know other aspects of patient experience. For example, did the hospital context/system facilitate patient understanding of their own condition and care (health literacy)? Could that be a lens you view the data gleaned from shadowing? Shadowing as a research methodology also requires more analysis in the paper. I don’t get a sense of the ‘rich’ description that the ethnographic shadowing approach should generate. It would be good to see what else that data revealed beside the annotation of components of the hospital journey, given you were trying to capture the broader experience of patients – viz Line 328 - patient mainly feels and remembers, while shadowing highlights what the patient experiences in the different contexts and going through one service and on to another, which professionals do not see since this falls outside the scope of their direct responsibility.
We have revised the whole paper in order to give greater value to shadowing and to describe the results obtained from this methodology. At the same time, we have tried to maintain the paper's goal of comparing different methodologies rather than focusing on the effectiveness of shadowing.
Specifically, we added the following points:
- as requested in the previous comments, in the ‘Result’ Section we have better distinguished the data coming from the shadowing from those from the interviews;
- we have included a paragraph in the "The information gap" Section with data collected from the hospital context and their impact on the patient's experience;
- we have included in the “Hospital patient journey” Section further data on what was observed by shadowing patients;
- we have included in the discussion considerations on the potential and limits of shadowing methodology when applied to the patient journey.
• Line 15 – delete “the’ – definite article.
• Line 26 – “professionals” – a possessive?
• Line 32 – comma after process
• Line 43 – vague reference to “some others”
• Line 87 – reference for phenomenological-hermeneutic approach
• Line 90 – unless that is the name of the hospital, only ‘Italian’ should have capitalisation; however, your use of the indefinite article makes me think it is not a proper noun.
• Use of appendix – perhaps not needed – the table could be condensed and summarised inside a table in the text or using words.
We have inserted the table in the main manuscript and we have named it “Table 2”.
• Lines 119-122 This is unclear - we need some researcher reflexivity here – what were the researchers’ roles in the delivery of patient care?
As requested by the editor, we have specified the relationship between researchers and participants in the Methods section. We also have specified in the ‘Data collection’ section that students had no role in patient delivery of care. Moreover, in the discussion we have considered the subjective interpretation of the researcher in the shadowing methodology.
• Line 136 – patient’s journey/experience or patients’ journeys/experiences?
• Line 140 – can you explain more about sampling decisions for professional staff, esp the nurses
We have specified the sampling technique. We introduced further specification in the text.
• Line 157 – Plutchik’s Wheels of Emotion needs some backgrounding – why is that appropriate and how did it fit with your phenomenological-hermeneutic approach and your research question? Table 2 reveals that patient emotions were captured, but was there any particular part of the 3 different standpoints which captured emotion?
As requested by the editor, we have added in the ‘Data Collection’ section more details in reference to Plutchik's Model and the rationale for its use in our study. In the 'The hospital patient journey' Section we have specified that the identified emotions coincide with what was detected by the shadowing and by the interviews with healthcare professionals, but they are different from what the patient reported during the interviews. In the table, renamed table 3, we have specified the column label.
• Line 180 – rules of long quotes – over 40 words – indented? Italics?
We shortened and distinguished the two quotes. We put all quotes into italics.
• Line 195 - “they began to experience a lack of autonomy and this could make them nervous (N2)” – Could you clarify what the coding stands for in your results? E.g. N or P or H? Also does one reference (N2) here mean only one person had this experience?
We have made the subject of each quotation explicit. We codified the number alone by connecting quotes with Table 2 (Subject / Number).
• Line 210 – verb aspect – going/gone – delete ‘having’
• Lines 233 on – was this data gained from the interviews or shadowing?
We revised the paragraph to better define the concept and to specify the source of the data.
• Line 227 – The relationship between Table 2 and patient-professional relationships could be clarified further.
Within the first paragraph of the "The covering patient-professionals relationship" Section, we created a link with the touchpoints represented in the renamed Table 3.
• Line 373/4 – where was the review of the shadowing methodology challenges?
We changed the statement to achieve greater consistency with the results achieved by this study.
• Page 2, line 15: “hospital patient journey experience” is an ugly noun cluster, please unpack – “the experience of the hospital patient journey”?
• Page 4, line 64 and in discussion: you talk a lot about different data collection methods and perspectives on the patient experience and mention a number of them – three complementary forms of which your study covers. However, one rather obvious method and perspective that you fail to mention is a hospital-stay diary completed by the patient themselves. This should at least be mentioned in discussion as another such method. A recent good example of this method is: Webster CS, Jowsey T, Lu LM, et al. Capturing the experience of the hospital-stay journey from admission to discharge using diaries completed by patients in their own words: a qualitative study. BMJ Open 2019;9:e027258. doi:10.1136/bmjopen-2018-027258
We have carefully considered the suggested study and we have updated our analysis by commenting on it in the introduction and citing it in the discussion.
• Page 4, line 70: “what he/she experiences IN real-time…”
• Page 4, line 72: “accurate and real data on the experience” – what does “real data” mean in this context? Who’s definition of real are you using? Better to use a different word here I think.
• Page 5, line 92: Line starting “Scheduled surgical patients were…” – this sentence doesn’t make much sense to me.
We reframed the sentence.
• Page 6, line 108: Sentence starting “Inclusion criteria were scheduled…” – this sentence doesn’t make much sense either. I am unsure how inclusion criteria get scheduled or performed? Do you mean the inclusion criteria were that patients must be scheduled for their procedure for the shadowing phase and must have had the procedure performed for the interviews?
We have clarified the inclusion criteria in the text.
• Page 6, line 113: “consent to participation in the study” – should be consent to participate…
• Page 7, line 137: “Professionals ranged…” Please make it clear that you are talking about healthcare professionals throughout – there are other kinds of professionals.
• Page 8, line 154: In my understanding content analysis and thematic analysis are not the same things – yet here you appear to suggest that they are? It looks more to me that you did a thematic analysis.
Amended. We conducted a thematic analysis.
• Page 8, line 160 (table 1): I am unconvinced that the unit of meaning is a good one to support the significance of the text, or the theme. “I didn’t understand anything”, to me does not demonstrate calming of the patient, or covering professional relationships – I am sure the patient would be much calmer if they did understand what was going on, and this is the anaesthetist’s professional obligation.
The literal translation of the text from Italian may have misrepresented the meaning of what we wanted to report. We have changed the example to report a clearer quotation.
• Page 9, line 173: “each actor allowed…” who is the actor here? The patients, clinician or researcher?
We have specified.
• Page 9, line 186 and elsewhere: I can guess that P1 means patient one (but please define), but what does PJ1, H1 etc mean? Please define on first use of each numbering scheme.
• Page 10, line 219: If patients ask the same questions over and over why does the hospital not supply them with a simple written information pack with frequently asked questions (FAQs)?
Even though it does not emerge from the interviews, the hospital already uses written information material. In our work we want to emphasize that, regardless of the patient's tools and information methods, it is always useful to evaluate whether these are effective and which is the best moment for the patient to receive all the information they need. We made this concept explicit in the discussion.
• Page 12, table 2: What is the significance of the filled dots vs the unfilled dots? Please explain or make consistent.
• Page 13, 241: we see the same quote as from Table 1 in the text here, why? Why not use another? Also it also seems odd to me that the anaesthetist would not address the patient by her name, rather than calling her “lady”, which actually seems rather rude.
We changed the quote in the Table 1. We have replaced the word “lady” with “my dear” to better convey the note of kindness that is meant in the Italian language “Signora”.
• Page 15, line 277: “simple ordinary surgical pathway…” Ordinary in this context sounds strange, do you mean routine?
• Page 15, line 296: “had not been passed on.” – or recorded in the notes?
• Page 17, line 324: “…perceptions and effectiveness of the information” – surely it is more about the patient’s ability to absorb the information in a stressful situation rather than the effectiveness of the information itself?
We have specified in the lines below.
• Page 18, line 359: “does not allow any generalization of results” – I would say that generalisation may be limited rather than entirely ruled out. For example, your findings are substantially similar to those in the BMJ Open paper I mentioned previously using the patient diary method.
Submitted filename: Response to Reviewers.docx
Decision Letter 1
24 Oct 2019
Exploring the hospital patient journey: what does the patient experience?
PONE-D-19-19443R1
Dear Dr. Gualandi,
We are pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it complies with all outstanding technical requirements.
Within one week, you will receive an e-mail containing information on the amendments required prior to publication. When all required modifications have been addressed, you will receive a formal acceptance letter and your manuscript will proceed to our production department and be scheduled for publication.
Shortly after the formal acceptance letter is sent, an invoice for payment will follow. To ensure an efficient production and billing process, please log into Editorial Manager at https://www.editorialmanager.com/pone/ , click the "Update My Information" link at the top of the page, and update your user information. If you have any billing related questions, please contact our Author Billing department directly at gro.solp@gnillibrohtua .
If your institution or institutions have a press office, please notify them about your upcoming paper to enable them to help maximize its impact. If they will be preparing press materials for this manuscript, you must inform our press team as soon as possible and no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact gro.solp@sserpeno .
With kind regards,
Additional Editor Comments (optional):
1. If the authors have adequately addressed your comments raised in a previous round of review and you feel that this manuscript is now acceptable for publication, you may indicate that here to bypass the “Comments to the Author” section, enter your conflict of interest statement in the “Confidential to Editor” section, and submit your "Accept" recommendation.
Reviewer #1: All comments have been addressed
Reviewer #2: All comments have been addressed
2. Is the manuscript technically sound, and do the data support the conclusions?
3. Has the statistical analysis been performed appropriately and rigorously?
4. Have the authors made all data underlying the findings in their manuscript fully available?
5. Is the manuscript presented in an intelligible fashion and written in standard English?
6. Review Comments to the Author
Reviewer #1: 1. Check for use of Tab instead of Table (see Lines 197 & 281)
2. Sentence (Line 397) doesn’t makes sense to me. Perhaps “In contrast to Gill (I’m still not sure though what the contrast is.)
Unlike what was pointed out by Gill [44], when dealing with the 397 patient journey perspective,
398 shadowing has an important potential for revealing invisible steps and spaces of the journey, more
399 than intimate spaces and micro-processes of the decision.
Reviewer #2: This is an excellent paper, and the authors have carefully addressed my review points.
My only very small remaining suggestion would be to use the Italian "signora" instead of "my dear" - the English translation doesn't really capture the original meaning, and signora is a well known term in English which seems more appropriate in the context of the quote.
7. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
Acceptance letter
18 Nov 2019
Dear Dr. Gualandi:
I am pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
If your institution or institutions have a press office, please notify them about your upcoming paper at this point, to enable them to help maximize its impact. If they will be preparing press materials for this manuscript, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact gro.solp@sserpeno .
For any other questions or concerns, please email gro.solp@enosolp .
Thank you for submitting your work to PLOS ONE.
PLOS ONE Editorial Office Staff
on behalf of
Dr. Rosemary Frey
Patient journey 101: Definition, benefits, and strategies
Last updated
22 August 2023
Reviewed by
Melissa Udekwu, BSN., RN., LNC
Today’s patients are highly informed and empowered. They know they have choices in their healthcare, which can put healthcare providers under a lot of pressure to provide solutions and meet their patients’ expectations.
Just like any customer, patients embark on a journey that begins before they ever contact the provider. This makes understanding the journey and where improvements can be made extremely important. Mapping the patient journey can help practitioners provide better care, retain a solid customer base, and ultimately identify ways to improve patient health.
- What is the patient journey?
The patient journey is best described as the sequence of experiences a patient has from admission to discharge. This includes all the touchpoints between the patient and provider from beginning to end.
The patient journey continues through consultation, where they meet the potential caregiver. That portion of the journey includes interactions with a doctor and support staff, how long they wait to be seen, and the steps taken for diagnosis and treatment.
The patient’s post-care journey includes follow-ups from the healthcare provider, post-treatment care, and billing. For example, if the patient has questions about post-surgery care or how to read their invoice, how quickly their questions are answered and their problems resolved will impact their satisfaction.
Mapping the patient journey helps healthcare providers improve patient satisfaction at every step of the way. By collecting data at each stage and conducting an in-depth analysis, providers can identify patient concerns and make the necessary improvements to meet their patient satisfaction goals.
What is another name for the patient journey?
The term “patient funnel” describes the journey patients take from first learning about a healthcare provider or healthcare product to actually making an appointment or purchase. This “funnel” can be applied to any type of business, describing the stages a customer goes through to obtain a service.
- Understanding the stages of the patient journey
Each stage of the patient journey is essential to a positive patient experience . Gathering and analyzing data can alert healthcare providers to potential issues throughout the journey.
Data collection at each of the following stages will give healthcare providers the information they need to make the necessary improvements:
1. Awareness
Awareness is where the patient journey begins. This is when they first research symptoms and identify the need to see a medical professional.
They may consider at-home remedies and get advice from friends, social media, or websites. Once they identify the need for a healthcare provider, they continue their research via review sites, advertising campaigns, and seeking referrals from friends and family.
Determining the way patients become aware they need healthcare and the sources they use for research is important. The data collected at this stage could suggest your organization has an insufficient social media presence, inadequate advertising, or a website in need of an update.
To remedy these shortcomings, you might consider adding informational blogs to your website, performing a social media analysis, or closely monitoring customer reviews.
This stage in the patient journey is where the patient schedules services with the healthcare provider.
This engagement is essential for acquiring new patients and retaining current patients. Patients will contact you in several ways to schedule an appointment or get information. Most will call on the first attempt to schedule an appointment.
This is a crucial touchpoint in the journey. A new patient may become frustrated and move on if they find it difficult to access your services or are placed on hold for a long period or transferred numerous times.
Patient engagement occurs in other ways, such as your online patient portal, text messages, and emails. Your patients may interact differently, so it’s important to gather data that represents their preferred means of communication. Work to make the improvements required to correct access issues and ensure efficient communication.
The care stage can include everything from your patient’s interaction with the front desk to how long they have to wait in the examination room to see a doctor.
Check-in, check-out, admissions, discharge, billing, and of course, the actual visit with the healthcare provider are other touchpoints in the care stage.
There are a couple of ways to gather and analyze this data. Most organizations choose to analyze it holistically, even if it’s collected separately. For example, you might gather data about the patient’s interaction with the front desk, the clinical visit, and the discharge process, but you may want to analyze the care segment as a whole.
4. Treatment
Treatment may be administered in the office. For example, a patient diagnosed with hypertension may have medication prescribed. That medication is the treatment. Gathering information at this stage is critical to see how your patient views the healthcare provider’s follow-up or responses to inquiries.
In most cases, treatment extends beyond the initial clinical visit. For example, a patient might require additional tests to get a diagnosis. Providing the next steps to a patient in a timely manner and letting them know the test results is crucial to patient satisfaction .
5. Long term
A satisfied patient results in a long-term relationship and referrals to friends and family. Most of the data collected at this stage will be positive since the patient is continuing to use your services.
Gathering data after the treatment stage allows you to expand on the qualities that keep patients returning for your services in the long term.
- Benefits of patient journey mapping
The patient benefits from their healthcare provider understanding their journey and taking steps to improve it. Healthcare providers also reap several benefits, including the following:
1. Efficient patient care
When they understand the patient journey, healthcare providers can provide care more efficiently and spend less time and money on unnecessary, unwanted communications.
2. Proactive patient care
Proactive patient care is aimed at preventing rather than treating disease. For example, women who are over a certain age should have an annual mammogram, smokers may be tested for lung disease, and elderly women may need a bone density study. These preventative measures can help keep disease at bay, improve health outcomes, and build trust with patients.
3. Value-based patient care
Patients don’t want to feel they are being charged unfairly for their healthcare. Focusing on the individual patient promotes satisfaction and yields positive outcomes.
The Center for Medicare and Medicaid Services (CMS) has issued recent guidelines for participants that help offset the costs of high-quality care through a reward system.
4. Retention and referrals
Patients who are happy with their journey will keep returning for healthcare, and happy patients equal voluntary referrals. Many providers offer rewards to incentify referrals.
- How to get started with patient journey mapping
Follow the steps below to start the patient journey mapping process:
Establish your patient personas
Journey mapping is a great way to identify your patient’s characteristics so that their experience can be further enhanced.
Some of the following determinations can help you pinpoint your patient’s persona and establish protocols to provide a better service:
How do your patients prefer to communicate? Are they more comfortable with phone calls, texts, or other methods?
How are most patients finding your services? Are they being referred by friends or family members, or are they seeing advertisements?
Would the patient prefer in-person communication or telecommunication?
What are the patient’s expectations of care?
This data can be complex and widespread, but it can give you the information you need to more effectively and efficiently communicate with your patients.
Understand the entire patient lifecycle
Each patient is unique. Understanding the patient lifecycle can avoid confusion and miscommunication.
To positively engage the patient, you’ll need to gather data not only about communication methods but where they are in the patient journey, their health issue, and their familiarity with the healthcare provider’s procedures and treatment options.
Understand the moments of truth
With a few exceptions, most people seek healthcare services when they are ill or have a healthcare issue. These situations can cause patients to feel stressed and anxious. It’s these moments of interaction where compassion, knowledge, and understanding can provide relief and reassurance.
When patients see their healthcare provider, they are looking for solutions to problems. It’s the provider’s opportunity to identify these moments of truth and capitalize on them.
Get the data you need
Healthcare providers can collect vast amounts of data from patients, but the data collected rarely goes far enough in analyzing and determining solutions.
Your patients have high expectations regarding personalized treatment based on data. They want personalized, easy access to medical information and records, responsive treatments and follow-up, and communication in their preferred format.
You need more than clinical data to give patients what they want. You also need personal data that sets each patient apart and ensures a tailored experience.
For example, it might be challenging for parents of small children to contact the clinic and schedule appointments at certain times of the day. As a healthcare provider, you’ll need to be aware of the best times to contact this individual and offer simple methods for scheduling appointments.
Another example is patients with physical disabilities. You can take steps to improve their access to and experience at the healthcare facility.
Encourage referrals and loyalty
Although engagement on social media and online forums is becoming more and more common, the best way for new patients to find you is through referrals. Referrals stem from satisfactory experiences and trust.
Get started today
Go from raw data to valuable insights with a flexible research platform
Editor’s picks
Last updated: 27 June 2023
Last updated: 22 July 2023
Last updated: 11 September 2023
Last updated: 10 October 2023
Last updated: 16 November 2023
Last updated: 28 September 2023
Last updated: 12 October 2023
Last updated: 25 November 2023
Last updated: 3 July 2023
Last updated: 27 January 2024
Latest articles
Related topics, log in or sign up.
Get started for free
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 04 December 2019
“Patient Journeys”: improving care by patient involvement
- Matt Bolz-Johnson 1 ,
- Jelena Meek 2 &
- Nicoline Hoogerbrugge 2
European Journal of Human Genetics volume 28 , pages 141–143 ( 2020 ) Cite this article
24k Accesses
18 Citations
25 Altmetric
Metrics details
- Cancer genetics
- Cancer screening
- Cancer therapy
- Health policy
“I will not be ashamed to say ‘ I don’t know’ , nor will I fail to call in my colleagues…”. For centuries this quotation from the Hippocratic oath, has been taken by medical doctors. But what if there are no other healthcare professionals to call in, and the person with the most experience of the disease is sitting right in front of you: ‘ your patient ’.
This scenario is uncomfortably common for patients living with a rare disease when seeking out health care. They are fraught by many hurdles along their health care pathway. From diagnosis to treatment and follow-up, their healthcare pathway is defined by a fog of uncertainties, lack of effective treatments and a multitude of dead-ends. This is the prevailing situation for many because for rare diseases expertise is limited and knowledge is scarce. Currently different initiatives to involve patients in developing clinical guidelines have been taken [ 1 ], however there is no common method that successfully integrates their experience and needs of living with a rare disease into development of healthcare services.
Even though listening to the expertise of a single patient is valuable and important, this will not resolve the uncertainties most rare disease patients are currently facing. To improve care for rare diseases we must draw on all the available knowledge, both from professional experts and patients, in order to improve care for every single patient in the world.
Patient experience and satisfaction have been demonstrated to be the single most important aspect in assessing the quality of healthcare [ 2 ], and has even been shown to be a predictor of survival rates [ 3 ]. Studies have evidenced that patient involvement in the design, evaluation and designation of healthcare services, improves the relevance and quality of the services, as well as improves their ability to meet patient needs [ 4 , 5 , 6 ]. Essentially, to be able to involve patients, the hurdles in communication and initial preconceptions between medical doctors and their patients need to be resolved [ 7 ].
To tackle the current hurdles in complex or rare diseases, European Reference Networks (ERN) have been implemented since March 2017. The goal of these networks is to connect experts across Europe, harnessing their collective experience and expertise, facilitating the knowledge to travel instead of the patient. ERN GENTURIS is the Network leading on genetic tumour risk syndromes (genturis), which are inherited disorders which strongly predispose to the development of tumours [ 8 ]. They share similar challenges: delay in diagnosis, lack of cancer prevention for patients and healthy relatives, and therapeutic. To overcome the hurdles every patient faces, ERN GENTURIS ( www.genturis.eu ) has developed an innovative visual approach for patient input into the Network, to share their expertise and experience: “Patient Journeys” (Fig. 1 ).
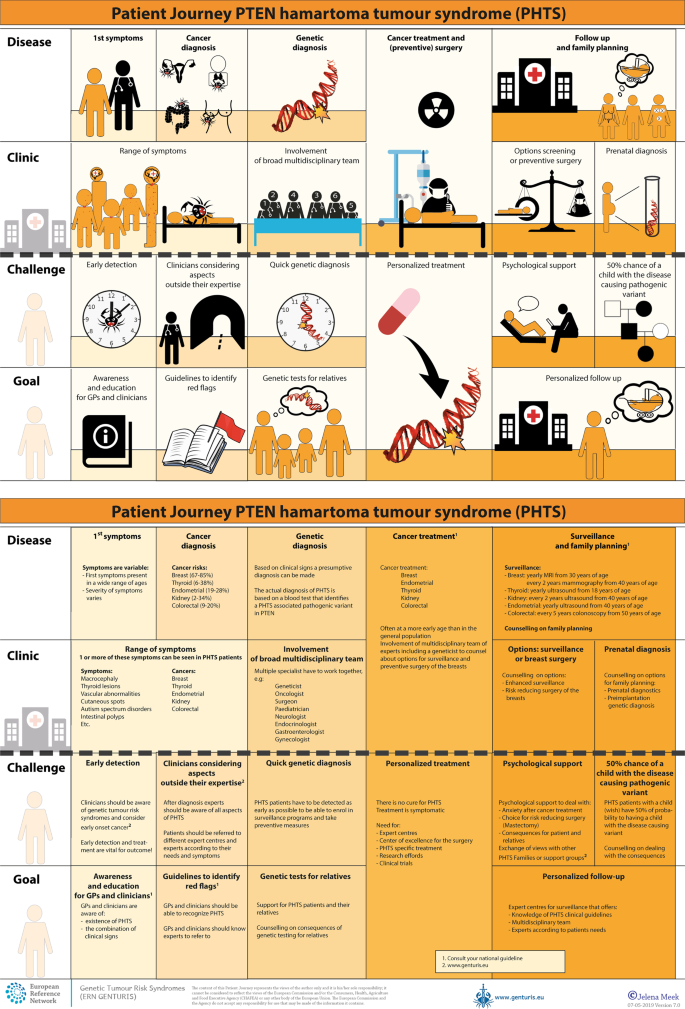
Example of a Patient Journey: PTEN Hamartoma Tumour Syndrome (also called Cowden Syndrome), including legend page ( www.genturis.eu )
The “Patient Journey” seeks to identify the needs that are common for all ‘ genturis syndromes ’, and those that are specific to individual syndromes. To achieve this, patient representatives completed a mapping exercise of the needs of each rare inherited syndrome they represent, across the different stages of the Patient Journey. The “Patient Journey” connects professional expert guidelines—with foreseen medical interventions, screening, treatment—with patient needs –both medical and psychological. Each “Patient Journey” is divided in several stages that are considered inherent to the specific disease. Each stage in the journey is referenced under three levels: clinical presentation, challenges and needs identified by patients, and their goal to improve care. The final Patient Journey is reviewed by both patients and professional experts. By visualizing this in a comprehensive manner, patients and their caregivers are able to discuss the individual needs of the patient, while keeping in mind the expertise of both professional and patient leads. Together they seek to achieve the same goal: improving care for every patient with a genetic tumour risk syndrome.
The Patient Journeys encourage experts to look into national guidelines. In addition, they identify a great need for evidence-based European guidelines, facilitating equal care to all rare patients. ERN GENTURIS has already developed Patient Journeys for the following rare diseases ( www.genturis.eu ):
PTEN hamartoma tumour syndrome (PHTS) (Fig. 1 )
Hereditary breast and ovarian cancer (HBOC)
Lynch syndrome
Neurofibromatosis Type 1
Neurofibromatosis Type 2
Schwannomatosis
A “Patient Journey” is a personal testimony that reflects the needs of patients in two key reference documents—an accessible visual overview, supported by a detailed information matrix. The journey shows in a comprehensive way the goals that are recognized by both patients and clinical experts. Therefore, it can be used by both these parties to explain the clinical pathway: professional experts can explain to newly identified patients how the clinical pathway generally looks like, whereas their patients can identify their specific needs within these pathways. Moreover, the Patient Journeys could serve as a guide for patients who may want to write, in collaboration with local clinicians, diaries of their journeys. Subsequently, these clinical diaries can be discussed with the clinician and patient representatives. Professionals coming across medical obstacles during the patient journey can contact professional experts in the ERN GENTURIS, while patients can contact the expert patient representatives from this ERN ( www.genturis.eu ). Finally, the “Patient Journeys” will be valuable in sharing knowledge with the clinical community as a whole.
Our aim is that medical doctors confronted with rare diseases, by using Patient Journeys, can also rely on the knowledge of the much broader community of expert professionals and expert patients.
Armstrong MJ, Mullins CD, Gronseth GS, Gagliardi AR. Recommendations for patient engagement in guideline development panels: a qualitative focus group study of guideline-naive patients. PloS ONE 2017;12:e0174329.
Article PubMed PubMed Central Google Scholar
Gupta D, Rodeghier M, Lis CG. Patient satisfaction with service quality as a predictor of survival outcomes in breast cancer. Supportive Care Cancer Off J Multinatl Assoc Supportive Care Cancer. 2014;22:129–34.
Google Scholar
Gupta D, Lis CG, Rodeghier M. Can patient experience with service quality predict survival in colorectal cancer? J Healthc Qual Off Publ Natl Assoc Healthc Qual. 2013;35:37–43.
Sharma AE, Knox M, Mleczko VL, Olayiwola JN. The impact of patient advisors on healthcare outcomes: a systematic review. BMC Health Serv Res. 2017;17:693.
Fonhus MS, Dalsbo TK, Johansen M, Fretheim A, Skirbekk H, Flottorp SA. Patient-mediated interventions to improve professional practice. Cochrane Database Syst Rev. 2018;9:Cd012472.
PubMed Google Scholar
Cornman DH, White CM. AHRQ methods for effective health care. Discerning the perception and impact of patients involved in evidence-based practice center key informant interviews. Rockville, MD: Agency for Healthcare Research and Quality (US); 2017.
Chalmers JD, Timothy A, Polverino E, Almagro M, Ruddy T, Powell P, et al. Patient participation in ERS guidelines and research projects: the EMBARC experience. Breathe (Sheff, Engl). 2017;13:194–207.
Article Google Scholar
Vos JR, Giepmans L, Rohl C, Geverink N, Hoogerbrugge N. Boosting care and knowledge about hereditary cancer: european reference network on genetic tumour risk syndromes. Fam Cancer 2019;18:281–4.
Article PubMed Google Scholar
Download references
Acknowledgements
This work is generated within the European Reference Network on Genetic Tumour Risk Syndromes – FPA No. 739547. The authors thank all ERN GENTURIS Members and patient representatives for their work on the Patient Journeys (see www.genturis.eu ).
Author information
Authors and affiliations.
SquareRootThinking and EURORDIS – Rare Diseases Europe, Paris, France
Matt Bolz-Johnson
Human Genetics, Radboud University Medical Center, Nijmegen, The Netherlands
Jelena Meek & Nicoline Hoogerbrugge
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Nicoline Hoogerbrugge .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Bolz-Johnson, M., Meek, J. & Hoogerbrugge, N. “Patient Journeys”: improving care by patient involvement. Eur J Hum Genet 28 , 141–143 (2020). https://doi.org/10.1038/s41431-019-0555-6
Download citation
Received : 07 August 2019
Revised : 04 October 2019
Accepted : 01 November 2019
Published : 04 December 2019
Issue Date : February 2020
DOI : https://doi.org/10.1038/s41431-019-0555-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Care trajectories of surgically treated patients with a prolactinoma: why did they opt for surgery.
- Victoria R. van Trigt
- Ingrid M. Zandbergen
- Nienke R. Biermasz
Pituitary (2023)
Designing rare disease care pathways in the Republic of Ireland: a co-operative model
- E. P. Treacy
Orphanet Journal of Rare Diseases (2022)
Rare disease education in Europe and beyond: time to act
- Birute Tumiene
- Harm Peters
- Gareth Baynam
Development of a patient journey map for people living with cervical dystonia
- Monika Benson
- Alberto Albanese
- Holm Graessner
Der klinische Versorgungspfad zur multiprofessionellen Versorgung seltener Erkrankungen in der Pädiatrie – Ergebnisse aus dem Projekt TRANSLATE-NAMSE
- Daniela Choukair
- Min Ae Lee-Kirsch
- Peter Burgard
Monatsschrift Kinderheilkunde (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

- Sales CRM Software
- Application Portals
- Call Center CRM
- Mobile CRM App
- Omnichannel Communication CONVERSE
- Reporting Dashboard SIERA
- Lead Management System
- Opportunity Management
- Sales Process Automation
- Sales Tracking
- Door-to-Door Sales
- Remote Team Management
- Field Sales CRM
- Merchant Onboarding App
- App UI/UX Customizer CASA
- Outside Sales CRM
- Field Force Automation
- Collections Management
- Field Force Tracking
- Event Campaign Management
- Bancassurance Management
- Marketing Automation
- Chatbot - Website
- Chatbot - WhatsApp
- Landing Pages
- Email Campaigns
- Lead Capture Automation
- Lead Engagement
- BTL Marketing Automation
- Advanced Marketing Analytics
- Hospitals and Clinics
- Hospice and Palliative Care
- Fertility Clinics
- Dental Care
- Diagnostics Labs
- ACQUISITION
- Patient Intake Automation
- Patient Appointment Scheduling
- Healthcare Call Center Solution
- Patient Experience Management
- Self-serve Patient Portals
- EHR Integration
- Physician Empanelment
- Security and Compliance
- Patient Engagement
- Higher Education
- Pre-schools and K12
- Training Institutions
- Overseas Education
- Student Recruitment Software
- Admission Portal
- Teacher Onboarding
- Publisher Portal
- Admission Software
- Credit Unions
- Securities and Trading
- Lending CRM
- Loan Origination System
- WhatsApp Lending Bot
- Debt Recovery Automation
- Bancassurance Solution
- PAPERLESS ONBOARDING
- e-KYC Solution
- Video KYC Solution
- Merchant Onboarding
- Merchant Lifecycle Management
- Travel and Hospitality
- Agriculture
- Home Improvement
- View by Industries
- [Download Free Template] How to create a patient journey map

Patient journey mapping is a process that helps you—as healthcare providers—to visualize the complete experience of your patients who seek and use your care services.
This includes every single touchpoint (whether online or offline) that a patient encounters in the process of finding a care provider, scheduling an appointment, to having the consultation, and even post-care interactions.
A good understanding of a patient journey map, and all the pitfalls that the patient can encounter while seeking care, can help you pre-emptively improve your operations to deliver a delightful and consistent patient experience .
In this article, we’ll dive deeper into various aspects of patient journey mapping, stages of a patient journey, how to create a patient journey map and the benefits you can realize by using the right tools.
If you’d rather jump to the steps to create a patient journey map, you can do that as well. Go to:
What is patient journey mapping?
Patient journey mapping is the process of visualizing the connection between various interactions and touchpoints patients have during their relationship with a healthcare practice.
Mapping healthcare journeys helps providers understand:
- What is the patient going through?
- What are the patient’s primary concerns?
- Is the patient able to cope with their diagnosis?
- Is information regarding the patient’s diagnosis easily accessible?
- Is the patient able to reach you to book a consultation easily?
- Is the patient satisfied with the care they’re receiving?
With this knowledge, providers can spot inconsistencies, find operational bottlenecks, and devise strategies to improve them.
Healthcare providers need to be obsessed with patient journey. The journey begins way before a patient visits the healthcare facility to interact with the provider, and it ends a lot after their treatment. A good patient journey map integrates various virtual and physical touchpoints. Uzodinma Umeh, Chief Medical Officer, Zuri Health
Before we get into the steps to create a journey map, let’s look at the stages a patient goes through before any consultation.
5 crucial stages of a patient journey
The 5 stages common in most of the patient journeys are:
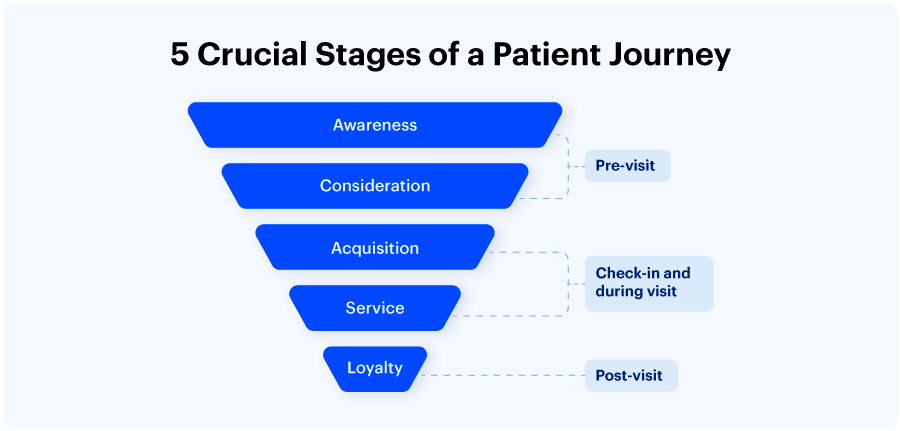
1. Awareness
The patient recognizes a need for care at this point and starts looking for providers.
The patient evaluates their symptoms, does research, thinks about potential medical issues that might need treatment, and may even interact with message boards.
It begins the moment when the patient experiences a symptom. Most of the time, they go online to find a treatment or a solution to their pain. Healthcare providers need to use this opportunity to position themselves virtually by offering a solution, allowing them to research treatments, and book appointments with ease. Uzodinma Umeh, Chief Medical Officer, Zuri Health
Online searches, review websites, advertising initiatives, networking, and friends/family referrals are a few examples of how patients find out about healthcare services.
However, patients may face certain challenges at this stage. Such as:
- Lack of information about their condition
- Inability to find a provider nearby who they think could help
- Feelings of fear and anxiety regarding their concerns
The key to reaching patients at this stage lies in your online presence. You can help your patients by:
- Publishing posts about the treatments you provide
- Publishing educational blogs posts on your website about the conditions and how to manage them
- Getting yourself listed on GoogleMyBusiness
It goes without saying, you should monitor the results of your efforts by using website analytics tools and collect patient feedback through surveys .
Baptist Health South Florida has nailed this stage by introducing an online triage tool on their website. It asks patients a series of questions around their symptoms and accordingly directs them to e-visit, ER, urgent care, or physician’s office.
2. Consideration
The patient analyzes their options to see if your healthcare facility can satisfy their needs. Referrals, coverage and perks, suggestions, accessibility, and ratings and reviews are all things that patients take into account during this stage.
When it comes to healthcare reviews and recommendations, 83% of patients trust their friends and family, while 62% trust reviews online from people they haven’t even met. This is exactly why healthcare businesses need to collect feedback and reviews physically and virtually to bring in patients from referrals. Chantelle Fraser, Vice President – Africa Sales, LeadSquared
Patients frequently interact with your website and social media accounts and call or email you. Additionally, if you are hard to get in touch with, they will go on to the next applicant.
At this point, you can find out more about your potential patient, specifically about their preferred method of communication, and make sure you provide it. For instance, if a patient prefers communicating via email, you should reach them on this platform.
Tools you can use to better connect with patients at this stage are:
- Email marketing solutions that help automate emails that reach the right person at the right time,
- Tools that help you segment visitors and create targeted ad campaigns,
- Chatbots help you reach patients with concerns in real time and get a deeper understanding of their concerns.
3. Acquisition
Direct patient contact with your organization is the first indicator of the acquisition stage.
As part of the booking and new patient acquisition process, you will interact with patients via phone calls, the user portal, texts, and emails.
The patient generally arranges a meeting and visits a doctor or takes a telehealth consultation for a preliminary checkup.
Common challenges patients face at this stage are:
- Lack of access to appointment booking portals and websites
- Inability to reach providers at odd hours (e.g., 2 AM in the morning)
- No-shows because of no reminder communications
- Lengthy wait times at hospitals
- Extensive paperwork before consultation
At this point, providers can use software to improve communications with patients. Such as:
- Appointment scheduling solutions that help providers and patients find convenient timings for consultations.
- Email automation tools that send notifications to patients before appointments to reduce the chance of no-shows.
- Patient intake tools help them fill out forms and answer pertinent questions before they visit the facility.
4. Service
The stage of service delivery has to do with the medical care you administer to your patients. The medical consultation itself, check-in and check-out, registration and discharge, and payment are all components of this step.
The type of service you provide will determine the patient’s satisfaction from your practice.
Common challenges providers face at this stage are:
- Difficulty locating comprehensive patient information across different touchpoints at the facility.
- Administering the necessary treatment and meeting patient expectations.
- In cases where the patient opts for home care, the inability to monitor and track their progress poses a significant challenge to the treatment process.
The bulk of patient issues is rarely solved in the medical office. The patient’s experience persists into the treatment phase after assessment and any related procedures. They might receive an in-patient or out-patient plan or receive medicine and get discharged.
At this point, you want to go beyond just calling to see how the patient is doing with their medicine and use the knowledge you have collected about them to deliver personalized care.
Tools that can help providers at this stage are:
- Billing and payment software that enables the speedy processing of invoices and collection of money through the patient or insurer.
- A tool that unifies patient data and offers visual reports on a healthcare dashboard that is easy to use and accurate in its data collection and analysis.
- A communication tool that allows patients to contact their healthcare provider whenever necessary and update their status as it changes.
- Feedback collection tools like patient satisfaction surveys and questionnaires to gather information and testimonials for future use.
5. Loyalty (on-going care)
The best way to retain and nurture patients over time is to carry out post-visit follow-ups and keep track of their recovery.
The patient journey also includes post-operation and post-visit care for your patients. You can use technology to take care of your patients by sending visit reminders, notify them of when their next vaccination is due, schedule house calls and much more. Collecting feedback and implementing it on a macro-level is another important post-visit step. Uzodinma Umeh, Chief Medical Officer, Zuri Health
Most healthcare providers often overlook this phase of the patient’s journey. Regardless of whether a patient’s treatment goes well or not, it is still necessary for the provider to follow up with them thereafter.
Challenges hospitals face at this stage are:
- Difficulty keeping in touch with patients as they recover or face issues during the aftercare process
- Measuring patient satisfaction and their response to the treatment
- Offering the necessary information to speed up recovery and keep patients aware of different reactions they may have when receiving care
Providers must keep an eye on the patient’s aftercare and monitor their interactions with them. This phase is crucial because it guarantees the patient’s long-term welfare and lowers the likelihood of readmission.
Tools that can help at this stage are:
- Tools that track and monitor the patient’s progress, like a healthcare smartwatch or diagnosis tools
- CRMs that help send notifications to patients to update them on recurring appointments and consultations
Note that these stages may differ from one patient to another. This is why it is vital to create patient journey maps to understand gaps in your service and meet patient needs.
How to create a patient journey map
Journey maps are mainly of the following four types:
- Current state : Useful for illustrating what your patients do, think, and feel as they interact with your practice with your present system.
- Future state : Useful for illustrating your patient experiences with your practice in the future (usually goes well with your plans to implement a new system/technology).
- Day in the life : This journey map illustrates what your patients do, think, and feel with or without your product or service.
- Service blueprint : It is generally a roadmap with action items and support processes.
Creating all four types of journey maps may not be required for your practice, especially when your goal is to understand your current standing. In the following section, we’ll learn how to create a patient journey map using the current state journey map.
Create a patient journey map in 7 simple steps
FullStory has come up with a simple and easy-to-remember technique for creating journey maps. It includes 7 D’s, which are as follows:
- Define: business goals
- Describe: personas or customer attributes
- Determine: touchpoints
- Design: the journey (lay out the steps a customer takes while buying a product/service from your brand)
- Designate: tag milestones, motivations, frustrations
- Decide: Flag events that need action
- Deploy: people, process, and technology to act upon 6
We’ll apply this technique with some modifications to create journey maps for the healthcare sector.
Step 1: Define your goals
Why do you want to create a journey map?
You might be facing certain challenges for which mapping a patient journey seems like a good starting point. For example,
- To reduce no-shows
- To increase retention
- To increase patients from referral sources
- To increase intake, and so on.
Answering the “ why ” part will give you clarity on the purpose of creating a patient journey map and help you sketch the journey in a definitive direction.
Step 2: Define your patient attributes
You must be getting leads from your outreach, marketing, or referral programs. You’ll need to know whether you’re attracting the right patients to whom you can serve.
Mapping patient attributes with the services you provide will help you tune your marketing, outreach, and referral programs. Lay out every single bit of information you have about your patients. Such as:
- Demographic info : location, age, gender, ethnicity, education, employment, etc.
- Engagement : appointment history, communication channels, feedback/satisfaction score, etc.
- Health goals : challenges, conditions, treatment history, barriers to getting care, etc.
Create an ideal patient profile based on the information you have about your patients. You can also use your CRM data to gain insights into how they came to know about you, their interactions with your facility, and more.

Explore LeadSquared’s Healthcare CRM
Purpose-built to increase patient intake, engagement, and retention.
Note: Create separate journey maps for each patient profile you create. It will help you analyze patient experiences more deeply.
Step 3: Determine touchpoints
Touchpoints are the ways in which patients interact with your practice. They can be online like scheduling apps, websites, ads, etc., or offline interactions like phone calls, OPD walk-ins, etc.
Some of the common touchpoints in the healthcare patient journey are:
- Appointment scheduling : WhatsApp, text messaging, phone calls, patient portals, mhealth platforms, provider’s healthcare apps, etc.
- Pre-check-in : appointment confirmations and reminders on email, WhatsApp, app notifications, text messages, phone calls
- Check-in and during care : intake process (digital or physical), video consultation, telehealth, insurance verification, etc.
- Post-visit : diagnosis notes, follow-up consultation scheduling, reminders, feedback via email, WhatsApp, app notifications, and text messages.
Depending on the nature of your practice the touchpoints will vary. The idea is to note down all the possible sources of interactions with your patients.
Step 4: Design a visual journey
Once you’ve identified the touchpoints, it’s time to create a visual journey that your team can easily understand.
You can plot:
- Journey stages
- Customer interactions and actions
- Your patient’s needs and pains
- Touchpoints
- Their sentiments during those interactions
Concurrently, mark the areas of improvement and who can own them.
Also, keep your ideal patient profile and goal cards side by side to ensure you’re moving in the right direction.
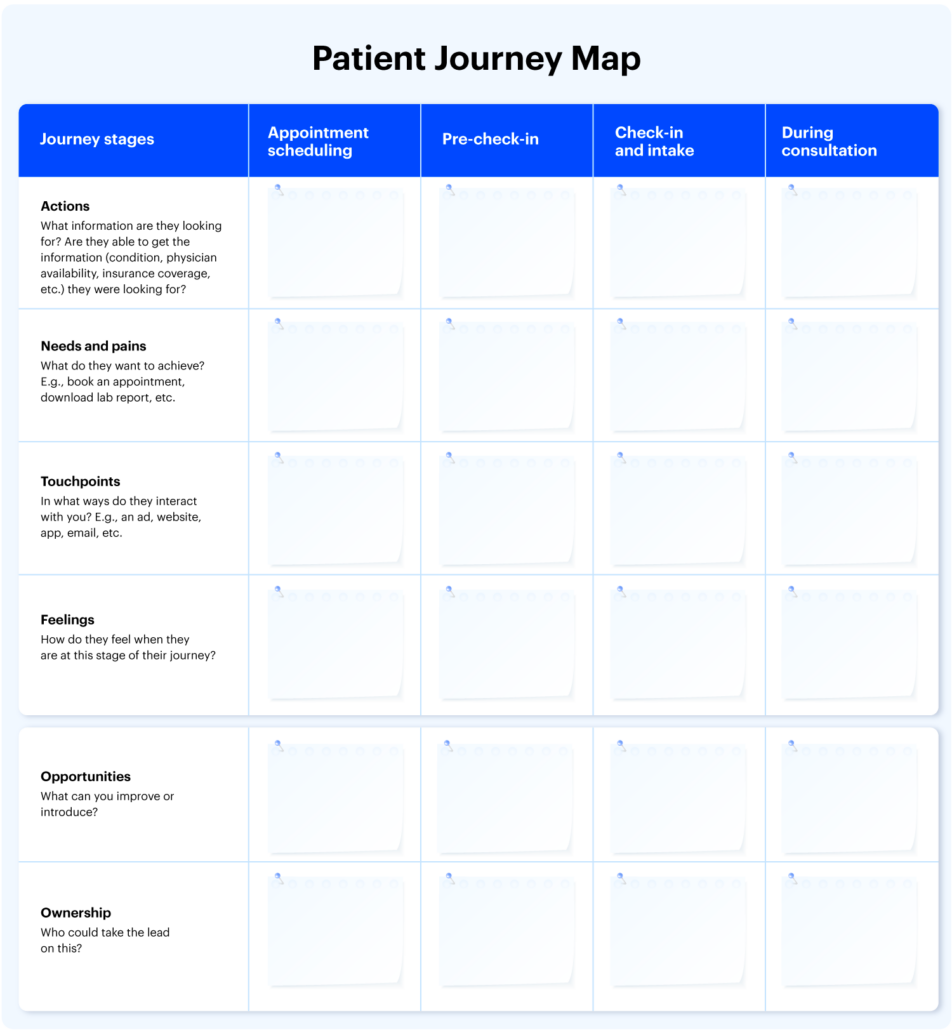
You can bookmark this page or download an editable PDF patient journey mapping template:
Step 5: Designate milestones, motivations, frustrations
This step of a patient journey highlights various kinds of friction a patient may encounter while contacting you for your product/service.
For example, patients may not book an appointment because of one of the following reasons:
- UI issues – If the interface through which they’re trying to schedule a consultation is not working at that time, patients may not be able to book an appointment.
- Cognitive load – If the UI (User Interface) is not intuitive enough or too complex to understand, or the patients find it difficult to navigate to the services they see, they may drop off.
- Emotional friction – What patients are feeling at that moment will determine their action on opting for your services.
This exercise helps the admin understand what to fix and how to fix it.
Step 6: Decide on the actions you need to take
Until step 5, the journey was looked upon through the patient’s lens. Now that there’s better clarity on patient experiences and hesitations, it’s time to look at the back-office tasks that can be improved.
It involves identifying the areas of improvement and how that can be done.
Step 7: Deploy people, process, and technology to achieve your goals
In this final step of creating a patient journey map, you assign roles, delegate tasks, and procure tools to act on the areas of improvement identified.
Best practices to follow while creating a patient journey map
When you’re just starting off, learn the journey mapping fundamentals and research existing journey maps for healthcare.
Here are some helpful resources:
- Neilsen Norman Group’s Journey Mapping 101
- Atlassian’s team playbook on Customer Journey Mapping
- Understanding Patient Journey webinar by LeadSquared
Once you’ve understood the basics, follow these best practices to create a patient journey map.
- Set clear goals . Define what you wish to achieve from your patient journey map.
- Do not mix all the information in one map. Create different journey maps for different patient profiles .
- Involve different stakeholders. Do not restrict it to one team or department for sharing their inputs.
- Keep it simple . You may not need fancy tools or lots of graphics and colors; a simple spreadsheet can do the work.
- Make it an iterative process. You may not have perfect journey mapping from the very first time. Take feedback, act on it, and improve all the way up.
Benefits you can realize by mapping patient journeys correctly
The goal of patient journey mapping is to improve patient experience across all touchpoints and derive better outcomes. In a nutshell,
Investing in patient experience essentially takes away the cost of advertising and acquisition. It also boosts referrals, recommendations, and NPS at the same time. Uzodinma Umeh, Chief Medical Officer, Zuri Health
Here’s the drill-down of benefits you get by mapping patient journeys efficiently.
1. Spot inefficiencies
Every time a patient expresses frustration or uncertainty about her next steps toward recovery, it’s an obvious sign that there are friction spots or unmet gaps in the healthcare system. A patient journey map can effectively battle such challenges and create a clear path for a patient’s progress.
2. Improve communication

By mapping patient journeys providers can understand the drop-offs occurring because of communication gaps and take measures to rectify their strategies.
3. Increase profitability
Net margins for hospitals that provide “excellent” patient care are typically 50% higher than those for hospitals that offer “average” patient care.
With a patient journey map, practitioners can identify the scope of improvement in operations and help their staff focus more on interacting with patients and caregivers.
4. Reduce wait time for patients
The average ER wait time in America is 145 minutes (even higher in some states; e.g., 228 minutes in Maryland, 195 minutes in Delaware, 176 minutes in Arizona, and so on). In India and other countries as well, it may take hours to get emergency admissions . These delays happen due to one or more of the following reasons:
- Examination of patient
- Time taken for consultation
- Emergency investigations or imagining
- Unavailability of vehicles for transport
- Lengthy admission procedures
By knowing what exactly is causing the delays and taking steps to correct them, providers can reduce waiting times for patients to a great extent.
5. Improve patient outcomes
A healthcare journey map can help identify the touchpoints where essential and relevant information can be shared with patients. Educating patients and keeping them abreast of their illnesses can lower their anxiety and bring better outcomes
Tools to create a patient journey map
As a matter of fact, you can use any UI design tool (e.g., Figma , Sketch , FullStory , etc.) to create a journey map.
However, there are dedicated tools to create journey maps with ready-to-use templates to make your work faster and easier. Some of which are:
- Creately
- TheyDo
- Custellence
- Miro
- LeadSquared
On a final note, you’ll be able to map your patient’s journey effectively when you’ve ample information about their interactions with your practice.
Healthcare CRM software is the best tool to collect and manage patient interaction data and make them accessible for various purposes like creating a journey map.
If you’re looking for one such tool,
A patient journey is the series of steps patients take to book an appointment, consult a physician, and pursue treatment with your practice. It involves both online and physical interactions.
Patient journey mapping helps you understand your customers’ experiences while interacting with your practice. With this exercise, you get to know their pain points, identify opportunities for improvement, and take measures to improve your services.

Padma is a Content Writer at Leadsquared. She enjoys reading and writing about various financial and educational topics. You can connect with her on LinkedIn or write to her at [email protected].
Table of Contents
- Share on Facebook
- Share on Twitter
- Share on WhatsApp
- Share on LinkedIn
Want to see LeadSquared in action?
- Customer Portal
- Performance Management
- Dev Platform LAPPS
- Help Portal
- Pricing SALES
- Pricing MARKETING
- Education CRM
- Healthcare CRM
- Insurance CRM
- Banking CRM
- Real Estate
- Marketplace CRM
- Manufacturing CRM
- What is CRM
- What is lead management
- What is vendor management
- What is sales management
- Case Studies
- Guides & Blogs
- Compare CRM
- CRM Glossary
- Sales Glossary
- Media & News
GET IN TOUCH
(+1) 732-385-3546 (US)
080-46971075 (India Sales)
080-46801265 (India Support)
62-87750-350-446 (ID)
- Legal & Compliance

Patient Journey Mapping: What it is and Why it Matters

How can healthcare organizations make every stage of the patient journey better?
How was your last experience in a healthcare facility? Think about every step of that patient care journey - the phone calls, in person meetings, wait times, communication and all of the healthcare professional/ patient interactions. It’s a lot.
Healthcare organizations are working diligently to improve patient satisfaction and quality of care by asking, “How can we make the patient experience better?” But that’s no mean feat, trying to capture the multitude of challenges patients face when navigating a healthcare journey. That makes improving it even more difficult.
A first, fundamental step to improving patient experience is understanding what that experience looks like today. This is where patient journey mapping comes into play. You can use patient journey maps to understand the highs and lows, pain points and gaps to begin pinpointing which interventions will be most impactful. Then you can assess which changes you have the power to make.
As a result, you’ll be better able to manage your patient’s journey, improve care pathways and meet—and exceed—patient expectations, needs, and wants.
What is Patient Journey Mapping?
Patient journey mapping works to identify and understand the details of all patient touchpoints within a specific healthcare experience. It helps you visualize the process patients go through to receive care, complete a treatment plan, and/or reach a desired outcome. When done correctly, patient journey maps make it easier for you to identify pain points, discover opportunities and re-align treatment and care approaches across the entire healthcare system.
What makes up a patient’s journey?
A patient’s journey represents the entire sequence of events or touchpoints that a patient experiences within a given health system, with a specific provider, or within a specific facility. These touchpoints are either virtual or in-person. They range from the mundane to the nerve-wracking or life-changing. They comprise events from scheduling an appointment online to reviewing post-surgery instructions with a doctor.
It’s key for healthcare professionals and clinicians to recognize the patient journey extends well beyond the most obvious in-person interactions at a treatment facility. The patient journey happens before, during and after a healthcare service: pre-visit, during-visit, and post-visit. These include but are not limited to:
- Finding the right service or practitioner
- Scheduling an appointment
- Submitting a list of current medications
- Arriving at the medical facility
- Identifying where to check-in.
These experiences can instil a sense of reassurance or unease before a patient even receives care. In essence, they set the tone and expectations for the physical visit. A frustrating or confusing experience during the pre-visit stage will impact the emotional state of the patient and family for the rest of their interactions.
During-visit
- Checking in at the front desk
- Waiting in the lobby to be called
- Discussion with nurses before speaking to a doctor
- Family waiting for updates in the lobby during a procedure
- Care from doctor and staff.
There are an infinite number of touchpoints during the delivery of healthcare. Each one will have a different level of impact on the patient’s experience.
- Post-care instructions at hospital
- Hospital discharge process
- Completing a patient feedback survey
- Paying for the medical treatment
- Post-surgery calls or online messages from the nurse or doctor.
The patient experience after a hospital visit plays a vital role in either reinforcing a positive experience or mitigating a negative one. Actions such as post-appointment follow-ups extend the care relationship and may help the likelihood of the patient sticking to the treatment plan
All these individual touchpoints are crucial to understand. Altogether, these positive and negative experiences — no matter how big or small — comprise the patient journey.
Who are the stakeholders?
The healthcare ecosystem is complex, involving multiple stakeholders and a wide range of internal and external factors, including:
- People (patients, their families and caregivers, doctors, nurses, administration, parking attendants, volunteers)
- Technology and systems (online registration, parking tickets, surgery updates, mobile app, website, social media)
- Facilities (hospital campus navigation, parking availability, building accessibility).
Investigation of all players and systems involved is essential to seeing the multidimensional layers impacting the experience. To do this, patient journey maps should include the perspectives of patients, providers, and staff - and those perspectives must be of the same journey. Often, an interaction that occurs from one point of view will show only one reality. However, further investigation will show the many contributing factors across the care delivery process. This is only apparent by examining multiple perspectives.
Once you understand the entire journey, with pain points, you’ll be able to identify patterns across patient personas and different demographics, and any gaps within the healthcare process. You can then begin asking important questions like:
- Which moments are most painful?
- Why do they happen?
- What must we change in order to improve the experience?
- Who must we impact?
- Which do we have the power to change?
Benefits of patient journey mapping
Patient journey mapping provides the opportunity to turn the healthcare experience from a primarily reactive experience to a proactive one. By building out care journeys for your patients, you can close any gaps in provision and establish robust preventative routines that ultimately help your patients stay healthier for as long as possible. Engaging consumers and patients based on where they are and what they want, builds trust and confidence. That retains patients in your system and encourages them to make friends and family referrals.
But how does the process work?
- Streamline patient processes and workflows: upgrading the usability and functionality of online patient portals, websites and mobile apps can put more control in the patients’ hands, increasing patient flow and cutting operational expenses.
- Increase staff efficiency : enhancing internal online tools and creating automation within systems can assist hospital staff in implementing protocols and schedules and help them anticipate and solve problems more easily. It can help to align the expected service delivery with the actual one.
- Clear routes and direction across medical facilities: hospitals can be incredibly complicated to navigate - whether it’s using the right entrance, finding parking or making your way to the cafeteria for a snack. Improving signage, making visible pathways, and using landmarks to help orient users can help patients and families readily access the resources they need.
- Improve communication between patients and providers: exchanging patient information and coordinating care can be a challenge for providers and a frustration for patients. This misalignment can be due to silos within organizations, incompatible technology systems or many other factors. Working to bridge the appropriate organizational or technological gap can help alleviate stress and anxiety.
- Develop seamless and timely patient and family updates: waiting while a family member is in surgery or communicating with a doctor to secure care for a child is typically an extremely stressful process. Families wait anxiously for updates which can be infrequent and lacking detail. Implementing a seamless system for families to communicate directly and receive regular updates, through an app or text, can help ease these pain points.
- Better ‘in-between visit’ care and check-ins with patients and families: communication between patients, including families and caregivers and providers can feel ‘hit or miss.’ Patients may be scrambling to answer phone calls or missing phone calls only to find themselves unable to get hold of the provider when they call back. Alternatively, providers are challenged to communicate critical information to a wide range of patients. Establishing better communication systems can improve patient engagement, build the patient’s confidence in the care they receive, and ease the care provider’s job.
In short, we’re talking happier patients who experience better communication and levels of empathy at every stage of the patient journey.
What tools and methods are used for creating a patient journey map in healthcare?
There are many ways to undertake patient journey mapping, but doing it well isn’t always as simple as it may seem. It’s not a single exercise, moving from A to B. It’s more complex, involving a series of tools.
Our team at Highland has helped a lot of our clients create their first journey map . Grab a bunch of sticky notes and pens to start your map. Our process tends to go like this:
- Chart the course -work out what you want to achieve (your goal); determine whose journey you’re mapping, the start and end points; create the persona(s); think about what the stages of the journey may be.
- Prepare to interview - list your potential questions being mindful that you want the interviewee to recount events rather than share opinions. Schedule interviews with a tool like Calendly. Look into other available data (such as patient feedback).
- Interviews and coding - we interview in pairs so that one can speak whilst the other takes notes. With permission, record the interviews. Afterwards, code the responses according to thoughts, actions, experience etc. We use a simple Google Sheet to do this.
- Building blocks - go through the interviews and notes. Start mapping. Use a specific color of sticky note for each Building Block and add points to the wall in their themes.
- Identify opportunities - “mine” the wall for opportunities, presenting ideas to the team. Together, prioritise the top three or four to tackle.
Repeat this whole process with another persona or goal to examine.
Explore this journey mapping process in more detail
The outcome of this process should be that healthcare professionals can look after patients better. Using patient data collection to underpin your decision-making can transform your organization’s culture to one of continuous improvement. By referring constantly to patient data, you can identify the key areas to amend and improve to better the patient experience. Satisfied customers, those who’ve experienced a near seamless patient journey, will rate your facility highly and they’ll be more likely to generate new referrals.
Improve your customer experience with Highland Solutions’ help
You may know your healthcare facility like the back of your hand, but you only know it from your informed perspective. Getting a 360º view of the patient experience is the first step to improving it. A huge challenge for healthcare leaders like you is to recognize, understand and address the fact that the overall experience is created by the cumulative interactions across the various touchpoints in the healthcare journey: pre-visit, during-visit, and post-visit.
Despite years of expertise, it’s easy for healthcare providers and leaders to develop blind spots for persistent issues in the care process. Partnering with a knowledgeable research team to conduct patient journey mapping will bring expertise and a fresh perspective to your quality of care. It’s not only about uncovering in-depth insights via patient journey maps, but also translating them into actionable strategies to help you bridge any gaps between current and emerging patient needs and the present state of your healthcare organization.
Once on the right track, you’ll be enabled to manage and grow relationships at every stage of the patient journey. The more patient-centric you become, the better experience you build, reaching a higher quality of patient care, patient retention and loyalty, and improved health outcomes and overall well-being.
Get in touch to find out more about how we can help you with patient journey mapping
“Working with Highland is a really powerful experience for a company to be able to gain insights. To have real conversations with patients unlocks new pathways, ones that may be uncomfortable and uncover change, but they empower you to move forward in a way that feels really constructive.”
Chris Whitworth, Vice President, Treatment

Download “The Essential Guide to Launching a Digital Product for Experts & Expert Firms”

The Step-by-Step Guide to Patient Journey Mapping
by Gaine Solutions | May 18, 2022 | Healthcare , Life Sciences

Customer journey mapping has been used for years in marketing and customer service. Now healthcare realizes journey mapping’s potential when used in the biotech and life sciences industry. Patient journey mapping offers providers and researchers a complete view of patients and their respective environments, which will help them mitigate risks and achieve more favorable outcomes.
Learn the five steps for patient journey mapping using big data and customer experiences and how it will help you offer patient-centric care.
Key Takeaways:
- Patient journey mapping outlines a patient’s journey from first realizing their health concerns through treatment.
- A patient’s journey map tells providers and researchers where common risks arise and how to influence patients for better outcomes.
- You need to collaborate with health care providers to ensure your patient journey mapping is complete.
- Big data, artificial intelligence, and digital technology make patient journey mapping possible in healthcare.
What is Patient Journey Mapping?
Patient journey mapping is tracking and analyzing your patient’s experiences, touchpoints, and treatment from when they first noticed symptoms or an issue through to their outcome. A patient map includes:
- Medical records
- Medications they took
- Prescriptions they refilled
- Treatment or therapies they underwent
- Lifestyle choices they make (like exercising or diet)
- Doctor or care visits
- Survey results

Image source: Voxco
These pieces help providers create a complete picture of how effective their treatment was or why a patient stopped treatment because they can understand a patient better and any influencing behaviors. In addition, when providers see how each piece plays a part in the patient’s outcome, they can also identify specific areas of concern or risks to avoid.
Why Patient Journey Mapping is Important
Healthcare and life sciences want to deliver top-quality care while minimizing costs and offering a positive experience for patients. However, with scattered patient information or incomplete records, that has been difficult in the past. Additionally, those in biotech and life science have traditionally worked through a healthcare system when delivering care, which puts further distance between them and the patient journey.
That scenario is no longer the case because of new digital technology like artificial intelligence and platforms that can collect and organize big data in healthcare .
Today, patients can access their healthcare information for themselves. This allows them to research their diagnosis and approach providers directly instead of going through their primary care physician or other medical providers.
This technology also helps those in healthcare and life sciences to understand more about patients and deliver better treatment options. As a result, you have a clearer picture of your product’s effectiveness and where you should adjust your treatment options to improve the patient’s experience. The information you gain from patient journey mapping in life sciences and biotech will also help you write educational material because you will have more accurate and specific instructions for patients based on real situations.
Below is a patient journey map example for a pneumonia patient.

Image source: NIH
5 steps to map your patient journey in healthcare and life sciences.
Take these five steps to help you create a patient journey map for healthcare and life sciences.
Video: Pharmaceutical Industry JOURNEY MAPPING in 3 Steps for Patients and HCPs
1. understand your purpose.
You wouldn’t start a journey without knowing your destination, and neither should you create a customer journey map without knowing your purpose for treatment.
One patient can generate nearly 80 megabytes of medical data annually. Without focus, you can easily drown in that amount of information and have a difficult time making relevant and valuable connections. Knowing your end goal will help you focus and organize your data.
2. Connect with Potential Patients
Once you have your goal, you are ready to begin mapping your patient’s journey, which starts with touching base with patients. You can bring patients in through your website, SEO, social media , or your network of providers.
When patients first contact you, you will want to start gathering relevant information that will help with patient mapping, including demographics, finances, and their medical history.
3. Gather Patient Health Data
Collecting data about your patients will many times be an active task. While automation and artificial intelligence can pick up passive information, you will also have to send out surveys and contact the patient to get feedback on their treatment throughout the process.
You will need data from every point along their journey from their first symptoms, consultations, costs, side effects, and influencing factors when a patient chooses to stop treatment. This data is relevant because it can help you find ways to avoid scenarios that might prevent patients from getting the treatment they need.
4. Partner with Other Medical Personnel
You must create a patient 360 view of each person you are mapping to understand their journey fully. This is a single view of the patient and their data instead of trying to analyze scattered information from siloed sources.
If you limit yourself to the information you can access, you will only see half the picture. Your patient’s primary care physician and other healthcare providers are key players in your patient’s journey map.
Digital health monitoring devices, electronic health records, and contacting providers directly are all ways you can get relevant data on your patient’s other medical touch points.
5. Consistently Check-In with Patients
Your patient wants information about their drugs, treatments, and procedures, and if they don’t get that information from you, they will go to outside sources. You can help control your patient’s journey and stay involved as their most trusted medical advisor and influencer by being a valuable source of information.
As your patient undergoes treatment, take time to contact them consistently and provide thorough records and information. This will help relieve your patient’s minds and answer their questions to avoid misinformation they might receive if they search for answers elsewhere. For example, Google reports that 7 percent of searches are health-related . Those are questions patients are asking a search engine over their provider.
Staying in touch will also build trust with the patient, which will help them feel more comfortable when sharing information. You may even receive more information from patients because they know they can trust you. This information will help you keep your patients on a journey to success.
Unify Your Customer Data in One Source
Your patient journey map will save you valuable time and resources while positively influencing patients’ outcomes. In addition, you can optimize your patient journey mapping in biotech and life sciences through a unified data collection and analytic tool, so you never worry about siloed or missing information again.
Contact us to learn about our platform that will help you map your patient’s journey and provide the best care.
Opt-in with Gaine for More Insight
Great welcome to the mdm a-team you may unsubscribe at any time., more articles like this.
- Life Sciences

CMS Prior Authorization Final Rule: A Guide For Payers and Providers

System of Record Vs. System of Reference: 5 Key Differences

Operational Data Store Vs. Data Warehouse: What Works Better?
- Skip to main content
- Skip to primary sidebar
- Skip to footer
- QuestionPro

- Solutions Industries Gaming Automotive Sports and events Education Government Travel & Hospitality Financial Services Healthcare Cannabis Technology Use Case NPS+ Communities Audience Contactless surveys Mobile LivePolls Member Experience GDPR Positive People Science 360 Feedback Surveys
- Resources Blog eBooks Survey Templates Case Studies Training Help center
Patient Journey Mapping: What it is, Benefits and 5 Steps to Do it

In the rapidly evolving landscape of healthcare, patient-centered care has emerged as a crucial paradigm shift. As hospitals strive to deliver exceptional patient experiences and improve outcomes, understanding the patient journey has become paramount.
A customer journey map is a powerful tool that shares patients’ path from their first encounter with a healthcare facility to their final discharge. By visualizing this complex expedition, hospitals can gain invaluable insights into patient needs, pain points, and opportunities for enhancement, thereby revolutionizing the delivery of care.
The following article delves into the significance of patient journey maps for hospitals and their importance in optimizing patient experiences, streamlining processes, and ultimately elevating the standard of healthcare.
What is a Patient Journey Map?
A patient journey is a methodology that enables the analysis of a healthcare provider’s processes and value chain but from the patient’s viewpoint. This includes their possible solutions, pain points, emotions, touchpoints and user actions throughout the journey.
The patient journey map employs visual representation to gain deeper insights into how patients engage with a healthcare facility throughout their care journey. This unique approach is an evolution of the customer journey map , tailored specifically to the healthcare context. By employing this method, healthcare providers can unravel the intricacies of patient interactions, uncovering valuable information to enhance the quality of care provided.
The concept of the Patient Journey Map mirrors that of the Customer Journey Map, seeking to uncover areas of enhancement in patient care across various healthcare providers, including hospitals, fertility centers, and more.
Just as a skilled cartographer carefully crafts a map to navigate uncharted territories, patient journey maps chart the course of a patient’s experience, revealing hidden insights, unveiling opportunities for improvement, and ultimately guiding healthcare providers toward a destination of unparalleled patient satisfaction .
What are the benefits of implementing a Patient Journey Map?
Engaging in the patient journey proves immensely valuable as it enables us to provide patients with an optimal experience, meeting the very expectations that arise when seeking healthcare services.
The emotional aspect tied to the Patient Journey Map can be profoundly impactful, considering the inherent uncertainties often associated with visiting a healthcare facility.
Considering the unique personalities, fears, behaviors, and attitudes of different patient archetypes play a pivotal role in creating a tailored and pleasant experience for them. Thus, the patient journey map becomes a valuable tool benefiting both patients and healthcare service providers.
● Enhanced Communication with Patients:
By understanding the patient journey, healthcare providers can establish effective and continuous communication throughout the entire care process, addressing any doubts or uncertainties. Keeping patients well-informed and updated through appropriate channels reinforces the quality of care provided.
● Elimination of Blind Spots:
Clear comprehension of each stage of the patient journey helps bridge the gaps between patients and services. From the initial appointment request to discharge and follow-up, identifying and addressing potential blind spots ensures consistent and satisfactory solutions tailored to each patient’s unique situation.
● Streamlined Resolution of Pain Points:
Mapping the patient journey and defining archetypes enables a deeper understanding of patient concerns, particularly identifying which aspects of the service have the most negative impact. Pain points such as waiting times, unclear explanations, lack of empathy, or impersonalized treatments can be simplified and resolved more effectively.
Learn About: Complaint Resolution
● Process Optimization:
A well-defined patient journey optimizes workflow and allows for more efficient handling of all processes. Staff members become better equipped to anticipate and address patient issues promptly, offering alternatives that instill confidence and satisfaction.
● Continuous Improvement:
Implementing a Patient Experience model involves measuring patient experiences through a feedback system . Continuously updating the database with relevant information about patient journeys and their experiences leads to ongoing improvement in response times, customer service processes, and overall service quality .
What is a Patient Persona?
The patient persona represents an imaginary profile that encapsulates potential patients’ needs, goals, illnesses, conditions, emotions, behaviors, and knowledge.
By creating patient personas, healthcare providers can enhance the accuracy and anticipation of care and diagnosis processes, ultimately improving the experience of individuals seeking healthcare services.
5 Steps to Build Your Own Patient Journey Map
1. define the experience to map:.
Before diving into the Patient Journey Map, it is crucial to determine the specific experience you intend to outline. By establishing your objectives and identifying the type of information you seek to gather and how it will be utilized, you can ensure a more efficient mapping process right from the start.
2. Identify your Ideal Patient:
The majority of data used to construct the customer patient care journey will come directly from patient-clients. Thus, a key step is identifying the patient persona, which can be singular or multiple. You must decide whether the map will encompass various patient profiles or if separate maps will be created for each target patient.
To create the patient persona(s), gather feedback directly from patients and analyze their behaviors and data. Pose questions such as:
- What initially led the patient to seek your services?
- Which competitors did they research?
- How did they discover your website or company?
- What factors differentiated your brand from others? What influenced their decision (or lack thereof) to choose your services?
- What are their expectations when interacting with your company?
- Can they articulate what they appreciate about your company and what frustrates them?
- Have they ever contacted customer service? If so, how was their experience?
Once you have defined the patient persona(s), you can identify the distinct stages of the customer journey when engaging with your company.
3. Divide the Phases of the Customer Journey:
Throughout the customer-patient care journey, patient-clients progress through several discernible stages.
Phase #1: Pre-Visit
● DISCOVERY:
The patient journey initiates with a phase characterized by learning and concern. Patients embark on their healthcare journey upon recognizing a need or developing a concern related to a health issue.
For instance, if an individual experiences symptoms associated with being overweight, they may begin researching options for scheduling an appointment with a medical specialist. At this point, potential patients discover their specific needs and commence the process of investigating suitable solutions. They may turn to the internet, seek recommendations from friends and family, or explore other avenues. During this stage, it is recommended healthcare systems should provide educational support to aid individuals on their journey of understanding.
● CONSIDERATION:
Following their research, patients reach the consideration stage, having discovered your service. At this point, they possess some knowledge about your healthcare facility’s location and offerings, leading them to believe it could meet their needs. However, patients have also explored your competitors and are contemplating multiple options.
During the consideration stage, potential patients meticulously assess the information they come across, including service descriptions, pricing, contact pages, online inquiries, and reviews. They also evaluate the ease of accessing relevant information before scheduling an appointment and the availability of operating hours, among other factors.
Phase #3: Visit
● APPOINTMENT & ENGAGEMENT:
Having gathered sufficient information and progressed through the consideration phase, the patient ultimately chooses your service. This marks their first contact with the health center, which can occur in person, over the phone, via chat, email, or other means of communication.
During this stage, the patient schedules their appointment. The company must streamline the application process and maintain effective and proactive communication. It is crucial for this phase to be completed without complications.
● SERVICE DELIVERY:
Within the visit phase is the service delivery stage, where patients interact with various service providers at the health center. From the moment the patient enters the premises, the company must ensure an exceptional service experience.
Service delivery encompasses multiple micro-moments, necessitating comprehensive attention throughout the entire journey. Every interaction matters, from the reception care and waiting times to the core service itself—meeting the patient’s objective of being evaluated by a doctor or specialist.
Phase #3: After the Visit
● RETENTION:
The Patient journey doesn’t conclude after the initial visit. A crucial third phase occurs post-encounter, where efforts should be dedicated to fostering patient retention and encouraging their return for subsequent visits. Building strategies that monitor the patient experience is essential in designing loyalty programs to ensure patients return for future services.
● RECOMMENDATION:
Part of the post-visit phase involves patient recommendations, which heavily depend on the overall patient journey experience provided by the company. If patients have had a positive service encounter, they are likely to recommend it to others, benefiting your business.
However, it is important to remember that negative experiences are equally shared, and if patients are dissatisfied, they may spread negative feedback.
Promptly addressing any negative comments is crucial to resolving issues and preventing unfavorable recommendations.
Phase #4: Identify Touchpoints
An additional vital step in mapping the customer-patient care journey is identifying the various touchpoints between the patient and the healthcare facility. These interactions occur at different stages throughout the patient journey, and understanding these touchpoints aids in developing strategies that facilitate effective communication.
- Seeking information about healthcare centers: discovering the existence of the healthcare provider and the services it offers.
Investigation:
- Reviewing patient-client feedback: researching comments and feedback from other patients about their visit experiences at the health center.
- Exploring promotions: searching for economic benefits such as discounts, promotions, and bundled service packages.
Acquisition :
- Appointment Request: Contact or visit the health center to schedule an appointment.
- Provision of Personal Data: The health center will request personal information to finalize the appointment booking.
- Appointment Confirmation: After providing the required data, the appointment for the agreed date and time is confirmed.
- Patient Reception: The patient arrives at the health center at their scheduled appointment time.
- Waiting Room: The staff guides the patient to the designated waiting area.
- Consultation: The patient’s turn to be attended by the specialist.
- Payment: The process of settling the payment for the service, which may occur at any point during the service phase, depending on the health center’s policies.
- Patient Recommendations: Patients offer positive or negative feedback about the health center and its services.
- Loyalty Program: Incentives such as offers, promotions, discounts, or a points system to encourage future visits.
Recommendation:
- Complaint: If the patient has had a negative experience, they may file a complaint with the health center.
- Online Reviews: Patients share comments or criticisms about the service by posting reviews on the internet.
4. Identify Contact Channels
Patients engage with the health center through various channels throughout the patient journey. These channels, such as the health center itself, can be physical or online, including social media, email, applications, websites, and online forms.
Identifying the most utilized contact channels at each stage of the customer-patient care journey is crucial. This allows for the development of tailored strategies for each channel, meeting patient expectations at each phase.
Working on the patient journey is crucial for healthcare providers to deliver a high-quality experience to patients. By mapping their interactions, providers gain a deeper understanding of their patient personas, allowing them better to comprehend patient needs, desires, and circumstances to provide the desired care.
Patient Journey Map Example
To better understand what a Patient Journey Map is, we have created this fictitious example using one of the most reputable medical institutions in the healthcare sector, the Massachusetts General Hospital, as a reference.
In this example, we have included some generic touchpoints that are usually the most common in the interaction between a hospital and a patient.
Through this example, it would be possible to visualize the points of interaction between both parties and the perception that patients have of them, which can be positive or negative. This serves as a clear indicator for making adjustments and learning from what has been done well.
The Office of Patient Experience plays a vital role in facilitating initiatives to assess and enhance the quality of care experienced by patients and their families. They are responsible for evaluating each of these touchpoints and ensuring that appropriate actions are taken.
The Mass General Hospital is a benchmark not only in terms of service level but also in the implementation of methodologies and actions that guarantee the satisfaction of their patients. A clear example of this can be seen in the results of their annual HCAHPS survey, where they score above the national average in various aspects.
Willingness to Recommend Hospital Scores below show the percentage of patients who would “definitely recommend” Mass General to their friends and family.
To see the complete study, we invite you to visit their website and learn about it.
More Examples of Patient Journey Maps
Seeking inspiration to craft your own Patient Journey Map? Your search ends here!
Explore a collection of remarkable examples from top-notch brands, unveiling their initiatives that delight customers and foster loyalty.
Get set to revolutionize your own Patient Journey!
Mass General Hospital is renowned for providing exceptional care and taking special care in understanding the perspective of its patients. They achieve this through different tools, such as satisfaction surveys, internal and external feedback, and HCAHPS surveys .
Mayo Clinic is characterized by its focus on patient satisfaction and its extensive technical deployment to gather user and prospect feedback.
Cleveland Clinic is often ranked among the best hospitals in the United States. This recognition is not only due to its incredible facilities, global expansion, and well-prepared staff but also because of its remarkable focus on the experience they provide to its patients and clients.
Singapore General Hospital is one of the largest and oldest hospitals in Singapore. It has been a major healthcare institution providing a wide range of medical services and treatments since 1821.
Johns Hopkins Medicine has long recognized the significance of a positive patient and family experience during hospitalization, which is why they maintain a specific focus on patient satisfaction to achieve an optimal experience.
How can you enhance your Patient Journey Map based on your acquired knowledge?
The insights and recommendations shared above are likely to have sparked ideas about the potential impact of these initiatives across various industries, not just healthcare.
The first crucial step is to embrace a customer-centric approach, keeping their needs and expectations at the forefront. By doing so, the actions you take will have a meaningful impact on your customers and yield multiple benefits for your business.
At QuestionPro, we offer a range of tools and features specifically designed to help you achieve this objective.
QuestionPro SuiteCX is a Customer Journey Mapping Software that simplifies the process of creating your customer journey.
With a vast selection of templates and the ability to personalize user/buyer personas while incorporating your own data, you can conduct precise visual analyses at every touchpoint throughout your patient journey.
Start delighting your customers today!
MORE LIKE THIS

NPS Survey Platform: Types, Tips, 11 Best Platforms & Tools
Apr 26, 2024
User Journey vs User Flow: Differences and Similarities

Best 7 Gap Analysis Tools to Empower Your Business
Apr 25, 2024
12 Best Employee Survey Tools for Organizational Excellence
Other categories.
- Academic Research
- Artificial Intelligence
- Assessments
- Brand Awareness
- Case Studies
- Communities
- Consumer Insights
- Customer effort score
- Customer Engagement
- Customer Experience
- Customer Loyalty
- Customer Research
- Customer Satisfaction
- Employee Benefits
- Employee Engagement
- Employee Retention
- Friday Five
- General Data Protection Regulation
- Insights Hub
- Life@QuestionPro
- Market Research
- Mobile diaries
- Mobile Surveys
- New Features
- Online Communities
- Question Types
- Questionnaire
- QuestionPro Products
- Release Notes
- Research Tools and Apps
- Revenue at Risk
- Survey Templates
- Training Tips
- Uncategorized
- Video Learning Series
- What’s Coming Up
- Workforce Intelligence
Calculates the ROI of investing in our queuing and self-service solutions Learn More
Unlock the full potential of our solutions!
- What is Patient Experience & Why It Is Importance ?
A Comprehensive Guide to Patient Journey Mapping
- Author: Wavetec
- Published: January 26, 2024
Is regulating patient experience at your healthcare service a challenging task? If your patients leave the hospital unsatisfied with the service, we have a solution for you!
Patient journey mapping is vital in understanding your patient’s experience at every step of interaction with the hospital, whether virtual or physical. This allows you to empathize with your patients, facilitate their experience, and contribute in uncertain and stressful times.
Parallel to the patient’s journey, healthcare systems face increasing challenges in patient management, regulating space constraints, limiting healthcare providers, and budgeting. By mapping the patient journey , you can pinpoint the shortfalls in your management services, improve facilities, and increase patient turnout.
The patient journey map must be curated in detail, accounting for various touchpoints and patient perceptions. The most accurate method of measuring healthcare quality is pairing patient journey maps with patient satisfaction scores, such as the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAPHPS) and a Net Promoter Score (NPS) .
Higher scores speak volumes about your healthcare services, increase patient retention, and promise returns.
What is Patient Journey Mapping?
Patient Journey Mapping is a strategic tool in healthcare that visually illustrates the entire patient experience, from initial contact to post-treatment follow-up. It involves mapping out key touchpoints and stages, such as appointment scheduling, diagnosis, treatment, and aftercare.
This process allows healthcare providers to understand the patient’s pathway through the healthcare system comprehensively.
Amidst the changing landscape of the healthcare industry, patients look for service providers that offer a personalized experience. Besides renowned healthcare providers, patients look for a human-centric environment that provides timely and efficient services.
Moreover, modern consumer requirements demand a digital transformation of healthcare services.
Healthcare managers can use patient journey maps to visualize the blind spots and pain points in a patient’s experience. A distinguished healthcare service sees journey mapping as a powerful tool that tells about a patient’s well-being and connects care providers with their emotional journeys.
You can make your practices to be more empathetic and make a difficult journey seamless.
The Benefits of Patient Journey Mapping
Investing in patient experience mapping carries benefits for both parties, care providers and patients. We have highlighted some benefits of journey mapping below:
Improved patient communication
Identifying unaddressed patient issues helps build a connection with the patient. Keeping them at the model’s center and informing them of changes before their visit reduces frustration and confusion.
Continuous patient care
With a streamlined workflow, staff members and care providers can remove uncertainties from a patient’s care journey. An integrated healthcare system removes loopholes, such as overbooked appointments, which otherwise lead to negative patient feelings.
Personalized care
Given the nature of the treatment plans and services offered by the healthcare industry, a one-shoe-fits-all theory does not apply to the consumers. By integrating patient data with business models, you can provide a customized experience to the patients.
Turn-out increases when patients receive automated appointment reminders and physician availability updates.
Improved Efficiency
Patient journey maps identify the demand for time management and sensitivity in healthcare. Feasibility arrangements such as pre-booking appointments, receiving digital laboratory reports, and online consultations boost patient satisfaction.
Patient retention and profitability
Patient feedback is crucial to introducing or revising policies, growth opportunities, and consistent revenues.

Seamless Patient Journey
With our intuitive interface, patients can easily register, check-in, and monitor their queue status. This reduces their anxiety, improves their overall experience, and fosters a positive perception of your healthcare facility.
7 Key Stages in the Patient Journey
Patient journey mapping differs for each hospital or clinic, depending on the care level. Most tertiary care hospitals identify three key stages when patients experience mapping .
Touchpoints of each step may differ slightly in pregnancies, emergency services, and outpatient departments.
Let’s read about the details of each stage below:
1. Awareness:
- This stage often begins with recognizing symptoms, changes in health, or routine checkups revealing potential issues.
- Patients may notice something is amiss, prompting them to seek further information or professional advice.
2. Consideration:
- Information gathering kicks into high gear. Patients may research their symptoms, explore potential causes, and consider various treatment options.
- Seeking advice from healthcare professionals, friends, or family members becomes a key part of this stage.
3. Decision:
- Armed with information, patients make decisions about their course of action. This could involve choosing a specific healthcare provider, deciding on a treatment plan, or committing to lifestyle changes.
- The decision-making process may also involve discussions with healthcare professionals to ensure alignment with the patient’s values and preferences.
4. Engagement:
- This is the active phase, where patients interact with healthcare providers, undergo diagnostic tests, and initiate the chosen treatment plan.
- Open communication between the patient and the healthcare team is crucial during this stage to address concerns, clarify expectations, and ensure a collaborative approach.
5. Treatment and Recovery:
- The chosen treatment plan is implemented, whether it’s medication, surgery, therapy, or a combination of interventions.
- Recovery involves monitoring progress, managing potential side effects, and adapting the treatment plan as needed.
6. Follow-Up and Maintenance:
- Post-treatment, patients often enter a phase of follow-up care. This can include regular check-ups, monitoring for recurrence, and adjusting treatment plans as necessary.
- Lifestyle changes and ongoing self-care may be emphasized to maintain health and prevent future issues.
7. End-of-Life Care (if applicable):
- In cases of terminal illness, this stage involves compassionate and supportive care. Palliative care aims to enhance quality of life, manage symptoms, and provide emotional and spiritual support.
- This stage emphasizes open communication about end-of-life preferences and ensures a dignified and comfortable experience for the patient and their loved ones.
Analyzing the Patient Journey Map
Once you have designed a patient journey map for your service, the correct way of utilizing the maps is to identify the pain points. Next, we enlist and discuss some common hurdles patients face that delay prompt care, including internal and external factors or barriers to healthcare.
1- Pre-visit
- The patient feels anxious about the medical condition.
- The website needs more information about the healthcare facility to make patients satisfied. Your website must be SEO-friendly and listed on Google to regulate patient management.
- During this stage, missed phone calls and confusing appointment scheduling tasks lead to care provision delays.
- Limited communication with consultants before visiting
2- At the healthcare facility
- Filling out the pre-appointment questionnaire is time-consuming and makes patients uneasy.
- Lengthy waiting times and mismanaged queues for appointments reduces patient satisfaction. Patients waiting at the facility can be guided using digital signage that communicates announcements, turns, and navigates around the healthcare facility.
- Explaining old symptoms and information to the same care provider at every visit frustrates patients.
3- Post-treatment plan
- Billing and initiating the hospital discharge process is often tedious.
- Receiving feedback from patients to measure patient satisfaction.
- Unable to monitor the patient at home and set up follow-up appointments creates mistrust between the patient and the doctor.
Gain valuable insights
Leverage our healthcare queue management system’s data to make informed decisions to improve the patient experience. We have seen up to a 35% increase in patient satisfaction.
Patient Journey Mapping Template
We have designed templates of patient journey maps to help you make the best one for your hospital system. As shown in the samples, patients visiting different departments have specific touchpoints. For example, a patient scheduling his appointment for the outpatient department will research the clinic and the primary caregiver.

However, the primary concern for patients requiring urgent care will be prompt ambulance services and treatment. Despite the differences, all patient journey maps are based on three key stages: pre-hospital care, in-hospital care, and post-treatment plans.

Patient Journey Improvement Solutions
If you want to enhance patient flow management and boost patient satisfaction at your hospital, we recommend using pre-engineered solutions. There are many ways to improve the quality of service you provide to your patients.
One such solution is the Wavetec patient flow system. Adopting a digital healthcare system can optimize patient-doctor interaction and improve investment returns.
We have put together the most impactful solutions your facility can sign-up for each stage of the patient journey map. Here’s what they are:
- Online appointment and booking
- Queue management – People counting, WhatsApp Queuing, Queue management applications, Digital Signage
- Patient application
- Self-check-in kiosks
- Integrated manager dashboards and analytics
- Customer feedback reports
- Curbside pickups
Let’s learn about each solution and how it will benefit your healthcare center.
1. Simplify Online Appointment Booking

Before visiting the facility, patients can schedule online appointments and ticketing on the website or patient application with their preferred physician. This service allows your patients to book seamlessly, check-in and receive wait time or canceled appointment notifications. Satisfying your customer before they arrive mitigates their already-high worry levels.
2. Patient Management

Waiting in queues for examination rooms and healthcare providers is a major source of concern for patients. You can reduce perceived wait times by giving patients a virtual waiting room. This can be done by signing up for WhatsApp Queuing and the Queue Management Mobile App. These services give patients virtual tickets and wait time notifications, allowing them to manage time effectively.

Walk-in patients and patients with pre-booked appointments can also use automated, self-service kiosks at the facility to check in or reschedule appointments. Patients can scan the displayed QR code or use biometrics technology to receive tickets via SMS, Email or WhatsApp.
You can manage the patient count in the waiting area using a real-time counter and digital signage . This helps emergency case patients to navigate the hospital without confusion.
3. Promoting Patient Satisfaction
Many patients must visit the healthcare facility multiple times to collect laboratory reports, prescriptions, and medications. You can facilitate this tedious process by providing delivery and curbside pickup options. This regulates unnecessary traffic at your hospital and saves time for patients.

Investing in Patient Applications is a great marketing tool and a one-stop solution to patient worries. Individuals can learn more about your facility’s services, access laboratory reports, initiate billing, and receive updates and reminder notifications. This is particularly useful in conducting telehealth rotations with expecting mothers and palliative care patients who cannot visit the facility often.
4. Patient Feedback

Receiving your consumer’s feedback and solving their queries ensures a successful approach to patient journey mapping. Wavetec has designed a customer feedback solution to measure customer satisfaction and follow up on your staff’s performance.
Additionally, you can get a management portal for the hospital staff and care providers. This can be integrated with patient data to give healthcare providers complete information.
Softwares such as Spectra include dashboard analytics and reports on the performance of each department to help you identify the shortfalls. This will help you build a congregated team that runs operations smoothly in the patient’s best interest.
Studies have shown that facilities using solution experience up to a 50% decrease in missed appointments, optimizing resource utilization and increasing revenue.
The modern healthcare system requires providers to be more involved in providing a seamless patient experience. In this blog, we highlight the role of patient journey mapping to help you identify touchpoints in a patient’s journey. Before, during, and after treatment, it is crucial to comprehend the patient’s viewpoint to ensure proper care.
Patient journey solutions are, therefore, integral in distinguishing your healthcare facility. Investing in patient applications, queue management software, receiving customer feedback, and analyzing it is vital in improving your standing.
Adopt our solutions, transform the healthcare industry, and make your approach more empathetic!
- No translations available for this page
Follow the patient flow by listening to the patient journey
Get the full story and understand the process – see the outcomes, be confident in your CX, and drive change with the voice of the customer.
Actionable customer feedback without survey fatigue. See Authenticx in action:
When is the last time surveys followed the entire patient journey?
Collecting data is only part of the equation. Understanding begins by listening to gather qualitative context and themes.

Unsolicited feedback is an unbiased, renewable source of customer insights that surfaces what’s truly top of mind for the customer in their own words.
Patient Flow vs. Patient Journey
Patient flow and patient journey are two interrelated concepts in healthcare that focus on different aspects of the patient experience. While both are crucial for optimizing healthcare delivery, they have distinct implications for healthcare management. Understanding patient flow vs. patient journey helps providers streamline processes and enhance the overall quality of care.
Patient flow refers to the movement of patients through the various stages of the healthcare delivery process, from the initial point of entry to the final discharge or follow-up. It encompasses the coordination of resources and personnel to ensure timely and efficient care.
Patient flow management involves healthcare process standardization and optimization , focusing on reducing waiting times, improving resource allocation, and minimizing bottlenecks within the system. Effective patient flow management is essential for maximizing the operational efficiency of healthcare facilities and ensuring that patients receive the care they need in a timely manner.
Key aspects of patient flow management include:
- Admission and registration: Efficiently managing patient intake, including collecting necessary information and verifying insurance details.
- Triage and assessment: Quickly and accurately evaluating the severity of a patient’s condition to prioritize care and allocate resources accordingly.
- Treatment and intervention: Coordinating the delivery of appropriate medical care , such as diagnostics, therapies, and consultations with specialists.
- Discharge planning and follow-up: Ensuring that patients have a smooth transition from the healthcare facility to their next phase of care, whether it be home care or rehabilitation services.
The patient journey, on the other hand, is a broader concept that involves the entire experience as patients navigate the healthcare system. It includes not only the clinical aspects of care, but the emotional, psychological, and social dimensions of the patient experience. Patient journey management aims to understand and optimize operations to ultimately build patient trust .
Key aspects of patient journey management include:
- Communication and information: Providing clear, consistent, and timely information to patients regarding their condition , treatment options, and expectations for recovery.
- Emotional support: Addressing the emotional and psychological needs of patients and their families, such as offering empathy and counseling services when needed.
- Patient-centered care: Empowering patients to actively participate in their care by involving them in decision-making and acknowledging their individual needs and values.
- Continuity of care: Ensuring seamless coordination and communication among healthcare providers across different care settings, promoting a sense of continuity and trust throughout the patient’s journey.
By recognizing the distinctions between patient flow and patient journey, healthcare providers can develop targeted strategies to optimize both aspects of care. This can improve the quality of healthcare services and foster a more patient-centered approach to healthcare delivery.
Patient Flow Optimization
Patient flow optimization is a critical component of healthcare management, as it directly impacts the quality and efficiency of care delivery. By focusing on healthcare workflow management and process standardization, healthcare providers can streamline patient flow and ultimately improve patient outcomes and satisfaction.
Here are some key concepts to be aware of when it comes to optimization:
- Healthcare workflow management: Streamlining processes and workflows within the healthcare facility can significantly enhance patient flow. This involves mapping out each step of the patient journey, identifying bottlenecks and inefficiencies, and implementing targeted solutions to address these issues.
- Operational efficiency: Focusing on healthcare efficiency metrics can provide valuable insights into areas for improvement within the healthcare facility. Key metrics may include patient waiting times, bed turnover rates, and the average length of stay.
- Resource management: Effective resource management is crucial for optimizing patient flow, as it ensures that the necessary personnel, equipment, and facilities are available to provide timely and appropriate care. This includes the strategic allocation of staff, such as nurses, physicians, and support personnel.
- Process standardization: Implementing standardized processes and protocols across the healthcare facility can help improve patient flow by reducing variability and enhancing consistency in care delivery. Standardization efforts may involve the adoption of evidence-based clinical pathways, best practice guidelines , and standardized documentation systems.
In addition to these strategies, healthcare providers should also focus on healthcare productivity metrics, such as staff utilization rates and the ratio of direct patient care to administrative tasks. By monitoring and optimizing these metrics , healthcare facilities can ensure that their staff is being used effectively and that resources are being allocated in the most efficient manner possible.
Patient Journey Mapping
Patient journey mapping is a powerful tool used in healthcare service design to visualize and understand the entire patient care journey. By creating a visual representation of the patient’s journey, providers can identify pain points, uncover opportunities for patient experience enhancement, and develop strategies to improve overall healthcare system design.
The process of patient journey mapping typically involves the following steps:
- Define the scope: Determine the specific patient population, healthcare setting, or condition to be addressed. This helps ensure that the mapping process remains focused and relevant to the intended audience.
- Gather data: Collect information on the patient care journey, including patients’ interactions with healthcare providers, the emotions they experience, and any obstacles they encounter along the way. This data can be gathered through interviews, surveys , and other research methods.
- Create the map: Develop a visual representation of the patient’s journey, highlighting key touchpoints, interactions, and experiences. The map should be detailed enough to provide a comprehensive understanding of the patient’s experience while remaining easy to interpret and analyze.
- Identify pain points and opportunities: Analyze the patient journey map to pinpoint areas of friction, unmet needs, or inconsistencies in care delivery. These pain points represent opportunities for healthcare service design improvements and patient experience enhancement.
- Develop targeted strategies: Based on the insights gleaned from the patient journey map, develop targeted interventions to address identified pain points and enhance the patient experience.
- Implement and evaluate: Put the proposed strategies into action and continuously monitor their impact on the patient experience. Adjust and refine the interventions as needed, based on ongoing feedback and data analysis.
Patient journey mapping helps providers identify areas for improvement and promotes healthcare patient engagement by fostering a deeper understanding of patient needs, expectations, and emotions. By placing the patient at the center of healthcare service design, providers can develop tailored interventions that address individual needs and preferences.
Related Resources
- Improving The Patient Journey
- Patient Feedback Software
- Patient Retention
- Patient Experience in Hospitals
- Analytics to Improve Customer Experience
- Patient Experience Survey
- Patient Experience Feedback
- Customer Experience Platform
How It Works
Gain a deeper level understanding of contact center conversations with AI solutions.
Pull customer interaction data across vendors, products, and services into a single source of truth.
Collect quantitative and qualitative information to understand patterns and uncover opportunities.

Confidently take action with insights that close the gap between your organization and your customers.
Patient Experience Management
Patient experience management is a comprehensive approach to understanding and improving the quality of care from the patient’s perspective. It encompasses all aspects of the patient’s interactions with the healthcare system, including the clinical, emotional, and logistical dimensions of care. Patient experience management is essential for ensuring patient satisfaction .
By prioritizing the patient’s perspective and implementing proven strategies for patient experience optimization, healthcare providers can create a more patient-centered care environment that enhances patient satisfaction and fosters long-term relationships.
Key aspects of patient experience management include:
- Communication: Ensuring clear, timely, and empathetic communication between healthcare providers and patients is critical for improving patient satisfaction. This involves not only providing information about medical conditions and treatment options but addressing patients’ concerns and expectations.
- Emotional support: Recognizing and addressing the emotional and psychological needs of patients is a crucial component of patient experience management.
- Patient-centered care: Patient experience management emphasizes the importance of patient-centric care delivery, wherein patients are actively involved in the decision-making process, and their preferences, values, and needs are respected.
- Continuity of care: Facilitating seamless transitions between healthcare settings and providers can help optimize the patient experience.
- Measurement and improvement: Regularly monitoring satisfaction and experience metrics is a critical aspect of patient experience management. By analyzing this data, healthcare providers can identify areas for patient satisfaction improvement, develop targeted strategies for enhancing the patient experience, and track progress over time .
Healthcare Process Management
Healthcare process management is a systematic approach to designing, implementing, and improving the various processes involved in the delivery of healthcare services. Its purpose is to enhance healthcare operational efficiency, optimize resource allocation, and improve patient outcomes.
Healthcare process optimization ensures that healthcare organizations operate efficiently and effectively while continuing to provide high-quality patient care. By identifying inefficiencies and areas for improvement within the healthcare system, organizations can enhance their quality of care and optimize the use of resources.
Key aspects of healthcare process management include:
- Process mapping and analysis: Healthcare process management involves spotting and mapping the factors and processes relevant to care delivery. This includes clinical workflows, administrative tasks, and support services.
- Healthcare process optimization: Once the processes have been mapped and analyzed, healthcare organizations can implement targeted interventions to optimize these processes. For example, they may decide to standardize protocols or adopt new technologies to streamline operations.
- Hospital resource management: Efficient management of resources, such as staff, equipment, and facilities, is critical for optimizing healthcare operational efficiency. Healthcare process management focuses on ensuring that resources are allocated in the most effective way possible.
- Healthcare utilization management: Process management also requires proper healthcare utilization, which refers to the appropriate use of healthcare services, procedures, and facilities.
- Continuous improvement: Healthcare process management is an ongoing effort that takes regular monitoring, evaluation, and refinement of processes and interventions. By embracing a culture of continuous improvement, healthcare organizations can adapt to evolving patient needs and ensure long-term success.
Authenticx for healthcare providers offers users business-critical insights for maximizing efficiency and improving the patient experience across the board. With Authenticx , healthcare organizations can determine how to manage processes more effectively by listening to and analyzing the collective patient voice .
Exponentially listen with confidence.
Aggregate topics, themes, and patterns from millions of conversations to drive relevant and impactful insights.
(818) 308-4108
Patient Flow vs Patient Journey
In this ever-evolving healthcare climate, two significant concepts have surfaced: patient flow and patient journey. While both might sound similar, they represent different yet interconnected aspects of patient management. Let’s dive into what sets them apart and why perfecting them matters in healthcare.
Understanding Patient Flow
Did you know that patient flow refers to how patients move within a healthcare setting? It’s all about processes, such as how patients get admitted, transferred, and eventually discharged, like how traffic flows on a highway. A smooth patient flow is all about getting the right patient to the right place at the right time, with no roadblocks or congestion.
But why is it so significant? Imagine ordering your favorite meal at a restaurant only to find out they’ve mixed up your order. Frustrating, right? That’s precisely how it works in healthcare. Poor patient flow can create bottlenecks that slow treatment, affecting patient satisfaction. It can also overwork healthcare professionals and strain resources.
However, when effectively managed, patient flow can drastically ramp up efficiency. It can reduce waiting times, optimize the use of resources, and even improve the quality of care provided. And let’s not forget its crucial role in ensuring a smooth and seamless healthcare delivery process, which brings us to our next topic.
Understanding Patient Journey
Now, let’s talk about something more personal – the patient journey. It’s like walking a mile in the shoes of a patient. Unlike patient flow, which is more about logistics and operations, the patient journey is about the patient’s experiences and narratives from their initial contact with the healthcare system to their recovery stage (hopefully).
Taking our restaurant metaphor a step further, the patient journey is your dining experience from the moment you step in until you pay the bill and leave. How was the ambiance? Was the staff friendly? Did they serve your meal on time, and most importantly, how was the taste? Similarly, in healthcare, it’s about how patients feel and what they experience.
The patient journey maps out every patient’s interaction with the healthcare system. Healthcare providers can use these insights to tailor their services and improve their patients’ experience. After all, happier patients make for better success stories, and these stories are what fuel healthcare providers to continue improving.
Comparing Patient Flow to Patient Journey
Now, let’s pit patient flow against the patient journey. It’s not a boxing match per se, but a comparison of two healthcare heavyweights. While it seems they could be interchangeable, there’s a distinct difference. The first focuses on operational efficiency, while the latter is about individual experiences and narratives.
Digging a bit deeper, patient flow is the groundwork – the basic framework ensuring that a healthcare system operates smoothly, just like how the kitchen needs to function efficiently to deliver your meal on time. On the other hand, the patient journey is more like the seasoning added to our dish. The distinctive blend of individual experiences, the emotional ups and downs, and the personal anecdotes make the healthcare experience unique for each patient.
Patient flow and patient journey might seem like two sides of the same coin, but they’re different and critically essential in their own ways. Perfecting both these aspects can truly pave the way for a holistic and patient-centric healthcare system.
Operational Efficiency vs. Personal Experience
In healthcare, operational efficiency directly translates into how quickly you can move patients from check-in to discharge while maintaining high-quality care.
On the flip side, personal experience is equally important. It’s the journey your patients embark on from the moment they step into your practice. This isn’t just about the treatment they receive but also about how they feel throughout their interaction with your healthcare system. A positive experience can mean clear communication, emotional support, and attention to individual needs.
While you strive for operational efficiency, remember that every patient is a person with unique fears, hopes, and concerns. Patients are not just numbers in a system; they’re individuals who want to be seen and heard. It’s essential to strike a balance – a streamlined healthcare process must also have room for personal touches that can alleviate anxiety and build trust.
Consider this: a study by Deloitte found that hospitals with higher patient-reported experience scores tend to have higher profitability. This suggests that investing time in personalizing patient experience doesn’t just benefit your patients; it can also positively impact your bottom line.
Leveraging technology can help. For example, a digital check-in system might speed up the admittance process while also providing an opportunity for patients to communicate their concerns and preferences, tailoring their journey from the outset.
However, technology alone won’t solve everything. Encourage your team to maintain a human connection. Small gestures, like a warm greeting or taking a moment to explain the next steps, can alleviate stress and contribute to a better overall patient experience without sacrificing efficiency.
In essence, combines the power of operational efficiency with the art of personal experience. Keep these dual objectives in harmony, and you’ll see smoother processes and happier patients who are more likely to return and possibly refer others to your practice. After all, healthcare is as much about healing hearts as it is about healing bodies.
The Impact of Patient Flow on Patient Journey
There’s no denying that patient flow and patient journey are inherently intertwined. A well-managed patient flow can significantly impact a patient’s journey and vice-versa. Consider this: if a hospital has good patient flow, patients are seen promptly, without unnecessary delays or obstacles. Sounds perfect, doesn’t it?
Now, think about it from a patient’s perspective. If you’re sick, the last thing you want is waiting in endless queues or being transferred from department to department without proper guidance. A smooth flow means less anxiety and confusion. It might even result in receiving full attention from doctors and not feeling rushed during consultations. And those factors make a huge difference in a patient’s healthcare journey.
Yet, an efficient patient flow doesn’t solely guarantee a good patient journey. Even if the hospital operates on a well-oiled patient flow, the patient journey could falter if the quality of care, interpersonal engagement, or empathy from healthcare providers is lacking. And then we have the subjective aspects, like a patient’s personal perception of their experience, which, I’ll admit, could be trickier and more fluid.
Case Studies
Let’s bring some real experiences into the mix. In one clinic, patients were experiencing long wait times due to inefficient patient flow, negatively affecting their overall journey. A thorough analysis revealed the need for better organization of clinic processes, such as scheduled appointments and staffing. After implementing changes, the clinic noticed a significant reduction in waiting times. Patients were happier! But more importantly, the staff also felt a reduced burden of chaos in handling incoming patients.
In another study involving a large metropolitan hospital, administrators made considerable changes to enhance patient flow. Hospital beds and staffing were utilized more effectively, reducing bottlenecks in patient admission and transition processes. The end result? A noteworthy increase in patient satisfaction scores. However, the hospital also understood that even with more efficient patient flow, the patient journey could be influenced by factors such as privacy, empathy from staff, and communication of clear treatment plans.
The Challenges in Balancing Patient Flow and Patient Journey
It all seems pretty straightforward until you get into it. Balancing patient flow and patient journey is more of a tightrope walk than an easy cruise. Healthcare professionals must ensure efficient operation without compromising on the empathetic, human side of healthcare.
Take wait times, for example. While shortening them helps improve patient flow, it shouldn’t compromise consultation time- a crucial aspect of the patient journey. Patients should not feel part of a conveyor belt assembly, right? Healthcare professionals should have ample time to understand their concerns, propose solutions, and ensure patients leave feeling well cared for.
Different patient expectations also pose a challenge. Each patient has unique needs, and defining what constitutes a good ‘journey’ might vary considerably. Therefore, the challenge becomes about personalizing experiences without interrupting seamless patient flow.
The tightrope walk involves creating a healthcare setup that ensures efficient patient flow while nurturing individual, personalized experiences that contribute to a meaningful patient journey. Not an easy feat, but one worth striving for!
Related Posts
Nursing burnout: causes, symptoms, and prevention techniques, how do first impressions affect your patient interaction, what are good clinical data management practices, the role of patient-centered care in modern healthcare, elevate your practice to the next level.
Let us show you how to save 2 hours a day.
Join the modern digital health era with Ambula
Medical office software
Clinic management software
Privacy Policy
© 2024 • Ambula Health • EMR Software
Call Us (818) 308-4108
Checkout Our EMR Software Deals!
Join Our Weekly Newsletter
Automated page speed optimizations for fast site performance
Patient Journey Mapping
Improve patient journey in your healthcare facility, understand your healthcare facility and its service processes from the patients’ point of view. create a patient journey map to understand the pain points in their journey and how to improve and streamline the processes to provide the best service..
- Customizable templates to identify, map, and plan patient experiences
- Infinite and intuitive canvas to visualize the entire process throughout the facility
- Import data from multiple platforms to analyze the customer feedback, reviews, and ratings
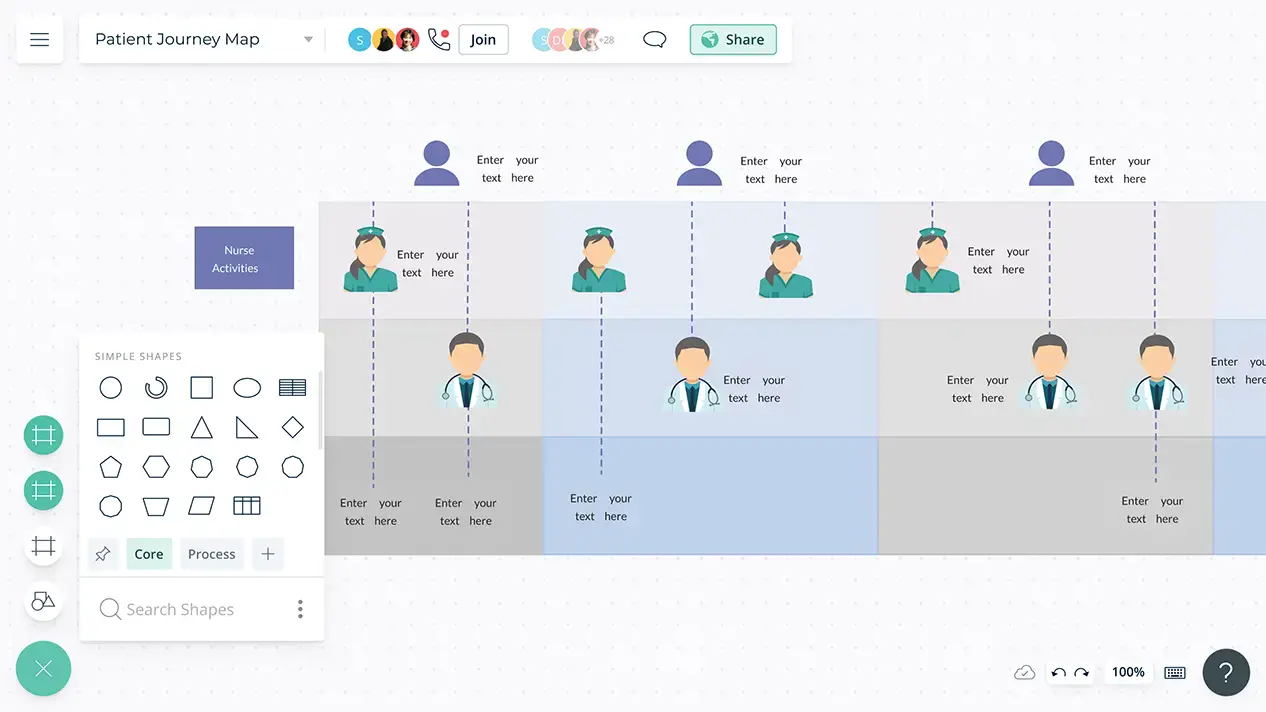
Visualize the Patient Journey Maps in Minutes
A library of customizable patient journey map templates to quickly get started identifying the relevant scenarios and current workflows.
Import data from Microsoft Excel, Google spreadsheet, or CSV to centralize all of your information onto one infinite canvas to visualize any stage of the patient’s journey.
Data-driven shapes to add more context and store information in one place.
Shape library containing 1000s of components to visualize the patient journey in detail.
Create Well-Structured Patient Journeys
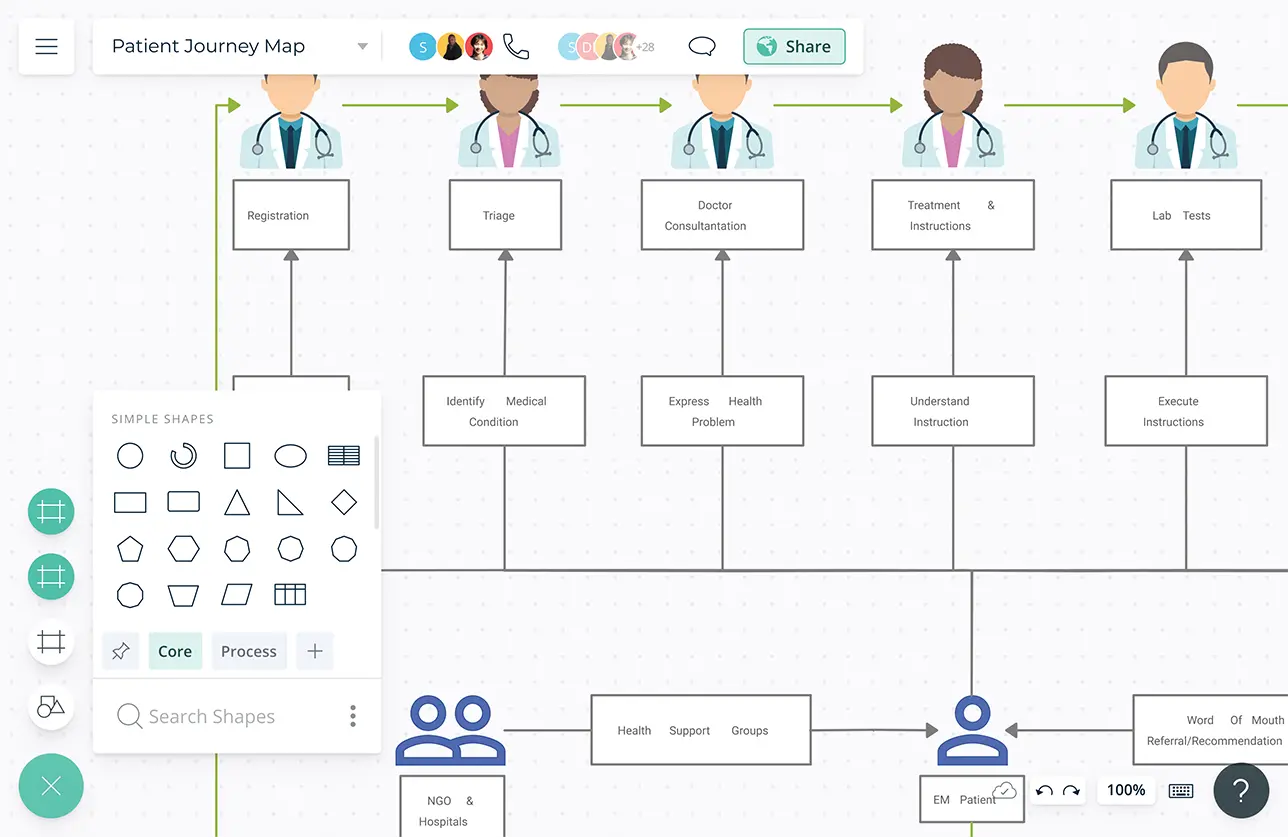
Advanced folder structure to structure the workspaces with similar content and processes.
Add data to each element on the canvas to store and track the records related to the average time and cost for treatments.
Video conferencing and whiteboarding to work closely with the teams in real-time.
Multiple access and role levels to streamline sharing, reviewing, and editing patient journey maps.
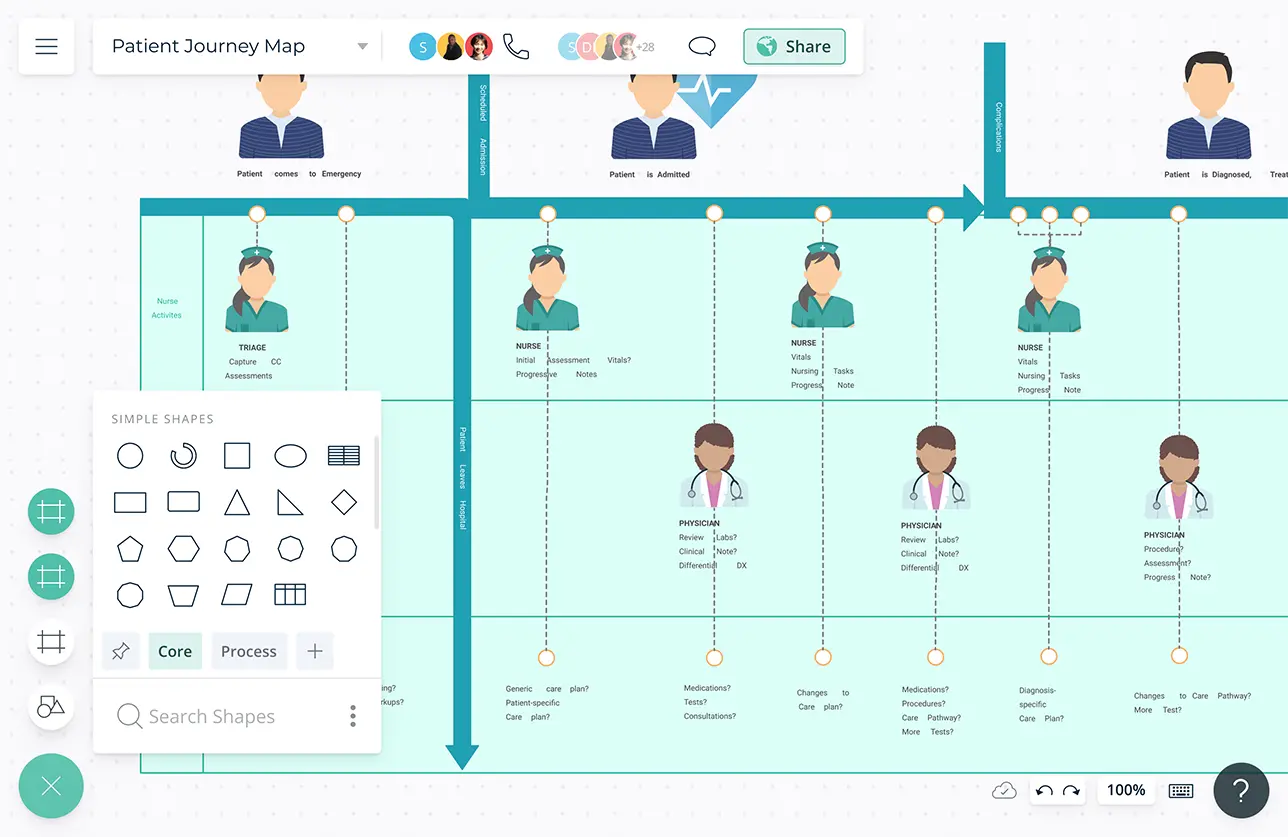
Easily Share Your Patient Journey
Connect to your favorite tools with Creately plugins for Github, Slack, Google Workspace, Confluence, and more.
Embed in any site, share with anyone via an email or link, and invite to collaborate on.
Export as SVGs, PDFs, JPEGs, and PNGs to publish, present, print, or share.

What is a Patient Journey Map?
Patient journey maps help obtain insight into the patient’s experiences during their care journey in a medical facility. It highlights all the patient’s pain points during their journey and helps health care workers and management to develop strategies to improve the patient journey.
How to Create a Patient Journey Map?
- Start by creating user personas for patients who belong to different segments. You can do this using a user persona template on Creately.
- Gather some information to understand the goals of the patients, especially what they aim to achieve at the end of their medical journey.
- Use Creately’s user-flow flowcharts to map out the different paths patients take when interacting with the healthcare system.
- Referring to the flowcharts, identify the minor and major touchpoints and the patient goals associated with them. Add them to your patient journey map.
- With the help of the information you have gathered, identify the potential pain points and blockers in your patient’s journey. You can add these to the journey map as well.
- You can share your patient journey map, using Creately’s real-time collaboration feature, with others in your team and other departments to get their input as well.
- Identify ways you can remove the roadblocks in the map with your team and apply the solutions to the patient journey map as you improve it.
- Embed the patient journey maps in your intranet or other internal websites or share them with edit or review access with everyone so they can easily access it and help update and improve it.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 13, Issue 1
- Streamlining patient flow and enhancing operational efficiency through case management implementation
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0009-0003-3746-6998 Sultanah Al Harbi 1 ,
- Baker Aljohani 2 ,
- Lamiaa Elmasry 3 ,
- Frenk Lee Baldovino 1 ,
- Kamille Bianca Raviz 1 ,
- Lama Altowairqi 4 ,
- Seetah Alshlowi 1
- 1 Case Management Department , Al Hada Armed Forces Hospital , Taif , Makkah , Saudi Arabia
- 2 Medical Administration , Al Hada Armed Forces Hospital , Taif , Makkah , Saudi Arabia
- 3 Quality Improvement and Patient Safety Department , Al Hada Armed Forces Hospital , Taif , Makkah , Saudi Arabia
- 4 Admission Office Department , Al Hada Armed Forces Hospital , Taif , Makkah , Saudi Arabia
- Correspondence to Dr Sultanah Al Harbi; sm.alharbi909{at}gmail.com
Background Improving patient flow in hospitals represents a worldwide healthcare challenge. The objective of this project was to depict the effectiveness of case management in improving patient flow in a tertiary hospital setting.
Methods Quality improvement methods, including quantitative pre-Lean and post-Lean design, the Plan-Do-Check-Act concept, the Single Minute Exchange of Dies and the ‘demand and supply approach’ of the Institute of Healthcare Improvement, were adapted to examine and modify factors influencing hospital patient flow.
Results This study (conducted from the last quarter of 2019 through September 2022) resulted in a remarkable improvement in patient flow, as evident from the reduction in average hospital length of stay (from 11.5 to 4.4 days) and average emergency department boarding time (from 11.9 to 1.2 hours) and the improvement of bed turnover rate (from 0.57 to 0.93), (p<0.001, p=0.017, p=0.038, respectively), with net cost savings of 123 130 192 million Saudi Riyals (US$32 821 239).
Conclusion Implementing a well-structured case management programme can enhance care coordination, streamlilne transitions, boost patient outcomes, and increase revenues within hospital settings.
- Continuous quality improvement
- Efficiency, Organizational
- Patient satisfaction
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjoq-2023-002484
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Effective patient flow management within hospital settings plays a pivotal role in influencing the quality of care, staff workload and patient outcomes. This highlights the crucial need for structured and coordinated processes to elevate the overall experience and optimize the allocation of resources.
WHAT THIS STUDY ADDS
This work accentuates the vital significance of case management in enhancing patient flow, ultimately leading to improved healthcare outcomes, operational efficiency, and cost-effectiveness. Through streamlining patient care and optimizing transitions between healthcare services, it contributes to more effective and economic healthcare systems.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
This study emphasizes the importance of sustainable improvement strategies in optimizing patient flow within hospital settings. It highlights the effectiveness of tailored interventions in case management programmes, in improving coordination of care, patient outcomes, and financial performance. Customizing interventions to fit the unique needs of each organization is crucial for successful implementation and the advancement of healthcare delivery practices.
Introduction
Patient flow is a crucial element of process management in hospitals. It describes the movement of patients through the different stages of required hospital care and considers whether they are subject to unnecessary delay. 1 Optimising patient flow in hospitals ensures that patients receive the best available care while saving time, effort and costs. 1 Failing to achieve hospital-wide patient flow puts patients at risk for suboptimal care and potential harm, as well as increasing hospital staff burden. 2 Poor patient flow is especially apparent when incoming emergency department (ED) patients cannot be immediately admitted into the hospital due to a lack of available beds. 3 When the supply cannot match the demand, patients experience lower quality of care and worse health outcomes. 4 This paved the way for the integration of case management (CM) into healthcare. 4
CM is a healthcare process where a professional helps the patient and their family navigate through a complicated set of services available within an organisation and their community to meet their healthcare needs in a cost-effective and coordinated manner. 5 Knowledge of healthcare costs and resource utilisation has accustomed CM to challenge interventions with questionable effectiveness in the healthcare process. 6 Case managers are the leaders in patient flow management; through working collaboratively with and coordinating care from all hospital departments, the case manager can identify and correct barriers to patient flow as they occur. This unique role positively impacts the quality of care and operational efficiency of the healthcare system. 5 Yet, further studies are necessary to confirm the effectiveness of CM interventions.
Al Hada Armed Forces Hospital (Taif, Saudi Arabia) is a tertiary care hospital and one of nine Armed Forces hospitals in the Kingdom. With a capacity of 420 beds and 3000 staff, this acute facility provides extensive medical and nursing services, including open heart surgery and kidney transplants. 7 Care is required for an average of a thousand patients per day. The CM department (comprising CM, bed management and discharge coordination divisions) was established at Al Hada Armed Forces Hospital in 2016 and was recognised by the Ministry of Defence Health Services (MODHS) in December 2019. An in-depth evaluation of the hospital patient flow parameters revealed notable inefficiencies. Therefore, this initiative was started in September 2019 and aimed at enhancing patient flow in the hospital, that is, facilitating timely and efficient patient movement throughout the hospital, ultimately enhancing overall operational efficiency. The specific objective was to shed light on the role of CM practices in making the intervention plan workable and effective. The secondary aim of the endeavour was to estimate the financial return of the new interventions.
Project team
A core team of stakeholders was assembled as a central part of setting up the project. This team comprised the director of the CM department, a continuous quality improvement and patient safety (CQI & PS) coach, a case manager or bed coordinator, representatives from medical administration, human resources (HR), materials management and other allied departments, as well as a nursing representative and the most responsible physician.
The project was launched in September 2019 by the MODHS, which is one of the strategic priorities at Al Hada Armed Forces Hospital. The project team established biweekly meetings for devising interventions, orchestrating implementation updates, refining strategies and overcoming obstacles arising along the way. In addition, daily and weekly huddles with hospital stakeholders and departmental champions were commenced. All introduced measures were communicated through visual management reporting systems to all hospital units.
Process measures
Percentage of compliance with multidisciplinary team review on the eighth day, percentage of early discharge planning for complex patients, percentage of patients discharged from the hospital units before 12:00, percentage of patients with documented preliminary discharge orders the night before discharge, median time (in min) until discharge, percentage of patients admitted to hospital units before 10:00, percentage of delayed admission (lasting >45 min), waiting time (in days) for elective admission and bed turnover rate ( online supplemental table 1 ).
Supplemental material
Primary outcome measures.
Primary outcome measures include average hospital length of stay (LOS, in days), average ED boarding time (in hours) and patient experience (percentage) ( online supplemental table 1 ).
Balancing measures
Balancing measures include mortality rate, hospital-acquired infection (HAI) rate and rate of hospital readmission within 30 days ( online supplemental table 1 ).
Baseline data were available for the ED boarding time, the average LOS and the hospital readmission rate. Other measures were initiated at the start of the project ( online supplemental table 1 ). Data for this project were retrieved from the patient census, reports from the bed management division and the admission office and patient flow indicators from the CQI & PS department. Shadowing 8 was also used for collecting observational data. Patient experience data were collected quarterly via patient surveys throughout the intervention. The data were forwarded to Press Ganey, 9 a third-party company assigned by the MODHS to collect and analyse patient feedback. The reports provided by Press Ganey were used to assess and track changes in patient experience throughout the entire intervention period.
For estimating study measures, data were retrieved weekly from the hospital management information system (WIPRO) and submitted to the CQI & PS department for analysis. All data were initially validated by the CQI & PS department to ensure accuracy and reliability. Subsequently, 10% of our data (through random sampling) was independently validated by other reviewers. If the results exceeded 90%, the data were considered valid. Moreover, the MODHS arranged multiple visits to our hospital to ensure the validity and reliability of the data collection. Continuous monitoring and evaluation were performed throughout the duration of the project, according to which decisions were made either to adapt, adjust or discard the intervention.
Return on investment (ROI) estimation
Estimation of the ROI 10 was used to calculate the net financial gains throughout the project, taking into consideration all the resources invested and all the amounts gained through increased revenue, reduced cost or both. ROI is estimated as the ratio of two financial estimates of net financial returns from improvement action divided by the financial investment in the improvement project. When an ROI is ≥1, the returns generated by improvement actions are greater than or equal to the costs for development and implementation, representing a positive outcome. Conversely, an ROI <1 indicates a net loss from changes in quality and utilisation, reflecting a negative outcome. Cost savings are derived from the difference between returns and cost investment.
The improvement plan was introduced through a series of three Plan-Do-Check-Act (PDCA) cycles, each lasting from 3 to 9 months. The objectives of the three consecutive cycles were reducing patient LOS, reducing median discharge cycle time and reducing the median time for elective admission ( figure 1 ). Most departments of the hospital were involved in the intervention. The inpatient wards (a total of 293 beds) were addressed. The nursery and critical care units were excluded since they have different performance indicator parameters. One pilot unit was chosen every cycle to check the effectiveness of the interventions.
- Download figure
- Open in new tab
- Download powerpoint
Outline of the objectives and approaches of the study. IHI, Institute for Healthcare Improvement; LOS, length of stay; PDCA, Plan-Do-Check-Act.
In the planning phase, the team applied the Donabedian approach 11 to evaluate the structure, process and outcomes of healthcare quality and services ( online supplemental file 1 ). The recommendations of the Institute for Healthcare Improvement (IHI) 2 were adapted to improve patient flow across the hospital and modified throughout the intervention to best suit our hospital-specific situation.
First PDCA cycle
The first PDCA cycle started in September 2019. This cycle aimed at reducing the average hospital LOS through the implementation of actions that ensured that patient stays were needed or necessary according to clinical criteria for discharge and standardised LOS. The Male Medical I unit was selected as the pilot unit.
At the beginning of this cycle, the root causes for exceeding hospital LOS at Al Hada Armed Forces Hospital were identified. The top causes of prolonged stays were poor coordination of care, the unavailability of monitoring systems for LOS and the limited availability of the necessary supplies and equipment required before patient discharge.
Interventions applied during this cycle were influenced by the recommendations of the ‘Ensiab Project’. 12 The interventions included the SAFER 13 discharge bundle and the implementation of the RED to GREEN visual management system (based on the NHS RED and GREEN bed days). 14 Flow improvement multidisciplinary teams (MDTs) were reinforced, led by a case manager for each hospital unit and daily morning MDT huddles were commenced. The objectives of MDT huddles were to monitor admission and discharge, and patient status (eg, requires moving, downgrading and discharging) and to timely identify challenges arising along the process. The IHI hospital inpatient waste identification tool 15 was used to recognise waste along the process. The case manager also attended the morning patient round of the primary care team. This was an opportunity to communicate observed data, patient updates and emerging problems and to coordinate the required patient care (during hospital stay and after discharge). These data and problems were relayed to the project team for analysis.
The RED to GREEN visual management system increased the engagement of all medical staff in the project. Moreover, CM succeeded in establishing effective communication with stakeholders, which helped them understand the necessary changes and encouraged them to provide their input and to be actively engaged in the change process. This resulted in the gradual mitigation of the resistance of staff members towards the introduction of major changes to hospital processes.
To address patient transition following hospital discharge, the project team developed community/internal and external communication programmes to contact the necessary community services and healthcare facilities. These programmes covered other Armed Forces hospitals and Ministry of Health hospitals in the Taif Region, as well as home healthcare, rehabilitation and psychiatry facilities. Moreover, the need for a long-term care unit was highlighted by the project team and this has become a major strategic goal at Al Hada Armed Forces Hospital in the next 5 years.
Since standardised hospital LOSs for diagnosis-related groups (DRGs) for Al Hada Armed Forces Hospital were not available, the project requested benchmark LOSs for common diagnoses from each medical department. These standardised LOSs were created and integrated into the hospital management information system (WIPRO). This was an important step in the project that enabled the uploading of the patient data onto the system for monitoring and analysis. The hospital LOS was closely monitored. An ‘MDT Review for 7-day outliers’ form was dedicated to monitoring patients exceeding hospital LOS. Moreover, physicians had to document in Progress Notes or Physician Orders justifying the reason for keeping the patient in the hospital.
Many of the patients at Al Hada Armed Forces Hospital were geriatric with complex conditions and comorbidities, affecting the patient discharge process. These complex patient populations were managed through the efforts of case managers in coordinating patient care with social workers and other members of the interdisciplinary care team and involving family members in the process. Details of the intervention are displayed in table 1 .
- View inline
First PDCA cycle interventions aimed at reducing average hospital LOS
Second PDCA cycle
At the beginning of this cycle, there was an observable prolonged median discharge cycle time. Shadowing of a randomly selected discharge order showed that the time required for completing the discharge process was 225 min. This resulted in a bottleneck in hospital operations. Thus, the aim of this cycle was to reduce the mean discharge cycle time. The pilot unit during this cycle was the Orthopaedics Medical and Surgical unit.
Lean methodology was applied to test parameters involved in the discharge process and to evaluate the outcome of the interventions. Value stream mapping 16 was used to trace patient flow throughout the discharge process, and Single-Minute Exchange of Dies 17 was used to determine the activities negatively impacting the patient discharge process. Two main factors hindered the patient discharge process: remarkable variability in how the discharge process was carried out and the preparation of the discharge prescription. This was caused by the absence of a preliminary discharge order.
Steps for early planning of patient discharge were thus commenced, taking into consideration the criteria for medical readiness of discharge (medical and surgical cases) for Al Hada Armed Forces Hospital. A discharge coordinator participated in morning rounds to monitor and streamline the discharge process and to collect and report data. One of the main interventions in this cycle was to enforce the preparation or documentation of preliminary discharge orders the night before discharge. This provided time for informing patients and their relatives and for performing final activities (such as revising test results, nurse education, informing family members to arrange patient discharge or hospital transportation and completion of paperwork) to make timely discharge possible. The involvement of several departments (eg, physiotherapy, social workers and health educators) was mandatory during this phase.
Waste contributing to extended discharge cycle time was identified in waiting times (waiting for a physician to clear the patient for discharge and waiting for family members to fulfil patient discharge) and in unnecessary motion within the process (submission of prescriptions by nurses to the pharmacy department and acquisition of necessary medical supplies and devices by family members from the materials management department (MMD)). Several interventions were introduced. A paperless prescription system was implemented via the Hospital Management Information System (WIPRO), eliminating the need for nurses to physically submit prescriptions to the pharmacy department. This allowed for fast preparation and delivery of take-out medications. Additionally, acquiring supplies and medical equipment from the MMD became the responsibility of case managers upon requisition by the attending physician and was individually delivered to patients prior to discharge. To improve the early discharge of patients (before 12:00), case managers and discharge coordinators were involved in anticipating referrals to special facilities so that continuity of care could be guaranteed. Interventions are detailed in table 2 .
Second PDCA cycle interventions aimed at reducing discharge cycle time
During the COVID-19 pandemic, there were delays in the discharge process and prolongation of LOSs due to constant review of infectious disease protocols and re-swabbing for patient clearance and discharge. The CM department tackled this challenge by conducting a continuous review of the plan of care for each patient, providing care coordination to the responsible physician and following up and expediting laboratory test results.
Third PDCA cycle
The third PDCA cycle of the initiative commenced in September 2021, not immediately after the second cycle, due to the COVID-19 pandemic. Nevertheless, the interventions of the first and second cycles were sustained throughout the pandemic. The Male Surgical 1 unit was the pilot unit for this cycle.
At the beginning of this cycle, a prolonged median time for elective admission was observed (6 days). The main root causes of long admission times were a mismatch between demand and supply of inpatient beds, a lack of knowledge of non-medical staff regarding necessary medical terminology and diagnoses and a lack of awareness of patients regarding hospital preadmission requirements.
The main intervention was the establishment of a bed management division (following the CM department) to act as a centralised bed management authority that handles all admissions and transfers throughout the hospital. Moreover, the Admission Office, previously under the department of patient affairs, was transferred to the authority of the CM department, bringing both elective and emergency admissions under the purview of CM. Recruiting additional staff was necessary to support the new division. Internal hiring (ie, rehiring of existing staff) proved to be a cost-effective approach that also ensured staff retention.
Bed management monitored and analysed hospital-wide patient flow patterns to predict volume and seasonal variations. Furthermore, the IHI Be a Bed Ahead: ‘The Pull versus Push System’ 18 was implemented to address delays in patient movement between care points. In addition, daily morning bed management huddles were commenced, where bed managers monitored patient admissions and managed bed capacity and demand issues with the care team in real time.
Education of non-medical staff pertaining to medical terminology and hospital patient flow processes was necessary to improve the admission process time yet proved to be challenging. Nevertheless, the project team hired an admission office manager with a background in nursing and experience in CM or bed management, making the education programme possible. In addition, several interventions were implemented to improve patient and family member awareness of preadmission requirements. Details of the interventions of the third PDCA cycle are detailed in table 3 .
Third PDCA cycle interventions aimed at reducing median time to elective admission
This project comprised three overlapping cycles of interventions starting in September 2019 through September 2022. The aim of the first PDCA cycle was to reduce the average hospital LOS. Regarding process measures used to evaluate these cycle interventions, the percentage of compliance with MDT review on the eighth day fluctuated throughout the first 12 months of the intervention, with the value exceeding the expected target beginning in April 2020. A 100% compliance was achieved in September 2020, and this compliance was sustained until the end of the project (p=0.009) ( figure 2A , table 4 ). The percentage of early discharge planning for complex patients increased from a baseline of 0% at the beginning of the intervention to 100% in February 2020 and sustained at 100% until the end of the project; nevertheless, the change was not significant ( figure 2B , table 4 ).
Process measures. (A) MDT compliance on the eighth day (%). (B) Early initiation of discharge planning for complex cases (%). (C) Patients discharged from the hospital units before 12:00 (%). (D) Patients with documented preliminary discharge orders the night before discharge (%). (E) Median time (in minutes) until discharge from an inpatient setting. (F) Waiting time (in days) for elective admission. (G) Delayed admission (lasting >45 min) (%). (H) Patients admitted to hospital units before 10:00 (%). (I) Bed turnover rate. Ave., average; BTR, bed turnover rate; MDT, multidisciplinary team.
Project measures, baseline versus postintervention
The second PDCA cycle was aimed at reducing discharge cycle time. To examine the impact of interventions, the following process measures were evaluated: percentage of patients discharged from the hospital units before 12:00, percentage of patients with documented preliminary discharge orders the night before discharge and median time until discharge. The baseline percentage of patients discharged before 12:00 was 20%. This measure rapidly increased, exceeding the expected target and reaching 63% in February 2020. It then plummeted between April 2020 and September 2020 due to the difficulty of attaining the interventions during the COVID-19 pandemic. The measure then gradually improved, from 30% in May 2019, exceeding the expected target in August 2020 (60%), and reaching 66% at the end of the initiative (p=0.001) ( figure 2C , table 4 ). The percentage of patients with documented preliminary discharge orders the night before discharge started at a baseline of 32% and steadily increased to achieve the expected target in July 2020, and reaching 85% at the end of the initiative (p=0.001) ( figure 2D , table 4 ). The baseline median time until discharge was estimated at 212 min in October 2019. This was rapidly decreased to 62.3 min in January 2020. The decrease was sustained until the end of the initiative, reaching 63 min at the end of the intervention. Yet, this 71% improvement was not statistically significant ( figure 2E , table 4 ).
During the third PDCA cycle, reducing the median waiting time for elective admission was the main target of the interventions. Process measures examined for this cycle included waiting time for elective admission, the percentage of delayed admissions (lasting >45 min) and the percentage of patients admitted to hospital units before 10:00. The baseline measure of waiting time for elective admission was 6 days in September 2021. The median values fluctuated thereafter, showing increases and decreases still below the expected target level. By the end of the initiative, the median time was reduced by 50% (3 days in September 2022); nevertheless, the change was not statistically significant ( figure 2F , table 4 ). Median delayed admission was estimated at 10% at baseline (September 2021). The measure gradually decreased, reaching 3% at the end of the initiative (p<0.001) ( figure 2G , table 4 ). The percentage of patients admitted to hospital units before 10:00 started at a baseline value of 19% (September 2021). This measure gradually increased to 92% at the end of the initiative (p<0.001) ( figure 2H , table 4 ).
Bed turnover rate, the process measure influenced by all project interventions, was initially estimated at 0.57 in September 2019. This gradually increased to 0.98 in February 2020, after which there was a rapid drop continuing until April 2020 due to the failure to sustain the interventions during the COVID-19 pandemic. The measure then gradually increased to 0.96 in October 2020, after which the increase was sustained, reaching 0.93 at the end of the initiative (p=0.038) ( figure 2I , table 4 ).
The outcome measures of this project were the average hospital LOS, the average ED boarding time, and patient experience. The baseline average hospital LOS was 11.5 in January 2019. The measure fluctuated remarkably until July 2020 (reaching 6.2), after which the measure was gradually reduced to 4.4 days at the end of the intervention (p<0.001) ( figure 3A , table 4 ). The baseline average ED boarding time was 11.9 hours in January 2019. This rapidly dropped until July 2019, after which the reduction was sustained, reaching 1.2 hours at the end of the intervention (p=0.017) ( figure 3B , table 4 ). Regarding patient experience, the domains of inpatient admission and discharge were specifically targeted. There was a gradual and sustainable improvement in patient experience of the admission process from a baseline of 85.1% in 2019 to 86.1% in 2022. Satisfaction with the discharge process increased from 83.5% at baseline in 2019 to 87.9% in 2022 ( figure 3E , table 4 ).
Outcome and balance measures (A) ALOS (in days). (B) ED boarding time (in min). (C) Rate of hospital readmission within 30 days. (D) Correlation of hospital LOS with mortality HAI rates. (E) Patient experience in the inpatient admission and discharge domains. Ave., average; ALOS, average length of stay; ED, emergency department; HAI, hospital-acquired infection; Q3, Quarter 3.
The balancing measures of the project were the hospital readmission rate within 30 days, the hospital mortality rate and the HAI rate. The hospital readmission rate was estimated at baseline in September 2019 (7.5%). This rapidly dropped to 1.2% in June 2020. The measure then gradually decreased to 0% in December 2021, with this value sustained to the end of the initiative. Nevertheless, this change was not statistically significant ( figure 3C , table 4 ). Regarding mortality, the baseline measurement in the fourth quarter of 2019 was 2.5%, which increased to 4.5% in the first quarter of 2020. This was followed by a steady decrease to 2.5% at the end of the intervention, which was not correlated with hospital LOS. On the other hand, the HAI rate started at 1.8% at baseline in the fourth quarter of 2019. This declined in the first quarter of 2020, reaching 0.8%, followed by a rise to 2.3% in the second quarter of 2020. The HAI rate steadily decreased thereafter, reaching 1.3% at the end of the initiative, being correlated with hospital LOS (p=0.037) ( figure 3D , table 4 ).
ROI estimation
ROI 10 was estimated to determine the economic impact of the intervention. ROI was calculated as the ratio of two financial estimates of net financial returns from improvement action (cost reduction due to reducing hospital LOS) divided by the financial investment in the improvement project (internal hiring of staff for the bed management division). Cost savings were derived from the difference between returns (cost reduction resulting from reducing hospital LOS) and cost investment (internal hiring of staff for the bed management division).
The reduction of hospital LOS at Al Hada Armed Forces Hospital resulted in net financial returns of 128 032 692 Saudi Riyals (SAR) ( table 5 ), while the financial investment in the improvement action was estimated at 4 902 500 SAR ( table 6 ). The net cost savings (ie, net financial returns−financial investment) were estimated at 123 130 192 SAR (US$32 821 239). Therefore, the ROI was estimated at 26.11.
Net financial returns due to the improvement plan
Financial investment in the improvement action
The Saudi population has grown exponentially in the last 20 years, leading to an increase in healthcare expenditure estimated at US$2.4 billion per year. 19 Like most countries around the globe, Saudi Arabia experiences challenges in providing cost-effective healthcare services while ensuring the quality of care in its public facilities. Healthcare transformation is a central goal of Saudi Arabia’s Vision 2030 . 20 Saudi Arabia has opted to restructure its healthcare system through privatising public hospitals, a globally implemented solution for overcoming the financial burden of inefficient and unsatisfactory healthcare systems. 21 Yet Vision 2030 sets the path for using innovation to enhance operational efficiency and financial sustainability in healthcare. 20 Thus, the adoption of innovative CM approaches aligns with and contributes to Saudi’s Vision 2030 .
The goal of this project was to streamline patient care, focusing on the role of CM as the main drive for the change package. The initiative started in September 2019 and was concluded in September 2022. The interventions were implemented via three overlapping PDCA cycles. All project measures (process, balancing and outcome) were continuously monitored. Hospital LOS has been established as a measure of the efficiency of healthcare. 22 Unnecessarily long hospital stays are associated with poor patient outcomes, including hospital-acquired infections and increased mortality, 23 as well as increased costs and negative patient experiences. 24 Long patient LOSs reduce the operational efficiency of healthcare systems, burden the staff and increase the cost of unnecessary bed occupancy 24 and the economic impact of adverse events. 25 26 We used average hospital LOS as the major outcome measure of this initiative. The average hospital LOS for all causes across the Organisation for Economic Cooperation and Development countries was about 8 days. Turkey and Mexico had the shortest stays (about 4 days), whereas Japan and Korea had the longest stays (over 16 days). 27
In the first PDCA cycle, CM focused on the coordination of patient care among all involved parties. One approach used in this project was enforcing the role of MDTs. MDTs make interprofessional education and collaboration possible. 28 29 This collaboration allowed for problem-solving and decision-making in real-time. Moreover, the CM introduced measures to overcome the delayed transition of patients to other care or community settings, a well-known problem in healthcare that delays patient discharge and unnecessarily prolongs LOS. 30 This was achieved by identifying patients with complex social and medical needs upon admission and by developing communication programmes addressing target care and community services. Proper transition of care has been shown to reduce hospital readmissions, 31 which is in line with the reduction of the hospital readmission rate in our study.
Discharge planning is currently an important element in managing healthcare systems. Several authors have declared morning hours unsuitable for preparing the preliminary discharge order and this should ideally occur the day before discharge, when the patient has been tentatively identified as ready to leave. 32 33 The planning of the discharge process was successfully tackled in the second PDCA cycle using several interventions. Discharge planning has been shown to be effective in reducing hospital LOSs, 34 35 which is in line with our results.
Bed management was addressed in the third PDCA cycle. CM created a central bed management authority, moving all relevant hospital sections under its umbrella. This made the orchestration of all hospital admissions and transfers possible, with the aim of monitoring hospital beds and providing empty beds for elective and emergency admissions, to match demand and capacity. This resulted in a successful reduction of waiting times for elective admissions and the ED boarding time and increased hospital operational efficiency. The role of bed management in improving patient flow and hospital operational efficiency has been confirmed in several studies. 36 37
The project team used internal hiring to recruit staff for the newly developed Bed Management Division. The advantages of internal hiring are multidimensional; short recruitment process, reduced recruitment costs, no need for advertising, and the fact that internal recruits are already familiar with the organisation’s culture and processes. 38 In addition to achieving staff retention, this proved to be a rapid solution, which resulted in 315 000 SAR in estimated cost savings that would have otherwise been incurred in the external hiring of non-Saudi staff.
Being a tertiary care facility, Al Hada Armed Forces Hospital is the destination of complex patients with comorbidities requiring special diagnostics and treatment plans. CM and MDT approaches are the most common interventions used to address complexity in hospital settings, where complex patients are identified and engaged to prevent worsening health and improve health outcomes and patient satisfaction. 29
Patients engaged in their own healthcare are believed to have better health outcomes and to be more satisfied with the service. 39 40 But this is hard to achieve in an inpatient setting. 39 Nevertheless, involving patients and their family members in discharge and admission planning (in the first and third PDCA cycles, respectively) proved to be an integral factor in the success of the improvement.
The importance of data-driven approaches for improving healthcare has been recently highlighted in the literature. 30 From the beginning of the project, CM integrated data-driven approaches into its process. This facilitated data analysis, collaboration of care and decision-making, making the study interventions successful. This is in line with the results of several studies using data-driven approaches in comparable settings. 30 32
Patient experience serves as a crucial outcome measure for assessing the effectiveness of hospital-wide patient flow improvements. 41 This study followed patient satisfaction with admission and discharge processes, which has shown a steady increase over the period of the intervention.
Reducing average hospital LOS has been found to reduce mortality rates. 42 However, this could not be demonstrated in our study. This could be explained by the complexity of the patient population at Al Hada Armed Forces Hospital. Moreover, increased mortality rates due to the COVID-19 pandemic further affected our findings. On the other hand, hospital LOS had a positive impact on the HAI rate in our study. This is consistent with the findings of various studies. 43 44
The net cost savings of the initiative amounted to 123 million SAR over the 3 years of the project. The financial revenue generated by the project was exceptional, with an ROI of 26. According to the Agency for Healthcare Research and Quality, 10 an ROI of 26 indicates that for every 1 SAR invested in the initiative, the hospital gained 26 SAR. This is in accordance with recent studies that have shown that managing patient flows through CM is not only beneficial to the patient but is also beneficial to the organisation. 32 34 The literature is divided on the cost-effectiveness of CM, 45 which is probably explained by the wide variability of CM approaches. Nevertheless, our interventions proved to be cost-effective in our hospital setting.
Lessons learnt
The changes implemented in this project—the utilisation of case managers, bed managers, discharge coordinators and admission officers, coupled with modification of hospital-related processes and a patient or family-centred care approach have resulted in significant improvements in patient flow and a reduction in unnecessary hospital stays, with favourable financial outcomes. This model embodies the potential for sustainability and exportability.
The sustainability of these improvements relies on continuous implementation and refining of the roles and processes involved. This requires effective communication among the supervising body, including regular huddles, to timely identify and address challenges arising during the process. Ongoing training programmes and heightened awareness among healthcare professionals can help maintain the momentum and ensure long-term success in patient flow enhancements. The changes involved in this project can also be exportable. Establishing dedicated CM departments in each military hospital in Saudi Arabia can further solidify these changes and provide a framework for future improvements. Interinstitutional communication is necessary to discuss the specific strategies for transfer and the sustainability of the interventions. Additionally, highlighting positive financial impact and patient benefit can emphasise the value of these interventions and their potential replication in other healthcare settings.
In summary, the lessons learnt from this project underscore the importance of prioritising patient safety, optimising efficiency, improving accessibility and implementing sustainable solutions. By incorporating these lessons into future initiatives, healthcare organisations can strive for continuous improvement in patient care and operational efficiency.
Limitations
The first PDCA cycle of our initiative coincided with two ongoing projects, NO WAIT 46 and the patient flow optimisation project 47 of the CM department. Therefore, it is challenging to quantify the extent of change solely attributable to the interventions of this initiative. Assessing the impact of the intervention on hospital staff and their satisfaction with the change would have been a valuable addition to the work, but this was not addressed in the study. Additionally, we acknowledge the limited scope of the patient experience domain in this study, which focused on the inpatient domain encompassing admission and discharge processes. While these aspects are crucial for patient satisfaction and overall experience, other important domains of patient experience were not addressed. Further research and study should explore all satisfaction domains of the patient journey related to hospital LOS, such as communication with healthcare providers, involvement in treatment decisions, pain management, and overall care coordination.
It is important to note that although the findings of this study align with previous research, the context of each healthcare organisation may vary, and the specific interventions implemented may differ. Therefore, it is essential to consider the unique characteristics and needs of each organisation when designing and implementing CM interventions.
This project demonstrates that CM can improve patient flow in a hospital setting through the roles of case managers, bed managers, discharge coordinators and admission officers and through modifying hospital-related processes (admission/discharge planning, MDT huddles and others), with a positive financial impact due to a reduction of the costs of unnecessary inpatient stays. This project also demonstrates that a sustainable solution, rather than a short-term intervention, can be successfully implemented. The current intervention can serve as a reference point for future improvement projects dealing with patient flow in hospitals and how it contributes to quality improvement and patient benefit.
Due to the remarkable results of this improvement project, it was recommended that this set of interventions be disseminated to the MODHS and its satellites. The project team has begun professional training programmes across hospitals in the MODHS with the objectives of creating awareness about patient flow, teaching methods of improving patient flow and setting the groundwork for establishing CM departments in each hospital.
While challenges and limitations were encountered, the study has provided valuable insights into the complexities of optimising patient flow in a hospital setting. By addressing these challenges and building upon the successes of this project, hospitals can continue to improve patient care, resource utilisation, and overall operational efficiency. This research contributes to the body of knowledge on patient flow optimisation and provides a framework for future studies and implementations in other healthcare settings.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
Acknowledgments.
We would like to express our sincere thanks to our leader Dr. Ahmed Mohammed Al Amri, the CEO of the Health Services Directorate of Saudi Arabia, for his unlimited support and guidance in improving patient flow in our healthcare system. We like to extend our gratitude to Dr. Noura Alnowaiser, Executive Healthcare Quality Director, and Col. Dr. Yasser Alotaibi, Deputy Director of Quality improvement and Patient Safety at the Ministry of Defence Health Division, for guiding and supporting us in achieving our goals along this journey. Special thanks to Dr. Alia Ellawindy for her invaluable guidance and expertise throughout the study and publication. Finally, we would like to convey our heartfelt thanks to all medical and non-medical staff who helped make this whole process a great success.
- NEJM Catalyst
- Rutherford PA ,
- Anderson A ,
- Kotagal UR , et al
- Rojas-García A ,
- Pizzo E , et al
- Giardino AP ,
- Proudlove N ,
- Jorgensen J
- Daniels S ,
- ↵ PressGaney [ Internet ]. n.d. Available : https://www.pressganey.com/
- Panteli D ,
- Quentin W ,
- Busse R , et al
- Alotaibi Y ,
- Alnowaiser N ,
- NHS improvement
- Wilson C , et al
- Griffin FA ,
- Kabcenell A , et al
- Marin-Garcia JA ,
- Vidal-Carreras PI ,
- Garcia-Sabater JJ
- Bin Che Ani MN ,
- Bin Shafei MSS
- ↵ Optimizing patient flow: moving patients smoothly through acute care settings. IHI innovation series white paper . Boston: Institute for Healthcare Improvement ; 2003 . Available : www.IHI.org
- Alasiri AA ,
- AlMubarak SH ,
- Alfayez AS ,
- Alanazi AT , et al
- Marshall A ,
- Vasilakis C ,
- Marfil-Garza BA ,
- Belaunzarán-Zamudio PF ,
- Gulias-Herrero A , et al
- Mull NK , et al
- Hoogervorst-Schilp J ,
- Langelaan M ,
- Spreeuwenberg P , et al
- Tang YF , et al
- Chassiakos YR ,
- Micallef A ,
- Buttigieg SC ,
- Tomaselli G , et al
- Kripalani S ,
- Theobald CN ,
- Anctil B , et al
- McDermott CM ,
- Venditti FJ
- Warren DS ,
- Stewart SL , et al
- Siddique SM ,
- Leas B , et al
- Proudlove NC ,
- Manning L ,
- Woollen J ,
- Wilcox L , et al
- Marzban S ,
- Agolli A , et al
- Lingsma HF ,
- Middleton S , et al
- Tuckman HP ,
- Patrick RH , et al
- Stewart S ,
- Robertson C ,
- Pan J , et al
- Klaehn AK ,
- Jaschke J ,
- Freigang F , et al
- Elkholi A ,
- Althobiti H ,
- Al Nofeye J , et al
- Alharbi S ,
- Alasmari A ,
- Hanafy E , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Contributors SAH is the main author and project team leader, guarantor of this work, accepts full responsibility for the work and/or conduct of the study, had access to the data and controlled the decision to publish. BA provided the ultimate leadership support for carrying out this study. LE research the cause of process variation, was involved in the selection and using the process improvement tools and aided in the analysis and interpretation of the results. FLB developed the research idea, was involved in designing the intervention along with the case management department and CQI & PS specialist. All authors discussed the results and prepared the manuscript.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- Open access
- Published: 22 April 2024
Respiratory drive: a journey from health to disease
- Dimitrios Georgopoulos ORCID: orcid.org/0000-0003-3689-9014 1 ,
- Maria Bolaki 2 ,
- Vaia Stamatopoulou 3 &
- Evangelia Akoumianaki 1 , 2
Journal of Intensive Care volume 12 , Article number: 15 ( 2024 ) Cite this article
1518 Accesses
1 Altmetric
Metrics details
Respiratory drive is defined as the intensity of respiratory centers output during the breath and is primarily affected by cortical and chemical feedback mechanisms. During the involuntary act of breathing, chemical feedback, primarily mediated through CO 2 , is the main determinant of respiratory drive. Respiratory drive travels through neural pathways to respiratory muscles, which execute the breathing process and generate inspiratory flow (inspiratory flow-generation pathway). In a healthy state, inspiratory flow-generation pathway is intact, and thus respiratory drive is satisfied by the rate of volume increase, expressed by mean inspiratory flow, which in turn determines tidal volume. In this review, we will explain the pathophysiology of altered respiratory drive by analyzing the respiratory centers response to arterial partial pressure of CO 2 (PaCO 2 ) changes. Both high and low respiratory drive have been associated with several adverse effects in critically ill patients. Hence, it is crucial to understand what alters the respiratory drive. Changes in respiratory drive can be explained by simultaneously considering the (1) ventilatory demands, as dictated by respiratory centers activity to CO 2 (brain curve); (2) actual ventilatory response to CO 2 (ventilation curve); and (3) metabolic hyperbola. During critical illness, multiple mechanisms affect the brain and ventilation curves, as well as metabolic hyperbola, leading to considerable alterations in respiratory drive. In critically ill patients the inspiratory flow-generation pathway is invariably compromised at various levels. Consequently, mean inspiratory flow and tidal volume do not correspond to respiratory drive, and at a given PaCO 2 , the actual ventilation is less than ventilatory demands, creating a dissociation between brain and ventilation curves. Since the metabolic hyperbola is one of the two variables that determine PaCO 2 (the other being the ventilation curve), its upward or downward movements increase or decrease respiratory drive, respectively. Mechanical ventilation indirectly influences respiratory drive by modifying PaCO 2 levels through alterations in various parameters of the ventilation curve and metabolic hyperbola. Understanding the diverse factors that modulate respiratory drive at the bedside could enhance clinical assessment and the management of both the patient and the ventilator.
Respiratory drive, defined as the output of respiratory centers to respiratory muscles, is crucial in the management of critically ill patients. Recent data indicate that in these patients, both high and low respiratory drive may adversely affect patient outcomes through multiple pathways [ 1 , 2 , 3 , 4 , 5 ]. While the definition of respiratory drive may appear simple, without understanding its determinants and underlying pathophysiology, the term 'respiratory drive' often remains ambiguous. It is imperative to understand that in critically ill patients, ventilatory demands, as reflected by respiratory centers output (RCO) per minute (RCO/min), may deviate from actual minute ventilation (V’ E ) due to various reasons [ 2 , 6 ]. Failure to consider this dissociation could hinder the recognition and management of high or low respiratory drive in critically ill patients. In this review, we aim to analyze the different aspects of respiratory drive to facilitate comprehension of the causes of high and low respiratory drive in spontaneously breathing or mechanically ventilated critically ill patients.
Basic principles of control of breathing
Components of control of breathing system
The control of breathing system consists of three parts, a central control system in the brain (central mechanisms), a motor arm (effector) which executes the act of breathing, and a host of sensory mechanisms that convey information to the central controller (feedback mechanisms) [ 7 , 8 , 9 , 10 ].
For simplicity, the central controller can be considered as comprising two groups of neurons [ 7 , 8 , 9 , 10 ]: the brainstem group and the cerebral cortex group. The former, oversees the automatic (involuntary) aspect of breathing, and is divided into pneumotaxic, apneustic, and medullary centers. Each center includes a diverse group of neurons with specific roles in the breathing process. The cerebral cortex group is responsible both for voluntary (behavioral) and involuntary regulation of breathing.
The effector system consists of the pathways that transfer stimuli from the respiratory centers to neurons and thereafter to the respiratory muscles [ 2 , 6 ]. The respiratory muscles involve the diaphragm, the main inspiratory muscle, as well as other inspiratory and expiratory muscles. Expiratory phase is usually passive at rest but may become active, characterized by expiratory muscles contraction, when high ventilatory demands exist [ 11 ]. Expiratory muscle contraction is common in critically ill patients [ 12 ].
The main feedback mechanisms of the control of breathing are: (1) chemical, (2) reflex, (3) mechanical, (4) metabolic rate, and (5) cortical [ 13 ]. Involuntary breathing is primarily regulated by chemical feedback and, to a much lesser extent, reflex feedback. Mechanical feedback, which involves changes in respiratory muscle pressure with volume (force–length) and flow (force–velocity) [ 14 ], is not relevant in critically ill patients since volume and flow are relatively small. Although the metabolic rate plays a key role in modulating the respiratory drive during exercise by linking CO 2 production and elimination, in critically ill patients metabolic rate affects respiratory centers indirectly via alteration in metabolic hyperbola [ 2 , 6 ]. Finally, the effects of cortical feedback are rather unpredictable, depending on the Intensive Care Unit (ICU) environment and patient factors (i.e., delirium). Furthermore, areas of the cortex (i.e., pre-inspiratory motor area) may be activated under certain circumstances for purposes that are largely unexplored [ 15 ].
2. Automatic act of breathing
The automatic act of breathing entails the rhythmic activation of inspiratory and under certain circumstances expiratory muscles, via electrical bursts (outputs) from respiratory centers located in the medulla oblongata [ 9 ]. During this act of breathing the respiratory center receives inputs from various sources (mainly chemical and reflex feedback) that, through a complicated process, are translated into an output with an oscillatory pattern (Fig. 1 ). This output regulates the whole respiratory cycle which can functionally be divided into three phases: inspiratory, post-inspiratory, and expiratory. The duration of these three phases, although not always discrete, determines the timing of the breath and consequently the respiratory rate, whereas the intensity of the output is referred to as “respiratory drive”. The system employs “gating” to modulate the inputs, which means that the same tonic input may have a different effect on the respiratory centers, depending on the phase of the respiratory cycle [ 16 ]. Notably the neurons that control the breath timing (gate function) are different than these that control respiratory drive [ 17 , 18 , 19 ]. Cortical influences may interrupt this automatic process at any level [ 20 , 21 ].
3. Chemical–reflex feedback mechanisms
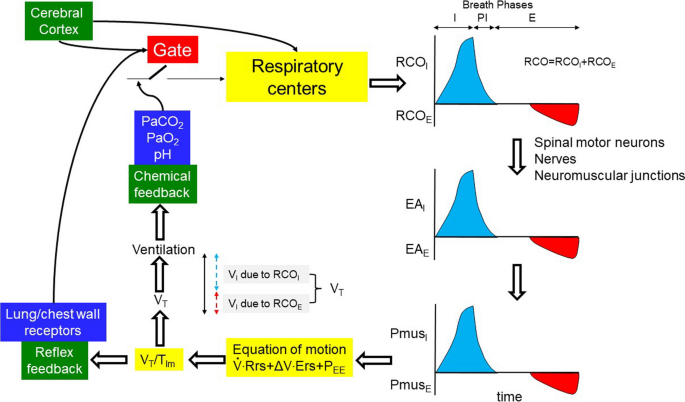
The inspiratory flow-generation pathway and the feedback mechanisms affecting it, in a normal subject during passive (no expiratory muscles activity) and active (expiratory muscles activity) expiration. For simplicity and demonstration purpose, RCO I always begins when expiratory muscles activity ceases. Assuming that Pmus E is able to lower lung volume below FRC (negative P EE ), rapid relaxation of expiratory muscles (rapid decrease in Pmus E ) passively generates inspiratory flow. When Pmus E decreases to zero, FRC is reached. At this point Pmus I increases and actively generates inspiratory flow. Notice, compared to passive expiration, the higher V T with active expiration, which corresponds to higher RCO during the whole breath (respiratory drive). Gate: the effects of afferent signals (inputs) on respiratory centers vary, depending on the breath phases (inspiratory, post-inspiratory, expiratory); RCO: total respiratory centers output during the breath (respiratory drive); RCO I , RCO E : respiratory centers output to inspiratory and expiratory muscles, respectively; EA I , EA E : electrical activity of inspiratory and expiratory muscles, respectively; Pmus I , Pmus E : pressure generated by inspiratory and expiratory muscles, respectively; P EE : elastic recoil pressure of respiratory system at end-expiration (zero at FRC, and positive and negative at volume above and below FRC, respectively); Ers: respiratory system elastance; Rrs: respiratory system resistance; ΔV: volume above end-expiratory lung volume; V T : tidal volume; V I : inspired volume; blue areas: RCO I , EA I and Pmus I ; red areas: RCO E , EA E and Pmus E ; I, PI, E: inspiratory, post-inspiratory and expiratory phases, respectively; black double edges vertical arrow: V T ; blue and red dashed double edges vertical arrows: contribution of inspiratory and expiratory muscle activity to V T
Chemical feedback consists of the response of the respiratory centers to changes in arterial blood gases (PaO 2 , PaCO 2 ) and pH [ 22 ]. PaCO 2 is by far the strongest stimulus, acting on the respiratory centers either directly or indirectly, through the others [ 22 ]. A wide range of chemical feedback changes modify the respiratory drive, while the respiratory rate increases when the drive increases several folds above that of resting breathing [ 1 , 23 , 24 , 25 ]. Reflex feedback, at least in adults, is much weaker and affects mainly the duration of the inspiratory and expiratory phases of the breath (i.e., Hering–Breuer reflex) [ 25 , 26 , 27 , 28 ].
4. Response to chemical stimuli
We will particularly focus on the response to PaCO 2 and PaO 2 . The normal response to hypercapnia involves a linear increase of V’ E as PaCO 2 increases. The slope of this increase varies widely in healthy individuals, with an average value of 2–3 l/min/mmHg and a range of 0.6–8 l/min/mmHg [ 23 , 29 , 30 ]. The slope increases when there is hypoxemia or metabolic acidosis and decreases during sleep, sedation or metabolic alkalosis [ 22 , 23 , 31 ]. The hypocapnic response depends on the state of sleep and wakefulness. During wakefulness, the V’ E –PaCO 2 relationship continues to be linear as PaCO 2 decreases. Nevertheless, the slope decreases rather abruptly, approaching zero at a certain PaCO 2 level (dog-leg). This means that a minimum amount of V’ E (wakefulness drive to breath) is maintained at PaCO 2 values well below this level [ 22 ]. During sleep or sedation, the PaCO 2 to V’ E relationship remains linear until PaCO 2 reaches a certain level where V’ E abruptly decreases to zero, resulting in apnea [ 32 , 33 ] (Fig. 2 ).
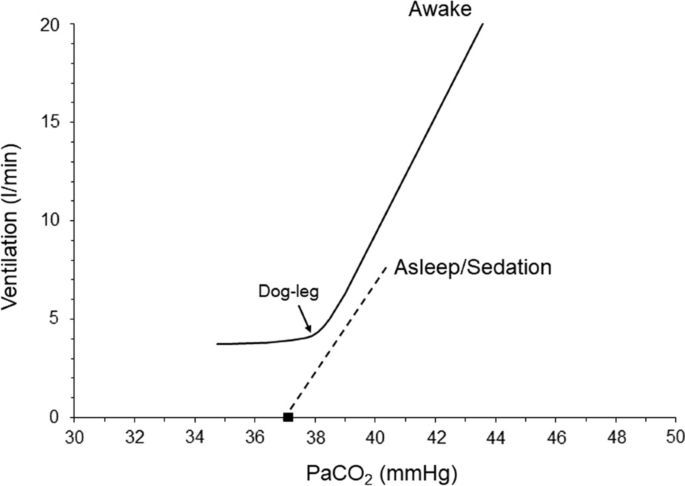
Ventilatory response to CO 2 in a healthy individual. Notice the difference between the ventilatory response during wakefulness and sleep/sedation. Black square indicates the apneic threshold
Hypoxemia increases V’ E , an effect that is modified by the PaCO 2 and acid–base status [ 22 , 23 , 30 ]. Acute progressive isocapnic hypoxemia increases V’ E in a hyperbolic manner; V’ E remains almost unchanged as PaO 2 drops to ≈ 60 mmHg, but at lower PaO 2 , it increases progressively with hypoxemia [ 34 ]. Although PaO 2 is a weaker modulator of respiratory centers output (RCO) than PaCO 2 , it may significantly affect RCO and thus V’ E by modifying the response to PaCO 2 [ 22 , 23 , 30 ].
Respiratory drive and inspiratory flow-generation pathway
Respiratory centers output to inspiratory muscles travels from the brainstem and upper cervical spine neurons to the nuclei of inspiratory motoneurons (C3–C5 for the diaphragm) and determines the rate of phrenic nerve activity increase, which in turn, determines the rate of diaphragmatic muscle pressure increase. The latter determines the rate of volume increase and thus, depending on the respiratory rate, V’ E (Fig. 1 ) [ 2 , 6 ]. At high ventilatory demands, the contraction of accessory inspiratory muscles supplements diaphragmatic pressure, further increasing the rate of volume expansion. Moreover, in this situation, the respiratory centers may stimulate expiratory muscle contraction. This could reduce the end-expiratory lung volume below functional residual capacity (FRC) [ 11 ]. Subsequent relaxation of expiratory muscles will generate inspiratory flow and contribute to final V T [ 12 ]. Since the aim of expiratory muscle stimulation is to aid in V T and alleviate the workload of inspiratory muscles [ 11 ], the term 'respiratory drive’ is defined as the total RCO to both inspiratory (RCO I ) and expiratory (RCO E ) muscles [ 6 ] (Fig. 1 ). The whole process described in a simplified manner, is collectively termed the ‘inspiratory flow-generation pathway’ [ 2 ].
When the inspiratory flow-generation pathway is intact, the resultant mean inspiratory flow, defined as the ratio between V T and mechanical inflation time (T Im ), aligns with that desired by the respiratory drive (RCO). In other words, the RCO per breath, corresponds to V T and RCO/min to actual V’ E . However, if there is any compromise in the integrity of the inspiratory flow-generation pathway, a dissociation occurs between the respiratory drive and the V T /T Im [ 35 ]. Consequently, a given respiratory drive yields a smaller V T /T Im and, all else being equal, lower V’ E (Fig. 1 and Additional file 1 : Figs. S2 and S3). Although during the involuntary breathing the main determinant of respiratory drive is chemical feedback [ 2 , 6 ], cortical inputs can highly affect respiratory drive when there is voluntary activity (pain, stress) [ 36 ]. However, at rest in the absence of voluntary activity, the cerebral cortex has an inhibitory influence on the respiratory center [ 37 , 38 ]. This explains why patients with cortical lesions may exhibit high respiratory drive.
Since PaCO 2 is the most important controller of the respiratory drive [ 2 ], it is important to briefly discuss what determines its value. At resting steady-state ventilation, PaCO 2 is the point where the metabolic hyperbola intersects with the ventilatory response to CO 2 curve [ 2 , 29 , 39 ]. The metabolic hyperbola graphically represents PaCO 2 as a function of V’ E , rate of CO 2 production (V’CO 2 ) and physiological dead space (V D ) to V T ratio as follows:
where k is constant (0.863) [ 39 ]. The ventilatory response to CO 2 curve describes V’ E as a function of PaCO 2 and depends on the (1) response of respiratory centers to CO 2 and (2) integrity of inspiratory flow-generation pathway [ 2 ].
Brain and ventilation curves
To elucidate the impact of defects in the inspiratory flow-generation pathway on respiratory drive, we have recently introduced the concepts of brain and ventilation curves [ 2 ]. The brain curve is a theoretical representation, outlining the desired V’ E set by the respiratory centers at a given PaCO 2 . In simpler terms, the brain curve is determined exclusively by the respiratory centers’ sensitivity to PaCO 2 , which is controlled by afferent information from peripheral and central chemoreceptors. The term 'ventilation curve' describes the actual V’ E produced by a given RCO/min. Unlike the brain curve, the ventilation curve is influenced not only by the respiratory centers’ sensitivity to PaCO 2 , but also by the integrity of the inspiratory flow-generation pathway (Fig. 1 and Additional file 1 : Figs. S1, S2 and S3). As discussed above, the brain curve is mainly determined by respiratory drive over a wide range of PaCO 2 [ 1 ].
When the inspiratory flow-generation pathway is intact, the brain and ventilation curves are identical. However, if the integrity of the pathway is compromised, the ventilation curve deviates (is shifted down and to the right) from the brain curve (Fig. 3 ). As a result, the metabolic hyperbola and ventilation curve intersect at a higher level of PaCO 2 than that desired by the brain (the PaCO 2 that would result from the intersection of the brain curve and metabolic hyperbola) [ 2 , 6 ]. Elevated PaCO 2 stimulates the respiratory centers, prompting an increase primarily in their output per breath (RCO, respiratory drive) and, to a lesser extent, in respiratory rate [ 1 ]. Consequently, factors that modify the positioning and inclination of the ventilation curve, the brain curve, and/or the metabolic hyperbola influence the respiratory drive [ 2 , 6 ].
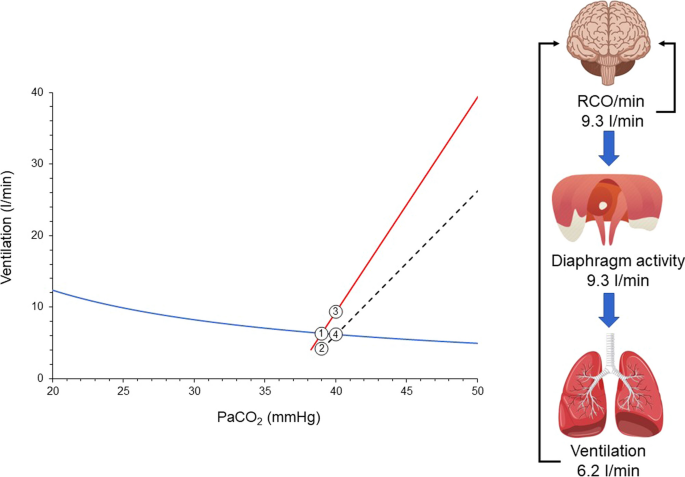
Brain curve (red line), ventilation curve (dashed black line), and metabolic hyperbola (blue line) in a spontaneously breathing patient with a disease affecting the inspiratory flow-generation pathway at the equation of motion level [e.g., restrictive disease (↑Ers), obstructive disease (↑Rrs), dynamic hyperinflation (↑P EE )]. Similar effects are anticipated if the integrity is compromised at higher levels of the inspiratory flow-generation pathway. PaCO 2 desired by the brain is 39 mmHg and this corresponds to RCO/min of 6.3 l/min (point 1). In an intact inspiratory flow-generation pathway, the brain and ventilation curves would coincide, resulting in an actual PaCO 2 of 39 mmHg. For simplicity, let us assume that the disease acutely compromises the integrity of inspiratory flow-generation pathway and as a result the ventilation curve is moved to the right with a downward slope. Brain curve and metabolic hyperbola are kept constant. Consequently, the RCO/min corresponding to 6.3 l/min decreases actual ventilation to 4.2 l/min (point 2). This decrease in ventilation triggers a gradual rise in PaCO 2 , stimulating the respiratory centers. RCO/min progressively increases (mainly due to changes in respiratory drive, RCO per breath) along the brain curve in response to the elevated PaCO 2 . As RCO/min increases, so does actual ventilation along the ventilation curve. A steady state is reached when RCO/min (point 3) yields actual ventilation at the intersection of the ventilation curve and metabolic hyperbola (point 4). At this point, PaCO 2 stabilizes at 40 mmHg, and respiratory drive, RCO/min, and ventilation cease increasing as the CO 2 stimulus remains constant. Despite ventilatory demands of 9.3 l/min, only 6.2 l/min are met, resulting in a deficit of 3.1 l/min. The respiratory centers activity and ventilatory output are projected to forebrain via the corollary discharge pathway (re-afferent traffic, black arrows) and create the sense of dyspnea. Given the relatively low RCO/min and unmet demands, this patient is unlikely to experience dyspnea, particularly during resting conditions
Causes of high and low respiratory drive
High or low respiratory drive results from alterations in the (1) brain curve, (2) ventilation curve and (3) metabolic hyperbola. In critically ill patients usually high or low respiratory drive is the result of combined changes in these three curves. Brain curve is altered by PaO 2 changes, acid–base disturbances, neurotransmitters affecting the brain stem and stimulation of various receptors mainly located in the respiratory system [ 30 , 40 , 41 , 42 , 43 ]. In general, hypoxemia, metabolic acidosis, and lung/chest wall receptors stimulations concurrently shift the brain curve leftwards and upwards, whereas hyperoxemia, metabolic alkalosis, and sleep or sedation shift it rightwards and downwards [ 30 , 44 , 45 , 46 ]. In critically ill patients breathing spontaneously, the inspiratory flow-generation pathway is impaired (Table 1 ), shifting the ventilation curve to the right and downwards. This causes a consistent deviation of the ventilation curve from the brain curve (Fig. 3 ). As a result, actual PaCO 2 is higher than that desired by the respiratory centers, which respond by increasing RCO/min along the brain curve. When RCO/min results in an actual V’ E at the intersection of the ventilation curve and the metabolic hyperbola, a steady state occurs. PaCO 2 stabilizes and RCO/min and V’ E do not increase further. Although the ventilatory demands are not met, the RCO/min does not increase further because the CO 2 stimulus remains constant (Fig. 3 ).
Mechanical ventilation may shift the ventilation curve either to the left or to the right of the brain curve, depending on the level of assist provided. The slope of the curve is heavily regulated by the mode of support [ 2 ]. Therefore, during mechanical ventilation, the theoretical PaCO 2 , determined by the intersection between metabolic hyperbola and brain curve, may be higher or lower than the actual PaCO 2 , causing a decrease or increase in respiratory drive, respectively. The decrease in respiratory drive during mechanical ventilation, resulting from leftward shift of the ventilation curve, is common and can induce unstable breathing [ 2 ] (see below). This is infrequent in unsupported breathing, occurring mainly in specific diseases or circumstances (congestive heart failure, sleep apnea syndrome, high altitude) [ 47 , 48 , 49 ].
The metabolic hyperbola determines both the desired PaCO 2 and the actual PaCO 2 levels. Consequently, its upward or downward shifts significantly impact these PaCO 2 levels, thereby affecting the respiratory drive. Increased V’CO 2 and V D /V T ratios shift the metabolic hyperbola upward, whereas decreases in these variables shift it downward [ 29 ]. In critically ill patients, changes in V’CO 2 are induced by alterations in metabolic rate, which can be influenced by the disease itself (e.g., sepsis), body temperature, or vigorous respiratory efforts [ 50 , 51 , 52 ]. Ventilator settings, breathing patterns, V’/Q’ inequalities, right-to-left shunt, and modifications in dead space influence V D /V T [ 39 ]. Notably, a rapid, shallow breathing pattern secondary to delirium or panic reactions may cause an upward shift in the metabolic hyperbola due to an increase in V D /V T .
Respiratory drive—from health to disease
To better understand the interaction between metabolic hyperbola and brain and ventilation curves let us follow the respiratory drive of an adult human from health to disease.
In a healthy individual the inspiratory flow-generation pathway is intact and thus the brain curve and ventilation curve are identical, over a wide range of PaCO 2 . Assuming that in a healthy adult (1) V’CO 2 and V D /V T are normal, 200 ml/min and 0.3, respectively; (2) the ventilatory response to CO 2 is 2.5 l/min/mmHg; and (3) the intersection point between the metabolic hyperbola and ventilation curve is at PaCO 2 of 39 mmHg (eupneic PaCO 2 ), the resulting actual V’ E is 6.3 l/min. Since the brain and ventilation curves are identical, the RCO/min corresponds to 6.3 l/min, identical to the actual V’ E (Fig. 4 A). Because there is no deficit between the ventilatory demands, as reflected by RCO/min, and actual V’ E , the automatic act of breathing remains unnoticed by the forebrain [ 53 , 54 ].
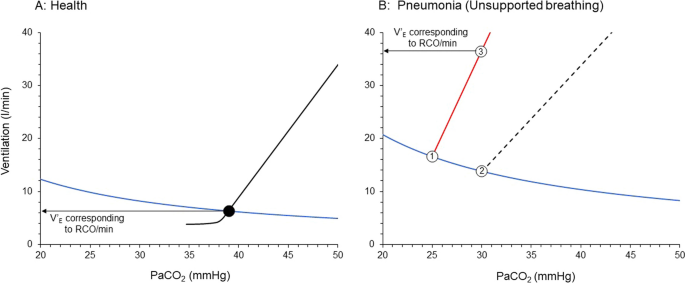
Brain and ventilation curves and metabolic hyperbola in a healthy subject ( A ) and when this individual suffers from pneumonia due to COVID-19 ( B ). A Health. Notice that brain and ventilation curves are similar (black lines) and thus the RCO/min corresponds to actual PaCO 2 and ventilation, set by the intersection point (black circle) between ventilation curve and metabolic hyperbola (blue line). B This human develops severe pneumonia due to COVID-19, causing increased V’CO 2 and V D /V T which move the metabolic hyperbola upward. The concomitant hypoxemia and metabolic acidosis shift the brain curve to the left and increases its slope (red line). Due to increased respiratory system elastance, a given RCO/min results in a lower ventilation and thus, the slope of the ventilation curve (dashed black line) is shifted downward. A dissociation between the ventilation curve and brain curve occurs. The desired PaCO 2 is 25 mmHg (point 1) and at this level of PaCO 2 RCO/min corresponds to 16.6 l/min. The actual PaCO 2 is 30 mmHg (point 2) and ventilation 13.8 l/min. PaCO 2 of 30 mmHg represents hypercapnia for respiratory centers which increase their activity along the brain curve. Respiratory activity stabilizes to a level corresponding to 36.6 l/min (point 3). Unmet ventilatory demands are 22.8 l/min. RCO/min: respiratory centers output per minute
Notably, even in healthy individuals, extreme hyperventilation may cause a deviation between brain and ventilation curves, due to dynamic hyperinflation and/or increases in respiratory system elastance as high tidal volumes approach the total lung capacity towards the end of inspiration [ 6 ].
Let us consider a scenario where this adult develops pneumonia due to COVID-19. The patient is febrile (39 °C) and visits the Emergency Department of the regional Hospital, reporting breathing difficulties (dyspnea). Clinical examination reveals tachycardia and signs of increased work of breathing, while arterial blood gases show hypoxemia (PaO 2 45 mmHg on 21% F I O 2 ) and hypocapnia (PaCO 2 30 mmHg). Acid–base balance evaluation demonstrates high anion gap metabolic acidosis. Chest X-rays are remarkable for diffuse opacities with loss of volume in the dependent lung regions. The patient has PaO 2 /F I O 2 < 300 mmHg on high-flow nasal oxygen and meets acute respiratory distress syndrome (ARDS) criteria [ 55 ].
Let us consider, the expected alteration in brain curve, ventilation curve and metabolic hyperbola in this patient. This approach was recently used to explain the pathophysiology of dyspnea on exertion in patients with pulmonary hypertension [ 6 ].
Unsupported spontaneous breathing
The inspiratory flow-generation pathway will be altered because of ARDS that induced a considerable increase in respiratory system elastance and slight increase in airway resistance [ 56 , 57 ]. Therefore, compared to healthy status, a given RCO (respiratory drive) results in a lower V T . Hence, at a given respiratory rate, the ventilation curve is shifted to the right with a decreased slope, causing deviation between brain and ventilation curve; the actual PaCO 2 is now higher than the theoretical PaCO 2 .
The brain curve shifts to the left due to increased respiratory centers sensitivity to CO 2 . The higher CO 2 sensitivity is attributed to (1) hypoxemia, (2) metabolic acidosis and stimulation of lung receptors by the inflammatory process and lung mechanics deterioration [ 23 , 30 , 40 , 41 ]. The resulting “theoretical” PaCO 2 , the one determined by the intersection of the brain curve and the metabolic hyperbola, will be much lower than in healthy state. Hence, even if the actual PaCO 2 will be low, and the patient will have hypocapnia, it will be interpreted by the respiratory centers as “hypercapnia” when the desired PaCO 2 is lower.
The metabolic hyperbola is shifted upward for two reasons. Firstly, V’CO 2 increases due to pneumonia, fever and excessive work of breathing [ 50 , 51 , 52 , 58 ]. Secondly, V D /V T is increased due to V’/Q’ inequalities (high and low), the presence of right-to-left shunt (atelectasis) and in situ thrombosis in small pulmonary arteries and capillaries vessels, all of which increase the physiological dead space [ 39 ].
Figure 4 B shows simulation of brain and ventilation curves and metabolic hyperbola, taking into consideration the pathology of this patient.
The brain curve is constructed assuming that the sensitivity of the respiratory centers increases by 60% from that in a healthy state, reaching 4 l/min/mmHg. The theoretical intersection point between the metabolic hyperbola and the brain curve is set at 25 mmHg, which is 5 mmHg lower than the actual PaCO 2 . The metabolic hyperbola is shifted upwards due to a 20% increase in V’CO 2 to 240 ml/min and a 67% increase in V D /V T to 0.5. Finally, the slope of the ventilation curve, mainly due to an increase in respiratory system elastance, decreases to 2 l/min/mmHg, resulting in a considerable deviation between the brain and ventilation curves. At PaCO 2 of 30 mmHg, actual ventilation is 13.8 l/min, while at this level of PaCO 2 the brain curve dictates that RCO/min corresponds to 36.6 l/min, a 22.8 l/min deficit between the ventilatory demands and actual V’ E . This high RCO/min is mainly due to an increase in RCO (respiratory drive) which augments respiratory muscles (inspiratory and expiratory) activity per breath. Respiratory rate may increase when respiratory drive is 3–5 times higher than the baseline [ 1 ]. The high respiratory centers activity and the unmet ventilatory demands are projected via the corollary discharge pathway to the forebrain and create the subjective symptom of dyspnea [ 53 , 54 ].
Consequences of high respiratory drive
The consequences of the high respiratory drive in this patient are numerous. Firstly, the high respiratory muscles activity per breath places the patient at risk of self-inflicted lung injury (P-SILI) [ 3 ]. Indeed, patients with a high respiratory drive may experience increased regional stress and strain in dependent lung regions due to the pendelluft phenomenon, characterized, early in inspiration, by the movement of air within the lung from nondependent to dependent regions without a change in V T [ 59 ]. Secondly, because of high elastance the transpulmonary driving pressure is high, contributing to lung injury [ 60 ]. Thirdly, the intense contraction of the diaphragm is associated with diaphragm damage [ 4 , 61 ]. This should be of great concern in this patient, as increased expression of genes involved in fibrosis and histological evidence for the development of fibrosis in the diaphragm have been reported in COVID-19 ICU patients [ 62 ]. Finally, the vigorous inspiratory efforts that lead to excessive negative esophageal pressure swings increase the trans-capillary pressure of pulmonary vessels and the afterload of the left ventricle, both of which are risk factors for increased capillary leak into the alveoli [ 63 , 64 ].
Estimation of respiratory drive
How can we estimate the respiratory drive in this patient? Although the respiratory drive cannot be measured directly in humans, it can be indirectly estimated via various indices. Since the inspiratory flow-generation pathway is compromised at the level of equation of motion, the V T /T Im no longer corresponds to respiratory drive and thus cannot be used as an index of it [ 2 ]. Provided that the inspiratory flow-generation pathway is intact up to the level of respiratory muscles, in order to estimate respiratory drive, we must obtain indices of respiratory motor output, such as electrical activity of the diaphragm (EAdi), trans-diaphragmatic pressure (Pdi), respiratory muscle pressure (Pmus), airway occlusion pressure (P0.1) and diaphragm thickening during inspiration (quantified by the thickening fraction, TFdi) [ 2 , 5 , 65 ] (Table 2 ). However, obtaining these indices requires expertise, and measuring them presents some challenges in spontaneously breathing patients with acute respiratory failure and distress. Therefore, clinical criteria of respiratory distress must be used to estimate the respiratory drive in this patient. It follows that the physical examination is of paramount importance in respiratory drive evaluation. Clinical signs of respiratory distress, such as hypertension, diaphoresis, tachycardia, accessory inspiratory (sternocleidomastoid, scalenes, external intercostals) and expiratory muscles (abdominals) contraction, nose flaring and intercostal retraction serve as reliable markers of high respiratory drive (Table 2 ). Despite the common belief that the respiratory rate is a sensitive index or respiratory drive, the latter should be markedly increased (3–5 times) before the former can change [ 1 ].
- Mechanical ventilation
The patient is admitted to ICU and although high-flow nasal O 2 therapy was applied, hypoxemia (SaO 2 85–88%) and respiratory distress continued. A decision to intubate was made. The patient was sedated and placed on volume control mode. Since vigorous respiratory efforts were not completely eliminated due to high respiratory drive [ 66 , 67 ], neuromuscular blocking agents were administered. The elimination of respiratory efforts combined with the decrease in body temperature using non steroid anti-inflammatory agents, decreased V’CO 2 production to 200 ml/min and moved metabolic hyperbola downwards. However, despite using a humidifier to prevent the decrease in dead space caused by heat and moisture exchange filters [ 68 ], V D /V T remained high, resulting in minimal downward movement of the metabolic hyperbola. Lung protective strategy was applied, hypoxemia was corrected, while PaCO 2 was maintained at 40 mmHg.
The next day paralysis was interrupted while sedation gradually decreased and stopped. When inspiratory efforts were resumed a premature decision to place the patient on pressure support (PS) was made, assuming that the high respiratory drive can be controlled by assisted mechanical ventilation. Nevertheless, the common belief that mechanical ventilation decreases respiratory drive due to unloading is disputed. Studies have shown that mechanical ventilation reduces respiratory drive indirectly by altering chemical feedback, primarily PaCO 2 levels [ 25 , 69 ]. Respiratory drive consistently follows chemical feedback, whether with or without mechanical ventilation. Therefore, during assisted mechanical ventilation, an intellectual theoretical assessment of brain and ventilation curves, and metabolic hyperbola, remains essential for understanding abnormalities in respiratory drive.
The patient continues to exhibit high anion gap metabolic acidosis. Although brain curve is slightly shifted to the right due to correction of hypoxemia, its slope continues to be high, since stimulation of receptors and metabolic acidosis are maintained [ 41 , 44 ]. Although the desired PaCO 2 by the respiratory centers increased slightly, the respiratory system mechanics were not improved and, therefore, the deviation between the brain and ventilation curves remains considerable (Fig. 5 ). At a given constant respiratory rate PS shifts the unsupported ventilation curve parallel to the left [ 2 ]. The actual PaCO 2 is 29.9 mmHg, 3.8 mmHg higher than the desired PaCO 2 and actual V’ E is 14.2 l/min. Because the actual PaCO 2 is higher than the desired, RCO/min increases along the brain curve to 30 l/min. Provided that respiratory muscles are not compromised, the activity of respiratory muscles also correspond to 30 l/min. This high activity of respiratory muscles is a risk factor for P-SILI and patient–ventilator dyssynchrony [ 3 , 70 ]. Additionally, at this level of respiratory drive there is recruitment of expiratory muscles which contract and decrease end-expiratory lung volume below that determined by PEEP [ 12 ]. This may potentially cause further lung injury (atelectrauma), derecruitment, and gas exchange abnormalities. Deterioration of respiratory system mechanics and gas exchange abnormalities move the brain curve to the left and metabolic hyperbola upwards [ 2 ].
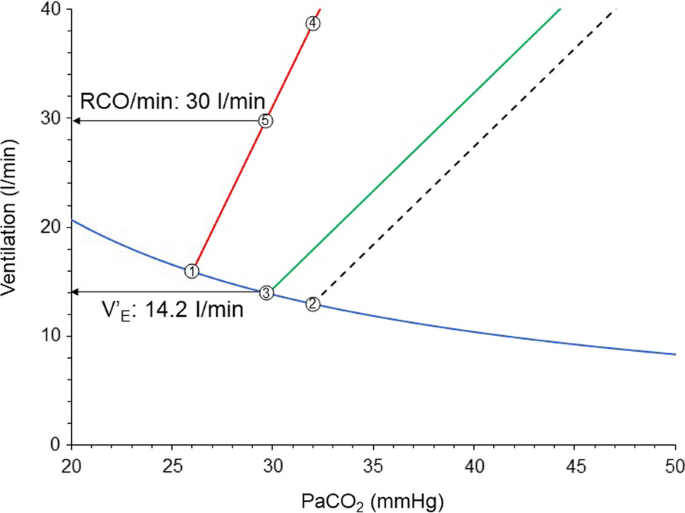
Brain curve (red line), unsupported (dashed black line) and supported with PS (green line) ventilation curves early in the course of critical illness of the patient of Fig. 4 . Point 1: desired PaCO 2 by respiratory centers; Point 2: theoretical PaCO 2 during unsupported spontaneous breathing; Point 3: actual PaCO 2 with PS during stable breathing (steady state); Point 4: RCO/min corresponding to desired V’ E with unsupported spontaneous breathing; Point 5: RCO/min corresponding to desired V’ E with PS ventilation; Notice the unmet demands without (difference in ventilation between points 2 and 4), and with PS (difference in ventilation between points 3 and 5). PS: pressure support; RCO/min: respiratory centers output per min; V’E: minute ventilation
Estimation of respiratory drive during mechanical ventilation
How can we estimate the respiratory drive in this patient? In mechanically ventilated patients respiratory drive can be quantitated using indices of motor output as described above. These indices, contrary to spontaneous breathing patients, can be obtained relatively easily [ 5 , 65 ]. Yet again, it is important to recognize that the presence of a disease that affects the inspiratory flow–generation pathway at or before the anatomical site of measurement always leads to underestimation of the respiratory drive. Respiratory muscles weakness is common in critically ill patients. Nevertheless, despite this limitation, indices of respiratory motor output may provide to the physician information for injurious high drive and assist the decision-making process (Table 2 ). Values for Pdi increase during the inspiratory phase (ΔPdi) ≥ 12 cmH 2 O and respiratory muscle swings during the breath (Pmus sw ) ≥ 15 cmH 2 O are associated with high drive which may be injurious, whereas driving transpulmonary pressure (ΔP lung ) ≥ 12 cmH 2 O and transpulmonary pressure swings (Plung sw ) ≥ 20 cmH 2 O indicate high lung stress and strain [ 4 ]. P0.1 higher than 4 cmH 2 O, easily measured in all ventilators, has an excellent accuracy to detect high effort per breath [ 71 ]. It has been shown recently that P0.1 higher than 3.5 cmH 2 O is associated with increased mortality [ 72 ]. The absolute drop in Paw during a whole breath occlusion correlates also with pleural and respiratory muscles pressures changes during the un-occluded tidal breaths [ 73 , 74 ], but its interpretation might be heavily affected by cortical feedback in awake patient and does not provide more information than P0.1. Finally, TFdi > 30% is an index of intense diaphragm contraction [ 75 ].
In this patient, due to deviation between the supported ventilation curve and brain curve unmet ventilatory demands are 15.8 l/min (30.0–14.2). For this reason, the patient exhibits signs of respiratory distress, which may force the clinicians to increase the level of assist. Since in this patient the desired PaCO 2 is 26 mmHg the PS level should considerably increase to achieve this value, resulting in excessive mechanical power applied on the lung [ 76 ] and increased afterload of the right heart [ 77 ]. The latter is attributed to high transpulmonary pressure which increases the pulmonary vascular resistance by creating zone II and I conditions in pulmonary circulation, potentially leading to acute cor pulmonale [ 78 ]. Therefore, this strategy increases the risk of lung injury and right heart dysfunction.
The indices of respiratory motor output and clinical examination, including dyspnea assessment [ 79 , 80 ], indicate injurious high drive (Table 2 ) and thus the patient was placed back to protective mechanical ventilation. Another attempt for fully assisted modes should be considered when the causes of alterations in brain curve, ventilation curve and metabolic hyperbola will be addressed. It is important to notice that during protective mechanical ventilation, if it is possible, complete inactivity of inspiratory muscles should be avoided in order to reduce the risk of atrophy [ 4 ].
After 3 days the patient meets criteria for assisted mode. Respiratory system mechanics and gas exchange abnormalities have been improved, indicating partial resolution of ARDS, while high anion gap metabolic acidosis has been resolved. The patient exhibits metabolic alkalosis mainly due to hypoalbuminemia.
The patient is placed on PS and a relatively high level of assist was used. At the same time a light sedation strategy is applied and if needed, an analgetic opioid is administered. Sedation, opioid, metabolic alkalosis and resolution of ARDS decrease considerably the sensitivity to CO 2 and shifts the brain curve to the right with a downward slope [ 31 , 43 , 45 ]. This rightward shift of the brain curve combined with high assist level [ 2 ], place the supported ventilation curve to the left of the brain curve (Fig. 6 A). Actual PaCO 2 and V’ E are 39 mmHg and 9.7 l/min, respectively. The desired PaCO 2 by respiratory centers is 42 mmHg and RCO/min at this PaCO 2 corresponds to 9.0 l/min. However, since the actual PaCO 2 is below 42 mmHg, the RCO/min decreases to that dictated by the PaCO 2 of 39 mmHg, which is 2.0 l/min. The respiratory drive is so low that the patient relaxes the diaphragm soon after triggering. This can be confirmed by indices of respiratory motor output as described above and TFdi. Values of ΔPdi and ΔPmus sw ≤ 3 cmH 2 O, P0.1 < 1.5 cmH 2 O and TFdi < 10% suggest low inspiratory muscles activity and thus low respiratory drive [ 4 ]. However, at presence of muscles weakness the limitation of these indices should be considered. It is of interest to note that P0.1 may be valid even in moderate to severe respiratory muscles weakness. It has been shown in an animal model of severe inspiratory muscles weakness, that P0.1 still increases reliably with increasing PaCO 2 , implying that the initial part of muscle contraction is relatively spared [ 81 ].
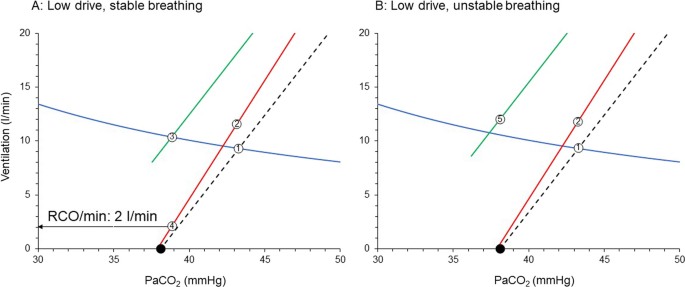
Brain curve (red line), unsupported (dashed black line) and supported with PS (green line) ventilation curves, relatively late in the course of critical illness of the patient of Fig. 5 . A High PS, stable breathing. B Unstable breathing with increasing PS. Point 1: PaCO 2 during unsupported spontaneous breathing; Point 2: RCO/min corresponding to desired V’ E with unsupported spontaneous breathing; Point 3: actual PaCO 2 with PS during stable breathing (stable ventilation); Point 4: RCO/min corresponding to desired V’ E with PS ventilation (stable ventilation); closed circles: apneic threshold; Point 5: Actual V’ E that results in apnea; Notice that with PS ventilation curve is shifted to the left of brain curve. See text for further explanation. PS: pressure support; RCO/min: respiratory centers output per min; V’ E : minute ventilation
Consequences of low drive
Now this patient is at risk of diaphragmatic atrophy. Indeed, it has been shown in animals that 12–18 h of PS, with a level of assist that caused diaphragmatic relaxation after triggering, resulted in diaphragmatic atrophy and contractile dysfunction [ 82 ]. Zambon et al. demonstrated in critically ill patients that there is a linear relationship between the level of PS and diaphragmatic atrophy rate [ 83 ]. Finally, Goligher et al. found that diaphragm atrophy is associated with a poor outcome [ 75 ]. Additionally, low respiratory drive is a risk factor of patient–ventilator dyssynchrony, mainly of the type of ineffective efforts [ 84 , 85 ], which may contribute to poor outcome [ 86 ].
Further increase in PS level moves the supported ventilation curve to lower PaCO 2 and when the intersection point is at PaCO 2 lower than apneic threshold repetitive apneas occur, and respiratory drive is hover around zero [ 87 , 88 ] (Fig. 6 B). PaCO 2 is close to apneic threshold. Non-steady state exists since the occurrence of apnea prevents PaCO 2 to decrease considerably below the apneic threshold and reach the steady state. V’ E oscillates between zero to approximately 12 l/min. In addition to diaphragm atrophy, the patient is now at risk of poor sleep quality due to microarousals occurring at the end of each apneic episode. These microarousals result in severe sleep fragmentation and very low levels of deep sleep (sleep deprivation), further compromising the already poor sleep quality in these patients [ 89 ]. It is of interest to note that poor sleep quality is a risk factor for adverse short and long-term outcomes [ 90 , 91 ]. The diaphragm may be also affected since it has been demonstrated that even one night of sleep deprivation in healthy individuals with normal function of the diaphragm may decrease inspiratory endurance due to reduction of cortical contribution to the respiratory centers output [ 15 ]. Finally, since the usual health care personnel response to apneas is to switch to control mechanical ventilation, unnecessary prolongation of mechanical ventilation is also a risk.
In the example provided above, we focus on a patient with pneumonia who developed ARDS. Similar reasoning should be applied to other diseases that affect the brain curve, ventilation curve, and metabolic hyperbola [ 6 , 35 ] (Fig. 7 ). For instance, this analysis demonstrated, contrary to general belief [ 92 ] that in patients with pulmonary arterial hypertension or chronic thromboembolic pulmonary hypertension the respiratory system is the main determinant of exercise limitation, with the cardiovascular system being an indirect contributor [ 6 ].
Determinants of brain curve (RCO/min/PaCO 2 ), ventilation curve (V’ E /PaCO 2 ) and metabolic hyperbola during unsupported spontaneous breathing (SB) and mechanical ventilation (MV). MV modifies the equation of motion by applying pressure (Paw) to the lungs, which acts in conjunction with the pressure generated by the inspiratory muscles (Pmus I ). During mechanical ventilation respiratory rate (Fr) may differ from the frequency of the electrical bursts (outputs) due to patient–ventilator dyssynchrony (i.e., ineffective efforts). Paw may change (curved arrows) Ers (recruitment/derecruitment/overdistension), Rrs (airway opening/closure) and P EE (dynamic hyperinflation). Notice that tidal volume (V T ) depends on a complex interaction of variables (Modifiers) determining brain curve, ventilation curve and metabolic hyperbola. RCO: respiratory centers output; Pmus: respiratory muscles pressure (inspiratory and expiratory); Ers: respiratory system elastance; Rrs: respiratory system resistance; P EE : elastic recoil pressure of respiratory system at end-expiration; V’: flow; ΔV: volume above end-expiratory lung volume; V’ E : minute ventilation; V’CO 2 : CO 2 production; V D /V T : physiological dead space to tidal volume ratio; PaCO 2 : partial pressure of arterial CO 2 ; PaO 2 : partial pressure of arterial O 2
Our analysis suggests that abnormalities in respiratory drive result from alterations in the brain curve, ventilation curve, and metabolic hyperbola. Considering the significant risks associated with both low and high respiratory drive, it is imperative to address and manage these abnormalities in all three curves. However, this task is complex, due to the significant interaction among the various factors that determine the curves (Fig. 7 ). In this process, it is important to recognize that respiratory drive can be increased by factors that: (1) impair the inspiratory flow-generation pathway (e.g., respiratory system mechanics derangements, dynamic hyperinflation, neuromuscular weakness) [ 35 ]; (2) increase the brain CO 2 sensitivity (e.g., metabolic acidosis, hypoxemia, receptors stimulation) [ 41 , 44 ]; and (3) shift the metabolic hyperbola upward (e.g., increases in V’CO 2 and/or V D /V T ) [ 39 , 50 , 51 , 52 ]. Conversely, respiratory drive can be decreased by interventions/therapy that (1) reduce brain CO 2 sensitivity (e.g., sedation, correction of metabolic acidosis or hypoxemia, metabolic alkalosis) [ 31 , 40 ]; (2) restore the integrity of the pathway from the respiratory centers to tidal volume generation (e.g., mechanical ventilation, mode of support, titration of ventilator settings, improvements in respiratory system mechanics and neuromuscular weakness) [ 80 , 93 , 94 ], and (3) shift the metabolic hyperbola downward (e.g., decreases in V’CO 2 or V D /V T ) [ 39 , 58 ]. By considering all factors that contribute to each of these three curves and employing inductive reasoning to understand their interactions, respiratory drive can be assessed at the bedside, facilitating a more informed decision-making process.
Availability of data and materials
Not applicable.
Abbreviations
Arterial partial pressure of CO 2
Arterial partial pressure of O 2
Respiratory centers output per breath
Respiratory centers output per minute
Minute ventilation
Functional residual capacity
Tidal volume
Respiratory centers output to inspiratory muscles
Respiratory centers output to expiratory muscles
Mechanical inflation time
CO 2 production
Physiological dead space
Ventilation–perfusion ratio
Patient self-inflicted lung injury
Electrical activity of the diaphragm
Trans-diaphragmatic pressure
Respiratory muscle pressure swings
Esophageal pressure
Airway occlusion pressure during the first 100 ms of inspiration
Absolute drop in airway pressure during a whole breath occlusion
Thickening fraction of the diaphragm
Intensive Care Unit
Pressure support
Acute respiratory distress syndrome
Akoumianaki E, Vaporidi K, Georgopoulos D. The injurious effects of elevated or nonelevated respiratory rate during mechanical ventilation. Am J Respir Crit Care Med. 2019;199(2):149–57.
Article CAS PubMed Google Scholar
Vaporidi K, Akoumianaki E, Telias I, Goligher EC, Brochard L, Georgopoulos D. Respiratory drive in critically ill patients: pathophysiology and clinical implications. Am J Respir Crit Care Med. 2020;201(1):20–32.
Article PubMed Google Scholar
Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med. 2017;195(4):438–42.
Goligher EC, Dres M, Patel BK, Sahetya SK, Beitler JR, Telias I, et al. Lung- and diaphragm-protective ventilation. Am J Respir Crit Care Med. 2020;202(7):950–61.
Article PubMed PubMed Central Google Scholar
Telias I, Brochard L, Goligher EC. Is my patient’s respiratory drive (too) high? Intensive Care Med. 2018;44(11):1936–9.
Mitrouska I, Bolaki M, Vaporidi K, Georgopoulos D. Respiratory system as the main determinant of dyspnea in patients with pulmonary hypertension. Pulm Circ. 2022;12(1): e12060.
Article CAS PubMed PubMed Central Google Scholar
Caruana-Montaldo B, Gleeson K, Zwillich CW. The control of breathing in clinical practice. Chest. 2000;117(1):205–25.
Del Negro CA, Funk GD, Feldman JL. Breathing matters. Nat Rev Neurosci. 2018;19(6):351–67.
Richter DW, Smith JC. Respiratory rhythm generation in vivo. Physiology. 2014;29(1):58–71.
Guyenet PG, Bayliss DA. Neural control of breathing and CO 2 homeostasis. Neuron. 2015;87(5):946–61.
Laveneziana P, Albuquerque A, Aliverti A, Babb T, Barreiro E, Dres M, et al. ERS statement on respiratory muscle testing at rest and during exercise. Eur Respir J. 2019;53(6):1801214.
Stamatopoulou V, Akoumianaki E, Vaporidi K, Stamatopoulos E, Kondili E, Georgopoulos D. Driving pressure of respiratory system and lung stress in mechanically ventilated patients with active breathing. Crit Care. 2024;28(1):19.
Younes M, Georgopoulos D. Control of breathing relevant to mechanical ventilation. In: Marini J, Slutsky A, editors. Physiological basis of ventilatory support. New York: Marcel Dekker; 1998. p. 1–74.
Google Scholar
Younes M, Riddle W. A model for the relation between respiratory neural and mechanical outputs: I. Theory. J Appl Physiol Respir Environ Exerc Physiol. 1981;51(4):963–78.
CAS PubMed Google Scholar
Rault C, Sangaré A, Diaz V, Ragot S, Frat JP, Raux M, et al. Impact of sleep deprivation on respiratory motor output and endurance: a physiological study. Am J Respir Crit Care Med. 2020;201(8):976–83.
Eldridge FL, Millhorn DE. Oscillation, gating, and memory in the respiratory control system. In: Terjung R, editor. Comprehensive physiology. Supplement 11: Handbook of physiology, the respiratory system, control of breathing. Bethesda: American Physiological Society; 2011. p. 93–114.
Kam K, Worrell JW, Janczewski WA, Cui Y, Feldman JL. Distinct inspiratory rhythm and pattern generating mechanisms in the preBötzinger complex. J Neurosci. 2013;33(22):9235–45.
Corne S, Webster K, McGinn G, Walter S, Younes M. Medullary metastasis causing impairment of respiratory pressure output with intact respiratory rhythm. Am J Respir Crit Care Med. 1999;159(1):315–20.
Costa R, Navalesi P, Cammarota G, Longhini F, Spinazzola G, Cipriani F, et al. Remifentanil effects on respiratory drive and timing during pressure support ventilation and neurally adjusted ventilatory assist. Respir Physiol Neurobiol. 2017;244:10–6.
Raux M, Straus C, Redolfi S, Morelot-Panzini C, Couturier A, Hug F, et al. Electroencephalographic evidence for pre-motor cortex activation during inspiratory loading in humans. J Physiol. 2007;578(Pt 2):569–78.
Mador MJ, Tobin MJ. Effect of alterations in mental activity on the breathing pattern in healthy subjects. Am Rev Respir Dis. 1991;144(3 Pt 1):481–7.
Cunningham DJ, Robins PA, Wolf CB. Integration of respiratory responses to changes in alveolar pressure of CO 2 and PO 2 and in arterial pH. Bethesda: American Physiological Society; 1986. p. 475–528.
Duffin J, Mohan RM, Vasiliou P, Stephenson R, Mahamed S. A model of the chemoreflex control of breathing in humans: model parameters measurement. Respir Physiol. 2000;120(1):13–26.
Georgopoulos D, Mitrouska I, Bshouty Z, Webster K, Patakas D, Younes M. Respiratory response to CO 2 during pressure-support ventilation in conscious normal humans. Am J Respir Crit Care Med. 1997;156(1):146–54.
Xirouhaki N, Kondili E, Mitrouska I, Siafakas N, Georgopoulos D. Response of respiratory motor output to varying pressure in mechanically ventilated patients. Eur Respir J. 1999;14(3):508–16.
Polacheck J, Strong R, Arens J, Davies C, Metcalf I, Younes M. Phasic vagal influence on inspiratory motor output in anesthetized human subjects. J Appl Physiol Respir Environ Exerc Physiol. 1980;49(4):609–19.
Hamilton RD, Winning AJ, Horner RL, Guz A. The effect of lung inflation on breathing in man during wakefulness and sleep. Respir Physiol. 1988;73(2):145–54.
Kondili E, Prinianakis G, Anastasaki M, Georgopoulos D. Acute effects of ventilator settings on respiratory motor output in patients with acute lung injury. Intensive Care Med. 2001;27(7):1147–57.
Tobin MJ, Laghi F, Jubran A. Ventilatory failure, ventilator support, and ventilator weaning. Compr Physiol. 2012;2(4):2871–921.
Duffin J. The chemoreflex control of breathing and its measurement. Can J Anaesth. 1990;37(8):933–42.
Nieuwenhuijs D, Sarton E, Teppema LJ, Kruyt E, Olievier I, van Kleef J, et al. Respiratory sites of action of propofol: absence of depression of peripheral chemoreflex loop by low-dose propofol. Anesthesiology. 2001;95(4):889–95.
Skatrud JB, Dempsey JA. Interaction of sleep state and chemical stimuli in sustaining rhythmic ventilation. J Appl Physiol Respir Environ Exerc Physiol. 1983;55(3):813–22.
Datta AK, Shea SA, Horner RL, Guz A. The influence of induced hypocapnia and sleep on the endogenous respiratory rhythm in humans. J Physiol. 1991;440:17–33.
Weil JV, Byrne-Quinn E, Sodal IE, Friesen WO, Underhill B, Filley GF, et al. Hypoxic ventilatory drive in normal man. J Clin Invest. 1970;49(6):1061–72.
Aubier M, Murciano D, Fournier M, Milic-Emili J, Pariente R, Derenne JP. Central respiratory drive in acute respiratory failure of patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1980;122(2):191–9.
Tipton MJ, Harper A, Paton JFR, Costello JT. The human ventilatory response to stress: rate or depth? J Physiol. 2017;595(17):5729–52.
Leitch AG, McLennan JE, Balkenhol S, McLaurin RL, Loudon RG. Ventilatory response to transient hyperoxia in head injury hyperventilation. J Appl Physiol Respir Environ Exerc Physiol. 1980;49(1):52–8.
Tenney SM, Ou LC. Ventilatory response of decorticate and decerebrate cats to hypoxia and CO 2 . Respir Physiol. 1977;29(1):81–92.
West JB. Causes of and compensations for hypoxemia and hypercapnia. Compr Physiol. 2011;1(3):1541–53.
Volta CA, Alvisi V, Bertacchini S, Marangoni E, Ragazzi R, Verri M, et al. Acute effects of hyperoxemia on dyspnoea and respiratory variables during pressure support ventilation. Intensive Care Med. 2006;32(2):223–9.
Linton RA, Poole-Wilson PA, Davies RJ, Cameron IR. A comparison of the ventilatory response to carbon dioxide by steady-state and rebreathing methods during metabolic acidosis and alkalosis. Clin Sci Mol Med. 1973;45(2):239–49.
Tojima H, Kunitomo F, Okita S, Yuguchi Y, Tatsumi K, Kimura H, et al. Difference in the effects of acetazolamide and ammonium chloride acidosis on ventilatory responses to CO 2 and hypoxia in humans. Jpn J Physiol. 1986;36(3):511–21.
Javaheri S, Shore NS, Rose B, Kazemi H. Compensatory hypoventilation in metabolic alkalosis. Chest. 1982;81(3):296–301.
Jacono FJ, Peng YJ, Nethery D, Faress JA, Lee Z, Kern JA, et al. Acute lung injury augments hypoxic ventilatory response in the absence of systemic hypoxemia. J Appl Physiol. 2006;101(6):1795–802.
Harper MH, Hickey RF, Cromwell TH, Linwood S. The magnitude and duration of respiratory depression produced by fentanyl and fentanyl plus droperidol in man. J Pharmacol Exp Ther. 1976;199(2):464–8.
Akada S, Fagerlund MJ, Lindahl SG, Sakamoto A, Prabhakar NR, Eriksson LI. Pronounced depression by propofol on carotid body response to CO 2 and K+-induced carotid body activation. Respir Physiol Neurobiol. 2008;160(3):284–8.
West JB, Peters RM, Aksnes G, Maret KH, Milledge JS, Schoene RB. Nocturnal periodic breathing at altitudes of 6300 and 8050 m. J Appl Physiol. 1986;61(1):280–7.
Mortara A, Sleight P, Pinna GD, Maestri R, Capomolla S, Febo O, et al. Association between hemodynamic impairment and Cheyne-Stokes respiration and periodic breathing in chronic stable congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 1999;84(8):900–4.
Younes M, Ostrowski M, Atkar R, Laprairie J, Siemens A, Hanly P. Mechanisms of breathing instability in patients with obstructive sleep apnea. J Appl Physiol. 2007;103(6):1929–41.
Viale JP, Annat GJ, Bouffard YM, Delafosse BX, Bertrand OM, Motin JP. Oxygen cost of breathing in postoperative patients: pressure support ventilation vs continuous positive airway pressure. Chest. 1988;93(3):506–9.
Rochester DF, Bettini G. Diaphragmatic blood flow and energy expenditure in the dog: effects of inspiratory airflow resistance and hypercapnia. J Clin Invest. 1976;57(3):661–72.
Uehara M, Plank LD, Hill GL. Components of energy expenditure in patients with severe sepsis and major trauma: a basis for clinical care. Crit Care Med. 1999;27(7):1295–302.
Parshall MB, Schwartzstein RM, Adams L, Banzett RB, Manning HL, Bourbeau J, et al. An Official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med. 2012;185(4):435–52.
Fukushi I, Pokorski M, Okada Y. Mechanisms underlying the sensation of dyspnea. Respir Investig. 2021;59(1):66–80.
Matthay MA, Arabi Y, Arroliga AC, Bernard G, Bersten AD, Brochard LJ, et al. A new global definition of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2024;209(1):37–47.
Auler JO, Saldiva PH, Martins MA, Carvalho CR, Negri EM, Hoelz C, et al. Flow and volume dependence of respiratory system mechanics during constant flow ventilation in normal subjects and in adult respiratory distress syndrome. Crit Care Med. 1990;18(10):1080–6.
Eissa NT, Ranieri VM, Corbeil C, Chassé M, Robatto FM, Braidy J, et al. Analysis of behavior of the respiratory system in ARDS patients: effects of flow, volume, and time. J Appl Physiol. 1991;70(6):2719–29.
Manthous CA, Hall JB, Olson D, Singh M, Chatila W, Pohlman A, et al. Effect of cooling on oxygen consumption in febrile critically ill patients. Am J Respir Crit Care Med. 1995;151(1):10–4.
Yoshida T, Torsani V, Gomes S, De Santis RR, Beraldo MA, Costa EL, et al. Spontaneous effort causes occult pendelluft during mechanical ventilation. Am J Respir Crit Care Med. 2013;188(12):1420–7.
Dreyfuss D, Soler P, Basset G, Saumon G. High inflation pressure pulmonary edema: respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am Rev Respir Dis. 1988;137(5):1159–64.
Goligher EC, Brochard LJ, Reid WD, Fan E, Saarela O, Slutsky AS, et al. Diaphragmatic myotrauma: a mediator of prolonged ventilation and poor patient outcomes in acute respiratory failure. Lancet Respir Med. 2019;7(1):90–8.
Shi Z, de Vries HJ, Vlaar APJ, van der Hoeven J, Boon RA, Heunks LMA, et al. Diaphragm pathology in critically ill patients with COVID-19 and postmortem findings from 3 medical centers. JAMA Intern Med. 2021;181(1):122–4.
Bhattacharya M, Kallet RH, Ware LB, Matthay MA. Negative-pressure pulmonary edema. Chest. 2016;150(4):927–33.
Magder S. Clinical usefulness of respiratory variations in arterial pressure. Am J Respir Crit Care Med. 2004;169(2):151–5.
Telias I, Spadaro S. Techniques to monitor respiratory drive and inspiratory effort. Curr Opin Crit Care. 2020;26(1):3–10.
Pohlman MC, McCallister KE, Schweickert WD, Pohlman AS, Nigos CP, Krishnan JA, et al. Excessive tidal volume from breath stacking during lung-protective ventilation for acute lung injury. Crit Care Med. 2008;36(11):3019–23.
Beitler JR, Sands SA, Loring SH, Owens RL, Malhotra A, Spragg RG, et al. Quantifying unintended exposure to high tidal volumes from breath stacking dyssynchrony in ARDS: the BREATHE criteria. Intensive Care Med. 2016;42(9):1427–36.
Prin S, Chergui K, Augarde R, Page B, Jardin F, Vieillard-Baron A. Ability and safety of a heated humidifier to control hypercapnic acidosis in severe ARDS. Intensive Care Med. 2002;28(12):1756–60.
Georgopoulos D, Mitrouska I, Webster K, Bshouty Z, Younes M. Effects of inspiratory muscle unloading on the response of respiratory motor output to CO 2 . Am J Respir Crit Care Med. 1997;155(6):2000–9.
Kondili E, Prinianakis G, Georgopoulos D. Patient-ventilator interaction. Br J Anaesth. 2003;91(1):106–19.
Telias I, Junhasavasdikul D, Rittayamai N, Piquilloud L, Chen L, Ferguson ND, et al. Airway occlusion pressure as an estimate of respiratory drive and inspiratory effort during assisted ventilation. Am J Respir Crit Care Med. 2020;201(9):1086–98.
Le Marec J, Hajage D, Decavèle M, Schmidt M, Laurent I, Ricard JD, et al. High airway occlusion pressure is associated with dyspnea and increased mortality in critically ill mechanically ventilated patients. Am J Respir Crit Care Med. 2024. https://doi.org/10.1164/rccm.202308-1358OC .
Bertoni M, Telias I, Urner M, Long M, Del Sorbo L, Fan E, et al. A novel non-invasive method to detect excessively high respiratory effort and dynamic transpulmonary driving pressure during mechanical ventilation. Crit Care. 2019;23(1):346.
de Vries HJ, Tuinman PR, Jonkman AH, Liu L, Qiu H, Girbes ARJ, et al. Performance of noninvasive airway occlusion maneuvers to assess lung stress and diaphragm effort in mechanically ventilated critically ill patients. Anesthesiology. 2023;138(3):274–88.
Goligher EC, Fan E, Herridge MS, Murray A, Vorona S, Brace D, et al. Evolution of diaphragm thickness during mechanical ventilation: impact of inspiratory effort. Am J Respir Crit Care Med. 2015;192(9):1080–8.
Gattinoni L, Tonetti T, Cressoni M, Cadringher P, Herrmann P, Moerer O, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med. 2016;42(10):1567–75.
Mekontso Dessap A, Boissier F, Charron C, Bégot E, Repessé X, Legras A, et al. Acute cor pulmonale during protective ventilation for acute respiratory distress syndrome: prevalence, predictors, and clinical impact. Intensive Care Med. 2016;42(5):862–70.
Bouferrache K, Vieillard-Baron A. Acute respiratory distress syndrome, mechanical ventilation, and right ventricular function. Curr Opin Crit Care. 2011;17(1):30–5.
Bureau C, Dres M, Morawiec E, Mayaux J, Delemazure J, Similowski T, et al. Dyspnea and the electromyographic activity of inspiratory muscles during weaning from mechanical ventilation. Ann Intensive Care. 2022;12(1):50.
Decavèle M, Bureau C, Campion S, Nierat MC, Rivals I, Wattiez N, et al. Interventions relieving dyspnea in intubated patients show responsiveness of the mechanical ventilation-respiratory distress observation scale. Am J Respir Crit Care Med. 2023;208(1):39–48.
Holle RH, Schoene RB, Pavlin EJ. Effect of respiratory muscle weakness on P0.1 induced by partial curarization. J Appl Physiol Respir Environ Exerc Physiol. 1984;57(4):1150–7.
Hudson MB, Smuder AJ, Nelson WB, Bruells CS, Levine S, Powers SK. Both high level pressure support ventilation and controlled mechanical ventilation induce diaphragm dysfunction and atrophy. Crit Care Med. 2012;40(4):1254–60.
Zambon M, Beccaria P, Matsuno J, Gemma M, Frati E, Colombo S, et al. Mechanical ventilation and diaphragmatic atrophy in critically ill patients: an ultrasound study. Crit Care Med. 2016;44(7):1347–52.
Leung P, Jubran A, Tobin MJ. Comparison of assisted ventilator modes on triggering, patient effort, and dyspnea. Am J Respir Crit Care Med. 1997;155(6):1940–8.
Vaschetto R, Cammarota G, Colombo D, Longhini F, Grossi F, Giovanniello A, et al. Effects of propofol on patient-ventilator synchrony and interaction during pressure support ventilation and neurally adjusted ventilatory assist. Crit Care Med. 2014;42(1):74–82.
Vaporidi K, Babalis D, Chytas A, Lilitsis E, Kondili E, Amargianitakis V, et al. Clusters of ineffective efforts during mechanical ventilation: impact on outcome. Intensive Care Med. 2017;43(2):184–91.
Meza S, Giannouli E, Younes M. Control of breathing during sleep assessed by proportional assist ventilation. J Appl Physiol. 1998;84(1):3–12.
Meza S, Mendez M, Ostrowski M, Younes M. Susceptibility to periodic breathing with assisted ventilation during sleep in normal subjects. J Appl Physiol. 1998;85(5):1929–40.
Georgopoulos D, Kondili E, Gerardy B, Alexopoulou C, Bolaki M, Younes M. Sleep architecture patterns in critically ill patients and survivors of critical illness: a retrospective study. Ann Am Thorac Soc. 2023;20(11):1624–32.
Dres M, Younes M, Rittayamai N, Kendzerska T, Telias I, Grieco DL, et al. Sleep and pathological wakefulness at the time of liberation from mechanical ventilation (SLEEWE): a prospective multicenter physiological study. Am J Respir Crit Care Med. 2019;199(9):1106–15.
Krause AJ, Simon EB, Mander BA, Greer SM, Saletin JM, Goldstein-Piekarski AN, et al. The sleep-deprived human brain. Nat Rev Neurosci. 2017;18(7):404–18.
Neder JA, Ramos RP, Ota-Arakaki JS, Hirai DM, D’Arsigny CL, O’Donnell D. Exercise intolerance in pulmonary arterial hypertension: the role of cardiopulmonary exercise testing. Ann Am Thorac Soc. 2015;12(4):604–12.
Georgopoulos D, Giannouli E, Patakas D. Effects of extrinsic positive end-expiratory pressure on mechanically ventilated patients with chronic obstructive pulmonary disease and dynamic hyperinflation. Intensive Care Med. 1993;19(4):197–203.
Kondili E, Prinianakis G, Alexopoulou C, Vakouti E, Klimathianaki M, Georgopoulos D. Respiratory load compensation during mechanical ventilation–proportional assist ventilation with load-adjustable gain factors versus pressure support. Intensive Care Med. 2006;32(5):692–9.
Download references
Acknowledgements
Author information, authors and affiliations.
Medical School, University of Crete, Heraklion, Crete, Greece
Dimitrios Georgopoulos & Evangelia Akoumianaki
Department of Intensive Care Medicine, University Hospital of Heraklion, Heraklion, Crete, Greece
Maria Bolaki & Evangelia Akoumianaki
Department of Pulmonary Medicine, University Hospital of Heraklion, Heraklion , Crete, Greece
Vaia Stamatopoulou
You can also search for this author in PubMed Google Scholar
Contributions
DG conceived this study. DG, MB, VS and EA drafted and reviewed the manuscript. All authors finally approved the content of the manuscript to be submitted.
Corresponding author
Correspondence to Dimitrios Georgopoulos .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
: Figure S1. Normal (Health). Intact inspiratory flow-generation pathway. Figure S2. Neuromuscular weakness. Figure S3. Dynamic hyperinflation in a patient exhibiting flow limitation during passive expiration.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Georgopoulos, D., Bolaki, M., Stamatopoulou, V. et al. Respiratory drive: a journey from health to disease. j intensive care 12 , 15 (2024). https://doi.org/10.1186/s40560-024-00731-5
Download citation
Received : 22 March 2024
Accepted : 12 April 2024
Published : 22 April 2024
DOI : https://doi.org/10.1186/s40560-024-00731-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ventilatory response to CO 2
- Metabolic hyperbola
- Critically ill
Journal of Intensive Care
ISSN: 2052-0492
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Exploring the hospital patient journey: What does the patient experience?
Contributed equally to this work with: Raffaella Gualandi, Cristina Masella
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft
* E-mail: [email protected]
Affiliation Department of Nursing, Università Campus Bio-Medico di Roma, Rome, Italy
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft
Affiliation Department of Management Economics and Industrial Engineering, Politecnico di Milano, Milan, Italy
Roles Data curation, Formal analysis, Investigation, Project administration
Roles Conceptualization, Supervision
- Raffaella Gualandi,
- Cristina Masella,
- Daniela Viglione,
- Daniela Tartaglini

- Published: December 5, 2019
- https://doi.org/10.1371/journal.pone.0224899
- Peer Review
- Reader Comments
To understand how different methodologies of qualitative research are able to capture patient experience of the hospital journey.
A qualitative study of orthopaedic patients admitted for hip and knee replacement surgery in a 250-bed university hospital was performed. Eight patients were shadowed from the time they entered the hospital to the time of transfer to rehabilitation. Four patients and sixteen professionals, including orthopaedists, head nurses, nurses and administrative staff, were interviewed.
Through analysis of the data collected four main themes emerged: the information gap; the covering patient-professionals relationship; the effectiveness of family closeness; and the micro-integration of hospital services. The three different standpoints (patient shadowing, health professionals’ interviews and patients’ interviews) allowed different issues to be captured in the various phases of the journey.
Conclusions
Hospitals can significantly improve the quality of the service provided by exploring and understanding the individual patient journey. When dealing with a key cross-functional business process, the time-space dynamics of the activities performed have to be considered. Further research in the academic field can explore practical, methodological and ethical challenges more deeply in capturing the whole patient journey experience by using multiple methods and integrated tools.
Citation: Gualandi R, Masella C, Viglione D, Tartaglini D (2019) Exploring the hospital patient journey: What does the patient experience? PLoS ONE 14(12): e0224899. https://doi.org/10.1371/journal.pone.0224899
Editor: Rosemary Frey, University of Auckland, NEW ZEALAND
Received: July 10, 2019; Accepted: October 23, 2019; Published: December 5, 2019
Copyright: © 2019 Gualandi et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
In the healthcare knowledge-based system, literature has given increasing attention over time to improving clinical knowledge, including by making use of the patient's insider perspective [ 1 – 3 ]. In particular, patient experience of healthcare and the delivery of care is emerging as an important area of knowledge, but one that is sometimes overlooked [ 4 , 5 ].
The Beryl Institute defines patient experience as “the sum of all interactions, shaped by an organization’s culture, that influence patient perceptions, across the continuum of care”[ 6 ]. Wolf et al. specify that interactions are “The orchestrated touchpoints of people, processes, policies, communications, actions, and environment” and patient perceptions are “what is recognized, understood and remembered by patients and support people”[ 7 ].
In the last few years, emphasis on the emotional drivers of engagements has led many authors to enhance the customer experience starting from an analysis of the customer journey [ 8 ]. In the hospital context, the patient journey is a key cross-functional business process where patient and providers share action and information flows between people and systems across various touchpoints. Providers aim to manage hospital patient flow in order to provide safe and efficient patient care while ensuring the best use of hospital resources (i.e.: beds, operating theatres, clinics and specialized staff). Poor patient flow may result in decreasing levels of productivity, increasing risk of harming patients and decreasing levels of quality perceived by patients [ 9 – 11 ]. Patients aim to receive the best care together with a high quality of service. As a matter of fact, the patient is the only actor who experiences the whole path by connecting each step of the journey. Therefore, hospitals can significantly improve the quality of the service provided by exploring and understanding the individual patient journey [ 12 – 14 ].
Many tools may be used to measure and understand patient experience [ 15 , 16 ]. Surveys are the methods mainly used to capture the patient experience and to evaluate the quality and safety of various clinical processes [ 17 , 18 ]. However, questionnaires or traditional static observation may not be well-suited to reveal all the aspects of patient experience [ 19 ]. In the complex hospital environment, multiple factors can affect the patient experience, including the time-space dynamics of the activities performed and the patients’ perceptions and emotions lived at the time of the experience [ 20 ]. Moreover, some authors emphasize that what the patient remembers is different from what he/she experiences in real-time, depending on the length of the recall period [ 21 , 22 ]. Therefore, as what the patient remembers may change over time, gathering accurate and immediate data on the experience lived also depends on the time of the interview.
A recent study reports how the use of unstructured diaries completed in a patient’s own words can capture the hospital-stay experience from the patient’s own perspective. However, it is not clear how real-time experiences are reported in relation to high-emotional situations or clinical activities that can interfere with the patient’s ability and willingness to write (i.e. during the transfer to the operating theatre or in the post-operative period, immediately after surgery). Furthermore, the authors show how study participants with a tertiary education wrote more in their diaries than those without [ 23 ]. This could potentially eliminate important aspects of the experience lived by vulnerable people.
Some authors have emphasized the value of shadowing for phenomenological research, by giving a more complete picture of the phenomenon in the real-time context of an organization [ 24 , 25 ]. Patient shadowing may have an especially valuable role in gaining insights into complex cross-hospital processes, in particular when dealing with vulnerable people who could be excluded from interview studies [ 26 , 27 ]. Furthermore, some studies have reported how, through shadowing methodology, it is possible to assess the lived experience of patients in a patient-centred perspective [ 28 , 29 ]. However, methodological and ethical issues of shadowing still need to be explored in greater depth [ 25 , 30 ].
While on the one hand patient experience is increasingly considered as a driver for health services improvement, on the other it is still not clear how to capture the whole patient experience in traversing hospital services [ 31 – 33 ]. Therefore, this study seeks to explore which aspects of the hospital patient journey experience may be captured by the three different standpoints: patient shadowing, health professionals’ interviews and patients interviews. Accordingly, it aims to answer the following questions: what does the patient experience through the hospital journey? How can it be captured?
Materials and methods
Study design.
This study was a qualitative study with a phenomenological‐hermeneutic approach using participant interviews and patient shadowing [ 34 , 35 ]. The Consolidated Criteria for Reporting Qualitative Research—COREQ checklist was used as a guideline to report the study data [ 36 ]. The study was undertaken in a 250-bed Italian academic teaching hospital. Orthopaedic patients undergoing total hip (THA) or knee arthroplasty (TKA) were selected in order to analyse a standard clinical path ( Fig 1 ). Urgently admitted patients were excluded due to the different clinical path they have to follow. The unit of analysis was the hospital patient’s journey starting from the first outpatient visit and concluding with the first follow-up visit. The study was approved by the Hospital Ethics Committee.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0224899.g001
Data collection
Between August 2016 and April 2017, a total of twelve patients and sixteen key professionals were invited to participate and all agreed. There were no prior relationships between researchers and patients; two researchers knew some healthcare professionals because they worked in the same hospital, though in different units and without patient care roles. The possibility of coercion was minimized by guaranteeing data anonymity, by requesting voluntary participation in the study and by dealing with issues on which the researchers had no power to influence anything or anyone at hospital managerial level.
A convenience sample of patients was selected based on whether their inpatient admission and follow-up visit fell within the observation period. Inclusion criteria were: patients scheduled to undergo surgery for THA or TKA, for the shadowing phase; patients who had had a THA or TKA ad were in follow-up, for the interviews. Exclusion criteria were: <18 years, inability to understand, not wanting to participate, inability to read/speak Italian. Patients were asked to participate in the study at the time they arrived in the hospital. The first author invited patients to participate in the study when they met at the hospital for preoperative tests or on the day of admission. Patients accepting the invitation were provided with further information about the project by the first author, and were asked to sign their consent to participate in the study and to the anonymous use of their data.
Eight patients admitted between August and September 2016 were selected for the shadowing phase. A shadowing methodology was used in order to provide an embodied understanding of patients’ experiences in context [ 26 ]. Two female students from the nursing and industrial engineering degree courses, with no roles in the delivery of patient care, were trained for data collection by the first author. In this way, the risk of not reporting negative feedback during the study by the participants, and subjective interpretations by the authors in capturing data, was minimized. Patients were shadowed from the time of hospital admission to the time of discharge, with the shadower observing the patient during daytime hours and completing a data collection form prepared by the research group. This involved recording every step of the hospital journey process, by analysing each touchpoint and including time, patient, caregiver, activity, shadower’s observations, and impressions. In particular, touchpoint observations indicated where patients and families go (setting), with whom they come into contact, how long the experience at each touchpoint takes (time), what patients and caregivers do, and a description of any comments of the patient and family, including any observable emotional state of the patient. By considering patients’ emotion as consistent responses to internal or external events, the Plutchik’s model was used as framework to understand its intensity in a positive or negative characterization [ 37 ]. In particular, Plutchik suggests emotions are low, medium or high-intensity, and if left unchecked, they can intensify. Accordingly, the patient's emotional journey was also assessed in reference to external events that altered the patient's emotional level.
Patient care procedures were not noted because they were not relevant for the current research objectives. The shadower observed the patients during all hospital transfers and entered the patients’ rooms only to verify their general state and to gather any statements about their experience. The shadower was mainly passive during the observation, but was active in informal conversations. This level of proximity made it possible for the patients not to perceive shadowers as intrusive or disrespectful of their privacy.
Between September 2016 and April 2017, four patients and sixteen healthcare professionals participated in face-to-face open interviews lasting 30–45 minutes and performed by the first and the third author. A few main open questions were identified by the research group in order to analyse the main steps of the patients’ journeys, the patients’ experiences, and their reported emotions. Patients were interviewed at the first outpatient follow-up visit ( Fig 1 ), scheduled one month after discharge from the ward, in order to include their perceptions of discharge.
In order to capture viewpoints representing various different roles, a collaborative purposive sampling technique was used among professionals with different level of professional experience who take care of orthopaedic patients. In particular, according to Benner’s stages of clinical competence [ 38 ], two nurses with experience of at least five years, identified as expert nurses by their managers, and three nurses with experience of up to four years, identified as competent nurses, were selected. In addition, two orthopaedic surgeons and one medical doctor under training were involved. Finally, three members of the administrative staff, the director responsible for the quality of care processes, and the head nurses of the units involved in the patient journeys (i.e.: two Ward Units, one Surgery Room, one Rehabilitation Unit), were interviewed.
All interviews were audio-recorded and transcribed verbatim with participant permission. Data from the field notes and the interviews were transferred to an Excel spreadsheet database to systematize them and for the subsequent analysis.
Data analysis
Data analysis was performed on three levels as suggested by Ricoeur [ 30 ]: a naïve reading, a structural analysis and a critical analysis and discussion. The first author performed a thematic analysis of the text material. In the structural analysis, the units of meaning (what was said) were reflected in units of significance (what the texts were talking about) from which the key themes emerged ( Table 1 ). Patients’ emotions, reported or observed, were classified according to Plutchik’s Wheel of Emotions [ 37 ]. After that, a critical analysis was carried out by the researchers in order to analyse the coding process, the categories and the meanings that emerged.
https://doi.org/10.1371/journal.pone.0224899.t001
The main characteristics of the participants involved in the study are reported in Table 2 . Patients involved ranged in age from 56–78 years with an average age of 67.3 years, and they were hospitalized on average 4.4 days. All had a regular clinical trajectory with no noteworthy complications. Healthcare professionals ranged in age from 29–61 years with an average age of 38.8 years and a work experience average of 10.6 years.
https://doi.org/10.1371/journal.pone.0224899.t002
The hospital patient journey
In the patient hospital journeys studied, seven main phases and forty-four consequent steps were traced by shadowing patients and interviewing the main actors. Table 3 shows which steps were identified from the interviews and which from the shadowing. In particular, the patient shadowing enabled more accurate reconstruction of all the steps, compared to what patients narrated after a period of time. This information can be obtained from the health professionals' interviews only by summarizing their different points of view. Furthermore, through shadowing it was possible to detect that within the hospital the patient went through eighteen different places and was in contact with more than fifty different health professionals. The patients’ emotions as reported by the health professionals corresponded to what was observed by shadowing, but they did not match the general state of serenity reported by patients when interviewed.
https://doi.org/10.1371/journal.pone.0224899.t003
The three different standpoints, (i.e.: patient shadowing, healthcare professional interviews and patient interviews) allowed different issues to be captured at the various phases of the journey. In particular, the shadowing was able to capture the 'connections' between one stage and another of the journey, such as movement from admissions to the ward and transport from the ward to the operating theatre, while the journey narrated by each professional and patient allowed the most significant touchpoints to be identified ( Table 3 ).
When interviewed about a month after discharge, patients remembered a generally positive experience, linked specifically to the success of surgery and to a good relationship with the professionals. They showed appreciation and satisfaction and they declared that there were no major problems to deal with. One patient reported "I was fine , look , I have to say the night of the surgery I was fine , the next day they also made me get up . They made me sit in the chair , my head was spinning a little , so it's not that ehm … then nothing else , everything else went well” (Patient 1); Another reported “What can I say ? Better than that I don't think it is; that… we may be worse , but I have not found that I was worse , and I have only good things to say about the professor and all his assistants” (Patient 3).
However, when shadowed, some discrepancies emerged. When going independently to the ward patients experienced confusion and anxiety, due to not having clearly understood indications, and to the waiting times before entering the assigned ward (Patient 5, 6, 7, 8, 9,12). Another critical step was the transfer and waiting in the operating theatre. They felt 'lost' when they were transferred and emotions of fear and anxiety emerged (Patient 10; 11). These experiences also emerged from the interviews with professionals (Healthcare professional 4, 6, 8, 12, 14 16).
Some other interesting points, detected by the shadowing, reveal how the hospital environment and management of patient flow can affect the patient experience, in particular on the day of admission. After the administrative acceptance, one patient took the wrong elevator and did not immediately reach the indicated ward. When arriving at the entrance of the ward, he found it difficult to use the intercom. When entering the ward, he was dissatisfied with the lack of staff to welcome him. When waiting in the room for surgery he showed apprehension and he reported a desire to have more information and to have a family member nearby (Patient 9). Another patient reported having received incorrect information to reach the ward and that the hospital directional signs were too small and difficult to read (Patient 1).
During the journey it is possible to identify some key steps, though with different levels of importance from patients’ and professionals’ perspectives. From the patient perspective and by shadowing the journey, the day of hospitalization was the most critical, and they experienced mainly negative emotions (Patient 5, 6, 7, 8, 9,12). From the interviews with the professionals it emerges that when returning to the ward after surgery patients were calm (Healthcare professional 7, 8, 16) but in the following days, they began to experience a lack of autonomy and this could make them nervous (Healthcare professional 13). Professionals involved in the pre-hospitalization phase report that waiting in the days before hospital admission can negatively affect patient experience. Patients can feel abandoned, if no one gives them information on the outcome of the outpatient clinic examination, or if all the procedures related to hospitalization are not properly programmed (Healthcare professional 1, 9).
Through analysis of the data collected four main themes emerged underlying both the shadowing and the interviews: the information gap; the covering patient-professionals relationship; the effectiveness of family closeness; and the micro-integration of hospital services.
The most significant issues are reported below.
The information gap
When interviewed, patients did not mention any problems with the information received in the course of their hospital journey. However, when patients were shadowed on arrival at the hospital, they did not seem to be aware of any information regarding their hospitalization (e.g. visiting hours for family members, the hospital route to the ward), but asked the first professionals they met. The patients seemed lost, especially after going through the admission process and on looking for their assigned wards. Moreover, when they arrived in the ward they needed information about their hospitalization, but healthcare professionals did not immediately assist them (Patient 5, 6, 9). This seemed to contribute to their state of anxiety about the surgery. This issue is confirmed by what the professionals reported. When they arrive at the hospital, patients put the same questions to any professional they come into contact with (Healthcare professional 4, 6). A nurse reports how each patient has "so many anxieties , fears , uncertainties , questions , as soon as he steps into the ward and I follow him , until he leaves the ward" (Healthcare professional 1). A head nurse reports "Family members also ask many questions . Many times it seems that what was already explained by the doctor , actually , has not sunk in ( … ) And so here they repeat the same questions many times , in different ways . What worries them a lot ( … ) is what will happen after discharge , when ‘I find him at home or in a rehabilitation clinic’” (Healthcare professional 13). Apprehension before surgery was observed in one patient, even though the patient claimed to have received very good information on how the surgery would be performed (Patient 2).
The time of waiting while the patient is in the operating theatre seems endless for family members, and waiting without information is a cause of anxiety (Healthcare professional 6). Professionals recognize the importance of informing the patient and family members about procedures, clinical pathways and pain management, before surgery (Healthcare professional 1, 2, 4, 7).
The covering patient-professionals relationship
The relationship between patient and professionals is a key issue for the quality of the service perceived by the patient, even when the health care provider fails to respond immediately to the patient's needs. Indeed, as many as 35 touchpoints occur throughout the patient journey ( Table 3 ). What the patient thinks and feels on this topic, emerges especially from the interviews, while the shadowing is not able to immediately capture thoughts or observations re-elaborated by the patient. In particular, when interviewed the patients remember, even after some time, some aspects of the relationship with professionals that are not directly related to clinical care, but which are perceived as being of value for the patients, since in these they receive attention as an individual. Even after some time, a patient remembered: “Early in the morning the nurse came to say goodbye before she went off duty , because I was being discharged later that day , so she wouldn't see me again . Really good . ” (Patient 3). A patient also remembered a rough response to a request for help to get dressed after the X-ray during outpatient clinic examination (Patient 2). Moreover, a patient pointed out how reassuring the relationship with the surgeon could be just before the surgery (Patient 3). One of the key moments appears to be the contact with the anaesthesiologist and the surgeon while the patient is waiting in the operating theatre: “Then the anaesthesiologist told me ‘Don’t worry , my dear , we do the epidural , we will sedate you’” (Patient 1). From the professionals’ perspective, the relationship with the patient is a key point to "buffer" a series of disruptions in the hospital journey and to reassure the patient: “ Patients always thank us because even if there is a gap in the organization and the patient has to wait a little , we apologize in the best way , with a smile" (Healthcare professional 3). As the nurse is the first person patients encounter when entering the ward, she knows she has the important role of reassuring patients by explaining to them how to orientate themselves in the ward and which procedures will be carried out, even if patients should already have been informed about all these things (Healthcare professional 4). Professionals recognize the importance of calming patients through interaction with the surgeon especially when they are waiting just before surgery (Healthcare professional 3, 13). An orthopaedist reports, “When you check or welcome the patient in the operating surgery where the surgeon and the anaesthesiologist are , the patient sees them and this helps him or her a lot , and so one thing that I think is in our favour ( … ) is communication , the possibility of having a point of reference” (Healthcare professional 3).
The effectiveness of family closeness
Family closeness is felt to be important for both patients and professionals, if programmed at the right times of the clinical journey. From the patient interviews and from shadowing it emerges that patients like family members to stay with them when waiting for surgery (Patient 4, 9). Once the surgery has been performed, when fears are diminished and pain is controlled, patients do not consider the presence of family members necessary, in particular immediately after returning to the ward from the operating theatre (Patient 1, 4). From the shadowing it emerges that after the first few days, when patients have recovered from the post-operative stage and close assistance has diminished, they then like to be with their family without interruptions for clinical-assistance reasons (Patient 10).
For professionals, family presence is important especially shortly before and after surgery, to reassure family members that the patient is doing well (Healthcare professional 5, 7, 13). When possible, professionals try to facilitate this, even outside regular visiting hours (Healthcare professional 13). In the days after surgery, “It is mainly relatives who come from outside the city who logically stay here , maybe in a hotel or some bed & breakfast , and would like to stay in the room all day; because they say–quite rightly , as I realize– : ‘But I have nothing else to do; my husband , my wife , my son is there . I'm with him’” (Healthcare professional 12). At this stage of the clinical journey, professionals do not see the closeness of family members as a need of the patient. Immediately after surgery, patients prefer to rest rather than having many people in their room. Conversely, the presence and closeness of family can greatly affect the patient experience in the rehabilitation period, especially when it comes to discharging elderly patients (Healthcare professional 15).
The micro-integration of hospital services
Even for a relatively simple routine surgical pathway, patients go through multiple stages. The behind-the-scenes coordination remains invisible to them and they are able to capture only some of the effects related to it. By contrast, professionals emphasize many critical issues in the management of the patient journey that affect the patient's experience.
When interviewed, patients reported the difficulty of having to move from one clinic to another during the outpatient clinic examination (Patient 1). Before hospital admission, an admissions office administrator shows how necessary it is to “decrease calls to the patient ( …), also depending on their age which is on average quite advanced …. cut out some calls that often from their point of view are unconnected . For instance , on one day I call you for admission , then the doctor calls you for blood tests , then another doctor calls you to arrange the meeting ( …), then if you take cardioaspirin the doctor calls you to give you information on cardioaspirin … All these calls could be grouped into maybe one by the doctor and one by the administrative staff” (Healthcare professional 10). At the time of hospital admission some critical points are revealed by the shadowing. After arriving at the hospital, patients waited an average of 21 minutes before being taken in charge by the Administrative Office to carry out admission procedures. At the end of the administrative registration procedures, patients made their own way to the ward, taking an average of 11 minutes. In this time, patients could get lost; they experienced anxiety about not getting to the right place, and waited outside the closed door of the ward without knowing what to do (Patient 5, 6, 7, 9). During their hospitalization, patients reported a lack of communication: a drug intolerance reported in their previous admissions had not been recorded in the notes. Orthopaedists reported critical issues concerning the management of operating theatres, such as delays in transporting patients from the ward to the operating theatre or delays in preparing the operating theatre for the next operation (Healthcare professional 2, 3). The accumulation of such delays could lead to the cancellation of the last scheduled patient, with a negative impact on the patient who had been waiting in a state of anxiety for many hours (Healthcare professional 2). A head nurse reported that waiting for transport to and from the radiology department for the post-operative radiography could slow down all the care processes, make the patient wait unnecessarily, and increase the pain, due to the temporary suspension of the continuous-infusion pain-killer (Healthcare professional 12). Finally, a patient reported that she was offered no choice when she was transferred to the rehabilitation unit recommended by the doctors, and she expressed the desire for a follow-up visit by the same doctor who had operated on her (Patient 1).
Exploring the individual patient journey can lead healthcare organizations to improve patient experience by focusing on the patient perspective, rather than the provider perspective [ 39 ]. Understanding what organizations can do to improve patient experience is critical [ 40 ]. However, the literature is still exploring the best methods to capture the patient's experience [ 17 , 23 , 30 ]. This study deals with the lived experience of orthopaedic patients by capturing the different points of view of patients and professionals on individual hospital patient journeys. Patients’ reported experience is analysed by shadowing them during hospitalization and by interviewing them at the end of the whole journey.
Historically, researchers and health care managers have focused on the study of how to achieve effective care through the definition of clinical pathways and by increasing patient adherence to treatment. However, reducing the patient's path to the clinical perspective may fail to reveal aspects that are relevant to patients, that influence their experience and their perception of quality of service [ 42 , 42 ]. In this study on patients’ hospital journeys, some important issues emerged through the shadowing of the hospital journey of the patients, and interviews with the key players. With the integrated use of these methods it was possible to identify which touchpoints are most critical for the patient, when family closeness is most effective, and how professionals can provide for the needs shown by patients over the entire journey. If on one hand the study of clinical pathways is now heading towards the active involvement of patients in decisions related to their own health issues [ 43 ], on the other hand the analysis of the hospital journey from a patient perspective can lead organizations to improve cross-hospital processes by creating procedures and focusing healthcare professionals on overall patient experience.
In line with Liberati's analysis [ 30 ], the shadowing method can contribute to patient-centredness by considering all the aspects of service delivery, not just the clinical one. In this study, both interviews and shadowing are able to “see the world from someone else’s point of view” [ 24 ]. However, the patient’s observations, focused on the whole service experienced, can reveal areas of potential improvement of the patient experience not otherwise identifiable. Shadowing highlights what the patient experiences in the different contexts and when going through one service and on to another, which professionals do not see since this falls outside the scope of their direct responsibility. Moreover, unlike using diaries completed by patients [ 23 ], this methodology allows the patient to be observed in the moment and in the spaces in which the relationship with the professionals takes place. However, this necessarily determines a subjective interpretation of what the researcher observes with respect to what the patient affirms.
Unlike what was pointed out by Gill [ 44 ], when dealing with the patient journey perspective, shadowing has an important potential for revealing invisible steps and spaces of the journey, more than intimate spaces and micro-processes of the decision. It is true that even now, in the healthcare sector, the provider establishes the patient path, while the patient is 'carried forward' through processes designed and managed by others.
In this study, when interviewed after time, patients focused on the overall clinical experience, forgetting other issues related to their hospitalization. For example, when interviewed, patients reported that they had had all the information they needed, while when shadowed shortly before the surgery the same patients appeared lost and asked for information from all the professionals they met. These data are also confirmed by interviews with professionals, who reported how highly emotional touchpoints, such as telling the patient they needed an operation, or the time immediately before transfer to the operating theatre, may affect patients’ perceptions and the effectiveness of the information [ 41 , 45 ]. As suggested by Ziebland, there is a difference between what patients said they experienced and what they actually experienced in real-life settings [ 20 ]. In this sense, the use of shadowing helps to understand the experience in a real time context. Moreover, it is always useful to evaluate whether the tools and information methods used for giving information to patients are effective, and which is the best moment for each patient to receive all the information they need, by considering their ability to absorb the information in a stressful situation [ 46 – 48 ].
In this study, both patients and professionals recognized the value of a personalized relationship in improving patient experience. Moreover, professionals report how a good relationship with the patient can compensate for the organization's inefficiencies. Interaction with the patient is especially important in the perceived patient-critical touchpoints. However, relevant steps of the journey are different from patients’ and from professionals’ points of view. From the patient’s point of view, the most critical steps occur when entering the hospital and just before surgery, where their emotional involvement is greater. On the other hand, from the professionals’ point of view, planning hospitalization and preparing patients for surgery is one of the most critical steps that affect patient experience. Indeed, patients, when interviewed, seem not to perceive critical issues in what happens ‘behind the scenes’, while professionals are able to identify issues related to the organization that can positively or negatively affect patients’ experience. These results highlight how frontline professionals are the key players in transforming organizational procedures into personalized care pathways, but the misalignment of views should be considered when improving the hospital journey by including the patients’ perspective.
The study has important limitations with respect to the sample and the setting considered and therefore its potential for generalization may be limited. The issues that emerged would need to be studied in depth in different care settings and with other types of patients to allow comparison of data and methodologies.
Patients’ experiences have become increasingly central to assess the performance of healthcare organizations and to redesign the services around the real needs of patients [ 20 , 41 , 42 , 45 , 49 ]. In this study, the analysis of the hospital journey from the patient perspective and the integration of three different standpoints, patient shadowing, healthcare professional interviews and patient interviews, highlights important areas of improvement otherwise hidden by the analysis of the clinical pathway only.
The nature of the study and its originality by subject matter and methods adopted can stimulate both academics and healthcare managers to explore important new fields. On the one hand, it is important to further investigate methodologies for capturing the patient experience and use it deeply and effectively at various organizational levels. In this way, shadowing seems to give a more patient-centric perspective, but it raises questions about its effectiveness as a single methodology for gathering the whole patient experience within a complex hospital process. On the other hand, the results of this study are a starting-point for healthcare managers who want to improve a key cross-functional hospital process in which the patient is the main actor. By considering the overall patient experience, as well as services performance and clinical pathways, they will able to create a distinctive value both for the patient and for the organization.
Acknowledgments
We are grateful to Eugenia Di Sabatino and Michela Ceri for their contribution to data collection.
- View Article
- PubMed/NCBI
- Google Scholar
- 6. The Beryl Institute Website, Defining Patient Experience. Available from: http://www.theberylinstitute.org/?page=DefiningPatientExp . Accessed April 20, 2019
- 10. Litvak E. Managing Patient Flow in Hospitals: Strategies and Solutions, Joint Commission Resources; 2nd Ed. Eugene Litvak Editor; 2010.
- 11. The Health Foundation. Improving patient flow. Learning report. The Health Foundation, 90 Long Acre, London WC2E 9RA; 2013.
- 19. Czarniawska B. Shadowing and Other Techniques for Doing Fieldwork in Modern Societies. ISBN: 978-91-47-08780-8. Liber/Copenhagen Business School Press; 2007.
- 20. Ziebland S, Coulter A, Calabrese JD, Locock L. Understanding and using health experiences. Oxford University Press; 2013.
- 37. Plutchik R. The Nature of Emotions: Clinical Implications. In: Clynes M., Panksepp J. (eds) Emotions and Psychopathology. Springer, Boston, MA; 1988.
- 38. Benner P. From novice to expert: Excellence and power in clinical nursing practice. Menlo Park: Addison-Wesley:13–34; 1984.

IMAGES
VIDEO
COMMENTS
Journey maps provide a way to visualize the internal and external factors affecting patient flow and the different paths patients must take in order to reach their care goals. ... Patient journey mapping is a great resource to use when defining patient satisfaction metrics and identifying gaps in how you currently gather insights.
Patient journey mapping is an emerging field of research that uses various methods to map and report evidence relating to patient experiences and interactions with healthcare providers, services, and systems. ... It is an emerging field with a clear patient-centred focus, as opposed to studies that track patient flow, demand, and movement. As a ...
Define the stages. Outline the patient journey by mapping out each stage and interaction with the healthcare system. This can include pre-visit, during a visit, and post-visit experiences. Tip: To speed up the process, run a journey mapping workshop with your team. It will help with the next step, too.
Process mapping enables the reconfiguring of the patient journey from the patient's perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital. Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the ...
The patient journey is the entire sequence of events that begins when the patient first develops a need for clinical care and engages with your organization. It follows the patient's steps as they navigate your healthcare system, from initial scheduling to treatment to continuous care.
Patient flow is the movement of patients through a healthcare facility. It involves the medical care, physical resources, and internal systems needed to get patients from the point of admission to the point of discharge while maintaining quality and patient/provider satisfaction. Improving patient flow is a critical component of process ...
Therefore, hospitals can significantly improve the quality of the service provided by exploring and understanding the individual patient journey [ 12 - 14 ]. Many tools may be used to measure and understand patient experience [ 15, 16 ]. Surveys are the methods mainly used to capture the patient experience and to evaluate the quality and ...
The patient journey is best described as the sequence of experiences a patient has from admission to discharge. This includes all the touchpoints between the patient and provider from beginning to end. A patient's journey begins before they even walk through the doors of a doctor's office or hospital. It may start when they research ...
Schwannomatosis. A "Patient Journey" is a personal testimony that reflects the needs of patients in two key reference documents—an accessible visual overview, supported by a detailed ...
Impact. Patient journey mapping is a rapidly growing approach for better understanding how people enter, experience and exit health services. This type of methodology has significant potential to inform new, patient centred models of care and facilitate clinicians, patients and health professionals to better understand gaps and strategies in health services.
Patient journey mapping is a process that helps you—as healthcare providers—to visualize the complete experience of your patients who seek and use your care services. This includes every single touchpoint (whether online or offline) that a patient encounters in the process of finding a care provider, scheduling an appointment, to having the ...
Patient journey mapping works to identify and understand the details of all patient touchpoints within a specific healthcare experience. It helps you visualize the process patients go through to receive care, complete a treatment plan, and/or reach a desired outcome. ... increasing patient flow and cutting operational expenses.
A patient's journey map tells providers and researchers where common risks arise and how to influence patients for better outcomes. You need to collaborate with health care providers to ensure your patient journey mapping is complete. Big data, artificial intelligence, and digital technology make patient journey mapping possible in healthcare.
4. Identify Contact Channels. Patients engage with the health center through various channels throughout the patient journey. These channels, such as the health center itself, can be physical or online, including social media, email, applications, websites, and online forms.
Patient Journey Improvement Solutions. If you want to enhance patient flow management and boost patient satisfaction at your hospital, we recommend using pre-engineered solutions. There are many ways to improve the quality of service you provide to your patients. One such solution is the Wavetec patient flow system.
Understanding patient flow vs. patient journey helps providers streamline processes and enhance the overall quality of care. Patient flow refers to the movement of patients through the various stages of the healthcare delivery process, from the initial point of entry to the final discharge or follow-up. It encompasses the coordination of ...
Therefore, hospitals can significantly improve the quality of the ser-vice provided by exploring and understanding the individual patient journey [12-14]. Many tools may be used to measure and understand patient experience [15, 16]. Surveys are the methods mainly used to capture the patient experience and to evaluate the quality and safety of ...
Patient journey analysis — also called patient flow analytics — allows us to observe the patient encounter at each stage, from symptom diagnosis to disease progression, treatment and resolution. Patient journey analysis involves a patient's interactions with doctors, health care providers and
Digging a bit deeper, patient flow is the groundwork - the basic framework ensuring that a healthcare system operates smoothly, just like how the kitchen needs to function efficiently to deliver your meal on time. On the other hand, the patient journey is more like the seasoning added to our dish. The distinctive blend of individual ...
Through a thematic analysis, we identified an understanding of the care pathway as both patient flow and the patient's journey and a dilemma between the two, and we discuss how the negotiation of conflicting institutional logics is a central part of care pathway implementation.
Use Creately's user-flow flowcharts to map out the different paths patients take when interacting with the healthcare system. Referring to the flowcharts, identify the minor and major touchpoints and the patient goals associated with them. Add them to your patient journey map. With the help of the information you have gathered, identify the ...
Results This study (conducted from the last quarter of 2019 through September 2022) resulted in a remarkable improvement in patient flow, as evident from the reduction in average hospital length of stay (from 11.5 to 4.4 days) and average emergency department boarding time (from 11.9 to 1.2 hours) and the improvement of bed turnover rate (from 0.57 to 0.93), (p<0.001, p=0.017, p=0.038 ...
Respiratory drive is defined as the intensity of respiratory centers output during the breath and is primarily affected by cortical and chemical feedback mechanisms. During the involuntary act of breathing, chemical feedback, primarily mediated through CO2, is the main determinant of respiratory drive. Respiratory drive travels through neural pathways to respiratory muscles, which execute the ...
Purpose To understand how different methodologies of qualitative research are able to capture patient experience of the hospital journey. Methods A qualitative study of orthopaedic patients admitted for hip and knee replacement surgery in a 250-bed university hospital was performed. Eight patients were shadowed from the time they entered the hospital to the time of transfer to rehabilitation ...