21 Tips for Traveling With Diabetes

Plan ahead for more fun and fewer worries.
Don’t let good diabetes management go on vacation just because you did. Traveling to new places gets you out of your routine—that’s a big part of the fun. But delayed meals, having unfamiliar food, being more active than usual, and being in different time zones can all disrupt your diabetes management. Plan ahead so you can count on more fun and less worry on the way and when you get to your destination.

Before You Go
- How your planned activities could affect your diabetes and what to do about it.
- How to adjust your insulin doses if you’re traveling to places in a different time zone.
- To provide prescriptions for your medicines in case you lose or run out of them.
- If you’ll need any vaccines.
- To write a letter stating that you have diabetes and why you need your medical supplies.
- Just in case, find pharmacies and clinics close to where you’re staying.
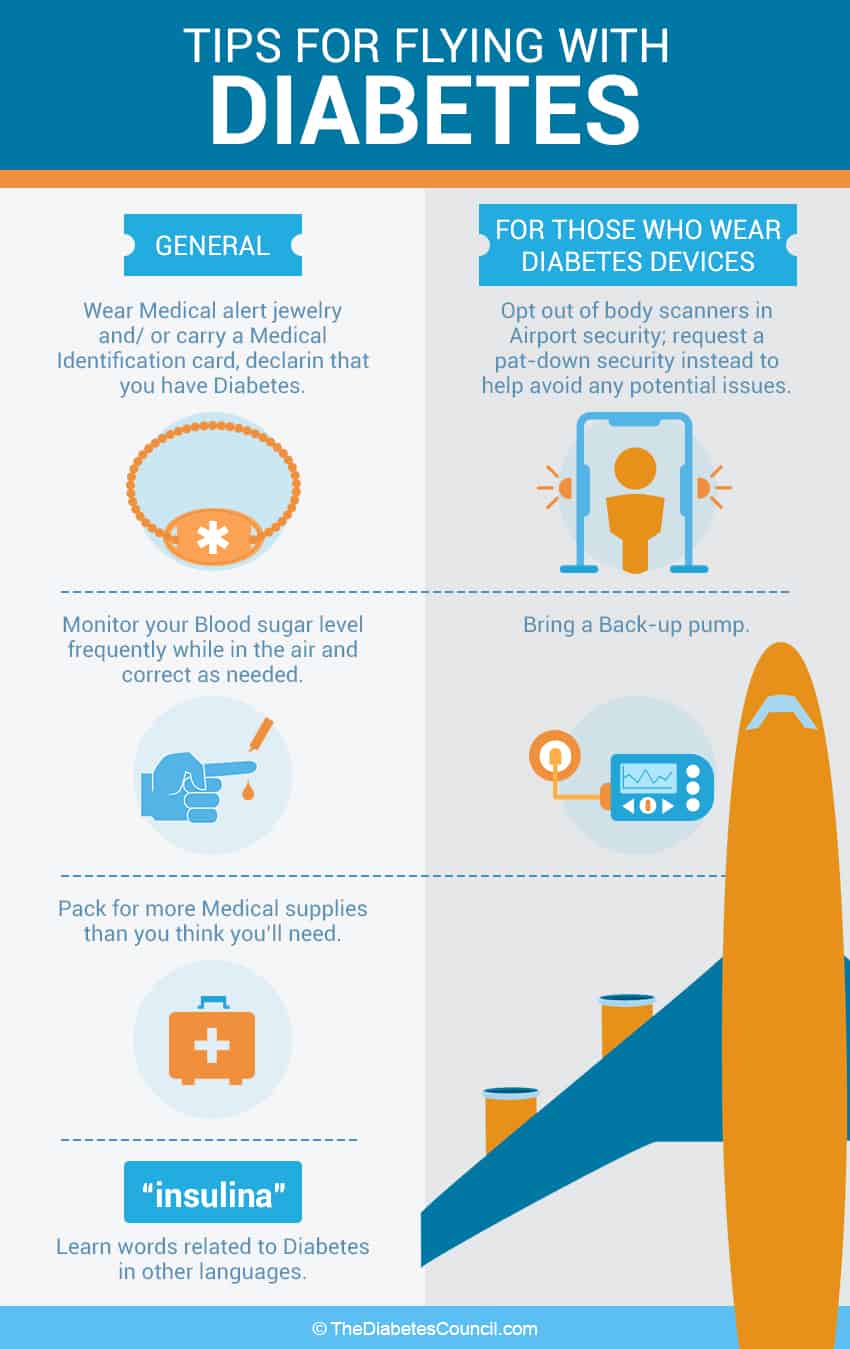
- Get a medical ID bracelet that states you have diabetes and any other health conditions you may have.
- Buy travel insurance in case you miss your flight or need medical care.
- Order a special meal in advance for the flight that fits with your meal plan, or pack your own.
- Put your diabetes supplies in a carry-on bag (insulin could get too cold in your checked luggage). Think about bringing a smaller bag to have at your seat for insulin, glucose tablets, and snacks.
- Pack twice as much medicine as you think you’ll need. Carry medicines in the original pharmacy bottles, or ask your pharmacist to print out extra labels you can attach to plastic bags.
- Be sure to pack healthy snacks, like fruit, raw veggies, and nuts.
- Get an optional TSA notification card [PDF – 23.8KB] to help the screening process go more quickly and smoothly.
- Good news: people with diabetes are exempt from the 3.4 oz. liquid rule for medicines, fast-acting carbs like juice, and gel packs to keep insulin cool.
- A continuous glucose monitor or insulin pump could be damaged going through the X-ray machine. You don’t have to disconnect from either; ask for a hand inspection instead.
- Visit CDC’s Travelers’ Health site for more helpful resources.
- Doctor’s letter and prescriptions
- Snacks and glucose tablets
- Extra insulin and diabetes medicines
While You’re Traveling
- If you’re driving, pack a cooler with healthy foods and plenty of water to drink.
- Don’t store insulin or diabetes medicine in direct sunlight or in a hot car; keep them in the cooler too. Don’t put insulin directly on ice or a gel pack.
- Heat can also damage your blood sugar monitor, insulin pump, and other diabetes equipment. Don’t leave them in a hot car, by a pool, in direct sunlight, or on the beach. The same goes for supplies such as test strips.
- Fruit, nuts, sandwiches, yogurt
- Salads with chicken or fish (skip the dried fruit and croutons)
- Eggs and omelets
- Burgers with a lettuce wrap instead of a bun
- Fajitas (skip the tortillas and rice)

Say goodbye to worry when you pack your diabetes supplies in a carry-on bag.
- Stop and get out of the car or walk up and down the aisle of the plane or train every hour or two to prevent blood clots (people with diabetes are at higher risk).
- Set an alarm on your phone for taking medicine if you’re traveling across time zones.
Once You’re There
- Your blood sugar may be out of your target range at first, but your body should adjust in a few days. Check your blood sugar often and treat highs or lows as instructed by your doctor or diabetes educator.
- If you’re going to be more active than usual, check your blood sugar before and after and adjust food, activity, and insulin as needed.
- Food is a huge highlight (and temptation!) on a cruise. Avoid the giant buffet, and instead order off the spa menu (healthier choices) or low-carb menu (most ships have one) or order something tasty that fits in your meal plan from the 24-hour room service.
- Don’t overdo physical activity during the heat of the day. Avoid getting a sunburn and don’t go barefoot, not even on the beach.
- High temperatures can change how your body uses insulin. You may need to test your blood sugar more often and adjust your insulin dose and what you eat and drink. Get more hot-weather tips here .
- You may be unable to find everything you need to manage your diabetes when you are away from home, especially in another country. Learn some useful phrases in the local language, such as “I have diabetes” and “where is the nearest pharmacy?”
- If your vacation is in the great outdoors, bring disposable wipes so you can clean your hands before you check your blood sugar.
Making Memories
Diabetes can make everyday life and travel more challenging, but it doesn’t have to keep you close to home. The more you plan ahead, the more you’ll be able to relax and enjoy all the exciting experiences of your trip.
- CDC’s Health Information for Travelers
- Diabetes Basics
- Living With Diabetes
- Diabetes Features
- CDC Diabetes on Facebook
- @CDCDiabetes on Twitter
To receive updates about diabetes topics, enter your email address:
- Diabetes Home
- State, Local, and National Partner Diabetes Programs
- National Diabetes Prevention Program
- Native Diabetes Wellness Program
- Chronic Kidney Disease
- Vision Health Initiative
- Heart Disease and Stroke
- Overweight & Obesity
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar
- Skip to footer

Everything You Need To Know About Traveling With Diabetes
Modified: Jun 16, 2020 by Lianne Fachetti, ABA · This post may contain affiliate links ·
Having diabetes does not mean you should be within the confines of your home. By doing some smart planning and thorough preparation, you can go anywhere whether it is a camping excursion, a cross-country train adventure, a relaxing cruise , or a trip to various countries. Although vacations can be fun and rewarding, you have to be aware that traveling can be stressful to your body as you stray away from your daily routine and diet plan . At the same time, foreign surrounding may also put your psychological well-being into an anxious state. All these changes can contribute to a fluctuation in your blood glucose level. To help you prepare for your upcoming trip, whether by car, air or boat, we have compiled an ultimate guide of useful information to educate you better on various topics concerning traveling with diabetes:
[accordions id="2133"]
Is it Safe to Travel as a Person with Diabetes?
Involving your medical team in your travel plans, hot climate vs. cold climate, tips on preparing for emergency situations, remember to get travel insurance, maintaining control of your blood glucose level while on vacation, how to pack your medications and diabetes supplies, how to safely dispose of your used supplies, traveling by air, traveling by sea, traveling by train, traveling by car, traveling by foot, eating during traveling, factors to consider during hotel stay, how to handle jet lag and switching time zones, travel dose = usual dose x (0.9 – no. of time zones you are crossing ÷ by 24), important information about insulin, useful information to keep on hand, gestational diabetes and traveling, over to our readers.

To avoid unexpected health issues that could possibly arise during your journey, you should consider going for a medical examination to ensure your diabetes is in stable condition and you are physically well to travel. It is important for you to ask your doctor whether you are fit to travel in your current condition as it can play a crucial role when purchasing your itinerary as well as your travel and health insurance .
You should always request that your doctor put his professional opinion in writing so that if you need to cancel your trip as a result of sudden health emergency situation, you have the doctor’s letter as a proof of evidence and get compensation for any incurred loss from your insurance company.
For more diabetes related information:
- 7 Mistakes Doctors Are Making with Diabetes
- Can Diabetes Bankrupt a Country?
- What are Blood Sugar Target Ranges? What is Normal Blood Sugar Level?
- Why Do Parents of Type 1 Kids Fear the Night?
Aside from the professional standpoint of view, you should ask yourself whether you are physically and psychologically prepared to take a trip. If you recently found out that you have diabetes or if you have never been on a trip before, you may consider wanting to go on a long vacation . Instead, you can choose to embark on a short excursion closer to home to test the water first. From there, if you are comfortable with managing your blood glucose level on the road, you can then ease yourself to going on longer journeys further away from home.
Planning your Schedule Timeline Before Taking Off
- Consult with your doctor about traveling and make sure that your passport has not expired (before planning a trip)
- Plan travel itinerary and make bookings (at least 3 months prior to trip)

- Arrange travel insurance and health insurance (3 months prior departure)
- Check vaccination requirements (sometimes vaccines require booster shots one month after the first vaccine shot) and talk with your doctor about getting the vaccination, paperwork, and prescription for the trip (2 months to departure)
- Ensuring that all your travel insurance paperwork and payment are confirmed, and all your medical needs have been prepared (1 month prior to departure)

As your medical team has much more experience dealing with their patients traveling, they can immediately offer you with a lot of crucial planning and preparation information regarding your destination and how to prepare accordingly for the trip.
Notify Your Doctor about Your Plans
Aside from getting the preliminary go-ahead letter from your doctor, you will need two more paperwork from your doctor:
- A letter that explains your current diabetes condition, your medication treatment and dosage. It should include a list of all the medical equipment and supplies , medicine, and emergency food and snacks you must hand carry with you at all times. This list is crucial if you are traveling by air or crossing the Canadian/Mexico border as it is a proof of evidence that you should be allowed to hand-carry all these items with you at all times. If you do not have this list with you, the airport security officers will have the right to confiscate your medication and supplies due to violations of the liquid policies. Aside from this list, your doctor should also list any medication and food allergies you may have.
- A prescription for your diabetes medication, insulin refill, and blood testing equipment. If an accident occurs where you lose or damage your medicine/equipment, you can immediately get a replacement by visiting the nearest pharmacy. Please note that in the United States, the prescription regulations and limitations varies from each state. And if you are traveling out of the country, you should research on the current diabetes laws concerning your medication and whether you can get a prescription for your current medicine in the destination countries. Sometimes, you may have to get a local brand and alter the dosage accordingly.
Consult with Your Dietitian and Diabetes Educator
Experts in their fields, your dietitian and diabetes educator have ample of information concerning medication and medical supplies, vaccination shots, diet plans and glucose counting skills, time zone adjustment techniques, and local food information.
If you wish to have variety and flexibility when it comes to dining on trips, you must learn how to count your glucose and calorie intake throughout the day. You can learn this skill from both your dietitian and diabetes educator. At the same time, your dietitian can offer you tips on what food choices to make when you are in a foreign country. If you are traveling to a location where starch is the main food group (for example, pasta and pizza are the common food staples of Italy, rice is the most common food staple in most Asian countries), your medical team can teach you how to gauge your food intake by using objects such as your phone or your hand as portion size estimation.
Aside from the usual infections and viruses to avoid, pregnant women should be aware of the Zika virus that can cause very serious cranial birth defects. As of now, there is very limited information on the treatment and prevention of the virus. It can be transmitted by mosquitos, sexual intercourse, blood transfusion, and laboratory exposure. As there are Zikainfection occurrences found around the world and even the United States, the Centers for Disease Control and Prevention has advised that all pregnant women should avoid prolong outdoor activities that may increase their chances of getting bitten by mosquitos and transmit the Zika virus to the unborn babies.
Risks of Long-distance Traveling
Studies have shown that the fluctuation of blood glucose level and the higher tendency for individuals with diabetes to experience dehydration raises the thickness of the blood and decreases the rate of blood flow. Consequently, this increases the chance for diabetes individuals to develop deep vein thrombosis (DVT). During long-distance traveling, extended periods of sitting makes the chance of developing deep vein thrombosis even higher. Once developed, you will experience frequent swelling, pain and soreness in your legs. If the blood clots travel to your heart or your lungs, you can experience sudden fatal complications such as pulmonary embolism, heart attack, and stroke.
Other Risks to Consider
Pregnancy can put you at a greater risk of dehydration and overheating in hot weather. Combined with physical activities that fluctuate your blood glucose level, you can increase your chance of miscarriage and premature birth. Common traveling diarrhea can also trigger severe low blood sugar level. If you experience an onset dizzy spell or seizure, you may pass out and injure your baby from the fall.
Extreme temperatures can make your blood glucose level go out of control. Under such circumstances, your body will be able to produce and process less insulin. At the same time, the extreme temperature can decrease the efficiency of your medical testing equipment and lower the effectiveness of your medications.
Traveling in Hot Temperature
To avoid dehydration and risking the chance of developing hyperglycemia, here are some tips to help keep your diabetes under control when traveling in hot temperature:

- Store your medication and supplies properly inside a temperature-controlled container. Avoid leaving them in the car as the interior can rise to 150 degrees in extreme cases.
- Avoid stressful physical activities during the daytime when the temperature is highest. Instead, stay in the shade or inside during the hottest part of the day.
- Check your blood glucose level more frequently so that you can adjust your medication and your diet accordingly to avoid drastic fluctuations
- Protect your skin by wearing breathable clothing, a hat, and sunscreen to decrease irritation and the development of fungal infection
- Apply sufficient amount of sunscreen to avoid sunburn. The skin condition can trigger inflammation reaction and increase your resistance to insulin
- Avoid caffeinated or alcoholic beverages as they will make you quickly dehydrated
- You may want to bring with you shoes that are slightly looser as your feet will likely s well a little from the extreme heat. Change your socks often and air out your shoes nightly to avoid bacterial growth
- Once you reach your destination, allow your body to adjust to the temperature change. Do not immediately jump into a busy schedule of sightseeing and any other physical activities. DO NOT OVEREXERT YOURSELF
Traveling in Cold Temperature

- Similar to extreme heat, extremely low temperature can make your insulin less efficient and kill the battery in your glucose monitor. When the outside temperature is below freezing, do not leave your medications and supplies in the car.
- Being in the cold temperature increases your chance of catching a cold or a flu. Before the trip, get a flu vaccination (consult your doctor first if you are pregnant).
- Wear thick socks and insulated shoes to protect your feet from possible cold sores and frost bites. Change out of damp socks and footwear as soon as possible. As diabetes patients have a higher chance of developing nerve pain and infection in their feet, cold sores, and frost bites can increase the chance of skin infection complications and may lead to gangrene
- Bundle up in warm clothing as cold temperature will trigger a spike in your blood glucose level. If your body is in a warm state, your blood glucose level will be less likely to fluctuate
- As your body can develop insulin resistance in cold temperature to keep you warmer, take caution what you eat as you can become more sensitive to sweet food. You may want to test your blood glucose level before and after your meals to get a better sense how your body is reacting in such weather condition
Tips on Adjusting to Different Climates
Aside from extreme temperatures, different climates can also affect your diabetes symptoms and your medical equipment. Although humid conditions may have very little impact on your blood sugar level, you may become much more susceptible to bloating and swelling of the feet. Your skin may develop a rash from the constant sweat and become prone to various skin infection such as athlete feet, gangrene, and yeast infection. To solve such problem, make sure to bring along foot powders and baby powder to absorb excess moisture. If you dislike powder, you can also put sweat control deodorant on your feet as it will help with the problem and make your feet less prone to blisters. When it comes to equipment problems, if you are a pump user, you may find it much more difficult to keep your pump infusion in place as your adhesive dressing keeps wrinkling and falling off from the moisture. To avoid such problem from arising, you may want to purchase a waist pouch to carry the pump instead.
As for arid regions, you can expect your skin to itch and chaff easily from the climate. Your current skin and hair regimen will be insufficient to keep you moisturize. If you are traveling to a dry area, you may want to switch to a more moisturizing shampoo and skin cream than your usual one. Dry regions can also pose a problem for your liquid medication and supplies. Once opened, the liquids may dissipate quickly from the heat. To avoid such problem, always keep your liquid supplies in ziplock bags when not in use.

When you have diabetes, always wear a medical ID bracelet no matter where you travel, whether you are within the country or in a foreign country. In case you have an accident or experience a hypoglycemic episode, the medical professionals will look for your ID to see how they can assist you. If you travel to a foreign country where English is not a common language, the American Diabetes Association (ADA) recommends that you should learn how to say “I have diabetes”, “I need medical help”, and “sugar” in the local language. If you have difficulty remembering or pronouncing the phrases, there are many translation mobile apps that can be of help. If you are not a mobile equipment user, you can always print out a translation page of common phrases and use it when various situations arise. Some of the other common phrases you will need to translate:
- Where is the nearest pharmacy?
- Where is the nearest washroom?
- I need help.
- No sugar please.
- No sauce please.
- Where is the nearest hospital?
When you are preparing for your trip, you will want to acquire a list of English-speaking doctors at your destination location from the International Association for MedicalAssitance to Travelers ( IAMAT ). Please note that the IAMAT will require a membership fee for such information and they will only refer you to English-speaking doctors that are within their clinic system. If you wish to compile a list of doctors without paying the fee, you can always visit the Embassy of United States website and search for the country you will visit. They will provide you with a list of contact numbers for various emergency situations such as passport loss, immediate financial assistance, and emergency medical help. You can also make a google search “ English-speaking doctors in _______ (insert your destination) ” as the local tourist websites may provide even more information concerning medical help. While you are doing your research, you should also plan and look up information on:
- What to do in the event you get sick while traveling/vacationing
- Scout for hospitals/clinics nearby
- Get to know the embassy in case something happens
- Do homework on the Transportation Security Administration and Diabetes rights about the destination
Travel insurance is essential when it comes to traveling for everyone no matter whether you suffer from diabetes or not. If you think that your current health insurance is enough to cover for your unexpected health expense oversea, you will find that the coverage is minimal. For more information about travel insurance, please refer to our article “ Diabetes Travel Insurance Guide ”.
Keep in mind that stress plays a significant role in your blood glucose fluctuation. Aside from the excitement of anticipation for the travel, the change in time zone and your daily schedule can really spike your blood glucose level. Even when you usually have a good control of your blood sugar, a walk around the city in a new surrounding and climate can throw your level out of the normal range due to all the undetected stress factors (for example, change in sleeping schedule due to time zone change, lack of sleep from jetlag, change in meal time schedule, adjustment to new local food choices). To ensure that your blood glucose level remains within your desired target zone, you need to monitor your fluctuation throughout the day before and after each physical activities and meals. Wherever you go, bring a handy source of glucose (for example, candy, glucose gel tablets, soda drink, or juice) to fix unexpected blood glucose drop. Small cans of juice and soda (they come in 5.5 oz. size) are available at many grocery stores .
While on vacation, insulin need changes from person to person; some people require an increase in insulin dosage during travel while others need to decrease their regular dosage. Time zone changes can really mess up the blood glucose level due to the lack of sleep and physical stress of adjusting to the change. For more information on how to adjust your medication schedule to the destination time zone, please refer to the section “ How to Handle Jet Lag and Switching Time Zones ”.
- All your diabetes-related medication
- All the insulin and syringe supplies you need for the trip
- Blood glucose testing monitor and strips (include extra new batteries for your monitor)
- Your emergency glucagon kit
- Over-the-counter medications such as anti-diarrhea tablets, antibiotic cream, anti-nausea medication, painkiller, stomach relief tablets
- Your diabetes identity card and logbook
- A supply kit of emergency snacks and glucose gel tablets for treating low blood glucose level
When you are packing, you should keep your backup medication and supplies in another bag so that in case you lose the original carry-on bag, you have the backup carry-on bag to fall back on. Other than the medical necessities you may need, you should consider other supplies that will be helpful to your trip. Some examples are sneakers, sunblock, hat, sunglasses, a mobile device with translation apps installed.
If you are traveling by air, you should always check the recent security changes in airport security as it will dictate how you will pack and plan for your travel. Here are some tips that can help make packing easier:
- Make sure all your medication are in the original bottle with their labels still intact so that the security can easily match your name on your flight ticket with the name listed on the medication bottle labels.
- Always have your doctor’s permission letter to travel and prescriptions (this includes any equipment prescriptions such as glucose monitor and insulin pump) ready.
- When you are packing your diabetes-related medication and supplies that come in liquid form: You may bring medical necessity liquids, medications and creams that are more than 100 milliliters or 3.4 ounces in your carry-on baggage. Remove these specific items from your carry-on luggage to be screened separately from the rest of your belongings. Please note that you do not need to place your liquid medication in a plastic ziplock bag.
- Ice packs, gel packs, and other medical-related accessories may be presented at the screening checkpoint in a frozen or partially frozen state. These accessories do not need to be accompanied by medication or liquids to be considered medical necessity. All medical supplies including syringes, IV bags, and insulin pumps must be screened before they are allowed to pass through the security checkpoint.
- Print out the regulations concerning carry-on items for medicine and medical-related supplies
- If you are a pump wearer, always have a backup for your travel. Before you pack for the backup, make sure that it works.
Air Travel and Pregnancy
If you do decide to travel by plane, you should check with the airlines on their regulations regarding pregnant women as some companies do not allow a woman over 35 weeks of pregnancy on board. Here are some advice that will help you be more comfortable during your travel:
- When you choose your seat, try to get a bulkhead seat or a seat next to the emergency exit as they have much more legroom than the other seats. If these options are not available, your next best choice is to pick an aisle seat as they allow you some more leg room and easy access to the washroom.
- Before you leave on your trip, make sure you have your doctor write you a permission note to prove that you are physically well to travel as well as a list of medication and supplies that you need to pack in your carry-on luggage so you can access it during the flight.
Here is a list of items you should have in your carry-on luggage medical kit :

- Your usual vitamins and supplements
- All your diabetes medication and supplies
- Urine dipstick for ketone level testing
- Your diabetes information logbook
- For safety reasons, always place your safety belt under your baby bump and across your lap.
- Once you have boarded the plane, let the flight attendants know that you have diabetes and require specific diabetes friendly meals. Although you may have selected the option when purchasing your flight tickets, there could always be errors. By alerting the attendants ahead of meal serving time, they can make sure to set aside a special meal for you.
- To avoid developing DVT and possible formation of blood clots, move and stretch your legs regularly while seated. Whenever you have a chance, stroll along the aisle for some exercise at least every half hour. If need be, you can always go to the end of the plane where there is some extra space for you to stand and stretch out. If there is heavy turbulence and you are unable to get up from your seat, flex and twirl your ankles to increase blood circulation. Should you have a family history of DVT, you may consider wearing pressure stockings during the flight.
- As mentioned earlier, dehydration can increase the chance of DVT. So remember to drink plenty of water to reduce the risk of dehydration. If you do not wish to constantly ask the flight attendants for water, simply ask them for a bottle of water that you can sip throughout the duration of the flight.
- If you are feeling light-headed and experiencing shortness of breath, ask the flight attendants to give you breathing oxygen (please note that there some airlines such as JetBlue that do not have medical oxygen onboard). Do not wait.
Tips for Going Through Security Checkpoints

Going through the airport security can be a real troublesome for anybody. With all the medication and supplies in your carry-on baggage, the process can turn into a nightmare. To avoid missing your flight, always give yourself plenty of time to check in and go through the security checkpoints. To make the process more straightforward, always immediately alert the security officer of your diabetes condition and supply them with your doctor’s note and prescription before putting any of your medication or supplies through the scanner. It is a great idea to label every medical item so that they do not need to ask you what each item is.
During the process, should you feel lightheaded or sense that your blood glucose level is dropping too low, alert the officers that you need your medication. If you do not explain your symptoms right away, the officers may suspect that you are either intoxicated, under certain drug influence, or coming under a virus such as Zika and deemed unfit for the travel. By being forthcoming with your condition, you will minimize any suspicion concerning your medication and supplies. During the process, remain calm. If for any reason the officer is not permitting you to carry any of your needed medication or supplies that are deemed safe to be stowed in your carry-on luggage, take out your printed regulation concerning your medication and supplies and calmly address the problem.
If such officer continues to be difficult and the discussion becomes uncomfortable, you can ask to speak to the Transportation Security Officer (TSA) Supervisor. If for any reason where the supervisor is unable to resolve the problem, you should ask for the TSA Customer Service Manager for assistance or contact 1-866-289-9673 . Do not let this single incident deter you from going on your trip. If you think that you have been treated unfairly or have been discriminated based on your medical condition, you can always report your experience to 1-800-DIABETES for legal assistance. You can also file a complaint to the Disability and Multicultural Division of the United States at [email protected] .
TSA Precheck Status

If you are a frequent flyer, you may want to look into the TSP Precheck program. It costs $85 for domestic security lines and $100 for international security lines. The status is good for 5 years. If you are approved by the program as a person with diabetes, you can by-pass many of the stringent checkpoint screening process. As a person with diabetes, you can use the TSA Precheck lanes where you do not need to remove your shoes, laptops, liquid items, belts, and jackets during the screening process. These steps can truly save you a lot of time and trouble explaining about all the medical supplies and medication you are carrying in your carry-on luggage.
Tips for Pump Wearers
Even though insulin pump manufacturers indicate that pumps can safely pass through the security systems without triggering the alarm to go off, it is always much easier to alert the security officers that you are currently using an insulin pump and would like a visual inspection instead. At the same time, you should explain to the officer that your pump cannot be removed for inspection because 1) it is connected to a catheter inserted under your skin, and 2) it is currently working to provide you with insulin.
Regulations Regarding Pump and Continuous Glucose Monitor
If you use an insulin pump or use a continuous glucose monitor (CGM), you must contact your airline before travel, if possible a few weeks before you fly. The Diabetes Association recommends that individuals with diabetes should always contact their airline to discuss the safety concerning medical devices they intend to take on board. Some airlines do require that you notify them of your medical equipment in advance and fill out additional paperwork before you fly. If you fail to alert them ahead of time, you may not be allowed to use your pump or CGM while in flight. For more information about airline regulations and your medical equipment, you should speak to your diabetes team about what you can do if the airline will not let you use your pump or CGM on board. You may ask "why is there such a big deal about insulin pumps and CGM?" The reason is that certain models have wireless functions that may interfere with aircraft navigation systems during take-off and landing. If your pump or CGM must use wireless to function properly, it may be a good idea to switch to another model that do not require a wireless function for your vacation purpose. If you do choose to use your wireless-included equipment, you may need to turn off your CGM and pump during the take-off and landing of the aircraft.
Dealing With High Altitude
Sometimes our devices and medication are made to work within a specific criteria, and when we are outside of that range, things do not work as planned. Meters often require the use of oxygen to work properly. Oxygen decreases in high altitude, and the performance and reliability of the meter also decreases.
You can find high altitude at many ski resorts around the country when you plan on doing your winter sports. There are several cities with high altitude across the globe that you must be aware of. Some of the more common cities of high altitude are:
- Colorado Springs, USA (1840 meters, 6040 feet)
- Mexico City, Mexico (2200 meters, 7220 feet)
- La Paz, Bolivia (3640 meters, 11940 feet)
It's estimated that the meter under estimates blood glucose levels by 1-2% for every 1000 feet or 300 meters. This means that if you live in La Paz, it can be off by up to 25%.
Some recommended tips are to:
- Check blood glucose levels as often as possible
- Listen to your body and see the ways it adapts to altitude.
- Cross check your blood glucose levels with multiple meters or methods.
- Speak to your doctor to help come up with a plan before going to a high altitude environment.

If you are going on a cruise, remember to pack your workout shoes. Unlike other ways of traveling, cruise ships have many exercise facilities and activities to offer. If you are not interested in any of the activities, you can still get a good workout by simply strolling through the huge cruise ships. And if you wish to join certain fitness activities, note that fitness instructors on the cruise ships are usually all certified trainers and are familiar with various medical conditions that may occur from an injury or an intense workout. However, in order to be safe, make sure you are aware of what your physical limitations are.
When it comes to cruise ships, the most devious attraction is the food. It is everywhere 24/7 and mostly free. There are so many restaurants , snack bars, cafes filled with all the gourmet pizzas and burgers. Even when you are at the pool, you cannot escape from the ice cream, soft drinks, and alcoholic beverages. As a person with diabetes, all these temptation can derail your blood glucose level VERY quickly. Instead of gorging on all the food immediately, pace yourself and let maître know what you need. He or she will let you know which dishes can be altered to fit your needs. To take it one step further, you can always tell your travel agent when you book your cruise, and submit your requirements in writing. Certain cruises will take the extra step to group you with other persons with diabetes individuals so that you can all support each other and share common experiences. They will make sure that your tables will have foods made specially for your medical needs. Instead of having the dessert of the day, the chef will make sure to provide fresh fruit or sugar-free dessert for your table.
When it comes to medical assistance, make sure to carry enough medicine and supplies that will last you the whole excursion because cruise ship does not have a pharmacy. If you think that you are getting close to running out a certain medicine or supply, you will need to wait until the cruise ship makes a shore stop when you can get to a local pharmacy to refill your order. As for medical treatments -- even though cruise ships do have medical facilities, they are usually not equipped to provide treatment for any complicated health emergencies. If something serious happens, the medical professionals will stabilize your condition and transport you to a hospital on-shore as soon as possible. With minimal traveling emergency coverage, your regular health insurance policies will not be enough to cover those fees. It is best to subscribe to a traveling insurance to avoid an insanely high medical bill.
For more information about traveling on a cruise ship, please visit our article “ Managing Your Diabetes on a Cruise ”.

If you are traveling via Amtrak, their long distance trains have full-service dining cars that serve hot meals prepared on-board by trained chefs. For First Class passengers, all Auto Train passengers, and passengers with sleeping accommodations, all meals are included in the train ticket prices. Coach Class passengers who wish to dine at the dining cars can do so for an additional charge. After boarding, it is best to alert the dining car staff members that you have diaetes when reserving your dining time. If you want to plan ahead and see what the dining cars have to offer, please visit the AMTRAK website for their updated dining car menus. To make it convenient for individuals with special diet needs, AMTRAK has provided a food fact guide for all their menu items so that you can easily count your glucose and calories intake.

If you are going on a road trip by driving, you should plan for frequent rest stops. Rest stops are not just for bathroom breaks. They are an excellent place to get out and stretch your legs after being stuck in the car for hours. Sitting still for too long during your trip can lead to blood clots. Try moving around every few hours. At the same time, you can check your blood glucose level, grab a small snack, and look at the map ahead. These days, with the available mobile apps, you can see whether the traffic will thicken due to car accidents. Instead of getting stuck in the traffic, you can pick another route or rest your eyes before you start the car again. You should never drive more than 12 hours at a time and should also never drive straight for 6 hours without eating a meal.
If you are driving, it is vital that you check your blood sugar level every 4 hours (more frequently if you are pregnant or have a tendency to experience hypoglycemia). You should be very aware of signs for low blood sugar level. If you feel slightly dizzy or lightheaded, safely pull over to the side of the road quickly and take a fast-acting sugary snack (for example, candy, juice, glucose tablet). Then, follow the treat with a meal as soon as possible. After the meal, take a reading of your blood glucose level. If the reading is less than 6 mmol/L, refrain from driving. If you feel that your condition is not getting better or even worsening, call for emergency health assistance right away. If you are the passenger, have the driver take you to the nearest emergency health facility. Do not wait.
One of the most important thing you need for a road trip is a cooler to keep all your medication and supplies at a relatively constant temperature away from the heat. If you think that the cooler may be getting a little too warm, you can always stop by a gas station and purchase a cool jug of water and a few drinks, and place them in the cooler to lower the temperature. Do not throw ice directly into the cooler as the extremely cold temperature change can damage your medicine and supplies. Aside from keeping track of your medical needs, you should keep plenty of food in your car in case you get stuck in a traffic jam, lose your way, encounter car problems, or simply cannot find a good diner.
An easy way to deal with food is to visit your regular restaurant or fast food chains. This way, you already know the menu and you can easily pick the food items for your needs. In addition, before you leave for your vacation, print out a fast food guide so that you can have more variety to choose from.
Car travel and pregnancy
If you are traveling by car, leave the driving to your companion. Do not try to drive by yourself. Here are some tips that will help you on your travels:
- Drink plenty of water and make frequent breaks to stretch your legs and visit the toilet to avoid DVT. For pregnant women, hormone and weight changes escalate the chance of blood clots. In addition, the fetus pressing upon veins reduces blood flow to the mother’s lower body especially the legs. When diabetes combines with pregnancy, the occurrence of DVT drastically escalates.
- Whether you are sitting in the passenger seat or the back seat, always wear your seatbelt. When putting on the safety belt, make sure to fasten the lap sash under your bump across your lap. Remember to adjust the shoulder sash between your breasts above your bump. This way, in the case of sudden jolts, the safety belt will keep you in place and decrease the chance of your placenta separating from your uterus.
- If you are sitting in the passenger seat, move your seat as far back from the dashboard as possible for more leg room and prevention against airbag impact in case of a car collision.
- If you are involved in a car collision, you should have a doctor check forinjuries no matter how minor it is.
- If you have contractions, pain, or bleeding after a car accident, see a doctor or emergency clinic as soon as possible. If you have a negative blood group, let the health professional know immediately as you may need to have an anti-D injection.
- Always subscribe to roadside assistance program in case of a breakdown so that you do not have to endure any harsh temperature that will increase your chance of experiencing blood glucose fluctuation. Always carry a mobile phone and update your family where you are during the trip.

Tips on Crossing the Canadian Border
Although you do not have to deal with the stringent liquid regulations travelers have to follow for air travel, you still need to be careful of what you can and cannot bring across the Canadian border on your road trip. When it comes to medicine and medical supplies, take only twice the amount of medicine you will need for the trip. If you are traveling back to the United States from the Canadian border without your doctor’s documentation, the border guards will have a right to confiscate your medication and supplies under the suspicion that you are smuggling these items for resale purposes (Canada offers many diabetes medications for a much lower price, and many individuals have attempted to sneak these things back to the United States for black market drug reselling purpose). When you are at the border, here is a list of what you should do:
- Be upfront about your diabetes condition and declare all medication and diabetes supplies you are carrying across the border (it is always helpful if you already have a printed list on hand)
- Carry all the medication in their original containers and do not peel off any labels so that the border guards can see that all prescription are under your name as stated in the passport
For more information on Canadian regulations see the Health Canada’s Web site.
Hiking is a great way to travel, control your diabetes, and enjoy the nature. However, remember that when you are engaging in any physical activity, always stay well hydrated. Before you start your hike, always carry your blood glucose testing kit and lots of snacks to treat low blood glucose level. Because you can be in an area where mobile phone reception is dismal and far from any medical help center, you have to test your blood sugar level regularly and treat your symptoms right away. DO NOT OVEREXERT YOURSELF . If you tire yourself too much, you can easily injure yourself on the trail by tripping over a branch or twisting your ankle. It is absolutely fine that you need to take more breaks to reach your destination.
One gadget you must carry is a GPS tracking system . Especially for beginner hikers, you can easily stray from a trail. If you think you are lost, remain calm. Study the trail map and assess your current situation with your teammates. By looking for signs and discussing the situation with each other, you will easily get back on track in no time.
When it comes to packing for hiking, always bring sunscreen, bug spray, a hat, and a bandana. It is also an excellent idea to bring along a whistle and glow stick in case you run into trouble and need assistance.
Another very important thing to consider before you set out for your hike is your footwear. Technology has really changed the weight and durability of all hiking and backpacking gear. If you get serious about hiking, the most important item to invest in is a good pair of hiking boots or shoes. They come in various types, from mid-calf boots that that offer a greater amount of support for more rigorous hiking, including backpacking, to boots that resemble running shoes with added traction. If you’re planning on doing more strenuous hikes, or hiking over rocky areas, footwear with good ankle support is best. No matter if you are taking a short hike or a long-distance camping hike, the comfort level of your footwear will make a significant difference in your performance as well as your enjoyment of the excursion.
To avoid overheating, it is a good idea to use a beer growler as a water bottle. This way, your water can stay cool and you can quickly cool yourself down by taking some sip of cool water. Boulder Bottle Co. has a 64 oz. insulated beer growler is perfect for keeping water and juice chilled during hiking and camping. For other options and sizes, just take a look on Amazon.
When it comes to eating while on a hiking trip, pre-packaged nutrient bars is a good way to go. You always want one serving size pre-packaged food for hiking and camping because any food you open and which is not stored properly can become bear and wolf bait. In minor cases, your backpack or tent will be ransacked. In major cases, they will not only damage all your medical supplies and also physically attack you for various reasons.

When you purchase your air, train, or cruise ticket, make sure to select the special diabetes food options. For air travel, when you check in, make sure to double check that they have your food that caters to your needs. Once you are seated, remember to let the flight attendant know that you have diabetes and require the special meals. Make sure to make your request at least 2 days before your departure.
While you are on your travels and if you take insulin, make sure to administer your dose when you see your food coming your way. If you give yourself the insulin too early, a delay in the meal can lead to low blood glucose. To be safe, always carry some snacks with you. So even if your meal is delayed or your order has been mixed up, you are not left waiting with an empty stomach.
Know The Customs of Countries and Their Meal Times
Even though you might be accustomed to certain meal times, they are quite different for other people as well. You might feel that lunch should be at 12pm, and should be 30 minutes or an hour, but things aren't always the same everywhere. In Spain the lunch might be longer, and the dinner might be at 9PM. You shouldn't always assume that everything will be the same there as it is here.
While you are staying at a hotel or resort, you should pay attention to several things.
- Exercising on Gym Equipment
For people who do not usually exercise a lot, you may suddenly want to take advantage of all the exercise equipment at the gym. Although exercising is great for diabetes, it is something that can put a strain on managing your blood glucose level under all these new adjustments. Instead of hoping on one of the cardio exercise machines right away, take advantage of the space and stretch out your muscles from the traveling. Make sure to give your legs and your ankles plenty of stretches and massage so that you can prepare your body for sightseeing and other active activities during the day time.
- Jacuzzis and Sauna
The extreme heat of a jacuzzi and sauna cause a spike in your blood glucose level and affect your body’s insulin absorption rate. If you are anticipating hot tubs and saunas in your trip, ask your doctor whether it is safe for you to enjoy these high-heat activities before your trip.
- Room Refrigerators
Hotel refrigerators are great for keeping insulin cool when you are traveling. However, always remember to double check the refrigerator temperature setting before storing your medicine. Often times, the hotel keeps the refrigerator at the lowest temperature setting, and it can ruin your insulin. If you find that the temperature is too cold, adjust the setting to the right temperature and let it readapt to the new temperature before putting your medicine in.

If your trip require crossing time zones, whether you are taking diabetes medication or requires insulin shots, you should talk to your doctor or diabetes educator about how you should adjust your medication schedule according to the zone change. When you meet with your doctor or diabetes educator, remember to bring your flight schedule and information on time zone changes so that your doctor or educator can help you plan the time and dosage of your medication or injection while you travel.
As a rule of thumb, eastward travel means shorter day and usually less dosage may be needed. On the other hand, westward travel means longer day and more insulin may be required to make the adjustment. To keep track of injection and meals schedule through changing time zones, always keep your watch set to your home time zone until the morning after you arrive.
If you are required to administer insulin injection while in flight, you should be careful not to inject air into the insulin bottle. In pressurized cabins, pressure differences can cause the plunger to fight against you and make it harder to measure insulin accurately.
Flying West (Longer Day Travel)
Here are some tips that will help you plan for your medication, insulin injection, and meal schedule:
- Before departure, administer the usual dose at the usual designated time of day
- When you begin your travel, keep your time set to your departure time zone and apply half of the usual dose at the standard time
- After this half dose, reset your time to the destination time (you can find this information out from the flight attendant or your smartphone world clock)
- Based on your destination time zone, apply the remaining half of the long-acting (basal) insulin at the same time schedule you usually administer the insulin (e.g. if you usually take insulin at 6pm in Vancouver, take your insulin at 6pm based to your new time zone)
- The next day, keep to the destination time, and give the usual full dosage at the usual time
(Please note that in order to accurately plan for your schedule alteration, you should consult with your doctor or diabetes educator.)
Flying East (Shorter Day Travel)
- Keep to the departure time and give a reduced dose at the usual time. The dose should be reduced by using this following formula:
Long Trip Tips & Tricks
Here are some tips for long trips.

For example: Crossing 5 time zones
- 5 ÷ 24 = .21 (Remember the order of division preceeds the order of subtraction)
- 0.9 — 0.21 = 0.69
- Travel dose = usual dose x 0.69
- After applying this reduced dose, reset your watch to the destination time zone
- According to your destination time zone, administer the usual full dose of insulin at the hour you usually take your insulin (e.g. if you usually take insulin at 6pm in Vancouver, take your insulin at 6pm according to your new time zone)
( Please note that in order to accurately plan for your schedule alteration, you should consult with your doctor or diabetes educator.)
For rapid acting insulin to cover food, take insulin with carbohydrate-containing meals—no matter the time zone or whether given by syringe, pen or insulin pump.
For further reading:
- Top Must Have Diabetes Supplies
- There's No Such Thing as the Perfect Diabetic
- Make Insulin Injections More Comfortable for Children with these Products
For insulin pump users, it is highly suggested that you stay on the departure time until arriving at the destination. Once there, change the clock on the insulin pump to the new time on arrival.
Twice-Daily Premixed Insulin Users
If you are a twice-daily pre-mixed insulin user, you should administer your usual insulin before departure at the usual time. Ask your diabetes team to prescribe you a rapid-acting insulin pen, which usually last for 4 to 6 hours. In the meantime, check your blood glucose level every 4-6 hours. If your blood sugar becomes too high, administer a small dose of the rapid-acting insulin every 4 to 6 hours (preferably with a meal) until it is time for your normal second pre-mixed insulin injection in the new time zone after arrival.
Combating Jet Lag
Jet lag and travel fatigue are important issues that can become increasingly more intense the more time zones that are crossed. With the lack of sleep, physical stress, and mental exhaustion, these conditions can cause poor judgment and may result in a dangerous medical mistake.
Travel fatigue can be minimized by booking flights that require less sleep disruption and minimal flight transfers (that is why flights with 3 or 4 transfers are much cheaper than direct flights). Getting plenty of rest and sleep before a trip can also make the time zone transition smoother. If you are traveling towards the west, expose yourself to as much daylight in the evening as possible. However, if you are traveling towards the east direction, you should maximize daylight exposure in the mornings. If this trick does not help, you can always take a short-acting sleeping pill, a small dose of melatonin or a PM Tylenol to fall asleep and stay asleep at a new location.

Accidents and mistakes can happen where you do not have enough insulin throughout your trip. In general, you should try to purchase the exact insulin brand and formulation that your doctor prescribed. However, if you are in an area where your regular brand is unavailable, you may switch for another brand's equivalent formulation (For example, Humulin R forNovolin R, NovoLog for Humalog). Changes in formulation (for example, from rapid-acting insulin to to short-acting insulin) will require medical supervision. In such circumstances, try to contact your doctor or a local doctor for advice.
Another important note to remember is that all insulin are made of strength U-100 in the United States. In other countries, insulin may come as strengths of U-40 or U-80 instead. Under such circumstances, you must buy new syringes to match the new insulin dosage to avoid messing up the intake of your insulin dose. For example, if you use U-100 syringes for U-40 or U-80 insulin, you will take less insulin than your correct dose and suffer from hypoglycemia later. On the other hand, if you use U-100 insulin in a U-40 or U-80 syringe, you will take too much insulin and may suffer from hyperglycemia.

Each country has its own preferred measurement when it comes to blood glucose level measurement.
Instead of measured in milligrams per 100 milliliters (mg/dl), the blood glucose level can be measured in millimoles per liter mmol/l). Here is a list of countries and their preferred unit of measurement for blood glucose level:
If you need to purchase local diabetes medication or insulin, it is a good idea to have this blood glucose conversion chart:
Overheating During Pregnancy
During your travel, if at any point you feel weak and light-headed or nauseous, immediately stop what activities you are doing. These symptoms can be signs that you are overheating and dehydrated. In such circumstances, follow these steps:
- Seek a close-by shaded area or an indoor place. Sip a glass of cool water and lie down to rest.
- If you still feel hot, lower your temperature by wiping your body with a cold, wet towel. Afterward, place an ice pack or a cold towel on your forehead and the back of your neck. If possible, have a fan turned on and circulate the air around you to help you cool down faster.
- If you feel dizzy, you may be low in blood sugar level. If possible, take your blood sugar test and proceed with your emergency care routine. If your test kit is not available, have some juice or a light snack to raise your blood glucose level. Alert your traveling companion of your situation and head back to your hotel so that you can rest up. If you think that your condition is deteriorating, seek medical help immediately. Do not wait.

Even if your diabetes and blood glucose level are in good control, you may have to seriously consider your options as there are many factors that may negatively impact your unborn child. The most obvious one is to avoid visiting developing countries that will require you to receive immunization shots for various diseases such as typhoid fever, yellow fever, mumps, and measles. Because most of these vaccines have not been thoroughly tested on pregnant women for apparent reasons, they may pose dangerous side effects on the development of the fetus. Infections such as malaria can severely increase the chance of premature labor, stillbirth, and miscarriage. The medication for treating malaria can also be harmful to the fetus and increases the chances of birth defects.
What about Women with Gestational Diabetes?
For women who have gestation blood glucose level, it is usually not a good idea to travel, and doctors often recommend against it. Aside from having diabetes, if you are 35 years old or over and pregnant for the first time, and/or are experiencing from these listed complications:
- Vaginal bleeding
- Multiple pregnancy
- High blood pressure
- Cervical problems
- Have pre-eclampsia
- Abnormalities of the placenta
- Prior ectopic pregnancy
- Prior miscarriage
- Prior premature labor
Traveling with Gestational Diabetes
If you must travel when you are pregnant, the second trimester is the safest time as you are least likely to experience complications. To avoid common cases of diarrhea, always eat well-cooked food and drink bottled water. You should avoid any pre-cut fruit, raw leafy greens, and salad as they are easily contaminated. Remember to always travel with at least one companion so that there is always help should a health emergency occurs.
Your doctor and your gynecologist will very likely deny permission for you to travel and even order you to maximize your bed rest duration. If you ignore your doctor’s recommendation, your health insurance and travel insurance will have the right to deny any of your claims and drop your coverage should a health-related emergency situation occur during your excursion. If such an event occurs, you will not only suffer from the complications but also face the expensive international medical care expenses.
On the other hand, if you have a relatively stable gestational diabetes condition and your gynecologist gives you the permission to travel, please refer to our more in-depth section on gestational diabetes .
Here at thediabetescouncil, we encourage our readers to share their experiences, best practices, tips and stories with everyone. Do you have any travelling trips as a person with diabetes that you would like to share with others to maximize the good times and the minimize the bad?
Please remember that all tips and stories shared will help someone else who may have not thought of it before. Safe travels from us to you and share your travel stories with us in the future.
TheDiabetesCouncil Article | Reviewed by Dr. Sergii Vasyliuk MD on June 05, 2020
References:
- https://www.cdc.gov/diabetes/library/features/traveling-with-diabetes.html
- http://www.diabetesforecast.org/2013/jun/35-top-tips-for-travel-with-diabetes.html
More Guides

About Lianne Fachetti, ABA
Lianne Fachetti holds a degree in Biopsychology. With a keen interest in both psychological and biological aspects of behavior forming, she has worked as a researcher at the UBC Brain Research Centre for seven years focusing on the research of memory formation, neural damage from epilepsy, and hormones' effects on behavioral changes. She is also a certified ABA therapist for autistic children.
Connect with us!
- Anti-Spam Policy
- Terms & Conditions
- Privacy Policy
You are using an outdated browser. Please upgrade your browser to improve your experience.
Skip to Site Navigation Skip to Page Content
- Physician Referrals
- Patient Resources
- Why UT Southwestern
Refine your search: Find a Doctor Search Conditions & Treatments Find a Location

Appointment New Patient Appointment or Call 214-645-8300
Diet and Nutrition; Prevention
Traveling with diabetes: Tips for packing, snacking, monitoring, and more
November 20, 2023
QUICK LINKS : Before your trip | During your trip | Travel checklist
By Shibbi Alexander, APRN, FNP-C, AGACNP-BC
For patients with diabetes, travel requires an extra layer of planning beyond booking flights, making hotel reservations, and researching excursions. But having diabetes shouldn’t stop you from exploring the world. You just need a precise plan to cover your health needs – whether you’re flying, driving, or cruising.
The most common travel challenges for people with diabetes involve changes in diet, activity levels, time zones, and environments, all of which could hinder your blood glucose control.
Questions about travel come up often in UT Southwestern’s Diabetes Self-Management Education Services clinic, and our specialists are adept at providing everything from health exams and packing tips to assisting with medical documentation.
Whether you’re taking a quick getaway or an extended trip, planning is the key to a safer, more enjoyable journey.
Before you travel
Do your research: Confirm the mode of travel, accommodations, access to food and exercise, nearby hospital/pharmacies, and access to emergency medication.
Contact your health care provider to ensure your blood sugar is under control and your vaccinations are up to date. You can also discuss your itinerary and how to handle potential challenges, such as:
- Learning how to adjust your insulin doses at different temperatures or altitudes, which can change how your body uses insulin.
- Filling prescriptions in different regions or abroad.
- Packing appropriately to stay on top of your blood sugar during the journey and at your destination.
- Getting prescriptions in case you lose or run out of medications.
- Asking your pharmacist to print extra labels you can attach to plastic bags.
- Getting a letter, if required, stating the need for medical supplies to carry and manage diabetes.
- Getting a medical ID bracelet stating you have diabetes.
- Ordering a special meal in advance for the flight, if applicable, or packing your own.
Simplify traveling
When it comes to medication and supplies, pack double the amount you’ll need. If you’re going for a week, pack two weeks’ worth of:
- Medications.
- Test strips.
- Continuous glucose monitor.
- Insulin pump and supplies, such as batteries, lancets and syringes.
Patients on an insulin pump should carry extra insulin in case of pump failure.
If you’re flying, keep medications in the original packaging. Your continuous glucose monitor or insulin pump can be damaged if it goes through an X-ray machine, so ask for a physical screening or metal detector at the security checkpoint. Consider enrolling in the Transportation Security Administration (TSA) pre-check online to make the process easier.
Diabetes travel checklist : Documents and supplies you'll need for a safe and satisfying trip
When flying or driving
Make sure you’re up to date on what is allowed through airport security . People with diabetes are exempt from the TSA 3.4-ounce liquid rule for medications, fast-acting carbs such as glucose tablets or gummy/hard candies in case of low blood sugar, and healthy snacks like fruit, raw veggies, nuts, green apples, berries, protein bars, peanut butter crackers, granola bars, and trail mix.
Carry gel packs to keep insulin cool, and alert TSA agents that you have these items and keep them separate during screening. You should print and carry an optional TSA Disability Notification Card [PDF] to expedite the process.
Patients with diabetes should pack medications and supplies in a carry-on, not a checked bag, for a couple reasons. First, insulin could get too cold in your checked luggage. Second, if your bags are lost or delayed, at least you’ll have your meds with you.
Also, higher altitudes may lead to incorrect blood glucose readings – approximately 1%-2% lower against each 300m/1000 feet rise due to lower oxygen pressure. Avoid injecting air into the bottle when drawing insulin from the vial while flying.
Follow these additional flying and driving tips:
- Stay hydrated.
- Walk up and down the aisle of the plane every hour to prevent blood clots.
- Remember to stop and get out of the car every hour to prevent blood clots.
- Set an alarm on your phone for taking medicine if you’re traveling across time zones, which can throw off your eating habits and exercise routine.
When it comes to eating, choose healthy food options at the airport or at roadside restaurants, such as:
- Fruit, nuts, sandwiches, yogurt.
- Salads with chicken or fish (skip the dried fruit and croutons).
- Eggs and omelets.
- Burgers with a lettuce wrap instead of a bun.
- Fajitas (skip the tortillas and rice).
Recognize your carbs: fruits, grains, starchy vegetables, dairy products, sweets, sauces, alcoholic drips. Try to avoid buffets, and space out your meals.
Identify yourself: Wear a medical ID bracelet stating you have diabetes. Always carry a health card with your emergency contact and doctor’s name and phone number.
Test often: Blood sugars can fluctuate with changes in food, exercise/activity, sleep, stress, hydration status, and medications at different time zones. Make sure to check blood glucose levels before meals, at bedtime, and as needed. Plan your schedule for insulin administration in different time zones.
If you’re flying, consider wearing knee-high compression stockings or thinner socks during the flight. Wear shoes that can be loosened in case of ankle or feet swelling. Pointing your feet and/or flexing your ankles can improve blood flow, decrease swelling, and lower the risk of blood clots.
If you’re driving, along with packing extra supplies and a cooler of healthy snacks, map out the closest pharmacies, rest stops, and medical centers on the route and near your destination.
Related reading: Diabetes and COVID-19: 5 tips to stay well during the pandemic
During your trip
Being on vacation doesn’t mean you can take a break from good diabetes management. Staying on track will reduce the risk of spoiling the trip – or worse, having a medical emergency.
Dining. One of the best parts of traveling is trying new foods. We recommend researching the popular cuisine of your destination, so you’re prepared to make healthy choices. While it’s OK to splurge once in a while, you’ll need to understand the amount of carbs you’re eating and adjust your meals and days accordingly.
Activities. Wear comfortable shoes and avoid walking with bare feet. Check your feet more frequently throughout the trip, particularly after hikes, long walks, and showering. Look for signs of blisters, cuts, redness, and swelling. Even a small cut or blister can get worse quickly, resulting in an infection or diabetic foot ulcer .
Environment. Keep an eye on the weather. Blood sugar often rises in cold weather because we may be more sedentary. In warm weather, it’s easier to get dehydrated, which interferes with how well the kidneys can filter excess sugar from the blood.
Traveling to a higher altitude can raise blood sugar levels; the higher you go, the more your oxygen levels decrease, which signals the body to create additional stress hormones. Those hormones interfere with how well the body produces and uses insulin. Your glucose meter also may not be as precise at high altitudes, so adjust your testing and medication as needed.
Test, test, test. It’s one of the most important things you can do while traveling. Stay on top of your blood sugar by checking it more than you would at home, especially if your routine changes or you experience unusual symptoms. If you’re hiking, biking, or doing other activities, pack extra snacks and medication in case of blood sugar swings. It’s a good idea to let someone know where you’re going and when you’ll be back in the event of an emergency.
Pay attention to your body. Check your blood sugar and adjust your medication, or contact your doctor if you experience signs of:
Hypoglycemia (low blood sugar)
- Fast heartbeat
- Irritability or confusion
Hyperglycemia (high blood sugar)
- Fruity-smelling breath
- Shortness of breath
- Stomach pain
Make sure your travel companions know you have diabetes, what symptoms to watch for, and when to seek medical care. Stay alert for signs of diabetic ketoacidosis , a medical emergency that requires immediate care. Symptoms include excessive thirst, frequent urination, vomiting, stomach pain, fruity-smelling breath, confusion, and fast, deep breathing. Go to the nearest emergency department if you have these symptoms.
Related reading: Protecting teens and young adults from Type 2 diabetes
After your trip
When you get home, jot down a few notes about what worked and what didn’t regarding your diabetes management. The next time you travel, you’ll have a baseline from which to plan. If you experienced any challenges, let your health care provider know and make an early appointment. They can provide follow-up care, if needed, and help you figure out how to avoid roadblocks in the future.
While having diabetes presents challenges for traveling, they are manageable and shouldn’t stop you from taking journeys and making memories. Talk with a doctor about your next adventure. A little planning can get you where you want to go, safely.
To schedule a consultation with a diabetes expert, call 214-645-8300 or request an appointment online .
Diabetes Travel Checklist
Documentation.
□ Health provider’s letter □ Your diabetes identification card □ Medical alert bracelet or necklace □ Extra prescription medications □ Health insurance card OR travel insurance
For international travel: International Association for Medical Assistance to Travelers (IAMAT) .
Medications
□ Pills, insulin, and any other injectables □ Needles or syringes □ Insulin pump infusion sets □ Cartridges/pods □ Insulin vials for filling cartridges □ Backup insulin pens (in case of pump failure) □ Extra batteries
Testing supplies
□ Glucometer □ Test strips □ Lancets □ Continuous glucose monitoring (CGM) sensors/transmitter/receiver □ Charger or cables for CGM □ Extra batteries □ Alcohol pads □ Hand sanitizer
Insulin storage
□ A small personal bag to carry insulin and supplies in your carry-on (most insulin can be left at room temperature up to 28 days.)
Low blood sugar management
□ Healthy snacks □ Peanut butter □ Fruits and juice boxes □ Hard candy □ Glucose tablets □ Glucagon injection
Miscellaneous
□ Labels on all medicines and supplies □ Portable sharps container □ Keto sticks □ Comfortable shoes
More in: Diet and Nutrition , Prevention

Next Article Food Is Medicine research hits home, help patients improve long-term health
More from Diet and Nutrition
Diet and Nutrition
Food Is Medicine research hits home, help patients improve long-term health
- Jaclyn Albin, M.D.
April 9, 2024

5 tips for a healthy Ramadan fast
- Zaiba Jetpuri, D.O.
March 15, 2024

Cancer; Diet and Nutrition
Ask the dietitian: How can good nutrition help cancer patients?
February 22, 2024

Dry January: The health benefits of going 31 days without alcohol
- Bethany Agusala, M.D.
December 27, 2023

6 tips for healthy, happy eating during the holidays
December 21, 2023

6 health benefits of pumpkin and its spices – beyond the latte
October 23, 2023

Weight-loss medications: The 5 most-asked questions
- Tonia Vinton, M.D.
October 6, 2023

Anti-obesity drugs are closing the gap between dieting and bariatric surgery
- Jaime Almandoz, M.D.
September 7, 2023

How diabetes reached epidemic proportions, and what we can do about it
- Ericka Walker Williams, M.D.
September 4, 2023
More Articles
Appointment New Patient Appointment or 214-645-8300 or 817-882-2400
- Share via Facebook facebook
- Share via Twitter twitter
- Share via LinkedIn linkedin
- Share via Email email
- Print this page print
Talk to us about diabetes
0345 123 2399
customer support
Travelling with diabetes
Travelling with diabetes means there are a few more things to think about before you set off. but living with diabetes shouldn't be a barrier to taking trips or holidays at home or abroad..
Plan to take two to three times the amount of insulin or other diabetes medication and equipment you’d normally use. This will give you peace of mind if you have to stay longer for any reason or if there are disruptions. If you’re travelling abroad, a little extra planning can go a long way to help you relax and enjoy yourself. Don't forget your doctor's letter and travel insurance . Use our tips below to skip to other information you need.
Organise medication with your healthcare team
- What to pack in your hand luggage .
- Flying with a CGM, insulin pump or Freestyle Libre
- Crossing time zones
- Looking after diabetes in hot climates
- Looking after diabetes in cold climates
Checklist for people travelling with diabetes
Check your airline’s guidelines for people with diabetes.
Contact your airline or other operator or look on their website for their guidelines for people living with diabetes. You may need to complete forms in advance, particularly if you use an insulin pump or continuous glucose monitor (CGM). You can also check health information for the country you’re visiting – follow the links on the Foreign travel advice page on the gov.uk website.
Get extra supplies of medication, device spares, and backup
Ask your healthcare team for prescriptions for extra insulin, other diabetes medication, and if you use devices, extra supplies and manual equipment. Flying with an insulin pump, CGM or Freestyle Libre shouldn’t be a problem. But it is sensible to have back up in case of a failure. Expect to take two to three times the amount of medication or supplies you'd usually need.
Get advice on adjusting insulin on long-haul flights
If you are going on a long-haul flight discuss this with your healthcare team. They will advise on any adjustments to your insulin injections or insulin pump - or medication that may be required if you are crossing time zones .
Request a travel letter about your diabetes
You should get a letter from your healthcare team stating you have diabetes and that you need to carry medical supplies. This letter is often requested by airlines and other operators and is helpful in the event of an emergency. It is also advisable to take a copy of a recent prescription with you in case you should need to get supplies whilst away.
The letter should include details about your medication, if for any reason you need to carry medication in containers over 100mls, and any devices that you use.
Download a medical awareness card
If you use a CGM, insulin pump, or Freestyle Libre, and are flying, download a Medical Device Awareness Card (PDF, 71KB) from the City Aviation Authority's website to go with your doctor's letter. The card is not essential, but it may make things easier. You show this to airport security officers with your letter, as it sets out the rules on screening if you wear a medical device.
Check insulin supply in the destination country
Before travelling, find out where you can get supplies of insulin at your destination in case of emergency. Contact your insulin manufacturer before the trip to see if your insulin is supplied in the country you are travelling to.
Insulin manufacturers - contact details
Managing insulin when crossing time zones.
Long-haul flights east or west involve crossing time zones. And you may need to adjust your insulin. Eastward travel will shorten the day, and generally mean a temporary reduction in insulin doses, whereas westward travel will extend the day, and possibly increase insulin requirements. Speak to your healthcare team for advice about adjusting your insulin doses. Have your flight details to hand including your departure time, the length of the flight, and the local time of arrival.
Time zones and tablets
If you take diabetes tablets, you are unlikely to have any particular problems. Very occasionally, it may be necessary to take extra tablets to cover a longer day. Do discuss this with your diabetes care team beforehand.
You may, on occasions, need to leave out one dose of tablets on a short day, when you are travelling on a long west to east journey. Speak to your diabetes care team about this well in advance of the trip.
Crossing time zones and using an insulin pump, CGM or Freestyle Libre
If you are going on a long-haul flight, you may cross different time zones. When crossing different time zones, you may need to change the time or date on some insulin pumps manually so you get the correct basal insulin dose. Speak with your healthcare provider before you travel to get their advice on which settings to change and when. If you use an app, the date and time on smartphones should automatically update when travelling across time zones. If you use a Freestyle Libre reader, you will manually need to adjust the time for accurate reports.
Storing insulin
If you're travelling somewhere hot, remember that heat can damage your insulin and stop it from working properly. Insulin damaged by heat may have a brownish colour, and clear insulin may become cloudy. Do not use insulin that looks like this.
When travelling with insulin, it is best to keep it cool by storing it in a hotel fridge (if there is one in your room) or in a cool bag (providing it does not freeze). A variety of cool bags and storage containers are available. If using a cool bag that uses plastic ice blocks, make sure that the insulin does not come into contact with the frozen plastic containers.
Get more information on managing diabetes in hot weather .
Storing insulin in cold climates
Insulin can freeze in very extreme temperatures but cannot be used if it has been frozen, so if you are planning to visit the arctic (or somewhere equally cold) make sure you keep insulin at room temperature or even on you in an inside pocket or pouch close to your body, to ensure it doesn’t freeze.
Get more information on managing diabetes in cold weather.
Get travel insurance
If you have diabetes, travel insurance is important. You want peace of mind that any emergency medical costs for your diabetes or any other medical condition is covered.
Make sure that any travel insurance covers pre-existing medical conditions like diabetes, as many don’t. It’s also really important you ask if they cover coronavirus in case you need treatment while you’re away. You can also check health information for the country you’re visiting – see the Foreign travel advice page on the gov.uk website.
UK residents travelling to the EU still have access to emergency and necessary healthcare. (See the guidance on travelling with an existing medical condition if you go to the EU ). However, we still advise that you get travel insurance because free health cover provided by the European Health Insurance Card (EHIC) and Global Health Insurance Card (GHIC) doesn’t cover certain things like emergency repatriation (if you need to come home) and not all countries give the same level of cover as the NHS.
If you have diabetes and planning a trip, we can help you get coronavirus-covered travel insurance with AllClear Insure My Diabetes .
What to pack in your hand luggage
- All diabetes medication
- Diabetes supplies – including sensors and other device spares
- Diabetes identity card or wrist band
- A letter from your doctor about your diabetes and treatment and if you use an insulin pump, CGM or flash glucose monitor.
- A prescription sheet
- Hypo treatments
- Extra snacks in case of delays like nuts, fruit or a sandwich.
Split meds between separate bags if you can, for example, if you’re travelling with a partner or friend, in case you lose something.
"Be prepared. I always travel with a backpack full of snacks, medication and everything I need. I don't rely on airport shops being open or other amenities. And when I'm in the mountains, I always have at least three snacks with me." Read Lee's story .
Can I carry insulin in my hand luggage?
Always carry insulin, other diabetes medication, device spares, hypo treatments and other diabetes supplies in hand luggage. It’s important to keep insulin in hand luggage as being in the hold can damage it as it’s so cold and luggage can be lost.
Sensors or other device spares must go in hand luggage as they can be damaged by hold luggage X-rays.
Medication restrictions at the airport
Carrying a doctor’s letter from your GP is requested by some airlines and is helpful to show airport security if there is any confusion.
Current security regulations state that liquid items are only allowed in your hand luggage if they are in containers 100mls or less. There is no restriction on the number of tablets you can take through airport security but they should be mentioned in your doctor’s letter.
Flying with an insulin pump, CGM or Freestyle Libre
It's sensible to look up the manufacturer's advice on flying with your particular device.
Insulin pumps are safe for use during air travel and you can continue to use CGM or flash glucose sensors whilst flying. Connect them to the handset or your phone using Bluetooth. They will still work if your phone is on airplane mode.
When you buy your ticket, contact your airline or other operator or look on their website for their guidelines for people living with diabetes. You may need to complete forms in advance, particularly if you use an insulin pump or continuous glucose monitor (CGM). If you don't do this, in some cases it may cause delay.
If you use a CGM, insulin pump or Freestyle Libre, security staff may ask to see evidence that you need to use one – so you’ll need a letter from your GP or healthcare team to say so.
You can also print off a Medical Device Awareness Card (PDF, 71KB) from the Civil Aviation Authority website to go with your letter. This sets out screening advice for you (the passenger) and the security officer carrying out the checks.
You should also speak to your diabetes team before you go. They can give your more advice about travelling with diabetes on planes. And should you need to remove your pump for any reason, they can provide you with any extra equipment like insulin pens and help plan your doses throughout your journey.
"Since I've been using the Dexcom CGM I’ve been surfing, I’ve been on solo holidays, I’ve been abroad. I’ve done all the things I wasn’t sure I’d be able to do when I first got diagnosed." Georgia.
Can CGMs, insulin pumps and Freestyle Libre sensors go through airport security scanners?
Not all diabetes technology can safely go through security checks at airports. It's important to speak with your healthcare team and look up the manufacturer's security scanning advice for your particular device. We have general guidance below.
Guidance on metal detectors and CGMs and pumps
Most types of CGM/Freestyle Libre sensors and insulin pumps can be taken through the metal detector arches that you walk through.
X-ray luggage scanners, body scanners and CGMS and pumps
Most types of CGM/Freestyle Libre sensors and insulin pumps - and any spare devices or sensors - should not be exposed to x-ray luggage scanners, hold luggage scanners or full body scanners. If you don’t want to remove your CGM/sensor/insulin pump to go through a full body scanner, ask for a “pat down” instead.
You should never be asked to remove a medical device from your body for screening. And you should be offered alternative methods of screening.
Carrying a Medical Device awareness card (PDF, 71KB) along with your GP’s letter reminds you and the security staff of the screening advice for medical devices.
What to eat on the plane
Airlines can provide information on the times of most meals so you can plan your insulin. It is best to order the standard meal, though this may not supply you with enough carbohydrates if you are on insulin or certain diabetes tablets. Cabin crew are usually able to provide fruit, crackers or rolls. On long flights, you may need snacks in between meals and at bedtime to prevent blood sugar levels going too low. If you use insulin, monitor your blood sugar levels frequently and be prepared to make changes to your dosage.
Looking after diabetes in hot climates
In hot countries, the biggest health threat is the sun, so keep covered.
Wear clothes that cover and protect your skin and make sure you wear high factor sunscreen. People often miss the backs of their hands and necks, so make sure you keep these covered and protected with sunscreen.
Sunglasses should also have a UV400 label to make sure they protect your eyes.
Take particular care of your feet if you have neuropathy which is numbness in your feet. This can mean you’re not aware skin is burning so protect them from the sun with socks or sunscreen. Make sure you wear well-fitting sandals on the beach, so they don’t burn on the hot sand.
Sunbathing and blood sugar levels
Sunbathing on the beach can make your blood sugar levels higher than normal because you're not being very active.
Your insulin may be absorbed more quickly from the injection site in hot weather too, and this increases the risk of hypos. You’ll need to monitor your levels more often and be ready to adjust your diet or insulin dose.
Be careful of misleading test results because the extremes of temperature may affect the accuracy of your blood glucose meter.
Find out more about diabetes and hot weather .
Looking after diabetes in cold weather and climates
In cold weather, your insulin may be absorbed more slowly at first, but can then be absorbed suddenly when you warm up later in the day. This can cause you to have a hypo. If your body also uses up more energy staying warm, for example shivering, this can lead to hypos too. So it can be useful to wear layers in colder climates which will both help to keep you warm and allow you to remove clothing if you need to as you warm up. Hypos are more dangerous in cold conditions. This is because they interfere with your body’s attempts to stay warm and increase the risk of hypothermia. So you may need to monitor your levels more often and be ready to adjust your diet or insulin dose if needed. Guarding against hypos is really important so remember your meter may not be accurate in cold conditions. If you are heading somewhere with extreme cold weather check the meter instructions for temperatures it will be accurate at and keep it wherever possible at room temperature. If you suffer from poor circulation or have neuropathy, it's particularly important to prevent frostbite, because the numbness in your feet can mean you don't feel the cold. Make sure you check your feet regularly in cold countries and take plenty of layers including spare socks.
Find out more about storing insulin .
Keeping to your diabetes routines when you're away
It’s important to remember your routines for managing diabetes when you’re abroad. Your job isn’t to avoid trying new things or enjoying yourself. It’s just to be aware that eating different foods, becoming more or less active or drinking alcohol can all make a difference to your blood sugar levels. So check regularly and keep yourself safe.
“As well as a letter from my GP, my phone comes with a health app that I’ve put information about my diabetes and medication in. In an emergency, people can access this without having to unlock my phone.” Lucy.
If you have a tummy bug or you find yourself unable to eat or drink, follow your sick day rules. If you develop covid symptoms while abroad or during travel, you must review the local regulations and follow local public health guidance if available. If the worst comes to the worst and you find you need to go to the hospital while away, don't be alarmed if your blood sugar levels are described differently. Some countries measure blood sugar in milligrams per decileter instead of millimoles per litre - take a look at our blood glucose conversion chart below.

Share this Page
© The British Diabetic Association operating as Diabetes UK, a charity registered in England and Wales (no. 215199) and in Scotland (no. SC039136). A company limited by guarantee registered in England and Wales with (no.00339181) and registered office at Wells Lawrence House, 126 Back Church Lane London E1 1FH


Our website uses cookies
This website uses cookies as well as similar tools and technologies to understand visitors’ experiences. By continuing to use this website, you consent to Columbia University’s usage of cookies and similar technologies, in accordance with the Columbia University Website Cookie Notice. (link opens in a new window)
Skip to content
Diabetes: Travel Tips
Make an appointment.
Our team is here to help you make an appointment with the specialists that you need.
Top of the page
Travel can make it hard to keep your blood sugar within your target range because of changes in time zones, meal schedules, and types of foods available. It's important to take extra medicines and supplies. Bring treatments for high and low blood sugar, such as quick-sugar foods and a glucagon kit. And try to eat and take your medicines as close to your regular schedule as you can.
If you need to see a doctor away from home, let the doctor know you have diabetes. And always wear medical identification. In an emergency, this lets people know that you have diabetes so they can care for you if you can't speak.
These tips can help you stay safe while you travel by car.
- Check your blood sugar level anytime you think it may be low.
- Carry glucose or sucrose tablets or other quick-sugar foods with you at all times.
Eat something to raise your blood sugar. And make sure it has risen to your target range before you drive.
Eat and take your medicine as close to your regular schedule as you can.
Keep sugar-free drinks and drinks with sugar in a cooler.
This will help it stay at a more constant temperature. Don't let the insulin touch the ice.
For short trips, take double your normal amount of diabetes supplies. For long trips, have enough extra supplies to last for 2 weeks more than the length of your trip.
Don't leave it in a hot or cold car or in the sun.
In an emergency, your medical ID will let people know that you have diabetes so they know how to care for you.
This will improve the blood flow in your legs.
These tips can help you stay safe when you travel by plane.
- Ask for a letter stating that you need to carry diabetes supplies. This may help when you go through airport security.
- If you'll travel across three or more time zones, ask about changing your medicine dose and timing.
For short trips, take double your normal amount of needed supplies. For long trips, have enough extra supplies to last for 2 weeks more than the length of your trip.
Luggage can get lost. And supplies may be damaged by the temperature extremes in the baggage area.
When you get ready to go through security, tell the officer that you have diabetes and are carrying diabetes supplies with you. Tell the officer you'd like to have your diabetes equipment (such as an insulin pump or continuous glucose monitor) checked by hand instead of going through an X-ray or scanner. Follow the instructions provided by your machine's manufacturer.
- Put your insulin into a small, wide-mouth thermos if you're not sure that temperatures will stay in a range that is safe for your insulin.
- If you draw up your insulin while flying, put in half the air you usually add to the insulin vial. This will adjust for altitude air pressure changes.
- If you normally use an insulin pump, think about switching to insulin injections during your flight. The change in air pressure may alter how the pump delivers insulin. Also, you may not be allowed to use all of the pump's features during the flight.
This will help blood flow in your legs. And if you take insulin, walking will make sure that your insulin works as it should.
International travel
Traveling to other countries can mean changes in time zones, meal schedules, and types of foods available. This may make it hard to keep your blood sugar within your target range. The following tips can help you prepare for travel abroad.
Get immunized at least 3 to 4 weeks before you travel. These shots can increase your blood sugar for a short time.
Ask for a letter stating that you have diabetes and need to carry syringes and other supplies with you at all times. Also, ask for an extra prescription for your insulin. You may need both to pass through customs with your supplies.
Carry prescriptions for all of your medicines and supplies. Ask your doctor to use generic names for your medicines.
You may not find your regular diabetes supplies where you're going. So take everything you need, including extra test strips, lancets, and batteries for your blood sugar meter.
- Take double your normal amount of diabetes supplies for short trips. For long trips, have enough extra supplies to last for 2 weeks more than the length of your trip.
- If you take insulin, pack a small disposable container with you to hold your used lancets and needles. Wide-mouth plastic soda bottles or water bottles work well.
- Pack a supply of over-the-counter medicines (ones that don't affect blood sugar levels) to treat minor illnesses such as a cold.
Luggage can get lost. And some supplies can be damaged by the temperature extremes in the baggage area.
When traveling by plane or any form of travel that requires screening, tell the security officer that you'd like to have your diabetes equipment (such as an insulin pump or continuous glucose monitor) checked by hand instead of going through an X-ray or scanner. Follow the instructions provided by your machine's manufacturer.
Get a phrase book, a translation app, or some other type of aid that will help you express your needs if you travel to a country where English isn't the main language.
- Related Information
- Travel Health
- Type 1 Diabetes
- Type 2 Diabetes
Current as of: October 2, 2023
Author: Healthwise Staff Clinical Review Board All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Author: Healthwise Staff
Clinical Review Board All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Topic Contents
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use . Learn how we develop our content .

To learn more about Healthwise, visit Healthwise.org .
© 1995-2024 Healthwise, Incorporated. Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Healthwise, Incorporated.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Travel Tip: Traveling with Diabetes

November 14th is World Diabetes Day so we thought it was the perfect opportunity to talk about traveling with diabetes. We know that traveling with medical supplies can be a nerve-wracking experience, especially when your medication includes needles and other sensitive equipment. So here are some tips to help make your trip as smooth as possible.
Notify the Officers
When you arrive at the checkpoint, let our officers know about your medical device and any other equipment prior to screening. If you have an insulin pump, glucose monitor or other medical device attached to your body, inform the officers where it is located before the screening process begins. Although not required, you can provide them with a TSA notification card prior to screening to discreetly describe the medical condition.
If you have questions or concerns at any time during the screening process, please ask to speak to a supervisor.
Screening Process
Passengers in standard lanes may be screened by advanced imaging technology, metal detector or a pat-down. If the standard lane does not have advanced imaging technology, or if you are eligible for expedited screening through TSA PreCheck ® , you may be screened by a walk-through metal detector. If you do not wish to go through screening by technology, inform the TSA officer and they will conduct a pat-down. Pat-downs are conducted by a TSA officer of the same gender, and you may request private screening at any time.
You will not be required to remove any medical devices attached to your body.
Medical Supplies
If you are traveling with medical equipment or supplies, they will need to undergo separate screening. The TSA officer will check the supplies and conduct any necessary testing. If your medical condition requires it, you are allowed to travel with a juice box or other liquid over 3.4oz., but be prepared for the liquid to receive additional screening.
In the event that your insulin pump or glucose monitor is attached to your body, the device is subject to additional screening, including visual inspection. You may be required to conduct a self pat-down of the actual device, followed by a test of your hands for any trace of explosives.
Still have questions? Visit our website for additional information.
If you have any additional questions or need assistance at the checkpoint, reach out to TSA Cares at 855-787-2227. Simply call 72 hours prior to your trip or visit our TSA Cares website . Knowing more about the process may help to relieve any stress and anxiety!
About This Blog
The purpose of this blog is to share the latest news and helpful information with the public. If you have questions about TSA or the information presented here, please contact our AskTSA customer care team on Twitter or Facebook .
TSA is committed to protecting privacy and securing personal information. For details, see our website Privacy Policy .
Stay informed on our latest news!

How One Woman’s Idea Is Changing Travel for People With Diabetes
After french traveler laura pandolfi was diagnosed with diabetes, she launched destination guides that help adventurers with the chronic condition stay healthy on the road..
- Copy Link copied

According to the International Diabetes Federation, approximately 425 million adults worldwide were living with diabetes in 2017. By 2045, it’s estimated this population will rise to 629 million.
Photo by Milada Vigerova/Unsplash
Abnormal sleeping schedules, unpredictable eating hours, and an abundance of local cuisine to taste: These are just a few of the reasons why it can be difficult to stay healthy while traveling. For the estimated 425 million people around the world living with diabetes, however, the task can be even more demanding.
In 2014, Laura Pandolfi was backpacking through Vietnam , Cambodia , Laos, and Thailand , when she started to feel that something was wrong with her health. “About half way through my trip, I fainted several times and generally felt very tired,” she says. “But I didn’t want to cut my travels short, so I waited until I returned home to have a medical check-up.”
When she returned to Paris a few months later, Pandolfi was diagnosed with Type 1 diabetes.
“After I was diagnosed, I stayed in the hospital for 10 days,” Pandolfi says. “One of the first questions I asked the doctors was if I would still be able to travel.
“I was used to feeling like an independent woman who travels the world alone and fears very little,” Pandolfi continues. “I couldn’t imagine my life without adventure.”

Laura Pandolfi explored California’s Death Valley wearing a FreeStyle Libre sensor from Abbott Diabetes Care Inc. The device automatically measures glucose readings without fingersticks.
Courtesy of Laura Pandolfi
Pandolfi’s doctors assured her she’d still be able to travel. But they warned her that she would have to be a lot more cautious—and the endeavor would be difficult. “I searched the internet and read everything I could about traveling with diabetes,” Pandolfi says. “The more I read, the more questions I had: How do I keep my insulin cool? What happens if I lose my diabetes supplies while in India? Can I buy glucose tablets in Mexico? Is the food diabetes-friendly in Peru? I had so many questions, so many doubts, and very few practical answers.
“The internet is full of general tips for traveling with diabetes, but there are very few location-specific resources,” Pandolfi says. “It became clear that diabetics needed their own travel guides, and that I could be the one to create them.”
Two years after her diagnosis, Pandolfi launched Sweet Trip , a collection of country-specific travel guides designed specifically for—and by —people with diabetes.
Diabetes-friendly destination recommendations
Sweet Trip travel guides, which are currently available in English and French, offer detailed information for diabetic travelers to Cuba, France, Mexico, and Portugal. (Diabetes-specific guides for Vancouver, Toronto, London, Madrid, Barcelona, Rome, Vienna, Thailand, Bali, Costa Rica, Hawaii, San Francisco, and New York will publish in 2019.)
Each guide is divided into three focused chapters that “represent the main pillars of leading a healthy life with diabetes,” Pandolfi says.
1. Local food and nutrition: The first section of each guide outlines the staples of local gastronomy—dishes, drinks, and desserts—and provides nutritional information about each. The Cuba guide, for example, identifies the country’s classic camarones enchilados dish as “very low in carbohydrates” and recommends that diabetic travelers complete the meal with an ensalada mixta and a side of arroz . In each guide, this section also includes a phrasebook complete with important translations of phrases like, “Without sugar please” (or S in azúcar por favor) so travelers can learn how to customize local dishes according to personal needs.
2. Health-care system and medical information: Within each country-specific guide, this section provides emergency phone numbers and addresses for local hospitals, pharmacies, and diabetes care facilities. It also contains a dictionary with translated medical terms organized into five categories—body parts, symptoms, medical exams, diagnostics, and pharmaceutical supplies—to help facilitate important communication with health-care professionals.
3. Active tourism: Because physical activities are an important part of diabetes management, a section of each Sweet Trip travel guide provides suggested itineraries for individual walking and biking tours. The Paris city guide outlines points of interest in neighborhoods like Montmartre and Pigalle and details the duration it would take to walk between popular tourist sites in each. All guides also offer options for exploring that aren’t physically taxing: The Portugal guide, for example, includes information about Lisbon’s 19th-century Santa Justa lift, which you can ride up a steep hillside for sweeping views of the city.

Sweet Trip travel guides are designed for and by people with diabetes Type 1 and Type 2.
Courtesy of Sweet Trip
Before publishing each country-specific travel guide, members of the Sweet Trip team actually make a trip to the destination featured, where they review and verify the information they’ve gathered with local doctors, nutritionists, and travel specialists.
“Diabetes is a serious subject—we’re very aware that the quality and accuracy of our content is fundamental to our readers’ health and safety,” Pandolfi says. “But travel should also be enjoyable,” she continues. “It shouldn’t prevent anyone from trying new activities, discovering new foods, or taking more liberties than usual.”
Technical tips for tackling air travel
It’s important that diabetic travelers find answers to their medical questions not only while traveling but also prior to departure. One solid resource is the American Diabetes Association (ADA), which provides an online fact sheet that answers frequently asked questions related to air travel and diabetes.
According to TSA requirements , diabetes-related supplies—such as insulin pens and pumps, syringes, cartridges, blood glucose meters, continuous glucose monitoring sensors, and diabetes tablets—are allowed to pass through airport security once they’ve been separated from other belongings and properly screened. TSA recommends that diabetic travelers arrive at airports prepared with prescription labels for their medications and medical devices, which should be packed separately from carry-on or checked luggage in a clear, sealable bag.
Of course, people with diabetes should travel with healthy snacks on hand to help maintain regular blood sugar levels. (Learn how to make one nutritionist’s favorite D.I.Y. travel treats .)
But according to the ADA, diabetic travelers should also consider carrying a “Diabetes Travel Letter” from a doctor specifying his or her patient status in the case of emergency. Sweet Trip’s website provides a free, downloadable template of this TSA-recommended medical letter.
View this post on Instagram A post shared by SWEET TRIP, Travels & Diabetes (@sweettriptravelsdiabetes) on Jul 9, 2018 at 9:36pm PDT
Beyond featuring tips for travelers with diabetes such as how to find the best diabetes travel insurance, the platform also serves as the gateway to an online community. Sweet Trip’s website is home to the Fridge Surfing Community , a volunteer network of “insulin hosts and fridge surfers” around the world who offer up their refrigerators to traveling diabetics in need of places to cool their insulin while traveling.
“More than a business, we want to build a community,” Pandolfi says. “We hope that, little by little, we can build a strong web of useful tips and resources for anyone traveling with diabetes. There are people with diabetes absolutely everywhere in the world—we should help each other.”
Sweet Trip guides range from approximately $10 to $15, although specific guide sections can be purchased at lower prices. All guides are also downloadable to smartphones and tablets upon purchase and can be used up to three times on one device. Sweet Trip encourages users to reach out with suggestions for diabetes-friendly travel guides in destinations they want to see featured.


Ways Diabetics Can Travel Abroad Optimally
T hrough many advancements in science and technology, travel has been made easier for those with extra needs such as medications, mobility aids, or medical assistance. In diabetes care, advancements in management such as in glucose monitoring, insulin delivery, and medications have helped people with diabetes be able to travel safely. With preparation and resources, diabetics can travel and now have a chance to enjoy travel to different places while managing their health.
Here’s a quick list of tips on how to navigate travel as a diabetic:
See Your Health Provider
As with any big travel plans, it is best to make sure that your body is as healthy as can be. This will also bring to light any health precautions you need to take. Some travel itineraries also have requirements such as vaccinations or medical documentation.
Schedule a pre-travel appointment with your healthcare provider to discuss your travel plans and your possible health needs. They can prescribe you extra medications for travel, instruct you on possible diabetes emergencies, and write letters regarding your condition. They can also recommend comprehensive programs to access while traveling to keep track of your health, such as diabetes weight loss programs which include glucose monitoring, meal planning, and activity trackers.
Check Your Supplies
Diabetics can travel but their management relies on strict blood glucose control and medications are an essential part of it. Travel preparation includes making sure that you have enough medications for the trip, as well as knowing beforehand how to travel with them.
Pack more than enough insulin or oral medications and testing supplies for the duration of your trip, plus extra in case of delays. Divide your supplies and medications between your carry-on and checked luggage to make sure you always have some in case of loss. Double check what you can bring in carry-on versus checked luggage based on regulations , and bring prescription labels and letters. Pack medications in clear sealable bags if in carry-ons for easy inspection at the airport.
Plan Your Meals
Sticking to a diet can be very difficult when traveling. Preparing your own meals can help make it easier, and this includes doing your research about your destination beforehand and planning where to get food and supplies.
Familiarize yourself with the local cuisine and foods available at your destination. This can give you an idea about what you may need to bring or buy ahead of time. Look up nearby markets and grocery stores to get ingredients from once you get there. If you have restaurants as part of your itinerary, browse their menus ahead of time to see what you can eat. Don't forget to bring an excess of prepackaged meals and snacks in case healthy options are not easily available.
Take Care of Yourself
Aside from making sure your medications are administered on time and mindfully eating healthy foods, keeping a healthy lifestyle and daily routine can help manage your diabetes better while traveling.
Always check your blood sugar levels regularly especially before eating and physical activity. Keep a record of your readings using a journal or a tracker in your online or phone programs to make adjustments if needed. Drink plenty of water and avoid sugary beverages to avoid blood sugar level fluctuations. Incorporate exercise or physical activity in your travel plans, but make sure that you keep track of your levels and have snacks handy in case of hypoglycemia. Practice stress-reduction techniques to help manage stress which can affect blood sugar levels.
Prepare for Emergencies
Any travel plan will not be complete without preparation for accidents and emergencies , especially when faced with language barriers or lack of supplies.
Before you go, research available healthcare and emergency care facilities in your destinations. Carry health identifications regarding your diabetes status, medications, and emergency contact information. Always pack extra medications and supplies. Remember, diabetics can travel! Familiarize yourself with dangerous signs and symptoms to know when to seek care. If going to a foreign country with a different language, learn key phrases to be able to communicate your condition.
The post Ways Diabetics Can Travel Abroad Optimally appeared first on Malorie's Adventures .

Traveling can be a breeze if you follow a few tips
General travel tips
- Be sure to get any required vaccinations at least four weeks before you travel, so you have time to deal with any possible side effects.
- Have a letter from your doctor stating that you need to carry medicines or supplies because some airlines and some countries require you to. Syringes and needles can present a problem when flying and when entering some countries.
- Carry a list of your medications (including the generic names and their dosages) from your pharmacist.
- Keep your medication, meal, and snack times as regular as possible.
- If traveling by air or car, try to do some form of activity during your journey: do simple stretches in your seat, circle your ankles, raise your legs, or move around periodically in the aisles.
- If traveling or hiking into remote areas, bring along a first aid kit and, if you use insulin, a Glucagon Emergency Kit to treat severe hypoglycemia.
- If you will be extremely active while traveling, you may need to decrease your diabetes medication, so be sure to discuss this with your diabetes educator or physician.
Carrying insulin and other supplies
- Always carry your insulin and supplies with you in your carry-on luggage. Do not place insulin in your checked luggage as the temperature fluctuations can damage it.
- When traveling by air, you may carry liquids such as insulin, juice or gels to treat hypoglycemia, etc., even in amounts greater than 100 ml. Just make sure they’re accessible and declare them to security when being screened.
- Syringes and needles are also allowed in your carry-on, as long as you are also carrying with you the injectable medication (e.g. insulin).
Storing insulin while travelling
- Insulin must be stored properly, as it will spoil if left in temperatures that are too hot or too cold.
- Insulin keeps its strength at room temperature for 30 days. If traveling in hot temperatures, store your insulin in an insulated bag. If traveling in cold temperatures, keep your insulin close to your body to stop it from freezing.
- You can carry a small sharps container to store used needles and syringes while traveling.
- Take spare syringes and insulin and backups of any other medications or medical supplies.
- If hand-washing facilities are not available, carry alcohol swabs, moist towelettes or hand sanitizer to clean your fingers prior to testing.
Adjusting insulin for time zone changes
- It is a good idea to speak with your doctor or diabetes educator prior to making changes to your medication schedule or dosage.
- When travelling east, your travel day will be shorter. If you lose more than two hours, you may need to take fewer units of intermediate or long-acting insulin.
- When travelling west, your travel day will be longer. If you gain more than two hours, you may need to take extra units of short-acting insulin and more food.
- If you are crossing time zones, you should discuss your meal and insulin schedule with your doctor or diabetes educator.
Adjusting oral diabetes medication for time zone changes
- Ask your doctor or diabetes educator for any recommended changes to medication timing and dosage.
Airport Screening
- You are not required to disclose that you have diabetes to screening personnel.
- You are not required to remove your insulin pump for screening. Just inform the Screening Officer that you are wearing one.
- Do not wear an insulin pump or CGM through the body scanner or place your insulin pump through the x-ray machine as they may affect the devices’ functioning. Instead, you can ask the screening officer to perform a physical search instead (in a private location, if you wish).
- Handheld metal detectors do not affect the functioning of insulin pumps or CGMs.
- If you have any comments or concerns about a recent experience at airport security, please contact the Canadian Air Transport Security Authority (CATSA) at 1-888-294-2202 (toll-free), TTY 613-949-5534, Fax 613-990-1295 or use CATSA’s feedback form on their website .
The Traveler's Checklist
Before you leave, remember to get:
- Travel health insurance
- A list of your medications
- Your diabetes treatment plan so doctors in the places you travel can understand your needs.
- That you need to carry syringes or needles for insulin pens and lancets as part of your insulin treatment. Having this will be helpful if your luggage is examined at airport security checkpoints.
- The supplies you need for your diabetes care. Be sure to keep your syringes, needles, pens, and lancets in the same boxes that they came in with the original prescription label on them.
- Any needed vaccinations
Ask your doctor, diabetes educator or health care team about:
- Illness management
- Low blood sugar management (and Glucagon for insulin users)
- Adjustments for meals, insulin and medications in different time zones
- Avoiding illness caused by contaminated food and water
- Tips for adjusting your medication if required
Packing list
- Telephone numbers of your doctor and diabetes educator
- Extra supply of insulin or pills for diabetes
- Blood glucose meter and logbook
- Fast-acting sugar to treat low blood sugar
- Snacks to cover delayed meals, such as crackers and fruit
- Extra supply of syringes, needles and an extra insulin pen if used
- Urine ketone-testing strips
Contact us for support
For support and more information about your rights.
Information and support services
1-800-BANTING (226-8464)
Related Content

People with diabetes have the right to drive and a license.

Find out more about obtaining or renewing insurance when you have diabetes.

Self-care in public places
It is important to be able to safely treat your diabetes, no matter where you are.
Home > Knowledge & support > Living with type 1 diabetes > Everyday life > Travelling
Travelling with type 1 diabetes
In this section, preparing to travel, work out what supplies you need.
Take some time to work out how much insulin, test strips, glucagon, glucose tablets, lancets, needles and set change equipment you need. When you’re packing, take three times as much medical equipment as you expect to use.
If you use an insulin pump, take insulin pens and insulin cartridges in case your pump fails, along with manufacturers’ helpline numbers for any countries you’re visiting.
Make sure you pack emergency supplies for the journey and for days out once you start your holiday.
Keeping insulin cool
Buy some medically approved cooling packs to keep insulin cool in hot weather while you’re out and about. Make sure they’re medically approved, otherwise you may not be able to take them through airport security .
Tips on packing
Divide supplies between bags just in case you lose one.
If you’re flying, don’t put any of your insulin in your checked-in luggage as it can freeze in the hold. Instead, keep it with you in your hand luggage.
Get information about where you’re going
Make sure you check the government website for information about where you’re travelling to.
It’s a good idea to check where the nearest pharmacy or hospital is so that you can get there quickly in an emergency.
Make sure you’ve got the documents you need
You will need to take a doctor’s letter with you to prove that you have type 1 diabetes and need to carry medical supplies. Your GP or Diabetes Healthcare Team can provide you with this.
Take a medical prescription with you in case you need to get supplies while you’re away, and a diabetes identity card or bracelet.
Print off a Medical Device Awareness Card to show airport security that you are carrying type 1 diabetes tech. If you don’t have a printer, you can email Rachel Crawford at [email protected] to arrange to have one sent to you. Get more information about taking tech through airport security.
Many airports provide a hidden disability lanyard for people travelling with type 1. Find out more about how to get one .
Prepare for varying insulin doses
You may find you need to vary insulin doses for very active holidays or places where the weather is hot or cold, which may affect your blood glucose levels.
If you’re doing activities like swimming for extended periods, test your blood glucose level regularly. In the evening and night, your blood glucose level could drop after periods of activity, so beware of night-time lows.
Learn more about managing your glucose levels around exercise and physical activity .
Insulin absorption is more rapid in a hot climate so watch out for after-meal lows, followed by a spike. If you’re on a pump, use the dual or square wave function.
Planning is key
Travelling with diabetes checklist.
Download the Diabetic Travelers Network’s checklist to help you plan for travel and make sure you take everything you need.
Travelling by plane
Do you need a doctor’s letter to take diabetes supplies on a plane.
You will need to take a doctor’s letter with you to prove that you have type 1 diabetes and need to carry medical supplies, especially when you go through airport security. Your GP or Diabetes Healthcare Team can provide you with this. This letter will also allow you an extra bag to carry diabetes supplies.
Can you take insulin on a plane?
Yes, but only as hand luggage (though you will need to put it in a separate plastic bag to go through security). Temperatures in the hold can drop to freezing which will affect the effectiveness of insulin.
Can you take insulin pens on a plane?
Yes. Keep your insulin pens in your hand luggage so you have easy access to them.
Can you take blood glucose meters on a plane?
Yes. Keep it in your hand luggage in case you need to check your levels whilst you’re in the air.
Can you take an insulin pump on a plane?
The reduction in atmospheric pressure on planes can sometimes cause them to deliver insulin by accident. This can be caused by air pressure, dissolved and/or visible bubbles or the plunger moving.
The following steps are recommended for insulin pump users going on flights:
- The cartridge should only contain 1.5ml of insulin
- Disconnect the pump before take-off
- After take-off, once the plane is at cruising altitude, take the cartridge out of the pump and remove any air bubbles before reconnecting (it’s recommended that you don’t disconnect your insulin pump for longer than an hour, but check with the manufacturer or your Diabetes Healthcare Team).
- After the aeroplane lands, disconnect the pump and prime the line with two units. Then reconnect the pump
- If there’s a flight emergency involving cabin decompression, disconnect the insulin pump
Can you take a continuous glucose monitor or a flash glucose monitor on a plane?
You can use continuous glucose monitors (CGM) or flash glucose monitors on a plane and connect them to the handset or your phone using Bluetooth. They will still work if your phone is on airplane mode.
Airport security
You can take some items, like insulin pens, safely through airport security. Other equipment – like insulin pumps – may be damaged by x-rays and scanners. Find out more about taking type 1 tech through airport security .
Food and travel
When you’re travelling, make sure you take snacks with you – don’t rely on having to find somewhere in case you need to eat quickly or treat a hypo.
Aeroplane food
Contact your airline before you travel to tell them you have type 1 diabetes so that they can accommodate you. You can also ask to be served your food first.
Long train and car journeys
If you’re going on a long train or car journey, make sure you have plenty of snacks with you in case you’re not able to stop when you need to.
If you’re buying food on the train, wait for it to arrive so that you can judge how much insulin you need.
Managing insulin across time zones
If the time zone change is less than four hours, you don’t need to change how you would normally take your insulin. Talk to your Diabetes Healthcare Team before you leave for your trip to get their advice on how to manage your diabetes across time zones.
You can find information about how to manage changes in times zones (going east to west and west to east) in the Diabetes Travel Network’s Guide to Traveling with Diabetes .
Type 1 diabetes and travel insurance
Travel insurance is available for people with type 1, although it may be slightly more expensive. You can usually find insurance to cover things like medical expenses and loss of insulin and devices (find out more about insuring type 1 technology ).
When buying insurance, you will need to give details about how your type 1 has impacted you, for example, if you’ve had any hospital stays within a certain period of time.
The Global Health Insurance Card
If you’re travelling in European countries (apart from Norway, Iceland, Liechtenstein or Switzerland) carrying a Global Health Insurance Card (GHIC) will entitle you to low cost or free medical care. Formally known as a European Health Insurance Card (EHIC), you can find out more on the government website .
Long-term travel
If you’re travelling over a period of weeks or months, you can still follow the guidance on this page. Ask your Diabetes Healthcare Team to prescribe enough supplies to cover the length of your trip (up to six months).
It may seem like a lot to pack in your suitcase, but it will prevent you having to spend time looking for places to get supplies when you’re away.
Insulin is available almost everywhere, but it’s a good idea to check if your insulin is available in the country you’re travelling to. You can do this by checking the manufacturer’s website. Sometimes brand names are different in each country, so make sure you know what yours is before you go.
If you need to get your supplies abroad, you can use your travel insurance .
Download the Diabetic Travelers Networks® ’ Guide to Travelling With Diabetes ‘ for information and tips on travelling with type 1.
This content was created in partnership with Julie Kiefer from the Diabetic Travelers Network®.
Shared stories

“You deserve to go on holiday, to have fun, to feel understood” – travelling the world with type 1 diabetes
“I have travelled to 28 countries and navigated through 3 different health care systems with type 1. It is through planning, and some trial and error, that I discovered what works and what doesn’t and gained the knowledge and experience to travel freely with type 1.”
You may also be interested in

Airport security and diabetes technology
Get information about how to get through airport security as smoothly as possible.

Type 1 technology
Learn about what technology is available to manage type 1 and how to access it.

Visiting or moving to the UK with type 1 diabetes
If you’re moving to the UK, discover information and guidance on navigating a new health system.
Explore more lifestyle topics
Food and nutrition.
If you have type 1 there are a few things you will need to be aware of when you eat and drink, but that needn’t stop you enjoying delicious and nutritious food.
Find information about different types of jobs, how to manage your type 1 at work and the laws in place to protect you from discrimination.
Whether you’re walking the dog, ballet dancing or training for a marathon, learn how to manage your glucose levels and insulin intake for exercising.
You can still drive if you have type 1 diabetes, but there are some extra steps you need to take to be legal and safe on the road.
Different types of alcohol can affect your blood glucose in different ways. Get tips and advice to stay safe with alcohol.
Recreational drugs
Drugs can impact how you manage your type 1 and stay safe. Learn about the effects of drugs on type 1.
Smoking and vaping
When you have type 1 diabetes, smoking can make it harder to manage your blood glucose levels and increase your risk of complications.
Visiting or moving to the UK
If you’re moving to the UK, understanding a new health system as well as everything else that comes with moving to a new country is a challenge.
We value your privacy
Customize consent preferences.
Diabetes and travel
You can travel anywhere with diabetes. You just have to prepare to avoid any problems.
Before you travel
- make sure your travel insurance covers health problems related to your diabetes
- find out where you can get your insulin in the place you're visiting, and take a recent prescription with you
- speak to your care team for advice about adjusting to different time zones
- if you're flying, get a letter from your GP or care team to say you have diabetes and need to take your treatment on to the plane (you may need to pay for the letter)
- if you use a pump or a continuous glucose monitor (CGM), check with your airline before you travel about taking it on board – some airlines require paperwork for medical equipment
Packing for your trip
- pack 3 times as much insulin, test strips, lancets, needles and glucose tablets as you'd expect to need
- split your medicines, IDs and equipment into 2 different bags, just in case 1 gets lost
- if you use a pump, pack insulin pens in case it stops working
- put insulin in your hand luggage – the hold of the plane will be too cold and could damage the insulin
- take a cool bag to stop your insulin getting too hot
- take some form of diabetes ID, like a medical alert bracelet, to tell others that you have diabetes
- take the contact details of your diabetic team, just in case you need their advice
- take plenty of snacks in case there are any delays
- do not put your pump through airport scanners or x-ray machines – let airport security know so they can check it another way
While you're away
- be prepared to test more while you're away – hot and cold weather can affect your blood glucose levels and increase your risk of a hypoglycaemia (hypo) or hyperglycaemia
- you may have to change your insulin dose depending on the temperature and different activities you're doing – speak to your diabetes team
- take care if you're sunbathing, as this can affect your blood glucose levels
Diabetes UK has more information on what to do when you travel .
Page last reviewed: 20 September 2021 Next review due: 20 September 2024

Diabetes and travel – 17 top tips to travel safe and stress-free

Travel can be a rich and rewarding experience, full of sights, sounds, and adventure. And diabetics don’t have to miss out on the excitement. It just takes a little more care and preparation. By planning ahead, you can ensure your diabetes and travel plans don’t become a problem.
So let’s take a look at some of the essential tips and strategies you should use to make the most of your trip. We’ll explore everything from how to manage travelling with diabetic supplies to selecting diabetic-friendly travel snacks.
Here’s what you’ll need to know:
- Talk to your doctor
- Pack extra supplies
- Keep medications easily accessible
- Protect your medications from extreme temperatures
- Be prepared for security checks
- Carry a medical ID
- Plan meals and snacks
- Stay hydrated
- Monitor your blood sugar regularly
- Wear comfortable shoes
- Protect your feet
- Stay active
- Inform your travel companions
- Plan for emergencies
- Manage stress
- Get sufficient rest
- Enjoy your trip
Tip #1 – Talk to your doctor
Depending on where you’re planning to go and what you’re hoping to do, it may be a good idea to talk to your doctor. They can help make any adjustments you may need to your medications and check you’re up-to-date with your travel vaccines (helping you take care of your overall health and well-being). They can also provide you with a letter explaining your condition and medications, which can be useful when going through security and entry checkpoints (like at airports, museums, galleries, etc.)
Tip #2 – Pack extra supplies
When travelling with diabetic supplies and diabetes medication, include some extra. Depending on what you’re using to manage your condition, you should consider things like insulin, syringes or insulin pens, blood test strips, medications, glucose tablets, etc.
As a rough guide, aim to have a few days’ worth of extra supplies in case of unexpected delays or emergencies.
Tip #3 – Keep medications easily accessible
While travelling, you need to make sure your diabetes medications are easily accessible. Keep them in your carry-on luggage and with you at all times, and avoid putting them in checked baggage. This will remove the risk of possible problems with lost or delayed bags and also mean you can manage your condition effectively during long transit periods.
Tip #4 – Protect your medications from extreme temperatures
Insulin and other medications can be sensitive to temperature, such as extreme heat or cold. To keep your medications safe, and usable, it’s a good idea to invest in accessories and equipment that can help you keep them at a stable temperature while you travel. For example:
- Cooling travel wallets (for insulin pens)
- Insulated diabetic travel cases
- Chargeable travel coolers
Tip #5 – Be ready for security checks
If you’re going to be passing through any security checkpoints, plan ahead and make the process as easy as possible. Tell security personnel about your condition, make sure your medications are easily accessible (see Tip #3) and have ready to hand a letter from your doctor (see Tip #1) explaining your disease as well as the medications and equipment to treat it that you may be travelling with.
Tip #6 – Carry a medical ID
Wearing a medical identification bracelet or necklace that clearly states you have diabetes can be incredibly useful in an emergency. When wearing one, first responders will know about your condition and can make sure you receive appropriate care.
Medical IDs come in many shapes and sizes, so there’s a good chance you’ll be able to find something you like and that works for you. Options include:
- Silicone wristbands ( type 1 / type 2 )
- Steel bracelets ( type 1 / type 2 )
- Steel bangles ( type 2 )
- Watch sleeves ( type 1 / type 2 )
- Medical zippers ( type 1 )
Tip #7 – Plan meals and snacks
What you eat and drink has a direct impact on your blood glucose level. So planning your meals and snacks in advance can play a major role in helping keep your blood sugar stable while you travel.
Research the food options where you’re heading, as well as what’s available along the way. And carry snacks so you can satisfy hunger or address low sugar as you travel – A good selection of travel snacks for diabetics will address both needs.
Nuts, seeds and whole-grain crackers have a low glycemic index and are excellent snacks for beating hunger without spiking blood sugar.
And glucose tablets , fruit juice and candy are worth carrying as well to help avoid and treat hypoglycemia (low sugar).
Tip #8 – Stay hydrated
Dehydration can affect your blood sugar level, so drink plenty of water as you travel. Keep a refillable water bottle with you, and take bottled water if you’re travelling through an area where clean water may not be readily available.
Tip #9 – Monitor your blood sugar regularly
One of the best ways to manage and maintain stable blood glucose levels is by following a routine. However, when travelling, maintaining a routine becomes much more challenging!
This disruption can have a significant impact on your blood sugar levels. So monitor your blood sugar regularly and adjust your insulin or medication to keep it stable. Continuous glucose monitors (CGMs) can be a great help with this, providing a constant insight into your blood glucose level. Even with a CGM though, it’s still a good idea to carry a glucose meter and test strips as a backup.
Tip #10 – Wear comfortable shoes
Whether you’re exploring a new city or trekking through nature, comfortable shoes are a must. Foot complications are a common problem for diabetics, and proper footwear can help avoid them.
Tip #11 – Protect your feet
Given how common foot complications are for diabetics, as well as wearing suitable shoes while travelling it’s also important to take proactive care of your feet. Every day, check your feet for any cuts, blisters or signs of infection – This is especially important if you’re walking long distances.
You should also keep your feet clean and dry and wear moisture-wicking socks (available for both men and women ).
And if you see anything of concern, don’t wait. Treat it immediately.
Tip #12 – Stay active
Regular physical exercise can help regulate blood sugar levels, increase insulin sensitivity, and improve overall health. So make sure to stay active while you travel.
As tempting as it can be to just relax all day by a pool or on the beach, fit in some exercise every day. Even going for a walk can make a difference.
And as an added bonus, a mindful stroll can be a fantastic way to explore a new place! Stroll through a local market, go on a hike, or take a cycle tour – You’ll support your health and see more on your travels.
Tip #13 – Inform your travel companions
If you’re travelling with other people, make sure they’re aware of your diabetes and know how to help you in case of an emergency. They don’t need to be experts – Just let them know what the signs and symptoms of hypoglycemia (low sugar) and hyperglycemia (high sugar) may be and what they can do to help you.
Also, letting guides know you’re a diabetic and that you’re carrying snacks to prevent hypoglycemia can help make sure you get the support you need, when you need it, particularly if you’re heading to an area where you’re not normally allowed to eat.
Tip #14 – Plan for emergencies
No one wants to have to face an emergency while travelling. But if you do, it’s best to be prepared.
Doing some basic research before you head off on your adventure can make it easier to handle any emergencies that do occur. Find out the emergency contact numbers, check what medical facilities are available, and see where the nearest pharmacies will be.
It can also be a good idea to invest in travel insurance. And when getting a quote, mention your diabetes. This will help make sure you get the right level of cover for your trip – The best travel insurance for diabetics could include coverage for things like 24/7 hour medical assistance, medical supplies, hospitals, and emergency evacuation.
This basic information and prep work can help give you peace of mind and security when tackling unexpected health problems.
Tip #15 – Manage stress
Stress can have a significant impact on your blood glucose level. Because of this, stress management can play an important part in diabetes care.
And this is true both at home and while travelling.
Practising relaxation techniques and managing your stress can help you keep control of your blood sugar when off on your adventure. Deep breathing, meditation, and yoga are all good options to consider (you can practise them practically anywhere), helping you stay calm and keep your blood glucose regulated.
Tip #16 – Get sufficient rest
Getting a good night’s sleep is vital not just for diabetes management but also to support your overall health.
Aim to get 7-9 hours of quality sleep each night to help regulate your blood sugar and maintain your general well-being. To support this, be physically active during your day, avoid caffeine and alcohol before going to bed, and try to keep your electronic devices (like your phone or tablet) out of your bedroom to set a more relaxing environment and avoid temptation.
Tip #17 – Enjoy your trip
Finally, don’t forget to enjoy the adventure! Travelling is a fantastic opportunity to explore the world, take on new experiences, learn, and grow as a person. Having diabetes may mean you need to plan and prepare more before you head off but it’s definitely possible to manage your diabetes effectively while travelling.
So follow these tips, stay on track with your diabetes management, and enjoy your trip!
Worth the read? Share it
Looking for more articles like this.

Discover how waxing and diabetes can go hand in hand. Learn about safe practices, benefits, and precautions for a successful hair removal experience.

Learn how to dispose of diabetic test strips, lancets and needles, and protect yourself, your community and the environment.

Explore the connection between diabetes and sex. Learn how to maintain a fulfilling sex life while managing diabetes.
Recent ARTICLES
Have a story to share.
Together, our experiences make us stronger. Send your story to us , and we'll help you share it with the diabetic community.
Want to keep up with the latest news, stories and recipes?

COMMENTS
Say goodbye to worry when you pack your diabetes supplies in a carry-on bag. Stop and get out of the car or walk up and down the aisle of the plane or train every hour or two to prevent blood clots (people with diabetes are at higher risk). Set an alarm on your phone for taking medicine if you're traveling across time zones.
Many travel packs are available to keep insulin cool. Other tips for traveling with diabetes. Other tips include: Take it easy for a few days after a long flight. Test your blood sugar according to your healthcare provider's advice. If you use insulin, check the bottle of insulin before each shot.
Here are a few crucial ways to prepare for any type of travel with diabetes: Get extra insulin, pump supplies, test strips, and a new prescription. ... Here are 5 tips when it comes to nutrition while traveling: Pack a variety of Ziplock bags with things like nuts, crackers, carrots, apple, roasted chickpeas, rice cake with peanut butter, and a ...
Traveling by Foot. Hiking is a great way to travel, control your diabetes, and enjoy the nature. However, remember that when you are engaging in any physical activity, always stay well hydrated. Before you start your hike, always carry your blood glucose testing kit and lots of snacks to treat low blood glucose level.
Avoid open-toe shoes like sandals or flip-flops. Exposed toes make injuries and infections more likely. Follow your daily foot care routine when you're away. For instance, wash your feet, dry ...
Diabetes travel checklist: Documents and supplies you'll need for a safe and satisfying trip. ... Related reading: Diabetes and COVID-19: 5 tips to stay well during the pandemic. During your trip. Being on vacation doesn't mean you can take a break from good diabetes management. Staying on track will reduce the risk of spoiling the trip ...
Travelling with diabetes means there are a few more things to think about before you set off. But living with diabetes shouldn't be a barrier to taking trips or holidays at home or abroad. Plan to take two to three times the amount of insulin or other diabetes medication and equipment you'd normally use. This will give you peace of mind if you have to stay longer for any reason or if there ...
Bring an empty water bottle with you to fill at a refill station in the airport terminal. If checking a bag, make sure to keep your diabetes supplies in your carry-on, as baggage can sometimes be lost. You should always have at least 3 days' worth of supplies in an easily-accessible location when traveling. However, if a situation does arise ...
Travel letter stating need for access to diabetes supplies. Prescription labels for all your medications, including insulin. Medical identification for diabetes and allergies. "Backup" prescriptions. List of all medications with instructions. Blood glucose monitoring supplies: extra meter. batteries.
Air Travel and Diabetes. We continue to advocate for the rights of travelers with diabetes. We work with the Transportation Security Administration (TSA) to ensure that passengers with diabetes have access to their diabetes supplies and equipment, especially during those times when the nation's security threat level rises and screeners must ...
Diabetes: Travel Tips. Overview. Travel can make it hard to keep your blood sugar within your target range because of changes in time zones, meal schedules, and types of foods available. It's important to take extra medicines and supplies. Bring treatments for high and low blood sugar, such as quick-sugar foods and a glucagon kit.
KNOW HOW TRAVEL CAN AFFECT YOUR BLOOD GLUCOSE LEVELS AND HOW YOU MANAGE YOUR DIABETES. Be sure to pack: Travel letter stating need for access to Diabetes supplies; ... you can also refer to the Centers for Disease Control and Prevention Tips for Travelling with Diabetes page. Points about pumps Special points about insulin pumps. ...
Insulin pump and insulin pump supplies (cleaning agents, batteries, plastic tubing, infusion kit, catheter and needle)—insulin pumps and supplies must be accompanied by insulin. Glucagon emergency kit. Urine ketone test strips. Unlimited number of used syringes when transported in Sharps disposal container or other similar hard-surface container.
November 14th is World Diabetes Day so we thought it was the perfect opportunity to talk about traveling with diabetes. We know that traveling with medical supplies can be a nerve-wracking experience, especially when your medication includes needles and other sensitive equipment. So here are some tips to help make your trip as smooth as possible.
Technical tips for tackling air travel. It's important that diabetic travelers find answers to their medical questions not only while traveling but also prior to departure. One solid resource is the American Diabetes Association (ADA), which provides an online fact sheet that answers frequently asked questions related to air travel and diabetes.
As the number of people who travel continues to increase, so too will the number of travelers with diabetes. This increase will come with new and more frequent requests for medical travel advice. This article equips clinicians with the tools to address patient concerns about travel and to empower patients to be prepared for emergency situations both abroad and at home. This includes ...
Here's a quick list of tips on how to navigate travel as a diabetic: See Your Health Provider. As with any big travel plans, it is best to make sure that your body is as healthy as can be. This ...
The American Association of Diabetes Educators suggests a plan of attack for ensuring your next travel adventure is safe and successful. The secret to any successful trip is to take plenty of time and plan far in advance of your departure - and that goes double when you have diabetes. For more information about how a diabetes educator can help
Do not place insulin in your checked luggage as the temperature fluctuations can damage it. When traveling by air, you may carry liquids such as insulin, juice or gels to treat hypoglycemia, etc., even in amounts greater than 100 ml. Just make sure they're accessible and declare them to security when being screened.
Talk to your Diabetes Healthcare Team before you leave for your trip to get their advice on how to manage your diabetes across time zones. You can find information about how to manage changes in times zones (going east to west and west to east) in the Diabetes Travel Network's Guide to Traveling with Diabetes. Type 1 diabetes and travel insurance
People with type 1 diabetes can travel, but they will need to plan carefully to make sure that they can monitor and correct their blood sugar levels. Find useful tips here. Health Conditions
Before you travel. make sure your travel insurance covers health problems related to your diabetes; find out where you can get your insulin in the place you're visiting, and take a recent prescription with you; speak to your care team for advice about adjusting to different time zones
By planning ahead, you can ensure your diabetes and travel plans don't become a problem. So let's take a look at some of the essential tips and strategies you should use to make the most of your trip. We'll explore everything from how to manage travelling with diabetic supplies to selecting diabetic-friendly travel snacks.