Blood Clots and Travel: What You Need to Know
More than 300 million people travel on long-distance flights (generally more than four hours) each year. 1 Blood clots, also called deep vein thrombosis (DVT), can be a serious risk for some long-distance travelers. Most information about blood clots and long-distance travel comes from information that has been gathered about air travel. However, anyone traveling more than four hours, whether by air, car, bus, or train, can be at risk for blood clots.


Blood Clots and Travel: What You Should Know
This podcast is designed to help people reduce their risk of blood clots during long-distance travel of four hours or more.
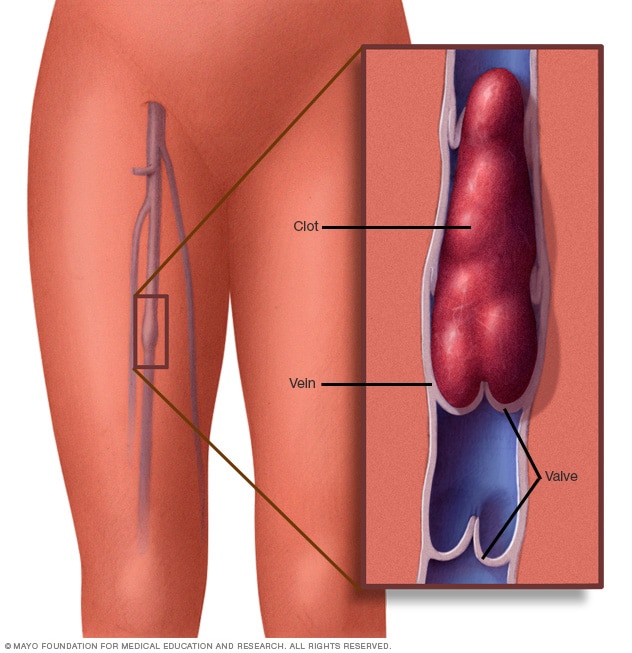
Blood clots can form in the deep veins (veins below the surface that are not visible through the skin) of your legs during travel because you are sitting still in a confined space for long periods of time. The longer you are immobile, the greater is your risk of developing a blood clot. Many times the blood clot will dissolve on its own. However, a serious health problem can occur when a part of the blood clot breaks off and travels to the lungs causing a blockage. This is called a pulmonary embolism, and it may be fatal. The good news is there are things you can do to protect your health and reduce your risk of blood clots during a long-distance trip.
Understand What Can Increase Your Risk for Blood Clots
Even if you travel a long distance, the risk of developing a blood clot is generally very small. Your level of risk depends on the duration of travel as well as whether you have any other risks for blood clots. Most people who develop travel-associated blood clots have one or more other risks for blood clots, such as:
- Older age (risk increases after age 40)
- Obesity ( body mass index [BMI] greater than 30kg/m 2 )
- Recent surgery or injury (within 3 months)
- Use of estrogen-containing contraceptives (for example, birth control pills, rings,patches)
- Hormone replacement therapy (medical treatment in which hormones are given to reduce the effects of menopause)
- Pregnancy and the postpartum period (up to 3 months after childbirth)
- Previous blood clot or a family history of blood clots
- Active cancer or recent cancer treatment
- Limited mobility (for example, a leg cast)
- Catheter placed in a large vein
- Varicose veins
The combination of long-distance travel with one or more of these risks may increase the likelihood of developing a blood clot. The more risks you have, the greater your chances of experiencing a blood clot. If you plan on traveling soon, talk with your doctor to learn more about what you can do to protect your health. The most important thing you can do is to learn and recognize the symptoms of blood clots.

My name is Amaris White and I want to share my personal experience with blood clots. My hope is that by sharing this information, you will learn the signs and symptoms of this potentially fatal condition and know how to protect yourself and others.
Recognize the Symptoms
Deep vein thrombosis (dvt).
About half of people with DVT have no symptoms at all. The following are the most common symptoms of DVT that occur in the affected part of the body (usually the leg or arm):
- Swelling of your leg or arm
- Pain or tenderness that you can’t explain
- Skin that is warm to the touch
- Redness of the skin
If you have any of these symptoms, contact your doctor as soon as possible.
Pulmonary Embolism (PE)
You can have a PE without any symptoms of a DVT. Symptoms of a PE can include:
- Difficulty breathing
- Faster than normal or irregular heartbeat
- Chest pain or discomfort, which usually worsens with a deep breath or coughing
- Coughing up blood
- Lightheadedness, or fainting
If you have any of these symptoms, seek medical help immediately.
For more information on blood clots
Blood Clots and Long Distance Travel: Advising Patients

View this video to learn more about how healthcare providers can advise their patients on long-distance travel and blood clots.
Protect Yourself and Reduce Your Risk of Blood Clots During Travel
- Know what to look for. Be alert to the signs and symptoms of blood clots.
- Talk with your doctor if you think you may be at risk for blood clots. If you have had a previous blood clot, or if a family member has a history of blood clots or an inherited clotting disorder, talk with your doctor to learn more about your individual risks.
- Move your legs frequently when on long trips and exercise your calf muscles to improve the flow of blood. If you’ve been sitting for a long time, take a break to stretch your legs. Extend your legs straight out and flex your ankles (pulling your toes toward you). Some airlines suggest pulling each knee up toward the chest and holding it there with your hands on your lower leg for 15 seconds, and repeat up to 10 times. These types of activities help to improve the flow of blood in your legs.
- If you are at risk, talk with your doctor to learn more about how to prevent blood clots. For example, some people may benefit by wearing graduated compression stockings.
- If you are on blood thinners, also known as anticoagulants, be sure to follow your doctor’s recommendations on medication use.
1 Gavish I, Brenner B. Air travel and the risk of thromboembolism. Intern Emerg Med 2011 Apr;6(2):113-6.
- Yellow Book chapter on DVT and travel
- World Health Organization
Join the Public Health Webinar Series on Blood Disorders
- Upcoming webinar
- View past webinars
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- ASH Foundation
- Log in or create an account
- Publications
- Diversity Equity and Inclusion
- Global Initiatives
- American Society of Hematology
- Blood Clots
Clots and Travel
- Agenda for Nematology Research
- Precision Medicine
- Genome Editing and Gene Therapy
- Immunologic Treatment
- Research Support and Funding
Blood clots can sometimes form in your legs during air travel because you are immobile for long periods of time, often sitting in cramped spaces with little leg room. The clinical term for this type of blood clot is deep vein thrombosis (DVT). The longer the flight, the more at risk you are for developing a clot. Flights lasting 8 to 10 hours or longer pose the greatest risk.
In some cases, the DVT will dissolve and go away on its own. However, in more serious cases, it can cause pain, swelling, and warmth of the affected leg, or it can break off and travel to the blood vessels of your lungs, causing pulmonary embolism (PE).
DVT and PE, collectively known as venous thromboembolism, are highly preventable (see prevention tips below). The U.S. Surgeon General has issued a Call to Action on DVT and PE to raise public awareness of these blood conditions and increase research on the causes, prevention, and treatment.
There are several symptoms that can be warning signs of blood clots, including the following:
- Swelling of the leg, ankle, or calf
- Redness or discoloration
- Increased warmth over the skin
Am I At Risk?
Your risk of developing a blood clot during air travel is increased by the following:
- Use of oral contraceptives
- Certain cancers
- Certain recent surgeries
- Age (increased risk for people over age 60)
- History of previous blood clots
- Family history of blood clots
- Chronic inflammatory diseases
- High blood pressure
- High cholesterol
- Prior central line placement
How Can I Prevent Blood Clots When I Travel?
There are some simple steps you can take to avoid developing a blood clot while flying. Make sure to stretch your legs and get some exercise. You can do this by walking around the plane every few hours and changing positions in your seat.
If you plan on traveling soon and have concerns about getting a blood clot, talk with your doctor about your risks and prevention. Depending on your physical condition, genetics, and medical history, you may want to see a hematologist, a doctor who specializes in blood conditions.
Deep Vein Thrombosis: A Patient's Journey
Where Can I Find More Information?
If you find that you are interested in learning more about blood diseases and disorders, here are a few other resources that may be of some help:
Results of Clinical Studies Published in Blood
Search Blood , the official journal of ASH, for the results of the latest blood research. While recent articles generally require a subscriber login, patients interested in viewing an access-controlled article in Blood may obtain a copy by e-mailing a request to the Blood Publishing Office .
Patient Groups
A list of Web links to patient groups and other organizations that provide information.

- May 27, 2022
Traveling and Blood Clots
Traveling for long distances by car poses a number of challenges to individuals due to long periods of time sitting behind the wheel or being cramped in the passenger seat. What if you’re flying? Same thing – sitting in a cramped, upright position with little legroom. Both modes of travel make it difficult to get up to walk or stretch.
A few simple exercises you can do when traveling in a car, a plane, or a train can help reduce cramping, and numbness, and even prevent a blood clot from forming. It’s about awareness, planning ahead, and being proactive before you climb into that car, or board that flight, or train.
Prevent blood clots while traveling
Blood clots are formed when blood is sluggish or constricted, such as when seated in an upright position with the knees bent and the hips stuck at 90-degree angles for extended periods of time. This leads to slowing and even pooling of the blood, especially in the abdomen and lower extremities.
While most individuals travel without any complications, some travelers are at an increased risk of developing blood clots. Those with a family history of clotting issues, obesity, smoking, and immobility place a person at an increased risk for the formation of blood clots due to poor circulation, limited mobility, and strain on the heart muscle overall.
Prevention is key. If you’re concerned about a long journey ahead of you, speak with your physician about exercise, hydration, and activity that may be coordinated to your mode of transportation. For example, if you travel by bus or plane, it’s often difficult to just get up and walk around. If driving, rest stops are the only way to get out and walk and stretch.
Several exercises to promote blood flow can be done in small or tight spaces, such as an airplane or bus seat to increase comfort and decrease the potential for pooling of blood. Some examples include:
- Slide your feet under the seat in front of you (or on the car floor well) and straighten your legs as much as you can, then circle your ankles
- Pressing your toes to the floor, lift your heels, contract, release, and repeat
- Seated ‘marching in place is a good way to keep the blood moving in the lower extremities
Perform exercises like these at least once an hour, more often if possible. When driving, frequent rest stops encourage walking and stretching that improve circulation.
Before traveling, be aware of the dangers associated with blood clots. No matter what type of travel is planned, plan and prepare.
Related Posts

Blood Clot Formation: A Hidden Danger of Dog Bites
Dog bites, while often considered in terms of immediate physical trauma and infection risk, carry another, less commonly discussed danger: the potential to cause blood clot formation. This post explores the complex relationship between dog bites and blood clots, aiming to raise awareness and understanding of this serious health risk. Understanding How a Dog Bite

The Link Between Falls and Blood Clots
When we think of the aftermath of a fall, bruises and perhaps a broken bone come to mind. However, there’s another less obvious but potentially dangerous consequence: blood clots. While a fall might seem like an isolated incident, its implications can extend far beyond immediate injuries, potentially leading to the development of blood clots. Understanding

Understanding Blood Clot Risks After a Hysterectomy
Understanding Blood Clot Risks After a Hysterectomy A hysterectomy, the surgical removal of the uterus, can be a life-changing procedure for many women, offering relief from various medical conditions such as chronic pain, heavy bleeding, or cancer. However, like any major surgery, it comes with its set of post-operative risks, including the development of blood

Managing Blood Clot Concerns After Your C Section
**Managing Blood Clot Concerns After Your C Section** Bringing a new life into the world is a momentous event, and for many, a C-section is a vital part of the journey. While it’s a common and generally safe procedure, like any surgery, it comes with its set of complications and risks, including the potential for

The Risk of Blood Clots After a Car Accident
Car accidents are traumatic events that can have lasting physical effects, some of which may not be immediately apparent. Among these potential post-accident complications, the risk of developing blood clots is significant yet often overlooked. Blood clots can pose serious health risks, including the potential for life-threatening conditions such as deep vein thrombosis (DVT) and

Is It a Blood Clot or Just a Muscle Cramp? Know the Difference
Experiencing leg pain or discomfort can be concerning, especially when trying to determine if it’s a blood clot or just a muscle cramp. Both conditions share similarities in their manifestation but have distinctly different causes and risks associated with them. Understanding these differences is crucial for addressing the issue appropriately and ensuring your health and
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
Approaches to the prevention of VTE in hospitalized medical and surgical patients and patients with cancer and stroke, as well as patients who are pregnant, are presented separately. (See "Prevention of venous thromboembolic disease in acutely ill hospitalized medical adults" and "Prevention of venous thromboembolic disease in adult nonorthopedic surgical patients" and "Risk and prevention of venous thromboembolism in adults with cancer" and "Venous thromboembolism in pregnancy: Prevention" and "Prevention and treatment of venous thromboembolism in patients with acute stroke", section on 'Approach to VTE prevention' .)
EPIDEMIOLOGY
The incidence of developing clinically important or symptomatic DVT after air travel is <0.05 percent [ 9,15 ]. Although some studies reported higher rates of DVT with >4 hours (2.8 percent) or >12 hours (3.6 percent) air travel, most of these DVTs were small, involving the distal (calf) veins and, likely, clinically unimportant [ 4,11,12,16-20 ].
The estimated risk of VTE conferred by prolonged travel by air or land (eg, car, train, bus) is variable (increased approximately two- to threefold). The highest risk is reported in those who spend longer periods of time traveling. In one meta-analysis of 14 studies, the pooled risk for VTE in travelers, compared with nontravelers, was 2.8 (95% CI 2.2-3.7) [ 9 ].
- Alzheimer's & Dementia
- Asthma & Allergies
- Atopic Dermatitis
- Breast Cancer
- Cardiovascular Health
- Environment & Sustainability
- Exercise & Fitness
- Headache & Migraine
- Health Equity
- HIV & AIDS
- Human Biology
- Men's Health
- Mental Health
- Multiple Sclerosis (MS)
- Parkinson's Disease
- Psoriatic Arthritis
- Sexual Health
- Ulcerative Colitis
- Women's Health
- Nutrition & Fitness
- Vitamins & Supplements
- At-Home Testing
- Men’s Health
- Women’s Health
- Latest News
- Medical Myths
- Honest Nutrition
- Through My Eyes
- New Normal Health
- 2023 in medicine
- Why exercise is key to living a long and healthy life
- What do we know about the gut microbiome in IBD?
- My podcast changed me
- Can 'biological race' explain disparities in health?
- Why Parkinson's research is zooming in on the gut
- Health Hubs
- Find a Doctor
- BMI Calculators and Charts
- Blood Pressure Chart: Ranges and Guide
- Breast Cancer: Self-Examination Guide
- Sleep Calculator
- RA Myths vs Facts
- Type 2 Diabetes: Managing Blood Sugar
- Ankylosing Spondylitis Pain: Fact or Fiction
- Our Editorial Process
- Content Integrity
- Conscious Language
- Health Conditions
- Health Products
How long does it take for a blood clot to travel around the body?

The risk of a blood clot traveling around the body is highest within the first 4 weeks after it initially forms. However, health experts are unsure of exactly how long it takes for a blood clot to travel around the body.
The above timeframe comes from an older 2014 article from the American Heart Association’s journal, Circulation .
A blood clot happens when various substances form a solid mass inside the blood vessels. These clots can form in one part of the body before breaking off from an artery or vein. The circulatory system can then carry this blood clot to blood vessels in different parts of the body.
In some cases, this can cause serious health problems. For instance, blood clots that originate in veins can travel to the lungs, leading to pulmonary embolism (PE). Blood clots that originate in the arteries can travel to the brain, causing a stroke.
This article explores how long it takes for a blood clot to travel. It also discusses possible signs that a blood clot is traveling and describes the treatment, outlook, and prevention for blood clots and their complications.
How long does it take a blood clot to travel?

Before a blood clot can travel, it must first break loose from the blood vessel it developed in.
An older paper in Circulation states that, on average, the risk of a blood clot breaking off is highest within the first 4 weeks of formation. This is because the blood clot is at its most fragile during this time.
It is difficult to know how long blood clots take to travel around the body. This is because blood clots can remain asymptomatic for some time. Some blood clots only cause symptoms after traveling to a different body part, such as the lungs or brain.
According to a 2022 review, scientists consider a blood clot to be acute if it starts causing symptoms 2 weeks after forming.
Learn about what causes blood clots .
Signs of a blood clot traveling
A person will not feel a blood clot traveling around their circulatory system . However, they may experience the following symptoms if the clot reaches the lungs or brain.
PE symptoms
The most common symptoms of PE include:
- shortness of breath
- lightheadedness
- sharp chest pain that worsens when breathing in
- cough, which may contain blood
- excessive sweating
- blue lips or nails
Learn about the different types of pulmonary embolism .
Stroke symptoms
The symptoms of stroke include:
- facial drooping
- arm weakness
- speech difficulty
- numbness or weakness in the arm , face , or leg
- difficulty with vision
- difficulty walking
- severe headache
Learn more about how a stroke feels .
What increases the risk of a traveling blood clot?
According to a 2016 review , factors that increase the risk of a blood clot traveling through the body include:
- high blood pressure
- hormone therapy
Is it possible to prevent a blood clot from traveling?
If a person notices the signs and symptoms of a blood clot , they should contact a doctor. Treating a blood clot can help prevent the blood clot from causing complications.
A doctor will typically prescribe anticoagulant medications within 5–10 days of a diagnosis. Other treatments will depend on where the blood clot is. Options include:
- wearing compression stockings
- thrombolytic therapy (drugs that dissolve blood clots)
- surgery to remove the clot
- vena cava filter, which involves inserting a filter into the large vein in the abdomen
Learn more Learn more about managing blood clots: What to avoid with deep vein thrombosis (DVT) Treatment and home management for blood clots
Treatment for a blood clot that has traveled
The treatment for a blood clot that has traveled depends upon where the blood clot has traveled to. For instance, if a blood clot travels to the lungs, it could cause PE .
According to the Centers for Disease Control and Prevention (CDC) , the mainstay of PE treatment is thrombolytic therapy. These medications can dissolve blood clots. Doctors may also prescribe anticoagulants, which can stop further blood clots from forming.
If a blood clot travels to the brain, it could cause an ischemic stroke . According to the National Institutes of Health , doctors also prescribe thrombolytics and anticoagulants to treat ischemic strokes. They might also prescribe antiplatelet medications, which can help prevent blood clot formation.
Because strokes can cause brain damage, people who have had a stroke may require long-term rehabilitation .
Learn about recovery from a blood clot in the lungs .
Outlook if a blood clot travels
The outlook for people whose blood clot travels depends on where the blood clot ends up.
According to a 2022 review, untreated PE is fatal in around 30% of cases. With prompt treatment, that figure drops to 8%. For ischemic stroke, a 2018 study estimates that around 11.1% of people die within 30 days of the stroke.
When to contact a doctor
A person should contact a doctor if they notice any signs or symptoms of a blood clot. These include:
- swelling that typically develops in one arm or leg
- pain or tenderness around the clot
- skin discoloration
- skin that is warm to the touch
It is important that a person seeks emergency medical attention if they experience any signs and symptoms of PE or stroke.
Scientists do not know exactly how long it takes for blood clots to move around the body. However, they do know that blood clots tend to come loose within 4 weeks of forming. During this time, the clots are still fragile.
Doctors treat PE and ischemic strokes with medications that dissolve blood clots. They may also recommend medications that help prevent future clots from forming.
Last medically reviewed on June 8, 2023
- Respiratory
- Blood / Hematology
How we reviewed this article:
- Ashorobi D, et al. (2022). Thrombosis. https://www.ncbi.nlm.nih.gov/books/NBK538430/
- Blood clot treatment. (n.d.). https://www.stoptheclot.org/about-clots/blood-clot-treatment/
- Koupenova M, et al. (2017). Thrombosis and platelets: An update. https://academic.oup.com/eurheartj/article/38/11/785/2758654
- Pulmonary embolism symptoms and diagnosis. (2023). https://www.lung.org/lung-health-diseases/lung-disease-lookup/pulmonary-embolism/symptoms-diagnosis
- Sennfält S, et al . (2018). Long-term survival and function after stroke: A longitudinal observational study from the Swedish stroke register. https://www.ahajournals.org/doi/full/10.1161/STROKEAHA.118.022913
- Stroke: Signs, causes, and treatment. (2023). https://www.nia.nih.gov/health/stroke
- Vyas V, et al. (2022). Acute pulmonary embolism. https://www.ncbi.nlm.nih.gov/books/NBK560551/
- Waldron B, et al. (2014). A patient’s guide to recovery after deep vein thrombosis or pulmonary embolism. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.113.006285
- What is venous thromboembolism? (2022). https://www.cdc.gov/ncbddd/dvt/facts.html
Share this article
Latest news
- Microplastics found in food and water may spread from the gut to the brain
- Could HIV drugs help keep Alzheimer’s at bay?
- New guidelines recommend GLP-1 drugs such as Ozempic to help treat type 2 diabetes in adults
- Calorie counting as effective for weight loss as time-restricted eating, new study finds
- Mediterranean diet tied to lower hypertension risk, 20 years' worth of data show
Related Coverage
Full recovery for blood clots in the lungs varies from person to person and can take several months or years. Read on to learn about the recovery…
A blood clot in the leg can cause swelling, discolored skin, and warmth in the surrounding area. Maintaining a moderate weight and exercising…
Learn about the risk factors for deep vein thrombosis (DVT). This article also discusses preventing DVT and when to contact a doctor.
What is a mechanical thrombectomy, and what does the procedure involve? Read on to learn how this treatment can help treat stroke and the criteria to…
Renal vein thrombosis is when a clot forms in or along the renal vein. Learn more here.
- Patient Care & Health Information
- Diseases & Conditions
- Pulmonary embolism
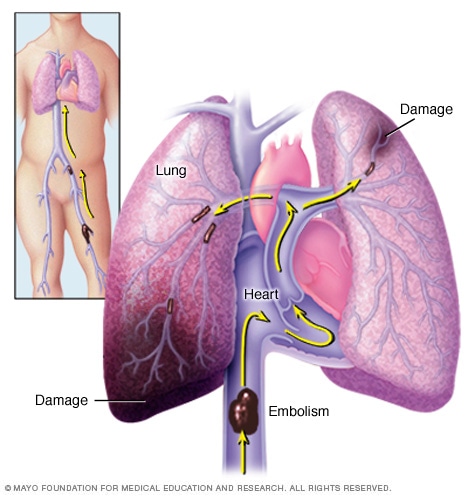
A pulmonary embolism (PE) occurs when a blood clot gets stuck in an artery in the lung, blocking blood flow to part of the lung. Blood clots most often start in the legs and travel up through the right side of the heart and into the lungs. This is called deep vein thrombosis (DVT).
A pulmonary embolism is a blood clot that blocks and stops blood flow to an artery in the lung. In most cases, the blood clot starts in a deep vein in the leg and travels to the lung. Rarely, the clot forms in a vein in another part of the body. When a blood clot forms in one or more of the deep veins in the body, it's called a deep vein thrombosis (DVT).
Because one or more clots block blood flow to the lungs, pulmonary embolism can be life-threatening. However, prompt treatment greatly reduces the risk of death. Taking measures to prevent blood clots in your legs will help protect you against pulmonary embolism.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Assortment of Compression Products at Mayo Clinic Store
- Assortment of Health Products from Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Pulmonary embolism symptoms can vary greatly, depending on how much of your lung is involved, the size of the clots, and whether you have underlying lung or heart disease.
Common symptoms include:
- Shortness of breath. This symptom usually appears suddenly. Trouble catching your breath happens even when resting and gets worse with physical activity.
- Chest pain. You may feel like you're having a heart attack. The pain is often sharp and felt when you breathe in deeply. The pain can stop you from being able to take a deep breath. You also may feel it when you cough, bend or lean over.
- Fainting. You may pass out if your heart rate or blood pressure drops suddenly. This is called syncope.
Other symptoms that can occur with pulmonary embolism include:
- A cough that may include bloody or blood-streaked mucus
- Rapid or irregular heartbeat
- Lightheadedness or dizziness
- Excessive sweating
- Leg pain or swelling, or both, usually in the back of the lower leg
- Clammy or discolored skin, called cyanosis
When to see a doctor
A pulmonary embolism can be life-threatening. Seek urgent medical attention if you experience unexplained shortness of breath, chest pain or fainting.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
A pulmonary embolism occurs when a clump of material, most often a blood clot, gets stuck in an artery in the lungs, blocking the flow of blood. Blood clots most commonly come from the deep veins of your legs, a condition known as deep vein thrombosis.
In many cases, multiple clots are involved. The portions of lung served by each blocked artery can't get blood and may die. This is known as a pulmonary infarction. This makes it more difficult for your lungs to provide oxygen to the rest of your body.
Occasionally, blockages in the blood vessels are caused by substances other than blood clots, such as:
- Fat from the inside of a broken long bone
- Part of a tumor
- Air bubbles
Risk factors
- Blood clot in leg vein
A blood clot in a leg vein may cause swelling, pain, warmth and tenderness in the affected area.
Although anyone can develop blood clots that result in a pulmonary embolism, certain factors can increase your risk.
History of blood clots
You're at a higher risk if you or any of your blood relatives, such as a parent or sibling, have had venous blood clots or a pulmonary embolism in the past.
Medical conditions and treatments
Some medical conditions and treatments put you at risk, such as:
- Heart disease. Heart and blood vessel disease, specifically heart failure, makes clot formation more likely.
- Cancer. Certain cancers — especially brain, ovary, pancreas, colon, stomach, lung and kidney cancers, and cancers that have spread — can increase the risk of blood clots. Chemotherapy further increases the risk. You also have a higher risk of blood clots if you have a personal or family history of breast cancer and are taking tamoxifen or raloxifene (Evista).
- Surgery. Surgery is one of the leading causes of problem blood clots. For this reason, medicine to prevent clots may be given before and after major surgery, such as joint replacement.
- Disorders that affect clotting. Some inherited disorders affect blood, making it more likely to clot. Other medical disorders such as kidney disease also can increase the risk of blood clots.
- Coronavirus disease 2019 (COVID-19). People who have severe symptoms of COVID-19 have an increased risk of pulmonary embolism.
Extended periods of inactivity
Blood clots are more likely to form during longer than usual periods of inactivity, such as:
- Bed rest. Being confined to bed for an extended period after surgery, a heart attack, leg fracture, trauma or any serious illness puts you at risk of blood clots. When your legs lie flat for long periods of time, the flow of blood through your veins slows down and blood can pool in your legs. This sometimes can result in blood clots.
- Long trips. Sitting in a cramped position during lengthy plane or car trips slows blood flow in the legs, which increases the risk of blood clots.
Other risk factors
- Smoking. For reasons that aren't well understood, tobacco use increases the risk of blood clots in some people, especially those who have other risk factors.
- Being overweight. Excess weight increases the risk of blood clots — particularly in people with other risk factors.
- Supplemental estrogen. The estrogen in birth control pills and in hormone replacement therapy can increase clotting factors in the blood, especially in those who smoke or are overweight.
- Pregnancy. The weight of a baby pressing on veins in the pelvis can slow blood return from the legs. Clots are more likely to form when blood slows or pools.
Complications
A pulmonary embolism can be life-threatening. About one-third of people with an undiagnosed and untreated pulmonary embolism don't survive. When the condition is diagnosed and treated promptly, however, that number drops dramatically.
Pulmonary embolisms also can lead to pulmonary hypertension, a condition in which the blood pressure in the lungs and in the right side of the heart is too high. When you have blockages in the arteries inside your lungs, your heart must work harder to push blood through those vessels. This increases blood pressure and eventually weakens your heart.
In rare cases, small clots called emboli remain in the lungs and scarring develops in the pulmonary arteries over time. This restricts blood flow and results in chronic pulmonary hypertension.
Preventing clots in the deep veins in your legs will help prevent pulmonary embolisms. For this reason, most hospitals are aggressive about taking measures to prevent blood clots, including:
- Blood thinners (anticoagulants). These medicines are often given to people at risk of clots before and after surgery. Also, they're often given to people admitted to the hospital with certain medical conditions, such as heart attack, stroke or complications of cancer.
- Compression stockings. Compression stockings steadily squeeze the legs, helping veins and leg muscles move blood more efficiently. They offer a safe, simple and inexpensive way to keep blood from pooling in the legs during and after surgery.
- Leg elevation. Elevating your legs when possible and during the night can be very effective. Raise the bottom of your bed 4 to 6 inches (10 to 15 cm) with blocks or books.
- Physical activity. Moving as soon as possible after surgery can help prevent pulmonary embolism and hasten recovery overall. This is one of the main reasons your nurse may push you to get up, even on your day of surgery, and walk despite pain at the site of your surgical incision.
- Pneumatic compression. This treatment uses thigh-high or calf-high cuffs that automatically inflate with air and deflate every few minutes. This massages and squeezes the veins in your legs and improves blood flow.
Prevention while traveling
The risk of blood clots developing while traveling is low but increases as long-haul travel increases. If you have risk factors for blood clots and you're concerned about travel, talk with your health care provider.
Your provider might suggest the following to help prevent blood clots during travel:
- Drink plenty of fluids. Water is the best liquid for preventing dehydration, which can contribute to the development of blood clots. Avoid alcohol, which contributes to fluid loss.
- Take a break from sitting. Move around the airplane cabin once an hour or so. If you're driving, stop every so often and walk around the car a couple of times. Do a few deep knee bends.
- Move in your seat. Bend and make circle movements with your ankles and raise your toes up and down every 15 to 30 minutes.
- Wear support stockings. Your provider may recommend these to help promote circulation and fluid movement in your legs. Compression stockings are available in a range of stylish colors and textures. There are even devices, called stocking butlers, to help you put on the stockings.
Living with pulmonary embolism?
Connect with others like you for support and answers to your questions in the Blood Cancers & Disorders support group on Mayo Clinic Connect, a patient community.
Blood Cancers & Disorders Discussions

43 Replies Fri, Apr 19, 2024

334 Replies Wed, Apr 17, 2024

25 Replies Wed, Apr 17, 2024
- AskMayoExpert. Pulmonary embolism (adult). Mayo Clinic; 2021.
- AskMayoExpert. Deep vein thrombosis (adult). Mayo Clinic; 2021.
- AskMayoExpert. Inferior vena cava (IVC) filters. Mayo Clinic; 2022.
- AskMayoExpert. Health considerations for air travelers: Venous thromboembolism. Mayo Clinic; 2022.
- Grillet F, et al. Acute pulmonary embolism associated with COVID-19 pneumonia detected by pulmonary CT angiography. RSNA. 2020; doi:10.1148/radiol.2020201544.
- Stevens SM, et al. Antithrombotic therapy for VTE disease: Second update of the CHEST guideline and expert panel report. Chest. 2021; doi:10.1016/jchest.2021.07.055.
- Ferri FF. Pulmonary embolism. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed Aug. 18, 2022.
- Your guide to preventing and treating blood clots. Agency for Healthcare Research and Quality. https://www.ahrq.gov/patients-consumers/prevention/disease/bloodclots.html. Accessed Aug. 18, 2022.
- Essien E-O, et al. Pulmonary embolism. Medical Clinics of North America. 2019; doi:10.1016/j.mcna.2018.12.013.
- Broaddus VC, et al., eds. Pulmonary thromboembolism: Presentation and diagnosis. In: Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed Aug. 18, 2022.
- Broaddus VC, et al., eds. Pulmonary thromboembolism: Prophylaxis and treatment. In: Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed Aug. 18, 2022.
- Froehling DA (expert opinion). Mayo Clinic. Aug. 29, 2022.
Associated Procedures
- Chest X-rays
- Extracorporeal membrane oxygenation (ECMO)
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book

Make twice the impact
Your gift can go twice as far to advance cancer research and care!

- Students & Professionals
How to Avoid Blood Clots When Flying: Advice from a Vascular Surgeon

Taking a flight or going for a drive that's longer than three hours? Then let's talk about blood clots . Why, you ask? For some travelers, blood clots can be a serious risk during long-distance trips, according to the Centers for Disease Control and Prevention . And recently, a fight broke out on a flight when a passenger with a history of blood clots allegedly couldn't get past another passenger to exit the plane after it landed, TMZ reports.
Roughly one in 1,000 people will develop a blood clot, according to the CDC . And immobility—like the kind you experience on a long trip—is a big risk factor, Thomas Maldonado , M.D., vascular surgeon and professor of surgery at NYU Langone Medical Center, tells SELF.
Here's what you need to know to protect yourself.
Blood clots are also known as deep vein thrombosis, as they typically form in the deep veins of the body that aren't visible through the skin. Most often, they form in the legs, though they can occur in any vein, Dr. Maldonado says. What makes a blood clot dangerous: the potential for it to move through the body's circulatory system.
"The situation is simple plumbing: You have arteries that bring the blood to the extremities, then you have veins return the blood back to the heart," Dr. Maldonado says. "When a clot forms in the veins, the clot can dislodge and travel back towards the heart and lodge in the lungs or heart."
If that happens, it can be dangerous—or even fatal.
While many associate blood clots with just flying, there's actually an increased risk for blood clots during any type of long-distance travel. "There’s nothing magical or special about flying at 33,000 feet that predisposes you to a blood clot," Dr. Maldonado says. "When you’re immobile for more than three or four hours at a time, you can develop a clot because blood tends to pool in the legs." People who are on prolonged bed rest also have an increased risk of blood clots.
When we’re sitting for a long period of time—and not engaging our leg muscles by stretching or walking—the mechanism that keeps blood flowing smoothly doesn’t work per usual. "Our calf muscles propel the blood back [to the heart and lungs], in addition to the natural circulation of the heart pumping," Dr. Maldonado says. "But when you’re on a long plane trip, you tend to be cooped up and immobile, and that’s a major risk factor."
He adds that people often become dehydrated on long trips, too, which is another risk factor for blood clots. When the body doesn't have enough fluids , blood vessels can narrow while blood can thicken, increasing the risk for blood clots.
"If you have a tender or painful leg , oftentimes in the calf, and it starts to swell , those are things that could make you suspect that you might have a blood clot," Dr. Maldonado says. Skin that is warm to the touch and redness of skin are also symptoms of deep vein thrombosis, according to the CDC .
By Julia Sullivan

By Alexis Berger
If you're experiencing one or more of these symptoms during a long-distance trip, Dr. Maldonado says it's not a "four-alarm fire" and a reason to rush off the plane, but the sooner you get the area checked out—typically by ultrasound—the sooner experts can diagnose a potential clot and intervene with treatment to prevent fatal complications. People with blood clots typically have to take blood thinners for three to six months to prevent their clot from growing and prevent new clots from forming. Sometimes, "clotbusting" medication is also needed to break up a clot.
While pain and swelling in the leg are, of course, uncomfortable symptoms, Dr. Maldonado says the clot traveling is still the most concerning issue. "That’s really what you want to avoid," he says. "And there’s not a good way to predict which clot will travel, but when you have a blood clot in the leg, you can develop a pulmonary embolism, and about a quarter of those people will die."
A pulmonary embolism occurs when a blood vessel in the lungs is blocked by a clot. "The pulmonary embolism symptoms are very traumatic," Dr. Maldonado says, and they include chest pain, shortness of breath, and difficulty breathing. If you're experiencing these symptoms, he says to seek help immediately. Pulmonary embolisms are also treated with clot dissolvers and blood thinners. But if the clot is very large and life-threatening, surgery might be necessary.
"The real key to blood clots is to understand your risks," Dr. Maldonado says. Risk factors include a family history of blood clots, pregnancy , taking birth control , smoking, being overweight or obese, having inflammatory bowel disease , and being over age 60, according to the Mayo Clinic .
If you have a series of risk factors—and you're going to be immobile for a long period of time—it's important to take steps to prevent a clot.
Prevention is simple: On a long-distance trip, try and stretch your legs and walk every few hours. If you're on a long flight, take advantage of those "the captain has turned off the seatbelt sign" moments and take to the aisle to get your leg muscles working. If you can't get up, try to at least move your lower legs—without kicking the seat in front of you, of course. The Mayo Clinic suggests raising and lowering your heels while keeping your toes on the floor, then doing the opposite by lifting and lowering your toes while keeping your heels still.
Dr. Maldonado adds that if you have a series of blood clot risk factors, you should stay away from dehydrating drinks like alcohol and caffeinated beverages while traveling and make sure to drink enough water . Compression socks are also helpful to wear when traveling, as they can help keep circulation moving.
Bottom line: You can prevent blood clots from forming, and you should know your risks and take the necessary precautions when traveling.
- Flying in Your Third Trimester Can Be Risky, Even if Airlines Allow It
- How to Survive a Long International Flight
- 6 Pro Travel Tips That Will Make Your 2017 Adventures a Breeze
Watch: 5 Weird Signs You're Dehydrated
SELF does not provide medical advice, diagnosis, or treatment. Any information published on this website or by this brand is not intended as a substitute for medical advice, and you should not take any action before consulting with a healthcare professional.

Your browser is out-of-date!
Internet Explorer 11 has been retired by Microsoft as of June 15, 2022. To get the best experience on this website, we recommend using a modern browser, such as Safari, Chrome or Edge.
How to Prevent Blood Clots During Long Travel
Reduce risk of deep vein thrombosis (dvt) while traveling.

Long-distance travel – whether by plane or car – usually does not cause health problems, but for some people it puts them at risk of developing deep vein thrombosis (DVT), a type of blood clot that can lead to complications.
DVT occurs when a blood clot forms in the deep veins of the body, usually in the leg, pelvis or arm. They can form during long travel and prolonged sitting in a confined space. Long periods of immobility can cause blood to pool in the legs, disrupting normal flow through the veins.
“Fortunately, you can do several things to reduce your risk of blood clots during long trips, such as moving your legs frequently or taking a break to stretch your legs,” says Ankur Chandra, MD , a vascular surgeon at Scripps Clinic Torrey Pines . “Activities like this help to improve the flow of blood in your legs.”
Understanding the signs and risks of DVT is important as well as when to seek care to prevent problems.
Is DVT a serious illness?
DVT can turn serious if a blood clot in the veins breaks off and travels to the lungs causing a blockage. This is known as a pulmonary embolism (PE) and can be life-threatening.
Symptoms of PE include:
- Shortness of breath
- Coughing up blood
- Faster than normal or irregular heartbeat
- Very low blood pressure
- Lightheadedness or fainting.
“If you have any of these symptoms, seek medical help immediately,” Dr. Chandra says.
Estimates suggest that 60,000-100,000 Americans die of DVT/PE (also called venous thromboembolism), according to the CDC.
Who’s at risk of DVT?
About half of the people with DVT have no symptoms at all, but there are several risk factors.
Anyone traveling more than four hours whether by air, car, bus or train can be at risk for blood clots, according to the Centers for Disease Control and Prevention (CDC). The risk is generally very small, but if someone has other risk factors, including:
- Recent surgery or injury
- Slow blood flow due to limited movement, sitting for long time or bed confinement
- Increased estrogen, often caused by birth control pills, hormone replacement therapy or pregnancy
- Heart disease, lung disease, cancer and its treatment or inflammatory bowel disease
- Older age, risk increases after age 40
- Previous blood clot or a family history of blood clots
- Catheter placed in a large vein
How is DVT diagnosed?
DVT often goes unnoticed because symptoms can be very mild. Blood clots typically occur only in one leg.
Symptoms include:
- Unusual warmth
- Redness or changes in skin color
“If you notice any of these symptoms, seek medical attention. Your doctor will examine your legs and may order an ultrasound test to evaluate blood flow through the veins and check for any blockage or obstruction,” Dr. Chandra says.
Because veins normally do not show up in an X-ray, occasionally a contrast material is injected into the vein to make it visible, and the images are taken as the material flows through the vein.
Treatments for DVT/PE
Medication is used to prevent and treat DVT. Anticoagulants, also known as blood thinners, are most commonly used to treat DVT or PE. In severe cases, the clot might need to be surgically removed.
“Early treatment for DVT is usually very effective,” Dr. Chandra says. “However, people who have one episode of DVT have a higher risk of recurrence.”
Wearing compression stockings may be recommended to help reduce the risk of DVT or treat symptoms. These special stockings put pressure on leg muscles and help blood flow from the legs back to the heart.
Immediate medical attention is needed to treat PE, which can also be treated with medication.
Reduce risk of blood clots
Talk with your doctor if you think you may be at risk for blood clots.
Reduce the risk of blood clots during travel by:
- Knowing signs and symptoms of blood clots
- Move your legs frequently during long trips
- Exercise your calf muscles to improve flow of blood
- Extend your legs straight out and flex your ankles
- Wear compression stockings
Related tags:
- Health and Wellness
- Wellness & Prevention
- Heart & Vascular

Blood Clot Busters: 6 Tips to Prevent VTE During Holiday Travel
While most forms of travel won’t raise your blood clot risk by much, it may still be a good idea to take some precautions.
Holiday travel can bring joy and connection, as well as hassles and stress. You may be particularly worried about traveling if you’re at a higher risk for venous thromboembolism (VTE), or blood clots that form in your veins.
Sitting for extended periods of time increases the risk for VTE, which can take the form of deep vein thrombosis (DVT), a clot that typically forms in the deep veins of the legs, potentially causing painful symptoms in the area. A clot may also travel to your lungs and restrict or cut off blood flow, known as pulmonary embolism (PE) — a potentially life-threatening emergency.
While it’s important to take the risk for blood clots seriously if you have underlying risk factors, most people can travel without any undue risk for VTE, according to David Garcia, MD , a professor of hematology at the University of Washington School of Medicine in Seattle. “The absolute risk of a blood clot due to air travel is going to be small for just about everyone,” he says, noting that air travel appears to carry a higher risk for VTE than other forms of transportation.
The overall risk for symptomatic DVT linked to air travel appears to be less than 1 percent, Dr. Garcia says, based on reviews of many studies on the subject. But one analysis found that the overall incidence of DVT from long-haul flights — whether or not there were symptoms — may be as high as 3 to 12 percent.
You may be at a higher risk for VTE if any of the following situations or conditions apply to you, according to the Centers for Disease Control and Prevention (CDC) :
- Personal or family history of blood clots
- Recent hospitalization, surgery, or injury
- Current or recent pregnancy
- Taking oral birth control pills or estrogen-based hormone replacement therapy
- Cancer or undergoing chemotherapy
- Congestive heart failure
- Inflammatory bowel disease
While there’s no way to absolutely avoid blood clots while traveling, some simple steps may reduce your risk for VTE during and immediately after travel — and maybe just as importantly, give you peace of mind. Here’s what you can do to take worrying about blood clots off your itinerary.
1. Stay Hydrated
When you’re dehydrated, your blood vessels narrow and your blood thickens, increasing your risk for blood clots, according to the American Heart Association . Staying hydrated can be a particular challenge when traveling, since you may not have easy access to water or other beverages at all times. That’s why it’s important to plan ahead — such as by filling up an empty water bottle once you get through security at the airport or stocking bottled water for a long car trip.
It’s also important to avoid beverages that can lead to dehydration when you travel. That means not drinking more than a small amount of alcohol, according to Garcia, and also not drinking large amounts of soda.
2. Break Up Your Travel
Since sitting for longer periods increases the risk for VTE, it stands to reason that shorter trips pose less of a risk, Garcia says. This is particularly true when it comes to air travel — the only form of travel that has been definitely linked to a higher risk for blood clots, according to Garcia.
“People who travel on flights of more than four to five hours have a slight increase in the risk of blood clots,” says Garcia. “Fortunately, the dangers they pose are usually not going to result in catastrophe within the span of two to six hours.”
If you experience symptoms of a blood clot while traveling, it’s important to seek medical care as soon as possible — another reason why shorter trips may be appealing to some people. “Don’t check into your hotel,” says Garcia, if you experience possible symptoms of VTE. “Don’t delay. Go get care right away after landing.”
3. Get Up and Move
Just because you’re on a plane — or train, bus, or boat — for an extended period doesn’t mean you need to stay glued to your seat. When possible, the CDC recommends standing up and, if space permits, walking around occasionally, ideally at least every two to three hours. If you’re traveling by car, plan to take breaks for stretching and walking around.
Garcia says that other forms of transportation may not pose the same level of risk for VTE as air travel because some of the risk linked to air travel could be due to lower oxygen levels in airplane cabins. Still, the potential benefits of movement apply to any form of travel that involves extended sitting.
4. Do Leg Exercises in Your Seat
If you can’t get up and move for some reason — or if you want even more movement — you can move your legs around while you’re in your seat. The CDC suggests the following seated exercises to reduce your blood clot risk:
- Raise and lower your heels, keeping your toes on the floor.
- Raise and lower your toes, keeping your heels on the floor.
- Tighten and release your leg muscles (certain areas or your whole leg).
Stretching out your legs in front of you is also a good idea, Garcia says, but this may not be possible in many travel situations.
5. Wear Compression Stockings
Properly fitted compression stockings are likely to reduce the risk for blood clots while traveling, says Garcia — in fact, this was the conclusion of a research review for which he provided commentary. Garcia compares compression stockings to the life vest found underneath your seat on a plane — unlikely to make a difference on any given flight but providing reassurance to many people.
6. Take Medications as Prescribed
It goes without saying that when you travel, you shouldn’t let it disrupt taking any regular medications — especially anticoagulants (blood thinners), taken to reduce your risk for blood clots, or less powerful clot-preventing antiplatelet drugs like aspirin. But for people who aren’t taking aspirin regularly on their doctor’s advice, taking it when you travel to prevent clots is not recommended, according to the CDC.
If you take a blood thinner, you should feel safe traveling, says Garcia. “Something I get asked a lot is: Do I still have to be concerned about blood clots if I’m taking a blood thinner? And the answer is absolutely not,” he says. “Whatever risk air travel might add is going to be washed out completely by the drug’s effects.” That doesn’t mean your risk for blood clots is zero, but it does mean you shouldn’t be unduly worried about this risk, especially if you take other precautions to prevent blood clots when you travel.
Schedule an Appointment
1-800-910-vein 1-800-910-8346.
- About Dr. Jimenez
- Our Philosophy
- Patient Experience
- Endovenous Laser Treatment (EVLT™) for Varicose Veins
- Cosmetic Sclerotherapy for Spider Veins
- Ultrasound-Guided Foam Sclerotherapy for Varicose Veins
- Ambulatory Phlebectomy for Varicose Veins
- Sclerotherapy for Varicose Veins
- Compression Therapy to Relieve Vein Symptoms
- Spider Veins
- Varicose Veins
- Venous Ulcers
- Patient Testimonials
- Before & After Gallery
- Destin Location
- Foley Location
- Pensacola Location
- Free Vein Screenings

Blood Clots and Travel: What You Need to Know
December 31, 2019

Traveling for long periods can wreak havoc on the body’s circulatory system. Whether you’re traveling by plane, car or bus, lengthy trips and prolonged periods of inactivity can lead to the formation of blood clots, particularly for those at risk of developing deep vein thrombosis (DVT). In some cases, this condition can cause painful physical symptoms that affect your comfort and overall health. At the Vein Center of Florida & South Baldwin, we are dedicated to helping patients restore and protect their vascular health. We encourage all those who travel for long periods to understand the risk factors of venous disease, how to prevent issues from developing, and how to secure your long-term vein health.
What is Deep Vein Thrombosis (DVT)?
Deep vein thrombosis occurs when a blood clot forms in the deep veins of the body, which are not visible through the skin. This condition most commonly develops in the legs due to extended periods of inactivity, such as long-distance trips. When the body is seated, the blood circulates more slowly, and gravity works against the veins as they attempt to send blood back up the legs. This process can gradually cause the blood to collect and pool in the vein, triggering the body’s clotting response.
In some cases, blood clots can dissolve on their own. However, in more severe cases, deep vein thrombosis can lead to painful symptoms and further medical complications if left untreated. If part of the blood clot detaches and travels to the lungs, it can cause a blockage, also known as a pulmonary embolism, which may be fatal. Understanding the risk factors, symptoms and preventative techniques can help prepare you for long-distance trips and ensure you remain in good vascular health during and after your journey.
Symptoms of DVT
Some patients who develop DVT experience no physical symptoms. However, the most common issues associated with blood clots include:
- Swelling in the foot, ankle or leg
- Cramping, throbbing or unexplained pain in the legs
- Enlarged veins
- The skin over the affected vein feels warmer than surrounding skin
- The skin over the affected area turns pale, reddish or bluish
If you experience any of these symptoms, seek medical assistance immediately. Dr. James Jimenez at the Vein Center of Florida & South Baldwin can examine your condition and overall health to ensure the problem is identified and managed effectively. He will work with you to select the most suitable vein treatment and suggest preventative techniques to help protect your long-term vascular health.
Risk Factors for Developing DVT
Various factors can increase your risk of developing deep vein thrombosis. Though this condition can occur at any stage of your life, the risk increases considerably after the age of 40. Beyond age, the most common risk factors include:
- Reduced mobility or inactivity (e.g., bed rest, flights or drives)
- Birth control pills or hormone replacement therapy
- Personal history or family history of blood clots
- Vein damage due to injury or trauma
- Serious medical issues, such as heart disease or cancer
How To Prevent Blood Clots While Traveling
Exercise and movement.
In confined situations, it can be difficult to move around while traveling on a plane or in a car. However, there are some simple exercises and movements that can help to boost circulation in the legs and thereby prevent the blood from collecting and clotting. These movements include:
- Standing up and stretching your legs whenever possible – On a flight, this means walking up and down the aisle every hour. In a car, this requires taking regular rest stops to walk around and stretch your legs.
- Recline your seat whenever possible
- When seated, lower the balls of your feet to the floor to help increase blood flow in the legs
- Keep your leg area clear of bags and other items to ensure you can stretch out regularly
- Bend and straighten the feet, toes and legs every half hour
Compression Stockings
Compression stockings help to promote blood circulation during extended periods of standing or sitting. They work by gently squeezing the limb and encouraging the vein and leg muscles to move blood more efficiently. Compression stockings can also help to prevent swelling and alleviate discomfort in the legs. If you have a moderate to high risk of developing DVT, wearing compression garments during long flights or drives can help to prevent blood clots from forming.
At the Vein Centers of Florida & South Baldwin, Dr. Jimenez offers graduated, prescription-strength compression hose for patients suffering from venous disease and associated symptoms. Compression therapy provides a simple and convenient way to ease discomfort, such as aching or heaviness in the legs, and boost circulation during long-distance trips and periods of inactivity.
Precautionary Measures
Healthy blood circulation is crucial for helping to reduce the risk of DVT. Avoiding alcohol and staying hydrated before and during travel can help to ensure the blood flows as smoothly and efficiently as possible. Avoiding sleeping pills is also advised as these are designed to slow down the body’s systems. Upon arrival at your destination, walking and moving around will help to restore normal circulation in the legs.
Schedule a Consultation at the Vein Center of Florida & South Baldwin
Taking preventive measures is crucial for protecting your vascular health while traveling. However, if you suspect symptoms of DVT or are concerned about your risk factors for developing venous issues, consulting a vein specialist is the most reliable and effective way to ensure you avoid further health complications.
As one of the leading vein experts along the Emerald Coast, Dr. James Jimenez is a highly recognized vein doctor with extensive experience managing all kinds of venous concerns and conditions. A pioneer in minimally invasive procedures, Dr. Jimenez has helped countless men and women achieve better vascular health with minimal side effects and little to no downtime. If you are concerned about your vein health or are preparing for a long trip, contact the Vein Center of Florida & South Baldwin at 1-800-910-8346 to schedule your consultation today . We can help to ensure a worry-free and relaxed journey.
6 In-Flight Exercises to Help Prevent Blood Clots, According to Experts

Whether you're planning a getaway, taking frequent business trips or visiting family for the holidays, traveling — especially over long distances — can put considerable pressure on your body.
Advertisement
In fact, long-distance flights that are generally more than four hours can put some travelers at serious risk for developing deep vein thrombosis (DVT), commonly known as blood clots, Ron Drainer, PT , physical therapist and therapy supervisor at SSM Rehabilitation Health Network, tells LIVESTRONG.com.
Video of the Day
And the longer the flight, the higher the risk of developing a clot. According to the American Society of Hematology, flights lasting 8 to 10 hours or longer pose the greatest risk.
"Traveling for long durations can definitely cause blood clots, and not just in planes, but also car or train rides," Drainer says. "While sitting for a long period, your circulation slows down, which contributes to the formation of blood clots."
If you experience any swelling greater than 3 centimeters in one lower limb compared to the other, generalized swelling of one leg, localized tenderness or pitting edema (swelling where an indentation is preserved when pressure is applied and then removed), seek immediate medication attention.
It doesn't help that most airplanes have limited leg room, cramped and confined seating space and less-than-ideal back support. These traveling conditions can have other negative effects on your body, too, according to Carina Sobel, PT, DPT, a physical therapist at International Multiple Sclerosis Management Practice.
During prolonged periods of sitting, certain muscle groups, such as the hip flexors and hamstrings, remain in a shortened position, resulting in muscle tightness, Sobel says.
"When we contract our muscles, they act like pumps that help to circulate blood and move it against gravity in order to return to the heart," Sobel explains. "However, if we are sitting still and not contracting our muscles very much, that pump system becomes a less effective and blood may begin to pool."
These health effects, including the development of blood clots, "can happen to anyone," Drainer says. But the good news is that there are several exercises and stretches you can incorporate into your in-flight routine to help prevent them.
Risk Factors for In-Flight Blood Clots
Air pressure changes during a plane flight, which, according to Sobel, can affect how much oxygen is getting into your bloodstream. When there is decreased oxygenation of blood in the body, it can trigger coagulation or the formation of a blood clot.
"Each vessel in the vascular system can be compared to a hose," Sobel says. "If a person is sitting for a long period of time, kinks may form in the hose or vessel, and this makes it easier for a clot, or thrombus, to form."
Several other factors could put someone at a higher risk of developing a travel-related blood clot, Sobel says. These are some of them, according to the CDC :
- Active cancer or recent cancer treatment
- Bedridden for more than three days
- Surgery or injury within the last three months
- Previously had a blood clot
- Heart failure and hypertension
- Pregnant or have recently given birth
- Take an oral contraceptive
- Undergoing hormone replacement therapy
Additional contributing factors that can increase your risk for blood clots include age (especially if you're over 65), obesity, smoking, dehydration or a family history of blood clots, Drainer says.
6 Exercises to Try
The ideal exercise to help prevent blood clots is standing up and walking, Sobel says. But space is a limiting factor, especially when traveling on a plane — sometimes it's not possible to get to the aisle.
Luckily, several beneficial movements can be done from your plane seat and the aisle, if that's an option on your flight.
All of these exercises and stretches increase the circulation of your lower extremities (including the ankles, calf, hamstrings and quads) and minimize the risk of blood clots, Drainer says.
"Each exercise should be repeated every 1 to 3 hours depending on a person's likelihood of developing a DVT," Sobel says. That means if you have one of the risk factors described above, try to do these every hour while traveling.
1. Seated Ankle Pumps
Ankle pumps are a great exercise to promote blood flow and circulation by activating the muscles in the lower leg and decreasing the risk of blood clot formation, Drainer explains. This muscle contraction helps to pump blood from the legs back up to the heart.
- Sit with your back against your seat and your feet flat on the floor. Ensure that your knees are bent at a 90-degree angle and your upper body is in an upright position.
- Lift your heels off the ground while keeping your toes in contact with the floor.
- Lower your heels back to the floor while raising your toes toward the ceiling.
- Repeat 20 times.
2. Seated Marches
This gentle exercise can help improve blood circulation throughout the cardiovascular system by contracting your leg muscles, Sobel says.
- Sit up tall so that you are not leaning against the back of your seat. Aim to sit on the edge of your chair, if space allows.
- Keep both of your feet flat on the floor with your knees bent at a 90-degree angle.
- Lift one knee about 2 to 3 inches while keeping your other foot in contact with the floor, mimicking the movement of marching. (Engage your core so that your lower back isn't curling or flexing.)
- Slowly lower the lifted knee back to the floor in its original position.
- Repeat the same motion with the other leg.
- Do this 10 to 20 times each leg.
3. Piriformis Stretch
The piriformis muscle runs from your lower spine through your butt to the top of your thighs. It can get aggravated by sitting for long periods of time, and when this muscle gets inflamed or tight, it can compress the sciatic nerve, which runs underneath it. Stretching can help prevent the piriformis from becoming tight, Sobel says.
While this stretch does not directly prevent blood clots, it can contribute to overall leg health and comfort, especially during extended periods of sitting from air travel. It can also relieve muscle tension within the glutes.
- Sit at the edge of your seat with both of your feet flat on the floor. Ensure your back is straight.
- Cross your right knee over your left knee so that your right ankle is near your left knee and pointed out to the side.
- Using your right hand, gently give yourself some pressure downward at your right knee.
- If you need more of a stretch, gently lean forward until you feel a stretch behind your right hip.
- Hold for 30 seconds.
- Return your right leg to its original position and repeat with your left leg.
4. Heel Raises
Heel raises are the optimal exercise to promote blood flow by contracting your gastrocnemius, which is the biggest muscle in your calf, Sobel says. You should complete this exercise only if you can stand from your chair or in the aisle.
- Stand in an upright position on a flat surface. Use the side or back of a seat to provide more stability and support.
- Position your feet about hip-width distance apart with your toes pointing forward.
- Raise both heels off the ground as high as is comfortable. You should essentially be standing on the balls of your feet.
- Pause at the top of the movement where your heels are lifted as high as possible.
- Slowly lower your heels back to the starting position.
5. Hip Flexor and Calf Stretch
When we're seated, the hip flexors are in a shortened position, making it easier for them to become tight. This stretch is a beneficial exercise for improving hip flexibility and will help lengthen the muscle, Sobel says. Do this stretch within a range that is comfortable and pain-free.
- Stand with your feet hip-width distance apart.
- Get into a shortened lunge position with your left leg forward.
- Think of elongating the front of the right hip by pushing your hips forward and keeping your trunk upright. You should begin to feel a stretch along the front of your right hip.
- Sneak in a gastrocnemius stretch by pushing your right heel into the ground, which you should feel in your right calf muscle, in addition to your hip.
- Release and switch legs. Repeat on the other side.
6. Seated Hamstring Stretch
This stretch promotes circulation and improves flexibility of the hamstring muscles, which can also become tight with long-duration sitting, Drainer says. When your hamstrings become stiff they can contribute to low back stiffness and pain.
- Sit with your hips at the edge of your seat. Fully extend one leg out in front of you, with your heel on the floor and your toes pointed up.
- Keep your chest up and your spine long and slowly lean forward, bending at the hips. You should feel the stretch in the back of your thigh.
- Hold the stretch for 20 to 30 seconds.
- Slowly return to an upright position and switch sides. Repeat 2 to 4 times on each side.
Other Ways to Prevent Blood Clots During Air Travel
In addition to the exercises and stretches above, experts say there are other things travelers can do in flight to reduce their risk of blood clots.
Stay Well-Hydrated
Dehydration can increase the risk of blood clots, so drinking plenty of water before and during your flight is important to prevent vasoconstriction, or the narrowing of blood vessels, Sobel says.
Travelers should also avoid drinking coffee and alcohol, as these liquids can cause vasoconstriction. "Water and other liquids will promote vasodilation and effective circulation of blood throughout the vascular system," Sobel says.
Wear Compression Stockings
Sobel says another thing that travelers can do to prevent blood clots is to wear compression stockings during a flight. Compression stockings can help improve blood flow in your legs since they provide gentle pressure to prevent blood from pooling.
Elevate Your Legs
If possible, try to keep your feet and legs elevated. Take advantage of open seats next to you or place a small bag or cushion under the seat in front of you and your feet on top. This can help reduce swelling, promote better blood circulation and lower the pressure in your legs, according to the National Blood Clot Alliance .
Walk Around
In general, moving, walking or standing can be challenging to do on a plane, especially when there is turbulence and limited space. However, if the flight allows, get up and walk around the cabin every couple of hours to help improve circulation. Consider selecting an aisle seat which can make it easier to get up and move around.
Avoid Taking Aspirin
According to the CDC, it is not recommended to take an aspirin to prevent blood clots when traveling. If you currently take aspirin or plan to take aspirin for other reasons, check with your healthcare provider first.
"Blood clots are a very rare but serious condition. Travelers should take the above exercises and advice to help prevent a DVT from forming," Sobel says.
- American Society of Hematology: Clots and Travel.
- Centers for Disease Control and Prevention. Blood Clots and Travel.
- National Blood Clot Alliance. In-Flight Fitness.
- North American Thrombosis Forum. Patients Are Asking: does Flying Increase My Risk for a Clot.
- Centers for Disease Control and Prevention. Prevent Blood Clots.
Report an Issue
Screenshot loading...
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
Pregnant Travelers

Pregnant travelers can generally travel safely with appropriate preparation. But they should avoid some destinations, including those with risk of Zika and malaria. Learn more about traveling during pregnancy and steps you can take to keep you and your baby healthy.
Before Travel
Before you book a cruise or air travel, check the airlines or cruise operator policies for pregnant women. Some airlines will let you fly until 36 weeks, but others may have an earlier cutoff. Cruises may not allow you to travel after 24–28 weeks of pregnancy, and you may need to have a note from your doctor stating you are fit to travel.
Zika and Malaria
Zika can cause severe birth defects. The Zika virus is spread through mosquito bites and sex. If you are pregnant, do not travel to areas with risk of Zika . If you must travel to an area with Zika, use insect repellent and take other steps to avoid bug bites. If you have a sex partner who lives in or has traveled to an area with Zika, you should use condoms for the rest of your pregnancy.
Pregnant travelers should avoid travel to areas with malaria, as it can be more severe in pregnant women. Malaria increases the risk for serious pregnancy problems, including premature birth, miscarriage, and stillbirth. If you must travel to an area with malaria, talk to your doctor about taking malaria prevention medicine. Malaria is spread by mosquitoes, so use insect repellent and take other steps to avoid bug bites.
Make an appointment with your healthcare provider or a travel health specialist that takes place at least one month before you leave. They can help you get destination-specific vaccines, medicines, and information. Discussing your health concerns, itinerary, and planned activities with your provider allows them to give more specific advice and recommendations.
Plan for the unexpected. It is important to plan for unexpected events as much as possible. Doing so can help you get quality health care or avoid being stranded at a destination. A few steps you can take to plan for unexpected events are to get travel insurance , learn where to get health care during travel , pack a travel health kit , and enroll in the Department of State’s STEP .
Be sure your healthcare policy covers pregnancy and neonatal complications while overseas. If it doesn’t get travel health insurance that covers those items. Consider getting medical evacuation insurance too.
Recognize signs and symptoms that require immediate medical attention, including pelvic or abdominal pain, bleeding, contractions, symptoms of preeclampsia (unusual swelling, severe headaches, nausea and vomiting, and vision changes), and dehydration.
Prepare a travel health kit . Pregnant travelers may want to include in your kit prescription medications, hemorrhoid cream, antiemetic drugs, antacids, prenatal vitamins, medication for vaginitis or yeast infection, and support hose, in addition to the items recommended for all travelers.
During Travel
Your feet may become swollen on a long flight, so wear comfortable shoes and loose clothing and try to walk around every hour or so. Sitting for a long time, like on long flight, increases your chances of getting blood clots, or deep vein thrombosis. Pregnant women are also more likely to get blood clots. To reduce your risk of a blood clot, your doctor may recommend compression stockings or leg exercises you can do in your seat. Also, see CDC’s Blood Clots During Travel page for more tips on how to avoid blood clots during travel.
Choose safe food and drink. Contaminated food or drinks can cause travelers’ diarrhea and other diseases and disrupt your travel. Travelers to low or middle income destinations are especially at risk. Generally, foods served hot are usually safe to eat as well as dry and packaged foods. Bottled, canned, and hot drinks are usually safe to drink. Learn more about how to choose safer food and drinks to prevent getting sick.
Pregnant women should not use bismuth subsalicylate, which is in Pepto-Bismol and Kaopectate. Travelers to low or middle income destinations are more likely to get sick from food or drinks. Iodine tablets for water purification should not be used since they can harm thyroid development of the fetus.
After Travel

If you traveled and feel sick, particularly if you have a fever, talk to a healthcare provider immediately, and tell them about your travel. Avoid contact with other people while you are sick.
More Information
CDC Yellow Book: Pregnant Travelers
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

IMAGES
VIDEO
COMMENTS
Blood Clots and Travel: What You Should Know. This podcast is designed to help people reduce their risk of blood clots during long-distance travel of four hours or more. Listen now. Blood clots can form in the deep veins (veins below the surface that are not visible through the skin) of your legs during travel because you are sitting still in a ...
Clots and Travel. Blood clots can sometimes form in your legs during air travel because you are immobile for long periods of time, often sitting in cramped spaces with little leg room. The clinical term for this type of blood clot is deep vein thrombosis (DVT). The longer the flight, the more at risk you are for developing a clot.
Blood clots are formed when blood is sluggish or constricted, such as when seated in an upright position with the knees bent and the hips stuck at 90-degree angles for extended periods of time. This leads to slowing and even pooling of the blood, especially in the abdomen and lower extremities. While most individuals travel without any ...
The incidence of developing clinically important or symptomatic DVT after air travel is <0.05 percent . Although some studies reported higher rates of DVT with >4 hours (2.8 percent) or >12 hours (3.6 percent) air travel, most of these DVTs were small, involving the distal (calf) veins and, likely, clinically unimportant [4,11,12,16-20].
Summary. The risk of a blood clot traveling around the body is highest within the first 4 weeks after it initially forms. However, health experts are unsure of exactly how long it takes for a ...
Prevention while traveling. The risk of blood clots developing while traveling is low but increases as long-haul travel increases. If you have risk factors for blood clots and you're concerned about travel, talk with your health care provider. Your provider might suggest the following to help prevent blood clots during travel: Drink plenty of ...
[Cindy Sayers] For most people, the risk of developing a blood clot—even during long-distance travel— is very small. However, your risk . increases. if you have other risk factors for blood clots, such as older age, obesity, surgery within three months of travel, or a family history of blood clots. Women who've
Immobility— that is, lack of movement—can result in slow, sluggish, or nonexistent blood flow, which increases a person's risk of a blood clot. Therefore, the most important measure to prevent blood clots during travel is to move around for at least five minutes every two hours. Even when passengers are confined to their seats in a plane ...
Doing exercises and staying hydrated are really the best tools we have on long flights.". If you've had DVTs in the past or are at high risk of recurrent blood clots, Dr. Bajakian recommends you talk to your doctor before taking a flight longer than 4 to 6 hours. In some extremely high-risk cases, she may prescribe a course of low-dose ...
Preventing Travel-Related Blood Clots: A "Passport to Safety". As holidays or vacation time approaches, it is never too early to think about protecting yourself from the risk of blood clots when you travel for more than four hours - whether it is by plane, train, car or bus. The National Blood Clot Alliance has published a one page ...
Long-distance travel is a risk factor for blood clots because it involves sitting for prolonged periods of time. ... For some travelers, blood clots can be a serious risk during long-distance ...
Air Health is a non-profit organization dedicated solely to the topic of travel-associated thrombosis, reports that 3-5% of air travelers will develop clots. Despite continued research, case reports, and a physiological basis for increased risk, not all experts agree that air travel is a direct cause of thrombosis due to a lack of large-scale ...
Airplane travel, especially flights longer than 4 hours, may increase your risk for blood clots, including deep vein thrombosis and pulmonary embolism. ... Lean how to prevent blood clots during travel. After Travel. If you traveled and feel sick, particularly if you have a fever, talk to a healthcare provider and tell them about your travel ...
Talk with your doctor if you think you may be at risk for blood clots. Reduce the risk of blood clots during travel by: Knowing signs and symptoms of blood clots. Move your legs frequently during long trips. Exercise your calf muscles to improve flow of blood. Extend your legs straight out and flex your ankles.
As the holiday season approaches, many of you will begin making travel plans to reunite with your loved ones or have a long overdue escape. Your to-do list can be extensive and stressful. Being an antiphospholipid syndrome (APS) patient and having an elevated risk of blood clots - particularly during long-haul travel - can add even more stress.
Raise and lower your toes, keeping your heels on the floor. Tighten and release your leg muscles (certain areas or your whole leg). Stretching out your legs in front of you is also a good idea ...
Learn more about how to prevent blood clots while traveling for long hours, especially for those at risk of developing deep vein thrombosis (DVT). Schedule an Appointment 1-800-910-VEIN ... Avoiding alcohol and staying hydrated before and during travel can help to ensure the blood flows as smoothly and efficiently as possible. Avoiding sleeping ...
That means if you have one of the risk factors described above, try to do these every hour while traveling. 1. Seated Ankle Pumps. Ankle pumps are a great exercise to promote blood flow and circulation by activating the muscles in the lower leg and decreasing the risk of blood clot formation, Drainer explains.
Embolisms are blood clots that break free and travel to other parts of your body. Less common, thankfully, are arterial clots. These occur when a blood clot clogs an artery.
During Travel. Your feet may become swollen on a long flight, so wear comfortable shoes and loose clothing and try to walk around every hour or so. Sitting for a long time, like on long flight, increases your chances of getting blood clots, or deep vein thrombosis. Pregnant women are also more likely to get blood clots.